A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling
v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
Dr. Mayank Khandelwal
3rd Year Resident (2024)
Department of Dermatology
Guwahati Medical College and Hospital (GMCH) Assam
Dr. Pankaj Adhicari
MD (Dermatology)
Professor and HOD
Department of Dermatology
Guwahati Medical College and Hospital (GMCH) Assam
Introduction
Melasma is an acquired disorder characterized by facial hyperpigmentation, influenced by multifaceted factors. Clinically, it presents as brownish patches or hyperpigmented areas on the skin, predominantly on the face. These patches are typically symmetrical and vary in size and shape, commonly appearing on the cheeks, forehead, upper lip, and chin. The borders
Randomised, Split-face, Comparative
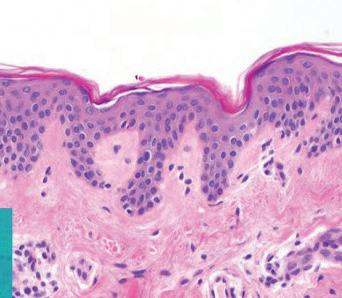
Melasma manifests histopathologically with increased melanin deposition in the skin, affecting either the epidermis, dermis, or both. In the epidermis, melanin accumulates predominantly in basal and suprabasal keratinocytes. Dermal melanin is found dispersed through out the superficial and mid dermis, often localized within macrophages clustered around small, dilated vessels. Unlike other pigmentary disorders characterized by inflammation, melasma typically exhibits sparse or absent inflammatory cells. The pathogenesis involves complex interactions, primarily triggered by exposure to sunlight. UV radiation stimulates the production of melanogenic factors such as alphamelanocyte–stimulating hormone, corticotropin, interleukin 1, and endothelin 1, which activate intraepidermal melanocytes. Additionally, prolonged UV exposure induces dermal inflammation and activates fibroblasts, leading to increased production of stem cell factors that further promote melanogenesis in the dermis.1 Plasmin, a key player in the plasminogen activator system, contributes
to melanogenesis by elevating arachidonic acid and prostaglandin levels in keratinocytes.2
Traditional treatments for melasma encompass topical depigmenting agents, chemical peels, derm-abrasion, and laser therapies, each offering varied outcomes. However, advancements in dermatological interventions have introduced promising alternatives. Intense Pulsed Light (IPL) emerges as a versatile option, capable of targeting both superficial pigmentation and underlying vasculature.3 Microneedling has emerged as a novel minimally invasive procedure used for transdermal drug delivery, including the application of Tranexamic acid (TxA). This method offers advantages such as uniform and comparatively painless drug administration. Moreover, microneedling stimulates collagen production in the upper dermis, which is beneficial in the treatment of conditions like melasma. This dual action of enhancing drug delivery while promoting collagenesis underscores the therapeutic potential of microneedling in dermatological treatments.2 Melasma presents a complex challenge in
dermatology, requiring a deep understanding of its causes. Recent research highlights the role of increased vascularity alongside traditional triggers. Tranexamic acid shows potential due to its effects on both melanin production and blood vessel formation. Combining advanced techniques like IPL and microneedling with tailored medication offers a comprehensive approach to treating melasma, emphasizing personalized care for better results.2, 3
Aim and objectives
To compare the therapeutic efficacy and safety of IPL & Tranexamic Acid (TxA) with Microneedling v/s Tranexamic Acid with Microneedling in the treatment of Melasma.
Materials and Methods
Study Period:
The study was conducted over a period of five months to evaluate the efficacy of a treatment regimen for melasma.
Study Type:
This research employed a prospective randomized split-face comparative study design. In this design, the right side of the face was designated as the
case group, where the intervention was applied, while the left side served as the control group, receiving either no treatment or a placebo.
Study Site: The study took place at the Department of Dermatology in a tertiary care center. This setting ensured access to specialized medical facilities and expertise necessary for the conduct of the study.
