The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.


The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.

On April 18, 2023, student nurses from across Illinois met for the 255h Annual Student Nurse Political Action Day (SNPAD). The event was held at the Bank of Springfield Convention Center in Springfield, Illinois.
This year, SNPAD brought together nearly 600 nursing students from 24 nursing schools for a day of learning, networking, and advocacy. The day’s events and conversations had a lasting impact on nursing students.
“The perspectives of leaders in the field of nursing at the Student Nurse Political Action Day inspired and empowered me and my peers. I personally felt educated on the current issues that nurses face and what it takes to make a difference in the dynamic field of health care. Student Nurse Political Action Day is an exceptionally educational and enlightening experience for any nursing student,” says Jonas Arvin Cosejo Sales, a Northern Illinois University nursing student who will graduate in 2024.
Many Nursing Schools Represented
Of the 24 schools represented, Illinois Wesleyan University had the most students attending! Thank you, Illinois Wesleyan University, for your strong commitment to political action and empowerment! See the full list below.
Generous Sponsors
The event is again supported by a generous gift donated in 2013 by the former Chicago Nurses Association. Sponsorship support also comes from the Illinois Public Health Association. Thank you to these sponsors for helping us make this important event possible!
STOP THE BLEED® Training
We appreciate Loyola University Medical Center’s willingness to provide STOP THE BLEED® Hands on Skills training to students and faculty in attendance. Hands on skills classes took place in the morning. Nearly 100 students participated in the workshop!
The day-long conference featured a keynote address by ANA-Illinois Executive Director Susan Swart, EdD, MS, RN, CAE, called “Human First, Nurse Second – Navigating the Chaos.” Her inspiring and empowering keynote gave practical advice for how new nurses can advocate for themselves and practice self-care in a health care environment.
Later, Debbie Broadfield and Kristen Rubbelke discussed “Hot Topics: What’s Happening in the 103rd General Assembly.” Both Kristen and Debbie work for Capitol Edge Consulting whose president is Sue Clark, a long-respected healthcare lobbyist who is often referred by legislators and staff as the “Voice of Nursing” under the dome. We were honored to have you share with us!
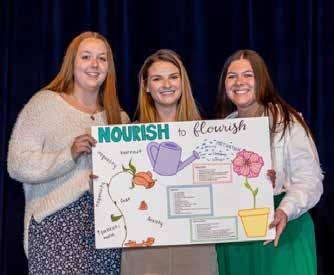
2023 Prize Winners
SNPAD included lots of opportunities to win money and prizes through both contests and drawings. Additionally, the poster contest winners will have their posters featured in the June issue of the statewide publication The Nursing Voice. Look for posters from Emily Brewer, Jenna Cheek, and Ellaire Barrett of Millikin University, who won $100 for their winning poster. Kayla Watts, also of Millikin University, won $50 for second place.
• Daisy Whitaker from Millikin University won the photo contest.
• Lydia Lansaw, Illinois College, won a $500 scholarship.
• Alexis Wright, Lewis & Clark Community College, won the $100 student giveaway drawing.
• Queen Kisoso, Olivet Nazarene, won the $100 faculty giveaway drawing.
Illinois Nursing Workforce Center, Chamberlain University, Herzing University, Purdue, Illinois State University, and ANA-Illinois had items that were won in drawings that ranged from Starbucks gift cards to books to backpacks.

Congratulations to all who won, and a big thank you to all who participated! Our warm appreciation to all who made the gifts possible.
After door prizes and winners were announced, student nurses and faculty marched to the Capitol to raise their voices and participate in political action.
“We walked shoulder to shoulder alongside, understanding that our collective voice can make a meaningful difference in the classroom, the workforce, and in the lives of others,” says Jonas Arvin Cosejo Sales.
The rally was the perfect ending to a powerful day.
“SNPAD was a great experience where we not only heard about the bills that will be impacting our career, but how to advocate for ourselves and maybe even fight for our legislation in the future. The day was filled with great speakers, and the march to the Capitol was the cherry on top!” says Faith Sidener, a University of IllinoisChicago nursing student graduating in May 2023.
THANK YOU
We are so grateful to all the student nurses and faculty who attended to learn how they can be engaged in the legislative process and in advocacy work to improve their lives and the lives of their patients. We know that in so many ways, the skills and lessons students learned at SNPAD are just the beginning of a lifetime of essential political action. Your involvement is so important, and we’re so thankful for all of you and all that you do!

INF Board of Directors

Cheryl Anema PhD, RN
I have to start my message by sharing how proud I am to be a part of the IL Nurses Foundation (INF). I started my professional service with the IL Nurses Association (INA) as a Delegate in 1983 for District 1. Back then the INA was the ANA affiliated state association. Over time I moved to the suburbs and became part of District 20, continuing in my service as a delegate, Director of the Board, and President. It was during that time that INA decided it was time to form a Foundation, and the IL Nurses Foundation was born. As you see, the ANA-IL (former INA) leadership began the Foundation so that nurses and supporters of nursing had a place to give back, a 501C3 organization.
I joined the INF Board as a Director representing the ANA-IL. When my term was up, I asked to stay on the Foundation Board. This led to stepping in as the President of the INF, a role I have loved. I have watched the ANA-IL and the INF continue to grow. IL is recognizing these professional organizations and the role they play in the advancement of nursing and healthcare in IL.
As president, I have watched the continued growth in the INF Committees, 40 Under 40 Program, INF Holiday Gala & Fundraiser, The Nursing Voice (the official publication of the INF), Nurses Week – Honor a Nurse,
Nurse of the Year Award, nursing grant program, and nursing student scholarships. A couple years ago the INF published its first book – Stories from Within: Nurses, Patients, Doctors, and Families Share Their Pandemic Experience – which is still offered on Amazon.com with all profits going to the Foundation. The State of IL released the first nursing license plate where people can purchase the plate directly from IL with $20 going to the INF. The INF is a sound Foundation and continues to grow and offer leadership, CEs, mentoring, and recognition of nursing professionals.
At this time, I have notified the INF Board of Directors that I will be stepping down as President of the INF this summer 2023. I will be available to transition to a new President who will lead the INF into the future. I look forward to see where the Foundation goes in the next years, but am confident that it will continue to grow and be recognized as the leading nursing philanthropic organization in IL.
I hope all of you will continue to support the INF through service and monies, as both are needed for the Foundation's success and growth. Look to the Nursing Voice for new opportunities of service, as well as a call for articles, creative impressions, and committee service. Thank you for the opportunity to serve the IL Community of Nurses and Nurse Supporters.

Araceli Orozco, BSN, RN-BC, IL PEL-SN, NCSN Lisell Zuniga, BSN, RN, PEL-CSN
Nurses have been working in schools since 1902 when Nurse Lina Rogers was assigned to work in New York schools (Selekman et al., 2019). School nurses care for diverse groups of students with chronic health problems such as diabetes, seizures, and asthma, provide medication education, health promotion, and follow infection control procedures. School nurses are also sought after in the school community since they are usually the only health experts on the premises.
School nurses come from a variety of nursing backgrounds and experience, but obtaining the Certified School Nurse (CSN) designation is a step further in the specialty of school nursing. The CSN designation helps advance the nurse’s expertise in the educational setting and interlocks nursing knowledge into one entity. The CSN designation not only highlights one’s nursing skills and expertise, but dedication to the practice. The CSN makes evidence-based decisions in Special Education (i.e., Individual Education Plan [IEP]) meetings and is part of a multidisciplinary team that works together to develop interventions for the least restrictive environment (LRE; Heward et al., 2017) in the school setting. These
● Illinois licensed nursing programs: RN, LPN
● Telemedicine nursing

● Traveling nurses and traveling nurse agencies Illinois’ largest, most trusted live scan fingerprint vendor serving Illinois agencies for over 20 years.
● Convenient walk-in locations – statewide
● Simple path for out-of-state print processing for nursing
● On-site mobile fingerprinting for large groups
AccurateBiometrics.com Toll free bilingual support: 866-361-9944
info@accuratebiometrics.com
interventions and accommodations allow students to receive a free appropriate public education (FAPE; Heward et al., 2017).
Chronic absenteeism was a concern prior to the Covid-19 pandemic, and has continued not only due to illness, but also due to mental health challenges. Postpandemic, school nurses have experienced a significant rise in their daily student census, including increased behavior, mental, and physical issues. Therefore, access to a nurse during school hours help improve student health outcomes and attendance rates due to preventive care and early identification of illness or infection. In addition, collaboration with school administrators, counselors, social workers, and so on is vital for running a successful school nursing practice.
School nurses practice with a holistic view using the “Whole School, Whole Community, Whole Child (WSCC)” model (ANA & NASN, 2022) and do their best utilizing available resources to provide safe, quality care to students. Similar to other areas of nursing, there is a shortage of nurses and decreased resources in schools. Regardless of the many challenges school nurses face, the practice of school nursing has its rewards, i.e., great hours, vacations, and memorable community connections. We are part of a community of school nurses who help students maintain optimal health for successful school outcomes (ANA & NASN, 2017). We would not change this for anything!
Araceli Orozco is a District Nurse in the West Chicago School District 33, and Lisell Zuniga is a Health Services Administrator in the Valley View School District 365.
References
American Nurses Association & National Association of School Nurses. (2022). School nursing: Scope and standards of practice (4th ed. , 1-40). https://www.nasn.org/nasnresources/resources-by-topic/scope-standards
Heward, W. L., Alber-Morgan, S. R., & Kondrad, M. (2017). Exceptional children: An introduction to special education (11th ed.) Pearson Education, Inc. Wolfe, L. C. (2019). Historical perspectives of school nursing. In J. Selekman, R. A. Shannon, & C. F. Yonkaitis (Eds.), School Nursing: A Comprehensive Text, (3rd ed., pp. 2-16). F. A. Davis.
Officers
Cheryl Anema, PhD, RN
Brandon Hauer, MSN, RN
Karen Egenes, EdD, RN
Directors
Maureen Shekleton, PhD, RN, DPNAP, FAAN
Linda Olson, PhD, RN, NEA-BC
Amanda Oliver, BSN, RN, CCRN
ANA-Illinois Board
Rep
Susana Gonzalez, MHA, MSN, RN, CNML
Jeannine Haberman DNP, MBA, RN, CNE
Zeh Wellington, DNP, MSN, RN, NE-BC

