THE EXECUTIVE CONNECTION
OF NORTH TEXAS
OUR YOUTH ARE IN CRISIS.



Amanda Brummitt, FACHE
Tom Peck, FACHE
Vanessa Lee
Kean Villarta
Byron Westbrook
Audrianne Schneider, FACHE
Kean Villarta
Mike Belkin, FACHE
Mark A. Riordan
Melinda Schmidt, MBA, BSN, RN
Bert Witherspoon
info@achentx.org
ACHE of North Texas
Editorial Office, c/o Executive Connection
300 Decker Drive, Suite 300
Irving, TX 75062
p: 972.413.8144
e: info@achentx.org
w: achentx.org
OFFICERS
President
Felixia Colón, FACHE, Sr. Vice President & Group Operations Officer, SCP Health
Immediate Past President
Dustin Anthamatten, FACHE, VP Operations, Corporate Methodist Health System
President-Elect
Aaron Bujnowski, FACHE, Director (Partner) & IDN Lead, The Chartis Group
Treasurer
Benton Sprayberry, FACHE, Market President – TX/OK, Main Street Health
Secretary
Patrick Brown, FACHE, Senior Vice President-Operations, National Group Surgery Partners
Diversity, Equity & Inclusion Officer
Ajith Pai, FACHE, President, Texas Health Harris Methodist Hospital
Southwest Fort Worth
The ACHE of North Texas e-magazine, The Executive Connection, is published triannually and includes information on the latest regulatory and legislative developments, as well as the quality improvement and leadership trends that are shaping and influencing the healthcare industry. Readers get indepth reporting on the issues and challenges facing hospital and health system leaders today. We make it our job to tell you about the great things the organization and Chapter are doing every day to ensure the health of our community. If you have any news and updates that you want to share with other members, please e-mail your items to info@northtexas.ache.org. Microsoft Word or compatible format is preferable. If you have a graphic or picture that you'd like to include, please send it as a separate file. The following are the types of information that our members shared in past ACHE of North Texas magazines, Advocacy Issues, Legislative Issues, Educational Opportunities, Awards / Achievements, Promotions (Members On the Move), Committee Updates, journal submissions, conference submissions, and workshop participations, sharing

Dr. Jim Allard, DNP, RN, NEA-BC, FACHE
ACHE Regent-at-Large, District 4 Chief Nursing Officer, Medical City Arlington
Noreen Butte, MD
Fraser Hay, FACHE
President, Texas Health Presbyterian Hospital Plano
Jared Lange
Director, Business Sustainability & Development, Parkland Health
Joseph Clayton Lawrence, FACHE
Regional President, Sound Physicians
Christina Mathis, MHA
Chief Operating Officer/Ethics & Compliance Officer, Medical City Plano
Trinette K. Pierre, DHA, RN, NEA-BC, FACHE, ACHE Texas – North Regent
Executive Consultant/Advisor, Career Consultant, Professor, TRImani Consulting, LLC
Kris Sanders, FACHE
SVP Northern Market Growth & Development, Children’s Health
Keith Thurgood, PhD
Clinical Professor & Program Director, MS Healthcare Leadership and Management, University of Texas at Dallas
Michael Talley, RRT, FACHE
VP of Clinical Operations & Virtual Care, CHRISTUS Health
Toya White, FACHE
Chief Operating Officer & Chief Nursing Officer, Texas Health Resources
Corey Wilson, FACHE
Chief Operating Office, Texas Health Harris Methodist Fort Worth
Timothy Wilson
SVP, Population Health Management, P3 Health Partners
Mary R. Wylie, DHA, MBA, MHA, FACHE
Vice President and Chief Operating Officer, Baylor Scott and White Medical Center Plano

I would like to thank all the First Responders and medical personnel who cared for the victims and those injured in the mass shooting in Allen, TX in May 2023. We send our sincerest thoughts and well wishes to those impacted by the tragedy. With this traumatic event and other mass tragedies that have occurred recently, it is imperative you take time for yourself and your family and appreciate the moments and time spent with loved ones. News and other media outlets are predicting this summer to be one of the highest travel records in the past several years. Given this, it is important to take time away to recharge, regroup and re-energize yourself, given the last few years in the pandemic.
I encourage all our ACHE Colleagues; if you have direct reports or peers who are on vacation, but making it a working vacation, you encourage them to stay off email and video calls.
As mentioned in our Spring 2023 Executive Connection magazine, our board has been intentional with our Diversity, Equity, and Inclusion (DEI) initiatives. Our first unified DEI mixer, “Better Together”, will be hosted on July 20, 2023. This event will include other ACHE communities such as National Association of Health Services Executives (NAHSE), National Association of Latino Healthcare Executives (NALHE), Asian Healthcare Leaders Community (AHLC) and Women’s Healthcare Executive Network (WHEN). This mixer will also include other healthcare organizations in the DFW metroplex: Healthcare Information Management Systems Society (HIMSS), North Texas Association for Healthcare Quality (NTAHQ) and Healthcare Financial Management Association (HFMA). We will also have in attendance, keynote speaker, Richard Hill, DHA, CPHQ, HACP-CMS, PCP, FACHE; Program Director, BSHM/Assistant Professor, Texas Tech Health Sciences Center. Kudos to ACHENTX DEI committee for organizing this event!
There are so many additional ACHENTX educational and networking events that will occur this summer. Please make sure you review our weekly newsletter or calendar events webpage at www. ACHENTX.org. Even though we’ve passed half of 2023, it is never too late to invest in your personal and professional growth. Look back at your New Year’s Resolutions list and do not feel guilty if you only have one or two items completed. Remember, it is never too late to start a new project. The only issue is not starting it at all. Hope you enjoy your summer!
At Texas Health, we will be there for you and your loved ones. With an experienced staff and technologically advanced care, our dedication is to your health. Whether you need 24-hour emergency care or wellness services, we’re equipped to handle your health care needs.


|



Thank you all for your dedication to continuing to advance healthcare as a profession. Your contribution is invaluable and much appreciated. Our communities are healthier because of you. While there is still much to do to ensure all people can receive the best healthcare services, and thus, be as healthy and holistically whole as possible, the strides you have made are only a glimpse at what can be if we work together to reach the goals of affordable, attainable, and accessible highquality healthcare services for all.
As we enjoy this summer season, we should remember to take time to care for ourselves and refresh our spirits before another busy fall season commences. Just as our vehicles will not function well without system checks and adequate amounts of oil, we are not able to function at our highest capability and capacity without caring for ourselves. Should we take better care of our vehicles than we do our most precious gifts — our bodies? Teslas, Porsches, and Lamborghinis may be nice to own, but they sit in our garages and are deemed useless if we are not well enough to drive them.
Remember, we cannot effectively care for others without first taking time to do much needed and well-deserved scheduled self-checks. Just as a mechanic drains our oil tanks and changes filters at set intervals, we must check under the hood, drain out built-up impurities, and unclog what has become blocked by life’s woes and work’s stresses. We must then refill our beings with pure, fresh oil. This process is required to keep us functioning well for the next 3,000+ miles.
So, what’s the level of your oil? Are you a few quarts low? Have there been incognito leaks here and there that ultimately ended up with you sitting on the side of the road during rush hour?
Have you been ignoring the “check engine” warnings that have been illuminating your internal dashboard? Or maybe you have uttered the words, “I can go another 300 miles before I address the ‘low oil’ warning of my internal computer system.”
You only need to sit disabled once to know that this is not the best option. Let us not assume that a service station is over the next hill on the dark and desolate highways we travel. We should take time out to refill our beings this summer and ensure we continue to schedule this most
important maintenance throughout the year. Those we love depend on us to get our much needed system checks completed on time. Would we put our loved ones in a car that may not be safe to drive? If we want the best for them, we would not. In the same respect, why give them less than our personal best and hope they will be fine without us being whole and healthy?
Cars can be replaced. We cannot. Take care of you.
Be blessed. Be safe. Happy Summer!
— Trin
My term as Regent for Texas Northern will end in early 2024. ACHE National is accepting selfnominations for this role. If you are interested in learning more about the duties of Regents, please contact:
Jennifer Connelly, Vice-President of Volunteer Relations jconnelly@ache.org or visit:
https://www.ache.org/ membership/elected-leaders-area/ official-notice-for-council-of-regents


