












Editor-in-Chief
Douglas B. Berkey, DMD, MPH, MS
Senior Publisher
Annie Zhao
Journal Manager
Sangamithrai S
Abstract Writer
Elaine Steinborn
© July 2025, Elsevier Inc. All rights reserved.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise—without prior written permission from the publisher.
Publication Information Dental Abstracts (ISSN 0011-8486) is published bimonthly by Elsevier Inc., 1600 John F. Kennedy Boulevard, Suite 1600, Philadelphia, PA 1910, United States. Months of publication are January, March, May, July, September, and November.
Customer Service Office: 11830 Westline Industrial Drive, St. Louis, MO 63146. Periodicals postage paid at New York, NY, and additional mailing offices. Annual subscription rates for 2018 (domestic): $144.00 for individuals and $71.00 for students; and (international) $194.00 for individuals and $105.00 for students.
USA POSTMASTER: Send address changes to Dental Abstracts, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043.
Copyright 2025 by Elsevier Inc. All rights reserved. Dental Abstracts is a trademark of Elsevier Inc. Dental Abstracts is a literature survey service providing abstracts of articles published in the professional literature. Every effort is made to ensure the accuracy of the information presented in these pages. Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editors or the publisher. The Editors and the publisher disclaim any responsibility or liability for such material. Mention of specific products within this publication does not constitute endorsement.
All inquiries regarding journal subscriptions, including claims and payments, should be addressed to: Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Tel: 1-800-6542452 (U.S. and Canada); 314-447-8871 (outside U.S. and Canada). Fax: 314447-8029. E-mail: support@elsevier.com (for print support); support@elsevier.com (for online support).
Notice: Journals published by Elsevier comply with applicable product safety requirements. For any product safety concerns or queries, please contact our authorized representative, Elsevier B.V., at productsafety@elsevier.com
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments contained herein. Health care practitioners must exercise their professional judgement and make all treatment-related decisions based solely on the specific conditions of each patient. Because of rapid advances in the medical sciences, independent verification of diagnoses and drug dosages should always be made.
The content is provided “as-is” and Elsevier makes no representations or warranties, whether express or implied, as to the accuracy, completeness, or adequacy of any content. To the fullest extent permitted by law, Elsevier assumes no responsibility for any damages, adverse events, or liability arising from use of information contained herein including for any injury and/or damage to persons or property, whether as a matter of product liability, negligence or otherwise.
Inclusion of any advertising material in this publication does not constitute a guarantee or endorsement of the quality or value of such product or service or of any of the representations or claims made by the advertiser. Printed by Sheridan at 450 Fame Avenue, Hanover, PA 17331

DentalAdvance .org is the gateway offering high-quality research, news, jobs and more for the global community of dental professionals.
Journal profiles with quick links to Tables of Contents, author submission information, and subscription details
Important information and valuable resources on how to submit a journal article
Dentistry Articles in Press from participating journals
Quick links to the leading dentistry societies worldwide Dentistry News from Elsevier Global Medical News (formerly IMNG)
Dentistry Jobs powered by ElsevierHealthCareers.com

Editor-in-Chief
DouglasB.Berkey,DMD,MPH,MS ProfessorEmeritus, SchoolofDentalMedicine, UniversityofColorado, Aurora,Colorado
AssociateEditor
DanielM.Castagna,DDS AssociateProfessor,DepartmentofPreventiveandRestorativeDentistry, UniversityofthePacific,ArthurA.DugoniSchoolofDentistry, SanFrancisco,California
P.MarkBartold,DDSc,PhD,FRACDS(Perio) ProfessorEmeritus SchoolofDentistry, UniversityofAdelaide Adelaide,Australia
RobBerg,DDS,MPH,MS,MA ProfessorandChair, DepartmentofAppliedDentistry, UniversityofColoradoSchoolof DentalMedicine, Aurora,Colorado
TylerH.Berkey,DMD GeneralDentist Aurora,Colorado
FionaM.Collins,BDS,MBA,MA ConsultantandEditor, GeneralDentist Longmont,Colorado
AnthonyJ.DiAngelis,DMD,MPH ChiefofDentistry, HennepinCountyMedicalCenter, Professor,UniversityofMinnesota, SchoolofDentistry, Minneapolis,Minnesota
RaulI.Garcia,DMD,MMedSc ProfessorandChairman, DepartmentofHealthPolicyandHealthServicesResearch, BostonUniversitySchoolofDentalMedicine, Boston,Massachusetts
MichaelSchafhauser,DDS GeneralDentist, St.Paul,Minnesota
JoeVerco,DClinDent PaediatricDentist NorthAdelaide,Australia

JULY/AUGUST2025
VOL.70 No.4
Commentary
Oral/SystemicLinkages246 OralMicroorganismsCausingSystemicInfections MeaningfulConnections247
BeMindful,Grateful,andCurious
TheFrontOffice
DentalCareerSatisfaction/MentalHealth248 FactorsContributingtoJobSatisfaction
IdentifyingStressesandSupportsforDental Practitioners
MotivatedbyProfitorNonmale ficenceand Bene ficence?
MakeYourImageConveyPositiveandEthicalBehavior
PrenatalOralHealth271 DeliveringOralHealthtoPregnantWomenandTheir Children
VitalPulpTherapy272 TreatmentOptionsforIrreversiblePulpitisin PermanentTeeth
SilverDiamineFluorideforIndirectPulpCappingof theFirstPermanentMolar
IndirectPulpCappingforSevereEarlyChildhood CariesLesions
WaterFluoridation277
NewerResearchintoCommunityWater Fluoridation’sEffectsonChildhoodCaries EthicsandthePublicHealthIssueofWater Fluoridation
LiteratureAppraisalsofCommunityFluoridation EarlyExposuretoFluorideandIQ
Hands-On Cannabis285
HealthConsequencesofCannabisUse
EatingDisorders286 Avoidance/restrictiveFoodIntakeDisorder
GeriatricDentistry289 PragmaticTreatmentApproachesForOlderAdults ManagingTMD292 IdentifyingandFacilitatingCareofTMD
MSDPrevention295 AssumingtheBestPostureforDentalCare
PediatricFirstPermanentMolars296 AddressingCariesandHypomineralizationofFirst PermanentMolars
Sepsis299 RecognizingSignsandSymptomsofSepsis
SugaryMedicines/Children302 AddressingSugaredMedicationsforChildren
VapingandOralHealth305
CounteractingMisinformationAboutVaping
Inquiry
CompleteDentures/Taste307 EffectofDenturesonTastePerception
CostEffectiveness/RootCanalTreatment308 DeterminingTreatmentBasedonCost-Effectiveness
DengueFever309
OralManifestationsofDengueFever
DentalAnxiety311
DentalTreatmentUnderGeneralAnesthesia
Endodontics/RestorativeDentistry313
RestorationsforEndodonticallyTreatedTeeth
OralMicrobiome315
ChangesintheOralMicrobiomeOvertheLifespan
OrthognathicPsychology318
PatientSatisfactionandImprovedQualityofLife AfterOrthognathicSurgery
PeriodontalTreatment319 Bene fitsofPeriodontalTreatments
VerticalDimension320 ControversiesRegardingtheVerticalDimensionof Occlusion
Extracts
322 IsThatReallyTrue?
Notes
TofacilitatetheuseofDentalAbstractsas areferencetool,allillustrationsandtablesincluded inthispublicationarenowidentifiedastheyappear intheoriginalarticle.Thischangeismeanttohelp thereaderrecognizethatanyillustrationortable appearinginDentalAbstractsmaybeonlyoneof manyintheoriginalarticle.Forthisreason, figure andtablenumberswilloftenappeartobeoutof sequencewithinDentalAbstracts.
StandardAbbreviations
Thefollowingtermsareabbreviated:acquiredimmunodeficiencysyndrome(AIDS),humanimmunodeficiency virus(HIV),andtemporomandibularjoint(TMJ).
Mostpeopledon’tdevelopsystemicdiseasefromoral flora,but it’spossible.Themouthishometomanymicrobialspecies,witha myriadofthemlinkedtosystemicdiseases.Amongthesofttissue infectionsthatcanoccurarenecrotizingfasciitis(NF),strep throat,andimpetigo.Oftentheseinfectionsresultfrombacteria enteringthebodythroughabreakintheskincausedbyacut,an insectbite,orsurgery.Dentistsneedtobeawareoftheprimary oralorganismscausinginfectionsandwheretheseorganismslive sothattheycaninstitutepropermeasurestoavoidtheirdisseminationthatleadstosystemicdisorders.
Aquicklistingofpossiblemicrobialspeciesinthemouthincludes Actinomyces,Capnocytophaga,Corynebacterium,Fusobacterium, Leptotrichia,Prevotella,Rothia,Selenomonas,Streptococcus,Treponema, and Veillonella.Skininfectionsarecommonlycausedby Staphylococcusaureus.
Saureus iscarriedbyabout30%ofthepopulationinthenoseand about20%intheoralcavity.Highlycontagious, Saureus canbe spreadbycoughing,talking,orcontactwithacontaminatedsurface.Thisopportunisticpathogencancauseinfectioninanopen woundorinpatientswithsystemicmedicalconditions.
Spyogenes causesinfectionsrangingfromstrepthroattoNF.It’ s foundinthepharynx,anus,andgenitaliabutalsoinhabitsdental plaque,whichlikelyrepresentspharyngealcolonization.Upto 10%ofthepopulationcancarryit.AftertheCOVIDpandemic, strepinfectionshavedecreased,sothepopulationmayhavelost someofitsimmunity.
Researchhasidenti fiedthegut-brainaxiswhereinintestinal micro floramayaffectthebrainandcouldbelinkedtomental healthproblems.Theremayalsobeanoralcavity brainaxis. Somespecies,suchas Porphyromonasgingivalis,cancausesystemic
diseaseifitentersthebloodstream,withcardiovasculardiseasea possibleresult.IthasalsobeenlinkedtoAlzheimer’sdisease. Fusobacteriumnucleatum hasbeenlinkedtogastriccarcinoma.
Dentalproceduresareknowntocausebacteremia,ascandaily oralhygienepractices.Althoughthechanceofgettingasystemic diseasefromoral floraisverylow,theactualprocesslinkingoral bacteriatosystemicdiseasesremainslargelyunknown.
NFresultsfrombacteriaenteringthebodythrougha breakintheskin,althoughsomecasesarecaused byfungiorviruses.Thesemicroorganismsrelease extensiveamountsofendotoxinsandexotoxins thatcausenecrosisoftissuesthroughoutthebody, alongwithseveresystemicsymptoms.Patientsmust undergoaggressivetreatmentssuchassurgical debridement,intravenousantibioticsorimmunoglobulin,oramputation.Septicshock,kidneyfailure,and deathcanresult.Aspirationbiopsiesandsamples fromtissuesinthewoundareneededtoidentifythe causative floraandindicatewhichantibioticismost appropriate.Empiricalantimicrobialsworkwell,and someorganismsstillrespondtopenicillin.Dentists needtobealerttotheriskoforalmicrobiota related systemicdiseasesandtakepreventivemeasuresto ensurethatpatientsareoptimallyprotectedfrom infection.
DarbyI:Themouthasreservoirforsystemicinfection. Austral DentJ 69:249-250,2024
Reprintsnotavailable
In2023,theUSSurgeonGeneralannouncedtherewasanationwideepidemicoflonelinessandisolationthataffectedabouthalf ofalladults.Socialdisconnectioncanhaveanegativeimpacton mortalityandisassociatedwithanincreasedriskforcardiovasculardisease,dementia,stroke,depression,andanxiety.Thelonelinessandisolationepidemicresultedfromtherapidgrowthof socialmedia,arti ficialintelligence(AI),andremoteworkand wasexacerbatedbytheCOVID-19pandemic,whensomany wereisolatedfromlovedones,thecommunity,andsupportsystems.Ourphysicalhealthandwell-beingcanbepositivelyinfluencedbysocialsupportandhumanconnection.Speci ficeffects havebeenreportedonourwell-being,theabilitytomaintain bodymassindex,adecreaseindepressivesymptoms,therelief ofsymptomsofpost-traumaticstressdisorder,andpositivealterationsinoverallmentalhealth.Wenowfaceapoliticallypolarizedclimatewithdeeplydividedgapsincommunities,broken trust,andisolation.Waystocultivatemoremeaningfulconnectionsindentalsettingsweresuggested,includingmindfulness, gratitude,andcuriosity.
Itcanbediffi culttoconcentrateandmaintainourfocusamidthe constantnotificationsanddigitalsignalswereceive.Wemay struggletoremainempathicinpatientcareandinourdailyinteractions.Mindfulnessinvolvesthemoment-to-momentnonjudgmentalawarenessofourthoughts,feelings,bodilysensations, andsurroundingenvironment.Itallowsustotakeabreathand seektounderstandothers’ perspectivesandemotionsrather thanconsideronlyourown.Thishelpsinbecomingmore responsivetotheneedsofotherpeople.
Withmindfulcommunication,welistencarefullytotheother personandobservetheircurrentstateandtheirbodylanguage. Thisallowsustoopenourheartsandmindsandseeourown emotionsandsensations.Asaresult,wecanrespondmore thoughtfullyandengagemorefullywiththeotherperson.
Expressingandreceivinggratitudehelpsusinitiate,maintain,and strengthenrelationships.Thisholdsinromanticrelationshipsas wellasfriendshipsandcanleadtocoworkersbeingevenmore helpful.Thankingsomeoneandreflectingonthosewefeelgratefultocanbuildpowerfulconnectionswithotherpeople.Through expressionsofgratitude,werealizeandshowotherstheirvalue inourlives.Buildingacultureofgratitudeinthedentalteamand practicecreatesahealthyenvironment,morepositiveemotions, andlesshostilityoraggression.
Reflectinggenuinecuriosityaboutapersonduringinterpersonal interactionscanhelptobridgeanygapbetweenthe2parties. Insteadofrushingtojudgment,whichpushespeopleaway,asking questionstobetterunderstandandreachtheheartofthemotivation,perspective,andbackgroundofothersshowsasincereinterestinlearningfromthemandtakesthefocusoffofourselves. Theabilitytoremaincuriousallowsustoopenourselvesto deepermeaningfulrelationshipsthatwemighthavemissed otherwise.Curiositycanfosterthegrowthofconnection.
Evenwiththeobstaclesthatwefaceinourcurrentenvironment,maintainingafocusonhumanconnectioncan remainthecoreofourdentalpracticeaswellasourpersonallives.Remainingmindful,grateful,andcuriouswill helpourpersonalhealthandwell-being,butwillalso strengthenconnectionswithothers.
YamamotoKK:Cultivatingmeaningfulconnectionsindentistry andbeyond. JCalifDentAssoc 53:2450327,2025
Reprintsnotavailable
About45,000dentistsareregisteredintheUnitedKingdom, withmostinprimarycaresettings.Inthepursuitofknowledge aboutworkforceretentionandthedevelopmentofeducation andtrainingopportunitiesfordentalprofessionals,asurvey wasconductedofdentists’ experiencesintheirprofessional careersandjobsatisfactionlevelsaspartoftheUKdental workforce.
Thenationaldentalworkforcewasprovidedanonlinequestionnaire,and875ofthe1240respondentscompletednearlyallof thequestions,makingthemthesubjectoftheanalysis.Thequestionsaskedaboutthechallengestothehealthandwellbeingof thedentalworkforce,currentprofessionalcareertrajectories, andwhetherornotthedentists’ careeraspirationshavebeen orarebeingmet.
Nearly56%oftheparticipantswerefemale,about75%were white,most(about81%)weregeneralpractitioners,themajority (about92%)workedinEngland,mostgraduatedfromaUK school(about88%),andthegreatestnumbers(about63%) servedinprimarycaresettings.
About41%reportedtheircareerplanswereasenvisioned, whereasabout58%notedchangesintheircareerplansover time.Inaddition,about42%wereplanningtochangetheircareersinthefuture.Mostofthemen(about47%)reportedtheir careerwasasenvisioned,whereasonlyabout38%ofwomensaw theircareersasontrackforwhattheyhadexpected.Allofthe ethnicgroupsexceptwhitepersonsreportedtheircareers werenotasenvisionedortheyhadhadtochangetheirplans. Theoverseasgraduatessigni ficantlylessoftenreportedtheir careerwasontrackcomparedtoUKgraduates.Peoplewho hadbeenintheirprimaryjobroleforlongerweresignificantly morelikelytoreporttheircareerplanwasasenvisionedand hadnoplansforchangingcareers.Dentistsinprimarycare weremorelikelytowanttochangetheircareerplansthanthose insecondarycare,universitypositions,communitydental
services,orarmedforces.Averagejobsatisfactionwasreported assignificantlygreateramongthosewhosecareerwasasenvisionedcomparedtothosewhohadachangeincareerplansor plannedtochangetheircareer.
Threemodelswereusedtoevaluaterelationships.Amongthe groupwhosecareerwasasenvisioned,jobsatisfactionandprimaryrolesettingweresigni ficantcontributorstotheirposition. Forthosewhohadadifferentcareerplanfromwhattheyenvisioned,jobsatisfaction,havingcountryqualification,andserving inaprimaryroleweresigni ficantpredictorsfortheirposition. Jobsatisfactionanddurationofprimaryjobrolecontributed significantlytothepositionofthoseplanningonchangingtheir career.
Jobsatisfactiondifferedsigni ficantlydependingonethnicity, countryofinitialqualification,primaryrolesetting,workexperience,currentmainrole,andnumberofrolesheld.Whitepeople hadhigherjobsatisfaction,asdidUKgraduates,thoseworking outsideaprimarycaresetting,specialists,anddentistswith extendedskills.Personswhohad2jobroles,whichprovided diversityintheircareer,alsohadhigherjobsatisfactionlevels. Signi ficantassociationswerenotedbetweenjobsatisfaction andethnicity,durationofjobrole,primarysettings,current role,numberofroles,andcareerplans.
Thefactorscontributingtothecareertrajectoryofdentists includedsex,jobsatisfaction,primaryrole,countryofqualification,anddurationofworkingexperience.Dentistsfellintothe categoriesofhavingacareerastheyhadenvisioned,having changedtheirplan,orplanningonchanging.Women’ scareer planstendedtonotfollowthepatterntheyenvisioned,along withpeoplewhoqualifiedoutsideoftheUKandbeingalessexperienceddentist.Thosewhosecareerhadgoneasenvisioned tendedtohavegreaterjobsatisfactionlevels,asdidthosewho werewhiteorAsian,whoservedforalongertimeintheirposition,whoprogressedintheircareer,andwhoheldmultiplejob roles.Lowerjobsatisfactionlevelswerereportedbydentists workinginprimarycaresettings.
Researchisneededtobetterunderstandthelongtermfactorsthataccompanydentists’ careerpaths. Inaddition,dentaleducationandtrainingandinterventionstosupportdentistsinreachingtheircareergoals needtobeclarified.Thesemeasuresareimportantto ensurethattheneedsofthepopulationaremetbya suitabledentalworkforce.
ClarkM,McGregorA,KairuddinANM,etal:Dentalcareers: Findingsofanationaldentalworkforcesurvey. BrDentJ 238:249-256,2025
Reprintsavailablefrom MClark,OralSurgeryDept,Newcastle DentalHos,RichardsonRd,Newcastle,NE24A1,UK;e-mail: megan.clark12@nhs.net
Allhealthcareprofessionalsareatriskformentalhealthchallengesrelatedtotheirwork,theirenvironment,andthebalance betweentimeandinvolvementinworkandlifepursuits.AsurveywasundertakenamongCanadiandentistsandstakeholders todeterminewhattheyseeasmentalhealthchallenges,what supporttheyfeeltheyneed,andwhatsupportcouldbeavailable tothem.
Thedatawerecollectedfromsemi-structuredqualitativeinterviewsaswellasasurvey.Thedentalparticipantswereidenti fied throughsocialmediaplatformsande-mailinvitations.Inaddition, directe-mailsweresenttostakeholders.Asaresult,36interviewswereconductedwithpracticingdentistsand17withstakeholders.Thestakeholderscamefromdentalassociations, regulatorybodies,academicinstitutions,insuranceorganizations, andotherrelevantorganizationssuchasorganizeddentistry groups.
The findingsweredividedinto2groups:(1)mentalhealthexperienceswithrespecttoworkpluspersonalandfamilialchallenges and(2)supportneedsandpotentialopportunities.
Thedentistsreportedawiderangeofmentalhealthexperiences, includingstress,anxiety,depression,burnout,obsessivecompulsivedisorder(OCD),post-traumaticstressdisorder (PTSD),andsuicidalideation.Somehadbeenformallydiagnosed byamentalhealthcarespecialist;othersself-reportedtheseissues andexperiences;andstillotherswerereportedbystakeholders. Thestakeholdersmentionedthepotentialrepercussionsof
untreatedmentalhealthconditionsthatcouldpresentariskforpatientwell-beingandmayinvolveregulatorybodiesifdentists refusetoseekhelporusetheavailableresources.
Theseresultswerecorroboratedbythesurveyresults.Fortyfourpercentoftherespondingdentistsreportedsufferinga mentalhealthissue.Whenthedentists’ genderwasconsidered, 59%ofthefemaledentistsand39%ofthemaledentistshadexperiencedmentalhealthissues(Table2).
Theworkenvironment,professionaldemands,andpatientcare challengesin fl uenceddentists ’ rangeofmentalhealthsymptoms,whichincludedstress,anxiety,andburnout.Sex/gender alsoin fl uencedtheirexperiences .Amongtheexperiences relatedtopatientcareresponsibilitieswerestressasaresult ofdealingwithpatientswhohaveunreasonableexpectations anddealingwithchallengingpatients,suchastheelderly,patientsfrommarginalizedcommunities,andincarceratedpatients.Dentiststendedtointernalizetheirpatients ’ anxiety, distress,andfear,whichexacerbatedtheirownmentalhealth struggles.
Dentistsalsoreportedproblemsrelatedtoethicalpractices, especiallyinvolvingpatientsfrommarginalizedcommunities. Thefeeschedulefordentistscaringforthesepatientsisvery limited,sotheymustchoosebetweennottreatingthepatients, providingsuboptimalcare,andrisking financialloss.Ethicalproblemsalsoaroseinrelationtopressuresfromof ficemanagers,the drivetorecommendprofitableprocedures,andbeinggivenunrealistictargets.Femaledentiststendedtobelievethesetargets conflictedwithclinicaljudgmentandthreatenedtheirmental healthandwell-being.Theyalsoexperiencedprejudicerelated totheirabilitytoperformsomeprocedures,suchasoralsurgery.
Table2. MentalHealthIssuesandSourcesofStressExperienced byDentistsWhoRespondedtotheSurveyStrati fiedbyGender
Characteristic
Mentalhealthissues
Female,% (n) Male,% (n)
Mentalorpsychologicalstressordistress31.9(62)22.2(41)
Burnout24.2(47)15.1(28)
Anxiety36(70)16.2(30)
Depression12.4(24)3.7(7)
Substanceuse/dependence4.1(8)0
Posttraumaticstressdisorder3.6(7)0
Sourcesofstress:workrelated
Workoverload41.7(82)32.4(60)
Stressofrunningapractice,managing people,meetingbudgets
45.6(89)51.3(95)
Uncertainty15.4(30)11.9(22)
Poorrelationswithcoworkers/colleagues13.9(27)8.6(16)
Poorrelationswithpatients/clients9.3(18)6.4(12)
Ethicaldilemmas6.2(12)9.2(17)
Lackofpsychologicalsafetyatwork, includingbullying,harassment, discrimination,orworkplaceviolence
Sourcesofstress:nonworkrelated
5.7(11)0
Physicalhealthproblemorcondition16.5(32)14.6(27)
Debt/financialsituation23.7(46)16.7(31)
Caringforchildren29.9(58)11.9(22)
Caringforothers(outsideofwork)16(31)9.2(17)
Timepressure/notenoughtime39.2(76)24.9(46)
Emotionalormentalhealthproblems19(36)8(15)
Note: Thepercentagewascalculatedbydividingthenumberof respondingdentistsineachcategorybythenumberofdentistswhohave completedthesurveyinfull.Incompleteparticipationwasnotincludedin thepercentagecalculation.
(CourtesyofMaraghaT,AtanackovicJ,AdamsT,etal:Dentists’ mental health:Challenges,supports,andpromisingpractices. JDRClinical TranslationalRes 10:100-111,2025.)
Theyfelttheywereunderaddedpressureandwerefrustrated withbeingseenaslesscompetentthanmaledentists.
Associatedentists experiencedalackofautonomyandcontrol overtheirschedules,withconflictsbetweenthemandtheirofficemanagersorpracticeowners.Thesedentistsfeltthey werebeingmicromanagedandexperiencedadverseeffects fromtheofficebureaucracyoractualbullyingexperiences. Someof ficepersonnelsetunreasonableandprofit-drivengoals forassociates,whosometimesleftthepracticeaftersigni ficant stress.About13%ofthedentistsexperiencedstressrelatedto poorrelationshipswithcoworkersandotherdentalpractice workers.Femaledentists,whetherinassociateorotherroles, felttheirpsychologicalsafetywasatrisk,butthiswasn’treported bymaledentists.
Theaddedresponsibilityofbeinga practiceowner ledtoconcerns aboutcompetitionaswellashowtomanagehumanresources, finances,andproductivity.Ownersarealsotaskedwithdoing troubleshootingandmanagingtechnologyissues,orderingsupplies,andkeepingtrackofinventory.Maintainingtrained,competentdentalstaff,includingreceptionists,assistants,andhygienists, wasreportedlyaspecialconcerninruralandremoteareas.
Practiceownersfelttheseresponsibilitiesalteredtheirperspectiveoftheprofession,especiallyalackofprofessionalsatisfaction. About49%ofthedentistsinvariousrolesreportedpractice managementresponsibilitiesasawork-relatedstressor.
Genderin fluencedtheparticipationofdentistsindifferentprofessionalroles. Femalepracticeowners citedaproblemofperceptionwiththeirstaffs,whooftensawthewomanaslessassertive, moredramatic,andlessproductivethanmeninthatrole.The respectandresponsestofeedbackthatfemaledentistsreceived withrespecttopracticemanagementandpatientcareduties werelacking.Femaledentistsoftenfelttheyshouldsuppress theiremotionssotheyseemstrongerandmoreincontrol likeaman.
Thesenegativeinfluencescausedwomentobelesswillingtoown apractice.Thosewhowereownerswereoftenmoreproneto sellingthepracticeandtakingonanassociaterolesotheycould balancepersonalandprofessionalresponsibilities.Morefemale dentistsreportedtheirworkloadasawork-relatedstressor comparedtomen.
Bothpracticeownersandassociatesexperiencedlonelinessand isolation.Thisisaparticularprobleminruralorremotesolo practices.Associatesmentionedfeelingalackofsupportfortheir workandhadnoonetocallon.
Youngerdentistsandthosewhohaverecentlygraduatedexperiencestressrelatedtotheeducationaldebttheyhaveincurred. Thisisexacerbatedbyuncertaintyaboutjobandmentorship prospects.Youngerfemaledentistsalsoexperiencephysiological changesrelatedtopregnancy,peri-menopause,andmenopause andcitedthesechangesasinfluencesontheirmentalhealth andwell-being.
Dentistsfromvaryingethnicitiescanexperienceracism,especiallyinruralandremotesettingswherefewermembersoftheir minoritygrouplive.Dentiststrainedinternationallycanexperiencedifficultyintegratingintoacommunity,strugglewithlanguagebarriers,andhavetroublebalancingthesupportoftheir immediateandextendedfamilies.
Caregivingresponsibilitiescanalsoin fluencedentists’ mental health.Femaledentistscitedchallengesbalancingtheirtraditional responsibilitiesrelatedtothehomewiththedemandsofowning
Table3. PromisingPracticesThatVariousCanadianOrganizationsHaveDevelopedandImplementedtoSupportDentists’ Mental HealthandWell-being
OrganizationProgram/InitiativeDescription
CDSPIMember’sAssistanceProgramTheprogramisavailabletodentistswhoaremembersofsome ProvincialandTerritorialAuthorities,includingBritishColumbia, Ontario,NewFoundlandandLabrador,andNovaScotia.
BritishColumbiaDentalAssociation (BCDA)
DentistWellnessProgram(DWP)AnearlyinterventionprogramfundedbyBCDA.Theprogramwas launchedinMay2019toassistpracticingdentistsindealingwith mentalhealthissues(includingaddiction)inresponsetodentists’ needforadentistwhocanrelatetotheirstrugglesandunderstand whathappenswithchallengingpatientsandpracticemanagement. Asapartoftheprogram,counselingservicesareavailableto dentists,dentalstaff,andtheirfamilies.
AlbertaDentalAssociationandCollegeWellnessProgramAconfidentialprogramthatinvolves11dentistswhoactas firstline respondersandreferdentistsandtheirfamilymembersto registeredpsychologists(foraquote,seeinterview16).
OntarioDentalAssociation(ODA)WellnessProgramandNewsletterTheprogramprovidesODAmemberswithaccesstoaphoneline staffedbydifferentdentistsattheotherend,inadditiontoproviding dentistswithaccesstoonlinecounseling.TheODAalsoaddresses issuesofmentalhealthintheirnewsletterandhasorganizedan onlineworkshoptodiscussmentalhealth,stressors,andcoping strategiesfordentists.
NewfoundlandandLabradorDental Association(NLDA)
RoyalCollegeofDentalSurgeonsof Ontario(RCDSO)
UniversityofSaskatchewanFacultyof Dentistry
WellnessCommitteeandNewsletterThecommitteehassetupawellnessboothintheAssociation’s annualconference.Theassociationhasalsodesignatedapagein theirnewsletterstodestigmatizehelp-seekingformentalhealth issues(seeinterview6foraquote).
WellnessInitiativeTheinitiativeaimstohelpdentistsaccessnecessarytreatment throughdesignatedfacilities,particularlythosewithaddiction issues(Stakeholder-3ON).
Students’ WellnessCommitteeand Faculty-SpecificInterventions
StudentshaveaMentalHealthandWellnessCommittee(see interview11).
TheFacultyofDentistryisliaisingwiththeUniversity’sWellness Centretoprovideasessionduringorientationweektodiscuss mentalhealth,self-care,andwell-beingofstudents
UniversityofTorontoFacultyofDentistryMentalHealthLunchandLearnsTheLunchandLearnSessionsaimtodiscussthementalhealthand well-beingofdentalstudentsthroughouttheircareersindental school,inadditiontoprovidingsupporttostudentsthroughthe Students’ ServicesOffices.
(CourtesyofMaraghaT,AtanackovicJ,AdamsT,etal:Dentists’ mentalhealth:Challenges,supports,andpromisingpractices. JDRClinicalTranslationalRes 10:100-111,2025.)
adentalpractice.Oftenthereiscon flictandablurringofthe boundariesbetweenhomeandwork,leadingtoguilttowardchildrenandfamilymembersaswellasoverwhelmandstresstoward theirworksituation.
Familymemberscanalsopresentchallenges.About30%offemaledentistsandabout12%ofmaledentistswerestressed regardingchildcare.Femaledentistscitedalackofsupport frompartnersandtheneedtosecuregoodchildcareduringtheir workdays.Non-work-relatedstressorsthatwereidenti fiedin additiontochildcareweretakingcareofothersintheirenvironment,timepressures,andemotionalhealthissues.
Variousorganizationalandsy stemicmentalhealthandwellbeingsupportresourcesandinterventionsareavailableto
providesupporttodentistsdealingwithmentalhealthchallenges(Table3).Someprogramsoffertraininginprevention andawarenessofmentalhealth.Therearealsothosethatsupporttheearlyintegrationofmentalhealthintothedentalcurriculum.Dentistswhohavedevelopedmentalhealthissues tendnottohaveformalevaluationprocessesandinterventions availabletohelpthemthroughtheseexperiences.
Dentistssuggestedintroducingtheconceptsofmentalhealth, coping,andstressmanagementskillsintothedentalschoolcurriculum.Dentalschoolsshouldbecomemoreinvolvedinpreparingstudentsfortherealityofpracticemanagementandpossible stressors.Businessmanagementcoursesshouldalsobepartof dentalschooltrainingtomakedentistsmoreabletobalance therigorofclinicaldentalpracticewiththebusinesssideofthe profession.
Mentalhealthinterventionsandresourcesneedtobedesignedto addresstheuniquecircumstancesofdentists.Thismayinvolve participationinonlinegroupswherediscussionsoftopicscan leadtotheidenti ficationofresources,issues,andstressors. Thesegroupscanhelpdentistsdealwithlonelinessandisolation andoffertherapeuticresponsestomanysituations.
Involvementinorganizeddentistrycanalsohaveapositive impactonmentalhealth.Dentistsreceiveasenseofcommunity andpurposewiththeseefforts.Thismayalsocreateasenseof communityamongwomenintheprofession,enhancingthesupportiveandempoweringroleoftheseorganizationswithrespect topracticemanagementandownership.
Amentoringinitiativehelpsyoungdentistsbridgethegapbetweenschoolandthejobmarket.Participatingdentistssuggested dentalassociationscouldcreateformalmentorshipprograms. Thesecansupportoverallmentalhealthandwell-being,increase theyoungdentists’ levelofassurance,andgivethemasenseof community.
Severalfactorscontributetothementalhealthstrugglesthatdentistsface.Amongthesefactorsaresex/ gender,practiceownership,ethicalpractices,isolationandloneliness,andempowermentforfemale practitioners.Mentoringinitiativesonthepartofdental associationscanincreasethesenseofcommunityand helptotransitionnewlygraduateddentistsintoworkingsituations.
MaraghaT,AtanackovicJ,AdamsT,etal:Dentists’ mentalhealth: Challenges,supports,andpromisingpractices. JDRClinicalTranslationalRes 10:100-111,2025
Reprintsavailablefrom TMaragha,DeptofOralHealthSciences, FacultyofDentistry,TheUnivofBritishColumbia,2199WesbrookMall,Vancouver,BCV6T1Z3,Canada;e-mail: tala.maragha@alumni.ubc.ca
In2024,aCBSNewsreportdocumentedatrendwheremarginallydiseasedandtreatableteethwerebeingextractedsothat dentalimplantscouldbeplaced.Thereportfocusedonthemotivationbeingprofitratherthanethicalpatientcareandquestioned thedentalprofession’sethicsinthesecases.TheAmericanAssociationofEndodontistsandAmericanAcademyofPeriodontologyexpressedconcernsabouttheproblemsexposedinthereport andwarnedthatextractionofteethisirreversibleandmayseriouslyimpactpatienthealthandqualityoflife.Chasingprofitwas discouragedwhenpatienthealthwasatrisk.Ethicalpractice dictatedthatpatientsbefullyinformedofalltreatmentoptions, especiallythosethatpreservenaturalteeth.Notcompletelyinformingpatientsoftheoptionsisabreachofacoretenetof theAmericanDentalAssociation’ s PrinciplesofEthicsandCode ofProfessionalConduct (ADACode),speci fically,patientautonomyorself-governance.Theethicsofextractionandtooth replacementwithimplantsversusperformingperiodontaltreatmentwerechallenged.
RemainingEthical
Patientswhoarediagnosedwithteethrequiringextraction andreplacementwithimplantsmustbeinformedofallthe reasonableoptionsavailablealongwiththeclinician ’ srecommendedapproach.CompliancewiththeADACoderequires thatthepatientcanrespondaf fi rmativelytothefollowing questions:
Didthecliniciandiscusstreatmentoptionsthatwouldretain andmaintainthenaturaldentitionsothatthepatientcan makeacompletelyinformeddecision?
Didtherecommendedtreatmentsatisfytheethicalrequirementofnonmaleficence(donoharm)andbeneficence(do good)?
Wasthetreatmentrecommendationtruthful(veracityor truthfulness)andnotmotivatedbyprofit?
Theevidence-basedliteratureshowsthatstrategicextraction shouldbedeferredwheneverpossibletoavoidcomplications foundwithperi-implantitis.Dentalimplantsthatareproperly placedhave5-yearsurvivalratesof85%to90%,butthesurvival ratedoesn’talwaysmatchthesuccessrate.Betweenabout15% and20%ofpatientswithimplantsdevelopimplantitis.Implantlevel datarevealperi-implantitisinabout9%to13%ofimplants.Bone lossanddepthofpenetrationoftheinflammatoryresponseis greaterinperi-implantitisthaninperiodontitis.Thetreatmentof peri-implantitisismorecostlythanthatofperiodontitisandthe long-termprognosisisworse.Noneofthesefactorsarebeneficial forthepatient.
SeveralresearchersreportmolarswithgradeIIfurcationinvolvementcanbetreatedandhaveameansurvivalofabout15years. Thetreatmentofperiodontitisandmaintenancetherapyas appropriatecanpreservethedentitionforasubstantialnumber ofyears.Withthisinformationinhand,extractionandreplacementwithdentalimplantswouldappeartonotbethe firsttreatmentrecommendation.
Implantsarebene fi cialwhenthepatients ’ teethhavebeen lostorarebeyondsaving.Oftenpatientswhohavecomplete
traditionaldenturesbene fi tsigni fi cantlyfromatransitionto implant-supportedfunctionandachievelife-changingesthetics.Dentistsaretrainedtoknowwhenteetharetruly beyondhelpandwhentheycanbesavedwithreasonable treatment.Patientbene fi tandnotpro fi tshouldguide recommendations.
Implantscanbewonderfulbutshouldn’tbeusedin everycase.Thenaturaldentitionhastheinnateability tohealwithpropertreatmentandmaintenance.Implantscan’tactuallyreplacethenaturaldentition. Thepatient’slong-termhealthandqualityoflife shouldguidethedevelopmentandrecommendation ofanydentaltreatmentplan.
HarrelSK:Dentistryhasbeenputonnotice. JAmDentAssoc 156:261-262,2025
Reprintsavailablefrom SKHarrel,DeptofPeriodontics,Collegeof Dentistry,TexasA&MUniv,3302GastonAve,Dallas,TX75246; e-mail: skharrel@gmail.com
Unethicalactivityisoftenconsideredsomeoneelse’ sproblem,withonlytheperpetratorbeingaccountable.Somewill trytojustifythewrongdoer ’sactionsbecauseofhisorher situationasasingleparentorseetheindividualunder fi nancialstress,leadingtothemisbehavior.Areweactuallyinnocentofanyintegritybreachorlapseinthehonestyof others.?Themanagementstylewechooseandthevalues weprojectasleadersin fl uencethebehaviorsofourdental team.Maintaininganethicalleadershipisessential.
Wechooseourmanagementstyleandvaluesandtrytomaintain animagethatwillconveythosechoicestoothers.Acommitment tointegritycaninfluenceourteamtoadheretothevalueswe have,whereasonethatisn’tsovirtuousmayencouragea flareupofapreexistingtendencytogoastray.Copingwiththedaily challengesintermsofpatients,colleagues,andeachothercan
becompromisedifwedon’thaveafocusonintegrityrather thanengaginginshadybehaviors.
Intimespast,Searsmanagersencouragedemployeestogrowproductioninautorepairorsalesquotas.Thegoalwastoincrease productivityandboostprofits.However,multiplecustomers complainedthatemployeesweremakinginappropriaterecommendationsandperformingunnecessarywork,leadingtolawsuits. Eventuallythecasesweresettledforabout$60million,butthe episodedestroyedthenationaltrustinSears’ autorepairdivision.
Leadersshouldactvirtuouslytomodelthetypeofbehaviorthatis desiredintheircompanyordentalpractice.Theemployeeshould thenbeabletotrustthattheleaderwillactintheemployee’sbest interest.Thiscreatesauthenticcommitmenttotheorganization anditsmission.Everyonecanbenefitfromthisworkethic.
ClinicalSignificance
Peoplearewatchingthosetheyinteractwithdaily, whichincludesthoseofuswhoaredentistsorother healthcareprofessionals.Ifwhattheyseeinour behaviordoesn’tappearaboveboardandethical, theywillquestionourgoodnessandmotivation.Any unethicalbehaviorwilleventuallybecomewhatpeople rememberwhentheythinkofourdentalpractice.It’s besttoprojectanimageofhonestyandactualcare forthoseweserve.
GrecoPMPAlleyesareonus. AmJOrthodDentofacOrthop 167:142-143,2025
Reprintsnotavailable
Theresponsibilitiesassociatedwithownershipofadentalpracticecanweighheavilyontheowner’sshoulders,butcanbe offsetbytherewardsofownership.Theseincludethesigni fi cant differencebetweenthewealthapracticeowneraccumulates andthatearnedbyanassociate.Iftheowneristhinkingof bringingonanassociatetosharetheburden,heorsheshould carefullyanalyzewhythiswouldbeagoodtime.Generally, thedecisionisalifestylechoice oraneconomicdecision.Lifestylechoicesaredesignedtosharetheburdenofpatientcare sothattheownercanhavemorefreedomand fl exibilityinhis orherlife.Economicdecisionsarebasedonthegrowthandrevenuecreationofthedentalpractice.Thesegoalsaren’tnecessarilymutuallyexclusive,butbeforetakingthestepofadding anassociate,thedentistshoulddeterminewhetherthemotivationisdrivenbyeconomicorlifes tyleconsiderations,thenlook atannualrevenue,numberofoperatories,newpatientsseen eachmonth,andplans(bothshort -andlong-term)forthepracticeandagoodassociate.
AnnualRevenue
It’sdifficulttohireandretainagoodassociateiftheannualrevenueofthedentalpracticeisn’tatorapproaching$1million. Annualrevenuelessthanthislevelisinsufficientfortheassociate toearnenoughtopayhisorherlivingexpenses,loanpayments, andotherbills.Generaldentalpracticestypicallyseeabout25% oftotalproductioncomeinthroughhygiene,soina$1million practice,about$750,000shouldcomefromthedentists,which isabout$62,500permonth.At30%ofcollections,whichisa
reasonablecompensation,theassociateearnsabout$9000per month,whichisn’tgreat.
Iftheannualrevenueislessthanabout$1million,gooddoctors willbehardto findandretain.Practicesthathireassociates beforereachingthisannualrevenuetendtohavethelowestsatisfactionlevelsandthemostissues.
Sixoperatoriesareneededtomaximizetheef ficienciesof bringingonanassociate.Withthisnumber,bothprovidersand thehygienistcanworksimultaneously.Thisallowsoverhead coststobereducedandof ficeproductivityincreased.Byhaving anextraprovider,revenuecangrowsignificantlywithoutadding daysthepracticeisopenandincreasingoverhead.
Practiceswithfewerthan6operatoriescanexpandthenumber ofdaysthepracticeisopen,whichofferssomeadvantages, includingexpandedavailability,whichcanbeadrawforpatients. Theownercanalsomentortheassociateadayor2eachweek whilefocusingprimarilyonnonclinicaltasks.Staffoverheadwill increase,buttheaddedrevenuegeneratedfromextradays shouldsignificantlyexceedtheaddedcost.
Beforeaddinganassociate,thedentistshouldevaluateifhisor herrevenuesareincreasingandwhy.Ifthepatientbase’sageis increasing,placingmorecrowns,bridges,implants,andveneers canaccountforahealthierpicture.Per-patientvaluemayhave increasedwithoutaddingnewpatients.Ananalysisofhowfar outthehygienedepartmentisbookedandthenumberofnew
patientsconsistentlyscheduledeachmonthshouldindicateifthe practiceisgrowingorifthepracticeislosingpatientsorfailingto convertnewpatientstolong-termpatients.Thisisespecially importantifthenewpatientnumbersareincreasingbutrevenue isn’t.Apracticeshouldsee20to25newpatientseachmonth whentheadditionofanassociateiscontemplated.
Beforehiringanassociate,thedentistshoulddecidehisorher plansforthepracticeandhowanassociatewould fitinto them.Short-termandlong-termplansneedtobeformulated. Thedentistmaydesireapartnership,ormaybeheorsheislookingtoretireandsellthepracticetotheassociate.Thegoalmaybe tosellthepracticetoathirdpartysomewheredownthelinewith orwithoutanassociatebecomingapartner.Theseissuesneedto bedecidedbeforehiringanyone.Atthetimeofhiring,theseplans shouldbediscussedtoavoidpoorcommunicationbetween ownerandassociate.Iftheassociateasks,theownershouldbe honestandestablishafoundationforagoodworkingrelationship.Planningaheadcanavoidlosingmoneythroughfalsestarts orbrokenplansandcanprovidecontinuityandstability.
Ifthedecisionwillbealifestylechoice,theannualrevenueshould beatorabove$900,000tomanagecash flowandkeeptheassociatebusy.Associatesaremorelikelytostaylongtermandwork hardtobuildgoodwillandgrowwiththepracticeiftheyare givengoodlevelsofproduction.Theownercandecidehow manydaystotakeoffwhilemaintainingasteadyincomestream. Thegoalistogivethepracticesufficientgrowthtoestablisha stronginfrastructurethatwillsupportthedentiststeppingback
Atsomepointinhistory,leaderswereputonpedestalsandworshipedasthosewhocoulddonowrong.Infact,noonewouldpresumetopointoutanymistakesormisstepsaleadermighthave takeniftheirservantswantedtokeeptheirheads.Asaresult, leadersoftendevelopedanarrogantdistancefrommeremortals. Manyhavelearnedtobethistypeofleader,demandingrespect withoutdoinganythingtoearnit.Ifanythingwaswrong,itwas theplebeianswhowereatfault.Formanyyears,inbusinessand evenindentaloffices,thistypeofleadershipwascommon.Changingtoanewleadershipmodelcanbejustwhatthedentalpractice needs.
withoutjeopardizingpracticegrowth.Inalifestyledecision,the owner ’sincomewillbesubstantiallylowerevenifannualrevenue ismaintainedorgrowingbecauseoftheaddedoverheadofthe additionalprovider.
Iftheannualrevenueisinsuf ficient,it’swisetoworkhardfor anotheryearandthensellthepracticeratherthanbringonan associate.Lower-incomepracticestendtocarryahighriskfor bothownersandassociatesleavingtherelationshipinfrustration. Theassociatedoesn’tmakeenoughincomeandtheownerfeels thepracticeisworseoffthanbefore.Thiscanundermineany chanceforthelifestylebalancethatwasinitiallysought.
Apracticeownermayfeellikethebusinessneeds addedhandstomakelifeeasierandtoachievethe growthneeded.Planstoaddanassociateshouldbe designedtocontinuallystrengthenthepractice,supporttheeconomicstatusofthepractice,andallow forthelifestyletheownerdesires.It’simportantthat thedentistknowhimselforherselfandunderstand whatisdesiredandthebestwaytogetit.
WoodJ:Howtoknowwhen(andwhy)tohireanassociate. Dentaltown 26:61-63,2025
Reprintsnotavailable
Thedentalpracticewasn’tthrivingandover100employees stayedforaveryshorttimebeforetheyranouttherevolving door.Theleadershipofthepracticeneededtobechanged. ThentheCOVIDpandemichit.Inthosedarkdays,aconsulting companyofferedabusinessfoundationscoursedesignedto openthemindsofpracticeownersandshowthemwhatthe futurecouldbecome.Thecourseleadersandotherpractice ownersbecameexamplestotheattendeesandmodeleda newleadershipstylewheretheownertookcareoftheteam byputtingtheneedsofothers fi rst,rewardinghardwork,and liftingothersup.Thedaywassaved.
Themantrathatledthechargeintoservantleadershipwas the missionofthepracticeistheboss. Withtimeandintention,the teamforgavetheonewhohadformerlyenslavedthem.With thenewapproach,everyonedevelopedanopenmind,relationshipswithothers,generouslistening,agenuinedesiretocare foreachother,andarecognitionthatweshould fi rstofallbe human.Noonepersonwasmoreimportantthananyother, andnopatientcomesbeforethedentalteam.
Thingsatthedentalpracticehadchanged.Ratherthanclockwatchingemployees,incredibleindividualscametoworkwith theteamalreadyinplace,provingtobebothinnovativeand inspirational.Thedentalpracticehadateamthathadworked togetherformorethanadecadeandsomecloseto2decades. Then2newemployeeswereadded,sotherewasatotalof15 workers.Butsomehowthenewassistantandassociate,who hadbeenwiththepracticeforlessthan4months,weren’t meshingwiththeothersandthecoursewasn’tsmoothlikeit usedtobe.
Noonewascomplainingaboutthesituation,buttheleader knewithadtobeaddressed.Thenewhireswereallowedto leaveearly,buttheremainder oftheteamgatheredinasmall roomtodiscussthesituation.Theleaderchosetositonthe fl oorinthemidstoftheteammemberswhowereinchairs oronacouch.Themessagethateveryonewasabovetheleader wasclear.
Theleadersharedthattheirpatientsseemedconfusedabout treatmentplanpresentationandtherewaslowacceptancein theassociate’sschedule.Inaddition,thenewassistantwas strugglingtolearntheof fi ceprotocols.Thenthequestion: Howdowesolvethis?
Eachteammembermadesuggestionsandofferedinnovativesolutionsthatwouldhaveneveroccurredtotheleader.Theteam collaboratedandconnected,showinghowmuchtheylikedeach otherandwereengagedinatrustingandsupportiverelationship thatwasbothunitedinpurposeandempoweredbytheirtask. Theimpossibleproblemwassolved.
Practiceownersshouldn ’tbetheonlyoneswhocansolvea problem.Infact,problemsareoftenbetteraddressedbythe teamastheysharetheirexperienceandexpertise.Connecting onahumanlevelcanresultinabetteroutcomethanwaitingfor the “importantleader” todictatethesolution.Becausethe leaderhadestablishedatrustingandsupportiverelationship amongtheteammembers,thewholeprovedtobegreater thanthesumofitsparts.
Teammembersaretalentedandhaveuniquestrengths anddegreesofknowledgethatneedtobenurtured. Combiningthetalentsoftheteaminvolvesletting themusetheirintelligence,independence,andinitiative inwhatevertaskisbeforethem.Thegreatestmagic happenswhentheentireteamactstogether.
AugustynM:Frompedestaltopartnership:Rede finingleadership. DentEcon 115:27-28,46,2025
Reprintsnotavailable
Motivationalinterviewing(MI)is anevidence-basedandpatientcenteredapproachtobehaviorchange.Itinvolvescommunicationdesignedtosupportapatient’smotivationtochangeby havingthepractitionerleadthepersontoconsiderabehavioral alterationwhilethemaintaininganeutralpositionregardingthe individual’sdecision.Theindividualisthenabletoovercomeany ambivalence,andhisorherchoiceishonoredastheresultof thepatienttakingcontrolofthesituation.Thisapproachallows
theessentialpatient-practitionerrelationshiptobemaintained. Thepractitionercanaskscalingquestionstoevaluatetheindividual ’sreadinessforchangeandtorevealanybarriersorfacilitatorstotheneededchange.Originallydevelopedforuseto promotebehaviorchangeinalcohol-dependentpatients,MI hasbeenusedsuccessfullyinma nyhealthcaresituations.The applicationofMIindentalsettingswasexplored,notingitscurrentusesaswellasinvestigationsintopotentialusesanddetailingthetrainingrequiredforadentalteam.
Frustrationwithchangeeffortsisoftenexperiencedwhencliniciansgiveadvicewiththegoalofpersuadingpatientstodothe rightthing,anapproachcalledthe fixingreflex.InMI,resistance tochangeisaddressedthoughtheinteractionbetweenpatient andclinician.Itavoidsthe fixingreflexandinsteadencourages “rollingwithresistance,” whichadoptsare flectiveandcurious attituderatherthanconfrontationorarguments.Clinicians acceptthecontextoforalhealthwithinthelivesoftheirpatients andmaintainanonjudgmentalapproachtoachievesuccessful outcomes.Patientsareseenasexpertsontheirownhealth, withthecliniciansupportingpatients’ journeytoidentifyinggoals that fitthemselvesratherthanspendingtimeandenergyjust impartingknowledge.
Healthbehaviorsarein fl uencedbymanyfactors,includingthe patient ’sbeliefs,income,andeducational,social,physical, mental,andsocialconsiderations.VarioushealthcarespecialtieshaveusedMItopromotepositivehealthybehaviors (Figure1 ).TheseincludeuseswithHIVpatientadherencetoantiretroviraltherapy,decreasingdepressionsymptomsinpatients,overweightissues,alcoholconsumption,andincreasing physicalactivity.SmokingcessationeffortshavebeenmoresuccessfulwithMIthanwitheffortstoconveybriefantismoking advice.
EvenbriefMIeffortscanleadtobeneficialchanges.Indentalsettings,timecanbealimitingfactor,sobriefinterventionsmaybe
allthatareavailable.Allmembersofthedentalteam,including students,canuseMItointeractwiththepatienteveninintervals ofjust5to10minutes.
Behaviorchangeisoftenanessentialcomponentinimproving patients’ oralandgeneralhealthandenhancingtheeffectiveness oforalhealtheducation.MIpositivelyinfluencesself-ef ficacy, whichisthebeliefthatonecanmaketherequiredbehavior change.Thisbeliefiscentraltobeginningandmaintaininghealthy behaviors.Higherpatientself-ef ficacyinoralhealthbehaviorshas beenrevealedinstudiesofdental-relatedsituationssuchas reducingtherisksofcaries,periodontaldisease,toothwear, andoralcancer(Figure2).Inaddition,MIhasprovedeffective inreducingtheneedfordentalgeneralanestheticsandin reducingpatients’ dentalanxiety.
DentalteammemberswillbenefitfromtraininginMIandwillbe morelikelytoseebetterpatientoutcomesinrelationtoreadiness forchangeoractuallymakingachange.Thistrainingcanbeoffered duringundergraduatelifeaswellasatpostgraduatelevels.
Dentalundergraduatesmustdevelopandshowevidenceofprofi ciencyincommunicationskillsbytheendoftheirundergraduateyears.Studiesofhygienistswhoattended14hoursof traininginMIandcompletedpre- andpost-trainingevaluations coulddemonstratesigni fi cantlyimprovedpatient-centered communicationskills.Evenwith3hoursoftraining,third-year dentalstudentswereabletousetheirMIskillsonapatient
Figure1. ExamplesoftherangeofhealthcaresettingsinwhichMIhasbeenreportedasused(thislistisnotexhaustive)(CourtesyofAimanH,KilgariffJK, MarksD,etal:Doesmotivationalinterviewinghavearoleindentistry? BrDentJ 238:166-171,2025.)
Figure2. ApplicationsforMIindentistry.(CourtesyofAimanH,KilgariffJK,MarksD,etal:Doesmotivationalinterviewinghavearoleindentistry? BrDentJ 238:166-171,2025.)
andcompleteanassignment.Thosewhoaccuratelyidenti fi ed thepatient’sreadinesstochangehadthemosteffectiveMIskills. ComparisonsofstudentstrainedinMIornottrainedinitundertooksmokingcessationinterventions.ThosewithMI traininghadasigni fi cantlygreaternumberofpatientsquitsmokingcomparedtothosewithouttheseskills.
TheuseofMIisalsoapplicable tonon-technicalskills,which arecognitiveandinterpersonalabilitiesessentialinclinicalsettings.Theseskillsincludecommu nication.Non-technicalskill developmentandassessmentstudieshaveindicatedtheneed forMItrainingtobeincludedinmedicalcurricula.
AbarriertointegratingMItechniquesintoundergraduate trainingistheabsenceofproperlytrainedclinicalmentors. EmbeddingMItrainingandproficiencyinitsclinicaluseintopostgraduatetrainingforexistingdentalteamsisneeded.
LittleevidenceexistsconcerningpostgraduateMItraining. Recognizingtheneedfornon -technicalskills,effective communication,andcare-coor dinationamongpostgraduate dentistswillhelptoin fl uencetheincorporationofMIinto thecurriculum.Dentalhygienistsalreadyhavebeenstudied fortheirtraininginanduseofMI.Dentalhygieniststrained inMIusebeforegraduationcontinuetoapplyitaftergraduation.It’ssuggestedthatperiodicrefreshertrainingmayhelp topromoteandsustainthevalueandlong-termuseofMI techniques.
TheuseofMIindentalsituationsappearstobevaluableandcan berecommended.Patientsareguidedtoexploretheirmotivationsforchange,recognizethebene fitsandbarriersforchange, andidentifytheirgoals.ThroughtrainingintheMIprocess,practitionersareabletoleadpatientstobetteroralhygienepractices, lesscariesdevelopmentorperiodontaldisease,andreduced dentalanxietyalongwithbettercopingstrategiesforpatients withdentalanxiety.
MIhasprovedtobeapowerfultoolforsupporting patientstoundertakepositivechangesthatleadto betterhealthoutcomes.Consistentevidenceshows it’sefficaciousandrelevanttousesindentalsettings. TraininginMIneedstobeincorporatedintoundergraduateand/orpostgraduateeducationtohelp dentalstudentsanddentistsdevelopstrongdentalpatienttherapeuticrelationships.
AimanH,KilgariffJK,MarksD,etal:Doesmotivationalinterviewinghavearoleindentistry? BrDentJ 238:166-171,2025
Reprintsavailablefrom HAiman:DundeeDentalHospand ResearchSchool,UK;e-mail: huma.aiman1@nhs.net
Dentalprofessionalscanencounterchallenginginteractions whiledeliveringcareandtheirtrainingdoesn’talwayscover howtohandletheseevents.Dentalschoolteachesstudents howtodiagnoseandtreatdentaldiseaseandmaycoverhow tohandlepediatricpatients,butadultpatientmanagementgenerallyisn’tcovered.Amongthescenariosthedentistmayfaceare angrypatients,patientswithdentalanxiety,thoserefusetreatment,andsomewhowillengageininappropriatebehavior.Guidanceisofferedforeachoftheseexamplesbasedonthe experiencesofactualdentists,wisdomgainedwhileteachingat dentalschools,advicefromcolleagues,andpersonalresearch.
DentalfeariscommonamongadultsintheUnitedStates,and patientsoftenmasktheirfearbyashowofanger.Clear
communicationmaypreventtheangerbyensuringthepatientis well-informed.Forexample,it’swisetowarnpatientsaheadof timeaboutpainfulaspectsoftreatmentandpossiblecomplications.Activelylistening,remainingcalm,andacknowledgingthepatient’sfeelingscandeescalatethesituation.Non-confrontational languageisessential,alongwithexpressionsofempathyandthe avoidanceofdefensiveness.Intermsofpersonalcare,it’swise tokeepingasafepositionduringinteractions.Inapatientinteraction,it’sOKtoagreeoragreetodisagree justtryto findcommonground.
Thedentistshouldalsoclearlysetthelimitsoftheinteractionand makesurethepatientknowswhat’sunacceptableandthe possibleconsequencesofexceedingthelimits,includingcalling lawenforcement.Whentheinteractionendangersthedentist orothers,thedentist’sgoalistoisolatetheaggressor,evacuate everyoneelse,andcallforlawenforcementhelp.


