




ParadigMS is an independent and non-profit international group of Multiple Sclerosis experts dedicated to improving Multiple Sclerosis patient care.
It contributes to an increased knowledge of Multiple Sclerosis Patient’s care by generalist neurologists and other care-givers (nurses, general practitioners,…) by translating science into clinically relevant medical education to the local level in individual countries.
ParadigMS is independent in the research it conducts, in the educational programs it elaborates, in the opinion that it expresses.
The foundation’s origin is European with board members working in 23 different European, Middle-Eastern and NorthAfrican countries.
Board Members should be active Multiple Sclerosis clinicians and researchers.
The author(s) hereby grant(s) ParadigMS the nonexclusive right to distribute and publish this slide deck on the ParadigMS platform (for users with an online account only). The author, who is compensated for the creation of this slide deck, retains the right to make changes to this slide deck as he sees fit.
ParadigMS is a non-profit foundation and does not sell or make a profit from the distribution of the educational slide deck to health care practitioners. ParadigMS can charge a fee to non-health care practitioners for the use of its digital platform that gives access to all educational content (including the slide decks).
The author remains responsible for observing all copyrights or other intellectual property rights related to the figures, data and research results used in the slide deck.
All ParadigMS slide decks are presented and peer reviewed at expert meetings. Once the peer review process is completed, the slide deck is published on the ParadigMS website and used in educational and training activities.
The experts and board members of ParadigMS
Laura Airas (Finland, University of Turku)
Raed Al Roughani (Kuwait, MS clinic at Ibn-Sina hospital & Amiri Hospitals Kuwait)
Mona Alkhawajah (Saudi Arabia, King Faisal Specialist Hospital & Research Centre Riyadh)
Thomas Berger (Austria, Medical University of Vienna)
Alexey Boyko (Russia, Russian State Medical University and MS Center)
Lou Brundin (Sweden, Karolinska Institutet Stockholm)
Andrew Chan (Switzerland, University Hospital Bern)
Florian Deisenhammer (Austria, Medical University of Innsbruck)
Paolo Gallo (Italy, University of Padova)
Nikolaos Grigoriadis (Greece, Aristotle University of Thessaloniki)
Hans-Peter Hartung (Germany, Heinrich-Heine-University Dusseldorf)
Christoph Kleinschnitz (Germany, Essen University Hospital)
Ralf Linker (Germany, University of Regensburg)
Melinda Magyari (Denmark, Danish Multiple Sclerosis Center)
Celia Oreja-Guevara (Spain, Hospital Clinico San Carlos Madrid)
Carlo Pozzilli (Italy, University of Roma La Sapienza)
Veronica Popescu (Belgium, University MS Center Pelt –Hasselt)
Maura Pugliatti (Italy, University of Ferrara)
Bart Van Wijmeersch (Belgium, University MS Center Pelt -Hasselt)
Patrick Vermersch (France, University of Lille)
Bassem Yamout (Lebanon, American University of Beirut Medical Center)
Magd Zakaria (Egypt, Egyptian Society of Multiple Sclerosis)
Tjalf Ziemssen (Germany, Carl Gustav Carus University Hospital Dresden)
Title of the presentation
Schumacher 1965
Poser 1983
McDonald 2001/2005/2010
Clinical diagnosis
Two relapses affecting two separate sites within the CNS
Laboratory-assisted diagnosis
Positive CSF and evidence for paraclinical abnormalities (MRI or VEP) at a separate site replaces second relapse
MRI-assisted diagnosis
MRI evidence for DIS and DIT replaces second relapse

McDonald Criteria
Ann Neurol 2001;50:121-7
CSF abnormality: –


OCB (preferably by IEF) and/or –
Elevated IgG Index –
WBC < 50/mm3
–
State of the art technology
In context with MS „positive CSF“ means detection of intrathecal synthesis of immunoglobulins as a surrogate of chronic immune activiation
Surrogates of acute inflammation, i.e. elevated cell counts are not suggestive of a „positive CSF“
Normal: <0.7








demyelinating neurol. diseases (n=295)
inflammatory neurol. diseases (n=197)
other neurol. diseases (n=137)
neuroborreliosis
n=18)



SAH excluded!
In 30% of MS patients
clonal expansion occurs without elevated total IgG!

IEF
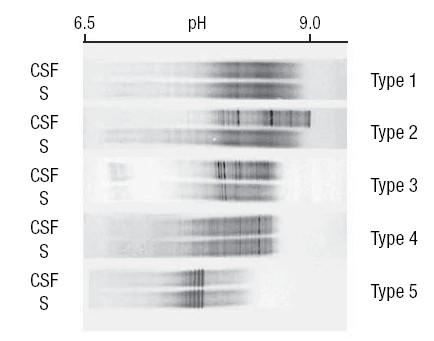 CSF Ser
CSF Ser




If imaging or other tests (for instance, CSF) are undertaken and are negative, extreme caution needs to be taken before making a diagnosis of MS, and alternative diagnoses must be considered.






that + IgG OB pose a risk for presenting a 2nd attack independently of MRI findings:


TintoreMetal.Neurology.2008;70:1079-1083.
TintoreMetal.Brain.2015;138:1863-1874.