ACHE National is currently accepting applications for the ACHE Nominating Committee. If you are interested in learning more about the application process, please visit:
https://www.ache.org/membership/ elected-leaders-area/call-for-nominations-slate

Steven has been in the healthcare industry for 20 years focused on workforce staffing and search. He is currently an executive search consultant with emphasis on the healthcare and life sciences sector. He is a partner with Caldwell Partners and serves on C-suite and Dean level search projects.
Steven believes that the current critical issue for healthcare organizations is the shortage of clinical staff, nurses, and physicians.
Steven has been a member of the ACHE for 12 years and is currently working towards his board certification. He just completed all the credit requirements and will sit for the Board of Governors Exam this year, 2023.
his career?
ACHE has been valuable for networking with other healthcare leaders and members. It has also been an incredible resource for educational materials to expand his understanding of the healthcare space outside of his focus on recruitment and staffing. Steven has enjoyed both the virtual and face-to-face opportunities.
Steven encourages early careerists to get involved by attending local chapter events. He advises attending as many as possible and networking intentionally. Set a goal to meet at least one new member or guest at each event and follow up with that individual to establish a network.
Most people consider Steven outgoing and gregarious. However, Steven is an introvert. He excels at public speaking and communicates for a living, but he mostly enjoys quiet time with family. Steven is originally from New Zealand and moved to the United States, Atlanta, Georgia, in 1999.
What Tammy is doing now
Tammy Phillips, CHCIO, CDH-E, FHIMSS currently serves as the Chief Information Officer for Advent Health Texas. Advent has four hospitals in Texas and she oversees technology for all of the facilities.
Tammy’s opinion on the most important issue facing Healthcare today
Tammy believes the most important issue for healthcare today is learning how to better leverage technology to support patient care and provider efficiency. She believes this would reduce cost and improve the efficiency of healthcare providers.
How long has Tammy been a member of ACHE?
She has been a member for one year.
Why is being a member important to Tammy? Has ACHE membership been a benefit to her career?
Tammy sees how membership can better her career because she has found the chapter meetings and networking events to be of great value. She has met leaders and professionals from other organizations within the healthcare space.
What advice would Tammy give early careerists or those considering membership?
Her advice for early careerists is to get involved by attending local chapter meetings. Chapter meetings provide a great opportunity to network and understand different business lines. She encourages them to be fearless and meet new people.
One thing that people don’t know about Tammy
Tammy has a brother named Charlie Brown and had a dog named Snoopy growing up.
John P. Carter is currently works as a healthcare consultant for Pinnacle Healthcare Consulting. He drives business development and is the brand ambassador.

John believes that the payor manipulation of reimbursements is the biggest challenge for healthcare. The percent of reimbursement is controlled by our federal government, but the volume submitted is not controlled. He believes that even if utilization is reduced, the cost of healthcare will continue to rise because payors will still reimburse for volume.
John has been a member of ACHE for almost eight years. John is an active member of the chapter who participates in many events and volunteers on the membership committee.
Why is being a member important to John? Has ACHE membership been a benefit to his career?
John has found membership to be beneficial since he became involved in volunteering and participating in local events over the past four years. Membership provides the opportunity to meet stakeholders across various sectors of healthcare.
John advises early careerists to get more involved in their local ACHE chapters. Events are held frequently and attending them provides incredible value. Events give one the opportunity to network and learn.
John was in a terrible car wreck when he was 17. He was tossed through the windshield but walked away from that terrible accident. John also served in our military. Thank you for your service, John.

Access TeleCare partners with hospitals of all sizes to build and sustain specialty telemedicine programs of excellence.
Built and led by physicians, our team designs Access TeleCare programs to deliver superior patient care.
We deliver consultative telemedicine to on-site health care professionals to allow more patients to be cared for locally –avoiding transfer and fragmented care.
From working in the client hospital’s EMR to working as part of the hospital’s medical staff, our goal is superior operational integration and clinical excellence for your patients.
We provide dedicated specialists for each hospital to promote an ongoing, collaborative, team-based relationship among patients, physicians, nurses and staff.
Features Include:
Minimizing length of stay
Maximizing CMI
Increasing census
Optimizing throughput
Increasing DRG reimbursement
What telemedicine programs can Access TeleCare build for your organization?
ANTIBIOTIC STEWARDSHIP

CARDIOLOGY
CARDIAC ARREST (CODE BLUE)
ENDOCRINOLOGY
GENERAL INTERNAL MEDICINE
GENERAL NEUROLOGY & ACUTE STROKE
HOSPITALIST
INFECTIOUS DISEASE
MATERNAL-FETAL MEDICINE
NEPHROLOGY
NOCTURNIST
PSYCHIATRY
PULMONOLOGY & CRITICAL CARE
RHEUMATOLOGY
To submit your update, milestone, award or accomplishment, CLICK HERE.
DANI-BREE BIALEK was recently appointed as Director, Physical Medicine & Rehabilitation for Methodist Richardson Medical Center.

JOHN P. CARTER, ACHENTX Networking Committee Chair, has recently joined Pinnacle Healthcare Consulting.


MITCHELL HERRON has joined Foremost Family Health Centers as Chief Operating Officer.
SHARAE LEMOINE graduated this spring from the University of Illinois with a Master of Health Administration.

ANGELA VINCENT MICHAEL, Director Performance Improvement, Methodist Health System won the Dallas Fort Worth Hospital Council’s System Award at the council’s 25th Annual Employee of the Year luncheon on April 19th.

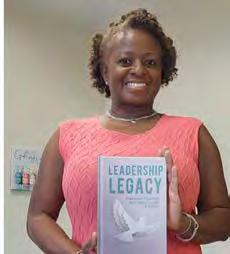
TRINETTE PIERRE has published her first book: Leadership Legacy: Using Insights from Your Past to Build a Legacy of Success.




