




www.dentalabstracts.com






www.dentalabstracts.com

Editor-in-Chief
Douglas B. Berkey, DMD, MPH, MS
Senior Publisher
Annie Zhao
Journal Manager
Sangamithrai S
Abstract Writer
Elaine Steinborn
© September 2025, Elsevier Inc. All rights reserved.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise—without prior written permission from the publisher.
Publication Information Dental Abstracts (ISSN 0011-8486) is published bimonthly by Elsevier Inc., 1600 John F. Kennedy Boulevard, Suite 1600, Philadelphia, PA 1910, United States. Months of publication are January, March, May, July, September, and November.
Customer Service Office: 11830 Westline Industrial Drive, St. Louis, MO 63146. Periodicals postage paid at New York, NY, and additional mailing offices. Annual subscription rates for 2018 (domestic): $144.00 for individuals and $71.00 for students; and (international) $194.00 for individuals and $105.00 for students.
USA POSTMASTER: Send address changes to Dental Abstracts, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043.
Copyright 2025 by Elsevier Inc. All rights reserved. Dental Abstracts is a trademark of Elsevier Inc. Dental Abstracts is a literature survey service providing abstracts of articles published in the professional literature. Every effort is made to ensure the accuracy of the information presented in these pages. Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editors or the publisher. The Editors and the publisher disclaim any responsibility or liability for such material. Mention of specific products within this publication does not constitute endorsement.
All inquiries regarding journal subscriptions, including claims and payments, should be addressed to: Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Tel: 1-800-6542452 (U.S. and Canada); 314-447-8871 (outside U.S. and Canada). Fax: 314447-8029. E-mail: support@elsevier.com (for print support); support@elsevier.com (for online support).
Notice: Journals published by Elsevier comply with applicable product safety requirements. For any product safety concerns or queries, please contact our authorized representative, Elsevier B.V., at productsafety@elsevier.com
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments contained herein. Health care practitioners must exercise their professional judgement and make all treatment-related decisions based solely on the specific conditions of each patient. Because of rapid advances in the medical sciences, independent verification of diagnoses and drug dosages should always be made.
The content is provided “as-is” and Elsevier makes no representations or warranties, whether express or implied, as to the accuracy, completeness, or adequacy of any content. To the fullest extent permitted by law, Elsevier assumes no responsibility for any damages, adverse events, or liability arising from use of information contained herein including for any injury and/or damage to persons or property, whether as a matter of product liability, negligence or otherwise.
Inclusion of any advertising material in this publication does not constitute a guarantee or endorsement of the quality or value of such product or service or of any of the representations or claims made by the advertiser.

DentalAdvance .org is the gateway offering high-quality research, news, jobs and more for the global community of dental professionals.
Journal profiles with quick links to Tables of Contents, author submission information, and subscription details
Important information and valuable resources on how to submit a journal article
Dentistry Articles in Press from participating journals
Quick links to the leading dentistry societies worldwide Dentistry News from Elsevier Global Medical News (formerly IMNG)
Dentistry Jobs powered by ElsevierHealthCareers.com

