









Editor-in-Chief
Douglas B. Berkey, DMD, MPH, MS
Senior Publisher
Annie Zhao
Journal Manager
Sangamithrai S
Abstract Writer
Elaine Steinborn
© May 2025, Elsevier Inc. All rights reserved.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise—without prior written permission from the publisher.
Publication Information Dental Abstracts (ISSN 0011-8486) is published bimonthly by Elsevier Inc., 1600 John F. Kennedy Boulevard, Suite 1600, Philadelphia, PA 1910, United States. Months of publication are January, March, May, July, September, and November.
Customer Service Office: 11830 Westline Industrial Drive, St. Louis, MO 63146. Periodicals postage paid at New York, NY, and additional mailing offices. Annual subscription rates for 2018 (domestic): $144.00 for individuals and $71.00 for students; and (international) $194.00 for individuals and $105.00 for students.
USA POSTMASTER: Send address changes to Dental Abstracts, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043.
Copyright 2025 by Elsevier Inc. All rights reserved. Dental Abstracts is a trademark of Elsevier Inc. Dental Abstracts is a literature survey service providing abstracts of articles published in the professional literature. Every effort is made to ensure the accuracy of the information presented in these pages. Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editors or the publisher. The Editors and the publisher disclaim any responsibility or liability for such material. Mention of specific products within this publication does not constitute endorsement.
All inquiries regarding journal subscriptions, including claims and payments, should be addressed to: Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Tel: 1-800-6542452 (U.S. and Canada); 314-447-8871 (outside U.S. and Canada). Fax: 314447-8029. E-mail: support@elsevier.com (for print support); support@elsevier.com (for online support).
Notice: Journals published by Elsevier comply with applicable product safety requirements. For any product safety concerns or queries, please contact our authorized representative, Elsevier B.V., at productsafety@elsevier.com
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments contained herein. Health care practitioners must exercise their professional judgement and make all treatment-related decisions based solely on the specific conditions of each patient. Because of rapid advances in the medical sciences, independent verification of diagnoses and drug dosages should always be made. The content is provided “as-is” and Elsevier makes no representations or warranties, whether express or implied, as to the accuracy, completeness, or adequacy of any content. To the fullest extent permitted by law, Elsevier assumes no responsibility for any damages, adverse events, or liability arising from use of information contained herein including for any injury and/or damage to persons or property, whether as a matter of product liability, negligence or otherwise.
Inclusion of any advertising material in this publication does not constitute a guarantee or endorsement of the quality or value of such product or service or of any of the representations or claims made by the advertiser.
Printed by Sheridan at 450 Fame Avenue, Hanover, PA 17331

DentalAdvance .org is the gateway offering high-quality research, news, jobs and more for the global community of dental professionals.
What you’ll find at DentalAdvance .org
Journal profiles with quick links to Tables of Contents, author submission information, and subscription details
Important information and valuable resources on how to submit a journal article
Dentistry Articles in Press from participating journals
Quick links to the leading dentistry societies worldwide Dentistry News from Elsevier Global Medical News (formerly IMNG)
Dentistry Jobs powered by ElsevierHealthCareers.com

