




2 0 2 5
◼ Patients seeking treatments that produce more subtle results see page 4
JAK inhibitors
n All pts receiving a JAK inhibitor must be up-to-date with vaccinations
by LOUISE GAGNON, Correspondent, The Chronicle
The use of systemic Janus kinase (JAK) inhibitors and topical JAK inhibitors for multiple conditions is having a highly favourable impact on skin health, according to leading Canadian dermatologists.
JAKs for atopic dermatitis (AD) Systemic JAKs for moderate-to-severe AD such as upadacitinib and abrocitinib are producing high efficacy and good tolerability in clinical practice, according to Dr.

Dr. Ashley O’Toole
Ashley O’Toole. “They have an extremely fast onset of action,” she noted. She is a dermatologist at the SKiN Centre for Dermatology in Peterborough, Ont., at the Campbellford Memorial Hospital in Campbellford, Ont., and Adjunct Professor, Queen’s University, Kingston.
n Have greater Breslow thickness at Dx
by JOHN EVANS, Senior Editor The Chronicle
Rates of melanoma skin cancer among the Māori population are growing in New Zealand, the nation with the highest melanoma mortality rate in the world. As with many other darker-skinned populations, the Māori tend to present later, with greater Breslow thickness and have poorer outcomes. However, research in this population faces several challenges. This message was part
“In terms of tolerability, acne is a side effect that can occur with Please turn to Melanoma page 10→
upadacitinib while gastrointestinal effects such as nausea may occur with abrocitinib. “There are ways to mitigate both side effects,” said Dr. O’Toole. “You can treat the acne [that may develop with upadacitinib], and you can counsel about how to reduce side effects like nausea, such as taking it [abrocitinib] with food.”
Dr. Michal Martinka, a dermatologist with Rejuvenation Dermatology Clinic in Calgary, noted that upadacitinib and abrocitinib have a long-lasting effect.
“They have a durable re-
n Topical JAK inhibitor offers benefit in pediatric patients with vitiligo
by LOUISE GAGNON Correspondent, The Chronicle
With increasing studies specifically in the pediatric setting, more and more agents approved for adult patients are becoming treatment options in pediatric dermatology.

Speaking at the annual pediatric dermatology update in Montreal organized by the pediatric hospital Centre Hospitalier Universitaire Sainte Justine, Meryem Safoine MD, PhD, a fifthyear dermatology resident at the University of Montreal/St. Justine Hospital, noted numerous therapies have recently become available for use by pediatric dermatologists.
n Share your experiences and observations with a worldwide community of practitioners and researchers. Follow developments in skin health as they occur.




OPZELURA (ruxolitinib) cream 1.5% is indicated for the topical treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older.1







OPZELURA is the treatment indicated in nonsegmental vitiligo





















































Please consult the Product Monograph at https://incytesolutions.ca/ OPZELURA_PM for contraindications, warnings and precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The Product Monograph is also available by calling 1-833-309-2759
* Comparative clinical significance has not been established. References: 1. OPZELURA Product Monograph. Incyte Corporation. 2. Data on File. Incyte Corporation.
OPZELURA and the OPZELURA logo are registered trademarks of Incyte. Incyte and the Incyte logo are registered trademarks of Incyte. © 2025, Incyte Biosciences Canada Corporation.




























Melanoma rates high in New Zealand Māori
At the Indigenous Skin Spectrum Global Summit, Dr. Monique Mackenzie spoke about the high rates of melanoma among New Zealand’s Indigenous Māori population. . . . . . . 1
Vender on PsO:
Combining targeted real-world data with advanced analytics

In this issue of THE CHRONICLE OF SKIN & ALLERGY, our reporters cover the pillars of dermatology practice including cosmetic dermatology, pediatric dermatology, medical dermatology, as well as laser and surgical dermatology.
Also, a new study showed that tapinarof cream 1% QD enables a high proportion of patients with mild to severe plaque psoriasis to achieve or exceed ambitious treat-to-target endpoints
Celebrating 30 years of dermatologic progress
From the News Resources of The Chronicle
8
Findings from a study published in Cureus (March 8, 2025; 17(3):e80247) show that postmenopausal dermatoses represent a significant, underrecognized issue related to women's health in India.
All eight issues of THE CHRONICLE OF SKIN & ALLERGY in 2025 will feature a countdown of the 30 key innovations, breakthroughs, and coursechanging discoveries and events that have dramatically changed dermatology
Chronicle Postgraduate Educational Supplement
14
In this issue’s postgraduate educational supplement, researchers performed a narrative review of studies outlining the advancements in acne scar treatment. The authors found that the varied nature of acne scars, highlights the need for personalized treatment strategies
19
This cross-sectional study included 200 cases of postmenopausal women with dermatoses in any area of the body treated at the Dermatology OPD, Sri Ramachandra Institute of Higher Education and Research between Jully 2022 and July 2024. Researchers circulated a semi-structured questionnaire to document data on age, presenting complaints, associated symptoms suggestive of any underlying autoimmune, connective tissue disorder or malignancy, personal and family history of diabetes mellitus, hypertension, endocrine disorders, cardiovascular diseases, dietary and menstrual history,

June 2025 • Vol. 31 No. 4
Published eight times per year by the proprietor, Chronicle Information Resources Ltd., with offices at 1460 The Queensway, Suite 212, Etobicoke, Ont. M8Z 1S4 Canada. Telephone: (416) 916-2476; Facs. (416) 352-6199.
E-mail: health@chronicle.org
ISSN No. 1209-0581
Contents © Chronicle Information Resources Ltd., 2025 except where noted. All rights reserved worldwide.
The Publisher prohibits repro-
duction in any form, including print, broadcast, and electronic, without written permissions.
Printed in Canada. The Chronicle of Skin & Allergy is a Canadian publication. The Publisher certifies that advertising placed in this publication meets Revenue Canada requirements for tax deductibility.
Subscriptions: $85.60 per year in Canada, $129.95 per year in all other countries. Single copies: $10.00 per issue (plus 13% HST).
socioeconomic history, sanitation history, and obstetric history. The mean age of the participants was 58.99±9.12 years. The age at which menopause started was 40 to 50 years for most participants (n=127, 63.5%). Occupation-wise, most participants were housewives (n=178, 85.5%). Wrinkles, observed in 149 patients (74.5%), were the common physiological change noted. Of the pathological changes, fungal infections such as tinea (n=29, 14.5%) were the most common. Among eczematous conditions, asteatotic eczema, observed in nine patients (4.5%), was the most common; as for papulosquamous disorders, psoriasis (n=22, 11%) was the most frequent condition. Seborrheic keratosis (n=43, 21.5%) was the most frequent benign tumor; regarding psychocutaneous disorders, lichen simplex chronicus (n=3, 1.5%) was the most encountered condition.
Canada Post Canadian Publications Mail Sales Product Agreement Number 40016917. Please forward all correspondence on circulation matters to: The Chronicle of Skin & Allergy, 1460 The Queensway, Suite 212, Etobicoke, Ont. M8Z 1S4
Ideas in the Service of Medicinesm Affiliated journals of the Chronicle Companies include The Chronicle of Cosmetic Medicine + Surgery, Women in Dermatology, Pediatric Chronicle, and Linacre’s Books/ Les Editions Linacre

“I
would say skin quality has become a much bigger topic in dermatology in the last couple of years, where it is not just about adding volume to the face but making sure the
skin is hydrated and smooth and has a dewy glow”
Dr. Michal Martinka, a dermatologist in Calgary

On the cosmetic front one of cosmetic medicine’s pioneers—and my good friend—Dr. Sheetal Sapra, discusses the role of biostimulatory agents, and he also provides some comments on the emerging neurotoxins. Drs. O’Toole, Lee, and Martinka also make significant contributions to this update, which is a good read for all of us (see page 4).
Medical Editor Wayne Gulliver, MD, FRCPC
John P. Arlette, MD, FRCPC
Benjamin Barankin, MD, FRCPC
Marc Bourcier, MD, FRCPC
Eric Goldstein, MD, FRCPC
Peter Hull, MD, FRCPC
Richard Langley, MD, FRCPC
Danielle Marcoux, MD, FRCPC
Editor, Cosmetic Dermatology Sheldon V. Pollack, MD, FRCPC
Melanie D. Pratt, MD, FRCPC
Denis Sasseville, MD, FRCPC
Jerry Tan, MD, FRCPC
Ronald B. Vender, MD, FRCPC
R.A.W. Miller, MD, FRCPC H. Eileen Murray, MD, FRCPC Kim Papp, MD, FRCPC Yves Poulin, MD, FRCPC
Founding Editor Colin A. Ramsay, MD, FRCPC (1936-2003)
Publisher Mitchell Shannon
Editorial Director R. Allan Ryan
Senior Editor John Evans
Assistant Editor Jeremy Visser
On the pediatric front we have many new agents for the treatment of seb derm, atopic dermatitis, and alopecia areata. JAK inhibitors as well as PD4s along with new antiIL13 agents are advancing our therapies for our pediatric patients (see page 1). On the JAK front we are observing the significant impact that the systemic JAKs abrocitinib and upadacitinib are making, with the topical JAK ruxolitinib also making a Client Engagment Cristela Tello Ruiz
Conference Organizer
Please turn to Message page 12→ Shannon Abbott
Media Consultants Cathy Dusome Darren Stallman
Comptroller Rose Arciero
n READER SERVICE: To change your address, or for questions about your receipt of the journal, send an e-mail to health@chronicle.org with subject line “Circulation,” or call during business hours at 416.916.CHROn (2476), or toll-free at 866.63.CHRON (24766).
n LETTERS: We welcome your correspondence by mail, fax (416.352.6199), or e-mail. Kindly use the co-ordinates listed above.
n ADVERTISING: For current rates and data, please contact the publisher.
n REPRINTS: The content of this journal is copyrighted. Please contact Mitchell Shannon for reprint information.
0 2 5

by LOUISE GAGNON, Correspondent The Chronicle
An emerging neurotoxin, a novel form of laser that is useful in all skin tones, hyaluronic acid gels for superficial injection, and the expanded use of biostimulatory agents are all topics that are trending in cosmetic dermatology.
Using hyaluronic acid gels
Injectable skin boosters (hyaluronic acid gels) are becoming increasingly popular as patients are seeking improvement in their appearance that appears more subtle, according to Dr. Michal Martinka.
“Skin boosters are injected into the skin itself to plump and hydrate the skin from within,” said Dr. Martinka, a dermatologist with Rejuvenation Dermatology Clinic in Calgary.
“They are different than traditional fillers, which are typically injected deep underneath the skin, into the fat pads, or directly onto the bone to provide a lift. The lighter products would be injected more superficially into
the skin, where the thicker, more viscous, or denser products would be injected deeper into the skin to provide that volume.



“I would say skin quality has become a much bigger topic in dermatology in the last couple of years, where it is not just about adding volume to the face but making sure the skin is hydrated and smooth and has a dewy glow,” said Dr. Martinka. “A very common concern I hear from patients is that they say their skin looks dull. They are asking to have radiant, healthylooking skin. Skin boosters give that brighter, dewy glow to the skin.”
Greater use of biostimulatory agents
Injectable biostimulatory agents such as poly-L-lactic acid and calcium hydroxyapatite are not new to cosmetic dermatology, but what is new is an increased focus on skin quality that has given risen to using these injectables for that reason.
“We use a lot more Sculptra and Radiesse, not necessarily for lifting and volumizing, but for skin texture and tone,” said Dr. Sheetal Sapra, Director of Dermatology at the Institute of Cosmetic and Laser Surgery in Oakville, Ont. “We use it in areas like the decollete, the chest, the arms, and the hands. When we inject Radiesse, we see the results right away, and with Sculptra it takes a little more time to see results.”

Biostimulatory agents are also helpful to address skin laxity that has developed associated with the use of medications such as GLP-1 RAs and resulting weight loss from those medications, noted Dr. Sapra. Emerging neurotoxin Trenibotulinumtoxin E, which has been submitted to the U.S. Food and Drug Administration for approval in

The FIRST and ONLY TOPICAL ANTI-ANDROGEN for patients with acne vulgaris*

Please consult the Product Monograph at https://sunpharma.com/wp-content/uploads/2023/08/Winlevi_Pm.pdf for important information about:
• Warnings and precautions including, only using PrWINLEVI® (clascoterone) externally; avoiding accidental transfer of WINLEVI® into eyes, lips, mouth, corners of the nose, or other mucous membranes; hypothalamic-pituitary-adrenal axis suppression; local irritation; susceptibility to systemic toxicity in pediatric patients; no available data on the use of WINLEVI® in pregnant women and no studies were conducted to determine the presence of clascoterone or its metabolite in human or animal milk.