Study Sample: A total of twenty-two cases of melasma were enrolled in the study. Participants were recruited based on specific inclusion criteria, which likely included age, melasma severity, and willingness to participate. Comprehensive history-taking and thorough examinations were conducted for each participant after obtaining informed consent. This step ensured that participants understood the study's purpose, procedures, potential risks, and benefits before agreeing to take part.
Ethical Clearance: Prior to the initiation of the study, approval was obtained from the Institutional Ethics Committee. This clearance ensured that the study protocol adhered to ethical guidelines and safeguarded the rights and welfare of the
participants throughout the research process.
This comprehensive approach in the materials and methods section ensures transparency and adherence to scientific standards, providing a solid foundation for evaluating the outcomes and implications of the study on melasma treatment.
The IPL and laser skin resurfacing machine operates through a combination of advanced technologies to deliver effective dermatological treatments. At its core, the system utilizes Intense Pulsed Light (IPL) technology, which emits broad-spectrum
light pulses that target specific chromophores in the skin, such as melanin or hemoglobin. This targeted light energy heats the pigment or blood vessels, effectively reducing pigmentation irregularities, redness, and vascular lesions. In addition to IPL, the integrates fractional non-ablative laser technology. This laser emits micro-pulses of laser light that penetrate the skin to create microthermal zones, stimulating collagen production and promoting skin rejuvenation. The fractional nature of the laser means that it treats only a fraction of the skin's surface at a time, leaving surrounding tissue intact and speeding up the healing process.
Furthermore, the features an Nd:YAG laser, which emits a specific wavelength of light that penetrates deeper into the skin, targeting deeper pigmentation, vascular lesions, and providing additional collagen stimulation. The ILP machine’s versatility lies in its ability to combine these technologies in a single platform, allowing practitioners to customize treatments based on the patient's skin type, condition, and desired
Figure 1: IPL and Laser Skin Resurfacing Machine
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
outcomes. Its precise control over parameters such as wavelength, pulse duration, and energy levels ensures safe and effective treatment delivery while minimizing risks and downtime for patients.
Overall, the IPL and laser skin resurfacing machine exemplifies cutting-edge technology in dermatology, offering comprehensive solutions for various skin concerns ranging from pigmentation disorders and vascular lesions to acne scars and signs of aging.
Selection Criteria
The study exclusively enrolled patients who satisfied all inclusion criteria and provided written consent to participate in the research.
• Inclusion Criteria:
1. Subjects aged more than 18 years with Melasma.
2. Subjects who have given the written consent for enrolment in the study.
• Exclusion Criteria:
1. Patients who are not willing to be a part of the study.
2. Subjects aged <18 years.
3. Pregnant & lactating women.
4. Patients with history of bleeding disorders, abnormal coagulogram or thromboembolism.
5. Patients who have taken any other melasma therapy within last 12 weeks.
6. History of hypertrophic scars or keloids.
7. Current use of oral contraceptive pills (OCP) or hormone replacement therapy (HRT).
8. Patients with photosensitive dermatoses.
Treatment protocol
In this study, each of the 22 patients underwent three sessions of intense pulsed light (IPL) laser treatment on the right side of their face, at an interval of four weeks apart. Additionally, microneedling (MN) procedures using a dermaroller with 1mm length microneedles were performed bilaterally on all patients' faces. Following microneedling sessions, 1.5 ml of tranexamic acid (TxA) solution (amp 500 mg/5 ml) was applied bi-monthly for a total of six sessions.
This combined treatment protocol aimed to evaluate the efficacy of IPL and microneedling with TxA in managing melasma, providing a standardized approach for assessing treatment outcomes and safety in a clinical setting.
Clinical evaluation
Clinical evaluation encompassed the calculation of the modified melasma area and severity Index (MASI) for both the right side [(MASI) (R)] and left side [(MASI) (L)] of the face, allowing for comparison between the two sides. Additionally, baseline and subsequent visit photographs were taken, and dermoscopic features were observed and
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
documented during each patient visit.
Patients self-assessed their melasma improvement using a six-grade Visual Analogue Scale (VAS) at weeks 0, 12, and two months following the final treatment (week 20), ranging from "Excellent" (0) for fading greater than 80%, to "No change or disturbing side effects".