Editor-in-Chief
DouglasB.Berkey,DMD,MPH,MS ProfessorEmeritus, SchoolofDentalMedicine, UniversityofColorado, Aurora,Colorado
AssociateEditor
DanielM.Castagna,DDS AssociateProfessor,DepartmentofPreventiveandRestorativeDentistry, UniversityofthePacific,ArthurA.DugoniSchoolofDentistry, SanFrancisco,California
P.MarkBartold,DDSc,PhD,FRACDS(Perio) ProfessorEmeritus SchoolofDentistry, UniversityofAdelaide Adelaide,Australia
RobBerg,DDS,MPH,MS,MA ProfessorandChair, DepartmentofAppliedDentistry, UniversityofColoradoSchoolof DentalMedicine, Aurora,Colorado
TylerH.Berkey,DMD GeneralDentist Aurora,Colorado
FionaM.Collins,BDS,MBA,MA ConsultantandEditor, GeneralDentist Longmont,Colorado
AnthonyJ.DiAngelis,DMD,MPH ChiefofDentistry, HennepinCountyMedicalCenter, Professor,UniversityofMinnesota, SchoolofDentistry, Minneapolis,Minnesota
RaulI.Garcia,DMD,MMedSc ProfessorandChairman, DepartmentofHealthPolicyandHealthServicesResearch, BostonUniversitySchoolofDentalMedicine, Boston,Massachusetts
MichaelSchafhauser,DDS GeneralDentist, St.Paul,Minnesota
JoeVerco,DClinDent PaediatricDentist NorthAdelaide,Australia
MAY/JUNE2025
VOL.70 No.3
Commentary
MeaningfulConnections166
BuildingConnections
MentoringandDEI167
InclusivityinMentoringRelationships
InclusioninDentistry
TheFrontOffice
Accommodation172
MakingReasonableAccommodations
CareConvergence173 InstitutingCollaborationsBetweenDentalandMedical CareProviders
CommunicationPolicies175 KeepingCommunicationSystemsCurrent Deepfakes176
TheDangerofFakesSpreadingMisinformation DentalTechnology177
InvestinginTechnology
HiringFramework179 RecruitingAssistantsandHygienists
Leadership180
ReachingLevelIVLeadership
Marketing181
ConvertingCallerstoNewPatients
PatientsReferringFriendsandFamily
PersonalityTypology184 Dentists’ PersonalityTraitsandDecision-Making Behaviors
SearchEngineOptimization185 EnhancingOnlineVisibilityforYourPractice
TheBigPicture
CurrentTrendsinDentistry187 WhatDentistsareDoingtoRemainSuccessful DentalCaries189
EarlyChildhoodCariesWorldwidePrevalence ApproachestoReduceEarlyChildhoodCaries
FutureofDentistry192 CurrentTrendsandAdvancesinDentistry GenerationalTransitions195 ChangingProfilesandPracticeModalities
PediatricDentistry
ChatGPT197 PediatricEducationMaterialPreparedByChatGPT DentalTrauma198 EpidemiologyandManagementofPediatricDental Trauma
EarlyChildhoodFluoride200 DispensingFluorideToothpasteToYoungChildren MyofunctionalTherapy201 NeurologicalRe-EducationThroughMyofunctional Therapy
Hands-On Cannabis204 DamagetoOralStructuresCausedByFrequent CannabisUse
E-CigarettesandOralCancer205 PatientGuidanceRegardingE-cigarettes
Endodontics207 IntraoperativeandPostoperativeTipsforRestoring EndodonticallyTreatedTeeth
FacialEsthetics210 ExpandingOralHealthCaretoFacialAesthetics ConcernsWhenDentalProfessionalsAddAesthetic Treatment
Training,Regulation,Safety,andEthics
IntraoralScanners213 ExpansionofIntraoralScannerUses
LipCancer217
IdentifyingLipCancer
OncologyandOralHealthCare218 ConcernsForDentalTeamsCaringForPatientsWith Cancer
Oral/SystemicConsiderations221
Non-HealingExtractionSocketProtocol
Peri-Implantitis223 NonsurgicalTreatmentforPeri-implantitis
Inquiry
AlveolarRidgePreservation226 ReducingAlveolarBoneRemodelingAfterExtraction
AntibioticsandExtractions/Implants227 ProphylaxisWithAntibioticsBeforeExtractionsin High-RiskPatients
AntibioticsUsedtoAvoidEarlyImplantFailure
CognitionandChewing229
MasticatoryFunctionandCognitiveStatusinOlder Adults
ToothLoss,CognitiveImpairment,andDementia
HalitosisandGIDisorders231 IdentifyingHalitosisRelatedtoGIDisorders
Oral/SystemicConnections233 LinksBetweenFlossingandCardiovascularDiseaseRisk
PediatricDentistryandSDF/ART234 ComparingSDFandARTasTreatmentForEarly ChildhoodCaries
ProbioticsandPeriodontitis235 CombiningProbioticswithPlaqueRemoval
SelectiveCariesRemoval237 Longer-termEvaluationofSelectiveCariesRemoval andCalciumHydroxide
Extracts
239 LivingLongerandBetter DistractedVersusMindfulEating
DentalWorld
FromtheExecutiveDirectore1 FromtheInternationalPresidente2 FromtheInternationalPresident-electe3 FromtheInternationalVicePresidente4 SectionNewse5
Notes TofacilitatetheuseofDentalAbstractsas areferencetool,allillustrationsandtablesincluded inthispublicationarenowidentifiedastheyappear intheoriginalarticle.Thischangeismeanttohelp thereaderrecognizethatanyillustrationortable appearinginDentalAbstractsmaybeonlyoneof manyintheoriginalarticle.Forthisreason, figure andtablenumberswilloftenappeartobeoutof sequencewithinDentalAbstracts.
StandardAbbreviations
Thefollowingtermsareabbreviated:acquiredimmunodeficiencysyndrome(AIDS),humanimmunodeficiency virus(HIV),andtemporomandibularjoint(TMJ).
Althoughtodaywehaveunprecedentedconnectivity,social disconnectionisrampant.Face-to-facecommunicationisuncommon,whichaffectsthequalityofourpersonalrelationships. SomeofthiscanbeblamedontheCOVID-19pandemic,when wewereoftenseparatedfromlovedones,ourcommunities, andoursupportsystems,leadingtolonelinessandisolation.Today’spoliticallypolarizedenvironmenthasonlyexacerbatedthe problem.TheUSSurgeonGeneraldeclaredanationwide epidemicoflonelinessandisolationin2023thatwasevidenced byreportsofexperiencinglonelinessfromabouthalfofthepopulation.Humansarehardwiredtoconnect,withsocialsupports andhumanconnectionsaffectingphysicalhealthandwell-being througheffectssuchassupportforourbodymassindex,decreasesindepressivesymptoms,fewersymptomsofposttraumaticstressdisorder,andbettermentalhealth.Socialdisconnectionshavenegativeeffectsonmortalityandincreasethe riskforcardiovasculardisease,dementia,stroke,depression, andanxiety.Fosteringmeaningfulconnectionscanbeachieved throughsimpleandsometimesobviousactivities,includingmindfulcommunication,gratitude,andcuriosityratherthanjudgment.
Digitalsignalsandnotificationscanmakeithardtofocusorfree ourselvesuptopracticeempathyindentistryandindailyinteractions.Mindfulnessistheabilitytobeinmoment-by-moment nonjudgmentalawarenessofourthoughts,feelings,bodysensations, andenvironment.Thisawarenessleadsustobetterunderstandthe perspectivesandemotionsofothersaswellashowwecanbest respondtotheirneeds.Insteadofplanningwhatwewillsaynext, weshouldlistencarefullytoothersandnoticetheirappearance, emotions,andbodylanguage.Allowingyourheartandmindto opentosocialinteractionsaswellasyourownemotionsandbody responsescanleadtoamorethoughtfulresponseandengagement.
Whenweexpressandreceivegratitude,relationshipswithone anothercanbebirthed,maintained,andstrengthened.Gratitude
strengthensromanticrelationshipsandfriendshipsandinspires coworkerstobemorehelpful.Notonlytheexpressionofthanks butalsoourengagementinreflectiononthoseforwhomweare gratefulcanhavepowerfulin fluencesonoursenseofconnection. Ourthankfulnesscanshowothersthevaluetheyoffertoour lives.Buildingacultureofgratitudeamongthedentalteamand practicecreatesahealthyenvironmentthatisfullofpositive emotionsandlesshostility.
Judgingotherpeopletendstopushthemaway,butasking questionshelpsusbetterunderstandandvaluetheirmotivations,perspectives,andbackground.Sincereinterestin learningaboutothersratherthanfocusingonourselvesbuilds connections.Remainingcuriousopensusuptodeeperand moremeaningfulrelationshipsthatweotherwisecouldmiss outon.
Humanconnectionisanessentialfoundationthat shouldbethecenterpieceofourdentalpracticesas wellasourpersonallives.Notmakingconnections withothersleadstocompromisedhealthandwellbeing.Thestepstobuildingconnectioncanbesmall butoffertheopportunitytolivelongerpersonallives, tohavelongerandmoresatisfyingcareers,andto createthrivingcommunities.
YamamotoKK:Cultivatingmeaningfulconnectionsindentistry andbeyond. JCalifDentAssoc 53:2450327,2025
Reprintsavailablefrom KKYamamoto,CollegeofDentalMedicine,CaliforniaNorthstateUniv,USA;e-mail: Karisa.Yamamoto@cnsu.edu
Inmentoring,amoreexperiencedindividual(thementor) guidesalessexperiencedindividual(thementee)andteaches, sponsors,advises,andservesasarolemodelfortheusually youngermenteetowardthedesiredgrowthinmutuallyde fi ned goals.Bothpartiesbene fi tfromthisrelationship,andanyorganizationinwhichthementoringtakesplacealsobene fi ts,with betterrecruitment,moreassuredretention,andacohesive workforce.Goodmentoringexperiencescanbeidentifi ed throughseveralcharacteristics(Box1).Anoverviewofthe variousmentoringmodelswasgiven,alongwithanexplanation ofculturalinclusivityinmento ringunderrepresentedgroupsin healthprofessionsandsuggestionsregardinghowmentoring canenhanceeffortstoachievediversity,equity,andinclusion (DEI)indentistry.
CoachingandSponsoring
Severalfactorscontributetothechoiceofmentoringmodel that fi tsasituation( Box2 ).Theseincludethementee ’sneeds, thementor’savailability,capacity,andskillset,andthetypeof mentoringthat fi tsthesituationandtypeofhelpneeded.Among theapproachesarecoachingandsponsorship. Coaching isa componentthatusesmentorswhoarewell-informed,strongly skilledininterpersonalrelations,abletoperformactivelistening well,andcapableofcreatingajudgment-freeenvironment. Sponsorship ,whichinvolvesadvocatingforthementeeand increasinghisorhervisibility,isariskierapproach,withthe sponsoringmentorriskinghisorherreputationshouldthe menteebeunsuccessful.
An informalmentoring approachcandeveloporganicallyor throughself-selectionbymentorormenteeandcanbeintegratedintovariousmentoringmodels.Theinformalapproach hasnoformalstructureortraining,nopresetgoals,andallowsfor fl exibilityandadaptationovertheevolutionofthe relationship.Amorerelaxedand fl uiddynamicdevelopsbetweenmentorandmentee.Incontrast, formalmentoring is highlystructured,withsettrainingroutinesandspeci fi cgoals. Mentorandmenteemustcommittofollowtheguidelinesand expectationsandadheretotheframeworkoftheformal model.Itcanalsobeintegratedintodifferentmentoring situations.
Traditional1-on-1mentoring,whichisalsocalled dyadic or vertical mentoring,involvesahighlyexperiencedprofessionalguidinga lessexperiencedmenteeandfocusesonpersonalsupportand long-termprofessionalrelationships.Surgicaltraininginthe20th centuryfollowedthismodel. Peermentoring pairsstudentswith studentsoryoungprofessionalswithyoungprofessionalstoprovidemutualsupportandcollaborativelearning.Itcanalsoincludea seniorlevelfacultymentor.Onthe flipside, reversementoring pairs youngermentorswitholdermenteestoshareknowledge,often thatrelatedtoculturaldifferencesortechnology.
Group-focused,E-mentoring,andFunctionalMentoring
Asinglementormayworkwithmultiplementeesorasingle menteemayworkwithseveralmentorsin group or multiple/ constellation/team-basedmentoring. Thegoalistoencourage diverseperspectivesandcollectiveproblem-solvingactivities. In e-mentoring,digitalplatformsconnectmentorsandmentees acrossgeographicboundariestomakementoringmoreaccessibleand flexible. Functionalmentoring isproject-focusedand pairsmentorandmenteeforspeci ficskilldevelopmentor projectcompletion.
Inadditiontoallofthesemodels, mosaicmentoring createsa networkofmentorsfromdiversebackgroundsandexpertise tosupportdifferentaspectsofthementee’sdevelopment.This approachcanbeusedtoacknowledgedifferencesandbridge gapsthatcouldotherwisecreatebarriers,oftenforperson groupswhoareunderrepresentedinhealthcare.Inthisway, theseindividualscanbesupportedintheirquesttoreachprofessionalgoals.Mosaicmentoringusesaculturallyresponsive approachtohelpsupportthementeeinmeetingneedsandgoals.
Viewingmentoringthroughthesocialconstructframeworkrevealstheimportanceofcommunityinmentoring.Socialinteractionsandinterpersonalexchangesarein fl uencedbythe perceptionsofbothmenteeandmentor,leadingtoculturally informedrelationships.Socialcapitalisrelatedtotheconnectionsamongindividualswholiveandworkinacommunity andcontributetotheeffectiveo perationofthatenvironment. Socialcapitalmodelsshowhowrelationshipsandnetworks contributetothesuccessanddevelopmentofindividualsand groups.Inclusivementoringvaluesandappreciatestheculture
Reciprocity: Ensureequalengagementfromboththementor andthementee,fosteringabalancedandinteractive relationship.
Learning: Focusonacquiringknowledgethroughactive participationandengagementinthelearningprocess.
Relationship: Establishandmaintaintrustasthefoundationof thementoringrelationship,ensuringbothpartiesfeelsecure andvalued.
Partnership: Adoptacurrentparadigmthatencouragesactive involvementandcontributionfrombothpartnersinthe mentoringrelationship,promotingmutualgrowth.
Collaboration: Engageinthesharingofknowledge,learning together,andbuildingconsensustoenhancethementoring experience.
Mutuallydefinedgoals: Clearlyarticulateandagreeon learninggoalstoensureasatisfactoryandpurposeful mentoringoutcome.
Development: Focusondevelopingskills,knowledge, abilities,andthinking,guidingthementeefromtheircurrent statetotheirdesiredfuturestate
(CourtesyofChatmonBN,CampbellKM,MoutonCP,etal:Inclusivityin mentorship:Shiftingparadigmsofinclusionindentaleducation. DentClin NAm 69:131-144,2025.)
andbackgroundofmentorsandmenteesandaddressesthe needforadiverseworkforceinhealthcaretoachievebetterpatientoutcomes,moreful fi llingmentorandmenteelives,anda meansfordealingwithbias,stereotypicthreats,andlackofculturalcompetence.
Barrierstoinclusivementorshipcanincludelowmentorexpectations,goalmisalignment,andlimitedmotivationsformentorship.Ifmenteesexperiencesituationsthatblocktheirsuccess andleadershipdevelopment,thehealthcareinstitutioncanalso suffer.Thecreationofinclusivementoringexperiencesrequires definingoutcomes,aligningexpectations,supportingmenteeaspirations,andtrainingmentorstodevelopskillsincrossculturalcommunication.Mentorsmustbewillingtoundergo appropriatetraining,accessresourcesonhowtoworkwithindividualsfromdifferentbackgrounds,andseekinformationon howtorecognizethenegativeimpactofbiasonthementoring relationship.Whenthediversebackgroundsandperspectives ofmenteesareunderstood,thementoringrelationshipis enhancedandthementeethrives.Menteestendtodesireto mirrorthecommunitytheyserve,whichundergirdssocialjustice andtheneedforequitablerepresentationandinclusivity.
Mosaicmentoring: Integratesmultiplementoringrelationshipsto addressthediverseneedsofmentees.Thisapproach leveragesdifferentmentors’ uniquestrengthstoprovide comprehensivesupport,fosteringpersonal,professional,and academicgrowth.
Dyadic-traditionalone-to-one: Atraditionalmentoring relationshipwhereonementorsupportsonementee.This modelfocusesonbuildingastrong,personalconnection, allowingfortailoredguidanceandsupportbasedonthe mentee’sspecificneedsandgoals.
Group/team-basedmentoring: Involvesmultiplementorsand menteesinteractingtogether.Thiscollaborativeapproach encouragespeerlearningandsupport,enhancesnetworking opportunities,andfostersasenseofcommunityandshared learningamongparticipants.
Functional/skill-basedmentoring: Focusesondeveloping specificskillsorcompetencies.Mentorswithexpertisein particularareasprovidetargetedguidanceandtrainingtohelp menteesenhancetheirabilitiesandachievetheircareeror academicobjectives.
Peermentoring: Involvesindividualsatsimilarstagesintheir careersoreducationsupportingeachother.Thismodelfosters mutuallearningandunderstanding,offeringrelatableadvice andexperiencesthatcanbeparticularlyvaluablefornavigating sharedchallenges.
E-mentoring: Utilizesdigitalcommunicationtoolstoconnect mentorsandmentees.Thismodelprovides flexibilityand accessibility,allowingforremotementoringrelationshipsthat cantranscendgeographicboundariesandoffercontinuous supportthroughvirtualinteractions.
(CourtesyofChatmonBN,CampbellKM,MoutonCP,etal:Inclusivityin mentorship:Shiftingparadigmsofinclusionindentaleducation. DentClin NAm 69:131-144,2025.)
thestudents.However,thecurrentdentalschoolfacultyandthe communityofpracticingdentiststendtobelessdiversethanthe studentsenteringdentalschoolorthedentalworkforce.Mentoringisneededtoadvancetheinclusivitythatcanprovide neededdiversityinpractitionersandteachers.However,the goalsoftheindividualcanbeatoddswiththegoalsoftheacademicinstitution,whichcanlimitprogressinthisarea.
Theapprenticeshipmodelhasbeentheprimarymeansforpreparingthenextgenerationofdentaleducatorsandoralhealth carepractitioners.Technologyandexperientiallearningopportunitiesarenowprovidedtotrainstudents,withfacultydevelopmentopportunitiesusedtotransitionandretainthosewhoteach
Theacademicinstitutionshouldcreateanurturing,inclusive environmenttofostermentoringopportunitiesandrelationships thatpreparestudentsfortheirroleasdentalprofessionals.Mentoringhelpsthemprepareandnavigatechallengesandbarriers theymayface.Tocreateasuccessfulandeffectivementoringopportunityrequirestrustandsafety,diverseperspectives,cultural competenceandawareness,mutualrespect,learning,and growth,retentionandsuccess,andopportunitiestoexpand thementoringnetwork.Increatingauthenticandmeaningful mentoringrelationships,biascanbemanagedandproductivity andsuccesscanbesupported.Bothmentorandmenteeshould understandthegoalsoftherelationshipandthetraining.The mentorlifecycle modelcanachievethesegoalsthroughits Box1. CharacteristicsofGoodMentoring
matchingprocess,contracting,useofmentormodelsordiagnostictools,appraisal,andpeerandgroupsupervision.
Themosaicmodelcanbeespeciallyimportantwhenaddressing cross-culturalcommunicationandmentoringdyadsorgroups thatoftendon’tmatchtheculturalidentityofthementee.This modelfocusesonthevalueofthediverseperspectivesandexperiencesthementoringrelationshipoffersandsupportsanenvironmentwherementorsandmenteescanlearnfromone another.Addingthemosaicmodelensuresthatmentoringis bothinclusiveandadaptabletothementees’ variouscultural backgrounds,whichaddstotheeffectivenessandsatisfactionof thementoringencounter.
Dentalmentorsshouldunderstandissuesrelatedtosocialand ethnic/culturalidentitydevelopmentwhentheyareworking withmentees.Identityhasmultiplelayersandisshapedbysociety, politicalpowers,environmentalencounters,personalexperiences,andotherfactors.Cultureshouldbeunderstoodinthe contextofeachindividualandtrainingincorporatedthataddresses thetenetsofself-identity,community,andindividualneeds.
Inclusionorinclusivityhasbeenvariouslydefined,buttheconcept’simportanceisclearwhenitiscoupledwithdiversityandequity(DEI)(Box1).ThediversityoftheUSpopulationhasbeen changingandincreasingsignificantly,sothatby2034,thenumber ofadultsoverage65yearswillbegreaterthanthenumberofchildrenunderage18yearsandnon-Hispanicwhitepersonswillno longerbethemajoritygroup.Ifhealthcareprovidersoptimally mirrorthepopulationdemographics,significantchangesinthis workforcewillbeneeded(Figure1).Decadesofinequityand injusticehaveoccurred,sothathistoricallyunderservedand marginalizedgroupsaremoresusceptibletosignificanthealth problemsandhighermortality.Morerecently,strongevidencebasedtieshavebeenestablishedbetweenmedicineanddentistry, withgoodoralhealthneededtoensureoverallhealth.Todevelop aworkforcethatmirrorsthepopulation,dentistrywillneedto managechallengesassociatedwithmovingforwardandinstitute approachesthatwillcreateinclusiveenvironments.
FromExclusiontoInclusion
Dentistryhasoftenbeenexcludedfrommedicalhealthcare becausethosewhotreatedteethweren’tconsideredqualified
Effectivementoringprogramsfordiversegroupsofindividualsmustaddressthesocialandethnic/cultural identitydevelopmentofeachperson.Mentorsmust beawareofthemanylayersofidentityandhowthey areshaped.Inclusivementoringindentaleducation isanimportantmeanstoachievethegoalofDEIand tocreateadiverse,supportive,andsuccessfulprofessionalenvironmentfordentalpractitioners.
ChatmonBN,CampbellKM,MoutonCP,etal:Inclusivityin mentorship:Shiftingparadigmsofinclusionindentaleducation. DentClinNAm 69:131-144,2025
Reprintsavailablefrom BNChatmon,1900GravierSt,Off5B14, NewOrleans,LA70112,USA;e-mail: bnwoko@lsuhsc.edu
tobeseenashealthcareproviders.Broaderhealthcarediscussionsanddecisionshaveomitteddentalinput,seeingdentistryas apracticethatisbetterseenasatradeandispracticedindependentlyratherthancollaborativelylikemedicine.Teethhavebeen viewedasdisposableandinevitablytobelost,whichlowered theirvalue.Inaddition,theconceptoforalhealthcarewasn’t embracedinthewaythatmedicalspecialtieswere.Asaresult, dentistrywaschallengedandhashadtoaddressthedynamics ofthedentalteam,themedicalsystem,andoralhealthdisparities, amongotherin fluences.
Amoreholisticandinclusivecaremodelisneeded,onethat viewsallthebodysystemsandthemouthasimportantcomponentsofhealthcare,puttingallcareprovidersonanequal footing.Humanmicrobiomeresearchhasindicatedtheneedto includetheoralcavityaspartofthebodyinachievinghealth carefortheentireorganism.
Dentalprofessionalswhopracticeoralsurgeryoftenhaveboth dentalandmedicaldoctoraldegrees,allowingthemtobe includedmorereadilyinobtaininghospitalprivileges,accessto surgicaltime,andrespectinboththedentalandmedicalworkforcesandinthegeneralcommunity.Incontrast,dentalhygiene
Box1. ExamplesofDefinitionsforInclusionintheContextofDiversity,Equity,andInclusion
AmericanDentalAssociation
Inclusion:Enablesustostrivetohaveallpeoplerepresentedandincludedandmakeeveryonefeelasenseofbelonging,notonlyfortheir abilities,butalsofortheiruniquequalitiesandperspectives.
AmericanDentalEducationAssociation
Inclusion:Thepracticeofleveragingdiversitytoensureindividualscanfullyparticipateandperformattheirbest.Inclusionisshared responsibilityofeveryonewithinthecommunity.Aninclusiveenvironmentvaluesdifferencesratherthansuppressingthem;promotesrespect, success,andasenseofbelonging;andfosterswell-beingthroughpolicies,programs,practices,learning,anddialogue.
FDIWorldDentalFederation
NationalHealthPolicy:ThenewdefinitionoforalhealthadoptedbytheFDIWorldDentalFederationGeneralAssemblyin2016haslaidthe frameworktoallowtheprofessiontoreflectonwhatoralhealthencompassesanditsimplicationfornationaloralhealthpolicies.Further,this definition,whichwasapprovedbyconsensusbyFDIconstituents,favorstheinclusionoforalhealthinallhealth-relatedpolicies...
OurValues
Cultureofinclusiveness:Wedeliberatelyandmeaningfullyengageandseekrepresentationfromthediverserangeoforalhealthprofessionals andthecommunitiesandindividualstheyserve.Thisisparamounttoachievingourmission.
InternationalAssociationforDentalResearch
SCIENCEPOLICY: Diversity,Equity,Inclusion,Accessibility,andBelongingStatement: Inclusionistherecognition,appreciation,anduseofthe talentsandskillsofallbackgroundsbycreatingawelcomingenvironmentthroughtheproactiveidentificationandremovalofthebarriersthat impedethesuccessofall.
NationalAcademiesofSciences,Engineering,andMedicine
EndingUnequalTreatment:StrategiestoAchieveEquitableHealthcareandOptimalHealthforAll.
Inclusion:Effortsusedtoembracedifferences;alsousedtodescribehowmucheachpersonfeelswelcomed,respected,supported,andvalued inagivencontext.
[WhiteHouse]ExecutiveOrder(14035)onDiversity,Equity,Inclusion,andAccessibilityintheFederalWorkforce
Theterm “inclusion” meanstherecognition,appreciation,anduseofthetalentsandskillsofemployeesofallbackgrounds.
(CourtesyofHalpernLR,KasteLM,SoutherlandJH:The “I” indiversity,equity,andinclusion:Thechallengeofinclusivityindentistry. DentClinNAm 69:1-15,2025.)
isoftenperformedbywomen,whohavehistoricallyfacedgender barriersaswellasadverseattitudestowardanypromotions, progress,andrespectfromotherhealthpractitioners.Increasing
preventionandaccessaregoalsrecognizedasimportantto healthcare,withdentalhygienistsactuallyservingaspreventive actionspecialists.Yetjust24dentalschoolsofferdentalhygiene
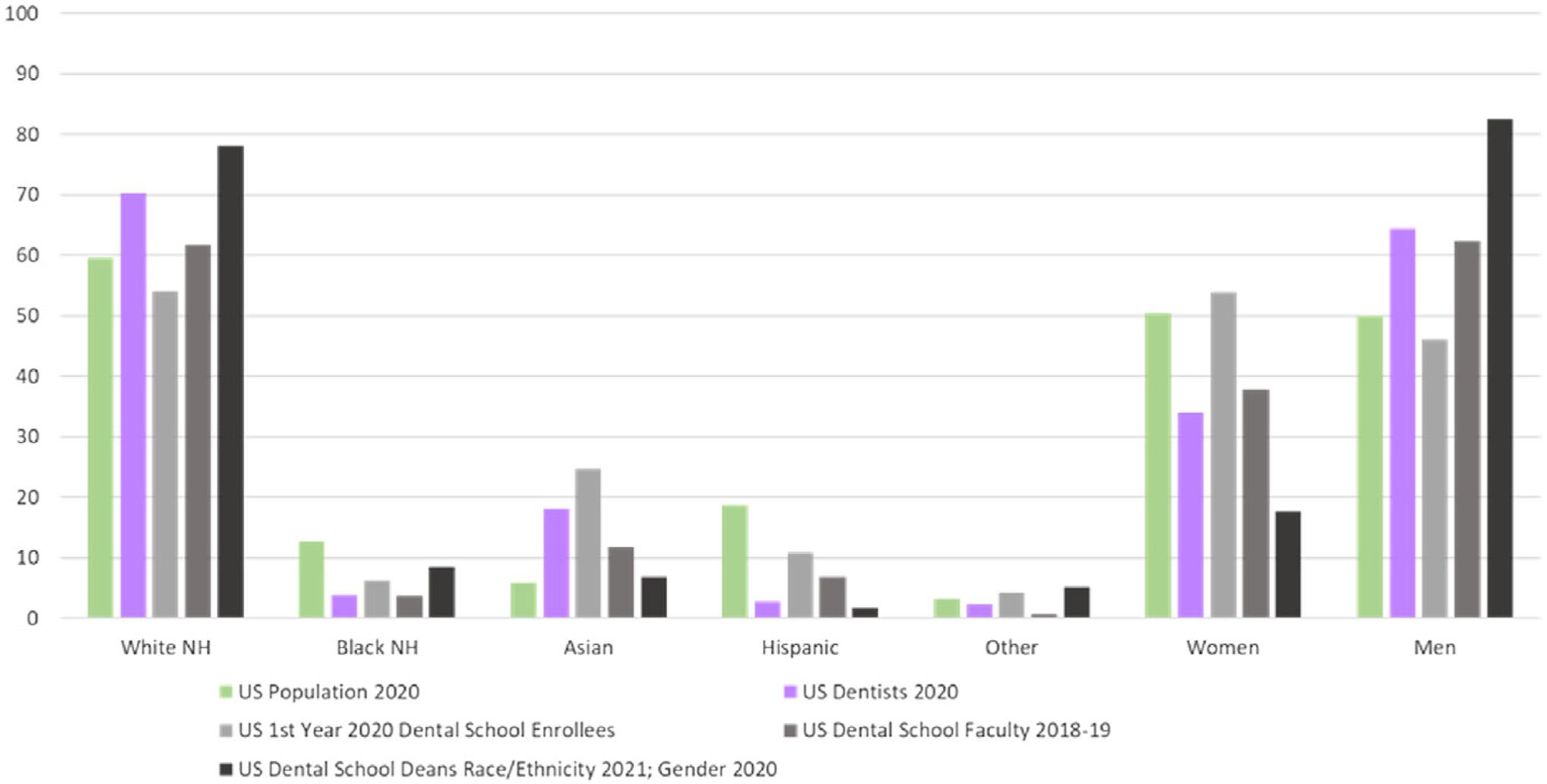
Figure1. Comparisonofselecteddemographicpercentagescirca2020bytotalpopulation,dentistworkforce, firstyeardentalstudents,dentalschool facultymembers,anddentalschooldeans.(CourtesyofHalpernLR,KasteLM,SoutherlandJH:The “I” indiversity,equity,andinclusion:Thechallengeof inclusivityindentistry. DentClinNAm 69:1-15,2025.)
programsandjust7%oftheseprogramscollaboratewithprogramsfordentalpractitionertraining.Aco-educationalgapexists thathasnotyetbeenresolvedevenwhentheprogramingdeliberatelypromotescollaborativepractices,includinginterprofessionaleducation(IPE).
Actionstohelpintegrateratherthanseparatethemedicaland dentalprofessionshavebeentaken,butuntildentistryisanintegralandacceptedcontributortotheprocess,noviablesolutions willbedevelopedtoaddresstheoralhealthcrisis.Dentistryhas beenexcludedfromUShealthcarecoverageviainsurance,with differentresponsescreatedinbothinsurancecoverageand managedcaresituations.Dentistryisn’tconsideredafullpartner inthe2003InstituteofMedicine(IOM)reportonUnequalTreatment.AlthoughMedicaidcoversoralhealth,eachstateisallowed tosetlimitstotheextentandtypeofcoverage.Medicarehasprovidedminimalcoveragefordentalstructuresorprocedures,and thedoublestandardbetweenmedicineanddentistryisseeninaccesstooralhealthcare,stilloftenviewingthemouthasoutside theconceptofhealth.
Seeingoralhealthincludedandintegratedintoprimarycareis widelydesired.TheAssociationofStateandTerritorialDental Directors(ASTDD)participatesinpolicydevelopmentandhas emphasizedtheimportanceofintegratingoralhealthintoprimarycareintheirpolicystatement.TheASTDDrolecaninfluencetheallocationofresourcestothevariousstatechief healthof ficers.
InclusivityinResearchandProgramFunding
TheNationalInstitutesofHealth(NIH)hasdevelopedcrossinstitutecollaborations,someofwhichintersectwithdentistry. Inaddition,federalagencieshavesupportedtrainingforhealth careproviderstodevelopaprimarycareworkforcethatcan addresstheexpansionoftheUSpopulation.The firstphasesof theseprogramsincludedmedicineanddentistry.
AssociationalActivity
TheAmericanDentalEducationAssociation(ADEA)StrategicDirectionsWorkgroupfor2019-2022emphasizedthe importanceofdevelopingandsupportinginclusiveenvironmentsamongfaculty,students,staff,andadministrators.Inaddition,theInterprofessionalEducationCollaborative(IPEC)
providedthemeansforinvolvingdentistryinIPEandcollaborativepractice.However,recentreportsdonotincludedentistry intheoutcomesassessmentofIPE.Dentistrymustengageboth externallyandinternallytoexplorehowtoexpandeffortsto promoteinclusivityindentalpractice.
Intersectionalityreferstotheefforttoprovideusefulandactionableinformationthatdealswithinequalitiesandincorporatesinclusionintheworld.Theeffortsaresimilartomediationbut focusonidentifyingandnamingthecomponentstobeaddressed. Anapplicationwasseeninthelackofequalityacrossallracial/ ethnicgroupsregardingtheincreasedrepresentationofwomen indentistryintheUSandUK.Asthebreadthanddepthofintersectionalityhaveintensi fied,somespeci ficfactorswereidenti fied thatmayaddtoinequalitiesanddisparities.Theseincludesocial determinantsofhealthandpersonalfactors,suchasproficiency inEnglish,health/dentalinsurancecoverage,religiouspractices, andgenderidentity.
Asdentistryevolves,inclusionisavitalaspectbothin dentaleducationandinexpandingtheworkforce. However,dentistrymustbepartofthediscussions anddecision-makingprocessesinvolvedinoverall healthcare.Oralhealthmustbeincludedingeneral healthinitiativesbasedontheevidence-supportedbidirectionalityoforalandoverallhealth.Dentaleducationandpracticemustdevelopinclusive,welcoming, andengagingenvironments.Theoralhealthcare teammembersshouldreceiveproperrespectand collaborativeopportunitieswithotherhealthcareprovidersastheyaddresshealthdisparitiesandinequalities.
HalpernLR,KasteLM,SoutherlandJH:The “I” indiversity,equity,andinclusion:Thechallengeofinclusivityindentistry. Dent ClinNAm 69:1-15,2025
Reprintsavailablefrom LRHalpern,DeptofDentalMedicine/ WMC/NewYorkMedicalCollege,MaceyPavilion,100Woods Rd,Valhalla,NY10583,USA;e-mail: halpernl@nychhc.org
TheAmericanswithDisabilitiesAct(ADA)allowsforreasonable accommodationstobemadesothatemployeeswithdisabilities cancontinuetoperformtheessentialfunctionsoftheirjobs.The processofseekingandobtainingsuchanaccommodationmaybe inquestioninsomesituations.Acasewaspresentedinwhichthe claimforaccommodationwasdenied.
OiryawaspromotedtotrainingcoordinatorattheMando AmericanCorporationbuthadseveralmedicalconditions thatimpactedtheworkingsituation.Theemployeehandbook statedthatemployeesseekingareasonableaccommodation foradisabilityhadtonotifythehumanresources(HR)department,butMandohadtherighttorequestmedicaldocumentation.Employeeswhowantedtoreportdiscriminationor retaliationalsohadtocontactHR.AlthoughMandoallowedemployeestotakeanapduringlunch,sleepingonthejobwasone ofthebehaviorsthatcouldresultinimmediatetermination. Oiryastatedthathissupervisorswereawareofhismedicalissuesandhadaccommodatedhimwhenhehaddif fi cultysleeping atnightandsleptatwork.Inaddition,theyknewthathesometimestookover-the-countermedi cationsthatresultedinmakinghimsleepy.
ThreecoworkersreportedOiryawasasleepathisdeskwhile notonanybreak,andthesupervisorissuedaLastChance Agreementratherthanaterminationnotice.Theprocess withthisagreementrequiredhimtorereadthehandbookand signaformstatinghehadreaditandwasawareofitscontent regardingthecompany ’smisconductpolicy.Hewasrequired tomeetallofthehandbook’sterms,beunderthetermsfor 2years,and,shouldhenotadheretotheterms,faceimmediate termination.Oiryaexplainedtheaccommodationsthathad beenextendedtohimandrefusedtosigntheagreement.He askedthathiscurrentsupervisor granthimaninteractiveprocess,includinganopportunitytorespondinwritingtothe agreement,advancenoticeinaformalwrittencomplaintstating thebreachesofpolicythatwerebeingalleged,afullevidentiary hearing,awrittendecision,andanopportunitytoappeal.His opinionwasthattherewasaninherentaccommodationinthe formofas-neededbreaksintheADApolicy.TheHR
departmentdecidedtoputeverythinginOirya ’ s fi leandnot pursuetermination.
Amonthlater,Oiryasufferedfoodpoisoningatacompanypizza partybutrecoveredafterpharmacologicaltreatment.Ten monthslater2coworkersapproachedhisnewsupervisorwith picturestakenthatshowedOiryaasleepathisdesknotduring lunch.TheHRdirectoragreedtotheterminationofOirya.He suedMando,sayinghehadn’tbeengivenareasonableaccommodationandwasbeingdiscriminatedagainstforrequestinganaccommodation.Severalmonthslater,Oiryaaddedacomplaint thathewasbeingwrongfullyterminatedandacomplaintthat hewasavictimofdisparatetreatmentbecauseanother employeeofMandohadbeengivenanaccommodationafterbeingfoundsleepingonthejob.Ajudicialmagistratedeniedboth claimsasbeinguntimely filed,andtheappellatecourtupheld thatdecision.
Theappealscourtshowedthattheplaintiffhadtoshowthat thedisabilityclaimedmustbecoveredundertheADA,that heorshewasquali fi ed,andthatheorshewascausedtosufferunwanteddiscriminationbecauseofthedisability.The courtalsoexpandedonthecharacteristicsofareasonableaccommodation,notingitwouldbeamodi fi cationoradjustmentthatallowstheemployeetoperformessentialjob functionsandcanincludevariousmodi fi cationsofthework scheduleoremploymentpoli cies.Onceclaimingadisability, theemployeehastheburdenofidentifyingthetypeofaccommodationheorshebelievesisreasonableandthataddressestheissuesheorsheisfacing.Theemployer’sduty toprovidetheaccommodationisn’ttriggeredunlessthe employeespeci fi callydemandsit.Theemployermustthen engageinaninformal,goodfaith,interactiveprocessthat statestheemployee’slimitationsandtheappropriatenessof theaccommodation.
Oiryarequestedafull,formalinvestigationofthecomplaint,an opportunitytodefendhimself,therighttomeaningfuldueprocess,andanappealifdesired.ThecourtfoundthatOiryadidn’t speci ficallydemandanaccommodationanddidnotshow MandodeniedhimareasonableaccommodationorthatMando
hadadutytoinitiateaninteractiveprocesswithhim.Thecourt statedthatheshowedhewasengagedinstatutorilyprotected conductandhadexperiencedanadverseemploymentaction, butcouldnotshowthatanycausalconnectionbetween theseelementswaspresent.Theretaliatorybehaviorwasn’t acceptedbecauseofthe10-monthdelay,sotheclaimofretaliationfailed.
Employeeswhohaveadisabilityofsometypeandrequesta reasonableaccommodationtocontinuemeetingthedemands oftheirjobcanbefoundinmanysituations.Some personsmaystatethattheindividualshouldsimplyseek anotherjob,andsome findthatsuchaccommodation shouldn’tbeconsideredabigdealandemployeesareentitled tosuchmeasures.
TheADAisthelaw,andareasonableaccommodation requestthatmeetstherequirementsshouldbeinstituted.Withtheshortagesintheworkforcethatexistin thedentalcommunity,it’sclearlydifficultto findand keepgoodemployees.Negotiationscarriedoutin goodfaithshouldbeundertakentoidentifyreasonable accommodationsthatworkforbothemployeesand employers.
JerroldL:Onbeingaccommodating. AmJOrthodDentofacial Orthop 166:616-618,2024
Reprintsnotavailable
Technologicaladvances,afocusonpersonalizingcare,andthe knowledgethatoralandsystemichealthconditionsareconnectedhasledtotheconceptofcareconvergence.Care convergencereferstotheintegrationofmedicalanddental care,withabetterunderstandingthatnotjustoralhealth butoverallhealthprofilesareimportanttopatientmanagement.Amultidisciplinaryapproachwithcollaborationandinformationsharingamongprovidersofbothoralhealthand systemichealthprovidesaholisticenvironmentforcare.The advantagesofcareconvergenceand5strategiesforcombining carewerediscussed.
Convergentcaremodelscanimprovepatientoutcomesbyaddressingsystemicconditionsthatcanin fluenceoralhealth.This collaborationcreatesacompetitiveedgeforthedentalpractice, whichcanoffervariousservicesandnewrevenuestreamsthat alignwithoutcome-basedcare.
Thesuccessfulintegrationoforalandsystemichealthcareusually restsonspeci ficstrategiesthatarethefocusofpractice.Rather thandoingmore,dentalpracticescandothingsdifferently,so thattheycanadaptexistingwork flowmodelsandavoidovertaxingtheteam.
Systemichealthassessmentscanbedoneaspartofthepatient’ s routineoralhealthcarevisits.Variousdiagnostictoolscanfacilitatetheincorporationoftheoverallhealthassessments, includingthefollowing:
Duringroutinecleanings,dentistscanusefullyintegrated work flowstoadministerscreeningquestionnairesfordetectingconditionssuchassleepapnea.Thesework flowsmayconnecttoanetworkofsleepspecialistsandprovide administrativesupportforthepracticetoprovideadiagnosis, treatment,andpaymentacrossthemedicalanddentalplans. Duringchairsidetime,thedentistcanobtainbloodsamples thatcanbeanalyzedformarkerstoidentifyinflammationor glucosecontrolproblems,forexample.Routinecheckups gainvaluewithoutinvestingsignificantfundsonnew equipment.
Salivarydiagnostictestsforperiodontalpathogensorinflammatorybiomarkerscanalsobeaddedchairside.Thispractice providesthedentalcareproviderwithactionableinsightinto thepatient’sdiseasestatusandhelpincraftingtreatment plans,providingfollow-upcare,andcollaboratingwithmedical careprovidersifasystemicproblemexists.Eventually,pointof-carediagnostictoolsmayoffertheabilitytoreliablydiagnosecommonoropharyngealcancers.Affordablepoint-of-
carediagnostictoolsmaysomedayusegenomicandprotein markeranalysisthatprovidesnoninvasive,real-timesolutions.
Newwaystocollaboratecanbeusedtointegratethepracticesof medicalanddentalcare.Oneinnovativeapproachistoestablish partnershipswithlocalphysicians,endocrinologists,andcardiologists,whichcanfacilitatecross-referrals.Notonlycanthe dentalofficerefertothemedicalcareproviders,butmedical careproviderscanrefertodentalpractices.Forexample,patientswithhighC-reactiveprotein(CRP)levelscanbereferred toacardiologistforevaluation,andtheseproviderscanreferpatientstothedentistforperiodontalcare.Oftentelehealthplatformsareusedtoconsultwithspecialists,withthesevirtual collaborationsprovingbothcost-effectiveandtime-efficient whileensuringcoordinatedcarewithoutaphysicalreferral.
Cross-referralstodentalspecialistscanalsoprovidecareconvergencethatenhancesoutcomeswithfewchangesintheexisting work flows.Periodontalevaluationscanbecoordinatedbefore andduringorthodontictreatment,sothatperiodontalissues canbemanagedearly.Prosthodontistsalreadycollaboratewith periodontistsfororalrehabilitation.
Digitaltoolstodaycanallowforstreamlinedcommunication andfreeclinicalteamsfromrepetitiveadministrativetasks. Thiscanbeseeninaugmentedteams,electronichealthrecord (EHR)integration,andpatientmanagementsystems.Arti ficial intelligence(AI)enablesconvergentcarebyassistingclinical teamstoanalyzeandvisualizediagnosesandautomateprocesses,includingbilling,inventorymanagement,andcoordinationofcare.EHRsystemscanbeintegratedthroughpublicly availableapplicationprograminginterfaces,sothatdentists cansharecriticalhealthdatawithprimarycareproviders. Evenwithoutcompleteintegration,digitalsolutionscanfacilitatetheexchangeofreportsandreferrals,whichreduces administrativebarriers.Eventuallytheseintegrativeprocesses maybecomebundledasastandardoffering.
Patientmanagementsoftwarethatincludesspacefortracking nondentalhealthmetricsallowsforsharingwithpatients, payers,andmedicalprofessionals.Thiscanbepartofacomprehensivecareplanthattracksclinicaloutcomesandthetotal costofcare.
Thefocusofroutinecareappointmentscanbeexpandedto includepreventivemeasuresthataddressoverallhealth.Carious lesionsmaybetreatedthrough fl uoridevarnishapplicationsfor thoseathighrisk.Incipientlesionscanbeaddressedwith
innovativenoninvasivetreatmentsthatallowfortargetedremineralizationof “watchareas” beforemoreinvasiveprocedures arerequired.Thismaintainsthehealthofnaturaltoothstructuresandfreesupchairtimeformorecomplexprocedures.
Patienteducationismorereadilyundertakeninadentalappointmentthaninmedicalappointments.Patientscanlearnhoworal healthaffectsconditionssuchasheartdisease,diabetes,andpregnancycomplications.Thisachievesenhancedpatientawareness andencouragespatientstobemoreengagedinoralcareroutines.Inaddition,treatmentplanacceptancecanbehigher, improvingoutcomes.Thepatient’sneedsandcontextforthe visitareimportantcomponentsofthisintegration.Thedentist andteamshoulddeterminewhatisappropriateastheybuildtheir relationshipwiththepatient.
Value-basedcarepaymentmodelsanddentalbene fitdesignsthat encouragepreventionandcross-disciplinarytreatmentplansare requiredforthebestoutcomesofcareconvergence.Untilthese paymentmodelsareadopted,convergentcaremodelscan enhancethevaluetothepatientanddentalpracticeevenin fee-for-servicesituations.Private-paypracticesleadthewayin educatingandempoweringpatientstocarefortheirhealthand choosetreatmentandbene fitplansthatenablecareconvergence.Whileawaitingthebroaderadoption,dentalpractices canprovidecomplementaryservicessuchasbundledcarepackagesandoutcometracking.
Ratherthanrequiringdentalpracticeteamstodomore,care convergencemeansdoingthingsdifferently.Withthetechnologiescurrentlyavailableandinviewofthosecominginthenear future,dentalpracticescantakestepstointegratemedicalpursuitsintotheirexistingpatientwork flows.
Thecareconvergenceapproachwillenhancepatient outcomes,buildstrongerrelationshipsamonghealth careproviders,andpositiondentalpracticesinthe broaderhealthcareecosystem.Careconvergence shouldbeconsideredasastrongtoolforpractice growthandbetteroverallhealthforpatients.
FilipovaM:Careconvergence:5provenstrategiestoelevate dentalcareandpatientoutcomes. DentEcon 115:14-16,2025
Reprintsnotavailable
Updatestothevariousformsofcommunicationusedinadental practiceshouldbedoneregularlytomaintainaproperdialogue withpatients.Officepolicymanuals,healthhistoryforms,and theuseofelectronicanddigitalcommunicationformsshould bereviewedtoensurethatpatients’ preferencesarebeing used,theinformationiscurrent,andtheelectronicordigital communicationssystemsareappropriatelyprotectedfromunauthorizedaccess.
Patientcommunicationchoicescancontributetoanincreaseinpatientnumbers,greaterlevelsofpatientsatisfactionandretention, andexpandingservicesandtreatmentacceptance.Theofficepolicy manualshouldspecifytheobjectivesofthepracticesothatthe dentalteamknowsthetargetedgoalsandhowtoachievethem.
Theuseofcontactmanagementsoftwarehasmadephonecalls topatientsregardingappointments,billing,andinsuranceissues theleastlikelymeansofcommunicationtobeselectedbypatients.Whenpatientsaregiventhechoice,mostwillselectemailortextsastheirpreferredmodeofcommunication.It’ s importantthatthepolicymanualsetsforththepractice’ s preferredproceduresforthiscontactandthatthepolicies ofHealthInsurancePortabilityandAccountability(HIPAA) arerespected.
Withthepreferenceforanelectroniccommunication,dental practitionershavelessphysicalorpersonalcommunication withpatientsbeforetheycomefortheirappointment.Thiscan beaddressedbytakingstepstobuildinstantrapportandcommongroundwithpatients.Thispatient-practitionerrelationship canresultinafullscheduleofpatients, filledhygienespots,a growthinpatientnumbers,andsuccessinmeetingproduction goalsandcollections.
Stepstotakeinbuildinggoodrelationshipswithpatientsinclude establishingcommonground;creatingrapportandtrustfrom the fi rstcontactmadewiththepatient;andprovidingclearexplanationsforpatients,whichmeanstakingcaretoavoidjargon, tonotspeaktoofast,andtonotmakestatementsabouttheprocedurethatareincompleteandcausefear.It’simportantto listenandmakeeyecontactwhenthepatientspeaks.Thedental teamshouldmaintaintransparencyintheircommunicationsso patientsarecompletelyadvisedandcanmakeanevidence-based decisiononcare.It ’sbesttotakethetimetoassesswhatthepatientknowsandthentailorfurthereducationtothatlevelof understanding.
Settingupthedentalrecordsandestablishingsuccessfulinsurancebillingrelyonacompleted,detailedhealthanddentalhistory form.Somepatientsmaynotseetherelevanceoftheirmedical healthhistorytohavingtheirteethcleaned,sothedentalteam shouldexplainhowimportantthisinformationis.
Onlineformsforthehistoryallowpatientstocompletethe informationbeforetheirappointment.Thisavoidshavingthe patientfeelrushedandpermitsthemtohaveresourcessuch asthenamesoftheirprescribeddrugsanddosagesathand. Oftenpatientsrequirereadingglassestocompletephysical forms,whichcanbeawkwardinthedentalchairsetting.As aresult,theformscanbeincompleteorinaccurate,especially inrespecttothemedicationsbeingtaken.Thiscanaffect dentalcare.
Updatestopasthealthhistoryformscanbedonebeforepatientscomefortheirappointmenteitherthroughaform accessiblethroughthepracticewebsiteorthroughcontact software.Anyformforthehistoryshouldprovidesufficient roomforpatientstolistalltheirmedications,dosages,and reasonfortakingthemedication.Patientscanbeembarrassed tolistsomemedications,sothedentalteamshouldreviewthe historyforanyconditionsthatwouldbetreatedpharmacologically.Patientsshouldalsobedirectedtolistvitaminsand over-the-counterproductsandwhytheytakethem.The dentalteammayneedtoaddressthequestionofwhythe medicationisbeingtakenatappointmenttimeandupdate therecordthen.Somepatientstakemedicationssporadically andthisshouldalsobenoted.
Artificialintelligence(AI),electronichealthrecords(EHRs), practicemanagementsystems,digitalwork flows,and3-dimensional(3D)printingmaybeusedbythedentalpracticeinpatient andpracticecommunicationmethods.TheAmericanDentalAssociation(ADA)offersguidancefortheuseofsocialmediain particular,asfollows:
Thestandardrulesregardingdiscrimination,privacy,and employmentpoliciesapplytotheuseofonlinecommunications(socialmedia).
Becausefreespeechandopendiscoursearecurrently favored,it’sillegalundertheNationalLaborRelationsAct tohavepoliciesthatprohibitemployeesfromdiscussingthe termsandconditionsofemploymentwithotheremployees.
Thepractice’sgeneralpoliciesoremploymentpoliciescannot
discouragelegallypermissiblediscussionsaboutworkingconditions,hours,orwages.
Socialmedialawisevolving,sothepracticemustmonitordevelopmentsandmakeappropriateupdates.
Neithercopyrightednortrademarkedcontentcanbeposted withoutthepermissionofthecontentowneroracitation,as appropriate.
Thepractice’ scon fidentialorproprietaryinformationcannot bedisclosed.
Anappropriatewrittenconsent,authorization,waiver,or releasesignedbythepatientorguardianmustbeobtained topostinformationaboutpatients,employees,orotherindividuals.Thisincludestestimonials,photographs,radiographs, oreventhenameoftheindividual.
Allpostingsshouldbemonitoredforcompliancebyadesignatedteammember.Ifthepracticehasapolicytomonitorsocialmediaandfailstodosoordoesnotactoninformation foundduringthemonitoring,thepracticecouldbeheldlegally liable.Inappropriate,derogatory,ordisparagingpostings shouldberemovedatthediscretionofthepractice,butit’ s besttoerronthesideofcaution.
Evenifamonitorisdesignatedtomanagesocialmedia,the dentist/ownershouldhave finalapprovalonpostings.
Employeesshouldn’tspeakonbehalfofthepracticeunless theyhavethedentist/owner ’sauthorization.
Communicationmethodsarechanging,andtherules forusingthenewerapproachesarealsoevolving.The dentalpracticeshouldensurethattheircommunication methodsareusedresponsiblyandinaccordancewith boththeneedsofthepatientsandtherulesofthe ADA,amongotherauthorities.Withtheadvances madeindigitalandelectroniccommunicationmethods, thedentalpracticecanreachmorepeoplewithgreater optionsincollectinghealthhistories,schedulingvisits, anddevelopinganetworkthatpatients findeasytouse.
VargasE:Howyoucanreassessdentalpracticecommunication policiesfor2025. DrBiscuspid.com, Dec10,2024
Reprintsnotavailable
Theterm deepfakes combinesdeeplearningandfakeasalabelof technologythatusesartificialintelligence(AI)algorithmsto createrealisticvideoandaudiorecordings.Oftentheserecordingsdepictthelikenessesandvoicesofhigh-pro fileindividuals suchasTomHankswithouttheirconsent.Thisprocessis donequiteeasilywiththeadvancesinAI,accesstolargedata sets,andincreasedcomputationalpower.Althoughthesetechnologiescouldpotentiallybeusefulforpositivepurposesineducationorentertainment,theycanalsobeusedmaliciously. Creatingmisleadingcontentwherethehigh-profileindividualendorsesormakesclaimsfortheefficacyofunprovenmedicalor dentalproductsiswellwithintherealmofpossibility.Celebrities tendtohaveasigni ficantimpactonconsumerbehaviorandindividualscanbeobliviousregardingtheneedforevidence-based recommendations.Thedeceptivepracticeofusingdeepfakes tospreadmisinformation,possibledangerousabusesrelatedto dentistry,andregulatorymeasuresneededtoaddressthesituationweredescribed.
Anyonewithahigh-endgaminglaptopandbasicskillscan generateadeepfakevideo.OpenAI’srevelationofSofa,a
video-generationAI,hasfurthercomplicatedthedifferentiation ofmisinformationandauthenticatingcontent.Althoughthey canbecomparabletoin fluencer-drivenadvertisinginthemisinformationthatisoffered,deepfakesdeceptivelyusewell-known figurestoendorseandrecommenduntestedproducts.Unapprovedmedicalordentalproductsmayactuallybeableto harmpatients.Thevideosunderminethepublic’strustinscience andmedicine.Incontrast,influencersusuallypromoteproducts transparentlyandaremotivatedbysponsorshipagreements.To behonest,somein fluencersmaypostvideosonsocialmediawith productsorsecretsthat “doctorsdon’twantyoutoknow about.”
Ifadeepfakeshowsawell-knowndoctorendorsinganewanduntesteddrugasamiraclecureforcurrentlyincurabledisorders, patientsarelikelytobeswayedtobelievetheproductoffersa realcure.Usuallynoevidenceofef ficacyorsafetythroughclinical trialsisoffered.Whentheagentdoesn’twork,thepublicconfusionandmistrustwouldincreasethedif ficultyimplementing properhealthmeasures.Iforthodonticdevicesaretoutedas abletoalignteethinaridiculouslyshorttime,ortherapiesfor rootcanalsorcavitiesarepromisedtobepainfreeandnoninvasiveforseriousdentalconditions,patientsmaybepersuadedto
trythesemeasuresandsuffersigni ficantharm.Thetechnology couldsigni ficantlyboostholisticorhomoeopathicdentistryand theanti-fluoridemovement,possiblyalteringpublicperspectives regardingdentalcare.
Productsthatareactuallyuselessorevendangeroushavebeen advertisedonsocialmedia.However,ifadentist’slikenessand voiceareimpersonatedwithouthisorherconsentandisused topromotetheseproducts,patientsmaybemisled,thedoctor’ s reputationcouldbeharmed,andthetrustofhisorherpatients couldbelost.Evensendingatakedownrequesttothesocialmediaplatformmaybeafutilepursuit.Boththeconsumerandthe personwhoseimagewasusedwithoutpermissionareatriskfor greatharm.Thedeepfakescreateaveneerofcredibilitythatleads unsuspectingconsumerstotrustinnon-trustworthyproducts. Forgoingproventreatmentstousethesealternativeapproaches canhavedirecthealthrisksforthepatient.
Patientsafetyandprofessionalintegrityareatthemercyofthese deepfakes.Immediateandfar-reachingdiscussionsareneededto setethicalguidelinesandregulatoryframeworksthatwillcurb thepowerofthefalseimages.Amongthemeasuresthatshould beinstitutedisamandatetoclearlylabeldeepfakecontenton socialmediaplatforms,similartowhatisaddedtoadvertisements andsponsoredcontent.Viewerscouldthendistinguishbetween whatisauthenticandwhathasbeenmanipulated.Inaddition, algorithmsneedtobeintegratedtodetectand flagillicit
TheGuidingLeadersorganizationoffersaleadershipanddevelopmentprogramforwomendentiststhatisfollowedupbyan alumnigroupchat.Thischatisaplacetoaskquestions,compare industrytrendsindifferentareasofthecountry,andoffer encouragementthroughoutone’scareer.Technologyisrelevant todentalpracticestoday,buttherearemanydetailsthatneedto beinvestigatedtodeterminewhattechnologyismostappropriateforaparticulardentalpractice.Dentistscanaskforpracticaladvicefromfellowpractitioners,ensuringthatthey recognizethebene fitsoftechnology,canidentifythetechnology thattheywouldusedaily,andlearnwhatinformationisneeded whenmakingapurchase.
Manypracticeshaven’tmadethemovetotechnology,andnew dentistsshouldbeawareofthevalueofseekingoutthose
deepfakes.Lawstoprotectpeoples’ imagerightsareessential. Onlinecontenthasrapidlyexpandedtohaveextensivereach, magnifyingthepotentialimpactofdeepfakes.Theregulationof theproblemwillrequireacomprehensivestrategythatuses technology,legalaction,andpubliceducationalongwith legislationatboththefederalandstatelevelstocombatmedical anddentalmisinformationspreadthroughdeepfakes.
Thepublictrustinhealthcarewasseverelyeroded duringtheCOVID-19pandemic.Havingdeepfakes launchedtospreadmisinformationaboutscientific topicscouldfurtherunderminehowpeopleviewand usescienti ficinformationandmedicalordentalrecommendations.It’snecessarytopreservewhatpublic trustremainsbysafeguardingagainstdeepfaketechnology. PatilS,LicariFW:Deepfakesinhealthcare:Decodingdigital deceptions. JAmDentAssoc 155:997-999,2024
Reprintsavailablefrom SPatil,RosemanUnivofHealthSciences, 10920SRiverFrontPkwy,SouthJordan,UT84095,USA; e-mail: spatil@roseman.edu
opportunitiesthatareforward-focusedandinnovative.Atthis pointinhistory,newdentistsshouldsurroundthemselveswith peopleopentochangeandthosewhoembracetechnologyas animportantpartofdentistry.Technologywillrequirealearning curvebeforeitcanbeproperlyused,buthavingatechnologyforwardviewpointoffersmanybenefits.Workflowsarestreamlined,acceptanceratesrise,patientperceptionisenhanced,referralsareincreased,andthereturnoninvestmentisworthit. Anotherbenefitisthefactthatthelatestproductsaredesigned foreaseofuse.
It ’simportanttoinvestintechnologythatwillbeusedandnot bedazzledbythehype.Amongthosetechnologiesusedevery dayareintraoralscanners,conebeamcomputedtomography (CBCT)units,in-offi cemills,andpracticemanagement software.
Intraoralscannershavechangedhowdentistspractice,allowing imagesoftheteethinrealtimethatarebothaccurateandcompletepicturesoftheoralcavity.Theinformationisshownina readilyunderstoodformat,sointraoralscannersareessential.
Digitalx-rayshavebeenwidelyadoptedformorethan30yearsand areessentialtomoderndentistry.Thedigitalunitsofferedreduced radiation,improvedimagequality,andreducedwaste,sothebenefitsfaroutweighedthecostofthesescanners.CBCTunitsnow producemoredetailed3-dimensional(3D)viewsofbonesand softtissueandproduceaccuratedimensionsofthejaw,canidentify periodontallyinvolvedareas,andcanassessthenasalcavity.It’ s essentialtoallotsufficientspacefortheseunits.
Patientslovetheideaofsame-daydentistryandnotwearingtemporariesforlongperiodsoftimeandhavingtotakeoffextratime fromwork.Dentistsarehappytheycantakecontrolof finaloutcomesandreducelaboratoryfees.Somemillsaresupportedby artificialintelligence(AI) powereddesignproposalsandcan drawfromanextensivearrayofdatabases.Thedesignsare highqualityand fitthepatient’suniqueneeds. Themillingsystemshouldoffermanufacturer-directsupportand continuingeducationalongwiththedevice.Afterbecoming comfortablewiththe firstmill,asecondorthirdmillmaybea goodpurchasesothatmultipledentistscanusetheunitswithout waitingforasingleunittofreeup.Thisalsosimpli fiesscheduling.
Forms,notes,appointmentschedules,reminders,follow-ups it allhastobeorganizedandeasytoaccess.Theuseofpractice managementsoftwarehasrevolutionizedtheprocess.Factors toconsiderwhenpurchasingpracticemanagementsoftware includethecomfortlevelandcapabilitiesoftheofficestaff;the officepriorities(speed,personalization,simplicity,etc);and howmuchthesoftwarecostsversusthefeaturesitoffers.
Technologyisexpensivebutifit’stherighttechnologyitwillpay foritself.Decidingontherighttechnologyrequiresthatseveral questionsbeaskedandanswered,asfollows:
Willitsavetimeand/ormoney? DoIneedit?
Canitbereasonablyimplemented? Whatarethe financingoptions?
Thetime/moneysavingsisthe firstquestiontoanswer.Ifthesoftwarewon ’tsaveeither,itisn’tagoodpurchase.Theanalysisto determinesavingsinvolvescalculatingthehourlyrateand comparingthetimesavingsthetechnologycanachieve.Ifthe dentistcanseemorepatientsorspendmoretimewithpatients, it’sprobablyagoodchoice.Ifitpaysforitselfinreducedlaboratoryfeesorincreasedcaseacceptancerates,it’salsolikely worthwhile,aslongasthetimetorecoupcostsisreasonable.
Thepractice’sneedsshoulddictatewhetherthetechnologyisa goodpurchase.Determiningwheremostofthetimeandmoney arespentwillallowthedentisttoplanhowtooptimizethepracticewithtechnology.
Ifthetechnologyistoocomplicated,thedentalteammay fi ndit hardtoimplementit.Apurchaseshouldn’tremaininthebox. Thedentalteamshouldbepartofthediscussionaboutwhat technologytoimplement,withthegoaltohavebuy-infrom everyonewhowillusethetechnology.
Financingoptionsshouldconsidertheannualpercentagerate (APR)andthemonthlypayments.Purchasingneartheendof theyearmayallowfortaxwrite-offs.A financialexpertcanguide thedentistindeterminingthewisdomoflargepurchases.It’ s alwayswisetoalsodoresearchsuchaslisteningtopodcasts, readingjournals,orspeakingwithtrustedfellowdentists.
Technologycanrevolutionizethepracticeofdentistry, butitmustbeneeded,used,andpurchasedwisely. Dentistsshouldenlisttheirdentalteamandevena financialexperttoensurethatthesequalificationsfor agoodpurchasearepresent.Maintaininganopen mindtowardtechnologywillbeakeycomponentin creatingadentalpracticethatwillbeseenastechnologicallysophisticatedandsmart.
BahI,MathewsL:Dentaltechnologypurchases:Strategiesand considerations. DentEcon 114:41-43,2024
Reprintsnotavailable
Theframeworkforhiringandstaffingfordentalofficesrequires anapproachthatisintentionaltoensurethatthebestcandidates areinterestedandcanbereached.TheAmericanDentalAssociation(ADA)HealthPolicyInstitutereportsthatdentalpractice capacityhasfallenby10%asaresultofopenassistantandhygiene positions,and9ourof10dentistsfeelit’sextremelyorverychallengingtosuccessfullyrecruitforthesepositions.Inaddition,a thirdoftheindividualsintheserolesplantoretireinthenext 5years.Fillingthesevoidswithtoptalentrequirescraftingan appropriateofferandchoosingchannels,screeningcandidates, andprovidingrecruitingpacketsandexperiences.Thelevelof recruitmentdependsonthesizeofthedentalpractice.
FeaturesoftheOffer
Theofferofemploymentshouldbeclearlyconveyedthroughthe messagebeingsentout,notingtheclinicalsituation,whatis offeredrelationally,andwhatthe financialaspectsare.Because thesecomponentsde finetheoffer,theremustbeclearanswers providedintherecruitmentad.Languageshouldbesimpleand direct,focusingontheelementsthatthepracticemostvalues andwhatcanserveassellingpointstothemarket.
Ifthegoalistohiresomeonewhowillfollowthepractice ’ sprocessandsystemwhentheyjointheorganization,thecorevalues ofthepracticeshouldbeemphasizedasthe firstthingpotential candidateswillsee.Thenatureoftheorganization,suchasdynamic,generous,orhumble,shouldalsobeinaprominentplace. Theimportanceofthe fitinthedentalorganizationshouldbe clearlyconveyed,sothatpotentialcandidatescanseethe first year ’spathintheposition.
Eachdentalpracticehasastoryandtellingthestoryofthedental teamcanalsobeadrawtocandidates.Thedentalpracticeshould trytomakethemselvesrelevanttothetopcandidates,withanavatar ofwhatisdesiredinanassistantorhygienistonthatdentalteam.
Variouschannelsandmediumsareavailable,andthechoice shouldbefocusedonwherethequalitycandidatesaremostlikely tobelookingforaposition.Digitalchannelsincludewebsites, paidads,landingpages,andsocialmediagroups,butalsojob boardssuchasIndeed,Monster,LinkedIn, DentalPost.net,IHire Dental.com,DentalJobs,net, DentalWorkers.com, DentReps.com,Hireclick,com,andDirect Dental.com.TheHandshake
appallowsanadtobedistributedtoallthedentalschoolswith whichitisaf filiated.
On-siteengagementscanbeheldatdentalschools,hygiene schools,andcontinuingeducation(CE)events.Referralscan comefromthedentalteamorpatients.Recruiterscanalsobe hiredtoseekoutprimecandidates.
Themedium’sefficacyshouldbetrackedthroughcandidateand leadtrackingsystemsandmeetingcadence.Responsestoads shouldbemeasured,withtheinitialresultsassessedandadjusted asneeded.
Adsshouldcarrynodatesifthepracticeiscontinuallyrecruiting candidates.Theyshouldberefreshedasneededandextraeffort madeifaspeci fictimetargetdevelops.Boththeadandtheavatar canbealteredtotargetspeci ficgroups.
Personsgraduatinginthenext6monthsmaybecontactedwhile theyareinschool,askingintheadiftheyaretryingtodetermine whattheirfuturewillbe.Communicatingwiththemaheadof timecanidentifydesiressuchason-sitetraining,whichmaybe accommodatedbyhiringthemasanassistantiftheareaallows fornoncertifiedindividualsinthisrole.
Incentivizingpatients,teammembers,theirfamilies,theirfriends, andpeersmayalsoleadtocontactswithgoodcandidates.It
s importanttoconnect,buildrelationships,andprovidevalue whenusingthesechannels.
Candidatescanbescreenedbythepractice ’shumanresources(HR)andoperationste am.Thisincludesareviewof theirapplicationsandpossiblyinitialZoomorphoneinterviews.Thedoctor,owner,orhiringleadershouldparticipate intheseinterviews.Inadditi on,topcandidatescanbeprovidedwithagift.
Therecruitingpacketcanbedigitalorphysical.Thegoalisto packagetheareawherethedentalpracticeislocatedinaway thathighlightstheof ficeandtheopportunitiesthatareinthatsituation.Consideringtheprocessasarealestatetaskwillhelpto identifyconveniencesforthecandidatesandtheirfamiliesand notegoodschoolsinthearea.Somepracticeswagorpamphlets onthepracticemayalsobeincluded.Adigitalpacketcaninclude allthepracticeinformation.
Thehiringmanagershouldmeetweeklywiththedentisttoreviewprogress.Itmaybepossibletoidentifytrendswhereleads comefrom,reviewfeedbackfromthemarketingtools,andidentifychangestothemessagingormediumneededtoimprove responses.
Withtheseelementsallinmind,thedentalpracticeshouldscale theirrecruitingeffortstothesizeofthedentalpractice,as follows:
Abaselinelevelissufficientforasingle-facilitypractice.Itincludesateammemberavatar,practicewebsite,jobdescription,offer,andGooglereviews.
Thebeginnerlevelisappropriatewhenthereare2to3practicefacilitiesandconsistsofaclearhiringprocess,proactive recruitingefforts,referralgathering,useofapracticerecruitingpacket,andanequityshare.
Attheintermediatelevel,whichwouldworkfor4to10 practices,acareerspageshouldbeincludedonthepractice website,andthereshouldbeanarearecruitingpacket,a long-termrecruitingstrategy,andbrandexperience considered.
Whenmorethan10practicesareinvolved,theadvancedlevelapproachisdesirable.Thisincludesadedicatedrecruitingwebsiteandrecruitingteam,on-siteengagement,and applicanttrackingsoftware(ATS)andcustomerrelationship management(CRM)softwarethatcanmeasurethereturn oninvestment(ROI)forallrecruitingefforts.
Leadershipskillsaredevelopedthroughprogressivestages,but becomingaworld-classleadercanbeinthecardsformany dentists.Dentistsarewell-trainedindentistrybutdental schooldoesn’tteachthemaboutleadingandtheyhaveno practicalrealityinwhichtoapplyleadershipskills.Leadership trainingrequiresleadingotherpeople,whetheritisthedental teamorpatients.Inbothofthesegroups,thepeoplehave theirowndesiresandbehaviorsandtheleadermustlearn toworkwithinthestylethat fi tseachsituation.Adaptation totheneedsofeachsituationisconstant.Mostrecently,dentistsaredealingwithstaffingshortagesandthedesiresof dentalteammemberstobebettercompensated.Meeting thesechallengesrequiresalevelofmanagementthathasn’t beenrequiredpreviously.The4levelsofleadershipmostdentistsgothroughandtheircharacteristicswereexplained,with afocusonLevelIVleadership.
Ifarecruiterishired,thedentist/hiringmanagershouldclosely monitorthesituation.Outsourcingcanbeagreathelp,butthe messagebeingdeliveredshouldbethepractice’ smessage.
Whenit’stimetomakeanoffer,thedentistshouldtakethe candidatetothebestplacesinthearea,sothatheorshecan seeallthethingstheareaoffers.Theteammembersshouldbe includedsotheycaninteractwiththecandidateandsothatthe candidatecanclearlyseethecultureoftheof fice.Beforethey aretakenouttodinner,thedentistshould findoutwhattheirfavoritedrinkandfoodaresothattheirexperienceispersonalized. Thebestcandidateshouldbegivenmanygoodreasonstojointhe dentalpractice.
ClinicalSignificance
Alloftheseeffortshopefullywillleadtotheopportunity tomakeanoffertoatleastonehighlyqualifiedand appropriatecandidate.Theformaloffershouldbe clear,open,andhonest.Anyquestionsthatarise shouldbeansweredsothecandidatecanhavetheinformationtomakeaninformeddecision.
Theultimatehiringandstaffingframeworkforassociatesandhygienists. DEOMagazine, Nov-Dec2024,pp24-26.
Reprintsnotavailable
The first3levelsofleadershiparecommonexperiencesamong dentists,butfewreachLevelIVcompetency.
Newleadersmayhavestrongclinicalskillsbuttheylackexperienceinmanagingadentalpracticeorleadingadentalteam.Often thestyleofrunningthepracticecouldbetermed “winging” it, whichrequiresthatthedentistrisetoeachchallengeandwork to figureoutwhatmustbedone.Typicallydentistsremainat thislevelfor1to3years.
Competentleadershipisdevelopedafterworkingandlearning throughexperienceforseveralyears.Thedentistisbuilding thepracticeandestablishingafoundationforsuccess.The
practicegraduallyneedsmorestaffforspeci ficpositions.The dentistspendsmostofthetimecaringforpatients.Thelevelof stress,chaos,andfatiguerisesasthedentisttriestojuggleimmediatedemands,catchup,adaptproceduresandsystems,andcorrectmistakessothatthepracticefunctionsmoreeffectively. DentistsusuallystayatLevelIIforjustafewyears.
Leadersbecomeoverwhelmedafterabout4or5yearsofpracticeandmaycontinueinthisstageuntilretirement.Thisisn’ta goodplace,andthedentistexperiencessignificantstressand frustrationwiththebusinesssideofpractice.Notonlydoes thedentistworktoohard,butheorshetendstoearnsignificantlylessthanhisorheractualpotential.LevelIIIleadersare responsibleforchairsideworkbutalsospendconsiderable timeoutsideofpatientscheduledhourshandlingadministrative andmanagementissuesforthepractice.Growthhasresulted inadegreeofbusyness,chaos,stress,andfatiguethatcanbedifficulttomanageeveryday.Burnoutcanoccuratthisstage.
LevelIViswheredentistshopetobeandinvolvesmuchless stress.Inaddition,thedentistislessinvolvedinadministrative areasandfocusesmoreonproductiveclinicalcareandreferral management.Typicallythedentistattendsthemorningmeeting thatisshortandrunbystaffmembers,thenfollowsupwitha schedulerunbythedentalassistants.Everyoneissowelltrained andhighlyskilledthatthedentist findsworkmorerelaxingand comfortable,withdelegationandtrainingservingasthekeysto attainingLevelIVleadership.
TheLevelIVleaderdoesn’tneedtospendtimesettinguptheday, managingtheteam,orhelpingotherpeopledotheirjobs.Heor shedoesn’tspendthetimeansweringquestions.Instead,team membersknowwhattodo,whentodoit,howtodoit,and whattheresultsshouldbe.Thisknowledgeresultsfromthe training,time,andeffortthedentistputinduringearlierstages. Alloftheteammembersnowthinklikeownersandaretrusted toperformtheirtaskswell.
Thefrontdeskpersonnelmayseetheirtasksaslimitedto handlinginsurance,collectingpayments,managingpatientrecords,greetingpatients,orderingsupplies,andhandlingthe schedule,butsalesisanothertasktheycanexcelat.Salesshould
Trustingdentalassistantstobeinchargeofschedulingresultsin thedentist’sgreaterrelaxationandcomfortinlettingthemanticipatewhatcomesnextandinguidingthedentisttotheproper roomandpatient.Dentistscanfocusondoingwhattheydo anddelegateothertaskstothedentalteam.Oftentheteam hasanopeningandclosingchecklistforeachdayandtheycompletetheirresponsibilitieswithoutsupervision.
TheLevelIVleaderhasbecomeanexpertatdelegation,andthe teamhastheskillsettoacceptthedelegation.Aslongastheteam memberislegallyallowedtodoatask,heorsheistrainedinit. Havinganownershipmindsetleadsteammemberstoquickly mastertheirtasksandfreethedentisttofocusondoingdentistry andhelpingpatients.
Dentistsatthislevelroutinelyreliedonthehelpofexpertadvisorsinpreviouslevelstoimplementupdatedsystemsandtrain theteamtobeabletousethosesystems.Theseadvisorsmay alsohelpthedentistwith financialplansandpreparationfor retirement.
LevelIVleaderstendtoexperienceexcitingandfulfillingdentalcareers.Theyhaveeliminatedthechaos, stress,fatigue,andburnoutfromtheirlivesbytraining andthentrustingtheirdentalteamtodotheirjobswell. Theirleadershipskillsareaccompaniedbyprofessionalandpersonalsatisfaction,andtheyattribute theirsuccesstoawell-trainedandhighlymotivated professionalteam.
LevinRP:Thedentistasaworld-classleader. DentEcon 115:8-10, 2025
Reprintsnotavailable
beviewedashelpingsomeonewhohasaproblemmakean informeddecisionabouthowtosolveit.Goodsalespersons listentotheproblemandidentifywhethertheyaretherightpersontohelp.Dentalofficesonlyconvertabout35%oftheirnewpatientopportunitieswhocontacttheof fice,whichmeansthat mostofthetime,salesaren’tbeingmade.Thereasonsforfailing
toconvertcallerstonewpatientswereexplained,andsomesales skillsthatwillhelpthedentalpracticegrowwereprovided.
Generally2keyreasonsexplainwhycallerstothedentalof fice don’tchoosetobecomenewpatients.The firstishavingcalls gounanswered.Peoplewhocalltheof ficehaveaproblemand arelookingforananswer.Ifthefrontdeskpersonistoobusy toanswerorhasgonetolunch,thecallerwillmoveontothe nextpossiblesolutiontotheproblem.Itisn’tnecessarytohire morepeople.Answersinsteadcanbeassimpleashavingthepersonnearesttothephonegrabitandtakedowntheinformation sothefrontdeskpersoncancontactthepersonlater.Inaddition, anarti ficialintelligence(AI)chatbotcananswerquestionsonthe practicewebsiteorGoogleadlandingpage.Onlinescheduling canbeencouragedbybeginningthepracticevoicemailwitha statementthatthenewpatientcangotothewebsitetoschedule avisit.Thegoalistopickupthemarketingleadswheretheyare andbeforetheyturnsomewhereelse.
Thesecondreasoninvolvestheassumptionsthatcanbemade whenpeoplecallin.Ifthecallerbeginsaskingaboutwhetherthe officeacceptshisorherinsurance,thefrontdeskperson shouldn’tjumptotheconclusionthatallthecallercaresabout isinsurance.Thecallerlikelyisconcernedaboutwhetherheor shecanaffordcare,whichisareasonableconcern.Frontdesk personnelcanalsoassumethatthecallerisjustpriceshopping whenheorsheasksaboutaprocedure.Patientswanttounderstandwhythepracticeisworthmoreandcanbeledtobecome apatientifthefrontdeskpersonexplainstheexperienceofthe dentistandwhyheorshecandotheproceduremorequickly orbetterthansomeonewhoischeapandmaytakelonger.
Learningtochangeacallerintoanewpatientdoesn’thappen overnightbutrequirespractice,role-playing,self-evaluation, andhelp.Severalskillscanbedevelopedthatwillhelpthefront deskpersonneltoimprovetheirabilitytosellthepractice.
Perhapsthemostimportantskillistoactivelylistenandunderstandpatients’ needsandconcerns.Whenthestaffmember reallylistens,heorshecanaskclarifyingquestionsandbeempatheticwiththecaller,whothenfeelsvaluedandunderstood.This beginstheprocessofbuildingtrust,whichcanleadtoaprogressionfrominquiryintoappointments.
Dentalvisitsarestressfulformanypersons,sothefront deskpersonnelshouldbesensitivetotheanxietyand
concernsofcallers.Empathywillacknowledgethecaller ’ s feelingsandcanleadtothecompassionofofferingreassurance.Thisapproachcansigni fi cantlyimprovethecaller ’ s senseofcomfortandbuildtrustthattheclinicalstaffwill beequallycaring.
Thefrontdeskpersonnelmustunderstandthedentalservices thattheofficeprovides.Theymustbeabletoanswerthecallers’ questionsaboutproceduresandproductsandwhattheadvantagesareforeach,andtheyneedtoprovideneededreassurance. Theanswersofferedshouldbeclearanddeliveredcon fidently. Bene fits,costs,andthevalueofthepracticeovercompetitors shouldalsobepartoftheconversation.
Callersoftenvoiceobjectionsorconcernsaboutcosts,time,or treatments,amongotherworries.Thefrontofficestaffmustbe abletoexplaintheadvantagestheof ficeprovideswithconfidence andmaintainempathyforthecaller.
Thecallershavelegitimateproblemsandtheydeservesolutions. Thefrontdeskpersonnelmustbeabletoarticulatehowtheofficecansolvetheproblembetterthananyotheroptionsandgive thecallerasolutionthatwillcalmanyfears.
Inclosingacall,thefrontdeskpersonnelshouldtakecharge andtellthecallerwhatthebestcourseofactionis.This canbestated,as “Let’sdothis...” andwilloftenhelpcallers infollowingthroughwiththesuggestion.Decisionfatiguecan bepresent,soit’sbesttonotaskbuttellthecallerabouthow theof ficecanprovideasolutiontotheproblem.Sometimes otherscenarioswilloccur,sothefrontofficepersonnel shouldsearchtheliteratureontypesofsalesclosesto fit varioussituations.
Thedentalpracticeshouldcounselfrontdeskpersonneltobepatientinlearningthesesalesskills.Itcanbehelpfultoengagein role-playingscenarios,hireacallconversionspecialist,oreven usecall-recordingtechnologysoactualcallscanbereviewed andevaluated.
Salescanbeconsideredanawfulthingbysomepeople.Inthe dentalsituation,thecallersarelookingforasolutiontotheir problem,andtheyareseekingitfromthedentaloffice.Those callsshouldbemanagedwithapositiveandcaringexperience thatcanleadtothecallerbecominganewpatient.
ClinicalSignificance
Salesarerequiredtogrowadentalpractice.Theycan beobtainedethicallywhencallerscontacttheoffice withquestionsorwithproblemsthatneedresolution. Ifthesecallsarehandledwell,thereputationofthe dentalofficewillbethatthisisaplacewherecaring peoplecan findanswersandhelp.Learningskillsto ensurethatencountersbyphonearemanagedwell shouldbeavaluedexerciseincaringaboutpeople whomayneeddentaltreatment.
WinansX:Thefrontdeskadvantage:Salesskillseverydentalofficeneeds. DentEcon 114:29-30,2024
Reprintsnotavailable
Referralsfromexistingpatientscanbetheultimatecompliment tothepractice.Havingsatis fiedpatientstellothersabouttheir greatdentistisfreeadvertising.However,manypatientsdon’t understandthevaluethesereferralshaveforadentalpractice, ortheymaybeafraidiftheytellothers,theschedulewill fillup andmakeithardtogetanappointment.Toensurethatpatients knowtheycanhelptomakethedentalofficemoreprosperous bytellingothers,somesimpleremindersandincentivescanbe offered.
Thedentistcan,atthecorrecttime,simplyaskapatienttoprovideareferral.Whenthepatientcomplimentsthedentistonthe careheorshereceived,it’seasytoexpressgratitudeforthekind words,thensuggestthatthepracticewouldbehonoredifthepatientcouldpassthosewordstohisorherfriendsandfamily members.Thestaffcanalsoengagepatientsdirectly.Thepractice canincludeincentivestostaffmemberstoaskforthesereferrals, includingabonusorotherperkswhenthereferralleadstoanew patient.
Patientswhocomplimentthedentistorstaffcouldbegivengift certi fi catesasathankyou.Certi fi catescancarrythe existingpatient ’ snameandbedesignedtobegiventothe prospectivepatient.Customizablegiftcerti fi catetemplates areavailableonlineforMicrosoftWordandotherprograms. Theoffercouldbeafreetoothbrush,adiscountforcare, orafreeexaminationand/orcleaning,allofwhichcanbe enoughtoinducethepatient ’ sfriendsorfamilytocometo thedentist.
Theof fi cecanalsopostsignsthatletpatientsknowhowmuch referralsareappreciated.Businesscardholderscanhave “ Thankyouforreferringothers ” inscribedonthemand beplacedinaconspicuousplacetosubtlysuggestreferring others.Check-inandcheck-outdesksareperfectforthese reminders.
Bulkmailore-mailcampaignstargetedtocurrentpatientscan includereferraloffersorgiftcertificates.Themailmergefeature ofMicrosoftPublishercanbeusedtocustomizethegiftcertificatesforeachpatient.Theycanbeincludedwithaletterright beforetheholidayseasonandthelettercanmentionwhata wonderfulgiftthecerti ficatescanbe.
Thenamesofeveryonewhoprovidesareferralcanbeaddedtoa basketanddrawnforaprize.Personalizedgiftcertificatesthat wereprovidedtothepatientsandreturnedbytheirfriendsor familycanbeputintothedrawing.Thenicertheprizeis,the morelikelypatientswillbeincentivizedtoprovidereferrals. Amongthepossibilitiesfortheprizearea flat-screentelevision, whichcostsmuchlessthanthereturnfromthenewpatients. Otherincentivesincluderestaurantgiftcards,donationstopatients’ favoritecharitiesintheirname,credittowarddentaltreatments,orfreebleaching.Thesemaybegivenoutthroughthe drawingorsimplytoeveryonewhoprovidesareferral.The dentalpracticeshouldcheckwithstateandlocallawstosee whatispermittedlegally.
Whenapatientrefersanewpatient,thepracticecansendagiftof thanksthatcanspurfuturereferrals.Inaddition,thegiftshould havethepractice ’snameonitsootherpeoplecanbecomefuture
referrals.Thegiftshouldbeofsufficientqualitythatthecurrent patientwilluseit.Forexample,coolersorfoldablechairsare goodforparentswhosechildrenplaysports.Whenotherparentsseethename,theymayaskwhatthepatientthinksofthe dentist.Womenwithprofessionalcareerscouldbesent flowers totheoffice,sothatcoworkerscanseethevaseandbecome futuredentalpatients.
Gettingpatientstoreferothersisanexcellentwayto growapracticewithminimalinvestment.Thosewho cometothepracticeonthewordofafriendorrelative aremorelikelytoaccepttreatment,moreeasilyretained,andmoreapttoprovidefurtherreferrals.
GangwischRP:Askandyeshallreceive. InsideDent 20:8,10,2024
Reprintsnotavailable
Toolsarewidelyavailablethathelpfutureemployersandstudentslearnmoreaboutthemselvesandthepeoplearound them.TheMyers-BriggsTypeIndicator(MBTI)providesan outcomeof4lettersthatindicateone’spersonalitytraits,speci fi callywhetherapersonisintrovertedorextroverted,if theyvaluedstructure,andwhethertheymakedecisionsbased onintuitionandfeelingsorfactsandlogic.Generationsofdental studentshavetakenthetestsot heybetterunderstandtheir personalitytraitsandcandevelopamindsetonwhichtobuild asuccessfulteamintheirpractice,academicsettings,business dealings,andpersonallifeaftergraduation.Thetrendsinpersonalitytraitsanddecision-makingbehaviorsamongdentists werestudiedatvariouspointsintimesince1964,noting possibleexternalfactorsthatin fl uencedchangesinthese trends.
A20-yearstudy(1964-1984)doneatCreightonUniversity SchoolofDentistryfoundthatmostdentistswereintroverted, valuedstructure,andbasedtheirdecisionsonfactsratherthan intuitionandfeelings.Babyboomerssharedthesepersonality traits,whichin fl uencedtheirpracticemanagement,practice culture,andpersonnelstructurewithmultigenerational employees.
Afollow-upin2018foundthatthemostcommonpersonality traitshiftedtoextrovertandfa ct-baseddecision-makingwas valued.Newtraitswerenotedinintroverteddentistswho
beganintegratingdecision-makingprocessesbasedonthepatient’spointofviewcoupledwithexternalfactors,facts,and logic.Otherfactorssuchassocialdeterminantsofhealth weregivenvalue,causingdentiststobecomemoreempathetic andunderstandingofthepatient’ sneeds.Thesechangeswere likelyin fl uencedbythetrendamongpatientstochooseactive lifestylesandprioritizetheirhealth.Thisledtosearchingforreviewsofdentistsandtheirpractices,whichincreasedthevalue ofpatients ’ comfortsothattheypreferredadentalhome focusedonoverallwellnessandoutcomesratherthanprice. Value-basedoralhealthcarewaschosenasawaytoimprove dentalpatientoutcomes.
In2024,thedentalpersonalitytypeschangedagain,withdentistsrevertingtotheintrovertedpersonalityandbasingdecisionsonfactsandlogic.Techn ologyhasmadeinformation readilyavailableandmayhavecontributedtothefocuson data-drivendecisionmaking.Inaddition,thepandemiccaused ashiftineducationfromin-persontoonlineplatforms,with somehybridcoursescontinuingtobeavailable,whichsupports introversion.
Whentheyareconcernedaboutothers,dentalstudentstryto considereveryone’sopinionsandensureeveryonehasavoice.In contrast,dentalstudentswhobasetheirdecisionsonfactsandlogic don’tusuallyconsiderothersintheirchoices.Theextrovertstudents thriveinlargegroups,buttheintrovertstendtobreakdownlarge groupsintomoremanageableone-on-oneconversations.
TheAmericanDentalEducationAssociationfoundthatthemost commontraitsofdentistswereasfollows(althoughtheseweren’t allthetraits):
Comfortablewithclosepersonalinteractions
Easytotalkto
Trustworthy
Goodcommunicator
Leader
Caringandconcerned
Passionateaboutprovidingcaretothoseinneed
ClinicalSignificance
Researchhasshownthatdentistsarebecomingmore fact-andlogic-basedintrovertsratherthanpersonandpatient-centeredextroverts.Patientswantto havedentistsremaincenteredontheirneedsanddesires,abletolistentotheirconcerns,andacting accordingly.Overall,itwouldbebestiftherecould beabalancebetweenthe2extremes.Dentistsneed tovaluethedifferencesofothersandestablishapracticepersonawithpatientsinwhichtheyandtheirpatientscanlearnfromoneanother.
WatanabeMK:Unboxingpersonalitytypologyindentistry. JCalif DentAssoc 52:2406979,2024
Reprintsnotavailable
Knowingaboutlocalsearchengineoptimization(SEO)isvitalfor maximizingyourdentalpractice’svisibilityinlocalonline searches.LocalSEOissimilartotraditionalSEO,withthesame goalofgivingthepracticegreatervisibilityinGooglesearches. However,theydifferinwhereusersseethepractice,howresults aremeasured,andhowthoseresultsareachieved.Adviceto guideyouinachievingthebestlocalSEOpossibleisoffered, withrecommendationsforactionsthatwillyieldthebestresults.
PlacementandMeasurements
LocalSEOcampaignsfocusonyourGoogleBusinessProfile (GBP)andGoogleMapsPack.TheresultthroughalocalSEO istheplacementofthepracticeintheGoogleMapsPackas wellasphonecallsandwebsitevisitsfromtheGBP.Tracking shouldfocusonthenumberofnewpatientsyousee,butpreviousmetricscanhelpinevaluatingtrends.
TraditionalSEOcampaignsfocusonrankingsforspeci fickey wordsandorganicvisitstothepracticewebsite.Theonlyways visitorscangettothewebsitearedirectthroughtheaddress, referredthroughalinkonanotherwebsite,paidthroughapaid adcampaign,andorganic,whichisfromaGooglesearchincluding theGBP.
TraditionalSEOonlyfocusesonorganictraf fic.Numberofnew patientsremainsthemostimportantinformation.Atraditional SEOsearchrelatedtolocalbusinessesislimitedtopaidGoogle ads,GoogleMapsPack,andtraditionalorganicsearches.
AnoptimizedlocalSEOapproachmightyieldbettertraditional SEOresults.Localcampaignsusuallyhave2parts:aGoogleMy BusinessOptimizationCampaignandaCitationCampaign. YourGBPisthefoundationofalocalSEOcampaignandisthe cruxofyourlocalpresence.TheGBPisfreeandcanbeobtained byvisiting business.google.com toclaimyourprofileandverify yourpractice.Fillingitoutcompletelyisessentialbecauseit’ sunknownwhatGBPfactorswilldrawinclicksfromsearchers. BecauseGoogleoftenupdatesthedatayoucanaddtothe GBP,it’simportanttomonitoringyourprofile.Tocheckthe strengthofyourprofile,youcanlogintotheGoogleaccount andGoogleyourbusiness’ name.TheProfileStrengthindicator shouldbegreenandsay “Looksgood.”
Googlerandomlyshiftsthemapspackpositionaroundaspartof theiralgorithm.It’sbesttofollowGoogle’srecommendations andoptimizeyourprofiletothebestofyourability,generatereviews,andrunacitationcampaign.
ThemostimportantrankingfactorforlocalSEOsearchesis proximity.Becausedentiststreatpatientsfrommultiplelocal areas,thiscanbefrustratingbecauseGooglelimitswhatiscalled local.Apracticecanberankedinmultiplelocalities,butit’ sunlikelythatyouwillrankinasecondareawherecompetitionof anysortispresent.
WhenoptimizingyourGBP,thenumber1rankingfactorisPrimaryCategory,followedbyon-pagesignals,whichincludeshavingyourname,address,phonenumber,andhoursonyour website.Reviewsarenextandshouldbe filledwithcurrent,positiveselections.
Theterm link isusedtodescribeonewebsiteconnectingto another,andhigh-authoritysitescansharetheirauthority.In localSEOcampaigns,linksusuallymeancitations,whichisalisting foryourbusinessonanaggregatorordirectory-typewebsite. Googlewantslocalbusinessestohavecitationsbecausethey believethemoreaccurateandconsistentcitationsabusiness has,thebettertheproofthatthebusinessislocal.Inacitation campaign,yousubmityourpractice’sinformationtomultiple listingsitessoyouwillhaveapresenceonthosesites.Some havemoreauthoritythanothers,sothegoalistolistyourpracticeonthetopsites.Aggregatorsareservicesthatsubmityour informationtoagroupofcitationproviders,suchastheYellow PagesandtheGPSlisting.Inthiscampaign,it’simportanttocorrectoldorincorrectlistingssotheinformationisasconsistentas possibleforGoogle.
Youshouldknowthatthereisnowaytoquantitativelystatethat your20citationswillplaceyouinabetterpositionthansomeone else’s19orthatyourtop10authoritycitationswillorwillnot placeyouaboveacompetitor’s100low-authoritycitations.No standardhasbeensetregardingthecorrectnumberofcitations tohaveorhowhavingmoreorfewercitationswillaffectlocal listings.
Althoughacitationcampaigncanberunmanually,withsubmissionsofinformationto50ormorewebsites,manycompanies providecitationsubmissionservices.Althoughtheycostmoney tomakethesubmissions,itmaybeworthwhiletohavethemtake onthistask.
Citationsshouldbeconsistentacrossthewebbutthisisn’t somethingtostressover.Ifmostareconsistent,afewerrantlistings
won ’tbeadealbreaker.It’simportanttoensuretheaccuracyofthe topsites,suchasGBP,Facebook,andAppleBusinessConnect.
Oncecitationshavebeensubmitted,theyusuallycan’tbe removedbutonlyupdatedunlessthebusinesscloses.Thismeans youdon’thavetokeeppayingforaservicetokeepthatcitation open,althoughyoumightwanttosoyoucankeepitcurrent.If youworkwithacompanyforcitationsubmissions,don’tbe trickedintopayingiftheythreatentoundothecitationworkif youleaveorstoppaying.
Thefollowingareimportanttorememberasyoudealwithlocal SEO:
YoumustowntheGBP,evenifagenciesmanageitfor you.
Onyourcontactpage,providewrittendirectionsusinglocal landmarkstoreinforcethefactthatyouarelocal. RegisteryourpracticewithAppleBusinessConnectbecause AppleMapsmaybeusedinsteadofGoogleMaps. Formetrics,focusonreportsofthenumberofcallsfrom yourGBPandhowmanyvisitorscometothewebsite fromGBP.
It’sOKtomanageyourGBPandcitationspersonallyorto handthetasktoanagencyforhelp.
LocalSEOwillhelpyourdentalpracticeappearinlocal searchresults.AnoptimizedGBPisbest,andthecitationcampaignwillhelptoensureyourpractice’s name,address,andphonenumberareconsistent acrosstheweb.
WankDA:Highvisibility. Dentaltown 26:44-48,2025
Reprintsnotavailable
Eachyear InsideDentistry surveysreaderstoidentifythetrends thataretakingplaceindentistry.In2024,theareasofmostinterestwerepracticemanagement,clinicalcare,andpurchasingand adoptingtechnology.Manypracticesadoptednewapproachesto managetherisingoverheadcosts,economicpressures,andshiftingpatientexpectations.Thecurrentstateoftheprofessionand howcliniciansarehandlingthechallengesinthese3areaswhile prioritizingexcellentpatientcareweredetailed.
Thenumberofrespondentswhosepracticeswereinthetop3 incomebracketsdeclined,butthepercentagewhousedpractice managementconsultantsremainedunchanged.Reimbursements aren ’tincreasing,soevenwithincreasedproduction,profitsare lower.Practicesthatworkwithmanagementconsultantstended tomaintainsteadynetincomes,showingthathavingtheright consultantcanidentifycriticalpointsandhelpcraftpersonalized approachestoshoreupincome.
Tobalanceprofitabilitywithkeepingcarecompetitivelypriced andaccessible,manypracticeshavedecidedtoincreasepatient volume.Somepracticeshavechosentodeliverhigh-quality caretopatientswhovalueit.Thesedentistshavedecidedto workatbeingabetterclinicianwhocandelivercomprehensive caretoremainprofitableratherthanseeingmorepatients. Theybelieveprovidingthislevelofcarecanbemorefulfilling thanscalingforvolume.Whilebothapproacheswork,thechoice isuptotheclinician.
Patientswantoptionsbecausetheyareoftenburdenedwithtight budgetsandlittleextramoneyforcomplexdentalcare.Asa result,making financingavailabletopatientsisanimportant component,with flexiblepaymentoptionsallowingpatientsto moveforwardwithneededtreatment.Signi ficantlymoredental officesareacceptingprivatedentalinsurance,offeroraccept alternativeplans,andconnectpatientswithhealthcare financing. Inaddition,somepracticeschangetheirwork flowstomakethe treatmentmoreaffordable.Digitaltechnology,forexample,can lowereconomicbarriers.
Establishedpatientsgivethebestnewpatientreferrals.Although dentalpracticesstillusee-mail,printads,anddirectmail,more arenowusingwebsites,socialmedia,andonlineadstoboost thenumberofnewpatients.Awebsiteisoftencheckedby referredpatients.It’simportanttotrackthereturnoninvestmentforthevariousmarketingoptionstoensureeachisworthwhile.Mostrespondentsdon’tseetheusefulnessofchatbotsin makingtheirwebsitesuccessful.
JoiningaDSOcanprovidemanybene fi tstopractitionerswho carelessaboutthebusinessaspectsofdentalcareandwho wanttofocusonpatientcare,arelookingtoselltheirpractices, wanttocollaborate,orareseekingabetterwork-lifebalance, amongotherinterests.Moredentistsareopentojoininga DSO,butthenumberofdentistswhoarenotatallopenor onlysomewhatopentothispathhasincreased.Thisindicates acoolingofinterestinDSOsandpossiblyanegativesentiment.
JoiningaDSOmaybeavoidedifthedentisthas,overtheyears, establishedthepatients,schedule,team,andprofessionalfulfillmentheorshedesires.Somedentistsrecognizethatittakes timetodeveloptheknowledge,skills,andbusinesssensetoprovideexcellentcare,createefficiencyatthechair,andmaximize profitability.Thesedentistswouldratherstayinasituationwhere allthosehavecometopassthanswitchtoaDSO.TheAmerican DentalAssociationfoundthatdentistsinDSOsaremoreoptimisticaboutcurrenteconomicconditionsthanthosenotinDSOs.
Overall,manyclinicaltrendsindentistryremainedstableor changedonlyslightly.Thisincludedthenumberofdirectrestorativeorcrownandbridgecasesdonemonthly,thenumberof endodonticproceduresdone,mostorthodontistsbelievingclear alignertherapyshouldbemanagedinperson,orcliniciansperformingsedationdentistry.Whiteningchairsideisnowbeing offeredbymorethanhalfofthesurveyrespondents,ajump fromthe8%reportedpreviously.
Withrespecttoimplant-support edrestorations,thepercentageofdentistswhoplacedscrew-retainedrestorationsjumped
by10%andthoseplacingcement-retainedrestorations decreasedby15%from2019to2022,butthesenumbers havestabilized(TypeofImplantRestorationsPerformed Figure).Sixty-ninepercentofthedentistsplacescrewretainedrestorationsand49%placecement-retainedones. Theexplanationforchoosingcementretentionwasthatscrew retentionisnotyetthestandardforeverythingandpractitionersaren ’tfamiliarwiththemoderncomponentsandscanningprotocols.Thecementretentionwasusedformany yearstoavoidmisalignedscrewchannelsandcompleximpressionprocedures.Itwilltaketimetobecomecomfortablewith advancedscanningandangledabutmentsandhexdrivers,which haveovercometheproblemswithscrewretention.
Sleepdentistryisbecomingmorespecializedbecauseofreduced reimbursements,higherlaboratorycosts,andtheincreased complexityinmedicalbillingandinsurancerequirements,allof whichmaketheprocessless financiallyviableandaccessiblefor generaldentists.Inaddition,commercialinterestshaveinserted themselvesintodentalsleepeducationandcausedconfusion overinconsistenciesbetweenprotocolsandworkflows.Even somelargedentalpracticescan’tovercomethesedrawbacks.
Overthepastyear,patientacceptanceofcomplextreatment planshasdropped,withjust54%ofthedentistssurveyedindicatingmostproposalsareaccepted.Only11%ofthedentists hadacceptanceratesexceeding80%and22%reportedacceptancerateslessthan25%.Thesetreatmentplanshavealways beenamajorcontributortothedentalpractice ’ssuccess,but arenowsufferingfrominflatedoverhead,patienthesitancy, highinterestrates,andDSOin fluences.Manycliniciansareperformingmoretransitionalbondingproceduresratherthan higher-costandmorede finitivetreatments.
Withrespecttoin-houseprocedures,aslightdecreasewasseen inmillingrestorationsandanincreasewasnotedin3Dprinting permanentrestorations.Inaddition,asmallincreasewasreportedinthepercentageofdentistswhocommunicatedinpersonorbyphonewiththelaboratoryonthemajorityoftheir complexcases.A12%increaseoccurredinthepercentageofrespondentswhopreferredtoavoidusingteledentistry.Many practicesappeartoberethinkingthevalueofremoteappointmentsnowthatthepandemicisover.
Inthepastyear,themajorityofdentistscontinuedtoworkwith 1to3distributorsordealers,withaboutafourthparticipating
ingrouppurchasingorbuyinggroups.Purchasingdecisions weremadebasedonclinicalresearchaccordingto80%ofthe respondents.Mostreliedontherecommendationsofkey opinionleadersandstudyclubresourcesratherthanother sources.Theonlineservicesmostoftenusedforpurchases werethewebsitesofmanufacturersanddealers,but5%more dentiststhaninthepasthaveturnedtoAmazon.Thissiteoffers morealternativeinstruments.Specializedimplantabutments andscrewsareusuallysourcedfromimplantcomponentwebsites.Althoughmostdentistsstillchoosetraditionaldentalsupplychannelsfortheirmaterials,themoderngrouppurchasing modelisgainingacceptance.
Surveyrespondentswhoreportedspending15%to30%of theirpracticebudgetsonnewtechnologydecreasedtheir spending.However,theprevious48%whospent10%or lessincreasedto58%.Theeconomylikelyledtothe decreasedspending,butpractitionerssaidtheystillmake well-consideredtechnologyinvestmentsbecausetheycanincreaseproductivity.Investmentsinnewtechnologyshould providea fi nancialreturn,enhanceworksatisfactionforclinicians,anddeliverbetterpatientexperiences(DentalTechnologyUsedFigure).Mostdentistscontinuedtouseair-driven handpieces,electrichandpieces,andcone-beamcomputedtomography(CBCT)machinesatthesamepercentagesasreportedinprevioussurveys.Increasedusewasnotedfor digitalradiographysensorsand3Dprinters,butadecrease wasnotedforlasers.Digitalimpressionsystemsareusedin signi fi cantlymorepractices,re fl ectingtheimprovedef fi ciency andconsistenthigh-qualityres ultsthatarenowobtained.In addition,thepricepointhascomedown,makingthisinvestmentmoreaffordable.
Althoughthe2023surveyreportedamorecriticalattitudetowardtheuseofdentaltechnologiespoweredbyAI,thepercentageofdentistswhoreportedintegratingsomeAImodulesinto theirwork fl owsdoubledin2024.Thepercentageofdentists whoindicatedtheyweremonitoringthedevelopmentsinAI andconsideringitfellfrom26%to19%,butthepercentages whoweren’ tconsideringAIproductsbutmaybeopento themandthosewhorejectedAIaltogetherremainedthe sameaspreviously.Thesetrends appeartoindicatethatthose whohadalreadymadeuptheirmindsremainedunchanged, butmanywhowereconsideringAIadoptedit.Teamsseemto stillbedecidinghowAI fi tsintheirwork fl ows(UseofArti fi cial IntelligenceFigure).Asigni fi cantamountoftrustisneeded beforeAIiswidelyaccepted.Futuredevelopmentsintechnologymaybringmorecontroltoproceduresandleadtogreater con fi denceregardingoutcomes.
ClinicalSignificance
Dentistsfacedanumberofchallengesin2024, includinghighlevelsofinflation,increasedoverhead, staffingshortages,lowinsurancerates,andincreased competitionfromDSOs.Manystillfoundwaysto remainprofitable,suchasofferingmore flexiblepaymentoptions,increasingpatientvolume,including bettermarketingonwebsitesandotherchannels,expandingtreatmentoptions,andaddingnewtechnologies.Eachpracticemustdeterminewhatisbestfor theirspecificsituation.Usingavailableresourcesto investinwell-consideredoptionsandthenworking tomaximizetheirimpactwillyieldthesuccessthe practiceseeks.
FialkoffS:Overcomingchallengestoprofi tability. InsideDent 20:16-18,20,22,24,2024
Reprintsnotavailable
Earlychildhoodcaries(ECC)manifestsas1ormoredecayed, missing,or fi lledtoothsurfacescausedbycariesintheprimarytoothofachildunderage6years.ECCispreventable, butremainsaglobalhealthproblemandcausesnegativeeffectsonthechild ’ squalityoflife,development,andgrowth patterns.ECCisfoundinasmanyashalfofthetoddlers acrosstheworld.Theprevalenceisbelievedtobesigni fi cantly in fl uencedbythefamily’ssocioeconomicstatus.Asystematic reviewandmeta-analysiswasdonetoinvestigateECCprevalenceandexperienceovera10-yearperiodandreportthe distributioninvariouscountri esandinrelationtosocioeconomicfactors.
ThedataweregatheredfromthePubMed,Embase,Scopus,and OpenGreyliteraturedatabases,alongwithahandsearchforspecificcountries.Thedatacollectedincludednumber,age,and genderofthepatients,cariesprevalenceexpressedasapercentage,andcariesexperience(decayed, filled,treated[dft]teeth). Meta-analysesweredoneforoverallECCprevalenceandexperiencebycountryofpublicationandsocioeconomicindicators,specificallygrossnationalincome(GNI)andinequalityindex(Gini index).
Onehundredpublicationswereincluded,with67reportingECC prevalence.PrevalencewashighestinthePhilippines(98.0%)and lowestinJapan(20.6%)andGreece(19.3%).InNorthAmerica, theUnitedStateshadthehighestprevalenceat53.0%;inSouth America,Argentinahadthehighestat85.8%;inEurope,thehighestprevalencewasinAlbaniaat84.1%;andinAfrica,Angolahad thehighestrateat57.9%(Figure2).
TheglobalestimatedprevalenceofECCwas49%.Thepooled cariesprevalencewas34%inCentral/SouthAmerica,36%inEurope,42%inAfrica,52%inAsia-Oceania,57%inNorthAmerica, and72%intheMiddleEast.
ThehighestdftwasfoundinthePhilippinesandthelowestwasin Japan.InNorthAmerica,thehighestdftwasnotedintheUnited States;inSouthAmerica,itwasfoundinColombia;inEurope,it wasinBosnia-Herzegovina;andinAfrica,itwasinMorocco.
AstatisticallysignificantconnectionwasnotedforECCprevalenceandgeographicalareas.ThehighestECCprevalencewas foundinAsia,whichhasalowGNIandahighunemployment rate.WhentheGiniindexwasconsidered,ECCprevalence rangedfrom39%forareaswithlowinequalityto62%forareas withnoinequality.LifeexpectancyandECCprevalenceranged
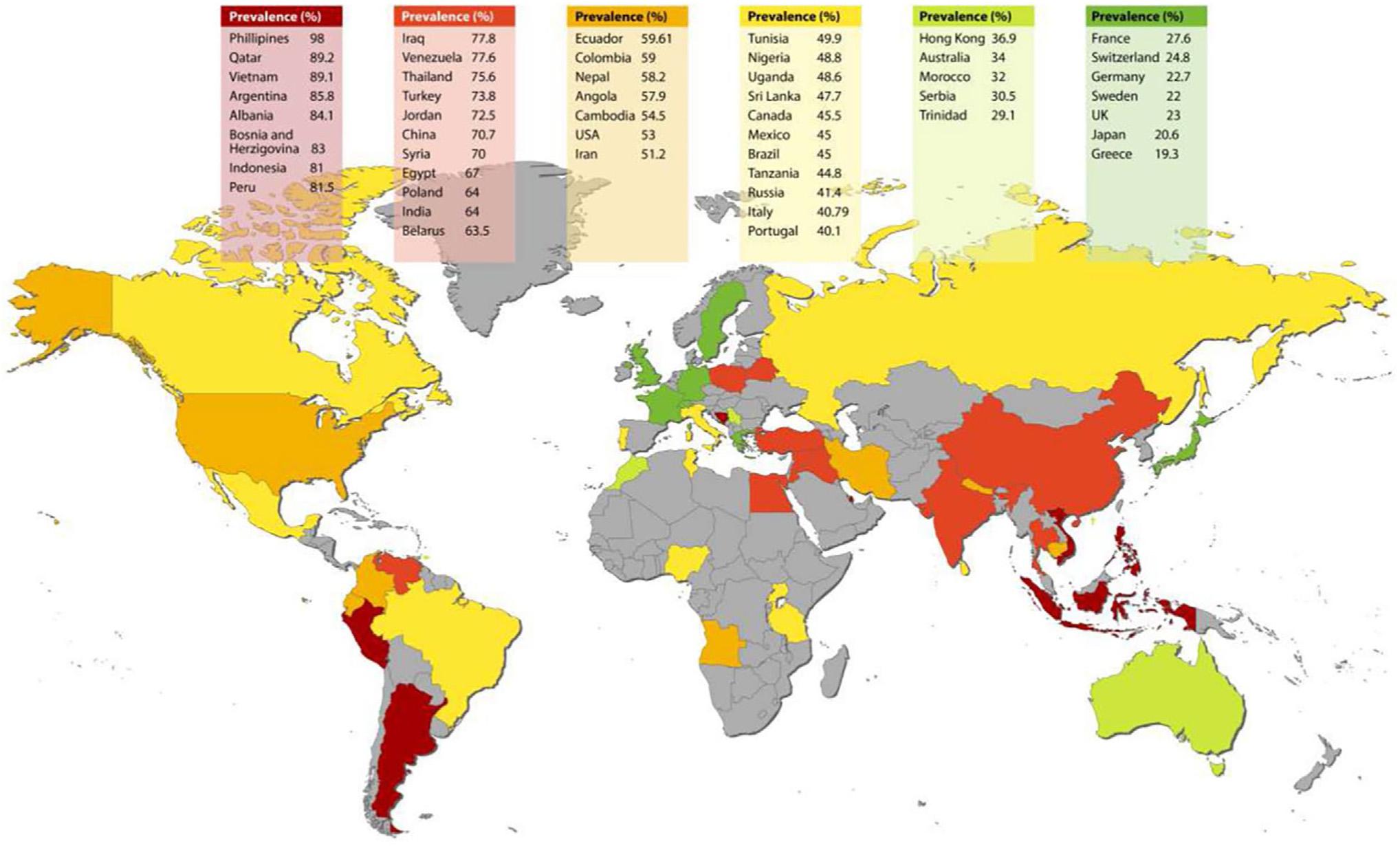
Figure2. WorldwideECCprevalencemap.Prevalencewascolorcodedasfollowing: A, <29%-lowprevalence(darkgreen); B, 29.1%-39%-mediumlow prevalence(lightgreen); C, 40%-49.9%-mediumprevalence(yellow); D, 50%-60%-mediumhighprevalence(orange);50%-80%-highprevalence (lightred); E, >80%-veryhighprevalence(darkred).(CourtesyofMaklennanA,Borg-BartoloR,WierichsRJ,etal:Asystematicreviewandmeta-analysis onearly-childhood-cariesglobaldata. BMCOralHealth 24:835,2024.)
from28%incountrieswiththehighestlifeexpectancy,whichwas morethan80years,to62%incountrieswithalifeexpectancy between71and75years.
Highmeandftwassignificantlyassociatedwithgeographical areas,withthehighestvaluesnotedinAsia.Thiswaslinkedto alowGNI,butnottounemploymentrate.
Countrieswiththehighestlifeexpectancyhadthelowestpooled meandftof1.34teeth.Thehighestdftwas5.18teethandoccurred incountrieswithalifeexpectancyof71to75years.Whenthe Giniindexwasconsidered,thelowestmeandftwas1.62teeth andoccurredincountrieswithlowinequality,withthehighest meandftof3.95teethfoundincountrieswithnoinequalities.
TheECCprevalenceratesvarywidelyacrossthegeographic areasintheworldbutremainhigh.Aclearlinkhasbeenfound betweenoralhealthhabitsandsocioeconomicdisparitiesincommunities.Amorein-depthlookintotheculturalandsocioeconomicdifferencesthatmayleadtoECCisneeded.
Thecurrentprogramsformonitoringandaddressing theissueofECCappeartobeinsufficientbecause ratesofECCremainhigh.Theindividualneedsincommunitiesandsocioeconomicrealitiestheinhabitants faceshouldbeconsideredinanyfutureprograms thataredeveloped.Researchisneededtodevelop personalizedandsociety-basedapproachesthat mayachievebetterpreventiveresultsinreducing ECCprevalenceandexperienceacrosstheworld.
MaklennanA,Borg-BartoloR,WierichsRJ,etal:Asystematicreviewandmeta-analysisonearly-childhood-cariesglobaldata. BMCOralHealth 24:835,2024
Reprintsavailablefrom AMaklennan,DeptofRestorative,PreventiveandPediatricDentistry,SchoolofDentalMedicine,Univof Bern,Freiburgstrasse7,Bern3010,Switzerland;e-mail: anastasia.maklennan@students.unibe.ch
Despiteprogramstopreventdentalcaries,theprevalenceofthis problemhascontinuedtorise,especiallyinyoungchildren.Oral diseases,includingearlychildhoodcaries(ECC),affectalmost3.5 billionpeopleworldwide,withuntreatedcariesthemostcommonhealthcondition.Newapproachesarebeingtakento addresscaries,buttheproblemofunequaldistributionofpreventivemeasuresremainstobeaddressed.Variousapproaches, includingmicrobialpathways,perinatalapproaches,genomics, socialdeterminants,teledentistry,epidemiologyandtherapeutics,andevidence-basedcare,wereexplored,notingthecurrent andpotentialstatusofeach.
Nitrogen-containingcompounds,whichwouldincludeurea,arginine,andnitrate,aremetabolizedbyoralbacteria.Asaresult,the intraoralpHrises,biofilmsarehealthier,andpathogenicbacteria andcariesareinhibited.Thereductionofnitratealsoisakey componentoftheenterosalivarypathwayfornitricoxideproduction,linkingtheoralmicrobiomewithsystemichealth.Patientscouldhaveahealthieroralenvironmentandbetter cardiometabolichealthwithhighersystemicnitricoxidelevels.
Theperinatalstage,whichincludesthepregnancyandpostpartum stages,offersanimportantopportunitytointerrupttheburdenof ECC.Mothersappeartohaveanin fluenceontheirchild’soral Candidaalbicans acquisitionintheearlyinfancyperiod.Thisincludestheinteractionsbetween Calbicans and Streptococcusmutans andtheirimpactonthechild’soralmicrobiome.Screening infantsandmothersfororalfungalcarriageandprovidingearly antifungalinterventionscanaccompanycurrentlyperformed ECCpreventionprotocols.MobileapplicationssuchastheA1 Cariesappcanpotentiallyprovidearti ficialintelligence(AI) poweredcariesdetection,aninteractivecariesriskassessment, evidence-basedcariesmanagement,andpersonalizededucation.
ToolsdevelopedbytheHumanGenomeProjecthavebeen appliedtothe firstgenome-widechildhoodcariesstudies.AsignificantassociationhasbeenshownbetweenECCandbittertastereceptorgenes.Inaddition,havingacariogenicbacterialcommunity atage2yearspredictscarieswilldevelopbyage5years.Twoyear-oldsinanoncariogenicbacterialcommunitywhohaveacariogenicgeneticbackgroundhaveariskofcariesonsetbyage5years similartothatofchildrenlivinginacariogenicbacterialcommunity.Furtherexplorationsareneededtobetterunderstandindividualandpopulation-specificriskfactorsforECC.
Cultural,economic,social,andpsychologicalfactorsin fl uence diseaseandcanhaveasigni fi cantimpactonhowweviewthe rootcausesofhealthandhealthpromotion.Socialdeterminants canexacerbatetheriskforECC,butchallengesremainin applyingthisknowledgetoassessmentandinterventiontools. Thecurrentmodelsshowthatfamily-levelpsychologicaland psychosocialfactorscanpredictECConset.Thevariablesare likelytooperatethroughbehavioralpatterns,oralhygienepathways,andhealthcareaccess.Attentionshouldbepaidtothesocialdeterminantswhencrafting preventionandintervention approaches.
Teledentistryofferstheabilitytoscreenvulnerableinfantsand toddlersandachieveone-on-oneinteractionswithyoungchildren,theirparents,andgeneraldentists,whichhasbeenespeciallyusefulfortriageandreferralstopediatricdentists.Having betteroralhealthoutcomesandestablishingadentalhome,especiallyinpoororunderservedruralorurbancommunities,are additionaladvantagesrelatedtoteledentistry.
Prospectivecohortstudiesandrandomizedcontrolledtrials (RCTs)haveprovidedclearevidenceofthecausationofcaries andtheef ficacyofinterventions.It’sbeencon firmedthat, comparedtoplacebo,38%silverdiamine fluoride(SDF)provides betterresultsinarrestingdentalcariesinUSchildrenwithsevere ECC.Theeffi cacyof10%povidoneiodineinreducingrelapsein childrenwho’vebeentreatedinthehospitalforsevereECCis underreview.Suchhigh-qualityclinicaltrialshelpinevaluating theef ficacyofinnovativetreatments.Consideringcariesa chronicdiseaseandtargetingevidence-basedstrategiestothose mostatriskmayhelptoreducedisparitiesincariestreatment.
Therearedistincttrajectorypatternsforcariesduringchildhood, sotheapproachtocariesriskandmanagementshouldconsider thelifecourseofthepatient.Thedevelopmentofrisk-based toolsformedicalsettingsandaccompanyingeconomicmodels canhelpinevaluatingthecost-effectivenessofrisk-based caries-preventiveapproachesthatbeginatage1year.
SomeprogresshasbeenmadeinreducingECCprevalencein children.Thisincludesabetterunderstandingofthemicrobial andgenomicinfluences,theroleofsocialdeterminants,and howteledentistryandinterprofessionalapproachescanimprove thereachoforalhealthcareproviders.Itremainstoaddressthe systemicinequitiesinoralhealthamongthemostvulnerable
childrenlivinginurbanandruralcommunitiesthathavelimited ornoaccesstooralhealthcare.
Multifacetedandmultimodalapproachesinperinatal andpostnatalcareaswellasadrivetoward evidence-basedcaremodelsareneededtomoveforwardwiththepreventionofECC.Theapproachesthat arealreadyunderwayholdpromise,butweneedto seethatnochildisleftbehindinthebattletoreduce earlydentalcariesworldwide.
Kopycka-KedzierawskiDT,FontanaM,MarazitaML,etal:Dental caries:Thewayforward. JDRClinTranslationalRes 10:4-6,2025
Reprintsavailablefrom DTKopycka-Kedzierawski,Deptof Dentistry,UnivofRochester,625ElmwoodAve, Rochester,NY14620,USA:e-mail: Dorota_kopyckaKedzierawski@urmc.rochester.edu
Dentistryconsistsofmanyspecialtiesthat,together,provide comprehensiveoralhealthcare.However,afterthepandemic anditseffectonaccessibility,thenumbersofpracticingdentists hasdeclined.Inaddition,socialandculturalinfluenceshave changedthedynamicsofdentalcare,patientbehaviors,andattitudestowarddentistry.Asadvanceshavebeenmadeinseveral dentalspecialties,oftendrivenbytechnologicalinnovationor research findings,newapproacheshavebeendevelopedand oralhealthcarehasshiftedtofocusmorepurposefullyonpreventionandcomprehensivepatientcare.Thetrendsbeingseen andadvancesinvariousspecialtieswerereviewed,withthe goalofpredictingwhatthefutureofdentistryintheUnited Kingdom(andelsewhere)maylooklike.
ThebudgetallocatedtoNationalHealthServices(NHS)dentistry includescutsthatmakeitunabletomeetthedemandfororal care.Ifthiscontinues,thestandardoforalhealthmaydeteriorate nationwide,leadingsomepatientstochoosetoseeprivatedental practitionersandotherstochoosenodentalcareunlessitisan emergencysituation.Oftenfamiliesareforcedtoremainonwaitinglistsforlongperiodsoftime.Ifsuchbacklogsandinsufficient resourcescontinue,dentistswilllikelychoosetoleavetheirNHS contractsandprospectivedentistswon’twanttoestablishthem.
Asurgeofdemandforpatientsmaydevelop,butthefundstopay fordentistrymaybelacking.Dentalstaffmemberswhoareoverworkedwilldevelophigherstresslevelsthatcouldaffecttheir performanceandpatientsatisfactionlevels.Eventuallypatients willstopcomingandchildhoodcarieswillbecomemore
common,allfromalackofprophylacticcare,education,and timelyinterventions(Figure1).
Privateaestheticdentaltreatmentisextremelyexpensive,makingitunattractiveformanyindividuals.Somewillseektohave theseproceduresdoneabroad,withTurkeycurrentlyseenas aprominentdestinationfordentaltourism.
Socialmediacanalsoinfluenceperceptionsaboutdentistry,oral aesthetics,andoralhealthawareness.Platformsencouragethe spreadofinformationandanecdotesaboutdentalpractices. Thishasthepotentialtoproducemisconceptions.
Withtheunavailabilityofappointments,childhoodcariesrates mayincrease,whichhasanextensiveimpactonthehealthof youngpatients.Theimpactofsocialmediainfluencersadvocating fororalhealthandaddressingtheavailabilityofdentalvisitsfor youngpatientsmaybeabletomitigatethisproblem.
Technologicaladvancesandtheintegrationofartificialintelligence (AI)arebeingviewedwithhopeconcerningtheabilitytorevolutionizeimplantdesigns,materials,andtreatmentapproaches. Dentalprostheticscouldbecomemoredurableandeffective,offeringmoresustainableandpossiblyaffordableoptions.
Researchintonew fillingmaterialsisfocusedonmaterialswhose propertiescloselymimicnaturaltoothstructures.Thiourethane-
Figure1. Impactassessment:ConsequencesofNHSdentistrybudgetcutsintheUK.(CourtesyofEshoT:Isthefutureofdentistryasbrightaswehope? Apersonalexplorationintodentistry’snationalandglobalprospects. BrDentJ 237:761-764,2024.)
based fillingmaterialsmayprovidelongevityanddurabilityfor enamelanddentinrestorations.Inaddition,bioactiveglass fillings mayincreaselongevityalongwithpreventiveef ficacy.These fillingsreleaseessentialmineralionsanddissolveoncontact withbodily fluids,formingapatitecrystalsontheirsurface.This permitsbondingonamicroscopiclevelwithapatitecrystalson thetoothsurface.Thesematerialsofferanextendedlifespan withlessneedforfrequentreplacementsandmaycreatedurable restorations.
It’sexpectedthatendodontistswillsoonfocusonregenerative approacheswherebypulptissuecanberevitalizedthroughtissue engineeringandstemcelltherapy.Theresultswouldbeamore biologicallysoundandlongerlasting.
Nickel-titanium fileshavebeenarecentdevelopmentforendodontistsandgeneraldentists,butcontinuoustestingisexpectedto resultinmore flexible,durable,andfracture-resistant files.These new fileswillenhanceefficiencyandleadtobetterclinicaloutcomes.
Clearalignersarethepreferredwaytoaddressaestheticconcerns,offeringadiscreteappearance,customizabilityandaquick turnoverthatdecreasestheprevalenceofcariesrelatedtoprolonged fixedbracesuse.Theabilitytoremovethealignersmeans thepatientcancleanallteethandachievebetteroralhygiene, evenwhenusedforpatientswithrestrictedhandmovements. Fixedbracestendtomakeyoungerindividualsfeelselfconsciousandcanleadtoonlinebullying.Theproblemiseven worseifthepatientmustwearextraoralappliancessuchasorthodonticchincupsandheadgear.
Adrawbackisthatself-ligatingbraceslackthecolorcustomizationoptionsthattraditionalbracesoffer,whichmaybeadisadvantageintheeyesofyoungerpatients.Practitionerswillhave tonavigatetheevolvingpatientpreferencesandsocialin fluences toachievetreatmentacceptanceandbetteroutcomes.
Increasingly,evidenceisbuildingthatsupportsalinkbetween periodontalhealthandsystemicwellness.Plaqueaccountsfor 20%oftheriskfordevelopingperiodontitis.Theremaining 80%prevalenceofnon-plaque-inducedperiodontitistendsto occuratyoungerages.Someofthenewerdrugsmayinadvertentlycompromiseperiodontalhealth,soacomprehensivepatientassessmentandpreventivemeasuresareessentialin caringforpatients.
Focalinfection,whichimpliesthatsystemicinfectionscanbe eithertriggeredorexacerbatedbyoralhealth,underscoresthe needtohelppatientsmaintaingoodoverallhealthsoadequate prophylacticdentalself-careisn’thindered.Lifestylefactorscan affectperiodontalhealthaswell.Patientsneedtobeeducated abouttheimportanceofeatingahealthydietandavoidinga sedentarylifestyle.
Lasertechnologyhasbeenintegratedintoperiodontalandsurgicalprocedures.Itoffersreducedpain,minimalbleeding,and fasterrecovery,soitsuseispopularwithpatientsand practitioners.
Digitaldentistryincludescomputer-aideddesign/computer-aided manufacturingthatprovidesmoreprecisetreatmentplanning andcustomization,betterclinicaloutcomes,andhigherlevels ofpatientsatisfaction.The3-dimensional(3D)printingoftooth structuresandothersystemictissueshasyettobeintroduced, butisexpectedinthefuture.
AIandpredictivemodelshavebeenusedtopredicttheprobabilityofpermanenttoothloss,alongwithotherbehavioralandlifestyleelements.Ageandregulardentalvisitsareprimary indicatorsrelatedtotoothloss,butsocioeconomicfactorsalso
influencetheoutcomes.AIisevolvingintopotentialusesindaily dentalcaresituationstocustomizetreatments.
Virtualandaugmentedreality(VR/AR)mayenhancepatient engagementandtreatmentplanning.Patientswhocanseethe treatmentoutcomesmaybemorelikelytoapprovetreatments andthosewithdentalanxietymaybelessanxious.VR/ARcan helpdentalprofessionalsvisualizeandmanipulate3Drepresentationsofthepatient’sanatomicalstructures,helpingthemto achievemoreaccurateandef ficientdeliveryoftreatment.
Radiation-freeimagingtechniquescouldnotonlybesaferforpatientsbutalsofordentalprofessionals.Thesetechniquesoffera moreclinician-friendlyapproachtomedicalanddentalradiography.
Teledentistryexpandsaccesstodentalcare,allowingthedentist tousedigitaltechnologiestoprovidedentalcare,consultations, education,andtreatmentatadistance.Patientsdon’thaveto bephysicallypresentinthedentaloffice.Advancesinteledentistrybeyondwhatwasachievedduringthepandemicallowdental professionalstoconsult,monitorprogress,anddeliverpreventiveeducationtopatientsregardlessofwheretheyarelocated.
Opportunitiesareopeninginmanydentalspecialties.Inaddition, technologicaladvancescanprovidetreatmentsmoreeffectively, makethemmoreaccessible,andkeepthemaffordable.With theseadvancesandahalttothelossofdentalpractitioners plusadequatefunding,therecouldbeanationalimprovement inthehealthcareofallpatients.
Newdentalmaterials,processes,technology,andprioritiescanhelpdentistrymoveforwardintreatingpatients.Thestaffingshortagesthatplaguehealthcare currentlycanbesomewhatrelievedbysomeofthese approaches,andpatientsmaybemoresatisfiedwith thetreatmentsandresultsthattheyobtainfroma dentalvisit.Dentalpractitionersmaybelesslikelyto leavetheprofessionandmorelikelytoexplorethe transformationsthatmaybepossible.
EshoT:Isthefutureofdentistryasbrightaswehope?Apersonal explorationintodentistry’snationalandglobalprospects. BrDent J 237:761-764,2024
Reprintsavailablefrom TEsho,MedicalUnivofPlovdiv,Facultyof DentalMedicine,HrisoBotev,3Plovdiv,4000,Bulgaria;e-mail: temidentist@gmail.com
Theoralhealthprofessionissignificantlychanginginanumberof waysandinresponsetovariousfactors.Oneofthewaysthese changesmanifestsisagenerationaltransitionthatwilllikelyaffect dentistryasacareerchoice,dentaleducation,andcollaborations betweenmedicalanddentalpractices.
ChartingtheagedistributionfortheUSdentistworkforcein 2001,2017,and2023,alongwithprojectionsinto2028,shows thechangesthathavealreadytakenplaceandthosethatwe mayseeinanother5years( Figure ).In2001,mostdentists wereintheir40s,withfewintheirearly30sortheirlate 60s.In2017,2largegroupsofdentistswereseen,with1group intheir30sandtheotherintheir60s.Thisrepresentsthebaby boomerdentistsnearingretirementastheyageintotheir60s, coupledwiththeexpansionofdentalschoolenrollmentbased onmoredentalschoolsbeingestablishedandhigherenrollmentsatexistingdentalschools.In2023,fewerdentistsintheir 60swereactiveandanincreaseofdentistsintheir30swas obvious.Notonlydidthegrowthofdentalschoolenrollment contribute,butthebabyboomerscontinuedtoretirefrom practice.
Theprojecteddentistworkforcein2028willshowmanyfewer babyboomerdentists.Inaddition,dentalschoolgraduations willcontinuetoincrease,sothattheaverageageofthedentists willbeyoungerthanitistoday.
Althoughitmayseemmerelyachangeintheageofdentiststhat hasoccurred,inactuality,therearechangesintheprofilesof thesedentistsandintheirpracticemodalityaccompanyingthe shiftinage.
Practicingdentistsage65yearsorolderare15%womenand81% White.Incontrast,the2023graduatesofdentalschoolwere55% womenand48%White.Inaddition,57%oftheincomingdental studentsin2023werewomen.Variousdentalworkforceoutcomesarerelatedtothesechanges.It’slesslikelythatfemale dentistswillowntheirpractice,andfemaledentistsaremore likelytotreatMedicaidbene ficiaries.Raceandethnicityalso contributetothesetrends,withdentistswhoareintheminority morelikelytotreatMedicaidbeneficiaries.Femaleandminoritizeddentiststendtomakeless,withnorelationshiptotheyears ofexperienceofthesepractitioners.
Figure. Agedistributionofthedentistworkforce. Source: Datafor2001,2017,and2023arefromtheAmericanDentalAssociationHealthPolicyInstitute analysisofADAmaster fileonOctober2,2024. Source: Projected2028dataarederivedfromtheAmericanDentalAssociationHealthPolicyInstitute dentistworkforceprojectionmodel.(CourtesyofVujicicM,FlynnB,MunsonB:Weareinthemidstofamajorgenerationaltransitionindentistry. JAm DentAssoc 156:85-86,2025.)
Youngerdentistsaremuchlesslikelytoowntheirpracticethan youngerdentists20yearsago.Theyarealsomorelikelyto choosedentalgrouppracticeandtobeaf filiatedwithdentalsupportorganizations(DSOs)thanolderdentists.Grouppractice andDSOaffiliationaren’tnecessarilyconsideredapathtoeventualpracticeownership.Thelevelofdentaleducationaldebt showslittlecorrelationwithchoiceofpracticemodality.
Overa5-yearperiod,mostnewdentiststendtoremainwhere theywereinpracticesizeandaffiliationwithaDSO.Solodental practiceisn’talwaystheirnextstep,withjust10%to14%ofnew dentistschoosingsolopracticeandmoreshiftingfromalarge grouppracticetoasmallerone.Thiswillhaveimplicationsfor variousstakeholdersinthefuture.
Thepracticeprofilesandmodalitiesofdentistsinupcomingyears differfromwhatwastrueforthepast20years.Asthegenerationaltransitioncomestoanend,it’sstillnotclearwhetherthese changesareapositivemoveoranegativeone.
Thechangesthathavebeentrackeddon’tnecessarily fallintothecategoryofproblematicorprogressivefor patients,providers,andotherkeystakeholders.Being awareofwhathashappenedandwhatwelikelywill seeinthenearfuturemaybringinsightsintotheimplicationsofthesenewpatternsandhelpinpreparingfor anewreality.
VujicicM,FlynnB,MunsonB:Weareinthemidstofamajor generationaltransitionindentistry. JAmDentAssoc 156:85-86, 2025
Reprintsavailablefrom BFlynn,HealthPolicyInst,American DentalAssoc,211EChicagoAve,Chicago,IL60611,USA; e-mail: flynnb@ada.org
Artificialintelligence(AI) supportedtoolssuchasChatGPT offertheabilitytomimichumanlanguageprocessingabilities andgeneratehuman-liketext.Indentistry,ChatBPTcanbe usedindigitaldatarecording,imaginganalysis,diagnosisand treatmentplanning,dentaltelemedicine,anddentalandpatient education.Itoffersconvenienceinconveyinginformationand canprovideinstantfeedback.Inpediatricdentistry,parentsare encouragedtobringtheirchildrenfortheir firstdentalvisit beforeage1year.Someofthetopicsthatarediscussedatthese earlyvisitsareearlychildhoodcaries(ECC), fluorideuse,and traumaticdentalinjuries.Becauseparentsmayaccessthe internettodealwiththeseissues,offeringthemaccurateand relevantinformationatthesevisitsisessential.Withoutguidance, ChatGPTcanmakelogicalerrorsorcreateinformationthathas nofactualbasis.Astudywasundertakentotestthequality, readability,andoriginalityofpediatricpatient/parentinformation andacademiccontentprovidedthroughChatGPT.
ChatGPT-3.5wasusedtocollectinformationfromanAImodel. Sixtyquestionsthatpediatricpatients/parentsmightaskwere developedintheareasofdentaltrauma, fluoride,andtooth eruption/oralhealth.Bothquestionsforthepatient/parentand thoseconsideredacademicconcernswereincluded.Ten experiencedpedodontiststrainedtousethemodi fiedGlobal QualityScale(GQS)evaluatedthequalityandsimilarityofthe answers,whereastheFleschReadingEaseandFlesh-Kincaid GradeLeveltestswereusedtoassessthereadabilityandgrade levelofthepatient/parentandacademicquestions.
ScoresforQuality,Readability,GradeLevel,andSimilarity
TheaverageGQSscoreforthepediatricpatient/parent questionswas4.3,whereasthatfortheacademicquestions was3.7.Thedifferencebetweenthe2wasstatisticallysignificant. Readingeaseanalysisfoundanaveragescoreof41.5forthe
pediatricpatient/parentquestionsand34fortheacademic questions.Thisdifferencewasstatisticallysignificantandindicatedthatthematerialwasunderstandableatacollegestudent level.TheFlesch-KincaidGradeLevelaveragescoreforpediatric patient/parentquestionswas12.7,whereastheaveragescorefor academicquestionswas13.7.Thedifferencewasn’tstatistically significantandindicatedunderstandabilityatcollegestudentlevel. Averagesimilarityrateforthepediatricpatient/parentquestions was8.4%,butthatfortheacademicquestionswas5.7%.The differencewasn’tstatisticallysignificant.
Nostatisticallysigni ficantdifferencewasnotedfortheaverage qualityscoresforthepediatricpatient/parentquestions regardingdentaltrauma, fluoride,andtootheruption/oral health.Fortheacademicquestions,thehighestaveragescores werenotedinquestionsabout fluorideandtootheruption/ oralhealth.Theseweresigni ficantlyhigherthantheaverage scoresfordentaltrauma.Forreadability,thehighestscore wasnotedfortootheruption/oralhealthandthelowestfor fluorideonthequestionsforpediatricpatient/parents,with thedifferencestatisticallysignificant.Thevaluesforreadability oftheacademicquestionsandpatient/parentquestionsdid notdiffersignificantly.
Comparisonofsimilarityrateshowedthehighestrateforthe pediatricpatient/parentquestionsregarding fluorideandfor thetooth-eruption/oralhealthamongtheacademicquestions. Thedifferencesbetweenthequestionsforthe2groupsweren’t statisticallysigni ficant.
TheanswersprovidedbyChatGPTwerereasonablyaccurate andusefulforthepediatricpatient/parentquestions,butless acceptableforacademicquestions.Amongtheacademic questions,thelowestscorewasnotedfordentaltraumaand theanswerswereinadequateforaddressingtechnicalandcase questionswithup-to-dateandclearinformation.
ClinicalSignificance
BeforeadoptingChatGPT-creatededucationalmaterialsinapediatricdentalpractice,thedentistshould reviewtheaccuracyofthematerial,especiallywithregardtoacademictopics.Inaddition,materialswritten atacollegestudentlevelmaybetoodifficultforpediatricpatient/parentgroupstofullyunderstand.Theinformationneedstobeatanefficientandreadily understoodleveltoprovideguidanceformostparents ofpediatricpatients.
NahirCB:CanChatGPTbeguideinpediatricdentistry? BMC OralHealth 25:9,2025
Reprintsavailablefrom CBNahir,DeptofPediatricDentistry,FacultyofDentistry,TokatGaziosmanpasËaUniv,Tokat,Turkiye;email: canannbayraktarr@gmail.com
Possiblyrelatedtotheactivelifestylesandsportsinwhichthey engage,traumaticdentalinjuries(TDIs)arecommoninchildren. Theseinjuriesmayaffectthehardtissuesofthetooth,involvethe pulp,orinjuresupportingstructuressuchasbone,ligaments,and gingiva.Immediateinterventionisoftenrequiredtoincreasethe chancesofsuccessfultreatmentandavoidlong-termcomplications.Inaddition,bothchildandparentsmustbereassuredto preventthedevelopmentofdentalanxietyordistress.The prevalenceofTDIsinpediatricpatientsvarieswidelybasedon geographiclocation,socioeconomicstatus,anddemographic factors.Treatmentusingconservativeprinciplescanhelpto preservethevitalityoftheinjuredtoothandavoidunnecessary extractions.Asystematicreviewwasdonetoupdatecurrent knowledgeoftheprevalence,types,management,complications, andpreventionofdentaltrauma(Figure1).
AsearchoftheScopus,WebofScience,andPubMeddatabasesfor studiesovertheperiodfrom2010to2024yielded12studiesthat wereeligibleforqualitativeanalysis.Theanalysiswasfocusedon epidemiology,diagnosisandtreatment,innovativetreatments,clinicaldecisionsupporttools,andtheimpactonthechild’squalityoflife.
Epidemiology
Studiesfocusingontheprevalenceofdentalinjuries,common causes,andimportanceoftimelyinterventionandeducation identi fiedaprevalenceofabout1.25%,withboysage7to12years beingaffectedmoreoftenthangirls.Causesinvolvedfalls,object
strikes,andbikeaccidents.Studiesindicatedvariouscommon injuries,includingEllistypeIVfracture,usuallyinvolvingthe maxillarycentralincisorsandaccompanyingsofttissueinjuries; subluxationandavulsioninprimaryteeth;andcrownfractures inpermanentteeth.Amongtheteethmostoftenaffectedwere maxillaryincisorsinbothdentitions.Therewasahigher incidenceofTDIsinpermanentthaninprimarydentitions, withtheyoungerchildrenmoreoftensufferingsofttissue injuries.Preventivedentalcareandeducationprogramsare neededtomanageandpreventchildhooddentalinjuries.
Studiesofspecialneedschildrenfoundthat23.1%ofthesepatients sufferedTDIsthatwereoftenrelatedtofallsandstrikingobjects. HigherTDIprevalencewasassociatedwithobesityandinadequatelipcoverageinsomeanalyses.Mostinjuriesoccurredat school,andonlyafourthoftheaffectedchildrenweretakenfor dentalcare.
Tomitigatelong-termdentalanomalies,childrenshouldbe broughtforearlyandaccuratediagnosis.Amongtheinjuries associatedwithlong-termconsequencesarecrownandroot dilacerationinpermanentincisorsthatdevelopaftertheprimary incisorswereinjured,whichcouldleadtointrusiveluxationsand avulsions.Thesecanproduceenamelhypoplaxiaanderuption disruptionsinpermanentteeth.Inaddition,earlytraumain primaryteethwasfoundtoleadtoenamelhypoplasiaandother complicationsinpermanentteeth.Asaresult,parentsanddental careprovidersshouldstresstheneedforpromptdiagnosisand treatment,withregularfollow-upsandprompttreatmentto preventorminimizelong-termcomplications.
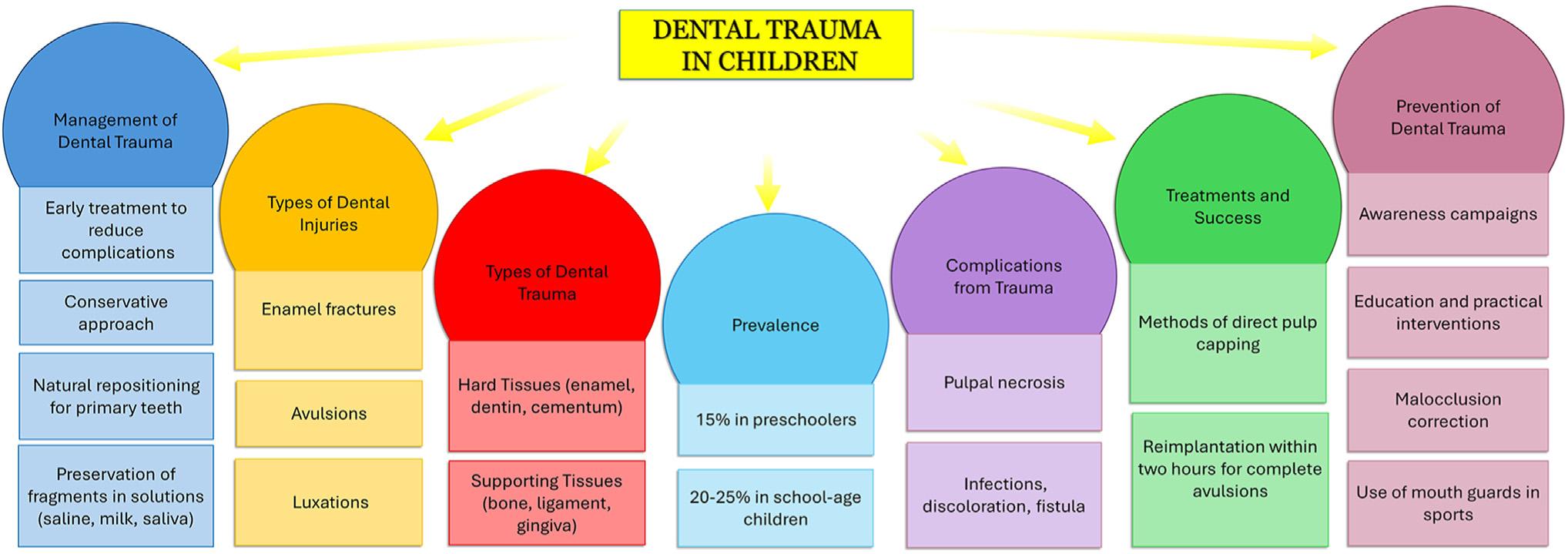
Figure1. Conceptmapofdentaltraumainchildren.(CourtesyofLaforgiaA,InchingoloAM,InchingoloF,etal:Paediatricdentaltrauma:Insightsfrom epidemiologicalstudiesandmanagementrecommendations. BMCOralHealth 25:6,2025.)
Variouspulpotomymaterialsareusedtomanagetraumatized immaturepermanentteeth.TheInnovativeBioCeramixwas comparedwithtraditionalcalciumhydroxide(CH)andachieved ahigherpulpsurvivalrate,althoughthedifferencedidn’treachstatisticalsigni ficance.TheBioCeramixproductalsoofferedeasier handlingpropertiesthanCH.Ifanewermaterialoffersbettersealingpropertiesandgreatereaseofuse,itmayprovetobeofvalue.
Deciduousautologoustoothstemcells(hDPSCs)that regeneratedentalpulpininjuredteethhasbeenimplantedinto rootcanals,followedbysealingwithmineraltrioxideaggregate (MTA).ThehDPSCssignificantlyimprovedvascularandneural formationandincreasedrootlengthandwidth.hDPSCsmay beusefulforsalvagingyoungteethandenhancingrootdevelopment.Thisproduct fitswellwiththefocusontissueregeneration andthecreationofaconductivemicroenvironmentforhealing.
Clinicaldecisionsupporttools(CDSTs)mayimprovedental traumamanagement.Whenstudiedfortheireffectonthe managementofprimarydentitionTDIs,significantimprovements werenotedindiagnosticandmanagementskills,especiallyamong dentalstudents.IntegratingCDSTsintoeducationprograms shouldbeconsidered.
Whenspecialneedschildrenwerestudied,thegroupswithcerebralpalsyandobesityhadhigherratesofdentaltrauma.Inaddition,amongpreschoolchildren,TDIsandcavitatedlesions negativelyaffectedoralhealth relatedqualityoflife(OHRQoL).
Whensocioeconomicfactorswereconsidered,lowerincome andmother’seducationallevelwerelinkedtocariesprevalence. ParentalperceptionofpoororalhealthcorrelatedwithanegativeOHRQoL.
Inpediatricdentistry,dentaltraumaindeciduousteethisboth prevalentandsigni ficant.Inaddition,theseinjurieshavelongtermconsequences.Commoncausesofthistraumaarefalls, sportsinjuries,andaccidentswithobjectsorbicycles.Earlydiagnosisandinterventionareneededtopreservethevitalityof injuredteethandpreventcomplications.ManagementofTDIs shouldbeimmediatetoimproveoutcomes.Conservativeapproachesareadvisable,alongwithfrequentfollow-upvisitsand monitoringforlong-termcomplications.
Dentalstudentsshouldbetrainedinearlyintervention strategiesandconservativeapproacheswhenmanagingpediatricdentalpatientstopreventlatecomplications.Policymakersshouldfocusonpreventive measuresandeducationalprogramstohelpinavoidingdentalinjuriestochildren.Followingrecommendationsbasedonevidencewillenhancethequalityof careandensurebetterlong-termoutcomesforchildrenwhosufferdentaltrauma.
LaforgiaA,InchingoloAM,InchingoloF,etal:Paediatricdental trauma:Insightsfromepidemiologicalstudiesandmanagement recommendations. BMCOralHealth 25:6,2025
Reprintsavailablefrom FInchingolo,DeptofInterdisciplinary MedicineUnivofBari “AldoMoro,” Bari70124,Italy;e-mail: francesco.inchingolo@uniba.it
Arecommendedmethodforavoidingearlychildhoodcaries (ECC)isbrushingyoungchildren’steethwitha fluoridecontainingtoothpaste.Specialinstructionsandwarningsare includedfortheuseof fl uoridetoothpastesforchildren.These statementsdealwiththedegreeof fluorideincludedinthetoothpaste(0.1%to0.15% fluoride)andtheamountoftoothpasteto use(apea-sizedamount; Table1).Parentsshouldbeawareof theseinstructionsandwarningsandshouldalsosupervisethe brushingoftheiryoungchild’steeth.Theyshouldalsoknow aboutothersourcesof fluoride,includingtablets, fluoridated salt,someinfantformulasthatarebasedonsoy,andartificially ornaturally fluoridatedwaterinthecommunity.Dentistsoften apply fluoridatedvarnishestwiceayearaswell,andthesecontain 5%sodium fluoride.Studiesindicatethatahighpercentageofchildrenage18to30monthsswallowallthetoothpaste,putting themselvesatriskfordevelopingdental fluorosis.However, about40%of3-to6-year-oldchildrenreceivemorethanthe recommendedpea-sizedamountoftoothpaste,withmostparentsusingmoretoothpastethanrecommended.Thereal-life doseof fluoridetoothpasteusedbyparentswhosechildren wereuptoage24monthswasinvestigated.
Parentsat5daycarecentersinGermanywereaskedtoplacea doseof2different fluoridetoothpastesthattheywouldnormally givetheirchildontoothbrushes.Theamountoftoothpasteon eachwasweighed.Anexampleoftherecommendedrice-sized dosewasperformed5timesbyexperienceddentistsusinga naturalgrainofriceasanexample.Thiswasusedasthestandard againstwhichtheparents’ samplesweretested(Figure1). Parentswerealsoaskedtoreportthetotalfrequencyoftooth brushingperday,whattheyknewabouttheconditionsofuse andwarningson fluoridetoothpastes,andwhethertheyused fluoridetabletsaswellasa fluoridetoothpaste.
The61parentsdosedameanof0.263goftoothpasteAand 0.281goftoothpasteB.ThetoothpasteAdosewas5.9times higherthanrecommendedandthetoothpasteBdosewas7.2 timeshigher.Thesedifferenceswerestatisticallysigni ficant.
Parentsreportedtheybrushedtheirchild’steeth2or3times aday.Whenaskedabouttheconditionsofuseandwarnings on fl uoridetoothpaste,about39%wereunawareofthese conditions,eventhoughtheyappearedonthepackageof fl uoridetoothpaste.Withrespecttotheuseof fl uoridetablets,about15%usedthemandabout85%didn’t(Table2 ).
Table1. Recommendationsofthe EuropeanAcademyof PaediatricDentistry onthedoseof fluoridetoothpastefor children,takenfrom[6].(Reproducedwithpermissionfrom ToumbaKJ,TwetmanS,SpliethC,etal:Guidelinesontheuseof fluorideforcariespreventioninchildren:AnupdatedEAPDpolicy document. EurArchPaediatrDent 20:507-516,2019.)
Age
Fromthe firsttooth upto24months Grainofrice1000 2–6yearsPea1000 >6yearsUptofulllength ofbrush 1450
(CourtesyofSudradjatH,MeyerF,FandrichP,etal:Dosesof fluoride toothpasteforchildrenupto24months. BDJOpen 10:7,2025.)
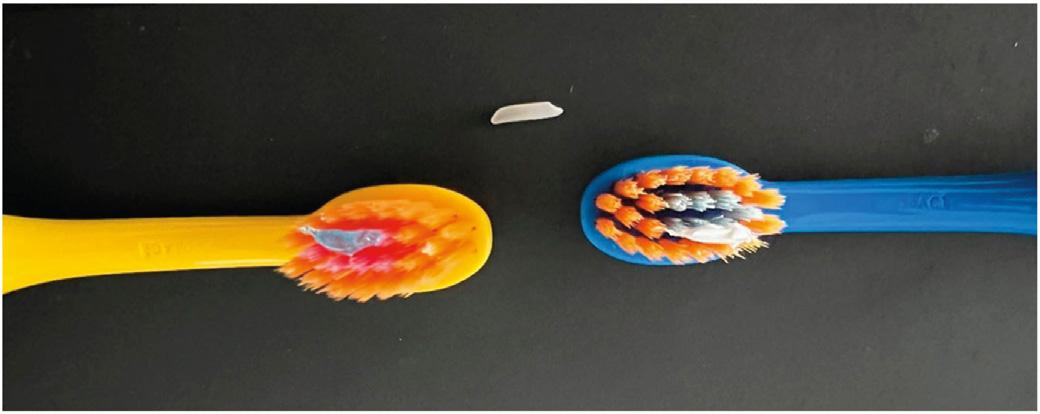
Figure1. Referencedoses.Photographofthereferencedoses(i.e.,agrain ofrice sizedamountoftoothpaste)asrecommendedfortoothpastesfor childrenagedupto24monthswith1000ppm fluoride[6,7]ortoothpaste A(left)andtoothpasteB(right)onchildren’stoothbrushes.Anaturalgrain ofricewasusedasmodel.Bothamountsweredosedbyanexperienced dentist(seeTable4forweightresults).(CourtesyofSudradjatH,MeyerF, FandrichP,etal:Dosesof fluoridetoothpasteforchildrenupto 24months. BDJOpen 10:7,2025.)
Table2. Sourcesof fluorideinfoodandbeverages(examples)
SourceFluorideconcentrationReference
Soybeanbeverages8.5–15.5mg/L[51]
Blacktea1.6–6.1mg/L[52]
Rice0.53–3.61mg/kg[16]
Bananas0.86–1.98mg/kg[16]
Coffee0.845–1.465mg/L[53]
Cow’smilk0.016–0.18mg/L[54]
(CourtesyofSudradjatH,MeyerF,FandrichP,etal:Dosesof fluoride toothpasteforchildrenupto24months. BDJOpen 10:7,2025.)
Thecorrectamountoftoothpastewasnotdispensedbythe parents.Theamounttheydispensedwas5.9to7.2timeshigher thantherecommendeddose.
Toreduceanoverabundanceof fluoridebeinggiven whenparentsbrushedtheirchild’steeth, fluoridefreetoothpastemaybeused.However,thesereplacementsshouldcontainananti-cariesagenttoprevent ECC.Thisapproachshouldpreventdental fluorosis andothersideeffectsof fluoride.
SudradjatH,MeyerF,FandrichP,etal:Dosesof fluoridetoothpasteforchildrenupto24months. BDJOpen 10:7,2025
Reprintsavailablefrom JEnax,DrKurtWolffGmbH&Co.KG, ResearchDept.Johanneswerkstr34-36,33611Bielefeld, Germany;e-mail: joachim.enax@drwolffgroup.com
Myofunctionaltherapy(MT)isusefulformanagingorofacial myofunctionaldisorders,whichcaninvolvethemusclesand thefunctionsofthefaceandmouth.Thedevelopingordeveloped craniofacialstructuresandtheirfunctionareshapedbyneurologicalre-educationthroughMT.Musclefunctionisoptimized,and structuralalignmentiscorrectedtopromotehealthygrowthand development.Thetargetedmuscleexercisesimprovetone, proprioception,andmobility,allowingforthecorrectionof habits,interceptivetreatmentofsleep-disorderedbreathing (SDB),andthepromotionoforofacialdevelopment.Thevarious rolesofMTinpediatricdentistrywereexplainedandrecommendationsweremaderegardingtheinterdisciplinaryapproachthat supportsMT.
Varioussituationscandevelopinchildrenthatmaybene fitfrom MT Figure1.TheseincludeSDBandairwaydevelopment,nonnutritivesuckinghabits(NNSH),andfacialgrowthand development.
SDBandAirwayDevelopment
AmongthetypesofSDBareobstructivesleepapnea,hypoxemia, upperairwayresistance,hypoventilation,andcentralsleepapnea. ThesymptomsassociatedwithSDBincludesnoring,bruxing, open-mouthbreathing,andapnea,whichcancausepoorsleep, daytimesleepiness,andbehavioraldisorders.Severalstudies
identifytheeffectofbreathingpatternsonfacialmuscles,function,andef ficacywithrelationtoupperairwayresistanceandfrequencyofcollapse.Snoringandadenotonsillaryhypertrophy showlinks,asdodentoskeletalanomaliessuchasanunderdevelopedmaxillaryarchandintricateocclusionpatterns.SDBdevelopmentisinfluencedbytongueposition,facialdevelopment,and oralhabits.
MTcanimproveSDBwithinabout6monthsbystrengtheningthe orofacialmuscles,promotingnasalbreathing,andimprovingthe tongue’srestingposition.ItcanalsoreduceSDBseverityby maintainingairwaypatencyduringsleep.Bothpediatricandadult populationscanhavelowerapnea-hypopneaindices(AHIs)with MT,andtheseimprovesnoring,oxygensaturation,and sleepiness.AdjunctivetherapywithMTcanhelptreatSDBwhile promotinghealthiersleephabits.
ProlongedNNSHcancausedentalmalocclusion,alteredtongue positioning,andorofacialdysfunction,allofwhichcanpredispose childrentoSDBanddisorderedcraniofacialgrowthanddevelopment.Theseabnormalitiescanleadtoahigherriskforupper airwaycollapseduringsleep.Someevidenceindicatesupto 68%ofchildrenhaveNNSHand38%haveanterioropenbite. Anterioropenbitemaybelinkedtogeneticfactorsandis associatedwithnonnutritivehabits,tonguethrust,andopenmouthbreathing.Theseproblematicconditionscancausespeech andfeedingdif ficulties,aswellasTMJdisorders.