Empathyisvital,andthedentistshouldrecognizethatsometimesthepatientsimplyneedstovent.Duringthistime,the dentistshouldfacethepatientateyelevel(notlookingdown atthepatient),remaincalm,listenwithoutinterruption,and offernonverbalandverbalcommunicationthatvalidatesthe patient ’sfeelings(Figure1 ).Agreeingthatthepatient ’ semotionsarevalidandtakingthetimetosummarizewhatthe
problemseemstobereassuresthepatientthatheorshe hasbeenheard.
Inthecaseofanangryorrudepatient,thedentistshouldalso quittakingitpersonally(QTIP).Patientsmaybereactingtoa myriadofsituations,includingpain,fear,jealousy,prejudice, insecurity,undiagnosedoruntreatedmentalillness,stress,or

antiauthoritarianfeelings.Thede ntistcandeescalatethesituationbymakingeyecontact,remainingcalm,breathing,staying professional,andQTIP.
Patientswhohavedentalphobiacanexperienceextreme distressyetknowthattheirfearsareirrational.Tellingthepatienttorelaxgenerallyisn’tsufficient.Dependingonthe severityoftheanxiety,patientsmayrequirepharmacological and/ornonpharmacologicalmanagement.Thepharmacological optionsincludenitroussedation,oralsedation,oralconscious sedation,intravenoussedation,orgeneralanesthesia.Thenonpharmacologicalapproachescanvarysigni ficantlyandinclude thefollowing:
Assess:Identifytriggersandavoidthem.
Shareinformation:Whilethisreducesthepatient’sfear,the amountofinformationthatmustbesharedwillvary.
Signaling:Tellthepatienttoraisethelefthandoruseafrog clickerifheorsheisuncomfortableorneedsthedentistto stop(Figure2).Ensurethatthepatientisclearaboutwhich handistoberaisedbecauseotherwiseheorshemay encountersharpinstrumentsifthewrongoneisused,or youmayfailtoseetheraisedhand.
Tell-show-do:Demonstrateeachstepoftheprocedurefor thepatient.
Distraction:Offeraudiobooksormusic.
Cognitivemodification:Focusonpositiveoutcomesasyou explainwhatwillhappenandwhy.
Emotionalsupport:Maintainawarm,friendlydemeanor. Physicaltools:Givethepatientastressballtosqueezeduring injections(Figure3).
Retrospectivecontrol:Conductadebrie fi ngafterthe appointment,askingthepatientabouthowtheexperience wentandifheorshedesiresthatyoudosomethingdifferent atthenextvisit.
Somepatientstrytocontrolthevisitandtellthedentistwhathe orsheshouldorshouldnotdo.Ifthepatientisn’tallowingthe dentisttodiagnoseortreatactivedisease,thepatientandthe dentist’slicenseareatrisk.Thedentistshouldaskthepatient toexplaintherationaleheorsheisusingtomakethesedemands. Somethingsmaybeoptional,butdiagnosticproceduresand treatmentsforactivediseasearen’t.Ifthepatientcontinuesto refuseessentialcare,the finaloptionistodismissthepatient.
Somepatientsaskinappropriatequestions,suchasthoserelated tothedentistbeingmarriedornot,whereheorsheisfrom, whenheorshegetsoffwork,orsuggestingasocialmeeting. Ratherthanignoring flirtatiouscomments,thedentistshould bedirectandmature,explainingheorshewon’tbesharingpersonalinformation.Refocusingthepatientonthedentalexaminationorprocedureandaskingthepatientaboutanyconcernshe orshehasareappropriateresponses.
Dentistsarehighlytrainedtodiagnoseandtreatdental problemsbutpatientscanpresentbehaviorsthat thedentisthasn’tbeenpreparedtohandle.Taking thetimetocalmpatientswhoarefearful,anxious,or angry;addressingissueswiththosewhorefusetreatment;anddirectlymanaginginappropriatecomments canhelptonavigatethesepotentiallychallenging situations.
JacobsonW:Betterbehavior. Dentaltown 26:45-49,2025
Reprintsnotavailable
Dentalpracticeemployeesdon’talwaysunderstandthespreadsheetsownersusetoshowproductivityandotherstatistics. Ownershopethesedocumentswillencouragetheirteamto jumpintoactionandhelptomeetgoalsthatwillhelpgrowthe practice.Theymaysetthegoalsthattheywanttheteamto
buyinto,yettheteammaynotseehowthosegoalscanbetranslatedintowhattheydo.Teamsneedtohaveapersonalrelationshipwiththedatabeforetheywillinfluenceperformance. Involvingtheteamindevelopingrealisticgoalsandhelping themseehowwhattheydo fitsintothosegoalsarevitalparts ofanowner’sjob.
Aquickwaytosetproductiongoalsistotaketheannualnumbers andincreasethembythesamepercentageusedtoincreasefees. Itmayseemlogical,butthisapproachhasproblems.
Theincreasedproductiongoalsaren’tsupportedbyaplanfor whattheteamwilldotoachievethenewgoals.Theresultcan beunachievablegoalsandfrustration.Inaddition,this approachisblindtotheimpactofsignifi cantpracticechanges. Amongtheseareincreasingthenumberofvacationdays, reducingorhiringhygienists,addingnewservices,orimplementingnewtechnologies.Anyproductiongoalshouldbe carefullycraftedtoreflectthesechangesandthechallenges thatcomewiththem.
Thedentistmustalsolinkanygoalstothepracticeexpenses. Withoutthislink,it’spossibletoachievegoalsandstillbeunable topayyourbills.Youneedtohavethecompletepicture which includesexpensesaswellasproduction.
Increasingfeesdoesn’talwaystranslateintoproducingorcollectingmore,especiallyifmanypatientshavePPOplans.Whatthe practiceproduces,charges,andcollectscanbesignificantly differentfromoneanother.
Tomakebettergoalsrequiresastep-wiseapproach.Theowner andteamshoulddevelopawishlistbudgetandanannualplanthat includesallproviderworkdaysandthepractice’shistorical collectionpercentage.Theproductiongoalssetwillthencover employeeraises,facilityimprovements,newtechnology,and compensation.Theteamshouldbemadeawarethatpracticeimprovementsandraisesaredependentonachievingthegoalsset, makingthegoalsrelevantandmorerealistic.
Thedentistmustinspireemployeestobecomemoreengagedin thepracticestatisticsbeforetheywillunderstandtheirrelevance. Approachestomakethesestatisticsmorerelevantandmeaningfulincludethefollowing:
Involvetheteaminsettinggoals.Beginbyhavingthem brainstormthingsthatwouldimprovethepractice,which couldincludenewtechnology,supplies,ergonomic
furniture,andthingsthatwillimprovetheirlives.Raises, teamoutings,continuingeducationopportunities,andpaid lunchesarealsoonthetable.Oncethesehavebeenidentified,theteamshouldresearchthepricesonthewishlist inordertodevelopabudget.Budgetinhand,theentire teamcandetermineifresultingproductionandcollection goalsareachievable.
Charttheteam’sprogresstowardfulfillingthewishlist.This willstrengthentheconnectionbetweenaccomplishingthe goalsandobtainingthewishlistitems.
Createtemplatesthatdepictdailyprocedurescorrelatingto productiongoals.Usingthisguide,theteamshouldevaluate ifthedayisscheduledtomeetthegoal.Ifitisn’t,theteam shouldbrainstormhowtomakeupfortheshortfall. Invitetheteamtobecomestatisticaldentaldetectives.Each personontheteamshouldbeassignednumbersthatrelate totheirjobascluestothepracticesystems.Theyshouldspeculatewhythepractice’sactualnumbersareatoddswiththe goal.Theteamshouldanalyzethemonth’sprogressorlack thereofandwhetheritwasananomalyoratrendcovering severalmonths.Allpossiblecausesshouldbediscussedbefore theproblemsolvingbegins.Theteamshouldn’tbeallowedto skiptosolutionswithoutaclearunderstandingofwhat happened.
Endeachmeetingbylistingtheactionsthatshouldbetaken. Thesewillfallintothecategoriesofwhattocontinuedoing becauseit’sworking,whattostopdoingbecauseit’snot working,andwhatshouldbestartedtoobtainabetterresult.
Includingthedentalteamincreatinggoalsforthe dentalpracticeisthebestwaytohelpthemunderstandthatwhattheydomattersinaverysolidway. Creatinggoalsthatarebasedonimprovementsthe teamdesiresshowshowmuchtheyarevalued.Seeing thattheachievementofthegoalsismetbytheirdaily workcanincreasetheirsenseofempowerment.
WeissS:Isyourdentalteamnumbtonumbers? DentEcon 115:26, 41,2025
Reprintsnotavailable
Costisanimportantreasonformanypeopletoavoidreceiving medical,dental,ormentalhealthcareorprescriptiondrugs. Oftencareisdelayedorskipped,potentiallyleadingtomore seriousconditionsandmoreexpensivecareneeds.Dentalcare hassomeoftheworstcosthurdles.Thirteenpercentofthepopulationfacedcostbarrierstodentalcarein2024,comparedto 4%to5%formedicalandmentalhealthservices,prescription drugs,andeyeglasses.Generally,thelackofinsurancecoverage andlowMedicaidreimbursementratesaretoblame,buteven insuredpatientsfacehighout-of-pocketcostsanddeductibles. Claimsareoftendenied,whichalsotendstodiscouragepatients fromhavingorcontinuingtreatment.Dentalpracticescantake onaproactiveroleinhelpingpatientsnavigatethechallenges andofferingexplanations,assistancewithpreauthorization, costestimatesandpaymentoptions,andsupportforappeals whenclaimsaredenied.
Itcanbeconfusingtodeterminewhattreatmentsarecovered, whatisthepatient’sresponsibility,andhowtochooseadentist. Whenthepatientselectsadentalpractice,providerscanhelpin explainingtheinsuranceplananditsbene fits.Inaddition,theycan cutthroughredtapeand “insurance-speak ” sothepatientcan receiveaclearexplanationofthecoveredservices,annualmaximums,deductibles,andcopayments.
Havinganindividualorateaminthedentalpracticewhocan guidepatientsthroughinsuranceandotherresourcesnotonly eliminatessurprisesbutcanbuildtrustbetweenpatientsandproviders.Patientsbecomemorecon fidentintheiractionsandmore willingtoseekdentalcare.
Changesaremadetoinsurancepoliciesyearly,andmanyare complexandtime-consumingfordentalproviders.Thepreauthorizationprocessclearlydeterminesapatient’ scoverage. Generally,planscover100%ofthechargesforroutineandpreventiveservices.Proceduressuchascrowns,rootcanals,gum surgery,dentures,bridges,extractions,andimplantsusually requirepreauthorization.Dentalproviderscanassistandpreventdelaysintreatment,surprisesinpaymentobligations,and coveragedenials.Althoughdelaysanddenialsstilloccur,patients willhaveanadvocatewhocanhelpnavigatethesituation.
Dentalservicecostsarerisingyearly,makingsome financialservicescompaniesholdoffoncoveringdentaltreatments.Asurvey
foundthat17%ofpatientsignoredarecommendedprocedure becauseitwasn’tcovered,andabout44%oftheseindividualsnoted thatthislackofcarecausedmoredentalproblems.Whencarewas delayed,22%foundthatotheroralhealthproblemsarose.
Providerscanguidepatientsthroughcoverageoptionsandoffer costestimatesand flexiblepaymentplans.Theseaccommodations canavoiddelaysintreatmentandfurtherdeteriorationoftheoral healthofpatients.Patientsshouldbeprovidedtransparencyintheir coverageandcostssotheycanmanagetheir financialresponsibilities.Financingandinstallmentpaymentsallowpatientstoreceive theimmediatetreatmentneededandpayforitovertime.
Patientsandpracticesbothbecomefrustratedwhendentalclaims aredenied.Thisprocessdelaystreatmentandcanleadtohigher costs.Denialsareoftenchallengedbypractices,which fileappeals andprovidesupportingdocumentationtojustifythecoverage.Recommendedtreatmentsaren’talwaysapprovedbyinsurancecompanies.Forexample,denialsarecommonforperiodontalscaling androotplaningproceduresdespitethefactthattheyareaccepted treatmentsforgumdisease.Theinsurancecompanylabelsthemas notmedicallynecessaryorexceedingcoveragelimits.
Reasonsfordenialofaclaimmayinvolvetheneedforpreauthorization,codingerrors,missinginformation,policylimitations, andnoncoveredservices.Providersshouldensurethatpatients knowtheircoveragelimitationsandadvocateonthepatient’ s behalfshouldaclaimdisputeensue.
Thecostofdentalservicesisrising,butreimbursementandcoverageforproceduresremaininsuf ficient tomeettheneed.Dentalcareproviderscanhelp patientsbyprovidingguidancethroughtheforestof coverageinformation,out-of-pocketcosts,andclaim denials.Patientsaremorelikelytokeeproutine checkups,followtreatmentplans,andachievebetter oralandgeneralhealthwhentheyhavethedental practiceastheiradvocate.
MitraniF:Helpingpatientsovercomecostbarriers,insurance disputestoaccessdentalcare. DentEcon 115:8-9,2025 Reprintsnotavailable
Socialmediaplatformsarepopularwithbothyoungandolderpersons,offeringeaseofuseaswellasspeedofcommunication.Asa result,it’snotsurprisingthatpatientsexpectandoftenwanttouse socialmediaplatformsandprivatemessagingtocommunicatewith dentalprofessionals.IntheUnitedKingdom,theGeneralDental Council(GDC)acceptsthatsocialnetworkingsitesandothersocialmediaoffereffectivecommunicationsinbothpersonaland professionalareas.Socialmediahasblurredtheboundariesbetweenpublicandprivatelife,however,sotheGDCoffersinsight intothestandardsexpectedofdentalprofessionals,whicharethe samewhetherthecommunicationisface-to-faceorviasocialmediaplatforms.Considerationsfordentalprofessionalswhousesocialmediatodirectlymessagepatientsincludetheneedtoprotect dataandtorespectprofessionalboundaries.
Organizationstendtobelegallyaccountableforhowtheycollect, store,use,anddestroypatients’ personalinformation.Dentalpracticesandsimilarorganizationshaveadutytoinformpatientsabout howtheyprocessdataintheircontrol.Usuallythisinformationis passedthroughaprivacynotice,butthedentalpracticemustensure thatthecommunicationclearlyconveystopatientshowtheirdata willbeused.Theprivacynoticemightincludeusingmobilephone numbersforsendingtextsthatremindpatientsofappointments. Ifthepatientconsents,thesetextmessagescanbesent,butthepatient’spersonalmobilephonenumbercannotbeusedforanything otherthanwhat’slistedintheprivacynotice.Ifthepracticeusesit otherwise,itmaybeabreachofthepractice’sdataprotectionpolicy andcouldleadtoapatientcomplaintorlegalaction.
Waystoensurethatcomplaintsandlegalactionareunlikely includethefollowing:
1.Beforeusingthepatient’scontactinformation,ensurethatthe patienthasconsentedtotheuseonthepractice’sprivacynotice.
2.Readthepractice’sdataprotectionpoliciesandproceduresto ensurethattheintendeduseisapproved.
3.Checkthepractice’semploymentagreementtoseeifthereare clausesregardingcompliancewiththepractice ’sinformation governance,confidentiality,anddataprotectionpolicies.Ensure thecommunicationiswithinthosepolicies.
Thedentalpracticeshouldneverstorepatientdataonapersonal mobiledevice.Thiswouldmakethepersonalinformationunsecuredshouldpublicnetworksbeused.Inaddition,personalmobiledevicescanbestolenorlost.
Inadditiontoadheringtothestandardsofthedentalpractice, dentalpractitionersmustadheretoprofessionalstandards whendirectlymessagingpatients.Boundariesbetweenpatients andpractitionersmustbemaintained.Usingpersonalplatforms forpatientcommunicationsratherthantraditionalmeanscan blurtheboundaries,withtheriskthatthepractitioner’sintentionsmaybemisunderstood.Havingaconversationabout appointmentavailabilitycandevelopintoadetaileddiscussion aboutthepatient’sdentalhealthortreatment,whichisprotected privateinformation.Withthispossibilityinmind,thedentalpractitionershouldcarefullyconsidertheappropriatenessofdirect messagingwithpatients.
UsingdirectmessagingplatformssuchasWhatsApp,Twitter,Instagram,andTikTokhasthepotentialforleavingpatientdataunprotectedandleadingtomisunderstandingsinpatient-practitioner exchanges.Thedentalteamshouldbeawareofthepitfallsand ensurethattheymaintaintheprivacyofthepatient’sdataaswell asrespecttheprofessionalcommunicationsofthedental practitioner.
Workplacecommunicationplatformsmayofferasecure andcompliantalternativetos ocialmedia.Theseplatforms ensurethattherecordsofpatientscanbemoreseamlessly integratedintothesystemsofthedentalpractice.Inaddition,theriskofblurringpr ofessionalboundariesis reduced.
TaylorJ-A:Privatemessagingwithpatients. BDJTeam 12:42-43, 2025
Reprintsnotavailable
Healthcarepractitionersmaybelievethattheycouldfacepotentialliabilityexposureiftheyreferpatientstoanotherpractitioner andthereferreddoctorcommitsmalpractice.Usuallythisisn’t true,withthedoctor’snegligencenotimputedbacktothemunlessthepractitionersknewthereferreddoctorwasincompetent orimpaired.Acasewaspresentedfrommorethan20yearsago, andthevariouscourts’ findingswereshared.
Girl,age6years,wasbroughttohergeneraldentistforroutine cleaningandexamination.Thedentistobservedcrowdingofthe girl’spermanentteethandreferredthepatienttothein-house orthodontistatoneoftheGeneralDentalServiceCorporation (GDSC)of fices.Theorthodontistreferredthegirltoanotolaryngologist(ENT)toassesshertonsils,adenoids,andairway.The orthodontist’sreferralindicatedthatthepatienthadtongue thrustandanopenbiteandaskedifthepatient’stonsilsandadenoidswereout.Theorthodontistalsotoldthechild’smother thatprovidinganyorthodontictherapywouldbeuselessuntil thetonsilswereremoved.
Twodayslater,attheENT’soffi ce,thechild’smotherexplained thatshehadbeentoldbytheorthodontistthatthepatient couldn’thaveherteethstraighteneduntilhertonsilswere removed.TheENTindicatedthathewasn’tconcernedabout thetonsilsandwantedtoconsultwiththeorthodontisttosee whatconcernshehad.TheENTobservedinhisnotesthatthe patienthadearinfectionsaboutevery2monthsforthepast 2yearsandwasmouthbreathingmostofthetimeduringtheexamination.Heindicatedanadenoidectomywasneededandthat theorthodontistwouldbecontacted.Aftertheconsultationwith theorthodontist,theENTsaidhebelievedthepatientwasa candidatefortonsillectomyandadenoidectomy(T&A)to improvethechancesoforthodonticsuccess.Themother’ s impressionbasedontheENT’scommentswasthatthechild’ s surgerywouldbedonefororthodonticreasons,andthepatient’ s medicalinsuranceauthorizedtheprocedure.
Thesurgerywentwellbutafewnightslater,thechildwasvomitingblood,collapsed,andwentintohypovolemicshockand eventuallycardiac/respiratoryarrest,causingbraindamage.As aresult,thepatientwasunabletotalk,eat,orclotheherself, requiredafeedingtube,woreaclamshellfrompelvistoshoulderstocounteractscoliosiscausedbymusclespasms,and needed24-hourpersonalcare.
ThefamilysuedtheENT,orthodontist,andgeneraldentistfor negligencebecausetherewasnomedicalreasontojustifythe surgeryandinformedconsenthadn’tbeenobtained.Theclaim ofnegligenceagainsttheENTwasbasedontherebeingnovalid reasonforrecommendingaT&Aforpurelyorthodonticpurposesandthefamilywasn’tinformedthattherewastheoption tohavethepatientmonitoredandreevaluatedinafewmonths. Theclaimagainsttheorthodontistwasbasedonimproperlyrecommendingsurgeryandfailingtoexplaintherisksandbene fitsof theprocedure,alternativestosurgery,orthecontroversyinorthodonticsregardingtheorthodonticbene fitsoftonsillectomy.
ThejuryfoundinfavorofGDSC,theorthodontist,andtheENT regardingtheinformedconsentclaimbutwasunabletodecide regardingthenegligenceclaim.Thecasewasappealed,noting thattheinstructionstothejuryweretonotbasetheirdecision ontheoutcomeofthesurgery.Theplaintiffarguedthatthisinstructionmisstatedthelaw(whichsaysthatphysicianscannot guaranteeagoodmedicalresultandabadresultisn’tevidence ofwrongdoingbythephysician).Theyfurtherstatedthatgiving thisinstructionessentiallydirectedthejuryinthetrialcourtto returnaverdictforthedefendants.Thecourtsidedwiththe plaintiffandfoundthatthetrialcourtshouldn’thavegiventhat instruction.
Regardingtheclaimforlackofinformedconsent,thecourt notedthatpatientshavetherighttomakedecisionsabout theirmedicaltreatmentandshouldbeprovidedwithsuf ficientinformationtomakethisdecision.However,patients claiminglackofinformedconsentmustprovethatthehealth careproviderfailedtoinformthepatientofamaterialfact relatedtothetreatment,thepatientconsentedtothetreatmentwithoutbeingawareorfullyinformedofthematerial fact,areasonablyprudentpersoninasimilarsituationwould nothaveconsentedifheorshewasinformedofthematerial fact,andthetreatmentproximatelycausedinjurytothepatient.Theplaintiffblamedtheorthodontistforrecommending thetreatmentandprovidingtheclinicalreasonstotheENT fortheT&A.Theorthodontistsaidhedidn ’tperformthe surgerysohewasn’tobligatedtoinformthepatientofanything.TheENTwastheonewhoperformedtheprocedure andshouldhavebeentheonetoobtaininformedconsent. Thecourtnotedthatmostcourtsdon’tholdareferring physicianresponsibleforobtaininginformedconsentfora procedurethatanotherpractitionerwasgoingtoperform. Afteroutliningsupportingcasesforthisdecision,thecourt
notedthattheorthodontistwasliablebecauseheretaineda degreeofparticipationandcontrolinregardtothesurgeon’ s treatment.Theyheldthataphysicianwhorefersthepatient toanotherphysicianandretainsadegreeofparticipationhas aresponsibilitytoproperlyadvisethepatientaboutthetreatmenttobeperformedbythereferredpractitioner.The referredpractitioner(theENT)shouldalsobeheldliable fornotobtaininginformedconsentwhenorderingaprocedureorparticipatinginthetreatmentorprocedure.
Attheappellatecourtlevel,itwasdecidedthattheorthodontist hadn’tparticipatedinorcontrolledtheT&Aperformedandhad onlyreferredthepatienttotheENTforanevaluation.Even thoughtheorthodontistexpressedconcernoverthepotential forthepatienttodeveloporofacialanddentofacialdeformities asaresultofhermouthbreathing,hehadn’t finalizedatreatment planforthepatient,diagnosedtonsillitisinthepatient,orscheduledorrecommendedthesurgicalprocedure.Itwasalsohis practicetoreferpatientstoanENTforevaluation,andanytreatmentwouldbebasedontheENT’sindependentevaluation.The ENTaf firmedthathewouldnothaveperformedaT&Ajust becauseanorthodontistrequestedit.Thedecisionofthecourt favoredtheorthodontist.
Thebestwaytoensureyouaren’tliableforthenegligentactionsofareferralyoumadeistoclearlystateinthereferral slip,form,orletterthatyouarerequestinganevaluationof theindividual’sspeci ficstructure(s)basedonhavingseenapotentialproblemduringyourexamination.Requestingthatthe referredpractitionercommunicatehisorher findingsandrecommendationstoyouisappropriate.Inthisway,thepatientis freetochoosethespecialistandyoudon’trefertoaspeci fic doctor.
Inthecasewhereyouareinanagencyrelationshipwiththe referredpractitionerorifyouexercisesomedegreeofparticipationorcontrolwithrespecttothetreatmentgivenbythedoctor,youcanpotentiallyopenyourselftolegaljeopardy. Actionsthatareincludedin “somedegreeofparticipation” includediagnosingthepatient,specifyingaproceduretobe done,helpingthepatientobtaininsurancecoverage,being involvedinschedulingtheprocedure,andprovidingpreoperative radiographsorothertestresultstothereferreddoctor.These canplaceyouatriskforlegaltrouble.
Referringapatientcanhavetheselegalpitfalls,butyoualsomust notsimplyignoretheneedtorefer.Somecourtsnotedthat “Whentreatmentisineffective,the[referring]doctormust knowit firstandrecommendotheraction. ” Indeterminingthe actiontotake,thereferringphysicianshouldconsiderthepatient’smental,emotional, financial,andanyotherstatusthat canhaveaneffectontreatment.
Thedutytorefertoanotherpractitionershouldbegovernedby theawarenessthatthepatient’sconditionisbeyondtheoriginal physician’sskills,knowledge,orcapacitytotreatwithalikelihood thattheresultwouldbesuccessful.Thepractitionerwho finds himselforherselfinthispositionshoulddisclosethesituation tothepatientoradvisethepatientthatheorsherequires anothertreatment.
Thereferringdoctoralsohastheobligationtomonitortreatmentgivenbyareferreddoctor.Generalpractitionersstill owethepatientthedutytoobserveandexerciseskillsand knowledgethatwouldbeusedinsimilarsettingsbyothercompetentgeneralpractitioners.
Thepotentialforreferralliabilityexistsbutwisepractitioners canmitigatetheliabilitybyadoptingprudentrequestsfor evaluationbyareferredphysician.Orthodontistsinparticular needtorecognizethatnoteverymalocclusioncanbesuccessfullytreatedorthodonticallyorwithadjunctiveinterdisciplinaryefforts.It’sarelieftoknowthatpractitionersinother dentalspecialtiesorinmedical fieldscanbehelpfulwhenthe needforareferralarises.Takingcaretorequesthelpappropriatelycanminimizeanychanceforlitigationshouldabad outcomeoccur.
JerroldL:Referralliability?Perhaps,perhapsnot. AmJOrthod DentofacOrthop 167:371-374,2025
Reprintsnotavailable
Internationaltravelforlow-costdentalcare,ordentaltourism,is becomingmorecommoninhigh-incomecountriesandfallsinto regionalratherthanglobalcategories.IntheUnitedKingdom, dentaltourismisincreasing,withabout48,000seekingdentistry outsideoftheUKin2014,butabout144,000in2016.Themotivationsfordentaltourismfallintocategoriesbasedonfactors suchasareducedtreatmenttimescale,increasedvarietyintreatmentoptions,thehighcostoftreatment,longwaitinglists,lackof dentalcareavailability,andlackoftrustinNationalHealthService (NHS)dentists.Dentalprofessionalshaveexpressedconcern overpossibleadversehealthconsequencesresultingfromdental tourism.Controversyhasescalatedbasedonnewspaperaccountsofthispublicandprivateissue,soaninvestigationlooked intothekeytopicsorissuesthatarerelatedtodentaltourismin theUKnewsmediaandhowthemediaframesdentaltourism.
Thenewspaperarticleswereidenti fiedusingtheLexisNexis database,thenthe10mostpopularnewspapersintheUK wereusedforthesearchstrategy.Atotalof131articlespublishedfrom2018on(mostin2022and2023)wereevaluated, with92.4%ofthesepublishedintabloidnewspapers,and106 publishedineitherthe TheSun or TheMail.
The5keythemesidenti fiedfromthenewspaperarticleswere pushandpullfactorstoleadtoseekingdentistryabroad; patient-reportedoutcomesandexperiences;warningsfrom dentalprofessionals;amplifyingsocialmediahype;andmedia shamingandstigmatizing.
Whereaspushfactorsleadpeopletoleavetheircountryofresidence,pullfactorsdrawpeopletoanothercountryfordentistry. Pushfactorsincludetheperceptionofhighcostsanddif ficultyaccessingdentalcareintheUK.Thepullfactorsincludecelebrity influence,affordabilityofthetreatment,andself-esteem.
Thesignificantlylowercostofdentalcosmeticproceduresabroad, especiallyinTurkey,comparedtothecostintheUKwasacommontopic.PatientsoftenchosedentistryoutsideoftheUKtosave
moneyanddidn’tconsiderthequalityofthework.Patientsalso citedtheirinabilitytoaccesscarefromNHSdentistsevenafter callingmultipleoffices.Thisleftthemwithfewoptions.
Celebritystatusandtelevisionwereoftenmentioned.Inaddition, personswhohadlowself-esteemorconfidencerelatedtotheir toothappearanceweremotivated,aswellasthoselookingfora quick fixtoimprovetheirappearanceandboosttheirselfconfidence.Itwasnotedthatsomepeoplewithmultiplevulnerabilitiesincludingself-esteemissuesweremoresusceptibleto predatorymarketing.
Manypeoplewhowentabroadtohavedentalworkdonefeltitwas worthittoobtainthecosmeticimprovementstheydesired.Some patientsacceptedthepainofthedentalproceduresasnecessaryto improvetheirconfidence,self-esteem,andself-evaluatedattractiveness.Othershadbadexperiencesanddescribedissuessuch as “deadstumps” andabscessesorpain.Sometimesirreversible harmandongoinganxietyoccurredthatinvolvedthepatient’ s physicalhealth,andexpensiveremedialcarewasrequired.
Patientsalsonotedtheyfeltmisinformedaboutallofthecomponentsofthecosmetictreatments.Bothmentalandphysicalharm wasexperienced,withsomeofthecasesreportedbypeopleon theirsocialmediaplatformstodeterothersfromtakingthesame courseoftreatment.Influencerssometimesdescribedthemselvesasvictimsofpoor-qualitydentalcareandconfusedabout whatprocedurestheyhadconsentedtoreceive.Somesawthemselvesashealthadvocates.Otherswereawareoftherisksand valuedtheimprovedaesthetics.
Thecarereceivedfromsomedentaltourismwassometimesat oddswiththeminimallyinvasivedentistrypracticedintheUK. Thearticlesofferingdentalprofessionals’ perspectivestended tobepaternalisticandgavelittlerecognitiontothestronglymotivatingfactorsthatledpatientstoengageindentaltourism.Dental professionalsunanimouslyagreedthattheUK’sapproacheswere preferredtomaintainhealthandimproveaesthetics.
Patientswhotraveledtoobtaindentalcarewerefacedwithfew regulatoryprocessesandnoaccesstolegalredressorfollow-up
careforanypooroutcomes.RemedialcarewassometimesprovidedbytheNHS,butsomeprivateprovidersactivelyavoided providingcareforpatientswhohaddentistrydoneabroad becausetheyfearedliabilityissues.
Mostnewspaperarticlesusedasinglepostfromsocialmediato frameperspectivesondentaltourism.Oftenthesepostsdocumentedthepatient’sjourney,complications,orenhancedaesthetics.The#TurkeyTeethhashtagwascommonlyusedto identifypeoplewhohaveallbeentosimilarplaces,hadsimilar procedures,underwentsimilarexperiences,andultimately achievedsimilaroutcomes.Theseindividualsusuallyhadstories ofchallenges,disappointments,andadditionalcostsforremedial care.
Socialmediaoftenreportedonsuccessstoriesandwererewardedwithlikesandfollowers,butpotentialcomplications werealsousedtogeneratebuzz.Usingemotionallychargedlanguage,journalistsdescribedthenumberofviewsfromvideos aboutdentaltourismasimmense.Bothpositiveandnegative commentswereusedtoengagereadersandproducestories thatgavemedicalenhancementproceduressignificantheadlines.
Thelanguageusedinmediapostsrangedfromsupportand encouragementtovictimblaming,stereotyping,stigmatizing, andshaming.Peoplewerediscreditedbydescriptionsofunrelatedcharacterlabelsandwerebrutallymockedbyonlinetrolls. Thelanguageusedtendedtoconveyscornoracomicaldismissal ofunpopularfacts.Manyheadlineslabeledpeoplewithanimal namesorridiculedtheappearanceoftheirteeth.
Somepatientswhohadfull-mouthtransformationsreceived praisefromrespondents,butotherssawthesameworkas distastefulorsomethingtobeavoided.Influencerswerewarned thattheywouldlivetoregrettheirchoices.Peoplewereoften referredtoasvain,fake-looking,orfoolishfornotchoosingto haveaminimallyinvasiveproceduredone.
Youngerpeopleandsocialmediausersseedentaltourismasa waytoimprovetheirappearancewithoutexcessivecosts,access dentalcarethatwasn’totherwiseavailable,andachievetheir goalsregardingaesthetics.Oftensocialmediatrendsin fluence theirchoicesandcanleadtosomenegativeandsomepositive outcomes.Mostofthedentalcareprovidedabroaddoesn’t conformtotheminimallyinvasivemodelusedinmoretraditional dentalof fices.
Journalisticdescriptionsofpeoplewhohaveundertakendentaltourismtogetcosmeticchangestotheir dentitioncanserveasinfluencesonotherstofollowor notfollowthesamepath.Theresultsofdentaltourism canbesuccessfulorunsuccessful,enhancingtothe patient’sfaceorproblematic,andatriumphora cautionarytale.Oftentheshort-termandlong-term risksassociatedwithaggressivecosmeticprocedures areunderplayed,butsomepatientssharepoorresults inmediapoststodiscourageothersfromfollowingin theirfootsteps.TheUKdentalprofessionstronglyadvocatesforminimallyinvasivedentalapproachesand evendiscouragestreatmentto fixproblemscausedby dentistryabroad.Themediahasnotalwayspresented anunbiaseddescriptionoftheprocess,whichcan alsoinfluencetheuseoravoidanceofdentaltourism.
DoughtyJ,MooreD,EllisM,etal:Contemporarydentaltourism: AreviewofreportingintheUKnewsmedia. BrDentJ 238:230-237,2025
Reprintsavailablefrom JDoughty,SchoolofDentistry,Univof Liverpool,UK;e-mail: janineyd@liverpool.ac.uk
Misconductindentistryisofconcern,withthequalityofpatient caredependingonadherencetothestandardsofpracticesetfor dentists.Cliniciansshouldbecomemorecarefulintheirprofessionalgrowthandconsiderwhatactionscanleadtodisciplinary actionsbythedentalboard.Thisincludesenhancingthedentist’ s ethicalawareness,professionalconduct,riskmanagement,
patient-centeredcare,professionaldevelopment,andpeer accountability.Beingawareoftheprofessionalstandardsand theconsequencesthatcanbeimposedshoulddeterdentalprofessionalsfromunethicalornegligentpractices,whichshould resultinincreasedpatienttrustandsafety.TheTexasStateBoard ofDentalExaminers(TSBDE)regulatesdentistsinTexas,prescribingdisciplinaryactiontothosewhoviolaterulesand
Figure1. DisciplinaryactiondistributionfromJanuary2000throughJuly 2016.Mostinfractionswereduetofailuretoobtainormaintainadequate dentalrecordsinaccordancewiththeTexasStateBoardofDentalExaminers.(CourtesyofHuangY-W,DowlatshahiS,AyilavarapuS,etal:An analysisofdentalboarddisciplinaryactionamonggeneraldentistsin Texas. JAmDentAssoc 156:225-233,2025.)
guidelines.Theseactionsincludeanagreedsettlementorderora hearingandsubsequentorderoftheboard.Thedisciplinaryactionsarepublicinformation.AreviewoftheTSBDEdisciplinary actiondatawasdonetoidentifyviolationsthatresultedindisciplinaryactions,withthegoalofhelpingpractitionersbeawareof theproblemareasandavoidfutureviolations.
TheelectronicsearchoftheTSBDEwebsitecoveringtheperiod fromJanuary2000throughJuly2016identi fied1056dentists whofaceddisciplinaryaction.Becausesomehadmultipleviolations,thetotalwas1707infractions.Thereviewofthedatarevealedrecurrentpatternsandthemes,withthemajor categoriesofinfractionsbeingdiagnosis,treatment,renewals,recordkeeping,andethicsandprofessionalism.
Thirty-ninepercentoftheinfractionsinvolvedinadequaterecordkeeping,23%inadequatetreatment,23%lackofethicsand professionalism,9%improperdiagnosis,and6%issueswithrenewals(Figure1).
Periodontics,operativedentistry,andprosthodonticswere theprimaryareaswheredisc iplinaryactionswereneeded andaccountedforabout30%each.Pediatricdentistry had12%,endodontics11%,oralsurgery7%,andorthodontics 5%.
Nearlyhalfofthetreatmentinfractionswerenotedinoperative dentistryandprosthodontics.Twenty-twopercentoccurredin
Figure3. Disciplinaryactionsbasedontreatmentinthecategoriesshown. Thenotapplicablegroupincludescasesthatcouldnotbeclearlyplacedin othermentionedcategories.(CourtesyofHuangY-W,DowlatshahiS, AyilavarapuS,etal:Ananalysisofdentalboarddisciplinaryactionamong generaldentistsinTexas. JAmDentAssoc 156:225-233,2025.)
endodontics,9%inoralsurgery,7%inperiodontics,and7%inpediatricdentistry,withorthodonticsonlyinvolvedin4%(Figure3).
Sixpercentoftherenewalsinvolveddentallicensesorpracticing withanexpiredlicense,failuretorenewaControlledSubstances Registration(CSR)certi ficatewiththeTexasDepartmentofPublicSafety(DPS)ortheDrugEnforcementAdministration(DEA), andprescribingcontrolledsubstanceswithanexpiredCSRcertificate.Seventy-onepercentoftherenewalsinvolveddentallicenses.Twenty-sixpercentwererelatedtoafailuretorenew orprescribingacontrolledsubstancewithanexpiredCSRcertificatefromtheTexasDPS.Just3%wererelatedtoafailureto reneworusinganexpiredCSRcerti ficatewithaDEAlicense toprescribeacontrolledsubstance.
Thirty-ninepercentofthecasesinvolvedissuesrelatedtoinadequateorimproperdocumentation.Failuretoobtainappropriate informedconsent(18%),omissionofapropertreatmentplan (16%),failuretoobtainanddocumentthepatient’svitalsigns (15%),lapsesinmaintainingrecordsofthetreatmentplanadministered(14%),lapsesinrecordingdiagnostic findings(9%),deficientcaptureoforupdatestomedicalhistory(8%),lackof periodontalcharting(6%),andnotobtainingappropriateradiographs(6%)allfellintothiscategory(Figure5).
Twenty-threepercentofallinfractionsinvolvedethicsandprofessionalism.Twenty-sixpercentwererelatedtoprescriptionerrors,whichrangedfromself-prescribingcontrolledsubstances fornon-dentalpurposestoattemptingtousethecredentialsof anotherprovidertoprescribecontrolledsubstancesfornon-
Figure5. Disciplinaryactionsbasedonrecordkeeping.Thenotapplicable groupincludescasesthatcouldnotbeplacedintheothermentioned categories.(CourtesyofHuangY-W,DowlatshahiS,AyilavarapuS,etal: Ananalysisofdentalboarddisciplinaryactionamonggeneraldentistsin Texas. JAmDentAssoc 156:225-233,2025.)
dentalpurposes.Twenty-threepercentoftheinfractionswere relatedtoimproperpersonalconduct.Theseinfractionsincluded improperlyobtained,used,ordistributedhabit-formingdrugs; drivingwhileintoxicated;assaultandcriminalconviction; consumingnitrousoxidefornon-dentalpurposes;possessing childpornography;falsifyingtestimonyunderoath;andattemptedsexualassault.
OtherinfractionsinvolvedfailuretoadheretotheTexasAdministrativeCodeguidelinesfordiscontinuingpatientcare(6%), improperbillingpractices(15%),andunauthorizeddelegation (10%).Improperbillingincludedbillingforservicesnotprovided, billingthepatientfortreatmentcodesnotcompletedordocumented,andbillingtheMedicaidprogramforservicesthat wereimproper,unreasonable,orclinicallyunnecessary.
Areasofconcernindentalpracticethatrequireattentionand interventionincludeddiagnosis,treatment,renewals,recordkeeping,andethicsandprofessionalism.Ineachcasetheinfractionscouldbeevaluatedtodetermineabetterwaytoproceed andavoidhavinginfractionsoftheguidelines.
Analysisofthereportedinfractionsallowedforan identificationofareaswhereinterventionsareneeded. Examplesincludethefollowing:
Fordiagnosticinfractions,dentistsmaybenefitfromaheightened senseofdiligenceandadherencetodiagnosticprotocols,with targetedinterventionssuchascontinuingeducationprograms focusedondiagnosticaccuracypossiblyofferingbenefitsto avoidinginfractions.
Treatment-relatedissueswereoftenseenwithyoungdentistswho arebusyandhaven’thadtheadvantagesofcontinuingeducation. Theymaylacktheclinicalskillsorfailtoappreciatetheimportance ofadheringtotreatmentstandards,whichmightbeaddressed throughenhancedtraining,peerreviews,andstricterenforcement ofclinicalguidelines.
Maintainingcurrentprofessionalcredentialsandensuringcompliancewithrenewalrequirementswouldhelpwithrenewalissues. Sendingouttimelyremindersmaybeamitigatingapproach. Theimportanceofmaintainingcomprehensiveandaccurate dentalrecordsmustberecognized.Specificdeficienciesthat werefoundinvolvedafailuretoobtaininformedconsent,alapse indocumentingtreatmentplansandvitalsigns,andomissions inupdatingmedicalhistoriesandperiodontalcharting.Dentalstaff maybenefitfromongoingeducationandtraininginproperdocumentationpracticessothattheregulatorystandardsaremetand patientcareremainssafe.
Prescriptionerrorsindicateaneedformorestringentcontrolsand oversightintheprescribingprocess.Improperbillingprocedures showthattheofficemustadopttransparencyandethicalconduct in financialtransactions.
Alloftheseareasneedtobeaddressedforthenumber andseriousnessofdentalpracticeinfractionstobe reduced.Thisstudyfocusedonasinglestate,so largerstudieswithmultiplestatesandspecialties shouldbeundertaken.
HuangY-W,DowlatshahiS,AyilavarapuS,etal:Ananalysisof dentalboarddisciplinaryactionamonggeneraldentistsinTexas. JAmDentAssoc 156:225-233,2025
Reprintsavailablefrom SEswaran,DeptofPeriodonticsand DentalHygiene,SchoolofDentistry,UnivofTexasHealthScienceCtratHouston,7500CambridgeSt,Suite6421,Houston, TX77054;e-mail: sridhar.veerkeralam.esw@uth.tmc.edu
Professionalguidelinescallingformoreattentiontoprenataloral healthwerepublishedin2013andendorsedbytheAmerican DentalAssociation,yettheratesofprenataloralhealthcarein theUnitedStatesremainlowandhaven’tgrown,withfewer thanhalfofUSpregnantwomenreceivingdentalprophylaxis. Thefactorscontributingtothissituationwereevaluated.
Pregnancyisknowntoincreasetheriskofdevelopingdentaldiseases,soprenataloralhealthcareshouldbeseenasessentialto theoralandgeneralhealthofpregnantwomenandtheirchildren. Deliveringperinataldentalcareduringpregnancyissafe,whereas notprovidingoralhealthcareprenatallyincreasestherisksofdiseaseforthepregnantwomanaswellasherchild.Pregnancyisa timeofincreasedneedfordentalcare,yetwomenfromracialand ethnicminoritiesandthoseinsuredbyMedicaidhavehigherrates ofcariesandperiodontaldisease,aremorelikelytoenterpregnancywithdentalproblems,andyetreceiveprenataloralcareat lowerratesthanotherwomen.Oftenlow-incomewomenare onlyabletouseMedicaiddentalbene fitswhentheyarepregnant orhavedeliveredachild.Thismakespregnancyanopportunity toaccessoralhealthcare.
Besidestheinfluencesoflowincome,minoritystatus,andinsuranceonlythroughMedicaid,pregnantwomenmayhave pregnancy-relatedcomorbidconditions.Thisincludesgestational diabetesandpre-eclampsia.Womenwiththeseconditionsshould nothavelowerratesofprenataloralhealthcarethanthosewithout theseconditions.Thecommoncomorbidconditionsraisetherisk ofhavingadifficultpregnancyandpoorbirthoutcomes,butthey alsoincreasetheriskofdevelopingoraldiseases.Thewomen whohavecomorbidconditionsarethepeoplewhoshouldreceive increased,notdecreased,attention.Oralhealthcaredeliveredto themwouldimprovetheoralandgeneralhealthofthesevulnerable individuals.
Otherbarrierstoprenataloralhealthcareincludelimitedaccesstodentalcarebuthighratesofcaries,gingivitis,andperiodontaldisease.Thisbarriermaybeovercomebyintegrating oralhealthscreeningsandrefer ralsintomedicalprenatalcare. Psychosocialandsociobehavioralfactorscaninteractwith oralhealthandoralhealthcare,possiblyidentifyingthosewho areatincreasedriskfordevelopingoraldiseasesiftheydon’t receiveprenatalcare.
Overcomingpatient-levelandprovider-levelbarrierstoprenatal oralhealthcarecanbechallenging.Womenwhosepregnancies arecomplicatedfaceincreasedcostsandmoretimeconstraints becauseofmorefrequentrequiredmedicalvisits,whichtheircohortswhohavenon-complicatedpregnanciesdon’tface.Ifthese womenprioritizetheirmedicalvisits,theymayminimizethe importanceoforalhealth.Thosepractitionerswhoprovideprenatalmedicalcaremaynothavethetimeorfreedomtoaddressthe woman ’soralhealthneeds.Inaddition,prenatalanddentalcare providersmaynotbeawareofthelinksbetweencomorbidconditionsandprenataloralhealthormaynotrecognizethatoral health relateddiseaseentitiesareapotentialareawherethey couldintervenetoimprovethewoman’sgeneralandoralhealth.
Somedentistsarereluctanttodeliveroralhealthcareprenatally. Someofthismaybetheresultofoutdatedconceptsbeingtaughtin dentalschool,suchasbelievingthatcertaintreatmentsmustbe restrictedtospecificpregnancyperiodsorthatdentalradiographs cannotbeobtainedinpregnantwomen.Somemayfeartherewill beariskforliabilityiftheytreatpregnantwomen.Today’sguidelinesspecificallystatethatprenataloralhealthcareisasafeand importantpartofprenatalcare.Withourgreaterawarenessof theacuterisksforthepregnantwomanandherchildrelatedto infection,dentistswhofailtoprovideneededandtimelyoral healthcaremaybetheoneswhowouldbeatriskforliability.
Oralhealthcareandprenatalcareprovidersmustpromoteoral healthduringpregnancyforallpregnantwomenwhoneedthese interventions.Forprenatalcareproviders,oralhealthscreening questionsshouldbeintegratedintotheoralhealthscreening questionnairetoidentifythewoman’soralhealthcareneeds. Performingoralhealthscreeningsandreferralsshouldbea partofprenatalhealthcare.It’sjustasimportantassmoking cessation,nutritionalcounseling,andHIVtesting.
Dentalcareprofessionalsshouldunderstandthatprenatalpatients needtohavepreventive,emergency,androutineoralhealthcare throughouttheirpregnancies.Theymaybenefitfromattending continuingeducationofferingsonpregnancyandoralhealthto ensuretheyhavethemostcurrentinformation.
Havinganoralhealthcarereferralsysteminahospitalormedical systemorbetweenamedicalanddentalofficecouldprovideevaluationsformorepregnantwomenandensurethattheyreceive oralhealthcare.Thecontinuedcareofthewomanandchild couldthenextendbeyondtheperinatalperiod,ensuringapool
ofpatientsfordentalcareproviders.Havingdentalandmedical electronicrecordintegrationandotherjointapproachesto carewouldacceleratethecaredelivered.
Dentistsneedtorecognizethatpregnancyoffersa windowofopportunitywhereoralhealthcarecanbe deliveredtothepregnantwomanandtoheroffspring. Oraldiseasesinapregnantwomencauseunnecessarypainand,ifleftuntreated,canintroducerisk factorsthatwillextendbeyondthepregnancy.When oralhealthcareisdeliveredduringthepregnancy andtheperinatalperiod,ithasthepotentialtobreak thecycleofpoororalhealththatcanpersist throughoutgenerationsinsomefamilies.
RussellSL,HuangSS,BirdC,etal:Addressingchallengesof prenataloralhealthcare. JAmDentAssoc 156:177-179,2025
Reprintsavailablefrom SLRussell,DeptofPediatricDentistryand CommunityHealth,RutgersSchoolofDentalMedicine,110BergenSt,Newark,NJ07103;e-mail: stefanie.russell@rutgers.edu
Makingdecisionsisadailytaskinthepracticeofdentistry,butthis isacomplexprocedurerequiringtheapplicationofclinicaland biomedicalknowledge,clinicalskills,problem-solving,and considerationofprobabilitiesofsuccessforthevariousoptions. Manyoptionsmustbeweighedtoeitheravoidorfallintocompliancewithvariousstandards.Theclinician’sexperienceandskills mustalsobebalancedwiththepatient’spreferencesandsocial status.Anonlinequestionnairewasdevelopedtodetermine thefactorsthatin fluencedentists’ approachestothetreatment ofirreversiblepulpitisinmaturepermanentteeth.
The17-questioninstrumentwasdistributedtoagroupofdental practitioners,withabout37%fromtheUniversityofQueensland,about33%fromotherAustralianuniversities,andabout 30%fromoutsideAustralia.Abouttwothirdsoftheparticipants workedintheprivatesector,withtheremainderpracticinginurbanareas.Atotalof262participantscompletedthesurvey. Approximately83%hadmorethan5yearsofexperienceand abouttwothirdsweregeneraldentists.
Theresultswereevaluatedaspractitioners’ opinions,in fluencing factorsforclinicaldecisions,andresponsestoacasescenario.
Mostpractitionerschoseextractionasthemostsuccessfulmanagementoption,followedbyrootcanaltreatment(RCT).Vital pulptherapy(VPT)wasrankedaslesssuccessful,withpulpotomy asthethirdmostsuccessfuloption,directpulpcappingasthe fourth,andindirectpulpcappingasthelast.Menandwomen differedintheirchoices,withmorewomenrankingdirectpulp cappingassuccessfulthanotherparticipants,andmensignificantlypreferringextraction.
Ageofthepractitioneralsoin fluencedthechoiceoftreatment. Thoseage25to35yearsconsistentlychoseextractionasthe mostsuccessfultreatmentcomparedtoolderparticipants.Asignificantdifferencewasnotedbetweenthe25and35agegroup andthoseoverage55years,withyoungerpractitionersfavoring extraction.Thoseage45to55yearsrankedpulpotomyasaless successfultreatmentmorethananyotheragegroup.
Experiencealsosigni ficantlyin fluencedtreatmentpreference. Thosewith1to5yearsofexperiencechoseextractionasthe mostsuccessfultreatment,withsignifi cantdifferencesbetween thisgroupandthosewithmorethan20yearsor11to15years.
PractitionersworkingintheprivatesectorsawRCTasmoresuccessfulthanthoseworkinginpublicorhospitalsectors.Graduates fromoutsideAustraliarankedpulpotomyasmoresuccessfulthan Australiangraduates.Inaddition,practitionersfromoutside AustraliafavoredextractionlessoftenthantheirAustralian counterparts.
PractitionerswerealsoaskedhowoftentheyperformedVPT, RCT,andtoothextractionforirreversiblepulpitis.Theprocedureperformedmostoftenwasextraction,withabout23%performingmorethan1extractionperweek.About13%of practitionersperformedRCTmorethanonceaweek.VPT wascarriedoutlessthanonceamonthbyabout71%ofthesurveyrespondents.
Participantswereallowedtogivemultipleanswerstoaquestion aboutbarriersthatpreventthemfromchoosingVPTforirreversiblepulpitisinapermanentmaturetooth.VPTwasconsideredinappropriateforachievinglong-termtreatmentresultsbymorethan 29%oftheparticipants.About22%to23%oftherespondents feltlackofknowledge,lackofaccesstomaterials,lackoftraining, andlackofconfidencewerebarrierstodoingVPT.Otherbarriers werepatientfactorssuchasage,preference,compliance,livingin ruralorremoteareas,medicalissues,socioeconomicstatus,and choiceofaspecifictreatment.Workplacerestrictionsonendodontictreatment,universitytraining,existingknowledge,uncontrolled pulpalbleeding,case-dependentfactors,cost-effectiveness,lackofa microscope,andconcernsoverlongevitywerealsoseenas barriers.
Patientpreferencewasthemostcommonlycitedreason(about 29%)formakingatreatmentdecision.Otherpatientfactorswere age,socioeconomicstatus,patient’seducationallevel,oralhygieneanddentitionstatus,motivationorcomplianceexpectations,preference,medicalconsiderations,demographics,and accesstodentalcare.
Theparticipantscitedvariousotherinfluences,includingthe dentist-patientrelationship,publicrestrictionsonRCT,costof MTA,preferenceofthereferringdentist,skillsandtrainingof thedentist,accesstomagnification,andtimeavailability.Dentists alsoconsideredtherestorabilityofthetooth,thelocationofthe tooth,whetherthereisanopenapex,severityofthecondition, anddurationofsymptoms.
Severalclinicalfactorswereidenti fied,with91%oftheparticipantsconsideringtherestorabilityofthetoothasthemainfactor. Periodontalstatus,radiographicstatus,presenceofspontaneous pain,andavailabilityofmagnificationwerealsocited.Participants mentionedpatientmotivation,compliance,andpreference;oral

Figure4. Illustrationofpercentageoftreatmentoptionsselectedby practitionersforthecasescenario:A27-year-oldpatientpresentsa cold-sensitivetooth45slightlytendertopercussionwithspontaneous pain.(CourtesyofAlfaisalY,IdrisG,PetersOA,etal:Factorsin fl uencing treatmentdecisionsinpermanentmatureteethwithirreversiblepulpitis: Aquestionnaire-basedstudy. AustralDentJ 69:293-303,2024.)
hygienestatus;publicguidelines;timeanddentist’sskills;access tomaterials;rootanatomy,toothmobility,andabilitytoplace adentaldam;aestheticsandfunction;persistentpain;statusas anabutmenttooth;previousdeeprestoration;pulpbleeding; cracksorfractures;andorthodonticconcerns.
Forty- fivepercentofthepractitionersselectedRCTasthebest treatmentfortheclinicalscenario(Figure4),followedbyindirect pulpcapping(about23%)andpulpotomy(about17%).Theleast selectedoptionwasextraction,withjust6%choosingthis approach.Approximately12%choseotheroptions,including restoreandreassessandchoicesbasedonthepatient’slocation, pulpexposure,orpatientpreferences.
Directpulpcappingwasselecteddependingonthepractitioner’ s placeofgraduation.ThosefromtheUniversityofQueensland tendedtochoosedirectpulpcappinglessoftenthanthosefrom otherAustralianuniversitiesandchoseitmuchlessoftenthan thosefromuniversitiesoutsideofAustralia.Generaldentists weremorelikelytochooseindirectpulpcappingthanpostgraduate studentsorspecialtydentists.Thespecialiststendedtochoosepulpotomy,whichgeneraldentistspreferredlessoften.Urbandentists weresignificantlylesslikelytochooseextractionthanthoseworkinginotherareas.
Theparticipantschoseextractionasthemostsuccessfultreatmentforirreversiblepulpitis.ThiswasfollowedbyRCT,then VPT.Manyfactorsin fluencedthedentists’ decisions,including thoserelatedtogender,age,yearsofexperienceasadentist,patient’spreferences,location,theuniversityfromwhichthe dentistgraduated,andguidelinesoftheplacewherethedentist practiced.
ClinicalSignificance
Manyfactorsinfluenceddentists’ decisions,butoverall, VPTwasnotacommonpracticeamongAustraliandentists.VPThasbeenshowntobeanefficient,minimally invasive,predictable,andcost-effectivealternativeto conventionalRCT,butthereseemstobeagapbetween theevidence-baseddataandclinicalpractice.VPTmay bechosenmoreofteniftheteachingofthisapproach wereincreasedinthedentalcurriculumandifhandsoncontinuingprofessionalcoursesweredeveloped.
AlfaisalY,IdrisG,PetersOA,etal:Factorsinfluencingtreatment decisionsinpermanentmatureteethwithirreversiblepulpitis:A questionnaire-basedstudy. AustralDentJ 69:293-303,2024
Reprintsavailablefrom CIPeters,SchoolofDentistry,TheUnivof Queensland,Rm7114,Level7,OralHealthCtr,288HerstonRd, Brisbane,Qld4006,Australia;e-mail: c.peters@uq.edu.au
The fi rstpermanentmolar(FPM)isespeciallysusceptibleto dentaldecaybecauseofitsfunctionalandmorphologicalcharacteristicsandhasthehighestincidenceofdentalcaries.Therefore, anycariouslesionsareaddressedintheirearlystages.Removalof adeepcariouslesionsfromtheFPMriskspulpexposureandmay
requirerootcanaltherapy.Indirectpulpcapping(IPC)isdoneto preservepulpvitalityandavoidirreversiblepulpalterations.IPC isminimallyinvasive,requireslesstime,andislessexpensive comparedtoconventionaltreatments.Thematerialsusedin IPCshouldideallyoffergoodadhesion,sealing,anddimensional stability,whilelackingsolubility,resorbability,andtoxicor

Figure3. RepresentativecaseofGROUP1(SDF)showingclinicalphotographsandradiographs. A-G, Clinicalphotographs(A, preoperative; B, preoperative withrubberdam; C, immediatepostoperative; D, 3months; E, 6months; F, 9months; G, 12months). H-K, Radiographs(H, preoperative; I, immediate postoperative; J, 6months; K, 12months).(CourtesyofZaghloulMAA,ElSayedMA,Al-GawadRYA,etal:Clinicalandradiographicevaluationofsilver diamine fluorideversusmineraltrioxideaggregateasindirectpulpcappingagentsindeeplycarious firstpermanentmolars:Arandomizedclinicaltrial. BDJ Open 11:4,2025.)

