
The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.


The Official Publication of the Illinois Nurses Foundation Quarterly publication direct mailed to approximately 4,500 RNs and electronically via email to 96,000+ RNs in Illinois.
The Illinois Nurses Foundation (INF) held its annual Holiday Fundraising Gala on December 2nd , 2023 at the DoubleTree by Hilton in Lisle. It was a joyful evening for the Foundation and all those that came to celebrate. Various organizations and supporters of the Foundation purchased entire tables for the event, which provided an excellent way to spend time with friends and family during the holiday season while supporting a great cause. The event offered the perfect blend of holiday cheer, networking, and excitement with the online silent auction, giving tree, raffles, and the 50/50 cash giveaway. Thanks to the overwhelming support of all the attendees, the Gala raised over $25,000!
Each year the Foundation's "Honor a Nurse" campaign grows. The project was designed to Honor nurses who have fought for the advancement of the profession and who inspire others to recognize their commitment to their patients and the work they do every day.
Nominations for the "Honor a Nurse" campaign were received throughout the year. The outpouring of stories collected were reviewed and narrowed down to five finalists, chosen by the Foundation Board members.

The 2023 Nurse of the Year award was then presented to Jennifer Sandoval. The story submitted to honor her read:
Dr. Jennifer Sandoval is a dedicated nurse with eight years of service at JESSE BROWN VA. Her exemplary work extends beyond patient care; she serves as a role model and educator at DePaul University, inspiring future nurses.
In volunteerism, Jennifer actively contributes to health initiatives, supports substance abuse programs, and grants wishes through Make a Wish for children with critical illnesses.
As a first-generation college graduate, proud Latina, and active member of various nursing organizations, Jennifer embodies the values of diversity and inclusivity.
Jennifer recently completed her DNP/FNP degree, she is a stellar role model for continuing education and enhancing the nursing profession.

these reasons, Jennifer Sandoval was nominated for the Nurse of the Year Award.
The other finalists included Cheryl Anema PhD, RN, Analia Elizalde DNP, APRN, FNP-BC, PEL-CSN, Susana Golzalez MHA, MSN, RN, CNML & Monique Reed PhD, MS, RN, FAAN. The stories submitted to honor them read:
Cheryl Anema PhD, RN
Dr. Cheryl Anema, a devoted nurse with almost 45 years of experience, has excelled in various roles, from bedside nurse to Dean of Nursing.
Notably, during the COVID-19 pandemic, she tirelessly advocated for her family, even when her family couldn't have visitors. Cheryl's commitment extends beyond her professional duties; she demonstrated exceptional compassion aiding a stranger in a roadside emergency.
Currently teaching NCLEX review courses nationwide, Cheryl ensures the success of new graduates. Her unwavering dedication to nursing and selfless acts make her a standout nominee.
For these reasons, Dr. Cheryl Anema was nominated for Nurse of the Year Award.
Analia Elizalde DNP, APRN, FNP-BC, PEL-CSN
Dr. Analia Elizadle, School Nurse, Health Services Coordinator and recent DNP graduate from Illinois State University, is a beacon of inspiration in education and nursing advocacy.
Serving as a mentor and advocate on the Illinois Association of School Nurses Board of Directors, Analia has passionately advanced the nursing profession, particularly in school nursing.
Her roles, including as Advocacy/Legislative Coordinator, reflect her dedication to promoting diversity, equity, and inclusion. Analia's pursuit of higher education underscores her deep commitment to nursing, making her an outstanding educator, role model, and supportive colleague.
For these reasons, Analia Elizadle was nominated for the Nurse of the Year Award.
Susana Gonzalez MHA, MSN, RN, CNML Susana is a dynamic leader, role model, and mentor, recognized for her unwavering commitment to nursing excellence.
Known for seeing and fostering potential, she tirelessly educates, guides, and advocates for the profession's advancement. Despite challenges, Susana remains actively involved, inspiring others to participate and contribute positively. A shining presence in the nursing community, she is widely recognized at events.
Susana's impactful contributions and dedication to the future of nursing make her an exceptional and admired nurse leader.
For these reasons, Susana Gonzalez was nominated for the Nurse of the Year Award.
Moniqe Reed PhD, MS, RN, FAAN
Dr. Monique Reed, a dedicated nurse leader, stands out for her commitment to community service, volunteer work, and impactful research.
As a faculty member, she plays a pivotal role in the graduate entry to the master's program, specializing in public/community health nursing, and provides guidance in doctoral research. Notably, Dr. Reed is the principal investigator for an NIH grant focused on preventing obesity in Black adolescent girls and their mothers, demonstrating over a decade of dedicated research in this area. Additionally, she serves as a liaison between the College of Nursing and an inner-city Chicago Public School's school-based clinic, showcasing her dedication to community health initiatives.
I hope this message finds you in good health and high spirits. As we embark on a new year filled with possibilities and opportunities, I am delighted to share some exciting updates from the Illinois Nurses Foundation.

Amanda Oliver BSN, RN, CCRN, CPST
First and foremost, I want to express my heartfelt gratitude to everyone who contributed to the success of our recent Holiday Gala & Fundraiser. We honored our Top 5 Finalists for Illinois Nurse of the Year and awarded our Nurse of the Year Award to Dr. Jennifer Sandoval. In addition, we recognized Dr. Maureen Shekleton with our Lifetime Achievement Award. We are so happy to recognize so many amazing nurses. Your support and enthusiasm have made the gala a resounding success, and the funds raised will undoubtedly play a crucial role in advancing our mission and vision.
Thank you to our Gala planning committee led by Dr. Zeh Wellington as Chair. The success of the gala funds our scholarships and we even raised over $1000 extra at the end of the event via our text-to-give campaign to enhance our scholarship fund. We look forward to next year’s gala which will be on December 7th, 2024. Save the date now to ensure you’re there!
I am excited to say that our new board members are commencing the start of their terms in January. Their diverse skills and experiences will undoubtedly enrich our
foundation, and I look forward to working closely with each of them to further our goals.
Looking ahead, we are gearing up for our first board meeting of the calendar year in February. This meeting will set the tone for the months ahead, as we discuss strategic initiatives, plan events, and chart the course for the foundation's future.
I am delighted to inform aspiring nursing professionals that scholarship applications are now open for undergraduate and graduate students until March 15. Visit illinoisnurses.foundation to learn more about the eligibility criteria and application process.
If you’d like to donate to our scholarship funds, please visit our website also where you can make your donation. This is a fantastic opportunity to support the next generation of nurses, so please spread the word.
Additionally, I want to draw your attention to our open grant applications. Whether you are seeking seed grants, small grants, or large grants, the Foundation is here to support your innovative projects. Applications are being reviewed in April, so don't miss the chance to bring your ideas to life.
I am excited about the year ahead and the collective impact we can make as a profession. Your dedication to nursing excellence is truly commendable, and I am honored to serve as your President. Let's continue to work together, support one another, and advance the nursing profession in Illinois.
Wishing you all a prosperous and fulfilling year.
Sincerely,
Amanda Oliver BSN, RN, CCRN, CPST
President Illinois Nurses Foundation
Dear Illinois Nurse Colleagues,
Happy New Year! 2024 is an important year to all the nurses of Illinois, as I begin my term as your President - together - we have the opportunity to advocate and promote patient care for our patients, enhance academia’s strategy to encourage and teach future nurses and uphold the rich traditions of nursing in Illinois. However, I need your help,




your voice, your partnership. ANA-Illinois, with over 5,000 members, has started off the year with a focused strategic plan aimed at promoting and advancing the nursing profession by advocating for legislative changes, helping frontline nurses and nurse leaders confront the pressures we are facing related to workforce shortages, unprecedented health care worker burnout and financial constraints.
“Nothing has ever been achieved by the person who says, ‘It can’t be done.’”- Eleanor Roosevelt.
This work would not be possible without your unwavering support, the guidance and leadership of the Board of Directors and the notable contributions from our Executive Director, Dr. Susan Swart, EdD, MS, RN, CAE.
Allow me to once again introduce our Board of Directors who have the courage to lead while promoting and improving the nursing profession in Illinois:
• Dr. Monique Reed PhD, MS, RN, Vice President
• Gloria E. Barrera MSN, RN, PEL-CSN, Secretary
• Dr. Jeannine Haberman DNP, MBA, RN, CNE, Treasurer,
• Samuel Davis Jr, MHA, RN, CNO, Director
• Dr. Stephanie Mendoza DNP, MSN, RNC-OB, C-EFM, Director
• Armando Valdez Martinez MSN, RN, MEDSURG-BC, CMSRN, NE-BC, CNML. Director
• Dr Hannah Shufeldt, DNP, MSHCM, BSN, RN Director- Recent Graduate
• Diana Ortega BSN, RN, Director.
I am proud of our combined achievements including encouraging legislative changes, developing further education opportunities, and making a positive impact for our patients. Also, I am equally proud (and enthusiastic) for our future. Please let me reinforce that our work is not done. With your help and collaboration, we have the opportunity to shape the future for our nursing profession in Illinois and beyond, and for that I am very excited, energized, and focused.
Thank you for your partnership,
Dr. W. Zeh Wellington, DNP, RN, NE-BC
President of the American Nurses Association (ANA)Illinois
INF Board of Directors
Officers
Amanda Oliver, BSN, RN, CCRN, CPST President
Brandon Hauer, MSN, RN Vice President
Karen Egenes, EdD, RN Treasurer
Directors
Maureen Shekleton, PhD, RN, DPNAP, FAAN
Linda Olson, PhD, RN, NEA-BC
Amanda Oliver, BSN, RN, CCRN
ANA-Illinois Board Rep
Susana Gonzalez, MHA, MSN, RN, CNML
Jeannine Haberman DNP, MBA, RN, CNE
Zeh Wellington, DNP, MSN, RN, NE-BC