As the number of young people presenting with chronic, persistent mental health conditions continues to rise, healthcare leaders are exploring ways to improve the overall system of care.
 MARK A. RIORDAN
MARK A. RIORDAN
Following a spate of tragic Fentanyl overdoses among North Texas teens and young adults, the editorial committee at Executive Connections thought it was an issue we should cover.
As we explored what these overdoses, many accidental, mean for us, the question became “What must we do to stem the tide?” The subject of the article kept changing. Eventually, we decided the issue was much bigger than teen deaths and near deaths from Fentanyl overdoses; it was the global youth mental health crisis.
Patients dealing with substance misuse and who may be self-medicating are almost always sending signals that something much more serious is going on with them, especially when we’re talking about a young person. We all know this as clinicians, parents, and former teens ourselves.
Persistent sadness, depression, anxiety, and even suicidal thoughts have been part of the transition to adulthood for many of us and others in our families. These feelings often last a lifetime. What can we, as health professionals, do to help? That was the question the committee members wrestled with. We decided to cover it adequately; we needed to dedicate space in multiple publication issues.
As with most disease states and conditions, traditional healthcare and insurance plans cover mental health issues in the acute phase with a certain amount of follow-up treatment. But mental health issues can be among the most intransigent conditions we encounter and treat. They are often resistant to available therapies and pharmaceuticals.

There are also social issues related to mental health. Not everyone believes that young people are a) in crisis or b) need medical attention or other interventions. We ignore our own mental health and often neglect to accept that others might be suffering from something real and
treatable, especially when it comes to the young people in our lives. We say whatever they’re suffering from is a phase; they’ll grow out of it. We did. Didn’t we?
Other than by miracle, almost all chronic conditions will worsen over time. They don’t regularly heal themselves. The same holds true for young people suffering from increasing rates of social isolation, anxiety, mood disorders, substance abuse, and psychoses. The statistics from the last 10-12 years are staggering.
According to a study published in JAMA this spring, Emergency Department visits among patients 6-24 years old decreased between 2011 and 2020, a promising sign. However, mental health-related visits among that same age cohort went up. Even more alarming, suiciderelated visits increased among children 6-12, adolescents 13-17, and young adults 18-24.
As the committee discussed these trends and began searching for solutions we could offer, it became clear that many, if not all of us, had personally encountered the system on behalf of a young person. Sadly, it also became apparent that the system — including social services, law enforcement, schools, and hospitals — could do better.
This is not an indictment of the highly trained, compassionate clinicians and professionals who’ve dedicated their lives to relieving this kind of suffering. It was instead a recognition of how society has relegated mental health issues to special units separated from our main functions for too long.
Committee members shared where the systems we rely on to help our children served them well. They also shared heart-wrenching stories of how and when the system failed them, neglected them, and sent them back into the world without alleviating their suffering and sometimes making it worse.
Continued on page 18
We decided we could be agents for change within our part of healthcare and in our part of the world. While we in healthcare deal with patients in different phases of the journey — inpatient and outpatient — we don’t treat the entire spectrum. Instead, we rely on partners in law enforcement, child welfare, and social services.
Just as other health-related conditions require more than just medical interventions, we must look to create better linkages with our partners. One question that came up several times was how can we better partner with them. We will cover this question in a subsequent article.
A friend who works with young people in the child welfare system said, “It’s tempting just to propose adding another outpatient clinic or more inpatient beds to address the need, but that might not be what the community needs or wants. Healthcare executives could lead by convening and investing in generative, authentic partnerships with communitybased organizations, youth leaders, and families to co-design strategies to improve youth mental well-being.”
The editorial committee decided to start this journey with the person, or people, in the mirror: Us. As I mentioned, people started sharing their stories once we started talking. Each story identified a problem. Some we have the power to address immediately without impacting budgets. Others will have budgetary impacts.
It’s clear we don’t have enough beds, and we certainly need more pediatric psychiatrists and psychiatric nurses, but we could also coordinate better with our partners, and we could be more inclusive of the concerns of families and patients.
We want to hear your stories and listen to your suggestions and ideas for how we can better address the global youth mental health crisis. Together we can make a difference.
Please send your comments or stories to Info@ACHENTX.org. Your privacy is very important to us and will be protected. We will only publish information that you expressly approve.
ONE IN FIVE U.S. CHILDREN (6-12) experience mental illness every year. Only half receive care or treatment.
40 PERCENT
Increase in high school students reporting persistent sadness or hopelessness
There was a 57 PERCENT INCREASE in the national suicide rate among YOUTH 10-24
ER visits among patients 6-24 decreased 3.3 million but mental health-related visits INCREASED from 4.8 MILLION to 7.5 MILLION.
Mental health-related visits increased among all age groups but most among PATIENTS 10-14.
Suicide-related visits INCREASED AMONG ALL AGE GROUPS.
National Trends in Mental Health Related Emergency Department Visits Among Youth 2010-2020, The Journal of American Medical Association May 2, 2023
Community-minded, mul�-specialty medicine







 Mihir Patel, MD Regional Chief Medical Officer
Mihir Patel, MD Regional Chief Medical Officer


