




◼ Numerous modalities available to manage BCCs see page 4
n New agents, additional indications improve options for patients
by LOUISE GAGNON, Correspondent, The ChronicleNew IL-inhibitors and additional indications for established IL-inhibitors are creating some valuable therapeutic options in dermatology, according to leading Canadian dermatologists.
IL inhibitors for prurigo nodularis (PN)
The IL-13 inhibitor dupilumab, which has represented a significant advance in the management of atopic dermatitis (AD), has re-
ceived approval by Health Canada for the treatment of PN, pointed out Dr. Brittany Waller, Assistant Professor of Dermatology, University of Saskatchewan, Saskatoon, and dermatologist with Origins Dermatology in Regina.

“In July 2023, dupilumab was approved for prurigo nodularis with promising data and clinical experience now emerging,” said Dr.
n Settings will have to be varied depending on skin colour of patient
by LOUISE GAGNON, Correspondent, The ChronicleFractionated lasers offer dermatologists the opportunity to treat a variety of conditions in a variety of skin types, according to Dr. Geeta Yadav, Medical Director and Founder of FACET Dermatology in Toronto.
Discussing skin resurfacing and treating excess pigment in the skin with use of a fractionated
Promising
n Stabilization and consideration of patient mental health are top prioritiesby JOHN EVANS, Senior Editor, The Chronicle
When managing patients with vitiligo, identifying the stability of the condition is key to informing care, and physicians should recognize that preventing progression has a significant impact on patient quality of life. These were some of the topics discussed by Dr. Iltefat Hamzavi, a metro Detroit-based dermatologist, during a round-up talk on vitiligo at the Fall 2023 Dermatology Update in Toronto.
Waller. “There has been a high unmet need for effective treatments for this condition.”
Dr. Charles Lynde, Director of the Lynde Institute for Dermatology in Markham, Ont., noted that dupilumab has represented a therapeutic leap in the treatment of AD and appears to offer benefit in other dermatologic conditions such as PN.
“Certainly, it's been a wonder drug for people with atopic dermatitis, shutting down their itching, and in terms of quality of life, making it so they can sleep properly,”

Dr. Hamzavi also serves as senior staff physician at Henry Ford Health System's Department of Dermatology and teaches medical students at Wayne State University. In late 2023 the International Vitiligo Task Force released new expert recommendations on the diagnosis and management of vitiligo, Dr. Hamzavi said (JEADV Nov. 2023; 37(11):2173-2184).
The new recommendations note a physician’s first goal when managing a patient with vitiligo “is going to be stabilization,” Dr. Hamzavi said. “Then the physician wants to repigment. And then in some cases, they have to know
“Where Dermatology Lives”
n Share your experiences and observations with a worldwide community of practitioners and researchers. Follow developments in skin health as they occur. Visit www.derm.city

60-70% of women and 50-60% of men report having some level of sensitive skin.1 Are you making laundry recommendations that protect your patients from potentially irritating ingredients like scents and perfumes?
Sensitive skin impacts patient quality of life
Painful and irritating — flare-ups of sensitive skin symptoms can have a profound impact on a patient’s day-to-day activities. Posing as a barrier to participating in the things a person needs (or wants) to do, unmanaged sensitive skin symptoms can quickly result in adverse physical and mental health outcomes for your patients.
Broadly defined as a condition that can cause itching, burning, stinging, and dryness of the skin, sensitive skin presents differently for each patient.1 Caused by many different factors, recent research shows that regular use of household items such as scented laundry detergents impacts the severity of a patient’s sensitive skin symptoms — something that, when left unaddressed, can decrease patient quality of life.2
When most patients think about clean clothing, they often associate it with a fresh and powerful scent.
With many laundry products offering freshly scented options, sensitive skin patients may not be aware of the irritation fragrance can cause.
In a recent 2021 multi-national study, it was found that 4.1% of participants reported having an allergy to fragrance ingredients added to everyday household products like laundry detergent.3
As a healthcare professional looking out for patients’ best interests, it is time to bring laundry into the conversation about their personal care routine. To better support your patients with sensitive skin, we recommend healthcare professionals:
• Create an open line of discussion with your sensitive skin patients to learn more about their current laundry practices.
• Discuss the potential risks of using laundry products containing scents and perfumes, even if labelled as “natural” or made as “Bio” products from locally produced vendors.
• Offer specific recommendations for a laundry regimen that is entirely fragrance and perfume-free for the best results.4
Help your patients build a fragrance-free laundry regimen
As one of the easiest ways to support patients with sensitive skin, recommending a fragrance-free laundry regimen like the Tide, Downy, and Bounce Free & Gentle collection is a great option.

Tide, Downy, and Bounce Free & Gentle Regimen. #1 Dermatologist Recommended.
Dermatologist-recommended and created with sensitive skin in mind, the Free & Gentle regimen is a simple three-step process:
• Step 1: Clean – Tide Free & Gentle’s Lift and Block cleaning action cleans to the fibre level and prevents soils from redepositing.
• Step 2: Protect – Downy Free & Gentle provides a conditioning benefit by reducing friction between clothes and skin.
• Step 3: Enhance – Bounce Free & Gentle provides an anti-static treatment that has been shown to repel pet hair.
When working with patients struggling with sensitive skin, it is essential to bring the laundry routine into the discussion. By highlighting the importance of a fragrance-free laundry regimen that is designed without potentially irritating perfumes and scents, healthcare professionals can help patients improve their quality of life, allowing them to get back to doing the things they love. To
M. J., Calderson, A. Evaluation of the relative mildness of commercial sensitive skin and baby laundry detergents. SkinMed. 2020; 1(18): 14-16.
Using fractionated lasers for treatment of melasma Dr. Geeta Yadav discusses the use of fractionated laser therapy to treat melasma. She notes that settings of the laser will be dependent on a patient's skin type and melanation. . 1
BCC Update 2024
Canadian dermatologists discuss new treatments available to treat BCCs in 2024, including the use of immunotherapy, in the form of the PD-1 inhibitor cemiplimab 4
Vender on Psoriasis:
Deucravacitinib in Japanese patients with moderate to severe PP, GPP, or EP: A phase III trial Also, the COMFORT-1 study aimed to evaluate the efficacy of piclidenoson, an A3 adenosine receptor, in treating moderate to severe plaque psoriasis. Piclidenoson was shown to have increasing efficacy over time with excellent safety and tolerability. 8
Chronicle Postgraduate Educational Supplement
In this issue’s postgraduate educational supplement, investigators reviewed factors that can influence sensitive skin, with an emphasis on built environment characteristics. The review showed sensitive skin is the outcome of interactions between individual attributes and environmental factors 21

Lutikizumab effective in HS patients, according to results of recent study
According to a recent study, lutikizumab 300 mg was shown to be more effective than placebo in hidradenitis suppurativa (HS) patients.
The data was recently published in a press release (Jan. 08, 2024).
Researchers performed a 16week, Phase II, randomized, double-blind study with 153 HS patients who had previously failed anti-TNF therapy. Patients were split into four groups: 100 mg lutikizumab every other week, 300 mg every other week, 300 mg weekly, and placebo

March/April 2024 • Vol. 30 No. 2
Published eight times per year by the proprietor, Chronicle Information Resources Ltd., with offices at 1460 The Queensway, Suite 212, Etobicoke, Ont. M8Z 1S4 Canada. Telephone: (416) 916-2476; Facs. (416) 352-6199.
E-mail: health@chronicle.org
ISSN No. 1209-0581
Contents © Chronicle Information Resources Ltd., 2024 except where noted. All rights reserved worldwide.
The Publisher prohibits repro-
duction in any form, including print, broadcast, and electronic, without written permissions.
Printed in Canada. The Chronicle of Skin & Allergy is a Canadian publication. The Publisher certifies that advertising placed in this publication meets Revenue Canada requirements for tax deductibility.
Subscriptions: $85.60 per year in Canada, $129.95 per year in all other countries. Single copies: $10.00 per issue (plus 13% HST).
According to the data, response rates were 48.7% in the 300 mg weekly group and 59.5% for 300 mg every other week. Primary endpoints included an HS Clinical Response and a skin pain NRS30 at week 16.
Both 300 mg groups had higher response rates and rates of improved skin pain NRS30 and HiSCR75 than placebo.
Lutikizumab was well tolerated with adverse events being similar in both treatment and placebo groups. The most common adverse events included diarrhea, headache, pruritus, contact dermatitis, eczema, and nasopharyngitis.
Canada Post Canadian Publications Mail Sales Product Agreement Number 40016917. Please forward all correspondence on circulation matters to: The Chronicle of Skin & Allergy, 1460 The Queensway, Suite 212, Etobicoke, Ont. M8Z 1S4 Ideas in the Service of Medicinesm
Affiliated journals of the Chronicle Companies include The Chronicle of Cosmetic Medicine + Surgery, Women in Dermatology, Pediatric Chronicle, and Linacre’s Books/ Les Editions Linacre



In this issue of THE CHRONICLE OF SKIN & ALLERGY, we continue to bring our readers important data and therapeutic updates on how better to manage common therapeutic scenarios, including vitiligo in all skin types and melasma with laser in our patients with skin of colour. Dr. Iltefat Hamzavi’s comprehensive review on the management and vitiligo, both today and in years to come, is a definite must-read (see page 1). As well, Dr. Geeta Yadav shares her vast knowledge on the use of energy-based devices in the management of melasma (see page 1). Her therapeutic approach results in better outcomes with fewer adverse events.
In this era of an epidemic of skin cancer, we present a review of the management of BCC (see page 4). Although most patients with BCC can be managed in our dermatology offices, some will require intervention by our Mohs surgery colleagues and occasionally will need management by both dermatology and oncology.
Medical Editor
Wayne Gulliver, MD, FRCPC Editor, Cosmetic Dermatology Sheldon V. Pollack, MD, FRCPC
John P. Arlette, MD, FRCPC
Benjamin Barankin, MD, FRCPC
Marc Bourcier, MD, FRCPC
Eric Goldstein, MD, FRCPC
Peter Hull, MD, FRCPC
Richard Langley, MD, FRCPC
Danielle Marcoux, MD, FRCPC
R.A.W. Miller, MD, FRCPC
“It’s important to have sunglasses on to prevent BCCs from developing around the eyes.”
Dr. Michael Stevens, Director, dermatologist and Mohs micrographic surgeon at Precision Dermatology & Skin Surgery in Bedford, N.S.
H. Eileen Murray, MD, FRCPC
Kim Papp, MD, FRCPC
Yves Poulin, MD, FRCPC
Melanie D. Pratt, MD, FRCPC
Denis Sasseville, MD, FRCPC
Jerry Tan, MD, FRCPC
Ronald B. Vender, MD, FRCPC
Founding Editor Colin A. Ramsay, MD, FRCPC (1936-2003)
Publisher Mitchell Shannon
Editorial Director R. Allan Ryan
Senior Editor John Evans
Assistant Editor Jeremy Visser
Cristela Tello RuizJoyce Pitter-Hinds
John-BaptisteMedia Consultant Cathy Dusome
Contacting The Chr onicle
n READER SERVICE: To change your address, or for questions about your receipt of the journal, send an e-mail to health@chronicle.org with subject line “Circulation,” or call during business hours at 416.916.CHROn (2476), or toll-free at 866.63.CHRON (24766).
n LETTERS: We welcome your correspondence by mail, fax (416.352.6199), or e-mail. Kindly use the co-ordinates listed above.
n ADVERTISING: For current rates and data, please contact the publisher.
n REPRINTS: The content of this journal is copyrighted. Please contact Mitchell Shannon for reprint information.

