










From patient-first clinical programs to research-backed approaches for better health, Temple Health is pioneering a new care model for women and babies.
Opening early 2025, Temple is investing in the region’s only hospital dedicated to women and families. Through deep community connections, quality-focused initiatives, and innovative care protocols, we’re reinventing maternal health in Philadelphia and setting a new standard for maternal outcomes nationwide.


Philadelphia County Medical Society
2100 Spring Garden Street, Philadelphia, PA 19130 (215) 563-5343
www.philamedsoc.org
EXECUTIVE COMMITTEE
Domenick Bucci, MD PRESIDENT
Walter Tsou, MD, MPH PRESIDENT ELECT
John M.Vasudevan, MD IMMEDIATE PAST PRESIDENT
David A. Sass, MD, FACP SECRETARY
Sharon Griswold, MD TREASURER
BOARD OF DIRECTORS
Victoria Cimino, MD, MPH
Brian Hannah, MD
Cadence A. Kim, MD, FACS
William King, MD
Pratistha Koirala, MD
Elana McDonald, MD
Max E. Mercado, MD, FACS
Ricardo Morgenstern, MD
Natalia Ortiz, MD, DFAPA, FACLP
Dhruvan Patel, MD
Graeme Williams, MD
Heta Patel
FIRST DISTRICT TRUSTEE
Michael A. DellaVecchia, MD, PhD
EXECUTIVE DIRECTOR
Mark C. Austerberry
Editor Kevin Bezler

Stanford with Friends: Interview at the PCMS Block Captains’ Meeting
Lynn Lucas-Fehm, JD, MD, becomes the 175th President of the Pennsylvania Medical Society
the Gap: How PA Navigate Connects Healthcare to WholePerson Care

Acclaimed Thoracic Surgeon
Larry R. Kaiser Joins



The following is an excerpt of Dr. Griswold’s (PCMS Treasurer) interview of Dr. Pratistha Koirala.
To the members of the Philadelphia County Medical Society, Health System Leaders, and our fellow physician trainees:
As physician trainees—medical students, residents, and fellows—we are dedicated to providing the highest quality of care to our patients. However, our ability to do so is increasingly compromised by training environments that prioritize productivity and profit over patient safety, education, and physician well-being. The conditions in which we work and learn have a direct and measurable impact on the quality of care we provide. We turn to PCMS for advocacy and action to ensure that our working conditions enable us to develop into competent, compassionate, and effective physicians. Investing in our wellbeing and education is not only a moral imperative but also a critical factor in improving patient outcomes.
The Right to Unionize: Strengthening Patient Care Through Advocacy
Many of us seek to organize and advocate collectively for improved working conditions, fair wages, and equitable treatment—not for our own benefit alone, but because fair working conditions lead to better patient care. Healthcare systems that suppress unionization efforts ignore the well-documented connection between physician burnout and diminished patient outcomes. The ability to unionize is about more than just labor rights—it is about advocating for a training environment that allows us to deliver the highest standard of care. We urge PCMS to publicly support our right to organize and to hold healthcare systems accountable for respecting this right. Open dialogue and good-faith negotiations will lead to a fairer and more sustainable training environment that prioritizes patient safety.
We entered medicine with a passion for healing and a commitment to serving our communities. Yet, the relentless demands of our training—excessive work hours, lack of access to mental health resources, and systemic burnout—are undermining our ability to provide safe and effective patient care. Research has shown that physician fatigue and burnout are linked to higher rates of medical errors, decreased patient satisfaction, and increased rates of adverse outcomes. When we are overworked and mentally exhausted, our ability to think critically, communicate effectively, and provide empathetic care is diminished. We ask PCMS to champion policies that prioritize reasonable work hours, adequate rest, and structured wellness programs, ensuring that the patients who rely on us receive care from physicians who are fully
Our cardiology experts never miss a beat when it comes to your heart health.


present, engaged, and capable.”
Fair Compensation and Benefits: Ensuring Physician Focus on Patient Care
Fair compensation is not just about economic stability—it is about allowing us to focus entirely on our patients without the added strain of financial insecurity. We call on PCMS to advocate for our healthcare systems to collaboratively come to the bargaining table.
Discrimination, harassment, and bias create toxic work environments that negatively impact both trainees and patients. When trainees experience mistreatment, it not only affects our mental health and job performance but
also undermines the trust and teamwork necessary for high-quality patient care. A culture that tolerates discrimination and abuse leads to increased medical errors, poorer communication, and diminished patient outcomes. PCMS must advocate for stronger protections, clear reporting mechanisms, and institutional accountability to ensure that we work in environments that uphold respect, diversity, and inclusion. A safe and supportive workplace for trainees translates to safer, more effective care for our patients.
We, the physician trainees, are not asking for privileges—we are asking for the fundamental rights and support necessary to provide safe, effective, and compassionate patient care. When our well-being is prioritized, our education is
strengthened, and our rights are respected, the entire healthcare system benefits. Patients deserve to be treated by doctors who are well-rested, well-trained, and fully supported in their roles. We call on PCMS to stand with us in this fight, using its influence to drive meaningful change. Together, we can build a future where trainees are not just surviving their training but thriving as the next generation of medical leaders, ensuring the highest quality of care for every patient we serve.
When physicians-in-training are given the tools and support they need, patients receive higher-quality, safer care.
PCMS Members: Please reach out to us at stat@philamedsoc.org and fill out the contact and interest survey: Physician Unionization Taskforce to connect with our efforts to support Physician trainees as they organize to support their efforts to improve their working conditions and patient care. •


By William King, MD, PCMS Board member


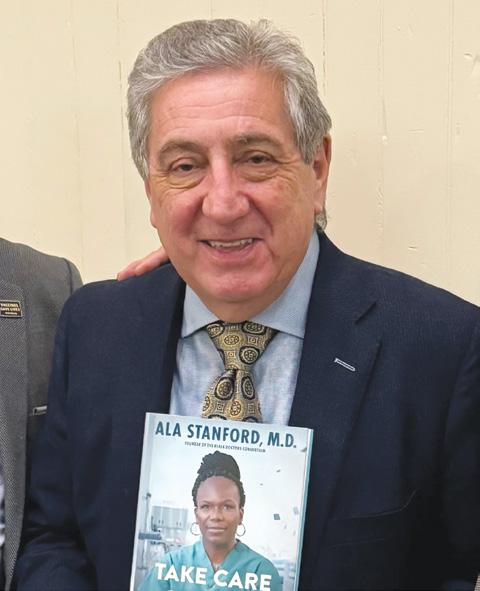
Physicians are professionals with demanding expectations and frugal praise for our colleagues’ diligent efforts to care for our patients. A surgeon’s lifesaving work, deemed a miracle by their patients, is met with faint praise, such as “not bad” or “pretty good” from their fellow doctors. The Philadelphia County Medical Society, full of such stern critics, has attempted to have conversations with an equally tough crowd, the Block Captains of Philadelphia. PCMS and the Block Captains have been in dialogue for decades, where we convey public health and wellness information and receive feedback from the frontlines of city public engagement. Following the drop in civic activities after the Covid-19 pandemic, PCMS has been working to bring back this once thriving dialogue. In 2023 we brought in a former US Surgeon General, Dr. Jerome Adams, to have a lively conversation moderated by our Immediate Past President, Dr. Vasudevan. In 2024 we faced the dilemma of seeking a local physician who could rise from among our anonymous ranks and attract the notoriously nonplussed Block Captains. Only a superhero would do. That left us Dr. Ala Stanford.
At this five-year anniversary of the Covid-19 Pandemic, we have all finally begun to recover from the physical,
psychological and societal trauma of those three years.1 As physicians we had the intellectual trauma of watching our governmental, academic, and scientific institutions respond with confusion, indecision, and bureaucratic mismanagement. This initial chaotic response was felt in Philadelphia as our federal agencies provided conflicting and poorly communicated guidelines, and our local health department relied on sclerotic distribution channels and inadequate emergency plans, leading to contracts for Covid-19 testing with fraudulent amateurs2 and demoralizing federal public health fiascos.3 Into this breach marched a physician leader only known by her fellow surgeons as a talented local pediatric surgeon, Dr. Ala Stanford. Within a period of a few months, her volunteer organization, soon labeled the Black Doctors Covid Consortium, became the indispensable resource not just for otherwise inaccessible Covid-19 testing in impoverished neighborhoods in Philadelphia, but for free, efficient, and reliable Covid-19 testing, supplies, information and vaccination, providing a level of professionalism and accessibility to the residents of the Delaware Valley that surpassed the efforts of local, county, state and federal agencies. We all wanted to know not just who Dr. Stanford was, but
Hourly Compensation:
Sign up to qualify for upcoming research studies and help us make a lasting difference! Simply complete a short form so we can find studies you best qualify for!