Figure1. Processdiagramofassessmentforneedofmyofunctionalinpediatricdentistry.(CourtesyofLeungCK,VanNoyM:Theroleofmyofunctional therapyinpediatricdentistry. JCalifDentAssoc 52:2400418,2024.)
MTcancorrectthesehabitsthroughneuromuscularreeducationandexercisesoftheorofacialmuscles.Tongueposture andnasalbreathingarealteredtoactivatetheparasympathetic responseandeliminatetheneedforNNSH.Oncethechildno longerexhibitsNNHS,therecanbeimprovementsinanterior openbit,craniofacialstructure,andcontinueddevelopment.
Althoughfacialdevelopmentbeginsinuterowhenthepalateis formedaroundthetongue,whichnearly fillstheoronasalcavity, itcontinuesafterbirth,withthetongueapplyingpressuretothe palateandshapingit.Thetongue’shighpositiononthepalateis
optimalatbirth,buteventuallynaturalpalatalexpansionoccurs andanidealfacialgrowthpatterndevelops.Notonlydoesthe tongueshapethepalate,butit’scriticalforproperbonegrowth. Somein fluencesthatcanleadtoaloweredpositionofthe tonguearemouthbreathing,muscleweakness,geneticpredispositionfortonguespace,anddetrimentalhabits.Thelowered tonguecanleadtoahighand/ornarrowpalate.
Duringcraniofacialdevelopment,theorofacialmusclesare crucial,withdysfunctioncausedbytongueposition,SDB,or NNSHleadingtoabnormalgrowthpatterns.MTpromotes normalmusclefunction,leadingtomoreappropriatecraniofacial
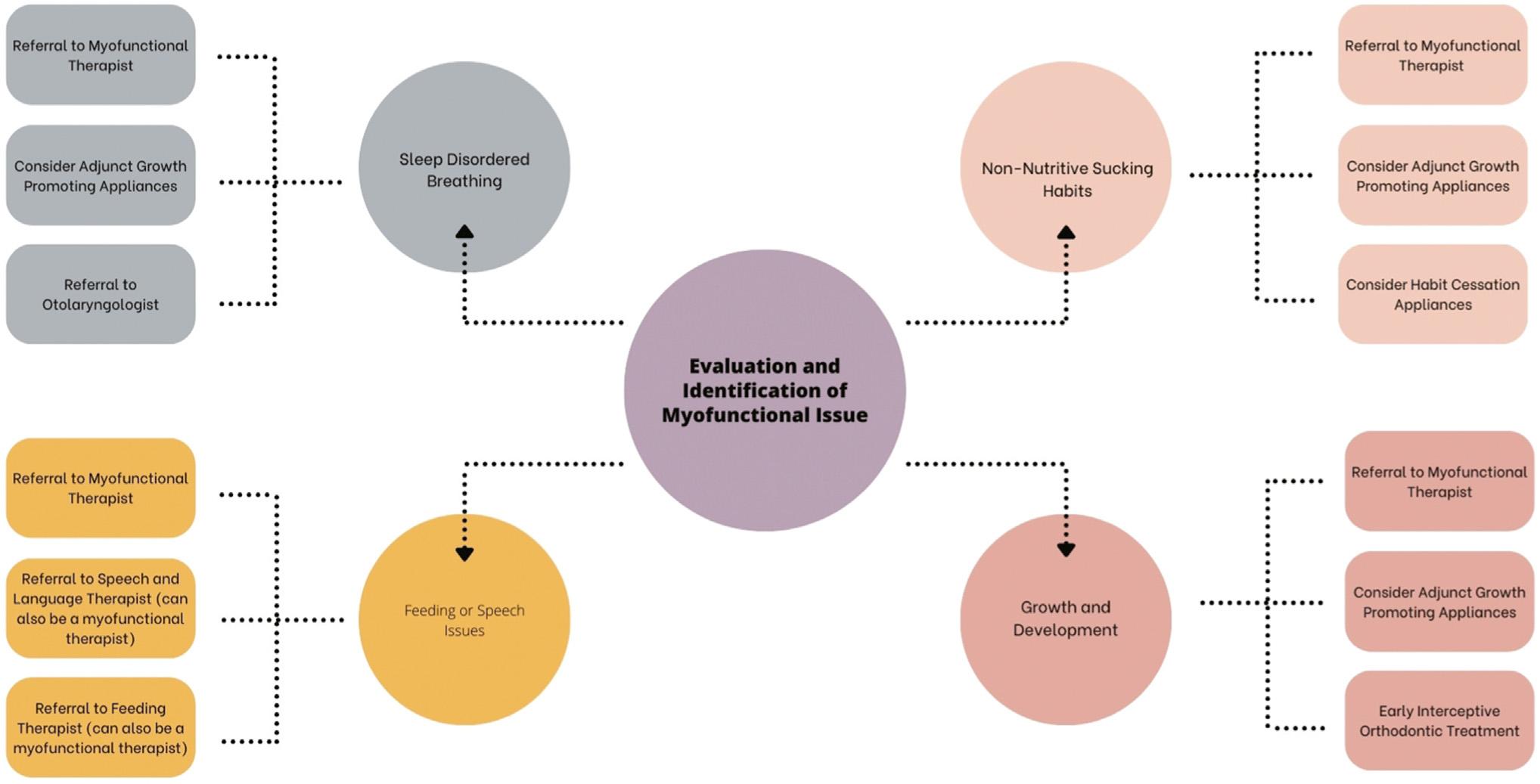
Figure2. Evaluationandidentificationofmyofunctionalissuesalgorithm.(CourtesyofLeungCK,VanNoyM:Theroleofmyofunctionaltherapyin pediatricdentistry. JCalifDentAssoc 52:2400418,2024.)
growthanddevelopment.EarlyinterventionwithMTcanhelp preventormitigatedevelopmentalissueswithbetterlong-term outcomesforchildren.
Collaborationsbetweenpediatricdentistsandmyofunctional therapistsareessentialincraftingearlyinterventionsand comprehensivetreatmentplansforchildrenwithorofacial muscledysfunctionandimproperoralhabits.Pediatricdentists ororthodontists,speech-languagepathologists,andotherdental professionalsshouldseekoutprofessionalscertifiedbyorganizationssuchastheInternationalAssociationofOrofacialMyology ortheAcademyofOrofacialMyofunctionalTherapy.Professional conferences,interdisciplinarystudygroups,andprofessionaldirectoriesoffereffectivewaystocontactqualifiedmyofunctional therapists(Figure2).
ClinicalSignificance
MThelpsinaddressingSDBandNNSHandmanaging theireffectsongrowthanddevelopmentinyoung children.Thefunctionsoftheorofacialmusclesare targetedbythedentalprofessionalandmyofunctional therapisttoimproveairwaypatency,promotehealth craniofacialgrowth,andhelpinreducingoreliminating detrimentalhabits.
LeungCK,VanNoyM:Theroleofmyofunctionaltherapyinpediatricdentistry. JCalifDentAssoc 52:2400418,2024
Reprintsavailablefrom CKLeung;e-mail: drc@seastar pediatricdentistry.com
Cannabisuseincreased60%between2002and2019inthe UnitedStates.Withtheexpansionoflegislation,increased prevalence,andchangingattitudestowardcannabis,it’slikely thatdentalprofessionalswillencounterpatientswhouse cannabis.Cannabisisassociatedwithvariouseffectsonthehumanbody.Itoffersreliefofpain,relaxation,releasefromanxietyanddepression,andantiemeticproperties,withcentral nervoussystemcannabinoidreceptorsandendocannabinoids underreviewforrolesaspossibletherapeuticagents.However,thehardandsofttissuesoftheoralcavitysufferdetrimental effectsfromcannabisuse.Amongtheproblemsareahigher incidenceofcariesinregularcannabisusers,xerostomialasting 16hours,increasedconsumptionofsweetandcariogenicfood anddrink,andperiodontaldisease.Inaddition,theprevalence ofolderadultswhousecannabishasincreaseddramatically, raisingconcernovercariesandtoothloss.Frequentrecreationalcannabis(FRC)useinadultswasevaluatedforitsinfluenceonuntreatedcoronalcaries,untreatedrootsurface caries,andseveretoothloss.
DatawerederivedfromtheNationalHealthandNutritionExaminationSurvey(NHANES)continuouscycles2015-2016and 2017-2018.Atotalof5656individualsage18through59years (averageage39years)whosecannabisusedatawereavailable wereincluded.Individualswhousedmarijuanaorhashishat leasteverymonthformorethanayearwereclassi fiedas FRCusers,withthosewhodidn’tfulfi llthiscriterionconsiderednon-FRCusers.Thedentaloutcomesevaluatedwereuntreatedcoronalcaries(atleast1toothinvolved),untreated rootcaries(atleast1toothinvolved),andseveretoothloss (fewerthan9remainingpermanentteeth).Otherfactors consideredwereage,sex,raceorethnicity,nativity,educa-
tionalattainment,familyincometopovertyratio,andalcohol consumption.
Theoverallprevalenceofuntreatedcoronalcarieswas22%,with thatofuntreatedrootsurfacecariesat11%.About5%ofthe samplehadseveretoothboss.Approximately29%oftheparticipantsreportedFRCuse.TheprevalenceofFRCusewashighest amongthenon-HispanicBlackparticipantsatabout37%,and menweremorelikelytoparticipateinFRCusethanwomen (about35%versus24%).
MoreFRCusershaduntreatedcoronalcaries(about28%) comparedtonon-FRCusers(about20%).Theproportionof FRCuserswithuntreatedrootsurfacecarieswasalmosttwice thatofnon-FRCusers,withratesofabout16%versus9%.Severe toothlosswasnotedinabout7%ofFRCusersandabout4%of non-FRCusers.
FRCusersweremorelikelytohaveuntreatedcoronalcaries,untreatedrootsurfacedentalcaries,andseveretoothlossthannonFRCusers.Theseassociationsremainedsignificantaftercontrolling forcovariatesandpotentiallyconfoundingfactors.ForFRCusers, theprobabilityofhavinguntreatedcoronalcarieswas17%higher thanfornon-FRCusers.Inaddition,theFRCusershadoddsofhavinguntreatedrootsurfacecariesandseveretoothlossthatwere 55%and41%,respectively,higherthanthosefornon-FRCusersaftercontrollingforthepotentiallyconfoundingfactors.
AdultswhoengageinFRCusearemorelikelytodevelopuntreatedcoronalcaries,untreatedrootsurfacecaries,andsevere toothlossthanthosewhodon’tusecannabisinthisway.
ClinicalSignificance
Dentistsshouldreviewtheirintakequestionnaireswith thegoalofspecificallyaskingaboutcannabisuse. Withthisinformation,dentalcareproviderscanidentifyandaddresstheeffectsofFRCuseandtalktopatientsabouttheproblemsassociatedwithfrequent cannabisuse.Oftenpatientsdon’trealizethedamage thatFRCusecaninflictontheirteethandoralsofttissues.Inaddition,additionallongitudinalresearchis neededtoevaluatetheeffectsofFRCuseonthenaturaldentitionoftheUSpopulationnowthatcannabis useisacceptableandevenlegalinmanyareas.
ClonanE,ShahP,CloidtM,etal:Frequentrecreationalcannabis useanditsassociationwithcariesandseveretoothloss. JAm DentAssoc 156:9-16,2025
Reprintsavailablefrom EClonan,114SquireHall,UnivatBuffaloS Campus,Buffalo,NY14214,USA;e-mail: elclonan@buffalo.edu
IntheUnitedKingdom,afreevapingstarterkitwasgivento1 millionsmokerstoencouragethemtogiveuptobaccoproducts, withtheambitiousgoalofmakingEnglandsmoke-freeby2030. Theterm electronicnicotinedeliverysystems (ENDS)refersto e-cigarettes,electronicvaporizers,andvapingpens.Theuseof e-cigarettes(“vaping”)hasincreasedexponentiallyfromtheir firstintroduction,makingitlikelythatthedentalteamwillneed toanswerquestionsfrompatientsaboutthesafetyandeffects ontheoralcavityofusingthesedevices.Althoughthese devicesaretoutedasasaferalternativetocigarettesmoking, thedentalteamshouldbepreparedtooutlinetherisksofvaping onoralhealth,anylinkstooralcancer,andotherinformationfor patients.
Althoughtheevidenceregardingvapinganditseffectsonoral healthisscant,thePubMeddatabasewassearchedtoidentify studiesofe-cigarettes,ENDS,vaping,oralcancer,andoralhealth. Themostrecentstudieswereselected.
ENDSproductsweredevelopedtoofferasaferalternativeto conventionalcigarettesmokingandarepopularnotonlywith smokersbutalsowithpreviouslynonsmokingadolescents,who enjoytheadded flavorings.ENDScompriseabattery-powered heatingelementtoaerosolizetheliquidforinhalation.Theliquid containsvariousingredientsthatoftenincludenicotine, flavoring agents,andpropyleneglycoland/orglycerin.Somearenicotine free,butthosecontainingnicotinevaryintheiramounts.Other
componentsincludetobaccoalkaloids,formaldehyde,glycerol, andheavymetals.Toxiccontentalsovaries.Asaresultofthese variations,thedeleteriousoralhealtheffectsdifferwiththeproductsinvolved.Thesecond-handtoxicexposuresviatheaerosol andexhaledvapehavenotyetbeenshowntoposeameaningful biologicalrisk.
TheprimaryappealofENDSistheirstatusasasaferalternative tocigarettesmoking.However,childrenexperimentwithvaping becausetheylikethe flavorsandbecausetheyseepeersusing them.Overhalfofneversmokershavereporteduseto “giveit atry” comparedtojustabout25%ofthosewhohaveever smoked.
TheeffectsofexposuretoENDSonoralhealthincludedysbiosis andchangestotheoralmicrobiomethatfosteranincreaseinthe numbersofopportunisticpathogens.ENDSmayhaveanadverse effectonhead,neck,andoralcells,producingaberrantmorphology, cytotoxicity,reducedviability,delayed fibroblastmigration,and genotoxicity.However,thedegreeofadverseeffectsissignificantly lessthanthatseenwithconventionalcigarettesmoking.
ENDSareasaferalternativetoconventionalcigarettesbasedon theirlowercontentoftoxicandcarcinogeniccompounds.However,it’sdif ficulttoestablishreliabletoxicityprofilesofthese productsbecausetheyvaryindesign,manufacturingmethods, andingredients.Althoughe-cigarettescontainsubstantiallylower amountsandfewercarcinogensthantobaccoproducts,thebasic
mechanismsofDNAdamagemaystillapply.Theriskofdevelopingheadandnecksquamouscellcarcinomaislowerwith ENDSthanwithcigarettesmoke.
Heavymetalcontentismuchlowerthaninconventionalcigarettes butchronicexposuresthroughsmokingtoheavymetalsincreases theriskofheadandneckcancer.FormaldehydeisaGroup1 humancarcinogenwithariskforcausingnasopharyngealcancer.
OncogeniceffectsrelatedtoENDScaninduceDNAdamage, oxidativestress,DNAdouble-strandedbreaks,apoptosis,necrosis,andgenotoxicityinvarioustypesoforalcells.TheENDSliquidscaninducechangesthatcontributetotumorigenesisin normalepithelialcellsandpromoteaggressivephenotypesin pre-existingmalignantcells.However,long-termprospective andlarge-scalecasecontrolstudiesareneededtoprovide furtherinformationregardinganycausalrelationship.
ENDSproductsaremoreeffectivethannicotinereplacement therapy(NRT)inhelpingconventionalsmokersquitsmoking. However,theeffectsofthelong-termuseofnicotineremain tobeidenti fied.Noadverseeventshavebeenlinkedtoeither NRTorENDS,butNRTusersaremorelikelytoexperience nauseaandENDSusersaremorelikelytoreportmouthor throatirritation.
Anumberofothereffectshavebeensuggested,asfollows:
ENDSmayincreasechemotherapyresistance.
E-cigaretteshaveadecreasedexpressionofimmune-related genesthatmaysupporttheassociationbetweenENDSuse andoralhumanpapillomavirusinfection.
ENDSmayhaveanindirecteffectrelatedtothelikelihoodof futuretobaccosmokingamongadolescentusers.
Poor-qualityevidencesuggestsotheroralsymptoms,suchasxerostomia,burningsensation,irritation,pain,oralulceration,nicotine stomatitis,hairytongue,andangularcheilitis,mayoccurwith ENDS.Inaddition,accidentshavebeenreportedthatcausedburns fromexplosionsandmalfunctionsthatinjuretheoralcavity.
Obtainingthepatient’ssmokingstatusshouldbethe firststepin deliveringanysmokingcessationcounseling.Smokingstatus questionsshouldbeincludedintheintakequestionnaireor confirmedverbally.Asimpletoolforthedocumentationof smokingstatushelpsclinicianscapturemeaningfulandcomplete
Table2. ASystematicTooltoCapturePatients’ ENDSStatus. (DatafromJoseT,HysJT,WarnerDO:Improveddocumentation ofelectroniccigaretteuseinanelectronichealthrecord. IntJ EnvironResPublicHealth 17:5908,2020.)
E-cigaretteuseCurrent – daily
Current – somedays
Former Passiveexposure
Never
DevicetypeRechargeablee-cigarette
Refillablee-cigarette
Disposablee-cigarette E-cigar E-pipe
Other
Numberofrefills/disposableunitsperday?
Cessationcounsellingprovided?
(CourtesyofCameronA,YipHM,GargM:Currentthinkingabouttheeffectsofe-cigarettesonoralcancerrisk. BDJTeam 11:470-473,2024.)
datarelatedtoENDSuse(Table2).Itprovidesforthestrati ficationofindividualoralhealthriskfactorsandofferstailoredcessationadvice.
Cliniciansshoulddocumentthepatient’sENDSuseaspartofthe healthrecordandofaholisticassessmentoforalcavitycancer risks.TheyshouldcounselpatientsthattheevidenceforENDS safetyislackingandthefullriskpro fileisn’tyetavailable.ENDS productsaresaferthanconventionalsmoking,butnonsmokers shouldn’tbeginusingthem.
ThevariousENDSproductscarrydifferingpotentialfor deleteriousoralhealtheffects.Forpatientswho choosetouseENDSproducts,dentalpractitioners canofferguidancebasedonthecurrentevidence. Thisindicatestheseproductsarelessharmfulthan conventionalsmokingbutcan’tbeconsideredsafe andrisk-free.Extensiveresearchisneededtobe abletoaccuratelyevaluatetheeffectsofENDSuse ontheoralcavity.
CameronA,YipHM,GargM:Currentthinkingabouttheeffects ofe-cigarettesonoralcancerrisk. BDJTeam 11:470-473,2024
Reprintsnotavailable
Oncetheendodonticclinicianachievesapicalpatencyandpreservesperi-cervicaldentin,variousintraoperativefactors relatedtoobturationand flare-upsofpainandswellingmust bemanaged.Inaddition,postoperativeconsiderationsthat arerelatedtotheoverallsuccessandlongevityofendodontic treatmentsmustbeaddressed.Tipsfordealingwithintraoperativeandpostoperativeissuesaswellasocclusionweresuggested,andtheprognosisrelatedtothesefactorswas determined.
Amongthefactorstobeconsideredintraoperativelyarethe lengthoftherootcanal fillingandthedensityandtaperofthe rootcanalobturation.
RootCanalFillingLength
Fewstudieshaveevaluatedtheeffectofleavingachemomechanicallydebridedrootcanalunfilled,butthoseavailableshowabout 40%to60%offailuresarerelatedtoinadequateobturationofthe rootcanalsystem.Thiscaninvolveover filling,underfilling,or poorquality filling.Currentthinkingisthatthequalityofthecoronalrestorationismoreimportantforperiapicalhealththanroot filling.Root fillingshouldstillbedonetomanageinfectionremainingaftercleaningandshapingandwillhelppreventmicroleakage ifthecoronalsealiscompromised.Thepatient’sspeci ficneeds shouldguidetheclinician’sdecisionratherthanusingthesame approachforallcases.Root fillingstowithin2mmoftheapex havesuccessratesof81%.
Theclinicianshoulduseelectronicapexlocatorstodetermine thepreciseworkinglength,avoidingover fillingorunderfilling ofthecanalsandensuringtheroot fillingisatthedesiredlength. Double-checkingtheworkinglengthisbestaccomplishedusinga cone-fitradiographwiththemastergutta-perchapointinplaceif noradiographwastakenearlier.The fillingmaterialshouldbein the0-to2-mmrangefromtheapex.Useofawarmvertical compactionorcontinuouswavecondensationcanaidoptimal fillevenincomplexcanalstructures.
Achievingagood3-dimensional fillcanavoidresidualinfectionafterchemomechanicaldebridement.Satisfactoryobturationshave significantlybettersuccessrates.Aradiographicallydenseroot fillingmayhelptodelaymicrobialseepageshouldacoronalsealfail.
Theuseofmagni ficationandillumination,lateralcondensationor warmverticalcompactiontocreateuniformandvoid-freeobturation,andcon firmationwithradiographswillensurequality obturationandimprovedprognosis.Sealerscanbeusedto fill anyvacantspacebetweenthedentalwallandthecore fillingmaterialandestablishagoodseal.Withtheuseoftraditionalsealers, it’swisetoensurethecore fillingmaterial fillsmostofthecanal space,thuspreventingsealer-relatedproblems.Thenewercalciumsilicate basedsealerssimplifytheprocessandreduceobturationtime.
Preparingandcreatingataperintherootcanalsfacilitatesirrigationandeffectivechemomechanicaldebridementandreduces theriskofextrudingirrigantsandobturatingmaterials.Overtaperingcanweakenrootsbycompromisingpericervicaldentin, whereasunder-shapingcancompromisetheprognosis.
Interappointment flare-upsofpainandswellinghaveapoorer treatmentoutcomeinmanycases,representingexacerbations ofperiapicalinflammationorinfection.Causesincludeinadequate asepsisordisinfection,improperirrigation,ormaterialextrusion. Amongtheeffectsofthese flare-upsareimpairedmouthopening, damagetotheprovisionalrestoration,andcompromisedprognosis.Ifmicroorganismsremainwithinperiapicaltissuesafter treatmentandprovokeaninflammatoryresponse,tissueirritation andperiapicalinflammationcanbeexacerbated.
Avoidingthiscomplicationinvolvesusingrubberdamisolation foranasepticoperating field;adoptingaconservativeandgentle approachduringcanalinstrumentation;usingintermittentirrigationtechniqueswithaside-ventedneedleto flushdebris anddisinfecttherootcanalsystem;andprovidingpatients withcleardirectionsregardinghowtoaddressdiscomfort, swelling,andothercomplications.Theclinicianshouldprescribeappropriateanalgesicsandrecommendmeasuressuch ascoldpacksoranti-inflammatorymedicationstoalleviate postoperativesymptoms.
Amongthepostoperativefactorstobeaddressedwhenseekinga goodprognosisarethecoronalsealandpost-endodonticrestorationsandthetimingofcuspalcoverage.Inaddition,theocclusionplaysasignificantroleintheprognosisofendodontically treatedteeth.
Table1. PrognosisBasedonVariousIntra-operativeFactors
StageCategoryFactorParameterstoconsiderPrognosis
Intra-operativeApicalpatencyPreviously untreated/Primary RCT
Peri-cervicaldentine (PCD)
NegotiableGood
Inabilitytoachievetechnical patency(debris/complex anatomy)
RetreatmentAbletoremoveasignificant amountoftheexistingroot filling material
Accesscavity preparation andremaining coronalwalls
ObturationLengthofrootcanal obturation
Densityofrootcanal obturation
Taperofrootcanal obturation
Intra-appointmentpain andswelling
Questionable(Forevery 1mmshortfromtheapical terminus – prognosis changesfromquestionable topoor)
Questionable
Inabilitytoremove fillingmaterialNon-SalvageablePoor
AdequatepreservationofPCD withUCACorCACforms
CACpreparationsneedingsome removaloftoothstructure, adequatecoronalresidualwalls
TACneedinggreaterremovalof toothstructure,adequate coronalresidualwalls
TACneedinggreaterremovalof toothstructure,compromised coronalresidualwalls
Root fillingextending0 -<1mmshortofradiographic apex
Root fillingsending attheradiographicapex (or1–2mmshort)
Root fillingswithbiomimetic sealersendingbeyondthe radiographicapex(overfilling)
Root fillingswithtraditionalsealers endingbeyondtheradiographic apex(overfilling)
Root fillingending>2mmshortof radiographicapex(underfilling)
Novoidpresentintherootcanal obturation
GoodGood
Fair
Questionable
CompromisedPoor
GoodGood
Fair
FairGood
Questionable
CompromisedPoor
GoodGood
Void(s)limitedtocoronalthirdFair
Withvoid(s)withinthe mid/apicalthird CompromisedPoor
Consistentlytaperedfromcoronal parttoapex
GoodGood
InadequatetaperFair
Inconsistentorirregulartaper (overorundershaped)
Asymptomaticbetween appointments(no flareups)
CompromisedPoor
GoodGood
Symptomaticbetween appointments( flareups) Fair
(CourtesyofEachempatiP,HarrisA,LambournG,etal:Toptipsfortreatmentplanning:Tooth-by-toothprognosis – Part3:Endodonticprognosis. BrDentJ 237:686-690,2024.)
CoronalSealandPost-endodonticRestorations
Teethwhoserootcanalshavebeenthoroughlydisinfectedcan developcoronalleakage,leadingtoendodonticfailure.Bacterial penetrationcannotbeguaranteedforanextendedduration; insteadtherestorationisdesignedtoprovidethelong-term integrityofthecoronalseal.Oncetheaccesscavityisrestored, theteethareoftengivenfull-coveragecrownsforoptimal
structuralsupportandprotection.Therestorationsprotect againstmicroleakage,defendagainstfracturefromocclusal forces,andprovidecontactsandcontoursthatsupportahealthy attachmentaroundthetreatedtooth.
Theneedforcuspalcoverageisdeterminedforeachindividualtooth. Factorstoconsiderincludetheremainingtoothstructure,any
StageCategoryParameterstoconsiderPrognosis
Post-operativeCoronalseal&post endodonticrestoration
Adequatecoronalrestoration:Awellbonded coronallysealingrestorationwhichappearsintact radiographically
Inadequatecoronalrestoration:Finalrestoration appearssub-optimalradiographicallywithopen marginsorpositivemargins
Inadequatecoronalrestoration:recurrentcaries, partialtemporary fillingsorno filling.
TimingofcuspalcoverageRestoredwithdirectorindirectdefinitiverestoration withnoorminimaldelay
Good
Questionable
CompromisedPoor
GoodGood
Restoredwithdirectorindirectdefinitiverestoration withdelayoflessthanfourmonths Fair
Restoredwithdirectorindirectdefinitiverestoration withdelayofgreaterthanfourmonths
Teethreceivingnodefinitivecuspalcoverage restoration
OcclusionCanineguidancewithnolateralexcursivecontacts onthetooth
Questionable
CompromisedPoor
GoodGood
Groupfunctionwithsmoothlateralexcursive contactsdistributedonallteeth Fair
Anyocclusalschemewitheccentriccontacts/ heavylateralloadingonthetooth
CompromisedPoor
(CourtesyofEachempatiP,HarrisA,LambournG,etal:Toptipsfortreatmentplanning:Tooth-by-toothprognosis – Part3:Endodonticprognosis. Br DentJ 237:686-690,2024.)
cracks,andtheopposingdentition.Mostposteriorteethwithatleast 1missingproximalwallwillneed cuspalcoveragerestorations.
Biomimeticdentistryisfocusedonpreservingtoothstructure andreplicatingnaturalbiomechanicswithminimallyinvasive preparationsandselectivecariesremoval.Modernadhesives andstress-reducedcavitypreparationminimizetheconfiguration factorandreducestressindentalcompositerestorations.The dentistshouldbecomefamiliarwiththebiomimeticdentistry principlesandchooseminimallyinvasivetechniquesandselective cariesremovaltoenhancelong-termsuccess.
Theapproachtorestoringendodonticallytreatedteethwill dependonfactorssuchasremainingwallvolumeandaccess cavitypreparation.Thetreatmentplanshouldbecustomized toeachpatient’sneedsandcircumstances.Anteriorteeth bene fitfromdirectcompositerestorationsifthemarginal ridgesareintact.Heavilyrestoredteethmayneedadirect compositeoranindirectrestoration.Posteriorteethcanbe restoredusingdirectcompositeifthemarginalridgesare intact.Heavilyrestoredteethinposteriorareasmaybe managedbestwithdirectcompositewithreinforcedultrahighmolecularweightpolyethylene fiber,withthepossible useofanindirectrestorationorcrownplacement.Ifaposteriortoothwascrownedpreviouslyandnowhaslostmarginal ridges,thebestchoicemaybeareinforcedcorewithaconventionalpost,areinforcedultra-highmolecularweightpolyethylene fiberpost,oranendocrown.
Teethwithrestorationsmademorethan4monthsaftertheendodontictherapyarenearly3timesmorelikelytobeextracted thanthoserestoredwithinthat4-monthperiod.Anotherspike infailureoccurs18monthsaftertreatment,suggestingthere maybeacriticalperiodforfracturedevelopment.
Ahighersurvivalisnotedforteethrestoredwithindirectrestorationswithin6monthsofendodontictherapycomparedtothat forthoserestoredwithdirect fillings.It’spossiblethatteethwith amorefavorableprognosisarerestoredwiththeindirectrestorations.Root- filledteethwithoutcrownshaveasatisfactorysurvivalrateforupto3years,butdeterioratethereafter.The outcomesafter5yearsforteethrestoredwithdirectandindirect restorationshavebeencomparable,butafter10years,those withindirectrestorationshavebetteroutcomes.
Dentalpractitionersshouldevaluatetheneedforcuspal coveragerestorationsduringfollow-upappointments,especially whentherestorationwasdelayed.Thiscanavoidcomplications andensurethebestoutcome.Patientsshouldbeeducatedabout theimportanceofatimelyrestorationafterrootcanaltreatment. Complyingwithrecommendedtreatmenttimelineswillimprove outcomesandlong-termsurvivalofthetooth.
Theprognosisofendodonticallytreatedteethappearstobe significantlyconnectedtotheocclusion,althoughevidence
forthisislacking.Properocclusionensuresevendistribution offorcesacrossthedentalarch,whichreducestheriskfor excessivestressonindividualteeth,whichwouldincludethose managedendodontically.Occlusalforcescanalterthe longevityofarestorationplacedonatoothwitharootcanal. Stabilityanddurabilityofrestorationscoupledwithalower riskoffailureaccompanyproperlydistributedocclusalforces.
Whenit’sdesirabletoavoidlateralforcesoncompromisedposteriorteeth,canineguidanceispreferredbecauseitdirects forcesawayfromtheseteeth.Groupfunctionisbestwhenthe goalistodistributeforcesacrossmultipleteeth.
Preoperative,intra-operative,andpostoperativefactorsinfluencetheprognosisofendodonticallytreated teeth.Toensurethebestoutcome,theclinicianshould conductpatient-speci ficassessmentsandtailorthe treatmentplantothatspecificpatient.Usingadvanced diagnostictoolsandfollowingevidence-basedpracticeswillenhancetheprognosisfortheserestorations andensurebetterlevelsofpatientsatisfaction. Communicationwithpatientsabouttheprognosisis essentialinfosteringinformeddecision-makingand obtainingtheoptimaloralhealthoutcomes.
EachempatiP,HarrisA,LambournG,etal:Toptipsfortreatmentplanning:Tooth-by-toothprognosis – Part3:Endodontic prognosis. BrDentJ 237:686-690,2024
Reprintsnotavailable
Aesthetictreatmentsofthefaceaffectnotjustthepatient’sphysicalappearance,butalsohisorherpsychologicalandsocialwellbeing.Thesetreatmentsincludedermal fillersandbotulinum toxin(BoNT-A)injections,whichareespeciallypowerfulboth aestheticallyandtherapeutically.Oralhealthproviders(OHPs) aretrainedasexpertsinheadandneckanatomy,musthave manualdexteritytoperformtheiroralhealthcarewell,andprioritizepatienthealthandsafety,makingreferraltospecialistsas needed.Thistrainingandtheseskillspositionthemtoaddsafe, expertlydeliveredfacialaesthetictreatments.Ontheoralhealth side,theycanmanageconditionssuchasbruxism,TMJdisorders, trigeminalneuralgia,sialorrhea,orofacialpain,andfacialasymmetrycausedbyfacialparalysis.Theyworkinaregulatedclinical environment,candealwithpatientanxiety,andhavetheknowledgetomanagemedicalemergenciesthatmightarise.Areview waspresentedtoidentifythetrainingandexpertiserequiredto deliverfacialaesthetictreatments,theethicalresponsibilityassociatedwiththesetreatments,andtheprioritizationofpatient safety.
Specializedtrainingandexpertisearerequiredinseveralareas tobequalifiedtopracticefacialaesthetics.OHPsmustbe
trainedincomprehensiveanatomicalknowledgeoftherelevantanatomyaswellaspossiblevariations.Theymustdevelop anabilitytoaccuratelyevaluatefacialfeaturesandpatientspeci ficalternatives.Clearunderstandingoffacialproportions, symmetry,andharmonyisneeded,alongwithknowledgeof aestheticunitsandhowtheyinteracttocreatenaturaloutcomes.TheOHPmustdevelopandapplyanaestheticsensibilitytorespectethnic,cultural,anduniquedifferencesforeach patient.
TreatmentplanningdependsontheOHP’sskillinvarioustreatmentmodalitiesandhisorherunderstandingofhowtheycanbe safelyusedincomplementaryroles.Relevantpharmacologyand physiologyshouldberecognizedandaccommodated.TheOHP mustalsobeawareofpossiblecomplicationsandalertthepatient beforebeginningtreatment.Pathwaystorecognizeproblems earlyandavoidormanageanyadverseeventsshouldbe established.
Patientsshouldbescreenedforpsychologicalin fluencesontheir requestforfacialaestheticprocedures.Thisincludestherecognitionofmentalhealthissuessuchasbodydysmorphicdisorder. Areferralpathwayforhelpinmanagingtheseissuesshouldbeestablished.OHPsshouldmanagepatientexpectations,notinginfluencesfromsocialmediaorothersources.
Thespecializedtrainingspeci fictofacialaesthetictreatments includesafocusontechniques,modalities,andtechnologies thatwouldbeemployed.Thisknowledgeshouldbekeptcurrenttomaximizetheprobabilityofobtainingoptimalpatient outcomes.
OHPsmusteducatethepatientabouttheaesthetictreatments, withevidence-basedinformationregardingtherisksandrealistic outcomesthatrefutesandreplacesanysocialmedia baseddisinformation.Theymustalsomaintaincurrencyregardingthesafest andmosteffectiveapproaches.Patientwell-beingmustbeprioritizedovercommercialissues,soOHPsshouldbepreparedto refusetreatmentiftheyaretopracticeethically.
Referraltootherspecialistsshouldbeconsideredwhenthe requiredtreatmentexceedstheOHP’sskills,sothatthepatient receivesholistic,ethicalcare.Thepatient’soverallhealthand long-termwell-beingshouldbeprioritized.
Intheabsenceofspecificregulationsorframeworksfor requiredtraining,theOHPshouldselectappropriateeducationalandskillstrainingfocusedonensuringpatientsafety. Althoughsomecomplicationscanbemild,theOHPshouldalwaysrecognizeseriousproblemsthatrequireimmediateresponses.ThisalsorequirestheOHPtostaycurrentwith
thebestevidence-basedinformationregardingtherisksof aestheticproceduressoheorshecantreatthepatientsafely. Inaddition,theOHPshouldconductthoroughconsultations withthepatienttoensurethathisorherhealthstatusand aestheticgoalsareappropriateforthedesiredtreatment. Basedontheseconsultations,theOHPshouldbeableto recognizewhenapatientisn’tanidealcandidate.
OHPshaveanopportunitytoexpandtheirclinical practicebymovingintofacialaesthetics.Theyare alreadytrainedinmanyoftheessentialareasand skilledinmanualdexterity.Withadvancedtraining, theyshouldbeabletomanagepatients’ psychosocial factorsandcommittoethicalpracticeinfacialaesthetics.Thiscareshouldbebalancedwiththepatient’slong-termhealthtoachieveexcellenceinthe outcomes.
SamizadehS:Theroleoforalhealthcareprofessionalsinfacial aesthetics:Acriticalexaminationoftraining,safety,ethicsand psychosocialimpact. BrDentJ 237:787-788,2024
Reprintsnotavailable
Addingfacialaesthetictreatmentstotheproceduresdonebya generaldentalpractitionercannotonlyprovidevarietybut alsodiversifypatientcareandaddanadditionalrevenuestream. Concernshavearisenbecauseofthelackofregulationoffacial aesthetictreatmentinpartoroverall.Dentalpractitionersand theirstaffwhoprovidethesetreatmentsshouldadheretoprinciplesinvolvingsafety,regulations,andethics.
Patientscanlegallyreceiveaesthetictreatmentfrompersonswho lackanymedicaltrainingorexperience.Dentalpractitionerswho choosetoperformtheseproceduresshouldensuretheyaredone safelyandresponsibly.Coursesareavailabletomembersofthe dentalteam,includingdentists,dentaltherapists,anddentalhygienists,andtheinstructioncanvaryinlengthoftimespent,cost,and content.Qualifyingtoperformtheproceduresdoesn’tguarantee competency.Dentalpractitionerswhowanttoperformaesthetic
proceduresshouldcarefullyevaluatetheirowncompetencyand seektrainingintheseproceduresasnecessary.
Facialaesthetictreatmentisn’tclassi fiedasdentaltreatment,but ifadentistprovidesit,theUKGeneralDentalCouncil(GDC)expectstheprovidertofollowtheirprofessionalstandards,which includesobtainingvalidinformedconsent.Ifthepatientisunawareoftherisksassociatedwithfacialaesthetictreatments, nothavingreceivedeffectiveexplanationsfromthedentalpractitioner,heorshecan’tprovidevalidconsent.Practitioners mustalsobeequippedandknowledgeableaboutthemanagement ofpotentialcomplicationsandmedicalemergencies.
Dentistsaretheonlydentalteammemberswhocanprescribe andadministerbotulinumtoxin,buttheGDCallowshygienists andtherapiststoadministeritiftheyhavebeentrainedandare
competentandindemnifiedtodoso.Whendentistsprescribe botulinumtoxin,theprescriptionshouldonlybegivenafterperformingafullassessmentofthepatientinpersonandnotvirtually.Fillertreatmentsareconsideredamedicaldeviceanddon’t fallundertheserestrictions.
TheGDCdoesn’tcommentonwhetheradentalnursecanoffer treatmentswithbotulinumtoxin.ThissuggeststhatGDCregisterednursesshouldnotdothis.
Dentistswhoofferbotulinumtoxintreatmentsshouldknowthe AdvertisingStandardAgency’s(ASA’s)rulesbeforetheypromotethisaction.Brandnamesmustnotbeadvertised,norcan thetreatmentbereferredtousingeuphemismssuchas ‘antiwrinkleinjections. ’ Thepostingofbefore-and-afterphotosonsocialmedia,beingtaggedinpatients’ photos,andpromotingthe medication’sbene fitsarealsoforbidden.
Dentalpractitionersshouldfollowtheguidancetodono harm,putthepatient’sinterests first(beforepersonalgain), andworkwithintheirknowledge,skills,professionaltraining, andabilities.Inaddition,theASA findsitunacceptableto
exploitpatients’ insecuritiesortoperpetuateharmfulgender stereotypes.
It’sinevitablethatregulationswillincreaseandlegal challengesfrompatientswillbecomemorecommon. Thesechallengesmayincludequestioningthetreatmentprovidedbydentalteammemberswhoaren’t trainedtoevaluatepatients’ mentalhealthstatus, whichisanimportantcomponentofaesthetictreatmentmanagement.Asaresult,dentalpractitioners shouldchoosepatientswithcare,remaincurrent withtherulesandregulationsthatareappliedto aesthetictreatment,workwithintheirlevelofcompetence,andmakesuretheyareproperlyindemni fied.
ThakrarB:Facialaesthetics – friendorfoe? BrDentJ 237:789-790, 2024
Reprintsnotavailable
Dentistsarewelltrainedinfacialanatomy,whichcanbean importantfoundationforperformingfacialaestheticprocedures preciselyandsafely.Alookatthenonsurgicalfacialaesthetic (NSFA)procedures(suchasinjectionsor fillers)andwhatis involvedwhentheseproceduresaredonebydentalpractitioners notedpossibleuses,regulations,andsafetyandethicalconcerns.
Althoughperhapsconsideredjustamedicaltechnique,NSFA methods,especiallythoseusingbotulinumtoxin(BoNTA)injections,havemanyusesfororofacialconditions.Theseinclude bruxism,TMJdisorders,chronicmigraine,andsialorrhea.BoNTA’seffectonmoodhasthepotentialtohelppatientswith depression.
Dermal fillersusedtoaugmentlipsandcheekscanalsobeapplied therapeuticallytomanagefacialasymmetryortrauma,provide contoursforstructureswheresurgeryiscontraindicated,and evenaccomplishwholefacevolumeregenerationafterfatatrophy,whichwastheinitialuseofsemi-resolvable fillersinHIVpatients.Othertreatmentsincludeplatelet-richplasmatherapy, whichisusefulmedicallyforwoundhealingandtissueregeneration,butalsohasaroleindentalimplantology.
Concernsoverpatientsafetyhaveledtosignificantchangesinthe regulationofNSFApractice.Withadesireforprofessional accountability,regulatorsarenowregisteredwiththeprofessionalstandardsauthority.TheJointCouncilforCosmeticPractitioners(JCCP)hasestablishedguidelinesandlimitationsthat ensureaestheticproceduresaredonebyappropriatelytrained andqualifi edpractitioners.Theseregulationsaredesignedto addresstherisksthatpatientsfacewhenpoorlytrainedandunregulatedpersonsperformtheseproceduresandmarketaestheticsonsocialmedia.
Avoluntaryregisterhasbeendevelopedtoserveasabenchmark forsafe,ethicalpractice.Formalqualificationsandtrainingare spelledout,withanemphasisoncontinuingpersonaldevelopmentandclinicalcompetency.Theregulationshavehighlighted theneedforstructured,rigoroustrainingprogramsineducationalsettingsthatfollowthestandardssetbytheJCCP.
Prescribingaestheticinjections,whichhasbeendonebydental careprofessionals(DCP),referringtodentalhygienistsandtherapists,maybefurtherrestricted.Itmaynotbepossibletoindependentlyaccessoradministerprescription-onlymedications. DCPscouldonlyofferaestheticserviceswhenclosely
collaboratingwithaprescriber,whichwouldbeadentist,doctor, ornursewithprescribingrights.Aformalconsultationbetween patientandprescriberisrequiredbeforeprescription-onlymedicinesareadministered.BecauseDCPscontinuetobeinterested inNSFA,trainingprogramsintheaestheticproceduresthat don’t’ requireaprescriptionareavailable.
Withthenationalinitiativetoestablishenforceablestandards, dentalpractitionersshouldbecarefultoevaluatepatients’ motivationsandhealthstatus,assesstheirunderstandingofpossiblecomplications,andcommunicaterealisticexpectations.Oftenthe socialmediapoststoutthetalentsofunregulatedand/orinadequatelytrainedproviders,shapingpatients’ expectationsthataren’t realistic.Dentalpractitionersshouldcountertheconsumer-driven desireforfacialaestheticswithprofessionalaccountabilityandan ethicalapproach,educatingpatientsonthelimitsoftheseproceduresandtheriskstheyface.Thepractitionermayevenrecommendthatthepatientnothavetheseinterventions.
ClinicalSignificance
Takingonfacialaestheticsasanadditionalofferingin thedentalofficerequiresskillandanatomicalknowledgebutalsoafocusonprotectingthepatientagainst misinformationfromthemedia,unrealisticexpectations,andunqualifiedpractitioners.Byholdingtothe standardsofsafetyandethicalbehavior,dentists maintaintheintegrityandsafetyoffacialaesthetics treatments.
StagnellS:Trainingandclinicalbene fits. BrDentJ 237:791-792, 2024
Reprintsnotavailable
Intraoralscanners(IOSs)canacquireintraoralopticalimpressions(IOIs)andrepresentdataasdetailedvirtualmodels.AdvancesinthehardwareandsoftwareofIOSshaveimproved efficiencyandaccuracyincomputer-aideddesignand computer-aidedmanufacturing(CAD-CAM),themostcommon useforthesetools.Whenimagingmethodsarecombinedwith IOSs,theyfacilitateoutcomesindiagnostics,treatmentplanning, andmonitoring(Figure1).Futuredevelopmentsmayleadto additionalapplicationsindentistryoverallaswellasoraland maxillofacialsurgeryspecialties.AdvancesinIOShardwareand software,diagnosticapplications,integrationintoclinicalsettings, andspecializedandemergingapplicationswerediscussed.
IOSmanufacturersaretheprimarydriversintheinnovationsof IOSsusedinpatientcare.Theseincludedevelopmentsinhardwareaswellassoftware.
Keyadvancesincludefasterscanning,noneedforscanningpowder,andbettercolorimageacquisition,allofwhichcanenhance efficiency,patientcomfort,andtheuserexperience.Thecore designisessentiallythesame,butuniqueergonomicfeatures differentiatethevariousmodels.Newdevicesmaybewireless andbattery-poweredsotheyaremoremobileandconvenient,
butthiscanreduceoperationaltimeandmaycompromiseconnectivity.Hapticfeedbackcanofferguidanceduringimageacquisition.Heatersarenowintegratedtomitigatecondensation duringextendeduse.AlthoughIOSscanbestandalonedevices, chairsidefabricationwhentheyarepartofanintegratedCADCAMplatform.SomeIOSdevicesofferautocalibration,reducing theneedforfrequentmanualcalibration.Adryoperating fieldis requiredtoavoiderrors.IOSshavedif ficultycapturingsubgingivalpreparationmargins.
Continuousimagecaptureisavailablethroughadvancedalgorithmsstitchingimagesseamlesslytooptimizescanning.IOSs cansimultaneouslycaptureandprocessthesurfacefeaturesand opticalinteractionsinaspecifiedareabyusingoversamplingand averagingmultiplemeasurementspoints.SomeIOSsaredesigned toscanandexportdata,whereasothersarecomprehensiveplatformsthatdelivermorethanintraoralopticalimpressions.Dental professionalscanaccessenhanceddiagnostics,patientcommunication,monitoring,andtreatmentplanning,andsoftwareapplicationscanbetailoredtothedesiredtasks.IOSscanminimizenoise andimageartifacts,omitunneededimagingdata,andexclude extraneouselementsfromtheimpressions.
TheformerclosedsystemsthatrestrictedCAD-CAMtoproprietarysolutionshaveevolvedintoopeninterfaceswhereimpressiondatacanbeexportedinatleast1standard fileformat,users
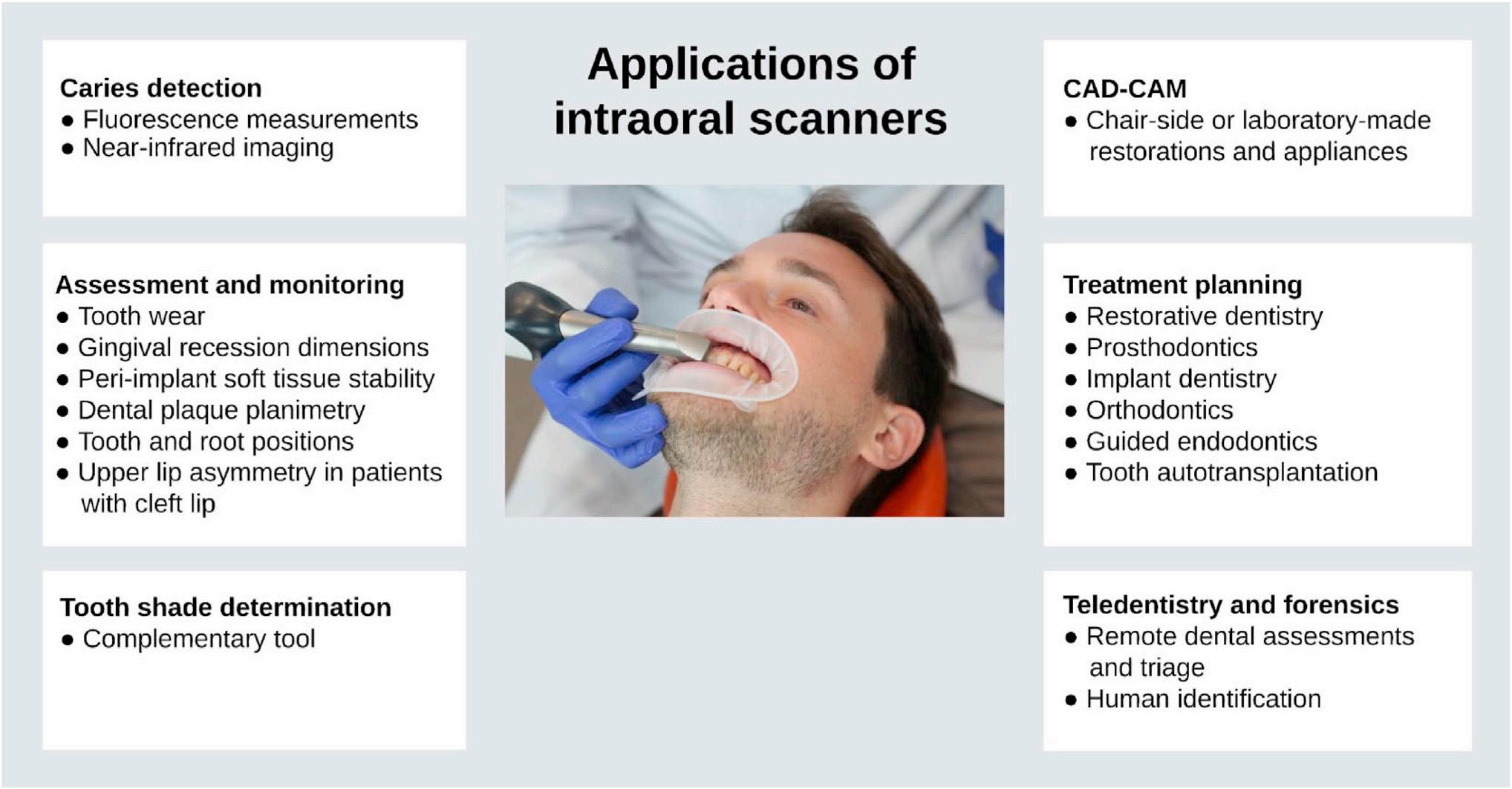
Figure1. Schematicdiagramwithanoverviewofthediverseapplicationsofcontemporaryintraoralscanners(IOSs).(CourtesyofEggmannF,BlatzMB: Recentadvancesinintraoralscanners. JDentRes 103:1349-1357,2024.)
havegreater flexibility,interoperabilityincreases,andcustomizationisenhanced.Datacanbestoredinseveral fileformats,with advantagesanddisadvantagesvaryingwiththeformat.
Thesoftwarecanperformin-depthanalysis,permittingprecise segmentationofeachindividualtoothfromtheimpression dataforuseindiagnosisandtreatmentplanningfororthodontics,orthognathicsurgery,andprosthodontics.Operatorscan performspaceanalysis,treatmentsimulation,movementprediction,andtoothshapeanalysis.Becausepatientconditions varysignificantly,boundarydetectionbetweenteethand gingivawilldiffer.Precisionisneededforreliablesegmentation outputs,soautomatictoothsegmentationcanbechallenging. Specializedtrainingisrequiredtouseafullyautomated, fault-awaresystembasedondeeplearning.Deepneuralnetworkswithunsupervisedpretrainingandsupervised finetuningcanachieveprecisetoothsegmentationinimpressions. Thisreducestherelianceonextensivelabeledtrainingdata andwillstreamlinetoothsegmentationprocessesandimprove diagnostictechnologies.
Manuallyplacedlandmarksondentalmodelsserveanessential purposefordiagnosticandoutcomeassessmentsinorthodontics.However,theprocessispronetoerrorsandistimeconsuming.Newsoftwarecombinesmachinelearningandlinear programmingtoautomaticallyrecognizeandlabeleachtoothand itslandmarks.Humanveri ficationisstillrequired,butidenti ficationismorepreciseandrapid.However,automateddigitalmodel analysescandifferfrommanualones,soprecisionmaystill requiremanualmethods.
Anotheradvanceisleadingtowardautomatedsystemsthatproducedentalchargesdirectlyfromimpressions.Thesoftwareis underpinnedbydeeplearning,makingitabletocategorizemolars accordingtothepresenceandtypeofrestorationpresent.
IOSscanperformusefultasksincariesdetection,toothwear monitoring,oralhygieneassessment,softtissueevaluation,and toothshadedetermination.
IOSsfordetectingcariesarebasedoneither fluorescencetechnologiesusinglightwithawavelengthof415nmornear-infrared imaging,whichuseslightwavelengthsbetween727and850nm. IOSscandetectproximal,occlusal,orbothcariouslesions.The diagnosticaccuracyachievedwith fluorescenceiscomparableto thatwithvisualexaminations,butfalse-positiveresultscanoccur ifbio filmispresentonocclusalsurfaces.Assessmentsofnearinfraredscanshavehigherdiagnosticaccuracywhendonebyexpertscomparedtonovices,showingthelearningcurveneededto optimizebene fits.Thediagnosticaccuracyofnear-infraredimagingIOSremainsequivocal.OptimizedIOSscanbevaluableadjunctsincariesdetectionandmayproducemorereliable assessments.RadiationexposureisreducedwithIOSscompared toothermethods.
Imagesuperimpositionsoftwarebasedonbest-fitalignmentallowsquantitativeassessmentofsurfacechanges.However,the
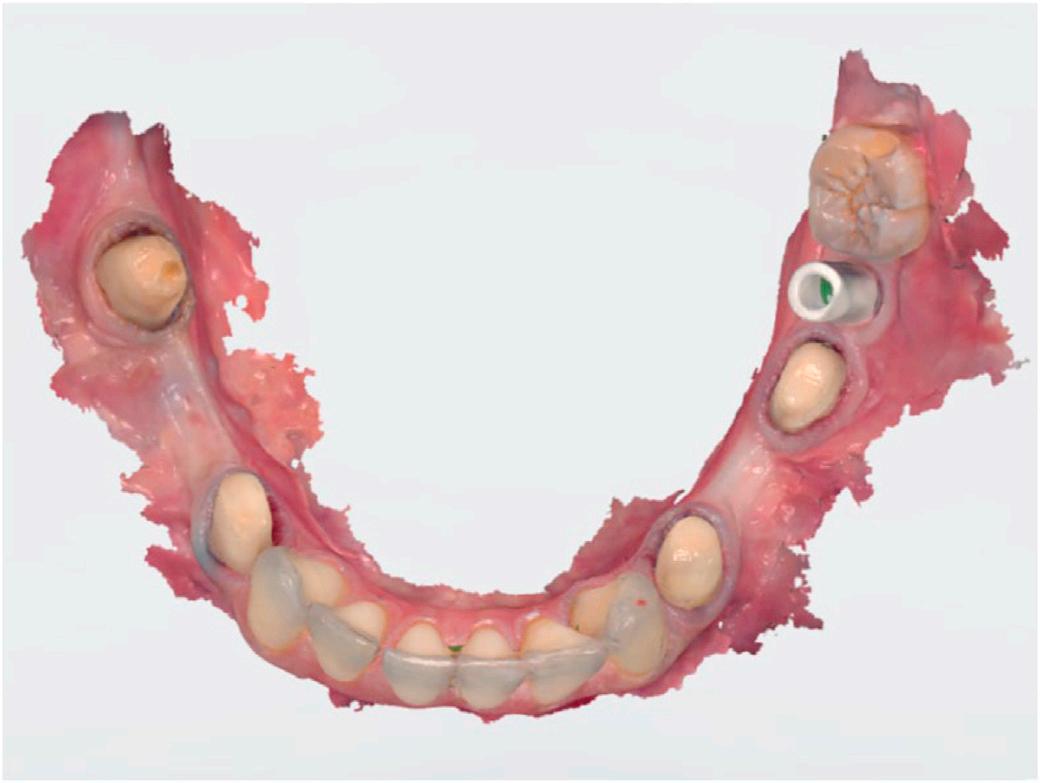
Figure2. Intraoralopticalimpressionofamandibulararchwithprepared teethandanimplantholdingascanbody.(CourtesyofEggmannF,Blatz MB:Recentadvancesinintraoralscanners. JDentRes 103:1349-1357, 2024.)
lackofstableoralreferencepointsmakesthisapproachproneto inaccuracies.AlthoughIOSscan’tpreciselydetectminutelevels ofwear,theycandetectandtrackchangesthatsurpassspeci fied thresholds.
Planimetricmethodstoquantifydentalplaquecoverageprovidea detailedlookattheindividual’soralhygienestatus.Periodontal andplaqueparametershavebeenevaluatedusingasmartphone athomeafternonsurgicaltreatment.Thepatientsreceivedautomatedmotivationalmessagesbasedonmachine learning supportedevaluationsofvisiblesupragingivalplaque andgingivalinflammation.Thisapproachmayallowpatientsto sendintraoralimagesviasmartphonesforpersonalizedoral healthcounseling.
Increasingly,IOSsareusedtoevaluategingivalrecessionand peri-implantsofttissuestabilityandtomonitorsofttissue changes.ClinicalandlaboratorystudiesshowIOSassessments aremoreaccuratethanconventionaltechniques,butprecision dependsontheoperator’sskill,thedeviceused,andthescan location.
IOSswithcolorimagingcanbeusedtodeterminetoothshade, theaccuracyofshadematchinghasbeenquestioned.IOSswith colormatchingtoolscanonlyprovidequalitativecolordata becausetheycan’tmaintainuniformilluminationandcandeviate fromtheoptimalangleforcolorreadings,makingthemmoreofa supplementarytool.