In this report, Canadian dermatologists discuss various approaches to management of superficial basal cell carcinomas (BCCs), locally advanced BCCs, and metastatic BCCs.
Surgical management
When treating BCCs on the body, if there is any degree of invasiveness, treatment can typically involve the use of wide local excision, according to Dr. Michael Stevens, a dermatologist and Mohs micrographic surgeon at Precision Dermatology & Skin Surgery in Bedford, N.S.
“For basal cell carcinomas on the body, the standard is still wide local excision,” said Dr. Stevens. “If it is indicated, Mohs surgery is considered the standard for basal cell carcinomas on the face. These are first-line options to treat BCCs for most patients who can tolerate surgery.”
A key advantage of Mohs surgery
is that it is tissue-sparing, said Dr. Ilya Shoimer, a dermatologist and Mohs micrographic surgeon and Clinical Assistant Professor at the University of Calgary.

“It [Mohs surgery] is the gold standard for treatment of a basal cell carcinoma,” said Dr. Shoimer. “The use of Mohs would be for sites where tissue preservation is important such as the eyelids, nose, mouth, and ears.”
Vismodegib, sonidegib, and photodynamic therapy Gorlin Syndrome, a condition where patients can have many BCCs, is not common, but it is a condition where clinicians agree that hedgehog inhibitors play an important therapeutic role.
The biggest concern [with Gorlin Syndrome] is the burden of basal cell carcinomas,” said Dr. Shoimer. “We need to figure out a way to keep the tumour burden down for these patients.
These are patients where hedgehog inhibitors are quite useful in trying to control their disease. We don’t want to be doing more than 100 surgeries on a patient with Gorlin Syndrome.”


Locations where surgery alone may be a challenge, such as BCCs that are proximal to the eye, can be an opportunity for a combination approach of a hedgehog inhibitor initially followed by surgery, explained Dr. Shoimer.
“The patient can start on a hedgehog inhibitor, and that can shrink it [the tumour] down, and you can perform the surgery on the remainder of the tumour subsequently,” said Dr. Shoimer.
While not as effective as surgery,



The Soluver products for wart treatment are formulated in a unique acrylic delivery system which eliminates the need for bandage covering while keeping occlusion.
Soluver Original minimizes irritation to the healthy skin surrounding the wart, locks in moisture with a durable, watertight covering and allows for superior penetration of salicylic acid.
Soluver Plus, with its higher percentage of salicylic acid, is ideally suited for resistant common or plantar warts.
photodynamic therapy (PDT) can also be a tool that clinicians can use to manage BCCs, specifically those that are superficial and for multiple small basal cell carcinomata as in Gorlin’s syndrome, said Dr. Mark Lupin, a dermatologist in Victoria. “We can clear some of the superficial basal cell carcinomas with PDT,” he noted.
One paper has highlighted the benefit of using PDT to treat carefully-selected BCCs (Molecules 2020 Nov; 25(22):5398).
A PD-1 inhibitor to treat BCCs Clinicians can now access immunotherapy, in the form of the PD1 inhibitor cemiplimab, as a treatment for BCCs, said Dr. Shoimer.
“If patients do not respond to a hedgehog inhibitor, there is now an option for using a PD-1 inhibitor,” Dr. Shoimer said. “It [cemiplimab] was approved for SCCs and it can now be used for locally advanced, unresectable BCCs that have not responded to a hedgehog inhibitor. Cemiplimab would be prescribed by a medical oncologist.”
Indeed, Dr. Lupin highlighted the benefit of having an immunotherapy as an available treatment for BCCs.
“We’ve been using cemiplimab for squamous cell carcinoma,” said Dr Lupin. “If a patient with a basal cell carcinoma fails a hedgehog inhibitor and where Mohs micrographic surgery may not be an option, there is cemiplimab.”
One study involving 54 patients with metastatic BCC demonstrated clinically meaningful anti-tumour activity including durable responses in patients with metastatic BCCs who had had disease progression or were intolerant to treatment with hedgehog inhibitors ( Annals of Oncology 2024; 35(2):221-228).
The study also found that side effects of immunotherapy mainly consisted of fatigue and diarrhea, making immunotherapy a generally better tolerated treatment than hedgehog inhibitors.
Dr. Lupin noted studies proposing using cemiplimab as a primary treatment for BCCs prior to treat-
ment with a hedgehog inhibitor will be underway.
Photoprotection
To help curb any further development of BCCs, patients should be using broad-spectrum sunscreens in daily life, pointed out Dr. Lupin. “There are sunscreens that protect against high-energy visible light,” he said, noting there is some evidence that topical antioxidants can confer additional protection.
Patients may forget to shield some sites from ultraviolet radiation and should be reminded to take measures to protect those sites, noted Dr. Stevens.
“It’s important to have sunglasses on to prevent BCCs from developing around the eyes,” said Dr. Stevens. “It’s also important to wear lip balm with SPF 30 or greater because we do see basal cell carcinomas on the lips. The top of the head and the ears are other areas that people forget about protecting, so it is important to cover the scalp and ears with a broad-brimmed hat.”
Non-proprietary and brand names of therapies: vismodegib (Erivedge, Roche); sonidegib (Odomzo, Sun Pharma Canada); cemiplimab (Libtayo, Sanofi-Aventis).
PrILUMYA®
treatment of adult patients with moderate-tosevere plaque psoriasis who are candidates for systemic therapy or phototherapy.
Please consult the Product Monograph at https://info.ilumya.ca/Product_ Monograph for important information relating to warnings and precautions, adverse reactions, drug interactions, and dosing information, which has not been discussed in this piece.
The Product Monograph is also available by calling our medical information department at 1-844-924-0656.
Current ILUMYA® Product Monograph, Sun Pharmaceutical Industries Limited.
© 2024 Sun Pharma, or its subsidiaries and affiliates. All rights reserved.
ILUMYA is a registered trademark of Sun Pharmaceutical Industries Limited. Used under license.
All other trademarks are the property of their respective owners.


Ronald B. Vender, MD, FRCPC comments on recent findings and developments, and answers clinicians’ questions
Deucravacitinib, an oral selective allosteric inhibitor of tyrosine kinase 2 (TYK2), has received approval in Japan for adult patients with plaque psoriasis (PP), generalized pustular psoriasis (GPP), and erythrodermic psoriasis (EP) who have not adequately responded to conventional systemic therapies. The approval stems from the outcomes observed in the global phase III POETYK PSO-1 and PSO-2 trials, which demonstrated improved efficacy compared to placebo in adults with moderate to severe plaque psoriasis. Additionally, findings from the POETYK PSO-4 trial, an open-label, single-arm, phase III study conducted in Japan, further support the efficacy and safety of deucravacitinib.
The POETYK PSO-4 trial in this study (J Dermatol 2024; 1–15) involved 74 Japanese patients (76.2%, 66.7%, and 37.5% of patients with PP, GPP, and EP, respectively). The primary endpoints, including the proportion of patients achieving a ≥75% reduction from baseline in the Psoriasis Area and Severity Index (PASI 75) and a static Physician's Global Assessment score of 0 or 1 (sPGA 0/1) with at least a two-point improvement from baseline at week 16, were met. At week 16, substantial proportions of patients achieved PASI 75 and sPGA 0/1 across all psoriasis subtypes, with responses generally maintained through week 52.
Although adverse events (AEs) were common, with nasopharyngitis and acne being the most frequent, deucravacitinib was generally well-tolerated among Japanese patients. Rates of serious adverse events (SAEs) and discontinuations were low, and no deaths were reported. These findings underscore the effectiveness and safety of deucravacitinib over 52 weeks in Japanese patients with moderate to severe plaque psoriasis, and to a lesser extent, in those with GPP and EP. These results from the regional POETYK PSO-4 trial in Japan, in conjunction with the analysis of Japanese patients in the global POETYK PSO-1 trial, provide robust evidence supporting the efficacy and safety profile of deucravacitinib in the treatment of moderate to severe psoriasis in Japanese populations.
This study shows that deucravacitinib is certainly effective in a Japanese population. This population requires separate clinical trials to determine its efficacy and safety, due to the different genetic responses that can occur to different medications. The Japanese population is different than the rest of the world due to its specific diet high in fish and low-fat food. In addition, the mean weight of the Japanese psoriasis patient is generally lower than those in North America or Europe. Pustular psoriasis is more common in the Japanese population and therefore finding medications that work specifically for pustular psoriasis or applying new indications to other medications that are not approved necessarily in North America for pustular psoriasis is important due to the increased incidence of this type of psoriasis that is very difficult to treat. Deucravacitinib has been shown to be helpful in this population. Side effects are extremely minimal. Whether or not this data could be extrapolated into a North American population is yet to be seen, however, since this would be off label use and not approved in the product monograph. Since there are no specific treatments approved for erythrodermic psoriasis one could consider deucravacitinib as a treatment option. However, the speed of response may not be as expected or as desired.
The study aimed to evaluate the efficacy and safety of piclidenoson (CF101), an A3 adenosine receptor (A3AR) agonist, in treating moderate-to-severe plaque psoriasis. A3AR is known to be overexpressed in psoriasis patients, and piclidenoson has been shown to inhibit IL-17 and IL-23 production in keratinocytes, key cytokines involved in psoriasis pathogenesis.
The randomized, double-blind phase III COMFORT-1 trial involved 529 patients randomized into different treatment groups: piclidenoson 2 mg b.i.d., piclidenoson 3 mg b.i.d., apremilast 30 mg b.i.d., or placebo (J Eur Acad Dermatol Venereol 2024; 1–9). After 16 weeks, patients initially on placebo were re-randomized into active treatment arms. The primary endpoint was the proportion of patients achieving ≥75% improvement
in Psoriasis Area and Severity Index (PASI-75) at Week 16 compared to placebo.
Results indicated that both doses of piclidenoson exhibited similar efficacy, with the 3 mg b.i.d. dose meeting the primary endpoint (PASI-75 rate of 9.7% versus 2.6% for piclidenoson versus placebo, p=0.037). The efficacy of piclidenoson continued to increase linearly throughout the study period. Furthermore, at week 32, a greater proportion of patients treated with piclidenoson 3 mg b.i.d. demonstrated improvement in Psoriasis Disability Index (PDI) compared to apremilast, with a trend towards significance (p=0.072). Piclidenoson also demonstrated a favourable safety profile compared to apremilast.
Piclidenoson showed increasing efficacy over time alongside excellent safety and tolerability. These findings support its further clinical development as a potential treatment for psoriasis.
New mechanisms of action are very interesting to investigate. It is also comforting to see that the specific interleukins associated with psoriasis, IL 17 and IL 23, are still the key cytokines responsible for the development and persistence of psoriasis. This new mechanism of action, A3AR, affects a different target, but in the end still is directed at reducing the interleukins mentioned above. Although this is an early study, it is promising to see that there is efficacy at least versus placebo and safety versus apremilast.
One important thing to note is that there seems to be a trend away from injectable treatments for psoriasis and back to the oral therapies. Oral therapies were once thought to be weaker than injectable biologics, but in newer studies, such as this one, TYK2 inhibitors, oral peptides, and other mechanisms of actions are trending toward effective oral therapy. Patients are interested in oral therapy instead of injectables quite often when given a choice. However, at present there needs to be a balance between safety and efficacy which presently pushes clinicians to choose injectable biologic versus oral therapy. However, in the coming years, I believe we will see the trend change toward more effective oral therapies.
We invite your comments and questions about this feature at www.derm.city. Dr. Ron Vender is a certified dermatologist with more than 30 years of clinical practice experience and over 100 clinical trials in psoriasis. He is founder and director of Venderm Innovations in Psoriasis, a center of excellence for Psoriasis offering a comprehensive management solution for individuals with psoriasis. www.psoriasis.vip
Developed with the help of Canadian Dermatologists specifically for psoriasis of the scalp, therapeutic shampoo contains the highest concentration of active ingredients to ensure results.
