Editor-in-Chief
DouglasB.Berkey,DMD,MPH,MS ProfessorEmeritus, SchoolofDentalMedicine, UniversityofColorado, Aurora,Colorado
AssociateEditor
DanielM.Castagna,DDS AssociateProfessor,DepartmentofPreventiveandRestorativeDentistry, UniversityofthePacific,ArthurA.DugoniSchoolofDentistry, SanFrancisco,California
P.MarkBartold,DDSc,PhD,FRACDS(Perio) ProfessorEmeritus SchoolofDentistry, UniversityofAdelaide Adelaide,Australia
RobBerg,DDS,MPH,MS,MA ProfessorandChair, DepartmentofAppliedDentistry, UniversityofColoradoSchoolof DentalMedicine, Aurora,Colorado
TylerH.Berkey,DMD GeneralDentist Aurora,Colorado
FionaM.Collins,BDS,MBA,MA ConsultantandEditor, GeneralDentist Longmont,Colorado
AnthonyJ.DiAngelis,DMD,MPH ChiefofDentistry, HennepinCountyMedicalCenter, Professor,UniversityofMinnesota, SchoolofDentistry, Minneapolis,Minnesota
RaulI.Garcia,DMD,MMedSc ProfessorandChairman, DepartmentofHealthPolicyandHealthServicesResearch, BostonUniversitySchoolofDentalMedicine, Boston,Massachusetts
MichaelSchafhauser,DDS GeneralDentist, St.Paul,Minnesota
JoeVerco,DClinDent PaediatricDentist NorthAdelaide,Australia
VOL.70 No.5
EndodonticCare Hands-On ArticaineAllergies377 TrueAllergytoArticaine
IndirectPulpCapping
SwimmingandTeethStaining386
DentalStainingandSwimmingExtentand Intensity
WaterlineTesting387 HowToShockandTestDentalWaterlines
WhiteCoatHypertension389 BloodPressureDiscussionsintheDentalOffice Inquiry
Mouthwashes392
ChoosingaMouthwash
Oral/SystemicConsiderations394
EconomicEvaluationsofPeriodontal TreatmentforType2DiabetesPatients
PosttraumaticStressandPoorOralHealth
OrofacialPain396
InitialTherapiestoRelieveOrofacialPain MeditationPlusTetracyclineforAphthous Ulcers
TMJ/SleepDisorders398 RelationshipsBetweenTMJDysfunctionand SleepDisorders
WeightedBlankets399 AcceptabilityandEffectivenessofWeighted BlanketsforPediatricDentalCare
WaterFilterTesting401 WaterFilterPitcherPerformance
404 Sleep andHowtoupYourShare WhattoPackforVacation
Notes
TofacilitatetheuseofDentalAbstractsas areferencetool,allillustrationsandtablesincluded inthispublicationarenowidentifiedastheyappear intheoriginalarticle.Thischangeismeanttohelp thereaderrecognizethatanyillustrationortable appearinginDentalAbstractsmaybeonlyoneof manyintheoriginalarticle.Forthisreason, figure andtablenumberswilloftenappeartobeoutof sequencewithinDentalAbstracts.
StandardAbbreviations
Thefollowingtermsareabbreviated:acquiredimmunodeficiencysyndrome(AIDS),humanimmunodeficiency virus(HIV),andtemporomandibularjoint(TMJ).
Doing nice things for other people feels good, but it feels even better when you do these things for no reason other than how it feels. Giving with authenticity beats giving with expectation, and the results of your generous giving will benefit everyone involved. The term esprit de corps is defined as sharing feelings of pride, fellowship, and loyalty among members of a group. This feeling is an essential component of generosity in an organization and must be modeled by the leader of the group. Having a mindset of abundance rather than scarcity and blending generosity into everything you do are attitudes that can contribute to a successful and satisfying personal and professional life.
Living generously tends to result in a generous return to you. This abundance mindset opens up opportunities that enrich your life. In contrast, acting from a scarcity view will lead to a paucity of opportunity and a withering of your organization as it reflects your cynicism and undermines those who work with you. Cutthroat conduct in business is always outdone by goodwill and generosity.
Generosity
The esprit de corps that you want to focus on is caring more about the well-being of employees and patients than about any other concern. Care for your employees will trickle down to these workers providing better care for patients, which leads to growth in your practice. Doing things that interfere with this cycle can compromise the results.
Generosity doesn’t mean giving patients a pass on their unpaid bills, because those who provide care, such as dentists, deserve to be paid. If you see a patient is struggling to pay, you can offer to work with him or her on a payment plan that fits his or her situation.
People who don’t ascribe to being a giver can take advantage of your kindness and goodwill. As a result, you may back off so you won’t be subjected to the pain of these incidents. People tend to fall into the categories of a giver, a taker, or a matcher. Givers give without expectation, takers take without limitation, and matchers value reciprocity. Most dentists are matchers who give often but attach strings to guard their self-interest. This protects them from the takers and keeps them safe, but whether this is the right thing to do depends. How you express your generosity and how you respond to skeptics, takers, and matchers will vary depending on your temperament. The best approach is to be upbeat and high energy. Having an eager anticipation regarding daily life and serving others can be your attitude both in business and in your personal life. This leads to an enduring willingness to help in any way you can.
The first step toward being generous is getting sufficient sleep and proper nutrition and taking care of your mental health. With these elements under control, your ability to be generous can thrive. You are content and can give freely without expectations because your needs have been met. Interactions with others can be a generous act that you get to enjoy, that allows you to embrace the camaraderie and collaboration, and that yields satisfaction related to having done a job well.
This mindset also draws people like you into your circle, which enhances your enjoyment of life. Others will continue to join in and outnumber the takers who might try to sabotage your joy.
People can tell when someone isn’t generous but instead is focused on the strings that are attached to his or her giving. It’s important to give without expectation so that you won’t be disappointed by others’ unwillingness to reciprocate.
Start the day well-nourished, rested, and in a good mood. Let this positive beginning carry you through the day, and spend your time helping others. This will make you successful and encourage the growth of your dental practice. Focus on what you can do for others, and eventually others will do the same thing for you. You will learn to consider every new blessing simply a bonus.
Murphy MB: Building a legacy of generosity: The power of giving. Dent Econ 115:54, 57, 2025
Reprints not available
Changes in health behaviors tend to gradually develop rather than take hold quickly. Sports, in particular, have proved resistant to change or at least slow to adopt health measures. For example, professional hockey players have seen damaged or missing teeth as a badge of honor or simply part of the game for many years. In 1979, the National Hockey League required all players entering the league to wear helmets, leading one coach to blame the “intellectual liberals” for demanding changes when he couldn’t recall any recent head injuries occurring during hockey play. Today, nearly all combat sports require mouthguard use to protect players’ orofacial integrity. The role of sports in mouthguard use and the value of wearing mouthguards were discussed.
National Basketball Association (NBA) star Steph Curry is widely known for his ability to sink long-distance (3-point) shots with unique skill. He is also widely known for how he keeps his mouthguard moving, removing it, readjusting it, and voraciously chewing it during any pauses in play. He’s been ejected from 3 NBA games in his career, with the infraction being throwing a mouthguard. Curry has likely influenced younger players to mimic not just his shooting form but also his distinctive mouthguard mannerisms. It’s
possible that he has protected children and youth basketball players from more chipping and tooth avulsions than any dentist has ever restored.
As mouthguards led to a widespread need for mouth protection during sports, many clinicians offered guidance regarding how to fabricate well-fitting sports mouthguards. In addition, more youth and college sports organizations now require mouthguard wearing because of their ability to protect against orofacial injuries during play. No conclusive evidence indicates if they protect against concussions, and little evidence shows that they improve athletic performance. Mouthguards are fun because they can be customized and allow athletes to create unique expressions in an atmosphere where regulations regarding uniforms and equipment tend to be strictly enforced.
Most professional athletes in high-impact sports now wear mouthguards, even if they aren’t required. This practice tends to trickle down and influence younger athletes.
Mouthguard use is seen by the American Dental Association as an appropriate requirement for 29 sports. As yet, no major basketball governing body requires them, but most NBA stars wear them voluntarily.
Seeing sports heroes wear protective gear such as mouthguards tends to exert a positive influence on youth sports participants. Even Steph Curry may be considered an honorary oral health advocate for his obvious engagement with his mouthguards. Taking up the wearing of mouthguards protects the teeth as well as other oral structures, which are vital areas of dental concern. Anything that promotes their use during hazardous sports participation is performing a valuable service.
Chaffee BW: Saving teeth, three (points) at a time. J Calif Dent Assoc 53:2477096, 2025
Reprints available from BW Chaffee, Univ of California San Francisco School of Dentistry, San Francisco, CA, USA; e-mail: benjamin.chaffee@ucsf.edu
The Trump Administration health care platform, Make America Healthy Again (MAHA), is designed to reform the health care system to focus on reducing chronic disease, prioritizing preventive health, increasing transparency in medical research, and restructuring federal programs. The American Dental Association (ADA) should be involved in these efforts, focusing on the specific aims of MAHA, how to advance the dental profession, and the importance of integrating oral health care into the proposed plans. A look at the priorities of MAHA and at the trajectory of oral health care in America’s future was taken to identify where progress is needed.
With the emphasis on chronic disease prevention, childhood health, lifestyle, diet, and nutrition, we face a significant opportunity to integrate oral health care more directly into national health policy determinations. Oral disease causes the United States economy a loss of $46 million each year. Prevention efforts are needed to address this problem.
Major Medicaid restructuring has been planned, with particular focus on funding reforms and restricting eligibility. These efforts risk a reduction in dental benefits coverage for lowincome families and are not in line with the evidence that supports the value of dental benefits in Medicaid programs. Coverage is essential to ensure better oral health, improve overall health and wellbeing, lower health care costs, and advance employment prospects.
Expansion of the Medicare Advantage (MA) programs is also planned. MA plans cover about half of the US population age 65 years or older, and most offer some dental coverage. Because challenges remain in these dental coverage plans, the ADA should advocate for better coverage standards, more transparency, better choices for consumers, and more equitable policies governing provider payments.
The safety and efficacy of community water fluoridation are being widely targeted for reform. The best available data and research must be incorporated into any decisions in these areas. Dental practitioners can participate in these efforts by spreading the word about the efficacy and safety of fluoridation, touting the science behind the practice, and educating both the public and policymakers about the effect of fluoridation on dental and overall health. With potential cutbacks coming in research funding, the ADA should ensure that efforts in oral health−related research remain strong.
At this point in time, we have the opportunity to incorporate oral health into overall health care, making it an essential part of the picture. The 4 key areas requiring our attention are dental insurance reform, oral health literacy, workforce issues, and prevention.
Dental care has the highest cost barrier levels, especially for adults. The current dental insurance model doesn’t function
properly. Areas requiring the most attention are the limits of annual benefits, the high costs patients must pay, the poorly structured administrative processes, a lack of transparency, and unregulated insurer loss ratios, but other areas must also be addressed. Coverage for the range of services needed to reach and maintain optimal oral health levels and the provision of adequate funding in US public insurance programs require reform as well. Dental care should be classified as an essential element in overall health and therefore worthy of proper coverage in insurance plans.
The extensive evidence supporting the linkage between oral health and overall health must be incorporated into the lives of everyday people, moving them toward taking preventive and health-affirming action. Persons who have chronic diseases such as diabetes, pregnant women, and those at risk for cognitive impairment such as Alzheimer disease must be established in a dental home so they can understand the link between oral and overall health and be supported in oral health behaviors.
A robust dental workforce of dentists and dental team members is needed to deliver the care required by US patients. This will require stronger efforts to recruit and retain dental care professionals and to overcome workforce shortages. Programs that train, develop, provide pathway initiatives, address loan repayment, and provide scholarship opportunities for dental team members in areas with inadequate dental coverage, including rural America, should also be established to ensure the future workforce will be adequate to the need for care.
Too many people in the United States don’t come for dental care until they experience infection and severe pain, which requires care that is more expensive than accessing ongoing care. With regular dental visits, dentists and dental hygienists can prevent many problems and save money for the US health care system. This pattern of dental care avoidance behavior is especially seen among low-income adults. Visiting the dentist regularly, brushing twice daily with a fluoride-containing toothpaste, flossing, eating foods low in added sugars and without ultraprocessing, and avoiding tobacco and alcohol products are behaviors that can reduce caries and inflammation.
The MAHA agenda is still in its infancy, so the ADA must remain engaged in efforts to include oral health as a national priority. It’s vital to ensure that oral health is seen as an essential ingredient in the overall health care structure that emerges from this new agenda. Achieving overall health for America will require a strong focus on oral health.
Kessler BH, Rosato RJ: Make American healthy again: What it could mean for oral health. J Am Dent Assoc 156:265-266, 2025
Reprints available from BH Kessler, American Dental Assoc, 401 N Michigan Ave, Suite 3300, Chicago, IL 60611-4250; e-mail: kesslerb@ada.org
Many dental professionals are hesitant to proactively introduce cosmetic options to patients. They may feel they’re overstepping or aren’t considering the patient’s affordability issues. They may also lack training and be uncertain how to confidently present these options. As a result, these practitioners miss the opportunity to improve both the patient’s life and the health of the dental practice. Patients may lack a clear understanding of cosmetic options and often won’t ask about them, instead making assumptions regarding cost or appropriateness of the cosmetic procedure. To overcome these issues, a plan was offered that addresses patient issues, offers a visualization approach, and promotes an understanding of the value cosmetic dentistry has for patients and dental practices.
Patients often make assumptions regarding cosmetic dental care based on a lack of knowledge, whether that involves the value of a confident smile, a misunderstanding of the dentist’s silence on the issue, their own self-perceptions or personality traits, or other issues. Most patients hesitate because of this lack of knowledge. Dentists may be waiting for the patient to initiate the conversation, creating a missed opportunity for care.
Having a confident smile can be powerful, enhancing self-esteem, confidence, personal relationships, and career success. However, many patients are unaware of the value they could see with a smile makeover. This extends beyond their personal enhancement to affect their interpersonal and professional interactions.
Often patients want a better smile but because the dentist is silent on the possibility, they assume that it’s not an option for them. They may assume that cosmetic procedures are only appropriate for people with severe dental issues or those who have a strong sense of their image. As a result, patients may see cosmetic treatment as only appropriate for those who are disfigured or vain, making it unnecessary as far as they are concerned.
Self-perceptions and personality traits can prevent patients from considering cosmetic treatments. Many don’t understand the impact even small enhancements can have. This may include whitening, bonding, or alignment correction. Both the patient’s appearance and his or her self-esteem may be impacted.
Overall, patients don’t ask because they aren’t aware of what’s possible, they forget to mention their interest, or the topic simply never comes up. The treatments are assumed to have a certain value only for certain patients.
Because patients don’t recognize what they don’t know, dentists need to take the initiative and show the patient the potential transformation that can be achieved and why it’s worth investing in. Visual tools such as intraoral photographs, scans, and artificial intelligence−powered radiologic detection software can simplify the clinical information and help patients better understand their oral health. The full-face smile simulation allows patients to see their potential transformation.
The full-face smile simulation is a natural-looking digital smile preview. Such simulations can be presented casually, yet they are a powerful tool to evoke emotion in the patient as well as a desire to engage in the experience. When patients see themselves with an improved smile, the procedure becomes more personal and impactful. This gives the patient some of the information needed to visualize outcomes and to be more confident and able to move forward with treatment.
For patients who assume full-arch reconstruction is too expensive, the dentist can show a side-by-side digital simulation of their current and potential smile. Seeing the transformation taps into emotions that drive buying decisions for procedures that will make them feel rather than those that are driven by logic.
Patients are more likely to accept costly treatment when they recognize the cosmetic benefits they will experience. Seeking care for worn teeth, bite issues, or missing teeth often leads the patient to view cosmetic procedures as needed repairs. Seeing the restorative effect on the smile makes the investment more satisfying, especially if full-arch reconstruction is done, when both enhanced oral function and significantly improved confidence and appearance result. Dental professionals can present the functional treatments as a health solution and a cosmetic enhancement, which shifts the focus from cost to value and increases the attractiveness of the process for the patient.
The financial impact of offering cosmetic dentistry can include significant growth opportunities. Practices offering cosmetic procedures have higher revenue, increased practice valuation, and higher profitability levels in the eyes of dental service organizations looking to purchase the practice.
Long-term financial health is also improved. The patients who receive cosmetic procedures are more likely to remain with that provider and agree to additional care from him or her. They also engage more often in preventive and restorative care and will refer others to that practice.
To overcome psychological and operational barriers to offering cosmetic dentistry will require the right approach, tools, and a proper mindset. This will allow for cosmetic conversations to take place. The specific ways to manage challenges include the following:
1. Implicit bias, where dentists assume only certain patients are interested. The solution is to make every appropriate patient a candidate for smile enhancement discussions.
2. Treatment inertia, where providers worry they will sound like a salesman. The solution is to shift their mindset from selling to educating.
Attracting great dental team members is based on principles related to career success, both short-term and long-term. Among the components of this process are the foundational goals of the practice. It should have high production levels, with a yearly increase in production goals. All the team members should come to work every day with an ownership mentality and pride in their work. Finally, the dentist should have a plan in place to reach financial independence at a specific age. Gathering an excellent team for the practice will require care in conducting the hiring process, in providing a structured interview, and in offering supportive onboarding techniques.
When a team member leaves the practice or isn’t performing at a satisfactory level and is let go, the dentist must have a strategy in place for seeking an excellent replacement, use ad language that targets the desired respondents, ensure good relationships exist
3. Workflow integration concern, where practitioners resist incorporating new technology. The solution is to make it easier to add digital smile previews to case presentations as standard practice. The practice may be to take a full-face, natural-smile photograph of each new patient.
Patients and dental practices both benefit from cosmetic dentistry. Patients become more confident and have renewed self-esteem when they undergo even minor improvements in their smile. Practices have more case acceptances and grow when dentists initiate the conversation about smile improvement. Using the digital smile simulations can break down barriers to these conversations and give the dentist the opportunity to explain the value of such treatments. Cosmetic dental approaches become a natural component of oral health care.
Reprints not available
with the remaining employees, and screen to eliminate people who aren’t the right fit.
Dentists should be proactive in defining how their practice will reach potential hires. Successful recruiting should result in potential hires who are eager to schedule interviews and get the job.
It’s essential to craft an ad focused on the types of individuals who would make good additions to the dental team. High-quality team members can become or may already be world-class performers. Often these individuals want to make a difference in the lives of patients. They desire a positive work experience with good team interactions that offers interesting, challenging, and rewarding employment. They aren’t in it for the paycheck but are energized and enthusiastic about the work, the team, and the environment where they will function.
The dentist should view team members as colleagues and not employees or subordinates. They should be encouraged to improve their patients’ lives and be proud to do their jobs.
A telephone screening should be instituted to determine if an individual would make a good candidate for the open position. Specific questions should be formulated to identify people who are or aren’t a good fit for the practice.
The interview should consist of 3 parts, with the first part focused on the candidate, the second part on the practice, and the third part making an offer of employment if the other parts go well. Although the ideal would be to conduct separate interviews for each of these topics, today’s tight labor market makes it essential to move quickly.
To learn about the candidate, the dentist should ask about his or her background, interests, strengths, weaknesses, and personality. People try to make a good impression during the interview, so the dentist should ask lots of questions and allow the candidate to talk at least half of the time to get to the person’s authentic personality. A checklist can be kept to guide this process of seeking to know the candidate more deeply as quickly as possible. It’s wise to ask questions that may be unexpected, such as what the person dislikes about his or her previous job.
The information given regarding the practice should create a positive image and outline the dentist’s vision for the practice going forward. It’s important to explain the mission of each employee and why he or she would come to work each day. Defining the culture of the practice should also be a part of this presentation. Many people desire to have more than a job and seek to belong to something special where they can contribute, will be welcomed by other team members, and will have support.
The dentist should be aware of how he or she feels during the interview. It’s important to hire someone who is the right fit even if he or she is less skilled than another, less likeable candidate. Personality and attitude can indicate whether an individual is a good fit for the practice.
The dentist should be prepared to make an offer. This includes knowing how much to offer, which can be based on what is being offered in online advertisements by other practices. The dentist should ensure that any offer is in line with current team compensation to avoid disruption in the team.
How an employee is onboarded will determine how they will perform. During the first 100 days of employment, the new team member will learn how the practice works, what the team is like, and the aspects related to the practice’s culture. The dentist should meet with new employees regularly to ask how they’re doing and offer any guidance or support that is needed. With this ongoing training and support, new employees will be given the foundation for performing at an exceptional level.
Excellent leadership is required to interest excellent employees in applying for an open position. The dentist should be prepared and not rush into hiring a warm body. He or she should set the parameters of the practice, the existing team, and the fit of any new employees. Taking steps to ensure that the team works well together and the new employee is given the opportunities to excel in the position will tend to yield a successful practice that is marked by less stress and more desire to invest in delivering excellent patient care.
Levin RP: How to attract a great team. Dent Econ 115:11-12, 2025
Reprints not available
Most dentists don’t build a hiring pipeline and are unprepared when they need to hire someone. At that point, dentists can be stressed and panicky, sometimes leading to poor hiring choices to avoid being short-staffed. Being proactive in hiring can allow the dentist to relax and choose an employee from the hiring pipeline who will fit well with the existing staff. The dentist must continually promote the practice as an excellent workplace and build relationships with local dental professionals and those who could become dental professionals. Team members should be reassured that this philosophy doesn’t mean you are looking to replace them, but is simply preparation for future needs. Several strategies can contribute to networking and help the dentist focus on cultivating a team of potential employees.
It’s important to establish that this practice is not only positive and supportive but is an outstanding place to work. The dentist should celebrate team members publicly, with clear expressions of his or her appreciation for the employees. Included in these ads, signs, or social media should be the assurance that the practice always welcomes new employees and patients. Social media for the practice should include fun, informal moments for the dental team. This is attractive to both patients and potential employees.
Employees should be engaged in team-building events. The dental practice may host charity races, volunteer activities, or other opportunities to build camaraderie. Local media should be contacted if photo opportunities exist.
In addition to conveying appreciation to the team, the dentist should give each employee rewards and recognition for excellent performance. If the team goes out together, they should wear branded clothing so the practice will be associated with their rewards.
The dentist should focus on finding experienced or credentialed employees who embrace growth. Often these people attend meetings of associations, conferences, and study clubs. The dentist may teach classes, host continuing education classes or
events, sponsor association events, or mentor students in local hygiene or dental assisting programs. The team may also be involved in scouting out potential colleagues when they attend conferences or other events. They may be given a referral bonus if they recruit a successful candidate. These activities build the dentist’s reputation as a supportive and accessible employer and establishes the practice’s reputation as a good place to work.
If candidates are few, the dentist may have to be willing to train potential team members. Working in an area other dentistry isn’t a barrier to being hired. Those who demonstrate exceptional customer service skills in retail, hospitality, or health care situations, for example, may become valued employees in the dental office. The dentist should take note of those who provide this degree of customer service in any situation and invite those who seem to be a good fit to come as patients. If they seem to be a good fit for the practice, the opportunity to work with the team may be offered.
Taking the time and effort to perform all the suggested strategies to reach out to excellent workers should create a pool of potential employees for the dental practice. The dentist should nurture these relationships and build connections, which can be strengthened by sending check-in e-mails periodically or offering holiday or birthday wishes. The dentist can also refer them to colleagues or invite them to events at the practice.
By building a pipeline of potential employees, the dentist can be prepared for the unforeseen loss of an employee and protected from the stress related to short-staffing. Taking these proactive steps can relieve stress and assure excellent patient care.
Weiss S, Perez H: 5 creative ways to “always be hiring” for your dental practice. Dent Econ 115:13-14, 2025
Reprints not available
When there are fewer patients and empty schedules, the dental practice can suffer from a poor bottom line. Returning to the fundamentals is a way to encourage patients to fill those empty chairs and improve the business stats. Several strategies can be used to reach out and draw patients back to their routine dental care or to encourage people who have neglected their oral health to check out your practice.
Returning to the basics can have a significant effect on the production of a dental practice. Strategies to use in the slow times vary from offering new services to revitalizing tried and true ways to encourage patients to come back to their dental home.
Offering only the basics means missing out on opportunities to capitalize on patients’ desire for more options and newer approaches. Adding cosmetic dentistry, clear aligners, dental implants, or sleep apnea treatments can differentiate your practice from others. Including big-ticket and specialized services can attract new patients who want more ways to improve their image. Even adding a free educational workshop or 2 to introduce patients to dental implants or orthodontics will showcase your expertise. Another free service is teledentistry consultations. Virtual interactions can allow patients to try you out without making an in-office visit.
Special pricing and discounts become especially alluring when money is tight, so patients may be eager to save some money. In addition, health savings account balances often must be used or lost, which can encourage patients to book some dental care rather than lose out on their health care bucks.
Referral programs are especially attractive because they encourage current patients to spread the word about the great dentist they have. Incentives for referrals can include a free service or discount. Spreading the word through an e-mail blast or social media post can also net some new leads. Adding a loyalty program that rewards repeat patients can increase the level of success.
You need to take a good look at your practice to see if it’s a place that feels welcoming and comfortable. If it isn’t, now may be the time to spiff up the furniture, add free Wi-Fi or coffee, or paint. Small touches to personalize care for each
patient can make all patients feel valued and remain loyal to the practice. When patients are feeling comfortable and happy, it may be time to ask for a referral or hand them a referral card to complete. Staff members can also be incentivized to make referrals by offering bonuses for successfully spreading the word.
To help patients stay on track with their dental care, you can offer automated referrals vial e-mail or text messages. Patients who miss an appointment can be quickly contacted to fill an empty slot. Having a consistent communication with patients keeps you on their minds. This may include sending out a monthly or quarterly newsletter highlighting new services, promotions, or dental team news, which can encourage patients to stay connected with you.
Your social media campaign should include patient testimonials, before-and-after photographs, and perhaps behind-the-scenes looks at the office. Social media offer easy, free ways to communicate with patients.
Patients who haven’t come in for 6 months or longer may need the push a reactivation campaign can supply. This may be a friendly phone call or e-mail or even a letter to remind them of the need to restart their care. Let them know that you’re still there and ready to help them—and adding a special incentive may seal the deal.
Patients may hesitate to schedule appointments because of the cost, so having flexible payment options can ease their minds. This may involve prepay discounts, an in-house payment plan, or third-party financing, but having a way to make payments easier and more manageable can keep patients coming back. Each patient should have access to all of the available options and should be given simple explanations of how they work. Once they feel they have control over their payment options, patients are more likely to agree to have major procedures.
Membership plans help both insured and uninsured patients by offering affordable and flexible options for dental care. The plans encourage members to stay with the practice especially during slow times, because they recognize the value they are getting. Signing up for the plan can include special offers and use patient testimonials to show how helpful they are.
Patients may be unaware of how great your services are, so it’s time to leverage modern technology so patients can visualize
their dental needs. This can include intraoral cameras or digital imaging—whatever makes them understand the value of your care. Patients need information and explanations to understand the value, so taking time to educate patients, telling them the what and why about each procedure suggested, can pay off in greater trust in your expertise and more acceptance of treatment plans.
Being present in your community is another way to connect with patients and the area where you practice, but it also testifies to the good you are doing for others. You may also want to sponsor local events, set up a booth at a health fair, or host an open house. People who see your name and face associated with good works are more likely to choose you as their dentist.
Slow times don’t last forever, so there will be an end to the challenges they present. Seeing down times as an opportunity to get back to the fundamentals and tune up your systems is a good perspective and helps to engage with current and potential patients. Improving the business’ presence in the community and keeping your name front and center will help to turn the slow times into highly productive seasons.
Wells B: Slow times call for proven measures, Inside Dentist 21:8, 10, 2025
Reprints not available
Having an internal employee manage brand recognition and public perception can be an excellent way to build trust with patients. This employee would manage social media marketing efforts, then develop the ability to helm campaigns that ensure the brand of the dental practice is well-publicized and wellregarded in the community and the dental world. The process of developing an in-house marketing manager was tracked.
The employee tasked with marketing responsibilities should demonstrate loyalty, be genuinely interested in marketing, understand social media, and be a trusted team member. Specific skills he or she should possess include being able to respond to reviews and comments quickly and professionally while using the practice’s voice; having skills in design and a sensitivity to meaningful moments worth sharing; demonstrating the ability to plan and execute content, organize community events, and build relationships with vendors and local media without the dentist’s hands-on oversight; and being excited to learn new skills and use marketing tools that both benefit the dental team and keep the practice current.
Beginning with a few extra hours a week, the employee should be able to manage the essential marketing tasks, including keeping the practice website and Google listing updated and accurate,
managing responses, and creating basic social media content. Posts 3 to 4 times a week can keep the relationship between the practice and patients solid and impactful. Content can include profiles of the providers with current pictures, patient testimonials (with consent), features about services, and contests.
Having an in-house manager allows for ongoing engagement, quick responses to reviews, control over the brand’s appearance and perception, and updated websites and business listings when there are changes in staff, hours of operation, or services offered. Patients will want to see how the practice responds to negative reviews or pubic social media complaints. The marketing manager can discuss these situations directly with the practice owner and employees and post quickly. This individual knows the patients, dentistry, and Health Insurance Portability and Accountability Act (HIPAA) protocols. Having this internal manager allows the dentist and other dental staff to continue to focus on providing needed dental care rather than having to spend time on marketing.
Even when the manager is only functioning on a part-time basis, results can be seen. These include growth in the follower pool, having people engage with content through likes and shares, and providing reviews more often. Compensation for the manager’s efforts can include an increase in hourly pay commensurate with the new responsibilities. This conveys the dentist’s confidence in the manager’s abilities and supports his or her passion to grow both personally and as a practice employee.
With expansion of the manager’s role and the practice’s engagement, the dental team may be free to reach beyond fundamental tasks into more sophisticated strategies. The marketing manager will have expanded responsibilities, including arranging for community engagement, creating and maintaining a consistent brand voice, managing digital advertisements, and running targeted campaigns. The platform analytics can be tracked, and more complex video and educational content can be developed.
The practice should provide for the professional development of the marketing team member through certifications and dentalspecific education. The creation of social profiles and business profiles, website management, and content development are free or cost little. Making these internal investments will provide more authentic results with less outlay for marketing.
Growth in the dental practice can be readily seen and appreciated. The practice will expand, existing patients will remain loyal, and rates of engagement will be beyond expectations. With the growth in followers across the social media platforms, the
practice can expand locations and services, allowing it to reach more patients and provide dental care to them.
Most practices underestimate the value and need for internal marketing, and persons with advanced skills in these areas are rarely seen. However, the internal marketing manager role is becoming critical for growth and success. Having a dedicated employee who can implement a flexible marketing plan will encourage the retention of current patients and expand the new patient population. Through investments in staff and the expansion of marketing capabilities and responsibilities, the practice can see a costeffective growth in its ability to engage with more patients and provide optimal care opportunities.
Nona J: The in-house marketing manager. Dentaltown 26:50-53, 2025
Reprints not available
Artificial intelligence (AI) tools can be used to target patients for marketing messages, personalize content, and analyze phone calls, among other tasks. The use of patient avatars can help the dental office improve many aspects of marketing and patient service, such as creating content, tailoring ads to the patient population, providing valuable feedback, responding quickly without bothering a busy office team member, and tracking calls to identify patterns.
You should begin by uploading an anonymized patient list. It’s vital that all of the data uploaded have been stripped of any personally identifiable information to maintain compliance with Health Information Portability and Accountability Act (HIPAA) requirements. The anonymized information can include demographics, treatment types, and zip codes, which can yield important insights without compromising patient identity. AI can then track patterns such as patient preferences, patient behaviors, age, income, and spending habits and create a patient avatar with the important characteristics of your patients. This “character sketch” of your ideal patient can be used to fashion an
appropriate dental website, create targeted social posts, and even answer the phone in ways that focus on patient needs.
The avatar can also run a check on your website to see if it addresses your target patients’ needs. AI can then give you suggestions for making adjustments that will achieve maximum appeal.
In addition, if your front desk team is busy juggling calls, checking in patients, and handling paperwork, AI chatbots can be trained to answer common questions, book appointments, and provide information about services. Patient calls are answered quickly, which has been shown to be an important feature for 85% of people, whose loyalty can be improved if the practice responds to calls quickly. The chatbot is like having an extra team member who is always available.
It can be taxing to come up with social media content and can require a considerable investment in terms of time. AI can be tasked to fulfill your goal, such as attracting patients who would want implants. AI can create a social media calendar so you have a
30-day dental social media strategy that includes ideas to post, hashtags, and visual suggestions. AI can suggest a mix of educational posts, patient testimonials, and reminders about the benefits of implants. The posts can include short videos or before-and-after images. All are created based simply on your instructions. You should still review it to make sure this approach feels natural. Some AI-generated content can feel too polished or stiff, so you may want to adjust it to make it feel real and relatable.
When crafting ads on Google or social media, it can be challenging to find the right words. AI can generate digital ad copy that fits your audience, giving you several versions. You can test out the variations, ask AI for alternative headlines, and receive tips on which keywords should be targeted.
AI learns from your feedback, so you may not want to simply accept the first response you get. With more feedback, AI offers better choices, eventually giving you just what you’re looking for.
For ChatGPT or any AI tool that is providing unacceptable responses, you should give them a “thumbs down” or simply respond that you don’t like that response. You are then directed to a feedback panel where you can register what you don’t like, if the response wasn’t on target, or if it seemed lazy. The feedback encourages AI to improve and give you more of what you want.
If you are using AI for phone calls, it has the capability of listening to the calls and providing detailed insights. Using real-time call
tracking, AI can review conversations and suggest patterns in patient questions, objections, or scheduling preferences. Reasons for missed appointments may also be identified. All of these insights can help in refining responses, adjusting language in marketing pieces, and handling common questions proactively. This saves time by summarizing what matters the most to you.
The prices of AI tools vary widely. Some AI tools are free and allow you to experiment with patient avatars or create content. If you’re trying out a subscription and in the free trial period, you can try cancelling the trial. Many platforms will offer a discount after cancelling a few times. Prices may actually drop by up to 75%.
AI changes how dental marketing is done today. From functioning as a patient avatar to managing social media, AI provides smarter, data-driven ways to engage with patients. Using these tools can add value to marketing tasks and avoid overburdening the dental team.
Winans X: How AI is changing the game in dental marketing (and how you can use it too). Dent Today 44:8, 10, 2025
Reprints not available
The onboarding process is an essential ingredient in the success of any business, but is especially important for small businesses. Ensuring that onboarding is effective and standardized can optimize the effects of even limited resources and can contribute to a lasting effect on the team. Several strategies can create a positive onboarding process, with some methods helping to prepare for the new hire and others focused on the onboarding process itself.
Onboarding should begin with a welcoming atmosphere for new hires where these individuals feel like they belong from the moment they begin their employment. This requires efforts
before the first day, when they should receive a welcome e-mail, introductions to their future team members, and an outline of what they should expect. The goal is for the first day to be organized and positive so the new employee doesn’t feel overwhelmed.
All of the things a new hire needs should be provided. Their workspace should be orderly, e-mail logins should be set up, and onboarding documents readily available, so that they can feel well cared for. If the new hire is located remotely, video tutorials and helpful resources should be delivered before the first day so the individual can have sufficient information to get up to speed quickly. Small businesses in particular can’t afford to ease into a position. With good preparation, new hires can quickly start contributing.
New hires need to know where they can find answers to their questions. To meet their needs, a system should be in place where they can access information they may need. A centralized digital folder can be created to provide all the key documents that outline everything from office procedures to team contacts. Even virtual employees should be given step-by-step guides and a list of frequently asked questions.
A dynamic, digitized standard operating procedure (SOP) manual should be provided that is easily accessed and continually updated. Having procedures included in the manual will maintain consistency in the work team. The digitized and cloud-based manual allows the new hire to obtain information without constantly interrupting team members with questions or having to rely on verbal instructions or paper copies that may not be as searchable. New hires tend to feel more independent with these resources, and seasoned team members can focus on completing their tasks.
Whatever was promised in interactions before hiring an individual should be honored. The interviewer is setting expectations for what the job will entail, whether that is the salary, benefits, job responsibilities, or flexibility. Promises made during hiring and onboarding should be kept to avoid frustration and a loss of trust and loyalty.
Because everyone learns in different ways, the onboarding approach should be tailored to meet the needs of each new hire. Whether this is a hands-on approach, written instructions, or visual aids, the method should be based on what the new hire shares as his or her preferred training method. It’s wise to ask new hires about their learning style and adapt the process to help them feel more confident and comfortable with the process.
Making a lasting impact on a new hire during onboarding may need to include emotional components. People want to feel
Risk management involves the forecasting and evaluation of risks coupled with the identification of procedures that can minimize or eliminate the impact of these risks. Orthodontic treatment involves some risk. Malpractice claims can be filed by a dissatisfied patient or parent if a problem arises that is related to the care delivered by the practitioner, whereas regulatory complaints
they matter, especially in a small business where everyone is important to the success of the operation. Onboarding is a time to connect with the new hires personally, noting their goals and aspirations and what they need to be successful. Showing genuine interest in who the individual is and not just what he or she does can be highly beneficial for the process. One approach may be to conduct structured reviews after 3 days, 3 weeks, and 3 months from the starting date. These aren’t performance reviews but are opportunities to see how the individual is doing through an open conversation. The new hire should be encouraged to share if added support is needed because his or her growth is an important investment in the future of the business.
To build a strong and successful team, the hiring process should create a welcoming environment, prepare the new hire for success, provide ready access to resources, and foster a culture of trust and growth.
The onboarding process is an essential part of creating long-term success. Not only should onboarding be a time of preparing the new hire to contribute to the vitality of the business, but the new hire should feel valued and connected to the business on a deep level. This will result in engagement, commitment, and loyalty even when resources are limited.
Greenberg J: All on board. Dentaltown 26:54-56, 2025
Reprints not available
are issued by a state dental board or other regulatory body in response to claims the practitioner failed to comply with governing rules. When any of these claims are filed, events are released over which the practitioner has little control, which is why risk management is important. A discussion of the most common causes of malpractice claims, the regulatory complaints seen most often, and how to avoid or mitigate claims was offered.
The most common causes of malpractice claims are undiagnosed or untreated periodontal disease, root resorption, impacted teeth, undiagnosed pathology, and decalcification and caries. Other events can also prompt a malpractice complaint.
The National Institutes of Health reports that 42% of adults over age 30 years have some degree of periodontal disease, with 8% having severe disease. All patients, but especially adults, should undergo screening for periodontal disease before treatment is begun. This screening may be done by the orthodontist or by the patient’s general dentist or periodontist through a referral from the orthodontist. The screening consists of periodontal probing and bitewing and periapical radiographs. Periodontal clearance should be documented in the patient’s chart, with a written communication from the general dentist or periodontist if they did the testing.
Once orthodontic treatment has begun, the orthodontist must continue to monitor the patient’s oral health, particularly if the patient has had periodontal disease in the past. If these measures aren’t taken and disease progresses, the patient can suffer increased bone loss or even tooth loss. The orthodontist will then be held responsible for the undetected disease progression.
Any orthodontic tooth movement can cause shortening or blunting of the roots. The problem is related to many diagnostic and treatment factors, but the orthodontist should diagnose the problem and monitor any root resorption through radiographs. Finding root resorption should prompt changes in the treatment plan to manage the risk of problems once the orthodontic appliances are removed. Patients and parents must be informed of the health of the teeth and supporting structures throughout treatment.
Among the more challenging treatments are those related to bringing impacted teeth into the arch. Often these teeth are engaged with other teeth, so the orthodontist must be aware of the vector of force needed to move the tooth without causing resorption of the roots of adjacent teeth or other problems. The orthodontist must inform the patient and parents about the risks and alternative approaches to recovering impacted teeth before treatment is begun. In addition, the orthodontist should obtain cone-beam computed tomograms of the area to aid diagnosis and treatment planning. In some cases, the teeth don’t move or become ankylosed during movement, with reciprocal movement. In these cases the orthodontist must reevaluate the situation before proceeding further.
Patients and parents should be informed of all these events as they occur.
When the orthodontist doesn’t diagnose pathological conditions, complaints about the care provided can be filed. The orthodontist can take measures to manage the risks, including the following:
• Keep good quality records that include the dental and medical history
• Perform in-person examinations
• Take intraoral and extraoral photographs and radiographs
• Develop pretreatment models
The orthodontist should thoroughly review all of these records, including progress records, and take note of anything that hasn’t been diagnosed. If it remains undiagnosed, a referral to a practitioner who can make the diagnosis is appropriate. However, it’s assumed that orthodontists are able to diagnose any existing pathology in the records or the oral cavity and make appropriate referrals for treatment. They should carefully read x-rays, record their observations in the treatment record, and inform the patient or parent.
Removable clear aligner therapy carries the risk of holding plaque or sugary fluids against the teeth for prolonged periods. As a result, patients who don’t follow appliance care and oral hygiene instructions are susceptible to decalcification and caries development. Patients must be properly educated and the orthodontist must conduct ongoing communication with parents and patients and the general dentist during treatment. Problems should be promptly addressed to prevent any claims against the orthodontist.
Among the other problems for which malpractice claims have been made are excessive enamel removal during debonding, etchant burns, accidental swallowing of appliances, and eye injuries. Many other situations can also prompt claims, but most can be minimized by establishing good quality systems and having properly trained assistants. If accidents happen, the orthodontist must be prepared to manage the situation and ensure emergency care is provided as needed.
Regulatory complaints are often filed by unhappy patients or disgruntled employees. Among the situations in the claims are the delegation of duties beyond the state dental practice act restrictions, improper sterilization, misleading advertising, or other situations in breach of the regulations. When the state
board investigates the complaint, they can examine any aspect of the orthodontist’s practice covered by the dental practice act, regardless of the complaint’s focus. It’s vital that the orthodontist is aware of what’s in the dental practice act and is following the rules.
Orthodontists can avoid or mitigate complaints by communicating clearly and properly with patients and parents, but also by understanding where claims are most commonly raised. Their diagnostic and treatment plans should be well-documented. A pretreatment conference with the patient and parent is required where the orthodontist identifies the recommended treatment, carefully explains the plan, and obtains informed consent. The American Association of Orthodontists and American Association of Orthodontist Insurance Company websites offer excellent informed consent documents. Many cases also should include additional, more detailed informed consent, and the orthodontist should be diligent in obtaining the needed consent.
Orthodontic treatment involves a degree of risk. Orthodontists should use the informed consent documents to initiate discussions of the risks of any proposed treatment so that patients and parents are properly aware of what they are agreeing to have. This discussion or discussions should be properly recorded in the patient’s record to provide evidence of the orthodontist’s careful adherence to risk management procedures.
Roberts CA, Varner RE: What is risk management (and why should I care?) Am J Orthod Dentofacial Orthop 167:379-381, 2025
Reprints available from CA Roberts, 338 Pheasant Run Ln, Findlay, OH 45840-7082; e-mail: crobaanoic@outlook.com
At the Minamata Convention on Mercury, a global treaty was proposed to protect the environment and human health by limiting the use of mercury. In the European Union (EU), the use of amalgam, which contains mercury, has been phased down and will soon be phased out, but the United Kingdom (UK) completed phase-down efforts in 2017 and is focused on completing the phase-down by 2030. In the UK, practices under the National Health Service (NHS) tend to restore posterior teeth using amalgam more often than any alternatives. Composite resin is the only reasonable alternative to amalgam within the time frame for the phase-down and phase-out efforts. Glass-ionomer cements (GICs) and derivatives may offer an alternative for small cavities, but no single material can replace amalgam in all applications. Health systems with limited resources favor amalgam because of the higher costs of alternatives. In addition, the properties and clinical performance of alternatives tend to be less desirable than those of amalgam. Amalgam and alternatives were compared based on their respective clinical outcomes, needed skills and safety, economic costs and comparisons, and the perspectives of patients, clinicians, and other interested parties.
Caries associated with restorations (CARS) is the primary way direct posterior restorations fail, followed by fracture, and pulpal or endodontic complications. The risk of CARS is lower with amalgam than composites, but the evidence remains imprecise, with failure mode differences over time. The differences in clinical outcomes tend to be primarily related to the technical difficulty in performing complete restorations rather than being caused by the use of amalgam.
CARS detection methods are associated with significant diagnostic difficulty, especially when composite restorations are considered. CARS can be seen more often at the gingival margin of restorations, making repeat restoration difficult, especially with composite. A defective restoration may allow an accumulation of biofilm, usually as a result of gaps between the restoration and the cavity wall. Peripheral gaps occur more often with composites because their process is more technically challenging and can predispose to postoperative sensitivity. Cariogenic biofilm accumulation is more likely to occur with composite than with amalgam.
About three fourths of tooth fractures occur in teeth that have 3 or more surfaces restored. Vital teeth are more likely to suffer favorable supragingival fractures than non-vital teeth. Fracture risk is diminished when indirect cuspal coverage restorations are placed in posterior root canal−treated (RCT) teeth and in vital teeth with biomechanical compromise. These restorations are more costly and require more time to place than direct restorations, making it less likely that they will be performed. As a result, tooth survival is reduced.
Amalgam preparations usually are box-like, closed, and upright and include sound tooth structure that provides mechanical undercuts. Composite preparations generally have more flare and are open with a saucer-shaped style, but they lack the mechanical retention form. The composite approach is considered more minimally invasive, but the box-shaped preparations have been reported to offer superior survival compared to the saucershaped ones. However, laboratory studies fail to consistently support this finding and tend to indicate that amalgam restorations have a higher incidence of failure. Often the difference is skewed because the number of amalgam restored teeth tends to significantly exceed the number of composite restored teeth. In many analyses, the difference in failure rates between the materials remains unproven.
Amalgam is compacted with firm pressure into the cavity and expands very little, which results in more precise marginal adaptation and few if any gaps. Composite materials shrink on setting and have a softer consistency that keeps them from adapting during placement. In addition, composite is placed in multiple increments to manage the depth of cure and reduce contraction stress, which increases the chance of gap formation. Specialized equipment is needed to form contact points with composite, also contributing to material fracture, food packing, and CARS.
Bonding agents are applied to the tooth to prevent composite from pulling away from the cavity walls during polymerization. However, the bond can be compromised by numerous factors. Cavities whose margins are located subgingivally are especially challenging. Complications include incomplete light curing of
composite, washout of uncured components, and gaps after degradation of the composite bond over time. Amalgam restorations don’t require these measures and have fewer sensitivities to technique.
Posterior composite restorations require significantly more time to place than amalgam restorations. Many UK primary care dentists feel there are too many choices to consider when composites are indicated and that the recommended equipment is relatively expensive. As a result, private practice practitioners tend to be the only ones who follow the NHS recommendations (Appendix 1). Some health systems charge a fee for placement of a rubber dam (RD). When more tooth structure is lost and the margins extend more deeply into subgingival areas, placing a well-adapted matrix-wedge assembly to directly restore a tooth becomes considerably more challenging. Amalgam is often preferred for these situations because marginal seal adaptation isn’t as critical as it is with composites.
Most primary care dental practitioners in the UK are confident placing posterior composites in standard situations, but about two thirds of 1500 practitioners who were surveyed had no or low confidence placing composite in patients with limited cooperation. Only 7% of this group felt uncomfortable with amalgam placement. Restorations of subgingival cavities with composite sparked low or no confidence in over half of practitioners, but only 4% of practitioners were troubled when amalgam was used. This may indicate a failure in the education of dental professionals regarding the use of composites for such situations.
Most new UK graduates have predominately used composite during their undergraduate experiences, but when they are trained under NHS provisions, they place more amalgam. Predictors of low rates of postoperative issues are being trained with composites for total posterior restorations and not using liners, but using sectional matrices. These practitioners are confident when placing subgingival composites, tend to use an RD, and are usually private practice dentists. The NHS incentivizes using amalgam, usually based on the relatively large discrepancies between the remuneration for composites and that for amalgam.
When a restoration fails, the provider must consider the longterm impact of the restoration on that tooth. Removing composite restorations is consistently more time-consuming, involves the removal of more sound tooth structure, and leaves more of the existing restoration when compared to the removal of amalgam restorations. Repair is arguably less destructive of tooth tissue than replacement and can slow the restorative cycle. How often repair is done by primary care UK dentists rather than removal and replacement is uncertain, with limited evidence available.
The evidence shows no clinically significant differences in the safety of amalgam versus that of composite for patients as well as for dental personnel. A localized lichenoid reaction in the mucosa adjacent to amalgam restorations occurs in rare cases. Reports of resin allergy among patients and dental personnel remain to be investigated. Health concerns regarding the monomers used in composite and the inhalation and ingestion of microplastics haven’t yet been studied.
Nearly all health care systems show that posterior composite restorations require more time and cost more than amalgam. This tends to disincentivize their use. Remuneration of NHS dental care is considerably lower in the UK than in the rest of Europe. Fees paid to dentists for treatment should be increased to help retain dentists in NHS practices, with the loss of dentists posing a significant problem.
Economic evaluations (EEs) can be based on data gathered from a clinical trial over the course of that trial or extrapolated over a lifetime using modelling techniques. All EEs and health technology assessments (HTAs) comparing amalgam with composite posterior restorations show amalgam is more effective in terms of restoration and tooth survival and less costly. Models simplify the restorative cycle and use data sources to inform how restorations fail, both of which aren’t relevant to the UK primary care perspective. Up-to-date information on restorations placed under NHS provisions in England and Wales remains limited.
Previous EEs focus on the survival of restorations and teeth, which are clearly important to stakeholders. However, composite and amalgam restorations vary in ways that are important to patients, clinicians, and others, such as those who pay the bills.
Cost remains the most important factor when patients choose a restoration. Composites offer patients clear aesthetic benefits, with patients willing to pay to have a white compared to a silvery-gray restoration. They are also willing to pay twice as much to have no postoperative pain, about the same amount for the restoration to survive 14 years instead of 5 years, and the same for the wait to be reduced from 6 weeks to 2 weeks. Most favor the use of amalgam for cost’s sake, but the other factors noted must be taken into account if patient satisfaction and uptake of services are valued—which they are. Patients can benefit if interventions are done before more advanced disease develops, avoiding pain, morbidity, and higher costs for treatment. Cost can be direct and out-of-pocket for the patient and insurer, but it can also be indirect and involve the loss of
work, a resulting effect on the employer, and an impact on the general productivity of society. Traditional EEs only consider costs from a single perspective. Indirect costs are seldom accounted for in evaluating restorations.
Patient access issues are at risk if evaluations don’t consider or value clinician perspectives. When practitioners aren’t valued, they may leave health services or their time demands may result in long waits for care. Dentists are leaving the NHS in record numbers because of remuneration issues as well as a loss of trust in the NHS after the new contract. Composites take longer to place, longer to replace, and will likely need more frequent replacement than amalgam. In addition, the cost of composites is higher than that for amalgam, although the EU ban may change that. The majority of UK primary care providers believe that an amalgam phase-out will impact their ability to do their job, create delays in care, and lead to a need for more indirect restorations and extractions. This would tend to exacerbate the current access issues.
Some Canadian HTAs find that the environmental impact of mercury released from amalgam is small. Although amalgam separation, disposal, and crematorium costs have been considered, the actual impact from composites remains unknown. Other potential environmental issues and costs associated with composite restorations must be further investigated.
Another perspective is related to which patients will be most affected by the phase-down and phase-out of amalgam. Generally, those most in need will be preferentially affected, and this includes those of low socioeconomic status, those with disabilities, and older patients, who often have comorbidities. Amalgam performs better in patient groups at high risk for caries.
The appearance of restorations tends to be less valued among lowincome groups than in higher-income groups. Phasing out amalgam risks access issues because of the increased clinician time needed to place composites and perform replacements, the loss of workforce numbers from public to private practice, and an increased cost shouldered by the patient. Treatment uptake would be reduced, leading to more significant dental disease, greater morbidity, loss of productivity, and wider health inequalities.
The current phase-down of amalgam use is being accomplished by using amalgam only if it’s deemed strictly necessary by the dental practitioner based on the patient’s medical needs. Primary care clinicians believe that placing an amalgam restoration in children or pregnant patients carries a risk for them, one they don’t care to bear. The consent process is compromised, as is the justification for use and the support provided by an indemnifier if a complaint arises. The shared decision-making process is
compromised as well. High-caries-risk children, whose cooperation can be limited, will be affected.
The ultimate goal of a minimal intervention philosophy is a cavityfree future where restorations are unnecessary. This would eliminate the need for any phase-out or phase-down for restorative materials. Composite may be selected for its ability to adhere to tooth structure and allow more minimal tooth preparation, provide a tooth-colored option, and result in high levels of patient satisfaction. This future isn’t reality and doesn’t face the fact that most of the health care systems’ constraints tend to favor the use of amalgam. Alternatives need to be developed that will have minimal environmental impact. The techniques used to restore various cavity presentations with composite require training so practitioners can use them in difficult situations. Organizations such as the NHS need to clearly define their goals and design a service that incentivizes the achievement of the goals with minimal unintended consequences.
Amalgam offers a simpler, quicker, and more costeffective option to place and replace restorations compared to composites. Fewer postoperative complications are also associated with amalgam. Composites can be effective for extensive cavities but require practitioners to develop more extensive skill levels and involve the use of expensive, timeconsuming specialized equipment that is seldom available in NHS dentist offices. With its low remuneration and the disincentivization of recommended expensive and time-consuming equipment for composite, the NHS is probably contributing to dentists failing to develop the greater skill levels composites require and is instead incentivizing the use of amalgam. In addition, patients have limited access to care, with those at greatest need disproportionately affected. An oral health crisis in the UK may be on the agenda if amalgam is phased out in the near future.
Bailey O: The long-term oral health consequences of an amalgam phase-out. Br Dent J 238:621-629, 2025
Reprints available from O Bailey, School of Dental Sciences, Newcastle Univ, Newcastle upon Tyne, UK; e-mail: Oliver.bailey1@ncl.ac.uk
Key: *, ≥ 76% use rubber dam, no liner, wedge; ≥ 51% use sectional metal matrices. **, P<0. 0001 (Chi2). NHS, National Health Service. CDS, Community Dental Services. (Reproduced with permission from Bailey O: The long-term oral health consequences of an amalgam phase-out. Br Dent J 238:621-629, 2025.)
Nearly 1 of every 2 people in the United Kingdom (UK) are expected to be diagnosed with cancer over their lifetimes. No good data indicate how many dentists will be diagnosed with cancer each year, but the number of cancer patients overall who return to their work is low, with clinical and psychological barriers contributing to these low numbers. Cancer treatment causes significant physical side effects that can make work attendance difficult. Mental health challenges are also seen in cancer patients and include anxiety, low self-esteem, and fear of discrimination. In addition, societal and professional stigmas regarding the cancer diagnosis are also seen. Becoming more aware of the adjustments promised to cancer patients by law and how cancer patients must manage the return to a workplace after or during treatment should help eliminate these stigmas. In addition, employees, colleagues, and cancer patients should be aware of the efforts being made to provide more support for patients who choose to return to employment after a cancer diagnosis.
Cancer patients are legally classified as disabled in the UK, which protects them from discrimination in the workplace. Employers are required to make reasonable accommodations to support employees during or after cancer treatment. Dentists diagnosed with cancer can opt to reduce their working hours; transition to an administrative, managerial, or teaching role; develop an extended return-to-work plan; or modify the practice so that appointment times are longer or treatments they deliver are less physically demanding. Those who manage the dental practice should facilitate an open discussion with employees with a cancer diagnosis to identify their ideal working arrangements. To
date, no large-scale studies have tracked how these adjustments have actually been implemented.
The UK’s General Dental Council has no specific policies regarding cancer but principles addressing safe patient care and fitness to practice apply. If a dentist is struggling with health issues and needs help in managing a practice while undergoing treatment, he or she should seek support and advice from relevant professional organizations as well as colleagues.
Many dental practitioners diagnosed with cancer cannot see how they can work during their treatment period. Yet even those with advanced cancer can benefit from a sense of purpose and of normality in the midst of their treatments. Connecting with others in the dental practice sustains a sense of identity and helps them feel a sense of accomplishment.
The cancer diagnosis also helps to reset priorities that are no longer sustainable. Patients may better understand the importance of balance, health, and celebrating the joy of living both personally and professionally as they go through the cancer experience.
A recent survey of more than 1200 working-age cancer patients found that these individuals face significant challenges when trying to remain employed. Fewer than two-thirds of cancer patients are still working or have returned to work 1 year after diagnosis. Financial difficulties and poor mental health can develop. In many cases, respondents said their medical teams or occupational health professionals didn’t discuss their Appendix 1. High advocated composite technique use by UK primary care clinical type
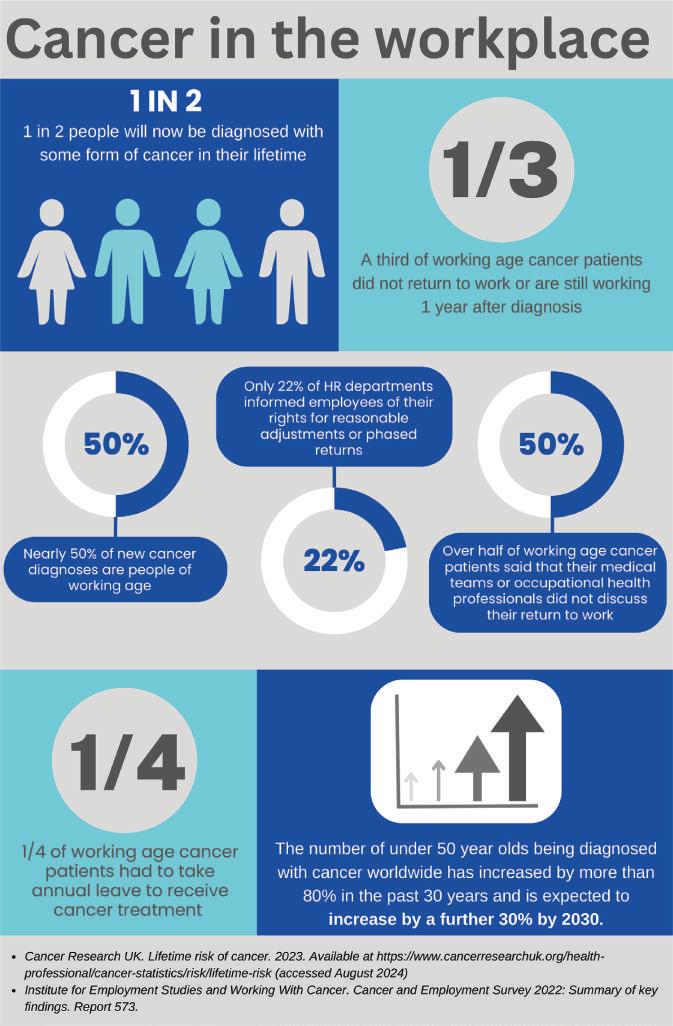
return-to-work options, and only 22% of the human resource departments informed patients about their rights to reasonable adjustments and phased return policies. In addition, about 25% of the patients had to use annual leave to receive their vital cancer treatment (Figure 1). These experiences indicate a systemic failure in supporting cancer patients in the workplace.
To offer employees undergoing cancer treatment and recovery a better experience will require employers to go beyond personal
compassion and adapt strong job redesign principles. For example, they should revise their policies to include written blueprints that reorganize tasks to reduce workloads and work intensity, develop phased return-to-work plans, and introduce vocational rehabilitation as an option for workers. The implementation of these plans should include comprehensive plans, preparation, capacity building, education, and awareness in the management team and a plan for empowering cancer patients to voice their specific concerns and needs. Often the employee is the best resource for determining how to craft a successful
Figure 2. Top tips for employers, colleagues and employees with cancer. (Reproduced with permission from Lockstone A: Cancel the cancer culture! Br Dent J 238:378-381, 2025.)
return to work. Employers need to ask, listen, and adapt to the needs of the employee undergoing cancer treatment.
Management team members should also understand that working-age cancer patients have a significant fear of losing job connections, experiencing a decline in their employment status, and suffering a loss of income because of their cancer diagnosis. To address this, any return-to-work plan should include a structured approach for a successful return to work as a high-priority and therapeutic component of the patient’s journey.
Plans should also recognize that each person’s experience with cancer is unique and involves variations in treatment plans and responses. The impact of returning to work will vary depending on cancer type and stage, age at diagnosis, treatment regimen, and the demands of the work situation. Dentistry is physically demanding and involves long hours of bending, precision handwork, and patient interactions. Some cancer treatments may not allow the individual to perform the job and will require the person to take time off work. Dentistry also involves sustained concentration and high-pressure situations. Some treatments can cause side effects such as fatigue, nausea, immune suppression, and cognitive changes that interfere with the ability to return to work. Cancers that involve a compromise of speech, swallowing, and performing the work required in dentistry may complicate the individual’s ability to return to the job. Sometimes the mental health consequences of treatments are significantly worse than the physical effects, and this must be recognized and managed.
Medical and dental professionals tend to believe that they should never become sick or take days off because they don’t feel well. This is outdated and unrealistic, as having a diagnosis of cancer will reveal. These professionals must, however, recognize that having cancer doesn’t mean losing clinical capabilities and rational decision-making abilities. Conversations with fellow employees shouldn’t be centered around cancer, but should be normalized
to everyday interactions. Having normal conversations is one of the primary reasons patients with cancer want to continue working.
Organizations such as Working With Cancer are advocating for more support for employees and employers. Dedicated cancer policies for the workplace are prioritized with the goal of eliminating any stigmas associated with cancer. For example, having a minimum of 12 weeks for a phased return should be adopted rather than the standard 4-week period currently used. Employees, colleagues, and cancer patients should be aware of the tips that can help in erasing stigmas and facilitating a return to work (Figure 2).
Society and professional training contribute to the presence of stigmas associated with a cancer diagnosis, especially in a working-age individual whose profession is in a health care field such as dentistry. Cancer patients need to be empowered to adapt their working life to their personal life while they are undergoing treatment and afterward. Engaging in open dialogue with employers and management should redefine how cancer is viewed in the workplace, making the cancer diagnosis a journey that is better understood by those in the dental workplace.
Lockstone A: Cancel the cancer culture! Br Dent J 238:378-381, 2025
Reprints available from A Lockstone; e-mail: alice.lockstone2 @wales.nhs.uk
A comorbidity is an unhealthy condition that coexists with other diseases. It can include diseases from various causes and is often related to inflammation, infection, and environmental and lifestyle responses. Two or more medical conditions coexisting with a primary diagnosis or diseases that occur at the same time in an individual are comorbidities. The diseases can occur separately or as a result of one another and can interact or change the trajectory of a medical condition. Periodontal disease is the sixth most prevalent disease in the world and develops in the oral cavity, where the second largest concentration of microbiota of bacterial species dwells. A review of the manifestations of periodontal disease and a proposal to consider it a comorbidity were offered.
Periodontal disease is a broader name for gum disease and includes such subclassifications as gingivitis, severe periodontitis, acute to chronic types, aggressive to slow-acting over time, active to stable, plaque- and nonplaque-induced, and localized or generalized. Its presence can increase systemic risks, but it can also be a part of the multiple systemic diseases that occur in humans. It involves inflammatory conditions that affect the soft and hard tissues around teeth. Its development depends on many factors, including host response, lifestyle, habits, genetics, medical systemic risks, overall oral health, infection, and the immune response.
Defining Morbidity and Comorbidity
Patients often ignore the dental professional’s words regarding their periodontal health, but considering it a comorbidity in the body may be a way to bring their attention to focus on how they care for their oral health. The morbidity realm consists of several components, such as the following:
• Morbidity is the state of having a specific disease or medical condition, whether mental or physical. When it worsens, it affects both the person’s health and his or her quality of life.
• Multimorbidity refers to having at least 2 chronic medical diseases that last more than 1 year. Multimorbidity decreases the patient’s already poor quality of life and increases the chances he or she will die prematurely.
• Mortality is death, which accompanies many comorbid conditions. Comorbidities tend to make mortality more likely to occur.
• Co/multi/morbidities are defined as diseases and medical conditions. A disease is an abnormal condition in a person’s body that results from various causes, including infection, inflammation, environmental influences, or genetic defects. A specific set of signs, symptoms, or both is characteristic of a disease. In contrast, a medical condition is a disease, illness, or injury that affects the physiologic, mental, or psychological systems of the body. However, a state of health, physical fitness, and an ailment can also be medical conditions.
Comorbidities occur through the interrelatedness of organ systems, the infection route, and the effects on multiple organ systems. Comorbidities involve chance occurrences between 2 conditions, overlapping risk factors, the relationship of a condition to the complications of another condition, and the possibility of a third condition causing the other 2 conditions.
Periodontal disease usually occurs in association with an inflammatory response engendered by a population of bacteria that triggers the immune system to respond. Cytokines and proinflammatory mediators are released, creating bone and tissue loss. As a low-grade infection, periodontal disease contains pathogenic bacteria that are spread through the body when the individual swallows, inhales, or has bacteria living in infected pockets. This spread of the infection compromises areas of the body that are susceptible to them but also can complicate other comorbid conditions.
To resolve the infection and maintain a healthy oral cavity and minimize bodily conditions, the individual must be treated. Once periodontal disease is present, it tends to recur, just as heart attack survivors are at risk for more heart problems to occur.
Not only does periodontal disease involve a host of local complications such as tooth and bone loss, gingival recession, abscesses, halitosis, pain, acute and chronic infection, tooth migration, and tooth mobility, but it also increases the number of complications systemically. The 10 most prevalent and costly chronic diseases are obesity, hypertension, high cholesterol, coronary heart disease, chronic obstructive pulmonary disease, asthma, chronic kidney disease diabetes, cancer, and depression. Periodontal disease is linked to all of these diseases.
By considering periodontal disease a comorbidity, both patients and physicians may regard its prevention and treatment as more important to the patient’s overall health. Improved oral health is an approach to avoiding the development of periodontal disease and maintaining a healthier overall status. This would eliminate periodontal disease from becoming a comorbidity of the patient’s other disease states.
James L: Periodontal disease: A co-morbidity? RDH Mag 45:23-25, 2025
Reprints not available
The current dental school tuition results in new graduates beginning their professional careers with substantial educational debt. In addition, dental wages have remained stagnant for several years, so that nearly two thirds of the dental graduates in 2001 still had a mean educational debt of about $108,000 in 2013. Decisions made after graduation can affect dentists’ career moves, including whether to specialize or work longer hours and when to retire. The US Bureau of Labor Statistics and the American Dental Association (ADA) cite expected dentists’ salary ranges per year as $100,000 to $300,000 within 5 years of graduation. Several variables determine dentists’ wages and should be considered when making career decisions. Dentists freely choose some of these situations but other variables are intrinsic to the dentist’s identity.
Location
Graduate dental students face the choice of practicing in a metropolitan or nonmetropolitan area. A metropolitan area has a high degree of social and economic integration and is an urban area with at least 50,000 inhabitants. The mean annual wages of dentists in metropolitan and nonmetropolitan areas (Figure) both follow a bell curve distribution, and dentists in both areas have comparable wages. The peak is about $200,000. Dentists also have wages comparable to those of most other health care professionals (except for pharmacists). US dentists working in areas designated a dental care Health Professional Shortage Area (HPSA), which has a population-
to-provider ratio of at least 5000:1, don’t differ significantly from those working in areas with smaller population-toprovider ratios.
The wages of specialists in dentistry are higher than the mean wages of general dentists (Table). Oral and maxillofacial surgeons earn the highest wages of all dental provider groups, with a mean annual wage of $334,310. Orthodontists earn a mean annual wage of $243,620 and prosthodontists $240,750.
Because of shifting practice modalities, greater consumerism, technologic innovations, and payment reforms, the dental practice model is evolving. Practice ownership by dentists is falling, with about 85% in 2005 but just 73% in 2023. Instead, dentists are more often deciding to associate with dental service organizations (DSOs), with these associations increasing from 10% in 2019 to 13% in 2022. In 2017, about 43% of US dental school seniors planned to work as an associate in an existing practice with a single owner dentist. By 2023, 36% of dentists were in 1 location with 1 dentist, 40% in 1 location with more than 1 dentist, and 10%, 3%, 2%, and 9% in locations with 2 to 9, 10 through 49, 50 through 99, and 100 or more dentists, respectively. It’s now more common for new dentists to practice in larger groups and belong to a DSO.
The median annual net income of dentist owners in single-owner practices is $172,040, whereas dentists in co-owned practices have a median of $230,070 and dentists who are employees earn a median of $168,390. Dentist employees of DSOs often
Figure. The y-axis denotes the percentage of areas (metropolitan or nonmetropolitan) where dentists work and the x-axis denotes the mean wages generated per dentist in those areas. Distribution of mean wages of dentists working in metropolitan and nonmetropolitan areas, analyzed according to data from the Bureau of Labor Statistics 2023, released in 2024. (Reproduced with permission from Park D, Gong S-G: Factors affecting wages of dentists in the United States. J Am Dent Assoc 156:277-280, 2025.)
receive benefits, including health and malpractice insurance, reimbursement for continuing education, offers of transitioning from associateship to ownership, and stock ownership. These benefits could add a value of about a thousand dollars a month to the associate’s salary.
New dentists may also choose to work in public health−facing units such as the Veterans Administration (VA) clinics and
Table. Mean Annual Wages of Dentists and Dental Provider Types.* Data from Occupational employment and wages, May 2023. US Bureau of Labor Statistics. Accessed June 23, 2025. https://www.bls.gov/oes/current/oes291021.htm.
community health centers that function in underserved areas. Legislation has established more standardized and competitive wages for these workers, comparable with national private practice earning averages.
The ADA reports an increase in the numbers of women entering the dental workforce, rising from about 16% in 2001 to nearly 37% in 2023. Pay gaps exist between male and female dentists, with women making just 79% of what men made in 2022. Reasons for the discrepancy have included suggestions that female dentists perform fewer surgical and more preventive procedures than male dentists, are more willing to accept lower financial compensation, are more likely to accept and treat Medicaid patients, and are consistently less likely to own their dental practice. Even so, much of the discrepancy remains unexplained.
* Source: US Bureau of Labor Statistics. (Courtesy of Park D, Gong S-G: Factors affecting wages of dentists in the United States: A guide for the graduating dentist in making career choices. J Am Dent Assoc 156:277-280, 2025.)
Greater diversity in dentists has also increased, with Asian dentists increasing from about 12% in 2005 to 18% in 2020. However, the percentages of Black and Hispanic dentists have remained steady. The earnings differences between White and non-White dentists as well as visible racial and ethnic minorities cannot be explained by differences in skill level, educational level, or location.
It’s hard to know how much dentists will be paid because of the variables that enter into the equation and changes in the make-up of the dentist population, among other factors. Dentists should be realistic about their expectations for their wages. In addition, it’s estimated that there will be a surplus of dentists by 2040, with the number of new dentists exceeding the loss of older dentists, so that eventually the dentist-to-patient ratio will exceed the growth in the US population. At that point, factors other than compensation may need to be considered. Already, some workers have found that factors such as relationships and balance in life, may contribute more to having a fulfilling career than what they are being paid.
Human trafficking is often concealed by the traffickers and overlooked by health care providers. From 50% to 80% of survivors have reported attending health care provider appointments during the time they were in captivity, with 27% seeing a dentist while being trafficked. Dental professionals are in a position where they can recognize and respond to trafficking victims, then report cases to authorities. To be effective in addressing human trafficking, the dental practitioner should be aware of what human trafficking involves and who might be victims or perpetrators, recognize the signs during dental care delivery, and understand how to report cases to authorities and how to support a trafficked individual. Taking a trauma-informed care approach can help to guide interactions between the dental team and patients.
Millions of people are trafficked globally every year, with many cases not reported. Traffickers exploit the vulnerabilities of their victims, including their unstable economic status, immigration status, homelessness, or previous trauma. In cases of human trafficking, individuals are exploited through force, fraud, or coercion for various purposes. The most common purposes are forced labor and commercial sex. Labor-trafficked individuals are often promised a better life but are subjected to extreme working conditions with little or no pay and can be physically abused by the traffickers. Sex trafficking employs various means
Park D, Gong S-G: Factors affecting wages of dentists in the United States: A guide for the graduating dentist in making career choices. J Am Dent Assoc 156:277-280, 2025
Reprints available from S-G Gong, Orthodontics Program, Faculty of Dentistry, Univ of Toronto, 124 Edward St, Toronto M5G 1G6, Ontario, Canada; e-mail: sg.gong@dentistry.utoronto.ca
to trap an individual and force him or her into performing sex acts. The purpose can be pornographic videos or the pleasure of other individuals or the trafficker. Any person under age 18 years who is involved in a commercial sex act is considered to be trafficked even if force, fraud, or coercion isn’t present.
Several misconceptions exist about human trafficking. First, people needn’t be kidnapped or taken across borders to be trafficked. Human trafficking doesn’t require any movement and can occur anywhere—suburbs, rural areas, urban areas, or even a home. Second, the traffickers are often known by the victims and may be family members, partners, or acquaintances who the victim met online. Kidnapping by strangers for trafficking is rare in the United States compared to the number of victims who know their trafficker.
The victims include all genders, races, ethnicities, and ages, with the common factor of being vulnerable. Children, young adults, those who are impoverished, immigrants, LGBTQ+ individuals, and disabled persons are among the most vulnerable persons. Traffickers use these unmet areas of need to control victims’ lives.
Perpetrators may be individuals with money, power, and prestige but may also be street pimps, family members, intimate partners, employers, and persons in organized criminal organizations. Often traffickers blend into society and are unrecognized as threats. Perpetrators may accompany victims to health care
appointments or take on the role of a legitimate employer. Dental clinicians and law enforcement individuals can find it difficult to identify them when they take these roles.
Dental professionals should be aware of indicators that suggest trafficking is taking place. Physical and behavioral indicators can provide clues to identify victims and perpetrators. Physical indicators include untreated dental conditions or advanced decay caused by neglect or signs of physical abuse such as bruises, scars, or burns in the mouth or face area. Oral trauma can indicate abusive behaviors. Behavioral indicators may be a patient who is unusually anxious, withdrawn, or fearful, especially when the controlling person is present. Victims may not know their personal information such as their address or employment history. Often the companion insists on answering questions, refuses to leave the room, and controls the patient’s documents, which is the primary sign of a trafficking situation.
Dentists and other dental professionals should employ traumainformed care principles when interacting with these patients. This approach shows the patient that the provider understands the prevalence of trauma in society, its impact on people, and the need to avoid more trauma.
The principles to be followed in trauma-informed care are safety, trust, and empowerment. Safety means ensuring the environment is both welcoming and nonthreatening. In building trust, the provider is being transparent about his or her intentions, respectful of the patient’s boundaries, and honest about the resources that can or cannot be offered. The environment offers empowerment by focusing on the patient’s autonomy and ability to make decisions.
Each person is approached as a potential trauma survivor, with the clinician remaining focused on the patient’s needs and taking care to avoid actions that trigger a trauma response. Traumainformed care shifts the focus away from being a rescuer to being a provider. In this role, the clinician creates a safe, trusting environment where the patient feels heard and seen. Listening to the patient without judgment or unsolicited advice can encourage survivors to seek resources or take steps that will allow them to escape the trafficking situation.
Screening should be performed to provide information that will indicate if trafficking is involved. Interviews of the patient should be conducted in private settings so the patient can speak freely. The questions and statements should be open-ended and neutral, with judgmental terms or assumptions avoided. Listening without judging and resisting the temptation to inject opinions or ideas will make the patient more comfortable. Patients who view the clinician as nonjudgmental and compassionate are more likely to share their circumstances and allow the clinician to offer them information about available resources that may be accessed. The clinician
should focus on supporting and providing helpful information rather than rescuing the individual.
Suspected trafficking cases should be reported in response to ethical and sometimes legal requirements. The steps to take include the following:
• Observe and document. Detailed notes should be taken that objectively document physical, behavioral, and contextual indicators without judgment.
• Consult with team members. Concerns should be shared with colleagues or supervisors to identify the best action to take.
• Contact authorities or hotlines. Law enforcement, child protective services, or the National Human Trafficking hotline should be contacted for guidance regarding the next steps. For minors, the state’s mandatory requirements for reporting abuse should guide the next steps. For adults, the state trafficking reporting laws should be observed, while recognizing that involving law enforcement may not always be the initial step and may actually exacerbate the situation. Hotlines can offer advice in cases where imminent danger isn’t a concern. The patient may have explicitly requested law enforcement involvement. Adults shouldn’t be pressured to call a hotline or seek help.
A report may raise challenges, such as fear of retaliation or harm to the victim, lack of concrete evidence, or reluctance of the patient to disclose or engage with law enforcement individuals. The trafficker may also refuse to leave. The guiding focus should be the safety of the patient and the office staff.
Various organizations also offer resources for dental professionals, such as hotlines, continuing education sources, training and support, and providing printed resources for patients to take with them.
Dental care providers should be aware of the possibility that a patient is being trafficked and take a traumainformed care approach. Dental practices should establish a plan of action that includes training for all team members so that they are comfortable asking screening questions and identifying any suspicious situations. Guidance for such plans can be obtained through various organizations, such as healtrafficking. org.
Swarthout K: A hidden crisis: Human trafficking and the role of dental professionals. RDH Mag 45:41-43, 2025
Reprints not available
More elderly patients are being seen in dental practices because of their improved socioeconomic status allowing greater access to health care and the advances in medical care that is allowing people to live longer. However, many of these older adults come with compromised medical conditions, which are often systemic and chronic diseases. As a result, the initial diagnostic process for beginning dental care should document any known medical conditions and prompt vigilance in observing patients to see if undiagnosed conditions may also be present. Systemic conditions may manifest through oral symptoms, so dental