Figure3. Digitaldesignofmonolithiccrownsformaxillarycentralincisors usinganintraoralscannerplatformthatincludescopy-and-mirrortoolsto optimizethedesignprocessandagridoverlaytoassistinprecisealignmentandproportionassessment.(CourtesyofEggmannF,BlatzMB: Recentadvancesinintraoralscanners. JDentRes 103:1349-1357,2024.)
AlthoughIOStechnologiesusedfordiagnosisaren’tyetbecome routinelyaccepted,theycancontributesignificantlybyeliminatingsomeofthediscomfortconventionalimpressiontaking causes.Thisraisespatientsatisfactionlevels.Thepredominate usesforIOSsisinfabricatingsingle-unitrestorations.Costis theprimarybarriertotheiruse,withbetterclinicalef ficiency themostcommonreasonforadoption.Largedentalinstitutions canhavedifficultyintegratingIOSsoftwarewithcurrentelectronichealthrecordsystems,ensuringdatasecurity,managing datastorage,andtrainingcliniciansandstaff.
TruenessandprecisionarethemeasuresofreliabilityandaccuracyinIOSs. Trueness isthedegreeofclosenessofintraoralopticalimpressions(IOIs)totheoriginalobject. Precision refersto theconsistencyofrepeatedscans.AlthoughIOSaccuracyhas improved,thelatestIOSsaren’tknownforthehighestaccuracy, withparticulardif ficultyinedentulousareas.Onlypreliminary stageimpressionswithIOSareadvisablewhencompletedenture fabricationortissuemovementcaptureisdone.
Augmentedaccuracyisneededforapassive fitofimplantsupportedrestorations.WhileIOSsofferacceptableaccuracy forsingleormultipleimplants,theyhavelimitedefficacyfor full-archimpressions(Figure2).Horizontallypositionedscan gaugeshelpwithaccuracy.
Whenusedforcrowns,marginalaccuracyisacceptableandcomparablebetweenIOSandconventionalimpressions(Figure3). Theclinicaloutcomesofimpressionsfor fixedprostheses, whethertooth-supportedorimplant-supported,arealsocomparablebetweenthe2approaches,butsubstantialvariationsinaccuracyarefoundbetweendifferentIOStechnologiesand differentgenerationsofaspeci ficIOS.
AccurateIOSsarecriticaltocomprehensivetreatment-planning platforms.Precise “digitaltwins” canbecreated,whichare3-dimentional(3D)modelsthatprovideaccurateanatomicaldetails andspecialrelationships.Proceduresthatusethemincludeorthodonticmini-implantplacement,endodonticaccesscavity preparation,insertionofdentalimplants,andtooth autotransplantation.
Prosthodontics,orthodontics,oralandmaxillofacialsurgery,teledentistry,andforensicdentistryofferopportunitiesforIOSuse. In prosthodontics, maxillomandibularrelationshipsrequireaccuracy,yetpresentcomplexitiesinachievingthisgoal.Polyvinyl siloxanehasbeenusedforfull-archscanningandphysicalbite recording,butscanningthebuccalsurfacesofaquadrantwith teethinmaximumintercuspalpositionwasmoreaccuratein staticinterocclusalregistration.Digitalbiteregistrationischallengingformultispanimplantrestorations.Digitalscanscan contributetodynamicmandibularmovementanalysis,butminor inaccuraciesinmeshalignmentpersist,causingintercuspalrelationshipstodeviatesignificantly.
Photogrammetrycaptureshigh-resolutionphotographsfrom variousanglesofimplantsandusesscrew-retained fiducial markersforreference.Advancedsoftwareallowstheidentificationofcommonpointsacrossphotographs,soaccurate3D modelsofdentalimplantpositionscanbecreated.Anadditional impressionusingIOIorconventionalmethodscapturesadjacent structures,butsupportfortheaccuracyofphotogrammetryin implantscansremainslimited.
In orthodontics, orthodonticalignerdevelopmentusesIOIsand virtualtreatmentplanning,butdiscrepanciesbetweenthedigital andconventionalmethodshavebeennoted.Inaddition,orthodonticsoftenrequiresfull-archscanswithcrowdedteethandappliances,afurtherchallengefordigitalapproaches.IOSshavethe advantageofnotrequiringbracketsandarchwirestobe removed.Rootpositionmayalsobecapturedfromdetailed3D toothmodelscreatedfromIOSs.
In oralandmaxillofacialsurgery,IOSshavebeenusedforpatients ofallages,whetherawakeorundergeneralanesthesia,indiagnostics,treatmentplanning,andorthopedicappliancefabrication.
AirwaysafetyisimprovedduringimpressiontakingwithIOSs, whichcanalsofabricateappliancesforinfantsandspeechenhancingobturatorprosthesesinchildrenwithcleftlipandpalatedeformities.IOSsaremoreaccessibleandlessexpensivethan extraoralfacialscanners,somoreinnovativedigitalsolutionsand costreductionsmaybeachieved.Somedefectsare,however, beyondtheabilitiesofIOSs.
Teledentistry canbene fitfromdatasharingthroughIOSsand enableremoteassessments.Approximatetrue-colorIOIscan helptodetectdentalsituations,butperiodontalconditionresults remaininconsistent.Addingbetterimagequalityandintegrating theIOSwithadditionalpatientdatafromradiographs,for example,couldmaketheIOSsmoreefficientforscreeningpatientsandperformingtriage.
Forensicdentistry canbene fitfromthespeedofIOSimaging.The identi ficationprocessmaybere finedifpreexistingimagingdata arealsoavailable.
IOSsremainextremelyeffectiveforCAD-CAMintegrationtofabricateindirectrestorationsandorthodontics toaidintreatmentplanning.Theycanalsobeintegratedwithvariousimagingmodalities,afacilitythat helpswhenpersonalizingtreatment.Challenges remainwithrespecttoadoptionbylargedentalinstitutions,accuracywhenscanningedentulousareasand implantsincasesoffull-archedentulism,andthe needforbetterdiagnosticaccuracy.Futureusescould evolveintheareasofprosthodontics,orthodontics, oralandmaxillofacialsurgery,teledentistry,and forensicdentistry.
EggmannF,BlatzMB:Recentadvancesinintraoralscanners. J DentRes 103:1349-1357,2024
Reprintsavailablefrom FEggmann,DeptofPeriodontology,Endodontology,andCariology,UnivCtrforDentalMedicineBasel UZB,UnivofBasel,Mattenstrasse40,CH-4058,Basel, Switzerland;e-mail: florin.eggmann@unibas.ch
Manydentalpractitionerscheckpatientsformouthcancer,but lipcancercanbeoverlooked.Theincidenceoflipcancerisfairly low,butthedentalteamshouldbeabletorecognizehealthylip tissuesandwhatisnormalforeachpatientaswellaswhatis abnormal.Oftenpatientsdon’thavesymptomsorconcern overaesthetics,buthaveaproblemthatrequiresreferral.The componentsofevaluatingpatientsforlipcancer,includingrisk factors,examination,andcommonsignsandsymptoms,and thetreatmentoflesionswerepresented,plusacasestudyto illustrateanactualpatient’ssituation.
Whentakingthepatient ’ smedicalhistory,potentialrisk factorsforlipcancershouldbediscussed.Theseinclude tobaccoandheavyalcoholuse,excessivesunexposure,actinic cheilitis,humanpapillomavirus(HPV),herpesvirusinfection (coldsores),andaweaken edimmunesystem.Thesun exposureleadstoabout90%oflowerlipcancers,withthe upperlipangleddownwardandprotectedbythenose.The exposureincludestheuseofarti fi ciallightfromsunbedsas wellasthesunitself.Menoverage40yearswithfairskin areatspecialrisk.
Mostlipcancersbeginassquamouscellcarcinoma(SCC)andare firstseeninthin, flatcellsinthemiddleandouterlayersofthe oralmucosaandskin.Lipcancersthataremelanomaaremore dangerousanddevelopinthelip’smelanocytes.Usuallythecancersarisefromthevermillionborder,spreadinglaterallytothe adjacentskinorbydeepextensionintotheunderlyingmuscles ofthemouth.Melanomasspreadquickly,sotheearlierthey aredetected,thebetter.Liplesionsareeasilydetectedandassessedvisually.Basalcellcarcinomaisamalignancycommon foundinupperlipareas.
Examination
Thedentalpractitionershouldbefamiliarwiththeanatomyand physiologyoftheupperandlowerlips,knowhowtoexamine them,andtakepropernotes.Severalorganizationsoffereducationalonlineresourcesthatcanguidepractitionersintofamiliaritywiththisregion.
Theexaminationshouldbeginwiththefacialskinaroundthelips, thevermillionandvermillionborder,andthecornersofthe mouth.Pullingbackthelipswiththe fingerstosteadythemucosa (gauzecanmakeitlessslippery)allowsthepractitionerto examinethenonkeratinized/wetmucosalsurfaceofthelipsand
thelabialsulcus/vestibule.Bothhandsshouldbeusedtofeel thelipsforswellingoramass.Thedentalpractitionershould thenrecordthelocation,size,shape,color,configuration,and consistencyofalllesionsandwhetherthereismucosalor gingivalbleedingorulcers.Thedentistshouldnoteanysores, lumps,blisters,patches,orulcersonthelipthatwon’theal; bleeding;painornumbness;andjawswelling.Thedentistshould alsoinstructpatientsinhowtoexaminetheirlipsandmouthat home.
Referralisoftenneededtoaspecialistwhowillperformproper therapy.Whenlipcancerisfound,surgeryisthemostcommon treatment.Smalllipcancersmayberemovedinaminorprocedurethathasminimalimpactonthepatient’sappearance.Larger lipcancerscanrequiremoreextensivetreatment.Suchinterventionsshouldbecarefullyplannedtopreservethepatient’sability toeatandspeaknormallyaswellasofferarestorationthatprovidesasatisfactorypostoperativeappearance.Radiotherapyor chemotherapymayberequired,butthelong-termsurvivalrate forlipcancerishigh.Newerapproachesincludeimmunotherapy, withresearchintoDNArepairandidentifyingmarkerstohelp withearlydetection.
Woman,75,wasafarmer’swifewhowasactiveinthecommunity andsawthedentistregularlyonayearlybasis.Atherregularvisit,a visiblelesionwasnotedonherlowerlip(Figure1).Extra-oralexaminationshowednofacialasymmetryorpalpablenodes.The lowerliphadevidenceofactinickeratosis,whichwasalight