ANA-Illinois Board of Directors
Officers
W. Zeh Wellington DNP, MSN, RN, NE-BC President
Monique Reed, PhD, MS, RN Vice President
Jeannine Haberman, DNP MBA, RN, CNE Treasurer
Gloria E. Barrera MSN, RN, PEL-CSN Secretary
Directors
Samuel Davis Jr MHA, RN, CNOR
Armando Valdez Martinez Jr. MSN, RN, MEDSURG-BC, CMSRN
Diana Ortega BSN, RN
Hannah Shufeldt MSHCM, BSN, RN
Stephanie Mendoza DNP, MSN, RNC-OB, C-EFM
Editorial Committee
Chief Editor
Lisa Anderson-Shaw, DrPH, MA, MSN
Members
Cheryl Anema PhD, RN
Deborah S. Adelman, PhD, RN, NE-BC
Linda Anders, MBA, MSN, RN
Ellen Bollino MSN, RN, ED, CEN
Nancy Brent, RN, MS, JD
Pamela DiVito-Thomas PhD, RN
Amanda Hannan MSN, RN
Irene McCarron, MSN, RN, NPD-BC
Linda Olson, PhD, RN, NEA-BC
Executive Director
Susan Y. Swart, EdD, MS, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
Article Submission
• Subject to editing by the INF Executive Director & Editorial Committee
• Electronic submissions ONLY as an attachment (word document preferred)
• Email: syswart@ana-illinois.org
• Subject Line: Nursing Voice Submission: Name of the article
• Must include the name of the author and a title.
• INF reserves the right to pull or edit any article / news submission for space and availability and/or deadlines
• If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted.
• INF does not accept monetary payment for articles.
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: syswart@ana-illinois.org
Article Submission Dates (submissions by end of the business day) January 1st, April 1st, July 1st, October 1st
Advertising: for advertising rates and information please contact Health eCareers, HEC_Nursing_Info@healthecareers.com
ANA-Illinois and Health eCareers reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.
Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. ANA-Illinois and Health eCareers shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations.

In Honor Donations
Shannon Clark
Betty Mushynski
Cheryl Anema
Liz Aquino
Jodi Bacon
Analie Elizalde
Daniel Fraczkowski
Nancy Garcia
Teresita Giatan
Susana Gonzalez
Brandon Hauer
Lisa Hernandez
Jenna Jones
Gerri Kaye
Stephanie Mendoza
Betty Mushynski
Shannon Niemi
April Odom
Amanda Oliver
Araceli Orozco
Mary Pedersen
Jedidiah Pedersen
Monique Reed
Jennifer Sandoval
Anne-Marie Springer
Susan Swart
Ashley Whitlatch
Memorial Donations
Adrienne Ozlowski
Anne MacKay
Ben Paterik
Bill O'Sullivan
Carmen Lydia Alvarez
Catherine Lagapa Hartmann
Charles Chesley Woodcock
Cindy Dejus
Danelle Kelly
Darla Wilson Bahr
Eleanor K Mays
Gloria Veliz
Helena Sibilano
Jennifer Ann Thomas
Josephine "Jo" Hott
Kenny Schwerman
Lawrence Minute
Nancy Bosco
Nancy Stork
Patricia A Tanner RN CCRN
Regina Martin, RN, BSN
Rita Phillips

The American Nurses Association - Illinois (ANA-Illinois) is proud to announce that registration is open for “Student Nurse Political Action Day 2024: There is no healthcare without NURSES.”, to be held on April 16, 2024, in Springfield.
Each year, Student Nurse Political Action Day brings together hundreds of nursing students from across the state in Illinois’ capitol for a day of learning, networking, and advocacy. We are excited to gather in Springfield again this year.
Our 2024 event will:
• spark discussion, encourage learning, and foster connection.
• deliver relevant and timely content for the current state of nursing in Illinois.
• energize and fuel the growth of future nurse leaders!
The event is $35 to attend and open to student nurses of all ages.
KEYNOTE Presented by: Marcus D. Henderson MSN, RN
Practice, Education and Administration
Please take a moment today to nominate a nurse deserving of recognition for the work they do.
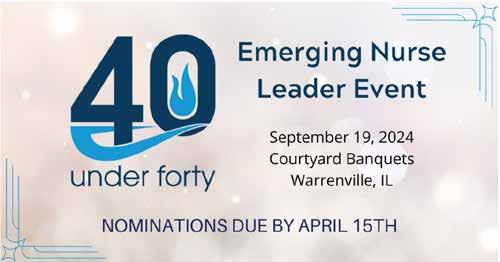
The Illinois Nurses Foundation is accepting nominations for the 10th Annual 40 Under 40 Emerging Nurse Leader Awards. The awards will recognize 40 Illinois RNs younger than 40 who positively represent their profession by participating in the community as well as professional organizations. Nominations are due April 15, 2024.
Winners will be chosen by their peers based on the following criteria: Positively represent the nursing profession by actively participating in the community and/or a professional organization.
The award is designed to recognized nurses in Illinois who demonstrate exemplary professional practice along with community engagement and/or advocacy on behalf of the profession and those we serve.
Awards will be presented on September 19, 2024.
Nominate someone today - https://portal4nurses.com/awards/inf/forty-under-forty

Marcus D. Henderson, MSN, RN is a PhD Candidate at the Johns Hopkins University School of Nursing and Doctoral Fellow in the SAMHSA Minority Fellowship Program at the American Nurses Association. Mr. Henderson is a dynamic speaker, leader, and psychiatric nurse with professional experience working in community-based, inpatient psychiatric, and academic settings. Mr. Henderson holds various local, state, and national leadership roles, including inaugural member of the National Commission to Address Racism in Nursing and the National Chairman of HOSA-Future Health Professionals. Mr. Henderson previously served as a member of the American Nurses Association Board of Directors and is a co-author of The Future of Nursing 20202030: Charting a Path to Achieve Health Equity report. Mr. Henderson received a BSN and MSN in Health Leadership from the University of Pennsylvania School of Nursing. He also holds a certificate in Health Care Innovation from the Perelman School of Medicine. For more information or to register visit https://nurseempowerment.net/SNPAD2024

For these reasons, Dr. Monique Reed was nominated for the Nurse of the Year Award.
This year, the INF Board of Directors awarded Dr. Maureen Sheckleton the inaugural Lifetime Achievement Award.

Dr. Maureen Sheckleton
Dr. Maureen Sheckleton has devoted her career to shaping the landscape of healthcare in Illinois, demonstrating a deep commitment to nursing leadership and education. In the late seventies, she embarked on her journey at Lewis University, where she, alongside Dr. Sharon Firlit-Zandel, designated and developed the RN completion program. As curriculum and accreditation coordinator, she secured the initial accreditation of the BSN program, laying the foundation for her enduring impact on nursing education.
Dr. Sheckleton's leadership extends across numerous prestigious nursing organizations. Her service in elected and appointed positions within the American Nurses Association (ANA), Illinois Nurses Association (INA), and Illinois Nurses Foundation (INF) reflects her dedication to advancing the nursing profession. As the founding president of the Illinois Nurses Foundation, INA President, 2nd Vice President, and Board member, she played pivotal roles in shaping nursing policy, practice, and philanthropy.
Dr. Maureen Sheckleton's influence on nursing education, practice, and policy has left an indelible mark on the profession. Her courage, evidence-based advocacy, and mentorship have empowered countless nurses to provide safe and quality care. Her legacy is not only in her impressive list of achievements but also in the thriving careers of those she has guided and inspired. She has served the Illinois Nurses Foundation for 22 years. She has served as a historian, mentor, educator, and friend to many. Dr. Shekelton has decided to step down from the INF Board of Directors at the end of this year to focus on traveling and her work in her community with various other organizations.
The INF strives to make this event a MUST ATTEND for all those in the nursing profession and its supporters. A very special thank you to each of our major sponsors, many donors, and the volunteers who worked to make this event a success. Thank you for all that you do to support Illinois Nurses Foundation!


We would like to recognize and thank the following donors who were instrumental in helping us achieve our goals in 2023. Because of their general support we gave away over $12,000 in scholarships and awarded $10,000 in grants through our grant program.
Oluwakemi Adeyemi
Lisa Anderson-Shaw
Cheryl Anema
Liz Ann
Elizabeth Aquino
Jordan Ashley
Dean Baron
Gloria Barrera
Steve Barrett
Jackie Barrett
Kate Barrett
Swati Bavisi
Eric Bergman
Elizabeth Bernanek
Nolan Bernicky
Becca Bigelow
Kathryn Booth
Rebecca Boston
Melissa Breth
Karena Brown
Andrea Buechel
Bridget Buechel
Tiffany Buford
Tarsis Buitrago Garcia
Dana Campbell
Meghan Carlson
Timothy Carrigan
Chad Carroll
Jie Chen
Susan Clark
Yalanda Comeaux
Yalanda Comeaux
Lisa Conley
Toby Connoyer
Lisa Coy
Stephanie Crawford
Sherri Crumley
Jan Daniels
Mackenzie Daniels
Sam Davis
Katherine de los Trinos-
Ocampo
Pam Di Vito- Thomas
Danuta Dodson
Kyle Doubrava
Ethel Doyle
Amy Driscoll
Latanya Dunn
Karla Echeverria
Karen Egenes
Eliseo Flores
Sarah Foggy
Dan Fraczkowski
Lou Freckman
Alani Frederick
Wilfrido Fuentes Aviles
Betty Gammon
Rani Ganesan
Leticia Garcia
Nancy Garcia
Cynthia Gonzalez
Susana Gonzalez
Susana Gonzalez
Ernest Grant
Anne-Marie Guerrier
Jeannine Haberman
Julie Hager
Mary Ellen Hand
Elaine Hardy
Joe & Nancy Harmon
Geneva Harris
Laresse Harris
Brandon Hauer
Colleen Haynes
Melissa Herlihy
Hannah Holmes
Kevin Hunt
Mehrun Hussain
Linda Irle
Evangeline Jackson
David Jones
Krista Jones
Jasmine Jones
Crystal Jordan
Brittany Judge
KATIE KEAN
Jenita Keaton
Jackie Kelley Kyonghui Kim
Yvette Kimble
Laurinta Kisielyte
Shannon Kissinger
Anne Kowalczyk
Karen Krutul
Megan Kupferschmid
Annie Lally
Tonkya Lemons
Faye Lewis
Katherine lluen-Nunez
Ruby lomeli
Jennifer Luer
Roy Maca
Jessica Madrigal
Sandra Manna
Erica McNerney
Carmel Medard
Socorro Mendoza
Stephanie Mendoza
Julio Mendoza
Jennifer Mensik Kennedy
Margaret Miller
Cynthia Mitchell