Nurses:
Caregivers/patients: $100+
A b o u t U s
At Root Cause Insights, we conduct research to design safer, more effective, user-friendly healthcare products.
and how we could be like her. Fortunately, she just wrote a book.
On the night of the Block Captains’ meeting, Dr. Walter Tsou, the head of the PCMS Public Health Committee, looked at the sudden cold snap ominously, and was even more discouraged by the knowledge that we had scheduled the event at the same time as a critical Philadelphia Eagles versus Washington Commanders game. Not even a fraction of the 100 registrants had arrived. Since when did they play Wednesday Night Football? And Ala Stanford is a huge Eagles fan with season tickets. As the program began, the crowd of diligent Block Captains streamed in and filled the room. After the introductions and applause, Dr. Ala Stanford and I engaged in a public conversation that revealed the incredible charisma, intelligence and intense humanity that underlay her incredible
Fight for Health Justice. Her response to the question “What is Health Justice?” clarified her response to injustice: “I am as angry and frustrated as anyone by the inequity in health care and health outcomes…. We can’t look at the fact of health inequity and simply throw up our hands in helplessness, as if it’s beyond fixing.” She helped explain the source of her determination. “The most important gift we possess is a shared belief that change is possible, and bad can be transformed into good.” We touched on the biography outlined in her book as she describes “the unfurling of my life as a young student who longed to be a healer, a doctor, a surgeon, then watch things eventually take an ugly turn as Covid-19 overtook the world, America, and my beloved hometown.” She explained much about common sources of her uncommon achievement; perseverance in the midst of adversity. “For all that I experienced continued on next page
Ala Stanford with Friends: Interview at the PCMS Block Captains’ Meeting continued from page 7



during my own personal and professional journey, I feel as if everything I endured prepared me for a role in delivering on a promise, one yet to be kept. My hardships lead to perseverance. The stacked odds led to determination. The disappointments lead to resourcefulness ... and the amazing team I recruited during the pandemic found ways to touch hundreds of lives every day, and the cumulative number grew to the thousands, then tens of thousands, then hundreds of thousands. And counting.” With these memories in mind, I asked Dr. Stanford to tell me about an architect of her audacious genius, her young mother’s insistence that she attend a very unusual school in impoverished North Philadelphia, the independent African Free School, Nihamu Sasa. Many of the older Block Captains responded knowingly to this era of innovation in small pockets of Philadelphia, a school where “We learned about African kings and queens, and how we were their proud descendants, something I would never have learned about in public school.” These reminisces about the effect of loving educators, neighbors, and leaders in the communities of Philadelphia was inspirational. Dr. Stanford quotes, “The ideology I absorbed was forged in service, giving back to your community, lifting it up.” The conversation concluded with questions from these current neighborhood organizers. The Block Captains pondered how their work could be inspired by the example of a bold young girl moved to change the world,
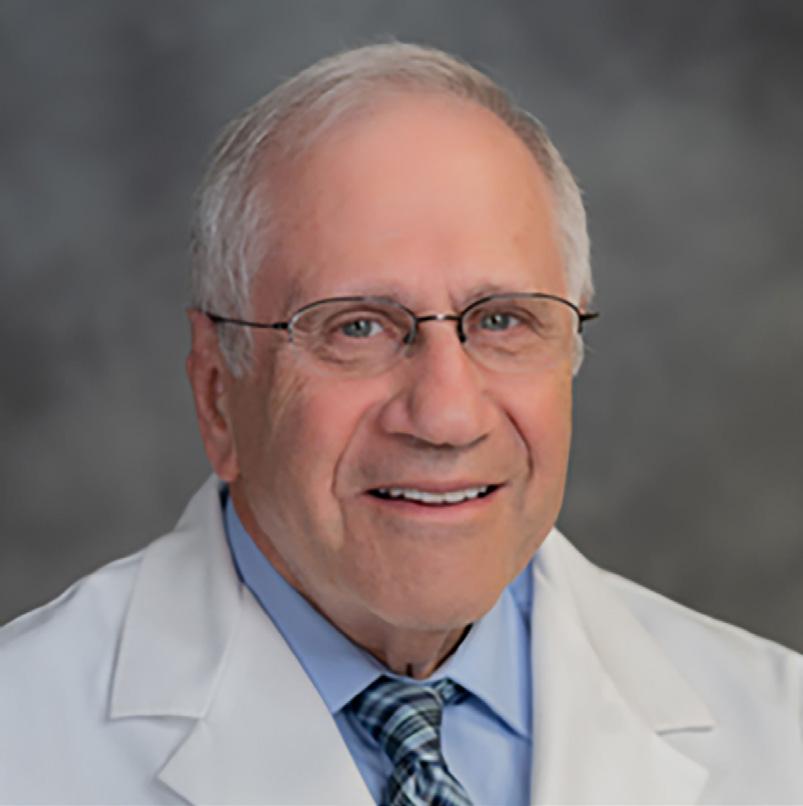
Dr. Harvey Lefton was a dedicated member of the Jefferson Health Northeast Medical Staff (formerly Aria Health) since 1976, where he had served on the Medical Executive Committee for many years. He also served as Chief of Gastrointestinal Disease, President of the Medical Staff, and was the 151st President of the Philadelphia County Medical Society.
His hard work, sense of humor, and unwavering devotion to both his patients and his colleagues will be profoundly missed.

then facing the greatest health challenge of our generation, able to rise to the moment and, with determination, pull together a force for good that turned the tide of tragedy in Philadelphia and saved countless lives. As we all basked in the camaraderie and feeling of mutual respect that she offered us, we were inspired to try harder in our efforts to understand our patients’ suffering, share in their struggles, and help them save and extend their own lives. Everyone picked up a copy of her book, provided by PCMS, hoping to learn anew. Maybe we all should read a little more. •
1The WHO declared the Covid19 Emergency a Pandemic March 11, 2020
https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meetingof-the-international-health-regulations-(2005)-emergency-committee-regardingthe-coronavirus-disease-(covid-19)-pandemic and Ended May 5, 2023
https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meetingof-the-international-health-regulations-(2005)-emergency-committee-regardingthe-coronavirus-disease-(covid-19)-pandemic
2https://www.whistleblowers.org/news/philly-fighting-covid-fiasco-highlights-howfraud-arises-in-times-of-crisis/
3https://billypenn.com/2020/04/10/city-closes-south-philly-test-site-despite-femareversal-looks-for-rapid-testing-instead/
4https://www.cnn.com/2021/06/24/health/philadelphia-black-doctors-covid-19vaccination-cnnheroes/index.html




Lynn Lucas-Fehm, JD, MD, has assumed the role of the 175th President of the Pennsylvania Medical Society as of January 1, 2025. A dedicated member of the Philadelphia County Medical Society, the Pennsylvania Medical Society, and the American Medical Association for many years, she previously served on the PCMS Board of Directors and held the position of PCMS President in 2011.
Bringing a wealth of knowledge and experience to this esteemed position at PAMED, Lynn has committed her career to advancing the field of medicine and advocating for the rights and well-being of both patients and healthcare providers. Her presidential year will emphasize practice choices and the evolving landscape of private equity in healthcare.
In today’s rapidly changing healthcare environment, physicians face numerous decisions regarding their practice. Whether joining a large healthcare system, remaining in private practice, or exploring new care models, each path presents unique opportunities and challenges. Lynn aims to highlight the potential risks associated with private equity in healthcare, which can affect patient care, diminish professional independence, and create


financial challenges that may influence the future of the field.
Her specific goals for the year include:
- Educational Initiatives: Launching a series of articles and educational resources on various practice models and the implications of private equity in healthcare.
- Advocacy: Advocating for policies that protect physician autonomy and uphold high standards of patient care when necessary.
- Research and Resources: Developing and disseminating resources to help physicians make informed decisions about their practice options.

When you’re ready to make a difference, we’re ready to help
We are proud to support Philadelphia County Medical Society by advising them for more than a decade.