• Conditions of clinical use, adverse reactions, drug interactions, and dosing instructions. The Product Monograph is also available by calling 1-844-924-0656.
*Comparative clinical significance unknown.
Reference:
1.
Continued from page 4
the treatment of moderate-to-severe glabellar lines, will offer patients a neurotoxin option with a very quick onset of action that has a limited duration of effect, noted Dr. Ashley O’Toole.
“The onset is so much faster than with botulinum toxin A, which usually has an onset about five to seven days after injection,” said Dr. O’Toole, who participated as a clinical trialist in the phase III program for the novel neurotoxin. “The onset is within hours. Even at the Hour 8 followup visits, some patients had clinical evidence of efficacy.” She is a dermatologist at SKiN Centre for Dermatology in Peterborough, Ont. and the Campbellford Memorial Hospital in Campbellford, Ont., and Adjunct Professor, Queen’s University, Kingston, Ont.
The neuromodulator’s rapidity of onset is accompanied by an abbreviated duration of action, pointed out Dr. O’Toole.
“Most neurotoxin injections that are on the market usually last three to four months for many people, but this one will last on average three to four weeks,” explained Dr. O’Toole. “It wears off much more quickly than traditional neurotoxins.”
For patients who are neophytes to neuromodulators, Dr. O’Toole shared that trenibotulinumtoxin E is a good starting point to see how patients respond to a neurotoxin and if they like the visual effect.
“Patients say they don’t want to look ‘frozen’ or they are wavering on the decision [to be injected with a neuromodulator],” said Dr. O’Toole.
“For such patients, this would be a nice option. It is a good entry into the neuromodulator space.”
Dr. Sapra agreed that the limited effect of trenibotulinum toxin E represents a minimal risk proposition for those who are reluctant to be injected with a neurotoxin.
“It is fast-acting and short-acting. This helps patients decide whether they like botulinum toxin or not,” said Dr. Sapra. “It is a way to ‘try on’ botulinum toxin. If a patient doesn’t like the results, the effect will wear off within a month.”
Cosmetic innovations for all skin types
A topical anti-aging serum, which contains the ingredient Epicelline, is an innovation in skin care that purports to turn back the clock and has been designed with all skin tones in mind, according to Dr. Monica K. Li.
“Based on clinical studies, Eucerin HyaluronFiller Epicelline serum significantly improved signs of aging after four weeks of use, such as fine lines and skin firmness,” said Dr. Li, who noted that clinical studies are underway currently to evaluate the effectiveness of the serum in more richly-pigmented individuals. “Of course, aging and signs of aging develop in all individuals, so the intent for this serum is to be beneficial, compatible and well-tolerated by the full spectrum of skin tones.” She is a dermatologist at Vancouver Skin MD and Clinical Assistant Professor at the University of British Columbia, Vancouver. An option in laser technology has emerged
that is agnostic with respect to skin pigment. UltraClear, touted as the first cold, ablative fractional laser for anti-aging, offers cold fractional resurfacing, according to Dr. Sapra.
“The unique thing about this laser is that it can be used in any skin type,” said Dr. Sapra. “When it delivers the pulses, they are not causing heat injury. This laser will be really safe to use.”
Research shows a new moisture treatment more than doubles objective measures of skin hydration by eight weeks while significantly improving patientreported satisfaction in all Fitzpatrick skin types. The treatment expands a welltested combination of hyaluronic acid, natural moisturizing factors, and skin barrier supporting lipids.
In an interview with THE CHRONICLE OF COSMETIC MEDICINE + SURGERY, Dr. Allison Sutton—founder and medical director of West Dermatology in Vancouver, and Dr. Jennifer Salsberg— codirector of AvenueMD Cosmetic Dermatology and Plastic Surgery in Toronto, discussed the treatment, supporting research, and which patients would most benefit from the formulation.
Dr. Sutton explained the new moisturizing cream, marketed by skinbetter science under the name Trio Luxe, adds three new active agents to the base formula used in skinbetter science’s established Trio rebalancing moisture treat
ment:
• Glycine, which is one of the amino acids that likely is playing a role with replenishing natural moisturizing factor and is found in lower concentrations in dehydrated skin


• Niacininamide, a form of vitamin B3 that plays many roles in the skin, which can help with skin hydration, brighten the skin, support collagen formation, and has anti inflammatory and antioxidant properties
• Olea Europea (olive) fruit extract, which can reduce redness
Trio Luxe has been evaluated in both a skin model study and a small clinical study.
In the skin model study, researchers observed an increase in aquaporins— water channels that transport water, urea, and glycerol, claudins, and hyaluronic acid synthase, while levels of hyaluronidase decreased.
For the clinical study, researchers recruited 27 female participants, 50 to 70 years of age, with Fitzpatrick skin types I to VI and moderatetosevere dry, dehydrated skin. The investigators evaluated skin hydration, safety, tolerability, and patient satisfaction over eight weeks. Key findings included:
• 41% increase in skin hydration at week 2, and 116% at week 8
• 100% said their skin looked younger and healthier
• 100% said their skin texture looked smoother, and fine lines and wrinkles were less noticeable
• 96% said their skin felt deeply hydrated and nourished, and they would continue to use this product
Dr. Salsberg said Trio Luxe can be recommended to patients who have very dry, dehydrated skin. It could also be a seasonal choice for patients who have more average to slightly dry skin but need an extra boost of hydration in the colder, very dry winter months.
Patients with very sensitive or reactive skin may also find Trio Luxe valuable. Trio Luxe has also been studied immediately postprocedure after nonablative skin treatments. Findings showed physicians can safely use Trio Luxe immediately postprocedure, potentially aiding the healing process or the aftercare process following those procedures.


“It’s
like somebody is stabbing you with needles. Every movement was agonizing. Any time anything touched it, I wanted to scream...”*
Hidradenitis suppurativa (HS) is a debilitating, chronic inflammatory skin disease that causes significant burden on patients’ lives.1
Timely and accurate diagnosis matters. HS is underdiagnosed, underrecognized by patients, and often misdiagnosed.2
1.

Ronald B. Vender, MD, FRCPC comments on recent findings and developments, and answers clinicians’ questions
Treat-to-target strategies in psoriasis management emphasize achieving stringent clinical endpoints, such as ≤1% body surface area (BSA) involvement or low absolute Psoriasis Area and Severity Index (PASI) scores, as recommended by the National Psoriasis Foundation (NPF) and the European Academy of Dermatology and Venereology (EADV). While these targets are often unmet with conventional topical therapies, tapinarof cream 1%—a nonsteroidal aryl hydrocarbon receptor agonist—has demonstrated efficacy in plaque psoriasis. This pooled analysis evaluated the proportion of patients achieving treat-to-target outcomes with tapinarof cream 1% once daily (QD) in the PSOARING phase 3 clinical program (Cutis 2024 October; 114(4):122-127, E1. doi:10.12788/cutis.1112).
Data were pooled from PSOARING 1 and PSOARING 2 (12-week, randomized, double-blind, vehicle-controlled trials) and PSOARING 3 (up to 40-week open-label extension). Analyses included 915 adults (mean age 50.2 years; 58.7% male) with mild to severe plaque psoriasis (PGA ≥2, mean baseline PASI 8.7, mean BSA 7.8%). Patients received tapinarof cream 1% QD, with intermittent or continuous dosing in the extension phase based on clinical response. Primary endpoints were the proportion achieving (1) ≤1% BSA affected and (2) absolute PASI scores ≤3, ≤2, and ≤1. Time-to-target analyses utilized Kaplan-Meier estimates.
At three months, 40% of patients achieved the NPF-recommended target of ≤1% BSA affected; 61% achieved this threshold at any time during the study (median time to target: ~four months). Additionally, 50% achieved a more stringent target of ≤0.5% BSA (median: ~6.5 months). Regarding PASI outcomes, 75% achieved an absolute PASI ≤3 (median: two months), 67% achieved PASI ≤2 (median: three months), and 50% achieved PASI ≤1 (median: six months). Efficacy was observed across the spectrum of baseline disease severity. Tapinarof demonstrated durable responses, with no evidence of tachyphylaxis and a remittive effect of approximately four months off therapy. The safety profile was favourable, with most adverse events being mild or moderate and not leading to discontinuation.
Results showed that tapinarof cream 1% QD enables a high proportion of patients with mild to severe plaque psoriasis to achieve or exceed ambitious treat-to-target endpoints, including those typically reserved for systemic or biologic therapies. These findings support tapinarof as an effective, durable, and well-tolerated topical option for achieving optimal disease control without restrictions on duration, extent, or application site
Tapinarof is a novel topical cream that’s steroid-free and works through the aryl hydrocarbon receptor pathway. In pooled data from phase 3 trials, many patients with mild to severe plaque psoriasis were able to reach goals that are usually reserved for systemic treatments—like reducing body surface involvement to less than 1%, or achieving very low PASI scores. What’s even more impressive is that the results lasted well beyond the treatment period for many patients, with no signs of the skin getting used to the drug or losing effect.
My take: We’ve been waiting for a high-performing topical that doesn’t come with steroid baggage—and tapinarof delivers. It’s an exciting option for patients who don’t want or can’t tolerate systemic drugs but still want results that go beyond "just good enough." This may reshape how we treat patients who fall in the moderate disease gap.
Real-world evidence (RWE) is increasingly recognized as a critical complement to randomized controlled trials (RCTs) in informing regulatory, payer, and clinical decision-making, particularly for complex, heterogeneous diseases such as those driven by type 2 inflammation. However, RWE data sources are often fragmented and inconsistently collected, limiting their utility for large-scale, hypothesis-driven research (Frontiers in Allergy DOI 10.3389/falgy.2022.951795). To address these challenges, the Immunolab platform was developed as a scalable, interactive RWE generation tool to facilitate comprehensive evidence generation in immunology, with a focus on diseases such as asthma, atopic dermatitis (AD), and chronic rhinosinusitis with nasal polyps. Immunolab leverages a large, de-identified electronic health record (EHR) and claims dataset from Optum, encompassing over 17 million patient lives and 33 type 2 immunological indications. The platform comprises three core analytical modules:
Immunolab enables rapid, large-scale analyses, supporting over seven million distinct insight-generation analyses across its modules.
The PJM module can perform approximately
• five million analyses across 70 predefined patient subpopulations, providing granular visualization of treatment escalation and comorbidity patterns.
The SM module executes up to two million
• analyses, generating 130 descriptive statistics per switch/augmentation event and identifying key demographic and clinical predictors of treatment change using SHAP-based model explanations. The H2H module facilitates up to 75,000 com-
• parative effectiveness analyses, with 150 descriptive statistics across 150 patient subpopulations and four therapeutic groups, enabling robust, confounder-adjusted comparisons between drug classes.
Collectively, these modules provide a scalable,
• hypothesis-driven framework for RWE generation, supporting rapid, reproducible, and clinically relevant insights into treatment patterns, drivers of therapy modification, and comparative effectiveness in immunological diseases.
Immunolab demonstrates the feasibility and value of an integrated, analytics-driven RWE platform in immunology, offering standardized, highthroughput tools for evidence generation at scale. The platform’s modular design and advanced analytic methodologies position it as a first-line resource for researchers and decision-makers seeking to address complex real-world clinical questions and optimize patient outcomes in type 2 inflammatory diseases.
Immunolab is a digital platform designed to make real-world data (RWD) more usable and insightful, especially in diseases like asthma, atopic dermatitis, and chronic sinusitis. It combines large health record and insurance datasets from more than 17 million patients and uses advanced analytics to explore treatment paths, understand why patients switch medications, and compare drug effectiveness in real time. Tools like Sankey diagrams, machine learning predictors, and causal inference models make the data visual and practical for researchers and clinicians.
Patient Journey Mapper (PJM): Describes longitudinal drug treatment patterns and comorbidities in
• defined patient cohorts using a patient-quarter framework, with outputs including Sankey plots and histograms.
Switch Modeller (SM): Utilizes machine learning (LightGBM) and SHapley Additive exPlanation
• (SHAP) values to identify and quantify key drivers of treatment switching and augmentation events. Head-to-Head Simulator (H2H): Employs causal inference methodologies (G-estimation, inverse prob-
• ability of treatment weighting) to estimate comparative effectiveness of drug classes across clinically relevant endpoints, adjusting for confounding using high-dimensional covariate data.
My take: As someone involved in both clinical care and trials, I find platforms like Immunolab incredibly valuable. It helps bridge the gap between what we see in tightly controlled trials and what happens in the real world. The ability to run comparative effectiveness studies using actual patient data could become a standard part of our evidence toolkit in the near future.
We invite your comments and questions about this feature at www.derm.city. Dr. Ron Vender is a certified dermatologist with more than 30 years of clinical practice experience and over 100 clinical trials in psoriasis. He is founder and director of Venderm Innovations in Psoriasis, a center of excellence for Psoriasis offering a comprehensive management solution for individuals with psoriasis. www.psoriasis.vip




Available as a cream, ideal for pruritus, and as a lotion with menthol for a cooling, soothing effect.
An antipruritic and anti-inflammatory lotion and cream containing hydrocortisone 1% (in acetate form), and pramoxine hydrochloride 1%, Pramox HC is the perfect treatment for minor skin irritations including:
• Rashes
• Itching and redness due to eczema
• Poison ivy, poison oak, and poison sumac
• Contact dermatitis
• Seborrheic dermatitis
• Psoriasis
• Insect bites
Available at Shoppers Drug Mart and most local drugstores.

Are the lesions in the above image truncal acne or something else?
A. Truncal acne
B. Folliculitis
C. Dermatologic manifestations of tuberous sclerosis
D. Steatocystoma multiplex
THIS REGULAR FEATURE OF THE CHRONICLE OF SKIN & ALLERGY IS SUPPORTED BY
Continued from page 1
of a presentation by Dr. Monique Mackenzie (Ngāti Tūwharetoa) at the first-annual Indigenous Skin Spectrum Global Summit, which was held on April 5, 2025, in Montreal.
Dr. Mackenzie is a Consultant Dermatologist at Skin Centre, Tauranga, New Zealand. She is the first Indigenous Māori Dermatologist in New Zealand. She has worked in Australia and the United Kingdom and has been involved in many initiatives to help grow Indigenous knowledge (Mātauranga Māori) and language (Te Reo Māori) in dermatology.

