OF NORTH TEXAS



POWERFUL GATHERING: The 2025 ACHE Congress on Healthcare Leadership




POWERFUL GATHERING: The 2025 ACHE Congress on Healthcare Leadership
EDITORS
Amanda Brummit, FACHE
Holly Hrabik
Sarah Sentmore
Kean Villarta
Bert Witherspoon, FACHE
CONTRIBUTING
Michael Belkin
Amanda Brummit, FACHE
Holly Hrabik
Susan Merritt
Sarah Sentmore
Audrianne Schneider, FACHE
Ken Villarta
Bert Witherspoon, FACHE
info@achentx.org
ACHE of North Texas
Editorial Office, c/o Executive Connection PO Box 224732, Dallas, TX 75222-4732
p: 972.413.8144
e: info@achentx.org
w: achentx.org
President - Ajith Pai, FACHE
President, Texas Health Harris Methodist Hospital Southwest Fort Worth
President-Elect - Kris Sanders, FACHE
SVP/Northern Market Growth & Development Children’s Health
Immediate Past President - ACHENTX Foundation Liaison
Aaron Bujnowski, FACHE
Managing Director, Health Industry Group | Health Systems Practice, Alvarez & Marsal Holdings, LLC
Treasurer - Sponsorship Committee Liaison
Tim Bowen, FACHE
President, Baylor Scott White - McKinney
Diversity, Equity & Inclusion Officer - Membership Liaison
Michael Talley, RRT, FACHE
VP of Clinical Operations & Virtual Care, CHRISTUS Health
The ACHE of North Texas e-magazine, The Executive Connection, is published triannually and includes information on the latest regulatory and legislative developments, as well as the quality improvement and leadership trends that are shaping and influencing the healthcare industry. Readers get indepth reporting on the issues and challenges facing hospital and health system leaders today. We make it our job to tell you about the great things the organization and Chapter are doing every day to ensure the health of our community. If you have any news and updates that you want to share with other members, please e-mail your items to info@northtexas.ache.org. Microsoft Word or compatible format is preferable. If you have a graphic or picture that you'd like to include, please send it as a separate file. The following are the types of information that our members shared in past ACHE of North Texas magazines, Advocacy Issues, Legislative Issues, Educational Opportunities, Awards / Achievements, Promotions (Members On the Move), Committee Updates, journal submissions, conference submissions, and workshop participations, sharing

Dr. Jim Allard, DNP, RN, NEA-BC, FACHE
ACHE Regent-at-Large, District 4
Vice President & Chief Nursing Officer, Advocate Christ Medical Center
Crystal Brown
Women’s Healthcare Executives’ Network Chair Vice President Operations/COO, Methodist Mansfield Medical Center
Noreen Butte, MD
Physician Advisory Committee Chair/Liaison
Senior Physician Executive/Pediatrician
Barton Gill - Student Council Liaison Chair, Dept of Health Administration & Health Policy, UNT Health Science Center
Brandon Goertz, PhD, FACHE
Advancement Committee Liaison President, Texas Health HEB
Nick Kagal, FACHE - Education Committee Liaison HX Client Success Manager, Press Ganey
Jared Lange - Networking Committee Liaison
Director, Business Sustainability & Development Parkland Health
Christina Mathis, MHA
Sponsorship Committee Liaison
Chief Executive Officer, Medical City Frisco
Angela Vincent Michael, FACHE
Membership Committee Liaison
Director, Performance Improvement & Project Deployment Office, Methodist Health System
Laura Parsons-Yanez
Networking Committee Liaison
Senior Manager, Quality & Patient Safety Walmart Health
Cassandra Self, FACHE DE&I Committee Liaison Professional Services & Finance Officer, Texas Health Resources
Jared Shelton, FACHE
ACHE Texas – North Regent President, Texas Health Harris Methodist Hospital Fort Worth
Cardell Velez - Mentorship Committee Liaison Associate Vice President, UT Southwestern
Timothy Wilson - DE&I Committee Liaison
SVP, Population Health Management, P3 Health Partners

ACHE of North Texas: Powered by You
If there’s one thing that continues to inspire me as President of ACHE of North Texas, it’s the incredible momentum our members bring to this chapter. Over the past two months alone, our collective efforts have resulted in one of the most active and engaged periods in recent memory—and it’s all because of you.
At this year’s ACHE Congress on Healthcare Leadership, we had an incredible showing. With over 300 members from North Texas in attendance, we were one of the most represented chapters in the country. It was an honor to help co-host the Pre-Congress Reception alongside our six fellow Texas chapters. That reception captured what’s best about ACHE: community, collaboration, and a shared vision for healthcare leadership that transcends any one organization or city.
And the energy didn’t stop at Congress. In just the past few weeks, we’ve packed in a remarkable lineup of events across North Texas:
• The Multi-Chapter Education Event at Texas Woman’s University (TWU) – Dallas, co-hosted with our East Texas and Texas Midwest colleagues, drew over 100 attendees.
• Our 2025 Mentorship Program launched with nearly 70 participants attending the program orientation, combined with a Networking Blitz at Scottish Rite for Children. This year’s Mentorship Program was one of our most competitive yet for our mentee applicants. To those who were accepted—congratulations. And to those who weren’t this year, please know that your interest is valued, and we look forward to helping you grow through other opportunities this year, and we encourage you to apply next year.
• Our Q2 In-Person Education event at Medical City Plano welcomed over 50 attendees, while the DFW Healthcare Student Summit at University of North Texas Health Science Center brought together nearly 60 future leaders.
• Cocktails with the Chiefs at Globe Life Field combined executive insight with a fun and memorable evening during the Rangers vs. Angels baseball game.
• We continued giving back with a community service event at Irving Cares, helping support local families in need.
• Our annual Women’s Conference returned to TWU-Dallas with 90+ registrants, creating another powerful space for connection and empowerment.
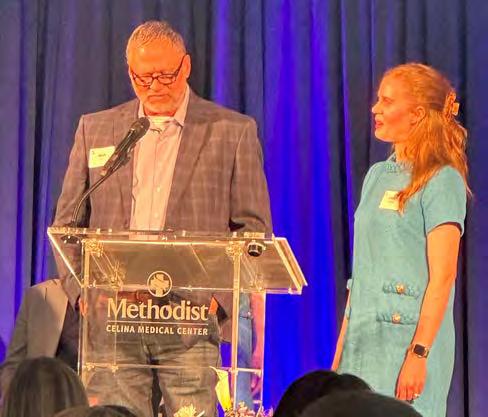
• And we had the rare privilege of previewing the new Methodist Celina Medical Center before it opened to the public—an exciting glimpse into the future of healthcare in our region.
All of this—every panel, every connection, every moment of service—was made possible by our members. You showed up. You gave your time. You brought others with you. That’s what makes our chapter not just successful—but exceptional.
As we look ahead to the rest of the year, I encourage you to stay engaged. Whether it’s attending the ACHE of North Texas Summit on November 6th, participating in a committee, or simply reaching out to someone new, you are shaping the future of healthcare leadership.
Leadership isn’t a solo act, it’s a shared journey. And sometimes the most powerful thing we can do is simply show up for each other, for our teams, and for the future of healthcare. Over these past months, I’ve seen how your presence—your willingness to engage, support, and lead—has kept our chapter moving forward. Thank you for walking this path together and for making ACHE of North Texas a place where leadership is lived out in community.

With gratitude,
Ajith Pai, PharmD, FACHE President, ACHE of North Texas


Does your head feel like it’s spinning with all the changes coming from the national, state, and perhaps even local levels related to our healthcare system? It seems like every time I check my news app, I see a splashy headline about a new outbreak, a seismic shift in public health policy, or a threat to reimbursement. It seems the only constant in our world is change.
How should we, as healthcare leaders, respond to this unprecedented time of change? While it may be tempting to tune it out or try to pretend it’s not happening, the fact of the matter is that we have a duty to lead. While some of the issues may seem overwhelming or beyond our influence, I believe we each have a responsibility to do what we can to prepare ourselves and our organizations for this change.
I recently heard a quote that resonated with me: “Leaders think and talk about the solutions. Followers think and talk about the problems.” We can each take action to help generate, share, and amplify the solutions needed to drive our healthcare system forward, and ACHE provides many opportunities to get involved and stay up-to-date with the latest issues facing our industry:
• ACHE of North Texas offers many valuable educational sessions throughout the year. Have you attended one yet in 2025? If not, I encourage you to sign up and hear from some of the healthcare leaders in our community who are making a difference. Knowledge is power, as they say, and being informed is a great way to stay ready.
• Become a Fellow of ACHE. Going through the process to become a Fellow will prepare you to “think about the solutions.”
• Consider serving as a mentor with ACHE or with ACHE of North Texas. Your experience and expertise can have a tremendous impact in helping to prepare the next generation of healthcare leaders for the challenges ahead.
• Volunteer on an ACHE of North Texas committee. Building a culture of collaboration and connection within our local healthcare community can have powerful results in North Texas and beyond.
The bottom line is that healthcare’s greatest challenges require the very best of us, and ACHE has the resources available to help each of us rise to meet them. I encourage you to get involved!