another round of cancer four years after the first bout and is doing extremely well.
After receiving my bachelor’s degree, I worked full-time and pursued my master’s degree at night. I’ve been blessed to work for amazing organizations throughout my career in marketing, communications, and media relations. I’ve also been on the front line of crisis communications for Ebola and COVID-19. I obtained my Fellow certification in 2007.
My journey to health care was interesting. As a kid, I couldn’t wait for the weekly episode of Medical Center starring Chad Everett. Instead of tea parties, I set up hospitals in the playroom I shared with my younger sister. Throughout my education, I excelled in English and history — and struggled with science — but I was determined to be a doctor. Early in my undergraduate studies, it became clear that lab work and dissection were not my gifts. I changed my major to journalism with minors in business and English.
During my junior year in college, my dad was on a business trip in Japan and collapsed. He had colon cancer and was in a Japanese hospital for several weeks. He returned to the U.S. on Father’s Day and needed major surgery. That summer, I took a full load of classes, worked my part-time job, and slept on the couch in the ICU waiting room to see him for 15 minutes at night and in the morning. During this time, I realized I wanted to take my marketing and communication skills and work in health care. My dad is now 90. He survived
This is not easy work, and I tell those interested in it that it is truly a vocation for me. My motivation comes from making a positive difference — and this is where I go when I need to reconnect. When I’m in a hospital, I will get away from my desk and walk around — there’s always someone who needs help finding their way, a colleague that needs encouragement, or a new story to discover (and tell). If I’m in a system or regional office, the same principle applies — there are always many opportunities to make a difference.
Recently, I found a podcast called The Doctor’s Art: On Meaning In Medicine (TheDoctorsArt. com). Stanford oncologist Tyler Johnson and medical trainee Henry Bair interview a variety of clinicians, leaders, educators, and other healthcare professionals to learn about their journey to medicine and how they find meaning in their work. Listening to these stories inspired me to think about my “why” and to learn more about others I’ve encountered on my healthcare journey.
I love my work and consider having a healthcare leadership role a privilege. I’m grateful for the leaders and mentors who have guided me on this journey, and I’m excited about continuing to learn, grow and pay it forward!
Are you willing to share your “Why?” Email the Communications Subcommittee at info@achentx. org, and we’ll be in touch!
Stories about the journey to a healthcare career and the motivation to stay.
AUDRIANNE SCHNEIDER, FACHE
Anticipation was high for students and student council members of the ACHENTX chapter on a cool, cloudy February morning. Attendees of the 3rd Annual DFW Healthcare Student Summit gathered at the University of Texas at ArlingtonFort Worth for a day full of wisdom sharing and knowledge-flexing. Presented by the Student Council Committee of the ACHENTX chapter, the summit was an environment where younger members aspiring for an environmental scan and insight into the future of healthcare in coming years could learn from seasoned healthcare professionals.
After a continental breakfast and some light networking, event organizer and student council committee member, Vincy John, called the summit to order and found her stride in thanking the crowd for coming. She shored up summit housekeeping issues and thanked sponsors for their support. Vincy found this was also an excellent opportunity to highlight the chapter’s new Platinum Sponsor — Children’s Health.
Focusing on “Advancing Healthcare in 2023”, moderator Dr. Arturo “Art” Gonzales, DPH, MS, LFACHE, kicked off the discussion by sharing a bit about the Healthcare Management Program at UTA. He was specifically proud of the internationality and diversity of the program and how it brought kudos from surveyors during their accreditation process.
Dr. Gonzales then moved onto introducing the first panel of the summit, “Navigating the Current Financial Landscape.”
• Rick McWhorter, CFO, Texas Health Resources
• Tammy Walsh, FHFMA, CHFP, CRCR, CEO and Founder of Paramount Healthcare Solutions
• Jason Fry, Administrator, Business Sustainability & Development, Parkland Hospital
• Caroline Znaniec MBA, MS-HCA, CRIP, Healthcare Provider Operations and Revenue Integrity Solutions Leader at Protiviti
Rick McWhorter, who came to healthcare via a certified professional accounting background, jokingly noted [that when discussing healthcare] “don’t forget about CPAs”, garnering a subtle giggle from the entire attendee group.
Dr. Gonzales asked the panel, “What are some of the current financial impacts healthcare is facing?”
Mr. McWhorter discussed how the state of Texas will begin unenrolling Texans from Medicaid once the pandemic is officially considered closed, noting that millions of Texans will be pushed unwillingly into the marketplace.
Tammy Walsh pointed to the revenue side of healthcare and described how she had seen a significant increase in bad debt from self-payors.
Carolyn Znaniec pointed to issues with complying with federal mandates for price transparency. She quipped, “there is no standard public structure, except for Maryland, for charges’’. The lack of standardization proves difficult to compare between systems — talking apples to apples. With the rise of independent consumerism, patients are now able to shop for their services but might find it tough to understand pricing. For more information on Maryland’s healthcare reform, visit sourceonhealthcare.org/states/maryland/
Dr. Gonzales then moved onto another question. “How do you budget for new services, lines, clinics, etc.?”
Jason Fry took a turn at answering this by first noting that this question must lead teams to demonstrate and espouse a forward, planning mindset. He went on to say that systems must be proactive and not so reactive by thinking about demographics and the reasons why a new project is needed. “You have to look at people, payor mix, and competition,” he said.
Tammy Walsh gave an example of how she recently worked through a project that was aimed at an Emergency Department cost savings but was accomplished by opening a new pain clinic.
Mr. McWhorter chimed in, starting “healthcare systems chase population.” He also noted that the social determinants of health play a large role in decision making processes.
Mr. Fry rebutted from the perspective of a Safety Net facility and argued that traditional return on investment may be negative. His example was the proliferation of outpatient service focus.
Lastly, Mr. Walsh made a profound statement noting that “accounting is black and white; finance tells a story”.
A short lunch break followed the first panel discussion with more networking. This made for a particularly great time for the students to interact with the panelists and ask more probing questions.
The second panel focus was on Quality. Aptly headlined as “Ensuring Exceptional Care during Challenging Times,” Dr. Gonzales introduced the panelists as leaders of quality for their systems.

• Joey Sudomir, MS, CHCIO – CIO, Texas Health Resources
• Angela Vincent Michael, FACHE, CPHQ, LLSBB – Director, Process Improvement at Methodist Health System
• Veronica Elliott, MSN, RN, CPHQ, LSSYB Director, Quality Services at Methodist Southlake Medical Center
• Jazz Patterson, Founder and President of Process Villagem
• Quintin Ficklin Jr., MHCI, LLSYB Health Informaticist at Methodist Health System
The first question posed to the panel was aimed at how healthcare systems are addressing quality, patient safety, and reliability.
Angela Vincent Michael opened up with an unwritten rule that initiatives should follow a typical framework for success to occur. Institute for Healthcare Improvement (IHI) model, PDSA/ Deming Cycle, and others are methods and models for improving quality.
Dr. St. John added that quality projects must impart sustainability values and then gave an example of a hospital that always utilized the same team members for quality projects over and over which lead to a certain degree of apathy and decrease in the potential functionality of the project.

Veronica Elliott explained how data can actually be a weakness if it is not used appropriately, specifically noting that data must be focused and patient-driven. Joey Sudomir added, “you manage what you measure.”
The next question Dr. Gonzales asked the panel was about best practices for creating a culture of quality improvement.
Veronica told a personal experience story, “I made it my mission to make it more fun.” She laughed at herself and told of how the staff of her facility had named her the “Grinch.” “However,” she went on, “by familiarizing front line staff and leaders, and breaking down perceptions and old nuances,” she was able to institute a culture of acceptance for quality projects.
The last agenda item for the Summit was a keynote address by none other than President and Chief Executive Officer of the Dallas-Fort Worth Hospital Council, Mr. Steve Love. Always a crowd favorite wherever he speaks, Mr. Love did not disappoint.
His address covered and recapped many of the items of discussion for the day. He also spoke of some elements of the political landscape that greatly affect healthcare. He opined that the very future of healthcare leadership sat in that room for the day. Being present there to learn beyond the scope of the classroom on how healthcare challenges will be met in the future were the essence of his final thoughts.

innovative care. award-winning team.
Children’s HealthSM is redefining incredible care. With the support of our executive team, we’re able to pursue groundbreaking research and innovative medical technology to offer better treatments every day. Together, we’re providing more incredible care for kids across Dallas, Plano and beyond.
LEARN MORE AT CHILDRENS.COM.

AFTER HOURS















Creating
To learn more, visit MethodistHealthSystem.org
Texas law prohibits hospitals from practicing medicine. The physicians on the Methodist Health System medical staff are independent practitioners who are not employees or agents of Methodist Health System. Methodist Health System complies with applicable federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex.



















Once again, Texas Women’s University (TWU) hosted the 2023 Women’s Healthcare Executive Network (WHEN) event on Friday, March 3rd, featuring Judy Hoberman as the Keynote Speaker focusing on empowering professional women. There were also four break-out sessions, addressing areas specific to women’s daily challenges in the workforce.
The event started with breakfast and networking, with Charmaine Christianson introducing our speakers and providing a quick overview of the session topics. It wasn’t easy to decide which session to attend as all were relevant to our daily challenges.
Lara Burnside addressed Paving the Way for Mindfulness. Margaret Base’s topic covered Paving your Resume and Interview. Lorie Thibodeaux discussed Paving Your Network, and Crystal Brown reviewed Paving a Path to Overcoming Imposter Syndrome. Due to time restraints, we could only attend two sessions, and I chose Lori Thibodeaux’s and Crystal Brown’s, as these topics piqued my interest.
Lorie Thibodeaux focused on the best way for introverts and extroverts to expand their networks and “network the right way” through avenues like LinkedIn or in-person events like the event we attended. For introverts, she suggested connecting with an extrovert to work the room as a partnership. In contrast, extroverts need to remember to listen to others instead of doing all of the talking.
Crystal Brown focused on self-doubt and feeling like you don’t belong at the table. One of the suggestions was to have a “tribe” that supports you and understands your goals in life and business. Your support group needs diverse individuals (men and women), and there should be listeners and action-oriented individuals to push you to the next level.
Judy Hoberman wrapped up the event with her keynote address focusing on empowering professional women. One of her suggestions was to have a coach. She illustrated this with an excellent quote “Even elite athletes have a coach,” as they always want to challenge themselves.
HER SUGGESTIONS WERE:
• Set personal development goals
• Practice Self-awareness
• Get Feedback
• Build your network
• Mentor the next generation
• Advocate for leadership development
The day concluded with the WHEN Committee providing door prizes and closing comments thanking the event sponsors, TWU, volunteers, and everyone in attendance.