Figure4. RepresentativecaseofGROUP2(MTA)showingclinicalphotographsandradiographs. A-G, Clinicalphotographs(A, preoperative; B, preoperative withrubberdam; C, immediatepostoperative; D, 3months; E, 6months; F, 9months; G, 12months). H-K, Radiographs(H, preoperative; I, immediate postoperative; J, 6months; K, 12months).(CourtesyofZaghloulMAA,ElSayedMA,Al-GawadRYA,etal:Clinicalandradiographicevaluationofsilver diamine fluorideversusmineraltrioxideaggregateasindirectpulpcappingagentsindeeplycarious firstpermanentmolars:Arandomizedclinicaltrial. BDJ Open 11:4,2025.)
carcinogenicqualities.Theymustberadiopaque,biocompatible, andhavebioactivity.Noneoftheavailablechoiceshaveallthese qualities.Althoughcalciumhydroxide(CaOH)wasusedfor years,concernshavepromptedthedevelopmentofabettermaterial,mineraltrioxideaggregate(MTA),whichisnowthegold standardforIPC.Itsdrawbacksarehighcost,dif ficultymanipulatingit,andlongsettingtime.Silverdiamine fluoride(SDF), whichisusedtoarrestcariouslesionsinprimaryteeth,has beensuggestedasanoptionforIPC,offeringsilver’santibacterial propertiesand fluoride’sremineralizingpotential.Inaddition, SDFinhibitstheproteolyticenzymesresponsibleforprotein degradationandblocksdentinaltubules,makingitadesensitizing agent.WiththelackofavailableresearchonusingSDFinIPC,a randomizedclinicaltrialwasdonetomeasuretheclinicaland radiographicsuccessofIPCovera1-yearperiodforMTAand SDF.
Thirty firstpermanentmolarswererandomlyassignedto receiveIPCwithSDForMTA.Thirteenboysand17girls (age9to14years,meanage10.75years)wererandomly dividedinto2groupsof15participantseach.Thesingle-step IPCtechniquewasperformed.Theclinicaloutcomeswere measuredatbaselineandafter3,6,9,and12months;radiographswereobtainedatbaselineandafter6and12months; andpostoperativepainwasrecordedonce.Successrate, radiographicsuccessrate,anddentinbridgethicknesswere comparedbetweenthe2groups.
BoththeSDF(Figure3)andtheMTA(Figure4)groupshad100% clinicalsuccessafter12months.Noriskforswelling,sinus,or fistulaorevidenceofthesewasdetected.
Bothgroupsalsodemonstrated100%radiographicsuccessafter 12months.Dentinbridgethicknesswassignificantlyincreasedafter12monthsinbothgroups,withnostatisticallysigni ficant differencebetweenthegroups.
SDFandMTAprovidedsimilarhighsuccessratesinpermanent teethrequiringIPC.Nodifferencesinclinicalorradiographic outcomeswerenoted.
SDFappearsabletoprovideanalternativetoMTAfor IPCinpermanentmolars.Thedentalpulptissues demonstratednoadverseeffectsforupto12months whenSDFwasused.
ZaghloulMAA,ElSayedMA,Al-GawadRYA,etal:Clinicaland radiographicevaluationofsilverdiamine fluorideversusmineral
trioxideaggregateasindirectpulpcappingagentsindeeply carious firstpermanentmolars:Arandomizedclinicaltrial. BDJ Open 11:4,2025
Reprintsavailablefrom MAAZaghloul,PediatricDentistryand DentalPublicHealth,FacultyofDentistry,CairoUniv,Giza, Egypt;e-mail: marwa_zaghloul@dentistry.cu.edu.eg
Earlychildhoodcaries(ECC)isdiagnosedforchildrenyounger thanage6yearswhohave1ormoredecayed,missing,or filled surfacesinprimaryteeth.Asevereform(S-ECC)includesany signofsmoothsurfacetoothcariesinchildrenyoungerthan 3years;1ormorecavitated,missing,or filledsmoothsurfaces inprimarymaxillaryanteriorteethinchildrenage3to5years; andadecayed,missing,or filledscoreof4ormoresurfacesfor childrenage3years,5ormoresurfacesforchildrenage4years, or6ormoresurfacesforchildrenage5years.Vitalpulptherapy (VPT)isaminimallyinvasive,conservative,andmoreprognosticallysuccessfulstrategyforprotectingpulpvitality.Indirectpulp capping(IDPC)isoneVPTapproachthatisusedforteethwith deepcariouslesionsapproximatingthepulpbutnotexhibiting irreversiblepulpitisorperiapicaldisease.InIDPC,thelesionis partiallyremoved,butleftinplacenearthepulptoavoidexposing it.Alayerofbiocompatiblematerialsealsoffthecavitybase,with laterrestorationofthecavitytodecreasethelevelofbacterial exposureandarrestthecaries,remineralizethedentin,andsupportpulpvitality.IDPChasreducedtechniquesensitivity,ismore costeffective,islessdestructive,andisassociatedwithhigher levelsofpatientacceptancethanothertreatments.Itssuccess rateinprimaryteethisatleast90%anddoesn’tdecreasesignificantlywithtime.Itisthereforethepreferredapproachforpreservingtoothpulpindeepcariessituations.Anevaluationwasdone ofthesurvivalrateofIDPCinchildrenwithS-ECCoveralong periodoffollow-up,withtheaddedgoalofindicatingpotential riskfactorsthatcaninfl uencetreatmentoutcome.
Themedicalrecordsof352children(186boysand166girls,mean age3.51years)withS-ECCin1197teethwereevaluated
Table1. TheResultofSurvivalRates
retrospectively.Sixhundredforty-nineteethwerelocatedanteriorlyand548wereinposteriorareas.AllreceivedIDPCwiththe childunderdentalgeneralanesthesia(DGA)betweenJanuary 2015andDecember2020.Evaluationsweredoneimmediately postoperativelyandafter6,12,18,24,30,36,42,and48months. Follow-uplastedamedianof19.75months,withthelongest periodbeing5.23years.
Forty-sevenchildrenhad67teeththatfailedtosurvive,with31 locatedanteriorlyand25posteriorly.Timetofailureaveraged 15.80months.
Survivalrateat6monthswas99.4%(Table1 and Figure3).After 48monthsthesurvivalwas82.3%.
Just2factorsweresignificantlydifferentbetweentheteeth thatsurvivedandthosethatdidnot.Tootharchposition andwhethercariesaffectedthemesialproximalsurfaceexertedsigni ficanteffectsonthesurvivalrateofIDPCinmultivariateanalysis.TheriskofIDPCprimarytoothtreatment failureinmandibularteethwas2.35timesgreaterthanthat ofmaxillaryteeth.Thefailureriskofalesionwithamesialsurfacewas2.76timeshigherthanthatofacavityinatoothlackinginvolvementofthemesialsurface.
IDPCwasshowntoachievehighsurvivaldataasatreatmentfor S-ECC.Havingthesurvivalratesremainhighforupto4years
Follow-uptimepoint(month) 612182430364248
Allincludedteeth99.497.695.493.691.288.186.482.3
Survivalrate(%)Toothlocation
Anteriorteeth99.397.294.794.092.389.985.895.8 Posteriorteeth99.497.796.393.290.286.386.379.6
(CourtesyofDaiS-S,HeS-Y,WangP-X,etal:Survivalanalysisandriskfactorsofindirectpulpcappinginchildrenwithsevereearlychildhood caries:Aretrospectivestudy. BrDentJ 238:51-56,2025.)