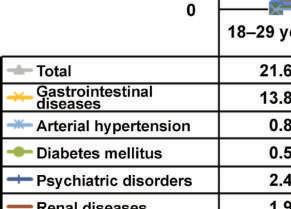
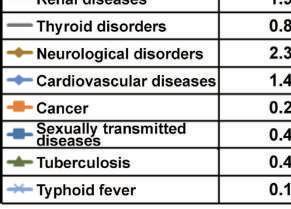
care practitioners are poised to identify comorbidities during their care process. Periodontal disease has a substantial impact on both one’s oral health and on general health and well-being, but is also believed to be associated with chronic degenerative conditions, cardiovascular diseases, and autoimmune diseases. The prevalence of systemic diseases in a large population of patients seeking dental care was investigated.
A total of 82,363 patients living in San Luis Potosí, Mexico, were selected for this review of dental school patients who came for


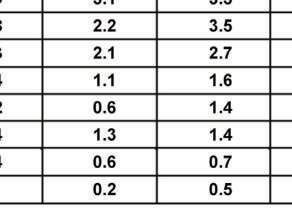



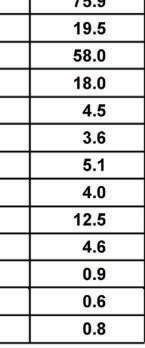
care between 2011 and 2019. The electronic medical records of these medically compromised patients gathered during a personal interview before care began were analyzed. The data included the patients’ age, sex, and general health.
The patients ranged in age from 18 to 107 years, with a mean of about 40 years. Nearly 63% of the sample were female. The primary reasons for seeking dental care were routine checkups, acute oral pain, infection, and dental rehabilitation.
Overweight was seen in 40% to nearly 45% of the patients age 30 to 79 years and in 39% of those age 80 years or older. Most patients denied smoking cigarettes, consuming alcohol, or taking illicit drugs.
About 13% of the population had more than 1 systemic disease. The overall prevalence of medical conditions was about 39%, with the highest prevalence seen in 2018 at about 41%. The conditions seen most often were gastrointestinal diseases (16.5%), with gastritis seen in 56% of these patients and colitis seen in 34%. Other conditions included arterial hypertension (14.1%) and diabetes mellitus (8.6%). The gastrointestinal diseases were reported across all the age groups, but the prevalence of hypertension, diabetes mellitus, and psychiatric disorders increased with the patient’s age (Figure 3).
Dentists are likely to see many patients who have comorbid conditions, so they should be prepared to treat them
appropriately. Many systemic disorders have an impact on and can be influenced by the patient’s oral health. All patients should undergo a personal interview during which the dental care provider collects a thorough medical history, performs a physical examination, and prepares to manage the patient holistically.
About a third of the patients seen had comorbidities, so dental undergraduate students should be trained to be able to detect and diagnose systemic disorders as part of the dental care protocol. This is especially needed for adult and older adult patients. In addition, researchers should continue to analyze the electronic medical records of patients who come for dental care to identify any changes in the prevalence of systemic comorbid conditions. The data can be used to develop reports and studies especially of older adults, with a focus on primary diseases that are related to the oral cavity.
Romo SA, Amaya-Larios IY, Macías KL, et al: Prevalence of systemic diseases in 82,363 patients at a dental school in San Luis Potosí, Mexico: A cross-sectional study. Dent Med Probl 62:31-39, 2025
Reprints available from SA Romo; e-mail: sarayaranda@fest.uaslp.mx
Odontogenic pain can have several causes and requires careful evaluation of the situation. Pain relief is the first priority, along with the drainage of any pus associated with an acute dental abscess. A plan must be developed to determine if the teeth can be restored and what follow-up care will be required. The goal is to effectively address the endodontic issues so that teeth that can be retained will be pain free and functional. Obtaining access to the cavity is the essential first step, with conservative treatment dictating the removal of some or all of the coronal pulp when there is vital but inflamed pulp remaining, followed by comprehensive care, including restoration, achieved in a single visit. In most cases, an access cavity preparation is created in association with coronal pulpotomy or total pulpectomy and temporization, so that root canal therapy can be done at a later appointment. If dental trauma has occurred, guidelines should be consulted to determine if root canal treatment is needed and when it should be done. The process of achieving endodontic access to the cavity was detailed.
Initial Areas of Concern
Endodontic treatment begins with accessing the pulp’s coronal area to identify the main root canal anatomy and perform biomechanical disinfection of the root canal system. Endcutting and non-end-cutting burs (Figure 1) are used to achieve this. The end-cutting burs cut through enamel, dentin, and restorative materials to access the coronal pulp chamber. The clinician then uses non-end-cutting burs to unroof the pulp chamber. This allows him or her to locate the canal orifice(s) and establish straight-line access. Once this is done, subsequent procedures can be undertaken, including coronal flaring, creating a reproducible glide path, calculating the working length of the bur, and carrying out biomechanical preparation and disinfection. Guides to the expected dental anatomy (Figure 2) allow correct selection of the bur or burs. The clinician should also consider the fact that the access cavity preparation depth varies depending on the depth of the coronal pulp horn and whether the tooth exhibits worn, heavily carious, or heavily restored qualities or has receded, with secondary or tertiary dentin deposition.
Access cavity preparation can be influenced by tooth factors, patient factors, and operator factors. Tooth factors include the significant variation seen in tooth anatomy, with crown morphology and the presence or absence of direct and indirect restorations complicating pulp chamber and root canal identification. Sometimes pulp chambers and canal orifices are obstructed by pulp stones, calcification, or cutting debris from the access cavity preparation. When accessing through indirect restorations, the excessive removal of restorative material and dentin can compromise the integrity of the restoration and cause fractures, chipping, or dislodgement. The tooth’s position in the arch can also be a factor, with posterior teeth suffering from decreased accessibility and visibility. Tooth inclination and rotation can alter orientation and increase the risk of perforation. Some teeth have poor-quality dentin, short clinical crowns, and obliterated root canal anatomy. In these situations, it can be challenging to identify the original root canal.
Patient factors can include physical limitations, including an inability to recline in the chair, which can restrict access and visibility. Some patients are anxious or have a strong gag reflex, especially if posterior teeth are involved. Having a mouth opening less than 25 mm can make treatment difficult, with poor access and visibility along with greater stress on the instruments.
Operator factors such as limited experience and misjudging the complexity of a case can complicate the access process. Not being well-schooled in the use of essential tools such as magnification can cause difficulties locating canals and performing disinfection. Obtaining proper training and having appropriate equipment can be costly and require significant financial investments.
A careful preoperative assessment is required to identify the complexity of the case and be prepared for potential problems. For teeth that are heavily restored with intracoronal or extracoronal restorations, dental caries, and cracks, the approach involves dismantling these restorations to fully evaluate the restorability of the teeth and reduce the risk of removing too

Figure 1. End-cutting round diamond bur, often used for endodontic access followed by a non-end-cutting tungsten carbide Endo-Z bur (Dentsply Sirona, USA), often used for deroofing of the pulp chamber. A Meisinger bur (Hager & Meisinger, Germany) is also shown and can be used for refining the access cavity and troughing to identify canal orifices (note the long shank which can aid operator visibility during access). A diamond-coated ET18D ultrasonic tip (Acteon, UK) is also shown and can be used for this purpose also. (Reproduced with permission from Elmatary A, Moawad E, Heidarifar O, et al: Endodontic access cavity preparation: challenges and recent advancements. Br Dent J238:469-475, 2025.)
much sound tooth tissue or making a perforation because the anatomical landmarks were missing.
Radiographic assessment is required to determine the size and height of the pulp chamber. Large pulp chambers are generally less complex than smaller and reduced pulp chambers. A measuring tool should be used with the radiographic viewing software to determine the distance from the top of the crown to the roof of the pulp chamber on periapical views and the distance from the top of the crown to the cementoenamel junction. This measurement can be influenced by foreshortening or elongation, but a bitewing radiograph can provide a more accurate view in these cases.
Good lighting and magnification are important aids in identifying canal orifice(s), developmental fusion lines, and the color change used to identify the pulp chamber floor. A round diamond or cylindrical bur is recommended to make the initial pilot hole into the pulp chamber, but whatever the choice, the operator should be aware of the length of the cutting diamonds, make regular
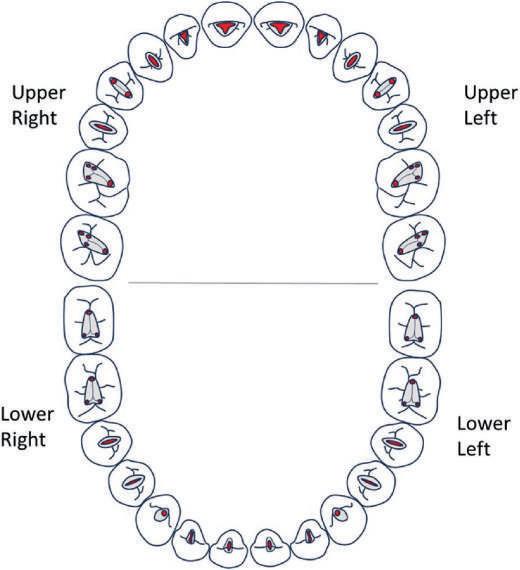
Figure 2. Classical access cavity shapes for upper and lower adult dentition. These can be modified to accommodate variations in anatomy identified on scouting of canals or from preoperative imaging, such as periapicals or CBCT. (Reproduced with permission from Elmatary A, Moawad E, Heidarifar O, et al: Endodontic access cavity preparation: challenges and recent advancements. Br Dent J238:469-475, 2025.)
stops and reassessments of the angle and orientation, and, most importantly, stop when the end is reached.
When the pulp chamber has been uncovered, it can be deroofed using a non-end-cutting tungsten carbide bur or diamond equivalents. This reduces the risk of perforation or damage to the pulp chamber. The non-end-cutting bur should remain parallel to the long axis of the tooth to avoid removing too much tooth tissue. An alternative method employs a slow-speed, rose-head, stainless steel bur to deroof the pulp chamber.
The floor of the pulp chamber is normally darker than the dentin walls, and canal orifices are always located at the junction between the walls and floor of the chamber. Developmental root fusion lines can map out the pulp chamber floor, and canal orifices are at the ends of these lines. Pulp stones can alter the identification of the pulp chamber floor and canal orifices. They should be identified preoperatively on the radiograph, where they appear as a glassy area against the surrounding dentin. Pulp stones can be effectively removed using piezoelectric ultrasonic instruments. Thinner tips or grooved profile instruments can also be used. If the clinician feels no “drop” when accessing certain teeth, slow-speed burs should be used along with ultrasonics, irrigation, and patience to locate the root canal orifices.
MIAC approaches are designed to preserve tooth integrity, removing only that tooth structure required for instrumentation and disinfection. Conservation of dentin is achieved by using flexible instruments, magnification, and 3-dimensional (3D) imaging techniques such as cone beam computed tomography (CBCT). It’s especially applicable in peri-cervical areas of the tooth, where the pulp chamber meets the root canal, in the distribution of occlusal stress, and to prevent cracked teeth. CBCT allows the clinician to visualize canal orifices, complex branching and anastomoses, and whether “additional” canals are present before access preparation is done.
MIAC requires perioperative radiographs, identification of the root canal system and its variations, and a determination of whether calcification is present. The access cavity can then be designed, with access guided precisely using dental magnification and small instruments with long shanks.
MIAC can be done through various techniques. These include the following:
• Traditional access cavity
• Conservative access cavity
• Conservative access cavity with divergent walls
• Ultraconservative access cavity (ninja access)
• Truss access cavity
• Caries-driven access cavity
• Restorative-driven access cavity
MIAC is associated with several risks and challenges and requires a highly skilled clinician along with specialized equipment. Among the limitations with this approach is difficulty adequately mapping the pulp floor to identify canal orifices, especially in teeth with multiple roots. This situation requires direct visual control, avoidance of high-speed burs, and the use of ultrasonic tips with longer shanks. The technique is more time-consuming, causing fatigue for the patient and clinician.
The MIAC approach can also risk missing canals, incompletely cleaning the entire pulp chamber and root canals. It can cause postoperative pain and sensitivity because of the incomplete removal of infected tissue. In addition, instrument fracture in the canal can occur because of the increased stress on them. The remaining tooth structure can still be at risk for postoperative fracture if appropriate restorative materials aren’t selected. In addition to these risks and challenges, no robust, long-term tooth survival outcome studies indicate that MIAC root canal −treated teeth have a better survival than those managed with traditional access cavity preparation.
CBCT can be especially helpful in locating canals when the tooth has reduced pulp chambers and calcified canals. When a small field of view CBCT is used, the radiation dose is low, so that benefits outweigh risks for the patient. If the patient’s clinician can’t locate the canal on a preoperative conventional periapical radiograph, a CBCT coupled with high magnification can identify the canal and result in minimal loss of additional tooth structure (Figure 8). A