Dear Healthcare Leaders,
As we navigate the evolving landscape of our current political environment, the importance of Diversity, Equity, and Inclusion (DEI) in healthcare has never been more critical. This moment calls upon us to reaffirm our commitment to creating an environment where every individual—patient and provider alike—feels valued, respected, and empowered.
Diversity brings a wealth of perspectives that drive innovation and improve patient outcomes. Equity ensures each person has access to the resources they need to achieve their best health. Inclusion fosters a culture where all voices are heard and respected, contributing to the rich tapestry of our healthcare community.
In these challenging times, let us champion DEI not just as a goal but as a core value guiding our decisions and actions. Together, we can break down barriers, challenge biases, and create a system that truly serves everyone. Your leadership is vital in shaping a future where diversity enriches our practices, equity transforms our policies, and inclusion is the heartbeat of our organizations.
Let us seize this opportunity to lead with courage, compassion, and conviction, ensuring that our efforts in DEI lead to meaningful change for those we serve and for generations to come.
Best,
Jim Allard, DNP, RN, NEA-BC, FACHE
Medical City Arlington
ACHE Regent-at-Large, District 4
You



Cardell Velez, MBA, ARRT (R)(CT)(N), NMTCB(CNMT) AVP, UT Southwestern
Cardell Velez, MBA, ARRT (R)(CT)(N), NMTCB(CNMT), is the Associate Vice President of Health System Operations and Imaging Services at UT Southwestern. He leads Health System Imaging Services for all UT Southwestern hospitals and clinics and oversees Guest and Patient Services. He came to UT Southwestern from Highmark Health/Allegheny Health Network in Pennsylvania, where he served as the System Vice President.
Cardell is an Air Force veteran who was raised abroad in a military family. While deployed to Baghdad during Operation Iraqi Freedom, Cardell was responsible for all radiologic support to Task Force 21 and 3,500 wounded prisoners of war during the movement from Abu Ghraib prison to Camp Cropper.
Cardell completed a Master of Business Administration from SMU Cox School of Business and holds a Bachelor of Science from Wayland Baptist University.
Why did you go into health care?
One of the earliest memories I have is going to work with my dad, who was a pharmacy tech in the Air Force. At the time, they were installing the very first automated individual pill packaging system, and I remember sitting on the floor, unwrapping M&Ms as fast as the machine could pack them, just completely fascinated by the whole process. That experience, even as a kid, made me curious about how things worked behind the scenes in health care.
All through high school, I dreamed of becoming a pediatrician. But when I graduated, life took a turn — I ended up meeting an Air Force Nuclear Medicine tech who told me all about his job. That conversation changed everything. I joined the Air Force as an x -ray tech, fully set on working my way into nuclear medicine.
Why do you stay?
I stay in health care because, at the end of the day, it’s the only field where I’ve truly felt a deep connection to the purpose behind the work.
How long have you been a member of ACHE? 12 years
Why did you join ACHE?
I joined ACHE to build meaningful professional relationships, find mentorship opportunities, and provide mentorship. Additionally, I want to stay informed about emerging healthcare trends.
What have you gotten out of, or do you get from your membership in ACHE?
It’s given me access to a network of experienced healthcare leaders who are open to sharing insights. I’ve also benefited from the educational resources and events that keep me up to date on industry trends and best practices.
Your advice to others on how to get involved in ACHE: Take advantage of the learning opportunities: ACHE offers excellent webinars, leadership development programs, and publications.
How would you encourage other members to maximize their ACHE memberships?
I’d encourage them to get involved in a committee. It’s one of the best ways to build lasting connections, develop leadership skills, and contribute to the work ACHE is doing in the region.
What advice would you give early careerists or those considering membership?
My advice is to dive in early and be intentional about your involvement. Don’t be afraid to reach out to fellow members for informational chats or mentorship; most are very open and willing to help.
Tell us one thing that people don’t know about you. I am Canadian.
At HDR, we’re helping our clients push open the doors to what’s possible, every day. hdrinc.com I 972-960-4000


Matthew Hoffman, DMin, BCC Director, Faith in Action Initiatives, Baylor Scott & White Health
With more than 30 years of working in the nonprofit, community development sector, Dr. Matthew Hoffman oversees the humanitarian aid and medical missions arm for Baylor Scott & White Health (BSWH). He does so as the director of Faith in Action Initiatives (FIAI), which functions as a medical surplus recovery organization (MSRO) for BSWH’s local and international humanitarian aid work.
In this role, his team collects overstocked medical supplies and decommissioned equipment to partner with qualified nonprofit organizations by resourcing them with these goods for the sake of advancing care to medically impoverished people groups here in the United States and internationally. As the director of FIAI, Matthew has overseen the establishment of clinics and hospitals locally and internationally in former healthcare deserts. According to the MedSurplus Alliance, BSWH is only one of three other healthcare systems in the United States that have such a MSRO embedded within it for the purposes of humanitarian aid.
Why did you go into health care? Why do you stay?
I came into health care as a trauma chaplain to bring care to people in some of the worst experiences of their lives. Within my journey as a healthcare chaplain, and because of my background in community and global health, I have really found a unique space to bring substantive care through humanitarian medical supply chain for people in need.
How long have you been a member of ACHE?
Just a couple of years.
Why did you join ACHE?
To enhance networking with leaders in health care.
Tell us one thing that people don’t know about you.
A couple of years ago, I was invited to give a TED Talk for TEDx Deep Ellum to speak specifically about my work in humanitarian logistics. That talk can be found on YouTube, “Humanitarian Logistics: Advancing Care for People and Planet.”


Emily Sander, MHA
I recently earned my master of health administration (MHA) from the University of North Texas Health Science Center(UNTHSC) in Fort Worth. Prior to my graduate studies, I received a bachelor of arts in Biology with a minor in Neuroscience from Centenary College of Louisiana in Shreveport. Within the MHA program at UNTHSC, I interned with the Cook Children’s Physician Network, where I analyzed no-show data within the Neighborhood Health Centers, revealing my passion for improving access to quality healthcare through community involvement. In July, I will begin an administrative fellowship at UT Southwestern and am looking forward to starting my career at an institution that values the expansions of care innovation to all patients.
What inspired you to pursue a career in healthcare leadership or administration? Originally from Omaha, NE, my time in Shreveport opened my eyes to the unequal distribution of healthcare in our country. While working as an administrative assistant at a rheumatology clinic that primarily served Medicare and Medicaid patients, I witnessed firsthand the social barriers many faced just to get to their scheduled appointments. Many patients in Shreveport do not receive preventative care due to these barriers, contributing to a very unhealthy community. Recognizing that these challenges exist in communities nationwide ignited my passion for expanding access to equitable healthcare. I knew a career in healthcare administration would empower me to help drive that change.
What has been the most impactful experience or lesson during your graduate studies so far?
The primary reason I chose UNTHSC was due to the MHA program’s placement in the College of Public Health. Every course, from finance to leadership, addressed how the different social determinants of health play a role in care delivery. The program at UNTHSC allowed me to continuously look at healthcare delivery through the lens of community health, keeping me rooted in my personal goals as an administrator.
How long have you been involved with ACHE, and what prompted your involvement?
I joined ACHE as a student member in my first semester at UNTHSC in fall 2023, encouraged by my professors to get involved early in my graduate studies. Nearly two years later, I’m incredibly grateful for the connections and opportunities ACHE has provided. From attending my first Women’s Leadership Conference at Texas Woman’s University to participating in the student case competition and experiencing my first Congress, ACHE has introduced me to a network of inspiring mentors and peers. I look forward to continuing my involvement and giving back to this incredible organization as I grow in my professional journey.
How do you recommend students maximize their ACHE student memberships?
The best advice I can give to students new to ACHE is to simply show up. Recruit a fellow student from your university or go independently and attend an event in the next few months that really interests you. Once you go to your first conference or summit, you will witness the value that ACHE provides to healthcare leaders and want to continue to attend every other event in your area!
What are your career goals following graduation?
I am beyond excited to start my fellowship at UT Southwestern and anxious for the knowledge I will gain over the next 18 months. I am looking forward to my departmental rotations and determining my niche within healthcare administration. My goal is to remain grounded in my inspiration for pursuing this career while continuing to grow my technical and leadership skills. I will strive to always place patient access and equitable care as my priority, and I hope to continue to obtain roles that allow me to impact the community I serve.
Tell us one interesting fact about yourself that your peers might not know:
I am an avid baseball fan! Growing up in Omaha, I attended the College World Series every year and have never let that tradition die. Any major league baseball, college, or high school game, you can count me in!




To submit your update, milestone, award or accomplishment, CLICK HERE.
CRISTAL RETANA LULE was promoted to Vice President, Community Relations at Children’s Health. She will also receive the Young Leader Award at the Texas Woman’s Foundation Annual Leadership Forum on May 8th.
PRIYA PATEL, PharmD, MBA co-founded OverbookMD, which aims to provide patients access to vetted medical and surgical specialists within 48 hours.
IDARA ATAKPO graduated in May with a Master’s in Healthcare Administration.
FRANKLIN FRU received his Doctorate in Healthcare Administration.
DR. RACHAEL HILL completed her post-doctoral studies and received a Master of Science in Data Science from the Texas Tech Rawls College of Business.
CARDELL VELEZ was promoted to Associate Vice President, Health System Operations and Imaging Services at UT Southwestern Medical Center.

A workplace you can have faith in.
At CHRISTUS Health, we unite under a shared mission: to extend the healing ministry of Jesus Christ.
Our organizational roots are strong, dating back more than 150 years. We continue to expand into new communities each year, adding more physicians and more services and bringing care closer to more people. Join a purpose-driven team where you can grow, inspire and lead.

By Bert Witherspoon, FACHE and Holly Hrabik, MHA, MBA
The 2025 ACHE Congress on Healthcare Leadership was a masterclass in connection, education, and inspiration. With more than 7,000 healthcare leaders in attendance, the event delivered an experience that far surpassed the expectations of a traditional conference.
This year marked the first time Congress was held in Houston, Texas—a notable shift from its long-standing home in Chicago. Amid the

warm Texas spring, returning attendees shared their appreciation for the region’s mild weather, joking that even the Houston humidity was a welcome tradeoff from the frigid Chicago winters of past Congresses. The venue itself, housed within a single, continuous convention complex, drew praise for its logistical convenience, allowing participants to move easily between sessions, networking events, and social gatherings.
The new location also offered a regional advantage—particularly for the North Texas Chapter of ACHE, which showed an exceptional level of commitment and engagement. According to registration data, nearly 300 members from the chapter were in attendance, a remarkable show of representation likely bolstered by the proximity of Houston to DFW. This strong presence created opportunities for deeper chapter engagement, leadership visibility, and collaborative representation on the national stage. It was announced that Congress will return to Houston for a second consecutive year in 2026, then shift to Nashville in 2027, and return to Houston in 2028, solidifying the city’s place in the Congress rotation for years to come.