1200 Howard Blvd.
Suite 300
Mount Laurel, NJ 08054
856.231.5575
Merrill Lynch, Pierce, Fenner & Smith Incorporated (also referred to as “MLPF&S” or “Merrill”) makes available certain investment products sponsored, managed, distributed or provided by companies that are affiliates of Bank of America Corporation (“BofA Corp.”). MLPF&S is a registered broker-dealer, registered investment adviser, Member SIPC and a wholly owned subsidiary of BofA Corp. Investment products:
Are Not FDIC Insured Are Not Bank Guaranteed May Lose Value © 2023 Bank of America Corporation. All rights reserved. | MAP5448947 Vault-BA1KP6 | MLWM-243-AD 470945PM-0323 | 03/2023
By sharing experiences and insights, Lynn hopes to foster a supportive environment for informed decision-making that upholds the integrity of the profession and ensures optimal outcomes for patients. Together, we can navigate the complexities of the evolving landscape and ensure that the Pennsylvania Medical Society remains a beacon of hope and excellence in patient care.
We invite you to join Dr. Lucas-Fehm and PAMED in evaluating the pros and cons of various practice models, including large versus small health systems, academic versus private practice, and private equity. If interested, please contact us at Stat@philamedsoc.org. •

By Beck Moore, CEO at Community Action Association of Pennsylvania
With over 1,300 searches, “Food Pantry” was PA Navigate’s most searched-for term in the first quarter of 2024.
Physicians are on the frontlines of addressing not only their patients’ immediate health concerns but also the broader social factors that profoundly impact well-being. Food insecurity is just one of the multitude of factors that exacerbate chronic conditions, delay recovery, and often lead to preventable Emergency Room visits. For many patients, these social determinants are not just lifestyle challenges – they are significant barriers to achieving better health outcomes.
As a trusted advocate for patients’ health, doctors and physicians understand the importance of treating the whole person. Yet, identifying and addressing social determinants of health (SDOH) can be a complex and time-consuming process. That’s where PA Navigate comes in.
This innovative, state-supported platform simplifies the connection between healthcare providers and local resources, enabling healthcare workers to efficiently refer patients to wraparound services like food pantries, housing assistance, and more. By leveraging PA Navigate, physicians and clinics can ease the burden of care coordination while ensuring patients receive the support they need to lead healthier, more stable lives.
When we talk about SDOH, we’re referring to the conditions in which people are born, grow, live, work, and age. These factors, such as access to nutritious food, stable housing, transportation, and employment opportunities, profoundly shape health
outcomes. Addressing them is essential to achieving true health equity.
Food insecurity, for example, is a critical social determinant but far from the only one. Imagine a patient who has diabetes but struggles to afford healthy food. Even with the best medical care, their condition will worsen without access to proper nutrition. Similarly, a patient experiencing unstable housing may find it challenging to manage their medication regimen or attend follow-up appointments. Each of these challenges underscores the interconnectedness of social conditions and health outcomes.



PA Navigate is a game-changer for simplifying referrals to community-based services directly from the healthcare setting. It’s a straightforward, user-friendly platform that helps healthcare providers connect patients with local resources in real-time. Whether referring someone to a food pantry, a housing program, or transportation services, PA Navigate makes it easy to bridge the gap between medical care and essential social supports.
For providers, it means spending less time navigating fragmented systems and more time focusing on what truly matters: patient care. And the best part? Physicians don’t need to be caseworkers – or even have one on staff – to make it work. PA Navigate empowers all types of practices, from small clinics to large healthcare systems, to offer care that truly considers every aspect of a patient’s well-being.
What makes PA Navigate so impactful is how it supports holistic care. Doctors often see the disconnect between what happens in the exam room and the challenges our patients face in their everyday lives. PA Navigate helps close that gap by giving us tools to address immediate medical needs while connecting patients to critical community resources.
When they integrate social determinants into their care plans, it strengthens the bond between doctor and patient. Patients notice when their provider cares about more than just their symptoms – it builds trust and shows a commitment to their overall health. And this approach doesn’t just improve individual outcomes; it helps reduce readmission rates and prevents avoidable Emergency Room visits, creating a ripple effect that benefits the entire healthcare system.
One of the things users love most about PA Navigate is its simplicity. Its intuitive design means that anyone can use it –no technical expertise required. Clinics and practices without case management staff are easily leveraging this tool to make meaningful connections for their patients.
Take, for example, a small primary care office. With PA Navigate, they can quickly find nearby food assistance programs
for a family struggling with food insecurity. On the other hand, a larger healthcare system can seamlessly integrate the platform into their existing workflows, streamlining processes and improving efficiency across the board.
The real beauty of PA Navigate lies in how it strengthens connections – between patients and providers, healthcare settings and community organizations, and medical care and social supports. These connections are critical for tackling the root causes of health disparities and fostering a healthier, more equitable society.
For providers, using PA Navigate is a way of saying to patients, “I see you. I hear you. And I’m here to help.” For patients, it’s a powerful reminder that their doctor truly cares about their wholeperson health. This kind of trust not only improves adherence to care plans but also leads to better outcomes overall.
We have a unique opportunity to influence not just the health of individual patients but the well-being of entire communities. Addressing social determinants of health isn’t easy, but tools like PA Navigate make it possible – and manageable. It’s more than just a referral system; it’s a bridge to holistic, equitable care that recognizes the full scope of what patients need to thrive.
I’m genuinely optimistic about the future of healthcare when I see solutions like PA Navigate in action. By embracing this innovative tool, we can close the gap between medical care and social supports, ensuring no patient’s health is limited by their circumstances. Together, we can build a healthcare system that works for everyone, one referral at a time.
If you are a community-based organization, nonprofit, or work with a local organization, please help connect them to the Community Action Association of Pennsylvania’s website, www. panavigatehelp.org, to connect to a Community Engagement Manager today! •
PA Navigate - Pennsylvanians can find help with various needs, including access to things like food, housing, utilities, transportation, and more - right in your local community. https://www.pa.gov/agencies/ dhs/resources/for-residents/panavigate.html
Video by Val Arkoosh https://youtu.be/Z5BDxfOSl7s

Valerie A. Arkoosh, MD, MPH, was appointed to lead the Pennsylvania Department of Human Services by Governor Josh Shapiro on January 17, 2023; Dr. Arkoosh officially became Secretary on June 29, 2023.
Prior to this role, Secretary Arkoosh served on the Montgomery County Board of Commissioners since January 2015, when she was appointed to fill a vacancy on the Commission. Arkoosh won election to a full four-year term in November 2015 and served as Commission Vice Chair until her election as Commission Chair in November 2016. She was the first woman ever to serve in this role. Arkoosh was re-elected in November 2019 and unanimously chosen by her colleagues to again serve as Chair in January 2020. Montgomery County is the third most populous county in Pennsylvania with over 856,000 residents. The threemember Board of Commissioners oversees a budget of more than $500 million and directs more than 2,800 employees charged with administering and overseeing county functions, including human services.

As a physician and public health professional, Secretary Arkoosh was at the center of Montgomery County’s efforts to combat the COVID-19 pandemic, leading a data- and science-driven approach to the unprecedented challenge. Arkoosh’s leadership was praised during the county’s response, especially her transparency and public communication throughout the pandemic. Secretary Arkoosh is also a staunch advocate for maternal health and reproductive rights, and she serves on the Pennsylvania Maternal Mortality Review Committee.
As Commission Chair, Secretary Arkoosh was committed to strengthening services for children, veterans, and seniors. She led the efforts to eliminate street homelessness of veterans and streamline delivery of human services. Recognizing the need for a strong, supported workforce in executing these goals, she instituted a $15 minimum wage and gender-neutral paid parental leave for Montgomery County employees. Drawing on her background as a physician, she oversaw a multi-pronged, integrated response to the opioid overdose epidemic, including issuing a standing order in 2015 to enable participating pharmacies in Montgomery County to dispense the overdose antidote naloxone at the request of any member of the public.
Upon obtaining her Master of Public Health in 2007, Arkoosh became deeply engaged in the national effort to achieve comprehensive health care reform. She led the National Physicians Alliance, a national non-profit organization of physicians, who, putting their patients before profits, joined a broad-based nationwide coalition for reform. During this time, she developed policy and legislative strategy, and promoted public engagement in Washington, D.C., Pennsylvania, and throughout the country. Dr. Arkoosh maintains comprehensive knowledge of the implementation of the Patient Protection and Affordable Care Act and its impact on individuals and the health care system.
Prior to stepping into public service, Secretary Arkoosh was Professor of Clinical Anesthesiology and Clinical Obstetrics and Gynecology at the Perelman School of Medicine of the University of Pennsylvania. Arkoosh is a graduate of the University of Nebraska College of Medicine and received a Master of Public Health from the Johns Hopkins Bloomberg School of Public Health. She performed her residency at Jefferson Medical College in Anesthesiology with a special focus in Obstetrics. She has an undergraduate degree in economics from Northwestern University.
Secretary Arkoosh lives in Springfield Township, Montgomery County, with her husband and their three children. •
By Reem Telhaoui, high school student from Germantown Friend School and Intern at the Philadelphia County Medical Society