ANA-Illinois Board of Directors
Officers
Elizabeth Aquino, PhD, RN
Monique Reed, PhD, MS, RN
Jeannine Haberman, DNP MBA, RN, CNE
Beth Phelps, DNP, APRN, FNP, ACNP
Directors
Samuel Davis Jr MHA, RN, CNOR
Susana Gonzalez, MHA, MSN, RN, CNML
Elaine Hardy, PhD, RN
Hannah Shufeldt MSHCM, BSN, RN Zeh Wellington, DNP, MSN, RN, NE-BC
Editorial Committee
Chief Editor
Lisa Anderson-Shaw, DrPH, MA, MSN
Members
Cheryl Anema PhD, RN
Deborah S. Adelman, PhD, RN, NE-BC
Linda Anders, MBA, MSN, RN
Ellen Bollino MSN, RN, ED, CEN
Nancy Brent, RN, MS, JD
Pamela DiVito-Thomas PhD, RN
Amanda Hannan MSN, RN
Irene McCarron, MSN, RN, NPD-BC
Linda Olson, PhD, RN, NEA-BC
Lanette Stuckey, PhD, MSN, RN, CNE, CMSRN, CNEcl, NEA-BC
Executive Director
Susan Y. Swart, EdD, MS, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
Article Submission
• Subject to editing by the INF Executive Director & Editorial Committee
• Electronic submissions ONLY as an attachment (word document preferred)
• Email: syswart@ana-illinois.org
• Subject Line: Nursing Voice Submission: Name of the article
• Must include the name of the author and a title.
• INF reserves the right to pull or edit any article / news submission for space and availability and/or deadlines
• If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted.
• INF does not accept monetary payment for articles.
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: syswart@ ana-illinois.org
Article Submission Dates (submissions by end of the business day) January 1st, April 1st, July 1st, October 1st
Advertising: for advertising rates and information please contact Health eCareers, HEC_Nursing_Info@healthecareers.com ANA-Illinois and Health eCareers reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.
Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. ANA-Illinois and Health eCareers shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations.
Dear Illinois Nurse Colleagues,

The Annual Nurses Day at the Capitol took place in Springfield, Illinois on March 7, 2023 and was attended by nurses from all around the state of Illinois. Registered nurses and advanced practice registered nurses attended to learn what is happening in Springfield and how to use their voice to make a difference.
The session provided attendees with the talking points necessary to educate their Senator and Representative on key issues of concern for nurses. Attendees heard from state health leaders, received education on advocacy, and found out how to connect with representatives and senators from their area. The event was successful in empowering and amplifying nursing's voices across the state.

Liz Aquino, PhD, RN
Thank you for joining us for Nurses Day at the Capital and/or Student Nurse Political Action Day in Springfield. Both events offer an opportunity to go to our state capital to stay informed and participate in advocacy efforts that impact the nursing profession. We had a very active legislative session with several workforce-related bills and by this message, we should know what bills were passed. We appreciate you for staying actively involved in our grassroots advocacy efforts to help inform legislators about the important impact their decisions have on our profession and healthcare. I would also like to congratulate the participants of the inaugural cohort of the Nurses Running for Elected Office Training Academy for completing the program and we look forward to the change they will create when elected to office someday soon! Stay tuned for the open application announcement to join the next cohort.
To learn more about events and opportunities to get involved—check out our website (ana-illinois.org) or social media platforms (FB, Instagram, LinkedIn, and Twitter). Don’t forget to tag us so that we can help promote the great work you are doing both professionally and personally!
Sincerely,

Elizabeth (Liz) Aquino, PhD, RN
President, ANA-Illinois
@LatinaPhDRN








NANCY J. BRENT, MS, JD, RN
Nursing roles in assistive living facilities are varied. They include conducting health examinations, communicating with family members, assisting with ADLs, and medication management.

Nancy J. Brent, MS, JD, RN
In the Illinois Assisted Living and Shared Housing Act, such a facility is defined as a “home, building, residence, or any other place where sleeping accommodations are provided for at least 3 unrelated adults, at least 88% of whom are 55 years of age or older” where specific requirements must be met. Requirements include a social model that is based on the premise that the resident’s unit is his or her home, mandatory services are provided (e.g., 3 meals/day, housekeeping), and a physical environment that is “homelike” (e.g, individual living units with small kitchen appliances and private bathing, washing and toilet facilities) are present.
Assisted living facilities (AFLs) in Illinois are highly regulated, especially in regard to medication management and nursing’s role in that management.
Prior to an admission to an assisted living establishment, each potential resident must complete an assessment by a physician and a written service plan established.
If the assessment indicates the need for medication management for a resident, the RNs, LPNs and/or APRNs working in the facility must adhere to the Act’s regulations governing medications.
The regulations indicate that an assisted living facility may provide:
• medication reminders
• supervision of self-administered medication
• medication administration as an optional service
Each medication option has specific requirements in the regulations.
Medication Reminders Requirements
Reminders include prompting residents to take predispensed, self-administered medications, observing the resident, and documenting whether the resident took the medication or not. If medication is stored by the resident in his or her unit, it shall be stored as described in the resident’s service plan and shall be inaccessible to other residents.


Supervision of Self-Administered Medication
This regulation is defined as assisting the resident in:
• Reminding residents to take medication
• Confirming that residents have obtained and are taking the dosage as prescribed
• Reading the medication label to residents
• Checking the self-administered medication dosage against the medication label
• Opening the medication container if resident is physically unable to do so
• Documenting in writing that the resident has taken (or refused to take) the medication
If supervision of self-administered medication is done by unlicensed personnel, it must be done under the direction of a licensed health care provider (RN, APRN, PA, or LPN).
A drug-reference guide, no later than 2 years from its copyright date, must be available and accessible for use by employees.
Medication Administration
This responsibility requires a licensed health care professional employed by the facility to administer routine insulin and vitamin B-12 injections, oral medications, topical treatments, eye and ear drops, or nitroglycerin patches. Non-licensed staff may not administer any medications.
A drug-reference guide, no later than 2 years from its copyright date, must be available and accessible for use by employees.
Medication Policies and Procedures Requirement
If a facility does provide medication administration or supervision of self-administered medication, medication policies and procedures must be approved by a physician, pharmacist, or RN and shall include instructions on:
• Obtaining and refilling medication
• Storing and controlling medication
• Disposing of medication
• Assisting in the self-administration of medication and medication administration, as applicable, and
• Recording of medication assistance provided to residents and maintenance of medication records.
Storage of Medications
Any medication stored by the assisted living facility must:
• Be stored in a locked container, cabinet, or area that is inaccessible to residents
• Not left unattended by an employee

• Be stored in its original labeled container, except for medication organizers, and according to instructions on the medication label
• Not be stored in a bathroom or laundry room
• Expired, discontinued, and those medications of deceased residents must be disposed of according to the facility’s medication policies and procedures
No medications shall be pre-poured except for those in medication organizers. Medication organizers may be prepared up to one month in advance by a resident or the representative, a resident’s relative, a nurse, or as otherwise provided by law.
A separate medication record must be maintained for each resident receiving medication administration and must include:
• The name of the resident
• The name of the medication, dosage, directions, and route of administration
• The date and time medication is to be administered
• The date and time of the actual medication administration
• The signature or initials of the licensed health care provider administering the medication.
Discussion
For those of you who are not working in ALFs but might be contemplating a move to one or helping a family member or friend with such a decision, the Act and its medication administration requirements are specifications to evaluate. Ask questions of nursing staff and administration concerning the requirements that fit your or your family members’ needs so that you know they are in place and being adhered to.
If your workplace is in an ALF, be certain to comply with the above regulations, both from a professional negligence and a professional licensure perspective. If your workplace does not include these requirements, you need to initiate necessary changes to include them.
If you are considering a role in assisted living facilities, these medication requirements will govern your practice in this nursing specialty.
There are also implications for your nursing practice, whether already working within a facility or contemplating a nursing role within an ALF.
One is to be involved in the design and layout of the stored medication room in the facility for administered medications. Advocating for storage of the medications at eye level height, a well-lit room, large enough space to avoid overcrowding of those medications stored, and features to minimize noise, interruptions and distractions are a few examples to consider.
Providing input into the documentation forms for medication administration is important so that the forms protect both you and the patient. Forms can be developed by you and the facility or purchased on-line, if they correspond to Illinois and facility requirements for medication documentation.
A third implication is to ensure that as RN or APRN, you are delegating medication responsibilities consistent with the Illinois Nurse Practice Act and its rules and regulations. Remember that delegation of medications can occur only after a comprehensive assessment of the patient/resident.
Another implication is to become an active member of the American Assisted Living Nurses Association. Keeping current of practice issues in this nursing specialty is not only a legal requirement, it is an ethical one as well.
You can read the entire Act at: https://www.ilga.gov/legislation.ilcs/ilcs3. asap?AcTID=1217&ChapterID=21
The Medication requirements can be accessed at; https://www.law.cornell.edu/regulation/illinois/Illadmin-code-tit-77-SS-295.5000
The Illinois Nurse Practice Act and its Rules can be accessed at: https://nursing.illinois.gov/
References Upon Request
This information is for educational purposes only and is not to be taken as specific legal or any other advice by the reader. If legal or other advice is needed, the reader is encouraged to seek such advice from a nurse attorney, attorney or other professional.
2023 List of Colleges Participating
Thank you to the 24 colleges and universities who included the political engagement of their nursing students in their nursing education:
• Bradley University
• Carl Sandburg College
• Graham Hospital
• Harper College
• Illinois Eastern Community College
• Illinois College
• Illinois Wesleyan University
• Joliet Junior College
• Lewis & Clark Community College
• Lewis University
• Loyola University Chicago, Marcella Niehoff School of Nursing
• Malcolm X – City College of Chicago
• Methodist College – UnityPoint Health
• Millikin University
• Northern Illinois University – School of Nursing
• Northern Kentucky University
• Purdue University – Northwest
• Olivet Nazarene University
• South Suburban College
• Southern Illinois University of Edwardsville
• St. John's College of Nursing
• UIC College of Nursing – Springfield Campus
• UIC College of Nursing
• Western Illinois University
2023 Exhibitors
Many thanks to the following 18 exhibitors for their generous support of SNPAD and student nurses!
• Blessing Rieman College of Nursing & Health Sciences
• Chamberlain University
• Emergency Nurses Association
• Herzing University
• Hospital Sisters Health System
• HSHS St. John’s College of Nursing
• IDFPR/Nursing Workforce Center
• Illinois College
• Illinois Public Health Association
• Lewis University
• Mennonite College of Nursing – Springfield
• Northern Illinois University School of Nursing
• Purdue University College of Nursing
• Student Nurses Association of Illinois
• University of Illinois Chicago – College of Nursing
• University of Michigan School of Nursing
• University of St. Francis
• Western Governors University