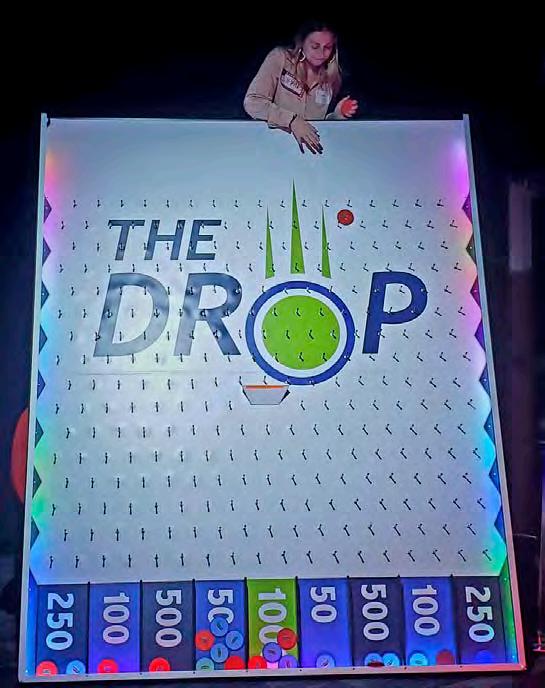
What do Steve Harvey, The Price is Right, and ACHENTX Member and Healthcare Leader John P. Carter have in common? Nope! It’s not awesome manly facial hair.
The answer is…
Friendly game show competition at the ACHENTX After Hours Networking Event back in March this year.
ACHENTX members gathered for an amazing session of contentious and proverbial style duke-it-out games fashioned after television game shows like Wheel of Fortune, The Price Is Right, and Family Feud.
Hosted by our local ACHE chapter at Game Show Battle Rooms in Addison, Texas, several chapter regulars and a few newcomers split up into two self-named teams, The Brain Stompers and The Show Stoppers, and spent an hour living their television game show dreams.
Members gathered in the lobby, were greeted by their Game Show Battle Rooms Host, rules were explained, and the fight was on to see who would dominate.
Paired against the other team, members competed in challenging word games, pricing strategy competitions, and “Plinko”-style fun. Answering questions in groups, solving moderately difficult puzzles, and strings of luck were the highlights of this bold yet friendly entertainment.
A lopsided victory seemed evident early on when The Brain Stompers took a wide lead.
Only to fall victim to a come-from-behind surge late in the game, they eventually lost to The Show Stoppers.
Afterward, members wagon-trained a few blocks away to nearby ODD Muse Brewing Company for some refreshments and a bit of braggadocious camaraderie. There they were able to sit and network in a very fun and cozy fashion to discuss roles, goings on at work, new projects, and celebrate a few victories amongst friends.
Despite the inherent natural competitiveness quickly spawned in the game show, all members in attendance commented on how much fun the entire event was and agreed that they all were lucky to have such a wonderful group to network with.



On Thursday April 6th, members and guests of the North Texas chapter of ACHE participated in a virtual event to review Telemedicine in the Healthcare Delivery System.
The event was moderated by Nick Kagal, FACHE, FHIMSS, who serves as Vice President of Marketing, Business Development & Customer Success at SpinSci.
• Mae Centeno, Chief Nursing Officer, Virtual Care Center and Virtual Care Delivery for Texas Health Resources
• Vicki Nolen LVN, MAPD, LSSYB, System Director, Clinical Excellence and Virtual Care at CHRISTUS Health
• Julie Hall-Barrow, EdD, President at Maxwell Telecare.
Nick’s opening statement was on point: telehealth has seemingly improved patient access, reduced overall cost of care and made an incredibly positive impact for certain specialties such as behavioral health.
However, there remain challenges regarding technology/internet connections, consistency of care, reimbursement, and regulations.
Mae shared a few of the ways Texas Health Resources (THR) has entered the telehealth space. THR provides patients a virtual companion. These are typically nurses who can
manage up to 15 virtual patients who are on observation to prevent slip and fall accidents and improve post-care compliance.
THR also provides urgent care quick visits via telehealth and an “at-home” program for inpatient care. The virtual care is provided by a team including a physician, an advanced practice provider and a Registered Nurse.
To support the virtual team, there are local community Emergency Medical Technicians and clinicians who can check in on patients as needed. To support the virtual services, THR uses several networks in case one goes down. There are also additional generators in case there is power loss.
Vicki shared some of the ways CHRISTUS is utilizing telehealth. The system offers remote patient monitoring, “at-home” care for patients, and virtual care for specialist visits.
Julie, who has been in the telehealth space for much of her career, discussed how the past few years have blown the walls down between society and virtual care delivery. She discussed how her organization leads programs for the homeless, providing care for them wherever they may be located. She also highlighted the value that primary care physicians provide acting as the leader-coach for patients to receive care outside of the hospital, thus reducing the cost of care.
The next question posed to the panel was regarding the issues related to funding for telehealth services.
Julie discussed the necessity of cyber security funding to protect private health information collected via telehealth. She discussed various
compliance issues that must be resolved for the use of collected health data. She also highlighted the challenges of technical components necessary to provide, store and protect health information.
Mae shared that she believes observing regulations will be key for the future of telehealth funding. The key issue in Mae’s opinion, is converting virtual care to be the safest and highest quality of care.
Vicki also discussed the technical components that are needed for physicians to provide quality care via telehealth. We must ensure that all providers have the best headsets, speakers, and laptops.
Nick asked about patient experience related to virtual care.
Vicki discussed that patients are typically very grateful to have clinical support and to learn more information about the disease and options of care.
Julie shared that in her experience, patients have always had a favorable opinion regarding telehealth due to the convenience and access. She noted that in addition to patient satisfaction, the past few years have seen provider satisfaction with telehealth improve. Providers were forced to use telehealth due to the pandemic and realized how convenient the service can be and how continuity of care is improved.
Mae focused her answer on the increased satisfaction of hospital patients due to telehealth. She discussed how virtual rounding has provided hospitalized patients more dedicated personal time with their care team.
Julie talked about how the pandemic changed the perspective around telehealth. Prior to the pandemic, providers were hesitant to use virtual care, concerned that outcomes may not
be positive, causing patients to be critical. Now providers feel the opposite — if they do not provide virtual care options, patients may be less satisfied with the overall care delivery.
They then addressed the geographical restrictions that may limit or hinder the delivery of telehealth.
Vicki discussed working with groups outside of the state where her organization is located. She advised organizations to follow the CMS federal rules, state rules, and medical board rules to ensure that compliance is met. These rules may be different in each state and with different boards.
Julie also shared that rules are different for various providers and staff. For example, rules for physicians are different from rules for advanced practice providers and medical assistants. She suggested that organizations create teams to keep track of rules and ensure compliance.
The conversation then moved to discussing how patients have adopted telehealth.
Mae spoke about how age groups from the early 20’s to the late 80’s have adopted primary care telehealth delivery. She said that the average age of patients for THR’s “at-home” care is 78 years of age.
She did also said providers in the inpatient space have been slower to adopt, likely due to fear of being replaced by virtual care. She stated that, in her opinion, humans will not be replaced, and that telehealth is just another way that providers can care for their patients.
Vicki focused on the workforce staffing issues as a hurdle to adoption. The shortage of clinical staff needed to provide high quality care limits how often providers can integrate the service into their delivery model.
The next question focused on the future of telehealth.
Vicki spoke about artificial intelligence helping to monitor patients to keep them safe while inside the hospital or receiving care at home.
Julie agreed and said that predictive analysis, that AI can provide, will help with patient care. She also highlighted how telehealth can be the answer for patients who live in rural America.
Mae focused her answer on the clinicians and the necessity to provide clinicians more training on telehealth. She believes that medical schools will be offering courses on telehealth and will be partnered with healthcare organizations to provide needed training to all levels of the clinical care delivery team.
Vicki expanded on the need for additional training related to telehealth. Clinicians understand how to read patients body language and observe how the patients and family behave during a face-to-face clinical encounter. She discussed how clinicians need to be trained on how to observe similar data via telehealth.
Julie and Mae both discussed how the future of telehealth may provide our clinicians additional careers after they no longer want to work in the face-to-face clinical setting. For example, nurses who can no longer stand on their feet all day, can provide outstanding quality care via telehealth.
Vicki and Mae talked about how the future of telehealth must include more internal oversight and management of the virtual services. As use of telehealth expands the federal government will be investigating telehealth reimbursements to ensure that there is no fraud or abuse.
Overall, the panel was highly enthusiastic regarding the future of telehealth and all agreed that the care model is here to stay.