Figure 8. A, Preoperative periapical radiograph of the 21, with an attempted access cavity by the patients’ general dental practitioner. B, Sagittal CBCT slice showing a clear and evident canal emanating from the palatal aspect of the current access cavity. C, Periapical radiograph showing completed root canal treatment for the 21, with the gutta-percha sealed with resin-modified glass ionomer cement, and the 21 now ready for internal/external bleaching. The canal was located using high magnification and the CBCT. (Reproduced with permission from Elmatary A, Moawad E, Heidarifar O, et al: Endodontic access cavity preparation: challenges and recent advancements. Br Dent J238:469-475, 2025.)
measuring tool used with the CBCT viewing software can guide the clinician in finding the depth of the access cavity more accurately.
Guided endodontics is especially helpful in locating calcified canals. Both dynamic navigation and static guides can be used. A CBCT is taken along with an intraoral scan/digitized impression of the arch. These are transferred into implant planning software and overlaid with each other. Virtual planning of the angulation and orientation of the model can show how the tip of the bur corresponds with both the start of the visible canal on the CBCT and remain in the long axis of the tooth. A stent can then be designed and 3D-printed; this seats on the tooth and neighboring teeth with minimal offset. A metal sleeve 1 mm in diameter is placed into the stent, through which the titanium drill can be thrust.
Guided access with a static guide can only be used in roots with no or only minimal curvatures and can lead to incisal/ slightly labially placed access cavities, which may alter the aesthetics. The technique can be difficult to perform if the tooth or adjacent teeth are heavily restored because these restorations cause scatter on the CBCT scan. A static guide is also difficult to use for posterior teeth because of the patient’s mouth opening, which impacts the stent seating and drill use. Experienced clinicians are often able to locate calcified canals without the stent, but the use of the guide can help clinicians with various degrees of experience locate canals efficiently and predictably. The static guide also can result in the loss of less-sound tooth tissue compared to conventional techniques. The risk of perforation is reduced.
After the root canal space is shaped and disinfected, a bacteriatight and fluid-tight seal must be placed. The goal of this obturation is to keep bacteria from entering the space and entomb any residual microorganisms in an environment that leads to their demise. Achieving an optimal seal requires specific materials and techniques. An overview of the basics of obturation, a description of the materials used and their advantages and limitations, and a step-by-step breakdown of the techniques employed in creating this sealing of the root canal system were offered.
Clinicians can face various challenges in preparing access cavities for endodontic treatment, especially with teeth that have complex presentations. Many factors contribute to the success or failure of access preparation and the predictability of endodontic treatment. Several tools are now available to facilitate the process and improve outcomes.
Endodontic access cavity preparation must be tailored to each patient’s unique presentation. Conservative methods can preserve tooth structure, but their success is linked to the training of the clinician as well as the quality of the equipment used. Having tools such as CBCT and magnification can provide more successful outcomes in complex cases, but each case requires careful preoperative assessment and guidance.
Elmatary A, Moawad E, Heidarifar O, et al: Endodontic access cavity preparation: challenges and recent advancements. Br Dent J238:469-475, 2025.
Reprints available from E Moawad; e-mail: Emad.moawad@liverpool.ac.uk
Root canal obturation is an essential part of root canal treatment, but is only effective if the root canal has been adequately disinfected to achieve a satisfactory reduction in the microbial load and the canal space has been prepared for adequate 3dimensional (3D) sealing on the apical, lateral, and coronal aspects. This is required for any residual organisms and their toxins to be deprived of access to the periapical tissues and to be trapped in an unfavorable environment for growth and survival. The seal should also favor periapical healing.
Single visit
Multiple visits
No pain or swelling Patient presents with pain/swelling
No remaining pus/exudate/blood Presence of a chronic abscess
Canals thoroughly disinfected for an adequate time
Sufficient time to complete the procedure
Complex treatments including perforation repair
Root canal filling material heavily contaminated/silver points
Canals still wet with exudate/ bleeding
Large periapical radiolucency
(Courtesy of Tait C, Camilleri J, Blundell K: Non-surgical endodontics –obturation. Br Dent J 238:487-496, 2025.)
Root canal treatments can be accomplished in 1 or multiple visits without affecting the outcome. In some situations, multiple visits are preferable (Table 1).
Calcium hydroxide releases hydroxyl ions and must be in direct contact with the bacterial wall to be effective. Therefore the calcium hydroxide delivery system must ensure that the canals are filled to length. In addition, nickel titanium files with an apical taper of at least 5% can create more space in the apical third of the canal for the exchange of irrigants. Adding the use of a smaller 30-gauge needle or specialized tips helps to destroy microorganisms in this area of the canal.
Completing treatment in a single visit removes the risk of recontamination between visits. In addition, it can benefit the patient in terms of saving time and money. The patient will also experience less discomfort because the procedure and any postoperative effects are experienced just once.
None of the materials available clinically meet the requirements for an ideal root canal filling material. Gutta-percha fulfills many requirements but is prone to microleakage, as are many of the other materials. The problem may result from differences in the thermal coefficient of expansion of the sealer and that of the tooth tissue, the presence of a smear layer, the consistency and quantity of the endodontic sealer, the solubility of the material, or the inadequacy of the obturation. Micro-spaces in the filled root canal may allow tissue fluids to penetrate into the root canal space. The transudate originates from blood serum that is degraded and diffuses into periradicular tissues. The serum contains microorganisms and their endotoxins, causing periradicular inflammation and possibly contributing to treatment failure. Hydraulic calcium silicate cements are bioactive materials that may eliminate these concerns for the development of microleakage.
GP is the most common core material, consisting of transpolyisoprene, zinc oxide, metal sulfates, and waxes or resins. It exists in an α-phase crystalline form, a β-phase crystalline form, and an amorphous form. Less shrinkage, lower viscosity, and poor stability at room temperature characterize the α- compared to the β-phase material. GP cones or points use the β-form. GP form doesn’t conduct heat, so that the apex temperature is always less than that of more coronal areas. On cooling, GP shrinks, making it technique sensitive. Some GP cones match specific nickel-titanium files, a situation essential in sealer-based techniques and considered a weakness in obturation.
Root canal sealers are used in endodontic obturation to fill voids, enhance adaptation between the core material and the dentin walls, and create an effective seal to prevent microleakage. They are useful in all obturation techniques, but can contain various chemical components and exert differing properties. The sealer chosen should be selected for its characteristics. The 3 primary sealer types are those that are zinc oxide eugenol based, resin based, and hydraulic cement based.
Zinc oxide eugenol−based sealers can be in powder and liquid or 2-paste systems. They are cost-effective and popular because of their highly radiopaque nature, which is able to make obturations distinctive on radiographs. However, eugenol interferes with resin setting and zinc interferes with hydraulic cement setting. In revisions of root canal therapy, the combination of eugenol and zinc can interfere with the setting reaction of hydraulic cement and epoxy-resin−based sealers, which compromises the outcome of the revision. Eugenol is also an irritant, causing sensitization when sealer remains beyond the apex. Shrinkage occurs with these sealers, so large volumes aren’t recommended. Zinc oxide eugenol−based sealers are used with warm vertical compaction techniques that require a minimal amount of sealer that remains separated from the heat carrier.
Resin-based sealers can be of the methylmethacrylate or epoxy resin types and are considered the gold standard for root canal obturation. These good adhesives help bond the GP cones together and are the sealer of choice for cold laterally compacted GP obturation. When compared to methacrylate-based sealers, their antimicrobial properties are just adequate. As a result, the final irrigating solution should be sodium hypochlorite to maintain a low bacterial count in the root canal space. The sealer shouldn’t come into contact with heat during warm vertical compaction.
Hydraulic cement sealers are based on the mineral trioxide aggregate (MTA) formulation and enhance the antimicrobial and biological characteristics of materials. These sealers release
calcium ions and stimulate the formation of hydroxyapatite, so they have been dubbed “bioactive” root canal sealers. They come as powder and liquid and are mixed before delivery to the root canal using a fine stainless steel instrument or a specific proprietary delivery system. Paper points can absorb moisture from the sealer and aren’t favored for delivery. In addition, instruments such as spiral fillers cause frictional heat that can result in faster setting of the sealer.
Sealers may be delivered as a single syringe with a plastic tip. These sealers are referred to as bioceramic, which can be misleading because the sealer’s chemistry varies and the name doesn’t indicate the exact composition. Most hydraulic cement sealers are composed of the hydraulic cement, a radiopacifier, additives to enhance sealers properties, and a vehicle. Various hydraulic cements are used, but only tricalcium silicates interact with water to produce calcium hydroxide and calcium silicate hydrate. Radiopacifiers vary, with zirconium oxide the most commonly used. These sealers don’t shrink unless they are desiccated, but they are highly soluble. The calcium hydroxide produced as a by-product of the tricalcium silicate and water interaction creates the antimicrobial and biological properties of these sealers. The sealers interact with dentin and create an alkaline etch with diffusion of mineral from the sealer into the dentin, creating a mineral infiltration zone and sealer tags.
This type of sealer has positively altered the principles of root canal obturation from quality of fill to a more biological approach where microbial contamination is eliminated. The sealers aren’t toxic and enhance bone differentiation, but should not be extruded beyond the apex because of their high alkalinity, which can create soft tissue burns and damage nerves near the root apices. Hydraulic cements are best used in sealer-based techniques such as single-cone obturation because of their biological properties and interactions with dentin. Water evaporation after mixing these materials with water can react with heat to cause the deterioration of sealer physical properties. The single-syringe sealers use alternative vehicles that don’t suffer this disadvantage.
For better success rates, obturation should be within 2 mm of the root apex and involve no voids. The GP at the end of the cementodentinal junction can range from 0 to 3 mm from the radiographic apex. Electronic apex locators are more accurate than working length radiographs in determining the apical constriction. A cone-fit radiograph should be taken after root canal preparation and disinfection to ensure accurate cone placement before obturation; to assess cone fit apically; to identify merging canals, obstructions, or ledges; and to provide a visual record of cone placement.
The techniques used for obturation can be cold techniques, such as cold lateral compaction and single cone with a calcium silicate
sealer, or warm techniques, including warm vertical compaction, continuous wave obturation, carrier-based techniques, or thermomechanical compaction.
In cold lateral compaction, a lightly coated cone (master cone) is placed to length, then a metal spreader is used to compact it against the canal wall. This allows a smaller GP cone (accessory cone) to be placed alongside the master cone. The process is repeated until no space remains. The sealer must be able to fill the spaces between the GP cones. The disadvantages of this approach are the total dependence of the apical seal on the sealer and the higher risk of creating vertical root fractures based on the forces generated during compaction.
In the single cone with a calcium silicate sealer technique, a cone matched to the size of the final shaping file is used. After disinfection and drying, the coronal two thirds of the root canal is gently filled with hydraulic calcium silicate sealer using the proprietary small-diameter tip. The cone is placed into the canal with a gentile pumping action. The sealer will then fill the apical third of the canal. Post-treatment radiographs confirm the position of the sealer.
This technique is sealer based, so sealer properties are key to success, with the use of hydraulic cement sealers recommended. It’s a simple technique that doesn’t need special tools. Chlorhexidine should be avoided as a final irrigant, with sodium hypochlorite followed by a calcium chelator preferred. Solutions reducing the pH should be avoided to guard against bacterial recolonization.
Warm vertical compaction was developed to prevent residual microorganisms and their by-products from reaching the periapical tissues. A tapered master cone coated in sealer is fitted 0.5 to 2 mm short of the working length and checked to ensure resistance to displacement. Heat is used to remove the coronal portion, then a cold plugger compacts the softened GP apically to achieve an apical seal. A small pellet of GP is placed in the canal and heated, then a cold plugger compacts and moves the softened GP apically. The process is repeated in the middle and coronal third of the canal.
Continuous wave obturation is a popular variation of warm vertical compaction that requires a tapered preparation and consists of a downpack and backfill, as follows:
1. In the downpack, a heated plugger is fitted snugly in the root canal 5 to 7 mm short of the working length. Once the master cone is checked for fit, it’s lightly coated in sealer and inserted into the canal. The heated plugger is gently pushed through the master cone for 3 seconds or less, then the heat is removed and light apical pressure held for 10 seconds to eliminate any space created by shrinkage during cooling. The heat
is reactivated for 1 second, then the plugger is withdrawn to remove the coronal GP. A flat plugger is used to compact the apical portion of GP.
2. In the backfill, many devices can be used, all with different gauge needles depending on the diameter of the canal. The device should reach the apical GP 5 to 7 mm short of the working length. Although the temperature on the readout may be 200◦ C, the tips all have temperatures under 100◦ C. Higher temperatures can damage the adjacent periodontal ligament space and bone.
The thermoplastic GP fills lateral canals, isthmuses, and internal resorption defects. Zinc oxide eugenol−based sealers are always used, but, since sealers decompose when exposed to heat, sealers shouldn’t be heated during obturation. The canal’s coronal area should be lightly coated with sealer and downpacked. During backfill, the needle tip should contact the apical GP and be maintained in this position for a few seconds. The injectable GP is then slowly extruded while slowly withdrawing the needle from the canal. When the canal orifice level is reached, the needle is removed and a flat plugger is used for compaction.
Carrier-based thermoplastic techniques use a solid plastic core with α GP, which gives the obturator more flexibility but makes it hard to remove, especially in narrow or curved canals. A cross-linked core material made from GP facilitates easier removal in retreatment cases and is available to fit in specific file systems. A verifier that matches the preparation is used, or the operator can ensure the shaping file fits passively in the canal to the correct working length. Depth rings on the obturator handle are used to set the working length using the silicone stop. The obturator is heated at 135◦ C while a small amount of sealer is placed in the coronal part of the canal. The heated obturator is placed in the canal to the working length within 10 seconds; the operator should avoid rotating or twisting it. The handle is removed, and coronal CP is compacted using a flat plugger. A heated instrument can be used to remove any material left in the pulp chamber. To avoid extruding excess material apically, minimal sealer should be used, with the obturator seated 0.3 mm less than working length.
Thermomechanical compaction employs a McSpadden compactor, which is placed in the canal, alongside the master cone coated in sealer, then driven at 5000 to 10,000 rpm to within 3 to 4 mm from the working length. Frictional heat warms, plasticizes, and compacts the GP toward the walls. The technique isn’t suitable for narrow, curved canals, and compactors can break in the canal. In addition, the soft GP can be extruded into periapical tissues. Concern has been raised over the heat created in the root canal. As a result and because compactors are no longer available, this technique is rarely used.
Several conditions can make obturation complex or prone to complications. These include having a wide or open apex,
Table 3. Step-By-Step Guide for Management of Complex Cases
Step 1
Magnification, preferably using a microscope, is recommended for this procedure
Step 2 The canal is dried using large paper points, ensuring these are measured just short of WL so the periapical tissues are not disturbed which can cause bleeding to enter the canal
Step 3 A specific carrier is used to dispense a small amount of material apically, trying to keep it from attaching to the canal walls
Step 4
Step 5
A flat plugger with a rubber stop 0.5mm shorter than WL is used to gently tap the material into place
Further increments are added and gently packed into place until 4–5mm has been achieved
Step 6 A radiograph is advisable at this point to ensure good adaption of the material apically
Step 7 The canal is then backfilled with thermoplastic GP, ensuring there are no voids
(Courtesy of Tait C, Camilleri J, Blundell K: Non-surgical endodontics –obturation. Br Dent J 238:487-496, 2025.)
internal inflammatory root resorption, overfill or overextension, and underfill or underextension.
When canals have wide apices, hydraulic calcium silicate cements have been used to create an immediate apical barrier. These materials are indicated when the apical opening is 0.70 mm or greater (Figure 15 and Table 3).
Internal inflammatory root resorption is rare and its cause is unknown. Often confused with cervical invasive resorption, its progression is stopped when the entire pulp becomes necrotic. The radiographic appearance of internal inflammatory root resorption is a round or oval and symmetrical widening of the canal that replaces the original canal shape. Cleaning of the space can be challenging, with a thermoplastic technique needed to fill the irregular shape with chemical disinfectant. Sometimes a master cone can be sealed apical to the lesion, with injectable GP used to fill the rest of the canal. If there is a perforation, MTA may be used, but the technique is challenging. Fiber posts may be needed where root dentin is thin because the GP won’t reinforce the structure.
Overfilling may occur when there is a lack of or loss of apical constriction caused by inflammatory resorption, an immature root apex, overinstrumentation, errors in selecting or placing the master cone, and the use of thermoplastic techniques. When calcium silicate sealers are used, “puffs” of sealer may be seen apical to the root apex. The hydrophilic nature of hydraulic cements in the canal can be problematic. The puffs indicate that the root canal anatomy has been prepared and filled, but overfilling should be avoided.
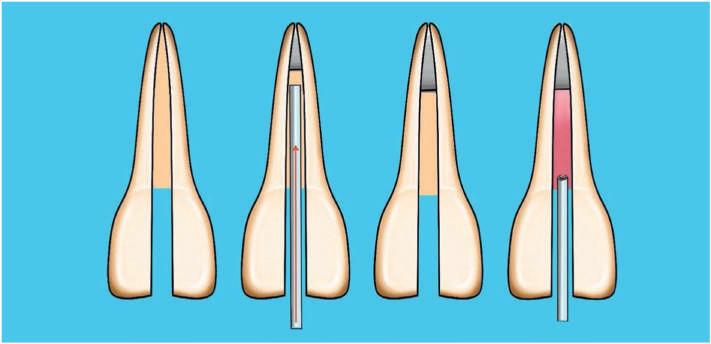
Figure 15. Diagram of technique for apical plug placement in wide apex. (Reproduced with permission from Tait C, Camilleri J, Blundell K: Non-surgical endodontics obturation. Br Dent J 238:487-496, 2025.)
Overextension of GP involves extrusion beyond the root apex but the GP doesn’t completely fill the canal system. As a result, residual microorganisms may negatively impact biological outcomes.
Poorly fitted GP points can result when the root canal has been adequately prepared but the obturation is short of the apex. This tends to have less effect on the root canal therapy outcome than overfilling, but if it occurs because the canal space was inadequately prepared, debris generated during instrumentation will remain in the apical third, so that the obturation is insufficient to reach the apex.
Clinical outcomes remain largely consistent despite differences in the sealer or obturation technique used. The success of obturation depends on many factors related to the entire root canal treatment process.
The guidelines offered highlight the importance of observing meticulous aseptic technique, receiving proper training, and having regular repeat evaluations to ensure the patient experiences long-term success. A holistic approach to endodontic treatment should be adopted for all aspects of the process, from diagnosis to obturation. Remaining informed about the advances in knowledge and techniques is essential to achieving the best patient outcomes.
Tait C, Camilleri J, Blundell K: Non-surgical endodontics obturation. Br Dent J 238:487-496, 2025.
Reprints available from K Blundell, School of Dentistry, Inst of Life Course and Medical Sciences, Faculty of Health and Life Sciences, Liverpool, UK; e-mail: kblund@liverpool.ac.uk
Teeth that require restoration after having root canal treatment come with concerns regarding how to return the health and function of the tooth to acceptable levels while maintaining prevention of microbial leakage into the root canal system and avoiding excessive tooth structure loss. The volume of the remaining natural tooth tissue is often the most significant factor in obtaining a sufficiently strong restored tooth. Various
factors contribute to the decision to restore a root-filled tooth and to the choice of a method to accomplish that restoration. The clinician should evaluate all the components contributing to a successful restoration of the tooth, assess specific tooth factors such as whether it’s an anterior or posterior tooth and what restorations are most appropriate, and select the materials that are optimal for addressing each patient’s unique situation.

Restorability
The tooth’s likely successful return to good function must be assessed, with special emphasis on patient factors. Among these factors are the tooth’s strategic importance, its periodontal status, and the need to retain the tooth for the role of abutment for a prosthesis, whether future or current. Some patient factors are desires, expectations, financial status, oral health, and response to stabilizing treatment, which can indicate the patient’s motivation to maintain a restored tooth. Analysis of all these factors should take place, followed by the development of a plan for the final restoration. Indexes have been developed to help the clinician determine the likelihood that the tooth will be restorable.
If microorganisms can enter the dentinal tubules and potentially reinfect the root canal system, the previous treatment becomes compromised. The clinician must avoid this by preventing reinfection through a well-disinfected and obturated root canal system, with a hermetic seal that prevents reinfection from the oral cavity. Sealing exposed dentinal tubules is possible using adhesive techniques, extending restorations over the dentin using a ferrule, or combining these approaches. Ideally, the tooth will have multiple layers of endodontic/restorative protection, with each one acting as an independent barrier. If the outer layer fails, the subsequent layers protect the root canal filling and allow for a more conservative subsequent restoration.
The restoration of form and function is essential to controlling occlusal or parafunctional loads on the restored tooth, especially if a post core was provided. Study models or a digital scan of the dentition can identify occlusal contacts in and between intercuspal position, retruded contact position, and protrusive and lateral excursions, as well as any parafunctional movements. An endodontically restored tooth should be part of a group function occlusal scheme rather than considered as a solo entity. If the canine is being restored, it should be considered as part of a group function scheme, with the understanding that it may
be associated with a slightly unbalanced smile line against the lower lip and function may also be compromised. The clinician should plan his or her changes using physical or digital models that will analyze the aesthetic and functional effects and see how the changes fit with the hoped-for result.
The perception of aesthetics differs from person to person. Often, simple access cavities can be restored using composite resin restorations, but shade matching must be considered if the restoration extends onto the labial/buccal aspects. The framing of the tooth by the gingival architecture influences aesthetics, so the clinician and patient should discuss the likely outcome, with the result of any compromises documented before treatment begins.
The greatest threat to a successful endodontically treated tooth is a loss of structural integrity tied to the endodontic access and preparation. Although more conservative forms of access are believed to result in durable endodontically treated teeth, no strong evidence supports this hypothesis. The ability to satisfactorily clean, disinfect, and obturate the root canal system may have more influence on the tooth’s survival than the technique employed during treatment. Other factors that influence outcomes are number of remaining walls in the tooth and the provision of cuspal protection.
As with all teeth, the restored tooth will be at risk for dental caries. To avoid this problem, the clinician should ensure postendodontic restoration margins fit accurately, overeruption of opposing teeth is prevented, plaque accumulation is minimized, and the tooth contacts and emergence profiles harmonize with the natural dentition. This helps to minimize compromises of gingival health or periodontal status.
It’s been suggested that the presence of a permanent restoration can significantly influence endodontic success. When root-filled posterior teeth receive a crown before 4 months, they are 3 times less likely to be to extracted that teeth restored after a longer time using composite or amalgam restorations. It’s logical
to provide the definitive restoration as soon as possible to avoid microbial contamination and protect remaining tooth structure.
The number of anterior teeth that need endodontic treatment has declined significantly. As a result, simple palatal access cavities can be restored using composite resin restorations. However, when large proximal cavities or restorations are also present or the access cavity has become large cervically, the clinician should consider how the final restoration can be retained and restore the tooth’s strength to resist functional loading. The likely loading applied to the retained tooth surface should be estimated when determining how much tissue should be retained for a ferrule.
Post-retained Restorations
Removing tooth tissue to retain a post weakens the remaining structure, and even adhesively luted posts cannot reinforce the root. The primary goals for any post are the retention of as much tooth structure as possible, provision of a microbial seal, and retention of a core. Posts are often used in anterior and premolar teeth when the coronal structure is inadequate to retain the core. The post system selected should match the posttreatment root canal morphology as closely as possible and disrupt the obturation as little as possible, while still mirroring the root structure’s biological shape. Threaded or parallel posts should be avoided.
Currently, the use of adhesive composite materials to reinforce that which remains has been widely adopted. Adhesively luted fiber posts don’t reinforce tooth structure but do help retain a composite core and provide benefits when coronal tooth structure provides a ferrule (Figure 2). The adhesive techniques maintain more coronal tissue, allow clinicians to have an adequate length of post with less disturbance of the root canal filling, and maintain an antimicrobial seal. Fiber posts are also less likely to cause root fractures than metal posts. The modern systems maximize retention of coronal structure and provide a longer ferrule and more favorable stress distribution.
The characteristics sought for anterior crown material include retaining as much tooth structure as possible, maintaining a microbial seal, withstanding expected loading, restoring form and function, and achieving aesthetics. Pressed-glass or other allceramic crowns can achieve many of these goals, especially when cemented adhesively to remaining tooth structure. Metal ceramic crowns may be indicated if more durability is required because of high loading or when a cast metal post and core system has been used. Regardless of the material chosen, it should maximize the ferrule effect but not compromise the biological width more than is necessary to distribute forces to the root surface and allow a sympathetic emergence profile to be developed.
The principles desired for anterior teeth are also applicable to posterior teeth. However, the magnitude of applied forces, usually axillary, is significantly greater in posterior teeth, with lateral loading exerted on nonfunctional cusps that have often been weakened by endodontic access or previous restorations. When marginal ridges have also been lost, tooth stiffness can be reduced by as much as 63%. Molar teeth are also more prone to caries and cracks and are considered complex teeth to treat and restore. Tooth-related factors that affect the prognosis of endodontically treated posterior teeth (ETPT) have been evaluated; the correct selection of a coronal restoration can reduce failures caused by these factors.
Direct restorations have the advantages of reduced invasiveness, no need for a laboratory stage, and costing less for the patient. Both the survival rates of restorations and those of the involved tooth should be considered when comparing direct and indirect restorations. Composites are aesthetically excellent, have a similar modulus of elasticity to dentin, and can be repaired easily. Short-fiber reinforced composite offers improved load-bearing capacity and crack-arresting mechanisms. Further evidence is needed to provide a good evaluation of indirect and direct restorations with fiber-reinforced composites. It’s known that composite restorations placed on endodontically treated teeth with both marginal ridges retained and having a maximum of 2 surface losses have comparable survival after 5 years to conservative, direct restorations with intact marginal ridges.
Several factors interact in complex patterns when restoring posterior teeth with an indirect restoration (Box 1). Indirect restorations increase the survival of root-filled teeth. Five- and 10year survival data for posterior teeth with a crown were 94% and 89%, respectively, but fall to 77% and 62% without a crown. Posterior teeth without a crown are about 6 times more likely to
Box 1. Clinical Considerations When Restoring an ETPT
(Reproduced with permission from Patel SR, Youngson C, Jarad F: Principles guiding the restoration of the root-filled tooth. Br Dent J 238:508516, 2025.)
require extraction after 8 years. Having a crown after root canal treatment significantly affects tooth survival.
Onlays allow for a more conservative tooth preparation but still provide cuspal coverage that protects the underlying tooth structure. They have a longer restoration margin length compared to a crown that must be sealed. They can be more difficult to prepare and avoid undercuts but conserve more tooth structure. Their marginal finishing lines are less templated than those of a crown preparation. There may also be a greater or lesser aesthetic compromise as the onlay tooth interface is usually visible, but in posterior areas, patients may not be as concerned. Often dentists choose a gold restoration in selected cases. So far, the evidence is inconclusive regarding which restoration survives longer when comparing resin and ceramic onlays or inlays. ETPT does present a risk factor for
poorer survival. Ceramic onlays were found to have 10-year survival rates of 91%, but the studies evaluated weren’t limited to ETPT.
Endocrowns are laboratory-made, full-coverage crowns with an integrated intracoronal extension and can be considered an extreme form of onlay. They offer macromechanical retention through anchorage in the pulp chamber and micromechanical retention through adhesive cementation. They tend to retain as much coronal tissue as possible and don’t need post-channel preparation, thereby offering fewer barriers to microbial sealing. Recent adaptations of the technique use tooth-colored core materials with adhesive techniques to enhance microbial seal. The ultimate crown has a cervical finishing margin and provides resistance form and an augmented marginal seal.
A thorough clinical assessment is required when selecting the proper crown material for each case (Table 2). The choices include metal ceramic, zirconia, glass ceramics, and gold.
The high strength and toughness of metal cores and the support provided to the veneering porcelain along with a low cost and acceptable aesthetics make metal-ceramic crowns (MCCs) the most common posterior crown material used. Zirconia is the strongest and most fracture-resistant ceramic available and has the lowest plaque accumulation of any ceramic. It can be monolithic or layered/veneered. Adding veneering ceramic to improve aesthetics can create chipping and micro-cracks that lead to failure of a zirconia crown, which is more common as a failure in bridgework or when an underlying zirconia core is less supportive. Monolithic zirconia is less likely to suffer micro-fractures and chipping and may be a better choice for ETPT cases, serving as an alternative to metal or metalceramic crowns.
Glass ceramics offer excellent aesthetic characteristics, but their strength and fracture resistance for posterior uses are inferior to those of zirconia. Various glass-ceramic choices are available and may differ in their survival rates. In general, their survival is slightly less than that of other crown materials, but they may still prove useful for EPTP in carefully selected cases.
Gold is a less aesthetic material than the other candidates and requires a demanding technique for optimal tooth preparation.
There has been a gradual loss of technician expertise, especially with laboratories moving to ceramic-based infrastructures. Little good evidence exists to document the survival of ETPT restored with gold crowns. They are considered an excellent option in non-aesthetic zones, especially in patients who have parafunctional habits.
The choices made in restoring endodontically treated teeth has moved from a focus on mechanical concerns to a more biologically based process. Clinicians can now produce results that are predictably longlasting, highly aesthetic and functional, and conservative of tooth structure while maintaining an effective antimicrobial seal for the endodontically treated tooth.
Patel SR, Youngson C, Jarad F: Principles guiding the restoration of the root-filled tooth. Br Dent J 238:508-516, 2025.
Reprints available from C Youngson, Emeritus Professor, Liverpool Dental School, Faculty of Health and Life Sciences, University of Liverpool, L3 5PS, UK; e-mail: c.c.youngson@liverpool.ac. uk
Imaging has a vital role in endodontics, guiding the process of diagnosis, treatment planning, and outcome assessment. Intraoral periapical (IOPA) radiographs and cone beam computed tomography (CBCT) are the modalities used most often in endodontics. IOAP offers accessibility in terms of availability and cost, simplicity, and low radiation doses. CBCT has enhanced benefits for more complex diagnosis and treatment planning. The radiographic findings should always be used in the light of the patient’s history of symptoms and clinical examination. Imaging can be employed in diagnosis and treatment planning, during treatment, and to assess the technical and biologic outcomes of treatment.
IOPA radiographs are generally taken after the clinician has obtained a complete dental history and performed a clinical assessment. Ideally, a paralleling technique is used to display the optimal image geometry of the tooth along with at least 3 mm of periapical bone. These images provide information regarding the pulp, root canal anatomy, and periradicular tissues that may influence the clinician’s diagnosis and treatment planning. For teeth with multiple roots and/or canals, a parallax rule can be used to determine root canal anatomy, so that root canals can be separated and overlap of anatomical structures eliminated (Figure 2). A vertical shift may also be used to help in diagnosing

Figure 2. A, B, Showing a lower left first molar (36) using paralleling technique and an angled IOPA radiograph revealing evidence of a radix molaris. More information was required before commencing endodontic treatment in this case and hence a low volume CBCT of the 36 was taken which confirmed the complex anatomical feature. C, D, Coronal view and sagittal view. (Reproduced with permission from Sarsam W, Davies J, Al-Salehi SK: The role of imaging in endodontics. Br Dent J 238:448-457, 2025.)
dental trauma that has produced oblique fractures that otherwise wouldn’t be visible. Unerupted teeth can also be found, along with large apical lesions. In specialist and hospital settings, which commonly handle complex cases, the use of a small fieldof-view CBCT may replace the use of occlusal views.
IOPA radiographs can be used to assess the complex curvature of canals by measuring root angulation. Canal morphology can be
classified as slight to no curvature, moderate curvature, or extreme curvature.
The extent of root resorption is often underestimated during conventional 2-dimensional (2D) imaging. This problem is especially notable when the lesion extends deep into the buccopalatal/lingual dimension. The classification systems used for external cervical resorption (ECR) can clarify the prognosis and

Figure 9. A, IOPA radiograph showing inflammatory resorption of the distal root of the 36 and periapical radiolucency of mesial and distal canals. B, CBCT axial slice showing the extent of the lesion, perforating the buccal cortical plate. C, Coronal view revealing severe curvature of the distolingual canal in the buccolingual plane which is not evident on the IOPA radiograph. (Reproduced with permission from Sarsam W, Davies J, Al-Salehi SK: The role of imaging in endodontics. Br Dent J 238:448-457, 2025.)