Gloria E. Barrera MSN, RN, PEL-CSN
Advocacy with the Illinois Association of School Nurses (IASN) during the pandemic, where did we start? Before I discuss, I want to briefly share my first experience with advocacy work on the hill. In 2014 I was flown to DC to speak to lawmakers about the health impact from methane emissions organized by the Alliance of Nurses for Healthy Environments (ANHE), what was clear to me then as it is now, is that we, school nurses, are the experts when it comes to public health issues that impact the communities we serve.
Fast forward to 2021, I was in my second year serving as President of IASN. The National Association of School Nurses (NASN) reached out to me in May to share that we were one of the state affiliates that were being selected to receive additional support and consulting from the Preston Group as it relates to advocacy efforts. Over the course of that summer and leading into fall, the IASN Board and the Preston Group met to discuss our issues, as we saw them, and to plan our next steps. That summer was busy to say the least, as many of us were holding our breath for what was to come for the 2021-2022 school year in regards to mitigating the impact of COVID-19. We made our advocacy efforts a priority, and we moved forward with them with our membership and our mission at the center of our decision. Our goals spoke to the lack of understanding and acknowledgment among a range of stakeholders about the critical role that school nurses play in schools throughout Illinois. To achieve the goals identified, Preston Group recommended that we undertake a multi-pronged education campaign designed to inform and influence stakeholders. They outlined our state’s top three priorities of addressing education shortages, including support personnel, digital equity for students and comprehensive student supports with regard to social-emotional learning and mental health. Both priority one and three were extremely relevant for school nurses. The Preston Group also recommended that we cultivate an inventory of legislative champions, as it would be critical to our success. Finding a legislative sponsor to advocate for an appropriation of ESSER funds, or other funding, for a study of school nursing capacity in Illinois was the first step. Such a project would require a relatively one-time modest investment of $250,000 and provide IASN with the objective data that we needed for our advocacy efforts going forward. We had a plan.
On October 15, 2021 I made the executive decision to reach out to the staff lobbyist for ANA-Illinois. I had worked with them in the past as an individual member of ANA-Illinois attending Nurse Day at the Capitol in Springfield. I knew that we needed their expertise, and I knew that our membership deserved this investment to get results. The Board unanimously approved IASN to enter into a contract with Capitol Edge Consulting on October 26, 2021. We were ready to get to work!
The consulting/lobbying agreement between the Illinois Association of School Nurses and Capitol Edge Consulting LLC went into effect as of January 1, 2022 for a period of 5 months, ending on May 31, 2022. Our work with Capitol Edge Consulting, LLC took off. Our goal was

clear: to establish with IASN strategies needed to achieve having a certified/licensed school nurse in every school district to supervise the health services programs. We identified outcomes regarding appropriation of ESSER funds, or another funding source, for a study of school nurse capacity in Illinois, including the potential of a legislative proposal. Familiarizing IASN to members of the Illinois General Assembly was another goal.
We kept our membership engaged and up to date with our agreement and partnership with Capitol Edge Consulting every step of the way. We shared the news via our Town Hall Meetings, an innovative idea created to share resources and education virtually under my leadership, and through our Newsblasts.
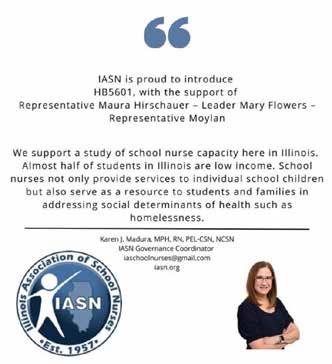
Once the new year came and legislators were in session, HB5601 was created. On January 31, 2022 House Bill 5601 was referred to the Rules Committee. House Bill 5601 called to appropriate $250,000 from the SBE Federal Department of Education Fund to the State Board of Education to complete a study for school nursing capacity in Illinois. Capitol Edge found our School Nurse Champion, Representative Maura Hirshauer from the 49th District, to introduce our Bill.
We began our Social Media Campaign on February 8th. Reaching out to legislators via Twitter proved most effective. The social media campaign flyers that I created included information from the bill, calling on legislators to support us. We held a Legislative Town Hall Meeting on March 24, 2022 with Capitol Edge Consulting to briefly train our members on advocacy and effective strategies to contact their legislators. A call to action alert, and sign on letter was sent to all 850+ members of IASN, with a Fact Sheet for talking points when making calls to individual legislators.
In total, with our grassroots social media push, and Capitol Edge working for us in Springfield we had 20 House Sponsors for our bill. IASN took advantage of every opportunity to speak about HB5601. IASN was present at Nurses Day at the Capitol, virtually, with ANA-Illinois to discuss our bill with our nurse colleagues across the state. IASN leadership, including myself, Bridgett Heroff and Cam Traut presented at the ANA-Illinois Nurse Staffing Summit on March 12, 2022 to discuss nurse workforce issues, solutions, challenges and best practices including school nursing during the pandemic and beyond.
The key to our success was keeping our membership engaged and informed.
I testified on March 29, 2022 at a subject matter hearing in Springfield on the nursing shortage and its impact on the specialty of school nursing. I made it clear that the data collected from the school nurse capacity study would help drive action for our work in optimizing student health, and learning for the future.
An excerpt from my testimony is below:
As a nurse, I use the nursing process, and the first step is always assessment.
We are the health care experts in schools, often the only healthcare provider a student may encounter. We demonstrated just how essential our role was as we mitigated the impact of COVID-19 these past three school years. But even before the pandemic,

we have been on the frontlines of bridging health care and education, providing care coordination, and advocating for quality student-centered care.
IASN’s goal is to have a Certified School Nurse in every school. First, we need to quantify how many school nurses are working in our schools.
What Illinois must have is the data, we have to conduct an assessment on the state of school nursing: Who is working where, how many schools is each nurse responsible for, and where is the most need? We have asked ISBE to help us gather such data with no effect to date. Therefore, IASN is seeking a monetary appropriation of $250,000 to conduct an Illinois School Nurse Capacity study; the appropriation is being requested through the SBE Federal Department of Education Fund to the State Board of Education for a grant or a contract with the Illinois Association of School Nurses to complete a study for school nursing capacity in this State. We thank and appreciate Representative Hirschauer for introducing HB5601 to bring awareness to this critical issue. I ask you to support funding for our request for money as the FIRST step in finding a solution to the school nurses shortage.
The first week of April, in conversation with Representative Hirschauer and ISBE, we learned that the requested ESSER funds were not available to be allocated for HB5601. This was confirmed on April 9, 2022, after many hours of negotiation and debate, when legislators passed the FY23 budget. Our team quickly shifted gears and House Resolution 817 was drafted. The House Resolution urged ISBE to work with IASN to complete a study to gather more in-depth data that can be utilized to develop a model for healthcare services provided in schools that can address specific community needs. The resolution urged ISBE to report the findings to the Illinois General Assembly by January 10, 2023. This resolution was introduced April 5 and passed on the last scheduled day of session, April 8. Both, IEA and IFT supported it. These gains could not have been met without the work of our members. On October 6, 2022 I testified on behalf of IASN at the Illinois State board of Education’s virtual Fiscal Year 2024 Budget Hearing. I noted that it had been 6 months since the resolution passed and we were ready. I requested the original $250,000 to be allocated for FY2024. Exactly two days later, on October 7, 2022 we were contacted by an Executive Director from ISBE to follow up on the school nurse study. On October 21, 2022 we were notified by ISBE that they were able to allocate $350,000 ESSER funds to fully support IASN in completing the study.
I shared my vision and goal to have an Inaugural Annual School Nurses Day at the Capitol in Spring, 2023 last summer, and I’m happy to report that it is set for May 3, 2023 under President Bridget Heroff's leadership! Our work with Capitol Edge continues and I have no doubt that we will continue to raise awareness and make positive changes to our profession here in Illinois. I am excited to see other IASN affiliates, and other nursing organizations follow our lead, because it starts with us. We are the experts, nursing is political, and our voices are powerful!
Linda L. Olson, PhD, RN, NEA-BC, FAAN
Lisa Anderson-Shaw, DrPH, MA, MSN
Theme:
There are approximately 65,000 residents in nursing homes and assisted living facilities in Illinois, with over 1,000,000 in the USA as a whole. The ethical principles of beneficence (doing good), non-maleficence (avoiding harm), autonomy (rights to informed decision-making), and justice (fairness) apply to nursing practice in long-term care and assisted living facilities. In addition, the provisions of the ANA Code of Ethics for Nurses with Interpretive Statements (2015) provide guidance for nurses and nursing practice.
Provision 1.1 of the ANA Code of Ethics focuses on respect for human dignity (2015. P. 1), and Provision 2 states that “the nurse’s primary commitment is to the patient, whether an individual, family, group, community or population (2015, p. 5). Provision 3 of the Code of Ethics states that “the nurse promotes, advocates for, and protects the rights, health, and safety of the patient,” with 3.1 focused on protection of the rights of privacy and confidentiality (2015, p. 9). Another resource is ANA’s Position Statement on “Nurses’ Professional Responsibility to Promote Ethical Practice Environments” (Stokes, 2023).