What set this Congress apart was the balance of thought leadership and meaningful relationship-building. Across four days of intensive programming, attendees participated in sessions that addressed real-time issues in the healthcare industry—ranging from artificial intelligence and operational innovation to workforce resilience and equity in care. Each session offered practical takeaways and emerging best practices from across the country’s most respected health systems. Notably, members of the North Texas Chapter of ACHE served as panelists, moderators, and speakers throughout the week, showcasing their expertise on the national stage. Their active participation reflected the strength and depth of our local chapter—a community rich in both talent and character, whose leaders continue to shape the broader conversation on healthcare improvement.
Several powerful themes emerged that speak to the deeper motivations and strategies of healthcare leadership today:
“You can’t win healthcare. Our purpose is in the agency of serving other people.”
This quote perfectly encapsulates the spirit of ACHE Congress—reminding us that leadership
is not about being the biggest or the first, but about showing up better for others. Several keynote speakers echoed this theme, reinforcing that success in healthcare isn’t measured solely in margins or market share, but in the quality of service, the compassion of care, and the integrity of systems.
“Bigger is not better—better is better.”
This was evident in the sessions focused on value-based enterprises vs clinically integrated networks and the evolving potential to partner with independent physicians in more innovative, less restrictive ways. The message was clear: better alignment, better care, better access— without always needing to consolidate or acquire.
The Congress made it clear that post-acute care—rehab, skilled nursing, long-term care—is no longer peripheral. These spaces are critical to strategic transformation. Health systems must now decide how to partner, buy, or divest with intentionality, recognizing these sites as essential to both outcomes and experience across the continuum.
The concept of a “coalition of the willing” came up in several conversations—an encouraging

move toward shared services and collaborative models between health systems, hospitals, and independent partners that prioritize community health over competition.
A major thread woven through many sessions—and echoed in informal discussions—was the internal side of leadership. How we care for our teams and ourselves. “When was the last time you bumped your knee? No idea. When was the last time you were embarrassed in a meeting? Easy recall from years ago.” Social pain is still a form of pain.”
Leaders must recognize that fear, shame, and psychological safety are not soft topics— they’re structural. When team members bring their social problems to us, they’re often communicating a deeper kind of hurt, and our ability to respond with empathy directly impacts culture and outcomes.
Similarly, many speakers emphasized mindfulness as a personal leadership practice, not as a trend, but as a tool. Finding what works for you—and doing it consistently—is key to long-term sustainability in leadership roles.
The concept of “yet” emerged as a powerful reframe tool for performance and development conversations: “You haven’t hit that key performance indicator yet. You’re not in that role yet.”It signals potential and possibility, aligning perfectly with a growth mindset that encourages resilience rather than resignation.
This ties into one of the most empowering frameworks shared at Congress:
“There are things that matter. There are things you can control. The intersection is what you focus on.” It’s a simple yet profound guide to prioritizing not just our work, but how we show up—with intention, focus, and compassion.
“May your choices reflect your hopes, not your fears.” — Nelson Mandela
It’s this spirit that makes the ACHE Congress not just a leadership development event, but a reawakening of purpose. In rooms filled with peers, ideas, and collective will, we are reminded that our true power lies not in title or tenure, but in agency, humility, and hope.
However, the value of the Congress extended well beyond the content. The environment fostered unparalleled opportunities to engage with new connections and deepen relationships with existing colleagues. The pace and design of the event allowed for organic conversations—conversations not rushed by the typical time constraints of other


industry events. Whether over coffee between sessions, in dedicated networking lounges, or during the evening receptions, participants found space to exchange ideas, share challenges, and form new alliances that will carry far beyond the walls of the conference.
A notable highlight was the Chapter Leaders Reception, where chapter leaders from across the nation convened to share insights and innovations from their local ACHE chapters. This gathering was rich with discussion on best practices, successful outreach campaigns, and strategies for engaging and growing membership. The reception provided a dynamic forum to collaborate, inspire one another, and reinforce the shared mission of advancing leadership excellence through collective effort.
The Congress also offered a powerful reminder of the shared mission within healthcare leadership. Keynote speakers delivered messages that challenged and inspired, while the Convocation Ceremony honored those who achieved Fellowship in the American College of Healthcare Executives—a moving celebration of excellence and lifelong commitment to the field.
The ACHE Congress stands as a rallying point for the profession—a place where leaders don’t just learn, but reconnect with the purpose behind their work. For those in healthcare leadership, attending this Congress is not merely beneficial—it is essential. The sense of community, momentum, and possibility it cultivates is unlike anything found elsewhere.
For anyone on the fence about attending a future Congress, know this: it is not just a professional investment—it is a deeply personal one. It is where careers are inspired, collaborations are born, and the shared calling to improve healthcare is reignited. And for those who may face financial barriers, there are scholarship opportunities available through the ACHENTX Foundation to help make this transformative experience accessible. Don’t miss the chance to stand shoulder-to-shoulder with thousands of peers who believe, as you do, that healthcare can and must be better—and to stand on the shoulders of giants who have come before us, paving the way with their vision, courage, and commitment. Let Congress be the place where you honor their legacy and take your next bold step forward with purpose and conviction.
By Susan Merritt
Students from across the United States gathered in Houston, Texas, from March 23 to March 27, 2025, to attend this year’s American College of Healthcare Executives (ACHE) Congress. This premier event provided future healthcare leaders with opportunities to network, learn from seasoned professionals, and contribute through volunteer service.
Students enrolled in an undergraduate or graduate health administration program had the opportunity to earn a complimentary ticket to attend Congress by volunteering as a Program Assistant (PA). Responsibilities included supporting ACHE staff, speakers, faculty, and attendees; assisting with seminars, receptions, and luncheons; and verifying name badges. In addition to their duties, PAs built strong bonds with fellow students and engaged in valuable mentorship experiences, creating connections that will support them well beyond Congress. For this conference, ACHE hosted 397 PAs.
Networking remained a cornerstone of the student experience. Throughout the event,

students engaged with peers and senior healthcare executives to discuss career paths, leadership development, and industry insights. These relationships are instrumental in helping students navigate their healthcare journeys and build a lasting professional network after graduation. During Congress, ACHE hosted a Student Associate Networking Reception, allowing students to connect with their peers.
ACHE hosted an Administrative Fellowship Fair for students featuring representatives from over 80 healthcare organizations. This fair offered a unique chance for students to explore fellowship opportunities, ask questions, hand out resumes, and make a meaningful first impression with potential employers.
TEXAS HEALTH SCIENCE CENTER AT FORT WORTH (UNTHSC)
UNTHSC proudly represented the ACHE of North Texas chapter with a strong student presence. Led by Barton Gill, Chair for the Department of Health Administration and Health Policy, students from this cohort took
advantage of attending Congress and making valuable connections with other seasoned healthcare executives. Students from this MHA cohort included: Philip Hamilton, Rosa Lozano, Darshan Amin, Alyssa Manzano, Emily Sander, Apinya Sangarunsilp, Ethan Livingston, Michael Hilton, and Sonia Pathirajamudali. Having a strong support system is crucial for any student or early careerist. Participating in events like Congress enhances educational experiences and enables students to gain insights from real-world situations.


















By Holly Hrabik, MHA, MBA
Every year, ACHE Congress provides a critical stage for healthcare professionals to connect, learn, and lead with purpose. In 2025, thanks to the generosity of the American College of Healthcare Executives of North Texas Foundation and ACHE of North Texas Platinum Sponsors, a new cohort of emerging leaders attended Congress in Houston through the support of ACHE Congress Scholarships. For these recipients, the experience was more than an educational opportunity—it was a turning point in their personal and professional journeys.

For Jacqueline Wagner, MHA, LSSBB, Director of Operational Design & Deployment at Texas Health Resources, the scholarship was a gateway to deeper learning and authentic leadership connections.
“ACHE Congress offered a wealth of information and insights that can significantly enhance my understanding of current trends and best practices in healthcare management,” Wagner shared. “The networking was incredibly valuable—to hear how others are addressing challenges and driving improvements inspired me deeply.”
Her favorite sessions included Brené Brown’s “Dare to Lead” and the hot-topic panel on Future Tech Trends and AI. “The message was clear— change is hard, but necessary. AI is here to give us time back, so we can focus on strengthening human connections.”

As an occupational therapist, Liliana Chavez brought a unique lens to Congress. She described the scholarship as an “opportunity to grow, connect, and leave inspired.”
“One of the most valuable takeaways was the emphasis on purpose-driven leadership, visibility, and the clinician-to-executive transition,” Chavez reflected. “I left especially inspired by the Women in Leadership and Innovation in Healthcare panel.”
Her experience underscores the importance of creating spaces that elevate diverse leadership perspectives and support career evolution across all clinical roles.