She said there had been a 4.3% increase in the age-standardized rate of melanoma in New Zealand’s Māori between 2000 and 2021.
Greater Breslow thickness
A study published in the World Journal of Surgery (Aug. 2010; 34(8):1788-1792) found that Māori patients showed a greater Breslow thickness at the time of diagnosis as well as a later presentation. “Breslow thickness also increased with age and was quite significant over the age of 70,” Dr. Mackenzie said. There were also significantly poorer survival outcomes.
Also, the distribution of melanoma showed it occurred more frequently on non-sun-exposed sites, and acral melanoma was of much greater incidence than in patients of European ancestry.
Dr. Mackenzie said there is a 156% excess
melanoma mortality percentage for the Māori population compared to their European counterparts. She identified several factors that may contribute to that finding:
• insurance
Poor access to health care and private health
Existing socio-economic disparities
• A lack of education in detection among both
• patients and healthcare providers
A misperception in the community that hav-
• ing a darker skin type protects you from skin cancers
There is an acute lack of clinical research in
• this population
“Data collection has been fraught in New Zealand,” said Dr. Mackenzie. “That's mainly around deciding on a definition for different ethnic groups. Historically, it's been inaccurately collected. Only about one in five Māori were documented as being Indigenous Māori with their national health index numbers.” She noted there is no accurate count of non-melanoma skin cancers in New Zealand’s Māori population.
Bottom Line: Rates of melanoma among New Zealand’s Indigenous Māori population are growing, while the nation already has the highest rate of melanoma mortality in the world. Similar to many darker-skinned populations, the Māori tend to present later, with thicker melanomas, and the acral form of the cancer is more common. Healthcare resource limitations and challenges with data collection complicate research in this field.
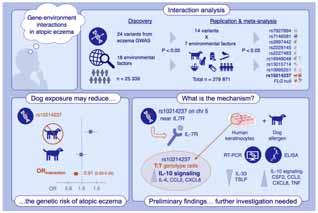
Findings from a new study suggest early-life exposure to domestic dogs may modify the effect of one genetic risk factor for atopic eczema (AE)— a single-nucleotide polymorphism known as rs10214237. This finding supports observational epidemiology that has shown a protective effect of dog ownership against AE.
In the study, published online in Allergy (June 4, 2025), researchers an-
alyzed data from 16 European studies to test for interactions between the 24 most significant AE-associated gene variants and 18 early-life environmental factors. They then tested for replication using a further 10 studies and in vitro modeling to independently assess findings.
The discovery analysis included 25,339 individuals and showed suggestive evidence for interaction (p<0.05) between seven environmental factors (antibiotic use, cat ownership, dog ownership, breastfeeding, elder sibling, smoking and washing practices) and at least one established genetic variant for AE—14 interactions in total.
In the replication analysis (254,532 individuals) the relationship between dog exposure and the rs10214237 gene variant was nominally significant (Odds ratio for the interaction =0.91 [0.83–0.99] p=0.025), with a risk effect observed only in those not exposed to dogs.
The investigators observed a similar interaction with rs10214237 for siblings in the discovery analysis (ORinteraction =0.84 [0.75–0.94] p=0.003), but the replication analysis was under-powered (ORinteraction = 1.09 [0.82–1.46]). They note the rs10214237 homozygous risk genotype is associated with lower interleukin (IL)-7 receptor expression in human keratinocytes, and dog exposure modelled in vitro showed a differential response according to rs10214237 genotype.
In their conclusion, the authors write that their interaction analysis and functional assessment provide preliminary evidence that early-life dog exposure may modify the genetic effect of rs10214237 on AE via the IL-7 receptor, supporting observational epidemiology showing a protective effect for dog ownership.




We’re seeking applications from dermatology residents across the country to propose innovative projects to address care gaps within common skin diseases in underrepresented populations, including Canadians with deeper skin tones, Indigenous people and other racialized groups.
The Skin Spectrum Summit, in partnership with Pfizer, will provide scholarship funds to support the development and implementation of your initiative.


Continued from page 1
“These treatments have been available in adult dermatology but are new in pediatric dermatology,” said Dr. Safoine.
Options in seborrheic dermatitis, AD, and alopecia areata
Roflumilast, which was already approved for the management of plaque psoriasis and inverse psoriasis in children aged 12 years and older, is now available for children aged nine and older with seborrheic dermatitis, based on data from a clinical trial of 457 patients, including those aged less than 18 years. “The study found 80 per cent of subjects had a significant improvement, and the adverse events were minimal,” said Dr. Safoine.
Only about one per cent of subjects in the STRATUM clinical trial experienced adverse events, with those adverse events being nausea, nasopharyngitis, and headaches.
Injectable lebrikizumab, which targets IL13, offers another choice in the management of atopic dermatitis (AD), said Dr. Safoine, noting the key clinical trials involving lebrikizumab had about 10 per cent of patients aged less than 18 years. More than half of patients in two different trials were able to experience at least 75 per cent improvement in lesion extent and severity (EASI-75) with lebrikizumab monotherapy, and the toxicity profile demonstrated less severe conjunctivitis than other injectable treatments.
“There appears to be a little less conjunctivitis than with dupilumab, but more than with tralokinumab,” said Dr. Safoine. “Real-world data will tell us more.”
There are emerging data suggesting the IL4Ra inhibitor dupilumab can offer value in treating alopecia areata when the condition is co-occurring with AD, pointed out Dr. Safoine.
“There are several case reports showing a benefit of dupilumab in alopecia areata,” said Dr.
“I t’s interesting to have a topical therapy available [for vitiligo]...one of the advantages is that it does not produce any systemic side effects.”
Dr. Meryem Safoine
Safoine, noting that Th2 pathway hyperactivity is also involved in the pathogenesis of AA.
Versatility of ruxolitinib
Still another AD treatment that also offers benefit in vitiligo, a condition for which no on-label treatment had been available, is the topical Janus kinase (JAK) inhibitor ruxolitinib. “The topical therapy [ruxolitinib] is approved in both AD and vitiligo,” said Dr. Safoine.
Data from TRuE-V1 and TRuE-V2, two randomized, placebo-controlled, double-blind studies that included 674 patients in total and 72 patients aged less than 18 years, pointed to an improvement of at least 75% in the Facial Vitiligo Area Scoring Index (F-VASI75) at 24 weeks.
“It’s interesting to have a topical therapy available [for vitiligo],” said Dr. Safoine, noting a topical treatment is attractive from a tolerability standpoint. “One of the advantages is that it does not produce any systemic side effects.”
Non-systemic adverse events such as pruritus at the site of application, and acne at the site of application were observed in the trials.
JAK inhibitor for hidradenitis suppurativa (HS) The Step-Up HS trial is exploring the benefit of the JAK inhibitor upadacitinib in adults and in patients aged 12 and older. A total of 38% of patients with HS who were taking upadacitinib compared to 24% of patients on placebo had a
Continued from page 3
significant impact on atopic dermatitis and vitiligo (see page 1).
For the treatment of hand eczema—which is a significant clinical challenge—Dr. Ben Barankin comments on how delgocitinib out-performs our best oral systemic treatment the retinoid alitretinoin.
On the melanoma front we see that melanoma continues to increase significantly, not only in the Caucasian populations but in Indigenous populations as well, as presented by Dr. Monique McKenzie during the 1st Indigenous Skin Spectrum Global Summit in Montreal. A dermatologist in New Zealand, she describes the 156% excess mortality rate in the Māori population in that country. Many other factors contribute to this terrible mortality, which makes this another article worth reviewing (see page 1).
In our fourth 30@30 feature celebrating the 30th anniversary of this newsmagazine, the transformative role of teledermatology is explored. Drs. Anna Chacon, Rachel Asiniwasis, Dr. Elena Netchiporouk, and Jaggi Rao describe how they implement teledermatology into their daily practice (see page 14). Dr. Rao, creator of DermConsult, Canada’s largest dermatology service, describes his many years and the number of significant advancements over the past 30 years. Other important 30@30 ranked developments include the role of microbiome research in dermatology, the role of nanotechnology in skin care, and their impact on advances in dermatology.
As always, THE CHRONICLE team invites and welcomes your comments on this issue, or any other topic in dermatology, at www.derm.city —Wayne P. Gulliver, MD, FRCPC, Medical Editor
clinical response, defined as a decrease of at least 50 per cent in the number of nodules and abscesses.
“We are always happy to see when there might be new treatments [for HS],” said Dr. Safoine. “Phase 2 data are promising, and there is a phase 3 study underway. There will likely be a new indication for upadacitinib [this year].”
Emerging treatment for molluscum contagiosum
The approval of berdazimer, a topical gel, by the U.S. FDA for the treatment of molluscum contagiosum in patients at least one year old represents another management choice for the skin infection, said Dr. Safoine. “The gel releases nitric oxide, which has antiviral properties.”
In clinical research, nearly half of patients (48.5%) treated with berdazimer topical gel each day had at least 75 per cent of their lesions resolved at 12 weeks. “A total of 30 per cent of subjects had complete resolution at 12 weeks,” said Dr. Safoine.
Trial data found that there were adverse events at the site of application including pain, erythema, pruritus, and dermatitis.
Integrating artificial intelligence (AI)
AI will not replace pediatric dermatologists, and AI tools are only as good as the information supplied to the tools, according to Dr. Safoine. “The AI tools need to be given good information,” she said.
It should be standard practice to confirm the information that AI tools such as ChatGPT generate, she added. “It is important to verify the references ChatGPT provides,” said Dr. Safoine. “Do not accept ChatGPT’s answers as facts.
One of the chief concerns in using AI innovations in medicine is privacy and the protection of patient information, stressed Dr. Safoine. “Do not enter confidential information into an AI tool that does not meet the required security standards,” she said Ultimately, AI tools will not replace dermatologists, but dermatologists need to use AI tools as adjuncts in their work. “We have to integrate AI into our practice,” said Dr. Safoine.
Non-proprietary and brand names of therapies: roflumilast (Zoryve, Arcutis); lebrikizumab (Ebglyss, Lilly); tralokinumab (Adtralza, LEO Pharma); dupilumab (Dupixent, Sanofi/Regeneron); ritlecitinib (LITFULO, Pfizer); ruxolitinib cream 1.5% (OPZELURA, Incyte); upadacitinib (Rinvoq, AbbVie); berdazimer topical gel (Zelsuvmi, Ligand Pharmaceuticals).
Always ready when you are, wherever you are
Chronicle's digital audio, e-newsletters, and web portal keep physicians updated reliably 24/7. Each is worthy of your time. And they're available without charge. Find them all at https://linktr.ee/dermcity

Since 2015, derm.city has been a leading hub and repository for dermatology information and interactive knowledge-exchange in video, text, images, and audio. It's the official site of The Chronicle of Skin & Allergy, now newly enhanced with added useful features. Thrice weekly updates on the latest findings in dermatology, summarized for quick learning. Visit derm.city at https://derm.city www.derm.city
A dermatology newsletter focused on ethnodermatology care from top physicians in the field, delivered to your inbox every Monday.
Supported by Bausch Health Canada


A biweekly newsletter on clinical and social issues affecting female patients and physicians, delivered straight to your inbox.
Supported by Galderma Canada
Dr. Geeta Yadav and expert dermatologists discuss clinical developments, news, trends and myths in acne treatment and research. First season of three episodes now available for listening and downloading.
Supported by Cipher Pharmaceuticals

a skin spectrum podcast

Dr. Neil Shear, dermatologist and Professor Emeritus at the University of Toronto, speaks with many guests from the world of dermatology, including Dr. Boluwaji Ogunyemi, Dr. Marc Bourcier, and Dr. Rachel Asiniwasis, to hear their stories and insights.
Dr. Ron Vender delves into recent psoriasis studies and comments articles about the efficacy of PASI scores, intermittent fasting for psoriasis, and biologic fatigue.
Supported by Sun Pharma Canada

Chronicle Podcast System • www.chronicle.ca "Ideas in the Service of Medicine"



The past three decades have seen teledermatology blossom into a global standard of care, revolutionizing access, outcomes, and the patient experience.
In the 1990s, the “store-and-forward” (S&F) model—where clinicians capture and transmit digital images and patient information for later review—emerged as a practical solution for remote dermatologic assessment. By the early 2000s, “real-time” (RT) teledermatology, using live video conferencing, brought synchronous, interactive consultations into daily practice (J Telemed Telecare 2022; 28(3):177-181). These modalities have been rigorously studied, with diagnostic concordance rates between teledermatology and in-person visits consistently surpassing 85% (Arch Dermatol 2012; 148(1):61-65; JAMA Dermatol March 1, 2017; 153(3):319-332).
Perhaps the most profound change has been in access to care. Teledermatology has bridged the gap for rural and underserved populations, reducing travel, wait times, and costs. A 2017 systematic review of teledermatology in skin cancer found between 49% and 97% of patients in reviewed studies did not require an in-person visit after teledermatology assessment, (JAMA Dermatol 2017; 153(3):319-327). During the Covid-19 pandemic, teledermatology proved indispensable, maintaining continuity of care when traditional clinics were shuttered (JMIR Dermatol May 5, 2021; 4(1):e25999).
The impact on patient outcomes is clear. One study found live interactive teledermatology led to changes in diagnosis in 70% of cases and management in 98%, with nearly 70% of patients showing clinical improvement (Arch Dermatol 2012; 148(1):61-65). Patient satisfaction has remained high, with multiple studies reporting rates above 85%, driven by convenience, speed, and reduced travel (J Am Acad Dermatol 2011; 64(4):759-772).
The past decade has seen the development of consensus guidelines from organizations like the American Telemedicine Association, ensuring quality and safety in teledermatology practice (JMIR Dermatol May 15, 2023; 6:e46121). Meanwhile, artificial intelligence and mobile applications are beginning to assist with triage and diagnosis for conditions such as skin cancer, promising even greater accessibility and early detection (Public Health Res Pract March 10, 2022; 32(1):3212204).
Teledermatology’s journey over the past 30 years is a testament to the power of innovation in medicine. As digital tools continue to evolve, teledermatology is poised to further democratize access, improve outcomes, and redefine the patient experience for decades to come.
THE CHRONICLE OF SKIN & ALLERGY, Canada’s premier clinical news magazine in the specialty of dermatology, is celebrating its 30th anniversary in 2025. In all eight issues of THE CHRONICLE in 2025, this feature will count down the 30 key innovations, breakthroughs, and coursechanging discoveries and events that have dramatically changed the specialty and the patient experience during the years 1995 to 2025.
Through a comprehensive survey on derm.city and via e-mail outreach to readers of Skin Spectrum Weekly, key opinion leaders and healthcare practitioners weighed in on the most impactful innovations in dermatology over the past three decades. These responses were collated to create a list of innovations based on perceived impact on patient outcomes and accessibility to medical care.
In 1995, treatments for psoriasis were limited, acne scars were permanent, and early detection of skin cancer relied primarily on visual clinical examination. Fast forward to today's groundbreaking therapies, cutting-edge technologies, and revolutionary approaches that have transformed the specialty of dermatology.
These advances are a testament to the continuous pursuit of research and innovation that have reshaped the lives of millions of dermatology patients. From the labs of researchers to the clinics of dedicated practitioners, these breakthroughs have not only advanced the understanding of skin health but also redefined patient care and outcomes.
This is the story of your specialty. As the top developments are counted down issue by issue, let’s imagine the possibilities that lie ahead in the evolving world of dermatology.