Lynn Mohr
Pamela Moore
Heather Moretti
Colleen Morley
Colleen Morley
Betsy Murphy
Peggy Norton-Rosko
Dr.Joy Nwankpa
Anne O'Boye
Leanne O'Brien
Esmeralda Ochoa
April Odom
Emmanuel Olaifa
Amanda Oliver Araceli Orozco
Charles Orth
Ann O'Sullivan
Jill Otruk
Tammy Padula
Rachel Powers
Jessica Prothe
Christine Radtke
Kaylea Reeves
Krystian Reformado
Lovey Reynolds
Joni Rials
Katie Riley
Eleanor Rivera
Linda Roberts
Christina Rodriguez
Karly Sachs
Haley Sachs
Juan Sanchez
Rocio Sanchez
Jennifer Sandoval
Roshni Shah
Mona Shattell
Maureen Shekleton
Jakw Simmons
Olivia Stanger
Susan Swart
Crista Theis
Karen Thomas
Chad Thompson
Jill Trzaska
Lisa Trzaska
L Nicole Tucker
Diane Vander Ploeg
Leta Vega
Elyssia Venson
Connie Vincent
Cheryl Vines-Crooks
Sierra Weathers
Zeh Wellington
Joan Widmer
Patricia Wienski
Shrese Williams
Drucilla Williams
Vicki K Young
Gary Zidek
Stephanie Zidek
Loyola University Medical Center
Smits Funeral Homes, LTD.
Rush University College of Nursing
Illinois League for Nursing InstaNurse Staffing Solutions Corp
National Association of Hispanic Nurses-Illinois
Chapter
Lewis University
Philippine Nurses Association of Illinois
Leon J Witkowski Jr DDS, Ltd
James Bobby Currin & Sons Inc
Walter W. Schultz Agency, Inc.
Sovereign Care Services
Advocate Health Care
ANA-Illinois
Saint Xavier University
Serenity One Hospice and Palliative Care
ASI/NE Healthcare Services, Inc.
Advantage International
Stepping Stone Financial Old National Bancorp Illinois Organization of Nurse Leaders Rush University Medical Center
Loyola Medicine
Northern Illinois University
School of Nursing UIC College of Nursing
Advocate Childrens Hospital
Northwestern Medicine Canning Thoracic Institute
Advocate Children's Hospital
Advocate Aurora Health
Northwestern Medicine
Edward-Elmhurst Health Illinois Association of School Nurses
















NANCY J. BRENT, MS, JD RN
QUESTION

Nancy J. Brent, MS, JD, RN
A nursing faculty member submitted a question about her school of nursing’s adopted policies and procedures governing students. She wants to apply them consistently and fairly but is worried about liability if a nursing student alleges a particular policy or procedure is unfair, unjust, or raises other legal concerns. The faculty member wonders about what components should be included in nursing education policies and procedures.
RESPONSE
If you hold a faculty position in a nursing education program, you know you are not immune to lawsuits by nursing students. Although the specifics of such suits are beyond the scope of this Practice Corner, the legal bases for reported lawsuits include defamation, negligent teaching, discrimination, and dismissals from a nursing school’s program.
Policies and procedures applicable to students during their student experience can form the basis for many of these allegations. Specific student allegations can include the policies and procedures being unfair, unclear, not in writing, changing regularly, or in violation of their constitutional (public academic institutions) or contractual (private academic institutions) rights.
Specific policies and procedures that may be utilized by students include those applicable to course and clinical syllabi, attendance policies, grading policies (both for
academic and course work), ethics policies, misconduct policies, plagiarism policies, and impaired student policies.
One way in which such suits can be prevented is by well-developed policies and procedures that are founded upon a risk management approach.
The Illinois Nurse Practice Act and its Rules provide some initial guidance on the development and utilization of school policies and procedures. They must first and foremost be developed by nursing faculty. In addition, they must be in writing, be consistent with the overall policies and procedures of the institution in which the program operates and be reviewed by nursing faculty on a regular basis.
Although there are many recommendations for applying adopted policies and procedures in nursing education programs, some can be suggested here. They include:
• Know the Illinois Nurse Practice Act and Rules pertaining to student policies and procedures and your role as a faculty member
• Know what the adopted policies and procedures in your nursing program are and apply them consistently and fairly
• Use disclaimers in student written documents, especially if you teach in a private university or college program, since what a private school states can be seen as a “contract” between the student and the nursing program (e.g., “The faculty reserves the right to change the course syllabus when needed.”)
• Use of well-developed clinical and academic evaluation forms
• Use of well-developed syllabi and other written documents governing student requirements
Linda L. Olson, PhD, RN, NEA-BC, FAAN
• Always inform students of applicable adopted policies and procedures, both verbally and in writing (e.g., syllabus)
• Use adopted forms for student notices governing grading, discipline, or other situations applicable to a student’s status in the nursing program
• Utilize resources available within your academic institution (e.g., tutoring availability, counseling services) consistent with adopted policies and procedures
• If holding a faculty position in a public nursing education program, apply students’ constitutional rights (e.g., due process)
• Exercise your faculty rights to evaluate students and make reasoned judgments about student performance, both academically and clinically
• Don’t answer/respond to a student question concerning a policy or procedure “on the fly”. Reserve the right to get back to the student after reviewing the applicable policy and procedure
• Be accessible to students
It is important to remember that generally speaking, courts are reluctant to overturn decisions by faculty when they make academic and disciplinary decisions concerning students. The courts see faculty as experts when making such decisions. Unless those decisions are arbitrary, capricious, discriminatory, or in violation of adopted policies and procedures, the determinations are most often upheld.
This information is for educational purposes only and is not to be taken as specific legal or any other advice by the reader. If legal or other advice is needed, the reader is encouraged to seek such advice from a nurse attorney, attorney or other professional.