Figure1. MrsJ,thepatientinCasestudy1.UsedwithpermissionfromDr RobertBate,BDS.(CourtesyofLoweA:Lookingoutforlipcancer. BDJ Team 11:464-469,2024.)
leukoplakiaofthevermillionandawhitishsheenovertheexternal lip.A10×10mmshallowulcerwasjustleftofthemidline.Itwas expressingkeratinasa flakyexophyticmassthatdetached,leaving agranularbasethatbledreadily.Themarginsofthelesionwere slightlyelevatedandhadacircumferentialwhitezone.
Thepatientexplainedthelesionwasahealingcoldsore,butithad beenpresentforseveralmonths,withsteadycrustingand occasionalbleeding.Lipbalmprovidedsoothingreliefsoshe couldfocusoncaringforherhusbandwhohadadvanced dementia.
Thedentalprofessionalreferredthepatienttothehospital, wherethelesionwasconfirmedtobeanearly-stage,superficial, well-differentiatedcarcinomaofthelip.
The findingsthatledtothediagnosisoflipcancerwereanonhealinglesiononsun-exposedskin,evidenceofsolarkeratosis, andamistakenviewthatitwasacoldsore.Thelesiononthelower lipwasjusttoonesideofmidlineandproducedkeratin.The
marginsshowedinfiltrationandraisededges.Coldsoresusually resolvein2weeks,sothislesionwasn’tjustacoldsore.Thelesion wouldlikelydevelopmoreadvancedfeaturessuchasaraised,exophyticulceratedmass,distortionandindurationofthelip,andpain.
Lipcancershavenotyetbeenclearlyidentifiedas mouthorskincancer.Exposuretosunlightisacausativefactorinmostcases,soit’swisetoweara broad-spectrumSPBlipbalmregardlessofone’s age,gender,orskintype.Preventioniskey,soprotectingthelipsfromultravioletlightisessential.
LoweA:Lookingoutforlipcancer. BDJTeam 11:464-469,2024
Reprintsnotavailable
Earlierdiagnosisandtailoredtreatmentplanscombinedwithan agingpopulationhaveledtomorecancersurvivorsindeveloped countries.Theadvancesincancertreatmentsarealsoassociated witheffectsonoralhealththatcanin fluenceoralhealthcaredelivery.Oralconditionsassociatedwithcanceranditstreatments, includingmucositis,infections,xerostomia,trismus,osteonecrosis,tastechanges,andulceration,canalterdentalcareoptions.In addition,cancerpatientsareathigherriskfordevelopingdental cariesandcanhavecompromisedoverallhealth.Theprimary caredentalteammayseethepatientbefore,during,oraftercancertreatment,andeachofthesestagespresentschallengesfor thedeliveryoforaltreatments(Table1).Thecurrentpractices andbeliefsaboutdeliveringprimarydentalcaretopatients whohaveorhavehadcancerwerediscussed.
The4onlinefocusgroupsincluded15dentalprofessionals(DPs). Sessionsrangedfrom44to75minutes(average59minutes).Ten themeswereidenti fi edandconcernsdiscussed.
Themostcommoncancersamongthepatientstreatedwere breastandprostatecancer,butotherssawhematologicalcancers suchaslymphoma,leukemia,andmyeloma.Patientswithhead andneckcancer,stomach,bowel,lung,andskincancerswere alsoseen,aswellassomereceivingpalliativecare.
DPsunderstoodthattheroleofallteammemberswastomanage andmaintaintheoralhealthofthepatients,whethertheywere pre-,mid-,orpost-cancertreatment.Dentistscitedthesuperior experienceofdentaltherapistswhoprovidedoralhygieneandinstructionstopatients.Becausethepatientswerebeingseenata veryemotionalperiodintheirlives,thedentalteamrecognized thattheyhadapastoralandsupportiveroleinadditiontoclinical care.OftenthepatientsandDPshadknowneachotherforalong timeandhadanestablishedrelationship.DPsalsorecognizedthe limitationstheyfacedwhendealingwithsomeoftheemotional andfunctionalissues,butwereclearthattheyhadaresponsibility tosignposttheirpatients.
Table1. StagesofCancerTreatmentandRelatedRolesofPrimaryDentalCareTeam
) Priortosurgical,systemicanticancertherapy
) orradiologicalintervention
) Duringsystemicanti-cancertherapyor radiologicalintervention
) Aftersurgical,systemicanti-cancertherapyor radiologicaltreatment
Providingpreventionandinformationabouttherisksofcancertreatmentonoralhealth. Eliminatinganyoralsourcesofinfectiontoavoidriskofsystemicspread(e.g.sepsis)
Eliminatinganyteethofparticularlypoorprognosisinanattempttoreducetheneedfor extractionsorminororalsurgeryinthefutureinsituationswherethepatientmaybeat riskof:
Medicationrelatedosteonecrosisofthejaw(MRONJ)
Osteoradionecrosis(ORN)
Addressingacuteproblemsincludingdentalpainandinfection.
Managementofdrymouthororalmucositis.
Managingoralmanifestationsofbacterial,fungalandviralinfectionsduetoincreased riskofinfection.
Considerationofincreasedbleedingandinfectionriskiftreatmentisbeingcarriedout. Ongoingprevention
Preventionofdentaldisease
Managingreducedmouthopening(trismusduetoeffectofradiotherapyonmuscles andothersofttissuescancauseproblemswithaccesstooralcavityforself-performed plaquecontrolandexecutingdentaltreatment)
Managementofdrymouthandassociatedoralsoreness.
ManagementofpatientsatriskofMRONJorORNwhoneeddentaltreatment. DiagnosisandreferralofpatientswithMRONJorORN.
Headandneckcancersurveillance-particularlyforpatientswhohavehadoralor oropharyngealcancer.
Considerationoflaryngectomiesortracheostomiesandanydietaryconsiderations. Maintenanceofprosthodonticrehabilitationsincludingimplantsupportedorretained prostheses.
(CourtesyofWemyssC,AbdulsalamA,BeatonL,etal:Experienceofprimarydentalcareteamsinmanagingtheoralhealthofoncologypatients. BMCOralHealth 24:1554,2024.)
Communication
MixedHealthCareMessages
DPsfeltmixedmessagesweregiventopatientsabouttheneed forcareduringcancertreatmentandtheimportanceoforal health.Someoncologyteamsadvisedpatientsnottoattend dentalappointmentsbeforeorduringtheirtreatments.Inaddition,oralhygieneadvicewasalsoinconsistent,withsomemedical teamstellingpatientstouseasofttoothbrush,whichisaninstructioncontestedbyDPs.
CommunicationBetweenDentalandMedicalTeams
Sometimescommunicationbetweenthedentalandmedical teamswaseffective,withoncologyanddentalteammembers supportiveofoneanother.Thistendedtovarybylocationand thedentalservicetheDPworkedin.Atothertimes,communicationdif ficultiesdeveloped,withtheoncologyteamadvisingpatientstohaveanoralhealthassessmentbeforecancertreatment, butnoformallinesofcommunicationexistingbetweenthe oncologyanddentalteams,socarewasn’twellintegrated.Sometimesthemedicalteamseemeddismissiveofanyconcernsover thepatient’soralhealth.Whenpatientsweren’tinformedabout theircareorwhenthemedicalteamdidn’tshareinformation, suchasthepatient’sprognosis,withthedentalteam,moreproblemsarose.
DealingwiththeExperience
Thephysicalandmentalexperiencesofpatientsandtheirquality oflifewhenoncarepathwayswereofconcernforDPs.Treatmentscausemanyphysicalproblemsforpatients.Thesitespeci ficsideeffectsoftreatmentforpatientswithheadand neckcancerwereespeciallydebilitatingandcarriedsigni ficant risks.Patientsandtheirfamiliesoftenbecameemotionalattheir dentalvisitsoverthingsthathadhappenedintheirmedicalvisits, orhadconcernstheyweren’tencouragedtoshareinothersettings.DPsdealtwithpatientswhohadgeneralhealthcareanxiety alongwithdentalanxietyandthementalstrainofdealingwith cancer.Sometimestheanxietywascausedbytheimmensevolumeofinformationpatientsaregivenastheygothroughtheir cancerjourneyandhowtheyfeltoverwhelmedasaresult.
Insomecases,patientswithcancerhadpoorpreexistingattitudes towardtheiroralhealth,andDPsquestionedwhetherpatients understoodtheimportanceoftheirdentalhealth.Manyfocus groupsnotedthatpatientshadtroubleunderstandingtheircancerdiagnosisandtreatment.Therewere,however,patients whoweretakingaproactiveapproachtotheirhealthcare, includingdentalcare.
Especiallyintheirpatients ’ pre-cancertreatmentstage,DPs facedchallengesintreatmentplanning.Thepre-cancertreatmentstagecanbechaoticandinvolveshorttimeperiods whenallnecessarydentaltreatmentmustbedonebefore cancertreatmentcanproceed.Poorpreexistingoralhealth wasachallengethatoftenrequiredcomplextreatment.Dependingonthecancertherapybeingprovided,theoralhealth treatmentcouldsometimesbeaggressive,makingitdiffi cult tomanagepatientexpectationsaftertheirrecentcancerdiagnosisandrequiringDPstoengageindif fi cultconversations withpatients.Thedentalteamfeltpressuredtomakedecisionsonteethwithaquestionableoruncertainprognosis. Oftenpatientshadheavilyrest oreddentitionsthatincluded severalcrownsorbridgeworkandhadbeeninplacefor yearswithoutcausingproblems.Whenthequalityofthe workhadthepotentialtocausefutureproblems,patients struggledtounderstandwhyallthisdentalworkhadtobe undone.DPsrecognizedthateachcasehadtobetakenon itsownmeritandthattreatmentplansshouldbecarefully craftedforeachindividualpatient.
DPswereoftenapprehensiveaboutwhatcanbesafely managedinprimarycareorfearedthetreatmentofcertain oncologypatients.Fearwasoftenrelatedtotheriskofinfectionorbleedingduringproceduresandwasbasedonprevious experiencesortraining.Afactorthatstronglyin fluencedDP apprehensionwastheinnovationincancercareoverrecent decades.Someapprehensionabouttreatmentresultedfrom alackofknowledge.
Secondarycarewastightlyrelatedtowhathappensinprimary care.Thepressuresandcapacityforcarewereofconcern,but itwasbelievedthatguidancecouldhelpbysupportingpatient managementinprimarycaresettings.DPsworkinginhospitals andsecondarycaresettingsusuallyhavemoreaccesstopatients’ medicalinformationandtooncologycolleaguesthroughthedigitalsystemsintheseinstitutions.
Continuityofcarewasanissue.DPssaidlackofaccesstoGDPs madethemunabletodischargesomepatientswhodidn’thavea GDPorwereunlikelytocontactaGDP.
Thewaydentistsworkingunderregulationsarepaidin fluenced whatcanandcannotbeprovided.Patientchargesareapplied invariouswaystooncologypatientsdependingontheregulationsinplace.
Table5. SummaryofSuggestionsforGuidanceand AccompanyingResources
Suggestionsfortopicstoincludeinguidance
Clearoralhealthmessagesandadvicefordentalandmedicalteams
Summaryofoncologytreatmentsanddrugsandassociatedsideeffects
Dosanddon’tsfordentalexaminationandtreatment
Treatmentplanningadvice
SuggestionsforAccompanyingResources
Patientinformation
Oncology ‘passport’ proformawhichwouldcontainthepatient’s diagnosis,treatmentandcontactdetailsforoncologyteamandusedto aidcommunication
Photographsofsideeffectstolookoutfor
ListofadviceDPsshouldprovidetoapatientpre-cancertreatment
Signpostingtofurthersupportforpatients(e.g.mentalhealthadvice)and furthersupportforDPs(whoandwhentocontactforadvice)
(CourtesyofWemyssC,AbdulsalamA,BeatonL,etal:Experienceof primarydentalcareteamsinmanagingtheoralhealthofoncologypatients. BMCOralHealth 24:1554,2024.)
Someparticipantsidenti fiedbarrierstosecondarycaredental serviceswhenfacedwithcomplexdentalproblemsfor oncologypatients.Referringpatientswiththesecomplex dentalproblemscausedpositiveandnegativeexperiencesfor thepatientandDPS.
FocusgroupDPsprovidedexamplesofwheretheybelieved theywouldneedsupport.Theywereoftenunawareofall thespecialty-speci ficguidanceavailableorofnewlyaccepted orevenpreexistingguidelines.DPsdesiredinformationabout howtomanagecancerpatientsandhowtoaccomplishtransfersamongmedicalprovidersanddentalpractices.Guidance andresourceswerefelttobelacking(Table5),including thingsasbasicaslea fletsforpatientinformation.However, DPsoftenmentionedsupportivecolleaguesinbothdental andmedicalteamswhoprovidedinvaluableinformationand guidance.
Theprimarydentalcareofpatientswhohaveorhavehadcancer iscommon,sothedentalteamshouldbeawareofwhatcanbe safelyprovided,theconcernsthatthesepatientsmayhave,and howbesttoapproachtheircareandmanagethechallenges theypresent.Communicationbetweenandamongcareproviders,understandingthefactorsthatinfluencecaredelivery, andobtainingandprovidingsupportforthepatientsasthey faceacomplexsystemareamongtheconcernsthatdentalteams mustmanage.
ClinicalSignificance
Dentalteamsarefacedwithnumerouschallengesas theyseektoprovidecareforpatientswithcanceror whohavehadcancer.Thetopicsbroughtupinthediscussionscanbeusefulindirectingtheprovisionofadditionalresourcesandincraftingeffectivecommunication systemsbetweentheoncologyanddentalcareteams. Additionalresearchintothesetopicsshouldhelpinaddressingthechallengesthathavebeenidentifiedand addothersthatmaynothavebeendiscussed.Additional supportinseveralareasisneeded.
WemyssC,AbdulsalamA,BeatonL,etal:Experienceofprimary dentalcareteamsinmanagingtheoralhealthofoncology patients. BMCOralHealth 24:1554,2024
Reprintsavailablefrom LBeaton;e-mail: lbeaton002@dundee. ac.uk
Mostdentalextractionshealwithoutcomplications,although somedeveloppain,swelling,bleeding,infection,andtrismus.A smallpercentageofpatientsexperiencedelayedhealing,usually relatedtoalveolarosteitisordrysocket,whichcausescontinuous,severe,deep-seated ‘bone’ paininoraroundthesocket beginning2to3daysafterextraction.Certainsystemicdiseases canalsocausedelayedhealing,includingalcohol-relatedliverdiseaseandnutritionaldeficiencies.Inrarecases,theextractionsite doesn’thealforweeksormonths,promptinganinvestigation intowhatisgoingonandreferralforspecialistcare.Areview oftheliteratureidenti fiedcaseswhereanon-healingextraction socketresultedfromaserioussystemicdiseaseormalignancy (oftenunknowntothepatient)orwascausedbysystemic therapy.
AsearchwasdoneinthePubMed,Embase,Scopus,ProQuest, andGoogleScholardatabases.Fiftycasesofnon-healingextractionsocketswereidenti fied.
The50casesinvolved28womenand22men(agerange26to 81years,averageage55.2years)whohadatotalof71teethextracted.Forty-oneoftheextractedteethweremandibularposteriorteeth.Reasonsforextractionwereusuallynonspecific, includingtoothmobilityorlooseness,swelling,periodontitis, pain,andinfection.Onewomanhadparesthesiaoftheright lowerlipandchinleadinguptotheextraction;shewassubsequentlydiagnosedwithmetastaticbreastcancertothemandible.