“Telemedicine and teledermatology are revolutionizing healthcare by breaking down geographical barriers, providing timely access to specialized care, and empowering patients with convenient, personalized dermatological solutions from the comfort of their own homes.”
—Dr. Anna Chacon, dermatologist from Miami

“Given that Canada is one of the world’s largest landmasses, this creates inherent inequities in specialist access, which is largely urban-based. At Origins Dermatology Centre in Regina, we provide a multidisciplinary model combining in-person and VC to serve highly ruralized and remote populations inherent to the Midwest. Furthermore, many of our patients are Indigenous, who are disproportionately more likely to live outside of urban areas. From our experience, a combined model of in-person and VC, tailored to each patient’s needs and circumstances, has shown to be the most efficient, accessible, and personalized approach.”
—Dr. Rachel Asiniwasis, Founder and Director, Origins Dermatology Centre, Regina.

“Teledermatology has revolutionized care delivery, particularly for patients in rural or underserved areas. In our onco-genodermatology clinic, we routinely follow up with patients living more than 100 km away to deliver genetic test results, provide genetic counselling, and initiate personalized cancer screening—all through secure telehealth platforms. For conditions such as severe cicatricial acne, rosacea, psoriasis, atopic dermatitis, chronic urticaria where diagnosis and management can be effectively guided by high-quality images and patient history, teledermatology has minimized travel burdens and streamlined care. That said, in my view, it cannot replace in-

person visits for patients with suspected or confirmed skin cancer, where total body skin exams and dermoscopic evaluation are essential for optimal care.”
—Dr. Elena Netchiporouk, Assistant Professor in the Department of Medicine at McGill University, Canadian Dermatology Association Regional Director for Quebec, 2024-2027
“Telehealth, particularly storeand-forward teledermatology, is a game-changing service for healthcare. Given that dermatology is a visual specialty, where background history can often be succinct and easily communicated, remote diagnosis is readily possible and subsequent therapeutic strategies can be implemented in a timely manner and over great distances. Particularly in Canada, where the geography is vast and skin specialists are relatively few, teledermatology has demonstrated success in the diagnosis and management of a variety of skin problems.”
—Dr. Jaggi Rao, Edmonton-based dermatologist, creator of ConsultDERM, Canada’s largest teledermatology service

Over the past 30 years, wound healing in dermatology has undergone a significant shift, driven by innovations that have markedly improved clinical outcomes, patient comfort, and quality of life. The move from traditional dry dressings to advanced moist wound care has accelerated healing and reduced infection rates, while negative pressure wound therapy has enabled the management of complex wounds previously considered inoperable, resulting in higher limb salvage and improved cosmesis. Bioengineered skin substitutes have expanded therapeutic options for chronic wounds and burns, offering functional and aesthetic benefits, especially in pediatric and high-risk populations (Plast Surg Int March 22, 2012; 190436, Int Wound J May 12, 2004; 1(1):59–77).
Biologically active dressings and growth factor therapies target the molecular drivers of wound repair, accelerating closure and reducing scarring in difficult-to-heal wounds. Stem cell therapies and 3D bioprinting represent the forefront of regenerative medicine, enabling personalized, high-quality tissue reconstruction with promising early results. Nanotherapeutics and smart dressings are ushering in an era of precision wound care, allowing for targeted drug delivery, real-time monitoring, and adaptive therapy.
Adjunctive modalities, including platelet-rich plasma, cold plasma, laser, cryosurgery, and maggot therapy, further enhance
Here are the 30 most significant clinical developments of the past 30 years, as selected by readers of The Chronicle of Skin & Allergy
the therapeutic arsenal, addressing specific challenges in chronic and complex wounds (Cells Aug. 6, 2022; 11(15):2439, Int Wound J May 12, 2004; 1(1):59–77, Sci Adv May 19, 2023; 9(20):eade7007, Clin Exp Dermatol March 21, 2024; 49(4):325-336, Front Immunol May 21, 2024; 15:1395479).
Dermatology has witnessed transformative advances in microbiome research and management. The introduction of high-throughput sequencing technologies has allowed for detailed mapping of the skin’s microbial landscape, uncovering the diversity and stability of individual microbiomes and their roles in health and disease (Clin Cosmet Investig Dermatol Aug. 10, 2023; 16:2153-2173, J Clin Invest Feb. 3, 2025; 135(3):e184315). This foundational knowledge has catalyzed the development of microbiome-based therapeutics, including live biotherapeutic products designed to restore microbial balance and directly inhibit pathogenic bacteria. Clinical trials have demonstrated that introducing beneficial commensal strains can reduce colonization by pathogens such as Staphylococcus aureus, leading to improved outcomes in conditions such as atopic dermatitis and acne (Exp Dermatol Dec. 2024; 33(12):e70019).
Topical and oral probiotics, as well as prebiotic-enriched moisturizers, have emerged as adjuncts in the management of inflammatory skin diseases, supporting barrier function and enhancing microbial diversity (J Eur Acad Dermatol Venereol Oct. 13, 2016; 30(12):2038–2047, Pharmaceutics March 3, 2022; 14(3):557). The recognition of the gut-skin axis has further broadened therapeutic strategies, with systemic modulation of the gut microbiome showing promise in conditions such as rosacea and atopic dermatitis (Microorganisms Nov. 11, 2019; 7(11):550).


Over the past three decades, nanotechnology has driven innovation in both medical and cosmetic practice. The introduction of nanocarriers—such as liposomes, solid lipid nanoparticles, and nanostructured lipid carriers—has improved drug delivery by enabling precise targeting and sustained release of therapeutics for conditions including psoriasis, acne, vitiligo, and melanoma. These advances have led to improved treatment efficacy, reduced side effects, and greater patient adherence due to less frequent dosing and enhanced tolerability (Int J Mol Sci Dec. 15, 2022; 23(24):15980).
Nanoparticle-based sunscreens, particularly those utilizing zinc oxide and titanium dioxide, offer broad-spectrum protection against both UVA and UVB radiation with improve cosmetic appearance (Nanotechnol Sci Appl Oct. 13, 2011; 4:95–112). In the realm of anti-aging and cosmeceuticals, nanotechnology has enabled the delivery of active ingredients deep into the skin, enhancing outcomes in wrinkle reduction, hydration, and skin firmness (Advances in Nanoparticles Feb. 2020; 9:1-22).
Wound healing has also benefited significantly from nanotechnology. Dressings and creams containing silver and gold nanoparticles have demonstrated accelerated healing, reduced inflammation, and improved antimicrobial protection, especially in chronic and hard-to-treat wounds (J Invest Dermatol Jan. 5, 2012; 132(3):964–975). Nanotechnology has paved the way for personalized, non-invasive therapies, including advanced diagnostic tools and vaccine delivery systems, marking a shift toward individualized patient care (Gels March 10, 2022; 8(3):173).
Continued from page 1
sponse,” said Dr. Martinka. “They are pills that patients take every day, and they have helped change the landscape of treating atopic dermatitis, and have been a tremendous tool in our tool kit for treating atopic dermatitis.”
The topical JAK ruxolitinib, which has been available in Canada for about six months, has demonstrated benefit in the management of mild-to-moderate AD and may control disease so that it will not progress to a more advanced state, Dr. Martinka added.
“Before, such patients would be using a highpotency topical steroid and then you may be cycling these patients between steroids and non-steroidal drugs,” said Dr. Martinka. “This [topical ruxolitinib] may actually reduce the number of patients that move on to systemic therapy.”
Treating chronic hand dermatitis
A prospect in the management of chronic hand dermatitis or chronic hand eczema is the impending availability of the topical JAK inhibitor delgocitinib.
“We will have a cream that beats our best systemic therapy [oral alitretinoin],” said Dr. Benjamin Barankin, dermatologist and co-founder of the Toronto Dermatology Centre. “As a topical therapy, it is a targeted treatment. You are getting an effect where it [the cream] is applied, compared to a pill, which does not provide a localized effect.”
Data from the Phase III head-to-head DELA FORCE trial concluded that delgocitinib was more effective and better tolerated compared to oral alitretinoin among adult patients with severe chronic hand dermatitis. The topical therapy showed a significantly greater decrease in Hand Eczema Severity Index (HECSI) scores at week 12 ( 67.6) compared to alitretinoin ( 51.5), with a treatment difference of 16.1 points, a difference that was highly statistically significant.
Feras Ghazawi, MD, PhD, a dermatologist in Ottawa, noted the indication for delgocitinib is specific and suggested it will be highly useful in the treatment of chronic hand dermatitis. “I really think it could become a valuable option for patients who need effective, steroid-sparing treat-
ments,” said Dr. Ghazawi, but added that longterm data are needed to support its efficacy and safety.
Alopecia areata and vitiligo respond to JAKs JAKs such as baricitinib and ritlecitinib, which have been available for the treatment of alopecia areata, are producing hair regrowth in patients



with severe disease, according to Dr. O’Toole.
“I think the response varies,” she said. “I have seen people who, within a couple of weeks, start to have fine, baby hairs return. It can sometimes take three months or six months [to see regrowth of hair], but it can take longer. I have seen that in real-life practice and in clinical trials. I think the message for prescribers is not to give up early, have that patience, and give them [systemic JAK treatments] time to respond.”
Dr. Martinka agreed that response of systemic JAK inhibitors to treat alopecia areata is not as quick as response to systemic JAK inhibitors to treat AD.
“It does take a little bit longer to start seeing those effects [in a patient with alopecia areata], in comparison to an atopic dermatitis patient who may see improvement of symptoms like their itch within one day of taking oral JAK inhibitors,” said Dr. Martinka. “Patients [with alopecia areata] on those medications are seeing good regrowth of their hair.”
Repigmentation of the skin in patients with vitiligo does not happen quickly with use of topical ruxolitinib, but the availability in Canada of the topical JAK inhibitor for the chronic condition is a welcome alternative to treatments such as topical steroids, according to Dr. Barankin.
“A lot of our patients [with vitiligo] are excited

that we finally have something for them,” said Dr. Barankin. “We do not have to worry about steroid atrophy as a side effect or worry about our patients having steroid phobia. Our patients generally prefer topical treatment over systemic therapy. It’s early days, but to be able to get a reasonable response with a very safe product is great.”
Minimize risk of infection with JAKs
Because of the risk of infection with the use of JAK inhibitors, clinicians make efforts to ensure that patients are up-to-date with their vaccinations, noted Dr. Barankin.
“It is recommended that patients have all their vaccinations before they start [on a JAK inhibitor], in particular vaccination to protect against varicella zoster,” said Dr. Barankin.
Dr. Ghazawi also reinforced the importance of immunization as well as screening for infectious conditions for patients who are starting on JAK inhibitors.
“Infection risk appears to be low overall, but it is something we still have to monitor closely,” said Dr. Ghazawi. “This is why we screen for TB [tuberculosis], hepatitis B, and hepatitis C. We counsel patients on the use of herpes zoster vaccination before we start JAK inhibitor treatment. I would say good clinical judgment and patient selection are key to minimizing infectious complications.”
There is no doubt that JAK inhibitors have a far-reaching influence on numerous conditions that stems from their interplay with the immune system, added Dr. Ghazawi.
“JAK inhibitors interfere with multiple cytokine pathways, specifically the JAK-STAT pathway,” Dr. Ghazawi said. “These pathways are involved in inflammation and barrier function. They have broad utility across inflammatory conditions, and that is why we often see fast symptom control.”
Non-proprietary and brand names of therapies: upadacitinib (Rinvoq, AbbVie); abrocitinib (Cibinqo, Pfizer); ruxolitinib cream 1.5% (Opzelura, Incyte Biosciences); delgocitinib (not approved in Canada); alitretinoin (Toctino, GSK); baricitinib (Olumiant, Lilly); ritlecitinib (LITFULO, Pfizer).