Figure3. Survivalcurveofallteeth(n=1197).Thesurvivalratesat6months,12months,18months,24months,30months,36months,42months,and 38monthswere99.4%,97.6%,95.4%,93.6%,91.2%,88.1%,86.4%,and82.3%,respectively.(CourtesyofDaiS-S,HeS-Y,WangP-X,etal:Survival analysisandriskfactorsofindirectpulpcappinginchildrenwithsevereearlychildhoodcaries:Aretrospectivestudy. BrDentJ 238:51-56,2025.)
indicatedthatIDPCcansuccessfullystopcariesprogression, avoidvitalpulpexposure,andrestoretoothfunction.
TheAmericanAcademyofPediatricDentistryhasrecommendedIDPCasthepreferredtreatmentformanagingdeepcariesinprimaryteeth.Morehigh-quality clinicalrandomizedtrialsofthismethodshouldbe donetobuilduptheevidence-basedfoundationfor IDPC.Furtherclari ficationoftheroleoftootharchpositionandmesialsurfaceinvolvementincariouslesions,whichwerefoundinthisstudytoinfluencethe IDPCoutcome,wouldbehelpful.
DaiS-S,HeS-Y,WangP-X,etal:Survivalanalysisandriskfactors ofindirectpulpcappinginchildrenwithsevereearlychildhood caries:Aretrospectivestudy. BrDentJ 238:51-56,2025
Reprintsavailablefrom FLiu,KeyLaboratoryofShaanxiProvince forCraniofacialPrecisionMedicalResearch,CollegeofStomatology,Xi’anJiaotongUniv,Xi’an,P.R.China;e-mail: liufei6630@gmail.xjtu.edu.cn
Communitywater fluoridation(CWF)effortstopreventdental cariesarenowbeingmetwithchallengestoprovethat fluoride addedtothewateractuallyofferssignificantbene fitsinterms ofcariesreduction.Amongtheelementsthatmustbeevaluated arepopulationburdenofdisease,oralhealthbehaviors,diet,and theavailabilityanduseofothercaries-preventionefforts.Thehistorical findingsoftheCochranereviewandthe findingsofmore
recentstudiesmustbeconsideredwhenCWFschemesare proposed.
Studiesdonein1975orbeforeconsistentlyshowthatCWFoffersaclearandsigni ficantpreventiveeffectontoothdecayinchildren.TheCochranereviewincludeddatafromprospective studiesandcontrolsthatcompared fluoridatedandnonfluoridatedcommunities.Theseolderstudiesfoundsigni ficant evidencethatwater fluoridationreducedtheincidenceofdental cariesandincreasedtheproportionofcaries-freechildren.
TheCochranereviewdoesn’tprovideevidencesufficientto informdecisionmakersontheimpactofremovinganexisting CWFintervention.Italsodoesn’tprovideevidencethatCWF changesthedisparitiesincariesrelatedtosocioeconomicstatus. Harmsweren’tsystematicallyassessedintheCochranereview, sonoconclusiveevidencewasgivenindicatingtheassociationbetweenoptimalCWFandotherhealthconditions.
Morerecentstudiesmustconsidertheeffectofadopting fluoride intoothpaste,whichappearstoreducethemagnitudeoftheeffectofCWF.Morecontemporarystudiesindicatethatinitiating CWFmayresultinslightlyfewerdecayed,missing,and filled (dmft)primaryteethovertime.Thedifferenceindmftisabout aquarterofatoothinfavorofCWF.Thereisgreatuncertainty aboutwhetheradding fluoridetowaterreducestoothdecayin permanentteethinchildren.
Theobservedbene fitsofCWFhavebeenreducedovertime,so theinitiationof fluoridationcannotbeginwithoutacarefulevaluationofcostsandhowtheschemewouldbeimplemented.Potentialharmsandbene fitsmustbeevaluated,alongwiththe economicaspectsoftheundertaking.IfCWFisdeterminedto
beanappropriateinterventionandisimplemented,itmustbe carefullymonitoredtoensurethatthedeliveryof fluorideisat aconsistentleveltoensureoptimalhealthoutcomes.Water companydatatendtoshowthatinconsistentconcentrationsof fluorideareaddedtothewater,soitcan’tbeassumedthatthe populationslivinginCWFareasactuallyreceiveoptimally fluoridatedwater.Thesituationshouldbecloselymonitoredtoguide effortstopreventvariationsandensureoptimalpotential bene fits.
TheoriginalCWFstudiesindicatedasignificantbene fitfrom fluoridationintermsofpreventingtoothdecay.Today,most toothpastescontain fluoride,sotheeffectofCWFisreduced. Newerstudiesindicatethisreductionanddon’tshowthe fluoridehavinganyimpactonthehighercarieslevelsfoundinsocioeconomicallydepressedareas.
ClinicalSignificance
Objective,criticalevaluationandassimilationof emergingresearchevidencemayindicatethatcaries preventionisn’tasrobusttodayasitwasbefore 1975.Newinformation,newinterventions,andnew methodologieshavebeendeveloped,changingthe findingsofmorerecentinvestigations.Thedental communityshouldbeopentoacceptingchangesin theevidenceevenifthechangesaren ’tinlinewith stronglyheldbeliefs.
O’MalleyL,ClarsonJ,LewisS,etal:Water fluoridationforthe preventionofdentalcaries. BrDentJ 238:241-242,2025
Reprintsnotavailable
Althoughcommunitywater fluoridationhasbeenwidelyused sincethe1940s,concernoverthepossibleadverseeffectsof fluorideonoralandgeneralhealth,including fluorosisandother negativehealthimpacts,ledtodebatesbeginningintheearly 1970s.Despiteevidenceoftheeffectivenessof fluorideinpreventingdentalcariesandthebeliefthatthispositiveeffectoutweighssafetyconcernsorhazardouseffects,thesedebateshave raisedabundantconcernandcitedtherightofindividualsto choosewhatisaddedtothepublicwatersupply.Ethicalissues
havealsobeenraisedregardingtherightsofindividualsversus thebene fitsforcommunitiesandsocietyingeneral.Ethicsreferstorules,actions,orbehaviorsthatareusuallyinformed bymoralphilosophy.Thosepertinenttopublichealthtendto bepracticalanddefineallowableactions,whereasthemoral theoriesrelevantinpublichealtharebasedonguidingprinciples andideasthatdefi newhatisrightandwhatiswrongandwhy. Oftenmoralsareself-determinedandincludeinfluencesranging fromfamilyandeducationtoreligion.Politicaltheoriescanalso shapepublichealthethicalperspectives.Themoral-based
philosophiesandpoliticalphilosophiesthatcontributetothe ethicalframeworksrelevanttocommunitywater fluoridation wereexplained.
Moral-basedtheoriescanbebroadlyclassifiedasconsequentialist andnon-consequentialisttypes.
Inconsequentialisttheories,themoralvalueofanactionisbased onitsconsequence,sotheactionthatprovidesthebestconsequencesisthemoralchoice.Problemsarisebecause “best” can beinterpretedinvariousways.Inutilitarianism,whichisaconsequentialmoraltheory,themoralchoiceistheonethatoffersutilitytothegreatestnumberofindividuals.Publichealthisa utilitarianeffortinthatitsgoalistoprovidethegreatestpopulationutilityforhealthandwellbeing.It’simpartialbecauseeveryone ’sutilityshouldcountequally.Utilitarianargumentsinfavorof justifying fluoridationwouldfocusonitsabilitytomaximizeoral healthbyreducingcariesevenifasmallnumberofindividualsare adverselyaffected.
Innon-consequentialisttheories,moralactsareindependentof consequences.Severaltheoriesfallintothiscategory,including deontologicaltheories,virtuetheories,andprinciplism.
Deontologicaltheories emphasizeobligationsandrules,andduty andobligationstoallindividualsmustbeconsidered.People shouldn’tbetreatedasmeanstoanend,soanypublichealth interventionmustconsidertheminoritythatwouldbeharmed. Inaddition,thereisadutytowardvulnerablegroupsthathave limitedin fluencethatmustbeconsidered,sothattheyshould bene fitfrom fluoridationandhavetheirneedsmetaswellas thosewhoaren’tsusceptibletoharm.
Virtuetheories arerootedinEasternphilosophyandemphasize behaviorssuchaskindness,courage,andhonesty.Theethical decision-makingprocessissimilartothatwithdeontologicaltheories,withnon-virtuousdecisionswithrespectto fluoridation beingthosethatdon’tincludetherighttochoosewhatisadded tothewaterorthosethatdon’tconsidertheneedsofthoseat highriskofcaries.Virtuetheoriesrequireasensitivebalanceof theclaimsofindividualandcommunity,butthelackofaframeworktodeterminewhatisandisn’tvirtuoushasbeenadrawback inapplyingthesetheories.
Principlism usesaseriesofethicalprinciplesthatareinformedby moraltheories.Thisapproachtopublichealthissuescanbemore practicalthansomeoftheothertheories.
Withallofthesechoices,manypractitionersapply4bioethical principles,speci fi callyautonomy,non-maleficence,bene ficence,
Table1. EthicalPrinciplesProposedasImportantintheJustificationofPublicHealthInterventions
AuthorsPrincipleDescriptor
Upshur
‘Harmprinciple’ Powershouldonlybeexercisedoverindividualsagainsttheirwilltopreventharmtoothers.Derived fromJ.S.Mill’sharmprinciple
Leastrestrictiveor coercivemeans
Morerestrictiveandcoercivemeansshouldonlybeusedwhenlessrestrictiveandcoercivemeans havefailed
ReciprocityPublichealthinterventionsmayrequiresacrificesandleadtocostsforindividualsorcommunities. Societyshouldseektocompensatethoseimpactedandfacilitatetheircontinuedroles TransparencyAllstakeholdersshouldbeinvolvedindecision-making,whichshouldbeaclearandaccountable process,andasfreefrompoliticalanddominationofspecificinterestsaspossible
Childress etal. EffectivenessIfinfringingmoralconsiderations,theremustbeevidencethatpublichealthwillbeprotected ProportionalityProbablehealthbenefitsmustoutweighadverseeffectsfrominfringementofmoralconsiderations, suchasautonomy
NecessityNotallinterventionsthatareeffectiveandproportionatearenecessary.Iftherearealternatives,the leastmorallyproblematicshouldbechosen
LeastinfringementOnmeetingthe firstthreeprinciples,infringementofmoralconsiderationsshouldbeminimised.For example,ifautonomyisinfringed,theleastrestrictivealternativeshouldbesought PublicjustificationWhereinterventionsinfringemoralconsiderations,thisshouldbejustifiedpublicly.Thisshouldbe democraticandtransparenttoestablishaccountability22 andbuildpublictrust
KlugmanSolidarityAutilitarianprinciple,builtonequity(benefitsshouldbesharedfairly),communityautonomy (communityrepresentativesdecide),andpaternalism(infringementofliberty),inwhichcommunities cometogethertoimprovehealth
EfficacyEvidencethattheinterventionshouldbesuccessfulinreachinggoals,isscientificallysound,and socially,politically,andculturallyfeasible
IntegrityThenatureandcultureofacommunityshouldbepreservedandrespected.Thecommunityshould beinvolvedindevelopinginterventionssotheyareconsistentwiththeirvalues
DignityAllincommunitiesareofequalworth,deservethesamemoralrespect,andshouldbetreated accordingly.Whereverpossible,theleastrestrictiveinterventionshouldbechosen
(CourtesyofPatelV,PatrickA,DyerTA:Theethicsofcommunitywater fluoridation:Part1 anoverviewofpublichealthethics. BrDentJ 238:311315,2025.)
Table2. AnOverviewofPublicHealthEthicalGuides/Frameworks
Authors/countryFormat
KassUSASixquestions
Childress etal. USAGeneralmoral considerationsmap
Factorsconsideredwhenassessinginterventionsand programmes
Thepublichealthgoalsoftheprogramme
Effectivenessoftheprogrammeinachievingitsgoals
Knownpotentialburdensofharmsoftheprogrammes
Minimisationofburdensandharmsandalternative interventions
Fairimplementationoftheprogramme
Burdensandbenefitsarebalanced
Productionofbenefits
Avoidance,prevention,andremovalofharms
Maximalbalanceofbenefitsoverharms
Distributionof/communicationofbenefitsandburdens
fairlyandensuringpublicparticipation
Respectofautonomouschoicesandlibertyofaction
Protectionofprivacyandconfidentiality
Maintenanceofpromisesandcommitments
Disclosureofinformation,honesty,andtruthfulness
Buildingandmaintainingtrust
Moralandethicalvaluesreflectedin framework
Wellbeing,benefits,minimisingharms, liberty,justice,autonomy,respect, distributivejustice
Wellbeing,utility,benefits,minimising harms,distributivejustice,procedural justice,autonomy,liberty,transparency
NuffieldUKTwoanalyticaltools:
Stewardshipmodel
Interventionladder
TannahillUKDecision-makingtool basedonevidence, ethicsandtheory
Stewardshipmodel
Protectingandpromotinghealth
Ensuringaccess
Reducingrisksofillhealth
Reducinginequalities
Interventionladder
Restricting/eliminatingofchoice
Guidanceofchoicesthroughincentivesanddisincentives
Guidanceofchoicesthroughchangingpolicy
Enablingchoice
Providinginformation
Doingnothingormeremonitoring
Evidence Theory
Ethicalprinciples
Wellbeing,benefit,minimisingharm, distributivejustice,fairness,liberty
Doinggood,minimisingharm,respect, empowerment,socialresponsibility, participation,openness,sustainability, accountability,equity
(CourtesyofPatelV,PatrickA,DyerTA:Theethicsofcommunitywater fluoridation:Part1 anoverviewofpublichealthethics. BrDentJ 238:311315,2025.)
andjustice.However,autonomyisusuallyrestrictedsomewhatbypopulation-basedpublichealthmeasures.Inaddition, non-male ficence,theprincipleofcausingnoharm,isfaced withadoubleeffectinthatthereareadverseeffectsthat canbetoleratedaslongastheywerenotintendedandthe primaryaimwastodogood.Bene ficenceisthecounterpoint tonon-maleficenceandcallsforactingforthebene fitof others.Justiceisaprincipleconsistentwithnotionsofsocial justiceandamelioratingdisadvantages,suchasinequitiesin resourcedistribution.
Theusefulnessofalltheseprinciplesisquestionablebecause oftheirlimitations.Mostdon ’tadequatelyaddressthebalance oftheindividualwithbene fi tstothepublichealthstatus. Publichealthprinciplism isbasedonthebeliefthatacommoncitizenshipexistsandacommunitycanhavesharedloyaltiesand dutiestoself.Byprotectingcommunityhealth,onecanprotecttheindividual’shealth.Therefore,publichealth
interventionssuchas fl uoridationthatarebasedon communalinterestextendtraditionalmedicalethicsandindicatetheneedforapublichealthperspectivetoethicalconsiderations( Table1 ).Variousprinciplesfocusedonpublic healthpolicymakinghavebeenproposed.
Liberalismandcommunitarianismarethe2mainpoliticalphilosophiespertinenttopublichealthethics. Liberalism isthe righttoself-determinationbasedontheconceptofautonomy, withanemphasisontheperson’srighttofollowhisorher ownconceptionofgoodandliveaccordingtopersonalbeliefs ofworthorvalue.Inaliteralperspective,publichealthinterventionsmaybechallenged,eveniftheintentionisforthe population’sgoodhealth.LiberalobjectionsrelatedtoautonomyincludetheharmprincipleofMillandtheinfringement ofpersonalfreedom.Arecentdevelopmentislibertarian
paternalism,whichpositsthatinfluencingwithoutcoercioncan allowindividualstomakerationalchoicesintheirbestinterest butstillbeinformedbypublichealthinterventionsand messaging.Thisnewapproachmaysupportthoseableto choosebutdoesn’taddressthesituationinwhichpersons areunabletodecideforthemselvesandisinconsistentwith populationapproachesthatbene fitsuchgroups.
Communitarianism focusesontheinterconnectionofindividuals andcommunities,withspecialconcernforhowaperson’sidentityisshapedbycommunity.Sharedresponsibilityisaparticular emphasis.Thefocusoncommunitymeansthatutilitarianperspectivesandeffortsaremoreconsistentwithcommunitarian politicaltheories,sopublichealthinterventionssuchas fluoridationaremorereadilyjusti fied.
Liberalandcommunitarianperspectivescancoexistbecausea population’sbestinterestswillalsobene fitindividuals.Because liberalperspectivesaccepttheneedtoavoidharmtoothers whenexercisingtherighttochoose,politiciansofallparties andbeliefscansupport fl uoridation.
Ethicalframeworkshavebeenproposedtohelpdetermine whetherinterventionsarejusti fi ed.Theseframeworksprovidede fi nitionsofvaluesandpostquestionsto “frame” decisions.Theytendtobroadlyapplyaprinciplismapproach (Table2 ).Thesestructurescanproveusefulasanalytical toolstoguidediscussions,butshouldn’tbeappliedrigidly andsimplistically.
Thegoalofpublichealthmeasuresistobenefitpeople bypreventingdisease,promotinghealth,andreducing oreliminatinginequalitiesintheseefforts.Therightsof individualsandtheneedsofcommunitiescancome intoconflict,andethicalanalysisisrequiredtodetermineifindividualpatientcareisappropriateforpublic healthinterventions.Variousprinciplesandethical frameworkshavebeensuggestedthatidentifyfactors tobeconsideredinanydeliberations.Fluoridationisa publichealthmeasurethatisundergoingpressureto weightherightsofindividualstobeprotectedagainst possiblenegativeeffects,todecidewhatisorisn’tput intothewater,andtoconsidertherightsofthepublic toobtainthepositiveeffectsoffewerdentalcariesin children.Thisissueisbeingdiscussedwidelyinthe UnitedStatesaswellasothernations,seekingtoidentifythebestwaytoapproachtheadditionof fluorideto drinkingwater.
PatelV,PatrickA,DyerTA:Theethicsofcommunitywater fluoridation:Part1 anoverviewofpublichealthethics. BrDentJ 238:311-315,2025
Reprintsavailablefrom TADyer,SchoolofClinicalDentistry, UnivofSheffield,19ClaremontCrescent,Sheffield,S102TA, UK;e-mail: t.dyer@sheffield.ac.uk
Theevidencefoundinthe1930sregardingtheinversecorrelationbetweennaturallyoccurring fl uorideinwateranddental cariesledtotheadditionof fl uoridetopublicdrinkingwater. Althoughtherewasanincreasedriskfordental fl uorosis, fl uoridationwasaneffective,cost-effective,andsustainablemethod toreducedentalcaries.Morerecently,addedconcern(without supportingevidence)hasbeenraisedthatlinkscancersand otherhealthproblemsto fl uoridation.Publichealthmeasures suchas fl uoridationaredifferentfromclinicalinterventions becausetheyareaddressingpopulationhealthandnotindividual wellbeing.Therightsofindividualsareoftenseenaslessimportantthanthebene fi tstothecommunity.Publichealthethicsfocusesonthehealthofpopulationsratherthanindividuals,but includesindividualrights whenconsideringwhetheran
interventionisfairandjust.Relativelylittlehasbeenpublished regardingtheethicalimplicationsof fl uoridationfromthe perspectiveofvariousmoral,ethical,andpoliticalphilosophies. Howtheethicsof fl uoridationhasbeenappraisedintheliteraturewasinvestigated.
AsearchwasdoneintheMedlineviaOVID,Scopus,WebofScience,CochraneLibrary,UniversityofSheffieldStarPlus,and GoogleScholardatabases.Othersourcesincludedreferencelists ofarticlesfoundinthedatabasesearch,handsearchesofkey journals,websitesofrelevantnetworks,andthepublicationsof organizationsandconferences,alongwithagreyliteraturesearch inOpenGrey.Atotalof51articlesfrom15countrieswereidentifiedandusedinascopingreview.
Thescopingreviewpresentedinformationinadescriptionofthe theoreticalandphilosophicalbasisofthestudiesandtheapparent stanceon fluoridation.
TheoreticalandPhilosophicalBasisofAnalyses
Moststudiesdiscussedtheethicsof fluoridationusingmoralbasedtheoriesandpoliticalphilosophies,whilecitingorimplying variousprinciples. Moral-basedtheories wereinformedbyor impliedconsequentialisttheoriessuchasutilitarianism.Forty studiesappearedtofollownon-consequentialisttheories,with 1offeringadeontologicaltheorythatsaw fluoridationasaviolationofinternationalagreementsonhumanrightsandbiomedicines.Principlismandpublichealthprinciplismofferedethical principlesconsidering fluoridationbeyonditsconsequences. Someauthorscitedprinciplesformedicalcare,includingautonomy,non-male ficence,bene ficence,andjustice.Thirty-six studiesaddressed fluoridationinrelationto1ormoreofthese principles.Inaddition,22studiesfocusedonautonomyornonmale ficence,bene ficence,andjustice,with6discussingall4principles.Publichealthprinciplismwasmentionedin6studiesas ethicalprinciplestobeusedinassessingtheethicsof fluoridation.
The politicalphilosophies werediscussedorimpliedin17studies withreferencetolibertyandfreedom.Communitarianismwasn’t directlycited,butitsprincipleswereimplied.
Variousothertheoriesandmodelswerealsousedinethicalarguments.Fluoridationwasconsideredintermsofaviolationof medicalethicsandtheNurembergcodein4studies,whereas 10usedtheNuf fieldBioethicsreportforpublichealthmeasures andthestewardshipmodel.Thelastproposesanintervention ladderencouragingapproachesthatarelessintrusive(loweron theladder)andallowforpublicconsultationtomakedecisions.
StanceonFluoridation
The3stancesadoptedintheliteratureweresupporting fluoridation,opposing fluoridation,andneutralwithrespectto fluoridation.
SupportingFluoridation
Fifteenstudiesthatsupported fluoridationreferredtotheethical positionsofprinciplismwithrespecttobene ficence,nonmale ficence,andutilitarianismasdeterminedbytheconsequencesorimpliedcommunitarianism.Thismeansthatthebenefits,minimalharm,andmoraldutyofthepolicywere determinedbythegoalofpreventingcaries,thusservingthe commongood.Someauthorsadvocatedforaddingthevoiceof society,especiallyfromthosememberswhosesituationcould beconsidereddisadvantaged.Professionalfreedomwasalso identi fiedasaright,sothat fluoridationwasn’tconsideredunduly restrictivetosocietyandservedatemporarycommongood.It wasrecommendedthatitbelawfullyregulated.
UsingtheprinciplesoftheNuf fieldframework,severalstudies presentedutilitarianarguments.Democraticdecision-making
wasimportantinimplementingpublichealthmeasures.The emphasisofindividualautonomyshouldn’tbeahindranceto communityhealthbene fitsandfewerinequalities.Fluoridation wasalsoseenasnon-coerciveinthatitrequirednolifestyle changecomparedtoalternativemeasures.Theimperativeofindividualconsentwaspresentedaspossiblyrequirednotonlyfor instituting fluoridationbutalsoif fluoridationistobe discontinued.
Communitarianandutilitarianprincipleswereusedinarguing thatwell-focusedpaternalismpromotesbroaderfreedomfor themany.Inaddition,theperspectiveofliberalismversusutilitarianismwaspresented,notingthatbioethicshasdevelopedin countriesthatareeconomicallydevelopedwithgoodaccessto information.Thusethicaldebatesmaydifferfromculturalinfluencesandmaynotberelevanttoothercountrieswheretheinformationneededforinformedchoiceisn’tavailable.
Sevenstudieswereassessedasopposing fluoridation.Mostcited individualethicalprinciplesasareheldinprinciplism.Somecited moral-basedconsequentialismandnon-consequentialisttheories.AstudyinAustraliaespousedalternativecariesprevention, notingthat fluoridationinfringesontheprincipleofautonomy andviolatestheprincipleofnon-male ficencebasedondental fluorosisandotherhealthrisksthathavebeenclaimed.The resultwasthattheethicaljustificationfor fluorideinthatcountry wasinsufficient.
Twoadditionalstudiesindicatedthat fluoridationismorallyand ethicallyunacceptableanddoesn’tcomplywiththeNuremberg codeofpracticeorothermedicalcodesandregulations.The conclusionwasthatconsumersshouldbefullyinformedabout therisksandbenefitsto fluoridation,whichtheycurrentlyarenot.
Twenty-ninestudiescitedmixedethicalviewpointsbutwere seenasneutralto fluoridation.Amongtheethicalstanceswere principlism,utilitarianism,liberty,andtheNuf fieldapproach. Mostofthesestudiesweredesignedtoappraiseethicsbut someconsidered fluoridationmoregenerally,althoughethics wasincluded.Often,thesestudiesacknowledgedthetensionbetweenautonomyandbene ficenceinpublichealthinterventions aswellastheneedforpublicdebateinmakingpublichealth decisions.
Onestudyfoundthatanti- fluoridationargumentshaveoverstatedcontroversiesthatidentifyharmsandview fluoridatedwaterasamedication.ThisstudyproposedthattheUnited KingdomDepartmentofHealth’sfundingoforganizationsthat support fluoridationandselectivereportingofresearchundermineitsscienti ficindependence.Thelimitationsofstudiesused tosupport fluoridesafetywerecited,includingthesmallsample sizes,anditwassuggestedthatselectiveuseofevidencecanunderminepublictrust.
Twopublichealthethicalframeworkswereusedinaneutral analysisoffoodforti ficationand fl uoridation.Aspectsofboth frameworkswerenotful filled.Theconclusionwasthattheethics ofpublicinterventionsshouldberevisitedregularly.
Principlismwasusedin1studytoassess fluoridation,butthis investigationalsoappliedtheidealsofefficacy,integrity,solidarity, anddignity.Itwasproposedthatefficacymaybeunclear,although thereisevidenceof fluoride’seffectiveness.Theauthorquestionedwhetherit’sfeasibletoseethiseffectivenessinthecurrent politicalandsocialclimate,butdidsee fluoridationasfavorablefor solidarity,althoughitwasunclearforintegrityanddignity.
Althoughethicalargumentswereusedinanotherstudy,they wereinthecontextofimpactsofvarioussocial,cultural,andreligiousphilosophies.Withrespecttoautonomy,theauthors consideredwhetherresponsibilityshouldbeshared,remainindividual,beprofessional,orinvolvethestate.Theyconcludedthat themostimportantaspectofanypolicyinvolvesengagement withthepublicandtransparencyofgovernmentintent.Bene ficenceandmaximizedcommongoodwereseenfromautilitarian perspective,butthein fluenceofprofessionalpowerintheprocesswasacknowledged.
Arelativelysmallbodyofliteratureexistsonthetopicofthe ethicsof fluoridation.Appraisalsoftheethicsof fluoridation tendtobecouchedintermsmoreoftenrelatedtomedical
Water fluoridationandtheuseof fluoridatedtoothpastearethe primarywaysusedtoprotectagainstdentalcaries.Theeffectivenessandsafetyof fluoridemustbeconstantlymonitoredtoensure publichealthisbeingenhancedandtoreassurethepublicthatwater fluoridationissafeandeffective.Theriskofdevelopingdental fluorosismustbebalancedagainstthebenefitintermsofpreventingdentalcaries.TheNationalToxicologyProgram(NTP)has raisedconcernabouttheeffectsof fluorideoncognitiveneurodevelopment,yetcredibleevidenceforanynegativeeffectislacking. Majorreviewshaveconcludedthat fluorideatthelevelsusedin water fluoridationprogramshasnonegativeeffectonchildneurodevelopment,yetotherreviewscontinuetoindicatethereare problems.Potentiallinksbetweenearlyexposureto fluoridein fluoridatedwaterandcognitiveneurodevelopmentweresought inapopulation-basedsampleofAustralianyoungadults.
carethatthantopublichealthinterventions.Oftentheethical approachwasn’tidenti fiedbutonlyimplied,butstudiestended tofavor,oppose,orexpressaneutralattitudetoward fluoridationasapublichealthmeasure.
Theappraisalsof fluoridationintheliteratureoften emphasizedprinciplesortheoriesthataren’tadequate toresolvethetensionbetweentheindividualconsent forandcollectivebenefitof fluoridationasapublic healthmeasure.Approachesdesignedtospecifically assesspublichealthinterventionsshouldbeusedin debatesovertheethicalstatusofcommunitywater fluoridation.
PatelB,DyerTA:Theethicsofcommunitywater fluoridation: Part2 howhastheethicsofcommunitywater fluoridation beenappraisedintheliterature?Ascopingreview. BrDentJ 238:336-343,2025
Reprintsavailablefrom TADyer,SchoolofClinicalDentistry,Univ ofSheffield,19ClaremontCrescent,Sheffield,S102TA,UK; e-mail: t.dyer@sheffield.ac.uk
Australia’sNationalChildOralHealthStudy(NCOHS)20122014providedthesampleof357participantsinthisstudy. NCOHSchildrenwereevaluatedfordental fluorosis,whichisa reliableclinicalbiomarkerfortotal fluorideintakeduringearly childhood.TheNCOHSalsocollecteddataonsocioeconomicfactors,oralhealthbehaviors,andresidentialhistorytoestimate fluorideexposureduringthe first5yearsoflife(%LEFW).Follow-up ofthesamplein2022-2023(whentheparticipantswereage16to 26years)measureddataoncognitiveneurodevelopmentusingthe WechslerAdultIntelligenceScale4th edition(WAIS-IV).Three groupswereformed:having0%LEFW,>0%to<100%LEFW, and100%LEFW.The%LEFWfrombirthtoage5yearswas usedtomaintainconsistencybetweenparticipants.Associations between%LEFWanddental fluorosiswereinvestigatedusing full-scaleintelligencequotient(IQ)scores(FSIQ).
Theproportionsofparticipantswhodidn’thaveaneurodevelopmentaldiagnosiswerecomparableamongthe3groups,andthe distributionsbysexandsocioeconomicfactorswerecomparable betweenthosewithandwithout fluorosis.Ahigherproportion ofparticipantswithoutdental fluorosisreportedlyhadaneurodevelopmentaldiagnosis.
ThemeanFSIQwas109.2,withaslightlylowerunadjustedmean FSIQamongthosewith0%LEFWthaninparticipantsintheother 2groups.Thosewhohad0%LEFWalsohadlowerFSIQscores thanthosewholivedallorpartoftheir first5yearsoflife exposedto fluoridatedwater.TheunadjustedmeanFSIQscores werecomparablebetweenthosewithandwithoutdental fluorosisontheirmaxillarycentralincisors.
TheadjustedFSIQscoresofthosewhohad100%LEFWwere slightlyhigherthanthoseoft he0%LEFWgroup.Inaddition, theadjustedestimateoftheFSIQscoresofthosewithdental fl uorosiswasn’tinferiortothatofthosewithoutdental fl uorosis.
Inmultivariableanalysis,FSIQ scoreswerecomparableamong thegroupswithdifferentlevelsof fl uorideexposureinearly childhood.WAIS-IVindexscoresshowednoassociations withlevelof fl uorideexposure.Neitherthepercentageof
LEFWnordental fl uorosisshowedanassociationwithFSIQ scores.
Earlylifeexposureto fluorideinAustralianchildrenhadnomeasureableeffectontheircognitiveneurodevelopment.
Theevidenceshowsthatchildren ’sexposureto fluorideinthe first5yearsoflifehadnonegative relationshipwiththeircognitiveneurodevelopment. Thecurrentwater fluoridationprogramsremainboth effectiveandsafeforyoungchildren.
DoLG,SawyerA,SpencerAJ,etal:Earlychildhoodexposuresto fluoridesandcognitiveneurodevelopment:Apopulation-based longitudinalstudy. JDentRes 104:243-250,2025