Figure1. SCCpresentingasanon-healingextractionsitewithanulcerative, mixedredandwhitedestructivelesionanderythemaofthelefthardpalate. (ReproducedwithpermissionfromRichardsetal., ‘Slowtohealorslowto diagnosecancer?’ BDentJ 230:518-522,2021.18)(CourtesyofUkwasA, ElbegoA,AlbegoM,etal:Non-healingextractionsocket:Adiagnostic challengeforgeneraldentalpractitioners. BrDentJ 237:911-916,2024.)
Table2. PotentialLocalandSystemicCausesofDelayedandNon-healingExtractionSockets(ListIsNotExhaustive)
LocalcausesSystemiccauses
Delayedhealing
Non-healing
Alveolarosteitis(drysocket)
Localinfection(egperiodontitisorinfected granulationtissue)
Foreignbody(Alveogylremnants)
Alveolarbonesequestrum
Tobaccosmoking
Osteomyelitis
Radiationtothejaws
PrimarymalignancyegSCC
Neoplasmsofmaxillarysinusornasalcavity
Odontogenictumouregameloblastoma
Langerhanscellhistiocytosis(monostotic)
Oldage
Obesity
Diabetesmellitus(particularlyuncontrolled)
Smoking
Alcohol-relatedliverdisease
Corticosteroidtherapy
Chemotherapy
Malnutrition/nutritionaldeficiency
Severeanaemiaorblooddyscrasia
MRONJ
Metastaticcancer
Langerhanscellhistiocytosis(polystoticand disseminated)
Sarcoidosis
Hyperparathyroidism
(CourtesyofUkwasA,ElbegoA,AlbegoM,etal:Non-healingextractionsocket:Adiagnosticchallengeforgeneraldentalpractitioners. BrDentJ 237:911-916,2024.)
Sixty-eightpercentofthecasesinvolvedadiagnosisofmalignancy, with24primaryand9metastatic.Amongtheprimarymalignancies, themostcommonwassquamouscellcarcinoma(SCC),whichwas seenin60%oftheprimarycancercases(Figure1).Amongthemetastaticlesions,3originatedinthelung,2inthebreast,andtheothers fromtheliver,kidney,andcolon(1each).Onepatientwith metastaticangiosarcomahadnooriginidentified.Fiveofthepatients withmetastaticdiseasehadnopriorhistoryofmalignancy.The averagewaitfordiagnosisofpatientswithmetastaticnon-oralmalignancieswas3months,with1patientwaiting6months.
Medication-relatedosteonecrosisofthejaw(MRONJ),often relatedtozoledronicacidordenosumab,wasfoundin10 women.Sevenpatientswhoweretakingrelevantmedication thatwasassociatedwithMRONJhadmetastaticbreast cancer,and1eachoftheremaining3patientswithMRONJ hadmetastaticthyroidcancer,rheumatoidarthritis,andosteoporosis.OnecaseeachwasfoundtoinvolveLangerhans cellhistiocytosis,ameloblastoma,osteomyelitis,invertedmaxillarypapilloma,browntumorofhyperparathyroidism,and sarcoidosis.
Table3. Pre-operativeFeaturesThatMayBeSuggestiveofIncreasedRiskofLaterExtractionSocketNon-healing*
History
Clinicalexamination
Radiographicinvestigation
Historyofcancer
Historyofradiotherapytotheheadandneck
Historyofanti-resorptiveoranti-angiogenetictherapy
Historyofimmunosuppression
Suddenloosenessofteethwithouthistoryoftrauma,orrecentdentaltreatment
Suddenonsetofnumbnessoftheliporchinwithnohistoryofrecenttraumaorfracturetothe mandible
Suddenonsetofnumbnessortinglingsensationoverthecheekorupperlip
Extremelymobiletooth/teethwithnoapparentfractureorperiodontaldisease.Thisshouldbe assessedinthecontextoftherestofmouth
Excessivebleedingonprobingwhichcannotbestoppedwithlocalmeasures
Severe(oftenirregular)destructionofbonesothatthetoothorteethappearasbeing floatingin air(Fig.3)
Toothassociatedwithapunched-outormultilocularradiolucencynotconsistentwithacyst
Tooth/teethassociatedwithapoorlydefinedradiolucencyormixedradiopaque/radiolucent lesi
Key:
*Ifapatientpresentswithoneormoreofthesemanifestationsbeforeextraction,theyshouldbescheduledforaregularfollow-upfollowingextraction oratleastaweeklybasis,andshouldbereferredifnosignsofhealingaredetectedasdescribed(2weeksifmalignancyissuspected).
(CourtesyofUkwasA,ElbegoA,AlbegoM,etal:Non-healingextractionsocket:Adiagnosticchallengeforgeneraldentalpractitioners. BrDentJ 237:911-916,2024.)
Completesealingofthesocketafterextractionofatooth shouldoccurinabout4to6weeks.Ifnosignofhealing occursbythispoint,thedentistshouldevaluatethepatient forpossibledisordersassociatedwithreducedhealing potential(Table2).Adelayindiagnosingandmanagingthesediseasesincreasestheriskofsignificantmorbiditiesandmoreinvasivetreatment.
Thedentistshouldtakecompletedental,medicalandsocialhistories(Table3).Inaddition,carefulextra-oralevaluationshould bedoneoftheregionallymphnodesandmouthopening.The extractionsocketandsurroundingarearequirecarefulevaluationundersufficientlighttodetectsignificantsignsofamore seriousproblem.Thiscouldincludeasinustrackorabscess, foreignbody,sequestrum,oroantral fistula,erythematous swellingaroundthesocket,oranexophyticgrowthfromthe socket.Radiographscanbetakenbutanyseverebonedestructionshouldbeassessedinthecontextoftheentireoralcavity andnotbelimitedtoperiapicalviewsbutalsoconsider orthopantomograms.Thesocketcanbecurettedandthespecimensentforhistologicevaluation.Referraltospecialistcareis appropriateforpatientswhohavenoproperhealingafter 4weeksorwitha2-weekurgentreferralifmalignancyis
suspected.Thepatientshouldbegivenathoroughexplanation ofthereasonforthereferralandprovidedacopyofthe referralform.
Dentistsneedtoremainvigilantafteranextractionto ensurethathealingproceedsaccordingtoanormal pattern.Ifthesitedoesn’thealwithin4to6weeks andtherearenoindicationstoexplainthedelay,the patientshouldbecarefullyevaluatedandsenttoa specialistforadditionalinvestigationsandadefinitive diagnosis.
UkwasA,ElbegoA,AlbegoM,etal:Non-healingextraction socket:Adiagnosticchallengeforgeneraldentalpractitioners. BrDentJ 237:911-916,2024
Reprintsavailablefrom AUkwas,UCLEastmanDentalInst,Univ CollegeLondon,UK;e-mail: abdouldaim.ukwas.09@ucl.ac.uk
Implanttherapycanrestoremissingteethandaddfunctionaland aestheticrestorationstothedentition.However,about22%of patientswithimplantsdevelopperi-implantitisthatcancause thelossofosseointegration.Preventingperi-implantdiseasesis vitaltolong-termsuccess,butpatientswithcertainriskfactors canbemoresusceptibleandlesslikelytoavoidthesedisorders. Theriskfactorsincludeasusceptibilitytoperiodontitis,diabetes mellitus,andthepresenceofabacterialbio filmontheimplant surface.Overall,thecausesofperi-implantdiseasesresemble thoseforperiodontaldiseasesaroundnaturalteeth.Regular maintenanceofgoodoralhealthisanessentialingredientof avoidingperi-implantdiseases.ThetreatmentinterventionsrecommendedforinclusioninnonsurgicalstepstotreatperiimplantitiswerebasedontheEuropeanFederationofPeriodontology’s(EFP’s)S3-levelclinicalpracticeguidelines.
ControlofLocalRiskFactors
Inadditiontothesystemicriskfactors,severallocalfactors canin fl uencethedevelopmentofperi-implantitis.These includetheoralbacterial fl ora,thetypeofrestoration
applied,failuretoprovidecleansingability,andaesthetics.Accesstooralhygieneisaprimaryrequirementtolowerthe riskofperi-implantitis.Inaddition,implantplacementshould beplannednotjustforaestheticsbutalsotoavoidniches thatcan ’tbereachedduringoralhygiene.Patientsat increasedriskforperi-implantitisinnonaestheticareasshould receivetissue-levelimplants,withbone-levelimplants reservedforaestheticregions.
Patientsneedregularmonitoringthatdocumentstheirplaque controlaswellasclinicalsignsofperi-implantitis,suppuration, increasedprobingdepth,andboneloss.Theseparametersshould berecordedonatleast4sitesaroundtheimplant,andanintraoralradiographshouldbeobtained.Patientswillrequirerepeated instructionsonhowtoachieveadequatecleaning.Toolsfor interproximalhygieneshouldbeadaptedtoincreasepatients’ efficacy.
Asystematicclinicalapproachisdesirable(Figure1).Supramucosal/mucosaltherapyandsubmucosaltreatmentcanbeperformedatthesameappointment.Supraconstructionis
Figure1. Therapeuticstepsfortreatmentofperi-implantmucositisandperi-implantitis.(CourtesyofMeyleJ,Fischer-WaselsL:Non-surgicaltreatmentof peri-implantitis. BrDentJ 237:780-785,2024.)
removedtofacilitateaccesstotheimplant’ssubmucosalareasif needed.Shallowpocketsmaynotrequirethisstep.
SupramarginalandSubmarginalInstrumentation
Allcalcifiedandnoncalcifieddepositsshouldbecompletely removedfromtheinfectedimplantsurface.Completecleaning isdif ficult,eveninvitro.Mechanicalcleaningusingsteelcurettes ortitaniumhandinstrumentsisn’trecommended.Plasticcurettes,metalcurettes,rotatingtitaniumbrushes,andanultrasonicscalingsystemwithacarbontipandpolishing fluiddonot
restorethebiocompatibilityofroughtitaniumsurfaces.Remnantsfromsoftcurettescanbehardtoremove.Evenso,curettes andultrasonicdevicesareusedforsubmarginalcleaningand debridement.Reducingdamagetotheimplantsurfaceisachieved byusingultrasonicdeviceswithplastictips(Figure5).Inaddition, theair-powderabrasivesystemwithsodiumbicarbonatepowder isunlikelytoharmthe fibroblast-titaniumsurfaceinteractionaftertreatingsmoothorroughsurfacesevenwhencontamination ispresent.Thebiofilmremnantscanberemovedusingtheperionozzlecombinedwitherythritolpowder.Thechitosan-based
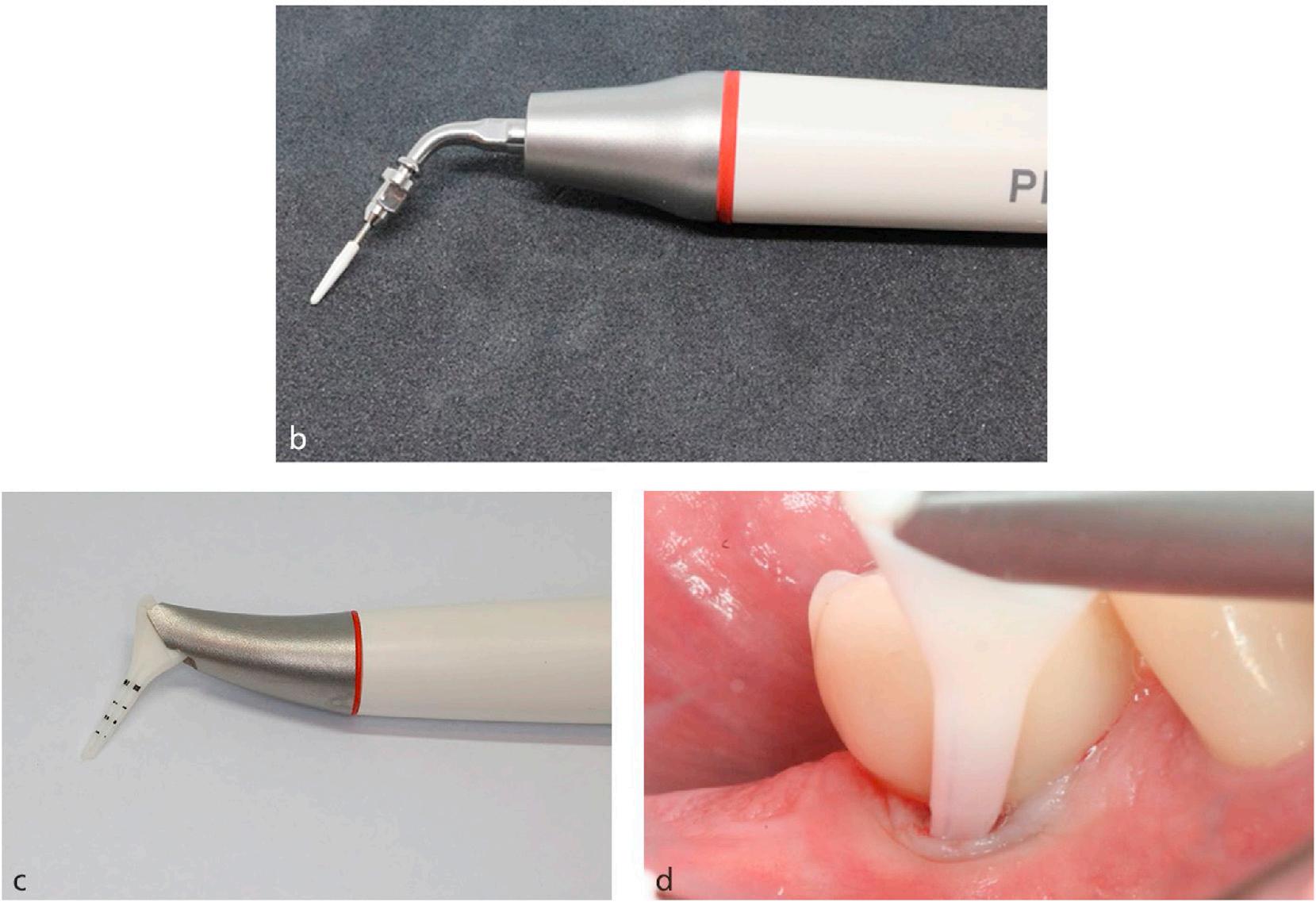
Figure5. Ultrasonic/air-polishingdevice. B, Ultrasonichandpiecewithtipmadeofpolyetherketoneinordertoreducedamagetotheimplantsurface. C, Handpieceforair-abrasivetreatmentwithnozzleforsubmucosaldebridement. D, Clinicalsituationwithperionozzleinsertedatimplantsite.(Reproduced withpermissionfromMeyleJ,Fischer-WaselsL:Non-surgicaltreatmentofperi-implantitis. BrDentJ 237:780-785,2024.).
Box2. CriticalEndpointsofNon-surgicalTherapyofPeriimplantitis(AccordingtoHerreraetal.2023).
Residualprobingdepths %5mm
Bleedinguponprobingat %1site/implant
Nosuppuration
(CourtesyofMeyleJ,Fischer-WaselsL:Non-surgicaltreatmentof peri-implantitis. BrDentJ 237:780-785,2024.)
oscillatingbrushhaslimitedef ficacyagainstlocalin flammation. Usingbiofilmdilutingagentshasbeenassociatedwiththelowest residualbleedingonprobingofalltheapproaches.
Chlorhexidine(CHX)solution flushinghashadlimitedeffectand wasunabletoresolvelocalinflammationinmostlesions.Useofa gelatindepositofCHXreducedbleedingonprobing,butresidual bleedingscoresindicatedincompletehealingofthelesion.The adjunctiveuseofantimicrobialsisn’trecommended,noristhe useofadjunctiveprobiotics.Newtherapiescombinethebio film resolutionbyhypochloriteincombinationwithchloramine,followedbylocaladministrationofhyaluronicacid.Signi ficantreductionswereseeninpocketprobingdepthsandclinicalattachment gainsaroundnaturalteeth.Hyaluronicacidhassomebene ficial aspects.
Laser-assistedtherapiesarelimitedintactilesensationandvisual control.Residualbleedingonprobingshowsthecleaningandbiofilmremovalareincomplete.Asaresult,theEFPS3guidelinesuggestsnotusinglaserseitheradjunctivelyorasmonotherapyinthe nonsurgicalsubmarginalperi-implantinstrumentation.
The7-day-longsystemicadministrationofmetronidazolealong withultrasonicinstrumentationandCHXrinsingachievedsignificantlybetteroutcomesafter12monthsandwassuccessfulin 56%ofthepatientsinthetestgroupbutjust25%ofthecontrol group.Routineprescriptionofsystemicantibioticsadjunctively tononsurgicaltherapyisn’trecommended.
Nonsurgicaltreatmentsshouldbeevaluated6to12weeksafter treatment.Duringhealing,patientsshouldbemonitoredregularlyandoralhygienereinforcedasneeded.Residualprobing depths,bleedingonprobing,andsuppurationshouldberecordedontheimplantleveltodocumentthecriticalparameters (Box2 ).
Nearlyallnonsurgicalinterventionscannotachievecomplete resolutionofperi-implantitis.Thepercentageofbleedingsites canbereducedsignificantly,indicatingapossibleef ficacyofthe intervention,butclinically,thesetreatmentsaren’tconsidered efficient.Completeresolutionofdiseaseusingnonsurgicaltechniquesisunlikely.
Currently,thetreatmentofperi-implantitisisfoundedonsurgicalinterventionsthatallowcleansingofthedefectsand implantsites,possiblere-shapingifneeded,andreconstructionofthedefecttoremovenichesandreestablishconditions leadingtore-osseointegration.Nonsurgicaltreatmentisless invasive,moreconservative,andoftenmorecomfortable forpatients.Itcanreduceinflammationandthebacterial loadbeforesurgicalinterventionsareundertaken.Therefore, nonsurgicalperi-implanttreatmentcanrenderlocaltissuesto aconditionwhereasurgicalinterventionismorereadily achievedandwhenfailureriskisreduced.Combiningnonsurgicalapproachesmayimproveoutcomes,andsynergisticeffectsmayenhancetheoutcomes.
MeyleJ,Fischer-WaselsL:Non-surgicaltreatmentofperiimplantitis. BrDentJ 237:780-785,2024
Reprintsavailablefrom JMeyle;e-mail: Prof.Dr.J.Meyle@tonline.de
Aftertoothextraction,spontaneoushealingresultsin3dimensionalalveolarboneremodeling,withthewidth decreasingbyabout3.8mmandtheheightreduction rangingfrom1.24to1.7mm.Thesedataarebasedon studiesthatincludedextractionsatanterioraswellaspremolarareas.Furtherstudiesindicatethatextractionsat molarsiteshavegreaterreductionsthanthoseatnonmolar sites.Alveolarridgepreservation(ARP)includesvarious regenerativetreatmentmodalities,suchastheuseofbone substitute(socketgrafting),soft-tissuegrafts(socketseal), oracombinationofboth.AlthoughARPiswellrepresentedbyitsabilitytoachieveaestheticresultsat maxillaryanteriorareas,itspossiblebene fi tsinmolarareas arelargelyunknown.SomereviewsindicateARPcanreduce boneresorptionaftertoothextraction,maintainalveolar ridgevolume,andavoidadditionalboneaugmentationproceduresinimplanttherapy.AsystematicreviewandmetaanalysisevaluatedtheeffectofARPatmolarextractionsites comparedtothatwithspontaneoushealingonhardtissue changesandtheneedformoreaugmentationduringimplant placement.
AsearchofthePubMed,Embase,WebofScience,Cochrane CentralRegisterofControlledTrails,andtheSystemforInformationonGreyLiteratureinEuropeidenti fi ed7studies thatwereapplicable.Thesein cluded4randomizedcontrolled trials(RCTs),2prospectivenonrandomizedclinicaltrials,and 1prospectivecasecontrolstudy.Theprimaryoutcomewas thechangeinalveolarridgewidthandheight,withsecondary outcomesofsinuspneumatizationandneedformore augmentationwhenimplantplacementisdone.Thestudies included237molarextractionsocketsin236patients (meanageabout49to59years,range21to70years). Thechangesindimensionwereevaluatedusingcone-beam computedtomography(CBCT).
ARPwasdonein126sitesandtheremainderself-healedwithout ARPintervention.Noneofthepatientshadactiveoruntreated periodontaldisease.Comparedtospontaneoushealing,ARP significantlyreducedthehorizontal,verticalmid-buccal,and verticalmid-lingualdimensions.Theridgewidthdifferences weren ’tstatisticallysignificantbetweenthe2groups.Using ARPreducedtheneedforadditionalaugmentationduring implantplacementcomparedtoself-healingafterextraction.
TheuseofARPlimitedhorizontalandverticalhardtissue changesatmolarextractionsitesduringsockethealing.More studiesareneededtoconfirmthese findings.
Longerfollow-uptimesandalargerpatientsampleare neededtocon firmthe findingsofthisreview.Itseems apparentthatARPcanreducesocketboneandridge changes,makingadditionalaugmentationprocedures inmolarregionsunnecessaryinmanycases.No consensushasbeenfoundregardingtheefficacyof thevariousproceduresorofthebiomaterialsused.
WeiY-P,HanZ-Y,HuW-J,etal:Alveolarridgepreservationat molarextractionsites:Asystematicreviewandmeta-analysis. J EvidBaseDentPract 2025:[102074]
Reprintsavailablefrom WHu,DeptofPeriodontology,Peking UnivSchoolandHospofStomatology,NatlCtrforStomatology, NatlClinicalResearchCtrforOralDiseases,NatlEngineering ResearchCtrofOralBiomaterialsandDigitalMedicalDevices, No.22,ZhongguancunSAve,HaidianDist,Beijing,100081,PR China;e-mail: huwenjie@pkuss.bjmu.edu.cn
Teetharemostoftenextractedbecauseofdentalcariesandperiodontaldisease,whichareinfectiousdiseasesthatcancause problemsforsupportingstructuresandleadtolocalandsystemic complications.Asaresult,systemicantibioticsareoftenprovided topreventpost-extractioncomplications.Thisuseofantibiotics isn’twellsupportedbyevidence,withseveralstudiesidentifying nobene fittousingantibioticstopreventcomplicationsoverthe useofnoantibioticsoraplacebo.VeteransAffairs(VA)dental patientstendtohaveahigheroralandsystemicdiseaseburden thanisfoundinthegeneralpopulation.Theyalsohaveahigher rateofcariesandmentalandphysicalcomorbidities,including depressionanddiabetesmellitus.Thispopulationwasstudied toevaluatetheeffectivenessofantibioticprophylaxistoprevent localandsystemiccomplicationsafteradentalextraction.
Theretrospectivecohortstudycoveredaperiodof5yearsand included385,880dentalvisitsof269,003patientswhohadan extraction,duringwhich122,810patientsreceivedantibioticprophylaxis.Theprimaryoutcomewaspost-extractioncomplications occurringwithin7daysoftheextraction.Thesecondaryoutcome wassubsequentmedicalcarerequiredthatwasrelatedtoapostextractionoralcomplicationwithin7daysoftheextraction.The effectofantibioticprophylaxisoneachoutcomewasevaluated.
Mostpatients(about93%)wereage65to79years,withabout 48%betweenages65to79yearsandabout32%betweenages 45and64years.About61%hadjust1toothextracted,andabout 59%hadnonsurgicalextractionsperformedattheirinitialvisit. Dentalprovidersperformedabout92%oftheextractions, with8%donebyoralsurgeonsand0.2%byresidents.About 3%hadahistoryoforalinfection,1%implanthistory,and1% oralinfectionatbaseline.Dentalpractitionersweremorelikely togivepatientswhohadsurgicalextractionsantibioticprophylaxiscomparedtothosewhohadnonsurgicalextractions.The mostcommonantibioticsprescribedwereamoxicillinand clindamycin.
Apost-extractioncomplicationoccurredinlessthan1%ofthe patients,with1%ofthesecomplicationsinpatientswhohad antibioticprophylaxisand0.8%inpatientswhohadnoprophylaxis.Diabeteswasasigni fi canteffectmodi fi eroftherelationshipbetweenantibioticprophylaxisandpost-extraction complication.
Inthe7daysafterextraction,just0.09%ofthepatientsreceived medicalcarerelatedtoapost-extractionoralcomplication.Antibioticprophylaxiswasn’tsigni ficantlyassociatedwithpostextractionmedicalcare.
Theuseofantibioticprophylaxisdidnotreducepostoperative infectionortheoccurrenceofdrysocketcomparedtonot receivinganantibioticprescription.Thepostoperativecomplicationratewaslessthan1%,soantibioticprophylaxisisunlikely toprovideabene fi tthatisgreaterthantheriskofadverse eventsassociatedwiththeuseoftheantibiotic.
Dentalprovidersshouldreviewtheirprotocolforusing antibioticprophylaxisafteradentalextraction.Itisrecommendedthatonlypatientswithacurrentsystemic infectionthatwillrespondtotheantibiotictreatment shouldbeprescribedthesedrugs.
McGregorJC,WilsonGM,GibsonG,etal:Theeffectofantibioticpremedicationonpostoperativecomplicationsfollowing dentalextractions. JPublicHealthDent 84:343-350,2024
Reprintsavailablefrom KJSuda,CtrforHealthEquityResearchand Promotion,VAPittsburghHealthCareSystem,3609ForbesAve, 2nd Flr,Pittsburgh,PA15213,USA;e-mail: ksuda@pitt.edu
Dentalimplantsareafrequentchoicetoreplacemissingteeth, usuallyasaresultofdentalcaries,periodontaldisease,ortrauma. Thisprocedureisgenerallysuccessful,butcomplicationscan occurearlyorlate.Iftheimplantislostinthe firstmonthsafter insertion,usuallyasaresultofosseointegration,thecauseisusuallybacterialcontaminationduringimplantsurgery,althoughfactorssuchassurgicaltechnique,implantcharacteristics,the surgeon ’sexperience,orahistoryofperiodontitisandsmoking cancontribute.Theriskofinfectionhasbeenaddressedbyprescribingantibioticsforpatientshavingimplantsurgery.However, noplacebo-controlled,randomizedclinicaltrial(RCT)hasshown thereisastatisticallysigni ficantrelationshipbetweenantibiotic prophylaxisandreducedratesofearlyimplantfailure.Even showingsucharelationshipdoesn’tmeanthatroutineantibiotic prophylaxisisclinicallyrelevant.Asystematicreviewandmetaanalysisweredonetoevaluatetheef ficacyofpreoperativeantibioticstopreventearlydentalimplantfailureandtodetermine thecertaintyoftheevidence.
AsearchwasdoneinthePubMed(Medline),WebofScience,and CochraneLibrarytoidentifyRCTscomparingantibioticprophylaxiswithnoantibioticsorplaceboinpatientswhowereconsideredhealthyandhadreceiveddentalimplants.Twelvestudies wereselected,with7includedinthemeta-analysis.Theprimary outcomewastheeffi cacyofpreoperativeantibioticstoprevent earlydentalimplantfailure;thesecondaryoutcomewastodeterminethecertaintyoftheevidence.Thelatterwasevaluatedusing theGradingofRecommendations,Assessment,Development andEvaluations(GRADE)approach,ratingtheRCTsashigh, moderate,low,orverylowincertainty.
The7studiesincluded929patientswhoreceivedantibioticsand 930whoreceivedplacebos.Twentypatientsintheantibioticgroup and31intheplacebogroupdevelopedearlyimplantfailures.In4 RCTs,theimplantfailureratewaslowerinthegroupsgivenantibioticprophylaxis,in2RCTs,theimplantfailureratewaslowerin thegroupreceivingplacebos,andin1RCT,therateofimplantfailurewasthesameinbothgroups.Overall,theimplantfailurerates wereverylowandlessthan6.5%inallgroups.
TwoRCTsmeasuredpatient-reportedoutcomemeasures (PROMs)forpainand/orqualityoflife.Noneofthe7RCTs
reportedanystatisticaldifferencesinthegroupsforearlyimplant failureorpostoperativeinfection.
Themeta-analysisofthe7studiesshowednosignificantdifferencesbetweengroups.Theantibioticgroupsandplacebogroups didnotdiffersignificantlyinanysub-groupmeta-analyses.
Amoderatedegreeofcertaintysupportedthehypothesisthat theeffectofantibioticprophylaxisinpreventingimplantfailure wassmall.
TwooftheRCTsconcludedthatroutineuseofprophylacticantibioticsmaybeadvisable,buttheother5foundantibioticprophylaxismaynotbeneeded.Thenumberneededtotreat (NNT)topreventearlyimplantfailurein1patientwas143, forwhichthecon fidenceinterval(CI)wenttoin finity.The routineuseofantibioticprophylaxiswouldlikelymeanthata verylargenumberofpatientswouldreceiveantibiotics unnecessarily.
Whenthenumberofpatientswithimplantfailureand thehighnumberofNNTpatientstopreventimplant failurein1patientareconsidered,itseemsthatthe routineuseofantibioticprophylaxisforimplantsurgeryisinappropriate.Usingantibioticscarriesarisk ofsideeffectsandanincreasedriskofantibioticresistance.Theprovisionofantibioticprophylaxisforallpatientswhohaveimplantsurgeryisn’tsupportedby significantevidence.Itmaybetimetodevelopnew clinicalguidelinesforantibioticprophylaxisinimplant surgery.
MomandP,Naimi-AkbarA,HultinM,etal:Isroutineantibiotic prophylaxiswarrantedindentalimplantsurgerytopreventearly implantfailure? – Asystematicreview. BMCOralHealth 24:842, 2024
Reprintsavailablefrom PMomand,DeptofOrofacialMedicine, FacultyofOdontology,MalmoUniv,MalmoSE-20506,Sweden; e-mail: Palwasha.momand@mau.se
Withtheagingofthepopulation,dementiaandcognitiveimpairment areseenmoreoften,especiallyamongolderindividuals.Inaddition, cognitiveimpairmenthasbeenlinkedtopoorqualityoflifeinolder persons.Variousriskfactorshavebeenproposed,withsomebeing modifiableandothersnot.Amongthepossiblymodifiablefactors arereducedmasticatoryfunction,toothloss,andchronicinflammationcausedbychronicperiodontitis.Poorcentralnervoussystem (CNS)functionandreducedmasticatoryfunctionhavebeenstudied, withsomeinvestigationsusingnumberofteethasasurrogate markerformasticatoryfunctionandothersusingocclusalbiteforce, color-changingchewinggum,andotherdirectmarkersofchewing ability.Asystematicreviewwasdonetodetermineifthereareassociationsbetweenobjectivelyandsubjectivelymeasuredmasticatory functionandcognitivestatusamongolderadults.
AsearchwasdoneinthePubMed,WebofScience,andCumulativeIndextoNursingandAlliedHealthLiterature(CINAHL) databases.Twenty-onestudiesmetthecriteriaandweredivided into11cross-sectionalstudiesthatobjectivelyevaluatedmasticatoryfunction,9cross-sectionalstudiesthatsubjectivelyevaluatedmasticatoryfunction,and1prospectivecohortstudy.The studiesusedvariousmeansforevaluatingcognitivestatus, includingtheMini-MentalStateExamination(MMSE),theHasegawaDementiaScale-Revised(HDS-R),theFrontalAssessment Battery,theJapaneseversionoftheMontrealCognitiveAssessment(MoCA-J),andtheClinicalDementiaRating(CDR)scale.
Amongtheobjectiveevaluationstudies,allofthecross-sectional studiesfoundpositiveassociationsbetweenmasticatoryfunction andcognitivestatusintheunivariateanalysis.Adjustmentsforconfoundingfactorscausedtheassociationstodisappearin2studies,1 studyfoundtheMMSEscorewaslowerinthegroupwithlow chewingabilityandmoderatechewingabilitywasariskfactorfor cognitiveimpairment,and4studiesshowedapositiveassociation betweenmasticatoryfunctionandcognitivestatus.
Ninecross-sectionalstudiesperformedsubjectiveevaluations ofmasticatoryfunctionandcognitivestatusincommunitydwellingadults,with8doneinolderadultsand1inmiddle-
agedorolderadults.Self-reportsofchewingabilitywereused in7studies.Allreportedapositiveassociationbetweenmasticatoryfunctionandcognitivestatusintheunivariateanalysis, butonly6showedthepositiveassociationpersistedafteradjustingforriskfactors.
Astudyof860community-dwellingolderadultsrecordedthe maximalocclusalforceatbaseline.Thismeasurewasassociated withcognitivestatusatfollow-upafter3years.Alowercognitive statusmeasureatbaselinewasassociatedwithfewerteethand lowerocclusalforce,butthelowerscoredidn’tpredictchanges inthenumberofteethortheocclusalforceafter3years.The authorsspeculatedthatnumberofteethandocclusalforceofindividualsuptoage70to80yearsmayberelatedtocognitive status.
Severalstudiesindicatedthatmasticatoryfunctionwaspositively relatedtocognitivestatus.Thereviewwasunabletoconclude whetherornottheassociationwascausal.
Thecurrentstudiesdon’tconclusivelyindicate whethermasticatoryfunctionaffectscognitivestatus. Variousmeasureswereusedtodeterminecognitive function,andthecut-offlevelsfortheMMSEwere inconsistentamongthestudies,makingithardto drawaccurateconclusions.Futurestudiesshould includelongitudinalinvestigationsaswellasinterventionstudiestodetermineifacausalrelationshipispresent.
MaekawaK,MotohashiY,IgarashiK,etal:Associationsbetween measuredmasticatoryfunctionandcognitivestatus:Asystematic review. Gerodontology 41:452-463,2024
Reprintsavailablefrom KMaekawa,DeptofRemovableProsthodonticsandOcclusion,OsakaDentalUniv,1-5-17Chuo-ku, Otemae,Osaka,Japan;e-mail: maekawa-k@cc.osaka-dent.ac.jp
Thelossorreductionofmasticatorysensorystimulationand toothloss associatednutritionaldeficitsmaycontributetoa linkbetweentoothlossandcognitiveperformance.Ithasbeen suggestedthatposteriorteethand/orocclusalpairsmaybe importantbasedonthefactthattheyareessentialformastication.Lossofposteriorteethorocclusalpairscompromises masticationandcontributestonutritionaldeficits,andchronic nutritionde ficitsmaycontributetotheriskfordementia.Inaddition,masticationstimulatesvariousdementia-relatedbrainareas, andtheunilateralandbilateraluseofposteriordentitionmay stimulatebrainareasdifferently.Metabolicsyndromeand obesity,alongwithotherdementia-relatedriskfactors,maybe linkedtothelossofposteriorteethorocclusalpairs.Chewing dysfunctionhasbeenassociatedwiththemorphologicalandfunctionaldeteriorationofhippocampalneuronsanddeficitsin learningandmemory.Theimpactofvariousdental health relatedstructuraland/orfunctionalmarkerswasinvestigated,notingtheeffectscreatedbyanteriorversusposterior toothloss,posteriorocclusalpairloss,andchewingabilityon cognitionaswellasthe11-yearcognitivedeclineriskandthe 15-yeardementiarisk.
Thedataweretakenfromthepopulation-basedFinnishHealth 2000(H2000)andHealth2011(H2011)Surveys.Thesample fromH2000comprised8028personsage30yearsorolder wholivedinFinland.Most(6360persons)alsoparticipatedin somepartofthefollow-upH2011survey.Theparticipants wereclassifiedintodentateoredentulousandtotalnumberof posteriorocclusalpairs(POP)present.Usingtheconceptofa shorteneddentalarch(SDA),POPlosswasclassifiedas>7teeth, 4-7,and<4remaining.Cognitiveassessmentevaluatedverbal fluency,immediaterecall,anddelayedrecall.Verbal fl uency wastestedbyhavingparticipantsnameasmanyanimalsas possiblein60sec.Theimmediaterecalltestconsistedofhaving participantsmemorizeandrepeat10wordsin90sec,whereas delayedrecallrequiredparticipantstorecallwordsfromthe wordlist5minutesaftertheimmediaterecalltest.Thedata fromthesetestswereevaluatedforassociationswithposterior occlusalsupport(POS)loss,anteriorversusposteriortooth loss,chewingabilitywithbaselinecognitionand11-yearcognitive decline,and15-yearincidentdementiarisk.
Participantswith4-7or<4POPwereolder,hadlowerlevelsof educationandincome,wereathighercardiovasculardisease (CVD)riskandhigherdepressivesymptomrisk,hadlower
overalltoothcount,haddifficultychewing,andhadahigherincidenceofdementia.
Anteriorandposteriortoothlosswasnotrelatedtothe11-year cognitivedecline.However,having<4POPwasassociatedwitha declineinverbal fluency.UnilateralinadequatePOSwasrelated toadeclineinimmediaterecall,whereasbilateralinadequate POSwaslinkedtoaverbal fluencydecline.Chewingchallenges wererelatedtoimmediaterecalldecline.Sensitivityanalysis foundnoassociationsforanteriororposteriortoothloss,but asigni ficantassociationforchewingdif ficultywasnotedwith immediaterecalldecline.Having<4POPshowedatrendforverbal fluencydeclineandwaslinkedtolowerdelayedrecalldecline risk.UnilateralinadequatePOSwasassociatedwithimmediate anddelayedrecalldecline,whereasbilateralinadequatePOS wasrelatedtooverallcognitivedeclineandtendedtoberelated toverbal fluencydecline.
These fi ndingswerealsofoundamongparticipantsage55years orolder.Althoughanteriortoothlosswasn ’trelated,posterior toothlosswaslinkedtoadeclineinoverallcognition,immediate recall,anddelayedrecall.Having4-7POPwaslinkedtoimmediaterecalldecline,whereas<4POPwasrelatedtodeclinesin verbal fl uencyandimmediaterecalldecline.UnilateralinadequatePOSwasrelatedtooverallcognitivedecline,whereas bilateralinadequatePOSwasrelatedtoverbal fl uencydecline. Chewingdif fi cultywasassociatedwithadeclineinimmediate recall.
Atotalof136participantsdevelopeddementia.Neitheranterior toothlossnorchewingdif ficultywereassociatedwithdementia, butparticipantshaving<15posteriorteethhadsigni ficanthigher dementiarisk.Having4-7or<4POPsigni ficantlyincreasedthe riskfordementia.Inaddition,bilateralinadequatePOSwas relatedtodementia.
Thelossofposteriordentitiontendedtoaffectcognitiveoutcomes.The15-yeardementiariskinindividualswithposterior toothlossandPOPlosswashigher.Associationsbetweenposteriortoothlossandcognitivedeclineweresigni ficantforparticipantsoverage55years.POPlosssigni ficantlycontributedto cognitivedeclinerisk.Unilateralandbilateraluseofposterior dentitionmaystimulatedifferentbrainareas,sothereareunclear outcomesregardingtheeffectsizeoftheselosses.Chewingabilitydidn’taffectdementiarisk,butdidcontributetocognitive decline.
ClinicalSignificance
Bothposteriortoothlossandocclusalpairlossappear tosigni ficantlyinfluencetheriskofdementia.Preservingnaturaldentition,especiallywhenposteriorteeth areinvolved,shouldbeapriority.Morewelldesignedstudiesareneededtoinvestigatethepotentialtooth-relatedmechanismsthatmightberelatedto cognitivedeclineandmaybealteredbydentalinterventions.
AsherS,SuominenAL,StephenR,etal:Associationoftooth location,occlusalsupportandchewingabilitywithcognitive declineandincidentdementia. JClinPeriodontol 52:24-39,2025
Reprintsavailablefrom SAsher,InstofDentistry,UnivofEastern Finland,Yliopistonranta1C,POBox1627,Kuopio,Finland; e-mail: samash@uef. fi
Halitosisaffects5%to65%oftheworld’spopulation,soit’soften seenindentalpracticepatients.Itmanifestsasunpleasantodors thatemanateconsistentlyfromtheoralcavityandcansignificantlyaffectone’squalityoflife.Patientswithhalitosiscanexperienceinsecurity,lowself-esteem,embarrassment,andpersonal discomfort,especiallyinsocialinteractions.Patientswithgastrointestinal(GI)disordersmayalsocomplainofhalitosis,butthe scienti ficliteraturerevealsthatjustasmallproportionofcases diagnosedashalitosisarerelatedtotheGItract.Conditions suchasgastritis,gastroesophagealrefluxdisease,xerostomia, andintestinaldiseasesarerelatedtohalitosis.Areviewofthe relationshipbetweenhalitosisandGIdisorderswaspresented.
AsearchwasdoneinthePubMedandWebofSciencedatabases toidentifystudiesofpatientswithGIdisorderswhohavehalitosis.Thepublicationsofferedinformationabouttheclassi fication,etiology,anddiagnosisofhalitosis;associationsbetween halitosisandGIdisorders;andguidancefordentalprofessionals whoaredealingwithapatientwhohashalitosis.
ClassificationandEtiology
Halitosiscanbegenuinehalitosis,whichcanbesubdividedinto physiologicalorpathologicaltypes;pseudohalitosis;orhalitophobia.Physiologicalhalitosisisatransientbadorderpresentinthe oralcavityuponwakingandiscausedbynocturnalhyposalivation.Itdisappearsaftereating,brushingtheteeth,ordrinkingwater.Incontrast,pathologicalhalitosiscanbeintraoralor extraoralandiscausedbyconditionsassociatedwiththeoral cavityorwithsystemicconditionsthatoriginatefromnon-oral
areas.Pseudohalitosisreferstoapatientclaimingtohavebad breaththatcan’tbedetectedbyhealthcareprofessionals.Halitophobiaistheexcessivefearofhavinghalitosiswhenitdoesn’t existandoftenoccursaftertreatmentofgenuinehalitosis.
Inmostpatients,halitosisoriginatesintheoralcavityandinvolves microorganisms.Anaccumulationofbacteriawhereorganic compoundputrefactionoccursisthesourceofthehalitosis. Themetabolismoftheoralmicrobiotacancreatevolatilesulfur compounds(VSCs).Halitosiscanalsoresultfromdeepcarious lesions,infectionsintheoralcavity,peri-implantdisease,pericoronitis,mucosalulceration,impactedfood,andacoatedtongue.
Extraoralhalitosisisseeninabout10%to15%ofcasesandcan resultfromrespiratorydisorders,GIdisorders,systemicdisorders,neoplasms,andsomemedications.Itcanpresentasignificantdiagnosticandtherapeuticchallengetohealthcare professionals.Afterexcludingthepossibleoralandotorhinolaryngologicalcausesfortheodor,thehealthcareprofessional shouldfocusonpossibleGIdisordersasthecauseofthehalitosis.
Thediagnosticapproachesincludetheorganolepticmethod,the sulfidemonitordevice,andgaschromatography. Organoleptic diagnosisinvolvesthepatientbreathingdeeplythroughthe nose,thenexpellingtheairthroughthemouthwhiletheexaminersmellstheodor.Thisisasubjectivemethodandisn’tprecise quantitativelybutisagoodqualitativemethod.The sulfidemonitor device ismoreobjectiveandcancorrelatethequantityofVSCin thebreathsamplewithspeci ficdisorders,qualityoflife,andmalodorintensity.Theportablemonitorcannotdistinguishbetween thetypesofsul fidesordetectotherVSCclasses. Gaschromatography differentiatesandidentifiesVSCsanddistinguishesthem