For Justin John, a healthcare operations leader, Congress sparked renewed purpose.
“Receiving this scholarship gave me an opportunity to immerse myself in transformative discussions that shape the present and future of healthcare,” he said. “Sessions on executive presence and organizational financial stability were especially impactful.”
John emphasized the vibrant atmosphere and the value of reconnecting with peers: “Engaging with dynamic leaders and mentors made the experience truly enriching.”
Amanda James, FACHE journeyed to Congress after significant personal and professional transitions.
“When I learned Congress was in Houston, I was thrilled. But by fall, my position had been eliminated,” she explained. “The scholarship made it possible for me to attend despite these circumstances. It was profoundly meaningful.”
Now with a new role in a value-based care organization, James found great value in Ginny Clarke’s presentation on authenticity and practical strategies from the session on investing in palliative care. “The genuine interest from speakers in continuing conversations left a lasting impression on me.”
For Nancy McDonald, FACHE, the scholarship affirmed her passion for healthcare leadership.
“It allowed me to attend Congress for the first time—it was so energizing,” she said. “I will never forget walking across the stage at Convocation with peers and mentors who make a real difference.”
McDonald was moved by Brené Brown’s keynote, which challenged outdated leadership models and uplifted courage, vulnerability, and emotional intelligence.
“The networking events sharpened my elevator pitch and interpersonal skills while also leading to authentic mentorship opportunities,” she added.
The stories shared by these scholars illuminate the ripple effects of professional investment— how a single opportunity can spark confidence, promote innovation, and build community. As these leaders return to their organizations, they carry with them not only new ideas and tools but also a renewed sense of mission.
Thanks to the unwavering support of ACHE of North Texas Platinum Sponsors below and the ACHE of NTX Foundation, the future of healthcare leadership looks brighter, bolder, and more connected than ever.
By Amanda Brummitt, FACHE
By any standard, Access TeleCare is a remarkable success story. But for Dr. Chris Gallagher— cardiologist, CEO, and proud Texan—it’s always been about more than just scaling a company. It’s about planting something meaningful in Texas soil and watching it grow into a national force for good in healthcare.
What started in Sulphur Springs, a small Texas community with big healthcare needs, has grown into a nationwide leader in inpatient telemedicine, with over 477 telemedicine programs implemented in Texas alone and 2,600+ nationwide. And yet, despite this impressive growth, Dr. Gallagher and his team have never lost sight of the mission: reduce unnecessary transfers, keep patients in their communities, and help hospitals generate more revenue by doing what they do best—care for their people.
Access TeleCare’s story begins in 2011. You may recall it from an article in the Spring 2024 magazine where Dr. Pritam Ghosh challenged us all to innovate fearlessly. Drs. Gallagher and Gosh began exploring how virtual care might improve access in under-resourced hospitals. A year later, the team began to expand services across Texas. By 2013, their telemedicine model was gaining traction, and on October 1 of that year, they saw their first virtual patient.
On the very first night, Dr. Ghosh managed a critically ill patient who would have otherwise been airlifted to a larger hospital. By morning, the ICU nurses, chief nursing officer, and hospital CEO were calling it a game-changer. That moment solidified what they had long believed: virtual care wasn’t just viable—it was transformational.
From the beginning, they knew success wasn’t just about having the right technology—it was about having the right people and the right program design. Access TeleCare built their care teams using small, tightly-knit pods of physicians, ensuring that partner hospitals work with a familiar and consistent group of clinicians. This “smallest effective pod” approach allows for continuity of care and stronger relationships, especially important in high-stakes specialties like critical care and neurology.
Today, Access TeleCare boasts a growing array of specialties, including acute behavioral health, nephrology, maternal-fetal medicine, neurology, infectious disease, pulmonary and critical care, cardiology, and hospitalist medicine—selected not just for scalability, but because they represent real gaps in care at hospitals across the country.
While Access TeleCare has deep roots in rural Texas, the company’s model now extends well beyond small-town hospitals. In fact, 65% of their programs today serve urban facilities, where they augment specific specialty gaps, like acute neurology or weekend ICU coverage.
“In rural hospitals, we are the solution,” Dr. Gallagher explains. “In urban settings, we’re usually part of the solution.”
In both cases, Access TeleCare designs programs around the hospital’s unique needs. Whether covering nights and weekends to support medical staff burnout or providing emergent teleneurology consults, the focus is always on filling gaps and strengthening the care continuum.
Virtual care is no longer an add-on—it’s becoming woven into the fabric of hospital operations.
Dr. Gallagher is quick to point out that technology is not the starting point—it’s the enabler. “This business starts with people,” he says. “You need the right people in the right roles at the right time.”
That said, technology still matters—especially when lives are on the line. Access TeleCare has invested in a proprietary system called Telemed IQ, which integrates seamlessly with hospital EMRs and automates consult routing across platforms. Their telehealth platform and carts boast 99.998% uptime, with multiple layers of redundancy to minimize downtime and delays in care.
In 10 months, the company successfully launched 300 new programs, made possible by aligning people, processes, and metrics. From hardware selection to clinician onboarding, every detail is mapped to ensure that patients and providers experience a reliable, consistent virtual encounter.

One of the clearest benefits of inpatient telehealth is its ability to reduce unnecessary transfers. Transferring patients—especially by air—adds cost, delays treatment, duplicates testing, and separates patients from their families.
“Patients want to be treated in their own communities,” says Dr. Gallagher. “We help hospitals make that happen.”
By embedding specialty care into local hospitals, Access TeleCare helps them manage more complex cases in-house, preserving revenue, improving outcomes, and reinforcing their role as the centerpiece of the community’s health ecosystem.
With growth comes risk, chief among them, mission drift. But Access TeleCare has remained steadfast in its values, thanks to what Dr. Gallagher calls “relentless re-centering.”
Every month, the company holds a town hall featuring a real patient story to anchor the team in their purpose. That clarity informs hiring decisions, service expansion, and even which partnerships they pursue. “We say no a lot more than we say yes,” he says. “And we’re better for it.”
Dr. Gallagher also credits his leadership development journey with helping them scale without losing sight of the mission. “I’ve had great mentors—both physician and non-physician execs—who’ve helped me stay grounded,” he reflects.
Being a virtual physician is not for everyone. It takes a unique blend of technical fluency and human empathy to build trust through a screen.
Access TeleCare trains every new provider in “Breaking through the Screen,” a specialized onboarding program that teaches virtual bedside manner, professionalism, and engagement techniques. Lighting, camera angle, and microphone quality—it all matters. So does the tone, language, and presence of the clinician.
“Our best physicians are the ones who know how to connect quickly and confidently,” Dr. Gallagher says. “It’s something we actively cultivate.”
Scaling a healthcare organization takes vision, but also financial and operational discipline.
“My advice? Be prepared to take longer and go slower than you think,” Dr. Gallagher advises. “And never lose focus on the clients and patients you already have.”
That philosophy has helped the company grow strategically, building long-term, sustainable partnerships rather than chasing quick wins.
As virtual care matures, the future will be shaped not just by telehealth but by the integration of AI, automation, and innovative care models. From virtual scribes to AI-powered triage and consult routing, the goal is always the same: improve efficiency and enhance access.
“Tech gets the attention, but the real innovation is in the care models,” Dr. Gallagher says. “We’re redesigning how care is delivered.”
The demand for care continues to outpace
the supply of clinicians. In this reality, access is everything. And that’s exactly what Access TeleCare provides—not just better care, but more access to care, delivered where and when it’s needed most.
Drs. Gallagher and Ghosh planted Access TeleCare in Texas soil with a clear vision: keep patients in their communities, support hospitals, and bridge critical care gaps with excellence and compassion. That vision has taken root, growing far beyond Sulphur Springs—but always with Texas at its heart.
As the healthcare landscape continues to evolve, Access TeleCare stands as proof that the right mix of mission, model, and mindset can scale care without compromising quality.
For hospitals navigating their own transformation, the lesson is clear: start with purpose, invest in people, and never lose sight of the patient.

In a world where healthcare is evolving faster than ever, it takes a grounded, visionary leader to navigate the complexities of culture, innovation, and strategy, without losing sight of the people at the center. Ryan Gebhart, FACHE, president at Baylor Scott & White Medical Center – Frisco at PGA Parkway, is that kind of leader, although he is far too humble to describe himself that way.
Rooted in faith, shaped by sports, and driven by service, Gebhart brings a uniquely human approach to transforming healthcare from the inside out.
Married to his wife Natalie for 13 years and raising three young kids, Ryan’s life is full of family, faith, and fields. “Every night of the week, you’ll find me at a sports field with one of my kids,” he says. “I love to compete. Playing baseball taught me about teamwork, perseverance, persistence, and glorifying God with what you’ve been given.”
By Amanda Brummitt, FACHE
That deep sense of purpose weaves through every part of Gebhart’s personal and professional story. “My calling is to glorify God by loving and serving others, whether it’s with my family or through healthcare leadership. That’s what guides me every day.”
As the son of a healthcare administrator, Gebhart had been immersed in the industry early on—tagging along to community events, volunteering in hospitals, and watching leadership up close.
“Healthcare grabbed me from a young age. If it wasn’t going to be Major League Baseball, it was going to be healthcare leadership.”
Gebhart’s career started, as a hospital concierge. “It’s funny,” he says, “My wife and I were newly married, broke, she was working two jobs, and I was working one job and pursuing my MBA. Knowing I was going into healthcare, I applied for
a second job as a hospital concierge. I thought it would be a great way to learn from the ground up—and it was.”
The lessons he learned there still shape how he leads. “That role taught me to own your area. Take pride in your job. Watch, observe, and listen to the customer. It was like being on the bench in baseball—paying close attention, soaking in what works and what doesn’t.”
Service isn’t just a part of Ryan’s work—it’s a family value. “Growing up, volunteering was just what we did—delivering meals at Thanksgiving, adopting families for the holidays, serving at the hospital.”
That spirit of giving has continued through his career and into parenthood. “During the pandemic, my family delivered food to people’s homes through Meals on Wheels. Some of the elderly folks just wanted to visit with our kids. That was powerful. It may not have been as efficient as a quick drop off, but the fellowship impacted us all.”
While opening a new medical center limits his time more now, Gebhart is intentional about the causes he supports. “As responsibilities grow, it becomes more important to focus. First, help your organization achieve its mission. Then, when there’s overlap with your personal and family passion, do it with your family. It’s about saying fewer yeses but making them count.”
When asked about transformational leadership, Gebhart said he leans into what he calls “dual transformation” in healthcare leadership. “You have to lead today’s healthcare—traditional, inhospital care and outpatient care—and also think boldly about tomorrow’s version: digital health,
new experiences, and delivery models that meet patients where they are.”
Leaders, he says, must remain agile and curious. “You can’t just sit back and let the industry change you. You must help shape that change. And at the core of that, it’s about having a heart for people.”
That people-first philosophy is baked into the cultural DNA Gebhart is building at the new Baylor Scott & White Health Medical Center in North Frisco. “We’ve been very intentional about defining what our culture will be and how it aligns with our system’s core values. We created behavioral anchors, built them into interviews, and now we’re embedding culture into everything we do—from management meetings to onboarding.”
Culture, he says, is a living organism. “You have to care for it. If you do, it will drive performance. A healthy culture leads to great patient care, strong outcomes, and a thriving business.”
When it comes to innovation, Gebhart believes it should always begin with the patient. “Too often, healthcare is built around the payment system. At Baylor Scott & White, we’re flipping that at a system level. We’re listening to the customer— where are the pain points? How do we fix them?”
That approach led to groundbreaking tools like the “Help Me Decide” feature on the MyBSWHealth digital platform. “Patients can describe symptoms in their own words and get triaged to the right level of care.
From thousands of interactions within MyBSWHealth, we see 70% of people who use the Help Me Decide tool are routed to more appropriate, often lower-cost care. That’s the kind of innovation that transforms healthcare.” Patient experience comes first. “If you earn trust and loyalty by creating exceptional experiences, the business outcomes will follow.”
“Talent is hard to find—and even harder to keep,” Gebhart says. His secret? Wellness and relationships.
“Our vision is empowering you to live well. We’re applying that to our team members, too. Our new hospital is designed as a wellness-forward campus—outdoor spaces, natural light, and healthy food. We’re pursuing WELL Certification not for the label, but for the framework it provides.”
Wellness also means fostering human connection. “Our leaders check in with team members regularly—not just about performance, but about how they’re doing as people. Are they okay? What do they need?”
That level of intentionality builds resilience, loyalty, and trust. “When your team knows you care about them as humans, they show up differently—for each other and for patients.”
In a high-pressure, fast-paced field like healthcare, Gebhart believes one of the most vital skills leaders can develop is learning to slow down.
“In baseball, as a hitter, you’re trained to slow the game down. As a hitter, you’ve got a split second to decide whether to swing. But to make the right decision, you’ve got to slow down enough to see the laces on the ball. That takes presence. That takes focus.”
It’s the same in leadership. “There’s so much coming at us every day. But if you’re moving too fast, you’ll miss what’s most important. Be quick to listen and slow to speak. Practice presence and purpose.”
He encourages leaders to evaluate themselves regularly—who they are, how they lead, and where they can improve. “Healthcare is a sacred calling. Our teams and our communities are counting on us.”
Be Bold. Be Different. Make an Impact.
Gebhart’s final word to aspiring and current leaders is simple: “It’s okay to be different.”
In a field as complex as healthcare, it’s easy to get swept up in metrics, operations, and noise. But for Gebhart, it always comes back to people and purpose. “People crave relationships. They want to feel seen, heard, and cared for. As leaders, our job is to create environments where that’s possible.”
And he encourages leaders to be bold in their faith and their values. “Get yourself going every day. Don’t waste a minute. Be intentional with your time. And don’t be afraid to serve others with everything you’ve got.”
It’s a lesson straight from the baseball field— and one that carries just as much power in healthcare.