The following six-grade Visual analogue scale (VAS) assessment was done by the patient at weeks 0, 12, & finally 2 months after the last treatment (week 20):1
(0) excellent: fading of melasma greater than 80%.
(1) Good: fading 60–80%.
(2) Moderate: fading 40–60%.
(3) Mild: fading 20–40%.
(4) Minimal: fading less than 20%.
(5) No change or disturbing side effects.
Statistical analysis
• Statistical analysis of the data was conducted utilizing SPSS (Statistical Package for the Social Sciences) software for Windows.
• Data were summarized using mean in quantitative data and using counts and relative percentages for categorical data.
• Wilcoxon signed-rank test was used in comparison of
before and after data within the same group.
• The mean of MASI scores of right & left sides of the face were compared using Chi-square test.
• P-values of less than or equal to 0.05 were considered statistically significant.
Results
The total cases enrolled in the study are 22, with mean age of 37.7 years.
Table 1: Demographic details
In this study, the research cohort comprises individuals aged between 18 and 56 years, with a male-to-female ratio of 2.01:1. The participants predominantly exhibit Fitzpatrick skin types IV (10 individuals) and V (12 individuals). Melasma duration ranges from 6 to 18 months, with centro facial (8 cases), malar (11 cases), and mandibular (3 cases) clinical types represented. The predominant pattern of melasma observed is epidermal (17 cases), followed by mixed type (5 cases). Among the participants, 5 males and 6 females report outdoor occupations. This demographic and clinical profile sets the foundation for evaluating the efficacy and safety of treatments combining Intense Pulsed Light (IPL) or Microneedling with Tranexamic Acid (TxA)
for managing melasma, offering insights into treatment outcomes across diverse patient characteristics.
Table 2: Age distribution between male and female cases
The table presents data on the distribution of individuals by gender and age groups. It shows that among males aged 18-29, there are 1 individual, while females in the same age bracket total 2, making a combined total of 3 individuals. In the next age category of 30-39 years, males account for 4 individuals compared to 6 females, resulting in a total of 10 individuals. Moving to the 40-49 age group, there are 2 males and 5 females, making a total of 7 individuals. Finally, in the 50-59 age range, there are no males recorded, but 2 females, totalling 2 individuals. Across all age groups, there are 7 males in total and 15 females, making a grand total of 22 individuals surveyed. This breakdown provides a clear demographic overview, highlighting how the distribution varies across different age brackets and between genders within the surveyed population.
Table 3: Comparison of Mean modified MASI (R) and MASI (L) scores with their reduction percentage at week 0, week 12 & week 20.
In this study evaluating the efficacy of melasma treatment using the modified Melasma Area and Severity Index (MASI), significant improvements were observed on both the right (MASI (R)) and left (MASI (L)) sides of the face over a 20-week period. At baseline (week 0), the MASI score for the right side was 7.21, decreasing to 3.84 at week 12 and further to 3.66 by week 20, translating to substantial percentage reductions of 46.7% and 49.2%, respectively, with highly significant p values of < 0.001 at both time points. Conversely, on the left side, the baseline MASI score was 7.13, which decreased to 5.08 at week 12 and to 4.95 by week 20, resulting in percentage reductions of 28.7% and 30.1%, respectively. The statistical significance varied slightly over time, with a p value of 0.05 at week 12 and < 0.05 at week 20. These findings indicate a more pronounced improvement in melasma severity on the right side compared to the left, highlighting potential asymmetries in treatment response. The study underscores the effectiveness of the treatment regimen in reducing melasma symptoms and emphasizes the importance A Randomised, Split-face, Comparative Study of
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
of ongoing evaluation to optimize therapeutic outcomes in clinical practice.