Figure3. InfographicoftheprevalenceofhalitosisforGERD,gastritiswith H.pylori infection,andIBD.(CourtesyofVianaKSS,EleuterioFHPF,MacielVG, etal:Associationbetweenhalitosisandgastrointestinaldisorders:Areview. JCalifDentAssoc 52:2426249,2024.)
fromothercompounds.Theequipmentisexpensiveandrequiresaproperlytrainedoperator,soit’snotavailableinmost dailyclinicalpractices.
Thepatientcanself-reporthalitosisorpeoplearoundthepatient maybeabletoreportthesituation.Self-reportstendtobequite accurateandcorrespondtothepresenceofhalitosisfoundusing theorganolepticmethodwhenthehalitosisismildtomoderate andstrong.
TheGIconditionsassociatedwithhalitosisarestomachinfection by Helicobacterpyloris,gastroesophagealrefluxdisease(GERD), anddisorderscausinggastriccontentretention.Thelastinclude inflammatoryboweldiseases(IBDs),whichcanaffectthecolon andsmallintestine,withulcerativecolitisandCrohn’sdisease includedasextraoraldisordersassociatedwithhalitosis (Figure3).ThemostcommonGIsymptomsinthesedisorders areabdominalpain,reflux,nausea,andesophagealandduodenal alterations.Medicationsusedtotreatthesedisorderscanalsobe associatedwithhalitosis.
Thehalitosistreatmentforthesepatientsisfocusedontheunderlyingdisorder.Thedentistshouldconductameticulousintraoralandoropharyngealexaminationandperforman organolepticevaluationtocon firmthebadbreath.Iftheseinvestigationsindicatethehalitosishasanextraoralorigin,thepatient shouldbereferredtothemedicalspecialistwhocanaddressthe underlyingdisorder.
GastritisandHpyloriInfection
Gastritisisanin fl ammationofthegastricmucosathatusually resultsfrominfectionscausedby Hpylori .Thesebacteria colonizetheGImucosaandcontributesigni fi cantlyto gastritis,gastricandduodenalulcers,andgastriccarcinoma.
Morethanhalfoftheworld’spopulationcarries Hpylori infection,withtheoralcavitypossiblyservingasanextragastricreservoirfor Hpylori .
Symptomscanbesignificantlyreducedoreradicatedifthemicroorganismiseliminated.However,chlorhexidinemouthrinseis ineffectivewhenusedfor Hpylori halitosis.
InGERD,retrograde fl uxofthestomach ’scontenttothe esophaguscausesunpleasantsymptomsandcomplications. Thesesymptomscanproduceadverseeffectsonthepatient’ s well-being,includingheartburn,regurgitation,esophagitis,Barrett ’sesophagus,andesophagealadenocarcinoma.Extraesophagealmanifestationscanalsobefound.Halitosisisa notablemanifestationandresultsfromvarioussources,such asthefollowing:
Theodorfromthetongue’sposteriordorsumareacomes mainlyfrompostnasaldrippingaccumulatinginthatregion. Theacidcontentfromthestomachcanreachthenasopharynxandcauseirritationofitswalls,producingreferred postnasaldrippingandtonguecoatingandresultingin halitosis.
Thefunctionoftheesophagealsphincterisalteredinpatients withGERD,sothatintestinalandstomachgasesreturntothe esophagusandproducebadbreath.
Directdamagecanresultwhenpepticacidentersthesupraesophagealmucosa.
IBDautoimmunedisordersmaycauseextra-intestinalproblems,evenreachingtotheoralcavity.Asigni fi cantassociation hasbeenfoundbetweenhalitosisandsevereulcerativecolitis, withanincreaseinthenumberofbacteriathatreducesul fi de
compoundsinthebowelcreatinghigherconcentrationsof hydrogensul fi de.
SomemedicationsusedforIBDmayhavesideeffectsontheoral cavity.Thisincludesreducingsalivary flowrate,whichleadsto hyposalivationandxerostomia.
Halitosiscanbecausedbyanumberofsystemicaswellasoral disorders.Oralhealthcareprofessionalsmayseepatientswith halitosiswhohavebeenreferredtothembecausethepatient’ s medicalprofessionalisunfamiliarwiththepossibleetiologyof theproblem.Afterhavingidenti fiedwhethertheproblemis oralorextraoral,thedentistshouldaddresstheproblemwith eitheroralhealthcaremeasuresorareferraltothepropermedicalprofessional.
ClinicalSignificance
Additionalresearchintothecausesandprocesses thatcanproducehalitosisisneeded.Studiesshould beundertakentoidentifytheexactmechanismsby whichVSCsareproducedinextraoralsitesandthen cometobeexpelledthroughtheoralcavity.Halitosis isjustasymptom,withvarioustestsrequiredtodeterminetheextraoralororalcauseoftheproblem.A multidisciplinaryapproachmayleadtobettermanagementofhalitosis.
VianaKSS,EleuterioFHPF,MacielVG,etal:Associationbetween halitosisandgastrointestinaldisorders:Areview. JCalifDentAssoc 52:2426249,2024
Reprintsavailablefrom KSSViana,DeptofDentalClinics,Oral SurgeryandOralPathology,SchoolofDentistry,Universidade FederaldeMinasGerais(UFMG),BeloHorizonte,Brazil; e-mail: karolinasilvaviana@gmail.com
Evidenceindicatesthatperiodontaldisease(PD)andcardiovasculardisease(CVD)areindependentlylinked.PDresultswhen pathogenicbacterialplaqueaccumulatesaroundtheteethand gingiva,causinganin fl ammatoryresponsethatcanprogressively damagethestructuressupportingtheteeth.PeoplewithPD haveaconsistentlyincreasingriskfordevelopingCVD,which causesathirdofalldeaths.Themechanismsthatmaycontribute tothislinkandcauseatherogenesisandthromboticevents includebacteremia,chronicin fl ammation,andendothelial dysfunctioncausedbythePD.ThetreatmentofPDcanlower theriskforCVDeventsandimprovethepatient’satheroscleroticpro fi leandvascularfunction.Conversely,thefailureto maintainoralhygieneislikelyaCVD-linkedriskfactor.Daily oralhygieneself-care(OHS)isanessentialpartoftheprimary preventionofPD.Researchershaven’talwaysfoundsuf fi cient supportfortheadjunctiveoralhealthbene fi tsof fl ossing comparedtotoothbrushingalone.However,homeinterdental cleaningdonecorrectlycanreducetheburdenoforaldiseases andimprovePDparameters.Withthisbackground, fl ossing mayimprovePDparametersandcouldofferaddedsystemic bene fi ts.Anationwidedatabasewasevaluatedtodetermine theimpactofself-reported fl ossingbehavioronCVDprevalenceandmortalityrisk.
ThedataweretakenfromtheNationalHealthandNutritionExaminationSurvey(NHANES)2009-2010,2011-2012,20132014,and2015-2016.Asampleof18,801individuals(meanage about53years)wasaskedtoprovide flossingbehaviordata. Theparticipantsweredividedintogroupsasfollows:not flossing (0days/week[d/wk]),occasional flossing(1-3d/wk),frequent flossing(4-6d/wk),anddaily flossing(7d/wk).Theprimary outcomewasprevalenceofmajorCVDeventsandwasbased onaskingparticipantsiftheyeverreceivedadiagnosisofcongestiveheartfailure,coronaryheartdisease,angina,heartattack,or strokefromahealthcareprofessional.Mortalitywasmeasured basedonNationalCenterforHealthStatisticsandtheNational DeathIndexdata.PlasmaC-reactiveprotein(CRP)levelswere alsomeasuredin3ofthe5NHANEScomponents.Covariates includedage,sex,race,ethnicity,educationlevel,smokingstatus, alcoholconsumption,energyintake,HealthyEatingIndex(HEI) score,andphysicalactivityusingthemetabolicequivalentsof task,bodymassindexandincome-to-povertyratio.
Theprevalenceofthe fl ossingcategorieswasabout31%not fl ossing,25%occasional fl ossing,about12%frequent fl ossing,
andabout32%daily fl ossing.Signi fi cantdifferenceswerefound forthecovariatesbasedon fl ossingbehavior.Thosewhodidn’t fl ossdailywereyounger,moreoftenfemale,hadhighereducationandincomelevels,andweremorelikelytoengageinleisure timephysicalactivityandlesslikelytosmokeordrinkalcohol. Daily fl ossershadlowerenergyintakeandbetterHEIscores thannon fl ossers.
Flossingbehaviorwasdirectlyassociatedwiththeprevalenceof self-reportedCVDeventsevenafteradjustingforcovariates. Eachadditionaldayof flossingsignificantlyloweredthelikelihood ofbeingassociatedwithaCVDevent.
Aninverserelationshipwasfoundbetween flossingbehaviorand all-causemortality.Theinverserelationshipremainedsignificant evenwhenadjustmentsweremadeforHEIscoreandenergy intake,metabolicsyndrome,andCRP.
Afteradjustingforageandsex,thedaily flossinggrouphada52% decreasedriskofexperiencingCVD-linkedmortalitycompared tothenonflossinggroup.Evenwithadjustmentsforvariouscovariates,theinverseassociationbetween flossingbehaviorand CVDmortalityremainedsignificant.
FlossinglessfrequentlywasaccompaniedbyhigherconcentrationsofCRPinthe2009-2010and2015-2016NHANEScycles.
Thisrelationshipremainedsignificantevenafteradjustingfor covariates.
Whenindividualshavepoor flossingbehavior,theyputthemselvesatriskforahigherprevalenceofCVDevents,ahigher riskfordyingfromaCVDcause,andhavingelevatedCRPlevels.
Dentalprofessionalsshouldencouragepatientsto flossdailyandinformthepatientsofthebene fitsofdoingthis.Inaddition,cardiologistsshouldadvisepatientstoimprovepersonaloralhygienepractices alongwithofferingthemguidancewithrespecttotheir dietandexerciseregimen.
PhilipN,TamimiF,Al-SheebaniA,etal:Theeffectofselfreported flossingbehavioroncardiovasculardiseaseeventsand mortality. JAmDentAssoc 156:17-27,2025
Reprintsavailablefrom NPhilip,CollegeofDentalMedicine,Qatar Univ,Office160C,BldgH12,Doha,Qatar;e-mail: nphilip@qu.edu.qa
Earlychildhoodcaries(ECC)affectschildrenunderage6years andisdefinedasthechildhavingatleast1decayeddeciduous tooththatwaslostduetocariesorrestored.InBrazil,ECCaffectsabout54%ofpreschoolers,usuallythosefromlowincomefamiliesand/orthosewholiveinruralareaswithout goodaccesstodentalcare.BothtreatmentandpreventivemeasuresareneededwithECC.Follow-upvisitsallowdentiststo determinewhichmeasuresaremosteffectivetoavoidprogressionofthecaries.Twomeasuresthathavebeensuccessfulare atraumaticrestorativetreatment(ART)andsilverdiamine fluoride(SDF).WithART,decayedtissuesareselectivelyremoved usinghandinstrumentsandthecavityisrestoredwithhighviscosityglassionomercement(GIC).ARTcanbeperformed inareaslackingelectricityandrunningwaterandcausesless
discomfortcomparedtoconventionalcariestreatment.Asa result,it’iswellreceivedbychildren.SRTisalow-cost,easily appliedtopicalcariostaticagentthatarrestscarieslesionsinchildren.It’snoninvasive,doesn’trequiretheremovalofdecayedtissueorsealingofthecavity,andisconsideredsafe.Theprimary adverseeffectswithSDFarethestainingoftheskinandthecaries lesion,butparentsareoftensatis fiedwiththeappearanceoftheir child’stoothafterSDFapplication.Theoutcomesachievedbythe 2methodswerecomparedinpreschoolersinBrazil.
The118preschoolers(age2to5years,meanage3.53years) wereevaluatedforgeneralhealthanddentalhistory,clinical andradiographicexaminationresults,andthedecayedormissing teethduetocariesor filledtoothindex(dmf-tindex).Theclinical
examinationnotedcariestissuetextureashardorsoft,andthe cariesactivitywasclassifiedasactiveorinactive.Parentsprovidedsocioeconomicandsociodemographicdata,dietaryinformation,informationaboutnonnutritivesuckinghabits,oral hygienebehaviors,and fluorideexposure.Recallexaminations weredoneafter6,12,18,and24months,notinghowmanyarrestedcarieslesionswereintheSDF(test)groupcomparedto theART(control)group.Secondaryconcernsincludedtime foreachtypeoftreatmenttobeperformed,possibleadverseeffects,parentalaestheticperception,childanxietybeforeandafter treatment,andbehaviorofthechildduringtreatment.
Ninety-eightchildrencompleted12monthsoffollow-upand46 completedupto24months.At6months,therateofarrestedcaries lesionswas84%intheSDFgroupand92.9%intheARTgroup.After 12months,thevalueswere91.5%fortheSDFgroupand90.2%for theARTgroup.Atthe18-monthfollow-up,theSDFgrouphada rateof72%andtheARTgrouphadarateof90.9%.At24months, theratewas72%fortheSDFgroupand95.2%fortheARTgroup.
Consideringtheteeththatwereratedasunsuccessfulbecauseactive carieswaspresent,5hadspontaneouspain(3intheSDFgroupand2 intheARTgroup)and2had fistulas(1ineachgroup).IntheART group,8childrenhadtherestorationcompletelyorpartiallyrebuilt after6months,7wereredoneafter12months,and1eachneeded repairatthe18-monthand24-monthfollow-upvisits.
Treatmenttimeaveraged6.08minutesintheSDFgroup,witha medianof6.00minutesintheARTgroup.TheARTgrouphada significantlylongermeantreatmenttimethantheSDFgroup.
Twenty-sixadverseeventsoccurred,with12intheARTgroupand 14intheSDFgroup.TheARTgroupreportedpainorsensitivityin theteethmostoften,withtheSDFgroupreportingspotsorpigmentationoftheskinormouthinmost cases.Sevenofthepreschoolers
hadadverseeffectsineachgroupaccordingtotheparents.TheSDF groupcomplaintsincluded2regardingtheappearanceoftheteeth.
Anxietywasevaluatedbutdidnotdifferbetweenthe2groups. Patientbehaviorwasalsosimilarinthe2groups.Positive behaviorwasobservedin45childrenintheSDFgroupandin 40childrenintheARTgroup.
TheabilityoftheARTandSDFtreatmentstoarrestdentincaries inprimarymolars,theanxietyofthechildren,theadverseeffects, theaestheticperceptions,andthepatients’ behaviorduringtreatmentdidn’tdiffersigni ficantlybetweenthe2groups.SDFwas appliedmorequicklysothepatienthadminimalchairtime comparedtoARTtreatment.
SDFwasfasterandlessinvasivethanARTintreating carieslesions.Thismightmakeitabetterchoicefor youngerchildren.TheaestheticsofSDFapplications wasaconcernforsomeparents.ARTwasaseffective asSDF,althoughitrequiredmoretimetoperformthe proceduresandwasmoreinvasive.
RodriguesGF,VolluAL,VargasTR,etal:Efficacyof30%silver diamine fluoridecomparedtoatraumaticrestorativetreatment inarrestingdentincarieslesionsinpreschoolers:Arandomized clinicaltrial. ClinOralInvest 29:3,2025
Reprintsavailablefrom AFonseca-Gonçalves,DeptdeOdontopediatriaeOrtodontia,FaculdadedeOdontologia,UFRJ,R.Prof. RodolphoPauloRocco,325,21941-617RiodeJaneiro,RJ,Brazil; e-mail: afgoncalves16@yahoo.com
Periodontitisaffectsabouthalfoftheglobalpopulation,makingit theseventhmostprevalentdiseaseworldwide.Thisdiseaseprogressesthroughthepresenceofdysbioticbio film,sotheprimary treatmentgoalistoreduceharmfulmicroorganismsandrestore ahealthy floraaroundteeth,whichcreatesabiologicallycompatiblerootsurfaceforreattachment.Theuseofprofessional
mechanicalplaqueremoval(PMPR)canachievethat,buteffectivenessvarieswithfactorssuchasthepresenceofdeepprobing depthsandhard-to-reachareas.Toaddressthissituation,it’ s beenproposedthatprobioticsbecombinedwithotheradjuvants tosubgingivalinstrumentation.Antibioticsareoverusedandhave contributedtothedevelopmentofresistantbacteria.Understandingthemechanismofactionofprobioticsastheymodify
themicro floraofperiodontalpatientsisanessentialelementin craftingeffectivetreatments.Probioticscompetewithperiodontalpathogens,reducetheimmunogenicityofthemicro flora, modulateimmunologicalandin flammatorypathways,andreduce inflammation.Theresultisimmunologicalhomeostasisandthe preventionofplaqueformationbyloweringsalivarypHandinhibitingthegrowthofbacteria.Aliteraturereviewidentifiedarticlesdealingwithadultperiodontitispatientsingoodgeneral healthwhoweretreatedwithPMPRandvariousprobiotics versusPMPRalone.Thegoalwastodeterminetheeffectiveness ofthevariousapproachesintermsofprobingpocketdepth (PPD)reduction,clinicalattachmentlevel(CAL)gain,and bleedingonprobing(BOP)reduction.
ThesearchwasdoneintheMEDLINE(viaPubMed),LILACS,CochraneCentralRegistryofControlledTrials(CENTRAL),GoogleScholar, ClinicalTrials.gov,andDANSEASYArchive databases.Thirty-threearticlescovering1290patientswere identi fied.Follow-upperiod(shortorlong)wasdonetostratify the findings,andsensitivityanalyseswereconductedbasedon probiotictherapyduration.Theprobioticsincluded Bifidobacterium,Bacillus,Lactobacillus,Streptococcus, and Saccharomyces alone orincombination.Theprimaryclinicalparametersassessed wereprobingpocketdepth(PPD),clinicalattachmentlevel (CAL),andbleedingonprobing(BOP).ThesecondaryparametersweremeanchangesinBOP,plaqueindex,andcolonyformingunits(CFUs).Networkmeta-analyseswerealsodone.
Inshort-termstudies,8probioticinterventionscombinedwith scalingandrootplaning(SRP)hadsignificantlygreaterreductions inPPDthanSRP+placebo(Splac).Themeandifference(MD) wasfrom0.18mmwithSRP+ BifidobacteriumlactisDN to 1.48mmwithSRP+ Lactobacillusreuteri. Inlong-termstudies, SRP+ LreuteriDA signi ficantlyreducedPPDwithanMDof 0.80comparedtoSplac.
Inshort-termstudies,16probioticinterventionscombinedwith SRPproducedsigni ficantlymoreCALgainthanSplac.TheMD wasfrom0.16mmwithSRP+ BlactisDN to1.05mmwith SRP+ Lacidophilus,Lrhamnosus,Blongum ,and Saccharomycesboulardii.Inlong-termstudies,2probioticinterventionscombined withSRPproducedsigni ficantlymoreCALgainthanSplac.The MDwasfrom0.32mmwithSRP+ Lreuterisingle to0.43mm withSRP+ Lreuteriincremental
Inshort-termstudies,4probioticcombinationswithSRPhada significantreductionofBOPcomparedtoSplac.TheMDwas
from13.26%withSRP+ LreuteriD to33%withSRP+ Lreuteri AA.Inlong-termstudies,4probioticcombinationswithSRP significantlyreducedBOPmorethanSplac.TheMDwasfrom 5.02%withSRP+ Streptococcusoralis,uberis, and rattus to 23.31%for Slreutincrem.
Studiesthatlastedamonthorlessdemonstratedheterogeneity oftheanalysisthatdecreasedfromconsiderabletonotimportant.Forthoselastingmorethan1month,theheterogeneityremainedgreaterthan70%.Noclinicallyrelevantchangeswere observed.Short-termstudiesofBOPretainedconsiderableheterogeneityatmorethan70%.Noclinicallyrelevantchangeswere noted.
ThebestprobioticregimenforPPDandBOPreductionandCAL gainis Lactobacillusreuteri. Whenthisprobioticwasusedin conjunctionwithSRP,itwasthemosteffectivewhetherthestudy wasashort-termorlong-termevaluation.Combining Lactobacillus with Bifidobacterium and Sacharomyces mayhaveabetter impactonCALgaininstudiesthathaveafollow-upofatleast 3months.
Thedurationoftheprobiotictherapydirectlyaffectedthesuccess oftheintervention.AlthoughmostprobioticscombinedwithSRP couldimprovePPDandCALoverSplac,thecertaintylevelswere verylow.Inaddition,nearlyallthestudiesshowedthatgroups withsubgingivalinstrumentationreceivingprobiotictherapyhad moreCFUreductionsthanthoseintheplacebogroup.
Probioticscombinedwithprofessionalmechanical plaqueremovalmayhavearoleinimprovingtheclinicalparametersusedtoevaluatetheresultsofperiodontaltherapy.Integratingprobioticsinto periodontaltreatmentprotocolscouldcontributeto avoidingadverseeffectsandnotexacerbatingthe problemofantibiotic-resistantbacteria.
DuartedeMendonçaC,PereiradaMataADS,AzevedoLFR, etal:Probioticsinthenon-surgicaltreatmentofperiodontitis: Asystematicreviewandnetworkmeta-analysis. BMCOralHealth 24:1224,2024
Reprintsavailablefrom DNdaSilvaMarques;e-mail: duarte.marques@campus.ul.pt
Techniqueshavebeendevelopedthatcanpreventunintended pulpexposure,makingthetotalremovalofdeepcarieslesions, alsocalledselectiveremovalto firmdentin(SRFD),aless preferredprocedure.Astep-wisecariesremovaltechnique (SW)wasintroducedthatincludesabreakbetweenthe2steps andaimstostimulatereactionsfromthepulp-dentincomplex. Becauseofshortcomingswiththistechnique,selectiveremoval ofsoftdentin(SRSD)wasdeveloped,whichinvolvesselectively removingthecarieswithinasinglesession.Thistechniquehas beenrecommendedforthetreatmentofdeepcarieslesionsextendingthree-fourthsofthewayintodentin.Fewstudieshave evaluatedthelong-termclinicaloutcomeofSRSDinpermanent
teeth.ThevitalityofteethtreatedwithSRSDorSRFDand whetherbaselinevariablesorcalciumhydroxide(CS)application affectsoutcomeswereevaluated.
The165teethin134patients(age13to44years,77femaleand 57male)weredividedintoanSRSD(test)groupandaSRFD (control)group.TheSRSDgroupwasdividedintoasubgroup ofSRSDwithCS(45teeth)andSRSDwithoutCS(45teeth). Teeththathadpulpexposure(PE)duringcariesremovalwereassignedtothePEgroup(29teeth).Thevitalityoftheteethwas testedthroughclinicalandradiographicexaminationafter5
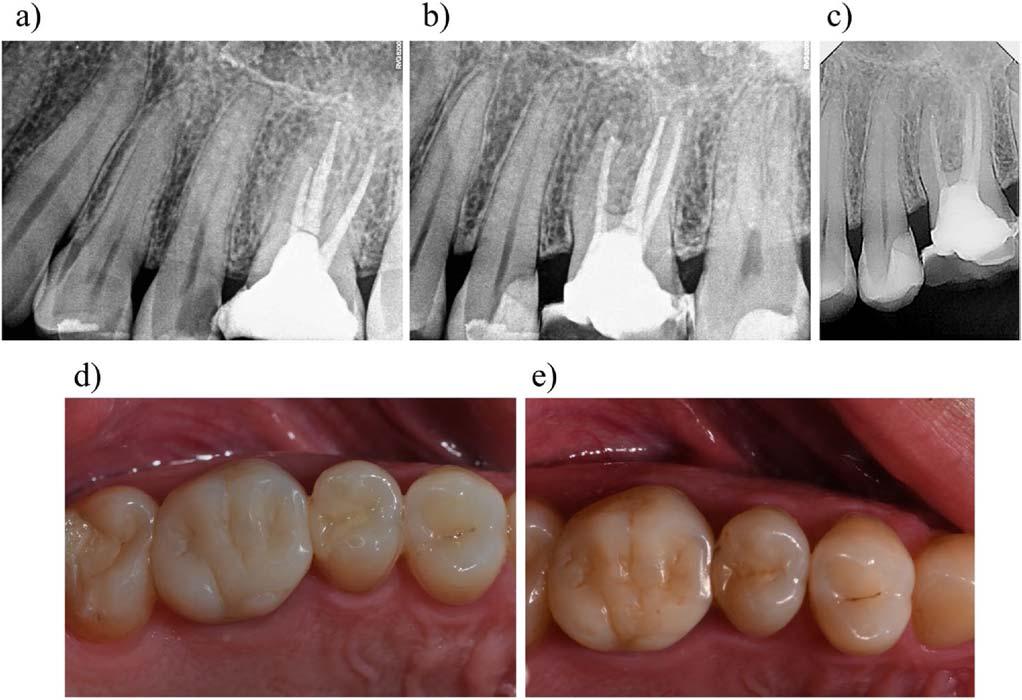
Figure4. Radiographyoftooth#25treatedwithSRSDwithCSat(A)baseline;(B)immediatelyaftertreatment;(C)at5-yearfollow-upwithdentinbridge formation,photographyofrestoration;(D)atbaseline;and(E)5-yearfollow-upwithacceptableFDIscores.(CourtesyofGozetici-C Ë ilB,C Ë etinT,BittarA, etal:Clinicaloutcomesofselectiveremovaltosoftdentinversus firmdentinfordeepcarieslesions:Arandomizedcontrolledtrialupto5years. ClinOral Invest 29:23,2025.)
years,whentherewere31teethintheSRSDwithCSgroup,34 teethintheSRSDwithoutCSgroup,33teethintheSRFDgroup, and22teethinthePEgroup.Restorationswereevaluatedfor integrityandqualityusingtheFDIWorldDentalFederation criteria.TheeffectofbaselinevariablesandCSapplicationon treatmentoutcomewasevaluated.
Inthe5-yearanalysis,thesuccessrateofSRSDwithCSwas100% andtherateforSRSDwithoutCSwasabout94%,bothofwhich weresignificantlyhigherthantheSRFDrateofalmost76%and thePErateofnearly82%.Amultivariateanalysisshowedhigher successratesforteethwithSRSDwithorwithoutCScompared toteethmanagedwithSRFD.
Thesuccessratesrelatedtobaselinevariablesweresignificantly higherforpremolarsthanmolars,forlesionsextending three-fourthsofradiographicdepthcomparedtothosemore thanthisfar,andforteethwithoutpreoperativesensitivity comparedtoteethwithmoderateorseverehypersensitivity. Similarresultswerenotedfortheimpactoftoothtypeon treatmentoutcome.Noneoftheotherbaselinevariableshada significanteffectonoutcomes.
Whensurvivedrestorationswereconsidered,dentinbridge formationwasmostlikelyinthePEandSRSDwithCSgroups (Figure4).Cavitytypeanddepthinfluenceddentinbridge
formation,withCSapplicationafterSRSDindeepercavities leadingtothisimprovedhealing.
ThesuccessrateofSRSDwasgreaterthanthatofSRFD.Toothtype affectedoverallsuccessandCSapplication,cavitytype,andradiographicdepthinfluencedtheformationofadentinbridge.
TheuseofSRSDwithorwithoutCSmayofferagood approachtomanagingdeepcarieslesions.CSoffers anantimicrobialeffectthatmightstimulatereactive andreparativedentinogenesis.
Gozetici-ÇilB,ÇetinT,BittarA,etal:Clinicaloutcomesofselectiveremovaltosoftdentinversus firmdentinfordeepcarieslesions:Arandomizedcontrolledtrialupto5years. ClinOralInvest 29:23,2025
Reprintsavailablefrom BGozetici-Çil,DeptofRestorative Dentistry,SchoolofDentistry,IstanbulMedipolUniv,Birlik Mah.BahçelerCad.No.5,Esenler,Istanbul34250,Turkey; e-mail: bgozetici@medipol.edu.tr
Nofountainofyouthhasbeenfoundyet,butresearchshowsthatgeneticsarejustonepartofourlengthandqualityoflife.Instead, lifestylechoicesplayasubstantialroleinhowwecanlivelong,healthylives.Dietandexercise thingsthatwecancontrol havea significantinfluenceonourlongevity.AmandaBoyce,HealthScientistAdministratorattheNationalInstituteonAging,explained, “Thequestionwereallyshouldbeaskingandfocusingoniswhatishealthyagingandhealthspan,notlifespan.” Currentscienti fi c evidenceindicatesthebest,mostactionablerecommendationsforlivinglongerandaginggracefullyinvolvediet,weightloss, limitingsitting,increasingexercise,andnotsmoking.
TryaMediterraneanorJapanesedietbecauseresearchconsistentlyassociatesthemwithimprovedlongevityanddiseaseprevention.Bothemphasize fishasasourceofproteinaswellasrichinbrain-boostingandheart-healthyfats;wholevegetables,whether freshorfermented;andfewheavilyprocessedfoodsorsugars.KristinKirkpatrick,anutritionistattheClevelandClinic,advises, “Focusononecomponentatatimeandmakesureit’ssomethingthat fitswithinyourpersonal,religious,and/orculturalpreferences.Forexample,ifyouenjoylentils,usetheminsteadofwhitericeinveggiebowls.Butifyoudislike fish,thenfocusonother sourcesofprotein.”
Obesityislinkedtocardiovasculardisease,diabetes,otherchronicillnesses,andashorterlifespan.Sheddingafewexcesspounds canhaveahighlybene ficialeffectonlongevityandoverallhealth.Learnabouttheidealbodyweightforyourage,sex,andheight.A lossofjust5%ofyourbodyweightcansigni ficantlyimpacteverythingfrombloodsugartobloodpressure.FrankB.Hu,Professor ofNutritionatHarvardT.H.ChanSchoolofPublicHealth,says, “Clinicaltrialshaveshownthatweightlossachievedthrough lifestylechanges,medicationssuchasGLP-1agonists,orweightlosssurgeriesisassociatedwithareducedriskofchronicdiseases, includingdiabetes,cardiovasculardisease(CVD),andcertaincancers,andprematuredeath.”
Todayweallowmoresedentaryhabitsinourlives,butscienceisshowingthenegativeeffectsofsitting.Husays, “Sedentary behavior,suchasprolongedTVwatching,hasbeenassociatedwithanincreasedriskofchronicdiseases,includingdiabetes, cardiovasculardisease(CVD),andprematuredeath.Thisheightenedriskisprimarilyattributedtoincreasedobesityandthe displacementofphysicalactivity.” Evenifyouexerciseregularly,sedentarybehaviorcarriesserioushealthrisks.Increaseyour physicalactivitythroughouttheday,evenifit’sjustwalkingaroundyourhouseorof ficeandevenifyoualreadyexerciseregularly.
Thebene fitsofregularexercisedon’tjustfocusonyourbodybutalsoonbrainhealthandcognition.Amongolderadults,cardiorespiratory fitnessisanexcellentindicatorofbrainhealth,includingmemory.Findwaystoincreasephysicalactivity,cutdownon sedentarytime,andenjoythehabitsoit’ssustainable.Adultsshouldgetaminimumof150minutesaweekofmoderate-intensity physicalactivity.Establishinghabitsthatsimultaneouslyreducesedentarybehaviorsandincreaseactivityisperfect.Boyceadds, “Youcanalsobuildphysicalactivityintoyoureverydaylife.Forinstance,getoffthetrainonestopearlyandwalkorbundle behaviorslikeonlywatchingTVwhileyou’reexercising.”
Thesciencestillsaysifyoustopsmokingyouwilllivelonger.AstudyledbyHushowedthat “ never ” smokingisakeyfactorfor prolonginglifeexpectancy.Othersaremaintainingahealthyweight,engaginginregularphysicalactivity,eatingahealthydiet,and onlyconsumingalcoholinmoderation.Smokingcessationlowersyourriskofeverythingfromcancerandheartdiseaseto diabetesandchronicobstructivepulmonarydisease(COPD)andcanaddupto10yearstolifeexpectancy.
Theexpertsgavethefollowingrecommendationsforlongevity:
Maintainahealthybodyweightthroughdietandexercise. Whateveryou’redoingforphysicalactivity,add30moreminutestoit. Moveyourbody.
Thinkholisticallyaboutthingsotherthaneating includingexerciseandsleep. Matchyourdietarypatterntoyour “why.” Ifyourwayisnotwantingtosufferdementialikeyourmother,payattentiontorelevantsupplements,adequateexercise,andanutrient-speci ficpatterncoupledwithstressmanagementandpropersleep. Don’tlookforaquick fixbutadopthealthylifestylehabitsifyouwantalongerlife.
[MammoserG:5Science-BackedWaystoLiveaLongerLife. Healthline.com, Jan2,2025]
Whenweareworking,playingwithoursmartphones,orgoingsomewhere,about70%to75%ofusarealsoeating.Being flexible withwhereweeatandhavingdistractionsatthesametimeaseatingcanseemlikemultitaskingandagoodthing.Studiesshowthe opposite:whenwe’redistractedwetendtoeatmore,weofteneatagainsooner,andasaresult,wegainweight.Distractionsalso preventusfromactuallytastingorenjoyingwhatwe’reeatingandwemissthesignalsinourbrainthattelluswe’vehadenough. Whenweeat,ourgutsreleasesatietyhormones,includingleptin,ghrelin,andGLP-1.Thesesignalourbrainsthatwe’regetting full,whichtakesabout20minutes.Distractionsaddcognitiveloadstoourbrainsthatcompetewithandreduceourabilitytosense howmuchwe’veeaten,howfullweare,andhowthefoodtasted.A2013studyledbyLottevanDillen,professorofsocial psychologyatLeidenUniversity,had42subjectssweetentheirownlemonadewithgrenadine.Someweredistractedbyan easycognitivetest,andothershadaharderone.Thosecalledontodothehardertaskadded50%moresugarysyruptotheir drinksbutdidn’treportthedrinkassweeterthanthosedoingtheeasiertask.
Adistractedbrainhaslessactivityintheinsula,wheretasteisprocessed,andtheprefrontalcortex,whichcarriesouthigher-level cognitiveprocesses.Theconnectivitybetweentheinsula,prefrontalcortex,andnucleusaccumbens,whererewardisprocessed, isdisrupted.Thesedistractionsblunttastessuchashigh-fat,bitter,sour,salty,andumamianddullourabilitytosmellfood.Allof thesesensesarepartoftheenjoymentoffood,soweenjoyitlessandtendtomakeupforourlackofenjoymentbyoverindulging, calledhedoniccompensation.
Eatingslowerandmoremindfullygivesusmoretimetosensesatietysignals,tastethefood,andreduceconsumption.Chewing morecanalsodecreasehowmuchfoodpeopleconsumeandhowhungrytheyreportfeeling.Eatingmindfullyincludesdecreasing distractions,planningmeals,andtryingsensoryeating.Manydistractionswouldberemovedifweputourmobiledevicesawayor switchedthemoff.Thiscanbeimpractical,unrealistic,andcertainlynotfun.KatyTapper,professorofpsychologyatCity UniversityofLondon,said, “Everyonehastoeat,anditissomethingthatbringsusalotofpleasureandisboundupinallsorts oftraditionsandoursociallives.” Shecautionsthatallthoseaspectsneedtobebalancedwithhealthyeating.Shefoundthat socializingwhileeatingisn’tassociatedwithahigherbodymassindexandspeculatedthatconversationtypicallyisn’tdonewhile we ’retalkingandpeopletendtoeatslowerinsocialsettings,makingthemmorelikelytosensethesignalsforfullness.
Mealplanningcaninvolvesettinghoursforeatinganddrinking.Duringthesetimes,thefocusshouldbeonthejoyfulnessofthe experience.Insensoryeating,younoticethetaste,smell,look,andfeelofthefood.Beingmoreawareofthesesensoryproperties canreducehowmuchyoueatandincreaseyourenjoyment.Easingintosensoryeatingmightbehelpedbypretendingtobeafood criticandimagininghowyouwoulddescribethefood.
Mindfuleatingincludespayingattentiontointernalfeelingsofhungerandfullness,noticingwhatpromptsyoutoeat,andtakinga nonjudgmentalviewoffood-relatedthoughts.Moreresearchisneededtoinvestigateallthatmakesupmindfuleatingandhow effectivethecomponentsareinachievinghealthyhabits.Evenifyouareeatingdistracted,youcanperiodicallybringyourattention backtothefoodyou’reeating.
[SimaR:DistractedEatingCanMakeUsGainWeight.MindfulEatingCanHelp. TheWashingtonPost, Jan9,2025]