Figure 11. A, IOPA of the 21 with a threaded post which appears to be well-aligned in the mesial and distal planes. B, CBCT sagittal view of the same tooth showing the post is misaligned with near palatal perforation. Note the beam-hardening artefact mimicking a fracture line. (Reproduced with permission from Sarsam W, Davies J, Al-Salehi SK: The role of imaging in endodontics. Br Dent J 238:448-457, 2025.)
treatment for these lesions. The circumferential spread of the lesion can be determined on 3D images, which is used in a recent ECR classification scheme.
The diagnostic yield from IOPA radiographs can be optimized by adhering to quality standards outlined in the European Guidelines. These cover evidence of optimal image geometry, correct anatomical coverage, good density and contrast, adequate radiograph numbers, and adequate image processing. X-ray holders should be used routinely. Intra-oral image receptors for endodontic imaging include dental film, solid-state digital sensors, and photostimulable phosphor plates.
If the diagnostic yield of the conventional radiograph doesn’t provide sufficient information, CBCT is an advanced imaging system that can be used to visualize the dentition and surrounding anatomical structures in 3D. This modality exposes the patient to more radiation; requires investments in equipment, maintenance, and space for the provider; and involves additional training of the operator in taking, interpreting, and reporting on the images. Clinicians must balance the benefits to the diagnostic process and treatment planning that CBCT offers against the risks of increased radiation exposure for the patient.
CBCT is more accurate than IOPA radiographs in detecting periapical radiolucencies and allows the analysis of the patient’s situation in different planes. This means the diagnosis can be made earlier, followed by prompt treatment and possibly a better prognosis. Teeth with complex anatomy that are analyzed with CBCT 3D imaging will yield more information. Less
anatomy loss also occurs with CBCT images compared to IOPA radiographs. The clinician may be able to gather information in the buccolingual plane not available through a 2D IOPA periapical radiograph, including hidden curvatures (Figure 9) and post alignments (Figure 11). Conventional 2D imaging can underestimate the extent of root resorption, especially when the lesion extends deep into the buccopalatal/lingual dimension.
CBCT may reveal a bone loss along a vertical root fracture (VRF) that wouldn’t have been seen on a IOPA radiograph, but unless some displacement of root fragments is present, cracks aren’t visible radiographically. Beam-hardening radiolucency and scatter from streak artefacts associated with radiopaque materials such as root fillings or metallic posts can also be misinterpreted. Currently, the evidence supporting the use of CBCT to routinely detect VRFs is insufficient.
The working length is determined by measuring the distance from the coronal reference point to the apical constriction using an EAL. Determining the working length radiographically is associated with several drawbacks. The EAL uses 2 or more frequencies to measure the impedance to determine the apical constriction’s location. As a result, EALs are more accurate than radiographs, so radiographs should only be used to confirm the working length when the EAL readings are inconsistent.
IOPA radiographs can be used during endodontic treatment to assess the angulation of access, identify possible complications, assess the canals after instrumentation is completed, and confirm the appropriate extension of master cones before obturation.
CBCT can also be used during treatment to detect narrow or calcified canals, provide a cone fit determination, and plan complex surgical cases. Appropriate cases for CBCT include large lesions and those close to important anatomical structures.
IOPA radiographs should be taken immediately after the root canal treatment is completed to evaluate the technical quality of the procedure. In addition, this baseline image can be used to monitor the site’s subsequent condition and evaluate treatment outcomes, which are determined after assessing the patient’s symptoms and clinical and radiographic evaluations. An IOPA should be obtained annually until the periapical tissues have healed completely or for 4 years when persistent lesions accompany post-treatment disease.
CBCT can detect periapical lesions more accurately than IOPA radiographs. However, insufficient evidence supports the use of CBCT routinely to monitor outcomes. Cases where symptoms
persist and conventional radiographs don’t provide good diagnostic information can be evaluated using CBCT. Additional information from CBCT imaging can influence endodontic treatment decisions in highly complex cases.
Magnetic resonance imaging (MRI) is noninvasive and uses nonionizing radiation. Currently it’s being evaluated for possible use in dentistry. Dental-dedicated MRI (ddMRI) is a new system that fits the hardware, software, and workflow for use in dentomaxillofacial indications. It has been used to detect signs of inflammation associated with endodontic problems in soft tissues. Its primary limitations are the time required for imaging and the application only in patients during treatment planning and follow-up when endodontic treatment is beginning or has already concluded.
Artificial intelligence (AI) has been applied clinically in endodontic treatments. These include the interpretation of both 2D and 3D images. AI algorithms can help reduce distortion from metallic restorations and some other causes. However, AI tools require further investigation by dental professionals.
Imaging is an essential part of endodontic diagnosis, treatment, and monitoring of the outcomes of care. Conventional radiographs are still the standard imaging method because of their accessibility, their lower radiation dose, and the higher resolution now possible. These qualities make them sufficient for diagnosing and carrying out the key stages of endodontic treatment in most cases seen in general dental practices. However, there are limitations associated with conventional intraoral radiographs and these can often be overcome by using CBCT, especially in more complex endodontic cases.
Sarsam W, Davies J, Al-Salehi SK: The role of imaging in endodontics. Br Dent J 238:448-457, 2025.
Reprints available from SK Al-Salehi, Inst of Dentistry, Queen Mary Univ of London, Turner St, London, E1 2AD, UK; e-mail: s.al-salehi@gmail.ac.uk
Root canal treatment to prevent or cure apical periodontitis relies on an accurate diagnosis and meticulous performance of each stage of treatment. Treatment strategy hasn’t changed for decades, but the tools used to achieve root canal system preparation have seen significant developments. Nickeltitanium (NiTi) files, more varieties of instruments to find and negotiate root canals, and enhanced efficacy of irrigants have also helped to make cleaning and shaping of the root canal system simpler and more effective. The objectives of root canal cleaning and shaping were explained, principles of effective glide path creation were noted, and the contributions of irrigation and proper biomechanical debridement of root canals were explored.
Cleaning, shaping, and filling are actions on which the objectives of root canal treatment are based. These objectives fall into those focused on biological status, the recommendations
regarding mechanical steps, and the technical phases that must be addressed.
Pulp necrosis removes the protection for the root canal space and allows for the growth and proliferation of microbial agents. This can eventually lead to inflammatory disease of the periradicular tissues. The root canal space consists of accessory canals, isthmi, branches, fins, and other forms in all parts of the canal, with each component being unique to each tooth. Because the entire root canal system can’t be mechanically prepared or cleaned, the biological objectives to focus on are disinfecting as much of the system as possible, removing potential nutrient sources, and blocking the recontamination of the root canal system.
Cleaning can be facilitated by making changes in the shape of the root canal systems using various endodontic instruments. This directly removes bacteria and nutrient sources from the system and facilitates the actions of antibacterial agents to

Figure 3. Burs designed for radicular access (top to bottom): Protaper Next X and X-gates. (Reproduced with permission from Tomson PL, Adams N, Kavanagh D, et al: Non-surgical endodontics: contemporary biomechanical preparation of the root canal system. Br Dent J 238:478486, 2025).
penetrate more deeply into the system to achieve greater disinfection. The mechanical objectives of this process are producing a continuously tapered preparation, maintaining the canal axis in the center of the root, and sustaining the original position of the foramen without enlargement.
The initial treatment of periradicular disease uses an orthograde approach to access the system through the crown. The goal is to disinfect dentin near the inflamed periradicular tissues. Coronal access is designed to remove the pulp roof and provide a clear path to reach the various parts of the root canal system. Technical preparation of the system is used during initial canal negotiation, coronal enlargement, apical exploration and glide path establishment, length determination and apical patency, and canal preparation. The initial canal negotiation informs the operator about how easy or difficult the case will be and helps in formulating a plan for case management. Small stainless steel hand files are used to determine the ease of file advancement, which indicates the size of the canal.
In coronal enlargement, canal size determines the enlargement needed. Hand filing uses a systematic approach according to a watch-winding method. Larger stainless steel hand files can be used next, with file size modified in accordance with the canal size. Irrigation accompanies this process, which can be timeconsuming in tight canals. In small canals the aim is to enlarge the orifice sufficiently to accommodate engine-driven instruments (Figure 3), then advancement can be more rapid and coronal curvatures can be straightened.
Apical exploration and glide path completion are done to establish a safe, efficient pathway for later instrumentation and is often the most challenging stage in therapy. Precise techniques are used to avoid complications such as blockages where dentin chips accumulate and block further progression; ledges where improper file handling causes deviations from the canal’s original path; or perforation, where the instrument breaches the canal walls and compromises progress.
The principles guiding glide path creation are to perform the initial negotiation using hand files and to progressively enlarge the access using engine-driven instruments. The engine-driven NiTi file can safely and efficiently create a glide path with minimal risk of transportation. Some systems use more than 1 instrument to achieve access. If full working length cannot be achieved initially, small stainless steel hand files can be used to penetrate deeper and negotiate the length of the canal.
Radiographs, tactile discernment, a paper-point approach, and use of an electronic apex locator (EAL) can determine canal length. EALs are considered a vital part of the dentist’s armamentarium, but instruments can differ depending on the manufacturer. The most reliable reference point for any EAL is the zero reading. To use the EAL correctly requires that the canal is patent. Modern apex locators are highly reliable in determining root canal length. This allows the operator to accomplish complete preparation and obturation with confidence.
Apical patency refers to maintaining the apical extent of the canal free of debris. A small file is used to pass through the apical foramen and reduce the risk of debris accumulating and compromising the procedure. A patency file may help remove bacteria present in the apical construction and foramen, but the operator must be careful to use only small instruments and avoid extending more than 1 mm beyond the foramen. Over-instrumentation can lead to enlargement/transportation of the foramen, extrusion of infected debris, and mechanical damage of the apical tissues. Although a patency technique has been suggested to have negative effects, it’s well established that observing this principle will double the odds of success. In addition, patency is a significant intraoperative factor that is associated with periapical health after root canal treatment.
The preparation should be straightforward once the glide path patency and working length of the canal have been established. The remainder of the root canal preparation can be done using stainless steel hand files or ultrasonic instruments, although engine-driven NiTi instruments are the most common choice. Evidence-based recommendations offer guidelines for the process, noting that the contemporary engine-driven techniques using NiTi instruments should be selected to manage apical periodontitis, with no particular NiTi instruments called out.
The design features of most interest include variable tapers, cutting flutes, the material, cross-section, and motion. The introduction of novel cross-sectional designs and metallurgy are the most recent innovations. The microstructure of the NiTi alloys has been optimized to improve flexibility and fatigue

Figure 6. WaveOne Gold primary (25, 0.07) instrument is pre-curved off central axis without permanent deformation due to reduced shape memory compared to conventional NiTi instruments. (Reproduced with permission from Tomson PL, Adams N, Kavanagh D, et al: Non-surgical endodontics: contemporary biomechanical preparation of the root canal system. Br Dent J 238:478-486, 2025).
resistance. Various thermomechanical processing modifications have significantly improved flexural fatigue resistance of the newer instruments compared to those using conventional NiTi alloy. This includes creating less bounce back, which makes the files feel rubbery when flexed compared to the immediate bounce back quality of other NiTi instruments. This feature allows light pre-curving of the instrument off the central axis of the instrument without permanently deforming it (Figure 6), which can be an advantage for placement in hardto-reach canals.
The engine-driven file design has incorporated the ability of the NiTi instruments to be used in a continuous rotating motion. Reciprocating motions are also available, with the principle behind reciprocation being the rapid repetitive process of engagement and disengagement of the file with the canal wall through precise clockwise and anticlockwise movements. These motions aren’t equal, so the file rotates through 360 degrees after a certain number of phases of motion, permitting the file to follow the canal more easily. Generally only a single reciprocating file is needed to prepare each canal.
Other file design innovations include the following:
• An off-centered cross-section is designed to reduce the surface area of contact between the file and the canal wall (Figure 7). This reduces the load on the instrument and allows room for debris to accumulate between file flutes and be
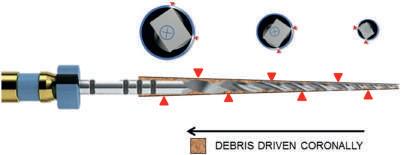
Figure 7. ProTaper Next file design with rectangle off-set cross-section along its length which results in only 2 points of engagement (red arrows). In principle, this creates space for debris to be driven coronally when in motion. (Reproduced with permission from Tomson PL, Adams N, Kavanagh D, et al: Non-surgical endodontics: contemporary biomechanical preparation of the root canal system. Br Dent J 238:478-486, 2025).
driven coronally, which will hopefully provide more efficient debris removal.
• Files with triangular or trapezoidal cross-sections to enhance cutting efficiency and reduce engagement with the canal walls.
• Files with offset centers of rotation that minimize canal binding and improve the efficiency of debris removal.
• Several manufacturers have decreased the diameter of the wire used to fabricate endodontic NiTi files from 1.2 mm to 1.0 mm, leading to a preservation of more coronal dentin and the evolution of canal shapes so that they are “skinnier” than previously. Having more pericervical dentin preserved is crucial for the long-term mechanical integrity of the tooth and is in accordance with minimally invasive dentistry principles.
Irrigation during endodontic treatment serves several purposes. When first accessing the pulp chamber, irrigant solutions flush out gross dentinal debris created by the cutting instruments. This improves visualization. With later exploration and preparation, irrigation lubricates canals, dissolves residual organic matter, and serves as an antibacterial agent.
None of the current irrigant solutions possess all the desirable properties to accomplish the purposes. However, sodium hypochlorite, ethylenediaminetetraacetic acid (EDTA), and chlorhexidine digluconate (CHX) are especially notable. Sodium hypochlorite (NaOCl) is the most popular irrigant solution and considered the current gold standard. It offers broadspectrum antimicrobial properties and the ability to digest organic matter. Concentrations of at least 3% are advocated to offset its cytotoxic potential, which causes a severe physiological response when extruded through the apical foramen into anatomical compartments. Frequent flushing can make up for the less potent solution. NaOCl cannot eliminate the inorganic components of the smear layer, which can harbor microorganisms.
EDTA is the second most popular irrigant and is often used in conjunction with NaOCl. It offers a chelating mechanism of action that eliminates the inorganic component of the smear layer.
The sequence of NaOCl followed by EDTA demonstrates a significant prognostic factor in the healing of periapical lesions in retreatment cases. EDTA exposure should be less than 5 minutes, although the ideal is 1 minute, to avoid increased dentinal erosion and reduced dentin microhardness, which may risk tooth fracture.
CHX is used at 2% strength and serves as a broad-spectrum antimicrobial solution effective as a root canal irrigant against a broad range of both gram-negative and gram-positive bacteria. It also has antifungal activity against common oral commensals that invade the root canal. As a final rinse, it’s absorbed into dentin and can function as an antimicrobial agent for up to 12 weeks. If CHX is used with NaOCl, an orange-brown precipitate can form that contains a cytotoxic substance (parachloroaniline [PCA]). This substance is carcinogenic in animals, so the use of both irrigants in the same patient is to be avoided.
Conventional irrigation should balance deep irrigant penetration against accidental extrusion, which is achieved by using an appropriate irrigating needle. This means avoiding needles with an open-ended design and larger gauge, which are more likely to bind to anal walls more coronally. Smaller gauge, side-vented, luer-lock designs are safer for disinfecting apical canals. Light finger pressure should be applied along with constant needle tip motion, which shouldn’t be advanced more than 2 mm from the working length. Operators may bend the needle or place rubber stoppers at this length to maintain length discipline during irrigation. In addition, use of a flexible polyethylene needle may offer good penetration into the canal, conform to the canal’s curvatures, and deliver irrigant at a high flow rate through 2 side vents.
If mechanical instrumentation is limited, operators must rely more on the chemical aspect of disinfection strategies. Several hand and mechanical agitation techniques can enhance irrgant activity and may prove more efficacious than conventional needle irrigation in eliminating residual dentin debris and the smear layer. They may also provide deeper penetration into the tubule. Both manual dynamic activation and gutta-percha point pumping can achieve smear layer and dentin debris removal from root canals.
Multisonic sound waves can also enhance cleaning efficiency so access cavities can be reduced in size, dentin can be preserved more effectively, and root canal treatment is easier with less compromise of tooth structure. Laser-activated irrigation has been applied to transfer energy through cavitation, creating intense liquid dynamics to achieve greater mechanical cleaning. A combination technique of NaOCl and EDTA can also be useful. The 1% to 5.25% NaOCl is used throughout canal exploration and preparation with frequent rinsing, then a 17% EDTA penultimate rinse is done less than 5 minutes after canal preparation, followed by a final rinse of sodium hypochlorite.
Biomechanical preparation and other approaches must be considered in a new light to come up with novel methods for disinfecting the root canals. It’s been suggested that dentin extracellular matrix components exist naturally and may have a use in material-directed pulp repair. Applying such types of innovative thinking is needed to improve the outcomes of root canal treatment.
Endodontics requires a sound understanding of the biological components of effective treatment. Advances in instruments and techniques are making root canal preparation easier and less time consuming. Some situations that were considered hopeless previously can now be addressed because of the developments in instrumentation and irrigation techniques. More biologically based treatment modalities for treating the root canal system may be developed that will make the shaping of root canals less important in the future.
Tomson PL, Adams N, Kavanagh D, et al: Non-surgical endodontics: contemporary biomechanical preparation of the root canal system. Br Dent J 238:478-486, 2025.
Reprints available from PL Tomson, University of Birmingham School of Dentistry, College of Medicine and Health, 5 Mill Pool Way, Edgbaston, Birmingham, B5 7EG, UK; e-mail: p.l.tomson@bham.ac.uk
Endodontic management that produces good outcomes requires systematic clinical assessment, accurate diagnosis, case complexity assessment, and treatment planning. These components were analyzed.
Histor y
The assessment begins with establishing a strong rapport with the patient, exhibiting empathy while collecting important information regarding his or her symptoms. Asking open-ended questions will encourage the patient to share concerns with the clinician. Use of the mnemonic SOCRATES may guide the collection of a thorough history, as follows:
• Site: Where is the pain located?
• Onset: When did it start?
• Character: What kind of pain is it—sharp, dull, throbbing?
• Radiation: Does the pain spread to other places?
• Associations: What other symptoms accompany the pain?
• Time course: Does the pain change over time? Does pain disturb your sleep?
• Exacerbating or relieving factors: What makes the pain worse or better?
• Severity: How severe is the pain on a scale from 1 to 10?
Having an accurate history is vital in establishing an accurate diagnosis and planning proper treatment.
Clinical Examination and Tests
The clinician should begin the clinical examination extraorally to determine if there is facial swelling or asymmetry. Systemic involvement may be indicated if the patient has pyrexia or difficulty swallowing or breathing. Airway restriction should prompt an urgent referral to the hospital. The TMJ and lymph nodes should be palpated to rule out TMJ dysfunction.
The intraoral examination focuses on potential causes of the symptoms reported. General dental hygiene status, oral soft tissues, and abnormalities should be noted. The clinician should palpate the mucosa around the tooth, looking for the contour and texture of the tissues, redness or yellowing of the tissue, fistulas, or discharge from soft tissues. Periodontitis screening is done, with a comprehensive periodontitis evaluation advised if there are deeper pockets. Isolated localized periodontal pockets around the tooth of concern may indicate an endodontic complication such as vertical root fracture (VRF), root perforations, or
a periodontally draining fistula tract. Periodontal pockets are usually formed because of bony destruction during a VRF progression, but no osseous defect or deep probing depth may be found in early stages of disease. These problems, along with recession, should also be identified.
The involved tooth should be assessed for remaining coronal tooth structure, state of existing restorations, fractures or cracks, discoloration, fremitus, or tenderness to percussion. Endodontic treatment may be indicated when coronal loss is significant. The retention of more than 2 mm of circumferential supragingival tooth structure and more than 30% of the original coronal tooth structure is needed to achieve restoratively predictable results after endodontic measures.
An occlusal examination is done to determine the occlusal load for any future restoration. In mixed dentition, both erupted and unerupted tooth positions should be noted, along with the condition and prognosis for questionable teeth.
Table 3. General Patient-specific and Tooth-specific Complexity Factors That Should Be Considered When Assessing Case Complexity18
Factor type Factor
General/patient-related factors
Tooth-specific factors
• Medical history
• Physical and psychological limitations
• Mouth opening
• Radiographic difficulties
• Complex diagnosis
• History of trauma
• The position of the tooth
• Inclination and rotation of tooth
• Pre-treatment before commencement
• Crown morphology and presence of extracoronal restoration (crown or overlay) (Fig. 2)
• Access to root canal system
• Root curvature (Fig. 3)
• Root canal morphology
• Apical morphology (Fig. 4)
• Canal radiographic visibility (Fig. 5)
• Previous endodontic treatment
• Iatrogenic incidents
• Root resorption
• Perio-endo (periodontic-endodontic) lesion involvement
(Data from Essam O, Boyle EL, Whitworth JM, et al: The Endodontic Complexity Assessment Tool (E-CAT): A digital form for assessing root canal treatment case difficulty. Int Endod J 54:1189-1199, 2021.)

2025.)
Sensibility tests include thermal tests and electric pulp testers (EPTs). Combining cold tests and EPT with clinical signs and symptoms will enhance diagnostic accuracy. A heat test using warm water in a syringe with a dental dam in place or warm gutta-percha points isn’t always practical but may be helpful. Selective anesthesia may help locate symptoms. In addition, laser Doppler flowmetry and pulse oximetry can help assess pulp vitality, but these tests aren’t always widely accessible in clinical practice.
Periapical radiographs (PAs) are preferred for endodontic assessments and are usually obtained using a beam-aiming device. They can identify periapical lesions, signs indicating bone resorption around the apex, and internal and external root resorption. Periapical radiolucencies can point to a range of conditions that have odontogenic and nonodontogenic origins. Both should be considered in the evaluation of the PAs to form an accurate diagnostic conclusion and determine the best treatment.