Linda Olson PhD, RN, NEA-BC
Artificial Intelligence (AI) is a term first coined by emeritus Stanford Professor John McCarthy in 1955 as “the science and engineering of making intelligent machines” (Stanford University, 2020 p.1). It includes machine learning, robotics, various other computer technologies, and the use of algorithms as tools to aide in decisionmaking. Although the current and future uses of AI are compelling, there are numerous ethical implications and challenges for nursing practice, education, administration, research, and regulation. The Code of Ethics for Nurses with Interpretive Statements (2015), in Provision 4.2 states that “nurses in all roles are accountable for decisions made and actions taken in the course of nursing practice. Systems and technologies that assist in clinical practice are adjunct to, not replacements for, the nurse’s knowledge and skill (ANA 2015, p. 15). In clinical settings, nurses use AI technologies to address complex health care issues and to support their care. AI can reduce the time used in documentation on the electronic health record, and predict the likelihood of patient falls and pressure sores. In nursing administration, AI applications are used in nurse staffing and in nursing education, to predict student attrition, program completion, and graduation (O’Connor, 2023). It plays an important role in analyzing health care data to improve diagnosis and outcomes. A challenge to use of AI is related to privacy, security, and safety, both for patients
and for students. Provision 3.1 addresses the “protection of the rights of privacy and confidentiality,” especially with respect to access to and disclosure of personal information (ANA, 2015, p. 9).
While ensuring that AI technologies support healthcare professionals, patients, researchers and scientists, the World Health Organization (WHO) identified the need for appropriate regulation and policy. The WHO called for examining the risks to people’s health when using AI technology (2023).
In its position statement on The ethical use of artificial intelligence in nursing practice, the ANA Center for Ethics and Human Rights identified the importance of nurses being informed about AI and involved in its’ development and appropriate integration into nursing practice (2022).
Nurses in all roles and settings need to ensure that use of AI is based on evidence that justifies its implementation into clinical practice and education. Nurse researchers and administrators must create an environment and structures that promote the benefits of AI and develop best practices. It is important that AI technologies are safe and protect privacy and confidentiality. Other ethics challenges include the potential for bias and discrimination and errors that can lead to incorrect decisions. It is important that AI systems be transparent to allow for being able to explain the results.
The development of AI technologies and their possibilities for problem-solving, decision-making, and learning is accelerating on a daily basis. The introduction of the ChatGPT generative computer tool that creates automatic written documents and has the ability to evaluate written documents provides opportunities for its appropriate and innovative uses in nursing education. At the same time, it results in concerns about potential plagiarism and impacts related to intellectual property (Parker, et.al., 2023; Schneidereith, 2023).
Now is the time for nurses to be knowledgeable about and involved in the development, design, implementation, and regulation of AI technologies. and their potential ethical impacts. To use AI appropriately, nurses need to assure that it supports the core values and ethical obligations of the profession (ANA, 2022).
References
American Nurses Association (2015). Code of Ethics for Nurses with Interpretive Statements. Silver Spring, MD: NursesBooks.org
American Nurses Association (2022). The Ethical Use of Artificial Intelligence in Nursing Practice. Position Statement by ANA Center for Ethics and Human Rights.
O’Connor, S., & Rose, L. (2023). Realizing the benefits of Artificial Intelligence for nursing practice. Nursing Times (online):118:10. https://www.nursingtimes.net/clinicalarchive/healthcare-it/realising-the-benefits-of-artificialintelligence-for-nursing-practice-18-09-2023
Parker, J.I., Becker, K., & Catherine, C. (2023). ChatGPT for Automated Writing Evaluation in Scholarly Writing Instruction. Journal of Nursing Education 62(12): 721-727. Schneidereith, T.A., & Thibault, J. (2023). The Basics of Artificial Intelligence in Nursing: Fundamentals and Recommendations for Educators. Journal of Nursing Education, 62(12): 716-720.
Stanford University Human-Centered Artificial Intelligence (2020). Artificial Intelligence Definitions. Retrieved: https://hai.stanford.edu/sites/default/files/2020-09/AIDefinitionsHAI.pdf
World Health Organization (2023). WHO calls for safe and ethical AI for health. https://www.who.int/news/item/1605-2023-who-calls-for-safe-and-ethical-ai-for-health#
Deborah S. Adelman, PhD, RN, NE-BC
Laura Kay Wood, DNP, RN, CMCN Professors, Graduate Nursing Program
Purdue University Global
“What! Are you kidding me? Pay to publish our accepted manuscript?” was how one of us reacted to a coresearcher telling them that the accepted manuscript would cost $600 to publish, something we had not been told when we submitted it and it was initially accepted. As we knew, there are predatory journals that snare authors this way. What we did not know was that legitimate international journals do not accept ads and have to charge authors to publish. We learned this after a nasty reply to the journal editor that we did not need to pay to be published and we wanted our copyright back. We did get the manuscript published elsewhere in the end, but with egg on our face.
The profession of nursing embraces the pursuit of scholarly writing, a standard of incorporating evidence and addressing bias, in a clear and concise manner to facilitate communication and critical thinking (Ayala et al., 2022). The goal of scholarship and scholarly writing promotes the dissemination of knowledge ensuring the continuity of quality patient care and effective information sharing among healthcare providers. The development of nursing as a discipline depends on this accurate and complete dissemination of information to use in practice, information and knowledge that are found within a reputable academic publishing community, considered trustworthy as the result of a vetted and verified best publication process. For a researcher or academic embracing publication, it is important to recognize what identifies as a legitimate journal to avoid submission to a predatory journal which can impact the legitimacy of their work, compromise its usefulness, and lead to the further scrutiny of past publications (Turale, 2023) as well as hinder future publication.
The issue of predatory journals is not a new one. In 2015, Shen and Bjork, in a seminal systematic review of the literature, concluded that 8,000 predatory journals collectively publish 420,000 papers every year, nearly a fifth of the scientific community's annual output of 2.5 million papers. The rise in the number of articles in predatory journals since then has been astounding, going from 53,000 to 420,000 between 2010 and 2014 representing an almost 800% increase. If there were 8,000 predatory journals in 2014, it is currently estimated at over 17,000+ predatory academic journals (Cabells, n.d.).
Predatory journals are deceptive, fraudulent, scientific-in-name-only journals marketed to authors through exploitative and unethical strategies and techniques which ultimately impact the validity of research results and the dissemination of knowledge, innovation, and best practice in nursing or any field. At the present time, predatory journals are considered one of the “greatest threats to science” (Duc et al., 2020, p. 318) affecting both novice and respectable researchers and authors alike who are either not aware they exist or in a hurry to be published. It is imperative that nurses understand how these journals work and how to identify them.
Trying to help all academics and students, Beall, a librarian at the University of Colorado in Denver, created a blog which listed predatory publishers between 2012 and 2019 (Elmore & Weston, 2020). Since the advent of Beall’s website, more tools and websites in support of the identification of predatory journals have been constructed including several by nursing journal publishers. Today, predatory journals can be found in reputable websites such as PubMed, PubMed Central, MEDLINE, and Scopus (Duc et al., 2020) making it even harder to identify whether a journal is legit or not.


The impact of predatory journals is a serious hazard to scientific research and not only negatively affects a researcher’s and author’s credibility, but also may impact an author’s or researcher’s choice of design and methodology when content is used in a research study or article that is discovered in a predatory journal that has published fabricated results or disseminated “knowledge” that has not been vetted through peer reviewers. Even genuine published work when presented in a predatory journal may render it useless to the scholarly community and lost to an audience dedicated to the dissemination and integration of best evidence-based practice (Duc et al., 2020; Elmore & Weston, 2020; Turale, 2023) because of the doubt a predatory journal creates about the legitimacy of the content.
A predatory journal’s main goal is profit, not scholarship, no matter the means or the impact upon scientific progression or a researcher’s or author’s reputation. Revenue is obtained through sending unsolicited emails requesting editorial board or journal reviewer participation as well as requests for manuscripts for upcoming issues or conferences. Using the names and reputations of these board members and peer reviewers can fool the prospective author or researcher into believing the journal is legitimate. The objective is to deceive with false claims and fast acceptance for publication for a fee without providing robust, if any, peer-review or editorial services. There is no check of any of the methodological elements used or statistical analysis of research results in the manuscript (Duc et al., 2020; Elmore & Weston, 2020; Turale, 2023).
It is important to thoroughly investigate a journal that is new to the prospective researcher or author and not simply rely on the testimonial of the journal editor or website. There are several ways to identify a predatory journal. These include: evaluating a journal’s manuscript

If you’re a nurse looking to implement change in your workplace, our doctorate in nursing is the program for you. Our experienced faculty provide one-on-one mentorship and prepare collaborative, compassionate nurses with in-demand leadership skills.
Learn more at northpark.edu/songradprograms
submission practices/author guidelines for depth and clear instructions, reviewing archived articles in past issues of the journal, and evaluating the journal’s website (Duc et al., 2020). One can also look for the impact factor (IF) of the journal which measures how many citations an article has over a year in other journals as well as the original journal. Clarivate Analytics, a company that collects bibliometrics and scientometrics, publishes the IF for any journal that is listed in the Science Citation Index Expanded® (SCIE) and Social Sciences Citation Index® (SSCI). Generally, an IF of at least 1 to 3 is considered good and indicates a trustworthy journal (The Board, 2016).
Journal manuscript submission features that should be considered questionable can be noted in their author guidelines and include such things as missing withdrawal or retraction policies, lack of information pertaining to digital preservation, submission requests that are sent through a personal email account, an unclear series of steps during the manuscript writing process, quick peer review processes missing constructive feedback, and/or article processing charges (APCs) that are unclear or introduced to the researcher after the manuscript has been accepted for publication and cannot be found on the submission website (Duc et al., 2020).
Predatory concerns that can be identified in archived journals are perceptible in the presence of copyright violations, the lack of implementation software to address plagiarism, journal titles and published articles not connected to the aims and scope outlined within the journal, digital object identifiers (dois) that cannot be confirmed within https://www.doi.org, and the International Standard Serial Number (ISSN) within the Directory of Open Access Journals (DOAJ) cannot be validated. Other issues include identification of multiple linguistic and grammatical typos, as well as front page logos and images that are blurry or uneven (Duc et al., 2020). Journal website predatory detection features are noticeable when a logo of the Committee on Publication Ethics (COPE) is present but no such affiliation exists, there is deliberate misrepresentation, there are unqualified editorial board members, or there are advertisements to publisher-sponsored conferences are either mismatched or not associated with academia. Other clues to watch for include spelling and grammatical errors, indexing reported as being by reputable databases appears fabricated, and fabricated lists of published articles claiming to have a high impact factor are listed on the publisher’s website (Duc et al., 2020).
Combating the prevalence and impact of predatory journals starts with the awareness that predatory journals do indeed exist and not every request to publish in an unknown journal is something to be excited about. Prior to a manuscript submission, it is the responsibility of the author and researcher who must decide whether a journal is trustworthy and should take the time to learn how to identify a predatory journal and scrutinize a journal’s website (The InterAcademy Partnership, 2022). Being vigilant, practicing due diligence to minimize risk, participation in robust academic and publishing training and awareness programs, the incorporation of resources such as the assistance of a librarian who has the training and resources to identify predatory journals, and consultation with researchers who have a well-established publishing history all provide an approach toward avoiding manuscript submissions to predatory journals (The InterAcademy Partnership, 2022; Turale, 2023). The following table features characteristics of predatory journals (Duc et al., 2020).
Table Characteristics of a Predatory Journal
Locate Journal Read about Editorial Process Read the Publication Process
Missing from traditional literature databases such as PubMed, PsycINFO, and CINAHL.
Displayed on unsecured and unprofessional websites.
Board members are not experts in the journal topics covered within the article.
Subject matter topics are quite wide. The peer review process may be very short, poor, or worse, nonexistent.
Find publication costs and processing charges misleading.
Low author submission fees.
Low author submission fees.
Accelerated publication process. The extremely high acceptance rate of journal submissions.
Inconsistencies identified in the publication processing.
Read an Edition of the Journal or an Article
Errors in the article titles.
Errors in the journal descriptions.
Conclusion
In the end, one should not take shortcuts to speed up publishing. The processes have been honed over decades to ensure that predatory practices that lack transparency and undermine public trust in and research integrity of the author and researcher do not result in ruined reputations and incorrect data and information are not disseminated (The InterAcademy Partnership, 2022). It takes time for a reputable journal to go through the peer review process with subject matter experts validating that what is published is credible, reliable, and valid.
References
Ayala, F., DeBoard, E., Waldrop, J., Pereira, K., Oermann, M. H., & Silva, S, G. (2022). Dissemination of doctor of nursing practice project findings: Benefits and challenges associated with publishing in healthcare journals. Nursing Outlook, 70, 846-855.nc. https:// doi.org/10.1016/j.outlook.2022.07.011
The Board of Trustees of the University of Illinois. (2016). Measuring your impact: Impact factor, citation analysis, and other metrics: Journal Impact Factor (IF). https://researchguides.uic. edu/if/impact#:~:text=About%20Journal%20Impact&text=The%20impact%20factor%20 (IF)%20is,times%20its%20articles%20are%20cited
Cabells. (n.d.). What is journalytics? https://learn.cabells.com/external/manual/journalyticsacademic/article/what-is-journalytics?p=45bf0b37eb068f380076713fd7aa06de5f2ec699708e 4e23b6df864634f8167a
Duc, N. M., Hiep, D. V., Thong, P. M., Zunic, L, Zildzic, M., Donev, D., Jankovic, S. M., Hozo, I, & Masic, I. (2020). Predatory open access journals are indexed in reputable databases: A revising issue or an unsolved problem. Review/Medical Archives, 74 (4), 318-322. https://doi. org/10.5455/medarh.2020.74.318-322
Elmore, S. A., & Weston, E. H. (2020). Predatory journals: What they are and how to avoid them. Toxicologic Pathology, 48 (4), 607-610. https://doi.org/10.1177/0192623320920209
The InterAcademy Partnership. (2022, March). Combating predatory academic journals and conferences. (Summary Report in English). https://www.interacademies.org/publication/ predatory-practices-summary-English
Leonard, M., Stapleton, S., Collins, P., Selfe, T. K., & Cataldo, T. (2021). Ten simple rules for avoiding predatory publishing scams. PLoS Computational Biology, 17 (9), e1009377. https:// doi.org/10.1371/journal.pcbi.1009377
There are some pointers to be aware of related to “phishing expeditions” that predatory journal editors can take to lure one in. One of the biggest errors is to search on one’s own and land on their website. These sites have malware that can garner information about ISP and email addresses. This information may be used to send emails asking one to attend conferences they sponsor or to publish in their journal. Most conference sponsors will publish what is called a symposium, a compilation of all presentations in the conference. Presenters receive a free copy of the symposium. However, with a predatory journal sponsorship, the presenters are often asked for a fee to guarantee publication of their presentations in the symposium or in the predatory journal. The presenter may be asked for a fee to obtain a copy of the symposium. None of these are how a legitimate conference sponsor would proceed. Be aware that this may vary with international conferences, because they do require a fee due to not receiving paid advertising and their costs need to be covered somehow (Leonard et al., 2021).