Greetings from the International Headquarters!
Spring has officially started here in and around the Washington, DC area, and this past week was the peak time for our cherry tree blossoms around the tidal basin. As many of you may know, this area is renowned for its many cherry trees which are a reminder of the renewal of spring and the spirit of international friendship since the trees were a gift from Japan.
The Pierre Fauchard Academy is off to a quick start this year. We have already conducted several induction meetings in the US, including in Arkansas, Hawaii, Illinois, Kansas, Louisiana, Massachusetts, Oklahoma, Pennsylvania, and Utah, as well as a joint induction meeting in Georgia for new Fellows from Alabama, Florida, and Georgia. Internationally, new induction programs were held in The Netherlands and Poland. We welcome all our new PFA Fellows!
By now, all PFA Fellows should have received an email from Elsevier (the publisher of Dental Abstracts and Dental World). This email, sent in mid-March, gave detailed instructions on how to log in to access your online subscription to Dental Abstracts / Dental World – a key part of your member benefit when you maintain your status as a current Fellow.
I am also happy to report that, thanks to the hard work of our Continuing Education Committee, we received acceptance as a Program Approval for Continuing Education (PACE) provider from the Academy of General Dentistry. Starting soon, all CE programs will adhere to the PACE requirements and CE credits will be available from PFA as an Approved PACE Program Provider.
The PFA Board of Trustees recently concluded its interim Board Meeting here in the Rockville, MD office. The Board spent a full day on strategic planning and a second day on the work of the PFA. The good news is that we are in excellent financial shape, and the addition of over seven hundred new Fellows in 2024 helped us reach our goal. The second big piece of news from the Board Meeting was a PFA Bylaw change agreed to by the PFA Board. This change entails the removal of the position of PFA Past President from the PFA Officers and Trustees, which will save our organization travel dollars. PFA Past Presidents had no official duties while serving as a member of the Officers and Trustees and going forward will officially become President of the PFA Leadership Foundation at the conclusion of their term as PFA International President.
The other item to report following our Board Meeting is the work of an ad hoc Committee that has been studying the current structure of PFA Regions and Sections and has also conducted an analysis of Section Dues. The Committee reported excellent progress to date, while much work remains. The only significant change to date is that PFA Trustees will now be able to re-organize Sections within their Region to maximize support.

I would also like to reemphasize that leaders listen to those around them, and that we look to you as leaders in dentistry for your guidance and support. As a leader it is, of course, always important to recognize that you may be in a position of leadership and to consider whether you are actually leading. Are you a leader of courage, or a leader of comfort? As John Maxwell once said, “He that thinketh he leadeth, and hath no one following, is only taking a walk.” PFA Fellows around the world are leading their communities to better oral health. As an organization, the PFA could ask for nothing better.
Please also remember to nominate your colleagues for Fellowship in our outstanding organization; the nomination form on the website is simple to complete.
Last but certainly not least, I look forward to seeing many of you at our Annual PFA Gala on October 25, 2025, in Washington, DC!
Sincerely,
—Mr robert Cattoi, Executive
Director
of the Pierre Fauchard Academy
The Pierre Fauchard Academy publishes the Dental World as a service to its Fellows and it is distributed as part of the Dental Abstracts Journal.
Please send change of address information or subscription inquiries to the Central Office of the Pierre Fauchard Academy at:
Pierre Fauchard Academy 103 North Adams Street, Rockville, MD 20850.
E-mail: centraloffice@fauchard.org Phone: +1 (240) 658-8070
Please send to the Dental World Office for possible publication any editorials, or articles and photos about PFA Section activities, or Foundation grants and scholarship activities. Please contact the Dental World Editor for more information.
Dental World Office: Email: drfionacollins@gmail.com
Dental Abstracts Senior Publisher: Annie Zhao, Elsevier
Dental Abstracts Editor-In-Chief: Dr. Douglas B. Berkey
Dental Abstracts Journal Manager: Sangamithrai S, Elsevier
Dental World Editor: Dr. Fiona M. Collins
Greetings to all Fellows.
The future of the Pierre Fauchard Academy looks bright, and we are in the process of growing at a record-breaking pace. We all play a part in this expansion, including our Trustees and Section Chairs who work tirelessly throughout the world. Our Leadership Foundation is also expanding and as it grows and funding increases, the Foundation will be able to offer more philanthropic scholarships, volunteer assistance, and continuing education.
Since humbly assuming my role as our International President, I have been reminded of the esteem in which the PFA is held internationally. Our Sections

look to our Trustees and Section Chairs to guide them and encourage participation, while we must all adhere to our bylaws. At times this can be challenging due to both the global nature of PFA and geographical distances from our international headquarters.
To date, I have met with Sections in several locations and regions while serving as our International President. In November 2024, I was welcomed in India to participate in three PFA induction ceremonies. A graduation was also scheduled for Sri Lanka in April. The first induction ceremony took place in Bengaluru (Bangalore) India, an area that is part of our Asia-at-large section and that is staying active in the PFA.

PIERRE FAUCHARD ACADEMY www.fauchard.org

Eighteen new Fellows were installed, and introduced themselves with a short bio – this proved to be a very meaningful way to enhance graduation. Thank you to Dr. Nagesh and Dr. Prasad who together planned this lovely and intimate event.
The second induction ceremony in the Asia-at-large Section was conducted in Delhi, India. While in Delhi, over one hundred dentists were installed as Fellows in a beautiful event that was sponsored by the company Cynodent. All details were meticulously arranged, and excellent continuing education courses were offered. This area is led by Dr. Anmol Bagaria (Chair) and Dr. Ashish Pandey (Co-chair), a dynamic duo that is inducting a large number of new Fellows in this area and beyond.
The third induction ceremony in India was held in Indore, India which is part of the oldest Section of the India Pierre Fauchard Academy. During this beautiful event more than one hundred new Fellows were inducted, and excellent continuing education courses were provided. A sincere thank you to Dr.

Maya Ramesh, Dr. Garg (Secretary), and Dr. Chugh (Vice Chair) for executing a well-orchestrated ceremony.
As Mother Theresa once stated, “I can do great things you cannot, you can do great things I cannot. Together we can do great things.”
A Vision for the Future: The Next Chapter for PFA Fellows
Dear Esteemed Fellows, The Pierre Fauchard Academy has long stood as a beacon of leadership, ethics, and professional growth in the dental community. However, with the evolving landscape of dentistry and as we continue to uphold the legacy of excellence in dentistry, it is essential that we look ahead, adapt, innovate, and strengthen our mission.
Our collective responsibility as Fellows is not only to preserve the values
that define our organization; it is also our responsibility to actively contribute to its growth. One of our primary goals is to expand Fellowship engagement by strengthening the bonds between members through collaborative initiatives, leadership programs, and global networking opportunities. By fostering a stronger sense of community, we can ensure that the PFA remains a vital platform for professional connection and advancement.
Another key focus is mentorship and professional development. As leaders in the field, we have an opportunity to guide young and emerging dentists, providing them with the wisdom
Our cherished PFA will succeed and grow in the coming years, and we will all assist in this worthwhile endeavor.
Sincerely,
—Dr. Cheryl braDforD billingsley, International President of the Pierre Fauchard Academy

and support that will help them excel in their careers. Additionally, innovative education is critical in staying at the forefront of the profession. By expanding our mentorship programs and increasing access to continuing education and skill-building resources, we can help shape the next generation of dental professionals while upholding the high standards of practice that define our Academy.
Our commitment to community outreach and service remains at the heart of our mission. Many PFA Fellows are already engaged in humanitarian efforts, serving underserved populations and promoting oral health initiatives worldwide.
Moving forward, we aim to increase our collective impact, ensuring that our contributions continue to make a meaningful difference in the lives of those in need.
As part of our strategic vision, we are also working to strengthen our global presence. Through new partnerships with academic institutions, dental organizations, and healthcare leaders, we can extend our influence and create more opportunities for Fellows to contribute to the profession on an international level.
As a valued Fellow, your insights, experience, and dedication play a crucial role in shaping this vision. We encourage you to get involved in PFA leadership, mentor the next generation, and participate in discussions that drive innovation within the Academy. Whether through leadership roles, humanitarian projects, or professional development initiatives, your contributions will help propel PFA into a new era of excellence. This is an exciting time for our Academy, and we welcome your thoughts,
ideas, and feedback on how we can collectively elevate our mission and impact.
Thank you for your continued dedication and passion for our profession. Together, we can ensure that PFA not only preserves its proud legacy but also thrives for generations to come.
Best regards,
—Dr. ghabi Kaspo, International
President-elect of the Pierre Fauchard Academy

‘Plus ça change, plus c’est la même chose’
Since time immemorial, change has been a constant feature throughout the world. Most recently, it seems that the pace of change has increased greatly, and that it will continue to do so.
For many reasons, societies and their organizations have always faced challenges, such as economic issues, changing social structures, communication and priorities, and intergenerational change. As the saying goes, the more things change the more they stay the same. Our response as the Pierre Fauchard Academy is to understand
the changes that occur and to embrace these.
In the most recent years, we have fostered an increase in communication and collaboration between Sections, such as joint meetings and induction ceremonies, and this trend continues. We also encourage the sharing of Best Practices among our Sections on what works best in engaging our Fellows and adding value. Plus, we are continuing to increase personalized communication, in particular at the Section Chair and Section level. In addition, while virtual events began as a necessity during the COVID-19 pandemic, this is no longer the case –we are now holding virtual events in addition to in-person events to increase
opportunities for participation when it is not practical or feasible to meet in person. Examples include induction ceremonies, such as the recent induction for the ‘Section-at-large,’ and the hosting of webinars. Engaging Fellows in goal setting is also of importance, especially at the Section level where most of our engagement and activities are focused.
As the Pierre Fauchard Academy continues to strengthen, I look forward to working with our Fellows in the coming years.
Sincerely,
—Dr. luis felipe JiMenez squella, International Vice President of the Pierre Fauchard Academy
The Western Australia Section hosted its annual lunch on November 24, 2024, at the Cottesloe Golf Club in Swanbourne, Western Australia. The highlight of the event was welcoming five new Fellows who have made significant contributions to the dental profession, above and beyond the call of duty. Drs. Nick Albatis, Sam Bennett, Lisa Bowdin, Graham Carmichael, and Mohammed El-Hakim were sworn in by Prof. Deborah Cockrell, Trustee for Region 8 (Australasia). We were also delighted to host Commodore (Ret.) Mike Deeks to speak on his years of experience as a submariner and naval officer, providing transferable lessons on leadership.
In keeping with the theme of our meeting, we launched our Fellow Leadership

Initiative. All Western Australia Section Fellows will be eligible for grants (up to $300) from PFA to attend a leadership or management course of their choice. Details to come.

The Hawaii Section of the Pierre Fauchard Academy held its Annual Dinner and CE Meeting at the Oahu Veterans Center in Honolulu on January 29th, 2025. We were delighted to welcome Dr. Dan Castagna, Past International President and currently Treasurer of the Pierre Fauchard Academy. Dr. Castagna administered the oath during the induction of three new Fellows – congratulations to Drs. Anthony Kim, Angela Chin
and Riichiro Sato, as well as Dr. Cecile Sebastian who was inducted at our Annual Gala Induction Ceremony in October 2024 in New Orleans. During our joint ACD/ICD/PFA meeting, the Ethics CE program was given by Dr. Karen Foster, ICD Regent for District 14.
Sincerely,
—Dr. nora harMsen, Section Chair for Hawaii


TheMassachusetts Section of the Pierre Fauchard Academy held its Annual Breakfast Meeting on January 31, 2025. Approximately 45 Fellows were in attendance, as well as Dr. Jay Skolnick, our new Trustee. During the meeting, Dr. Robert Lewando was awarded the Distinguished Dentist Award for his years of service, especially his work in
the access to care arena and in insurance company policy.
Dr. Richman announced that she would be stepping down as Chair of the Massachusetts Section, and that Dr. Cherie Bishop, a long-term Fellow, would be assuming the position of Section Chair for the 2025-26 year. Dr. Moriarty will continue in her position as Vice Chair.



The Oregon Section Annual meeting was held in conjunction with the International College of Dentists and the American Collee of Dentists meetings, as most of our members are involved with multiple honors societies. During the meeting, we inducted Dr. Julie Spaniel as a new PFA Fellow. Dr. Spaniel is an outstanding dentist and philanthropist, and she provided us with an update on her most recent projects running a school and opening a dental clinic in Kenya.
We also discussed future coordination of our annual event with the ICD and ACD, and recruiting efforts, and made a plan to work together on a new annual event which would include speakers, mission trip planning, and social time.
Sincerely,
—Dr. anthony raMos, Section Chair for Oregon

Our mission as Fellows in the Pierre Fauchard Academy is to recognize and develop outstanding leadership in our profession, internationally.
Central Office:
Robert Cattoi, Executive Director 103 North Adams Street, Rockville, MD 20850
E-mail: centraloffice@fauchard.org
Phone: +1 (240) 658-8070
Fax: +1 (240) 266-9188 www.fauchard.org
Cheryl Billingsley, President Virginia, USA
Ghabi Kaspo, President-elect, Michigan, USA

Pankaj Patel, Immediate Past President, Kenya
Luis Felipe Jimenez, Vice President, Chile
Robert Cattoi, Executive Director, Maryland, USA
REGION 1—Europe
Paul O’Dwyer, Ireland
REGION 4—Midwest USA
Kim Gardner, Ohio, USA
REGION 7—Latin America
Federico Perez Diez, Mexico
REGION 10—Central USA
Lucynda Raben, Kansas
REGION 2—Northeast USA Jay Skolnick, New York
REGION 5—Western USA CR Anderegg, Washington, USA
Dan Castagna, Treasurer, California, USA
Pankaj Patel, Secretary, Kenya
Dan Castagna, Treasurer, California
REGION 8—Australasia Deb Cockrell, Australia
REGION 11—Africa Tom Ochola, Kenya
REGION 3—Southeast USA Paul Obrock, Tennessee
REGION 6—Canada Lisa Bentley, Ontario
REGION 9—Asia
Ricardo R. Gatbonton, The Philippines
EDITOR—Dental World Fiona M. Collins, Georgia
Ghabi Kaspo, President, Michigan, USA
Robert Cattoi, Ex officio, Maryland, USA