Patients appreciate the convenience and access of telehealth. Providers will continue to use the model of care as another option to provide the triple aim of healthcare delivery.

On May 16, 2023, ACHENTX held its Networking Blitz event at Texas Health Resources Corporate in Arlington, TX. Coordinated by the Networking and Membership Committees, this biannual event allows members to get to know each other in meaningful ways through fun activities, meeting chapter leadership, networking over dinner, and topical discussions.
The special guest for this event was Kris Sanders, FACHE, who is the Senior Vice President of Northern Market Growth and Development at Children’s Medical Center Plano. Kris emphasized the importance of utilizing LinkedIn when making relationships. After sharing her career journey, she also shared tips and advice for networking, including going to events with a “buddy” who can introduce you to other individuals. Kris is also active in the community with various non-profit and leadership organizations. She encouraged others to discover their “why” and their career motivators. Finally, she took questions from the crowd of over 50 diverse attendees which was composed of students and working professionals.


Special thank you to Texas Health Resources for hosting this event.









SpinSci Technologies hosted the second quarter education event on April 27th, which focused on staff retention and mentoring.

Moderated by Nick Kagel, FACHE, experts on the first panel discussed effective management techniques used to retain staff. The conversation began with acknowledging the numbers of people leaving health care and ways to encourage more to enter the field. The group agreed that a key tenet to success is to look at the diversity in the community, have a staffing model that supports diversity, evaluate the staff support framework, and identify a clear path for growth.
Panelists shared the following retention tools:
Acknowledge burnout and offer help. This should be a consistent conversation — emphasizing that caring for the whole person is important.
Look at what’s important to the staff, knowing that not everyone wants the same things.
• For example, tuition reimbursement is important to some while pet insurance may mean more to others.
• Are there additional employee tools available through your existing Employee Assistance Program?
• Would a flexible staffing model make life easier at home?
• Be sure to provide a “Total Rewards” or “Total Compensation” statement that shows all benefits, not only compensation.
Establish meaningful connections from the beginning. Consistent touch points (at least once per month) are crucial as well as learning more about an employee’s career and education aspirations as well as their life overall.
Create a pipeline. There’s a fundamental talent shortage. It’s important to get entry-level staff interested in growing and showing them some options (i.e., tuition reimbursement, mentoring, etc.). Help people see a wide variety of careers and start early (K-12) — including Lab, Pharmacy, Physical Therapy and other paths.
The manager skill set is imperative to retention. When hiring managers, look for empathy, authenticity as well as good communication and listening skills.
After dinner and networking, panelists discussed the different types of mentoring and the attributes of an effective mentor or coach.
Moderated by Jennifer “J” Alexander, FACHE, the conversation began by identifying the differences between mentoring (developmentdriven), sponsoring (advancement-driven), and coaching (performance-driven).
The panel also defined the different types of mentors (formal, informal, peer, thought leaders and being a mentor-in-the-moment).
The first step with any type of mentoring is to create a safe and trusting environment. It’s also important to build a personal relationship.
Some tips for mentors include: prioritizing mentoring, building on your own skill set, and practicing active listening.
For those seeking to mentor, opportunities include volunteering (i.e., join a committee/ ACHENTX), building your network, defining what success looks like to you, and enjoying the journey.
For new leaders to an organization, it’s important to support them through activities like the daily safety huddle. J finished the discussion with some Q&A from the audience, sharing stories and emphasizing the benefits for both mentors and mentees.
Christi Nguyen, FACHE, closed the session by thanking the panelists and announcing a donation in honor of their service to the ACHE North Texas Leadership Legacy Fund.
PANEL 1: Managing for Morale –Effective Management Techniques to Retain Your Staff
• Nick Kagel, FACHE; VP Marketing & Business Development, SpinSci Technologies (Moderator)
• Katie Bata Heeter, FACHE; SVP Human Resources Strategic Business Services, Baylor Scott & White Health System

• Kathi Cox; COO, Ambulatory & Virtual Channel, Texas Health Resources
• Priti Jain; Regional Director of Specialty Clinics, Texas Health Physicians Group
PANEL 2: Developing Mentoring and Coaching Skills
• Dr. Jennifer “J” Alexander, FACHE; Operations Manager of Imaging Systems & Services, UTSW (Moderator)
• John E. Phillips, FACHE, President, Methodist Dallas Medical Center
• Jackie Sifuentes, MBA, LSSYB, Manager of Patient Capacity Ambulatory Services, Children’s Health
• Tanya Stinson, MHQS, CMBB, MCBA, CRP, Founder of Leaning Towards Change, LLC and Supervisor of Data Governance, Texas Health Resources
On April 25, 2023, in spectacular fashion, guests were welcomed to the rooftop area of Stirr Addison where an amazing assortment of lite bites and small-plate foods were beautifully arranged for all. As tradition dictates, cocktails were served and members had access to full-bar privileges for purchase.
Jenny Givens gave a warm welcome and thanked all of the sponsors before she introduced the moderator and turned it over to the panel.
The panel discussion revolved around the benefits of Artificial Intelligence (AI) in healthcare with a specific note of best practices and pitfalls to avoid when implementing AI in your hospital or healthcare system.
James Sherer, JD, of BakerHostetler’s Digital Assets and Data Management Group, moderated the panel discussion.
Panelists included Dr. Julie Balluck, DNP, RN, NEA-BC, Chief Nursing Officer at Texas Health HEB, Emily Fedeles, JD, CIPP/E, Vice President and Associate General Counsel of Privacy at Medidata, Albert Karam, MS, MBA, VP of Data Strategy and Analytics for Parkland Center for Clinical Innovation, and Dr. Ron Nelson, DBA.
Moxi, from Diligent Robotics, was the first item of discussion. Moxi is an AI-driven robot that assists hospitals in mundane, repetitive, non-patientfacing tasks at scale such as fetching supplies from storage, delivering PPE to provider areas, and distributing medications.
Panelists were sure to ease any angst and trepidation of those whose hospitals haven’t used
these types of robots by reminding attendees that “Moxi isn’t the Terminator”. But they did note that AI Robots are trending and changing the landscape of some employment. However, there are still many jobs that are required for behindthe-scenes control of these devices ensuring that the robots are staying on task and productive.
When asked by Sherer how other integrations have contributed positively to healthcare environments, Albert Karam pointed out that during the pandemic, bed capacity created a small and constant scare among leaders, but that Parkland used machine learning to predict how many patients were expected to arrive at their hospital, how many beds would be needed, how many ventilators would be needed, and then created a daily forecast model that was reviewed as far as two weeks out for their specific situation.
Albert specifically noted that “it [the machine learning] is entirely dependent on the data”.
Near the end of the panel discussion, the venue’s own technological issues with microphones and audio systems began to have problems. Panelists were able to expedite their final thoughts and comments before a robust round of laughter eased the awkwardness when a guest mentioned how technology was great when it is great, but just as the microphone issue proved, when it’s not, it can be a real issue.
Guests applauded the panel and moderator and continued to enjoy the remainder of the evening by networking and fellowship.