The Chronicle of Skin & Allergy, in partnership with the Dermatology Industry Taskforce on Inclusion, Diversity and Equity (DiTiDE), sponsored a short essay competition for Canadian dermatology residents in 2024.
This contest was open to any resident enrolled in a dermatology training program at a Canadian medical school, with enrolment confirmed by their Program Director. Entrants submitted a 350- to 500-word composition reflecting on matters relating to inclusion, diversity, and equity. Three winners were announced
The selected essays will be published in each issue of The Chronicle during 2025.
Ahmad AlAbdulkareem, MD, MSc of McGill University was recognized for his essay “The hidden wound in surgical dermatology ”.
DiTiDE is a volunteer working group composed of Canadian life sciences managers and executives, dermatologists, patient association leaders, and allied parties committed to improving the patient experience and outcomes of under-represented skin types and underserved ethnicities through developing physician education and resources.
The 4th annual short-essay competition for Canadian dermatology residents is now open for entries. Details are available at http://derm.city/for-residents.
The power of colour, as a means of communication, a vessel of health, and a portrayal of everything that we are, cannot be overstated, not least to the potential readers of this piece. Indeed, in my own mother tongue’s dialectal way of polite informal greeting, the colloquial phrasing literally translates to “What’s your colour?” Historically, albeit darkly, it references the cutaneous cyanosis heralding pre-terminal hypoxia seen during a 17th-century plague epidemic.
Dermatology is uniquely colourful, and by extension, its best practice is inherently dependent on acknowledging and understanding the diversity of its patients and their needs. Despite the well-intentioned aspiration for medicine to be colour-blind, the obligatory ethical duty is to confront and rectify deep-rooted systemic shortcomings, historical and contemporary, to achieve equitable care for all.
Much like general dermatology, the underrepresentation of darker skin complexions in surgical dermatology, in patients and dermatologists alike, is alarming. Concerns about inadequate resources for patients, students, and residents are well-known. Surgical dermatology is also susceptible to a unique set of challenges; not only are darker tones underrepresented, but the clinical course itself, from indications to outcomes, is notably different. Additionally, the media absence of surgical dermatology in darker skin, at least compared to general dermatology, may undermine this population’s awareness of the subspecialty, and worse, further contribute to their alienation.
Raised in Kuwait, educated in Ireland and the U.K., and starting dermatology residency in Canada, I have been privileged to observe surgical dermatology in diverse demographics. In darker skin, I found surgical interventions for inflammatory dermatoses and dyspigmentation to far outnumber those for tumours and growths. Skin phenotype may explain some of the discrepancy, but this also raises issues about the adequacy of training and/or exposure. It also underlines a potential mismatch when defining successful outcomes, especially if dyspigmentation or abnormal healing is either a pathologic or an iatrogenic feature. This is complicated by how Canadian provincial health insurance plans largely deem both concerns to be merely aesthetic, disregarding true biological predisposition and exemplifying the harm of colour-blind medicine. Additionally, the lack of representative visual content can translate into insufficient explanation and suboptimal consent.
These observations, compounded by an already overstretched workforce grappling with oncology-heavy and aging demographics-driven waitlists, may hinder accessibility, amplifying enduring health equity gaps.
It is easier to highlight deficiencies; yet, celebrating successes is equally important. There has been an encouraging trend toward rightfully abandoning colour-blind dermatology. Concerted reforms such as diversity-focused meetings, workshops, educational content, outreach and mentorship programs, and literature revisions collectively aim to enshrine diversity, promote inclusivity, and help uproot entrenched racial disparities.
Despite the evident necessity of corrective measures, it was unfortunate that they were recently questioned and politicized by some regional peers, with attempts, using colour-blind rhetoric, to sunset these programs, arguing they result in further “othering” patients of colour. The onus is therefore on us to fortify our commitment to resolutely eradicate implicit bias, passive racism, and historical injustices, and to candidly address unresolved tensions within the profession; such wounds dermatology cannot heal by secondary intent.
Dr. Ahmad AlAbdulkareem graduated from the Schools of Medicine at the Royal College of Surgeons in Ireland, and at Cardiff University where he earned a master’s degree in clinical dermatology with a dissertation focus on keratinocyte carcinomas. He then completed his internship with the Ministry of Health in Kuwait before joining the dermatology program at McGill University.


Seyedeh Hoda Qoreishi,1 Nasim Gholizadeh,2 Ghasem R
ahmatpour Rok ni,2 Mahsa Babaei,2,*
1School of Medicine, Islamic Azad University, Tonekabon, Iran
2Department of Dermatology, Mazandaran University of Medical Sciences, Sari, Iran
* Correspondence: Mahsa Babaei (mahbabaei95@gmail.com; mahsa.babaei@stanford.edu)
Keywords: acne vulgaris, scar, therapeutics
ABSTRACT
Background: Acne‐induced scarring remains a formidable challenge, compelling patients to explore surgical interventions. This study aims to delve into and showcase recent strides in acne scar treatment, with a specific focus on innovative therapies.
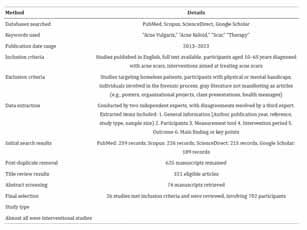
Methods: Conducting a narrative review spanning studies from 2013 to 2023, this paper provides a general overview of interventions. The review included English‐language studies with full‐text availability. Rigorous data screening and extraction by two independent authors covered diverse facets, including study particulars, participant profiles, measurement tools, intervention durations, outcomes, and key findings. The initial search was performed within PubMed, Scopus, Google Scholar, and the gray literature.
Results: Ultimately, 26 studies meeting inclusion criteria were included and reviewed for final analysis.
Conclusions: Recognizing the varied nature of acne scars, this narrative review underscores the need for personalized treatment strategies, considering scar type and severity. The study also emphasizes the potential necessity of combining treatments for optimal results. Despite substantial progress, ongoing research and more extensive studies are imperative to continually refine acne scar treatment outcomes, ultimately enhancing the well‐being of those affected by this condition.
INTRODUCTION
Acne vulgaris is a persistent inflammatory skin condition that may lead to enduring post‐inflammatory scarring.1 A recent 2023 study revealed that 47% of participants diagnosed with acne experienced the consequences of acne scars.2
Severe acne lesions can result in permanent scars, causing psychological distress.3 The extent and severity of scarring in acne are greater when treatment is delayed.4 Acne scarring can be categorized into two main types. The first involves increased tissue formation, including hypertrophic and keloid scars. The second, more common type involves tissue loss and includes ice pick, rolling, and boxcar‐type scars.5
Treating acne scars is a complex process due to numerous variables that must be considered. Different scar morphologies are among the primary factors influencing the treatment approach.6 The degree of scarring is cru-
cial in determining the appropriate treatment approach, with severe scarring requiring different strategies than mild scarring.7
The treatment of acne scars remains a controversial topic, with an increasing demand from patients for a less invasive approach with consistent efficacy and fewer side effects.8 Several studies have demonstrated that treatments, including micro needling and laser procedures, have shown beneficial results in patients with acne scars.9,10 Despite recent advances in treatment technologies, comprehensive studies have not fully caught up with the current knowledge and practices in many centers. In this study, our focus was on advancements in acne scar treatment and the exploration of novel therapies in research.
Search strategy
The search was performed within the following databases: PubMed, Scopus,
and ScienceDirect, and articles published between 2013 and 2023 were included. To mitigate the occurrence of missing data, a search was conducted on Google Scholar using the keywords “Acne Vulgaris,” “Acne Keloid,” “Scar,” and “Therapy.”
The inclusion criteria comprised studies published in English with full text available, involving participants aged 10 to 65 years diagnosed with acne scars at any stage of the disease. Included interventions were those aimed at treating acne scars. However, studies with interventions specifically targeting homeless patients, participants with physical or mental handicaps, and individuals involved in the forensic process were excluded. Grey literature that did not manifest as articles, such as posters, organizational projects, class presentations, health messages, and similar literature, did not meet the eligibility criteria.
Data extraction
To identify eligible studies, two independent experts assessed titles and abstracts from databases and additional sources. Subsequently, the same two experts reviewed the retrieved full texts. Any disagreements were resolved through consultation with a third expert. In cases where data were unavailable, requests were made to the study authors. Two experts were tasked with the data extraction process for the retrieved studies. The following items were extracted:
1. General information (Author, publication year, reference, study type, sample size)
2. Participants
3. Measurement tool
4. Intervention period
5.Outcome
6. Main finding or key points
7. A summary of methods and results is presented in Table 1.
The initial search generated 259 records from PubMed, 226 from Scopus, and 215 from the ScienceDirect databases. Additionally, 189 articles were identified through Google Scholar. After eliminating duplicates, 625 manuscripts remained. Through title review, the pool of eligible articles was narrowed down to 321. Subsequent abstract screening
resulted in retrieving 74 manuscripts. The primary objective of the study was to select research focusing on various treatment methods for acne scarring, leading to a substantial reduction in eligible articles. Ultimately, 26 studies met the inclusion criteria and underwent review. Table 1 illustrates the study selection process. Almost all studies were interventional, encompassing a total of 702 participants in this comprehensive literature review. Further details and key findings are presented in Tables 2 and 3.
The treatment of acne scars involves the use of a variety of methods, each chosen depending on the type of scar to be treated.
The integration of lasers, light‐based technologies, and energy‐based approaches has become essential in the field of acne and acne scar treatments. This encompasses a diverse range of lasers, including those using infrared wavelengths and pulsed dye lasers (PDLs), as well as light devices such as blue light, red light, and broadband light.10 The management of acne scars utilizes different types of lasers, which can be classified as either ablative or non‐ablative. Ablative lasers, including the carbon dioxide laser and Erbium YAG laser, work by focusing on water absorption to vaporize and eliminate damaged scar tissue. On the other hand, non‐ablative lasers, such as NdYAG and Diode lasers, stimulate dermal fibroblasts to encourage the generation of new collagen. An example of a non‐ablative laser system used in this context is the 675‐nm RedTouch laser from Deka Me.La, Italy.14,24,34 In a study, researchers found that Fractional CO2 (FX CO2) laser resurfacing is effective in enhancing atrophic acne scars. Significant improvements were observed in acne scar atrophy both one month and six months after the procedure, regardless of the treatment interval. The interval between treatments did not impact the degree of improvement in scar atrophy, patient satisfaction, or the occurrence of postoperative adverse effects.34
Recent clinical perspective emphasizes integrating lasers, light‐based, and energy‐based technologies in treating acne and acne scars. Both ablative (e.g.,
Reprinted with permission © 2025 The Author(s). Journal of Cosmetic Dermatology published by Wiley Periodicals LLC. This is an open access article distributed under the terms of the Creative Commons Attribution Licence CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Content has been edited to conform with the Canadian Press Publication Style Guide Chronicle.Academy develops bespoke structured learning programs for clinicians providing in-depth education to professionals in the healthcare industry.