4% salicylic acid to loosen scale







10% crude coal tar solution to slow cellular turnover and to provide anti-itch
Conditioning base formulation leaves hair soft & manageable



Available at Shoppers Drug Mart or through your local pharmacist.





laser during a webinar, Dr. Yadav noted that energy-based devices have evolved to offer efficacy in a series of treatments without leaving patients itchy and looking extremely raw and swollen, as is the case with a traditional ablative laser.

“A non-ablative fractionated laser does not damage the epidermis in the same way [that an ablative laser does],” said Dr. Yadav. “You can do surface treatment and deep treatment [with a fractionated laser], and allow skin to remain intact between treatments and therefore the downtime is less. Additionally, the risk of side effects is a lot lower.”
While treatment with an intense-pulsed light (IPL) device is considerably gentler on the skin than an ablative laser, they cannot be used on all skin types and a series of treatments with an IPL device often fail to show noticeable differences in removing brown spots, for example, Dr. Yadav noted. “Patients may find that they do not see brown spots fade with numerous treatments with IPL.”
Using fractionated lasers in darker skin types and treating melasma Fractionated laser, which delivers pulses across a wide range of density and energy levels, is an option for darker skin types, said Dr. Yadav, noting about half of her patient population are patients with brown or black skin.
“My patients may come to me saying that they are nervous about being treated with a laser and they don’t think it can be done,” said Dr. Yadav. “The truth is you can absolutely use a laser [for patients with brown and black skin]. How you choose your settings is going to vary depending on the patient in front of you. There really isn’t a cookie-cutter approach. If you look at the operator manuals, conservative settings will be recommended. Finding a balance between getting the best effect out of your laser, but also being safe for the patient is the sweet spot. Make sure that you and your team have good operator skills and that you are driving the device.”
Melasma recurs, so one-time treatment with a fractionated laser will likely not suffice to keep melasma at bay, noted Dr. Yadav.
“Keep in mind with melasma, that it can come back,” said Dr. Yadav. “It doesn’t come

“
My patients may come to me saying that they are nervous about being treated with a laser and they don’t think it can be done... the truth is you can absolutely use a laser [for patients with brown and black skin]. How you choose your settings is going to vary depending on the patient in front of you.”
Dr. Geeta Yadav
back because of what you do in treatment with the device. It comes back because of the nature of the condition.”
A multi-modal approach, involving a fractionated laser and topical treatments, can be employed for managing melasma, she added. In terms of topical agents for melasma management, hydroquinone offers temporary lightening of the skin, but it is not advisable to use hydroquinone on an ongoing basis, according to Dr. Yadav. “I would prefer if patients do maintenance treatments with something that is more sustainable, like tranexamic acid.”
Reducing pain, advising against sun exposure, delaying treatment due to sun exposure Pain control for patients needs to be highly individualized and can include various approaches, said Dr. Yadav.
“Different blends of topical numbing can be used,” said Dr. Yadav, noting numbing agents should be left on the skin for 30 to 60 minutes prior to the procedure. “You can also consider using facial nerve blocks, which are fairly straightforward to perform.”
One of the important counselling points is to tell patients to avoid the sun for several days after undergoing laser resurfacing treatment and to use sunscreen if they do go out in the sun, noted Dr. Yadav.
“I think sunscreen is very important and having an elegant sunscreen that is a full titanium zinc block is probably going to be the least irritating to the skin,” she said. “Carrying a sunscreen [that is available at] your practice to make sure that patients can use it. And obviously a gentle cleanser is needed. You do not want to use a cleanser that is going to be too harmful or foaming. A cream cleanser would be good to use.”
If patients have skin that suggests they have had significant recent sun exposure, it is not an ideal time to perform laser treatments, pointed out Dr. Yadav.
“Try not to treat anybody immediately after they have had sun exposure because that will cause dyspigmentation or risk of dyspigmentation,” said Dr. Yadav. “Wait at least a month be-
fore you treat them. Summertime is not an ideal time [for treatment].”
Using eye shields and decreasing risk of herpes zoster
If treating around the eyes, clinicians should remember to place eye shields in the eyes, stressed Dr. Yadav.
“You need to anesthetize and lubricate the eyes, so you can put in the eye shields,” said Dr. Yadav, noting eye shields are available in different sizes.
Another tip that Dr. Yadav offered is to prescribe medications to patients to avoid the development of herpes zoster.
“Every practice may have their own acyclovir or valacyclovir protocol,” said Dr. Yadav. “I used to prescribe acyclovir or valacyclovir only if a patient had herpes zoster, but I do it now for everybody
“I have had very young patients break out [with herpes zoster] after chemical peels or after laser resurfacing,” stressed Dr. Yadav. “There are really no contraindications with valacyclovir, so it is really an easy thing to prescribe. It will cover you when it comes to mitigating that kind of outcome with your patients.”
Continued from page 3
In our clinical practice feature (see page 1) you’ll find out all that is new and exciting with respect to IL inhibition, including everything from new therapies such an oral anti-IL-23 inhibitor for psoriasis, the use of anti-IL-13 inhibitor for prurigo nodularis, anti-IL-17 for the treatment of hidradenitis suppurativa, and the anti-IL-36 for the treatment of generalized pustular psoriasis. In these pages, readers will find reports of significant new and innovative therapeutic advances in Canadian dermatology.
As always, THE CHRONICLE team invites and welcomes your comments on this issue, or any other topic in dermatology, at www.derm.city
—Wayne P. Gulliver, MD, FRCPC, Medical Editor
Continued from page 1
Dr. Lynde told THE CHRONICLE OF SKIN & ALLERGY. “It is showing it is useful in prurigo nodularis. This is a terrible disease where nothing before has seemed to work effectively.”
Another potential therapy for PN that may prove effective is the IL-31 inhibitor nemolizumab, noted Dr. Lynde. “It is progressing in trials with a goal to it being another management option for PN,” he said.
Dr. Gurbir Dhadwal, a dermatologist at Guildford Dermatology in Surrey, B.C., and at St. Paul’s Hospital in Vancouver, agreed that IL inhibitors are addressing a need when it comes to PN.


“[Dupilumab] works really well,” said Dr. Dhadwal, who is also a clinical instructor at the University of British Columbia. “It has the same safety profile as for atopic dermatitis. We already know how to prescribe the drug, so it's an easy shift to use it for prurigo nodularis. It remains to be seen when nemolizumab will come out for prurigo nodularis. It should be a good drug for prurigo [nodularis] because it really targets itch directly.”
Other IL inhibitors to treat hidradenitis suppurativa Dr. Ashley O’Toole, a dermatologist with the Skin Centre for Dermatology in Peterborough, Ont., expressed enthusiasm about the U.S. FDA approval of secukinumab for HS and anticipates the therapy will become a tool in the HS toolbox in Canada in 2024, coupled with continued exploration of bimekizumab this year as a potential future treatment for HS.
“We have been waiting for this [secukinumab] for several years,” said Dr. O’Toole.
“Some dermatologists have used secukinumab off label for HS and have had good success. We have participated in a clinical trial on secukinumab for HS. I am excited at the prospect of being able to offer it to patients in a real-world setting. Bimekizumab is being studied for HS and that may represent another option further down the road.”