Reprintsavailablefrom LGDo,SchoolofDentistry,Facultyof HealthandBehaviouralSciences,TheUnivofQueensland, HerstonOralHealthCtr,7th Flr,Herston,Queensland4006, Australia;e-mail: l.do@uq.edu.au
Theuseofcannabisisbecomingmorecommon,withseveral countrieslegalizingitsuseformedicinalpurposesandsome evenlegalizingitsrecreationaluse.Marijuanacanbeconsumed invariousways,includingthesmokingofhand-rolledcigarettes (joints),hollowed-outcigars(blunts),pipes,waterpipes (bongs),orcigars;theingestionoffoodordrinks(edibles); andtheuseofcompoundsofthecannabisplant,suchascannabidiol(CBD),whichistakensublingually.Withthewideruseof cannabis,dentalprofessionalsaremorelikelytoencounterpatientswhoadmittousingcannabisrecreationally.Guidancethat ispracticalandevidencebasedispresentedregardinghowto recognizetheimpactofrecreationalcannabisonoralandgeneralhealthandhowdentalpractitionerscanhelppatientsand referthemtoavailablesupportservicesanddealwithlegal issues.
Cannabisusehasbeenassociatedwithseveraladverseoralconditions,suchasreducedsalivary flow,whichleadstoxerostomia, andreducedsalivarybufferingcapacity,whichincreasestherisk ofcariesandperiodontitis.Long-termcannabisuseincreases theprevalenceofgingivalin flammationandtheaccumulationof plaque.Inaddition,tetrahydrocannabinol(THC),whichisthe primarypsychotropicagentincannabis,stimulatesappetite, causingfrequentconsumptionofcariogenicfoodsanddrinks. Chronicin flammationoftheoralcavity,leukoplakia,andimmunosuppressionthatcanleadtooralcandidiasishavealsobeen linkedtocannabisuse.Someevidencehasconnectedcannabis usetomalignanciessuchasoralcancer.
ClinicalConsiderations
Thedentistshouldlookforsignssuchasdrymucosa,increased plaquelevels,andperiodontaldeteriorationinpatientswho reporttheregularuseofcannabis.Theclinicalexamination plusadetailedpatienthistoryshouldindicateifthesechanges arerelatedtocannabisuse.Dentistsshouldalsoconsider refusingtotreatacannabis-intoxicated(high)patientbecause heorshehasareducedabilitytoconsenttotreatment.
Cardiovasculareffects,includingtachycardiaandarrhythmias, havebeenlinkedtocannabisandcancomplicatedentalproceduresthatarestressfulorincludetheuseoflocalanestheticswith vasoconstrictors.Patientcooperationandanxietylevelscanalso becomeproblematicbecauseofcannabis’ psychoactiveproperties.Druginteractions,includingwithopioidsandsedatives, canbeaconcern.
Bothcognitivefunctionanddecision-makingpropertiescanbe compromisedwithregularcannabisuse,makingsomepatients skiporalhygieneorappointments.Whendevelopingpersonalizedpreventivecareplansforpatientswhousecannabisregularly,thedentistshouldkeeptheseissuesinmind.
Oralhealthcareprovidersshouldmaintainanonjudgmentalattitudeandasupportiveapproachtopatientswhousecannabis.To betterunderstandthefrequency,duration,andmethodofuse, thedentistshouldaskopen-endedquestionsaspartofthe comprehensivemedicalandsocialhistory.Adietdiarymaybe usefulintrackingirregularsnackingbehaviors.Allofthisinformationwillhelpinformulatingarisk/susceptibilityassessmentand hopefullyleadtoopenandhonestdialoguebetweendentist andpatient.
Dentistsshouldalsoadvisepatientsregardingtheoralhealthrisks associatedwithcannabisuse,notingespeciallybehaviorssuchas theneedforenhancedoralhygiene,properhydration,regular dentalvisits,andmodificationsofthepatient’slifestyle,specifically,reducingoreliminatingcannabisuseifthat’sappropriate. Thedentistshouldmaintainapatient-centeredcarefocus, ensuringthisadviceisinformativeandsupportive.
Servicesareavailabletoassistpatientswithsubstanceabuse.In theUnitedKingdom(UK),theNationalHealthService(NHS) offersspecializeddrugandalcoholserviceswherethepatient canreceivecounseling,joinsupportgroups,andevenreceive pharmacologicalinterventions.ThelocalDrugandAlcohol RecoveryServices(DARS)canprovideadditionalassistance.
Thepatient’sgeneralmedicalpractitionermaybeabletorefer thepatientforspecialistservices.TalkToFrankcanprovide adviceandsignpostuserstosupportgroups.Throughlocal referralpathwaysandsupportnetworksthedentistcanprovidecomprehensivecareforpatients’ generalanddental healthneeds.
IntheUK,recreationalcannabisisillegal,withpossessionleadingtocriminalcharges.Thedentist’sroleistoprovidesafe, effective,andnonjudgmentalcareandnottoenforcelegalrules. Providerscandocumentpatients’ disclosurestokeepaccurate andcon fi dentialrecordsaboutcannabisuse;advisepatientson legalimplications;reassurepatientsthathisorherprimaryfocus isonthepatient ’shealthandwellbeing;andworkalongside medicalcareprovidersandsupportservicestotreatpatients holistically.
Dentalpractitionersarelikelytohavepatientsintheir practiceswhousecannabis.Dentistsshouldbeable torecognizethesignsofcannabis-relatedoralhealth problemsandundertakeempatheticandeffective communicationtohelpsuchpatients.Theseindividualsrequireacomprehensiveapproach,including clinicalvigilance,supportiveeducationandreferrals, andanonjudgmentalattitudethroughouttheprocess.
DaveM,PatelN:Theclinicalimplicationsofcannabisusein dentistry. BDJTeam 12:137-139,2025
Reprintsnotavailable
Avoidance/restrictivefoodintakedisorder(ARFID)hasonly recentlybeenidenti fiedasaneatingdisorder.It’scharacterized byapersistentdisturbanceineatingthatleavestheindividualunabletomeethisorhernutritionalorenergyneeds.Long-term medicalandpsychosocialproblemscanresult(Table1).TheARFIDdiagnosisreplaces ‘feedingdisorderofinfancyandearlychildhood’ intheWorldHealthOrganizationclassificationofdiseases. ARFIDpatientsaren’tconcernedabouttheirweightorshapeand theavoidanceorrestrictionoffoodsisnotrelatedtoculturalor religiousreasonsorpre-existingmedicalconditions.ARFIDcan developatanyage,andtheglobalprevalencehasbeenestimated tobebetween5%and11%,withchildrenandmenmorelikelyto beaffected.ThesignsanddiagnosticelementsofARFID,itspsychosociologicalimpactandcomorbidconditions,treatments,and dentalimpactweredetailed.
Characteristics
ARFIDoccursas3subtypeswithspeci ficsignsofeach.Theseare lowappetite,sensorylimitations,andaversive,asfollows:
Thosewithlow-appetiteARFIDhavelimitedintakeofspeci fic typesandquantitiesoffood,takealongtimetoeat,andhave dif ficultyeating.
Amongthesensoryproblemsthatlimitintakeoffoodare aversionstocertainfoods,inhibitingsensoryelements,and profoundrigidityineating.ARFIDindividualscanbehighlyselectiveinthetypesoffoodtheywilleatandcanbecome extremelyanxiousaboutnewfoods.Tastes,texture,smells, appearance,ortemperatureofthefoodcanbecome problematic.
Aversivetypecanleadtothepatientbeingviewedashavinga poorappetiteandbeingunabletoenjoyfood.Oftenaversion orrestrictionisrelatedtoaneventorfearofchokingor vomiting.
Thecharacteristicsandpresentationoffoodavoidancecanbea mixofthese3types(Box1).Comparedtopatientswithanorexia orbulimia,patientswithARFIDtendtobemorelikelytohavea medicaloranxietyconditionandlesslikelytohaveamood disorder.
Althoughnouniversallyaccepteddiagnosticmethodhasbeen developed,helpfulinvestigationsincludeapsychologicalevaluation usingastructuredclinicalinterview,self-reportingquestionnaires, amedicalevaluation,growth-developmentalassessments,and testsfornutritionaldeficiencies.ThediagnosisfocusesonthenatureoftheARFIDpresentation,withmedicalconditionsconsideredsecondarytonutritionaldeficienciesorcoexistingdisorders.
Table1. SummaryoftheDSM-5DiagnosisfromARFID1
CriterionA
Eatingdisorderresultingina persistentfailuretomeet necessarynutritionaland/or energyneeds
Criterion8
CriterionC
CriterionD
DatafromAmericanPsychiatricAssociation. DiagnosticandStatistical ManualofMentalDisorders, 5th ed.AmericanPsychiatricPublishing: Arlington,VA,2013.(CourtesyofHamidS: ‘Fussyeating’ oravoidant/ restrictivefoodintakedisorder? BrDentJ 238:271-274,2025.) Box1.
1.Weightlossinchildren/inadequate growth/delayedgrowth
2.Significantnutritionaldeficiencies
3.Relianceonenteralfeedingororal nutritionalsupplements
4.Substantialimpairmentin psychosociologicalfunction
Theconditionisnotaffectedbyfood availabilityorculturalnorms
Thediagnosisshouldnotinclude anorexianervosa/bulimianervosa (althoughcomorbiditymayexist)or personalconcernsofweightorbody shape
Thecausecannotbeexplainedbyother medicalconditions(egallergies)or eatingconditions(eganorexianervosa)
Theavoidanceoffoodoreatingcancausesocialanxietyandchallengetheindividual’sself-confidenceandabilitytomanagerelationships.Youngpeoplemayavoiddailysocialgatheringsand interactionswithpeers.Parentsmayclassifytheirchildasa ‘picky eater,’ rebellious,orattention-seeking.Seeingthattheindividual hasuncommoneatingpatternsorretreatsfromsituations involvingfoodsshouldprompttheconsiderationthatthereisa possiblemedicalcondition,withhelpneededfromageneralmedicalpractitioner.
Selectivefoodintakeoravoidanceiscommonlyseeninindividuals withautismspectrumconditions,anxiety,orattentionde ficit hyperactivitydisorder.TheseconditionscancoexistwithARFID. ThedistinguishingfeatureofARFIDisthattheoutcomeofthe conditionresultsinamedicalproblemorproblems.Theresearch onARFIDhasfocusedonyoungerindividuals,butinolderpatients,restrictive-likesignsthatleadtoreducedappetitecanbe relatedtomedicationsusedtotreattype2diabetes.
Aninterdisciplinaryapproachisrecommended,involvingmedical practitioners,psychotherapists,dietitians,andeducationalsupportpersonnel.Thegoaloftreatmentistomanagethepatient’ s physicalhealthconditionsandpreventhisorhermedicaldeterioration.Dietaryhabitsshouldbeassessedtoidentifythefoods beingavoidedandwhy.Nutritionalde ficienciesandweightloss areoftenmanagedwithmultivitamins,mineralsupplements, andmedicationsthatincreaseappetite.Educatingthepatient andadvisingaboutalternative ‘safe’ foodscanhelpbringdeficienciesintobalance.
Physicalappearance
Weightloss
Growthappearanceofchildlessthanexpected.
Medicalhistory
Developingnutritionaldeficiencies,suchasanaemia,through nothavingenoughironinthediet
Needingtotakesupplementstomakesurenutritionaland energyneedsaremet
Episodesofhospitalisationandtheneedfornasogastric feeding.
Eatingbehaviours
Eatingareasonablerangeoffoodsbutnotenoughtostay healthy
Notalwayssurewhenhungry
Feelingfullafteronlyafewmouthfulsandstrugglingtoeatmore
Takingalongtimeovermealtimes/findingeatinga'chore'
Missingmealscompletely,especiallywhenbusywithsomething else
Sensitivitytoaspectsofsomefoods,suchasthetexture,smell, ortemperature
Appearingtobea'fussy'or'pickyeater'
Alwayshavingthesamemeals
Alwayseatingsomethingdifferenttoeveryoneelse
Onlyeatingfoodofasimilarcolour
Attemptingtoavoidsocialsituationswherefoodwouldbe present
Beingveryanxiousatmealtimes,chewingfoodverycarefully, takingsmallsipsandbitesetc.
(CourtesyofHamidS: ‘Fussyeating’ oravoidant/restrictivefoodintake disorder? BrDentJ 238:271-274,2025.)
ThegoalofpsychologicaltreatmentistohelpARFIDpatients thinkandreactdifferentlytonewfoodsorthosetheyhave avoided.Therapistscanlistandrankfoodbyacceptanceandanxietycaused,thenuseagradedexposureapproachtohelpthepatientacceptnewfoods.Patientswhoassociateeatingwith vomitingandchokingbene fitfromthisapproach.Foodchaining, wherenewfoodsthathavesimilarqualitiesareintroduced,can helpwithsensoryaversions.Thesequentialoralsensory approachcanhelpyoungerpatients.Playandsensoryexperiencescanalsohelpchildrenbetterunderstandhealthyeating.
Nopharmacologicalinterventionshavebeenapprovedtoease ARFID,butsomestudieshaveinvestigatedantipsychoticdrugs. Thesetendtoimprovegeneralappetiteandreducepsychological distress.
Familyandcaregiversupportarekeycomponentsoftreatment. Thegoalistocreateanenvironmentthathelpspatientsunderstandsafefoodsandthosethatproduceanxiety,createstructure androutineatmealtimes,makechangestothehomeenvironmentasneeded,andteachpatientshowtomanageanxiety.
NostudieshaveconfirmedtheimpactofARFIDongeneraloral healthandwhetherit’srelatedtoanincreasedprevalenceof
Figure1. PossibleoralmanifestationsofARFID.(CourtesyofHamidS: ‘Fussyeating’ oravoidant/restrictivefoodintakedisorder? BrDentJ 238:271-274, 2025.)
dentalcaries,periodontitis,orsystemicsofttissueoralmanifestations.Poororalhygieneisthemostcommonfeature,with thepatient findinghavingatoothbrushortoothpasteinthe mouthfear-inducingoruncomfortable.Thetaste,texture,and sensationofthetoothpastemaycauseanaversiontoapplying topical fluorideaswell.
Withthisunderstanding,it’slikelythatpoororalhygienewould leadtoahigherriskforperiodontitisandcariesaswellasoromucosalconditionssuchasangularcheilitis,ulcers,andinflammation ofthelips,tongue,andintraoralmucosa.Neuromuscular developmentandunderdevelopedoromotorskills,causing problemswitheating,mayoccurinyoungerchildrenwithARFID (Figure1).
Thedentalteamshouldbefamiliarwiththesignsandsymptoms ofARFIDandrecognizebehaviorssuchasareluctancetobrush theteethorunusualorselectiveeatinghabits.HavingaheightenedanxietyovertheoralexaminationmayindicateapsychomedicalconditionsuchasARFID.Supportforthemanagement ofARFIDinvolvesamultidisciplinaryapproachthatincludes careforthegeneralphysicalwellbeingofthepatient,psychologicalcounseling,dietaryassistance,andencouragingcommunicationwithschoolsorworkplacesettingstoaccommodatethe patient’seatinghabitsormedicalneeds.Dentalrecallsshould beshortenedsopreventivemeasuresandobservationsforcaries aswellasperiodontalandsofttissueproblemscanbecarriedout
regularly.Ifthepatienthasanxiety,aroutinedentalexamination maybechallenging,sothepatientmaybereferredtospecialized centersforaninitialexaminationundersedation.
ThediagnosisofARFIDshouldpromptdentalcare providerstoaddressanypoororalhygienehabits andseekindicationsaboutwhytheseeffortsaren’t made.Ifthechildhasahistoryof ‘fussyeating,’ a mentalhealthdisordermaybeinvolved.Furtherinvestigationiswarranted,alongwithareferraltoamedical practitioner.TreatingapatientwithARFIDislikelyto bechallenging,butpreventingpatientsfromdevelopingasenseofinadequacyorbeingjudgedfortheir dentalconditioncanhelptoovercomethedifficulties ofaconditionsuchasARFID.
HamidS: ‘Fussyeating’ oravoidant/restrictivefoodintakedisorder? BrDentJ 238:271-274,2025
Reprintsavailablefrom SHamid,14aLeytonRdDentalPractice, 14aLeytonRd,Harpenden,AL52TQ,UK;e-mail: shabazhamid@icloud.com
Withtheagingpopulation,dentalpractitionersmaybecalled upontoprovidemanypatientswithrestorativecare.Insomesettings,dentaltherapists(DTs)maybeabletomeettheneedsof theseolderpatients,includingdirectaccesscare,patientassessment,andpersonalizedcareplanning.However,bothgeneral dentalpractitionersandDTsmayrequireguidancewhenfaced witholderadultswhohavecomplexdentalneeds.Alinkbetween dependencyandtreatmentplanningchoicesmaybeachievedusingtheSeattlePathway(Table1).Thisguidetotreatmentchoices fordentaldiseasefocusesonmatchingthelevelofdependency withappropriatecarechoices.Thelimitationsofthepatient canbeconsidered,whetherphysicalormental,andapragmatic approachisencouraged.TheapplicationoftheSeattlePathway andtheuseofredorgreen flagstoindicateproblematicorpragmatictreatmentapproachestomultipledentalsituationswere discussedwithrespecttoriskorsusceptibilityassessments,examinationsanddiagnoses,andtreatment.
Whenolderpatientscomeforcare,severalaspectsofthestandardhistorypathwayneedtobeconsidered.Theseincludethe patientcomplaint,patientwantsandwishes,medicalhistory,specialconsiderations,andconsentissues.
Oftentreatmentisguidedbythepatient’spriorities,butwith olderadults,it’sthecaregiverswhomayvoicecomplaintsrather thanthepatient.It’simportanttodeterminewhoiscomplaining andwhattheproblemis.Ared flagisraisedifthefamilydesires savinghopelessteethbutthepatientisn’tconcernedoverthis.A green flagcanbegivenifthepatient,evenonewithlimitedcapacitytoconsent,clearlyindicateswhatheorshewants,suchasthe removalofapainfultooth.Withincreaseddependencyandlower lifeexpectancy,howwellthepersonisfunctioningandwhether theriskofinterventionoutweighsthebene fitshouldbe considered.
Ifexpectationsareunrealisticorresourcesarelimited,thedental practitionershouldbehonestaboutthefeasibilityofthevarious approaches.Ared flagisjusti fiedifthepatienthasunrealisticexpectationsorlimitedpossibilitieswiththeavailableresources. Ontheotherhand,agreen flagisappropriateifclinicianandpatientcanagreeandchooseapragmaticviewofwhatcanbe achieved.
Riskassessmentismoreaccurateifthedentalpractitionerhasa goodunderstandingofthepatient’smedicalhistory.Thisincludes anycomplexmedicalsituationsthatexistandwhetherthese wouldbenegativelyimpactedbyprovidingdentaltreatment,if theyactuallyprecludedentaltreatment,andwhetherthe complexitywouldaffectthesuccessofdentalinterventions. Amongthediseasecomplexitiesthatarecommoninolderpatientsarerespiratorydisease,cardiovasculardisease,type2diabetes,liverdisease,andkidneyissues.Patientsmaybeundergoing oncologytreatments.Inaddition,frailtyanditsaccompanying pain,infection,fatigue,andpoorphysicalstrengthaswellaspolypharmacyleadingtoadversedruginteractionsthatcandiminish cognitionandfunctionandcausedrymoutharecommonly seeninolderpatients.Drymouthcancontributetoproblems eating,speaking,andsleeping;greaterprevalenceoforaldiseases andinfections;anddiscomfortinwearingdentures.Asaresult, patientscanhaveapoorqualityoflifeandimpaireddailyfunction.
Olderadultscanalsohavediffi cultywithmobility,instability,falls, incontinence,cognitivedecline,sensoryimpairment(suchas hearingandvisionloss),andimpairedcommunication.Personalizedcareplanningmusttakealloftheseintoaccount(Box2).A red flagisindicatedforadependentpatientwhohasmultiplecomorbidities,polypharmacy,andcognitivedecline.Green flagsare appropriateforpatientswholiveindependentlyandareingood healthwithgooddentalpreventivehabits.Dentalpractitioners mustalsobeawarethatchronologicalage,biologicalage,and overallhealthcandiffersigni ficantly,soassumptionsbasedjust onagearelikelytobeinaccurate.
Manypatientspresentwithacombinationofredandgreen flag indicatorswhentheabilitytogiveconsenttotreatmentisconcerned.Mentalcapacityrequiresunderstandingandusinginformationtomakedecisionsandbeingabletocommunicatethose decisions.Olderadultsoftenhavedesignatedindividualstoserve astheirmedicaldecisionmakersbeforetheylosecapacity,and thedentalcareprovidershouldensurethattheseindividuals areinvolvedinchoicesforcare.
Thementalcapacityofolderadultscanchange,withmentalcapacityoftenspeci fictothedecisiontobemade.Ifthepatient cannotdecideforhimselforherself,theclinicianmustactin thepatient’sbestinterestandchoosetheleastrestrictiveoption. Forconsent,red flagsareappropriatefordecidingtoundertakea complexcaseforapatientwhocannotconsentforhimselfor
Table1. SeattlePathway2
Assessment Adoptappropriate recallintervals
Identifyconditions threateningoralhealth
Developstrategicoral healthcareplantoinclude professionalandself-care
Treatment RoutineConsiderlongtermviability ofrestorationsand prostheses,Plan treatmentoutcomesfor easymaintenance.
Levelofdependency
Identitycausesofincreased dependency(forexamplestroke, polyphamacydementia)
Partcipatewithothermedical servicestoassesshealthlisks generally.
IncreasedfrequencyofrecallReassesslong-termviabilityof oralhealthrelatedprevention
Examinepatients'physical, cognitiveandsocialcontextfor barrierstoemergencypalliative andelectiveoralcare
Monitortheburdenoforalcareon thepatientsandothers
Increasevigilanceforsignsof elderabuse
Identity,repairorreplace strategicallyimportantteeth guidedbytheprincipleof 'shorteneddentalarch'withor withoutimplants.tomaintainoral function
Repairandmaintainstrategically importantteethwith conservativetreatments (forexample,Atraumatic RestorativeTechniqueARTwith fluoridatedglassionomer)and designoralprosthesesto simplifyoralhygieneandprevent infection
Offerpalliativetreatmenton demandfromthepatientto controlpainandinfectionand maintainsocialcontactsand activities.
Planforongoingmaintenance includingrestorativeandsurgical treatments,tomaintainfunction andpreventorcontrolinfection orpain
Useprosthodonticattachments betweenoverdenturesand abutmentteethorimplantsto simplifyhygieneand maintenance
(ReproducedwithpermissionfromPrettyIA,EllwoodRP,LoECM,etal:TheSeattleCarePathwayforsecuringoralhealthinolderpatients. Gerodontology 31(Suppl1):77-87,2014.Courtesyof TarnowskiA,EmanuelR:Wavingthe red or green flagforpragmatictreatmentoptionsinolderadults. BDJTeam 12:24-28,2025.)
Box2. SpecificConsiderationsAffectingPersonalizedCare Planning
- Medications(interactions,bleeding,andMRONJ)plus polypharmacy
- Frailty
- Allergies
- Mobilityandphysicalaccess
- Hearingandvisualimpairments
- Dysphagia
- Oralcareissuesandassistancefromdependents
- Cognitiveissues,dementia
- Socialhistory
(CourtesyofTarnowskiA,EmanuelR:Wavingthe red or green flagfor pragmatictreatmentoptionsinolderadults. BDJTeam 12:24-28,2025.)
herself.Complexpathologyortreatmentrequiringaddedmeasuresmaybeabetteroption.Inthesecases,documentationof thesupportforthedecisionandapersonalizedcareplancan helptoensureallpartiesareonboard.Ifthereisaclearagreementontheplan,thefamiliesarepragmaticandsupportive, andtheindividualswithpowerofattorneyandthoseproviding careareonboard,agreen flagcanberaised.
Table2. RedandGreenFlagsTable
Thepatient’slevelofcooperationandavailableresourcescan interferewiththethoroughnessofanexaminationanddiagnostic process.Thedentalpractitionermayberestrictedinhisorher abilitytoprovidecarebeyondanyimmediateandapparentissue. Olderadultswhoarereluctanttoallowassessmentsorradiographsaregivenared fl ag.Thosewhoareindependentand don’tlimitassessmentsordiagnosticprocesseswouldhavea green flagtoproceed.
Treatmentisaccomplishedinseveralphases,includingimmediate measures,controlofdisease,rehabilitationoffunctionandaesthetics,andongoingcare.Thesephasesoftreatmentareintrinsicallylinkedtothepatient’sprioritiesandreflectgoalsinachieving theultimatetreatmentoutcomes.
Immediatecareinvolvesemergencymeasurestomanageacute conditionsandgivethepatientreliefofpain.Amongthetreatmentsprovidedinthisphaseareextractions,drainageofinfections,medication,smoothingsharpteeth,andrestorations.It reflectsthepatient’stopprioritiesandisessentialforpatient comfortandsafety.Sometimessubsequentreferralisneeded toaccomplishfurthercare.
Oncethepatient’spainisrelievedandnofurtherdamageislikely, patientscanreceivepreventivecareandstabilization.Often
RiskassessmentGreen
c/oAresymptomspresentedbypatientorcarerclear?
Isthereaclearpatientorcarerrepottedproblem?
Arepatientwantsandwishesachievable?
HPCArethereconcernswithsleeping,eating,acfivitiesorbehaviour?
MHIsthereamedicalcomplexity,whichmaybedetrimentallyaffectedbyprovidingdentaltreatment?
Isthereamedicalcomplexitythatprecludesordinarydentaltreatment?
ConsentDoesthepatienthavecapacitytoconsent?
Ifthepatientcannotconsentisthetreatmentintheirbestinterestandleastrestrictive?
DiagnosisIsexaminationandradiographspossible?
Whatisthediagnosis,severityandextentofdentaldisease?
TreatmentWoulddeferringtreatmentworsenthefutureforthepatient?
Usefulnesstopreservedentalconditionasitis?
Isthepatientabletoco-operatewithconventionaltreatmentandLA?
Isaminimalinterventionapproachpossible?
Complexityofthetreatment
DependencyIsthepatientabletoattendwithnodependencyissuesandcompleteacourseoftreatment?
MaintenanceDoesthepatienthaveareasonableabilitytomaintain?
(CourtesyofTarnowskiA,EmanuelR:Wavingthe red or green flagforpragmatictreatmentoptionsinolderadults. BDJTeam 12:24-28,2025.)
standardclinicalinterventionsandminimallyinvasiveapproaches tocareareappropriate.
Therestorativephasefocusesonrestoringfunctionandtooth appearance.Olderadultsmayvaluethislessthanprevious phases.Thepersonalizedcareplanshouldbereviewedtoensure itisachievableandagreedtobeforeproceeding.
Thedentistusesthismaintenancephasetosupportoralhealth andensurelong-termsuccessoftheprevioustreatments.Asdependencyincreases,deteriorationismorelikely,sorestorative careshouldnotfocusondiligentdailycare.Dentalpractitioners shouldconsiderwhetherdeferringtreatmentwouldadversely impactthepatient’scondition,ifthecurrentdentalcondition shouldbepreservedoriffunctionalimprovementsareneeded, andifminimallyinvasiveapproachesareadvisable.Thepatient’ s abilitytocooperatewithtreatmentunderlocalanesthesiaand thecomplexityofanytreatmentrelativetotheclinician’ sscope ofpracticeandexperienceshouldalsobeconsidered.
Red flagsindicateapatientwhocan’tmanagetreatmentinthe dentalcareorwhocan’tmaintainthetreatmentoutcome.If thetreatmentdoesn’timprovefunctionoraestheticsand improvequalityoflifeforthepatient,ared fl agisappropriate. Green flagsareissuediftheclinicianandpatientcanagreeona
pragmaticvisionforwhatcanbeaccomplishedandwhenthe planisunderstoodandthepatienthasagreedtoitandiswilling toberesponsibletomaintainitorplanforfailureifthepatient’ s conditiondeteriorates.
Withagreaternumberofolderandpossiblyfrailadult dentalpatientsinthefuture,dentalpractitionersneed toplanforhowtomanagecomplexrestorativetreatmentsandcomplicationsrelatedtothepatient’sgeneralandpsychologicalhealth(Table2).The personalizedcareplansforthesepatientsshouldbe brokendownintotheircomponents.Thenthedental practitionercanevaluateifthereareobviousenablers, leadingtogreen flags,orbarriers,denotedbyred flags.Basedonthisevaluation,thedentalcareprovidercanchoosehowtoproceedandnegotiatethe situationwitheachpatientmoreaccurately.
TarnowskiA,EmanuelR:Wavingthe red or green flagforpragmatictreatmentoptionsinolderadults. BDJTeam 12:24-28,2025
Reprintsnotavailable
TMDreferstomusculoskeletaldisorderscommonlycausing non-odontogenicorofacialpain.Qualityoflifeisdiminishedin affectedpatients,whoareoftenthoseage20to40years,and thereisanadverseimpactontheeconomycausedbythesepatients’ reducedproductivity.OftenTMDisassociatedwithand exacerbatedbystressandanxiety,andmanypatientsareseen ingeneraldentalpractices.DentistsshouldunderstandtheinvestigativeanddiagnosticprocessforTMD,befamiliarwiththeconservativemanagementoptions,andknowwhentoreferpatients forsecondarycareservices.
TypesofTMD
Morethan12disordersareconsideredTMD,causingpainand dysfunctionofthejoint,masticatorymuscles,orassociatedstructures.ThemyogenousTMDgroupconsistsofmyalgia,local
myalgia,myofascialpain,myofascialpainwithreferral,andheadache.ThearthrogenousTMDgroupincludesdiscdisplacement withreduction,withreductionandintermittentlocking,without reductionwithlimitedopening,orwithoutreductionorlimited opening;osteoarthritis;subluxation,andarthralgia.
Thepatientsmostoftenaffectedarethoseintheir20sand30s. Biological,psychological,andsocialfactorscombinetoproduce thesymptoms,butTMDismorecommoninthosewithjaw injuryortraumaand/orparafunctionalhabits.Possiblemedical comorbiditiesincludeirritablebowelsyndrome,insomnia, depression,and fibromyalgia.
ThemostcommonsymptomsofTMDarenoise,pain,andmovement.Thenoisecanbeclicking,popping,orcrepitusintheTMJ thatcanbereproducedwithjawmovementssuchaschewingor

Figure1. Noticethecondylemovesduringopeningandcanbeeasierto locatetheTMJ.(ReproducedwithpermissionfromCampbellV,Mehmet T,HeffernanA:Toptipsforthemanagementoftemporomandibulardisorders. BrDentJ 238:14-17,2025.)
openingthemouthwide.ThepaincaninvolvetheTMJ,ear, temple,and/ormusclesofmastication.Occasionallyitcanextend intotheneck.PalpationoftheTMJ,masseter,ortemporalismusclecanproducethepain,andjawmovementorfunctioncan exacerbateit.Themovementisdescribedasreducedmouth opening,intermittentlocking,and,rarely,subluxationonexaminationorduring flare-upsinpatientswithchronicconditions.In addition,TMDpatientsmayalsohavesymptomsofsystemicconditions,suchasrheumatoidarthritis.
ObservationsRelatingSymptomstoDiagnosis
Patientsshouldprovideathoroughhistoryandundergoaclinical examination,butcliniciansmaynoticepossibleTMDsymptoms duringthepatient’sinitialvisit.Thedentistshouldbeableto linktheseobservationstoadiagnosisofTMD.Findingsrelated topain,noise,andmovementlistedhereshouldpromptthecliniciantoconsideraTMDdiagnosis:
Forpain:
Myalgiaispainofthemasticatorymusclesandcanbefeltonlyat thepalpationsite.Itmayalsoinvolvethemyofascialmuscleand befeltatthesiteofpalpation,withintheboundariesofthat muscle,orreferredtoareasbeyondthemuscleboundaries. PatientswitharthralgiaexperiencepainintheTMJ. TheTMDisthesourceforheadachepain.
Fornoise:
Clicking,clunking,popping,orgrindingnoisescanbeexperienced.Mostaremorecommonwitheatingbutsomeaccompanyyawning.Allseemveryloudtothepatient.