Lisa Anderson Shaw DrPH, MA, MSN

Linda Olson PhD, RN, NEA-BC
Many ethical challenges in caring for the residents in nursing homes and other long-term care facilities are reported in the literature and in research. These include the everyday ethical challenges, such as a lack of resources (staffing, time, equipment) as well as the more difficult ethical dilemmas associated with end-of-life care issues and decisions. Employees who responded to a questionnaire about ethical challenges in nursing homes identified the top three challenges as lack of resources, end-oflife issues, and coercion (Bollig, et.al., 2015). Conflicts in values are associated with missed care, moral distress, and turnover of both nurses and other nursing staff (Munkeby, et.al., 2021). On an encouraging side, there are many long-lasting and close relationships between nurses and their patients and families in long-term care.
Another vulnerable population that creates ethical challenges is in areas in which access to care is often compromised, such as in rural areas. Health care access and services can be challenging for many people no matter where they live. In the United States, the majority of states have large rural populations. (See map picture) Barriers to health care include insurance status, transportation to healthcare services, mobility and illness status.
A snapshot of Illinois includes estimated urban/metro population at 12,716,164 and a rural population of 1,434,356. (Miller, 2022)) To qualify as an urban area, the territory identified according to criteria must encompass at least 2,000 housing units or have a population of at least 5,000. (A shortage of nurses has been developing in Illinois for many years and officials say things could get worse. Due to the COVID-19 crisis, many Illinois nurses decided to retire or leave the profession all together. The outcome of this led to a shortage of nurses in Illinois, especially in the small and rural areas of downstate Illinois. (Bessler, 2022)
This shortage of nurses in Illinois has a large impact on the number of nurses in Illinois now and in the near future. Based on the 2020 RN workforce report prepared by the Illinois Nursing Workforce Center, “Illinois will face a shortage of nearly 15,000 RNs by 2025. Plus, while 52% of the almost 195,000 RNs in Illinois are over the age of 55— with 27% planning to retire in the next 5 years—less than 8,000 nurses graduate each year.” (Swart, 2022)
The practice of nursing in rural areas can be very satisfying. Rural health nurses practice community health and are very important in bridging access to care for those living in communities with small populations and are geographically isolated. Rural nurses are needed in these areas and are often seen as leaders and change agents in the communities they serve. Challenges of being a community nurse in rural and small areas can include isolation and lack of economic and professional support. Rural nurses often have higher demands for their services in small communities. Such communities typically depend on 1-2 community health nurses to address and meet all of the individual health needs of the community. (Leeper 2011). Working in a rural environment where nurses are part of the community can be an advantage, as people will often trust those nurses’ health advice. The ethical issues with working in rural areas as a health care provider often center on confidentiality and trust, which is included in ANA Code Provision 3 that states “the nurse promotes, advocates for, and protects the rights, health, and safety of the patient” (2015, p. 9).
To deal with ethical challenges in long-term care and assisted living facilities, it is important to have ongoing ethics education, with time for discussion and reflection, to engage residents and their families in participation in decision-making about their loved ones as well as about facility policies and procedures, and to encourage open communication among nursing staff, physicians, and administrators. When nurses feel free to express their views, as well as their differences in opinion about treatment and care of the residents without fear of retaliation, a more positive ethical climate and healthy work environment is created. We could take some lessons from the Scandinavian countries, which are considered as providing exceptional care for older people that focuses on the community as a whole (Suhonnen et.al., 2015).
References American Nurses Association (2015). ANA Code of Ethics with Interpretive Statements. Nursesbooks.org
Bessler, K. (2022, Sept. 22) The Center for Square Illinois, News Partner. https://patch.com/ illinois/chicago/illinois-grappling-nurse-shortage-officials-say-it-will-get-worse Bollig, G., Schmidt, G., Rosland, J. H., & Heller, A. (2015). Ethical challenges in nursing homesstaff’s opinions and experiences with systematic ethics meetings with participation of residents’ relatives. Scandinavian Journal of Caring Sciences, 29, 810-823.
Leeper, J. (2011, March 20) Clinical Advisor. https://www.clinicaladvisor.com/home/yourcareer/weighing-the-pros-and-cons-of-rural-nursing/#:~:text=%E2%80%9CThe%20rural%20 nurse%20is%20a,all%20of%20their%20health%20needs
Miller, V. (2022, Dec.29). Census redefines rural and urban. Chicago Sun Times. https://chicago. suntimes.com/2022/12/29/23531600/census-redefines-rural-and-urban Munkeby, H., Moe, A., Bratberg, G., & Devik, S. A. (2021). ‘Ethics Between the Lines’-Nurses’ experiences of ethical challenges in long-term care. Global Qualitative Nursing Research, 8, 1-11.
Stokes, L. (2021). ANA position statement: Nurses’ professional responsibility to promote ethical practice environments. Online Journal of Issues in Nursing (OJIN) https://ojin.nursingworld. org/table-of-contents/volume-28-2023/number-1-january-2023/responsibility-to-promoteethical-practice-environments/
Suhonnen, S., Stolt, M., Katajisto, J. Charalambous, A., & Olson, L. (2015). Validation of the Hospital Ethical Climate Survey for older people care. Nursing Ethics, 22(5), 517-532. Swart, S. (2022, April 4). ANA Illinois. ANA-Illinois calls for action on nursing shortage at Illinois Senate Health Committee Meeting. https://www.ana-illinois.org/news/ana-illinois-calls-foraction-on-nursing-shortage-at-illinois-senate-health-committee-meeting. 2023, March 29.

https://dph.illinois.gov/content/dam/soi/en/web/idph/files/publications/128-16-ohp-hiv-factsheet-rural-communities.pdf accessed 4.15.23

“Nurses Delivering Care and Supporting Our Community”
Written by: Jackie Smith, RN, and Carolyn Rimmer-Owens, RN
Email: jackielsmith93@gmil.com / owenscarolyn1312@gmail.com
The 35th Annual National Black Nurses Day was celebrated on Friday, February 24, 2023, at Apostolic Faith Church, where Horace E. Smith, MD, is the Bishop. The National Black Nurses Day Planning Committee is a coalition of professional nurses comprised of the Chicago Chapter National Black Nurses Association, Alpha Eta Chapter of Chi Eta Phi Sorority, Inc, and Beta Mu Chapter of Lambda Pi Alpha Sorority.

The newly appointed chair of NBNDPC, Marilynn Parker, MSN, MSED, RN, APRN, FNP, also served as the Mistress of Ceremony.
The National Black Nurses Day Planning Committee has remained faithful in celebrating NBND as proclaimed by the Honorable Charles B. Rangel and the House of Representatives in 1989.

Geneva Gore, RN, led the audience in singing the Black National Anthem.



“Lift Every Voice and Sing,” written by James Weldon Johnson and J. Rosamond Johnson in 1900. She also sang a heartfelt rendition. Of “Take My Hand, Precious Lord” which was written by Rev. Thomas A. Dorsey in 1932.

Dixon-Taylor, RN, delivered the Invocation.

Shenetta Wilson of the Apostolic Health Ministry gave the welcome address and thanked the committee for continuing to honor African American men and women in nursing.




Carolyn Rimmer- Owens, RN, and Shannon King, RN, performed the Libation Ceremony in memory of the life and legacy of nurses who have made their transition within the last year; Joann Dean, RN, accepted the flower for Ms . Helen McCorkle, RN (CCNBNA), Monique Gill, RN (Lambda Pi Alpha), Ida Keith, RN ( CCNBNA/Chi Eta Phi), Carolyn Roberts ( Lambda Pi Alpha), and Dr. Shirley Howard, RN ( CCNBNA), were all recognized during this ceremony.





Top Row: Latonya Cannon, RN, President of Lambda Pi Alpha Sorority. Ethel Walton, RN, President of Chicago Chapter National Black Nurses Association. Bottom Row: Denise Heath, RN, standing in for Jennifer Reed, RN, President of Alpha Eta Chapter of Chi Eta Phi Sorority, Inc. Each organization’s President gave a warm welcome and shared some of its history with the audience.
Illinois State Senator Mattie Hunter, who represents the 3rd District is the senate secretary for the Illinois Legislative Black Caucus, and the Majority Caucus Whip was the keynote speaker. Her speech highlighted her legislative efforts in creating a more equitable and inclusive healthcare system in Illinois that would lead to reform that could reduce maternal and infant mortality and improve access to mental health care.
Senator Hunter said she was honored to pay tribute to black nurses for their contributions and sacrifices and to nursing students, other medical professionals, and valuable community members. She spoke about the discrimination and unequal pay that black nurses faced but how they never wavered in their commitment to providing passionate and excellent care to their patients. She discussed black nurses’ challenges and obstacles and how they worked to break down barriers to pave the way for a better future.
Senator Hunter told the audience that the COVID19 Pandemic highlighted the critical role of nurses in providing direct care to COVID19 patients, serving as leaders, and advocating for support in their communities. “However, during the COVID19 pandemic, we saw its effects on, and how racism intensified on black Illinoisans.”
Some of the causes Senator Hunter cited are structural racism, insufficient investment in black communities, and the conditions under which people live and work, all contribute to health inequalities. “ In 2019, NYU school of medicine analyzed data showing that Chicago had the largest life expectancy gap in 30 years”.
She reported that these health disparities were exacerbated by limited access to quality health care, lack of healthy food options, and unsafe living environments. Senator Hunter shared the results of a study showing that a black person’s life expectancy is less than that of a white person. She gave an example of a person in the Streeterville community living to the age of 90 and someone in Englewood living only to the age of 60.
Senator Mattie Hunter told the audience she has been passionate about fixing the healthcare system all of her life but that the pandemic revealed many of its flaws.
She promised to continue to serve by using her voice and advocating for equitable health care for underserved members of Illinois.
Senator Hunter encouraged the audience to get involved in working with our legislative officials stating “we need your voice to help us make informed decisions regarding healthcare-related legislation.” She said nurses could get involved by calling their elected officials, attending town hall and community meetings, submitting witness slips, and testifying in Springfield, and through virtual venues. She stressed the importance of working together to address healthcare disparities and inequities.
She thanked the nurses for their tireless work and unwavering commitment to their patients. Her message to the students was not to lose sight that they are making a difference and that there are many people who believe in them. Her speech was powerful and thoughtprovoking.


Olivia Simone Murphy (Marquette University), Faith Chopkurui Rotich (Chicago State University), and Kylie Norman( University of Arkansas at Pine Bluff), not present, were awarded scholarships for academic excellence
Nurses Honored for their Exemplary Service in the areas of Maternal and Mental Health Care.

Myna Shegog , RN( Captain James A Lovell Federal Health Care Center), Cedric Neloms, RN (Hartgrove Hospital ), Twana Johnson, RN (Loretta Hospital ), Juliana Ndukwu, RN (Weiss Memorial Hospital), Mary Chigozie, RN ( Roseland Hospital), Carol Alexander, DNP, RN, ( KAM Alliance, Inc. Mental Health Clinic), Pamela Pearson, DNP, RN( University of Illinois), Samantha Williams, RN (Northwestern Memorial Hospital Prentice Women’s Hospital), Joscelyn Wynter, RN (Loretto Hospital) and Kimberly Morris-Carpenter, RN (Advocate Lutheran General Hospital).