Internal medicine physician Dr. Conklin woke up bright and early, brewed his quotidian cup of joe, and began his morning rounds from home, connecting with his resident, Sweeney, through video conferencing – nothing unusual. Besides, in this day and age, virtually connecting with patients and coworkers is crucial for an efficient medical practice. However, what if I told you that Dr. Conklin isn’t from this day and age? What If I told you that he is from 1976 –and he’s actually living in 2076?
Let me explain: Dr. Conklin is a fictional character created by William A. Sodeman, Sr., M.D., in his article “Internal Medicine – 2076” published in the Philadelphia County Medical Society Bicentennial Edition 1976. Through this ordinary, unremarkable primary physician, Dr. Sodeman illustrates his prediction for internal medicine one hundred years in the future. With Conklin’s everyday use of his “visuphone” – Sodeman’s 2076 version of video calling or FaceTime – it’s safe to say that Dr. Sodeman was, surprisingly, on the right track. As we approach the halfway mark, we can use Sodeman’s predictions to quantify our progress in internal medicine in the past fifty years and identify areas of growth for the next fifty, including field demographics, revolutionary medications, and cures.
Before powering up his “visuphone,” Dr. Conklin reflects on the Jefferson Medical College class of 2076’s graduation, which he attended the previous day. He remarks that “forty percent of the new medicos were women.” Besides the Medical College’s renaming to Sidney Kimmel Medical College in 2014 –which Sodeman couldn’t possibly have predicted thirty-five years in advance – this prediction is an understatement.
The college’s 2028 graduating class is remarkably 54% women, surpassing Sodeman’s prediction by 14%, fifty years ahead of schedule. Disappointingly, however, the other half of this prediction hasn’t met this degree of progress. Sodeman notes that “the word [‘minority’] was not even mentioned as a seemingly large number crossed the stage for their diplomas,” expressing the ideal where representation in medicine is equitable. Today, however, only 16.8% of the class of 2028 are from underrepresented groups in medicine and 28% are from nonwhite ethnic groups. This means 72% (the vast majority) are from white ethnic groups. Although this still is not ideal, it still represents significant progress. Since 1976, the Sidney Kimmel Medical College has made many steps towards equity and inclusion including launching initiatives and programs. If we continue these efforts and maintain this upward trend, we may eventually reach a more balanced and truly inclusive future in medicine.
Other predictions of Sodeman’s include skyrocketing medical school tuition costs, the introduction of an alcohol additive “sofram,” which prevents alcohol from affecting the liver, and the eradication of chronic bronchitis thanks to air pollution control. While gender balance in medical schools has progressed more than expected, Sodeman’s prediction about the rising costs of medical education is, unfortunately, still on track. He jokes that by the year 2076, Jefferson Medical College’s tuition will be a whopping 1200 “macrodollars” (one macrodollar is equal to 10 dollars) due to inflation. This prediction is, once again, an understatement; tuition at Sidney Kimmel Medical College is currently $61,500 (or 6150 macrodollars), as compared to about $6000 (60 macrodollars) in the late 1970s,
showcasing just how drastically inflation has affected the cost of education.
The elimination of liver cirrhosis and chronic bronchitis, however, remains a distant hope. Still, Sodeman’s prediction that widespread education on smoking will reduce chronic bronchitis is largely on track. As newer generations are warned of the dangers of cigarette smoking more frequently, chronic bronchitis rates have generally declined. However, air pollution continues to be a significant environmental challenge and negatively affects our lungs. It is hopeful that, for both the well-being of the environment and our respiratory systems, we can make significant progress in reducing air pollution over the next fifty years.
Lastly, after being briefed on his last patient of the day, who has a widened mediastinum and two new nodules, our futuristic Dr. Conklin exclaims, “It’s a pleasure to make a diagnosis of leukemia.” This statement might seem like a shocking and downright insensitive thing to say in today’s world. But, Dr. Conklin isn’t living in our medically-inferior time. In 2076, leukemia, Hodgkin’s lymphoma, and other lymphomas are completely curable, so a diagnosis no longer carries the same weight of despair. Although this may seem far from our current reality, it may not be as far as you think. Thanks to HPV vaccinations and routine Pap Smears, we’re closer than ever to eliminating cervical cancer. Although leukemia and cervical cancer are very different, and they are still a challenge today, we’ve made incredible progress in the past fifty years. Who knows what advancements we’ll make, what diseases we’ll cure, and what groundbreaking medicines we’ll discover in the next fifty? •
By William A. Sodeman, Sr., M.D. 1
On June 17, 2076, Dr. John Conklin sat down at his desk after finishing his breakfast to start his daily activities in his practice of Internal Medicine. His routine consisted of calling the hospital on the visuphone, receiving the morning report on his hospitalized patients (to whom he could see and talk to along with his resident on the visuphone) to adjust orders and treatment. He then communicated by the same means with those patients at home who wanted advice before he proceeded to his office activities. Later in the day, he visited his hospitalized patients personally.
Before reaching for the visuphone, he sat silently and reviewed the events of the previous day when he had, as part of his 25th class reunion, attended the graduation ceremonies of the Jefferson Medical College. Tuition is still going up – 1200 macrodollars2; otherwise, how different things were! Yesterday they graduated 340 new M.D.s and 107 physician assistants. Forty percent of the new medicos were women. At his graduation they were still counting minority groups. But yesterday the word was not even mentioned as a seemingly large number crossed the stage for their diplomas. How well we had all finally blended together. He did recall another statistic which impressed him aside from the forty percent women. It was the number of graduating M.D.s who had majored in their premedical years in engineering – twenty-one percent. How medicine had changed! Electronics and computers everywhere! And a new breed coming into medicine to take over.
Conklin suddenly straightened up to the work of the day. He reached for the visuphone control, tapped out the hospital number, asked for his resident, Sweeney, and Sweeney’s smiling face appeared on the visuscreen. They traded amenities and


Sweeney then stated that there were only five patients needing discussion this morning. “The first,” said Sweeney, “is Perkins in Room 206. His congestive heart failure worsened overnight.” He flipped on the read-out on the monitor attached to Perkins and back to the instantaneous figures appearing thereon – digoxin level 1.2 ng, Na 124, Cl 88, ylic acid 26 I.U. Conklin asked to increase the dose of ylic acid to get a blood level of 50 I.U. or more. “It’s the best new drug for the myocardium since Foxglove. But you can’t expect much for an aging circulation in a man of 92. Ever since we’ve been able to control atherosclerosis and myocardial infarction, we’ve been left with the true aging process itself. And that we have not yet been able to influence. Ylic acid may be the answer. Perkins is on his second heart transplant in 12 years, and the aging process which was accelerated in the first transplant necessitated the second. It looks as if the same thing is going on again. We disposed of atherosclerosis as part of the aging process and here we are – still stymied!”
Sweeney went on the second case, Carson in Room 212, a patient with hepatic cirrhosis. He explained that the encephalopathy was progressing despite controls on protein intake and other measures. “He’s our rarity as a cirrhotic,” said Conklin. “I finally found out how his alcoholism caught up with his liver. Ever since the law required sofram in all alcoholic products twenty years ago, cirrhosis has disappeared. The mechanism by which sofram protects the liver is not yet clear. But it really works! Carson made his own booze for the past fifteen years. He’s been unprotected. He’s worth a clinic for the students, as rare as a lobar pneumonia. I’m trying to get a sofram derivative, under investigation by the M-SD-Schering-SKF combine, which may be useful intravenously in arresting the cirrhotic process. Continue Carson’s supportive measures, and I’ll check in on him later today.”