John Hawkins knows the Texas Legislature and more than a thing or two about how the U.S. Congress works, as well. With the bi-annual Texas Legislative Session winding down, the Chief Executive Officer of the Texas Hospital Association (THA) spent his lunch-hour on May 15th sharing insights and lessons learned over a 35-year career in advocacy.
With just two weeks left in the Session, Hawkins said now is not a good time to reach out to your state senator or representative. Instead, he advised playing a longer game. One that starts with getting to know who represents you and finding ways to connect with them directly between legislative sessions and elections.

“Start early. Get to know them when not in session,” said Hawkins. “Invite members of your delegation to your facility. Use THA as a resource. We can help you invite them.”
Even though there are a handful of licensed clinicians serving in the Legislature, Hawkins suggested becoming a trusted resource for members.
“They’re not experts,” he said. “They’re looking for folks who are to help them understand our issues.”
Hawkins tells a story about a system in Houston that shows members of the Legislature how hard systems must work to secure prior authorizations, chasing payment delays and otherwise battling with payors to ensure access to care.
“They show them the bullpen of people it takes to do all this,” he said, and that those are resources that are being diverted from bedside care delivery to perform these administrative tasks.
Another thing ACHENTX members can do to influence the policymaking process, Hawkins said, is joining and participating in THA’s political action committee HOSPAC.
During Session, Hawkins and his team are working the Legislature nonstop, advocating for hospitals, health systems and the more than 400,000 people who work for them.
Oftentimes Hawkins said, the work is more about stopping bad legislation than passing legislation. “That’s the biggest takeaway,” he said. “The process is set up to NOT pass legislation.”
That’s not necessarily a bad thing, he added. “Only the budget is a must pass every two years. Otherwise less regulation is written in the state constitution. So, things get a little bottled up, which creates a high threshold to get things passed.”
Of note this late in the Session, Hawkins said were several bills. A bill prohibiting facility fees, while technically defeated, is still being closely watched so it doesn’t become a lastminute amendment on a late-moving piece of legislation. There were also bills requiring cash paying customers and the uninsured to use a system’s lowest contracted rate, which Hawkins explained was rate-setting in the form of dubious policy. THA opposes all these bills.
As Session races toward its final day, Hawkins and his team were focused on keeping Medicaid and trauma programs at their current funding levels. Something he called a “do no harm approach” where he is quick to remind legislators about the financial challenges hospitals continue to face even as the National Health Emergency has ended.
THA’s mission doesn’t stop when Session ends. Hawkins said he will continue to focus on how to make sure we’re growing with our communities, that policymakers understand hospital operations and economics better, especially regarding inflation’s impact on operating margins where there’s no relief in sight for the nearly 50 percent of hospitals with negative operating margins. Moreover, he acknowledged that maternal mortality remains an issue as well as more state funding for behavioral health initiatives and programs.
The THA provides members many tools and briefings to stay briefings stay abreast of and knowledgeable about the issues facing hospitals and health systems in Texas.
Advocacy Communication Tools
• Health Care Advocate - weekly
e-newsletter to membership
• Membership Action Alerts
• Membership Information Alerts
• Advocacy one pagers –specific topics, specific regions, education, advocacy.
• Facebook, Twitter, Website
• Digital campaigns including geo-location
• Texas Hospitals blog
While these vehicles are largely designed to keep THA’s members informed, Hawkins said they are widely disseminated among legislators, too, so they have a chance to learn more about the many issues health leaders grapple with every day.
The average legislative office handles the following during the 140-day session:
• 7,000 + bills
• 6,000 + telephone calls
• 5,000 + drop-in visitors
• 8,000 + letters
• 40,000 + emails
• 600 + invitations
• 140 Days isn’t the time to make introductions.
• Give Hospital Tours to Elected Officials
Congressional, State and Local Leaders Engage with Elected Officials
• Attend Local Meetings
• Be a Trusted Resource on Health Care
• Trustees are Critical to the process
• Engage with THA!
• VOTE in Elections!
• 76% of voting age population is registered BUT only 8% of registered voters voted in 2018 Primary Election
• 60% of registered voters voted in 2016 presidential election.
SUMMARY:
• 46/100 voting age Texans vote and decide elections in presidential years.
• 6/100 voting age Texans vote and decide elections in off year elections.
YOUR VOTE DOES MATTER
Austin State Rep. Donna Howard won by just FOUR votes!
The discussion about ethical challenges in healthcare leadership was lively, energizing and thought-provoking. Moderator Mark Schnitzer, MD, FACHE, Medical Director for Baylor Scott & White Quality Alliance, opened the session by asking about the differences between leaders and managers.
Archana Mahimkar, Senior Director Clinical Quality, Improvement, and Safety for Walgreens Health, made the point that leaders aren’t born — they are made through “…hard work, making mistakes, learning and moving on.” It’s the job of the leader to set the example of what is right and true through his or her actions and relationships and she stated, “Ethical leadership is the only way.”
Melanie Roberts, Chief Compliance and Ethics Officer for Parkland Health, encouraged leaders to take a look at their organization and determine where it is in the journey as well as going back to the mission. Asking questions like, “How does the mission tie to the values?” and “What does the community and customer expect from us” can provide a meaningful start to the process. She advised involving employees in the work, having a plan for ethical lapses and providing positive incentives to do the right thing.
Javier Montemayor, North Texas Division Ethics and Compliance Officer for HCA, emphasized that effective reporting systems are driven by the culture and that it’s important to ask the
question, “Do we have an ethical challenge?” when situations are brought forward. He also advised implementing a consistent approach toward conflicts of interest and to define who in the organization would be required to complete a conflict of interest questionnaire (which should be clear and concise, 5-7 questions, automated and completed within the first 90 days of employment). The discussion concluded with the challenge to pause and reset after COVID — and determine if there’s a better way to do this versus pre-pandemic processes.
Dr. Schnitzer closed the session by thanking the panelists and announcing the donation in honor of their service to the ACHE North Texas Leadership Legacy Fund.
• Archana Mahimkar, Senior Director Clinical Quality Improvement and Safety, Walgreens Health
• Javier Montemayor, Division Ethics and Compliance Officer, North Texas HCA Facilities, Rapides Regional Medical Center, Louisiana HCA Healthcare
• Melanie Roberts, Chief Compliance and Ethics Officer, Parkland Health
On April 18, 2023, at the CHRISTUS Health headquarters in Irving, Texas, ACHENTX met for one of the most popular event series hosted by our chapter, Breakfast with the EVP.
The event began with a warm welcome from chapter member and Networking Committee member John P. Carter, where he gave updates and delivered announcements, as well as thanked our sponsors for their participation and support.
Mr. Carter then introduced the event’s speaker, Sam Bagchi, MD, Executive Vice President and Chief Clinical Officer, of CHRISTUS Health System.