You want a partner who really understands the local needs of your hospital, and who puts patients and community first. A partner who listens to your unique challenges and comes to the table with solutions. That’s Sound. Our physician-founded and physician-led medical group is all about doing and being better — for our partners, our clinicians, and our patients.
A better partnership in hospital medicine, and in all our specialties.
Mihir Patel, MD, MBA, CPE CEO, Hospital Medicine

In our continuing series of profiles of ACHE North Texas Life Fellows and Retired members, we are pleased to shine the spotlight on Michael (Mike) C. Waters, LFACHE. He is best known for his 24-year tenure as President and Chief Executive Officer of Hendrick Medical Center in Abilene, TX. For more than two decades, he guided the organization through an extraordinary period of growth, adding numerous facilities and services to meet the increasing healthcare needs of his growing community. Notable service enhancements included expanded obstetrics, open heart surgery, expanded pediatric services, geriatric, and rehabilitation, as well as expanded oncology services. He also was instrumental in expanding a family practice residency program in collaboration with Texas Tech University Health Sciences Center. At his retirement in 2004, the hospital’s Board of Trustees voted to name the trauma center in his honor.
Mike came to Hendrick from Baptist Memorial Hospital in Kansas City, MO, where he was Executive Director. He also served nine years
with the Memorial Hermann Hospital System in Houston, TX, and he was a Commissioned Officer in the U.S. Public Health Service with the Indian Health Program in New Mexico and Oklahoma.
He began undergraduate work at Baylor University in Waco, TX, received a Bachelor of Science degree in Sociology from Lamar University in Beaumont, TX, and a Master of Science in Hospital Administration degree from the University of Pittsburgh’s School of Public Health.
After graduating from high school, Mike’s first job was in the business office of the Baptist Hospital of Beaumont, TX, as part of a summer work program. “I arrived at work at 8 a.m. and by 10 a.m. I knew I wanted to be a hospital administrator,” he recalls. “I had no doubt.” Throughout his career he has brought his experience and leadership insights to boards including ACHE where he was chairman of the Board of Governors from 2000 to 2001, Texas Hospital Association where he served as chairman from June 1989 to May 1990, Kansas
City Area Hospital Association, American Hospital Association, and the American Protestant Hospital Association. He continues to serve as a board member for the Eunice Chambliss Hospital House and Hardin Simmons University, both in Abilene, TX.
His many awards and accolades include the Lifetime Service Award from ACHE, the Distinguished Service Award from the American Hospital Association, the Earl M. Collier Award of Distinguished Hospital Administration from the Texas Hospital Association, and the Distinguished Alumnus Award from the Graduate School of Public Health at the University of Pittsburgh.
His dedication to the well-being of others continues today as a 15-year volunteer at Baylor University Medical Center in Dallas. He also serves as a mentor for ACHENTX. Outside of healthcare, Mike enjoys hunting, fishing, and studying the Civil War. He and his wife also enjoy spending time with their four grandchildren.
What are the biggest changes you’ve seen over your career in healthcare?
Mike: The evolution of information technology, the introduction of the hospitalist into the care team, and the hospital ownership of physician practices. Of course, artificial intelligence must also now be added to the list.
What’s the best advice you received from a colleague, mentor, or friend that has helped you in your career endeavors?
Mike: Never stop learning, and use your ears 10 times as much as your mouth.
When did you join ACHE ?
Mike: I joined ACHE in 1966 as a student affiliate.
Why have you remained a member of ACHE? What value do you receive from your ACHE membership at this point in your career?
Mike: I have remained a member of ACHE for the continuing education and the relationships with colleagues.
If you were speaking to a new MHA graduate or a young healthcare professional just starting his or her career, what one piece of advice would you give him or her?
Mike: My strong advice would be for them to become bilingual in Spanish. They will become a hero to many of their employees, and they will also be able to communicate effectively with many patients. Trust with both groups will be greatly enhanced.
What would you tell him or her about the value of ACHE membership?
Mike: ACHE membership will be priceless to you for your career. Affiliate now and stay with the College, and you will never regret it. When I was Chairman of the College in 2000, I spoke all over the U.S. and Canada. I would brag that there were 24,000 affiliates. Today, there are twice as many, and they are all your colleagues.

By Michael Belkin
For Jen
Rodosta Barrera, Executive Vice President
of
Strategic Initiatives
at Children’s Health in Dallas, leading one of the most ambitious pediatric healthcare projects in the country is more than a professional milestone, it’s a mission rooted in empathy, foresight, and transformation.
What began as a career in communications and grant writing has evolved into a two-decade journey through community health and health care systems, culminating in a leadership role that places her at the intersection of strategic growth and meaningful care delivery. “I didn’t set out to work in health care,” Jen reflects. “But once I saw the impact of purpose-driven work in community health, there was no turning back.”
Jen’s passion for healthcare took root at a federally qualified health center where she encountered firsthand the challenges and rewards of serving underserved populations. That experience led to nearly 10 years at Ascension Texas, where she honed her expertise in strategic planning, capital investment, and health system transformation.
Now, she brings that expertise to Children’s Health, where she spearheads the planning and development of a state-of-the-art pediatric hospital in partnership with UT Southwestern Medical Center. Scheduled to open in 2031, the hospital will serve a rapidly growing pediatric population, linking directly to UT Southwestern’s campus through a symbolic and literal bridge that unites clinical care with academic advancement.
“Pediatric care isn’t care for small adults,” Jen explains. “It demands a different level of sensitivity, design, and specialization.”
From wider hallways to accommodate families and equipment, to developmental considerations that influence aesthetics and functionality, every detail of the new hospital is centered around the specific needs of children and their caregivers.
With the Dallas-Fort Worth pediatric population projected to double by 2050, the new Dallas pediatric campus includes space to add more beds or other clinical services built into the design to support future expansion.
Children’s Health has already demonstrated what scalable, thoughtful expansion can look like through the recent completion of its Plano campus expansion. In December 2024, Children’s Medical Center Plano opened a new eight-story, 395,000-square-foot tower that nearly tripled the hospital’s bed count and significantly expanded its emergency and specialty care capabilities.
Jen and her team leveraged best practices from the Plano design into the new Dallas pediatric campus to incorporate the values of comfort, innovation, and family-centered care. Both facilities were designed with healing and humanity in mind, from larger patient rooms that can accommodate two caregivers, circadian lighting, and nature views to interactive features shaped by direct family and team member feedback. “Over 1,000 people participated in our design process, from physicians and nurses, to operations team members, teens, children, and their families. Their feedback and engagement was paramount to creating a building that is not only beautiful, but functional.” A Scalable Blueprint for the Industry

While these projects are deeply rooted in North Texas, their implications extend nationally.
The Children’s Health and UT Southwestern partnership offers a potential blueprint for other health systems tackling workforce shortages, access barriers, and rising pediatric complexity.
“We’re building for the future, not just today,” says Jen. “And we’re doing it in a way that balances innovation, community relevance, and financial sustainability.”
In this sense, her work is not only strategic but scalable, offering replicable models for hospitals across the country seeking to modernize pediatric care while remaining anchored in local needs.
In an era of constant change, Jen’s leadership is marked by adaptability, inclusion, and a steady focus on purpose. Over the next few years, beyond campus construction, Jen is focused on people. This includes partnering with operations and clinical teams to develop new processes, coordinating patient relocations and service transitions, and recruiting and training next-generation talent in partnership with UT Southwestern to ensure continued leadership in pediatric care.
Her leadership approach reflects a blend of operational rigor and emotional intelligence.
“Strategic planning is only successful if people feel supported and seen throughout the process,” she says. “Empathy and adaptability are not soft skills—they’re success factors.”
For early-career professionals seeking to rise in healthcare, Jen offers clear guidance: “Find the mission that moves you. When your work aligns with purpose, it becomes more than a job—it becomes your impact.”
As Children’s Health prepares for its next chapter with the new Dallas pediatric campus, Jen Barrera stands as a model of thoughtful, mission-driven leadership. Her work highlights the power of aligning purpose with performance—and shaping a future where every child in North Texas has access to care designed with them in mind.
In healthcare, vision without execution is just aspiration. Jen Rodosta Barrera brings both— with empathy, discipline, and a belief that pediatric healthcare can be transformed not only by innovation, but by leadership that starts and ends with the patient.

JANUARY 28, 2025
By Kean Villarta
On January 28th, ACHE of North Texas held its first Breakfast with the President event of the year, featuring Eulanie Lashley, President of Texas Health Hospital Mansfield. After a hearty breakfast, the hosts held a fireside chat with Eulanie, moderated by Vice President,Chief Operating Officer Carine Moura.
Eulanie shared her humble beginnings growing up in Antigua and going to university in the US. She credits her successes to God and having a foundation in humility and Christ-centered principles. She is a leader who is passionate about lifting up the employees they serve, and she reminded everyone to “never give up” in their professional journeys.
Eulanie shared her leadership vision as well, including growth strategies for hospital expansion, innovation, and patient-centered care, and lessons from her previous roles at AdventHealth, where she worked for 15 years. After the fireside chat, attendees also received a tour of the hospital’s upcoming expansion.