“Our third patient is Mrs. Simpson in 222,” countered Sweeney. “She’s the 52-year-old diabetic who had the pancreatic transplant last year, and has been leading a pretty normal life until three months ago. You have not seen her yet this time, Dr. Conklin. You told her to come in yesterday, and we have worked her up for you to see later on today. We do have some data. Her fasting blood sugar this morning was 440. She’s not acidotic. There are no signs of rejection of the pancreatic transplant, of course, and blood insulin levels are slightly high.” Conklin replied, “Sounds pretty good. The transplant is working. We haven’t had a transplant rejection in several years. Thank God we conquered that problem forty years ago. It appears that Mrs. Simpson is developing difficulty in insulin utilization. That’s our biggest problem today with these older diabetics. Put her on diabetic diet 8 and check her for any hidden infection. I’ll see her later today.”
“Okay,” said Sweeney. “Our next problem is Henry Nixon. You saw him yesterday. He’s our ‘pink puffer.’ It appears his hypoventilation is progressing. His ABGs show his PO2 to be 55 and his PCO2 is 35. He was running a PO2 of 70 to 75. He’s breathless, of course, and his forced expiratory time is more prolonged.”
“His pan lobular emphysema is obviously progressing,” said Conklin. “We better have Dr. Evans see him about his oxygen therapy. Repeat his FEV1 and the ABGs before Evans arrives.”
“We certainly are lucky that we have few of the ‘blue bloater’ types anymore, with their disturbances in ventilation-perfusion relationships and their impaired CO2 sensitivity. Education on smoking and our controls on air pollution have reduced chronic bronchitis with its recurrent mucopurulent exacerbations; and with our control of infection, we keep the bronchi pretty clean now. You should have seen the problems with infections when I was a resident. Most of that is gone now. We’re out of major infections with the bronchi, but still in trouble with the alveoli. Sure, we’ll still have difficulties with inhaled irritants and acinar inflammation, the absence of ATT, and imbalance of proteolysis and protease inhibition. But we’re getting there. I’ll talk to Evans about Nixon later.”
“Our last patient is Mrs. Groves. She has developed a rash.”
“Sweeney, put her in front of the visuscreen in her room and let me see her. I’ll wait till you get in there. Have them switch the connection.”
The switch was made and the shoulders, back, and abdomen inspected. A few petechiae were found. “Hold up the new chest film to the visuscreen,” said Conklin. He inspected it and suggested that the mediastinum looked a bit wider than previously. He asked to see the previous film and suggested the neck be palpated for lymph nodes again. Sweeney complied and said he felt two he had not felt before. “Looks like Hodgkins,” said Conklin. “The fever, anemia, and blood picture fit. I hope it’s Hodgkins. That we can cure. It’s a pleasure to make a diagnosis of Leukemia, Hodgkins, and the other lymphomas since KL-122 and its derivatives have turned out to be truly cures. I hope we can come closer to cures with Ca and Sa. But it doesn’t appear to be in the cards yet. We’ll lay plans for Mrs. Groves’ program this afternoon.”
“That’s it, Dr. Conklin.”
“Thanks, Sweeney. See you later.”
Dr. Conklin turned off the visuphone. He turned to his appointment book for the morning office hours. “Oh no,” he said as he checked off five to fifteen names. “Always neurosis, neurosis, neurosis.” •
1Vice President and Dean Emeritus and Professor of Medicine Emeritus, Jefferson Medical College of Thomas Jefferson University; Clinical Professor of Medicine, Medical College of Ohio at Toledo.
2With inflation averaging 6% per year in the past century, the factor of 600% had caused readjustment of the dollar 10:1. A macrodollar is ten dollars.
As Donald Trump is installed as the 47th President of the United States, his nominees for various cabinet and other leadership government positions will soon be queried, their records sharply reviewed and then voted on for confirmation by the members of the U.S. Senate. One of the most controversial of the proposed nominees is Robert F. Kennedy, Jr. (RFK Jr.), nominated to become Secretary of the U.S. Department of Health and Human Services (HHS), one of the largest federal departments per the federal budget.
HHS administers approximately 115 programs that aim to “protect the health of all Americans and provide essential human services, especially for those who are least able to help themselves.” With a yearly budget of approximately 1.7 trillion dollars, the largest portion by far is given to the Centers for Medicare and Medicaid Services (CMS), followed by the National Institutes of Health (NIH), and the Health Resources and Services Administration (HRSA). Some of the other operating divisions of HHS include the Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), Substance Abuse and Mental Health Services (SAMHSA), the Indian Health Service, the Agency for Toxic Substances and Disease Registry, and the Administration for Children and Families (which oversees Head Start, refugee resettlement, and human services emergency preparedness programs amongst others). The importance of these programs for the wellbeing of the U.S. population cannot be overstated. It is said that HHS touches the lives of more Americans than any other Federal agency.
RFK Jr., a graduate of Harvard University and the University of Virginia Law School, has a somewhat remarkable background regarding environmental law. He litigated or assisted in numerous environmental lawsuits: 1. to keep waterways and estuaries free of contamination; 2. to replace a nuclear power plant with renewable
energy thereby significantly decreasing carbon emissions; 3. to make dozens of municipal wastewater treatment plants compliant with the Clean Water Act; 4. to alter mining practices to prevent mountaintop removal and slurry pond construction; and many more significant cases. He joined and started various environmental law firms, and founded and co-directed for years the Environmental Litigation Clinic at Pace University School of Law, which became a model for similar law clinics in the U.S. In 2017 he and his partners successfully sued Monsanto on behalf of plaintiffs who developed non-Hodgkin’s lymphoma after exposures to the glyphosate-based herbicide, Roundup. RFK Jr. has also worked in Latin America and elsewhere to aid indigenous tribes and others in opposing large extractive projects on their land and/or to stop the construction of proposed dams. He opposes fracking and the development of LNG sites, and approves of the Green New Deal. RFK Jr. has written a number of books concerning these topics, has been the subject of a number of related movies, and received awards for his work.
While RFK Jr.’s environmental work has often been praised, in more recent years he has focused more of his energy in the realm of public health where his statements and proposals have tended to raise great concern amongst those who work in the healthcare field. Some matters may not be particularly controversial, such as his desire to look into such things as the effects on children of ultra-processed foods with dyes and other additives; however, many are. Some examples are noted:
1. RFK Jr. wants to increase access to unpasteurized milk, despite the well-known health risks, and has stated that he will end the FDA’s “war on public health” including its “aggressive suppression” of many such things, including raw milk, stem cells and vitamins.

2. For many years RFK Jr. has widely promoted vaccine misinformation including the well-disproved claim that “autism comes from vaccines.” With regards to the Covid-19 vaccine, he stated that the Covid vaccine is ”the deadliest vaccine ever made.” Additionally he stated that “there’s no vaccine that is safe and effective.” He thought the restrictions to limit the spread of Covid were unnecessary, and made incorrect comments about the Covid virus tending to target various ethnic groups more than others. He is a founder of an anti-vaccine activist group and opposes any school mandates.
3. While fluoride in drinking water at recommended concentrations has been proven to protect teeth from decay, RFK Jr. has linked fluoride to many types of ailments and he has long campaigned about his recommendation to remove all fluoride from public water.
4. He repeatedly stated that HIV / a virus is not the cause of AIDS, but linked its cause to “poppers” / recreational drug use, and has claimed that “most HIV-infected Africans showed no sign of illness.”
5. He supports a ban on standard-of-care transgender healthcare treatments for youth.
6. He has threatened limiting access to FDA-approved abortion medications; and, amongst other issues,
7. He has repeatedly claimed that school shootings are occurring because of youth perpetrators having been prescribed antidepressants, but no such linkage has been found.
RFK Jr. has stated that he wishes to look at chronic diseases with special consideration of Big Food, Big Agriculture, and Big Pharma. That is well and good, but it is because of what is noted above and much more that many in healthcare believe that lots of
the advances that have occurred in public health and medical care, including the great reduction in many diseases due to vaccines and other preventive measures, will be reversed should RFK Jr. be confirmed as head of HHS. It is expected that any Secretary of HHS will understand and use accepted scientific knowledge, value evidence-based medicine and not engage in or proliferate wild conspiracy theories or plain falsehoods. The well-being of the country’s residents is far too important. Perhaps the knowledge and skills of RFK Jr. can be better utilized elsewhere. •
Please send your comments to stat@philamedsoc.org.
To read more about actions to take regarding the nomination of RFK Jr., consider reading: https://doctorsforamerica.org/wp-content/ uploads/2025/01/DFA-Position-Statements-onTrump-Nominees.pdf.
If you wish to sign a letter opposing RFK Jr.’s confirmation, please read more at: https://committeetoprotect.org/stop-rfk-jr/.
By College of Physicians Fellows Robert G. Sharrar, MD, MSC, FCPP, Susan