OCB+ in 60-70% of CIS patients
Conversion to CDMS best investigated in ON:
– Nilsson et al., J Neurol 2005: Risk for CDMS after 15 years in OCB+ 49% vs. 23% in OCB- (p=0.02)
– Soderstrom et al., Neurology 1998 (n= 143, 72% OCB+)
fig: Probability not to develop MS
OCB+ (n=103) vs. OCB- (n=40)


OCB+
sensitivity for CDMS 96%
specificity 42%
PPV 49%
NPV 95%

• Besides intact immunoglobulins, terminally differentiated B cells (plasma cells) produce Light Chains in excess.

• Immunoglobulins and Free Light Chains (FLC) accumulate in CSF in case of an intrathecal B cell activity
• 3 IgG isotypes: IgG, IgA, IgM

• 2 subtypes: -FLC�� & -FLC��

Data will be added once published……





The concordance was higher between OB and KFLC indexes compared to OB / KFLC indexes and IgG index
The highest concordance occurred between OB and KFLC-6.6, followed by OB and KFLC-5.9

Multicentric: MS n=675, CIS n=90, OIND n=297, NINDC n=559 (no MRI data available)

KFLC index cut-offs:
-MS/CIS vs NINDC: 8.92
-MS/CIS vs OIND: 11.56
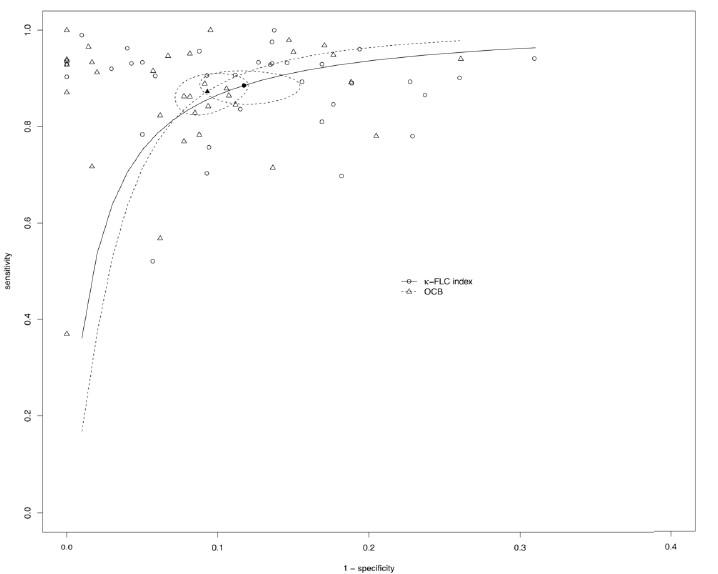
Diagnostic performance, KFLC index vs OB

The KFLC perform slightly better than OB

MOGAD (n=26)
NMOSD (n=18)
ADEM (n=10)
idiopathic myelitis (n=29);
Idiopathic optic neuritis (n=29)
Neurosarcoidosis (n=17)
CNS vasculitis (n=21);
Sjögren syndrome (n=5)
Neurolupus (n=5)
Behçet’s disease (n=5)
Idiopathic LETM (n=10)
Undefined demyelinating disease (n=17)
Autoimmune encephalitis (n=72);
Pachy/Leptomeningitis (n=7)
Aseptic meningitis/meningoradiculitis (n=10)
TolosaHunt (n=4)
Vogt-Koyanagi-Harada syndrome (n=3); CAAri (n=6)
Relapsing meningoencephalomyelitis (n=2);
Hypophysitis (n=1
KFLC index in patients with CIS (Multicentre, n=88)

KFLC index: similar levels if OB negative, regardless of clinical status (CIS-CIS vs CIS-MS)


Single centre, n= 214 CIS. Results: General characteristics
ArrambideGetal.Brain.2022;45:39313942.

The risk for second attack was very similar between KFLC-5.0 and KFLC-6.6
The highest risk for DIS and DIT was demonstrated for KFLC-5.9
ArrambideGetal.Brain.2022;45:39313942.
Both KFLC-5.0 and KFLC-6.6 had the highest sensitivity and a better specificity, with a slightly higher accuracy than OB
Although the IgG index had the highest specificity, its sensitivity was lower than that of OB and KFLC indexes, yielding the lowest accuracy. Its NPV was also the lowest although the PPV was similar to that of OB and KFLC indexes

Results: Estimating cut-offs by outcome
KFLC index cut-offs vary according to the outcome

CSF is a highly specific and sensitive tool for the diagnosis of MS
There is also a prognostic value
CSF examination is important for differentials
New markers (FLC) will increase availablilty, prognostic value and diagnostic performance

The sponsors give a sponsorship for the creation of the educational materials and communication activities without any influence on the content of the presentations.