Dr. Waller echoed that the FDA approval of secukinumab in October 2023 for HS will prove useful in daily practice. “As the only approved IL-17A inhibitor approved for HS, this agent shows promise in reducing inflammatory nodules and flares,” said Dr. Waller. “I look forward to eventually using this agent in Canada for this indication.”
Dr. Dhadwal agreed that another management choice for HS will be encouraging.
“We have some patients being treated offlabel [with secukinumab] for compassionate use,” said Dr. Dhadwal. “It will be good to have broad access, so we have an alternative therapy. HS patients are some of our highest burden patients, so it would be good to have another option. If we would have two IL-17 inhibitors [secukinumab and bimekizumab] and adalimumab for HS, we would then possibly have more choice in terms of patient-specific factors. If a patient has a comorbidity, for example, then you could select which drug would make more sense for that patient.”
The IL-inhibitor spesolimab has a specific but vital role to play in the management of generalized pustular psoriasis (GPP), according to Dr. Lynde.
“A dermatologist may see one or two [cases of GPP] in their lifetime unless they have a very specialized clinic,” said Dr. Lynde. “These people can be very sick. You're often called to the hospital about a patient that may be even in the ICU. It
is important to know that there is a treatment that quite remarkably changes people’s lives. A patient can go from being in the ICU to being out the door [of the ICU] the next day [with spesolimab].”
Dr. Dhadwal echoed the phenomenal impact that spesolimab can produce in patients with GPP. “It is not clear how much of an impact it will have overall, but the drug is amazing for what it’s used to treat. GPP is such a rare disease that it’s definitely not something we see every day, but this therapy is game-changing for these patients,” he said.
Oral IL inhibitors under study
The exploration of an oral IL inhibitor is garnering much interest and enthusiasm as a Phase III study gets underway, noted Dr O’Toole.
“That is really exciting,” said Dr. O’Toole. “In our clinic, we are doing a study with an oral anti IL-23 agent. It is very effective, and it has a very rapid onset of action. You may worry that a pill would be tough on the stomach, but patients have not had any significant adverse events at this point. It seems very well-tolerated.”
Published results of a phase II dose-finding trial that involved several Canadian investigators revealed that following 16 weeks of once- or twice-daily oral administration, treatment with the IL-23 receptor antagonist peptide JNJ77242113, achieved greater efficacy than placebo in patients with moderate-to-severe plaque psoriasis (N Engl J Med 2024; 390:510-521).
Dr. Lynde noted that the oral form of an IL inhibitor does not appear to necessitate any compromise on therapeutic potency. “We may actually have in a pill, a drug that is approaching the same efficacy as an injection,” he said.
Non-proprietary and brand names of therapies: dupilumab (Dupixent, Sanofi); nemolizumab (not approved in Canada); secukinumab (Cosentyx, Novartis); bimekizumab (Bimzelx, UCB Canada); adalimumab (Humira, AbbVie); spesolimab (Spevigo, Boehringer Ingelheim).



how to depigment, which is a challenging process.”
Why treat vitiligo?
The discussion of vitiligo management starts with the question of why treat it at all, Dr. Hamzavi said. “Why are we treating it in lighter-skinned individuals, when we can't always see it? Why are we treating it when some communities in the United States and also across the world feel vitiligo is a natural element?”
He cited a study he co-authored (JAMA Dermatol Aug. 2023; 159(10):1124-1128) that examined the impact of vitiligo on patients’ mental health and quality of life, and also investigated the endpoints patients were seeking.
“ This was about 3,900 patients from an initial database of 5,000 people found on social media who selfreported vitiligo,” he said. Findings from that study showed that while repigmentation was a major patient
goal, “one of the primary goals is to stop [vitiligo] from getting worse.”
“Sometimes, physicians aren’t happy because they don’t see much improvement in depigmentation,” Dr. Hamzavi said. “But when you stop it from getting worse, people can learn to live with [the amount of depigmentation they have].”
More than half of patients in that study (2,078 of 3,541 [58.7%]) reported diagnosed mental health conditions, including anxiety (1,019 of 3,541 [28.8%]) and depression (866 of 3,541 [24.5%]). In particular, findings from the Patient Health Questionnaire–9 depression screener showed that 55.0% of patients (1,948 of 3,541) had moderate-to-severe depressive symptoms. Patients from India had the highest rates of these symptoms (271 of 303 [89.4%]) compared to patients from other regions.
“That's almost triple the average base of depression,” Dr. Hamzavi said. “This is not a disease that's just
a depigmentation. It's a disease of wellbeing and mental health.”
The rates of depression in vitiligo are correlated to the intensity of the depigmentation, darker skin types, and involvement of the face or hands, he said.
These are all variables that go into deciding whether a physician should treat a specific patient, Dr. Hamzavi said. “If a patient has a vitiligo patch on the chest, and they're not bothered by that at that time, or maybe their subculture doesn't consider it an issue, maybe you don’t want to treat. But if a physician starts seeing the tips of the fingers involved, or a little spot on the top of the forehead, maybe the physician has to get more aggressive [with treatment] if the patients would be bothered by it on their face. This speaks to the issue of stabilization.”
Categorizing vitiligo
The key differentiator for types of vi-
tiligo is whether it is segmental or non-segmental, Dr. Hamzavi said. When classifying patients, physicians should determine if their vitiligo is segmental—only present on one segment of the body—or nonsegmental, and whether it is focal, stable, or unstable.
Roughly 15% of vitiligo patients have the segmental variety, he said. This form is generally treated with traditional phototherapy and topical agents. If patients with segmental vitiligo do not respond to those therapies, surgical approaches are “dramatically effective in this population,” Dr. Hamzavi said.
Segmental vitiligo typically has a Blaschkoid distribution, and eventually “burns out”, with 85% of cases never progressing again, Dr. Hamzavi said.
He noted that it is important for physicians and patients to recognize the amount of time treatment takes to show results. It takes three to six
Please turn to Vitiligo page 20→
Anonprescription, doubleconjugated AHAretinoid (ethyl lactyl retinoate) cream may represent a treatment option for dermatology patients who were previously not candidates for retinoids due to tolerability. This product, marketed under the name AlphaRet Overnight Cream by L’Oreal, has been available in the U.S. for several years and is now available in Canada through skinbetter science (https://www.skinbetter.ca).
In interviews with The Chronicle of Cosmetic Medicine + Surgery (Autumn 2023; 11(1):2223), Drs. Sam Hanna and Sonya Abdulla (Toronto) discuss the challenges of retinoid treatment and features of an AHAretinoid that may make this type of treatment accessible to a wider patient population. Some of their key points include:
• Alpha hydroxy acids and topical retinoids are valuable tools in a dermatologist’s armamentarium; however, tolerability issues can make them unsuitable for some patients
• Dermatologists may recommend intermittent use of retinoids, such as reducing treatment frequency during the winter, and having patients pause use if they develop irritation, to manage tolerability


• Ethyl lactyl retinoate combines a retinoid with lactic acid, allowing for a slow release of the effects of both agents
• The lactic acid in the double conjugate molecule acts as a humectant, improving both skin penetration and hydration
• The slowrelease of the doubleconjugated molecule and the humectant effects of the lactic acid improve overall tolerability, making retinoid treatment more accessible to patients who have sensitive or rosaceaprone skin and
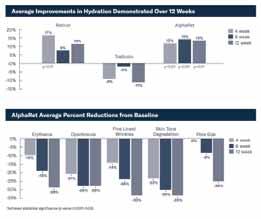
may not have previously been able to use retinoidbased skincare products
• A headtohead comparison study (Journal of Cosmetic Dermatology Dec. 2017; 16(4):542548) that compared AHAretinoid to tretinoin 0.025% cream and retinol 1.0% cream showed significant benefit by week 12 for AHAretinoid vs its comparators for four markers of sun damage. AHAretinoid also exhibited significantly better tolerability than the tretinoin, and comparable tolerability to the retinol

• AHAretinoid may be a way to introduce patients to a positive aging plan and to “protect the investments” that they are making if they are considering other noninvasive aesthetic procedures


Skinimages.ca is a comprehensive and easily accessible digital database of dermatology and dermatopathology images categorized according to six skin phototypes.

You are invited and encouraged to share your diagnostic expertise by submitting images to skinimages.ca. We accept high quality images, of at least two megabytes. Please use jpg or tif files. This open-access resource aims to create an educational database to raise the standard of care for patients of all skin types, fostering inclusivity and equity in dermatologic education. Your contributions can play a vital role in achieving this goal. If you have questions, please contact skinimages.ca at admin@derm.city

Dr. Yvette Miller-Monthrope is a Toronto based dermatologist and dermatopathologist. She is an assistant professor of medicine at the University of Toronto and the medical director of the pigmentation disorders clinic at Women's College Hospital. She has special interests in diverse skin types, inflammatory dermatoses, curriculum development and clinical-pathological correlation.
SUPPORTED BY