CO2, Erbium YAG) and non‐ablative lasers (e.g., NdYAG, Diode) effectively enhance scar appearance, with FX CO2 laser resurfacing showing significant, consistent improvements in atrophic acne scars. A great piece of literature approves the efficacy and safety of laser treatments for acne scars; however, side effects including risk of skin infection, inflammation, hypersensitivity reactions, and keloids have been associated with this treatment method.24
Microneedling is a technique that utilizes fine needles to create numerous tiny holes in the skin. These minuscule punctures, made by the micro‐pen machine, stimulate the skin's natural regenerative process, leading to the production of collagen and elastin.9 Consequently, this method effectively improves wrinkles, fine lines, pimples, wounds, and pores. However, a significant issue with microneedling is that clinical outcomes often depend on subjective assessments by physicians and/or volunteers. Furthermore, the histopathological responses following microneedling treatment are relatively limited.19 Microneedling effectively treats wrinkles, fine lines, and scars by stimulating collagen production, though outcomes often rely on subjective assessments, which typically involve physicians or volunteers evaluating the improvement in skin appearance, such as reduction in wrinkles, fine lines, and scars, based on personal judgment rather than objective measurements.
A commonly employed method for treating acne and acne scars is chemical peeling. This procedure involves the controlled removal of superficial skin lesions by exfoliating and eliminating a portion or the entire epidermis, with or without the dermis.26 The process stimulates the regeneration of new epidermal and dermal tissues. Various peeling agents are available, with the most popular ones being salicylic acid, glycolic
acid, pyruvic acid, lactic acid, mandelic acid, Jessner solution, trichloroacetic acid, and phenol. Each of these agents has unique characteristics and indications for treating various skin conditions and types of scars.9,35
A specific study demonstrated the effectiveness of a trichloroacetic acid superficial peel followed by manual dermasanding in separate sessions for treating mild and moderate acne scars. The improvement became more significant with repeated dermasanding sessions.26 The patient's skin type, acne activity, and the type of acne scarring all influence the choice of the best chemical peel. Combination peels are frequently chosen because they help reduce the possibility of negative effects.36
Chemical peels can be used in conjunction with other procedures to treat acne scars and produce better clinical results.37 They work by removing the topmost layer of the skin, and by promoting skin renewal, they can help improve the appearance of mild to severe acne scars. However, it is worth noting that chemical peels may not significantly improve cases of more extensive scarring that extends deeper into the skin.36
The effectiveness of these methods in promoting skin renewal and improving scar appearance is of increasing importance in recent clinical practice. Various peeling agents, such as salicylic acid and trichloroacetic acid, are tailored to specific skin types and scar conditions.
Generally, glycolic acid provides effective superficial exfoliation and texture improvement but may not suffice for deeper scars and can irritate sensitive skin. Salicylic acid penetrates pores to combat active acne, although its drying effect can be a downside. Lactic acid is gentler and hydrating, making it suitable for sensitive skin, but may also deliver slower results. Medium‐depth peels, like trichloroacetic acid and Jessner's solution, can significantly enhance skin texture but come with downtime
and potential risks of irritation and hyperpigmentation. For deep scars, phenol peels offer profound and long‐lasting effects, though they require extensive recovery time and can lead to complications. Retinoids, while effective for both acne and scarring, demand consistent use and sun protection, while enzyme peels provide gentle exfoliation with minimal downtime but may be less effective on deeper scars. Combining peels with other treatments enhances results, though deeper scars may need additional approaches.9,26,35,36,37
Dermal fillers have become essential in both medical and cosmetic dermatology. These fillers are categorized as temporary, semipermanent, and permanent.20 The first two classes are biodegradable and have varying half‐lives, while permanent fillers are non‐biodegradable. When using fillers, they prompt a distinctive response in the extracellular matrix (ECM), enabling the identification of different filler types through histopathological examination.38 The use of dermal fillers in the treatment of atrophic acne scars is supported by data from clinical research. These fillers include silicone, collagen, hyaluronic acid, polymethylmethacrylate (PMMA)‐collagen gel, polyacrylamide, poly‐L‐lactic acid (PLL), and calcium hydroxylapatite (CaHA). The tolerability and safety of dermal filler implantation are influenced by the filler's properties, the doctor's skill and knowledge, and the patient's unique traits. Dermal filler injections to improve acne scars entail a soft‐tissue augmentation procedure.39 Collagen synthesis is boosted by hyaluronic acid fillers (HAFs). However, semipermanent or biostimulatory fillers such as PLL and CaHA, as well as permanent fillers, are used to promote collagen formation more forcefully.20
These agents play a crucial role in soft‐tissue augmentation and collagen synthesis. Temporary, semipermanent, and permanent fillers like hyaluronic acid, PLL, and CaHA are used based on their properties and patient needs. Fillers improve atrophic acne scars, with safety and effectiveness depending on filler type, physician expertise, and patient characteristics.
Limited research indicates that PRP can be used as an adjuvant therapy for atrophic acne. Autologous PRP is obtained from the patient's blood and contains a concentrated number of platelets.19 PRP acts as a supplementary therapy for treating atrophic acne scars alongside main therapies, including microneedling, fractional carbon dioxide laser (FCL), and subcision.40 One study showed that autologous PRP can be introduced as a cost‐effective and
well‐tolerated office procedure for treating acne scars without significant side effects.41
The impact of PRP on the treatment of acne scars may be attributed to its ability to expedite the generation of hyaluronic acid.42 Hyaluronic acid draws water into its matrix, resulting in swelling, increased volume, improved skin turgor, and enhanced tissue lubrication.40 Additionally, native hyaluronic acid has been shown to promote cell proliferation, stimulate ECM synthesis, and regulate collagen fiber diameter, leading to improvement in atrophic scars.43
PRP is a promising adjuvant treatment, which enhances main therapies like microneedling and lasers by promoting hyaluronic acid generation, which improves skin volume and texture. PRP is cost‐effective, well‐tolerated, and boosts collagen synthesis, aiding in scar improvement. There is an ongoing interest in adopting this effective method for the treatment of various dermatologic disorders by dermatologists and patients.
S. Orentreich and N. Orentreich created subcutaneous incision‐less surgery, sometimes referred to as subcision, as a less invasive method to repair acne scars in 1995.44 The scar's fibrotic strands must be broken, and the epidermis must be separated from the underlying connective tissue. This procedure causes the growth of new connective tissue, elevation of the acne scars' recessed surface and enhances their appearance.42 Vempati, et al's retrospective analysis revealed that subcision was a successful method of treating atrophic acne scars. The research revealed four main subcision tool types: needles, cannulas, wires, and blunt‐blade instruments. These tools are widely used to treat atrophic acne scars. The depth of the scars, a person's preferences, and the particular mix of therapies being utilized are among the elements that influence the instrument selection.25
While needle‐based subcision using conventional hypodermic or Nokor needles has been effective, its utilization is limited due to various issues. These include the need for multiple insertion sites, discomfort for patients, potential damage to neurovascular structures, needlestick injuries, and bleeding.19 Additionally, one should take into account any post‐operative adverse effects such as bruising, hematoma, scarring, nodule formation, and post‐inflammatory hyper‐ or hypopigmentation.16 Various tools—needles, cannulas, wires, and blunt‐blade instruments—are used based on scar depth and patient needs. Despite its success, needle‐based subcision poses risks such as discomfort, neurovascular damage, and postoperative effects like
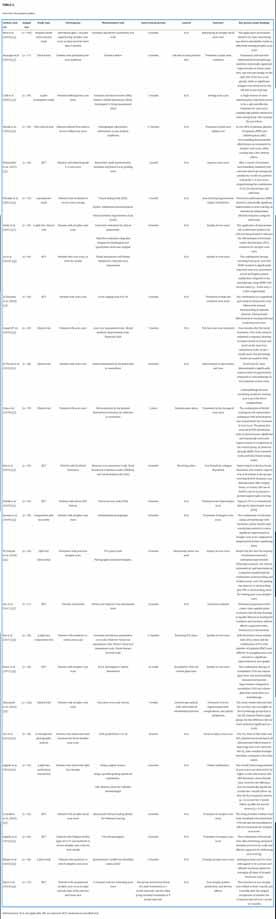
bruising and pigmentation changes.
microneedling (RFM)
RFM represents a significant advance in conventional radiofrequency (RF) devices when it comes to skin tightening, offering enhanced safety and efficacy. This technique enables efficient energy delivery into the dermis while causing minimal disruption to the epidermis, especially when using insulated needle devices.18
It involves a controlled skin injury that triggers the development of rejuvenated and healthy skin and benefits common skin problems, including acne scars and wrinkles. The use of devices that monitor tissue characteristics, including temperature and impedance, further contributes to optimizing patient outcomes and ensuring safety during the procedure.13
Given its benefits, RFM should be considered the new standard for treating acne scarring, particularly in individuals with darker skin types. Additionally, it is an effective minimally invasive solution for neck rejuvenation and treatment of skin laxity in this area.13,45 A study indicated that treating moderate and severe acne scars with microneedling and fractional RF is effective.30
RFM is considerably advanced over conventional RF devices in skin tightening, particularly for acne scars and wrinkles. RFM ensures efficient energy delivery with minimal epidermal disruption, especially with insulated needles. This technique promotes rejuvenated skin development and optimizes patient outcomes through tissue monitoring. RFM is especially recommended for treating acne scars in darker skin types and for neck rejuvenation, offering a minimally invasive solution for skin laxity. Studies confirm its effectiveness for moderate to severe acne scars.
Cryotherapy is a treatment method utilizing liquid nitrogen to freeze the affected area, causing the breakdown and destruction of scar tissue. It is a commonly used physical approach to treat acne and has been used for many decades. Research has been conducted on the use of contact cryotherapy for treating hypertrophic acne scars. Though the precise mechanism for scar reduction is still unknown, one idea contends that the physical harm brought on by freezing and thrombosis causes collagen to remodel, which improves the scars.5,46 The main disadvantage of cryotherapy is the formation of permanent light spots on the treated skin. Additionally, it is essential to recognize that cryotherapy may not be effective for all types of acne scars, as the most suitable treatment option depends on the specific type of acne scar.47
This method is associated with a long‐standing use and ongoing re -

search, particularly in treating hypertrophic scars. While its mechanism for scar reduction is not fully understood, it likely involves collagen remodeling due to freezing‐induced physical damage. However, the formation of permanent light spots is a notable disadvantage. Patient acceptance may vary due to the risk of side effects, while dermatologists may consider cryotherapy as one of several options depending on scar type and patient preference.
The use of 5‐FU for scar treatment was initially proposed by Fitzpatrick in 1999. Studies have confirmed that 5‐FU tattooing is more effective than intralesional corticosteroids alone. However, the most effective approach for scar treatment appears to be the combination of 5‐FU injections with intralesional corticosteroids and PDL treatments.14,22
Dermabrasion is a procedure involving manual sanding of the epidermis and upper dermis to remove them. It can be done using hydrogen peroxide and sandpaper to control bleeding, or with a rotating motorized handpiece equipped with various tools including serrated wheels, diamond‐embedded fraises, and wire brushes. The removal of superficial skin layers during this process promotes a smoother wound‐healing process and stimulates the formation of new collagen.48
Dermabrasion is a skin‐resurfacing technique aimed at enhancing the appearance of acne scars and other skin imperfections. This procedure employs a rapidly rotating device to eliminate the outer layer of the skin, facilitating the growth of smoother and rejuvenated skin.27 Dermabrasion can be performed as a standalone procedure or in combination with other cosmetic treatments. However, there is a rare risk of infection or scarring associated with dermabrasion. In cases where scarring occurs, steroid medications can be utilized to help minimize their appearance as a result of the dermabrasion procedure.48
Dermabrasion can be performed alone or in combination with other cosmetic procedures. However, there are risks of infection and scarring, albeit rare. Patient acceptance may vary due to these risks, while dermatologists consider dermabrasion a viable option for scar treatment, especially when combined with other modalities for enhanced results.
With their efficiency and low risk of side effects (AEs), silicone dressings offer a practical and efficient solution for treating hypertrophic acne scarring. These dressings are thin silicone gel or membrane sheets placed topically on acne scars.49 Their therapeutic impact is at-