Malika Booker-Williams, RN, accepted the special recognition award on behalf of her mother, Dr. Sandra Webb Booker, RN, past committee Chair of The National Black Nurses Day Planning Committee, for her 35 years of dedicated service.

with the Honorable Senator





Hunter.

On behalf of the ANA-Illinois Nominating Committee and Board of Directors, the Nominating Committee invites you to participate in the 2023 ANA-Illinois Board of Directors Call for Nominations. In the coming months, the Nominations Committee will seek your help in identifying and encouraging strong and emerging leaders to seek board service and serve on the Nominations Committee. In 2023, the ANA-Illinois membership will select 9 colleagues for the following positions:
• President
• Secretary
• Two (2) Directors
• Two (2) Nominations Committee Members
• Three (3) ANA Representatives (2 reps/1 alternate)
Candidates may only apply for ONE of the following positions: president, secretary, director, or Nominations Committee member. Candidates may apply to run for ANA representative or for ANA representative and one of the elected positions noted above (i.e., President, Secretary, Director, or Nominations Committee member).
The Nominations Committee members will be reaching out to members to encourage members from across the state to run for the open positions.
The Nominations Committee is charged with creating a ballot with two candidates for each open position. In order to ensure candidates for each position on the ballot, the Committee may request that candidates consider another elected position. Leaders and emerging leaders are encouraged to consider running for a position.
ALL TERMS ARE FOR 2 YEARS




The Illinois Nurses Foundation’s Editorial Committee would like to get feedback from our Nursing Voice readers. The brief survey will help the committee better tailor our content to our readers wants and needs. We appreciate taking a few minutes to complete our survey at the link below or QR code. https://www.surveymonkey.com/r/J3SG63X