A review of factors influencing sensitive skin: an emphasis on built environment characteristics
Xiangfeng Chen,1 Jing Wen,2 Wenjuan Wu,1 Qiuzhi Peng,3 Xiangfen Cui,4,* and Li He,1,5,*
1Department of Dermatology, First Affiliated Hospital of Kunming Medical University, Kunming, China
2The Centre for Modern Chinese City Studies, East China Normal University, Shanghai, China
3Faculty of Land Resources Engineering, Kunming University of Science and Technology, Kunming, China
4Faculty of Environmental Science and Engineering, Kunming University of Science and Technology, Kunming, China
5Yunnan Institute of Skin Health, Kunming, China
*Correspondence: Li He, drheli2662@126.com; Xiangfen Cui, cui1987rainny@163.com
Keywords: sensitive skin, influencing factors, socioeconomic attributes, behavioral characteristics, natural environment, built environment
Background: Sensitive skin (SS) is a condition characterized by hyperreactivity. Impacting around 37% of the worldwide population and exerting an influence on the quality of life for affected individuals. Its prevalence rate has increased due to factors such as elevating stress levels and deteriorating environmental conditions. The exposome factors influencing SS have extended from demographic, biological attributes, and lifestyle to external environments. Built environments (BEs) have demonstrated as root drivers for changes in behaviors and environmental exposure which have the potential to trigger SS, but the review of the associations between BEs and SS is currently lacking.
Objective: This review aims to achieve two primary objectives: (1) Examine exposome factors that exert influence on SS at the individual and environmental levels. (2) Develop a theoretical framework that establishes a connection between BEs and SS, thereby offering valuable insights into the impact of the built environment on this condition.
Methods: An extensive literature search was carried out across multiple fields, including sociology, epidemiology, basic medicine, clinical medicine, and environmental research, with a focus on SS. To identify pertinent references, renowned databases such as PubMed, Web of Science, and CNKI were utilized.
Results: SS is the outcome of interactions between individual attributes and environmental factors. These influencing factors can be categorized into five distinct classes: (1) demographic and socioeconomic characteristics including age, gender, and race; (2) physiological and biological attributes such as emotional changes, skin types, sleep disorders, and menstrual cycles in women; (3) behavioural factors, such as spicy diet, cosmetic use, alcohol consumption, and physical exercise; (4) natural environmental features, including climate conditions and air pollution; (5) built environmental features such as population density, green space availability, road network density, and access to public transportation, also have the potential to affect the condition.
Conclusion: The importance of interdisciplinary integration lies in its ability to ascertain whether and how BEs are impacting SS. By elucidating the role of BEs in conjunction with other factors in the onset of SS, we can provide guidance for future research endeavors and the formulation of interventions aimed at mitigating the prevalence of SS.
INTRODUCTION
According to the World Health Organization’s projections, chronic non-communicable diseases (NCDs) are anticipated to account for a staggering 80% of an-
nually global deaths by 2030.1 This shift signifies a remarkable transition, with NCDs superseding infectious diseases as the primary drivers of the overall disease burden.2 Conditions such as obesity, cardiovascular diseases, and respiratory ailments are at the forefront of this transformative landscape.
Skin disease stands as one of the most prevalent human ailments,3 and many of them are also NCDs. Notably, an analysis conducted for the Global Burden of Disease Study in 2017 revealed that the rising population growth and aging demographics in China have led to a substantial disease burden associated with skin conditions.4 Among these conditions, sensitive skin (SS) represents a commonly encountered clinical symptom and sign, primarily manifesting on the facial region. When exposed to physical, chemical, and psychological stimuli, individuals often experience subjective sensations such as burning, tingling, itching, and tightness. Objective signs such as erythema, scales, and telangiectasia may or may not accompany these symptoms.5
In 2016, the International Pruritus Research Forum defined SS as the unpleasant sensation triggered by external stimuli that typically do not elicit skin symptoms.6 The etiology of SS remains elusive, potentially involving sensory nerve dysfunction,7 heightened vascular reactivity,8 barrier impairments,9 and immune-inflammatory mechanisms of the skin.10 Additionally, the surge in SS cases is associated with environmental pollution and unhealthy lifestyles. Globally, the prevalence of SS is estimated at 36.9%,11 with some regions reporting prevalence rate as high as 50 to 70%. The presence of SS may negatively impact the quality of life for affected individuals.12 Lower self-confidence, mental disorders13 and the economic burdens resulting from its high prevalence and recurrent nature impose substantial hardships on patients.
The interconnection between health and the environment has garnered increasing attention, particularly in the realm of public health research concerning the built environments (BEs). The BEs encompass the manmade spaces in which individuals engage in daily activities, work and leisure.14 Empirical studies have extensively linked BEs to a range of health-related behaviors,15,16 mental conditions,17,18 NCDs such as obesity,19 cardiovascular disease,20 and respiratory disease.21 Despite the growing body of research, the relationship between the BE and SS remains understudied. Previous epidemiological investigations on SS predominantly focus on individual
sociology and lifestyles of the population, including age, gender, dietary habits, and cosmetic usage as well as natural environmental stressors such as sun exposure, air pollution, and temperature.22,23 This review aims to address the aforementioned research gap by providing a comprehensive profile of the influencing factors at individual and environmental levels. Furthermore, this study also puts forward a theoretical framework to elucidate the potential pathways linking the BEs to SS based on the established mechanisms that underpin the associations between BEs and health.24,25
We conducted systematic searches in reputable databases, including PubMed, Web of Science, and CNKI (China National Knowledge Infrastructure), to identify relevant references published since 1997. The search strategy employed multiple combinations of the terms “sensitive skin” within the title/abstract, encompassing epidemiology, prevalence, socioeconomics, gender, ethnicity, skin type, emotional change, menstrual cycle, sleep, diet, spicy food, cosmetics, smoking, drinking, exposure, sun exposure, temperature, humidity, particles, pollution, and the built environment. Our literature review did not uncover any studies directly addressing the built environment and SS. However, we did find evidence suggesting that the occurrence of SS is associated with exposure to natural environment, mental conditions, and patterns of sleep and diet, all of which have been linked with BEs. Additionally, we checked the references cited in the identified papers to ensure the inclusion of all pertinent literature. The evaluation process involved assessing the title and abstract against our inclusion criteria.
Subsequently, a full-text review was conducted to determine if the article met our standards. Inclusion criteria comprised studies written in English that focused on the epidemiology of SS. Studies that did not specifically focus on SS were excluded. The flowchart (Figure 1) depicted the process for the inclusion and exclusion of literature.
As illustrated in Figure 1, our literature review did not uncover any studies directly addressing the built environ-