Dr. Bagchi began his presentation with the history of the CHRISTUS Health System. He noted that CHRISTUS is a Catholic, faith-based system with hospital and healthcare locations in three states — Texas, Louisiana, and New Mexico — and three other countries — Chile, Mexico, and Colombia.
He detailed how their mission began with French priest Claude Marie Dubuis, eventually Bishop of Texas, who came to Texas in the mid-nineteenth century. Bishop Dubuis penned a letter to a friend in France for help caring for the ill and injured. Three Catholic nuns went to assist Dubuis, and CHRISTUS was born as a health system with a mission to provide healthcare to everyone.
Dr. Bagchi went on to discuss his journey in healthcare, beginning with an internal medicine residency in Boston. He made specific mention of how the hospital created its own Electronic Medical Record (EMR) before it was even a “real thing.” This was his introduction to
health information as a sub-specialty of his career pathway.
He later found himself in Dallas, Texas at Methodist Healthcare System as the Chief Medical Informatics Officer, and eventually on to CHRISTUS.
Dr. Bagchi described how he became a selfproclaimed “technology-driven healthcare leader”. Through his work, he recalled episodes of his grumbling about healthcare inefficiencies [because of the lack of technology use]. With a reference to a YouTube influencer with an appropriate moniker of Dr. Vader, Dr. Bagchi emphasized that physicians should “use their power for the Good Side”.
He went on to discuss that physician burnout is real. He quipped that “A sleep-deprived, disruptive physician leader is not good.” He described how he is confident that systems can encourage physicians to overcome burnout by using advanced software to improve inefficiencies. He gave an example of a platform where physicians can and should utilize artificial intelligence to generate patient notes and narratives in the EMR.
Dr. Bagchi wrapped up his address with comments about cultural differences. Despite most cultural differences seeming vastly dissimilar on the periphery, many are congruent or even identical when discussed in the same context and after scratching through the surface.
He was awarded by the audience with a round of applause before members broke to continue networking or depart to begin their workload for the day.
The 2023 ACHE Congress on Healthcare Leadership took place in Chicago on March 20-23, 2023. With over 5,000 attendees and 150+ education and networking sessions, this year’s theme was “Bolder, Brighter”. Our ACHENTX chapter was well-represented with members speaking at sessions, attending networking events, and being recognized at the Convocation Ceremony for attaining their Fellow status.



The 2024 Congress will take place on March 25-28 in Chicago, Illinois.
Special thanks to Pinnacle Healthcare Consulting for hosting the ACHENTX Cocktails at Congress Reception.



Kartika M. Ayyappan
Asheki C. Brooks
Melissa Bryant
Lucky Denenga, PT, DPT
John Fadimiroye, MSHA
Saadia Farooq, MD, MBBS
Donita Fleming
Breann Gwinn
Joan Hale
Jonathan L. Ives
Ingrid Kindipan, PhD, MSN, RN
Archana Mahimkar
Ankit Mehta
Gunveen Mehta
Stephen J. Page
Pratyusha Pedaprolu
Joe Price
Mark Riordan
Nyomie Rodriguez
Kelton Schweitzer
Stacy Sears Lamb, RPh
Carlos Sepulveda
Jacob Stercula
Jennifer Styers, APRN, NP
Kelechi L. Wabeke
Leah Wade, BSN
Courtney Wakefield
Katy Wright
Wenjun (April) Yang, BS, MHA
Idowu M. Adegbaju, RN
Alyssa Aldrich
Daniel O. Beck, MD
Vanita Brinkley, BS
Valeria Chavez
Makensie Cowart
Kim Cummings, SPHR
Farhad Eghrari, BS
Angie K. Fraticelli, MHA
Donald Friedman
Prathima Guntipalli, MD
Sean D. Hammerle
Brian M. Huber
Alyssa Hutto
Mary J. Jimenez
Sam Johnsen, MHA
Srikanth Jyothinagaram, MD
Kendra King
Rebecca Longino
James McGlothlin
Salina Morrow
Nanette L. Myers
Tiffany Ogundipe
Michelle M. Olson, MD
Dena Palmer
Sandra Pang
Richard Patterson
Laura Rasor
Priscilla Reyes
Andrea Sartin
Manon K. Tesche
Gary V. Trepanier, MPH
Edward Van Horne, MBA
Christopher J. Wainerdi, MBA
Melissa Williamson
Shannon Wishin
APRIL
Fatima Abraham, DHA
Lydia Ameka-Bunei
Ranae Beck
Deniro Brown, RN, MSN
Jonathan Buchanan
Robert A. Burke, III
Andrew Caraveo
Mandy J. De Vries, MSc
Sharbari K. Dey, PhD
Lisa A. Donaldson
Victor Fishman, PhD
Jake Frost
Blanca D. Garcia
Niko Harrell, BS
Carl A. Heath, DC
Matthew T. Hoffman, DMin
Jaylin M. Johnson, MHA
Selin M. Mathew
Garrett A. McCaskill, DHA, MBA
Michelle Murray
Velisiwe S. Nkomo, RN
Patrick I. Omoragbon, RN, BSN
Jose Peralta, BSHA, MBAHC
Kevin Reeves
Missy Staben, BS
Rebekah Stewart, JD, MBA
C. Paulette Thomas, MD
Victoria Washington
Trisha Watson, MBA
Tanisha Wilcots, MSN, RN, NE-BC
Martin Williamson, Jr., RN
Nathan Wylie
David Zavala
MAY
Rebekah Abernathy
Renata Aburime
Jonathan Dietz
Nancy M. Green
Kollier J. Hinkle, MD, MS
Traci Holton
Onyemaechi Igwe
Albert Karam, MBA, MS
Merlyn Kavalam
Cristobal Kripper
Katie Kuri
Christopher LeBlanc
Sharae Lemoine
Chad Martin, MBA, RRT
Rochell D. Melton
Chaplain Stacey R. Merlin
Destiny Oribhabor
Kelsey L. Petty, MHA
Aimee Plowman
Jake Thomas
Rachna Varma

MARCH
Jabeen P. John, PharmD, FACHE
APRIL
Paul C. DeBona, FACHE
MAY
DeLancey Johnson, FACHE
FEBRUARY
William H. Craig, LFACHE
Brandi L. Crawford, FACHE
MARCH
Kyle A. Cavin, FACHE
Debbie Cox, FACHE
Amber Long, FACHE
APRIL
William Garner, DrPH, FACHE

MAY
Stuart L. Archer, MBA, FACHE
