At Lewis our graduate nursing students are living with intentionality, aspiring to make a difference wherever they are. Equipped with leading-edge knowledge and skills, you’ll continue to see the world in new ways
HIGHLIGHTS
Offered in multiple formats designed for the working nurse Programs can be taken parttime for added flexibility
Turale, S. (2023). Protect your scientific reputation: Beware of predatory journals! Nursing Practice Today, 10 (2), 81-83. https://doi.org/10.18502/npt.v10i2.12828 (815) 836-5610
Admission starts throughout the year –no GRE required Faculty are doctorallyprepared practitioners Employer partnerships provide tuition discounts
grad@lewisu.edu lewisu.edu/nursing
DNP – Leadership MSN/MBA MSN Healthcare Systems Leadership Nursing Education
• Family Nurse Practitioner (FNP)
Adult Gerontology Primary Care Nurse Practitioner (AGPCNP)
Adult Gerontology Acute Care Nurse Practitioner (AGACNP) Psychiatric Mental Health Nurse Practitioner (PMHNP) School Nurse POST-MASTER’S CERTIFICATES OF ADVANCED STUDY (all Nurse Practitioner tracks) POST-MASTER’S NON-DEGREE PROGRAMS
(Nursing Education and Healthcare Systems Leadership)
Jennifer DeMay, RN ( jenstedman45@gmail.com)
Jesse Scala, RN ( jessejscala@gmail.com)
Felicia Napolitano, RN (felicianapolitano9411@gmail.com)
Instructor: Jie Chen, PhD, RN ( jchen2@niu.edu)
Graduate level nursing students at Northern Illinois University conducted a literature review to analyze the effectiveness of various interventions on the management of polypharmacy in adults aged 65 and older. Polypharmacy is generally defined as the concurrent use of five or more medications daily (Masnoon et al., 2017) and is a growing concern in healthcare, particularly among older adults aged 65 and older. This issue is of significant importance, given that approximately 14% of the United States population falls within this age group and over one-third of prescription medication spending is attributed to this demographic (Varghese et al., 2022).
The consequences of polypharmacy can be severe, leading to adverse drug reactions, increased healthcare costs, reduced quality of life, and increased mortality (Davies et al., 2020). Patients often see multiple providers or specialists who may prescribe new medications during visits. New medications can also be prescribed to treat an adverse medication reaction disguised as a new medical condition, leading to a prescribing cascade. Polypharmacy is also related to unaddressed barriers and nonadherence due to side effects, financial burden, and time consumption that can lead to acute exacerbations of disease states, decreasing quality of life, and increasing the likelihood of falls and associated injuries (Xue et al., 2021). Nurses at all levels play a crucial role in caring for older adults experiencing polypharmacy.
An assessment of scholarly articles published between 2016 and 2023 relating to polypharmacy in the older adult population of the United States was conducted primarily using CINAHL and PubMed databases. Eight primary research articles were ultimately selected for further review. The majority of available research was noted to be in the primary care setting with communitydwelling older adults.
Inappropriate prescribing and successful medication reduction without compromising outcomes were noted to some degree in all studies. Sustainability of deprescribing was a concern, as some studies showed deprescribing outcomes were short lived. The use of electronic prescribing tools offered support for clinical decisions in advanced practice. Purposeful collaboration between providers, pharmacists, and patient caregivers also showed promising results. Using written education in the form of pamphlets or brochures was noted to motivate patients and families to review their own medications, and providing information in a repeated fashion improved outcomes and facilitated more involvement for cognitively impaired older adults. The studies emphasize the importance of facilitating discussions surrounding medication with patients and families in clinical practice, addressing patient barriers to adherence, and ensuring medication profiles align with the patient's goals of care. Awareness of the phenomenon, vigilance in prescribing, and providing adequate time to communicate with patients and their families regarding their medications are all methods that can be used to lower the risk of the negative effects associated with the complex issue of polypharmacy.



You rose to meet the challenges of the last few years. You’ve been through more than most people can imagine. And you’ve got a lot more to give.
Do more for yourself, to do more for others. That’s where Oak Point University comes in.
We offer:
• Nurse Educator — MSN
• Family Nurse Practitioner (FNP) — MSN
• Adult-Gerontology Primary Care NP (AGPCNP) — MSN
• Adult-Gerontology Acute Care NP (AGACNP) — MSN, certificate
• Psychiatric-Mental Health NP (PMHNP) — MSN, certificate
• Doctor of Nursing Practice with Urban Health/Policy focus
learn more at oakpoint.edu/power-forward