Figure2. Measuringmouthopeningfromincisaledgeswithplasticruler. (ReproducedwithpermissionfromCampbellV,MehmetT,HeffernanA: Toptipsforthemanagementoftemporomandibulardisorders. BrDentJ 238:14-17,2025.)
Discdisplacementwithreductioncausesaclicking/popping soundasthediscsitsanteriortothecondylewhenthemouth isclosedandonopeningthecondyletranslatesforward (Figure1).
Forlimitedmotion:
Patientsmaymentionhavingdif ficultyopeningtheirmouth, withasenseofrestrictionorfeelingliketheirjawislocked openorclosed.
Patientsmayalsobeabletomanuallyreducethejawbackto itsnormalposition.
Discdisplacementcaninvolvereductionandintermittent locking,butreductionmaybeabsent. Subluxationcanoccur.
UsingtheSOCRATESmnemonic,clinicianscanchecksite,onset, characteristic,radiation/referral,associations,timecourse,exacerbatingorrelievingfactors,andseverityofthepain.Three screeningquestionnairescanbeusedtofacilitatediagnosis, notetheimpactofanxietyanddepression,andassesspainintensityquantitatively.
Athoroughextraoralandintraoralexaminationisrequiredand addressesthefollowing:
Palpatethemusclesofmasticationforenlargementor tenderness. PalpatetheTMJ. Notenoises,associatedpain,andtenderness. Investigatewherethepainiscentered,whetherinthemuscles ofmasticationorthejointitself. Measuremouthopeningandanatomicalreferencepointsusingadisposablepaperorplasticruler(Figure2)oran

Figure3. Mirrorhandleillustratingwheretopalpatethemedialpterygoid muscle.(ReproducedwithpermissionfromCampbellV,MehmetT,Heffernan A:Toptipsforthemanagementoftemporomandibulardisorders. BrDentJ 238:14-17,2025.)
autoclavablemetalone.Ifnoneareavailable,thenumberof fingerbreadthsthepatient’sopeningmeasurescanbeclassifiedasnormal(3to4 fingers)orabnormal(2orfewer fingers).
Intheintraoralexamination, thecliniciancanpalpatethe medialpterygoidmusclebyinsertinga fi ngermediallyto theramusofthemandibleandinferiorlytothemaxillarytuberosity( Figure3 ).Heorsheshouldalsoobserveforsignsof toothsurfaceloss,tonguescallo ping,andridgesonthebuccal mucosaorbilaterallineaalba.T hesewillindicateparafunctionalhabitssuchasgrindingandclenching.
ManagingPatientExpectations
TheclinicianshouldclearlycommunicatetothepatientthatTMD isachronicconditionbut fluctuatesinitsexpression.Nocureis possible,butsymptomscanbemanagedsotheimpactonthepatient’squalityoflifeisminimized.Withthisapproachandproper education,patientscanbecomeexpertsatmanagingtheirown symptoms.It’salsoessentialthattheyunderstandthattheconditionisbenignandwon’tprogress.
Abiopsychosocialapproachisideal,whichmeansbeginningwith conservativemeasuresandhavingpatientsconsiderpossible sourcesofstressintheirlivesandtakemeasurestomanagethese proactively.Cognitivebehaviortherapy(CBT)reducestheintensityofpaininTMD,buthavinglessstresswillalsobebene ficial.
Between75%and90%ofTMDpatients’ symptomsimprovewith conservativemeasuresalone.Amongthesemeasuresareeducationandpainrelief,self-exercisetherapy,thermalmodalities,selfmassage,dietmodi fication,andcurbingparafunctionalhabits.
Painreliefgenerallyisachievedwithoralnonsteroidalantiinflammatorydrugs(NSAIDs),withibuprofengelappliedto theskinatthecondylesorcoupledwithwarmorcoldcompressestomanageextra-oralpain.Jawexercisesandphysiotherapyhelptorelaxthemusclesandallowadisplaceddiscto bereturnedtoitsnormalposition.Eatingasoftdiet,avoiding openingthemouthtoowidely,andreducingchewingbycutting foodupforeaseineatinghavebeenhelpful.Patientscanalsodiscontinuerepetitivehabitssuchasnailbitingorchewinggumand learntostifleorsupportayawntoavoidstressingtheTMJ.Some patientsrespondtosplints,buttheyaregenerallynotconsidered theprimarytreatmentmodality.Thesplintsneedtobecomfortableforthepatientandareusuallywornatnighttocounteract grindingandclenchingduringsleep.Somepatientswithawake bruxismmayalsowearthesplintduringthedaytime.
Whenconservativemeasuresdon’tachievepainrelief,it’ s likelythatarestrictionlimitingmouthopeningoraclosed lockispresent.Becausethisaffectsqualityoflifeandnutritionalintake,areferralforsecondarycareisappropriate. Thereferralshouldincludealistoftheconservativemeasures thathavebeentaken.
Varioustreatmentscanbedoneinsecondarycarefacilities. Theseincludemagneticresonanceimaging(MRI)oftheTMJto identifydiscdisplacement;pharmacotherapysuchasduloxetine, cyclobenzaprine,oroff-labelneuromodulatordrugssuchastricyclicantidepressants,selectiveserotoninreuptakeinhibitors, benzodiazepines,andgabapentin;botulinumtoxintypeAinjections;TMJsurgery;TMJmeniscopexy;orcompleteTMJreplacementandsubsequentreplacement.
TMDtreatmentrequiresthedentalpractitionertobe cognizantofthecausativefactors;thepossiblestructuresinvolved;thepain,noise,andmotioneffects;and factorsthatexacerbatethepatient’scondition.Conservativetreatmentsaregenerallyabletomanage mostpatients’ symptomsandimprovetheirquality oflife.PatientsshouldbeawarethatTMDischronic andhasnocure,butismanageableinmostcases withlifestylechangestominimizestressandanxiety andprotectthestructuresthatareinvolved.
CampbellV,MehmetT,HeffernanA:Toptipsforthemanagementoftemporomandibulardisorders. BrDentJ 238:14-17,2025
Reprintsnotavailable
Dentalprofessionalsareathighriskfordevelopingmusculoskeletaldisorders(MSD),withtheneck,back,shoulder,and wristthemostcommonsitesofpain.Clinicians,whetherdentists,dentaltherapists,ordentalhygienists,adoptstaticpositionsandholdthemforanextendedperiodoftimesothat theycanseewellandgainproperaccesstothepatient ’sworking site.Oftentheseposturesandthelengthoftimetheyareheld canleadtothedevelopmentofMSD,producediscomfortin deliveringcare,andshortenthedentist’scareer.MSD-related paincausesreducedproductivity,frequentabsences,andsometimesevenearlyretirement.Dentalprofessionalsneedtoequip themselveswiththetoolstopreventandmanageMSDand therebyavoidlong-termconsequences.Sometoptipsare offeredtoaddressstandingandseatedposture,sittingata screen,adjustingthepatient,useoflightingandsharpinstruments,purchasingasaddleseatandloupes,andmovingand stretchingregularly.
Posturereferstohowyouholdyourbody,whethermoving(dynamic)oratrest(static).Posturediffersdependingonwhether youarestanding,operating,orsitting.
Thespinehas3curvesthatneedtobemaintained.Ifyou’ ve developedpoorpostureovertheyears,youneedtoretrain yourbodytoachievegoodposture.Weightdistributionisan essentialpartofposture,withthebodybuilttodistributeits weightacrossyourjointstoreducestrainandstress.Toachieve agoodweightdistribution,youshouldstandwiththefeethip widthapartandtheanklebonesunderthehipbones.Keepthe kneessoftandnotlocked.Gentlytiltthepelvisbackwardandforward,thenallowittosettleinaneutralposition.Shrugtheshouldersafewtimes,thenbringthemdownandbacksotheshoulder jointsareoverthehipjointsandhorizontal.Relaxthearmsdown atyoursides,letyourneck,jaw,andeyesrelax,andfeelthe crownofyourheadlift.Thesemovementswillmakeyoufeel tallerandmoreevenlybalanced.
SeatedPosturefortheDentist
Beginbysittinginastable,upright,symmetricalposition,withthe lowerlegsvertical.Lookperpendiculartothesurfaceyouare workingonbydirectvisionorinamirror.Theoralcavityshould beatmid-sternumheight.Placetheforearmshorizontalorno morethan25degreesupfromhorizontalandtucktheelbows in.Don’ttilttheheadmorethan20degreesinanydirection.
Maintainthispositionfor80%ofyourworkingtime,moving thechairorthepatientsoyoucanrestinthisposture.Theother 20%ofthetime,youcanworkonpatientswhocan’tliesupine (pregnantwomenorbariatricpatients).Keepthedeliveryunit atelbowheighttoavoidreachingtoofar.Toavoidprolonged staticposturing,getupandmoveregularly.
SeatedPosturefortheDentalNurse
Situprightandhigherthanthecliniciansothatyoureyesare about10cmabovethedentist’seyes.Standupifyouneedto.
Adjusttheheightofthedesk,chair,table,orscreentoachieve optimalseatedposition(Figure4).Withbothfeet flatonthe floor,lowerlegsvertical,maintaina90-degreeanglebehind theknees.Situpstraightbutrelaxtheshouldersandallowthe backofthechairtosupportyou.Ensureyourshoulderjoints areaboveyourhipjoints,andkeepyourarms fl atonthedesk ortable.Thetopofthescreenshouldbelevelwithyoureyes, andthescreenshouldbeaboutanarm’slengthaway.
Oncethepatientissupine,getintogoodpostureyourself.Ensure thepatienthasplacedhimselforherselfintotheangleofthe chair.Adjustthedoublearticulatingheadrestcorrectly.This maytakepracticewithacolleaguetodeterminethemost comfortableposition.Theheadrestshouldsupportthepatient’ s headonthemastoidboneatthebackoftheskull.Insertawipeablecushionorfoldedtowelifthereisalonggapbetweenthe chairandheadrest.Adjusttheheadrestsothepatient’schinis upwhentreatingupperteethanddownwhentreatinglower teeth.Havethepatientadjusthisorherheadasneededto achievethebestposition.
Theproperuseoflightingrequiresthatyoupositiontheoperatinglightsothelightisparalleltoyourlineofsight.Usethe mirrortoreflectthelightintotheoralcavitywithoutcreating shadows.Ifthelightisonyourloupes,don’tforgettousethe operatinglightsothatthedentalnursecanseeaswell.
Sharp,ergonomicallydesignedinstrumentsarebestfordental work.Theyshouldhavealargediameterandatexturedgrip. Thetexturingmakesiteasiertograspandisbene fi cialduring scaling,reducingtheamountofforceneeded.Minimizehandfatiguebyensuringtheinstrumentsarekeptsharp.

Figure4. Howtositatascreen.ContainspublicsectorinformationpublishedbytheHealthandSafetyExecutiveandlicensedunderthe https:// www.nationalarchives.gov.uk/doc/open-government-licence/version/3/ (CourtesyofRobinsonC,MysoreD,McCollE,etal:Toptipsforpreventing musculoskeletaldisordersandoptimisingposturefordentalprofessionals. BDJTeam 12:10-13,2025.)
Ergonomicseatsandmagnificationloupesareagreatinvestment thatcanhelpinachievinggoodposture.Ergonomicseats,especiallysaddleshapedones,allowyoutositwithacorrectlyaligned spine,soit’simportanttotryseveraloutuntilyou findtheright seatforyou.Tilttheseat5to15degreestoachieveacloserpositiontothepatientwithoutstrainingtheback.Ifthechaircan’t betilted,youcaninsertawedge-shapedcushion.
Magni fi cationloupeswithadirectlightsourcehelptoprovide bettervisionandimproveposturewhilereducingmusculoskeletalpain.Youshouldchooseloupesthatsuityourdailyneeds, havea40-degreeangleofdeclination,andhavealightthat goeswiththem.Generaldentistryneedsnomorethan3.5x magni fi cation,withhighermagni fi cationreservedforspecialty dentistry.Refractiveloupeshelptoensureyourneckwillstay upright.
Staticmusclepainoccurswhenaconstantloadonthemusclesis maintainedforalongperiodoftime.Youshouldstandupand movebetweenpatients.Walkingorbikingtotheof ficeorgoing forashortwalkatlunchtimehelpstocombatstaticmusclepain. Stretchingoftheneck,shoulders,lowerback,hands,andwrists shouldbedoneregularly,especiallybetweenpatientsandat theendoftheday.Duringlongprocedures,takeafewseconds toevaluateyourpostureandthestatusofanymusclestrain. Evenwhennotattheof fice,youcando10minutesofstretching eachdayorjoinaPilatesoryogaclasstostretchtheentirebody. Youmayalsoseekadvicefromaphysiotherapist,osteopath, chiropractor,ormassagetherapist.
Takingafewminutestoensureyourbodyisrelaxed andreadytoassumeahealthyandstablepostureso youcanworkwithoutpainisapracticalwaytokeep fromdevelopingMSD.Thetipsgivenwillhelpin assumingthecorrectpostureforthetaskathand andcancontributetoahealthierwaytoperform dentistry.Thebenefitsde finitelyoutweightheminor adjustmentsneeded.
RobinsonC,MysoreD,McCollE,etal:Toptipsforpreventing musculoskeletaldisordersandoptimisingposturefordental professionals. BDJTeam 12:10-13,2025
Reprintsnotavailable
AddressingCariesandHypomineralizationofFirst PermanentMolars
Thehealthofthe firstpermanentmolar(FPM)isanessential considerationbecausethistoothcanbecomecompromised andcausesignificantnegativeimpactsforthechild,thefamily, andthehealthcaresystem.Thepreventionorarrestofdental diseasessuchasdentalcariesormolar-incisorhypomineralization(MIH)requiresanunderstandingoftherisksFPMsface, sharingthedecisionforcarewithbothpatientandparents,and selectingthebestcourseoftreatmentthatminimizesthechance thatfurtherinterventionswillbeneededinthefuture.
AcompromisedFPM(cFPM)ismostofteninvolvedwithdental cariesorMIH.Thesedisorderscanhaveasigni ficantimpact, bothdirectandindirect,onthepatient,family,andsociety.
FPMsarethepermanentteethmostsusceptibletodentalcaries. Byage15years,aboutaquarterofFPMteethwillhaveobvious caries,comparedtojust9%ofthesecondpermanentmolar. BecausetheFPMisthe fi rstpermanenttoothtoerupt,itspends
thelongesttimeinthemouthandthereforeismorelikelyto developdentalcariescomparedtotheadjacentpermanentteeth.
MIHisadevelopmentalabnormalitythatcausesreducedmineral contentintheenamelofFPMsandsometimesalsoofincisors.Evidenceappearstoindicatethatepigeneticchangesinthegenome, causedbyenvironmentalfactors,maybethemostlikelycauseof MIH.About27%ofchildrenwhoarediagnosedwithMIHwillneed clinicalinterventionsbecausethepoormineralcontentleadstoa lackofstructuralintegrity,causingmechanicaldeteriorationof toothstructureandpost-eruptivebreakdown.Themacroscopic appearanceoftheteethiscompromised,makingthemharderto treatandincreasingtheirsusceptibilitytodentalcariesbecause theyaccumulateplaqueandbacteriapenetratetheirenamel.
Variousmeasurescanbetakentopreventthedevelopmentof cFPMsduringtheperiodswhencompromisesaremostlikely tooccur.Thesemeasuresincludeoralhygieneandtoothbrushing, fluorideapplications, fissuresealants,andtheuseofsilverdiamine fluoride.Inaddition,publichealthmeasurescanhelp topreventdiseaseatapopulationlevel.
Preventionofplaqueaccumulationcanbeachievedbyfocusingon cleaningaroundtheeruptingtooth.Dentalprofessionalsshould teachthechildandparentstochangethetoothbrushposition fromamesial-distalplacementtoabuccal-lingualdirectionwhen thetoothispartiallyerupted,thenreverttothenormalpositionafterit’sfullyerupted.Parentsshouldalsoassistthechildwithtoothbrushinguntilthechildcomprehendstherightapproachandhasthe manualdexteritytobrushindependently.Plaquedisclosurehelps bothchildandparenttounderstandthescopeoftheproblem andmaymotivatethemtoachieveoptimalplaqueremoval.
Fluorideexposuremaintainsaconcentrationintheplaquebiofilmthatencouragestheremineralizationofthetoothsurface. Fluoridedeliverycanbeintoothpaste,water,milk,mouthrinses, toothgels,orvarnish.Fluoridatedtoothpasteisoneofthemost effectivemethods,withtwicedailybrushing,supervisedbyparentsifneeded,therecommendedpractice.Fluoridevarnishcan beappliedtoFPMsandadherestothesurface,providingslow releaseof fluoridetovulnerableareas.DryingtheFPM fi rstincreasesadherence.
Aresin-based fissuresealanthasbeenassociatedwithareduction intheabsolutecariesriskof11%to51%forupto48months. Whenadhesivesystemsareusedbeforeapplyingthe fissure sealant,increasedpenetrationandretentionrateshaveoccurred. Cavitatedenamelandmicrocavitiesindentincariouslesions bene fitfromresin-bonded fissuresealants.Childrenwithmild
hypomineralizationoftheFPMcanalsoreceive fissuresealants. Patientsshouldundergoregularclinicalandradiographicexaminationstorevealanylesionprogression.
Thesesealantsaresuperiortoglassionomersealantsintermsof clinicaleffectiveness,sotheirplacementshouldbea first-line choice.However,childrenwithlimitedcomplianceorwho havecompromisedmoisturecontrolmaybenefitfromaglass ionomersealantasaninterimoption,reservingtheresin-based sealantforlater.
Silverdiamine fluoride(SDF)maybeconsideredwhentheFPM hasbecomecavitatedandthechildisuncooperativeorthetooth isinavulnerableposition,suchaspartiallyerupted,sothata restorationcan’tbeplaced.SDFusebuysthedentalprofessional sometimebeforede finitivemanagementstrategiesmustbeemployed.ThedrawbackswithSDFincludetheblackdiscoloration ofthetooth,whichshouldbediscussedwiththepatientandparentsbeforeusingtheSDF.Ifit’sdeterminedthatthechildneeds anFPMrestoredwithSDF,thedentalprofessionalshouldusea total-etchapproachtoovercomereducedbondstrengthsbetweencompositeandSDF-treatedenamelanddentin.
Communitywater fluoridation,supervisedtoothbrushingprograms,andtaxationofsugar-sweetenedsugarbeveragesaremeasurestakenatapopulationleveltopreventoraldisease. Adopting,implementing,andencouraginguseofamultifocused preventiveapproachisawaytosigni ficantlyreducehavingyoung patientsenteracontinuouscycleofrestorativetreatmentthat wearsawayatthenaturaldentition.
ItcanbechallengingtodeterminethebestinterventionforprotectingFPMsfromcompromiseortomanageatooththathas becomecompromised.Alldecisionsshouldbemadejointly withthepatient,theparents,andtheoralhealthcareprofessional.Youngpatientstendtofavorthisapproachifatrusting relationshiphasbeenformedwiththeclinician.Oralhealthpractitionersshouldbetrustworthy,sharealltheneededinformation,andevidencetheirconcernforthepatient’swell-beingto gaintheconfidenceofayoungperson.Parentsandguardians mustalsobeincluded.Theseindividualscanencouragetheirchildrentoexpresstheiropinionsandpreferencesratherthan dictatewhattheyassumearetheirchild’sviews.
Beforemakinganychoice,thedentalcareprofessionalmustfully assessthechild’sdevelopingdentitionaswellasevaluatethepatient’sandparents’ abilitytounderstandandcomplywithtreatmentneeds.Thepossibletreatmentsshouldbediscussed,with considerationsatthepatientlevel,themouthlevel,andthetooth level(Table1).
Table1. FactorstobeConsideredWhenTreatmentPlanningcFPMs
PatientlevelMouthlevelToothleve
PatientpreferencesNumberofaffectedcFPMsSizeandlocationofdefect
RelevantmedicalhistoryOveralldentalhealthNumberofsurfacesinvolved
Ageandlevelofco-operationDentaldevelopmentalegbifurcationofsecond permanentmolars
Presence/absenceofsymptomsOrthodonticneed,suchaspresence/absence crowding,hypodontiaetc
Presence/absenceofpost-eruptivebreakdownin hypomineralisedtooth
Pulpalinvolvement
CurrentaccesstogeneraldentalservicesPresenceofthirdpermanentmolarsHistoryofdentalabscess/facialcellulitis Accesstospecialistcare (paediatricdental/orthodontic)
(CourtesyofTaylorGD,BulmerV:Advancesinknowledgeandpracticebenefitingthehealthandmanagementof firstpermanentmolarsinchildren. BrDentJ 238:92-98,2025.)
DentalcariesandMIHaredifferentconditions,sothereare differentinterventionsthatmustbeconsideredbasedonthe conditionpresent.InMIH,mostoftheotherposteriorpermanentteethareunaffected,sotheoptiontoextracttheFPMis moreoftenfavored.However,recentresearchindicatesrestorationandretentionofhypomineralizedmolarsismoreinlinewith minimalinterventiondentistryandfavoredbypatientsinparticular.Indentalcaries,allthepermanentteethareatrisk,withthe
choiceofinterventionbasedonthepatient’sandparents’ engagementinthepreventivestrategies.Thediseaseburdenmaybe minimalandfavorarestorativeapproachtomanagement.
The3generalmanagementstrategiesforcFPMsareactivemonitoring,restoration,andextraction.Itshouldbenotedthatlittleclinicalevidencefavorsrestorationorextractionovertheother option.

Figure4.A-D, Ahypomineralizedlowerleft firstmolar(36)withpost-eruptivebreakdown (A) whichhasundergonepartialhypomineralizedenamel removal (B) andthencompletehypomineralizedenamelremoval (C) leavingthemarginsoftherestorationonsoundenamel (D).(CourtesyofTaylorGD, BulmerV:Advancesinknowledgeandpracticebenefitingthehealthandmanagementof firstpermanentmolarsinchildren. BrDentJ 238:92-98,2025.)
Inactivemonitoring,it’sacceptedthatthetoothislikelyto worsenwithoutintervention.Therisksassociatedwiththis approachincludeahighchancethatdentalpainandsubsequent infectionorsepsiswilloccur.Thisoutcomeshouldbediscussed withthepatientandparents.Anyfuturetreatmentwillhaveto dealwithamoredif ficultcompromisedFPM,aremoreexpensive,andwillbeassociatedwithlesscertainresults,eventually leadingtoextractionofthetooth.
Withtheadvancesinrestorativematerialsandtechniques, restorationisoftenaviableoptionforFPMswithdentalcaries. Extendedetchingandapre-restorationrinsewithsodiumhypochloritehavebeensuggestedtoovercomedecreasedbond strengthsandhigherfailureratesinhypomineralizedenamel comparedtorestorationstosoundenamel.Totalremovalof allhypomineralizedenamelhasalsobeensuggested,ashasaselectiveremovalofthecompromisedenamel.Theseoptions reducetheriskofiatrogenicpulpexposurethatcouldmitigate againstbondingproblems(Figure4 ).Theymayalsoovercome structuralissuesrelatedt ohypomineralizedenamel.
Ifthepulpisexposedorthepatientdevelopssymptoms,endodontictreatmentsuchasvitalpulptherapiescanbeusedfor cariousaswellashypomineralizedmolars.Vitalpulptherapieshaveasuccessrateofabout91%forpartialaswellas coronalpulpotomies.Thedrawbackistheperpetuationof therestorativecyclewithincreasinglylargerrestorationsuntilnotoothsubstanceremainstorestoreandextraction mustbedone.
Ifthetoothisextracted,thereisnoneedtomaintainarestoration,whichsomepatientswillprefer.Youngpatientsandadults tendtoperceiveextractionasmoreinvasivethanrestoration. Extractioninayoungchildoftenrequiresrepeatedadjunctive treatments,includingsedationandgeneralanesthesiafortreatment.Theseareassociatedwithclinicalrisksandcosts.
Ifextractionistheonlyfeasibleoption,spontaneousclosureof thespacecouldoccur,negatingtheneedfororthodonticspace closureorprostheticreplacement.Theoralcarepractitioner shouldbeawareofradiographicprognosticfactorsthatimprove thechancesofspontaneousclosure,althoughthesefactorsdon’t guaranteeitandunfavorabletoothmovementortippingofadjacentteethcanstilloccur.
TheextractionofanupperFPMmightbedonetocompensatefor extractionofthelowercFPM.Thisshouldbedonewithcautionand reservedforpatientswhohaveaclearocclusalrequirementor whentheupperFPMwillbeunopposedforasignificanttimeperiod.
RemovalofcFPMswilllikelyhaveanimpactonthirdpermanent molarposition.It’sbeennotedthatthirdmolarsofpatients whosecFPMswereextractedbetweenages8and11years havemovedsignificantlymoremesiallythanthemolarsofpatientswhohadnoextraction.Asaresult,thethirdmolarmay eruptintoamorefavorablepositionandreducebothimpaction andassociatedmorbidities.
WhenFPMsareatriskorcompromised,thedental careprofessionalmustinstitutemeasurestoprotect themaswellasintervenetokeepthesituationfrom progressing.Throughouttheprocess,thepatient andparentsshouldbeapartofthedecision-making process,withtheoptionsselectedbasedoneachindividualcase.
TaylorGD,BulmerV:Advancesinknowledgeandpractice bene fitingthehealthandmanagementof firstpermanentmolars inchildren. BrDentJ 238:92-98,2025
Reprintsavailablefrom GDTaylor;e-mail: Greig.taylor@newcastle.ac.uk
Sepsisdevelopswhenthebodyhasanabnormalresponseto aninfection.Forunknownreasons,thebody’simmunesystem occasionallydealswithaninfectionbyattackinghealthyorgans andothertissues.Asaresult,sepsisistheleadingcauseof deathintheworld,withamortalityofmorethan20%,but
morethan40%ofsurvivorsalsosuffersigni ficantconsequences,suchaspost-traumaticstressdisorder(PTSD),amputations,failureofmajororgans,braindamage,chronicpain, andchronicfatigue.Thosewhosesepsisiscaughtearlyand treatedcanmakeafullrecovery,butthesegoodoutcomes couldbeimprovedbygreaterpublicandprofessional

Figure1. Signsandsymptomsofsepsis.UsedwithpermissionfromFirstAidforLife www.firstaidforlife.org.uk and www.onlinefirstaid.com.(Courtesyof HammettE:Sepsis acompleteguide. BDJTeam 12:80-82,2025.)
awarenessofthesignsandsymptomscharacteristicofsepsis. Unfortunately,theearlysignalsofsepsisareoftenmissed, evenbyprofessionalhealthcareproviders.Sepsisfactswere shared,includingitscauses,possibledamageproducedinthe body,andthepatientsmostcommonlyaffected.Thekeysto recognizingandtreatingthesignsandsymptomsofsepsisin adultsandchildrenwereoutlined.
Sepsisbeginswithaninfectioninthebody.Thisinfectionmay occuraftersurgeryortraumaandcanmayaffectstructuresin anyareaofthebody.Theinfectionsseenmostofteninclude pneumonia,urinarytractinfections,intra-abdominalinfections, skininfections,woundscausedbytraumaorsurgery(including dentalinfections),andsofttissueinfectionssuchasalegulcer.

Figure2. Signsandsymptomsofsepsisinchildren.UsedwithpermissionfromFirstAidforLife www.firstaidforlife.org.uk and www.onlinefirstaid.com (CourtesyofHammettE:Sepsis acompleteguide. BDJTeam 12:80-82,2025.)
Thebacteriainvolveddon’tnormallycauseillness.Between2% and3%ofcasesoccuraftertrauma.Meningitiscausesabout1% ofcasesinadultsbutabout10%ofcasesinchildren.Viralmeningitisisn’tusuallylife-threatening,butbacterialmeningitis,which ismuchlesscommon,canleadtosepsis.However,bothtypesof meningitisareserious,andcommonearlysignsandsymptoms shouldberecognizedsotreatmentcanbestarted.
Theinflammationrelatedtosepsisinjuresthebody’stissuesand organs,withitsspreadinvolvingthebloodstream,sothesepsis cantravelthroughoutthebody.Thebreakdownincirculation canaffectalltheorgansofthebody,includingthebrain,lungs, heart,skin,andkidneys.Ifcirculationtotheextremitiesis compromised,amputationcanberequired.
Sepsiscandevelopinanyoneandnosinglespeci ficsignordiagnostictestcanidentifyit.Themostcommonpatientsarevery youngchildren,olderadults,andthosewithunderlyinghealth conditions,buteven fitandhealthypersonscandevelopsepsis. Personswhohavedentalworkcanhavebleeding,whichallows theingressofbacteriaandthedevelopmentofinfections.Dental professionalsmaygivepatientswhoaresuspectedtohavean infectionacourseofantibiotics,especiallyiftheyhaveacompromisedorweakenedimmunesystem.Patientsshouldbeurgedto completethecourseofantibioticstoensurethebestresponse.If theinfectionissevere,itmayrequiredrainagetoreducepainand swelling.
Healthcareprofessionalsshouldexplaintopatientswhatthe earlysignsofinfectionareandadvisethemtointervenewith earlytreatmentorseekprofessionalcare.Patientsshouldalso bemadeawareofthemoreserioussignsandsymptomsofsepsis sotheyknowwhattolookforandwhenurgentmedicalcareis required.Somepatientsmayneedtotakeprophylacticantibioticsbeforeanyinvasivedentaltreatmenttoguardagainst infection.
Theinitialsymptomsofsepsisinadults(Figure1)canresemble the fluandfeelingseriouslyunwell.Theindividualmayhavesigns offeverwithcoldhandsandfeetorevenanabnormallylowtemperaturebutfeelingveryunwell.Amongthecommonsignsand symptomsarethefollowing(occurringinnoparticularorder):
Dislikeofbrightlights
Stiffneck
Vomiting
Severemusclepain
Drowsiness,withdifficultystayingawake
Pale,blotchy,orspottyorrash-coveredskin
Convulsions/seizures
Feverwithcoldhandsandfeet
Confusionandirritability
Inchildren(Figure2),thesignsandsymptomsofsepsiscan includehavingthefollowingconditions:
Abnormallycoldtothetouch
Mottled,bluish,orverypaleskin
Rashthatdoesn’tfadewithpressure
Breathingveryfast
Convulsions
Extremelethargyordif ficultywakingup
Forchildrenunderage5years,thereshouldbeconcernifthe childisn’tfeeding,isvomitingrepeatedly,andhasn’turinatedor hadawetdiaperfor12hours.
Anyofthesesignscanindicateaseverelyillchildwhoshouldbe takenurgentlytothedoctor,withtheadultmentioningaconcern thatthechildmayhavesepsis.
Sepsisisaseriousproblemthatcanhavelifelongconsequencesor resultindeath.Boththepublicandhealthcareprovidersshouldbe awareoftherangeofsignsandsymptomsthatmayindicatethata simpleinfectionhastriggeredthebodytooverreactandbecome septic.
Sepsiscanaffectanyone,withmorethan240,000 peopledealingwithsepsiseachyear.IntheUnited Kingdom,anestimated5peopledieofsepsisevery hour.Becausetheearlysignsandsymptomscanbe difficulttoconnecttosepsis,everyoneshouldbe educatedaboutwhattolookfortodetectitasearly aspossible.Dentaltreatmentoftencausesbleeding, whichcanopenthedoortobacteriaenteringthe bodyandultimatelycausesepsis.Dentalcare providersarediligenttotakemeasuresthatensurea cleanfacilityandcleanlinessamongthoseproviding care,butpatientswhohaveanyofthesignsof possiblesepsisshouldbecarefullymanagedto ensurethebestpossibleoutcomes.
HammettE:Sepsis acompleteguide. BDJTeam 12:80-82,2025
Reprintsnotavailable
Bittermedicinesaren ’tunusualtreatmentsforchildren,but themostcommonwaytohelpthemedicinegodownisto usesugar-basedsyrupsratherthanpillsortogivethechild asugarydrinktowashthecapsuleortabletdown.Sucrose isthemostcommonsugaraddedtomedicationsandhas theadvantagesofbeinginexpensive,non-hygroscopic,and easytoprocess.Thedownsideofsucroseisitspotentialto contributetothedevelopmentofdentaldecay.Dentalcaries, themostprevalentdiseaseoftheoralcavity,anduntreated dentalcariesinpermanentteeth,themostcommonhealth conditionintheworld,arewidelyfoundandrequire concertedeffortstominimizetheirdamage.Untreatedcaries causespain,leadstoinfection,andcanrequireextractionsof teethundergeneralanesthesiainchildren.Schooldaysare missed,parentshavetotaketimeoffworktovisittheir child ’sdentist,andtoothextractionsareexpensive,sodental cariesaffectsmuchmorethanthechild ’soralhealth.The cariesprocess,howtoreducecariesriskorsusceptibility, theadvantagesanddisadvant agesofsugar-containingand sugar-freemedicines,andrecommendationstoreducethe dentalriskofsugar-containingmedicineswerediscussed.
Thecauseofdentalcarieshasmultiplecontributingfactorsbut essentiallyinvolvestheinteractionofatooth,bacteria,fermentablecarbohydrates,andtime.Theseinteractionsofthesecomponentscaneventuallydestroytoothsubstanceiftreatment isn’tinitiated(Figure1).
Thehost-microbialinteractioninvolvesseveralsteps.Itbegins withdentalplaqueformation,inwhichbacteriaattachtotooth surfacestoformplaque.Acidisthenproducedasthebacteria fermentsugarsandothercarbohydratesinfood.ThepHofthe environmentbecomesloweredasaresult.Thisacidicenvironmentdissolvesordemineralizestoothenamel.Remineralization canoccuriftheacidicenvironmentisneutralizedandthepHof theoralcavitybecomesstabilized.Duringremineralization,mineralssuchascalciumandphosphate,whicharepresentinsaliva, areredepositedintotheweakenamel.Iftheacidicenvironment isn’tstabilized,thedemineralizationcontinues,eventuallypenetratingtheenamelandattackingthedentin,whichisweaker
thanenamel.Decaythencanreadilyspreadthroughthetooth andcausecavities.
TheStephancurveillustrateshowtheoralpHdipsafter eatinganddrinkingfermentablecarbohydrates(Figure2). HavingapHlessthan5.5allowsdemineralization,making thisthecriticalpHforenamel.Remineralizationrequiresa riseinpHabove5.5.Ifthisrisedoesn ’toccur,thelonger theoralpHremainslessthan5.5,themoresusceptibleteeth aretocariesdevelopment.
Effectivetoothbrushingremovesmuchofthesoftdentalplaque, withtheadditionof fluoridetoothpastehelpingtostrengthenthe teeththroughremineralizationofthetoothsurface.However, dietisthemostimportantcomponentinreducingdentalcaries. Bylimitingthefrequencyandamountofsugarconsumedeach day,thetimeteetharesusceptibletodecayisalsolimited.Dentiststrytoeducatepatientstoonlyconsumesugarsatmealtimes andlimitanysugar-containingsnacks.
Ifchildrenaretakingsugar-basedmedicines,especiallyifthemedicinesaregivenatnon-mealtimesmultipletimesaday,thecariogeniceffectisincreased.It’sespeciallyimportanttoavoidsugary medicinesatbedtimebecausesalivaisn’tabletoeffectivelyremineralizethetoothsurfacesatnight.