US Acute Care Solutions (USACS) is the nation’s leading physician-owned provider of hospital-based emergency and inpatient medicine. Our national reach and scale allow us to focus on being the best acute care practice in the country.
Patient-centered care is at the forefront of everything we do. Our mission is simple: to care for patients. It’s where USACS began, and it’s where we begin each day. By living our core values, Servant’s Heart and Owner’s Mind, we’ve helped dozens of hospitals and health systems improve their quality and service.

6,000+
2,400,000 VISITS at 68 hospitals 772 PHYSICIANS 351 APP s
USACS staffs 68 hospitals in Texas, where we serve more than 2,400,000 patients each year through our emergency, hospital, critical care, and observation medicine services. We partner with several renowned health systems, including Ascension Seton, Baylor Scott & White, CommonSpirit, Emerus, Houston Methodist, Tenet, and Texas Health, to provide exceptional, high-quality, patient-centered care to communities across Texas every single day. We host an emergency medicine residency program and several fellowships at Dell Seton Medical Center at The University of Texas and staff two pediatric emergency departments, providing an array of clinical settings for our clinicians.






By Melinda Schmidt, MBA, BSN, RN
Moderator
Dr. Jim Allard, DNP, RN, NEA-BC, FACHE, VP & Chief Nursing Officer, HCA Healthcare
Dr. Charlene Kesee, DBA, FACHE, FACMPE, Clinical Department Administrator, UT Southwestern
Diana Mendoza, MPAS, PA-C, Director, APPs
Pediatric Specialties, UT Southwestern
Dr. Karen Holmes, PA, Orthopedic Surgery, Baylor Scott & White
On February 27, 2025, ACHE of North Texas hosted an engaging and well-attended educational session titled “Utilization of PA/ NP Workforce in the Current Healthcare Environment.” With more than 75 healthcare leaders and professionals in attendance, the session provided a robust dialogue around the evolving role of Advanced Practice Providers (APPs) in today’s complex care delivery landscape.
Each panelist shared the structure of their respective organization’s PA/NP model, revealing a variety of approaches tailored to practice groups, hospital service lines, and even pediatric subspecialties. While organizational models differed, all panelists emphasized the shared goal of maximizing APP contributions to clinical efficiency and patient care outcomes.
Panelists acknowledged that internal culture, not regulatory hurdles, is the most persistent barrier to optimal APP utilization. Dr. Holmes highlighted efforts at Baylor Scott & White to address physician understanding through targeted education. Notably, BS&W has launched a new RN-to-APP pipeline program, demonstrating a commitment to APP career progression and sustainability.
A recurring theme was the importance of intentionality in APP engagement. Dr. Mendoza emphasized working closely with practice partners and leveraging the Office of Advanced Practice Providers to support recruitment and retention. Dr. Kesee emphasized the importance of involving current team members in the recruitment process to offer candidates a comprehensive view of the work environment. At the same time, Dr. Allard pointed to initiatives such as a Friday “comp day” that have directly improved retention.
Empowering APPs with a voice in organizational decision-making was another key point of alignment. Dr. Holmes shared that APPs now hold leadership roles, including positions on the board of governors and medical executive committees. Across the panel, there was consensus that visibility, advocacy, and inclusion are critical to embedding APPs into the organizational fabric.
Measuring impact is central to success. From dashboards to Press Ganey and Qualtrics feedback tools, organizations are leveraging data to inform decision-making, track performance, and pinpoint areas for growth. Dr. Kesee noted the expansion of APP-specific metrics beyond surgical domains to foster inclusion and transparency.
Highlighting the value of APPs in rural and underserved settings, panelists shared inspiring examples. Dr. Mendoza described a cancer urgent care clinic led by advanced practice providers (APPs) that successfully diverts patients from emergency departments, while Dr. Holmes discussed rural clinics effectively managed by APPs with physician oversight.
Panelists also highlighted future-focused initiatives, including APP leader pathways, soft skills retreats, and fellowship programs. Dr. Holmes emphasized the need for creativity in using APPs to impact quality metrics and reduce 30-day readmissions—a goal shared by all institutions represented.

The panel discussion highlighted the crucial role that PAs and NPs play in transforming healthcare delivery. From rural outreach to executive leadership, APPs are being empowered as integral members of the care team. However, cultural evolution, purposeful engagement, and continuous measurement remain essential for unlocking their full potential.
ACHENTX thanks our esteemed panelists and moderator for sharing their valuable insights and for continuing to champion innovation in workforce strategy.





In today’s healthcare environment, different is good. We are a 100% physician-owned partnership, and we’ve been that way since day one.
Ownership creates stability.
Stability creates engaged physicians.
Engaged physicians make better decisions.
Explore the difference at vituity.com/healthcare-services
By Sarah Sentmore, MHA
Krista Stepney, CEO of KD Speaks, LLC
Megan Carter, President & Founder of MC Health Care Consulting LLC
Kimberly King-Webb, Senior Vice President, Chief Human Resources Officer, Christus Health
Therese Gopaul-Robinson, Keynote Speaker & Consultant of Therese Gopaul-Robinson Company
Judy Hoberman, President of Judy Hoberman and AssociatesThe ACHENTX Women’s
The ACHE of North Texas Women’s Conference offered a powerful, transformative experience centered on growth, connection, and bold action. The day began with a warm welcome from the Women’s Healthcare Executives Network (WHEN) Committee Chair, Crystal Brown, who encouraged attendees to “fill your cup today”— setting the tone for a day of empowerment and inspiration.
Throughout the sessions, key themes emerged: authentic leadership, intentional living, and the power of community.
Judy Hoberman reminded attendees that community is the new currency. Her session emphasized that true community — built on trust, vulnerability, and support — can silence
imposter syndrome, boost confidence, and create a sense of belonging. “You don’t have to have a big network,” she shared. “You just need the right network.”
Dr. Megan Carter encouraged women to simplify to create impact. Her message centered on reclaiming time and energy by practicing calendar triage, leveraging the power of subtraction, and using tools like AI to reduce daily stress. Her call to action: prioritize your well-being and lead with values-aligned energy.
Krista Stepney closed the conference with a dynamic keynote on “Bold From Within: Unlock the Power That’s Already Yours.” She introduced the concept of “micro boldness”— small, intentional acts of courage that compound into powerful transformation. By rewiring the brain and practicing courage, women can overcome fear and hesitation, leading to greater impact and innovation. “You already have the power within you,” she declared, urging women to challenge fear and step boldly into their purpose.
The ACHENTX Women’s Conference left attendees feeling inspired, equipped with practical strategies, and reminded that boldness begins with one small, intentional step.






By Audrianne Schneider, FACHE
ACHE of North Texas members assembled more than 200 bags of food and stocked the shelves at Irving Cares, which provides food assistance to those in need. Irving Cares (irvingcares.org) identifies and addresses the needs of the Irving community and partners with clients to develop solutions that lead to self-sufficiency.


By Bert Witherspoon
Held for the first time in a private suite at Globe Life Field during a Texas Rangers game, the 2025 ACHE of North Texas Cocktails with the Chiefs brought together a powerhouse panel to address the ever-rising cost of healthcare employee benefits. Moderated by W. Scott Hurst, FACHE (Patient Physician Network), the panel featured Larry Childress (Lockton), Chris Gay (Evry Health), Angela Ripper (Unum Group), and Dr. Dominic Vu (USI Southwest). Panelists candidly discussed the complex web of responsibility shared by payors, brokers, employers, and employees. Key topics included pharmacy benefit management, self-insurance strategies, and the disruptive cost of gene therapies. The panel also tackled workforce trends like unlimited PTO and the post-COVID shift in generational workplace expectations. With spirited discussion, high-level insights, and sweeping views of the ballgame, the evening blended education, networking, and entertainment, highlighting the urgency and opportunity for innovation in employee health and wellness benefits. APRIL 16, 2025




APRIL 19, 2025
By Melinda Schmidt, MBA, BSN, RN
On a rainy spring day, graduate healthcare students from across North Texas converged at the University of North Texas Health Science Center for the 2025 DFW Healthcare Student Summit. Planned and hosted annually by the Student Council Committee of ACHE of North Texas, this year’s event, under the leadership of Chair Brianna Garza, delivered an enriching and insightful program, leaving attendees inspired and well-equipped for their future roles in healthcare leadership.
Opening the summit was Jared Shelton, President of Texas Health Fort Worth Hospital, whose compelling keynote address on “Crisis Management & Prevention” drew profound connections between the Ebola outbreak of 2014 and the more recent COVID-19 pandemic. Shelton emphasized that effective crisis leadership hinges on emotional stability, clear communication, adaptability, and humility, highlighting the critical necessity of deferring to subject matter experts in times of crisis. Attendees were deeply impacted by his vivid storytelling and actionable insights, as evidenced by attendee Weston Mulqueen’s reflection on Shelton’s emphasis on humility and collaboration.
A subsequent panel discussion amplified these themes, featuring diverse healthcare leaders including Crystal Brown and Timothy Wilson, who underscored the importance of preparedness, communication, and agility during crises. Particularly notable was Brown’s recounting of a significant technological outage


affecting millions, which underscored the necessity of flexible, backup strategies. Wilson’s practical advice on intentional communication resonated deeply, as he suggested leaders ask themselves three critical questions before communicating during a crisis: Does this need to be said? Does it need to be said now? Does it need to be said by me?
The second keynote from Patricia T. Driscoll, Professor at Texas Woman’s University, shifted focus to healthcare policy as a driver of innovation and change. Driscoll articulated how
policy can—and must—evolve, using examples from the rapid adoption of telehealth and expanded nursing roles during the COVID-19 pandemic. A central takeaway, highlighted by attendee feedback, was Driscoll’s assertion that genuine policy impact often originates from incremental, grassroots changes driven by frontline healthcare workers.
The panel on “Policy and Reform in U.S. Healthcare” further addressed urgent industry concerns, such as the ramifications of reimbursement cuts, the critical role oAf digital health technology, and the ongoing nursing shortage in Texas. Panelists called for immediate and strategic investment in nursing education, as Texas faces a projected deficit of 60,000 nurses by 2032. The importance of a diverse and culturally competent healthcare workforce was also a major discussion point, underscored by increasing legislative pressures on diversity, equity, and inclusion initiatives.
Reflecting on the day, attendee surveys echoed a shared sentiment of inspiration and a newfound sense of responsibility. One student noted, “My main takeaway from the summit was realizing that my peers and I are the next generation of leaders who will tackle these healthcare challenges.” Another attendee appreciated the summit’s practical format, suggesting peers view the event as a “case study environment” that provided direct access to the wisdom and experience of current healthcare leaders.
Networking sessions proved invaluable, with many students making meaningful connections with peers and industry mentors, paving the way for future collaborations and professional growth. The event left attendees feeling informed and inspired, ready to apply newfound knowledge to their emerging careers.
The summit’s success, driven by the careful planning of Brianna Garza and her dedicated team, established a robust foundation for future student council initiatives. Garza shared her enthusiasm, noting, “We were proud of the event, and our council members are even more motivated for future events based on the success we experienced.”
In conclusion, the 2025 DFW Healthcare Student Summit was not just an educational event but a powerful catalyst, equipping the healthcare leaders of tomorrow with the insights, strategies, and confidence needed to navigate and influence the future of healthcare in North Texas and beyond.