As evident from table 4 and above graph, there was a significant decline in the MASI scores of both the sides of the face from baseline to week 20, however it was more on the right side, with a P value of <0.001 at week 20 (on follow up). In the dermoscopic evaluation of patients, various findings were recorded, including multiple brown dots and globules, pseudo-reticular brown pigment network, arcuate and annular structures, perifollicular sparing, bluish-gray colour, and telangiectasia.Significant improvements in most dermoscopic features were observed bilaterally on the face of all patients at both week 12 and week 20 compared to baseline (week 0), as evidenced by serial photographs taken at specific points on the face during follow-up visits. However, reductions in telangiectasia and absence of spared areas were more pronounced on the right side of the patients' faces.
face at week 12
At week 12 of the study, comparative Visual Analog Scale (VAS) scores for the right and left sides of the face were analyzed across four categories (VAS 1, VAS 2, VAS 3, and VAS 4). For VAS 1, equal scores were observed in 2 patients each for both right and left sides. Specifically, 12 patients with VAS 2 were on the right side, compared to 7 patients on the left side. VAS 3 scores showed 6 patients on the right and 10 patients on the left side. Finally, VAS 4 scores indicated 2 patients on the right and 3 patients on the left side. These findings highlight varying degrees of facial pain experienced by patients, with differences noted between the right and left sides across the measured categories.
Figure 1: Comparative line graphs showing the decline in MASI score in both the groups
Figure 2: Comparative VAS score of Right & Left sides of
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma

At week 20 of the study, the comparative Visual Analog Scale (VAS) scores for the right and left sides of the face were assessed across four categories (VAS 1, VAS 2, VAS 3, and VAS 4). In VAS 1, comparable scores were noted in 1 patient for both sides. Specifically, VAS 2 scores showed 14 patients on the right side and 8 patients on the left side. For VAS 3, 6 patients reported scores on the right side and 10 patients on the left side. VAS 4 scores indicated 1 patient on the right side and 3 patients on the left side. The analysis of VAS scores provided by the patients indicated a notable difference between both sides of the face at weeks 12 and 20 compared to baseline measurements. Moreover, upon comparison of VAS scores between the right and left sides of the face, a statistically significant difference favouring the right side was observed, with a p-value of 0.004.
Patients reported no severe or significant adverse effects following treatment. Minor complications, such as transient erythema, mild burning or discomfort, and mild pain, were only reported post-micro needling. Importantly, noinstances of hyperpigmentation or other adverse reactions were noted following laser treatment on the right side of the face.
Figure 3: Comparative VAS score of Right & Left sides of face at week 20
Patient 1
Patient 2
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
Discussion
The substantial decrease in mean Melasma Area and Severity Index (MASI) scores observed on both sides of the face at weeks 12 and 20, with a p-value <0.05 in present study, aligns with findings reported by A. I. Tahoun et al. (2020) and F. Y. Saleha et al. (2019). These studies demonstrated the superiority of Micro-needling with Tranexamic Acid (TxA) over Micro-needling with Vitamin C and standalone micro needling, respectively.2
Table 4: Comparison of Mean age of the patients of melasma in different studies

In the present study conducted in 2022, the sex ratio was reported as 2.14:1, indicating a higher prevalence of female participants compared to males. This contrasts with earlier research by Mamta Bhura et al in 2021, where the sex ratio was notably higher at 5:1, suggesting a greater representation of females relative to males in their study cohort. Similarly, Achar A et al in 2011 reported a sex ratio of 4:1, emphasizing a similar trend with a predominance of female subjects. In contrast, L. Budamakuntla et al's study in 2013 documented a more pronounced disparity with a sex ratio of 9:1, highlighting a significant predominance of females in their research sample. These findings underscore variations in sex distribution across different studies, reflecting potential demographic differences and highlighting the importance of considering sex ratios in interpreting study outcomes and implications for clinical practice.
Table 5: Comparison of Sex ratio of the patients of melasma in different studies.
In the present study, the addition of IPL laser treatment to the right side of the face resulted in further enhancement, particularly evidenced by a more pronounced decline in MASI scores on the right side (MASI) (R), with a p-value of <0.001 at week 20.
Results from a randomized controlled trial conducted by Wang et al. (2004), which investigated IPL
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
treatment combined with hydroquinone versus hydroquinone alone in patients with refractory melasma, similarly support our findings. They reported a significant improvement in the IPL group compared to the control group, indicating the efficacy of IPL in melasma management.