In the fall of 1786, a group of 24 physicians met to establish the College of Physicians of Philadelphia. The object of the College, as stated in its original constitution, was “to advance the science of medicine, and thereby to lessen human misery, by investigating the diseases and remedies which are peculiar to our country… by stated times for literary intercourse and communications; and by cultivating order and uniformity in the practice of physic.” The earliest recorded meeting of the College occurred on January 2, 1787.
According to Benjamin Rush, the new institution was a collage of physicians and a medical society and would benefit the profession and the public. As a college, the institution would address principally matters of public concern and could offer advice to legislative bodies on matters affecting the health and happiness of the citizens. As a medical society, its members could collect and publish medical observations and inquiries and hold meetings, cultivate a botanical garden, and collect a library.
Today, the College has a botanical garden, an internationally recognized library, a medical museum containing human specimens of medical interest, and many educational and mentoring programs. However, the efforts of the College to address public concerns and advice to regulatory agencies on matters affecting the health and happiness of the citizens are less well known. The purpose of this paper is to describe the long history of efforts that the College has made to address public health issues.
The information in this article is from The College of Physicians of Philadelphia: A Bicentennial History by Whitfield J. Bell, Jr., Science History Publications, U.S.A. 1987. In its almost 250year history, the College has addressed many public health issues
facing our community. Its efforts in public health have varied over time and reflect the conservative opinions of the Fellowship, who wanted its recommendations to be based on sound scientific data, and the more liberal opinions of some of the Fellows who wanted the College to be more active.
In the summer of 1793, an outbreak of yellow fever was recognized by Benjamin Rush, who had treated several individuals with “bilious fever.” At that time, the cause, mode of transmission, and treatment were unknown. The mayor asked the College “to consider what steps should be taken” to control the outbreak. Fellows met and made the following recommendations: all unnecessary intercourse with infected persons should be avoided, and infected persons should be placed in large and airy rooms with strictest regards to cleanliness. Houses with infected persons should be marked, and the city should establish a large and airy hospital for individuals who could not be accommodated at home. They also recommended that the streets and wharves of the city be as clean as possible, and that individuals avoid all fatigue of body and mind. There was no known treatment. Rush recommended mercury administered liberally and bleeding, while Adam Kuhn, another Fellow, recommended chamomile tea, bark or laudanum, wine, lemonade, fresh fruits, and baths of cold water. The only preventative method was to flee the city.
Governor Mifflin asked the College if the disorder was imported or not, and what measures ought to be pursued to purify the city from any latent infections, and how to prevent
future occurrences. Since the College was unaware of any instance in which the disease yellow fever was generated in the city, they felt that the disease was imported by some of the vessels which arrived after the middle of July. They recommended that every house, especially those with cases, be cleaned and aired out, the walls be whitewashed, and gunpowder burned in every room. The College recommended that quarantine requirements be strengthened, and the Board of Health be empowered to do what was necessary to prevent importation.
Recurrent yellow fever outbreaks occurred in late summer throughout the 1790s. In 1798, the College published a summary of its “Proceedings…relative to the Prevention of the Introduction and Spreading of Contagious Diseases” and a review entitled “Facts and Observations relative to the Nature and Origin of the Pestilential Fever, which prevailed in this City, in 1793, 1797, and 1798.” The College’s recommendations for the care of patients with yellow fever and stronger quarantine measures were unchanged.

of streets, houses, and bedding, and a proper diet. They also recommended that hospitals should be prepared to receive the sick. During the epidemic, a weekly newsletter was published, which contained reports of outbreaks and public health measures elsewhere, the experience and recommendations of physicians and hospitals in Europe, and statistics comparing the morbidity and mortality from cholera in previous time periods.
The College established the Committee on Public Hygiene (Health) in 1834. The first report of the Committee made several general recommendations for the sanitary conditions of the city and urged that all existing laws and ordinances concerning public health be enforced. The College asked the committee to investigate discharges from manufacturing plants into the pool, from which water was drawn into the reservoir atop Fair Mount. The Board of Health asked the College about draining and filling the ubiquitous ponds of stagnant water. The College petitioned the legislature to provide parks and shaded walks in newly incorporated districts of the city.
Jenner published his observations on vaccination with cowpox in 1798, and the College received several reports on successful cases of vaccination in early 1801. The vaccine was received in Philadelphia in November 1801 and was used by John Redman Coxe to vaccinate his family and Benjamin Rush’s children. Although the College did not officially endorse vaccination against smallpox, the active Fellows of the College recommended it for general use in April 1803 to prevent smallpox. Pennsylvania Hospital offered free vaccination to the poor in 1809.
A cholera epidemic spread across Europe in 1831-32, and the Philadelphia Board of Health, fearing its resources were inadequate, requested the College to prepare a report on all facts regarding the cholera epidemic. The cause, mode of transmission, and treatment were unknown. The Committee of seven Fellows reviewed the history of cholera, its predisposing conditions, and the character of its victims, and stated that it was not contagious and not transmitted by personal contact, and that quarantine was not recommended. The committee felt that the best means of prevention was sanitation, and recommended the cleaning
In the middle of the 19th Century, the College was mainly concerned about the living conditions of the poor, who lived in crowded tenements on narrow streets with poor ventilation. Hydrants supplied water at the end of the street, with common privies nearby. The streets were unpaved, never cleaned, and contained clogged and overflowing sewers. In 1843, the College endorsed the city’s proposal to purchase the Lemon Hill estate to protect the purity of the Schuylkill water supply. In 1874, the College asked the Philadelphia Fountain Society to place urinals in places of daily resort.
In 1888, S. Weir Mitchell, President of the College, told the Fellows that their most important duty was “that of incessant watchfulness of all public interests in which questions of health are concerned.” He mentioned quarantine, sanitation, water supplies, sewerage, sales of poison, and abattoirs in the preceding three years. Because of the College’s concerns about the appearance of cholera in Asia and Europe in 1883-1884, the College called on the Philadelphia City Council to prepare for a cholera outbreak before it was too late. The College asked for the Board of Health to be strengthened to make house-to-house visits in areas of high risk, establish dispensaries, and prepare hospitals to receive the sick.
continued on next page
FEATURE continued
College of Physicians of Philadelphia and Public Health
continued from page 21
The discovery of the tubercle bacillus by Robert Koch in 1882 led to a great deal of discussion at the College on how to control tuberculosis. Many thought tuberculosis was only “moderately contagious” and that there was a hereditary component. One member, Larry F. Flick, called for registration of patients and a municipal hospital for treatment in1890. Others felt that registration of patients would not lead to any measures of real value, and that strict attention by the attending physician to disinfection, ventilation, and separation of the sick from the well was adequate. In 1915, the College recognized that tuberculosis was a communicable disease transmitted from person to person, and that the Health Department should have the power to hospitalize patients who were a menace to family and neighbors.
The Committee on Public Health & Preventive Medicine was established in 1912 to “add to the usefulness of the College and further the original object for which the College was founded.” It was:
1.) To investigate matters of special importance concerning Public Health, to report upon the same to the College and to recommend methods of dealing with them.
2.) To inform the College of all steps of an unusual nature taken by the Federal, State, or Municipal governments in connection with the problems of public health, and acquaint the College with the character and purpose of proposed legislation relating to health and disease.
3.) It shall “when the necessity arises and subject to the approval of the College, make arrangements as may render Expert Knowledge of the College upon Hygiene, Sanitary Science and Preventive Medicine available for the uses of the Public Authorities.”
4.) Conduct authoritative popular lectures at the College’s expense.
The Committee discussed various issues, including child labor laws, the conditions of the streets, the successive public health directors, the development of a health code in simple language, pollution by oil refineries, Pennsylvania’s compulsory vaccination law, and the physical condition of the nation’s young people, to name a few. In the 1930s, it held sessions on medical insurance, group practice and treatment for preventative services.
Although the College has had various committees on Public Health throughout its history, the current Section on Public Health and Preventive Medicine was established in 1994. The purpose of the Section was to bring the public health community together to promote the study of public health problems, particularly in the greater Philadelphia area, and to promote the institutional, professional and government responses to these issues. You do not have to be a Fellow of the College to be a member of the Section. The Section is composed of Fellows of the
College and representatives from local county health departments, the School District of Philadelphia, academic public health programs, and community organizations performing public health functions.
The Section conducts Grand Rounds on important public health issues, advocates for public health, and sponsors an annual Student Poster Session for students to present their capstone projects, and Public Health Day for professional public health workers to present their work. The Section also has an annual Public Health Recognition Award for an individual, organization, and student who have done outstanding public health work.
The College of Physicians has a long history of commitment to public health. In 2022, the College inaugurated the Susan and Stanley Plotkin Chair in Public Health and hired a DrPH epidemiologist as the Director of Public Health and Editor of the History of Vaccines’ online project. In 2023, the College purchased the adjacent property to provide additional spaces for meetings and gatherings of various health care organizations. The College is uniquely situated to honor its mission to advance the cause of health, while upholding the ideals and heritage of medicine. Public Health has always been of concern to the College, as reflected in its motto Non Sibi Sed Toti: Not for oneself but for all.
Philadelphia suffers from many important public health issues that need to be addressed, such as poverty, gun violence, teenage pregnancies, and low high school graduation rates. Fortunately, Philadelphia is blessed with a strong and vibrant medical and public health community. Philadelphia has five medical schools (Drexel, Jefferson, PCOM, Temple, and the University of Pennsylvania) and eight schools of Public Health (Arcadia, Community College of Philadelphia, Drexel, Jefferson, LaSalle, Temple, University of Pennsylvania, and West Chester), with several hundred students working on degrees in public health. The Philadelphia metropolitan area also has strong county Health Departments and many community groups currently working on these issues. The problem is that these groups are not working together.
The College is uniquely situated geographically, has a large Fellowship with many Fellows interested in public health issues, and a Section on Public Health and Preventive Medicine that has been active for many years. The College cannot solve these problems on its own. However, the College can bring together diverse medical, governmental, and community groups to address these important public health issues. The Section can also help these community groups evaluate their programs to make them better. The College is a place where public health people can meet to discuss common issues, network, and support the projects they are working on. •
By
The College of Physicians of Philadelphia, the oldest and most distinguished private medical society in America, has appointed acclaimed thoracic surgeon and health system executive Dr. Larry R. Kaiser, MD, FACS, FCPP, President and CEO. Dr. Kaiser has had a longstanding relationship with the College, having served as a Fellow (since 1993), the Treasurer of the College’s Board of Trustees, Chair of the Finance Committee, and Co-Chair of the Campaign Committee.
“Dr. Kaiser has the experience and demonstrated leadership capabilities needed to move the College forward at this critical time in our history,” said Dr. Erica R. Thaler, MD, FACS, FCPP, Chair of the College’s Board of Trustees. “We welcome him as President and CEO, and I look forward to working closely with him in implementing the College’s strategic plan, new campus plan, and new capital campaign.”
Dr. Kaiser assumed his duties as President and CEO of the College in January 2025. The organization also includes the Mütter Museum and Historical Medical Library. Dr. Kaiser said that he is honored to be chosen by the