• To print your license or download an electronic copy to your phone, just head to the IDFPR website https:// idfpr.illinois.gov/applications/getmylicense/LoginProf. asp?ViewOption=ind
• Tips for first time registration for individual online account matching process may be found here: https:// idfpr.illinois.gov/Forms/Online/Renewal%20Tips%20 Individual%20Accounts%202021-12-15.pdf
For most licensees, this will be the first time logging into your IDFPR Online Services Portal Account. You will need to Register and MATCH to your existing license record. If you applied for your initial license via the IDFPR portal, you can use the username and password created at that time. For those requiring additional assistance with the login process, please contact IDFPR by emailing fpr.lmu@illinois.gov. Please enter "RENEWAL" in the subject line of your e-mail.
• To change your email address, address or phone number, please click on this link to update the information: https://idfpr.illinois.gov/applications/ LicenseReprint/
• IDFPR knows how critical it is to military families to begin working as soon as they come to the Prairie State. Illinois law includes several provisions designed to help military Service Members and Spouses who are an active duty member or whose active duty service concluded within the preceding two years before application. In addition to expedited review of your application (30 days), the Department’s dedicated Military Liaison will work with you and your military installation’s military and family support center to help you through the licensing process. Learn more online here: https://idfpr.illinois.gov/ Military.asp You may also email the Military Liaison using this email address: fpr.militarylicense@illinois.gov
• The IDFPR “Requirements of an Internationally Educated Nurse” document is available online here: https://idfpr. illinois.gov/Renewals/Apply/Forms/CGFNS_02.pdf Resources on this document include the names of Board of Nursing approved vendors for items required to apply for an Illinois nurse license. Information includes that endorsing an active license from another state requires: an application by Endorsement. A Credential Evaluation Service (CES) Report is not required if the
nurse resources available!
state of original licensure required a report at the time of original licensure. An English equivalency test is not required as long as the nurse applying for endorsement took and passed the NCLEX® licensure examination.
• Learn more about the nursing profession in Illinois on IDFPR’s Nurses webpage: https://idfpr.illinois.gov/ PROFS/Nursing.asp
• Complaints against any individual or entity regulated by the Division of Professional Regulation may be filed by contacting the Complaint Intake Unit. For a complete list of professions regulated by DPR, please click https:// idfpr.illinois.gov/Forms/Brochures/DPR.pdf
Please note: Pursuant to Illinois law (20 ILCS 2105/2105-117), all information collected by the Department during an examination or investigation of a licensee, registrant, or applicant is confidential and cannot be publicly disclosed. This includes complaints and any information collected during an investigation. Exceptions to this law exist only for law enforcement, other regulatory agencies with appropriate regulatory interest, or a party presenting a lawful subpoena. The Division of Professional Regulation online complaint form may be found here: https://idfpr.illinois.gov/ Admin/DPR/Complaint.asp
• On the IDFPR Nurses web page ,there is a list of all 136 Illinois Board of Nursing approved RN/Registered Nurse and LPN/Licensed Practical Nurse pre-licensure nursing education programs: https://idfpr.illinois.gov/ Forms/DPR/NurseSchools.pdf
• IDFPR is providing renewal assistance for individuals and businesses that are having difficulty with the online renewal process. These steps will help licensees better navigate the account matching process on the Department's updated online portal. For those requiring additional assistance, please email: fpr.lmu@ illinois.gov
o Assistance for Individuals: https://bit.ly/3mb8C7U
o Assistance for Businesses: https://bit.ly/3E5Fll8
• A complete copy of the Nurse Practice Act and the Rules may be found on the IDFPR website, idfpr.illinois.gov, or on the Illinois Nursing Workforce Center’s website: https://nursing.illinois.gov/nursepracticeact.asp
Governor JB Pritzker announced the state's public health emergency will end on May 11, 2023, aligning the state with the federal government's decision to end the national public health emergency. Learn more here: https://www.illinois.gov/news/press-release.25998.html
• In March 2023, the Division of Professional Regulation (“DPR”) began notifying COVID-19 temporary practice permit holders via email of the expiration date and providing information on the process of applying for Illinois licensure by endorsement or reinstatement. Learn more here: https://idfpr.illinois.gov/FAQ/ COVID19/IDFPR%20COVID-19%20Temporary%20 Practice%20Permit%20FAQs.pdf
• Frequently Asked Questions (FAQs) with information about what’s next for COVID-19 Temporary Practice Permit Holders may be found here: https://idfpr. illinois.gov/FAQ/COVID19/IDFPR%20COVID-19%20 Temporary%20Practice%20Permit%20FAQs.pdf
• The Department is working with the legislature to potentially allow individuals to continue to practice on their In-State COVID-19 Temporary Reinstatement Practice Permit, and their Out-of-State Temporary Practice Permit provided that they submit an application for restoration or reinstatement of their license to the Department on or before May 11, 2023. For questions regarding new temporary practice permit applications, please email fpr. covidtemporaryapplication@illinois.gov
• The list of health care professional temporary practice permits granted in Illinois may be found here: https://www.idfpr.com/Forms/COVID19/Temp%20 Practice%20Permits.pdf
• IDFPR’s Division of Professional Regulation has issued a notice to remind physicians and other healthcare professionals that any advice or treatment provided to a patient must conform with evidence-based medicine and standards of care and that failure to do so may subject the individual to disciplinary action. Find it here: https://www.idfpr.com/Forms/COVID19/ IDFPR%20statement-physicians.pdf
• The State of Illinois Coronavirus Response Site: The COVID-19 Vaccine Plan, up-to-date information on what Illinois is doing protecting the health, safety, and well-being of Illinoisans can be found at https:// coronavirus.illinois.gov/s/
Are you a Registered Nurse (RN) licensed in Illinois who is looking for an opportunity to share your knowledge and experience with future nurses?
The Illinois Department of Financial and Professional Regulation (IDFPR) and the Illinois Nursing Workforce Center (INWC) have been teaming up with higher education institutions across the Land of Lincoln bringing YOU a series of FREE webinars about the graduate faculty nursing programs in Illinois for you to consider!
The purpose of these 60 minute webinars is:
• To highlight Illinois graduate nursing education colleges and universities that have graduate faculty education programs educating new nursing faculty;
• To recruit nurse educators for Illinois nursing education programs;
• To have webinars available as a resource once completed they are available on IDFPR YouTube page: https://www.youtube.com/@IDFPRmedia
The final webinar is on April 19, 2023. The nursing education programs presenting are: Blessing-Rieman College of Nursing and Health Sciences; McKendree University; Oak Point University; Olivet Nazarene University; University of St Francis, Leach College of Nursing. Signup for the event can be found here: https:// ILGraduateNursing5.eventbrite.com
The past webinars celebrating Illinois graduate education programs preparing nursing faculty are available on IDFPR’s YouTube page. Please feel free to share and distribute as you see fit!
This is a link to the YouTube October 19, 2022 webinar: https://www.youtube.com/watch?v=61Ce-vaut-g
• Dr. Becky Hulett, Elmhurst College;
• Dr. Fred Brown, Rush University College of Nursing;
• Dr. Kay E. Gaehle, Southern Illinois University Edwardsville;
• Dr. Caroline Kreisl Wilson, St. Xavier University-DE.
This is a link to the YouTube December 14, 2022 webinar: https://www.youtube.com/watch?v=0R4gkGJ72vc
• Dr. Donna Martin, Lewis University;
• Dr. Kim Schafer Astroth, Mennonite College of Nursing at ISU;
• Dr. Carole Eatock, St. Francis Medical Center College of Nursing;
• Dr. Teresa Krassa, University of Illinois – six campuses.
This is a link to the YouTube February 15, 2023 webinar: https://www.youtube.com/watch?v=7djPr4Mq2G4
• Dr. Alison Ridge, Benedictine University;
• Dr. Suline Li, DePaul University;
• Dr. J. Ann Raithel, Chamberlain College of Nursing;
• Dr. Kate Coulter, Northern Illinois University
This is a link to the YouTube March 15, 2023 webinar: https://www.youtube.com/watch?v=Y9UcccfJgxU
• Dr. Nancy MacMullen, Governor’s State University;
• Dr. Theresa Schwindenhammer, Methodist College;
• Dr. Kate Coulter, Northern Illinois University;
• Dr. Elizabeth Carson, St. Anthony College of Nursing
Each webinar panel member shares essentials such as program entry requirements, per cent of classes online, balance of current work, classes and requirements with family and professional development. Please join us in preparing future nurses.
The Illinois Nursing Workforce Center website (https:// nursing.illinois.gov) includes links to:
• Graduate nursing education programs https:// nursing.illinois.gov/Gradeducation.asp
• Graduate nursing education programs with focus areas leading to systems focused roles https:// nursing.illinois.gov/PDF/2022-06-08a_INWC_Grad_ NsgEd_FocusAreaLeadSystFocusRole_Ltrhd.pdf
• Established relations with community colleges across the state, useful for transfer of credits to the graduate program https://nursing.illinois.gov/PDF/2020-05-06_ ILBSNcPgms_Partnerships_Final.pdf
• IDFPR nurse page https://idfpr.illinois.gov/PROFS/ Nursing.asp
Susan Hovey PhD, RN, CNE, Clinical Assistant Professor, University of Illinois at Chicago College of Nursing, Springfield, Il 62703 slhovey@uic.edu
Michele Shropshire, PhD, RN, Associate Professor, Mennonite College of Nursing at Illinois State University, Normal, IL mdshrop@ilstu.edu
Keywords: group-based reminiscence, older adult, assisted living, mental health
As lifespans increase, many people will develop a chronic condition or physical limitation that may require them to enter an assisted living environment. According to the National Center for Health Statistics (2019) projections, 27 million individuals will utilize some type of long-term care service, including assisted living environments by 2050; at the same time, aging in place continues to be a strong community health initiative (U.S. Department of Health and Human Services, 2017). Healthcare professionals working in assisted living environments have an opportunity to help promote optimal social and emotional functioning, inhibit cognitive and/or physical decline, and promote person-centered care. And, by providing meaningful therapy and exploring activities to improve health for older adults in assisted living untimely transitions into a nursing home may be prevented. Importantly, a priority for person-centered care is to improve health for older adults living in assisted living environments and support those who work to facilitate aging in place among older adults. Maintaining positive mental and emotional health for older adults in assisted living environments is of vital interest to the public, policy makers, and healthcare stakeholders.
Assisted living environment services are often used by individuals with chronic conditions, such as chronic pain, physical disability, and functional limitations. Healthcare professionals caring for older adults not only focus on physical ailments but are attentive to their mental, social, and emotional health (Cowling, 2015). Within assisted living environments, social stimulation is important to prevent cognitive decline and depression, which may prematurely necessitate the need for higher, more costly levels of care, such as nursing home care (Mason et al., 2014). It remains imperative for nurses and other healthcare professionals caring for this population to address the whole person: body, mind, and spirit (Cowling, 2015).
Reminiscence
Reminiscence is defined as “a method or technique to recall past memories” (Westerhof et al., 2010, p. 698). Reminiscence is not a new concept. The importance of reminiscence for older adults was first explored by Butler in 1963 and has continued to be studied since that time (Webster et al., 2010; Westerhof et al., 2010). Although group-based reminiscence therapy may vary based upon specific facility preference, the over-arching objectives for group-based reminiscence therapy are to encourage socialization, promote discussion around historic artifacts, and encourage participants to share memories and/or generational experiences relating to the historic artifact. (Pinquart & Forstmeier, 2012).
Fundamental elements of reminiscence therapy include organizing the session with an identified time, date, and location. A facilitator will display germane historical artifacts, then describe and discuss the significance of the items. Commonly, the facilitator will foster group discussion by sharing positive memories and/or discussing the historical meaning of the artifact which often elicits sharing of generational experiences by older adults participating in the discussion (Stinson, 2009). Throughout the literature, reminiscence therapy ranges from individual reminiscence sessions with a single caregiver to group reminiscence sessions with one or more facilitator(s) (Abdel-Aziz & Ahmed, 2021; Gallagher & Carey, 2012; Smiraglia, 2015; Soniya, 2015; Stinson, 2009; Tadaka & Kanagawa, 2007; Watt & Cappeliez, 2000). Despite the variations, facilitated discussion which encourages participants’ discussion of the artifact, personal memories, and generational experiences remain significant components.
Group discussions often focus on objects and pictures from time periods in the 1920s, 1930s, 1940s, and 1950s to elicit participant memories of past experiences (Smiraglia, 2015). Among the literature, one-hour sessions discussing pictures, music, household
objects, and newspapers are the most common groupbased reminiscence therapy (Gallagher & Carey, 2012; Smiraglia, 2015; Soniya, 2015; Stinson, 2009; Tadaka & Kanagawa, 2007; Watt & Cappeliez, 2000). Groupbased reminiscence therapy is a natural occurring, nonpharmacological approach that may offer cognitive, social, and physical stimulation to older adult participants (Webster et al., 2010; Westerhof et al., 2010).
Psychologists have used reminiscence therapy to assist clients to review life experiences with the goal of addressing unresolved conflicts by bringing them into conscious awareness (Cook, 1984). Today, elements of reminiscence are being explored as means to prevent or address mental health concerns, such as loneliness, depression, and/or anxiety. Notably, reminiscence therapy has been shown to improve short-term memory, psychological and emotional well-being, improve quality of life, increase socialization, self-esteem, life satisfaction, and social adjustment while preventing and/or reducing social isolation, loneliness, and depression in older adults (Chiang et al., 2010; Gallagher & Carey, 2012; Gil et al., 2022; Abdel-Aziz & Ahmed, 2021; Tam et al., 2021).
The aim of the study is to determine whether Senior Reminiscence Therapy (SRT) decreases depression and loneliness in older adults living in assisted living environments. The purpose of this study is to assess the feasibility of studying Senior Reminiscence Therapy in assisted living environment.
Feasibility studies are valuable in health research, as modifications to design and methods may occur for future larger studies (Lancaster et al., 2004; Orsmond & Cohn, 2015). As reminiscence therapy may offer positive mental health benefits to older adults residing in assisted living environments, we conducted a feasibility study to determine if our study protocols, data collection methods, and instruments were suitable for use among older adults residing in these environments.
A community partnership between the local county museum of history and two assisted living environments were established to facilitate the study. The assisted living facilities are located in a large mid-western state and provided a setting for the six-month SRT intervention. Participants were recruited using convenience sampling. Inclusion criteria were that the participant reside in an assisted living facility and be 65 years of age or older. Any resident with overt psychiatric disorders and/or physical limitations that prevented participation were excluded. Five people consented to participate and completed the six-month study.
The Principal Investigator (PI) obtained permission and letters of support from authorized administrators from each assisted living setting prior to Institutional Review Board approval as required. Recruitment, implementation of the intervention, and data collection did not occur until after Institutional Review Board approval.
Recruitment for this study began two weeks prior to the start of the SRT intervention. During this time, the PI set up a recruitment table in the lobby of each assisted living facility with a 30x40-inch poster describing the aim of the study and details of participation. The PI was always present to answer questions when the recruitment table and poster were on display. A total of 38 participants approached the recruitment table and received information verbally. Participation in the study was voluntary and all individuals were invited to attend the SRT intervention sessions regardless of involvement with the study. To enroll in the study, persons were asked to state the purpose of the study prior to signing the informed consent. Informed consent was obtained from each participant, and each participant completed a baseline questionnaire before attending the first SRT session. Depending on preference, participants completed the written informed consent process and questionnaire in a private conference room or the individual’s private room, with the researcher physically present and available to answer questions. In a six-month period, four reminiscence therapy sessions were offered at each assisted living facility. Data were captured at baseline, following the second reminiscence therapy, and post-reminiscence therapy completion.
The SRT sessions occurred in groups and used items from eras ranging from the 1920s to the 1960s, including kitchen utensils and appliances, toys, games, tools, photographs, and vintage dresses. Utilization of these items provided participants with the opportunity to recall, engage, learn, and socialize with other participants in attendance. Participants sat in chairs set up in audience format as the facilitator displayed historical artifacts and provided a 2-5 minute description of the item. Afterward, the facilitator led participants in group discussion to recall their memories and experiences.
All SRT sessions were led by a facilitator with a master’s degree in historical administration and a baccalaureate degree in history. The lead facilitator has conducted museum-based SRTs for over five consecutive years and furnished scripted sessions to provide consistency. Using inquiry-based facilitation, the facilitator, an employee from the county museum of history, encouraged participants to recall memories, share experiences, and connect with other group participants. The therapy intervention lasted approximately 45-60 minutes.
The study included a convenience sample (n=5, 3 female [60%] and 2 male [40%]) with an average age of 85.8, SD=3.70 and widowed 100%. Qualitative comments from participants illustrated a positive evaluation of the SRT sessions. Analysis of the data provided rich insight into the participants perspectives and satisfaction with the SRT sessions. One participant wrote, “Enjoyed it, brought back fond memories.” Participants also requested future themes they would like incorporated into the reminiscence therapy intervention.
Although 47 individuals attended the SRT sessions, only five participants enrolled and completed the feasibility study. The inclusion and exclusion criteria established for this study is appropriate. It is not too inclusive or restrictive. The biggest obstacle was recruiting and enrolling participants in the study. The residents at the assisted living facility were curious, friendly, and anxious to attend the sessions, but were reluctant to sign an informed consent and complete the surveys. Trust is an essential aspect of the research process with older adults and an extended presence by the researcher in an assisted living facility could help build a trusting relationship. Older adults tend to be suspicious about un-known persons requesting information from them. Older adults may also be suspicious of the researcher sharing data that may “get them in trouble.”
The characteristics of the participants were consistent with the range of expected characteristics as outlined in the literature. What was surprising with our sample demographics was all participants were widowed. Spousal loss is a life-changing event leading to social isolation that can have negative consequences on a widower’s physical health and mental well-being. A significant association exists between being widowed and lower psychological well-being compared to older adults with married status who did not lose their spouse (van Boekel, Cloin, & Luijkx, 2021). All participants in this feasibility study were widowed and may have lower psychological well-being. Only including participants who are widowed could skew study results.
What we learned was allowing for more recruitment time may increase the number of participants. In addition to establishing a trusting relationship with the residents, we recommend that researchers foster relationships with gate-keepers, such as well-liked staff or socially adept residents within the facility. This phenomenon is documented in the literature (Shropshire et al., 2020). In addition, SRT intervention brochures and flyers with study information should be distributed via the resident mail system two months prior to the start of study recruitment.
The questionnaire utilized in this study was appropriate and feasible for the population. Participants were able to understand and answer the questions without difficulty. On average, each participant took an hour to complete the questionnaire and the environment was conducive to completing the questionnaire. Four out of five participants chose to complete the survey in the privacy of their own room with the researcher present in case participants had questions. What we learned
was the participants prefer paper and pencil surveys over an electronic version of the survey. Researchers need to be available to answer questions while participants complete the survey but must be careful to protect their anonymity and take every measure not to interfere with the resident completing the questionnaires.
Acceptability and Suitability of Intervention
We found the assisted living environment conducive to the SRT sessions and older adults residing here to be responsive and receptive to SRT intervention. Although only five residents consented to complete the questionnaires, approximately 15 residents attended each SRT session. The SRT intervention lasted over 60 minutes. This time period was sufficient, but some participants verbalized they wished the therapy intervention could be longer in the future.
What we learned was it is not possible to have this activity last longer than 60 minutes. The assisted living facilities have several activities scheduled in their activity room each day, so scheduling this room in advance for the SRT sessions is imperative. In addition, residents in assisted living often have a full schedule during the day with several options for activities. All participants in our study were mobile, three participants were out of the facility on a community outing for the second SRT intervention and data collection. The researcher needs to ensure that the SRT sessions do not interfere with scheduled outings when setting up the schedule. The researcher should consider scheduling the SRT sessions at mid-morning before participants leave for scheduled activities.
Resources
The SRT sessions were conducted in the facility’s activity room, which was equipped with tables and chairs. The artifacts were displayed on the table for the residents to observe during and after the therapy intervention. The facilitator for this study had a master’s degree in historical administration and a baccalaureate degree in history. A script was used to share historical information about the artifacts and ask questions to encourage participants to recall memories, share experiences and connect with other participants in attendance. Although scheduling can be challenging, the SRT sessions fit in the daily life activities of the participants. The 60 minutes sessions do not create a burden for the participants.
What we learned was anyone can facilitate SRT sessions. An individual with a degree in history or historical administration is not required. Artifacts can be visual or auditory or both. Plus, incorporating more pictures of local and/or historical places of significance may result in a richer discussion among participants. To provide consistency a script is needed to share information about the artifacts and encourage participation by asking the same open-ended questions across facilities. These sessions can be created on a limited budget with very few resources. The most time consuming piece will be assisting residents in completing the survey. For the feasibility study, participants were asked to complete the survey pre-, mid-, and post. Because a researcher needs to be available with the participant as they fill out the survey, the PI might consider administering the survey only pre- and post- if they are completed in the privacy of the residents room, but if a pre-, mid-, and post- survey is administered asking the participants to complete them in a group setting to reduce researcher time is warranted..
Preliminary Evaluation of Participant Responses
The small sample size of this feasibility study would not yield reliable or precise estimates of differences in loneliness and depression even with a nonparametric test. The administration of the questionnaires was used to design a future, larger confirmatory study. Based on participants responses, our study suggests SRT intervention decreased perceived loneliness in participants. Loneliness may have negative physiological implications for older adults in assisted living environments and when an older adult relocates to a new living environment (such as an assisted living facility), loneliness can occur. Loneliness may be a precursor to physiological problems, such as depression, decreased appetite, and sleep disturbances (Bohlmeijer et al., 2008). Decreasing loneliness can result in social, cognitive, and emotional benefits for older adults in assisted living environments and meaningful activities derived from evidenced-based interventions is essential to support healthy aging initiatives, such as Aging in Place (U.S. Department of Health and Human Services, 2017). This feasibility study offers valuable insight into person-centered, meaningful therapy to engage and stimulate older adults residing in assisted living environments.
What we have learned is SRT sessions appear to reduce loneliness, but capturing depression with a questionnaire may not adequately depict changes due to the SRT intervention. A mixed method approach may be required. This is consistent with results by Hobbs et al. (2021) who found that scores on questionnaires differed from patients’ own view of mood changes. Questionnaires may only capture a subset of the participants experience, so results may be misleading (Hobbs et al., 2021).
Limitations
There are limitations in this study. First, there was a small sample size; therefore, statistical analyses could not be performed. Participants were encouraged to attend all sessions in the six-month study parameters, but some sessions conflicted with participants’ medical appointments, other offered activities, and/or family visits. Therefore, some participants were unable to attend all sessions and did not complete questionnaires for missed sessions.
It cannot be dismissed that six months may have been too brief to detect any substantiated difference in depression and loneliness scores. For future studies, offering the intervention for more than six months may be warranted when testing for a significant change in depression and loneliness.
Assisted living environments serve older adults by providing personalized care in a residential setting. These communities not only assist older adults with their physical needs, but also their emotional and mental well-being. Activity directors and nursing staff are capable with training to lead a reminiscing intervention. Reminiscence therapy intervention has been shown to improve social, emotional, and mental well-being in older adults. Addressing these psychosocial health concerns in older adults with nonpharmacological therapy is necessary. This is one of many therapies that can improve health outcomes and accomplish the health initiative of aging in place.
Conclusion
This feasibility study has demonstrated the SRT intervention is appropriate and wellreceived by older adults residing in assisted living environments. Reminiscence therapy eased their feelings of loneliness and elicited “fond memories” in participants. As leaders in assisted living facilities plan therapy interventions and activities for residents, meaningful activities such as a group-based reminiscence therapy may be pivotal for best
health outcomes. The mental and social health benefits of the group-based reminiscence therapy may go far beyond the provision of entertainment for older adults. Themed therapy intervention, such as the ones performed in this study, offer mentally engaging, social experiences that allow ample opportunity for participation from residents. Through the reminiscence therapy, participants may recall and share memories that contribute toward a community identity, facilitate human connection, and decrease perceived loneliness and depression. The health benefits of group-based reminiscing for older adults specifically residing in assisted living environments has limited research (Gallagher & Carey, 2012) and warrants examination in the future.
References
Abdel-Aziz, H. R., & Ahmed, H. A. A. (2021). The effect of group reminiscence therapy on selfesteem and emotional well-being of older adults. Central European Journal of Nursing & Midwifery, 12(4), 513–520. https://doi.org/10.15452/CEJNM.2021.12.0027
Bohlmeijer, E. T., Westerhof, G. J., & Emmerik-de Jong, M. (2008). The effects of integrative reminiscence on meaning in life: Results of a quasi-experimental study. Aging and Mental Health, 12(5), 639–646. https://doi.org/10.1080/13607860802343209
Chiang K, Chu H, Chang H, Chung M, Chen C, Chiou H, & Chou K. (2010). The effects of reminiscence therapy on psychological well-being, depression, and loneliness among the institutionalized aged. International Journal of Geriatric Psychiatry, 25(4), 380–388. https:// doi.org/10.1002/gps.2350
Cook J. B. (1984). Reminiscing: how it can help confused nursing home residents. Social Casework, 65(2), 90–93. https://doi.org/10.1177/104438948406500204
Cowling, W. R. (2015). The scope and standards of holistic nursing practice. Journal of Holistic Nursing, 33(4), 288. https://doi.org/10.1177/0898010115614094
Gallagher, P., & Carey, K. (2012). Connecting with the well-elderly through reminiscence: Analysis of lived experience. Educational Gerontology, 38 (8), 576–582. https://doi.org/10.1080/03601 277.2011.595312
Gil, I., Santos-Costa, P., Bobrowicz-Campos, E., Silva, R., de Lurdes Almeida, M., & Apóstolo, J. (2022). Effectiveness of reminiscence therapy versus cognitive stimulation therapy in older adults with cognitive decline: A quasi-experimental pilot study. Nursing Reports, 12(2), 339–347. https://doi.org/10.3390/nursrep12020033
Hobbs, C., Lewis, G., Dowrick, C., Kounali, D., Peters, T. J., & Lewis, G. (2021). Comparison between self-administered depression questionnaires and patients’ own views of changes in their mood: a prospective cohort study in primary care. Psychological Medicine, 51(5), 853–860. https://doi.org/10.1017/S0033291719003878
Lancaster, G.A., Dodd, S., and Williamson, P.R. (2004). Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice, 10 (2), 307-312. https://doi.org/10.1111/j..2002.384.doc.x
Mason, Dickson, E. L., McLemore, M. R., & Perez, G. A. (2021). Policy & politics in nursing and health care (Mason, E. L. Dickson, M. R. McLemore, & G. A. Perez, Eds.; Eighth edition.). Elsevier. National Center for Health Statistics. (2019). Long-term care providers and services users in the United States, 2015-16: Data from the national study of long-term care providers. Department of Health and Human Services: DHHS Publication.
Orsmond, G. I., & Cohn, E. S. (2015). The distinctive features of a feasibility study: Objectives and guiding questions. OTJR: Occupation, Participation and Health, 35(3), 169–177. https://doi. org/10.1177/1539449215578649
Pinquart, M., & Forstmeier, S. (2012). Effects of reminiscence interventions on psychosocial outcomes: A meta-analysis. Aging & Mental Health, 16 (5), 541–558. https://doi.org/10.1080/1 3607863.2011.651434
Shropshire, M., Stapleton, S.J. & Dyck, M.J. (2020). Barrier and insights found in research recruitment of assisted and supportive living facilities. Nursing Science Quarterly, 33(2), 116–121. https://doi.org/10.1177/0894318419898159
Smiraglia, C. (2015). Museum programming and mood: Participant responses to an object-based reminiscence outreach program in retirement communities. Arts and Health: International Journal for Research, Policy and Practice, 7(3), 187-201. https://doi.org/10.1080/17533015.2015.1010443
Soniya, G. (2015). Reminiscence therapy to reduce depression among elderly. International Journal of Nursing Education, 7(2), 160-164. https://doi.org/10.5958/0974-9357.2015.00095.1.
Stinson, C. K. (2009). Structured group reminiscence: An intervention for older adults. Journal of Continuing Education in Nursing, 40 (11), 521-528. https://doi.org/10.3928/00220124-20091023-10
Tadaka, E., & Kanagawa, K. (2007). Effects of reminiscence group in elderly people with Alzheimer disease and vascular dementia in a community setting. Geriatrics and Gerontology International, 7(2), 167-173. https://doi.org/10.1111/j.1447-0594.2007.00381.x
Tam, W., Poon, S. N., Mahendran, R., Kua, E. H., & Wu, X. V. (2021). The effectiveness of reminiscence-based intervention on improving psychological well-being in cognitively intact older adults: A systematic review and meta-analysis. International Journal of Nursing Studies, 114, 103847–103847. https://doi.org/10.1016/j.ijnurstu.2020.103847
U.S. Department of Health and Human Services. (2017). Aging in Place: Growing Older at Home. https://www.nia.nih.gov/health/aging-place-growing-older-home
van Boekel, L. C., Cloin, J. C. M., & Luijkx, K. G. (2021). Community-dwelling and recently widowed older adults: Effects of spousal loss on psychological well-being, perceived quality of life, and health-care costs. International Journal of Aging & Human Development, 92(1), 65–82. https://doi.org/10.1177/0091415019871204
Watt, L., & Cappeliez, P. (2000). Integrative and instrumental reminiscence therapies for depression in older adults: Intervention strategies and treatment effectiveness. Aging and Mental Health, 4 (2), 166-177. https://doi.org/10.1080/13607860050008691
Webster, J. D., Bohlmeijer, E. T., & Westerhof, G. J. (2010). Mapping the future of reminiscence: A conceptual guide for research and practice. Research on Aging, 32(4), 527–564. https://doi. org/10.1177/0164027510364122
Westerhof, G. J., Bohlmeijer, E., & Webster, J.D. (2010). Reminiscence and mental health: A review of recent progress in theory, research and interventions. Ageing and Society, 30 (4), 697–721. https://doi.org/10.1017/S0144686X09990328