In the present study, we found that the right side of the face, treated with IPL, exhibited greater improvement in telangiectasia compared to the left side.
A study by A. I. Tahoun et al. (2020), comparing tranexamic acid versus Vitamin C with micro-needling, reported a statistically significant reduction in the prevalence of telangiectasia on the right side of the face (treated with tranexamic acid) compared to the left side. This finding supports the role of tranexamic acid in addressing the vascular component of melasma, as suggested by Geddes et al. (2016).2
Furthermore, the greater improvement in telangiectasia observed on the right side of the face (IPL-treated side) in our study aligns with the findings of a study on IPL laser treatment in melasma by Zoccali et al. (2010).4
These findings suggest that the IPL laser has a synergistic role with TxA in tackling the vascular component (telangiectasia) of Melasma.4
falling into Excellent (4.5%), Fair/Moderate (27.2%), and Poor (4.5%). In contrast, the control group results were more dispersed, with 45.4% in Fair/Moderate, 36.3% in Good, 13.6% in Poor, and only 4.5% in Excellent. Wang et al. (2004) showed a more varied distribution for cases, with 12% rated as Excellent, 23% as Good, 35% as Fair/ Moderate, and a notable 30% as Poor. Their control group had a significant majority (79%) in the Poor category, with no Excellent outcomes, 14% Good, and 7% Fair/Moderate. Zoccali et al. (2010) reported that nearly half of their cases (46%) achieved Excellent outcomes, 30% Good, 13% Fair/Moderate, and 11% Poor. There is no control data presented for Zoccali et al. (2010) in the image.
A comparative analysis of the outcomes from three different studies— the present study conducted in 2022, Wang et al. (2004), and Zoccali et al. (2010)—focusing on cases and controls across four outcome categories: Excellent, Good, Fair/Moderate, and Poor.
In the 2022 study, for cases, the majority of outcomes (63.6%) were categorized as Good, with smaller percentages
Overall, the present study from 2022 indicates a higher proportion of Good outcomes for cases compared to Wang et al. (2004), which had a considerable portion of Poor outcomes. Zoccali et al. (2010) demonstrated the highest percentage of Excellent outcomes for cases among the studies. For controls, the 2022 study shows a more balanced outcome distribution compared to Wang et al.
Table 6: Results of different IPL studies in melasma
A Randomised, Split-face, Comparative Study of Intense Pulsed Light & Tranexamic Acid with Microneedling v/s Tranexamic Acid with Microneedling in the Treatment of Melasma
(2004), where the majority were classified as Poor.
Overall, these findings suggest that the combination of IPL and TxA offers a comprehensive approach to treating melasma, addressing both pigmentary and vascular aspects of the condition. This underscores the importance of tailored, multifaceted treatment strategies in effectively managing this challenging dermatological condition.
Limitations
• The entire procedural process is notably lengthy, requiring a significant time commitment from both healthcare providers and patients.
• Patients often require extensive counselling to ensure they arrive punctually for their appointments, adding to the logistical challenges of managing their care effectively.
• This counselling is crucial as there is a substantial risk of patients being lost to follow-up if they do not adhere to the recommended schedule of treatments.
• Moreover, the use of laser procedures adds a financial burden as they are typically expensive, potentially limiting accessibility for some individuals.
These factors collectively underscore the complexities and barriers associated with laser treatments in clinical practice, highlighting the importance of addressing logistical and financial considerations to optimize patient care and treatment outcomes.
Conclusion
Although underutilized in the realm of hypermelanosis, IPL stands out as an effective tool in its treatment. It can target a wide range of cutaneous structures, including deeper pigmentation and vasculature. Microneedling by creating several micro channels, delivers the medication more evenly and deeper into the skin. Thus, it helps to reduce both, epidermal and dermal hyperpigmentation. Microneedling followed by TXA is successful in melasma treatment, adding IPL laser to this procedure has additional benefits, especially for dermal pigmentation and for tackling telangiectasia associated with melasma in acomprehensive manner.