Figure 4. A traumatized tooth 21 with immature root development, resulting in an open apex. (Courtesy of Essam O, Umerji S, Blundell K: Endodontic assessment, complexity, diagnosis and treatment planning. Br Dent J 238:441-447, 2025.)
The conditions most often identified are periapical granulomas, periapical abscesses, and periapical cysts. PAs can also reveal caries, assess restorations, note pulp stones, and evaluate pulp chamber size. Other conditions that can be detected are widening of the periodontal ligament space, loss of the lamina dura, apical and lateral radiolucencies, and bone loss caused by perforations or root fractures. The clinician should take 2 or more PAs at different angles to identify unusual anatomic situations or superimposed pathologic conditions. Most endodontic lesions aren’t detectable on PAs until they reach the cortical and cancellous bone junction, so the absence of an apical radiolucency doesn’t indicate the absence of pathologic conditions.
Bitewing radiographs can also provide valuable insights into root morphology and pulp chamber position. With these images, the clinician can see the alignment and morphology of the roots, especially in multirooted teeth, and show the depth and location of the pulp chamber relative to the coronal structure. Bitewings can also suggest variations in canal anatomy, which should prompt further examination.
If 2-dimensional radiography results are inconclusive, cone beam computed tomography (CBCT) can provide detailed 3-dimensional imaging and achieve greater diagnostic accuracy.
After careful consideration of the patient’s symptoms, clinical examination results, and test results, a definitive or provisional diagnosis should be formulated. Both pulpal and periodontal diagnoses should be included, with the pulpal diagnosis covering the status of the dental pulp, whereas the periodontal diagnosis relates to the status of the periapical or radicular periodontium. Pulpitis may be an appropriate diagnosis for cases where the pain is poorly localized and triggered by thermal sensitivity. For severe pain that is induced through hot stimuli, remains over time, or occurs spontaneously without a trigger, irreversible pulpitis is a more likely diagnosis. Late-stage signs of irreversible pulpitis can include tenderness on biting or palpating adjacent soft tissues. In contrast, periodontitis of the periapical or periradicular tissues is more likely with well-localized, constant, throbbing pain that thermal stimuli have no effect on. The patient often has severe sensitivity to biting, feeling like the tooth is elevated, and possibly swelling.
Pulpal diagnosis has changed with the introduction of a classification system based on clinical symptoms. The 3 main classifications are mild reversible pulpitis, severe reversible pulpitis, and irreversible pulpitis. Other classification systems focus on the various stages of inflammation as more of a continuum.
Endodontic cases can vary widely in their complexity, but preemptively identifying cases that are more difficult can avoid some of the complications and adverse outcomes that could occur. Clinicians should identify which cases are within their scope of practice and refer accordingly. Factors to be recognized
in identifying complexity can be classified as patient-related factors and tooth-specific factors (Table 3 and Figures 3 and 4). The tooth-specific factors can be divided based on clinical history, tooth positioning, periodontal involvement, coronal/restorative factors, and endodontic factors.
Cases can be assessed using tools that systematically evaluate and collate factors to determine complexity. Contemporary digital assessment tools include mobile and web-based applications. Cases are determined to belong to 1 of 3 different categories based on risk for procedural errors and untoward outcome, with suitability for management based on 3 tiers of clinical experience. The difficulty grade can be increased by a single highly complex factor or an accumulation of multiple lowercomplexity factors. Complexity correlates with clinical expertise required and chair time expected, potential risks, and challenges involved in treatment.
The determination of the complexity of a case and evaluation of the challenges expected should be part of a comprehensive consent process and can inform appropriate management done by a qualified and experienced practitioner. An objective assessment summary can help in treatment planning and guide primary care providers in delivering effective communication and justification of the need for care to their patients. The assessments can be added to the patient’s clinical record to document that the clinician is operating within his or her competence. Case assessment tools for complexity-based triaging can improve patients’ access to primary care and referral services. Having a standardized and improved learning experience at the undergraduate and postgraduate level as well as in endodontic research are other benefits to using the case-management tools.
The objectives for treatment planning in endodontics are to ensure successful treatment of the pulp and/or periapical tissues, to maintain natural tooth structure, and to restore function. With the pulpal and periodontal diagnoses in hand, the options for treatment can be discussed, including no active treatment, vital pulp therapy, endodontic treatment, retreatment, endodontic surgery, or tooth extraction. The patient’s medical history should be considered as part of a holistic treatment plan. Whether endodontic treatment is appropriate at the present time or if a health care concern should be addressed first is an important consideration. Chronic health problems such as diabetes or corticosteroid therapy can impact the patient’s immune response and healing ability, which can have an adverse effect on tooth survival after endodontic treatment. The discussion with
the patient should consider the drugs being taken and whether retaining teeth or roots at the gingival level may be advantageous, even if they are structurally compromised. Anything that might compromise the endodontic outcome should be included in discussions with the patient before care begins. Referrals may be required, with the timing determined by what is in the patient’s best interests.
Other considerations in treatment planning are patient preferences, lifestyle, and financial situation. Patients who are in acute pain present significant challenges, especially if they were squeezed into the schedule. The process of collecting information to formulate appropriate diagnoses and the consideration of all the other factors that can influence treatment outcome often require both time and patience in delivering endodontic care. It’s essential to build trust and rapport with the patient, to be honest, and to remain transparent so that patient discussions will be productive and based on the patient’s best interests.
Endodontic patients can come for care with a multitude of different symptoms and require careful and detailed workups before an accurate diagnosis can be made. The clinician must use the tools provided to assess how complex the case is and if he or she is qualified and capable of providing excellent care. In addition, the situation must be carefully explored to ensure there aren’t any patient-related situations or tooth-related factors that can lead to a higher risk for failure of any treatment. The discussions about treatment options, prognoses, potential complications, and the institution of a provisional plan for care should be open and transparent about the challenges that may derail the process. Establishing trust between patient and practitioner equips patients to make better informed decisions about their care.
Essam O, Umerji S, Blundell K: Endodontic assessment, complexity, diagnosis and treatment planning. Br Dent J 238:441-447, 2025
Reprints available from O Essam, Dept of Restorative Dentistry, School of Dentistry, Univ of Liverpool, Liverpool, UK; e-mail: obyda.essam@liverpool.ac.uk
Local anesthetics (LAs) are used daily in dental inpatient and outpatient settings and are associated with a very low incidence of severe adverse reactions (ADRs). However, dental care providers must remain vigilant concerning the potential for ADRs. True allergic reactions appear to be rare, but can affect the therapeutic decisions of not just dental practitioners but also of surgeons, anesthesiologists, and other care providers. Reactions can be an immediate IgE-mediated reaction (type I) or a delayed T-cell −mediated reaction (type IV). The tools that prove most useful in identifying a true allergy are skin testing (prick and intradermal) and provocative subcutaneous challenge tests. Skin-prick testing (SPT) is performed with undiluted LA and controls. Intradermal testing (IDT) is performed with preservative-free, single-dose vials. The test sites are evaluated after 15 minutes. Subcutaneous provocation or challenge testing (SCCT) is done in skin test −negative patients as the gold standard to definitively exclude or prove an allergy. Articaine is one of the anesthetics used most often in dentistry, but the frequency of allergies to it remains unknown. The number of cases of confirmed allergic reactions to articaine in patients over the past 25 years was determined.
A comprehensive search of the PubMed-MEDLINE database was conducted. Ten case reports and 6 case series were found, from which 29 patients had documented authentic allergies to articaine.
The 18 patients whose age and gender were documented included 7 men and 11 women ranging in age from 8 to 65 years (mean age about 34 years). The women were 7.4 years older than the men. All of the patients had previously undergone at least 1 dental treatment where articaine was used as the local anesthetic.
The onset of allergy reactions occurred within 1 hour or after more than 24 hours. The allergies were confirmed through various skin tests, subcutaneous challenge tests, or patch tests. Twenty patients had an IgE-mediated type I allergy and 5 had a delayed type IV allergy, with 1 patient having a fixed drug eruption. The type of allergy wasn’t specified in 4 cases. In 3 cases, the patients had SPTs; in 11, IDTs were performed; and in 9
cases, SCCTs were done. To verify a delayed type IV allergy, 3 patients had a patch test.
A type I allergy was confirmed solely by IDT in 10 patients, SCCTs provided confirmation in 6 patients, and SCCTs plus SPT were performed in 2 patients. Patch tests yielded 2 positive results, but in the patient with a fixed drug eruption, only the SCCT was positive. The specific kind of skin testing wasn’t specified in 5 patients.
The clinical signs associated with skin testing ranged from swelling, discomfort, and pruritus to angioedema and generalized urticaria and edema. Allergic symptoms lasted 15 days or less. None of the patients experienced anaphylactic reactions or death. Three patients had cross-reactivity among the amide family, but other amides were tolerated in all but 1 case.
Although true allergies to articaine are very rare, dental care providers should be prepared to manage patients who suffer an allergic reaction. Patients should undergo a complete clinical history and standard allergological procedure to accurately diagnose the reaction.
If an allergy to articaine is suspected, the dentist should refer the patient to an allergy specialist or clinic for testing. SCCT is the ultimate procedure to confirm or exclude an allergy should skin testing prove negative or unclear. A suitable alternative agent should be kept on hand and substituted for articaine as appropriate. Patients should be informed about any LA that should be avoided and which ones cause no problems.
Halling F, Neff A, Meisgeier A: True allergies to articaine: A 25year analysis. Dent J 13:180, 2025
Reprints available from A Meisgeier; e-mail: axel.meisgeier@med. uni-marburg.de
Dental composites offer pleasing aesthetics and minimally invasive approaches to restoring dental caries and other defects. However, these materials are prone to recurrent caries, marginal defects, wear, and discoloration. The replacement or repair of defective existing composite restorations accounts for about half of all dental procedures done. The choice to repair or replace composite restorations is a clinical decision that faces dentists worldwide. Replacement involves removing the entire restoration and creating a single homogenous resin restoration. While it’s more aesthetically pleasing and offers better marginal seal, it can cause pulp irritation and unnecessary removal of sound tooth structure. Repair removes only the defective areas of the restoration and is a more minimally invasive approach that requires less time and is cost-effective. Minimally invasive techniques have been shown to increase the prognosis and longevity of the tooth. A population of Australian dentists was surveyed to evaluate their opinions, attitudes, and practices regarding repairing or replacing dental composites.
The survey was done on a convenience sample of dentists registered with the Australian Health Practitioner Regulation Agency. A 16-item questionnaire was made available online. The questions explored the frequency of restoring or repairing restorations, the perceived prognosis of a repaired restoration compared to a replacement, the reason for the practitioner’s decision, and the surface treatment used for the repair and why it was selected.
One hundred dentists (51% male) responded, with 93% general dentists and 7 specialist registered dentists. Seventy-seven percent work in private practice, 14 in a public practice, 6 in both, and 3 in a university (teaching) environment. Thirty-two percent had been in practice for more than 10 years, and 80% obtained their dental degree in Australia.
Six never repair restorations, 29 rarely replace composite restorations, 45 sometimes repair composite restorations, and 21 often repair composite restorations. None reported always repairing these restorations. For 55 participants, the prognosis of repaired restorations was seen as worse than that for replaced restorations. However, 30 thought the prognosis was comparable for the 2 options, 7 believed the repaired restoration had a better prognosis, and 8 weren’t sure how the prognosis differed between the 2.
Seventy-eight respondents felt partial loss or fracture of a restoration was the most likely reason to repair a composite restoration, with 61 indicating a noncarious marginal deficiency or overhang was a reason. Other reasons for repair included open contact, loss or fracture of a cavity wall, removal of marginal staining, recurrent caries, restoration of occlusal anatomy, or improvement of the color.
Repair was preferred to replacement for several reasons, with the most likely being the fact that repair was more conservative of tooth structure than replacement, followed by repair causing less pulpal irritation than replacement. Other reasons to favor repair included the remaining the portion of the restoration could stand the test of time, repair was quicker or easier, repair was more affordable, and repair didn’t require local anesthesia. Women tended to value conservativeness, less pulpal irritation, and quickness as reasons for repair, whereas those with more years of experience ranked marginal staining as an indication for repair.
The most important patient factor influencing the dentists’ decision to repair or replace a composite restoration was the caries risk of the patient, followed by patients’ finances, poor patient oral hygiene, medically compromised patients, and the patient being over age 65 years. Twenty-two of the participants didn’t allow patient factors to influence their decision to repair or replace a restoration.
When situational factors were considered, the most important was previous (failed) attempts to repair, followed by the tooth serving as an abutment for a prosthesis. Forty-nine of the participants said that restorations placed by another dentist influenced their plans for a restoration. Eleven reported no influence on their decision based on situational factors.
Tooth-level factors considered when deciding to repair rather than replace a restoration included proximity of the restoration to the pulp, volume of the restoration, number of restorative surfaces, and age of the restoration. Whether the margins were supragingival or subgingival also had some degree of influence. The occlusal load and involvement in guidance, the location of the restoration in the mouth, and the presence of marginal staining all had some effect on the repair or replacement decision.
Participants chose replacement over repair based on the lack of predictability or the prognosis of the repaired restorations,
a negative personal experience, a lack of knowledge regarding appropriate surface treatments, and negative feedback from other dentists. The least likely reason to forego repair was the difference in reimbursement for the 2 treatment modalities.
Of the composite surface treatments used by participants when bonding new composite to old composite, the most common one was acid etching, following by applying the bonding agent and curing, roughening with a diamond bur, and placement of retentive features. Other surface treatments were roughening with pumice, air abrasion, applying bonding agent and not curing, applying silane primer, applying flowable composite as an initial increment, and applying glass-ionomer cement as an intermediate material. None of the participants used laser irradiation or chose to simply rinse and dry when bonding new composite to old composite. The choice of surface treatments was based on personal experience for 72 dentists and based on university teaching for 44 participants. Eleven participants were of the belief that the treatment achieves an adequate bond to old composite but would change if they had more time during appointments. Twenty-two felt their treatment achieves adequate bond but would change if they had access to more equipment and materials.
Many Australian dentists still consider the repair of composite restorations as an inferior treatment to replacement. However, most agree on the indications for repairing and on surface conditioning techniques.
High-quality evidence is still lacking regarding composite repair techniques, with many dentists relying on personal experience to guide their choices. With a focus on minimally invasive dentistry and the conservation of tooth structure, repair of restorations is an important component of dental practice.
Khanna R, Han J, Liang E, et al: The current attitudes and practices of dentists in Australia towards composite repair: A cross-sectional survey study. Austral Dent J 70:49-57, 2025
Reprints available from R Khanna, 1 Parklands Dr, Southport Queensland, 4215, Australia; e-mail: rohit.khanna@griffithuni. edu.au
Dental sealants are a proven way to prevent dental caries, penetrating the pits and fissures of occlusal surfaces and forming a physical barrier against microbial colonization along with a favorable surface so patients can perform better oral hygiene. Sealant materials fall into the categories of resin-based sealants (RBS), glass ionomer sealants (GI), and polyacid-modified resin sealants. RBS products are used most widely and offer fluoride-releasing components. GIs also release fluoride over time and are moisture tolerant and easy to place, with resin-modified versions offering greater durability and reduced moisture sensitivity. The polyacid-modified resin sealants combine the adhesive and fluoride-releasing properties of GI and the strength of RBS, but also offer ease of application, which is highly valued when the patient is young or uncooperative. A review of the challenges in RBS dental sealant use, tips for practicing effective retention and application techniques, and some special considerations in sealant placement were offered.
Today, dental hygienists must maintain and enhance their proficiency in essential preventive procedures such as dental sealants while addressing concerns such as patients seeking nonfluoride interventions and the removal of fluoride from water supplies in the future. This requires comprehensive training, hands-on experience, and consistent professional development to ensure the highest skill levels. Hygienists must also be aware of technical aspects related to the use of dental sealants, specifically, the product qualities, strengths, and drawbacks as well as evidence-based guidance in their use.
Barriers and Misconception s
Proper application techniques, determining which teeth to seal, and skepticism regarding these materials contribute to an underutilization of dental sealants in practice. Among the concerns are the exposure of children to BPA, but the hygienist should be prepared to explain to parents that the minute amount of BPA exposure from sealants is far less than the daily exposures children experience. To avoid

any disagreements over this concern, sealant materials should be selected that are free of BPA.
The American Dental Association (ADA) supports the use of sealants and their many benefits. They offer primary prevention against caries, halt the progression of early and noncavitated caries when done correctly, and are covered by many dental plans.
Sealants differ in forms, viscosities, colors, and filler content, all of which influence their physical properties, flowability, and wear resistance. Unfilled or low-filled sealants have a low viscosity and deeper fissure penetration, with better retention. They require no occlusal adjustment and wear down quickly. Incorporating fillers improves wear resistance and reduces shrinkage, increases durability, and lengthens the period of effectiveness.
The literature indicates that there is no significant difference in retention rate or caries development when filled and unfilled RBS products were compared over the course of 2 years. Thus, the choice of sealant should be tailored to factors such as fissure type, patient age, and habits.
Steps can be taken to promote the effective retention of skills and consistent techniques in sealant application. The staff should be trained on sealant placement using hands-on sessions with
extracted teeth or typodonts. The training should address contamination, curing mistakes, and incomplete preparation with the aim of reducing mistakes and improving outcomes.
The tools used should be assembled so the procedure can be accomplished smoothly and efficiently. This includes isolation materials, curing light, sealant material, acid etch gel, mouth mirror, explorer, prophy brush, cotton pellets, and articulating paper (Figure 1).
The team should be educated in the proper preparation of the tooth surface using mechanical as well as chemical debridement. For the mechanical approach, which is the traditional method, an air polisher or pumice slurry is used to eliminate plaque and debris, which promotes retention. This method works for enamel preparation, but chemical cleaning achieves better bacteria removal and better retention. The chemical method uses 1 drop of over-the-counter 3.5% hydrogen peroxide, which penetrates into grooves to remove plaque and kill bacteria. A cotton swab or microbrush can be used for removal. The goal of these debridement measures is to provide a clean surface and optimal sealant adhesion.
The grooves should be carefully examined for signs of caries. Applying a small amount of silver diamine fluoride (SDF) may improve detection efforts.
Moisture control is essential for sealant placement. Contamination with saliva can increase microleakage and reduce bond strength.
Phosphoric acid etching significantly lowers microleakage, making this a better method than air abrasion and laser conditioning. The 37% phosphoric acid application can be done for 15, 30, 45, or 60 seconds, with the longest duration having the highest shear bond strength. The difference between a 30- and 60-second etch is minimal, so a 30-second etch may be clinically acceptable.
In some cases, it will be necessary to remove excess moisture to improve sealant retention. The moisture may collect in the grooves, where a “water chase” or prime-and-dry material may provide a clean, dry enamel surface. The dry and uncontaminated field should be monitored to ensure that it remains intact.
The sealant material should be applied precisely so that it penetrates deep pits and fissures. An explorer can be used to manipulate the material into challenging areas. No excess material should be left to interfere with occlusion or cause premature wear.
Light curing using verified output strength is needed to achieve adequate polymerization. The light is placed close and perpendicular to the sealant surface. Manufacturer’s instructions for curing time should be followed for the best results, with careful inspection to detect any uncured material.
For optimal retention of hypomineralized teeth, the hygienist must overcome their increased resistance to etching that results from reduced microporosity compared to normal teeth after acid etching. It’s important to establish enough micropores on the enamel surface. If enamel hypomineralization is present, the etch times should be extended to boost microporosity.
The hygienist should avoid using fluoridated prophy paste or applying fluoride varnish before the dental sealant is placed. Fluoride inhibits the etching process by reducing the enamel’s ability to form the microporous texture needed for optimal sealant retention. The fluorapatite layers that fluoride creates are more resistant to acid and less prone to etching.

Figure 3. Voco’s sealant (Grandio Seal) being spread on occlusal surface without using an explorer tip. (Reproduced with permission from VoidHolmes JD: Perfectly placed, perfectly sealed: 10 best practices in dental sealant application. RDH Mag 45:32-35, 2025.)
When cannulas are used, the hygienist should avoid the large, blunt-ended ones because they can’t effectively penetrate intricate grooves. An explorer must be used to guide the material when these large cannulas are used because the blunt profile can’t match the tapered design and access the fine details (Figure 3).
Dental professionals can provide optimal sealant application by following the instructions offered. This will require a proper selection of the materials and tools used. Paying close attention to the details will lead to reliable, durable prevention of dental caries.
Void-Holmes JD: Perfectly placed, perfectly sealed: 10 best practices in dental sealant application. RDH Mag 45:32-35, 2025.
Reprints not available
An in vitro study was done to assess the success of indirect pulp capping (IPC) procedures over a 40-year span of time. IPC is generally not used today because of the modern understanding
of caries excavation. Selective excavation is now preferred to the “complete” and aggressive caries excavation carried out in the past. The long-term clinical performance of restorations using IPC was evaluated.

Figure 3. Development of pulp vitality over 40 years. (Reproduced with permission from Frankenberger R, Koch A, Plohmann L, et al: The outcome of old-school indirect pulp capping over 40 years: A practice-based retrospective evaluation. Dent J 13:182, 2025.)
A review of 1412 dental records yielded 159 patients with 366 IPC teeth whose treatments were delivered from 1969 to 1980. The teeth had caries in the inner third of the dentin, were free of symptoms, and had no pulp exposure. Caries lesions were excavated thoroughly but the pulp was not exposed. Posterior teeth were restored with amalgam, and anterior teeth received direct resin composite fillings. Treatment success was defined as maintaining vitality of the tooth beyond 365 days, with loss of vitality considered failure. The outcome of treatment was measured at 1 and 6 months as well as 1, 2, 5, 10, 20, and 40 years. The possible influences on survival rates included the following: age, gender, tooth location/position, dates of vital therapy, number of filled surfaces, types of primary restoration material, treatment on each tooth, and last dates of surveillance.
Sur vival over the First Year after IPC
A total of 336 of the 366 indirectly capped pulps survived the first year (92%). During the first 10 days, survival rate dropped from 100% to 97%, then to 95% in the first 30 days, and to 94% after 3 months. This means the success rate of IPC was 92% because only failures until 12 months were defined as being related to the IPC treatment.
In the first month, 18 IPC treated teeth failed, with 5 being extracted and 13 receiving root canal treatment. A total of 23 teeth had failed after 3 months, with 2 removed and 4 receiving root canal treatment. Failure remained unchanged for 4 months, but from the ninth to the twelfth month, the failures rose to 30 teeth.
Over the 39 years of observation, pulp vitality loss occurred in a linear pattern. Vital pulp testing revealed there were 88% of the teeth that were vital after 2 years, 80% after 5 years, 70% after 10 years, 57% after 20 years, and 32% after 40 years. The annual failure rate was 1.7% (Figure 3).
The probability that an IPC treated tooth and subsequent 2surface filling would survive 40 years was 36%. Survival probability was significantly higher for these teeth than for teeth lacking information about the filling size. A statistically significant difference was noted in the survival curves based on cavity size. Either 2- or 3-surface filling was done in the 336 teeth examined most often. One-surface fillings were placed about half as often. Overall, the cavity size had no negative impact on survival over the 40 years of observation.
Wisdom teeth had a higher survival rate than other teeth, with 93% after 2 years. When considering the survival rates after 5 years to be 66%, the wisdom teeth value was relativized. Survival rates of wisdom teeth were worse than those for anterior or posterior teeth. Posterior teeth were the largest cohort and had 262 of 296 teeth surviving in the first 2 years. Survival rates didn’t differ significantly when based on tooth position.
The long-term success (40 years) of teeth receiving IPC done using zinc-oxide-eugenol cement was excellent. More failures occurred in the first 3 months than the rest of the period, with larger defects associated with more frequent loss of pulp vitality.
The annual failure rate after 40 years of clinical service was just 1.7%, which is an excellent result. Today’s approaches differ significantly from those used 40 years ago, with selective removal of caries considered a more advisable approach than using IPC.
Frankenberger R, Koch A, Plohmann L, et al: The outcome of old-school indirect pulp capping over 40 years: A practicebased retrospective evaluation. Dent J 13:182, 2025.
Reprints available from R Frankenberger, Dept of Operative Dentistry, Endodontics, and Pediatric Dentistry, Medical Ctr for Dentistry, Univ Medical Ctr Giessen and Marburg, GeorgVoigt-Str 3, D-35039 Marburg, Germany; e-mail: frankbg@med.uni-marburg.de
Sleep bruxism (SB) is a masticatory muscle activity that occurs during sleep in about 15% of the adult population. It has a phasic or a tonic (rhythmic or nonrhythmic) pattern and isn’t considered a movement disorder or sleep disorder in healthy persons. Its diagnosis and treatment remain challenging, but risk factors have been identified, as follows: exogenous factors such as smoking, heavy alcohol intake, caffeine, medications, or illicit drugs; psychosocial factors such as perceived stress and anxiety; sleep disorders, especially arousal; and comorbidities, which include obstructive sleep apnea (OSA) and gastroesophageal reflux disease (GERD). Recent research indicates a possible link to the neurotransmission of the serotonin and/or dopamine pathway, with severe SB possibly co-occurring with lower serotonin blood levels but not with the blood levels of enzymes involved in the serotonin synthesis pathway. Genetic factors have now been suggested, such as the polymorphisms in the genes encoding dopamine and serotonin receptors possibly being linked to a predisposition to SB and SB pathogenesis. A potential association may exist between SB and OSA in adults, with similar links to genes encoding dopamine receptors in children. Children have an increased risk based on their consumption of sugar, length of screen time, and sleep habits. The current management efforts for SB were noted, with new approaches suggested.
SB management has focused on minimizing the negative effects of this disorder. To this end, treatment has used intraoral appliances, physical therapy, biofeedback, and botulinum toxin injections. Psychotherapy and stress-coping strategies have been used to eliminate potential risk factors. Some drugs may reduce the number of SB episodes, and the treatment of comorbid conditions such as OSA and GERD has been undertaken. For OSA treatment, the use of continuous positive airway pressure (CPAP) and mandibular advancement devices has been helpful.
No evidence clearly indicates which management technique is the most effective.
Based on the latest research, some new methods of treatment have been suggested. These are combining issues such as lifestyle, daily habits, sleep hygiene, and diet (Figure 1). The goal is to eliminate risk factors instead of focusing on SB’s negative consequences.
The patient with SB should be aware of the harmful effects of chronic stress and poor sleep quality and take measures to alleviate stress and improve coping strategies. Among the everyday behaviors that can reduce stress are maintaining a good work-life balance; engaging in regular physical activity, especially outdoor and nature-related activities; and doing breathing exercises. If patients continue to struggle with the stress, practicing mindfulness, meditation, and cognitive behavioral therapy (CBT) may prove helpful.
The structure and quality of sleep can be impacted by following good sleep hygiene habits. This includes avoiding the consumption of alcohol and coffee, smoking, and sugar intake at bedtime. Screen time should be limited, as should exposure to blue light. The sleep environment should be quiet, dark, and at a proper room temperature so the individual can sleep the appropriate number of hours. Having a regular bedtime is also helpful.
Light exposure affects the human circadian cycle, with blue light exposure from electronic devices stimulating the nervous system and leading to problems with sleeping. A 2-hour exposure to blue light (460 nm) before bed suppresses the secretion of melatonin. In addition, a 1-hour exposure to bright light or blue light increases stress hormone levels in saliva. The use of