ment and SS. However, we did find evidence suggesting that the occurrence of SS is associated with exposure to natural environment, mental conditions and patterns of sleep and diet, all of which have been linked with BEs. As a result, the scope of our search was broadened to incorporate the term “built environment” in conjunction with factors such as air pollution, sun exposure, mental conditions such as anxiety and depression, and lifestyle elements like sleep and diet (Figure 1). The influencing factors can be classified into five categories: (I) demographic and socioeconomic attributes; (II) physiological and biological characteristics; (III) lifestyles; (IV) natural environmental features; (V) built environmental features.
Age
Research indicates a higher prevalence of SS in the young group than their elder counterparts. Notably, a French epidemiological survey comprising 5,000 individuals revealed that individuals under the age of 35 years exhibit a higher prevalence of SS, surpassing 60% of the population within this age range.26 Similarly, a survey conducted in South Korea found that the younger group ranging from 15 to 44 years old displays a greater likelihood of developing SS compared to individuals over the age of 45.27 Correspondingly, another study involving 22,085 women in China revealed that the younger group, specifically those aged 20 to 30, is more susceptible to sensitive or highly SS in comparison to the elder group, aged 30 and above.28 These findings suggest a plausible mechanism wherein the nerve innervation function in the human body, related to touch and pain, diminishes as individual age.29
Extensive empirical studies have consis-
there was no significant difference between the socio-professional categories in SS.39 Hence, further research is required to shed light on the influence of occupation on SS.
Emotional change
Emotional change has been identified as a contributing factor to the development of SS.32,34 Individuals with SS are more likely to experience discomfort, such as tingling and itching, during the periods of emotional fluctuation compared to individuals without SS.27 Moreover, there is a significant correlation between the occurrence of SS and anxiety, suggesting that anxiety may play a role in the manifestation of SS symptoms.13 Additionally, depression has been associated with SS, where facial flushing is recognized as the primary clinical manifestation.31
Spicy food
Capsaicin, a biologically active component found abundantly in peppers, interacts with the Capsaicin receptor, a transmembrane channel protein widely expressed in skin tissue.50 The activation of the Capsaicin receptor, known as TRPV1, stimulates the release of neuropeptides and excitatory amino acids from free nerve endings, ultimately leading to the sensation of pain in the cerebral cortex.51 Studies have revealed that individuals of Asian descent exhibit increased susceptibility to SS when exposed to the stimulation of a spicy diet.35 A survey conducted among college students in China further confirmed that a spicy diet serves as a risk factor for SS.32 Moreover, experimental evidence has demonstrated that inhibiting the expression of TRPV1 can be effective in treating SS.52
tently shown that women are more prone to SS than men. Notably, a study based on 3,012 participants in India found that the proportion of women experiencing “sensitive” or “very sensitive” skin is significantly higher (36.7%) compared to the men (27.9%).30 These findings are consistent with multiple investigations conducted domestically and internationally, which consistently demonstrated that women are more likely to develop SS than men.23,31,32 One plausible explanation for this disparity could be the significant differences in epidermis and dermis thickness between males and females,33 with males exhibiting a greater thickness. Consequently, the skin of males is less permeable than that of females, making it less susceptible to the effects of irritants or allergens. Additionally, the periodic hormonal fluctuations experienced by women contribute to increased SS.34
While no significant racial differences were observed in the prevalence of SS, variances in sensory perception among different races have been documented. For instance, European Americans tend to exhibit heightened sensitivity to wind, Asians are more sensitive to spicy food, and Hispanics display relatively lower responsiveness to alcohol.35 There are also reports suggesting that African Americans have a higher incidence of SS compared to European Americans.36 As human skin exhibits individual differences, further parallel studies are required to ascertain the true racial disparities in SS.37
Medical personnel wear masks for extended durations while on duty, and studies have documented skin-related symptoms, such as redness and itching, associated with mask-wearing among medical staff.38 However, a survey revealed a prevalence of SS found that
Compared to neutral skin, dry, oily, and mixed skin exhibit varying degrees of damage to the skin barrier function, rendering them more susceptible to SS and inflammatory skin diseases.40,41 Epidemiological studies have further confirmed that these skin types are risk factors for SS diseases.28,42
Individuals with poor sleep quality exhibit an increase in transepidermal water loss (TEWL) compared to those with good sleep quality, consequently leading to the damage of skin barrier.43 Sleep disorders contribute to an elevation in oxidative stress, resulting in alterations in skin homeostasis and the disruption of inflammatory pathways, ultimately leading to the dysfunction of the skin barrier.44,45 Impaired skin barrier function and reduced water content in the stratum corneum are significant pathophysiological characteristics observed in individuals with SS.46 An epidemiological survey conducted across multiple countries, including Brazil, China, France, Russia, and the United States, found a higher prevalence of SS among subjects with sleep disorders.47
The presence of estrogen receptors in the epidermis impacts skin hydration and the functionality of skin barrier, as estrogen levels directly influence these factors.48 Muizzuddin’s research demonstrated that the strength and dryness of skin barrier, as well as the sensitivity to lactic acid stinging, vary in response to fluctuations in estrogen levels during the menstrual cycle.49 A questionnaire survey involving Dutch women revealed that approximately 42% of premenopausal women experienced an increased sense of SS prior to and during the menstrual cycle.34
Cosmetic usage
Research indicates a positive correlation between the frequency of cosmetic usage and the prevalence of SS.53 Specifically, when women utilize multiple types of cosmetics and makeup removers on a daily basis, it can easily trigger SS.28 Brenaut carried out a metaanalysis of 13 surveys, which collectively identified cosmetics as a common trigger for SS, and excessive or improper usage exacerbating this reaction.54 One potential explanation for this phenomenon is that frequent and simultaneous use of cosmetics may thin the stratum corneum on free ending is compromised, leading to a significant increase in nerve sensation input and signal release, resulting in uncomfortable sensations.55 Additionally, a thinner stratum corneum can enhance the penetration of capsaicin, thereby increasing SS.56
Pavithra carried out a proteomic analysis on primary human keratinocytes exposed to long-term cigarette smoke condensate, revealing that the differentially expressed proteins were predominantly associated with the integrity of the epithelial barrier and the anti-inflammatory response.57 Moreover, excessive smoking over 20 cigarettes per day for at least two years can disrupt the homeostasis of the epidermal permeability barrier.58 Studies simulating cigarette smoke exposure have further shown that prolonged and/or repeated exposure to high levels of toxic smoke pollutants can impair the function of the epidermal barrier.59 Multiple epidemiological investigations have also confirmed a positive correlation between smoking and the prevalence of SS.60,61
Epidemiological studies have established a link between alcohol consumption and an increase in the prevalence of SS.35 It is believed that the decompo-
Figure 1: Flowchart for literature selection.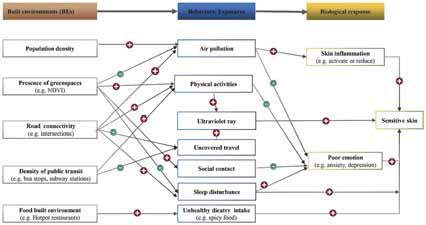
sition of ethanol into acetaldehyde induces vasodilation, leading to facial burning and flushing.62,63
Prior research has demonstrated that various stimuli, including pain sensation, may undergo changes during and after exercise, potentially attributed to the activation of exercise-induced opioid substances.64 Limbs exhibit a decrease in skin thermal sensitivity only after high-intensity exercise.65 The tingling, burning and itching symptoms associated with SS are also connected to sensory nerve dysfunction in the skin.66 In addition, research has found that spending more time exercising is associated with a lower risk of developing depression,67which potentially reducing susceptibility to SS.31
Environmental features encompass natural elements, which are those aspects of the environment existing without significant human modification or intervention. This category comprises variables such as sunlight exposure, temperature and humidity, and air pollutions.68
A large body of literature has examined the effects of ultraviolet (UV) rays from sunlight on the skin. UV rays are categorized into UVA, UVB, and UVC based on their wavelengths, with UVC being absorbed by the ozone layer.69 UVA primarily impacts the dermis and promotes oxidative damage to DNA, while UVB mainly affects the epidermis.70 Studies have indicated that exposure of human keratinocyte to UVB radiation can disrupt the hydration of stratum corneum.71Numerous experiments utilizing UVB irradiation on epidermal mice have revealed epidermal barrier dysfunction, including increased epidermal thickness, elevated TEWL, and reduced water content in the stratum corneum.72,73 Furthermore, UVB radiation induces oxidative damage and trig-
gers inflammatory reactions to keratinocyte on the skin surface,74-76 herein contributing to the development of SS.
A survey performed on the Chinese population highlighted the gender and radiation dose-related changes in stratum corneum function caused by ultraviolet radiation.77 Building upon this, Francesca and his collaborators discovered a significant cumulative effect of UV and O3 in reducing skin barrier-related proteins, such as silk fibroin and skin protein.78 Epidemiological investigations have confirmed that sunlight represents a significant factor influencing the prevalence of SS.32,79,80
Temperatures exceeding 43°C have been shown to directly activate TRPV1.81
TRPV1 is a specific member of the transient receptor potential (TRP) superfamily of ion channels which are found in various tissues throughout the body.
TRPV1 leading to the sensation of heat and pain.50 Research has found that the expression of TRPV1 in SS is enhanced, leading to overload of harmful stimuli.82 Therefore, patients are prone to experiencing abnormal heat and pain sensations. In the case of SS, inflammatory mediators can significantly lower the activation threshold of TRPV1.83
Epidemiological studies have identified changes in temperature and humidity as triggering factors for SS.54,80 Individuals with SS are particularly sensitive to TEWL and ambient temperature.84 Research has demonstrated that low humidity is more likely to induce SS.23,54
The prevalence of SS has been associated with air pollution.22,85 Among air pollutants, fine particulate matter (PM2.5) has been extensively studied. PM2.5 exposure in human keratinocytes has been shown to increase Cyclooxygenase-2 (COX-2)/Prostaglandin E2 (PGE2) levels, leading to the downregulation of expression of silk fibroin.86,87 Treatment of human and mouse skin equivalents with PM2.5 has also been found to inhibit the
expression of fibronectin and increase TEWL, thus compromising the integrity of the skin barrier.88 Additionally, PM2.5 can disrupt the morphology and structure of keratinocyte, further compromising the skin barrier.89 Previously, it has been found that exposure to nitrogen dioxide (NO2) increases the TEWL value of skin, leading to damage to the skin barrier.90 Low concentration of carbon monoxide (CO) can inhibit the release of tumor necrosis factor-α,interleukin-1β, and interleukin-10 reducing inflammatory response, therefore CO may reduce damage to the skin barrier,91 It has been shown that ozone (O3) exposure will lead to various skin inflammation through redox pathway,92 At the same time, O3 therapy can be applied to the clinical treatment of various inflammatory skin,93,94 but its role in SS needs further research. Air pollution can cause anxiety in people,17 and the prevalence of SS is significantly correlated with anxiety.13
DISCUSSION
Environment encompasses natural environment and built environment, the built environment is defined as encompassing all buildings, spaces, and products that are created or modified by people.14 Factors within this domain include population density, the availability of green spaces, access to food stores, and the connectivity of streets.95
The growing body of evidence supports the notion that the BEs plays a significant role in development of NCDs through changes in environmental exposure and health-related lifestyles. For instance, individuals residing in densely populated communities often face a higher risk of obesity.96 As reported, a densely populated community are likely to emit more air pollutants97 that contribute to an increase in risk of obesity.98,99 Moreover, population density has a positive correlation with PM10 concentration,100 and elevated PM10 levels have been shown to compromise