By Sarah Sentmore, MHA
The second quarter ACHE North Texas educational event featured two insightful panels focused on ethical leadership and the evolving role of digital marketing in healthcare.
Panel 1: Ethical Challenges in Healthcare Leadership Panelists
R. Bryan Day, FACHE, Director of Operational Design and Deployment, Texas Health Resources
Sondra Davis, PharmD, FACHE, Vice President Operations, Medical City
Dr. Michael Rubin, Director of Clinical Ethics, UT Southwestern
Panelists Dr. Michael Rubin, Sondra Davis, and moderator R. Bryan Day emphasized the critical role of ethical leadership rooted in patient-centered values, transparency, and trust. Ethical principles like honesty, kindness, and accountability must guide both strategic decisions and daily operations. Ethics should be operationalized through clear frameworks, regular training, and inclusive decision-making that involves staff, subject matter experts, and community voices. Communicating not just what policies exist, but why they exist, strengthens accountability and engagement. Managing vendor relationships, conflicts of interest, and resource allocation requires well-defined policies and proactive oversight. Creating a culture where staff can report concerns anonymously and without fear of retaliation is essential for maintaining integrity across the organization.



Panel 2: Social Media in Customer Satisfaction and Community Outreach Panelists
Bert Witherspoon, FACHE, Chief Operating Officer, Texas Vision and Laser Center
Makala Pollard, Director of Brand Management, Texas Health Resources
Melissa Weston, Senior Vice President of Marketing, US Radiology
Moderated by Bert Witherspoon with panelists
Melissa Weston and Makala Pollard, this session focused on leveraging digital platforms to enhance consumer trust and access.
Speakers emphasized the need for dedicated social media teams informed by brand, legal, and human resources guidance. Data tracking from engagement to booking is essential for demonstrating return on investment, making collaboration with finance teams vital. Organizations must adopt a Large Language Model Optimization strategy to remain visible and trusted. Clear governance, brand-aligned employee participation, and legal compliance are necessary for safe, strategic digital growth. As innovation accelerates, organizations must ensure their digital presence reflects both ethical standards and brand consistency, while empowering employees to contribute meaningfully.
Together, both panels emphasized that ethical clarity and digital innovation must evolve to best serve patients and communities.
















ACHE Multi-Chapter Healthcare Forum – Transforming Healthcare
The two-day conference united individuals from the ACHE of North Texas and ACHE of East Texas chapters, along with Texas Midwest Healthcare Executives. Keynote speaker Ed Marx inspired attendees to reimagine patient experience as an ethical obligation, rooted in empathy, shared decision-making, and personalized care. He emphasized running healthcare as a service, not a process, and leveraging digital innovation to create meaningful, patient-centered experiences that connect the heart and mind of leadership. He stated, “As leaders, connect the brain to the heart. That’s where transformation happens.”
A special thanks to Texas Woman’s University-Dallas for hosting us for this event and Compass One Healthcare for our meals and snacks.
By Holly Hrabik
Moderator
Ajith Pai, PharmD, FACHE, President, Texas Health Harris Methodist Hospital Southwest Fort Worth & Texas Health Hospital Clearfork
Panelists
Steven Curley, MD, Medical Director, Precision Oncology
Mark Kruzel, MD, Medical Director in Oncology, Quest Advanced Diagnostics
Alex Melton, VP of Engineering, Invene
Precision medicine offers a patient-centric, data-driven approach that translates complex information into targeted treatment and improved outcomes. With diagnostics and therapies advancing rapidly—especially in oncology—patients now arrive informed, expecting personalized care. This shift challenges providers to stay current and deepen conversations.
Yet, significant hurdles remain. Clinical trials are harder to design due to highly individualized treatments, and U.S. enrollment now lags behind China. Many companies conduct trials offshore for faster approval pathways. Meanwhile, commercial payers may not cover genomic tests, limiting access or pushing them into bundled payments.
AI can streamline administrative and diagnostic work, but it must enhance—not replace— clinical judgment. As precision medicine moves into primary care, including potential multicancer blood tests, providers need education and support.
Healthcare leaders must balance innovation with accessibility, policy, and provider readiness. Precision medicine is here, but realizing its full potential requires alignment across science, payment, and people.

By Audrianne Schneider, FACHE
Moderator
Darin Szilagyi, FACHE, FHFMA, SVP Marketing and Communications, Platinum Dermatology Partners
Panelists
San Banerjee, MBA, VP Product Development – Health Services, CVS Health
Lance Lunsford, MBA, FACHE, Co-Founder/ Senior Partner, Groundswell Health
James Schleck, Co-Founder, Growth Verticals, Founding Partner, Tea Leaves Health
This panel focused on launching a new product or service in health care, things to consider when taking it to the market and when to engage Marketing. One example is the activation of the
virtual care platform during the pandemic. The following key tenets apply across the board:
• Look at the effect on patient experience (and other key stakeholders).
• Evaluate the value streams (ensure a shared understanding of what the value streams look like).
• Determine a financial ROI.
• Tell the story – define the product narrative. Get outside perspectives and gather patient input.
• Value has a shelf life – act fast, execute well, and communicate results to stakeholders. Be clear about the problems and the process.
• Marketing should be brought in early – they bring tools and data that help drive business decisions – and they are the storytellers that drive stakeholder adoption.
By Sarah Sentmore, MHA
Moderator
Crystal Brown, VP & COO, Methodist Mansfield
Panelists
Allan Akinradewo, VP Talent Acquisition, Methodist Health System
Frances Dare, Senior Director, Provider Practice Lead, Cognizant
Lance Lunsford, MBA, FACHE, Co-Founder/ Senior Partner, Groundswell Health
Texas healthcare leaders continue to navigate a dynamic landscape shaped by the lasting impacts of the COVID-19 pandemic. Workforce fatigue, rural hospital closures, and persistent gaps in Medicaid funding remain significant challenges. Addressing the needs of a multigenerational workforce demands greater flexibility and more strategic approaches to talent acquisition.
AI is helping streamline hiring for critical roles, yet long-term success depends on internal mobility, leadership development, and an engaged workforce. While technology offers promise, disparities in access, especially in rural areas, exist. The panelists emphasized the importance of embedding health equity into core strategies, strengthening community partnerships, and shifting toward
prevention-based care. As the industry continues to evolve, rebuilding trust and delivering sustainable value will require a people-centered approach that aligns innovation with purpose, equity, and long-term impact.


By Holly Hrabik
Moderator
David Friederichs, Managing Director, Innovacer
Panelists
Brian Felty, Chief Market Payor and Financial Officer, Southwestern Health Resources
Benjamin Hagan, Assistant VP – Benefits, AT&T Services, Inc.
Shannon Huggins, SVP, Contract Strategy & Pop Health, Methodist Health System
William Scott Hurst, MBA, FACHE, President & CEO, Patient Physician Network
This panel explored how health systems can better partner with employers to improve population health. As more employers move to self-insured models, they’re paying the highest care costs with limited ROI—and often lack the bandwidth to optimize health plans. Traditional insurance models, driven by brand and entangled ownership, haven’t adapted to what people truly need: accessible, value-based care.
The most successful approaches center on strong primary care and tight referral networks. Leaders emphasized the need to shift from “wellness” to “wellbeing,” focusing on long-term habits rather than surface-level engagement. With growing provider shortages and rising costs, health systems must stop protecting logos and start acting as true partners— delivering care models that meet employer needs, manage chronic conditions earlier, and support the evolving workforce. Employersponsored care is more than a benefit—it’s a critical opportunity to influence health outcomes across entire populations.


By Melinda Schmidt
Moderator
Bert Witherspoon, MS, MBA, LP, FACHE, COO, Texas Vision & Laser Center
Panelists
Patrick Crocker, Assistant General Counsel, Texas Health Resources
Audrianne Schneider, FACHE, Owner, J29 Marketing Group, LLC
Rebecca Tucker, SVP, Channel Integration, Texas Health Resources
The discussion centered on culture, communication, and leadership. Witherspoon opened by affirming, “Culture can eat strategy for breakfast.” Tucker emphasized teamwork as a strategic foundation, while Crocker described microcultures as barometers of team cohesion.
Panelists stressed empowering voices, especially the quiet ones, and understanding individual motivators beyond compensation. Schneider encouraged authenticity and inclusion, and Tucker advocated for open dialogue—even when uncomfortable—to drive innovation.
The panel highlighted the importance of dyads, triads, and interprofessional collaboration, noting these structures thrive when leaders genuinely listen.
ACHE’s Better Together initiative underscores this shift: diverse, empowered teams deliver stronger results.