A State Board of Nursing (SBON) complaint may be filed against a nurse by a patient, colleague, employer, and/or other regulatory agency, such as the Department of Health. Complaints are subsequently investigated by the SBON in order to ensure that licensed nurses are practicing safely, professionally, and ethically. SBON investigations may lead to outcomes ranging from no action against the nurse to revocation of the nurse’s license to practice. This case study involves a registered nurse (RN) who was working as a traveling nurse on an oncology floor.
Summary
The insured registered nurse (RN) involved in this matter was a traveling nurse working on an oncology floor. The RN took a dose of pregabalin capsules out of the automated medication dispensing cabinet and requested that another nurse on the floor, who was also a traveling nurse, administer it to her patient. The second nurse took the medication and gave it to a patient. The second nurse soon realized she had given the medication to the wrong patient. She immediately called the physician on call and notified the Charge Nurse that the wrong patient had received a dose of pregabalin. The RN then recorded the medication error in the patient healthcare information record per hospital policy.
While the RN and the second nurse told the physician on call and the Charge Nurse what actually happened with the pregabalin dose, both also agreed to record the improperly administered pregabalin dose as a waste on the Controlled Substance Discard Record. The RN then went to the pharmacy to obtain a new dose of pregabalin for her patient. When the pharmacist asked why she needed another dose, the RN