tributed to the synergistic effect of pressure and moisture, inhibiting collagen formation by fibroblasts. The only negative effects linked to silicone dressings are localized skin maceration and pruritus (itching). Though silicone dressings are beneficial for various types of scars beyond hypertrophic acne scars, such as post‐surgical scars and burn scars, as they help flatten and soften scar tissue while promoting optimal healing in a hydrated environment. Additionally, they can improve scar colour and texture, reduce itchiness, and are suitable for sensitive skin, making them a versatile option in scar management. It is important to keep in mind that patient compliance may be a challenge, particularly when dressings must be applied to highly visible locations including the face. Some patients may choose to apply the dressings at night, but doing so may lessen their effectiveness.5,50 Using silicone dressings for hypertrophic acne scarring highlights their efficacy and low risk of side effects, primarily localized skin maceration and itching. Dermatologists generally accept silicone dressings as a practical and efficient treatment option, especially for less visible scars. However, patient compliance, particularly when applied to highly visible areas like the face, can pose challenges. Some patients may opt to apply dressings at night, potentially reducing their effectiveness.
Mesotherapy is a cosmetic procedure involving the injection of a blend of vitamins, minerals, and nutrients into the skin to rejuvenate and repair it, making it highly effective in treating acne scars and various skin issues. This treatment provides targeted wound repair and skin regeneration, making it suitable for all types of scars.51 Often combined with microneedling, creating tiny punctures in the skin to stimulate the body's natural healing process and enhance collagen and elastin production, mesotherapy further aids in reducing the appearance of acne scars.52 However, it is essential to consider that mesotherapy is not recommended for individuals with specific conditions, including active acne, eczema, psoriasis, or rosacea. Additionally, those prone to easy bruising or having blood disorders, HIV, herpes, chronic illnesses, or recent surgery within the past six months may not be suitable candidates for this treatment.53 However, patient acceptance may vary, as mesotherapy is not recommended for individuals with specific conditions like active acne or certain medical histories, which may limit candidacy.
Despite not being a new technique, carboxytherapy, which involves the controlled administration of CO2 in
popigmentation, dermal atrophy, and telangiectasia.5 In cases where corticosteroid treatment proves ineffective, other intralesional options such as 5‐fluorouracil, bleomycin, and verapamil have been used with positive outcomes. These agents work by inhibiting the proliferation of dermal fibroblasts.58
Punch methods are effective for treating cases of severe atrophic acne scarring, especially when other methods have not been very successful. The procedure involves a punch excision, where a circular incision is made approximately equal to the size of the scar. Depending on the case, the scar tissue may be removed and then sutured, replaced with a graft, or elevated to match the surrounding skin level using sutures or adhesive skin closure material.59,60 Punch techniques have been demonstrated to be successful, notably for treating ice‐pick scars, even if the success rates of this procedure are mostly based on case studies.5 The dangers of this strategy, meanwhile, include graft failure, graft depression, and the development of sinus tracts. But when done correctly, punching techniques present a viable approach to treating more severe atrophic acne scars.61
intradermal or subcutaneous doses, is increasingly gaining recognition among esthetic medicine doctors, dermatologists, and cosmetologists worldwide.21 Carboxytherapy shows promise as a valuable tool in the treatment of atrophic acne scars.54 In a study evaluating acne scar treatment, carboxytherapy and microneedling were compared; 32 patients received six sessions of each treatment on opposite sides of the face, resulting in a significant reduction of all acne scar types (icepicks, boxcar, and rolling) for both procedures.55
Carboxytherapy is considered a safe method for managing acne scars. The associated side effects are minor, with the most common complication being small bruises at the sites of needle insertions. However, these bruises usually disappear within a few days without leaving any lasting marks.56 This is highly accepted by patients, dermatologists, and esthetic medicine doctors.
Intralesional corticosteroid injections are a widely used and effective treatment for hypertrophic acne scarring. Their mechanism of action involves reducing fibroblast proliferation and promoting collagen degradation.57 However, there are potential side effects associated with corticosteroid injections, including the development of hy-
Soft‐tissue augmentation, which involves injecting collagen fillers including hyaluronic acid, CaHA, PLL, silicone, and autologous fat, is a successful treatment for superficial atrophic acne scarring. By stretching dermal fibroblasts, these fillers restore lost tissue volume and promote collagen formation. For the best cosmetic outcomes, multiple treatments might be necessary, although they have proven to be quite effective in healing atrophic acne scars. Rolling scars respond particularly well to hyaluronic acid.5,62 It should be emphasized that these procedures only provide transitory results, necessitating additional visits to maintain the desired cosmetic results. Recently approved treatments include autologous fibroblast transfer and PMMA microspheres suspended in bovine collagen for people seeking more long‐lasting remedies.60 This is a successful treatment for atrophic acne scars, with good acceptance among patients and dermatologists.
For skin and scar regeneration, using adult stem cells (SCs) is becoming more and more practical. Bone marrow (BM), adipose tissue, the umbilical cord, and skin tissue are just a few of the tissues from which SCs can be obtained.33 The potential for BM‐derived SCs (BMSCs) to aid in tissue repair or regeneration in a variety of tissues, including the heart, blood vessels, broken bones, tendons, cartilage, and skin, has been demon-
strated. It is clear that BMSCs are naturally present in healthy skin and that they play a part in host defense, inflammatory responses, and epidermal formation. Researchers are investigating the use of autologous agents as dermal fillers for repairing scars and wrinkles as a result of this increased interest.63 A novel approach for treating acne scars, SC therapy, has shown encouraging outcomes. A topical SC‐conditioned medium (SC‐CM) may improve the effectiveness of FCL in treating atrophic acne scars, according to one study.64 Further study is necessary to fully evaluate the efficiency and safety of SC therapy for acne scars, though, as it is still in its early phases of development.65 Patient acceptance is influenced by the novelty of the approach and the need for more evidence regarding its effectiveness. Dermatologists are likely to monitor developments in SC therapy for scar treatment but may approach it cautiously until more data is available regarding its benefits and risks.
The effectiveness of combination therapy for healing acne scars has been investigated in numerous studies.50,66 For instance, in a meta‐analysis of research, PRP and an ablative FX CO2 laser were combined to treat acne scars. Results from exploratory clinical trials showed that when the laser and PRP were combined, as opposed to laser treatment alone, patients' improvement rates were noticeably higher.67 PDL and FX CO2 laser therapy are two more treatments for acne scars that have been the subject of studies,31 fractional carbon dioxide (CO2) laser resurfacing with punch elevation,68 fractional erbium‐YAG laser and PRP,11 microneedle fractional RF and topical polylactic acid,13,69 and autologous cell regeneration techniques with dermabrasion.48 In general, in most studies that utilized a combination of the mentioned therapeutic methods, the results have shown that the combination of these methods leads to a significantly stronger improvement in treatment outcomes compared to individual treatments.
Despite the efforts to present a perfect literature review, there are still some shortcomings. The studies were included in this study if they were published in English owing to the inclusion criteria. Also, the full text of one article was not available. Additionally, there were various tools for the measurement of outcomes. Although the search strategy was designed precisely and a snowball search of included studies was considered, there may be some missing data. There is a need for conducting more studies to complement the findings of the current study.
The management of acne scars presents
a complex challenge, and diverse therapeutic methods have been developed to address these issues. Laser and light‐based therapies, including FX CO2 laser and photodynamic therapy, have shown promising outcomes in treating both acne and acne scarring. Additionally, microneedling, chemical peels, and dermal fillers play significant roles in improving the appearance of acne scars. Other viable options for acne scar reduction include PRP therapy, subcision, RFM, cryotherapy, and fluorouracil treatments, which have all yielded positive results. Combinations of treatments have demonstrated improved effectiveness compared to individual approaches. Soft‐tissue augmentation with fillers including hyaluronic acid, CaHA, and PLL can provide temporary improvement for atrophic acne scarring. The selection of the type of treatment should be based on the type and severity of the condition, as well as the general health of the patients.
Written and verbal informed consent has been properly obtained from the patients and their guardians. All content of this research adheres with the ethical guidelines developed by the Committee on Publication Ethics (COPE) during the 2nd World Conference on Research Integrity in Singapore in 2010. All parts of this study meets the Code of Conduct (the Ethics Code) and adheres to the legal requirements of the study country, Iran.
The authors declare no conflicts of interest.
The authors received no specific funding for this work.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
1. Eichenfield DZ, Sprague J, Eichenfield LF: Management of acne vulgaris: A review. JAMA 2021; 326(20):2055–2067.
2. Liu L, Xue Y, Chen Y, et al: Prevalence and risk factors of acne scars in patients with acne vulgaris. Skin Research and Technology 2023; 29(6):e13386.
3. Heng AHS, Say Y‐H, Sio YY, Ng YT, Chew FT: Epidemiological risk factors associated with acne vulgaris presentation, severity, and scarring in a Singapore Chinese population: A cross‐sectional study. Dermatology 2022; 238(2):226–235.
4. Chilicka K, Rusztowicz M, Szyguła R, Nowicka D: Methods for the improvement of acne scars used in dermatology and cosmetology: A review. Journal of Clinical Medicine 2022;
11(10):2744.
5. Lanoue J, Goldenberg G: Acne scarring: A review of cosmetic therapies. Cutis 2015; 95(5):276–281.
6. Goodarzi A, Behrangi E, Ghassemi M, et al: Acne scar: A review of classification and treatment. Journal of Critical Reviews 2020; 7(5):815–823.
7. Boen M, Jacob C: A review and update of treatment options using the Acne Scar Classification System. Dermatologic Surgery 2019; 45(3):411–422.
8. Salameh F, Shumaker PR, Goodman GJ, et al: Energy‐based devices for the treatment of acne scars: 2022 International Consensus Recommendations. Lasers in Surgery and Medicine 2022; 54(1):10–26.
9. Ali B, ElMahdy N, Elfar NN: Microneedling (Dermapen) and Jessner's Solution peeling in treatment of atrophic acne scars: A comparative randomized clinical study. Journal of Cosmetic and Laser Therapy 2019; 21(6):357–363.
10. You H‐J, Kim D‐W, Yoon E‐S, Park S‐H: Comparison of four different lasers for acne scars: Resurfacing and fractional lasers. Journal of Plastic, Reconstructive & Aesthetic Surgery 2016; 69(4):e87–e95.
11. El‐Taieb MA, Ibrahim HM, Hegazy EM, et al: Fractional Erbium‐YAG laser and platelet‐rich plasma as single or combined treatment for atrophic acne scars: A randomized clinical trial. Dermatology and Therapy 2019; 9: 707–717.
12. Bhat YJ, Rehman F, Hassan I, et al: Fractional laser resurfacing for acne scars: Our experience at Tertiary Care Hospital of North India. Journal of Cutaneous and Aesthetic Surgery 2023; 16(1):42–48.
13. An MK, Hong EH, Suh SB, Park EJ, Kim K: Combination therapy of microneedle fractional radiofrequency and topical poly‐lactic acid for acne scars: A randomized controlled split‐face study. Dermatologic Surgery 2020; 46(6):796–802.
14. Tawfik AA, Fathy M, Badawi A, Abdallah N, Shokeir H: Topical 5 fluorouracil cream vs combined 5 fluorouracil and fractional Erbium YAG laser for treatment of severe hypertrophic scars. Clinical, Cosmetic and Investigational Dermatology 2019; 12:173–180.
15. Bazargan AS, Ziaeifar E, Abouie A, et al: Evaluating the effect of tranexamic acid as mesotherapy on persistent post‐acne erythema: A before and after study. Journal of Cosmetic Dermatology 2023; 22:2714–2720.
16. Kareem IMA, Fouad MA, Ibrahim MK: Effectiveness of subcision using carboxytherapy plus fractional carbon dioxide laser resurfacing in the treatment of atrophic acne scars: Comparative split face study. Journal of Dermatological Treatment 2019; 31(3):296–299.

18. Eubanks SW, Solomon JA: Safety and efficacy of fractional radiofrequency for the treatment and reduction of acne scarring: A prospective study. Lasers in Surgery and Medicine 2022; 54(1):74–81.
19. Shoaib MAE, Hekal AAEF, Gaber MAE: Subcision with blunt cannula in combination with injection of PRP and microneedling in treatment of acne scar. Egyptian Journal of Hospital Medicine 2023; 90(2):3223–3230.
20. Wollina U, Goldman A: Fillers for the improvement in acne scars. Clinical, Cosmetic and Investigational Dermatology 2015; 8:493–499.
21. Bagherani N, Smoller BR, Tavoosidana G, et al: An overview of the role of carboxytherapy in dermatology. Journal of Cosmetic Dermatology 2023; 22:2399–2407.
22. Soares MTP, Roth DMP, Arbache S: Acne scars: 5‐fluorouracil (MMP Technique), in Minimally Invasive Aesthetic Procedures: A Guide for Dermatologists and Plastic Surgeons, ed. Costa A. (Springer, 2020), pp. 637–642.
23. Abdel‐Maguid EM, Awad SM, Hassan YS, et al: Efficacy of stem cell‐conditioned medium vs. platelet‐rich plasma as an adjuvant to ablative fractional CO2 laser resurfacing for atrophic post‐acne scars: A split‐face clinical trial. Journal of Dermatological Treatment 2021; 32(2):242–249.
24. Meghe SR, Khan A, Jangid SD, et al: Shedding light on acne scars: A comprehensive review of CO2 vs. erbium‐doped yttrium aluminium garnet (Er:YAG) laser therapy. Cureus 2024; 16(4):e57572, 10.7759/cureus.57572.
25. Vempati A, Zhou C, Tam C, et al: Subcision for atrophic acne scarring: A comprehensive review of surgical instruments and combinatorial treatments. Clinical, Cosmetic and Investigational Dermatology 2023; 16:125–134.
26. Al‐Hamamy HR, AL‐Dhalimi MA, Abtan AF: Evaluation of treatment of acne scars with 25% trichloroacetic acid chemical peel followed by manual dermasanding. Journal of Cosmetic Dermatology 2021; 20(6):1750–1755.
27. Bagatin E, Freitas THP, Rivitti‐Machado MC, et al: Adult female acne: A guide to clinical practice. Anais Brasileiros de Dermatologia 2019; 94:62–75.
17. Mamizadeh M, Jowzi M, Ghorabi ST, et al: Comparing the effectiveness and patient’s satisfaction in employing two approaches of subcision and microneedling with subcision and laser CO2 fractional in the treatment of acne scar. Journal of Pakistan Association of Dermatologists 2023; 33(2):499–506.
28. Kim SH, Lee SJ, Lee JW, Jeong HS, Suh IS: Clinical trial to evaluate the efficacy of Botulinum Toxin Type A injection for reducing scars in pa-
tients with forehead laceration: A double‐blinded, randomized controlled study. Medicine 2019; 98(34):e16952.
29. Kar BR, Raj C: Fractional CO2 laser vs fractional CO2 with topical platelet‐rich plasma in the treatment of acne scars: A split‐face comparison trial. Journal of Cutaneous and Aesthetic Surgery 2017; 10(3):136–144.
30. Chandrashekar BS, Sriram R, Mysore R, Bhaskar S, Shetty A: Evaluation of microneedling fractional radiofrequency device for treatment of acne scars. Journal of Cutaneous and Aesthetic Surgery 2014; 7(2):93–97.
31. Bailey JK, Blackstone BN, DeBruler DM, et al: Effects of early combinatorial treatment of autologous split‐thickness skin grafts in red duroc pig model using pulsed dye laser and fractional CO2 Laser. Lasers in Surgery and Medicine 2018; 50(1):78–87, 10.1002/lsm.22702.
32. Kwon HH, Park HY, Choi SC, et al: Combined fractional treatment of acne scars involving non‐ablative 1,550‐Nm Erbium‐glass laser and micro‐needling radiofrequency: A 16‐week prospective, randomized split‐face study. Acta Dermato‐Venereologica 2017; 97(8):947–951.
33. Gozali MV, Zhou B: Effective treatments of atrophic acne scars. Journal of Clinical and Aesthetic Dermatology 2015; 8(5):33–40.
34. Bjørn M, Stausbøl‐Grøn B, Braae Olesen A, Hedelund L: Treatment of acne scars with fractional CO2 laser at 1‐month versus 3‐month intervals: An intra‐individual randomized controlled trial. Lasers in Surgery and Medicine 2014; 46(2):89–93.
35. El‐Domyati M, Abdel‐Wahab H, Hossam A: Microneedling combined with platelet‐rich plasma or trichloroacetic acid peeling for management of acne scarring: A split‐face clinical and histologic comparison. Journal of Cosmetic Dermatology 2018; 17(1):73–83.
36. Kontochristopoulos G, Platsidaki E: Chemical peels in active acne and acne scars. Clinics in Dermatology 2017; 35(2):179–182.
37. Castillo DE, Keri JE: Chemical peels in the treatment of acne: Patient selection and perspectives. Clinical, Cosmetic and Investigational Dermatology 2018; 11:365–372.
38. Joseph JH, Shamban A, Eaton L, et al: Polymethylmethacrylate collagen gel–injectable dermal filler for full