Board of Trustees for this role and looks forward to working with the Board and the Fellowship to fully realize the potential of the College.
“I believe that the incredible resources of the College and the Fellowship offer a platform for the College to be a leading voice in connecting the history of medicine to the critically important issues of modern medical practice and scientific research,” Dr. Kaiser said.
Dr. Kaiser has enjoyed a distinguished career as a thoracic surgeon and a leader in academic medicine. Most recently, he has served as a managing director with Alvarez and Marsal, a global management

consulting firm, and has deep experience in healthcare administration. Before that role, Dr. Kaiser served as the President and CEO of the Temple University Health System for nearly a decade and was the inaugural Lewis Katz Dean of the Temple School of Medicine.
He has previously served as President of the University of Texas Health Science Center at Houston and held a variety of leadership positions at the University of Pennsylvania, including Chief of General Thoracic Surgery, Founder and Director of the University’s lung transplantation program, Director of its Center for Lung Cancers and Related Disorders, the inaugural Eldridge Eliason Professor of Surgery, and Co-Director of the Thoracic Oncology Laboratory. In 2001, he was named the 13th John Rhea Barton Professor and Chair of the Department of Surgery and Surgeon in Chief for the University of Pennsylvania Health System.
Dr. Kaiser’s appointment to lead The College of Physicians is a significant milestone highlighting the institution’s longstanding commitment to “advance the cause of health while upholding the ideals and heritage of medicine.” To learn more, visit https://collegeofphysicians.org. •



Who doesn’t love the promise of new love? There’s a giggly feeling no matter your age as you realize that you want to spend at least the next few months with someone, plus the gambler’s thrill of pulling the lever one more time, hoping this will be the relationship that lasts forever.
For those who follow the modern, app culture gamesmanship of dating, date three tends to be a fulcrum point. Even if the dreaded situationship forms, date three is the moment where you know whether interest is real enough to justify indefinite attention, or just a passing fancy.
So, planning date three with Dat, the adorable management consultant I was courting, we decided to talk about whether we were going to be having sex with other people anytime soon.
No, this isn’t the stereotypical, fabled promiscuity of the gay community immediately rearing its head. Truth be told, Dat and I were taking it slow and hadn’t even been intimate with each other yet. But in the already fraught world of queer sexual health, a new risk was starting to
By Blake Weil, 3rd Year Medical Student at TJUH
emerge in the form of MPox, at the time called Monkeypox.
For those unfamiliar with MPox, it’s a variola virus quite similar to smallpox, or cowpox, or any number of other poxes I won’t name. MPox causes painful, scarring, blistering lesions; not only a health risk, but a vanity risk, a true double whammy.
The lesions are painful enough that the infected find it difficult to sit or lie down, and the recovery time is two to four weeks in total isolation, way too long for two ambitious swells like Dat and I to suffer. While not a true STI, it is spread through skin to skin contact, and was beginning to tear through the gay community after a suspected initial outbreak at a European music festival, and Mpox has become at least an STI in connotation.
Dat and I had met on Hinge, like the approximately ⅔ of queer couples that meet online. I was about to start medical school, he was wrapping up a PhD before being swallowed up by a big-three consulting firm, and he made me laugh, and think, and spoke six languages. We had coffee in the park, and then dinner
and a show as I took him to an avant-garde burlesque I was reviewing for a magazine, themed after reality TV. We stole our first kiss in the somewhat grimy bar where the show was held, in the mirrored infinity room in the back, and I was definitely interested in date three.
Of course, there were complications. Dat was about to leave for Vietnam for three months about three weeks from when we were planning our third date, and both of us thought it inauspicious to start something official with the oncoming separation. And so we decided that we had to navigate the murky sexual politics of how to grapple with the fact that no matter what our feelings were, it seemed like the safe, adult thing to do to try to get the vaccine.
Then again, the vaccine rollout was a nightmare. We’d jokingly feign shock that the U.S. government didn’t seem altogether invested in the health of gay men, and spent about a week individually calling the Philadelphia MPox hotline, trying desperately to get a limited vaccine. National shortages were the norm, while
an increasingly panicked public prepped blame for what seemed poised to be a second pandemic.
The breakthrough came when I realized New Jersey had vaccines to spare for anyone willing to show up. Specifically, they had them in Asbury Park. I had developed an affection for Asbury Park, the famous beach town home of Bruce Springsteen, back as an intern in the market research industry, my prior life before medicine. I worked in Plainsboro, New Jersey, which had about as much gay life as the moon. As a young recent grad, this was intolerable, so I would make the hour-or-so long pilgrimage by car every Friday night to go dancing at Paradise. Paradise, attached to the Empress hotel that dominates the boardwalk skyline, is a large (for New Jersey) gay club that had no cover in the summer if you showed up before eight. After three weeks of this, and a routine of where I liked to eat on the boardwalk (three Korean tacos and a cannoli), I fell in love. And Paradise, in the daytime at least, was now distributing vaccines.
So, date night. I got a real fast car, Dat wants an MPox vaccine. Not to mix musical metaphors, but could I make it any more obvious?
My date night is absolutely not the first time the queer community has mixed fun and an attempt to mitigate health disaster. For the unsqueamish among you, I’ll leave you to google the, shall we say, modern, alternative, non-penetrative sexual practices many activist groups promoted during the early days of the HIV-AIDS epidemic. With a thriving bathhouse scene, providing alternate spaces for group sex, with ironclad rules to prevent transmission, was a tremendous form of harm reduction.
My mind personally turns to a friend who worked in public health for the state of New York. With rising rates of meningitis, the laissez-faire kisses and cocktails of Fire Island felt like a looming disaster. Then again, who on vacation, thinking more about brunches and flings than epidemiology, really wants to go to the clinic for a shot? Leaning into the culture to try to motivate a response, my friend organized an entire drag clinic;
doctors and staff all in elaborate nurses uniforms, exaggerated falsettos telling everyone it was “time for their injection.” As you can imagine, this was the hit of the season. Crisis averted, and potentially hundreds of lives saved.
But, you’re all wondering… what did the date look like? First of all, you should realize that our arms ballooned to enormous size with the irritation of the newly-approved subcutaneous injection administration, so hand holding was out of the question. I was, in fact, quite angry after dose one, being informed that this was going to leave a scar, which no one had warned me about up until this point. Dat felt much better; growing up in Vietnam he already had a scar from his smallpox vaccine, and figured this would now be a matching set.
We got lunch at my aforementioned favorite Korean taco place, and I overindulged on the unlimited kimchi bar, and Dat got us two enormous pecan praline milkshakes. I browsed for some used records, and Dat played some pinball. We tried to ignore the elephant in the room, before falling into teasing banter about the men who would steal each other away while we were separated. Perhaps, we would say with a winking eye, there were even mutually safe conquests we had seen sucking the free lollipops at the Paradise back bar, under the nurses’ watchful eyes. Yes, this was awkward and ridiculous. So is being queer in a country where that doesn’t win you any points. So is life. You try to survive, and you try to have fun doing it. We did date five at Asbury Park two weeks later when we needed our second dose.
It’s about now I should tell you that I broke up with Dat about three months after he got back, because he never texted me, and he was obsessed with carnivorous plants as a sort of creepy status symbol, and he was super mean to some friends of mine at a Passover Seder. Live and learn. Glad I got the shot.
So, I’m left with a poem I wrote the day of, this story I wrote a few months later, and a little pink dot on my arm, and am here trying for the life of me to find the moral.
At the end of the day, though, the moral is pretty obvious for those of you who are no longer nervous about touching your patients, or having your doctor touch you. There was no outbreak. The storm never came. This isn’t to say the threat wasn’t real; quite the contrary. Gay men saw a plague coming, and said not again. We had awkward conversations, we stood in line for hours, we dealt with endless calls to the vaccine manufacturer trying to figure out if ascending lymphangitis was normal, or if the provider used a dirty needle. Okay, that might have just been a me thing.
And at the end of the day, we made it fun. Fun for ourselves, fun for others trapped in line with us, fun sharing gossip as we sat in the back of clubs and churches and rec centers waiting to see if anyone would pass out from an allergic reaction. Not to paraphrase Mary Poppins, but especially when dealing with the health dread of the marginalized, fun is an ingredient of humanity that makes medicine tolerable, and gets healthcare to the people who need it. Consider the case study of Iora Health out of Boston, turning pap testing into a monthly “pappy hour” with wine and cheese to try to make the unbearable tolerable. Medicine is expensive, and public health is underfunded, but what’s more expensive? A couple of nurse costumes, a bottle of mediocre cabernet, or countless preventable hospitalizations?
In any case, I hope I can make my patients smile one day. All I can do is hope they survive, and try to have some fun doing it. •