Carolyn Dickens PhD APRN ACNP-BC FAANP
Lauren Diegel-Vacek DNP APRN FNP-BC FAANP
The nursing profession is experiencing a workforce crisis that took root long before the COVID-19 pandemic. A national survey of approximately 50,000 nurses in 2022 by the Journal of Professional Regulation revealed that half of respondents reported feeling, “emotionally drained”, “at the end of their rope” and “burned out” several times a week (Martin, et al, 2023). Drivers of burnout include nurse-to-nurse bullying and the rising incidence of verbal abuse and physical violence from patients and families directed toward nurses (Ouying, 2023 & Craft, et al., 2020). These stressors add to the pressure nurses face to balance a workload of medically complex patients while assuring quality care and patient safety. This confluence of factors has influenced the number of nurses leaving the workforce and may accelerate the national nursing shortage projected to reach crisis levels by 2030 (Auerbach et al., 2022; American Nurses Foundation, 2022; American Association Colleges of Nursing, 2022). One surprising component of the projected shortage is the number of younger nurses planning to exit the nursing workforce within their first five years of employment. Reasons cited by younger nurses for their dissatisfaction include, among other things, the incivility of patients, families, and nurse colleagues (Atashzadeh, et al., 2021). The ANA defines incivility as, “one or more rude, discourteous, or disrespectful actions that may or may not have a negative intent behind them”, (ANA, n.d.). Most nurses don’t report incivility or rudeness experienced at the hands of family or patients due to feeling the behavior is non-reportable or tolerating it is just a reality of the job (Joint Commission, 2021; Townsley, et al., 2023). However, experiencing disrespectful behavior contributes to the development of psychological conditions, including burnout, and can result in patient harm due to the negative impact incivility has on communication and teamwork (Lewis, 2023). Most alarming is the higher risk of suicide among nurses in comparison to other healthcare providers (Olfson, et all, 2023) demonstrating the need for healthcare systems to address nurse burnout and support mental health.
It’s time for nurse leaders in academic and practice settings to collaborate to be the driving force to promote real change. In the academic setting, faculty can change the current trajectory of incivility in nursing education by examining their implicit biases and experiences of incivility with faculty colleagues (Kroning & Annunziato, 2023). Faculty should be models of empathetic and equitable treatment of both their colleagues and their students. Nursing education needs to include content that enables students to identify and mitigate incivility. One example of integration of civility education into a nursing curriculum is a learning module utilizing roleplaying. Students identify and practice constructively addressing conflict and negative behaviors of colleagues, patients and families in a safe environment by implementing the evidence-based strategies they have learned (Clark & Gorton, 2019). Nearly 70% of students who participated in this educational experience reported applying these strategies in their practice. In clinical settings, nurse leaders and unit managers need continuing education focused on developing their leadership skills to manage conflict and implement zero-tolerance policies for incivility (Healthy Workforce Institute, 2024; Kroning & Annunziato, 2023). Empathetic nurse leaders create a culture of support and empowerment for staff nurses that can buffer feelings of powerlessness and burnout (Hall, et al., 2022). Only through the collaboration of nurse leaders across the continuum of academia and practice settings can we effectively address and stop the cycle of incivility in nursing.
References: Civility Crisis in Nursing
American Association Colleges of Nursing. (2022). Nurse shortage fact sheet. October, 2022 https://www. aacnnursing.org/Portals/0/PDFs/Fact-Sheets/NursingShortage-Factsheet.pdf Accessed 1/10/24
American Nurses Association. (n.d.). End Workplace Violence. https://www.nursingworld.org/practice-policy/workenvironment/end-nurse-abuse/ Accessed 1/23/24 American Nurses Foundation. (2022). Pulse on the Nation's Nurses Survey Series: Annual Assessment Survey, November 2022. https://www.nursingworld.org/practice-policy/ work-environment/health-safety/disaster-preparedness/ coronavirus/what-you-need-to-know/annual-survey--thirdyear/ Accessed 1/23/24.
Atashzadeh Shoorideh, F., Moosavi, S., & Balouchi, A. (2021). Incivility toward nurses: A systematic review and metaanalysis. Journal of medical ethics and history of medicine. 14, 15. https://doi.org/10.1 8502/jmehm.v14i15.7670
Auerbach, D., Buerhaus, P., Donelan, K. & Staiger, D. (2022). A Worrisome Drop in the Number of Young Nurses. Health Affairs Forefront, April 13, 2022.DOI: 10.1377/ forefront.20220412.311784 https://www.healthaffairs.org/ content/forefront/worrisome-drop-number-young-nurses Accessed 1/10/24
Clark, C. & Gorton, K. (2019). Cognitive Rehearsal, HeartMath, and Simulation: An Intervention to Build Resilience and Address Incivility. Journal of Nursing Education, 58 (12), 690697.
Craft, J., Schivinski, E. L., & Wright, A. (2020). The Grim Reality of Nursing Incivility. Journal for nurses in professional development, 36 (1), 41–43. https://doi.org/10.1097/ NND.0000000000000599
Hall, V. P., White, K. M., & Morrison, J. (2022). The Influence of Leadership Style and Nurse Empowerment on Burnout. The Nursing Clinics of North America, 57(1), 131–141. https://doi. org/10.1016/j.cnur.2021.11.009
Healthy Workforce Institute (2024). A call to action: Stop Nursing Incivility. https://healthyworkforceinstitute.com/ Accessed 1/15/24
Joint Commission. (2021). Quick safety. Bullying has no place in health care. https://www.jointcommission.org/-/media/tjc/ newsletters/quick-safety-issue-24-june-2016-6-2-21-update. pdf Accessed 1/28/24
Kroning, M., & Annunziato, S. (2023). New strategies to combat workplace incivility and promote joy. Nursing, 53(1), 45–50. https://doi.org/10.1097/01.NURSE.0000891960.69075.73 Lewis C. (2023). The impact of interprofessional incivility on medical performance, service and patient care: a systematic review. Future healthcare journal, 10 (1), 69–77. https://doi. org/10.7861/fhj.2022-0092
Martin, B., Kaminski-Ozturk, N., O'Hara, C., & Smiley, R. (2023). Examining the Impact of the COVID-19 Pandemic on Burnout and Stress Among U.S. Nurses. Journal of nursing regulation, 14 (1), 4–12. https://doi.org/10.1016/S2155-8256(23)00063-7 Ouyang, H. (2023). Stabbed. Kicked. Spit on. Violence in American hospitals is out of control. New York Times. 10/24/23. https://www.nytimes.com/2023/10/24/ opinion/emergency-room-hospitals-violence. html?searchResultPosition=2 Accessed 1/24/24
Olfson, M., Cosgrove, C. M., Wall, M. M., & Blanco, C. (2023). Suicide Risks of Health Care Workers in the US. JAMA, 330 (12), 1161–1166. https://doi.org/10.1001/ jama.2023.15787
Townsley, A., Li-Wang, J., & Katta, R. (2023). When Patient Rudeness Impacts Care: A Review of Incivility in Healthcare. Cureus, 15(6), e40521. https://doi.org/10.7759/cureus.40521
Margaret Miller, MSN, RN, Retired
Monroe County Retired Nurses are ready for Nurse Honor Guard (NHG) to conduct services for local nurses who have passed away. This ceremony will honor the nurse and his or her service and career during a visitation or funeral service. The NHG Committee began work on this project in August 2023, following designs used by others in the state, and were ready to present their completed project to the October 25th membership meeting.
Contacts with three funeral home directors were made explaining the NHG ceremony for deceased nurses and all three were supportive. An information sheet was then developed for the funeral home directors with NHG committee chair and co-chair contact information.
After receiving information from the funeral home, the committee chair or co-chair will contact the family and make arrangements for having the Nurse Honor Guard recognition service.
Two to five volunteer retired nurses will participate in a NHG ceremony. They will wear black slacks, white shirts, and the Nurse Honor Guard sash. A small table will be set up with a few symbolic articles, from a historical point of view, of nursing in the area of the casket, if appropriate. The Nightingale lamp on the table will be lit with a battery candle before the ceremony. Many of the articles being used for the ceremony have been donated from storage of the nurses or by an anonymous donor.
The ceremony itself will take five minutes or less and will consist of a short introduction honoring nursing and the nurse, and an inspirational poem, “She/He Was

There,” will be read. Lastly, a small bell will be rung, while the nurse’s name is read, releasing her/him from their duties. Afterwards, a laminated copy of the poem and a white silk rose will be presented to the family.
The retired nurses are excited to begin this program and twelve members have volunteered to participate in ceremonies. INA member Eileen Berlin served as Chair of the Nurse Honor Guard Committee and INA member Margaret Miller serves as consultant and corresponding secretary of the Monroe County Retired Nurses, which was organized in 2006.


• As required by the Illinois Nurse Practice Act, all nurses shall complete continuing education prior to license renewal. All RNs shall complete 20 hours of approved continuing education per two-year license renewal cycle. All APRNs shall complete 80 hours of approved continuing education in the advanced practice registered nurse’s specialty per two-year license renewal cycle.
• Beginning with the 2024 RN renewal, Illinois RNs who provide health care services to and have direct patient interaction with adults 26 years of age and older will be required to complete a one-hour course in diagnosis, treatment and care of Alzheimer's disease, along with other dementia types. CE Curriculum will involve how to identify and diagnose Alzheimer's, effective communication strategies and management and care planning. This course may count toward the regular CE requirements (Public Act 102-0399, 20 ILCS 2105/2105-365).
• There are new requirements beginning in 2024, including completing 1.0 CE hour implicit bias awareness training. The Division of Professional Regulation (DPR) webpage has implicit bias awareness CE information: https://idfpr.illinois.gov/dpr. html. Implicit bias is a form of bias that occurs automatically and unintentionally, that nevertheless affects judgments, decisions and behaviors.
• The CE requirement for implicit bias awareness training and the CE requirement for sexual harassment prevention training, each 1.0 CE hour, is included in the number of hours already required under the individual Nurse Practice Act and Rules. This does not increase the number of hours required to renew a license, which is 20.0 CE hours. For details, please see the CEU FAQ sheets on the Nursing Workforce Center website: https://nursing.illinois.gov/nursing-licensure/continuing-education.html
• The Illinois Department of Financial and Professional Regulation (IDFPR) is providing renewal assistance for individuals and businesses that are having difficulty with the online renewal process: https://idfpr.illinois.gov/dpr.html. These steps will help licensees better navigate the account matching process on the Department's updated online portal.
• For US residents with an Illinois nurses license, to change your email address, U.S. mailing address or phone number, please click on this link to update the information: https://idfpr.illinois.gov/fpr-applications/licensereprint.html. This form is not for international residents who must download a paper form found on that same page.
• Military families: Members and Spouses who are an active duty member or whose active duty service concluded within the preceding two years before application. In addition to expedited review of your application (30 days), the Department’s dedicated Military Liaison will work with you and your military installation’s military and family support center to help you through the licensing process. Learn more here: https://idfpr.illinois.gov/military.html. You may also email the Military Liaison using this email address: fpr.militarylicense@illinois.gov
• To print your license or download an electronic copy to your phone, just head to the IDFPR website https://idfpr.illinois.gov/fpr-applications/getmylicense/loginprof.html
• The IDFPR “Requirements of an Internationally Educated Nurse” document is available online here: https://idfpr.illinois.gov/content/dam/soi/en/web/idfpr/ renewals/apply/forms/cgfns-02.pdf. Resources on this document include the names of Board of Nursing approved vendors for items required to apply for an Illinois nurse license.
o Information includes that endorsing an active license from another state requires: an application by Endorsement.
o If the state of original licensure required a Credential Evaluation Service (CES) report at the time of original licensure, a (CES) report is not required for the licensure endorsement process.
o An English equivalency test is not required as long as the nurse applying for endorsement took and passed the NCLEX® licensure examination.
• On the IDFPR Nurses web page, there is a list of all 138 Illinois Board of Nursing approved RN/Registered Nurse and LPN/Licensed Practical Nurse pre-licensure nursing education programs: https://idfpr.illinois.gov/content/dam/soi/en/web/ idfpr/forms/dpr/nurseschools.pdf
• A complete copy of the Illinois Nurse Practice Act and the Rules may be found on the Division of Professional Regulation (DPR) Nurses webpage: https://idfpr.illinois.gov/ profs/nursing.html or on the Illinois Nursing Workforce Center’s website: https://nursing.illinois.gov/ nursing-licensure/nursing-act-rules.html
• Tips for first time registration for individual online account matching process found here: https://idfpr.illinois.gov/Forms/Online/Renewal%20Tips%20Individual%20 Accounts%202021-12-15.pdf. For most licensees, this will be the first time logging into your IDFPR Online Services Portal Account. You will need to Register and MATCH to your existing license record. If you applied for your initial license via the
IDFPR portal, you can use the username and password created at that time. For those requiring additional assistance with the login process, please contact IDFPR by emailing fpr.lmu@illinois.gov. Please enter "RENEWAL" in the subject line of your e-mail.
• Complaints against any individual or entity regulated by the Division of Professional Regulation may be filed by contacting the Complaint Intake Unit. For a complete list of professions regulated by DPR, please click https://idfpr.illinois.gov/content/dam/ soi/en/web/idfpr/forms/brochures/dpr.pdf
• Please note: Pursuant to Illinois law (20 ILCS 2105/2105-117), all information collected by the Department during an examination or investigation of a licensee, registrant, or applicant is confidential and cannot be publicly disclosed. This includes complaints and any information collected during an investigation. Exceptions to this law exist only for law enforcement, other regulatory agencies with appropriate regulatory interest, or a party presenting a lawful subpoena. The Division of Professional Regulation online complaint form may be found here: https://idfpr.illinois.gov/admin/dpr/complaint.html
• On May 11, 2023, Governor Pritzker ended the state of Illinois' public health emergency. All Variances, Proclamations, and Guidance issued by IDFPR for the duration of the Gubernatorial COVID-19 Proclamation have now ended. Find the latest information at: https://idfpr.illinois.gov/covid-19.html
• The State of Illinois Coronavirus Response Site: The COVID-19 Vaccine Plan, up-todate information on what Illinois is doing protecting the health, safety, and wellbeing of Illinoisans can be found at https://coronavirus.illinois.gov/s/