Conflict of interest: None
References
1. Doolan BJ, Gupta M. Melasma. Aust J Gen Pract. 2021;50(12):880-
885. doi:10.31128/AJGP-05-216002
2. Tahoun AI, Mostafa WZ, Amer MA. Dermoscopic evaluation of tranexamic acid versus Vitamin C, with microneedling in the treatment of melasma: a comparative, split-face, singleblinded study. J Dermatolog Treat. 2022;33(3):1623-1629. do i:10.1080/09546634.2021.1871 582
3. Wajieha S,Faria A, Khawar K,et al Efficacy of intense pulsed light in melasma. Journal of Pakistan Association of Dermatologists. 2014;24 (3):212-216.
4. Zoccali G, Piccolo D, Allegra P, Giuliani M. Melasma treated with intense pulsed light. Aesthetic Plast Surg. 2010;34(4):486-493. doi:10.1007/s00266-010-9485-y
Oral Candidiasis Associated with Geographic Tongue: A Case Report
differentiation. Vitamin supplements were administered to correct any potential deficiencies that might impair mucosal health, and regular gargling was advised to maintain oral hygiene and reduce microbial load. Remarkably, within 3 to 4 weeks of starting this regimen, the patient exhibited significant symptom improvement, indicating a gratifying and rapid response to the prescribed therapy. The erythematous and grey lesions on the tongue began to resolve, and the overall appearance of the oral mucosa improved significantly. This rapid resolution of symptoms highlights the efficacy of the combined treatment strategy in managing the complexities of oral candidiasis and geographic tongue. The successful outcome in this case suggests that such a comprehensive approach could serve as a potential protocol for treating similar cases in clinical practice, offering hope for patients suffering from chronic and resistant forms of oral mucosal conditions.
Before treatment
After treatment
Figure 1: Erythematous, irregularly shaped lesions on the dorsum and lateral borders of the tongue
Diagnosis
The diagnosis of oral candidiasis is essential for effective treatment and management of this common fungal infection, primarily caused by Candida species. Oral candidiasis, often referred to as thrush, manifests as white lesions, redness, and discomfort in the oral mucosa. Accurate diagnosis involves a combination of clinical evaluation and various diagnostic methods. Exfoliative cytology, where cells are collected from the oral mucosa and examined for abnormalities, is particularly valuable. Imprint specimens using a spatula or filter paper help transfer cells to culture media for identification. Stains like KOH, Gram, and PAS are used in microscopic examination
to detect Candida species, characterized by yeast cells, hyphae, and pseudohyphae. The germ tube test specifically identifies Candida albicans by the presence of germ tubes, differentiating it from other Candida species. Salivary assays effectively diagnose oral candidiasis by detecting Candida albicans antigens and antibodies in saliva, using techniques like ELISA to confirm active infection. Oral mucosal biopsies provide detailed evaluation by examining tissue samples for Candida hyphae and inflammation. Biochemical methods identify Candida species through tests like carbohydrate fermentation and chromogenic media. Immunological methods, including immunofluorescence and Western blotting, detect immune responses, while genetic techniques like PCR and qPCR amplify and quantify Candida DNA. These methods together offer comprehensive insights into the presence and severity of oral candidiasis.3,4
Treatment
The management of oral candidiasis involves three fundamental principles which include accurate and timely diagnosis, addressing underlying predisposing
factors, and selecting the most appropriate antifungal therapy. Antifungal agents are categorized into three major classes: polyenes, echinocandins, and azoles. Polyenes include amphotericin B and nystatin. Nystatin functions by binding specifically to ergosterol, a crucial sterol component of the fungal cell membrane. This interaction creates pores or channels in the membrane, increasing its permeability and leading to leakage of intracellular contents, which ultimately results in fungal cell death. Amphotericin B, also a polyene, shares a similar mechanism by binding to ergosterol and forming membrane pores. However, amphotericin B is more frequently employed in systemic infections due to its broader antifungal spectrum and increased efficacy. Conversely, nystatin is primarily used topically, particularly in formulations for treating severe localized infections.5
Anidulafungin, caspofungin, and micafungin are echinocandins used in the treatment of oral candidiasis. These agents target the fungal cell wall by inhibiting the synthesis of 1, 3-β-D-glucan, a crucial component of the cell
Oral Candidiasis Associated with Geographic Tongue: A Case Report