Figure1. Extensivedentalcariesinachild.(CourtesyofHowardJ,Dave M,ReynoldsL,etal:Thebittertruthregardingsugarymedicinesinchildren. BDJTeam 12:116-120,2025.)
Figure2. TheStephancurve – aftermealsareconsumed,theincreaseinsugarreducesoralpHbelowthecriticalpHofenamel(pH5.5),resultingintooth demineralization.(CourtesyofHowardJ,DaveM,ReynoldsL,etal:Thebittertruthregardingsugarymedicinesinchildren. BDJTeam 12:116-120,2025.)
Sucrose-containingmedicinescauseadropindentalplaquepH, andlong-termuseofsugaryoralmedicationhasbeenlinkedto rampantdentaldecay.Asaresult,clinicianshaverecommended theuseofsugar-freemedicinesinpatientswithchronicdiseases.Someevidenceindicatesthattheuseofsugar-freemedicationsforpatientsathighbaselineriskforcariesisespecially appropriate,whereastheuseofsugar-freemedicinesforlow caries-riskindividualswhohaveashort-termillnessmaybe lessclinicallyjusti fi ed.
Sugar-freedrinksandsnackscanalsohelpreducetheriskof dentalcaries.It ’simportantthatchildrennotbegivensweet drinksorsugarysnackstomakethemedicinemorepalatable tothem,whichwouldbecounterproductivewithrespectto cariesreduction.
Someevidencepointstothefactthattheprescriptionof sugar-freemedicineslong-termforchildrenwhoaremedicallycompromised,havepoororalhealth,suffersocialdeprivation,havelearningdisabilities,orrequirerestrictedeating patternsisespeciallyimportant.It'sbeenshownthatsocial deprivationisnotonlyariskfactorforpoororalhealth butalsoanindicatorofmoreseveredentaldisease.Having learningdisabilitiescanbeassociatedwithastruggleto
copewithdentaltreatmentwhenitisneeded.Therefore, effectivecariespreventionstrategiesareespeciallyimportant inthesehigh-riskpatients.
Parentsandcaregiversshouldbeeducatedregardingtheeffectsofsugarinrelationtotoothdecay.Theyshouldalso betoldwhenamedicationcontainssugarandinstructedto givethemedicationatmealtimes.Medicationsthatareprescribedtobegivenatbedtimeshouldbeadministeredatleast 30minutesbeforethechildgoestobedtoallowtimeforthe oralenvironmenttoregainneutralstatusbeforebrushingthe teeth.Ifthesugar-containingmedicationmustbegivenata timeseparatefrommealtime,thechildshouldusea fluoride-containingmouthwashaftereachdosetominimize theriskoftoothdecay.
Thehealthcarepractitionerswhoprescribemedications, especiallyforchildren,shouldbeawareoftheeffectsof sugar-containingmedicinesonteeth.Thepreferenceshould beforsugar-freemedications.Inaddition,electronicprescribingsystemsshoulddefaulttosugar-freeformulations,if
Table1. CommonlyPrescribedSugar-containingMedicinesforPaediatricPatientsandSugar-freeAlternatives.
MedicationwithsugarPrescribedfor
Sugarcontent g/5ml*
Sugar-freesubstitution
Loratadine5mg/5mloralsolutionAllergicconditions3.0gLoratadine5mg/5mloralsolutionsugar free
Piritonsyrup(chlorphenamine2mg/5ml oralsolution)
Amoxicillin125mgand250mg/5mloral suspension
Allergicconditions2.4gChlorphenamine2mg/5mloralsolution sugarfree
Bacterialinfections2.7gAmoxicillin125mgand250mg/5ml sugar-freeoralsuspension
Azithromycin200mg/5mloralsuspensionBacterialinfections3.7gAzithromycin200mg/5mloralsuspension sugarfreeavailablebyspecialorder
Cefalexin125mgand250mg/5mloral suspension
Ciproxin(ciprofloxacin250mg/5mloral suspension)
Clarithromycin125mgand250mg/5ml oralsuspension
Co-amoxiclav250mg/62mg/5mloral suspension
Co-trimoxazole80mg/400mg/5mloral suspension
Bacterialinfections
3.0gCefalexin125mgand250mg/5mloral suspensionsugarfree
Bacterialinfections1.4gConsiderprescribinganalternativesugarfree fluoroquinoloneantibiotic
Bacterialinfections3.1gConsiderprescribinganalternativesugarfreemacrolideantibiotic
BacterialinfectionsUnknownCo-amoxiclav250mg/62mg/5mloral suspensionsugarfree
Bacterialinfections2.5gCo-trimoxazole40mg/200mg/5mloral suspensionsugarfree
Flucloxacillin125mg/5mloralsolutionBacterialinfections3.2gFlucloxacillin125mg/5mloralsolution sugarfree
Metronidazole200mg/5mloral suspension
Phenoxymethylpenicillin125mgand 250mg/5mloralsolution
Bacterialinfections1.7gConsiderprescribinganalternativesugarfreeantibiotic
Bacterialinfections2.9gPhenoxymethylpenicillin125mgand 250mg/5mloralsolutionsugarfree Lactulose3.1-3.7g/5mloralsolutionConstipationUnknownLactulose10g/15mloralsolution15ml sachetssugarfree
Lansoprazole15mgorodispersibletabletsGastrointestinalulceration,GORD,H. Pyloriinfection 13.8mgConsiderprescribinganalternativePPI
Morphinesulfate10mg/5ml oralsolution
Pain2.3gMorphinesulfate10mg/5mloralsolution sugarfreespecialorder
Brufen(ibuprofen100mg/5mlsyrup)Painandinflammation3.3gIbuprofen100mg/5mloralsuspension sugarfree
Paracetamol120mgand250mg/5mloral suspensionpaediatric
Painandpyrexia3.0gParacetamol120mgand250mg/5mloral suspensionpaediatricsugarfree
*These figuresrelatetoatleastoneUKlicensedproduct.
(CourtesyofHowardJ,DaveM,ReynoldsL,etal:Thebittertruthregardingsugarymedicinesinchildren. BDJTeam 12:116-120,2025.)
possible.Ifnosugar-freealternativeisavailable,themedicationsshouldbeprescribedtobegivenwithmealsiffeasible.
Sugar-freemedicinesshouldbepromotedinpharmacies.Inaddition,pharmacistsshouldbegiventheauthoritytodispensesugarfree-preparationsasappropriate.
Sugar-containingmedicationsshouldhavelabelswarningabout theriskoftoothdecayandadvisingthatthesemedicationsbegiven atmealtimes.Noncariogenicsweetenersshouldbepreferred oversucrosefordrugs.Thesecompaniesshouldalsoexplore developingsmallertabletsandcapsulesformedicationsthatchildrenwillbetakingtohelpthemhandlesolidformulations.
ClinicalSignificance
Pain,infections,andtroubleeating,sleeping,andsocializingcandevelopinchildrenwhohavedental caries.Usuallythetoothdecaycanbeprevented, withdietbeingthemostimportantriskfactorthat canbemodifiedtopreventcaries.Onecomponent thatcanbeaddressedissugar,withmodificationsof thediettokeepingestedsugarstoaminimum.Dental andotherhealthcarepractitionerscanhelpbyprescribingmedicationsthataresugarfreeaswellasinstructingthatsugar-supplementedmedications shouldbetakenwithmealsifthesugarcan’tbeeliminated.Manycommonlyprescribedsugar-containing medicationshavesugar-freealternatives(Table1).
HowardJ,DaveM,ReynoldsL,etal:Thebittertruthregarding sugarymedicinesinchildren. BDJTeam 12:116-120,2025
Reprintsavailablefrom MDave,DivofDentistry,Coupland3Bldg, TheUnivofManchester,OxfordRd,Manchester,M139PL;email; manas.dave@manchester.ac.uk
E-cigarettesandothertypesofvapingdeviceswereinitiallyintroducedaswaystohelpsmokersquitusingcigarettesandothertobaccoproducts.Thesevapingdevicesweretoutedasasafe alternativetosmoking,buttheirreceptionbyyouthandyoung adultsledtotheirwidespreaduseasrecreationalproducts.Innovationsindesignsand flavorshaveincreasedtheappeal.Despite thesupposedsafetyofvaping,ithasbeenlinkedtoanincreased riskforasignifi cantspectrumofhealthrisks.Thehealthimplicationsofvaping,prevalentmisconceptionsaboutthispractice,and proposedpublichealthinterventionsthatareneededtoaddress therisksofvapingwerepresented.
Non-oralHealthEffects
Vapinghasbeenassociatedwithanincreaseinlunginjuries,the exacerbationofasthma,chroniccoughing,andotherrespiratory systemdisturbances.Inaddition,severalcardiovascularsystem problemshavebeennoted,includinganincreasedriskfor myocardialinfarctionrelatedtotheexposuretonicotineand otherchemicalsduringvaping.Thecentralnervoussystemhas alsobeenaffected,withincreasedmooddisordersandnicotine addictiondevelopingwithuse.Eventheimmunesystemhassufferedsuppressionoftheimmuneresponseandanincreaseinthe riskofcancer.
Multipleoralhealthproblemsarerelatedtovaping,asfollows (Table1):
Thepropyleneglycoline-liquidscandecreasesalivary flow, causingdrymouthanddiscomfort.
Propyleneglycolalsoresultsintheproductionofdiacetyland methylglyoxal,whichhavedetrimentaleffectsonoralhealth. Salivaisreducedandwhenthisiscombinedwithsugarye-liquids,anenvironmentfavorabletodentalcariesdevelopment results.
Chemicalssuchasnicotine,glycerol,volatileorganiccompounds,and flavoringagentshavebeenlinkedtoperiodontitis. Thediminishedsalivaandaccumulatedresiduescausepersistentbadbreath.
Theoralmicrobial floraisaltered,increasingtheriskofinflammationandmakingusersmoresusceptibletoinfectionssuch ascandidiasis.
Gumdisordersandtoothlossareassociatedwithchronic usage.
Enamelandtoothstructureareweakenedbytheacidicagents usedine-liquids.
Nicotineexposureimpairsblood flowandslowsthehealing processoforalwounds.
Prolongedexposuretonicotine-containingliquidscancause teethtodiscolor.
Table1. OralHealthImplicationsofVaping
Sr.noOralimplications
1Increasedriskofperiodontitis
2Guminflammationandbleeding
3Reducedsalivary flow
4Drymouth(Xerostomia)
5Irritationoforaltissues
6Alteredoralmicrobiome
7Erosionofdentalenamel
8Toothdecay
9Developmentoforalulcers
10Increasedriskoforalinfections
11Increaseinriskoforalcancers
12Flavor-inducedcytotoxicity
(Courtesyof.ShrivastavaSR,BobhatePS,BadgeA:Counteringoral healthimplicationsandmisconceptionsofvaping. JIntOralHealth 17:82-84,2025.)
Overheatingcausesburnsofthelips,gums,andpalate. Thechemicalsinvapeaerosolscanimpairtastebudfunction. Long-termexposuretocarcinogenicsubstancesinaerosols canincreasetheriskfororalcancer.
Mostpeoplebelievethatvapingonlyaffectsthelungsanddoesn’t causeoraldiseases,althoughawholelistofconditionsareactuallycausedbyvapingtosomedegree.Vapinghasalsobeenpromotedasahealthysmokingalternativebutevenaerosols generatedbythevapingcancauseoralcancerandperiodontal disease.
Someclaimthatvapingisn’taddictive,butthenicotine-containing flavoredliquidsusedareactuallyhighlyaddictive.Astudyinthe UnitedStatesreportedthat44%ofrespondentsquitsmoking andtookupvapingbecausetheybelieveditwassafe.About 12%sawvapingasnotbadforone’shealth.Amongadolescents age13to19years,asignificantproportionbelievethate-cigarettesarelessaddictivethanothertobaccoproducts.Wearing bracesorotherdentalapplianceswhilevapingcanincreasethe riskforinflammationintheoralcavityanddiscolorthegums.
Spreadingthetruthaboutvapingandhealthwillrequirevarious approaches.It’svitaltocreateawarenessaboutthespeci fic oralhealthrisksassociatedwithvapingusingavarietyofoutreach
campaigns.Theseincludesocialmediaplatforms,whichiswhere themisconceptionsabouttheuseofvapingareoftenspread. Peoplewhousevapingdevicesshouldalsobeencouragedto attenddentalcheckupsregularlytodetectanyoralhealthissues. Userscanalsobetaughttoperformself-examinationsperiodicallytodetectorallesions,ulcers,orotherearlylesions,then reportthemtotheirdentalcarepractitioner.
Thosewhovapeneedtoconsumeplentyofwatertooffsetthe reducedsalivaryproduction,thetendencytodevelopdental caries,andtheoraldiscomfort.Brushingand flossingatleast twiceadaycanpreventtheaccumulationofresiduesandbacteria inthemouth,combatinggumdiseaseandtoothdecay.Those whovapeshouldalsoconsumeadietrichinantioxidants,vitamins,andmineralstopromotepositiveoralhealthandprevent bothgumdiseasesandoralcancers.Supportandresources shouldalsobemadeavailabletothosewhovapetohelpthem quitthehabitandminimizetheriskforcompromisesoftheir oralhealth.
Aquestionnairefoundthat29%oftherespondents werewillingtoquitvapingusingmedications.Inaddition,35%werewillingtoquitusingmobileapplications.Theseresultsindicateadditionalwaysthat publichealthinitiativescanreachpeoplewhoarevapingwiththemessageabouthowdangerousandunhealthyvapingactuallyis.Gettingthemessageout andprovidingsupportforthosewhowanttoquitvapingandhavebetteroralhealthinthefutureareimportantwaysdentalcareproviderscanhelptocounteract themisinformationaboutthesafetyandvalueofvaping.
ShrivastavaSR,BobhatePS,BadgeA:Counteringoralhealth implicationsandmisconceptionsofvaping. JIntOralHealth 17:82-84,2025
Reprintsavailablefrom SRShrivastava,DeptofCommunity Medicine,DattaMegheMedicalCollege,Off-CampusCtrof DattaMegheInstofHigherEducationandResearch,Hingna Rd,Wanadongri,Nagpur – 441110,Maharashtra,India;e-mail: drshrishri2008@gmail.com
Tasteisdetectedthroughthetastebuds,whicharelocated throughoutthemouth,althoughmostarepresentonthetongue. Adultshaveabout14,000tastebudsintheoralcavity.Thesensationoftasteoccurswhenthesubstancethathasa flavorandsaliva interactwiththespecificreceptorforthat flavoronthetastebuds. Tasteperceptionguidestheacceptanceorrejectionoffoodand theresponsetostimulito flavor.Tastedisorderscanproduce nutritionaldeficienciesandstressinindividualsandcaninfluence theirmentalhealth.Adiminishedawarenessoftaste(hypogeusia) hasbeenreportedbypatientswhowearconventionalcomplete dentures.Thesedentalaidscovertheentirepalateandobliterate thetastebudsandmechanoreceptorsinthatstructure,whichdetractsfromthestimulationofafferentsomaticnervesandalters sensorystimuli,sothat flavorsaren ’tperceivedcorrectly.Taste changescanalsoresultfromhyposalivationanddifficultyswallowing,whichcanchangeeatinghabits,leadingtopreferencesfor sweetandcreamysubstances.Thenewhabits,especiallyinelderly patients,cancausenutritionalandmetabolicdisorders,masticatorymuscleatrophy,anddecreasedchewingability.Theliterature hasconflictingoutcomesforstudiesoftheeffectofconventional completedenturesontastesensations.Asystematicreviewwas conductedtoclarifywhethertasteperceptionisalteredinedentulouspatientswearingcompletedentures.
AsearchofthePubMed/MEDLINE,CochraneLibrary,andScopusdatabasesuntilJune2022wasdone,alongwithamanual searchinthereferencelistsofincludedarticlesandthemainjournalsonoralrehabilitationandotolaryngology.Sevenarticles wereincludedinthereview,with3randomizedclinicaltrials and4nonrandomizedclinicaltrials.
Atotalof287participants(meanage60years)wereincludedin thereview.Onehundred fifty-sixhadonlymaxillarycomplete
dentures.Only1studyinvestigatedtheeatinghabitsandnutritionalproblemsoftheincludedpatients.
Measurementsofsalivary flow,volume,andpHinpatientswith andwithoutcompletedenturesshowedsalivary flowincreases whendentalprosthesesareworn.Theunstimulatedsalivary flowwasmorebasic.
Nostatisticallysignifi cantdifferenceswerenotedinthetime requiredfor flavoridenti fication,whethercompletedentures wereorweren ’twornin2studies.Athirdfoundthatwearing completedenturesincreasedthe flavoridenti ficationtime.
Tasteperceptionthresholdwastestedinseveralstudiesusingsolutionswithdifferentconcentrationsof flavors.Themost commonlyusedsolutionsforsalty,sweet,sour,andbitter were,respectively,sodiumchloride,sucrose,citricacid,andquinine.Differentstudiesfoundthatdifferent flavorswerethemost difficulttoidentify.
Somestudiestestedtasteperceptionusingpaperstripssoaked inthe fl avorsolutionincontactwiththeoralmucosa.Dif ficultyin fl avoridenti fi cationwasreportedforhardpalate andbackofthevestibulesites.Dentureswerenotedto reduce fl avorperception,withbittertastethemostdif fi cult toidentify.
Thehypothesisthatcompletedenturesdidn’tinterferewithtaste perceptionwaspartiallyaccepted,with4ofthestudiesnotingthe useofcompletedenturesinterferedwithtasteperception.In addition,mostofthecompletedenturewearerswereelderly, withphysiologicalandbiochemicalchangesrelatedtoagingthat interferedwithtaste.Thisincludedafewertastebuds,adecrease inretronasalandorthonasalsmellandtaste,andareductionin theperceptionofsaltyandsweet flavors.
ficance
Conventionalcompletedenturesmayinterferewiththe perceptionofthe4primarytastes(sweet,salty,sour, andbitter)inedentulouspatients.When flavorisn’t wellperceived,thepatientmayexperiencepoorfood acceptanceandreducedsatietyprocesses.Older adultstendtoalsoexperiencechangesintheirability totasterelatedtoage-relatedfactors,suchastheeffectsofmedicationontheirabilitytodistinguish flavors.
AvelinoMEL,Vila-NovaTEL,CostaRTF,etal:Doestheuseof conventionalcompletedenturesinfluencetasteperception?A systematicreview. JProsthetDent 133:438-444,2025
Reprintsavailablefrom SLDMoraes,UnivofPernambuco(UPE), RectoryS/NGovernadorAgamenonMagalhaesAve,Santo Amaro,Recife,Pernambuco50100010,Brazil;e-mail: sandra. moraes@upe.br
InSweden,signi fi cantimprovementshavebeenmadeinoral health,includingafallinedentulismandpartialedentulism. Theoralhealth relatedqualityoflifeisnegativelyimpacted bymissingteeth,whicharealsolinkedtoincreasedcardiovasculardiseaserisk.Withthisinmind,patientsoftenchoose nottoacceptextractionforseverelydecayedteethwithpulp necrosis,butmaychoosetohaverootcanaltreatment(RCT) beforerestorationwithanindirectpostandcore(PC).The SwedishNationalBoardofHealthandWelfare recommends RCTbasedonitslowcostinrelationtoitsgainedeffect. RCTplusPChassurvivalratesbetween86%and93%,but thisapproachpresentsatechnicallychallengingtask,with generaldentalpractitionersoftenfeelinginsuf fi cientlyequippedtoperformit.Inaddition,about22%oftheRCTsinmolarsarereportedtoendinextractionbeforetreatmentis completedwithapermanentroot fi lling.Analternative approachisextractionandreplacementwithanimplantsupportedsinglecrown(ISSC).Systematicreviewsshow ISSCstohavehighsurvivalrates,butthistreatmentiscomplexbiologicallyandtechnica lly,withalossofimplantsoccurringinsomecases.Ifthisoccurs,the fi nalsolutionistaking advantageofneighboringteethtoserveasabutmentsfora fi xeddentalprosthesis.ISSCsalsohaveahighinitialcost, makingitimpracticalforsomepatients.Expectedutilitytheory(EUT)hasbirthedtheprocessofclinicaldecisionanalysis, inwhichmodelssuchasdecisiontreesareusedtovisualize thevariousoutcomesofasituation.Whenadecisionistobe basedoncost-effectiveness,theoutcomesincludecostsand probabilities,whichareusuallybasedonpublishedhigh-
qualityscienti fi cliterature.Thesecostsandprobabilitiesare usedtocalculatetheexpectedcostsfortheoutcomes, thentheoutcomewiththelowestexpectedcostisconsideredthemostcost-effective.Asensitivityanalysiscanbe usedtodeterminethethresholdvaluesforwhen1option becomesmorecost-effectivethantheother.Adecisionanalyticapproachwasusedtocomparethecost-effectivenessof RCT+PCwiththatofISSCina fi ctionalseverelydecayed fi rstmandibularmolarwithanecroticpulp;Swedishgeneral dentalpracticeservedasthecontextforthismodel-based undertaking.
Nopatientsorpatientdatawereused,withthemodel-based cost-effectivenessstudyusingdataonoutcomesbasedonSwedishsources,whenavailable.Costswereliftedfromthereference pricelistestablishedbythe SwedishDentalandPharmaceutical BenefitsAgency.
Adecisiontreemodelwasusedtovisualizethetreatmentscenarios.The2modelsdevelopedbeganwitha firstmandibular molarwithadeepcarieslesionanddentalpulpnecrosis.The first treatmentoptionwasRCT+PC,andthesecondwasextraction andimplantplacement(EI), finishingwithanISSC(EI+ISSC). Applyinganewtreatmentstepwasconsideredanactivechoice, withsurvivalorlossofatoothorimplantbasedonprobabilities. Theoutcomewasmeasuredafter1and5yearspostoperatively. Thesensitivityanalysisillustratedhowmuchtheprobabilityvalue couldbechangedbefore1treatmentoptionwouldbecome morecost-effectivethantheother.
The5-yearsurvivalprobabilityforRCT+PCwas70%,whereas thecorrespondingprobabilityforEI+ISSCwas98%.Thecostfor thedifferentbranchesafterchoosingRCTwasbetween15,860 Swedishkrona(SEK)and33,105SEK.Expectedcostforchoosing RCTwas17,400SEK,butexpectedcostforchoosingEIwas 18,800SEK.
The5-yearsurvivalprobabilityforRCT+PCwas69%,withthe probabilityforEI+ISSCremainingat98%.TheRCTbranchcost variedfrom15,860SEKto54,290SEK.ExpectedcostforRCT was19,500SEK,butthatforEIremainedat18,800SEK.
Indecisiontree1,thelowestestimatedcostforchoosing RCT+PCwas15,860SEK,andthehighestexpectedcostwas 33,105SEK.AllofthepossibleexpectedcostsofRCTwerebetweenthese2points.
TheexpectedcostofISSCwas18,800SEK.ForRCTtocostless thanthat,theprobabilityvalueforRCTwouldhavetobeatleast 83%.
Indecisiontree2,thelowestcostforRCTwouldstillbe15,860 SEK,butthehighestcostwouldbe54,290SEK.ForRCTtobe morecost-effectivethanISSCinthisscenario,theprobability valueofRCTsurvivalwouldneedtobeatleast93%.
Themodelanalysisgivesasimplifiedversionofrealitytoillustrate thecost-effectivenessdifferencesbetweenchoosinganRCTfollowedbyPCoranextractionandISSC.Basedonthecurrent stateofevidence,RCTanddentalimplantsprovidenearlyequivalentalternativesbasedoncost-effectiveness.Theprobabilityof toothsurvivalafterRCTandPCmustbeintherangeof83%to 93%tobemorecost-effectivethanextractionandISSC.
Theprognosisofthe2optionscouldbechangedby evenasmalldeteriorationinthepreoperative,intraoperative,orpostoperativeconditionsforRCTand PC,shiftingtoextractionandISSCbecomingamore cost-effectiveoption.ItshouldbenotedthattheresultsofthisstudyarebasedonSwedishstudiesand thecostsandeconomicsonSwedishdentalcare, meaningtheycannotbedirectlyuniversalized.
SavolainenN,FriskF,KvistT:Isrootcanaltreatmentandanindirectcoronalrestorationofamandibular firstmolarcost-effective comparedtoextractionandanimplant-supportedcrown?Adecisionanalyticapproach. ActaOdontolScand 84:95-103,2025
Reprintsavailablefrom NSavolainen;e-mail: nikki.savolaine@rjl.se
Denguevirus(DENV)infectionistransmittedbymosquitosusuallyinendemicareas,withmostcasesbothasymptomaticand self-resolving.However,denguefevercancausemild flu-like symptoms,includingfever,nausea,muscleandjointpain,and headaches.Complicationscandevelopinaminorityofpatients, includingreducedplateletcount,whichcanevolveintodengue hemorrhagicfeveranddengueshocksyndrome,bothofwhich canbefatalbecauseofthecoagulationabnormalities,plasma leakage,severebleeding,respiratorydistress,and fluidloss. Thesemoreseriousformscanleadtohypovolemicshockand multi-organfailure.OralmanifestationsofDENVinfectionare uncommon,butdentalhealthcarepractitionersshouldbeaware oftheoralsymptomssothediseasecanbeidenti fiedearlyinpatientshavingdentalprocedures.Theoralsymptomsinclude gingivalbleeding,oralulceration,lingualhematoma,andbilateral
inflammatoryswellingoftheparotidglands.Theclinicalimplicationsfordentalpractice,thepossibleoraloutcomesrelatedto DENVinfection,andmanagementoptionsforaffectedpatients werediscussed.
Ascopingreviewwasdone,withsearchesconductedintheMedline,WebofScience,Scopus,Embase,CochraneLibrary,andLILACS/BBOdatabases.Forty-onestudieswereincludedinthe review,covering42,817patients(meanagerange8to44years).
Thestudiescamefrommostlytropicalandsubtropicalregions (Figure2),withAsiaaccountingfor61%ofthem,SouthAmerica

Figure2. GlobalmapshowingthedistributionofDENVstudies.Search flowchartaccordingtothePRISMA2020statement.(CourtesyofdeAraujoLP, WeisshahnSK,doCarmoET,etal:Oralmanifestationsofdenguevirusinfection:Ascopingreviewforclinicaldentalpractice. BMCOralHealth 25:138, 2025.)
22%,NorthAmerica7%,CentralAmerica5%,andOceaniaand Europe2%each.Themostcommonlyrepresentedcountries wereBrazilandIndia.
The Aedesaegypti mosquitowastheprimaryvectorin78%ofthe studies,with Aedesalbopictus in5%.Acombinationofbothvectorswasdocumentedin17%.
Themostfrequentlyreportedoralmanifestationwasgingival bleeding(51%),whichwasfoundin21studiesacrossseveral countries.Oralulcerationsoccurredin10%andwereoftensevere,causingsignificantdiscomfortorcomplications.Pharyngitis wasseenin10%andoral/oropharyngealpseudomembranous candidiasisin7%.Othersymptomsincludedbilateralinflammationoftheparotidglands,lingualhematoma,hemorrhagicplaques,bluemucosa,submucosalhemorrhageofthehardpalate, pinkspotsonthesoftpalate,andLudwig’sangina.Comprehensiveoralexaminationsareneededtodetectosteonecrosisof thejawandangularcheilitisinthesepatients.
TheoralclinicalpresentationofDENVinfectioncanrangefrom mildsymptomstoseveremanifestations,illustratingthe complexityoftheinvolvement.Dentalprofessionalscandetect oralmanifestationsinearlydiseaseandimprovepatient outcomes.
Dentalprofessionalsneedtobetrainedtobecome awareofpossibleDENVinfectionintheirpatients, especiallyiftheypracticeinendemicareas.When patientsaresuspectedtohavedengue,dentists shouldbeawareofthemeasuresassociatedwithearly diagnosisandmanagementandavoidtheuseof nonessentialmedications,especiallyantiinflammatoryagents,antibiotics,andmedications thathaverenal,hepatic,orhematologictoxicity. Furtherresearchisneededtoidentifythepathogenesisoforalmanifestationsofdengueandtodevelop standardizedprotocolsfortheclinicalassessment andmanagementofinfectedpatients.
deAraujoLP,WeisshahnSK,doCarmoET,etal:Oralmanifestationsofdenguevirusinfection:Ascopingreviewforclinical dentalpractice. BMCOralHealth 25:138,2025
Reprintsavailablefrom LPdeAraujo,SchoolofDentistry,Catholic UnivofPelotas(UCPel),CampusdaSaude,AvFernandoOsorio, 1586-PelotasPelotas,RS,Brazil;e-mail: lucas.araujo@ucpel. edu.br
Dentalanxietyaffectsabout15%oftheworld ’spopulationand canexistaloneoras1ofmultiplemorbidconditions.Someindividualsexperiencenegativedentaltreatmentandsubsequentlydevelopdentalanxiet y,whereasothersexperiencea traumaticeventofsometypethatleadstotheiranxiety.Those whoexperiencesexualabusemaybetriggeredbydentaltreatmentsituationstorelivefeelingsreminiscentoftheabuse.Asa result,theymayavoidevenurgentlyneededdentaltreatment, leadingtoadeteriorationoftheirdentitionandbothfunctional andsocialconsequences.Ifthepatientsuffersfromsevere dentalanxiety,dentaltreatmentmayonlybeaccomplishedby usinggeneralanesthesia(GA) .Thedentalinterventionsare neededtoavoidthedangerofallowingodontogenicinfections toremainuntreated,whichcancausetheinfectiontospread toothersites,resultinginsofttissueabscesses,sinusitis,or osteomyelitis.Thesepatientsmayalsoovermedicatethemselveswithanalgesics,andthepersistentuseoftheseagents canhavenegativeeffects.Providingdentaltreatmentunder GAisoftenpracticedtomanagefearfulchildren,butanypatient withseveredentalanxietycouldreceivedentalcareunderGA. Unfortunately,manycountrieshavealimitedsupplyofGAfor dentalpatients,withlongwaitinglists.Astudywasundertaken todescribethedentalstatusofpatientswithseveredentalanxietyradiologically,todepicttheirmentalandgeneralsomatic healthpro fi le,andtoevaluatepossibledifferencesinoral,generalsomatic,andmentalhealthstatusbetweenpatientswithand withoutareportedhistoryofabuse.
Panoramicx-rayswereobtainedforthe56participants,and theirgeneralhealthvariableswerecollectedfromtheirpatientrecords.Ofthe38womenand18men(meanage 37.9years)whoparticipated,27hadareportedabuseexperience(RAE).
RadiographicDentalFindings
Alloftheimagesexhibitedatleast1variablethatcouldn’tbeassessedforeachtoothorrootremnant.Thesuboptimalimage qualitywasmostprevalentintheareafromcaninetocaninein bothjaws.Thiswasseenmostofteninaninabilitytoassessapical radiolucenciesandcarieslesions.Anaverageof71%oftheteeth ineachimagecouldbeassessedforcaries,withabout55%ofthe teethorrootremnantsassessableforapicalradiolucencies.
Ofthe14patientswithfewerthan20teeth,13(93%)hadatleast 1apicalradiolucency.Twelve(86%)hadevidenceofatleast1 toothwithcaries.Ofthe42patientswith20ormoreteeth,apicalradiolucencieswerenotedin64%anddentalcariesin81%.
Seventy-fivepercent(42)ofthepatientshadatleast1mentalor generalsomaticdisorder.Psychiatricdisordersotherthansevere dentalanxietywerereportedbyabout55%(32)ofthepatients. Nonspecificpsychiatricdisorderwasreportedbyabout21%, withfewerpatientsreportingpost-traumaticstressdisorder (PTSD),anxiety,anddepression.Mixedsomaticconditions(about 36%),oralconditionsandhabits(about21%),anddevelopmental anomaliesorgeneticconditions(about16%)werealsofound. About63%ofpatientsreportedusingatleast1classofmedication, withthemostcommonlyusedbeingpsychopharmacologicalagents (about36%)andanalgesics(about34%).About57%ofpatientstook painmedicationstomanagethedentalpaintheywereexperiencing.
Ageandgenderweresimilarbetweenthepatientswithand withoutRAE.Inaddition,the2groupsweresimilaronnumber ofteeth,missingteeth,rootremnants,teethwithrestorations, root- filledteeth,teethwithcarieslesions,andteethwithapical radiolucencies.
Table4. PredictiveContributionofReportedAbuseHistoryandGenderonReportedPsychiatricDisorders,OtherDisorders,andUseof AnalgesicMedications
Abuse1.500.014.48(1.42,14.16)1.360.033.91(1.19,12.85)1.670.015.32(1.54,18.41) Gender0.520.401.68(0.50,5.65)0.830.232.29(0.60,8.77)-0.210.750.81(0.22,2.97)
OR, Oddsratio; CI, confidenceinterval.
Note: Binarylogisticregressionincluding2dummycodedindependentvariables:Abuse(1, reportedabuseexperience, 0, noreportedabuseexperience) andGender(1, female, 0, male).Dependentvariablesforallmodelswerecodedas 1 =yesand 0 =no.Themodelsexplain18.4%A/17.4%B/18.0%C (NagelkerkeRsquare)ofthevarianceobservedinthedependentvariable.
(CourtesyofAardalV,HolC,RønnebergA,etal:Whorequiresdentaltreatmentundergeneralanesthesiaduetopainandseveredentalanxiety? FindingsfrompanoramicX-rayimagesandanamnesis.ActaOdontolScand84:78-85,2025.)

Figure1. Numberofparticipantswithspecificradiological findingsandtheircombinations. AR, Apicalradiolucencies; RR, rootremnants.(Courtesyof AardalV,HolC,RønnebergA,etal:Whorequiresdentaltreatmentundergeneralanesthesiaduetopainandseveredentalanxiety?Findingsfrom panoramicX-rayimagesandanamnesis. ActaOdontolScand 84:78-85,2025.)
Differenceswerestatisticallysigni fi cantbetweenthosewith andwithoutRAEintherateofpsychiatricdisordersother thanseveredentalanxiety,mix edconditions,andincreased useofanalgesicmedications.Evenwhenadjustedforgender, statisticalanalysiscon fi rmedthatpatientswithRAEhad greateroddsofhavingpsychiatricdisorders,mixedsomatic
conditions,andusinganalgesicmedicationthanthosewith nohistoryofabuse( Table4 ).
Patientswithseveredentalanxietywhowerereceiving dentaltreatmentunderGAhadpoordentalhealth,with
dentalpathologyanddentalpain.Theyalsohadhigherrates ofreportedpsychiatricconditionsotherthandentalanxiety andevidencedmixedsomaticconditions.Havingahistoryof abusewasalsolinkedtoahigherlikelihoodofhavingpsychiatricorsomaticconditionsandahigheruseofanalgesics.
Abouthalfoftheparticipantsinthisstudyreportedan abuseexperience,whichledthemtoavoiddental care.Asaresult,theirdentalhealthwaspoor.Inaddition,thesepatientsweremorelikelytodeveloppsychiatricproblems.Thesepatients,whoarealready sufferingfromseveredentalanxiety,areatan increasedneedforthedeliveryofdentalcareunder GA,especiallysincetheirdentalproblemstendtobe seriousandotherwiseunmanageable.
AardalV,HolC,RønnebergA,etal:Whorequiresdentaltreatmentundergeneralanesthesiaduetopainandseveredentalanxiety?FindingsfrompanoramicX-rayimagesandanamnesis. Acta OdontolScand 84:78-85,2025
Reprintsavailablefrom VAardal,OralHealthCtrofExpertisein RogalandNorway,Postboks130Sentrum,4001,Stavanger, Norway;e-mail: vilde.aardal@throg.no
Endodonticallytreatedteeth(ETT)oftensuffertoalossof toothstructurethatweakenst heirresistancetomechanical stressandmakesthemmoresusceptibletofracture.Restorationsarefocusedonprotectingtheremainingtoothstructure andpreventingfurtherfailure.OptionsforrestorationforposteriorETTincludefull-coveragecrownsorothercuspal coverage,whichrequiresfewerrepeatinterventionsthanthe optionofdirectrestorations.Bothcoronalleakageandcoronal fracturesarelesslikelywithfull-coveragecrowns,althoughthe supportforcrownsoftenfailstoconsidertheremainingtooth structure,whichispositivelycorrelatedwithfractureresistanceforETT.Atoothlackingbothmarginalridgesisathigher riskforfracturethanatoothwithonlyanocclusalcavity.Fullcoveragecrownsalsorequirethe removalofsoundtoothstructureinmanycasesanddon ’t fi twellwiththeprinciplesofminimalbiologicalcostandconservativemanagement.Direct restorationspreservetoothstructure,costlesstoperform, reducetreatmenttime,andpotentiallyallowforendodontic repeatinterventionsandchairsiderepairs.Theevidencesupportingthelong-termsurvivalofETTthatreceiveddirectrestorationsislacking.Arandomizedclinicaltrialwasdoneto assessthesurvivalandsuccessofdirectcompositeresinrestorationscomparedtometal-ceramiccrownstorestoreETTwith minimalstructuralloss,speci fi cally,forteethhavingatleast3 intactaxialwalls.
The53participantshadcomeforrootcanaltreatmentof molarteeththathadatleast3remainingaxialwallsmeasuring 2mmthick.Inonegroupofpatients,theteethwererestored withdirectcompositeresinrestorations.Intheothergroup, theteethwererestoredwithadirectcompositeresinrestoration,followedbyafull-coveragemetal-ceramiccrown.Evaluationsweredoneatbaselineandannuallyfor3years.The assessmentincludedclinicalandradiographicevaluations, includingbitewingandperiapicalradiographstodetectmarginaldefects,recurrentcaries,andsignsofinfection (Figure1).Athoroughperiodontalexaminationwasalsoperformed,includingbleedingonprobingandpocketdepth measurements.
Thesurvivalcurvesafter3yearsshowedthesurvivalrateforthe crowngroupwas93.3%andthatforthedirectrestorationgroup was76.7%.Thesesurvivalratesdidn’tdiffersigni ficantlyfromone another.
Sevendirectrestorationsfailed,4ofwhichinvolvedfractures. Twoparticipantswithfractureswerebruxers.The2failuresin thecrowngroupshowedsymptomaticandradiographicsigns ofapicalpathologyrequiringendodontictreatment.

Figure1. Bitewingandperiapicalradiographstakenatthe36-monthfollow-upappointment.Image A showsanendodonticallytreatedmolarrestoredwithan occlusalcompositeresinrestoration;image B showsandendodonticallytreatedmolarrestoredwithanocclusal-proximalcompositeresinrestoration;and image C showsanendodonticallytreatedmolarrestoredwithametal-ceramiccrown.(CourtesyofAbu-AwwadM,HalasaR,HaikalL,etal:Directrestorationsversusfullcrownsinendodonticallytreatedmolarteeth:Athree-yearrandomizedclinicaltrial. JDent 156:105699,2025.)
Statisticalanalysisshowedparafunctionalhabits(bruxism)was theonlysignificantpredictoroffailure.Parafunctionwasassociatedwitha12.8-foldincreaseintheriskofaneventcomparedto noevent.
Signi fi cantdifferenceswerenotedbetweentherestorationand crowntreatmentswithrespecttoseveralUSPublicHealthService(USPHS)criteriaafter3years.Restorationsperformed worsethancrownsintermsofcaries,surfacetexture,and
marginalintegrity,withborderlinesigni fi canceformarginal discoloration.Crownsperformedworsethanrestorations withrespecttoperiodontalassessment,withmoreteeth receivingcrownsshowingincreasedbleedingonprobing,a slightincreaseinpocketdepth,andthepresenceofperiapical infection.Overtime,directrestorationsdeterioratedsigni ficantly,withcaries,margindiscoloration,marginintegrity,and fractureshowingevidenceofthisdecline.Crownsshowedno signi fi cantdeteriorationwithtime.
ETTwithminimalstructurelosswasmanagedwithcomparable survivalandsuccessratesforthedirectrestorationsandfullcoveragecrowns.Crownstendedtobemorepredictable,particularlyifthepatientdemonstratedbruxism.Directrestorations weremoreappropriatewhentheocclusalloadwasreduced, withendodonticmonitoring,andwhencostwasaconcern.
The3-yearsurvivalandsuccessratesfordirectcompositerestorationsweresimilartothoseformetalceramiccrownsforendodonticallytreatedmolars withminimalstructuralloss.Directrestorationsare mostappropriateformolarsthathaveminimallossof structure,thosewithreducedocclusalloads,when endodonticmonitoringisdone,andwhen financiallimitationsexist.
Abu-AwwadM,HalasaR,HaikalL,etal:Directrestorations versusfullcrownsinendodonticallytreatedmolarteeth:A three-yearrandomizedclinicaltrial. JDent 156:105699,2025
Reprintsavailablefrom HPetridis,UnivCollegeLondon,Eastman DentalInst,Rm238,RockefellerBldg21UniversitySt,London, WC1E6DE,UK;e-mail: c.petridis@ucl.ac.uk
Theoralmicrobiomeconsistsofdiversemicrobialcommunities thatdifferbasedonmanyfactors.Somemicrobiotacomefrom theenvironment,somehavetheabilitytoadheretooralsurfaces andobtainnutrientsfromtheecosystem,otherscancompete withorcopewithothermicroorganisms,andstillotherscan resistadverseconditionsandevadehostdefensemechanisms. Theindigenousoralmicrobiomeundergoesrapidphenotypic changesinresponsetoenvironmentalstressors,thencanreturn toanormalstateoncethesestressorsarecontrolled.Signi ficant ecologicaldisruptionscanoccurandresultinthemostcommon oraldiseases:dentalcariesandperiodontaldiseases.Areviewof thecurrent findingsregardingthecompositionandfunctionsof thepredominantmicrobialcomponentsofahealthyoralmicrobiomeatdifferentagesandindifferenthabitatswaspresented.
Theneonate'soralmicrobiomevarieswidelyandissignificantly influencedbythetypeofdelivery,thetypeoffeeding,andthe changetosolidfoodandtootheruption.
Vaginallydeliveredinfantstendtohaveanoralmicrobiome stronglyin fl uencedbytheclosecontactbetweenmother andchild,sothatmaternalskinandgutmicrobiotaarethe primarysources.Cesareansectiondeliveriesintroducemicrobesfromthematernalskinandthehospitalenvironment. Thesalivaofavaginallydeliveredchildhasgreatermicrobial diversityandmorecloselyresemblesthemother'ssalivary microbiotathanthesalivaofachilddeliveredbycesarean section.Vaginaldeliveryalsopromotesearlycolonization withoralyeast,especially Candidaalbicans. Thesedifferences indeliveryaremoreapparentinsamplescollectedshortlyafterbirthandtendtodisappearbyage3months.
Otherfactorsthatin fluencetheearlymicrobiomeinclude maternaluseofantibioticsandcontinuousexposuretoand transmissionofthemother'soraltaxatothechild.Theprofiles ofbiologicalandadoptedchildrenareequallysimilartothose oftheirmothers,indicatingtheroleofasharedenvironment anddirectcontact.