stated that she had accidentally dropped the other capsule on the floor and had disposed of it in the sharps container.
The pharmacist later ran a report on the automated medication dispensing cabinet to track how much pregabalin was dispensed the date of the incident. While the pharmacist expected to find two doses administered to the correct patient that day and one dropped/wasted dose, she found that two were administered to the correct patient and one had actually been administered to the wrong patient. The pharmacist reported this discrepancy to hospital administrators, who initiated an internal investigation into the nurses’ conduct.
The RN later admitted to hospital personnel that she was untruthful to the pharmacist about wasting the pregabalin. Both nurses stated that they had been untruthful about wasting the medication so that the RN’s patient would not be charged twice for the dose of pregabalin due to their mistake.
The hospital investigators also concluded that the RN falsified the signature on the Controlled Substance Discard Record. The signature on the record was illegible. When the RN was asked who had signed the record, she gave the name of another nurse who worked on the floor. This statement was soon revealed to be untrue when it was discovered that the nurse the RN named had not been working on the date of the incident.
At the conclusion of their internal investigation, hospital personnel terminated the RN’s contract and reported the RN to the State Board of Nursing (SBON). The hospital also complied with the subsequent SBON investigation into the RN’s alleged conduct.
At the conclusion of their review of the facts of the matter, the SBON admonished the RN for failing to follow appropriate procedure for obtaining a second dose for the correct patient. The SBON also lamented that the RN documented false information about the medication error in the Controlled Substance Discard Record without any need to do so- she had already disclosed the medication error.
The SBON decided to place the nurse on probation for three years. The total costs incurred to defend the nurse in this case exceeded $7,000 (Note: Monetary amounts represent the legal expenses paid solely on behalf of the insured registered nurse.)
Nurses can reduce risks associated with medication errors by following suggested actions:
• Remember that no medication safety method is infallible. Understand that while technologies such as bar-code scanning can help reduce medication errors, this and other medication safety methods are not immune to system or human error. This is why it is important to employ multiple, concurrent safety measures, including consistently verifying the “six rights” when administering medications to patients:
o Right patient;
o Right drug;
o Right dose;
o Right route;
o Right time; and
o Right documentation.
• Know the medication(s) being administered to the patient. Although nurses do not prescribe, and only rarely dispense medications, they are responsible for administration. Nurses represent the last line of defense to prevent medication errors from reaching the patient. Therefore, they must understand why the patient is taking a specific medication, as well as interactions, side effects, or adverse reactions that may occur.
• Eliminate sources of distraction and interruption, as much as possible, when administering medication.
• Follow established medication protocols. If “work-arounds” persist, consult with the facility’s nursing leadership about opportunities to improve medication protocols and systems, and methods to enhance staff monitoring and compliance.
These are illustrations of actual claims that were managed by the CNA insurance companies. However, every claim arises out of its own unique set of facts which must be considered within the context of applicable state and federal laws and regulations, as well as the specific terms, conditions and exclusions of each insurance policy, their forms, and optional coverages. The information contained herein is not intended to establish any standard of care, serve as professional advice or address the circumstances of any specific entity. These statements do not constitute a risk management directive from CNA. No organization or individual should act upon this information without appropriate professional advice, including advice of legal counsel, given after a thorough examination of the individual situation, encompassing a review of relevant facts, laws and regulations. CNA assumes no responsibility for the consequences of the use or nonuse of this information.
This publication is intended to inform Affinity Insurance Services, Inc., customers of potential liability in their practice. This information is provided for general informational purposes only and is not intended to provide individualized guidance. All descriptions, summaries or highlights of coverage are for general informational purposes only and do not amend, alter or modify the actual terms or conditions of any insurance policy. Coverage is governed only by the terms and conditions of the relevant policy. Any references to nonAon, AIS, NSO, NSO websites are provided solely for convenience, and Aon, AIS, NSO and NSO disclaims any responsibility with respect to such websites. This information is not intended to offer legal advice or to establish appropriate or acceptable standards of professional conduct. Readers should consult with a lawyer if they have specific concerns. Neither Affinity Insurance Services, Inc., NSO, nor CNA assumes any liability for how this information is applied in practice or for the accuracy of this information.
Nurses Service Organization is a registered trade name of Affinity Insurance Services, Inc., a licensed producer in all states (TX 13695); (AR 100106022); in CA, MN, AIS Affinity Insurance Agency, Inc. (CA 0795465); in OK, AIS Affinity Insurance Services, Inc.; in CA, Aon Affinity Insurance Services, Inc., (CA 0G94493), Aon Direct Insurance Administrators and Berkely Insurance Agency and in NY, AIS Affinity Insurance Agency.
Author: Willis L. Drake.
Credentials: First time author at the age of 79; and at age 82 this is my second book.
E-mail: willisdrake@mdirecord.net
For the majority of her young life, living in East St. Louis, Illinois, Mary Ann Byas aspired to become a registered nurse. After a year of attending SIU (Southern Illinois University Carbondale, IL); Mary as a seventeen year- old young adult, submitted her letter of inquiry to the Homer G. Phillips (HGP) School of nursing in 1959. HGP was considered one of the country’s prestigious nursing schools, particularly among the best AfricanAmerican nursing schools.

Nurses want to provide quality care for their patients. The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.
❑ Mastercard ❑ VISA
Credit card number Expires CVV
City, State, Zip Code:
Preferred Phone Number:
Please mail completed form & check to: ANA-Illinois
Atten: Nurses-PAC
PO Box 636 Manteno, Illinois 60950
Mary had to compete with local Missouri in-state and out-of-state nursing students from across the United States who sought enrollment at HGP. Therefore, the outof-state students, as Mary was, had to be among the top applicants to be admitted to HGP Nursing School.
She was accepted in the 1959 HGP freshman nursing class that had a total of twenty-nine students. Twentytwo were from Missouri, and seven students collectively were from the states of Michigan, Illinois, Arkansas, Tennessee, Mississippi, Texas, and North Carolina.
Mary received a financial aid grant from the state of Illinois which paid her tuition, and she received a fifteen dollars weekly stipend. The condition for her grant specified that after graduating from nursing school, she would be obligated to work as a registered nurse in the state of Illinois for three years. We repaid the loan, and Mary was released from all obligations she had to the Illinois State government for employment purposes.
Expected publication date: April 2023 I hope this book serves as an inspiration to all to know that Mary’s internal strength was that she “had faith in God.” She was “Destined and Determined To Be A Nurse.”
From a young age, Mary Ann felt destined to become a nurse. Although she was a shy child, that did not stop her from dreaming big. Instilled with encouragement from her parents and a strong work ethic from her grandparents, Mary Ann was determined to achieve her dream.
However, the road to fulfilling her dream was not smooth. Missteps, hardships, obstacles, and setbacks threatened to derail Mary Ann’s achievement of her dream. But with steadfast determination, faith in God and the call on her life, and the support and help of true angels—one of them her loving husband, Willis—Mary Ann persevered and fulfilled her dream of becoming a registered nurse.
This moving story of this remarkable woman’s faith, courage, determination, and perseverance is a testament to God’s grace and provision. Despite the mistakes we make and the obstacles and hardships we may encounter in life, we will achieve our dreams—if we are destined and determined.
College-age women and men who feel called to the nursing profession will be inspired, encouraged, and motivated by Mary Ann’s story, as well as discover her kindred spirit of love and compassion.



You rose to meet the challenges of the last few years. You’ve been through more than most people can imagine. And you’ve got a lot more to give.
Do more for yourself, to do more for others. That’s where Oak Point University comes in.
We offer:
• Nurse Educator — MSN
• Family Nurse Practitioner (FNP) — MSN
• Adult-Gerontology Primary Care NP (AGPCNP) — MSN
• Adult-Gerontology Acute Care NP (AGACNP) — MSN, certificate
• Psychiatric-Mental Health NP (PMHNP) — MSN, certificate
• Doctor of Nursing Practice with Urban Health/Policy focus learn more at oakpoint.edu/power-forward