Painting is a two-dimensional visual expression of art using elements such as shapes, lines, colors, tones, and textures to produce sensations of volume, space, movement, and light on a flat surface. The medium can be oil, fresco, acrylic, tempera, ink, watercolor, and others. The form can be mural, easel, panel, panorama, and others. Nurses put their hearts into patient care daily and when away from patient care, some put their hearts into painting. The two artworks by Laura Kay Wood, featured in this edition of Hearts of Nursing column, “Calm” and “Vitality” respectively were created using watercolor on canvas.


Editor’s note: Not only are they adept at patient care, but many also excel in fine arts, performing arts, culinary arts, and other activities that only confirm the many “hearts” of nurses. This new column features activities that showcase what is also meaningful and precious to nurses. We invite you to contribute an article, a play you participated in, a poem you composed, a recipe, a musical instrument you play, and other talents that must tell the world, nurses do not have a “heart” for patient care only, but also in all aspects of human interaction. Please submit your contribution via the link: syswart@ana-illinois.org
2020 came.
COVID from a Nurse
COVID reigned and patients died While their nurses cried.
COVID from a Nurse 2
You can’t see much. Me Covered by masks, gloves, gowns. I See your breath stop.
COVID from a Patient Who is there? Covered Only eyes showing. So scared. Can’t breathe. Help me please.
Haiku is a type of short form poetry that originated in Japan, consisting of three phrases composed of 17 phonetic units (like syllables) in a 5-5-7 or 5-7-5 or 7-55 pattern (as long as it adds up to 17, in any order). Haikus were originally written as opening stanza for a larger poem but over time, they began to be written as stand-alone poems. Poetry writing is a popular activity, and many nurses have the passion for it. Share with NV yours. For submission, send via email to kristy@ sysconsultingsolutions.com or irenest0800@yahoo.com
Caring for loved ones with dementia isn’t just a responsibility; it’s a profound journey intertwining respect, dignity, and the essence of human connection. My experiences, particularly witnessing my grandmother’s resilience after losing two husbands and later living with us, illuminated life’s fragility. This highlighted the pivotal role of respect and dignity in caregiving. Watching my mother selflessly care for her mother, displaying patience in communication, and offering unwavering support epitomized life’s holistic nature rooted in human connection.
Years later, our family faced upheaval when my mother received a dementia diagnosis, catching us off guard and ill-prepared. The scarce medical guidance provided no clear direction or support, leaving us adrift in uncertainty, lacking resources or a roadmap. We grappled with the stark reality that, while her appearance remained unchanged, her behavior altered drastically, and we had no clue how to deal with this as she slipped away slowly before our eyes. This pivotal time ignited a determination within me: to create a specialized dementia course tailored for families and caregivers like ours.
Envisioning this course, my commitment was to alleviate the confusion and distress faced by families dealing with dementia. Understanding that quality care hinges on comprehensive knowledge, it wasn’t just about disseminating information; it aimed to be a transformative, easily digestible journey that could empower caregivers with a deep understanding of the disease.
This course's uniqueness wasn’t solely in its content but in its essence. Designed as a self-paced journey, it recognizes diverse caregiver needs and schedules. Moreover, the course is certified for 10 Continuing Education Credits (CEs), enriching both personal caregiving and professional expertise for nurses and social workers.
The ten core modules cover various aspects: from exploring the brain’s anatomy and the progression of dementia, to addressing safe environments, multicultural competence, medical diagnoses, treatments, delusions, hallucinations, and their causes. It delves deeply into effective communication, caregiver stress, considerations on sexuality and intimacy, and education on palliative care, hospice, and ‘End of Life Care’. The end of each course culminated with reality- based simulations, granting learners a firsthand perspective of dementia.
“This initiative emerged from a profound belief: no family should navigate the complexities of dementia alone. If this course could offer a clearer, more accessible understanding of the disease and what caregivers may encounter along their journey with a person with dementia (PWD), it would honor my commitment to make dementia care more approachable and compassionate. By enhancing caregivers’ comprehension of the disease, this course aims to empower them to deliver quality care with purpose, passion, and pride.”
Aishling Dalton Kelly www.aishlingcareacademy.com
Course title: Dementia has a face and a name.
Completion time 5 hours (10 CEUs)
Certificate of completion



The Department continues to receive inquiries regarding continuing education required for Registered Professional Nurses (RN) by the license renewal deadline of May 31, 2024. The questions and answers listed below will provide clarification. Please note that a complete copy of the Illinois Nurse Practice Act and the Rules may be found on the IDFPR website (https://nursing.illinois. gov/nursing-licensure/nursing-act-rules.html). Nursing re-licensure CE information is available on the Illinois Nursing Workforce Center’s website at https://nursing. illinois.gov/nursing-licensure/continuing-education.html
The implicit bias awareness training CE requirement is required of all persons who hold a professional license issued by the Division of Professional Regulation (DPR) and are subject to a continuing education (CE) requirement beginning after January 1, 2024. The DPR webpage has implicit bias awareness CE information at https://idfpr.illinois.gov/dpr.html
Implicit bias is a form of bias that occurs automatically and unintentionally, that nevertheless affects judgment, decisions, and behaviors. Any training on implicit bias awareness applied to meet any other State licensure requirement, professional accreditation or certification requirement, or health care institutional practice agreement may count toward the one-hour implicit bias awareness training requirement for license renewal.
A licensee may count the one-hour completion of this course towards meeting the credit hours required for re-licensure continuing education (Public Act 102-004, Admin Code Title 68: Section 1130.500 https://www.ilga.gov/commission/jcar/ admincode/068/068011300E05000R.html)
This requirement shall become effective for all applicable license renewals occurring on or after January 1, 2024. Use this link to the DPR webpage with implicit bias awareness CE information: https://idfpr.illinois.gov/ dpr.html
Alzheimer’s Disease: Beginning with the 2024 RN renewal, Illinois RNs who provide health care services to and have direct patient interaction with adults 26 years of age and older will be required to complete a one-hour course in diagnosis, treatment, and care of Alzheimer's disease, along with other dementia types. CE Curriculum will involve how to identify and diagnose Alzheimer's, effective communication strategies and management and care planning. This course may count toward the regular CE requirements (Public Act 102-0399, 20 ILCS 2105/2105-365).
Sexual harassment prevention training CE requirement: A law went into effect on January 1, 2020, which requires individuals with licenses issued by the Illinois Division of Professional Regulation (DPR) that require continuing education (CE) to renew their license, to also complete one hour of CE on the topic of sexual harassment prevention training.
The Illinois Nurses Foundation’s Editorial Committee would like to get feedback from our Nursing Voice readers. The brief survey will help the committee better tailor our content to our readers wants and needs. We appreciate taking a few minutes to complete our survey at the link below or QR code. https://www.surveymonkey.com/r/J3SG63X

How many hours of Continuing Education (CE) will I need for 2024 license renewal?
• This new one hour of implicit bias awareness training CE course is intended to fit into the licensee’s regular CE requirements. RNs will be renewing their licenses in 2024, with one of the 20 hours of required CE to be an implicit bias awareness training course, while another one of the 20 hours of required CE must be sexual harassment prevention training.
• For APRNs and FPA-APRNs will be renewing their licenses in 2024, one of the 80 hours of required CE must be this new one hour of implicit bias awareness training course, while one of the 80 hours of required CE must be sexual harassment prevention training.
• LPNs will begin renewing their licenses in late Fall 2024, and one of the 20 hours of required CE must be this new implicit bias awareness training course. Another one of the 20 hours must be a sexual harassment prevention training course.
What are the CE Course Rules for Illinois LPNs, RNs, APRNs and FPA-APRNs renewing their licenses in 2024?
The NPA Rules regarding CE requirements indicate that courses shall only be provided by existing Divisionapproved continuing education providers or sponsors or by persons or entities who become Division-approved continuing education sponsors.
How do I know if the sponsor is approved or licensed? Is there a list of approved CE Sponsors and Programs for Illinois nurse license renewal in 2024?
CE sponsors must either be pre-approved per Nurse Practice Act Rule 1300.130 or must have a CE sponsor license. The list of pre-approved CE Sponsors and Programs is in the Rules for the Administration of the Nurse Practice Act, Section 1300.130: https://www.ilga.gov/commission/jcar/ admincode/068/068013000A01300R.html
c) Pre-Approved CE Sponsors and Programs
1) Sponsor, as used in this Section, shall mean:
A) Approved providers of recognized certification bodies as outlined in Section 1300.400(a).
B) Any conference that provides approved Continuing Medical Education (CME) as authorized by the Illinois Medical Practice Act.
C) American Nurses Credentialing Center (ANCC) accredited or approved providers.
D) Illinois Society for Advanced Practice Nursing (ISAPN).
E) American Academy of Nurse Practitioners (AANP).
F) Nurse Practitioner Association for Continuing Education (NPACE).
G) American Association of Nurse Anesthetists, or National Board of Certification and Recertification for Nurse Anesthetists (NBCNA).
H) National Association of Clinical Nurse Specialists (NACNS).
I) American College of Nurse Midwives (ACNM).
J) American Nurses Association-Illinois (ANAIllinois).
K) Illinois Nurses Association or its affiliates (INA).
L) Providers approved by another state's board of nursing.
M) Nursing education programs approved under Section 1300.230 or 1300.340 wishing to offer CE courses or programs.
N) Employees licensed under the Hospital Licensing Act (210 ILCS 85) or the Ambulatory Surgical Treatment Center Act (210 ILCS 5)
O) Any other accredited school, college or university, State agency, federal agency, county agency or municipality that provides CE in a form & manner consistent with this Section.
Please note that this is not a complete list. In addition, organizations may obtain CE sponsor licenses issued by the Department. Use IDFPR’s License Lookup tool at https://www.idfpr.com/LicenseLookUp/LicenseLookup. asp (be sure to use “Nurse CE Sponsor” as the profession).
This is my first time renewing my Illinois LPN, RN, APRN or FPA-APRN license – do I need to complete the one hour of implicit bias awareness training CE prior to license renewal in 2024?
No, a renewal applicant shall not be required to complete one hour of implicit bias awareness training prior to the first renewal of an Illinois LPN, RN, APRN or FPA-APRN license.
What is the fee for Illinois LPN, RN, APRN or FPA-APRN license renewal in 2024?
The fee for the Illinois RN, APRN or FPA-APRN license renewal in 2024 shall be calculated at the rate of $40 per year or $80 at the time of renewal. For Illinois LPNs whose license renewal begins in late Fall 2024 and ends January 31, 2025, the fee for the renewal shall be calculated at the rate of $40 per year or $80 at the time of renewal.
Additional Continuing Nursing Education information, including a FAQ sheet and a list of pre-approved CE sponsors is available on the Illinois Nursing Workforce Center Website https://nursing.illinois.gov/nursinglicensure/continuing-education.html