lung function,101,102 consequently impacting cardiovascular health.103 Interestingly, research have indicated that an increase in coverage ratio of greenspaces benefits to lower the prevalence of obesity,104 hypertension and cardiovascular disease,105,106 as well as reduce the mortality of cardiovascular disease.107,108 This relationship can be attributable for that urban greenness promotes physical activity109 and mitigates exposure to PM2.5.110 A survey conducted in Apulia found the impact of green space use on depressive symptoms, and the mediating role of perceived social support in the association.111 Nighttime artificial light (ALAN) has emerged as a risk factor for physiological functions, with a significant correlation observed between higher levels of nighttime outdoor light and poor sleep patterns.112 Notably, Artificial Light at Night (ALAN) is likely to reduce sleep duration,113 which is more prevalent in communities with higher poverty levels.114 Moreover, sleep disturbance may play a role in anxiety and depressive disorders.111 Besides, research studies have demonstrated that the exposure to ALAN during adolescence could potentially elevate the risk of developing atopic diseases during youth.115 Further research is warranted to substantiate causal relationships, particularly those related to circadian rhythm disorders and endocrine pathways. Additionally, a high density of road intersections increases the likelihood of walking and cycling.116 Utilizing public transportation necessitates walking or cycling to bus transits, resulting in elevated levels of moderate physical activity.117,118 As observed, physical inactivity in both adults and children elevates the risk of overweight/obesity.119-121 Conversely, engaging in physical activity helps to decrease the prevalence and mortality of cardiovascular disease.122,123 Furthermore, a higher density of fast food restaurants has been associated with a greater prevalence of obesity124 due to the residential surrounding food BEs have potentials to alter residents’ dietary behavior and quality,125,126 thereby affecting their health.
Overall, the BEs exerts an influence on individual health through changes in exposure to environmental hazardous stressors and health-related lifestyles.25 SS, identified as a common clinical symptom, results from various internal and external factors. Given the close relationships between BEs and individuals’ daily routines, it is plausible that BEs may also have potential impacts on SS.
The relationship between the BEs and the development of SS has not yet been fully explored. Based on identified pathways from BEs to other NCDs, our study aims to establish a theoretical framework connecting BEs and SS, providing
Figure 2: Potential pathways linking BEs to SS. The plus and minus signs in the chart represents positive and negative associations between the two linked variables. NDVI corresponds to the normalized difference vegetation index.a scientific foundation for future epidemiological investigations, basic research, and clinical studies. As previously mentioned, SS development may be influenced by factors such as population density, the availability of green space, street design, and the food environment, Additionally, natural environmental exposure and individual behaviors serve as mediating pathways that can contribute to human skin inflammation and the emergence of adverse emotions, ultimately culminating in the manifestation of SS. When skin inflammation occurs, a substantial quantity of inflammatory cytokines and chemokines is released, leading to heightened sensitivity of nerve fibers within the epidermis and an increased responsiveness to external stimuli.127,128 The association between negative emotions, such as anxiety and depression, and SS has primarily been explored through epidemiological surveys, which have demonstrated a positive correlation. However, there remains a dearth of experimental research evidence on this subject (Figure 2).
Exposure to PM2.5 and emotional change are likely to exhibit mediating role in the association between Population density and SS. High population density has been found to be correlated with an elevated risk of anxiety.129,130 Notably, anxiety itself has been linked to a higher likelihood of developing SS.13 Furthermore, studies have indicated that as the population density of cities increases, so does the concentration of PM2.5.131 Through experimental verification, researchers have demonstrated that PM2.5 can activate the skin’s inflammatory process, resulting in the release of inflammatory factors such as TNF-a and IL-1. This activation can trigger skin nerve fiber sensitivity and impede the repair of the damaged skin barrier.132,133 Hence, it can be inferred that high population density may contribute to an increased prevalence of SS by elevating anxiety levels and raising PM2.5 concentrations.
Urban intervention of greenspace was anticipated to promoting general, mental and physical health. The influence of green spaces on mitigation of the particulate matter concentrations has been extensively researched, revealing various mechanism that are contingent upon environmental and vegetation characteristics.134 A study conducted in Spain involving 39 schools found that higher levels of greenery within and surrounding schools are correlated with reduced levels of traffic-related pollutants.135 Increased levels of ambient particulate matter have been linked to a higher prevalence of SS.136 Moreover, poor emotions such as depression, anxiety, and stress137 have been recog-
nized as risk factors influencing SS.138 Empirically, urban green spaces have been reported to encourage residents to engage in physical activities,139,140 which helps to alleviate anxiety,141 thereby protecting against the occurrence of SS. Given the aforementioned association, it is speculated that green spaces could reduce ambient air pollution and increase outdoor activity time, thereby lowering the prevalence of SS through the reduction of exposure to air pollution and alleviation of anxiety levels. In addition, higher tree canopy cover was associated with more favorable sleep,16 so it is speculated that green spaces can reduce SS by improving sleep.
Additionally, a significant statistical correlation has been observed between the proximity of green spaces to residences and the indoor microbial diversity index.142 Exposure to urban green spaces has the potential to increase the diversity of skin microorganisms and alter the composition of human microbiota.143 However, the results from different studies examining the differences in microorganisms between SS patients and normal individuals have been inconsistent.144,145 Consequently, further research is warranted to ascertain the alterations in microorganisms associated with SS.
The density and connectivity of the road network and the availability of public transits play a significant role in influencing residents’ travel mode.146,147 Although encouraging physical activities, active modes of travel, such as walking and cycling, can increase exposure to ultraviolet radiation, which has been shown to potentially trigger SS conditions. Conversely, motorized modes of travel like busses, self-driving, and subways reduce physical activities but can minimize exposure to ultraviolet radiation. People have experienced higher exposure to air pollutants at intersections,148 and dense intersections have adverse impacts on sleep.149 Therefore, it is speculated that intersections could increase ambient air pollution and sleep disturbance, thereby potentially increasing the prevalence of SS.
A spicy diet is a potential risk factor for SS. Health status is associated with the local food environment.150,151 The proliferation of hotpot and barbecue establishments in residential and workplace areas may contribute to increased consumption of spicy foods, thereby potentially influencing the occurrence of SS. The number of hotpot and barbecue shops serves as an indicator of the built environment, but empirical research is necessary to determine their impact on SS.
SS, characterized by heightened skin reactivity, is influenced by various internal and external factors. Our study indicates
a higher prevalence of SS among women compared to men, with its occurrence diminishing with age. Emotional fluctuations, skin type (dry, oily, or mixed), sleep disturbances, menstrual cycles, consumption of spicy foods, improper cosmetic use, smoking, alcohol consumption, and physical activity also impact SS. Furthermore, environmental factors such as sun exposure, airborne particulate matter, temperature, and humidity contribute significantly. Notably, the connection between the built environment and SS has not been previously explored. Hence, an analysis has been undertaken to summarize the influence of the built environment on individual behavior and the natural environment, with the objective of uncovering a potential indirect connection between the built environment and SS (refer to Figure 2 for comprehensive details).
Health outcomes result from intricate interactions between human biology and the environment. Existing research demonstrates that gene–environment interactions can influence various chronic conditions like obesity,152 cardiovascular diseases,153 and respiratory disorders.154 Recent genome-wide association studies have identified genetic variations in the 2p21 region associated with self-reported SS in the Han population.155 Moreover, Yang et al. reported reduced expression of CLDN5 in the facial skin lesions of SS patients from the Han population compared to unaffected individuals.156 Nonetheless, further scientific validation is required to ascertain the extent to which gene–environment interactions contribute to the development of SS.
The comprehension of how the built environment influences health constitutes an essential component in the development of effective strategies geared toward the promotion of physical and mental well-being. Lifestyle factors, encompassing engagement in sports activities, dietary choices, and stress levels, are all subject to influence by the building environment, and they hold a pivotal role in the management of chronic diseases. The creation of an environment that fosters healthy behaviour has the potential to contribute to the management of diseases such as obesity, cardiovascular disease, and skin diseases. The skin, functioning as the interface between the human body and the environment, is notably susceptible to the influences of the built environment. Understanding how building environments impact skin diseases is crucial for comprehending the role of environmental factors in skin health. This knowledge, once acquired, can provide valuable insights for urban planning decisions, inform public health interventions, and guide individual behaviours to cultivate a skin-friendly environment, thereby contributing to the reduction of the prevalence and severity of skin diseases.
This article explores the potential indirect relationship between the built environment and SS by investigating traditional factors influencing SS and the impact of the built environment on individual behaviour and the natural surroundings. To establish such associations, a comprehensive approach encompassing geography, public health, and clinical medicine is necessary. We recommend conducting a large-scale epidemiological survey on SS, analyzing epidemiological data, and delving into the pathways and mechanisms through which the built environment influences SS. Ultimately, enhancing the built environment can serve as an effective strategy for the prevention and management of SS.
XCh: Writing – original draft, Data curation, Formal analysis, Methodology, Supervision, Writing – review and editing. JW: Data curation, Methodology, Writing – review and editing, Formal analysis. WW: Data curation, Formal analysis, Methodology, Writing – review and editing. QP: Methodology, Writing – review and editing. XCu: Methodology, Resources, Supervision, Writing – review and editing. LH: Funding acquisition, Methodology, Resources, Supervision, Writing – review and editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Yunnan Province Clinical Center for Skin Immune Diseases (ZX2019-03-02) and Yunnan Province Clinical Research Center for Skin Immune Diseases (2019ZF012).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10. 3389/fpubh.2023.1269314/full#supplementary-material
Please visit Derm.city for a complete list of references.
Chronicle's digital audio, e-newsletters, and web portal keep physicians updated reliably 24/7. Each is worthy of your time. And they're available without charge. Find them all at https://linktr ee/dermcity

Since 2015, derm.city has been a leading hub and repository for dermatology information and interactive knowledge-exchange in video, text, images, and audio. It's the official site of The Chronicle of Skin & Allergy, now newly enhanced with added useful features. Thrice weekly updates on the latest findings in dermatology, summarized for quick learning. Visit derm.city at https://derm.city
A dermatology newsletter focused on ethnodermatology care from top physicians in the field, delivered to your inbox every Monday.
Supported by Bausch Health Canada


A biweekly newsletter on clinical and social issues affecting female patients and physicians, delivered straight to your inbox.
Supported by Galderma Canada
Dr. Geeta Yadav and expert dermatologists discuss clinical developments, news, trends and myths in acne treatment and research. First season of three episodes now available for listening and downloading.
Supported by Cipher Pharmaceuticals

a skin spectrum podcast

Dr. Neil Shear, dermatologist and Professor Emeritus at the University of Toronto, speaks with many guests from the world of dermatology, including Dr. Boluwaji Ogunyemi, Dr. Marc Bourcier, and Dr. Rachel Asiniwasis, to hear their stories and insights.
Dr. Ron Vender delves into recent psoriasis studies and comments articles about the efficacy of PASI scores, intermittent fasting for psoriasis, and biologic fatigue.
Supported by Sun Pharma Canada


weeks for immunology to stabilize with topical treatments and then six to 12 weeks more for the first melanocytes to start repopulating the area, he said. “So don’t change the course of treatments too quickly, unless the patient becomes unstable.”
Koebnerization, confetti-like lesions, and trichrome vitiligo—lesions with a partially-depigmented band between normal and depigmented regions—are three variables that indicate instability in vitiligo, Dr. Hamzavi said. Those signs are also components of the Vitiligo Signs and Activity Score (VSAS), he added.
Physicians should consider doing a full skin examination for their patients, even if the patient only expresses concern about a particular lesion in a visible area, Dr. Hamzavi said. If any of the three signs of instability are present, the patient’s vitiligo will progress.
He noted that acral vitiligo should be considered an “emergency.”
“If a physician starts seeing fingertip involvement, they must treat aggressively. Once the pigment is lost from the fingers, treatment will not repigment that back with any [treatment] available today,” he said. Hopefully, there will be advances in treatment but at this time acral vitiligo cannot be repigmented with the available options
As part of any vitiligo treatment regimen, it is important for physicians to take photographs of the patient’s skin at all stages, Dr. Hamzavi said. “You need pictures because patients will forget what their lesions used to look like. They will tell you it's not even better at all.”
Photographs not only support a physician’s credibility to patients
they aid physicians in knowing when to adjust treatments, he said.
Topical calcineurin inhibitors are likely the gold standard of treatment due to their low cost, but ultra-potent topical steroids 14 days out of a month are also an option, Dr. Hamzavi said. Topical Janus Kinase (JAK) inhibitors are not currently available for vitiligo in Canada, he said, but may become available in the country soon “we hope.”
Maintenance is also important, Dr. Hamzavi said, citing a study of calcineurin inhibitors. That study found that among patients who stopped treatment completely after repigmentation, 40% had their vitiligo relapse. In contrast, only 9% of patients who continued with maintenance treatment with the same calcineurin inhibitor twice a week relapsed.
Because of the long time from the start of treatment to repigmentation, and the risk of relapse, physicians should “view vitiligo as a scar that you want to avoid,” said Dr. Hamzavi. He compared it to articular change in arthritis or sinus tunnel formation in hidradenitis suppurativa. “You want to avoid that as much as possible.”
Ongoing maintenance therapy will also likely be needed for patients successfully repigmented with systemic IL-15 inhibitors, he said.
Another factor to consider while managing a patient with vitiligo is thyroid disease. “In our clinical experience. If you don’t control the thyroid disease, it’s harder for the clinical response [to vitiligo treatment] to occur,” said Dr. Hamzavi.
Phototherapy is a crucial part of vitiligo management as it is currently the only way to encourage melanocytes in depigmented areas