face atrophic acne scar correction. Dermatologic Surgery 2019; 45(12):1558–1566.
39. Forbat E, Ali F, Al‐Niaimi F: The role of fillers in the management of acne scars. Clinical and Experimental Dermatology 2017; 42(4):374–380.
40. Hesseler MJ, Shyam N: Platelet‐rich plasma and Its utility in the treatment of acne scars: A systematic review. Journal of the American Academy of Dermatology 2019; 80(6):1730–1745.
41. Gulanikar AD, Vidholkar R: Efficacy of platelet‐rich plasma in acne scars. Clinical Dermatology Review 2019; 3(2):109–114.
42. Deshmukh NS, Belgaumkar VA: Platelet‐rich plasma augments subcision in atrophic acne scars: A split‐face comparative study. Dermatologic Surgery 2019; 45(1):90–98.
43. Asif M, Kanodia S, Singh K: Combined autologous platelet‐rich plasma with microneedling versus microneedling with distilled water in the treatment of atrophic acne scars: A concurrent split‐face study. Journal of Cosmetic Dermatology 2016; 15(4):434–443.
44. Ahramiyanpour N, Rastaghi F, Parvar SY, et al: Subcision in acne scarring: A review of clinical trials. Journal of Cosmetic Dermatology 2023; 22(3):744–751.
45. Lotfi E, Kaveh R, Nezhad NZ, Iranmanesh B, Hosseini SA, Ahramiyanpour N: Endo‐radiofrequency subcision in the treatment of acne scars: A pilot investigative study. Lasers in Medical Science 2023; 38(1):154.
46. Meymandi SS, Moosazadeh M, Rezazadeh A: Comparing two methods of cryotherapy and intense pulsed light with triamcinolone injection in the treatment of keloid and hypertrophic scars: A clinical trial. Osong Public Health and Research Perspectives 2016; 7(5):313–319.
47. Rho N‐K: Revisiting the role of local cryotherapy for acne treatment: A review and update. Journal of Clinical Medicine 2022; 12(1):26, 10.3390/jcm12010026.
48. Chen Q, Yu N, Liu Z, et al: The clinical efficacy of ReCell autologous cell regeneration techniques combined with dermabrasion treatment in acne scars. Aesthetic Plastic Surgery 2020; 44:535–542.
49. Nor NM, Ismail R, Jamil A, Shah SA, Imran FH: A randomized, single‐blind trial of clobetasol propionate 0.05% cream under silicone dressing occlusion versus
intra‐lesional triamcinolone for treatment of keloid. Clinical Drug Investigation 2017; 37:295–301.
50. Kannangara A: Acne scar management. Global Dermatology 2015; 2(5):183–186.
51. Vedamurthy M: Mesotherapy in aesthetic medicine, in Cosmetic Surgery: Art and Techniques, ed. Costa A. (Springer, 2013), pp. 205–218.
52. Lee J.C., Daniels M.A., and Roth M.Z.: “Mesotherapy, Microneedling, and Chemical Peels,” Clinics in Plastic Surgery 2016; 43(3):583–595.
53. Hasan I, Kumar P, Ahmad H: Mesotherapy strategies and techniques: A view. Journal of Pharma and Ayurved Research 2020; 1(1):46–56.
54. Al Taweel AAI, Al Refae AAAS, Hamed AM, Kamal AM: Comparative study of the efficacy of platelet‐rich plasma combined with carboxytherapy vs its use with fractional carbon dioxide laser in atrophic acne scars. Journal of Cosmetic Dermatology 2019; 18(1):150–155.
55. Moftah NH, El Khayyat MA, Ragai MH, Alaa H: Carboxytherapy versus skin microneedling in treatment of atrophic postacne scars: A comparative clinical, histopathological, and histometrical study. Dermatologic Surgery 2018; 44(10):1332–1341.
56. Stolecka‐Warzecha A, Chmielewski Ł, Deda A, Śmich A, Lebiedowska A, Wilczyński S: The influence of carboxytherapy on scar reduction. Clinical, Cosmetic and Investigational Dermatology 2022; 15:2855–2872.
57. Sánchez Viera M: Management of acne scars: Fulfilling our duty of care for patients. British Journal of Dermatology 2015; 172(S1):47–51.
58. Trisliana Perdanasari A, Torresetti M, Grassetti L, et al: Intralesional injection treatment of hypertrophic scars and keloids: A systematic review regarding outcomes. Burns & Trauma 2015; 3:3.
59. Faghihi G, Nouraei S, Asilian A, et al: Efficacy of punch elevation combined with fractional carbon dioxide laser resurfacing in facial atrophic acne scarring: A randomized split‐face clinical study. Indian Journal of Dermatology 2015; 60(5):473–478.
60. Hession MT, Graber EM: Atrophic acne scarring: A review of treatment options. Journal of Clinical and Aesthetic Dermatology 2015; 8(1):50–58.
61. Bhargava S, Cunha PR, Lee J, Kroumpouzos G: Acne scarring
management: Systematic review and evaluation of the evidence. American Journal of Clinical Dermatology 2018; 19:459–477.
62. Solomon P, Ng CL, Kerzner J, Rival R: Facial soft tissue augmentation with Bellafill: A review of 4 years of clinical experience in 212 patients. Plastic Surgery 2021; 29(2):98–102.
63. Klinger M, Marazzi M, Vigo D, Torre M: Fat injection for cases of severe burn outcomes: A new perspective of scar remodeling and reduction. Aesthetic Plastic Surgery 2008; 32:465–469.
64. Kwon HH, Yang SH, Lee J, et al: Combination treatment with human adipose tissue stem cell‐derived exosomes and fractional CO2 laser for acne scars: A 12‐week prospective, double‐blind, randomized, split‐face study. Acta Dermato‐Venereologica 2020; 100(18):1–8.
65. Phonchai R, Naigowit P, Ubonsaen B, Nilubol S, Brameld S, Noisa P: Improvement of atrophic acne scar and skin complexity by combination of aqueous human placenta extract and mesenchymal stem cell mesotherapy. Journal of Cosmetics, Dermatological Sciences and Applications 2020; 10(1):1–7.
66. El‐Domyati M, Moftah NH, Nasif GA, et al: Amniotic fluid‐derived mesenchymal stem cell products combined with microneedling for acne scars: A split‐face clinical, histological, and histometric study. Journal of Cosmetic Dermatology 2019; 18(5):1300–1306.
67. Chang H‐C, Sung C‐W, Lin M‐H: Combination therapy with microneedling and platelet‐rich plasma for acne scarring: A systematic review and meta‐analysis. Dermatologic Surgery 2020; 46(8):1118–1122.
68. Faghihi G, Keyvan S, Asilian A, Nouraei S, Behfar S, Nilforoushzadeh MA: Efficacy of autologous platelet‐rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: A split‐face randomized clinical trial. Indian Journal of Dermatology, Venereology and Leprology 2016; 82:162.
69. Cachafeiro T, Escobar G, Maldonado G, Cestari T, Corleta O: Comparison of nonablative fractional erbium laser 1,340 nm and microneedling for the treatment of atrophic acne scars: A randomized clinical trial. Dermatologic Surgery 2016; 42(2):232–241.
Have a comment about the articles in this issue? Share your knowledge and opinions with peers worldwide.
Researchers note pyoderma gangrenosum (PG) is a challenging inflammatory skin disorder, and while corticosteroids offer a rapid response, their long-term risks necessitate alternative treatments. In that context, the investigators compared the long-term effectiveness of biologic therapies versus systemic corticosteroids in PG management.
They conducted a retrospective analysis of 15 PG patients from two centres—one in Sydney and one in Milan. The patients received either biologic therapies (n=8) or corticosteroids (n=7), with ulcer healing outcomes assessed at weeks 16, 28 to 32 and 54.
At week 16, corticosteroids led to faster ulcer reduction and re-epithelialisation. However, biologic-treated patients showed sustained improvement over time, supporting their role in long-term PG management.
RC Ingurgio, A Alfano, L Gargiulo, et al: Using biologics to reduce long-term corticosteroid use in pyoderma gangrenosum: Real-world evidence from two centres, in Australasian Journal of Dermatology (May 27, 2025, online ahead of print).
Researchers identified the treatment goals and preferences of young atopic dermatitis (AD) patients and their caregivers and explored heterogeneity among subgroups. For this study, investigators conducted a web-based survey among children (6 to 11 years), adolescents (12 to 17 years), and young adults (18 to 30 years) with AD and caregivers of AD patients. Survey questions included multiple-choice, four-point Likert scale, and open-ended questions. Goals and preferences were stratified by age, gender, disease severity, current treatment, visible lesions, and atopic comorbidity. The authors included 286 respondents.
Prioritized treatment goals were 'no itch', 'preventing new lesions', and 'no lesions'. Prioritized treatment characteristics were 'high effectiveness' and 'long-term safety'. Young patients (6 to 30 years) considered convenience of treatment more important than caregivers, while caregivers considered short- and long-term safety more important than young patients. Pediatric patients (6 to 17 years) considered psychosocial goals more important than young adults.
LP van der Rijst, MS de Bruin-Weller, NPA Zuithoff, et al: Treatment goals and preferences of pediatric atopic dermatitis patients, young adults, and caregivers, in The Journal of Dermatological Treatment (May 27, 2025, online ahead of print).

What is the red lump on this woman’s neck?
THE EDITORS invite your participation in this regular feature of the journal. Please send all images and correspondence to: Medical Editor, The Chronicle of Skin & Allergy
(416) 916-2476 E-mail: health@chronicle.org
What THE LAY PRESS is saying about . . .
Dermatology news your patients may be reading
An article on the AOL web portal (June 5, 2025) emphasizes that while SPF makeup offers some sun protection, it shouldn’t replace traditional sunscreen. New York Citybased dermatologist Dr. Dendy Engelman explains that most SPFinfused makeup products, such as foundations, primers, and powders, don’t contain high enough SPF levels to fully protect skin, especially in the small amounts typically applied. She said that it is better to think of makeup with SPF as a bonus. Los Angeles-based dermatologist Dr. Asmi Berry recommends using a broad-spectrum sunscreen with at least SPF 30 as the final skincare step before applying makeup. She adds that lightweight, non-greasy sunscreens with gel or serum textures tend to layer best. She also says that to reapply sunscreen throughout the day without disturbing makeup, options such as SPF powders, setting sprays, or gently dabbing sunscreen on with a sponge work best.
An online article at NPR (June 2, 2025) explores the growing trend of using beef tallow as skincare, driven by TikTok influencers promoting it as a natural cure for dry skin, acne, and signs of aging. Tallow, a rendered animal fat, creates a moisture barrier like other fats, but dermatologists caution it's not superior to plant-based oils and lacks humectants found in traditional lotions. Dr. Delila Foulad, a dermatologist at UCLA Health who specializes in treating skin and scalp disorders, warns that it can clog pores, worsen acne, and cause allergic reactions, especially for those with eczema or psoriasis. Despite claims on TikTok that it is safe and better than most commercial moisturizers, she urges patch testing before widespread use. Sociologists say the appeal of beef tallow lies in growing distrust of synthetic ingredients and a cultural preference for more natural products. While tallow likely won’t harm most users, experts stress consulting a dermatologist over following social media trends.
An article in Drug Topics (May 18, 2025) emphasizes the importance of suicide risk management in dermatology. The article highlights a review published in JAAD Reviews that underscores how visible or stigmatizing skin conditions can lead to depression, anxiety, and, in some cases, suicidal ideation, especially in teenagers and adults with chronic conditions. While earlier studies found mixed evidence, recent research links conditions like hidradenitis suppurativa and melanoma to higher suicide risk. One meta-analysis found depression in 27.2% of patients with acne, psoriasis, or atopic dermatitis, and anxiety in 28.8%. Suicidal thoughts ranged from 0.45% to 67% across studies. The authors urge dermatologists to recognize psychological distress and collaborate with mental health professionals when needed. The review concludes that dermatologists are in a unique position to identify mental health risks early and improve outcomes through coordinated support.
A study from the University of Maryland School of Medicine (Feb. 21, 2025) describes a newly discovered skin disease identified in a patient with severe erythroderma affecting 80% of his body. After traditional treatments failed, researchers developed a novel diagnostic test using peripheral blood immunophenotyping to pinpoint the inflammatory drivers, specifically elevated interleukin-13 and interleukin-17. Targeted biologic therapy with dupilumab and secukinumab led to full remission. The patented test, based on flow cytometry, allowed for precise immune profiling and real-time monitoring of cytokine and disease-causing cell levels. The authors say this case demonstrates how precision diagnostics can lead to effective, personalized treatment for previously unclassified skin conditions. The study highlights the potential of this approach to transform care for patients with chronic, unexplained inflammatory skin diseases. Researchers are now working to expand the test’s application to other conditions.
At Organon Canada, we’re deepening our focus on dermatology. With a dedication to supporting healthcare professionals and their patients, we are contributing our expertise to advance skin health.
more about Organon Canada’s commitment to dermatology. Visit organon.ca
The 昀rst and only PDE4i indicated in the topical treatment of seborrheic dermatitis*
ONCE-DAILY STEROID-FREE* PDE4i
ZORYVE is indicated for topical treatment of seborrheic dermatitis in patients 9 years of age and older.


Designed for simple administration
• Can be used on all a昀ected areas of skin, including the face, body, and/or scalp†
• Once-daily topical application
Please consult the Product Monograph at www.arcutis.ca/zoryve-pm-hcp for contraindications, warnings, precautions, adverse reactions, interactions, dosing, and conditions of clinical use. The Product Monograph is also available by calling us at 1-844-692-6729.
PDE4i: phosphodiesterase 4 inhibitor
*Comparative clinical signi昀cance has not been established.
†When they are not wet.
‡Subject to restrictions. For program terms and conditions, go to www.zoryveassist.ca and click “Terms and Conditions”.
Reference: 1. ZORYVE® Product Monograph. Arcutis Canada, Inc. October 2024.
ZORYVE AssistTM Patient Assistance Program is designed to provide 昀nancial support to eligible patients receiving a ZORYVE prescription.‡