wall. This class of drugs is fungicidal against Candida species and has minimal toxicity to human cells. They are administered exclusively via the intravenous route. Anidulafungin is known for its stability and long half-life, allowing for less frequent dosing, while caspofungin is effective against a broad range of Candida species and has a similar mechanism of action. Micafungin also targets β-1, 3-D-glucan synthesis but is distinguished by its potent activity against certain resistant Candida strains and its extensive use in treating invasive fungal infections.5 Azoles, including clotrimazole, miconazole, fluconazole, and others, inhibit the fungal enzyme lanosterol 14- α -demethylase, essential for ergosterol synthesis in fungal cell membranes. This disruption impairs cell membrane integrity and inhibits fungal growth. Clotrimazole and miconazole are commonly used topically, while fluconazole is preferred for its effectiveness and favorable pharmacokinetics. Newer azoles like posaconazole, voriconazole, and isavuconazole are effective against resistant Candida strains. Geographic tongue typically requires no treatment, but symptomatic
cases may benefit from topical corticosteroids, antihistamines, or tacrolimus, along with avoiding irritants like spicy foods and alcohol.5,6,7
A comprehensive treatment regimen for oral candidiasis and geographic tongue typically involves a multifaceted approach combining topical, systemic, and supportive therapies to address both the fungal infection and mucosal inflammation. Combination of tretinoin and clindamycin gel can aid in reducing inflammation and clearing abnormal lesions on the mucosa. Isotretinoin capsules a potent retinoid, helps normalize epithelial cell differentiation and reduce inflammation. It can be effective in treating severe or recalcitrant cases of geographic tongue and oral candidiasis. Vitamin supplements with vitamins, particularly B vitamins and zinc, can help support mucosal health and address any deficiencies that may be contributing to the condition. Gargling with an antiseptic or antifungal solution can help reduce fungal load in the oral cavity. Common solutions include those containing chlorhexidine or diluted antifungal agents, which can aid in controlling
Oral
Candida and maintaining oral hygiene. Maintain rigorous oral hygiene by brushing the teeth and tongue regularly with a soft brush, and ensure dentures (if applicable) are thoroughly cleaned and disinfected daily. Removing dentures overnight or for at least six hours can also help reduce fungal growth. Long-term adherence to treatment and monitoring of underlying or contributing factors are crucial for successful management. This comprehensive approach addresses the complex nature of oral candidiasis and geographic tongue, aiming to resolve current symptoms while preventing recurrence and managing any contributing factors.8
Discussion
Oral mycosis the most frequently isolated pathogen, accounting for over 80% of cases. Candida albicans is a dimorphic yeast capable of existing in both hyphal and yeast forms depending on environmental conditions. Less commonly, other Candida species implicated in oral candidiasis include Candida glabrata, Candida tropicalis, Candida krusei, Candida guilliermondii, Candida lusitaniae, Candida parapsilosis, Candida pseudotropicalis, and
Candida stellatoidea. Nonalbicans Candida species have a higher colonization rate in patients aged 80 years and older compared to younger individuals. Candida species are part of the normal oral microbiota in immunocompetent hosts, with approximately 30 to 60% of adults and 45 to 65% of infants harboring these yeasts in their oral cavities. In most cases, these species exist as commensals rather than pathogens. The oral cavity hosts diverse microbial communities that maintain health through a delicate balance. Disruption of this balance, or dysbiosis, can lead to diseases such as oral candidiasis. Candida albicans interacts with streptococci for colonization, benefiting from their nutrients and adhesion sites. High sugar intake exacerbates interactions with Streptococcus mutans, contributing to dental caries. Saliva plays a crucial role in defense, with antimicrobial peptides like histatin-5 targeting Candida. Immune responses, especially Th17 cells, are vital in managing Candida growth. Differential diagnosis of oral candidiasis includes conditions like oral mucositis, erythroplakia, leukoplakia, and infections such as herpes and syphilis.5,6,9
Non-pharmacological treatments for managing oral candidiasis include maintaining rigorous oral hygiene and cleaning dentures daily. Dentures should be soaked in cleaning solutions like chlorhexidine and removed during antifungal rinses for better mucosal contact. Soft brushing of the mucosal surface and allowing dentures to air dry postdisinfection can help remove Candida. Probiotics, such as Lactobacillus, and probioticrich foods like yogurt can restore oral flora balance and inhibit Candida growth. Proper denture fit and cleaning are crucial to prevent infection recurrence. Though rare in immunocompetent individuals, oral candidiasis can lead to severe complications in immunocompromised ....... patients, including systemic dissemination and candidal esophagitis in those with HIV/AIDS.5,9
Addressing predisposing factors and providing patient education on oral hygiene are crucial for resolving the infection, preventing recurrence, and ensuring long-term oral health.