so repigmentation can occur, Dr. Hamzavi said.
“We will need to find some way to move the melanocytes, and [phototherapy] is the best we've got,” he said. “If a physician can’t do phototherapy today, they can’t treat most vitiligo patients.”
Phototherapy can be provided in the office setting or home-use units are available, he said, and it can be combined with topical calcineurin inhibitors or oral steroids. Some extension studies of phase II research on topical JAK inhibitors have shown combination with phototherapy seems to be safe and more effective in a small group of patients, but more research is needed to fully assess safety and efficacy, he said.
“Phototherapy, in general, works better for the face, and narrowband works better than PUVA [psoralens plus ultraviolet-A]. And in general, it takes about 12 months to see that optimal result,” said Dr. Hamzavi.
Most patients begin to show response to phototherapy after 24 sessions, and stabilization can take up to 72 sessions. If a patient is not responding after 24 sessions, they are probably not going to respond to phototherapy.
Many systemic agents are approved for managing vitiligo, with different biological targets and their strengths and weaknesses, Dr. Hamzavi said.
These include systemic corticosteroids, azathioprine, methotrexate, mycophenolate mofetil, cyclosporine, and minocycline.
“Oral minipulse steroids are the gold standard today,” he said. “That is two to four milligrams of dexamethasone on Saturday and Sundays at eight o’clock in the morning to try to match the cortisol cycles. That in
combination with phototherapy is helpful because it takes three months for phototherapy to kick in. So if this combination is employed on unstable disease, it can dramatically improve the patient’s condition. But the physician must do both because the oral steroids will continue until the phototherapy can kick in. And then the phototherapy must be maintained.”
Other systemic agents Dr. Hamzavi mentioned that are being explored but are not yet approved include the JAK inhibitor upadacitinib, the JAK-3 / tyrosine kinase inhibitor ritlecitinib, an IL-15-targeting antibody, and the melanocortin 1 receptor agonist afamelanotide.
Surgical therapy
There are a range of surgical options for vitiligo, Dr. Hamzavi said.
He cited a systematic review (JAMA Dermatol 2021; 157(3):307316) that evaluated a range of these options for safety, efficacy, and costeffectiveness.
“Split skin grafting or non-cultured epidermal suspension (NCES) were the preferred options for surgery [in that paper],” he said. He noted that punch and blister grafting approaches are used less often in North America. NCES are now approved by the U.S. Food and Drug Administration for the treatment of vitiligo, he said.
Finally, Dr. Hamzavi said physicians should not forget the mental health of their patients with vitiligo
“You are treating their wellbeing. Sometimes just being that person who listens to them and acknowledges their discomfort can also be helpful. That's the primary target. It is not the depigmentation, it is the person in front of you. Be patient, research into vitiligo is picking up steam.”
Have a comment about the articles in this issue?
Share your knowledge and opinions with peers worldwide.
EVALUATING THE UTILITY OF DLQI IN RANDOMIZED CONTROLLED TRIALS
Researchers conducted this review to generate further evidence of the Dermatology Life Quality Index’s (DLQI) utility in randomized controlled trials and to cover all diseases and interventions. They screen 3,220 publications published from Jan. 1, 1994 to Nov. 16, 2021. Of those, 454 were included for analysis, comprising 198,190 patients.
The minimal clinically importance difference (MCID) was reported in the analysis of 15.0% of studies, but only 1.3% considered full DLQI score. Forty-seven (10.4%) of the studies investigated statistical correlation of the DLQI with clinical severity assessment or other PRO/quality of life tools; and 61–86% of studies had within-group scores differences greater than the MCID in ‘active treatment arms’. The Jadad risk-of-bias scale showed that bias was generally low, as 91.8% of the studies had Jadad scores of ≥ 3; only 0.4% of studies showed a high risk of bias from randomization. Some 13% had a high risk of bias from blinding and 10.1% had a high risk of bias from unknown outcomes of all participants in the studies. In 18.5% of the studies the authors declared that they followed an intention-to-treat protocol; imputation for missing DLQI data was used in 34.4% of studies.
J Vyas, J R Johns, F M Ali, R K Singh, J R Ingram, S Salek, A Y Finlay: A systematic review of 454 randomized controlled trials using the Dermatology Life Quality Index: experience in 69 diseases and 43 countries, in the British Journal of Dermatology (March 2024; 190(3):315–339).
PREVENTING LASER-INDUCED PIH WITH ISOBUTYLAMIDO THIAZOLYL RESORCINOL
This study evaluates the efficacy and safety of isobutylamido thiazolyl resorcinol (ITR) for the prevention of laser-induced post-inflammatory hyperpigmentation (PIH). Some 24 subjects with solar lentigines were included. Three lentigines on each patient were randomized to treatment with ITR twice daily, once daily, and no application for 2 weeks. Thereafter, physicians treated the lentigines with 532-nm QS Nd: YAG laser. Four weeks postlaser treatment, PIH incidence was significantly lower in the ITR twice-daily group compared to the no-application group (20.83% vs. 50%, p=0.028). There was no statistically significant difference in relative melanin index, mean luminance score, and hyperpigmentation score between treatments at all visits. No serious adverse events were reported.
V Vachiramon, N Sakpuwadol, T Yongpisarn, T Anuntrangsee, P Palakornkitti: Efficacy of isobutylamido thiazolyl resorcinol for prevention of laser-induced post-inflammatory hyperpigmentation: A randomized, controlled trial, in Journal of Cosmetic Dermatology (March 18, 2024, online ahead of print)

What are the lesions on this patient’s neck?
A . Scleroderma B. Vitiligo
C. Chemical leukoderma
D Nevus anemicus
THE EDITORS invite your participation in this regular feature of the journal. Please send all images and correspondence to:
Medical Editor, The Chronicle of Skin & Allergy 1460 The Queensway, Suite 212, Etobicoke, Ont. M8Z 1S4 Telephone: (416) 916-2476
E-mail: health@chronicle.org
An article on the website Cosmetic Business (Mar.14, 2024) reports that Gen Alpha, a generation of kids born after 2010, has recently taken the spotlight. Despite their young age, their intense interest in skincare routines sparks both fascination and concern among adults. According to the article, Gen Alpha’s beauty industry debut has not been positive, with the ‘Sephora kids’ controversy and 10-year-olds adopting multi-step skincare routines using products designed for aging skin. The publication also notes that Gen Alpha’s active engagement with social media allows them to explore and discover new beauty brands, trends, and products, often seeking guidance from influencers, customer reviews, and even experts. Additionally, they often turn to millennial parents and Gen Z siblings for information and product access.
In an article on the Cleveland Clinic website (Mar.14, 2024), Dr. Christine Poblete-Lopez, a dermatologist based in Cleveland, emphasizes the importance of identifying potential signs of melanoma in moles on the skin. Dr. Poblete-Lopez says that while most moles are harmless and nothing to worry about, it is important to watch for certain variations that may indicate the development of melanoma. She introduces the ABCDEs of skin cancer—asymmetry, border irregularity, colour variation, diameter, and evolution—as key indicators to watch for. Dr. Poblete-Lopez also advises seeking medical attention if any of these characteristics are observed in moles, particularly if there are changes or if new moles appear. Additionally, she discusses factors that may increase melanoma risk, such as numerous moles, history of indoor tanning, fair skin, and family history of melanoma, highlighting the importance of regular skin selfchecks and dermatologist visits for early detection and treatment.
In a Medscape (Mar. 22, 2024) article, Dr. Howa Yeung, assistant professor of dermatology at Emory University in Atlanta, discusses the unique care required for transmasculine patients with acne, emphasizing the impact of hormone therapy on skin health and mental well-being. According to Dr. Yeung, testosterone therapy significantly increases the risk of acne, even in adults, with data showing a rise in acne diagnoses following hormone initiation. Various studies highlight the prevalence and characteristics of acne in transmasculine individuals, including its association with serum testosterone levels, body mass index, and smoking. Specifically, Dr. Yeung mentioned a 2021 study he co-authored that linked current moderate to severe acne in transmasculine patients taking testosterone to higher levels of depression and anxiety. Additionally, the use of chest binders, although beneficial for self-esteem, can contribute to skin issues.
An NBC News (Mar. 11, 2024) article reports that the American Academy of Dermatology faced controversy in February when dozens of members proposed ending its diversity, equity, and inclusion (DEI) programs, arguing they could do more harm than good. This sparked debate within the organization, with many dermatologists expressing opposition to the resolution. Ultimately, the academy’s advisory board voted against the proposal and instead decided to expand its mission to prioritize diversity and address inclusion issues within the field. The decision follows testimony from several dermatologists of many races who opposed the resolution, highlighting the importance of DEI initiatives in strengthening dermatology programs. Black dermatologists, who make up only 3% of dermatologists in the U.S., see the decision as a step forward in promoting diversity and addressing racial disparities within the field.
The 昀rst and only PDE4i indicated in the topical treatment of plaque psoriasis*

FOR AGES 12+
ZORYVE is indicated for topical treatment of plaque psoriasis, including treatment of psoriasis in the intertriginous areas, in patients 12 years of age and older.
Designed for simple administration
• Can be used on all affected areas, including intertriginous areas
• Once-daily topical application
Please consult the Product Monograph at http://arcutis.ca/zoryvepm-hcp for contraindications, warnings, precautions, adverse reactions, interactions, dosing, and conditions, of clinical use. The Product Monograph is also available by calling us at 1-844-692-6729.
PDE4i: phosphodiesterase-4 inhibitor
*Comparative clinical signi昀cance has not been established. †Subject to restrictions. For program terms and conditions go to www.zoryveassist.ca and click Terms and Conditions.
Reference:
1. ZORYVE Product Monograph. Arcutis Biotherapeutics, Inc. April 27, 2023.
The ZORYVE AssistTM Patient Assistance Program is designed to provide 昀nancial support to eligible patients receiving a ZORYVE prescription.†
When your patient presents with moderate-to-severe plaque psoriasis,
TREMFYA® (guselkumab) is indicated for the treatment of adult patients with moderate-to-severe plaque psoriasis who are candidates for systemic therapy or phototherapy.1

TREMFYA® is also indicated for the treatment of adult patients with active psoriatic arthritis. TREMFYA® can be used alone or in combination with a conventional disease-modifying antirheumatic drug (cDMARD) (e.g., methotrexate).1
TREMFYA® provincial funding is now available in most provinces for patients with PsO or PsA.1,2-10 *
Restrictions may apply. Refer to the respective provincial listings for full coverage details and restrictions. 2-10 *
ONE dedicated BioAdvance®
Please consult the Product Monograph at www.janssen.com/canada/our-medicines for important information relating to warnings, precautions, adverse reactions, interactions, dosing, and conditions of clinical use that has not been discussed in this piece.
The Product Monograph is also available by calling 1-800-567-3331.