Figure1. Keydifferencesobservedinoralmicrobiotabetweenbabies whoreceivedonlybreastmilkcomparedwiththosewhoreceivedformula.(CourtesyofCorr eaJD,CarlosPPS,FariaGA,etal:Thehealthy oralmicrobiome:Achangingecosystemthroughoutthehumanlifespan. JDentRes 104:235-242,2025.)
Cleardisparitieshavebeenfoundbetweenbreastfedand formula-fedinfants.Breastmilkprovidesessentialnutrientsas wellasanarrayofmicrobes(Figure1).Inaddition,breastmilk componentssuchasimmunoglobulinAandGmaternalantibodiesinhibitthegrowthofsomebacteriaandfostertheattachmentofcommensals.Formula-fedinfantsharborahigher abundanceof Actinomycetota and Bacteroidota,especiallyinthe genus Prevotella ,comparedtobreastfedinfants.Breastfedinfants haveahigherprevalenceof Pseudomonadota andstreptococci speciescomparedtoformula-fedinfants.Overall,thedifferences inoralmicrobiotacompositionbasedontypeoffeedingtendto bemostpronounceduptoage2years.
Beforetootheruptionoccurs,bacteriacolonizemucosalsurfaces.Withtheintroductionofsolidfoods,whichoftenoccurs aroundthesametimeastootheruption,asignificantchange takesplaceintheoralmicrobiota.Solidfoodscontainnutrients forthemicrobialcommunity,andteethcreatenewnichesfor theaccumulationofplaque.Theinfant'smicrobiomeresembles thatofadultsmorecloselythanthatofotherinfants.Ifsolidfoods areintroducedandbreastfeedingisdiscontinuedbeforeage 12months,theinfanttendstohavehigherbacterialdiversityat age2years.
Aschildrentransitionfrompredentatetohavingaprimarydentition,theoralmicrobiotabecomescolonizedbyobligateanaerobesratherthan Streptococcus.Theearlycolonizersdeplete oxygensothatanaerobicspeciescanthrive.Changescontinue throughthemixedandpermanentdentitionphases.Whenthe permanentteetharrive,therearemore Actinomyces species andhighanaerobeconcentrationscomparedtotheprimary dentitionsituation.Caries-freeoralstatusisassociatedwith highproportionsof Porphyromonascatoniae and Neisseria flavescens
Theonsetofpubertybringswithitsigni fi cantshiftsintheoral microbiota,markingadistinctphaseintheoralecosystem. Endogenoushormoneexposuresaffectthecompositionof theoralmicrobiome,alteringtheabundanceofexistingbacteria ratherthanintroducingnewones.Theoralmicrobiomeofadolescentsismorediverseandsharesmoreinterindividualsimilaritiesthanthemicrobiomeinadults.Studieshaveidenti fi ed differinggroupsofmicroorganismsaspredominantatthis time.Althoughnostudiesspeci fi callydealwiththemetabolism oftheoralmicrobiotainhealthyadolescents,themostprevalentbacteriainadolescentssuggestvariousfunctions.Lactate maybeconvertedintoweakeracids,orbacteriacandegrade glycoproteins,proteins,pepti des,andaminoacidsintoshortchainfattyacids,ammonia,an dsulfurcompounds,whichare linkedtooralmalodor.
Theoralmicrobiomeisin fluencedbymultiplephysical,biological,mental,andpsychosocialstressorsdirectlyorindirectly throughoutadulthood.Itcanbeextremelydif ficulttoidentifya “universal” oralhealthmicrobialprofileforadults.The “normal ” oralmicrobiomevariesbetweenindividualsandbetweenoral samples.Supragingivalplaqueistheleaststablemicrobiotain theoralcavity,butataspecieslevel, Fusobacteriumperiodonticum onthetonguedorsumand Fnucleatum insupragingivalplaque havestrongtime-varyingbehavior.
Acorecommunitydoesappeartopersistentlyinhabitcertain oralniches.Subgingivalplaquehasdemonstratedthehighestdiversity,withkeratinizedgingivahavingthelowest.Streptococci maybefoundinallsites,but Simonsiellamuelleri onlyinhabits thehardpalate. Calbicans isfoundinverylowproportionson thepalate,supragingivalbio film,andoralrinsesamples.Viruses arefoundinmucosalsitesandsupragingivalbio film,withmost beingbacteriophagesthattargetspeciesof Streptococcus and Aggregatibacter.
Youngeradultshavehigherdiversityinthesupragingivalbiofi lm, althoughnodifferencesbetweenagegroupsarefoundforbuccal mucosamicrobiota. Neisseria declinesafterage40years,but Lactobacillus spp, Gemellasanguinis,and Streptococcusangiosus hasbeenfoundtoincreaseinthesupragingivalbiofilmsofthose olderthanage60years.Healthyadultsmayharbormorethan 100species.
Thecoremetabolicpathwaysmaybenichespeci ficorbroadly availableacrossmanymicrobiomes.Forexample,somehealthassociatedoraltaxacanconvertdietarynitratetonitriteinsaliva, whichisthenconvertedtonitricoxide,whichreducesblood pressure,improvesvascularfunction,andhasantimicrobialactivityagainstperiodontalpathogens,thuscontributingtooralas wellassystemichomeostasis.

Figure2. Oralmicrobiotathroughoutlife.Keyfactorsinfluencingthecompositionoftheoralmicrobiotaalongwiththemaincomponentsofthemicrobial communityateachlifestage.Thelineindicatestheincreaseordecreaseindiversity.(CourtesyofCorr^ eaJD,CarlosPPS,FariaGA,etal:Thehealthyoral microbiome:Achangingecosystemthroughoutthehumanlifespan. JDentRes 104:235-242,2025.)
Thehumanmicrobiomeisnowknowntobeakeycomponentin thepromotionofhealthyagingandlongevity.Age-relatedchanges inhostbiology,suchaslow-gradeinflammationandcellularsenescence,canchangethemicrobiomeovertime.Oralsenescence alsochangestheoraltissuesandincreasestheirsusceptibilityto drymouth,periodontitis,cancer,androotcaries.Havingpoor oralhealthpredictsthedevelopmentoffrailtyandmaycontribute toagingprocesses.It'slikelythatthereisabidirectionalrelationshipbetweenagingeffectsontheoralmicrobiomeandthemicrobiomethatpromotesahealthylifespan.
Mostofthedifferencesbetweenyoungandolderadultsare relatedtoanincreaseinlowabundanttaxa,suggestingthat coredominantbacteriaareresponsibleformaintaininghealth statusduringaging.However,conflicting findingsbetweenyoung andolderadultsareevenmorepronouncedincentenarians, includingdiversityinsalivaandplaqueinGermancentenarians andsigni ficantlylessdiversityinItaliancentenarians.
Themostcommonoraltaxainolderadultsare Streptococcus spp, Veillonella spp, Gsanguinis, Pmelaninogenica, Fnucleatum, Hparainfluenza, Rothia spp, Gemellaadiacens, Prevotelladenticola, Prevotellahisticola,and Neisseria spp.Olderadultshadreduced coloniesof Porphyromonasendodontalis, Lautropiamirabilis, Rothia aerea, Cardiobacteriumhominis,and Gemellamorbillorum .
Thedataonthemetabolismandfunctionalityoftheoralmicrobiomeinhealthyolderadultsremainlimited.However,it's
possiblethatmaintainingcommensalspeciesinvolvedinnitrate reduction,argininemetabolism,anti-in flammatory,andimmunomodulatoryprocessesthroughoutagingismorelikelytopromotebene ficialeffectsintheoralhealthofagingadults(Figure2).
Ahealthyoralmicrobiometendstoberesilientand relativelystableevenatolderages,butthemain coregenerainindividualsmayevolve.The first2years oflifeseemtodeterminetheoralmicrobiomemakeup thatwilllastforseveralyears.Duringpuberty,the physiologicalchangesfavortheovergrowthofsome microorganisms.Adulthoodisatimeofmoresignificantstabilityuntiltheagingprocessbegins.More notablechangesareseeninaging,suchasanincreaseinraretaxa.Alargearrayofhealth-related pro filesexistsoverthehumanlifespan.
Corr^ eaJD,CarlosPPS,FariaGA,etal:Thehealthyoralmicrobiome:Achangingecosystemthroughoutthehumanlifespan. J DentRes 104:235-242,2025
Reprintsavailablefrom JDCorr^ ea,Ponti ficCatholicUnivofMinas Gerais,AvDomJoseGaspar,500Coraç aoEucaristico,Belo Horizonte,MinasGerais30535-901,Brazil;e-mail: jo_odonto@ hotmail.com
Patientswithdentofacialdeformitiesoftenexperiencelowselfesteem,alackofself-confidence,socialchallenges,anddistress regardingtheirfacialfeatures.Orthognathicsurgery(OGS)isundertakentoaddresstheskeletal,facial,anddentalabnormalities, withthegoalofimprovingmusculoskeletalfunctionand psychosocialwell-being.Amongtheproceduresperformedare LeFortIosteotomy(LFI),bilateralsagittalsplitosteotomy (BSSO),andgenioplasty.Aftersurgery,patientsmustadjustto theirnewappearance,makingpre-andpost-treatmentevaluations importantinmeasuringthepatient’ssatisfactionandqualityoflife. Acomprehensiveassessmentwillincludepsychologicaleffects, oralhealth,andfacialaesthetics.Thegoalofsurgeryistoofferbenefitsthatoutweightherisks.Clearcommunicationwiththepatient aboutpotentialoutcomesisvital.Aliteraturesearchwasdoneto identifystudiesthatassessedthepatient’spsychologicalfactors indicatingsatisfactionandanimprovedqualityoflifeafterOGS.
ThedatabasesofPubMed,GoogleScholar,APAPsychNet,ScienceDirect,Medline,Embase,Cochrane,andothersweresearchedfor relevantstudies.Twenty-ninestudieswereidentified,covering13 prospective,5prospectivecohort,3randomization,4quasiexperimentaldesigns,and5usedpropensityscoremethodsto constructamatchedcomparisongroup.Thetargetpatientswere adolescents(age12to18years)andadults(age18to65years) withClassI-IIIcraniofacialmalocclusionthatrequiredorthognathic treatment.
Patientswereassessedpreoperativelytoidentifyconditionssuchas bodydysmorphicdisorder(BDD),anxiety,ordepression,allof whichcaninfluenceoutcomes.Postoperativetestswere designedtoaddressconcernsaboutsurgeryandrecovery,as wellasthepatient’sdevelopmentofbetterself-esteem,reduced anxiety,andbetterbodyimage.Thetoolsusedtoevaluatethe patientsincludedthoserelatedtoqualityoflife(QoL)indicators, theOrthognathicQualityofLifeQuestionnaire(OQLQ),the 36-questionShortFormHealthSurvey(SF-36),andtheOralHealth ImpactProfile(OHIP).
Follow-updatacollectionwasconductedfor3weeksto60months, with25ofthestudies(about86%)indicatingOGSwaseffective basedonpatientsatisfactionscores.Moststudiesshowedapositive
patientoutcomewhentheOQLQ,SF-36,andOHIPscoreswere consideredseparately.Fivestudies(about17%)notednoeffect oranegativeassociationfor2studyoutcomes.Themajorityof studiesshowedOGSpositivelyaffectedQoL,improvedpsychologicalwell-being,andachievedaesthetictransformations.
TheOQLQ,OHIP,andSF-36measuresshowedimprovedoral health,physicalfunction,andreducedlimitationsonroles,giving patientsapositiveexperience.Signi ficantQoLimprovements weremadeinpatientshavingLeFortIosteotomyandBSSO. Themostsigni ficantdifferenceswerenotedintheoralfunction andphysicallimitationdomains.
Cliniciansmustaddressfactorssuchastheroleofbodyimage, self-esteem,andstressinpatientoutcomesthroughcarefulpatientselection,psychologicalevaluations,clearcommunication, andmanagingexpectationswhenpatientsarecandidatesfor OGS.It’simportantthatsocialandemotionalsupportisoffered before,during,andaftersurgery.
Thissystematicreviewidentifiedfactorsthatcontribute toapositiveassociationbetweenOGSandpatient satisfactionandimprovedQoL.Thesefactorsinclude enhancedoralandphysicalfunction,improvedfacial aesthetics,andreducedpsychologicaldiscomfort. Theconsistent findingsofthestudiessurveyedshow themultifacetedbenefitsofOGSinmanagingdentofacialdeformities.Conductingapsychologicalevaluation afterOGScanencouragethepatient’sadaptationto newfacialfeatures,changesinself-esteemlevels, andoverallsatisfactionwiththeexperience.
AlkaabiS,AlsabriG,AlyammahiA,etal:Psychologicalandquality oflifeoutcomesfollowingorthognathicsurgery:Acomprehensivesystematicreview. AdvOralMaxillofacSurg 18:100522,2025
Reprintsavailablefrom SAlkaabi,DeptofOralandMaxillofacial Surgery/OralPathology,AmsterdamUMC-locationVUmc,De Boelelaan1118,1081HZAmsterdam,theNetherlands;e-mail: salem.alkaabi@ehs.gov.ae
Periodontaldiseases,suchasperiodontitisandgingivitis,arethe mostprevalentoraldiseasesintheworld.Gingivitisresultsfrom theaccumulationofbacterialbiofilms(plaque),andperiodontitis isachronicinflammationthatprogressivelydestroysthesoftand hardtissuesthatsupporttheteeth.Fourstagesofperiodontitis havebeenidentified,basedonseverityofdisease,with3grades basedonrateofprogressionmodifiedbythepresenceofsmoking anddiabetes.Severeperiodontitisincreasesinadultsage30years andreachesitshighestrateatage40years,withadegreeofstability inolderpatients.Oralhealthcareprovidersaddressthechallenge ofthishighprevalenceofadultperiodontaldiseasethrough periodontaltreatment(PT),buttreatmentmustbedoneatappropriateintervalstoachievethebestoutcomes.Patientstendtohave fewornosymptomsthattranslateintoanurgentneedforcare,so theyoftenmissfollow-upvisits,resultinginprogressionofthedisease.Anobservational,follow-up,register-basedstudywasdone toestimatethebenefitofPTafteranoralhealthexamination (OHE)andafollow-upOHE.
Atotalof42,533adults(age18to80years)visitedpublicoralhealth careclinicsinHelsinki,FinlandbetweenJanuaryandDecember 2009foranOHE.TheOHEconsistedofanassessmentofalloral tissues,adiagnosis,atreatmentplan,andtheassignmentofanindividualrecallinterval(IRI).Recallintervalsrangedfrom0to 60months.Thepatient’speriodontalstatuswasrecordedusing theCommunityPeriodontalIndex(CPI),withthemouthineach caseconsideredin6sextants.Atotalof16,040patientsattended afollow-upOHEbetween2010and2015basedontheirIRI (meanfollow-uptime2.2to2.6years),wherethechangeinCPI wasnoted.
Ahealthyperiodontiumwasrecordedfor4.6%ofthe16,040patients.Deepperiodontalpockets(CPIscoresof3or4)wererecordedin24%ofpatients.ThosewithCPIscore4hadthehighest meanage(61years).Thisgroupalsohadthefewestnumberof teethpresent.About91%ofthepatientgrouphadteethpresent in6sextants.ThemostprevalentCPIscorewas2inallsextants inboththeoriginalOHEandinfollow-upOHEs.
IftheCPIscorewas1orhigher,thepatienthad1PTormore,dependingonhowseverethegingivitisorperiodontitiswas.Ten percentofthepatientswhowereidentifiedasneedingPTdidn’t receiveit.SevenpercentofthepatientshadaCPIscoreof1or 2.Sextant2hadthebestresponsetotreatment.Atleast1better sextantwasachievedin56%ofthepatientsduringthefollow-up
OHE,with7%havingallsextantsbetter.DuringPT,thosepatients whoseCPIscorewas4hadmoreextractionsthanpatientswithany otherCPIscore.
ThemodelsconstructedwiththedatashowedthatCPIimproved iftheperiodontaldiseasewasmanagedwithPTdeliveredbyan oralhealthcareteam.PTandchronicdiseasesshowednosignificantinteractions,butdiabetesorseverementaldisorderswere associatedwithapooreroutcomeafterPTinallsextantsduring thefollow-upOHE.MenalsohadpooreroutcomestoPTthan womenwhenallsextantswerecombined.
PTafterOHEwasanimportantfactorinachievingbetterperiodontalhealth.Havingmoretreatmentswasassociatedwithabetteroutcomethanbeinglimitedtoasingletreatment.Theoutcome waspoorerinpatientswithdiabetesorseverementaldisordersand formen,butchronicdiseasesandPTshowednosignificant interactions.
Periodontaldiseaserequirestreatmentwithfollow-up visitstomonitortheoutcomeandtodeliveradditional treatmentsifindicated.Inaddition,patientsmustbe committedtobetteroralhygienehabits,including frequenttoothbrushingtwiceadayandinterdental cleaning.Patientsmustalsomakehealthylifestyle changes,suchasquittingsmoking.Theoralhealth careteamshouldmonitorpatientswithperiodontal diseasestomanageanyprogressionofdisease. Thesebehaviorsneedtobetaughttopatientsso thattheyknowtheirresponsibilityintheprocess. Patientsshouldalsosharewiththeiroralhealthcare teamanyriskfactorstheyhave,suchasdiabetes andseverepsychoticmentaldisorders.PTshould beginimmediatelyaftertheoralhealthcareevaluation andbeconductedbytheoralhealthcareteam,which mayrequirereferraltoaspecialistforadvancedcases.
HaukkaA,KailaM,HaukkaJ,etal:EffectsofperiodontaltreatmentonperiodontalstatusinFinland:Aregister-basedstudy. ActaOdontolScand 84:128-136,2025
Reprintsavailablefrom AHaukka,DeptofPublicHealth,POBox 20,FI-00014UnivofHelsinki,Helsinki,Finland;e-mail: anna.k.haukka@helsinki. fi
Theverticaldimensionofocclusion(VDO)isdescribedasthe distancebetween2anatomicpointswheninmaximalintercuspal position.Thepointsoftenselectedarethetipofthenoseandthe chin.IdealVDOhasbeenconsideredimportantwhenassessing facialaestheticsandprovidingmasticatoryfunction,butseveral mythshavearisenthathavepromotedcontroversyaround VDOdentalconcepts.Forsomepatients,alteringtheVDOis consideredanessentialcomponentoftheirprostheticororthodontictreatmentplan.Otherpatientsareadvisedtoaltertheir VDOforfunctionalreasons,oftenbasedonsupposedly abnormalmorphologicalfeatures.TheVDOtopiccanbe confusingwhenfacedwiththemanyapproachesforregistering theVDO,usingtechniquesthatrangefromtraditionalfaciallandmarkstoadvancedtechnologicalapproaches.It’salsonotuncommonthatclinicianswilldebatewhetheranalteredVDO willaffectTMDsymptoms.FourmythsregardingVDOinrestorativedentistrywereexplored,andguidancerelyingonevidentiary findingswasofferedbasedonthecurrentliteratureplusa surveyof862generaldentistsandprosthodontists.
YouMustAllowforaProlongedTrialorGradualProcessto AlterVDO
Nearly88%ofthesurveyrespondentstestanewVDObecause ofconcernoverthepatient’sreactiontothenewocclusion, 85%observethatpatientsdowell,and53%worryabout TMDsymptoms.Sixpercentreportedtherewasalegalrequirementtotestthenewbitewithtemporaryrestorationsintheir countries.Only9%believedthatthereisn ’tanyneedtotestthe newVDO(Figure4 ).Inreality,prolongedtrialphasesarerarely needed,withpatientsusuallyadaptingwelltoanewVDOwithin ashortperiodoftime.Noevidenceshowsagradualincreaseis needed.Thestomatognathicsystemhasthecapacitytomake neuroplasticchanges,andthetemporomandibularjoint(TMJ) andmusclesadapttothisprocess.Someevidenceindicate thatsofttissuemanagementorspeechproblemsmayjustify theuseoftemporaryrestorationsforanextendedperiodof time.
Someclinicalscenariosmayjustifycautionandaddedpreparation,suchaspatientswithanactiveTMDorhistoryofTMD, whoshouldbediagnosedcorrectlyandtreatedbeforeprosthetic
measuresareinstituted.Inaddition,theclinicianshouldbeaware thatpatientswhosepsychologicalpro fileindicatesdepression andanxietymaybeatriskforchronicTMD.Thepatient’ spsychologicalhealthcanimpairtheeffectivenessofthetreatment andtheadaptiveresponsestoanincreasedVDO.Insleepapnea patients,anincreasedVDOmayimpacttheupperrespiratory tractandnegativelyaffecttheseverityoftheobstructivesleepapnea.Anotolaryngologicalevaluationisneededtopinpointthe siteofairwayobstructionandidentifythebesttreatments. Finally,anexcessiveincreaseinVDOcanleadtolipincompetence,whichhasadverseeffectsonmasticationandphonetic functions.Orthodontictreatmentmaybeadvisablebeforeprosthetictreatmentcanbedone.
ARestoredVDOIsn’tStableOverTime
Almosthalfofthesurveyrespondentsbelievedtherestored VDOisn’tstableovertime,whichlikelyre flectseitherthe fixed musclelengththeoryortheadaptablemuscletheory.The fi rst arguesthatanyVDOchangesaretemporaryandwillrevertto theoriginalstate,whereasthesecondtheorysaystheVDOis flexibleandlong-lastingchangesarepossiblebecausethemuscle willadapt.Researchindicatesthatadultskeletalmusclesadjust theirlengthandareadaptable.Thishasbeenshowninsurgical limblengtheningandtendontransfersandextendstomasticatory muscles,whichadjusttheirlengthwithinamonthafterVDOalterations.Bothresearchandclinical findingsindicatethatamodifiedVDOisverylikelytobestableovertimeaftertheadaptation.

Figure4. Thedistributionofpatients’ adaptivecapacityaftervertical dimensionofocclusion(VDO)elevation.(CourtesyofLassmann Ł,Calamita MA,ManfrediniD:Mythssurroundingverticaldimensionofocclusionin restorativedentistry:Ascopingreview. JEsthetRestorDent 37:94-105, 2025.)
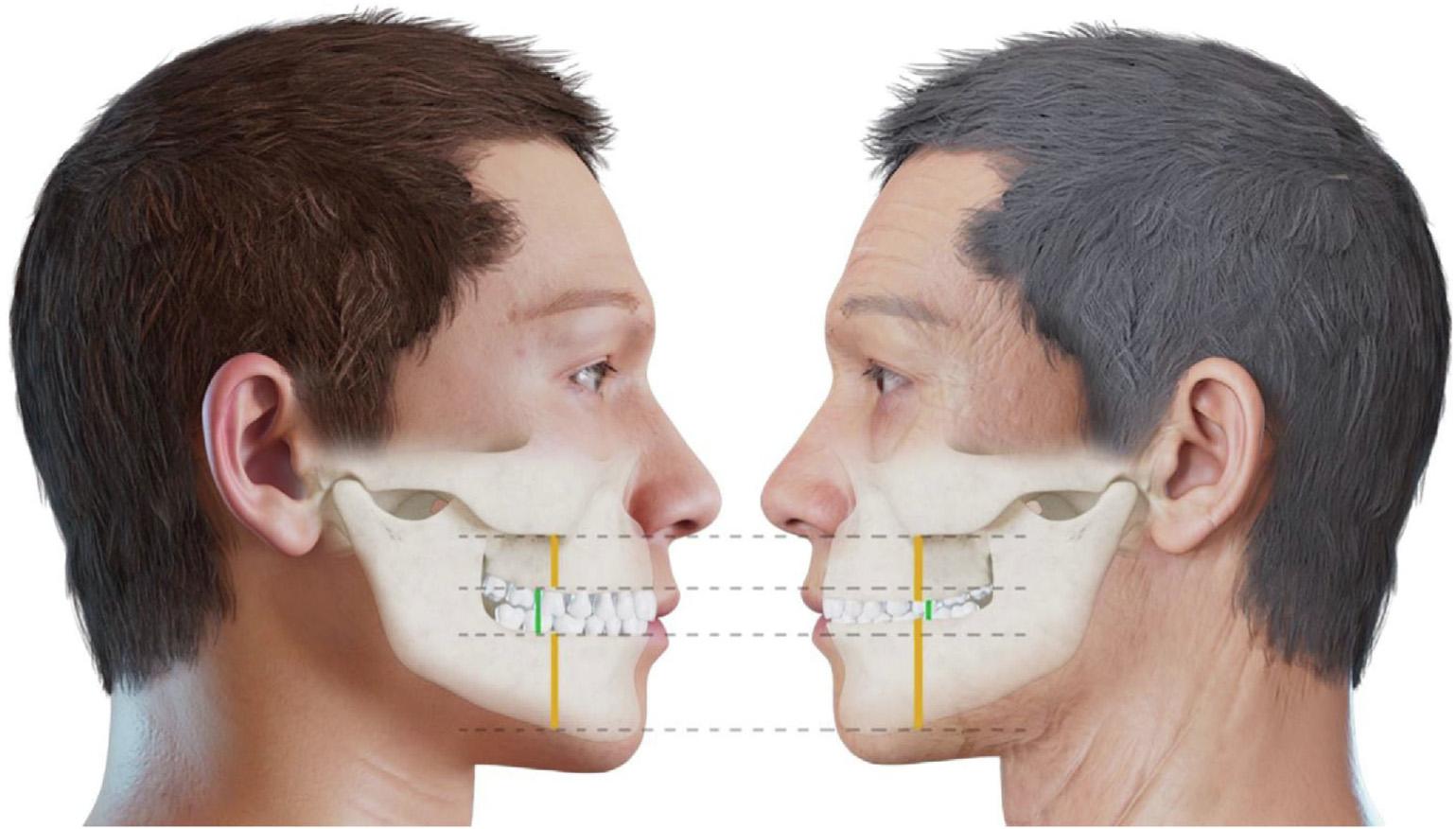
Figure7. Dento-alveolarcompensation.(CourtesyofLassmann Ł,CalamitaMA,ManfrediniD:Mythssurroundingverticaldimensionofocclusionin restorativedentistry:Ascopingreview. JEsthetRestorDent 37:94-105,2025.)
Toothweardoesn’tnecessarilyleadtoVDOlossandisoften accompaniedbysomedegreeofdentoalveolarcompensation. Evenwithsubstantialtoothwear,VDOandfaceheightcan remainconsistentbecauseofthiscompensation(Figure7). ManydentistsassumetheVDOisreducedwhentheyobserve wornteeth.Currently,nopropertoolsexisttopreciselymeasureVDOlossinthesesituations.
MethodstoDetermineVDOforCompleteDenturesAre EquallyEffectiveforWornDentition
ThetechniquesusedtodetermineVDOfordentatepatients differfromthoseforedentulouspersons.Thetraditionalways todetermineVDO,whichinvolvetheuseoffaciallandmarks, phonetics,anddeglutition,maybeusefulformobileprosthodontics,buttheymaynotbedirectlyapplicableforpatientswhose dentitionisworn.Amorepreciseapproachfordentatepatients isneeded.
ChangesinVDOAreaDirectCauseorCureforTMD
Currentliteraturedoesn’tsupportanycausalorcurativerolefor VDOchangesinpatientswhohaveTMDsymptoms.Nodirect linkexistsbetweenVDOchangesandTMD.Evidenceisaccumulatingthatindicatesadiminutionofocclusalfeaturesshouldserve asadeterminingfactorinTMDtreatment.
ManycommonbeliefsaboutVDOalterationsandtheireffectson patientadaptation,whetheragradualprocessandtrialphaseare
required,thestabilityofmodifiedVDO,andlinksbetweenVDO andTMDwereshowntobeinaccurateandmisleadingbasedon published findingsandtheclinicalwisdomofpracticingdentists andprosthodontists.VDOalterationsarenotonlystablebut thefacialanddentalstructuresarealsoadaptabletothese changes.Inaddition,traditionalmethodsusedtodetermine VDOincompletedenturesaren’tsuitablefordealingwith worndentition.Dentatepatientsrequireatailoredapproach ratherthanrelianceonthetraditionalmethod.
Evidencesupportstheadaptabilityofthestomatognathicsystem,sonoprolongedtrialphaseisneeded afterVDOalterations.Evidencedoesn’tsupportany linkbetweenVDOandTMD.Alongwiththeother guidanceprovided,it’simportantthatdentalpractitionersrelyoncurrentevidenceandclinicaljudgment andnotnecessarilyontraditionalapproachesor assumptions.
Lassmann Ł,CalamitaMA,ManfrediniD:Mythssurrounding verticaldimensionofocclusioninrestorativedentistry:Ascoping review. JEsthetRestorDent 37:94-105,2025
Reprintsavailablefrom Ł Lassmann,One&OnlyInst,Gdanski, Poland;e-mail: zlassmann@hotmail.co.uk
Surveysshowthatoursocietyisvulnerabletoacceptingmisinformation,especiallythroughsocialmedia andthatincludeshealth misinformation.Isitpossibletoknowifasourceistrustworthy?Howcanweprotectourselvesfrominaccuratehealth information?
Massmediaandsocialmediadisseminationhelpsinformationtravelfast,whichisgreatforaccessibilitybutnotnecessarilyfor accuracy.Ina2024USconsumerstudy,morethanhalfofrespondentsobtainedhealthinformationfromsocialmediaand 32%reliedonfamily,friends,andcolleagues.Respondentsadmittedthattheydidn’talwaystrustthesesourcesbecausehealth misinformationmaybemisreported,misinterpreted,orotherwiseinaccurate.A2024UKsurveyfoundthat94%ofthepopulation hadwitnessedmisinformationbeingcirculatedonsocialmedia.Howcanweknowiftheinformationisaccurate?
DawnHolfordoftheSchoolofPsychologicalScienceattheUniversityofBristol,UK,isabehavioralscienceresearcherwhospecializesinthepsychologyofcommunicationanddecision-makingandhasstudiedstrategiestopreventandrebuthealthmisinformation.Shehasfoundthattounderstandwhywemightfallforhealthmisinformation,weshouldexamineour “attituderoots.” Thistermreferstothebeliefsandideasthatwehaveconsolidatedinourmindssincewewereyoung.Theyarenowpartofour psychologyandserveasmotivationaldriversofhowweprocessinformation.Theserootsaren’tgoodorbadinthemselvesbut simplymotivateusandareshapedbyourlifeexperiencesandthoughtpatterns.
Emotionscanalsobepartoftheseroots.Anxiety,forexample,maybefeltaboutsomethingwhosemechanicswedon’tunderstand andthatcanincludemedicalexaminations,medications,andvaccines.Holford’steamexamined11differentattituderoots concerningmisinformationaboutvaccination.Theyincludedfearsaboutpossibleadversemedicaloutcomes,variousreligious views,andresistanceaboutbeingtoldwhattodo(reactance).Theteamdeterminedthatpeopletendtoseekandinterpretinformationthatalignswiththeirexistingpatternsofthoughtandinquiry.Beinganxiousaboutgoingtothedoctororhavingmedical procedurescouldmakeusmorelikelytoadoptmisinformationthatconsolidatesthatfear.Andthat’sconsistentwithhowhuman brainswork theyareverypronetoconfirmationbias,whichmeansselectivelyseekingevidencethatsupportsthebeliefsand anxietieswealreadyhave.Thistendencyisextremelystrongandcanbeverydif ficulttodislodge.
Holfordalsoclari fiedwhoismostsusceptibletomisinformation.Shesaid, “Peopletendtobelieveinformationmoreifthatinformationalignswiththeirideology.” Inaddition,certainpsychologicaltraitscanin fluenceoursusceptibilitytomisinformation, suchasactivelyopen-mindedthinking.Shewarnsthat “Whichgroupwouldbemoresusceptibledependsonhowmisinformation iscraftedtocreatealignmentwithpeopleofthatgroup’sbeliefs.”
Whenaskedwhypeoplemightmistrusthealthinformationfromofficialsources,Holfordsuggestedthatfakeinformationspread withmaliciousintentbybadactorscanarisefromreal-lifenegativeexperienceswithinthehealthsystemitself. “Togivesome examples,” sheexplained, “wewouldbemoresusceptible[to]disinformationthatvaccineswereintendedasaforeignplotto sterilizepeoplelikeusifwe’dhadpreviousexperiences mostofthetimelegitimate! thatshapedourattituderootofdistrust ofsay,colonialgovernments.” Thiscouldalsobeseenwithbeingdeniedtimelytreatmentduetogenderbias,orwithexperiences ofracisminhealthcare,orsimplythroughpoorexperienceswithinstitutions,allofwhichcouldamplifyouranxietyandmakeus moresusceptibletofalsehealthinformation.Narrativescanevenbecraftedsotheycouldtargetmorethan1group.
Holfordandhercolleaguesaredevelopingastrategytheycall “jiu-jitsuinterventions” tohelppeopledealwithhealthmisinformation.Holfordexplainshowthisstrategyworks: “Weconceptualize ‘jiu-jitsuinterventions’ as[tryingto]usemisinformation againstitself.[ ]Injiu-jitsu[aBrazilianmartialart],youdon’ttryto fightwithanopponentheadon,butratherletthemattack andleveragethatforceto fightback.Inthisway,weareabletochallengewhatmayseemlikeastrongerandinsurmountablefoe. WhichIthinkisimportantwhenwelookatthescaleofthechallengewithmisinformation.Soourinterventionslookatwhatare
thefeaturesofmisinformation,whatitisthatmakesitsticky,thatmakespeoplesusceptibletoit,andweusethosetobuildpeople’sskillstodefendthemselvesorothersagainstmisinformation.”
Twotypesoftheseinterventionsarepsychologicalinoculationagainsthealthmisinformationandempatheticrefutationofmisinformation.Psychologicalinoculationislikeavaccineinthatitwarnspeopleagainstthetacticsofmisinformation,suchas cherry-pickinginformation,playingonouremotions,orrelyingonfakeexpertstoappearcredible.Whenpeopleexperiencesmall dosesofthesetactics,theyunderstandhowtrickymisinformationcanbeandbuildprotectivemeasuresagainstit.Empathetic refutationinvolvesthedevelopmentofinterventionsthatarealignedtotheindividual’sattituderoots,demonstratingempathy tomakecorrectingmisinformationfeellessthreateningsoit’smorelikelytobereceived.
It’simportanttocheckanddouble-checkthesourceofinformation.Called lateralreading, thistechniquehelpslookforthecorroborationoffacts.Afterencounteringthehealthinformation,wewouldlookoutsideofthatsiteorplatformforothersources thatwillverifyitscredibilityandseesourcesindependentoftheoriginalsource.Becauseofourtendencyistoacceptincorrect informationthatalignswithwhatwewanttohear,it’svitaltoemploythelateralreadingtechnique.Holfordemphasizesthatthose whodisseminatehealthinformation,suchasmedicalnewswebsites,haveadutytoperformmoreexactingfact-checkingbefore releasinginformationtothepublic.
Holfordsays, “Ironically,governmentalpublichealthorganizationsareoftentheplaceswheretheinformationisreliable because theyareaccountabletocitizensinawaythatothercontentgeneratorswouldnotbe.Manyalsomakeanefforttoshareinformationusingaccessiblelanguage.Andbecausehealthisaprettybroadarea,it’softengovernmentalorganizationsthathavethe remitandthewherewithaltocoordinatetheexpertiserequiredtocheckinformation.” Sheadmitsthatwedon’talwaystrustour owngovernments.Inthatcase,Holfordrecommendslookingtosourcesthataremoreglobal,suchastheWorldHealthOrganization(WHO).IntheUK,effortstogatherexpertadviceacrossawiderangeofhealthtopicsinclude PatientInfo.
Questionstoaskwhensearchingforatrustworthysourceareasfollows:
Whatdoestheconsensusacrossmultiplecrediblesourcestellus?
DoesthisseemtooalignedwithwhatIalreadybelieve?
Holfordalsorecommendsthatweseekoutatrustedhealthproviderorcommunityhealthrepresentativewecantalktoandask foradviceonwheretolook.
[CohutM:HowDoYouKnowIfAHealthInformationSourceIsReliable? MedicalNewsToday, Feb5,2025]
TikTokofferscozymaxxingasanewself-caretrend.Itfocusesoncreatingacomforting,stress-freeenvironmentthatoffersmentalhealthbene fits.Youcanchangeintopajamas,lightacandle,wrapyourselfina fluffyblanket,enjoyyourfavoritecomfortshows, orlistentogentlemusic.Theself-caretrendfocusesonengagingincozy,comfortingritualsthatpromotestressreliefandcalm. KenFierheller,apsychotherapistatOneLifeCounselling&Coaching,describescozymaxxingas “intentionallycuratingyourhome andhabitstoprioritizerelaxationandcoziness.” Henotesthattheprimaryreasonforitsappealisburnout,whichleadspeopleto seekwaystocreatepocketsofpeaceintheirlives.Toomanystressorsinourlivesalsomakeusdesiremomentsoffeelingsafeso wecanrelaxandde-stress.
RitikaSukBirah,counselingpsychologistandfounderofReflectwithDrRitz,notedthat, “Peopleareincreasinglyrejectingthe glori ficationofbusynessandhustleculture,optinginsteadforself-careandbalance.” Birahnotesthattheaftereffectsofthepandemichaveledpeopletoprioritizetheirmentalhealthand “adeeperappreciationofcomfortandsafetywithinpersonalspaces.” Otherfactorsincludeeconomicstress,climateanxiety,andpoliticalinstability.
Amongthementalhealthbene fitsofcozymaxxingarereducedstress,improvedemotionalregulation,andbetterqualityofsleep. Birahsays, “Acozy,predictableenvironmentsignalssafetytothebrain,reducingcortisol(thestresshormone)andpromoting relaxation.This,inturn,canleadtoareductioninstressandanxiety.” Consciouslyrelaxingmayallowforre flection,whichhelps
inmanagingemotions.Amongthecomfortingpracticesyoucanincorporateincozymaxxingarejournalingandsippingtea,which supporttheparasympatheticnervoussystem,thebranchofthenervoussystemresponsibleforrestanddigestfunctionsasopposedto fightor flightreactionstostress.Improvedsleepcanberelatedtohavingaclutter-free,invitingspacewhereyoucan winddown.Thatbettersleepqualityhelpswithemotionalbalance.
Ifcozymaxxingisn’tdonewithinsomeparameters,itcanleadtoavoidancebehavior.Conductingmentalhealthcheck-inswhen practicingself-carecanincludeaskingyourselfifyou’rewithdrawingfromothers,avoidingresponsibilitiesorrecharging,ormovingenough.Birahexplains, “Excessivecozinesswithoutmovementcancontributetophysicalhealthissuesorlethargywhileusing cozinessasanescapecanleadtoprocrastinationordifficultyfacingstressors.” It’swisetosetatimelimitforthecozyritualto avoidbecomingisolatedorengaginginexcessiveescapism.Ifyourstressandanxietybecomedif ficulttomanagealone, finda therapistorconnectwithamentalhealthprofessionaltogetsomeprofessionalsupport.
Birahadvisesthatyoubeginbycuratingyourspace,addingsoftlighting,blankets,warmcolors,andscentssuchaslavenderor vanillatocreateacalmingenvironment.Thenintroduceacomfortingritual,likeaddingawarmdrink,reading,orstretchingbefore bedtosignalyourrelaxationintention.Takingtimeforabathwithgentlemusicandacandlecanalsobepartofcozymaxxing. Expertsadvocateleavingsmartphonesandotherdevicesoutsidethespacetoavoidaddingorcontinuingthestresstheseitems create.Incorporatinggentlemovementintoyourdaycanalsobecalmingandcozy.Thisincludesyoga,stretching,orashortwalk incomfortableclothes.Thiscozytimedoesn’thavetobesolitary.Beingwithotherscanhelpcreateasenseofrechargingand sharinginthecozyrituals.Itcanbecomeamovienight,asharedteatime,oraslowSundaybrunch.
Cozymaxxingrequireslittleeffortbutisaneffectivewaytosupportmentalhealthandrestoration.Itshouldn'tbeusedtoavoid responsibilitiesordifficultsituations.Cozinessshouldbebalancedwithmovement,connection,andpurposetocreateasustainable,healthy,self-carepracticeforbothphysicalandemotionalhealth.
[StokesV:TikTok’ s ‘Cozymaxxing’ TrendCouldImproveYourMentalHealth,ExpertsSay. Healthline.com,March12,2025]