Figure 1. Sleep bruxism (SB) management methods, including the methods used so far and novel approaches. (Reproduced with permission from Więckiewicz M, Smardz J, Martynowicz H: Lifestyle, daily habits, sleep hygiene, and diet: Proposal of a new approach for sleep bruxism management. Dent Med Probl 62:5-7, 2025).
electronic devices during daylight as well as at bedtime can result in short sleep duration, delayed sleep onset, and an increase in sleep deficiency. Similar problems are seen in children, with studies linking screen time to increased frequency of bruxism.
Some reports suggest autonomic nervous system dysfunction may be related to arousal during sleep, leading to cardiovascular implications among patients with SB. Sympathetic activity increases heart rate variability, inflammation, oxidative stress, endothelial remodeling, and hormonal disturbances, all of which can lead to hypertension and other cardiovascular problems. Physical activity and other habits that influence the cardiovascular system may benefit patients with SB.
Substances that may influence the severity of SB include caffeine, excess sugar, narcotics, and some medications, all of which should be limited. Substances that have a beneficial effect on the nervous and muscular system, reduce stress, and improve sleep include microelements such as magnesium, calcium, potassium, zinc, and iron; vitamins B and D; and possibly omega-3 fatty acids, which support overall nervous system health. If neurotransmission, especially that related to the serotonin system, is
indeed related to SB, patients should consume a diet rich in tryptophan, which includes carbohydrates and proteins. Examples include fish, bananas, seeds, avocado, and eggs. Dietary fiber consumption may also improve SB, since at least 1 study showed students with SB had a significantly lower dietary fiber intake than those without SB.
SB is a complex and as yet not fully understood condition that offers both diagnostic and therapeutic challenges. The latest research indicates that treatment methods should focus on patients’ lifestyle, daily habits, sleep hygiene, and diet.
Various factors other than those observed traditionally may be linked to SB. In addition to making changes in lifestyle, daily habits, sleep, and diet, the research suggests there may be a genetic component. Ensuring that patients focus on obtaining effective treatments for co-occurring conditions as well as on improving their lives and health behaviors may be able to provide better resolution of the challenges of SB.
Więckiewicz M, Smardz J, Martynowicz H: Lifestyle, daily habits, sleep hygiene, and diet: Proposal of a new approach for sleep bruxism management. Dent Med Probl 62:5-7, 2025.
Reprints available from J Smardz, Dept of Experimental Dentistry, Wroclaw Medical Univ, Poland; e-mail: joanna.smardz@umw. edu.pl
Mental health is a state in which the individual recognizes his or her full potential, copes with the stresses of life, works effectively, and contributes to society. Resilience, although seen as a valuable commodity, is less clearly defined but essentially is seen as the ability to bounce back from significant adversity by positively adapting to the changes. It tends to exist along a continuum rather than either being present or not. The level of resilience varies as a result of factors such as the environment, interpersonal
interactions, and personal resources, including emotional intelligence, autonomy, cognitive flexibility, self-determination, and self-worth. Dentists who perceive themselves to be resilient tend to deal with stress intuitively, but those who are less naturally resilient usually rely on deliberate strategies such as mindfulness, exercise, and speaking out to assert themselves. It’s likely that resilience-enhancing education and strategies aren’t widely available to support all members of the dental team. A survey was conducted to identify the factors that may support or erode resilience to dental environmental stress for the various dental
team members, with reports from the representative participants about how they operationalized their resilience.
A sample of 22 participants was gathered that reflected dental professionals from different regions and working environments. Seventeen semi-structured interviews were conducted online, and 5 were done face-to-face at a dental conference. The interviews were recorded, transcribed, and subjected to a thematic analysis. Eleven themes were identified (Table 3).
The themes related to the working environment dealt with patient expectations, pressures, and team dynamics. Most participants identified patient expectations as a primary factor that challenged their resilience. Participants who worked in the National Health Service (NHS) system were especially mindful of this factor, although those in the private referral sector also saw it as an issue.
Pressures based on time management, financial concerns, and workloads were also prominent themes related to working. Both clinical and dental laboratory workers expressed time pressure as a challenge. The clinical workers said the pressure arose form their own patient schedule and their support for the clinician’s schedule. The dental laboratory workers saw time pressures emerging from unrealistic expectations from dentists about turnaround times for their work. In addition, having poor communication led to problems in satisfying patients’ concerns. Practice owners experienced financial pressure, but other team members also saw external pressure to meet quotas, for example. Often the workload for workers in management positions, especially the paperwork demands, meant they had to take work home to complete it. Participants who were working in academia noted that their workload made it difficult to maintain a work-life balance.
Anxiety in the working environment arose from workers feeling out of their comfort zone. Dissatisfied patients, especially when dentists were newly qualified, were also a source of stress. There was concern over how well their competence was perceived by the lead dentist.
Issues with team dynamics illustrated the importance of good team work and clear communication for all dental workers. Some participants saw having a hierarchal system as a barrier to improving their working conditions and as a hindrance to approaching management with a concern. Dental technician (DT) and clinical DT participants felt the lack of communication was a problem. This led them to feel disconnected and unclear about their role. Lack of regular feedback from the dentist contributed to a sense of isolation. Often the only communication they received was to point out a problem with the laboratory work.
Theme 1: factors challenging resilience
Theme 2: factors enhancing resilience
Theme 3: positive emotions enhancing resilience
• Expectations associated with working environment
• Pressures associated with working environment
• Team dynamics
• Taking a balanced view
• Engaging with support networks
• Achieving work/life balance
• Diversity and variety in role
• Organisation
• Sense of purpose
• Gratitude
• Positive relationships
(Reproduced with permission from Harris M, Eaton K: Exploring dental professionals’ perceptions of resilience to dental environment stress: a qualitative study. Br Dent J238:395-402, 2025).
Resilience in the team dynamics also suffered from a lack of autonomy, especially by workers in support positions. Clinicians in the corporate setting cited the lack of autonomy as deleterious to resilience.
Taking a balanced view of the situation, engaging with supporting networks, achieving work-life balance, experiencing diversity and variety in the individual’s role, and instituting organization were among the issues that dealt with putting things into perspective. Study participants were able to achieve balance by viewing things from different aspects and consistently maintaining a positive mindset and self-acceptance. Accepting individual roles and responsibility could be challenging, but it was important to recognize the bigger picture and accept the degree of control one had over situations. Optimism for the sustainability of a dental career was an important attitude for newly qualified participants. Shifts in mindset could be important to enhance resilience.
Supportive networks were mentioned by all of the participants to some extent. Some expressed the importance of having a mentor to thrive in their position. Mentors were seen as especially valuable early in a dental career, but their support remained a strong influence even at a more advanced practice position. Peer support networks, outside support networks, and family support systems were all of value, but participants weren’t necessarily looking for solutions their problems in these relationships.
Achieving a work-life balance was mainly viewed as evidence of resilience by those who had the ability to separate their work from their home life and not take work home. Working in private practice was seen as structured and easily left behind to focus on home life. Those working in academia found digital technology to be intrusive on home life, creating a tension in this area. Having a set holiday schedule tended to compensate academic practitioners for the long hours spent at other times of the schedule.
Overall, having a reduced working week was perceived as achieving a good work-life balance, but it was more likely to be true of those at the end of their careers when they had the financial stability to choose not to work so much.
Some participants valued diversity and variety in their everyday practice as a way to maintain their enthusiasm for work. Education and training were pursued by some as a way to enhance personal and professional development. Others chose to engage in activities that served dentistry as a whole.
Organization was a key element for enhancing resilience for most participants. Some dental nurse participants felt that working outside of their paid hours so they could have an organized day was part of their routine. Clinicians who had control over their day saw this autonomy as vital to their feelings of providing the best treatment for patients. Flexibility and insight into their interpersonal skills was also seen as important.
The attitudes seen as contributing to resilience included a sense of purpose, gratitude, and positive relationships. All participants believed their role fulfilled their sense of purpose and made a difference in the lives of others. Strong sentiments were expressed by more experienced participants as they outlined why they remained in the dental profession. Participants also noted that a positively functioning team was important. Being able to work in unique circumstances underscored the sense of making a difference.
Participants were cognizant of the stresses of their profession, but felt a sense of contentment and gratitude for the role they were allowed to take. Being grateful for having a skill set that served the greater good was commonly expressed.
Along with these attitudes, participants experienced contentment related to working in an environment that facilitated
complete trust from the public. These positive relationships were very much expressed by the majority of participants. Good relationships with other team members were also considered a key feature of their resilience.
The dental team experienced resilience in their environment regardless of the stressors related to their work. Many experiences were common to all types of dental workers, but some were unique to certain groups. To further enhance the sense of mental health and resilience, some may require the expansion of coping or preventive strategies.
Knowing that they are able to function well and contribute to the good of others were common themes among dental team members. A range of issues will influence resilience and mental health for these practitioners, and further investigation and interventions may be needed to improve life for some dental team members.
Harris M, Eaton K: Exploring dental professionals’ perceptions of resilience to dental environment stress: a qualitative study. Br Dent J238:395-402, 2025.
Reprints available from M Harris, School of Dental, Health, and Care Professions, Faculty of Science, Univ of Portsmouth, Portsmouth, UK; e-mail: marina.harris@port.ac.uk
Swimming is well-recognized as a popular sport in Australia, with an estimated 6 million Australians swimming annually at various levels ranging from recreational to competitive. Brown-yellow extrinsic staining on swimmers’ anterior teeth is believed to result from interactions between disinfectants and chemicals such as chlorine in swimming pools. Salivary proteins are denatured, forming deposits on the teeth that consist of both organic and inorganic components. The prevalence of this staining found in various studies ranges from 12% to 91%.
Stain formation correlates with the amount of time spent swimming in chlorinated pools, with more than 6 hours of training a week determined to be the length of time needed to increase the risk of dental stains. Stains in the aesthetic smile zone can be distressing to children and their families, especially because this stain is more tenacious than calculus and can’t be removed by frequent brushing or frequent professional cleanings. The prevalence of dental staining in children swimming competitively was compared to that in the general Australian population, and the impact of dental staining on oral health−related quality of life was explored.
Four swimming clubs and a total of 100 competitive swimmers and 100 age-matched controls (age 9 to 17 years, mean age 12.5 years) participated in this study. All participants (or their parents for those age 12 years or younger) completed a survey, then intraoral frontal clinical photos of the swimmers were obtained using a digital single-lens reflex camera. Photos of the dentally age-matched group served as controls. The degree of staining was measured using the Lobene Stain Index, then a Global Stain Score (GSS) was calculated for each participant. Estimated lifetime swimming hours were calculated for each participant.
A relatively regular pattern of professional dental cleaning and tooth brushing was found among the participants. Staining prevalence in the swimmers was 83%, but it was 44% in the control group. The odds of staining among swimmers significantly exceeded that of the control group.
A significant positive correlation was noted between GSS and actively avoiding smiling, total lifetime swimming hours, and practice time. A significant negative correlation was found between GSS and the consumption of colored beverages. GSS didn’t show any other significant correlations with external stainrelated factors. The difference between the GSS of swimmers and that of age-matched controls was statistically significant. Staining prevalence across the low-, medium-, and high-volume
swimmers was greatest for the low-volume swimmers and lowest for the high-volume swimmers.
Dental staining was common in young swimmers among the Australian population. It was significantly greater among competitive swimmers than non-swimmers and wasn’t associated with oral hygiene practices or the consumption of colored beverages.
Swimming hours and length of practice sessions were associated with both the extent and the intensity of dental staining in young swimmers. GSS and smile avoidance were related, with staining negatively associated with the youths’ oral health related quality of life.
Patel J, Cai S, Huong B, et al: Competitive swimming and dental staining among Australian children. Austral Dent J 70:42-48, 2025
Reprints available from J Patel, UWA Dental School, The Univ of Western Australia, 17 Monash Ave, Nedlands, WA 6009, Australia; e-mail: jilen.patel@uwa.edu.au
Dental unit waterlines (DUWLs) must meet the standard set by the Centers for Disease Control and Prevention (CDC) guidelines, which is the Environmental Protection Agency’s standard of <500 cfu/mL. The American Dental Association (ADA) and the Occupational Safety and Health Administration (OSHA) agree. A system must be in place that ensures water used for patient care and for employee safety meets or is less than this threshold. The only way to know the water is safe is to test it. Water that is over the standard could adversely affect the health of those who are exposed to it. Dental staff must know the source of the water and how to shock it and test it to ensure the standard of care is met.
Centralized System or Water Bottles
The dental team must know where the water that comes out of the air/water syringe, handpiece, scaler, etc comes from. If it
comes from city plumbing and goes directly into the chair, you need to decide if you want to install a centralized system to provide an antimicrobial agent that treats the biofilm that grows in the lines. A service tech can install a cartridge in the junction box on the chair that delivers this antimicrobial agent into the lines. Inline systems can eliminate some daily waterline maintenance but require a service tech to remediate issues. If a boilwater advisory is called, the office must close until the water is safe again.
The other option is to have the chairs retrofitted to have a bottle reservoir system. Dental unit water bottles permit more autonomy over the water protocol, with the option to choose from various products, the ability to remain open during a boilwater advisory, and the ability to shock the lines as needed. Bottles have the downside of becoming empty during a procedure. The Association for Dental Safety (ADS) and ADA recommend dental unit water bottles, but each office is free to decide what works best for them.
With a dental unit water bottle, you can choose what water to fill it with, including distilled water, store-bought spring water, tap water, or even sterile water. Sterile water isn’t sterile after it enters the dental unit—just something to consider. You should look at the instructions for use (IFU) for both the chair and the treatment product to determine what water is best for your practice.
Shocking is using a high-level disinfectant to blast through the biofilm sitting in the DUWLs, and many products are available (Box on page 44). They vary in strength, so it’s good to check the IFUs for the dental chair to see if it makes recommendations or advises about products not to use. You should follow the IFUs to avoid damaging the chair or not providing an effective disruption of the biofilm.
It’s also important to check the chair and treatment product IFUs for recommendations regarding the testing routine (Box on p. 45). If none are present, the ADS recommends monthly testing until you have 2 consecutive passes, then doing quarterly testing. If a test fails, you should go back to monthly again.
The test options are mail-in or in-office methods. Both will monitor the DUWLs. The advantages of chairside tests are convenience, confidentiality, and lower cost. Mail-in tests provide third-party validation and more precise results. A mix of the 2 approaches can also be used, perhaps doing a mail-in once a year and the chairside tests the remainder of the time.
If you don’t follow the instructions for the chairside test closely, the result can be inaccurate (Table 1). Some tests use a colorchange method, but you must be able to distinguish colors clearly. Some grow microbes on a paddle, which can require an incubation temperature to avoid a delay in getting the microbes to grow.
• Choose a product and read the IFUs.
• Put the shock product into the dental unit water bottle.
• Run it into every line that can get water.
• Leave it in for the recommended time (not longer or shorter).
• Flush the lines with warm water thoroughly into a sink or bucket (not into your suction).
(Reproduced with permission from Hill A: The basics of dental unit waterlines. RDH Mag 45:44-46, 2025.)
Things to note Will NOT work past expiration date Will NOT work past expiration date If you have trouble distinguishing color, results will be challenging to read If you have trouble distinguishing color, results will be challenging to read IFUs state this is a screening test and cannot be used to certify water as safe or unsafe
(Reproduced with permission from Hill A: The basics of dental unit waterlines. RDH Mag 45:44-46, 2025).
• Read the IFUs.
• Determine how many lines you are testing.
• Decide if you are doing pooled sampling or individual lines.
• Wash hands and don gloves.
• Flush lines for 30 seconds.
• If pooled sampling, take equal amounts from each line.
• Start with the air-driven handpiece (or the air will blow out the whole sample).
(Reproduced with permission from Hill A: The basics of dental unit waterlines. RDH Mag 45:44-46, 2025).
The most popular mail-in tests are R2A and flow cytometry. R2A is the gold standard and takes the water sample and incubates it on an agar plate, then the laboratory checks for microbial growth in 5 to 7 days. Flow cytometry has proved to be very accurate and uses lasers and fluorescence to detect all bacteria—both living and dead. Live biofilm loves dead or damaged bacteria to hide in and to use as food. Flow cytometry requires just 20 minutes to complete.
All the lines that can get water should be tested, whether they are used or not. An unused line is termed a dead leg and can often serve as a source of biofilm. It should be capped off at the source by a service tech or be flushed regularly if it remains open.
When collecting the sample, follow the IFUs for the method you’ve selected. For a mail-in test, you must freeze an ice pack for shipping and ensure the laboratory is open to receive the sample. You can test each line individually or take a pooled sample, which means taking equal amounts from each line in 1 operatory. If you pass, all the lines are good; if you fail, shock all the lines again.
Disinfecting an operatory’s water lines is essential to ensure that the water is safe for use for patients as well as dental staff. The keys to doing it right are following the IFUs for each step of the process and testing regularly.
Hill A: The basics of dental unit waterlines. RDH Mag 45:4446, 2025
Reprints not available
Taking the patient’s blood pressure in the dental office may be the introduction to a discussion about a possible health concern. Some patients will claim a high reading is just “white coat” syndrome and it only occurs at the dentist’s office. The hygienist is uniquely positioned to invest the time to talk to patients about what a high blood pressure reading means and why there is a reason to be concerned.
If the patient responds to the a high blood pressure reading with the news that he or she has white coat syndrome, the hygienist can ask whether, if this is a response to stress, his or her blood pressure changes in other stressful situations and how this
instability might affect their heart health. It’s good to determine where else they screen their blood pressure, and if they don’t do it elsewhere, question how they know it’s only high in the dentist’s office.
Medically, having a significantly elevated blood pressure reading but a normal pulse is unusual because stressors tend to increase tachycardia. Citing this truth may make the patient more interested in determining if the pressure is more than just stress.
White coat hypertension isn’t a benign condition, because uncontrolled, persistent, and isolated instances of hypertension can be more dangerous that hypertension that has been diagnosed and is being treated. About 40% to 50% of people with white coat hypertension will progress to sustained hypertension
Source: https://www.hear t.org/-/media/Files/Health-Topics/High-Blood-Pressure/HBP-rainbow-char t-English.pdf Reprinted with permission. American Hear t Association, Inc.
and many won’t seek care in time to avoid a cardiovascular event causing morbidity or mortality. Patients who have white coat hypertension are twice as likely to die from heart disease as those who are taking antihypertensive medications or who have healthy blood pressure scores. They are also 3 times more likely to suffer a heart attack in the future.
Only blood pressure that is under 120/80 mm Hg is normal despite how the patient feels. Hypertension is often asymptomatic until serious symptoms occur during a cardiac event. The American Heart Association (AHA) defines hypertension as a systolic reading of at least 130 and a diastolic reading of at least 80 (Table 1). Most adults can experience an increase of 10 points in a medical setting compared to readings taken at home; the reading returns to normal in about 10 minutes. Although many people see higher values as white coat hypertension, elevated numbers actually reflect internal events that increase the risk of a heart attack or stroke and require further evaluation. Values exceeding 160/100 mmHg may require medication or an adjustment to current medications, possibly delaying dental care that requires local anesthesia until things have stabilized.
To determine if a patient has isolated or chronic hypertension, he or she should undergo 24-hour ambulatory monitoring, but currently this service is limited in health care. Efficient at-home monitoring followed by a visit to the
physician, blood work, and a referral to a specialist may be indicated. Patients should be given a copy of their in-office reading and of the AHA guidelines and be shown how to use the device at home. Often a wrist cuff is beneficial as long as it’s correctly positioned on the radial artery and held at heart level. This allows the collection of data that can then be reviewed with their physician.
Ideally, physicians will do a thorough cardiac workup based on scientific evidence rather than just express an expert opinion or perform standard or unreliable testing. Among the noninvasive tests that can be done are genetic testing to identify genetic markers, a 2-hour oral glucose tolerance test (OGTT) to screen for diabetes, and ultrasounds and scans to discover any hidden red flags. Arterial obstruction assessment may reveal percentages of concern. Lifestyle modifications are a critical part of these discussions, one that hygienists are welltrained to perform using motivational interviewing.
Hygienists know the associated risks of hypertension and can take time with their patients to provide important information about the relationship between cardiac and oral health. They can share facts such as the following:
• Patients with periodontal disease have double to triple the risk of a heart attack or stroke, and those who smoke or have diabetes have even higher risks.
• The risk of death increases by 20% to 25% for patients who don’t brush their teeth at night, 30% for those who never floss, and 50% for those who haven’t seen a dentist for 1 year.
• High percentages of oral pathogens are seen in the arterial blood clots sampled from at-risk patients, possibly indicating that oral infections related to decay or periodontal disease may trigger half of all heart attacks.
• Patients with periodontal disease and hypertension are at significantly higher risk for developing Alzheimer’s disease.
These observations regarding the oral-systemic disease link can encourage patients to take their blood pressure and their oral health seriously.
Hygienists advocate for their patients’ health and safety. If a patient’s blood pressure is elevated at a medical visit, it’s likely elevated at other times. Hygienists can encourage patients to continue their at-home monitoring and talk to their primary care physician about how to mitigate heart attack and stroke risks. Organizations such as the National Network of Healthcare Hygienists can provide access to efforts to become more integrated with the medical side of patient care.
Dental health and systemic health have shown many linkages and common risk factors. High blood pressure revealed during a visit to a healthcare provider shouldn’t be dismissed as white coat
hypertension but should be further investigated to ensure that it isn’t a precursor of serious conditions such as heart attacks and strokes. The hygienist can play an important role in educating patients about the risks of what they call white coat hypertension.
Patients can be insistent about calling their high blood pressure in a dental or medical setting just white coat syndrome. It would be easy for a hygienist to give up and end the conversation regarding blood pressure, but hygienists should be vigilant on their patients’ behalf and encourage them to see that they are treating the whole patient and not just their oral health. Intervening may well save a life.
Reprints not available
The prevention of gingival diseases and dental caries is based on the regular removal of microbial dental plaque. Dental care practitioners stress optimal oral hygiene practices to their patients, including mechanical plaque removal through brushing and flossing plus using mouthwashes that contain antimicrobial agents. Having fewer microbial agents in the oral cavity helps to minimize the risk of inflammation, subsequent periodontal tissue destruction, and the progression of carious lesions. When mechanical plaque removal is insufficient, chemical agents that target pathogenic microorganisms can be vital, which has led to research on the development of tailored antimicrobial agents designed for individual use. The compounds being studied include essential oils, natural extracts, and synthetic agents. The research is targeted at identifying which agents have the optimal efficacy against oral pathogens and still minimize their adverse effects on oral tissues. The cytotoxicity, apoptotic potential, and genotoxicity of 11 mouthwashes were evaluated to identify those that achieve the optimal mouthwash attributes, one with nontoxic, nonallergenic, and nonirritating ingredients
Healthy human gingival fibroblast cells (hGF cells) were derived from 2 healthy individuals. The mouthwashes studied were Colgate 2 in 1, Colgate Optic White, Colgate Plax, Curasept, Elmex, Kloroben, Listerine Cool Mint, Listerine Zero, Meridol, Oral-B Pro Expert, and Sensodyne Pronamel. All were assessed for cytotoxicity using the xCELLingence system, for apoptotic effects using the IC50 concentrations through Annexin V and Caspase-3 assays, and for antibacterial effect on Streptococcus mutans and Lactobacillus rhamnosus using a modified microdilution method. The active ingredients are chlorhexidine in Curasept and Kloroben; cetylpyridinium chloride in Colgate Plax, Oral B Pro Expert, and Sensodyne Pronamel; and sodium fluoride in Colgate 2 in 1, Colgate Optic White, Colgate Plax, Elmex, Oral B Pro Expert, and Sensodyne Pronamel. Meridol contains stannous fluoride, Elmex and Meridol contain olaflur. Listerine Cool Mint and Listerine Zero are essential oil based and contain thymol, eucalyptol, and menthol (Table 1).
The cytotoxic effects on hGF cell lines were greatest for Meridol, with the others ranked as follows: Elmex, Colgate 2 in 1, Colgate Plax, Colgate Optic White, Sensodyne Pronamel, Oral B Pro Expert, Kloroben, Curasept, Listerine Cool Mint, and Listerine Zero. The Annexin V assay showed that only Colgate Plax, Kloroben, and Oral B Pro Expert had significant apoptotic effects at the IC50 doses. The Caspase-3 assay showed no mouthwashes had a significant apoptotic effect on the hGF cell line. In addition, no significant genotoxic effects were noted for the IC50 concentrations of the mouthwash formulations on the hGF cell line using the H2AX assay. Chlorhexidine is generally considered an antiviral mouthwash and used in concentrations of 0.12% and 0.2%. Extended use of concentrations above 0.2% causes adverse effects, so long-term chlorhexidine use at these levels can be problematic.
The modified microdilution method showed Colgate Plax, Sensodyne Pronamel, and Kloroben were more effective mouthwashes against S mutans. Colgate Plax was the most effective mouthwash against L rhamnosus
The antibacterial efficacy of the various mouthwash formulations is often tied to their unique compositions. Essential oil−based mouthwashes are promising alternatives with significantly reduced cytotoxicity compared to formulations with chlorhexidine or cetylpyridinium chloride. Essential oils may balance the antimicrobial effects with better cellular compatibility, possibly offering safer and still effective products to achieve oral hygiene.
The essential oil based mouthwashes may be a safer choice for use, especially long-term use. They have less cytotoxicity, are more biocompatible, and offer efficacy as antibacterial agents.
Table 1. Composition of Mouthwashes Used in the Present Study
Mouthwashes
Colgate 2in1
Colgate Optic White
Colgate Plax
Manufacturer Ingredients
Colgate-Palmolive, New York, USA
Colgate-Palmolive, New York, USA
Colgate-Palmolive, New York, USA
Curasept Curaden AG, Kriens, Switzerland
Elmex Gaba International, Therwil, Switzerland
Kloroben Drogsan, Istanbul, Turkey
Listerine Cool Mint
Johnson&Johnson, New Jersey, USA
Listerine Zero Johnson&Johnson, New Jersey, USA
Meridol Gaba International, Therwil, Switzerland
Oral B Pro Expert Protecter&Gamble, Ohio, USA
Sensodyne Pronamel GlaxoSmithKline, London, UK
Water, Sorbitol, Hydrated Silica, Glycerin, Sodium Lauryl Sulfate, Aroma, Tetrasodium Pyrophosphate, Sodium Saccharin, Cocamidopropyl Betaine, 0. 24% Sodium Fluoride, Cellulose Gum, Xanthan Gum, Limonene, CI 77,891
Water, Glycerin, Propylene Glycol, Sorbitol, Tetrapotassium Pyrophosphate Polysorbate 20 Tetrasodium Pyrophosphate Zinc Citrate, PVM/MA Copolymer, Aroma, Benzyl Alcohol, 225 ppm Sodium Fluoride, Sodium Saccharin, Cl 42,051.
Water, Glycerin, Propylene Glycol, Sorbitol, Poloxamer 407, Aroma, Cetylpyridinium Chloride, 0.05% Sodium Fluoride, Methylparaben, Menthol, Sodium Saccharin, Propylparaben, CI42051.
Water, Xylitol, Propylene Glycol, PEG-40 Hydrogenated Castor Oil, Ascorbic Acid, Chlorhexidine Digluconate, Aroma, Sodium Fluoride, Poloxamer 407, Sodium Benzoate, Sodium Metabisulfite, Sodium Citrate, CI 42,090.
Water, PEG-40 Hydrogenated Castor Oil, Olaflur, Aroma, Potassium Acesulfame, 250 ppm Sodium Fluoride, Polyaminopropyl Biguanide, Hydrochloric Acid.
0.15% Benzidamine Hydrochloride, 0.12% Chlorhexidine Gluconate, Sorbitol, Propylene Gly-col, Aroma, Mint Essence, Patent V Blue, Quinoline Yellow
Water, Alcohol, Sorbitol, Poloxamer 407, Benzoic Acid, Sodium Saccharin, Eucalyptol, Aroma, Methyl Salicylate, Thymol, Menthol, Sodium Benzoate, Cl 42,053.
Water, Propylene Glycol, Sorbitol, Poloxamer 407, Sodium Lauryl Sulfate, Benzoic Acid, Sodium Saccharin, Eucalyptol, Aroma, Methyl Salicylate, Thymol, Menthol, Sodium Benzoate, 220 ppm Sodium Fluoride, Sucralose, Cl 42,053.
Water, xylitol, PVP, PEG-40 hydrogenated Castor Oil, Olaflur, Aroma, 250 ppm Stannous Fluoride, Sodium Saccharin, CI 42,051.
Water, Glycerin, Polysorbate 20, Aroma, Methylparaben, Cetylpyridinium Chloride, 0.05% Sodium Fluoride, Sodium Saccharin, Sodium Benzoate, Probilparaben, Cl 42,051, Cl47005.
Water, Glycerin, Sorbitol, Poloxamer 338, PEG-60 Hydrogenated Castor Oil, VP/VA Copolymer, Potassium Nitrate, Sodium Benzoate, Cellulose Gum, Aroma, 450 ppm Sodium Fluoride, Methylparaben, Propylparaben, Cetylpyridinium Chloride, Sodium Saccharin, Xanthan Gum, Disodium Phosphate, Sodium Phosphate, Cl 42,090.
(Reproduced with permission from Çogulu D, As ¸ ik A, Yılmaz Susluer S, et al: In vitro analysis of various mouthwashes: Cytotoxic, apoptotic, genotoxic and antibacterial effects. Clin Oral Invest 29:183, 2025.)
Cogulu D, As ¸ ik A, Susluer SY, et al: In vitro analysis of various mouthwashes: Cytotoxic, apoptotic, genotoxic and antibacterial effects. Clin Oral Invest 29:183, 2025
Reprints available from A As ¸ ik, Dept of Pediatric Dentistry, Faculty of Dentistry, Izmir Tınaztepe Univ, Izmir, Turkey; e-mail: asli.asik@tinaztepe.edu.tr
Among the most significant noncommunicable diseases worldwide, periodontal disease (PD) and type 2 diabetes mellitus (T2DM) are not only highly prevalent and preventable but also related to each other through preventive and therapeutic avenues. T2DM and PD share an inflammatory nature, with individuals with T2DM being more susceptible to severe PD, which can exacerbate poor glycemic control. Advanced glycation end products (AGEs) formed in diabetes contribute to metabolic and microvascular dysregulation, and their accumulation can lead to a more severe form of PD. The elevated systemic inflammation associated with PD promotes insulin resistance, making control of diabetes more challenging. These and other linkages suggest that controlling PD in persons with T2DM could contribute to the management of the vicious cycle created by both diseases—and this could affect the global economy as well. The economic burden of T2DM is about $1.3 trillion and that of PD is about $330 billion. A systemic review was done to evaluate the efficiency of periodontal treatment in improving diabetes-related outcomes in patients with T2DM and PD, with an updated and comprehensive synthesis through economic evaluations (EEs).
A literature search was conducted in the EBSCOhost (Dentistry and Oral Sciences Source), Econlit, LiLACS, PubMed, SciELO, Scopus, Tufts Medical Center Cost-Effectiveness Analysis (CEA) Registry, and Web of Science databases. The studies assessed the efficiency of periodontal treatment versus no treatment or other dental treatments. Eleven studies were selected for analysis.
Cost-benefit Analysis
The EE of 7 studies showed periodontal treatment reduced the total health care costs in 5 studies, the diabetes-related care in 2, inpatient costs in 4, outpatient costs in 1, and diabetes-related and other drug costs in 2. When the intervention was provided by a periodontist, the intervention was cost-saving compared to no comprehensive periodontal care for T2DM patients. Supragingival scaling needs elevated the therapeutic effectiveness and a cost ceiling of $53 to reach the classification of being a cost-effective intervention. For nonsurgical periodontal treatment to be classified as a cost-effective treatment to stabilize periodontitis, it had to have an effectiveness probability of at least 30% while maintaining costs less than $649.
In the British health system, periodontal treatment was considered cost-effective because it was below the benchmark willingness-to-pay threshold In the United States, it was cost saving from the perspective of the health care system with a saving of $5904 and a gain of 0.6 quality-adjusted life year (QALY) per capita. The effectiveness increased in patients with poor metabolic control.
When an exploratory meta-analysis was done using a fixed effects model, the total incremental net benefit (TINB) was $12,348 in high-income countries when periodontal treatment was included in the management of T2DM. Relatively similar health and health-related economic outcomes were noted for countries using Organisation for Economic Co-operation and Development (OECD) indicators.
Periodontal treatment to manage T2DM was not only effective in improving metabolic control but also cost-effective and even generated cost savings for health care systems and providers in some settings. Improving the health outcomes of patients in various countries will require making appropriate and timely decisions because of the high human, economic, and social costs of T2DM. These costs are especially related to all the complications that must be managed. EEs were useful in guiding allocation decisions that will optimize the resources available, improve the patients’ health status, and result in increased well-being for the population involved.
Including periodontal therapy in the treatment of patients with T2DM could reduce the costs and provide a cost-effective intervention that improves outcomes, such as metabolic control and reduced complications. Further studies are needed to provide more exact effect estimates and make proper recommendations for including periodontal therapy in the comprehensive treatment of type 2 diabetes. The efficiency of periodontal treatment performed by a specialist-based or general practitioner perspective should also be evaluated. A societal perspective, including outcomes such as presenteeism or absenteeism, would be helpful and may even address homelessness and employability.
Saenz-Ravello G, Castillo-Riquelme M, Cuadrado C, et al: Efficiency of periodontal treatment to improve type 2 diabetes mellitus outcomes: A systematic review and meta-analysis of economic evaluations. Community Dent Oral Epidemiol 53:135151, 2025
Reprints available from M Baeza, Ctr for Surveillance and Epidemiology of Oral Diseases, Faculty of Dentistry, Univ of Chile, Olivos 943, Independencia, Santiago, 8380544, Chile; e-mail: mbaeza.paredes@odontologia.uchile.cl
Posttraumatic stress disorder (PTSD) is a disabling mental health condition that develops after experiencing a serious traumatic event (TE). Examples of TEs include war, physical and sexual assault or abuse, natural disasters, threats, and the death of loved ones. The attack on the World Trade Center (WTC) on September 11, 2001 is an example of a TE that caused PTSD in persons exposed as first responders, survivors, those who lost family members, and witnesses to the events that occurred. The symptoms of PTSD are recurrent, involuntary, distressing occurrences that may include flashbacks or memories of the event, nightmares, or a sense that the events are ongoing, and physiological reactions to internal or external cues that reflect aspects of the TE. The likelihood of PTSD developing after a TE depends on factors such as gender, traumatic experiences early in life, and the specific TE. The WTC attacks and ensuing PTSD are linked to a higher risk for developing chronic health conditions such as asthma, heart disease, gastroesophageal reflux symptoms, and cancer. Oral conditions related to the attack and subsequent PTSD diagnoses have not been investigated. Periodontal disease is a chronic inflammatory disease of tooth-associated structures seen in about 40% of adults in the United States. Adverse events in early life have been associated with periodontitis, showing that trauma can have a long-term effect on oral health. The World Trade Center Health Registry (WTCHR) was created to examine associations between this TE, WTC-specific PTSD diagnoses, and various symptoms among waves of survivors. The enrollees in 2020 reported receiving a diagnosis of periodontitis by a physician and made selfreports of missing teeth. These were considered in the context of PTSD and with the modifying effects of posttraumatic growth (PTG) that mitigated the impact of TE on health and by the effects of social support.
The 2020 enrollees constituted wave 5 and included 27,648 individuals. They self-reported a doctor’s diagnosis of PTSD and the year first diagnosed. They also completed a PTSD checklist of symptoms, noting the maximum, minimum, and first
non-missing total PTSD symptom score, with a PTSD symptom score of 33 or greater considered probable PTSD. The outcomes were periodontal disease, teeth lost, and person-time (follow-up time in years). Modifying factors were identified using a PTG inventory and a social support scale.
About 17% of the enrollees reported having been diagnosed by a doctor with PTSD after 9/11, with 7.4% reporting a doctor’s diagnosis of periodontitis. The average age of the patients in wave 5 was 64 years. Among those with PTSD, there were 355 new periodontitis cases, and an incident rate of 7.6 per 1000 for periodontal disease in those with PTSD plus a rate of 4.3 per 1000 person-years in those without PTSD. Even after adjusting for covariates, the incidence rate ratio remained statistically significant.
The average follow-up from a post-9/11 PTSD diagnosis to a periodontal disease diagnosis was 15.3 years. Average followup was 16 years for those without PTSD and 13 years for those who self-reported a doctor’s diagnosis of PTSD
Forty-seven percent of the 22,975 patients had no missing teeth, 39% had lost 1 to 5 teeth, and 2.3% were edentulous. As the proportion of enrollees with PTSD increased, the count of missing teeth increased, rising from 16% in those not missing any teeth to 21% in edentulous participants. The number of current smokers also increased from 13% among those missing 1 to 5 teeth to 35% in edentulous individuals. Depression increased from 18% of those missing 1 to 5 teeth to 28% in edentulous participants. A dose-response association was noted between a self-reported doctor’s diagnosis of PTSD and the missing teeth.
Poorer health outcomes were noted among individuals who developed PTSD after the 9/11 terrorist attacks. Oral health effects included periodontal disease and missing teeth.
PTSD related to the 9/11 TE appears to be an independent risk factor for developing poor oral health. Patients with PTSD tend to experience chronic stress and low-grade inflammation throughout the body, including the oral cavity. In addition, dental avoidance/anxiety tends to be common among patients with PTSD secondary to sexual trauma and torture, but it wasn’t ascertained if PTSD secondary to acts of terrorism causes similar dental anxiety. In addition, although social support tends to be a protective factor against the negative effects of trauma, the association between PTSD and poor oral health outcomes wasn’t modified by social support or PTG in this group of survivors.
Akinkugbe AA, Midya V, Crane MA, et al: Long-term oral health effects of traumatic events among World Trade Center Health Registry enrolees, 2003-2020. Community Dent Oral Epidemiol 53:170-179, 2025
Reprints available from AA Akinkugbe; e-mail: aderonke.akinkugbe@mssm.edu
Craniomandibular disorders cause myofascial pain and mechanical limitations, which can interfere with the orofacial functions and decrease quality of life. Chronic pain and limits on function can cause anxiety and depression, so patients should be afforded an initial relief of pain. Being in such pain along with the complex nature of these disorders makes clinical assessment difficult, with patients having muscle tension or spasms that confuse the source of the pain and complicate the symptom analysis. Performing functional diagnostic procedures can become extremely challenging in the presence of muscle pain and tension. Practitioners can alleviate orofacial pain using nonpharmacological interventions, including manual physical therapy, exercise therapy, laser or heat therapy, oral appliances, physiotherapy, psychotherapy or cognitive therapy, support groups, meditation, or acupuncture. All are aimed at achieving muscle relaxation and improving local blood flow and analgesia, which will relax the patient and relieve the stress and strain on masticatory structures. The best technique will be dictated by the cause of the pain, patient preferences, and the clinical setting. The Aqualizer occlusal splint, physiotherapy consisting of active and passive physical exercises to relax the orofacial muscles, and dry-needle oral acupuncture were used in pilot studies, then the results were evaluated for subjective and clinically diagnosed orofacial pain, maximum mouth opening, and neck mobility, as well as the clinical applicability of the initial pain therapies tested.
The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) was used to diagnose myalgia in 28 patients (average age about 33 years, range 20 to 65 years) using a visualanalog scale (VAS) and intraoral and extraoral palpation of muscles, measurements of maximal mouth opening, and scoring of neck mobility. A clinical assessment was carried out during the first session, before therapy, after 2 weeks, and after 4 weeks. The initial pain therapies tested were the Aqualizer dental splint; physical therapy, consisting of progressive muscle relaxation, stretching exercises for the cervical and thoracic muscles, stretching of the mandible using a rope, relaxation of the tongue retraction muscles, clenching of the mandible, protrusionretrusion movements of the mandible, distraction of the mandibular condyle, intraoral and extraoral massage of the masseter, massage of the temporal muscle, lateral pole of the condyle, and the masseter and medial pterygoid muscles, isometric mandibular exercise, tuning of the chewing muscles, and localization of the tongue tip; and dry-needle oral acupuncture.
The scores for each parameter didn’t differ significantly between any of the sampling times, except for intraoral pain at the initial evaluation. Intraoral pain was significantly different only between physiotherapy and oral acupuncture. The changes in the clinical
parameters were all significant for the Aqualizer and physiotherapy approaches except for mouth opening. Mouth opening showed no significant differences in the oral acupuncture group, with only muscle pain and neck mobility demonstrating significant improvement. A significant change was also noted for both the Aqualizer and physiotherapy groups between the first and third testing times.
Patients wearing the Aqualizer showed general improvement of all parameters except for 2 patients whose mouth opening decreased slightly after treatment and 1 patient who had no changes; 1 patient who had a slight decrease in mouth opening and no change in neck mobility; 1 patient with no improvement in neck mobility; and 1 patient who reported via VAS that the pain was worse. Patients having physiotherapy tended to show improvement except for 1 whose mouth opening worsened; 1 who had no change in intraoral pain; and 1 with a light decrease in mouth opening and no change in neck mobility. Patients undergoing oral acupuncture showed improvement except for 1 patient with worsening in mouth opening, muscle pain, and VAS score; 1 with no change in mouth opening and worsening of intraoral pain and VAS; 5 patients with light worsening or no improvement of 2 parameters; and 2 patients with worsening of 1 parameter. In general, the patients’ conditions improved, except for 1 subject in the acupuncture group, who experienced worsening.
The 3 methods evaluated were able to improve the general condition of the patients in a relatively short period of time. Acupuncture achieved a less positive result than the Aqualizer and physical therapy sessions. Intraoral pain was significantly reduced through physiotherapy, despite the fact that the initial condition of the physiotherapy patients was more severe than that of the other groups.
Pain relief in patients with orofacial myalgia is beneficial and can be accomplished using nonpharmacological therapeutic approaches. Observation of 3 methods indicated that they achieved general improvement in the patients’ condition, but may present both advantages and disadvantages. Acupuncture achieved less improvement in patients’ conditions than the other methods, but may have been hampered by using the dry-needle pricks for just 5 seconds. The Aqualizer produced generally positive results but has the drawbacks of breakage of the appliance in 1 case and causing a dropout of 1 patient who disliked the feeling of the splint in his mouth. Physiotherapy sessions required intense communication between the therapist and patient to ensure the exercises were correctly performed. Physiotherapy has the advantage of improving posture, body awareness, as well as the mobility of the spine and TMJs; it also positively affected mandibular position. Tongue exercises were especially relevant and required active participation of the patient as well as regular practice. This need for dedication may represent a drawback in some cases.
Simma-Kletschka I, Artacker N, Balla M, et al: Initial therapeutic approaches for orofacial myofascial pain: Three pilot studies. CRANIO J Craniomandibular Sleep Pract 43:489-501, 2025
Reprints available from I Simma-Kletschka, Office for Complementary and Alternative Medicine in Dentistry, Orthodontics and Oral Health, Arlbergstraûe 139, Bregenz 6900, Austria; e-mail: dr.i.simma@aon.at
Recurrent aphthous ulcers (RAUs) are a painful oral mucosal disorder that occurs during infancy or adolescence. Causative elements include stress, dietary influences, nutritional deficiencies, and immune system dysfunction. Tetracycline is traditionally used to treat RAUs, with the ability to reduce the inflammation and promote ulcer healing. However, it
doesn’t address the underlying cause and can have side effects such as upset stomach and tooth discoloration. In addition, the overuse of antimicrobial agents can produce antibioticresistant bacteria, which can complicate later infections. The prevention of RAUs includes changes in lifestyle to limit stress and promote relaxation. Heartfulness meditation (HM) is a form of meditation that focuses on developing compassion,
inner peace, and a deeper connection with oneself and others. It reduces stress and promotes a more relaxed feeling that supports the body’s natural healing ability. Some studies indicate HM may have a positive influence on the body’s physical and mental health. Since RAUs are related to stress, which is considered a triggering factor for these ulcers, it was proposed that HM would offer potential benefits in managing RAUs.
The study population consisted of 54 patients (mean age about 28 years, range 18 to 45 years) who had ulcers for more than 24 hours. They were randomly assigned to 3 groups with 18 in each group: Group 1 underwent the HM program, group 2 underwent tetracycline treatment, and group 3 received both HM and tetracycline. The HM practice included a sequence of 5 to 7 minutes of relaxation and 20 minutes of meditation, plus an evening session of 15 minutes of rejuvenation when patients were guided to visualize stress and heaviness leaving their bodies as smoke or vapor. A bedtime prayer meditation was recommended for 5 minutes before sleeping. The tetracycline was given to all group 2 participants as a capsule mixed with a small amount of saline and applied to the ulcer 3 times a day. The group 3 participants received a combination of the tetracycline and HM practice. The outcomes measured were severity of pain and duration of ulceration, with pain evaluated using a visual analogue scale (VAS) on days 1, 3, 5, and 7. Duration of ulceration was recorded in days.
When pain intensity was measured on day 1, no significant differences were seen between the 3 groups. When it was measured on day 3, pain scores for groups 1 and 2 were comparable, but group 3 participants had a significantly lower pain score. Similar findings were noted for days 5 and 7.
All groups had a gradual reduction in pain scores from day 1 to day 7, but group 3 had more pronounced effects on day 3 than the other groups. HM reduced the pain intensity in the shortest time interval, with the group 1 and 2 participants having comparable results.
Group 2 had the longest time for ulcer healing of 8 days, whereas group 3 had healing within 7 days. The difference was statistically significant. The combination of tetracycline and HM produced the lowest pain scores and the most rapid healing of ulcers.
Combining HM and conventional tetracycline reduced pain and healed the ulcers of RAUs more quickly than either method in isolation.
HM plus tetracycline reduced the severity of pain and resulted in more rapid healing of RAUs than the use of just tetracycline or just HM. The potential impact of HM on brain activity may contribute to disrupting the pain cycle, but more study is needed to determine the specific effects created by HM on pain. Performing meditation as part of a daily routine may offer potentially positive effects that benefit one’s physical and mental health, so HM may be combined with medical treatment to produce the best results.
Yadav M, Rathore N, Katiyar A, et al: Effectiveness of heartfulness meditation in the management of recurrent aphthous ulcers. Dent Med Probl doi:10.17219/dmp/168912
Reprints available from G Minervini; e-mail: giuseppe.minervini @unicampania.it
Sleep disorders (SDs) can disrupt the body’s ability to properly integrate the functional systems of the body and may affect the performance of daily tasks. Although many types of SDs exist, those related to oral and dental conditions are among the more recent conditions that are being researched. How these disorders are related to the mouth and its
components, such as the TMJ, remain controversial. The TMJ connects the skull bones with the mandible and is considered the most important and complex joint in the body. TMJ dysfunction (TMD) not only directly affects the TMJ but also concerns the muscles involved in jaw movement as a result of trauma, disc displacement, and neuromuscular fatigue, causing headaches, neck pain, and joint noises, among other
signs and symptoms. The correlation between TMD and SDs remains unclear, but understanding it could help in diagnosing both disorders. The existing literature was searched to determine if there is any association between SDs and TMJ dysfunction in adults.
A search of the PubMed, Embase, Web of Science, and Scopus databases identified 18 studies that were deemed appropriate for the systematic review. Ten were case-control studies, 1 a cohort study, and 6 cross-sectional, 1 of which was a retrospective cohort study that investigated sleep disorders, sleep bruxism, obstructive sleep apnea, insomnia, sleep fragmentation, gastroesophageal reflux disease (GERD), and snoring and their possible relationship to TMD.
Positive Associations
Seven studies identified a positive association between TMD and sleep bruxism (SB). Three of these directly linked pain and its intensity with worsening of SB and TMD. Two evaluated other symptoms, including teeth grinding and ringing in the ears, which were worsened in patients with TMD and SB.
Seven additional studies noted associations between TMD and other conditions that may be linked to SDs. One of these focused on the fact that all TMD patients had problems with snoring and the more severe the TMD condition associated with obstructive sleep apnea (OSA), the more snoring was present during sleep. Two studies found a strong association between TMD and OSA, with the severity of TMD and its painful symptoms worsening with OSA. Two others showed many patients who had OSA at some point also had a degree of TMD occurring together or consolidated over time. Another of these studies noted a positive association between insomnia and TMD, with increased pain from the TMD linked to worse insomnia symptoms. Patients with TMD had more awakenings, and those with more painful TMD had more turbulent sleep and worse conditions when
they had respiratory disorders as well. The seventh study indicated a possible positive association between painful TMD and GERD related to esophageal acidification causing an increase in rhythmic muscle activity and producing teeth grinding and clenching. Cases of chronic GERD included more patients with painful TMD.
Two studies found no relationship between TMD and SB. One of these noted that the intensity of SB wouldn’t be related to the worsening or improvement of TMD pain.
The current literature offered no clear relationships between TMD and SB, but was often positive for relationships between TMD and OSA, insomnia, snoring, and GERD.
Dentists who are managing patients with TMD need to be aware of the different etiologic factors involved in these disorders. They need to ask patients about their nighttime routine, identify possible SDs, and make referrals to sleep specialists as indicated. A multidisciplinary approach is essential to managing TMD.
Mendes ATP Tardelli JDC, Botelho AL, et al: Is there any association between sleep disorder and temporomandibular joint dysfunction in adults? – A systematic review. CRANIO J Craniomandibular Sleep Pract 43:426-437, 2025
Reprints available from ACD Reis, Dept of Dental Materials and Prosthodontics, Ribeirao Preto Dental School, FORP-USP, Av Do Cafe, s/n 14040-904, Ribeirao Preto, SP, Brazil; e-mail: andreare73@yahoo.com.br
Acceptability and Effectiveness of Weighted Blankets for Pediatric
Dental fear and anxiety (DFA) is the term used to describe negative emotions that are experienced because stimuli in a dental environment are perceived as threatening. DFA affects up to 42% of
children and is associated with adverse oral health−related outcomes, including poor oral health, irregular dental attendance, behavior management challenges, and sometimes the need for pharmacological interventions. Weighted blankets can provide
deep pressure touch sensations that reportedly provide a calming effect on the nervous system. The sensory inputs fostered by the weighted blanket can mediate sensory responsivity and adaptive behaviors. Weighted blankets have been used to improve sleep and calm anxious patients. In the dental setting, weighted blankets have proved to be a calming influence during stressful dental encounters as well as routine prophylactic visits in older adolescents and adults. Their efficacy was tested in a pediatric dental clinic with children age 6 to 12 years receiving various types of dental care.
The participants included 20 child-caregiver dyads and 9 dental practitioners who were second-year dental residents in an advanced practice pediatric dentistry residency program. The high-quality soft cotton weighted blankets were about 10% to 20% of the child’s weight and of an appropriate length. The weights were nontoxic PET pellets in pocketed construction to ensure an even distribution of weight across the blanket. The blankets covered the child from shoulders to feet and were only used for the first part of treatment in noncontinuous care settings. The children were informed they could request the blanket be removed at any time and could keep the blanket on during waiting gaps and later treatment if so desired. The child, caregiver, and dentist independently completed self-reports immediately after the appointment, with items focused on the feasibility, acceptability, appropriateness, and effectiveness of the weighted blanket use.
The weighted blanket was used for an average of 32.4 minutes, with an average active treatment time of about 16 minutes. Eleven patients had routine dental care and 9 received orthodontic treatment.
Caregivers and dentists overwhelmingly reported the intervention was acceptable, appropriate, and feasible. The blanket was reported by the children, caregivers, and dentists to be easy to use, comfortable, and compatible with dental care. Although the dentists reported being familiar with the use of weighted blankets in dental and nondental settings, the caregivers and children were usually not familiar with their use in any location.
Children who had a waiting time during treatment tended to want to keep the blanket on, with 85% making this request. Nine of the 20 children spontaneously reported that they liked the blanket, noting it felt soft and comfy. Three caregivers wanted to purchase a weighted blanket for their home and 2 had them already.
Three children had a problem with the blanket, with 1 having it fall off, 1 seeing it as too hot, and a third not liking the experience because it made him think the procedure would be much more serious.
Most of the participants agreed or strongly agreed that using the weighted blanket seemed to help the child relax. Caregivers and dentists felt the blanket use during treatment made it easier for the child to tolerate the dental care and would improve the child’s experience at the dentist. Caregivers overwhelming agreed that the weighted blanket would improve care for children who were fearful at the dentist. Sixty-five percent of participant dyads spontaneously made comments supporting the perceived effectiveness or advantages of the blanket. Caregivers and dentists agreed they would share the experience with other parents.
Use of a weighted blanket for children undergoing dental care proved to be feasible, acceptable, appropriate, and effective in making children feel comfortable and at ease. All of the participant groups overwhelmingly expressed enthusiasm and saw the blanket as potentially being useful in future visits.
Weighted blankets appear to offer a simple, costeffective strategy to calming children who might be nervous or have dental fear or anxiety. The use of deep pressure touch sensations was acceptable to the child, caregiver, and dentist in most cases, with few problems occurring. The children undergoing routine, noninvasive pediatric dental care were generally enthusiastic about having the blanket available.
Stein Duker LI, McGuire R, Hernandez J, et al: Feasibility, acceptability, and perceived effectiveness of weighted blankets during paediatric dental care. Int J Paediatr Dent 35:519-528, 2025
Reprints available from LI Stein Duker, Chan Div of Occupational Science and Occupational Therapy at the Ostrow School of Dentistry, Univ of Southern California, 1540 Alcazar St, CHP 133, Los Angeles, CA 90089, USA; e-mail: lstein@chan.usc.edu
The fluoridation of community water supplies has been a significant factor in the prevention of dental caries in the United States. About 75% of the US population benefits from fluoridated public drinking water. However, public confidence in the safety of tap water for drinking has been shaken by several incidents, resulting in a shift to bottled water and water filtration and purification systems (WFPS) in US households. These negative perceptions are most common among younger adults, Non-Hispanic Black and Hispanic individuals, those with lower education and income, and renters. This has led to a potential loss of the benefits provided by community water fluoridation (CWF) and raised concerns about the dental health implications of drinking bottled water. The WFPS market is growing, driven by concern over tap water quality and safety. Water filter pitchers are popular because they are simple, affordable, and portable. The pitchers use replaceable cartridges filled with activated carbon and ion-exchange resin. Some carry the Seal of Acceptance of the American Dental Association (ADA), but the actual research on water filter pitchers’ effect on fluoride concentrations in tap water is lacking. This investigation sought evidence of the effect of water filter pitchers in the United States on fluoride concentrations in tap water, but also measured other minerals that have an important role in oral health.
Nine water filter pitcher models (A through I) were used in this study. The fluoride levels in water were determined to be about 0.7 mg/L. The pitchers and filters were prepared following manufacturers’ instructions (Table 1), then water samples were collected immediately afterward. The 20-mL samples were collected after 1, 5, 10, 30, 50, 75, and 100 L of water had passed through the filter. Unfiltered tap water was collected immediately before and after each pitcher was studied. Fluoride concentration was measured using a fluoride ion-specific electrode. Mineral concentrations were determined using an atomic absorption spectrometer equipped with background correction and cathode lamps at wavelengths of 422.7, 285.2, 589.0, and 766.5 nm to analyze calcium, magnesium, sodium, and potassium, respectively. The average concentrations of each mineral in unfiltered tap water was 1.1 fluoride, 62.2 calcium, 28.4 magnesium, 96 potassium, and 36.0 ppm sodium.
Filters F and G decreased fluoride concentrations. All but I and H decreased calcium concentrations. Filters E, D, and G decreased magnesium concentrations. Filters I and D increased potassium concentrations. Filter A increased sodium concentrations but C decreased them.
As the filters aged, all of the mineral concentrations were affected, but to varying degrees. The most pronounced effect on mineral concentrations overall was shown by filter G. Fluoride concentrations didn’t return to baseline values using filter F (Figure 1), with filters C and G making significant reductions in fluoride concentrations initially but having no effect after 100 or 50 L, respectively.
Filter G had the greatest impact on calcium concentration, which never returned to baseline values. Filter F initially reduced calcium concentration but had a sudden increase, although it never returned to baseline levels. All of the other filters decreased calcium concentration initially, but showed a gradual increase before reaching or nearly reaching baseline levels.
Filter G prevented magnesium concentration from returning to baseline values. Filters A, B, and D significantly reduced magnesium concentration initially but had no effect after 30 to 50 L.
Initially, filter A increased potassium concentrations, but then they gradually decreased over time. A significant fluctuation was seen with filter D, with a sharp initial rise, then a rapid decline. Filters C, D, and G showed similar patterns.
Filter G had the most impressive impact on sodium concentration, but it returned to baseline levels after 75 L. Filter B had sodium fluctuations, but a final stabilization at baseline values after 50 L. Filter F decreased sodium levels, showed a gradual increase, then a final drop to baseline after 50 L.
Water filter pitchers varied in their effects on fluoride and other minerals in drinking water. Some filters effectively removed fluoride as claimed, some didn’t, and some showed unexpected fluctuations in mineral concentrations.
Table 1. Studied Water Filter Pitchers and Their Characteristics
Effect on calcium, potassium, magnesium, and sodium*
“Preserves certain healthy minerals in water”
Does not remove fluoride
Rinse 15 s with cold water Fill then empty the pitcher 3 times before use
Every 40 gallons/151 liters
A Brita Everyday pitcher, standard filter, (36050) Activated carbon granules Ion exchange resin
“Preserves certain healthy minerals in water”
Does not remove fluoride
Rinse 15 s with cold water Fill then empty the pitcher one time before use
Every 40 gallons/151 L
B Pure 7 cup pitcher filtration system Activated carbon granules Ion exchange resin
No statement about removal/retention
Removes more than 98.4% of fluoride
Every 150 gallons/every 2–5 months Fill then empty the pitcher twice before use
C Epic water filter Pure water filtration jug Proprietary blend of water filtration media within three activated coconut carbon
No statement about removal/retention
Soak the filter with cold water for 15 min then rinse for 10 s No statement about fluoride removal/ retention
Every 40 gallons/every 2 months
D Drink Soma Soma 10 cup pitcher Activated coconut shell carbon Charcoal
“Preserves certain healthy minerals in water”
No statement about fluoride removal/ retention
Rinse few seconds with cold water Fill then empty the pitcher 3 times before use
Every 60 gallons
E Clear 2 O Gravity water filtration pitcher (GRP200) Nano alumina fibers onto microglass filaments creating a non-woven filter media with a strong electropositive charge ( ) that removes sub 1-micron contaminants via electroadsorption, not just mechanical filtration
(no information provided)
Removes more than 99.54% of fluoride
Priming the filter by attaching the filter to a priming bag and running the water till it fills the bag then forcing the water out of the filter (to be repeated three times)
Every 100 gallons
F Clearly filtered Gravity-Fed Water Pitcher model (CF-PRF) 3 stages of filtrations First stage: woven mesh screening layer Second stage: granulated coconut carbon layer Third stage: proprietary composite shell
Removes calcium, potassium, magnesium, and sodium up to 100%
Removes more than 99% of fluoride
Clean with warm water and soap then rinse
Every 25–30 gallons
G Zero water 10 cup readypour pitcher 5 stages ion exchange
“Preserves certain healthy minerals in water”
Rinse 15 s with cold water Fill then empty the pitcher one time before use Does not remove fluoride
Every 40 gallons/151 L
H Brita Stream model (36238) Activated carbon Proprietary dual-layer filtration technology
Effect on fluoride*
Pre-use instruction
Product/model Filtration process Filter replacement
Table 1. Continued Code
Rinse 15 s with cold water Fill then empty the pitcher one time before use Does not remove fluoride “Preserves certain healthy minerals in water”
Every 120 gallons/every 6 months
Effect on calcium, potassium, magnesium, and sodium* I Brita Long last model (OB06)
Patented pleated filter and proprietary active filtering agents in a housing, made without BPA
* Information gleaned from product packaging or manufacturer’s website. (Reproduced with permission from Hazzazi LW, Soto-Rojas AE, Martinez-Mier EA, et al: The effect of water filter pitchers on the mineral concentration of tap water. J Public Health Dent 85:21-28, 2025).