By Sarah Sentmore, MHA
Moderator
Kris Sanders, FACHE, SVP, Northern Market Growth and Development, Children’s Health Plano
Panelists
Sarah Hereford, Director, Forvis Mazars
Steve Love, President & CEO, Dallas-Fort Worth Hospital Council
Tammy Walsh, FHFMA, CRCR, CEO, Paramount Healthcare Solutions

Financial sustainability in healthcare requires more than sound budgeting. It calls for strategic foresight, operational discipline, and the agility to adapt to ongoing disruption.
Leaders continue to face pressure from high staffing costs, supply chain instability, and
increasing denial rates—challenges made more complex by a payer mix dominated by Medicare and Medicaid. Rural hospitals, in particular, are struggling to recruit physicians and maintain access to care, often turning to virtual services to fill gaps. As systems recover from the COVID-19 era, many are reevaluating workflows, leveraging data to guide capital planning, and exploring new revenue streams. Managing population health, improving internal alignment, and integrating technology such as AI are becoming essential strategies. With payers shifting risk to providers, organizations must be proactive in contract negotiations, pricing transparency, and applying for grant opportunities. Long-term financial health will depend on the ability to align mission, operations, and innovation with measurable outcomes.
By Holly Hrabik
Moderator
Richard Greenhill, DHA, FACHE, Chief Transformation Officer, Quality Insights
Panelists
Joe Longo, SVP/Chief Digital Information Officer, Parkland Health
Niyati Patel, Program Manager, Strategy & Business Development, MD Anderson
David Vequist, PhD, Director, Center for Medical Tourism Research, Incarnate Word University
Healthcare is increasingly global, driven by digital health expansion, cost disparities, and consumer demand for value. Patients are crossing borders for care—seeking lower costs, faster access, and comparable quality. Procedures like CABG, which can cost $120K in the U.S., are available abroad for $15–20K. Centers of Excellence and private facilities abroad attract patients through transparent pricing, reputation, and digital marketing.
Medical tourism follows a bi-modal pattern: both uninsured and affluent patients travel, while middle-income Americans tend to stay local. COVID-19 accelerated global collaboration and telehealth adoption, while exposing gaps in digital access and care continuity. Women, who make most healthcare decisions, account for 51% of medical tourists despite being more risk-averse.
Foreign providers are often more consumercentric—an area where U.S. systems must improve. With 70% of patients searching online for healthcare, systems must prioritize digital presence, bundled services, and reputation. U.S. leaders must adapt or risk being left behind.

By Sarah Sentmore, MHA
Moderator
Corey Wilson, FACHE, COO, Texas Health Harris Methodist Fort Worth
Panelists
Felixia Colon, FACHE, SVP, SCP Health
Dr. David Gonzales, Regional President of Hospital Medicine & Emergency Medicine Services, Sound Physicians
Don Taylor, MHA, Director, Alliance for Physician Leadership and Director of Practice, UTD
A successful strategy requires more than a wellwritten plan. Cory Wilson opened the panel by stating, “Strategy falls when there is a gap between ideation and implementation.” For a strategic plan to succeed, it must be supported by clear execution, cross-functional alignment, and the ability to adapt. Panelists emphasized that strategy should be embedded in an


organization’s culture, reflected in daily work across clinical, operational, and financial teams. Every team member should understand how their role connects to the broader vision. Communication, training, and consistent leadership are essential to bridging the gap between planning and action.
Success should be measured through a blend of financial, operational, and clinical indicators, including cost savings, service line revenue, productivity gains, and patient outcomes. Strategic plans must be reviewed regularly and remain grounded in mission and values, while flexible enough to respond to evolving external pressures.
AI is increasingly used for forecasting, data analytics, and operational planning. However, challenges remain around governance, training, and clinical integration. Ultimately, an effective strategy relies on clarity, accountability, and shared ownership across the organization.
By Holly Hrabik
Moderator
Aaron Bujnowski, FACHE, Managing Director, Alvarez and Marsal
Panelists
Chris Core, Chief Growth Officer, US Radiology Specialists
Lee Mathew, Administrator, USPI
Mergers and acquisitions are among the most disruptive events in an employee’s career—and their success hinges not just on strategy, but on people. Healthcare leaders must lead through both transformational and situational lenses: clearly articulating mission and vision at the macro level, while adapting communication for frontline staff just learning about the change.
Cultural alignment, not just operational integration, determines whether the benefits of scale—talent retention, best practice adoption, and cost efficiencies—are realized. Leaders must identify informal influencers, invest time in listening, and foster a sense of ownership across all levels. Over-invest in communication using a “drumbeat” strategy: consistent, transparent, and multi-modal messaging that builds psychological safety.
Involve your board early, choose advisors wisely, and resist overpromising. Employees won’t remember every detail—but they will remember how you made them feel. M&A success in healthcare depends on thoughtful leadership, intentional engagement, and people-first execution. MULTI-CHAPTER

By Bert Witherspoon, FACHE
Moderator
Jeff Stewart, FACHE, VP
Strategic
Marketing, CHRISTUS Health
Panelists
Stacy Covitz, Chief Marketing & PR Officer, Methodist Health
Fernand “Fern” Fernandez, Chief Marketing and Communications Officer, Children’s Health
Daphne Tam, MS, Founder and Principal, DT Communications
The Strategic Marketing Panel brought together healthcare leaders to emphasize the critical role of marketing in organizational strategy and patient engagement. Panelists
Jeff Stewart (CHRISTUS Health), Daphne Tam (DT Communications), Stacy Covitz (Methodist Health System), and Fern Fernandez (Children’s Health) underscored the need for marketing to


be integrated early in strategic planning. They discussed leveraging consumer insights and data-driven methods to track effectiveness.
The panel highlighted the importance of managing reputational risk through proactive crisis communication planning, with Children’s Health offering a model of pre-scripted responses for IT failures and other issues. They also addressed the growing influence of social media and the need for coordinated authentic influencer strategies, recognizing that influencers are now their own channel of communication. Navigating political and social climates with sensitivity and alignment to organizational values was another key theme. The session called on organizations to better educate internal stakeholders about marketing’s value and to strengthen ties between marketing, legal, and compliance functions for long-term resilience.
Denise Braddy, MBA, BA
Sebastian Busto, MBA
Ashlee Byers
Tiffany Capeles, FACHE
Christina R. Coyle, DNP, MBA, RN, NEA-BC, FACHE
Eric Dickerson
April Green
Adrian S. Hall, MBA
Peter Harris
Rochelle R. Hartmann
Christopher Hendricks
Emily Hildrey, MPH
Laura A. Hochwalt, RN
SSG Omolola T. James
Carol C. Jiwan, MSc, MHA
Keondra Jones
Ajay K. Kharbanda
Vu Le
Julie A. Lively, MS
Karla L. Lux
Marisol Magana
Naman Mahajan
Richard Nayak
Sarai Olvera
Ellie R. Ortiz
Keshondra Porchia, CPC
Anaya Rhodes
Leslie Rios
George Sapp
Emily Sedgwick, MD
Sheila Shoemake
Heather Sieracki
Tracey Taylor
Kasandra Thomas, BSN
Kyran K. Vaughn
Lloyd S. Walter
Jenny Wang
Colin G. Weems
Cameron G. Werner
Mary H. Williams, MS
Shamon Willis
MARCH
Brandon Bays, MHA
Nikia Bell
Steven Bender
Melissa J. Bove
Vincent Brown, Jr., MBA
Justin Burton, MBA, BSN, RN
Angelica Cage
Ngoc Van Cantrell
Debra I. Culmer
Anthia P. Dasari
Cris C. Daskevich, FACHE
Aaron C. Davis
Ana Maria De Leon, BSN
Jocelyn C. Fuller
James Griffin
Michelle Hopkins, MBA, BSN, RN
Penny L. Johnson, MBA
Shadetra Johnson
CAPT Maggie Johnson Glover, PhD, RN
Tiffany Krabbe
Keviesha Lacy
T. Douglas Lawson, PhD
HM2 Keandre Livingston
Lori Mathieu, MSN
Jennifer Mayhan, MSN, MSHA
Christine C. McCracken, OTD, FACHE
Goodwin McCutcheon
Leah Miller
Aly O’Bryan
HM2 Aaliyah S. Ostrom
Capriana A. Oyedeji
James M. Perez, MHA, CMPE
Toya Rand
Stephen R. Randall
Kayla M. Singleton, MHA, BSN, RN
Kristopher Stepps, MD
Tamera S. Sutton
Kelli Thomas-Drake
LaQuanda Thompson
Sydney Tischler
Joseph Young
APRIL
Andrea Airhart, BSN
Alyssa Aldrich, FACHE
David Anton
Viv Babber, MD
Suzette Bagalman, FACHE
Sebastian Bauer Hollaender, MBA, MHA
M. Glen Boles, FACHE
Tiffany Bradshaw
Amanda E. Calongne
Kevin W. Carroll
Britnie Chanheuang
Ravin Cline
Jonathan E. Dayton
Benjamin J. Derry
Cassandra Dike
Michael D. Dinwiddie
Donni Do
Jeff Ellison
Fernand Fernandez
Jerry S. Findley, EdD
Amanda Fisher
Haley Fleischer
George B. French, RN, FACHE
Casey R. Galloway
Joshua M. Glenney
Jacqwan N. Goldwire, BS, LPN
Mathew W. Gurksnis
Anthony Haskins
William Henderson, MBA
Kennetra Holloway
Grace A. Irving, EMBA, MA
Kandace Jamison
CPO Curtis D. Jones
Zaurez Khan
Martin Marinov, MD
Alexander M. Melton
Lauren Miller
Dr. Phil Odoemena, DHA, MBA
Beatrice N. Onubuike, MSN, RN, NEA-BC
Ekta Pathare, FACHE
Jasmine Rainey
Robert Ray, PhD, MBA
Victoria Rodino, PhD, MPA, MPhil
Christopher J. Rodriguez, MBA
Ahana Shetty
Lt Col Allen Solenberg
Bruce Taylor
Rachael Tudgay
Brandi Vines
Will Warren
Andrea Wooden
FEBRUARY
Saul Cordero, PE, FACHE
MARCH
Ozioma Olowu, PharmD, FACHE
Laura B. Tillett, FACHE
Judy Travis, FACHE
APRIL
Gurbinder Jassar, PharmD, FACHE
Allece Merchant, RN, FACHE
Nanette L. Myers, FACHE
Shane B. O’Neill, FACHE
FEBRUARY
Brent N. Adams, FACHE
Mari J. Finley, DNP, RN, APRN, FACHE(R)
Heather Jones, FACHE
Jim R. Kendrick, Jr., FACHE
John E. Phillips, FACHE
Gail E. Seaman, FACHE
APRIL
David E. Domingue, FACHE
Jenese M. Holland, FACHE
Tyler Krohn, MD, MBA, FACHE
Christi Nguyen, DNP, RN, NEA-BC, FACHE
Colin P. O’Sullivan, DHA, FACHE
Ajith Pai, PharmD, FACHE
Ekta Pathare, FACHE
Thanh Tran, FACHE