Conclusion
Oral candidiasis presents significant challenges in both diagnosis and management.
Despite advancements in understanding the pathogenesis and immune response, accurately diagnosing oral candidiasis can be complicated by its clinical overlap with other oral conditions and variability in patient presentations. Effective treatment requires a nuanced approach that includes antifungal therapy tailored to the severity and type of infection, as well as addressing contributing factors to prevent recurrence. Additionally, ongoing research is needed to bridge gaps in our understanding of host-pathogen interactions and to develop novel therapeutic strategies. Ensuring comprehensive patient management and addressing both clinical and systemic factors remain crucial for improving outcomes in oral candidiasis.
References
1. Akpan A, Morgan R. Oral candidiasis. Postgrad Med J. 2002; 78(922):455-459. doi:10.1136/pmj.78.922.455.
2. Singh A, Verma R, Murari A, Agrawal A. Oral candidiasis: An overview. J Oral Maxillofac Pathol. 2014; 18(Suppl 1):S81-S85. doi:10.4103/0973-029X.141325.
3. Vila T, Sultan AS, MontelongoJauregui D, Jabra-Rizk MA. Oral Candidiasis: A Disease of Opportunity. J Fungi (Basel).
Oral Candidiasis Associated with Geographic Tongue:
A Case Report
2020; 6(1):15. Published 2020 Jan 16. Doi: 10.3390/jof6010015.
4. Coronado-Castellote L, Jiménez-Soriano Y. Clinical and microbiological diagnosis of oral candidiasis. J Clin Exp Dent. 2013; 5(5):e279-e286. Published 2013 Dec 1. doi:10.4317/ jced.51242.
5. Rajendra Santosh AB, Muddana K, Bakki SR. Fungal Infections of Oral Cavity: Diagnosis, Management, and Association with COVID-19. SN Compr Clin Med. 2021; 3(6):1373-1384. Doi: 10.1007/s42399-021-00873-9.
6. Quindós G, Gil-Alonso S, Marcos-Arias C, et al. Therapeutic tools for oral candidiasis: Current and new antifungal drugs. Med Oral Patol Oral Cir Bucal. 2019; 24(2):e172-e180. Published 2019 Mar 1. doi:10.4317/ medoral.22978.
7. Shareef S, Ettefagh L. Geographic Tongue. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi. nlm.nih.gov/books/NBK554466/
8. Taylor M, Brizuela M, Raja A. Oral Candidiasis. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih. gov/books/NBK545282/
9. Taylor M, Brizuela M, Raja A. Oral Candidiasis. In: StatPearls. Treasure Island (FL): StatPearls
Publishing; July 4, 2023.
MUMBAI 202
MUMBAI 2025
1 Day Conference, Hands on Workshop and Exhibition
AESTHETICCON Mumbai 2025 is just the event for you with practical insights shared in the Conference, tips while training in the Hands on workshop and interaction
AESTHETICCON Mumbai 2025 is just the event for you with practical insights shared in the Conference, tips while training in the Hands on workshop and interaction with product manufacturers.
Spend the day catching up and meeting with your fellow Dermatologists colleagues.