Figure 1. Fluoride concentration as a function of water filter pitcher and filtration volume. [Color figure can be viewed at wileyonlinelibrary.com.] (Reproduced with permission from Hazzazi LW, Soto-Rojas AE, Martinez-Mier EA, et al: The effect of water filter pitchers on the mineral concentration of tap water. J Public Health Dent 85:21-28, 2025).
Consumers need to carefully research what water filter pitchers can and cannot do, especially in respect to fluoride and essential minerals. It’s vital to replace the filters regularly, and users should look for filters with clear replacement indicators to have the most consistent performance. Water quality should be monitored regularly, and manufacturers should be contacted to get accurate information about their filter technologies.
Hazzazi LW, Soto-Rojas AE, Martinez-Mier EA, et al: The effect of water filter pitchers on the mineral concentration of tap water. J Public Health Dent 85:21-28, 2025.
Reprints available from LW Hazzazi, Indiana Univ School of Dentistry, Oral Health Research Inst, Dept of Biomedical and Applied Sciences, 415 Lansing St, Indianapolis, IN 46202, USA: e-mail: loai.hazzazi@gmail.com
Sufficient sleep is essential for good health, with insufficient amounts causing negative effects on the central nervous system, immune system, respiratory system, digestive system, cardiovascular system, and endocrine system. Over time, insufficient rest is a major risk factor for hypertension, diabetes, obesity, depression, heart attack, and stroke. Despite the constant warning about the importance of getting good rest, about 84 million American adults—roughly 33%–report that the quality of their sleep is fair or poor and only about 35% get the recommended 8 hours each night. Poor sleep has been blamed on exposure to blue light or checking social media, but a new study from Norway finds that spending time on your mobile phone at bedtime can cause poorquality sleep or insufficient sleep. Each 1-hour increase in screen use raised the risk for insomnia by 59% and shortened the duration of sleep by 24 minutes. The actual content of what you’re watching on your phone makes no difference, and the color of the light is less important than the fact that it’s bright and at bedtime.
Blue-wavelength light is beneficial during the day and increases our attentiveness, improves our mood, and shortens reaction times. Some evidence shows blue-light exposure at bedtime dysregulates melatonin, which promotes and maintains sleep. A recent study showed that bright light in general is likely a problem for sleeping. Leah Kaylor, a clinical psychologist and author of a book on sleep, said, “We still have the same neural circuitry as our caveman ancestors whose lives and activities were ruled by the sun. Since we still have the same circuitry, we can easily confuse the brain by being in the presence of light close to bedtime.” Jonathan Cedernaes, a sleep expert at Uppsala Universitet, Sweden, noted, “I think it’s important to acknowledge that we inter-individually differ considerably in how light is able to suppress melatonin – about 50-fold.”
Børg Sivertsen, senior researcher at the Norwegian Institute of Public Health, found that students who exclusively used social media had the lowest rates of insomnia and the longest sleep duration compared to those who engaged in other screen activities or a mix of activities.” Social media and the socialization it supports may actually be protective of sleep. Sivertsen speculated, “Adolecents tend to be more socially and emotionally reactive, making social interactions more stimulating and harder to disengage from before sleep.” He noted that late-night social screen use could shift their already delayed sleep phase further.
Kaylor was surprised at the Norwegian study’s conclusion regarding social media activities and was concerned that gaming wasn’t tracked, since it has been linked to sleep disruption elsewhere. She said, “Overall, I find the results interesting but not strong, and more research needs to be done to truly support the claim that social media use in bed before sleep is protective. That claim is quite a stretch.”
To get a good night’s sleep, you can take a few simple steps:
• Limit screen use in bed and just before bedtime and instead engage in passive activities such as listening to music or audiobooks.
• To avoid blue light’s effects, turn on your phone’s night-time blue-light filter.
• Silence your notifications during sleep and use the phone’s Do Not Disturb mode. Charge it in another room to avoid being awakened by noises or stray light from the phone.
• Set up and follow a consistent bedtime and wake-up time, which your body can learn and apply as an adaptation to your circadian rhythm that will meet your sleep needs.
[Berman R: 1 Hour of Screen Time at Bedtime Reduces Sleep by 24 Minutes, Study Finds. Healthline, April 1, 2025]
No one wants to get sick, especially while traveling. Doctors advise taking a few extra precautions so you don’t develop a terrible cold, digestive problems, COVID-19, or other health issues. We made a quick checklist of things doctors do and what they pack when they travel to avoid getting sick.
Mask up in the airport and on the plane.
Face coverings can offer protection in multiple ways, such as keeping you from touching your nose and mouth with your hands. Dr Barbara Bawer, of the Ohio State University Wexner Medical Center, noted, “Although COVID is no longer as large of an issue as it was, given that I am in close quarters with the same circulating air on an airplane, I still wear a mask on all flights and in the airport.” She suggests packing at least a couple of high-quality masks such as N95s to reduce germ transmission in crowded indoor situations.
Wash and sanitize your hands frequently.
Dr Heather Viola, of Mount Sinai Doctors-Ansonia, says, “First and foremost, I constantly wash my hands, always carrying with me hand sanitizer that contains at least 60% alcohol to prevent the spread of germs. Many airlines are giving out alcohol-based disinfectant wipes when you board. I use these to clean my seat, headrest, armrests, tray table, and entertainment screen—basically, anything you may touch while sitting in your seat.” Packing your own alcohol-based disinfecting wipes is also useful.
Stay hydrated.
Maintaining a healthy water intake was a priority for all of the doctors interviewed. Viola said, “I always travel with electrolytes— packets of dissolvable electrolytes—for water or vitamin water. This is a good way to keep hydrated with more than just water and help prevent in-flight nausea or dehydration.”
Take immune system boosters.
Because the plane cabin is dry, microorganisms can circulate freely, so carrying a few vitamin C tablets can boost your immune system and help your body fight off airborne germs. Viola noted, “Nasal saline spray or nasal mists can also help fight germs as they keep your nasal passages moist, which enhances your body’s own germ-flushing activity. You can even apply a small amount of Neosporin or petroleum jelly just inside the nostrils—using a Q-tip if your hands aren’t washed—to create a barrier between you and the airborne germs.”
Avoid peak travel times.
Avoiding the crowds and the accompanying sense of stress can cut down on potential exposures to germs. Traveling in the middle of the day can allow you to get a good night’s sleep before or after your flight.
Prioritize your rest.
Bawer suggests getting good rest before a flight and sleep while traveling when that’s appropriate. She advises, “When returning home, give yourself some time to readjust back to your daily schedule and environment. Try not to return home at 11 PM or midnight and then have to head straight to work the next day. Give yourself a few hours or, if able, an entire day at least to recover, get caught up on laundry or grocery shopping or other needed chores, and get plenty of rest.” Fatigue can tax your immune system, decrease your endurance, and put you in a bad mood.
Don’t overschedule.
Reduce your stress wherever possible. Don’t overschedule your trip. Keep it flexible and allow yourself to enjoy the travel. Stress induces sickness, especially in new environments.
Eat a well-balanced diet.
Bawer said, “Eat a well-balanced diet leading up to the trip to get your body and immune system ready to fight anything it comes into contact with and on the day of travel as well. Most people don’t eat as healthy while on vacation but try to incorporate fruits and vegetables with all meals to keep your immune system at the highest level.” It’s also important to pack health snacks and a refillable water bottle so, if the flight is delayed or late, you have something to eat.
Know what travel vaccines and medicines to take.
Dr Henry M Wu, of Emory University School of Medicine, is director of the Emory TravelWell Center. He advises, “I make sure I am up-to-date on vaccines before travel. Flu and COVID-19 are so common among travelers, and even a mild case can ruin a trip. Also, for international travel, there are additional vaccines that might be recommended or required, or even malaria prophylaxis for some areas. I suggest travelers check the CDC [Centers for Disease Control and Prevention] travel website or see a travel medicine specialist for advice.” Bawer adds, “Consider getting a prescription for diarrhea medicine if traveling to another country where traveler’s diarrhea may be an issue . . . Focus on eating foods that have a shell and don’t need washing and drink bottled water. Also, use this to brush your teeth. This can help avoid traveler’s diarrhea from developing.”
Keep up with sun protection.
Whether it’s at home or on vacation, you should apply and reapply a broad-spectrum sunscreen with an SPF of at least 30 every day. If you’ll be spending a lot of time outside during your travels, keep up with your sun protection regimen. Dr Sarah Battistich, of NYU Langone Health’s Virtual Urgent Care, suggests, “Sunburn and heat-related illnesses are some of the most easily preventable causes of a ruined vacation. Don’t forget sunscreen, long sleeve shirts—linen is great for hot climates—and hats. The bigger and more packable the hat, the better.”
Buy insect repellent.
Wu said, “If it’s an outdoorsy trip or I’m going to tropical areas, I make sure to pack bug repellent. Mosquitoes, ticks and other biting bugs can transmit many infections.” Wu added, “It isn’t always easy to find these things on the fly, so preparing in advance will eliminate the chance I am caught off guard.”
Pack over-the-counter medications.
Acetaminophen for pain or fever, ibuprofen for pain, an antihistamine such as Benadryl, and Pepto-Bismol for stomach upset— take it all. Battistich said, “My doctor’s travel kit includes some preventatives and some emergency rescue meds.” This includes anti-nausea medications and remedies such as SeaBands, ginger packets, and aromatherapy sticks. She added, “There’s evidence that taking Pepto-Bismol tablets before and during travel can help reduce the risk of traveler’s diarrhea. I also pack very basic wound kits with Band-Aids, antibiotic cream, and if going to a hot and humid climate, or when hiking and backpacking, I will also often bring an antifungal cream.”
[Bologna C: 12 Things Doctors Always Do When They Travel to Avoid Getting Sick. Huffpost, May 3, 2025]