Betsy Murphy, MS, RN, HNB-BC, CIAYT
This research poster was presented in September 2023 at the Society for Integrative Oncology International Conference.
Introduction
The cancer experience is stressful for both patients and oncology healthcare professionals. There are many ways that mindfulness interventions can be beneficial to support cancer patients and oncology staff. Evidence shows that mindfulness programs can help reduce anxiety, stress and cancer related fatigue (CRF)in patients experiencing cancer as well as improve emotional regulation. Compassion fatigue is prominent among oncology nurses. It has been reported that 37% of oncology nurses experience compassion fatigue symptoms, and 44% of inpatient oncology nurses experience burnout (Finley & Sheppard, 2016) . There is an increased risk of burnout in oncology nurses due to the increase in exposure to suffering and loss. Mindfulness programs for oncology health professionals have been shown to decrease burnout symptoms and improve anxiety and stress.
Methods
Through a search conducted using Pub Med and Google scholar and key words (mindfulness & oncology patients/healthcare workers) primarily, 4 journal articles were selected which provided meta-analysis of clinical research that provided Mindfulness Based Stress Reduction (MBSR) or similar Mindfulness-based interventions (MBI) for oncology patients. The articles range from 2006 – 2022. According to Ott et.al from 2000 to 2005, 9 research articles were published in peer-reviewed journals that investigated the use of mindfulness meditation. In 2019, Mehta et.al. identified 124 clinical trials that investigated the benefits of mindfulness for oncology patients. It was also reported that feasibility and cost effectiveness of MBSR and MBI programs as an ancillary treatment for cancer patients makes these integrative therapies especially valuable. Journal articles discussing the benefits of oncology staff participating in MBSR and MBI programs were also found using the same search methods. Most of the studies involved nurses as the primary subjects, as the prevalence of compassion fatigue and burnout has been extensively reported in this population. One study included all oncology staff which showed positive results with mindfulness interventions. There were few studies that addressed oncology staff exclusively; however, mindfulness interventions for healthcare providers continue to provide measurable benefits and are considered in this presentation.
Discussion
There are many studies involving the use of MBSR and MBI’s for oncology patients across a variety of cancer diagnosis which support the value of this integrative oncology approach. Evidence shows improvements in psychological and physical symptoms common in patients undergoing cancer treatment that includes reduction in anxiety, stress, and depression as well as improved cancer related fatigue and pain symptoms. Of note also is the feasibility and cost benefit of providing mindfulness training within the clinical setting with implications for potential prevention of further complications related to a cancer diagnosis and treatment.
The effect of mindfulness training for oncology healthcare professionals has also been shown to improve psychological and professional wellbeing; thus, providing benefit to reduce burnout and compassion fatigue and improve patient care. See below table demonstrating similar benefits of MBSR and MBI’s in both patients and clinicians. The investigation of this topic has shown that oncology nurses can be at higher risk for compassion fatigue given the exposure to poor prognosis, severe pain and death. The limitation of oncology specific data regarding MBSR for oncology health professionals is acknowledged in this presentation, which demonstrates the need for more homogenous studies of this nature.
BENEFITS OF MINDFULNESS INTERVENTIONS
Oncology Patients
Reduction of Anxiety, Depression, and Stress
Reduction of Pain
Improvement of Immune Response (T Cell)
Improvement of Cancer Related Fatigue
BENEFITS OF MINDFULNESS INTERVENTIONS Oncology Healthcare Providers
Reduction of Anxiety, Depression, and Stress
Reduction of Compassion Fatigue
Reduction of Emotional Exhaustion
Improvement of Presence & Empathy
Reduction of Caregiver Stress & Anxiety Cost Effective
Cost Effective
Conclusion
Mindfulness-based interventions provide measurable improvements in both physical and psychological symptoms in cancer patients and the professionals that care for them. Mindfulness across the Cancer Continuum: A Review of Mindfulness Benefits for Oncology Patients and Staff
Bibliography
Bilgiç, Ş., & Pamuk Cebeci, S. (2022). Compassion Fatigue in Oncology Nurses in Turkey. Holistic Nursing Practice, 36 (5), 304–310. https://doi.org/10.1097/hnp.0000000000000540
Chayadi, E., Baes, N., & Kiropoulos, L. (2022). The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: A systematic review and meta-analysis. PLOS ONE, 17 (7), e0269519. https://doi.org/10.1371/ journal.pone.0269519
Delaney, C. (n.d.). Mindfulness Meditation for Nurses: A Healthy Coping Tool for Emotionally Hazardous Work. Www.academia.edu. Retrieved August 13, 2023 from https://www. academia.edu/41652439/Mindfulness_Meditation_for_Nurses_A_Healthy_Coping_Tool_for_ Emotionally_Hazardous_Work
Duarte, J., & Pinto-Gouveia, J. (2016). Effectiveness of a mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: A non-randomized study. International Journal of Nursing Studies, 64, 98–107. https://doi.org/10.1016/j. ijnurstu.2016.10.002
Eckstein, J., Rana, Z. H., Caravan, S., Sharma, R., Potters, L., & Parashar, B. (2022). Burnout in Radiation Oncology Physician Workforce: The Impact of Mindfulness and Fulfillment. Advances in Radiation Oncology, 100971. https://doi.org/10.1016/j.adro.2022.100971
Hooper, C., Craig, J., Janvrin, D. R., Wetsel, M. A., & Reimels, E. (2010). Compassion Satisfaction, Burnout, and Compassion Fatigue Among Emergency Nurses Compared With Nurses in Other Selected Inpatient Specialties. Journal of Emergency Nursing, 36 (5), 420–427. https://doi. org/10.1016/j.jen.2009.11.027
Kieviet-Stijnen, A., Visser, A., Garssen, B., & Hudig, W. (2008). Mindfulness-based stress reduction training for oncology patients: Patients’ appraisal and changes in well-being. Patient Education and Counseling, 72(3), 436–442. https://doi.org/10.1016/j.pec.2008.05.015
Mehta, R., Sharma, K., Potters, L., Wernicke, A. G., & Parashar, B. (2019). Evidence for the Role of Mindfulness in Cancer: Benefits and Techniques. Cureus, 11(5). https://doi.org/10.7759/ cureus.4629
Ott, M. J., Norris, R. L., & Bauer-Wu, S. M. (2006). Mindfulness Meditation for Oncology Patients: A Discussion and Critical Review. Integrative Cancer Therapies, 5(2), 98–108. https://doi. org/10.1177/1534735406288083
Nissim, R., Malfitano, C., Coleman, M., Rodin, G., & Elliott, M. (2018). A Qualitative Study of a Compassion, Presence, and Resilience Training for Oncology Interprofessional Teams. Journal of Holistic Nursing, 37(1), 30–44. https://doi.org/10.1177/0898010118765016
Perry, B., Toffner, G., Merrick, T., & Dalton, J. (2011). An exploration of the experience of compassion fatigue in clinical oncology nurses. Canadian Oncology Nursing Journal, 21(2), 91–97. https://doi.org/10.5737/1181912x2129197
Wu, S., Singh-Carlson, S., Odell, A., Reynolds, G., & Su, Y. (2016). Compassion Fatigue, Burnout, and Compassion Satisfaction Among Oncology Nurses in the United States and Canada. Oncology Nursing Forum, 43(4), E161–E169. https://doi.org/10.1188/16.onf.e161-e169

Franklin University continues to lead, inspire and compassionately educate a diverse student body of healthcare professionals in the new College of Nursing

info@ilnursesfoundation.com


Nurses want to provide quality care for their patients.
The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.
❑ Mastercard ❑ VISA
Credit card number Expires CVV
To access electronic copies of the Nursing Voice, please visit https://www.healthecareers.com/nurse-resources/nursing-publications/ illinois
Signature:
Date:
Printed Name: E-Mail:
Address: City, State, Zip Code:
Preferred Phone Number:
Please mail completed form & check to: ANA-Illinois
Atten: Nurses-PAC PO Box 636 Manteno, Illinois 60950