Although the COVID-19 pandemic highlighted a loss of trust in medical care, distrust in many communities is not new
By Monica Webb Hoope, Clinical Psychologist and Deputy Director of the National Institute on Minority Health and Health Disparities at the National Institutes of Health
Since the COVID-19 pandemic shook the globe five years ago, headlines and public conversations have focused on the public’s trust – and the lack of it – in science and medicine.
But trust, mistrust, and distrust – we’ll get to the meaning behind those terms – have been changing shape in the U.S. for decades. Surveys show declines in trust in health care, especially among populations that historically have been harmed by medical research and scientific abuses whose legacies persist today.
As a licensed clinical psychologist, behavioral scientist, and health disparities researcher, I have witnessed these effects up close on a professional level:
A middle-aged Black American patient with late-stage head and neck cancer, whom I treated for anxiety and depression some years ago, delayed seeking medical care because of prior negative experiences with doctors (such as perceived disrespect and the hesitation of clinicians to touch him during physical exams); a preference for natural remedies (such as herbs and vitamins); costly medical bills; and a history of repeated clinic visits for other symptoms with no diagnoses but multiple prescriptions. By the time he sought help, the lump on his neck had grown to the size of a large apple, and the cancer had spread to other organs.
Still another example was a woman who is a member of my own family. A mother of six, she had such negative experiences in medical settings over the years and during previous pregnancies –feeling ignored and minimized, not given pain medication when needed, and discriminated against because of her race by White doctors – that she skipped all prenatal care and went to the ER only when she went into labor with her last three children, requesting cesarean sections based on her past deliveries.
And I’ve been affected by these concerns on a personal level through my own experiences in medical settings, and simply by the fact that I’m a Black American woman in a field that has historically marginalized people like me. I was moved to partner with a community advisory board I worked with on research called the Forward Movement Project, which asked patients and residents from medically underserved populations to weigh in on health care concerns. The findings from this study and other research and surveys make clear that today many Americans deliberately avoid seeking out health care or participating in medical research until they have no other choice, reflecting personal and community experiences with these institutions that have led to widespread and deeply rooted medical distrust.
From Distrust to Confidence: Can Science and Health Care Gain What’s Missing? continued from page 27

The psychological concepts of trust, mistrust, and distrust are interconnected, yet distinct and nuanced.
Trust refers to a belief in the reliability or ability of an individual or institution. In health care and science, it’s essential for cooperation and compliance with health interventions, treatment plans, and science-based clinical guidelines as well as clinical trial participation. Studies show that patients who trust their clinicians are more likely to follow medical advice, seek help when needed, and maintain ongoing care.
Mistrust involves a vague unease or a gut feeling of skepticism, often based on past experiences, but has not yet become full-stop rejection. The sources of the doubt may not always be clear. In health care, mistrust may lead to hesitating to accept information, expressing concern about the motives for a treatment plan, or seeking second opinions specifically for validation. The scientific literature often refers to mistrust for science and medicine especially among racial and/or minority populations, but distrust is the more accurate term.
Distrust is more severe than mistrust, and reflects a firm belief that doctors, scientists, and/or health care institutions are untrustworthy, often rooted in personal or community experiences
of harm or betrayal. It can result in underutilization of health care services, belief in conspiracy theories, or outright rejection of medical advice.
And, unfortunately, history is replete with cases that fuel distrust for many people.
The U.S. Public Health Service Untreated Syphilis Study at Tuskegee is one of the most infamous examples of institutional betrayal, fueling deep distrust in science and health care, particularly among Black Americans.
From 1932 to 1972, Black men with syphilis were misled into believing they were receiving free health care but were deliberately left untreated, even after penicillin was found to be a cure. This unethical study symbolizes racial exploitation in medicine. Although its ongoing impact on distrust is debated, Tuskegee has left a legacy of institutional distrust for many Black Americans.
And there are other egregious examples of human exploitation and intentional harm in science and health care that targeted specific communities.
The eugenics movement in the early 20th century in the U.S. aimed to eliminate what its proponents considered “undesirable” traits within the population. This movement sought to “improve” FEATURE continued
the human gene pool by promoting traits associated with White individuals and those without visible disabilities who were considered the most “fit.” Consequently, Black women and Latinas, including many Puerto Rican women, endured decades of coerced sterilization that persisted into the 1970s.
Even more recently, in 1989, members of the Havasupai Tribe, a small, economically disadvantaged Tribe of 650 people, asked an Arizona State University professor for help in understanding and addressing the increase in diabetes in their community. They supplied genetic samples, only to later learn that those samples were also used for purposes they had not consented to – including research on inbreeding and alcoholism. They brought a lawsuit against the university that was settled in 2010 with the samples returned, a monetary settlement, and help obtaining funding for a health clinic.
The COVID-19 pandemic brought distrust in science and health care to the forefront, particularly among Black or African American, Latino or Hispanic, American Indian or Alaska Native, and Native Hawaiian or Pacific Islander populations, who experienced disproportionately high rates of infection, hospitalization, and death – especially in 2020, 2021, and 2022.
Despite the rapid development of COVID-19 vaccines thanks to years of mRNA research, vaccine hesitancy and low uptake were widespread.
Although political discourse, misinformation, and disinformation played roles, vaccine hesitancy among populations experiencing health disparities stemmed from historical roots as well as ongoing experiences of discrimination and neglect within the health care system.
The hesitancy, particularly in communities hardest hit by COVID-19, didn’t surprise me. Many patients I encountered expressed concerns like, “We don’t want the vaccines at all” or “We don’t want the vaccines first.” People feared they would receive a “bad batch,” questioning why underserved communities were suddenly prioritized for the first time in modern U.S. history.
Ironically, the prioritization was due to public health leaders’ aim to promote racial and ethnic equity in vaccine access. But the long-standing and justified distrust left many skeptical – showing just how challenging building trust in many communities will be. This distrust extends beyond vaccines, affecting areas such as cancer treatment, maternal health, and mental health services, where access and outcome disparities persist.
The conversation around distrust in science and medicine tends to focus on racial and ethnic minority populations, though a Gallup Poll indicated that only 36% of U.S. adults overall say they have a great deal of confidence in the medical system, compared with 80% in 1975.
Moreover, other populations experiencing health disparities – including sexual and gender minority groups, people with low socioeconomic status, people living in underserved rural areas, and people with disabilities – also report trust-related concerns for clinicians or the health care system because of the way they are treated.
These concerns are ripe for repair. But building trust will require hard work and showing trustworthiness and genuine engagement with the people who have the least confidence.
My own research on distrust in science and health care, the Forward Movement Project, offered an approach for examining these significant issues. We created a community-academic partnership to understand some aspects of the multilayered factors related to trust or distrust. Our community advisory board members were involved in every step of the research process – from identifying priorities to developing an intervention – giving them a sense of ownership and agency that are critical to rebuilding trust. We first went on a “listening tour,” hosting town hall-style meetings with members of underserved communities.
The research participants spoke candidly about their personal experiences, as well as those of their family and friends, within medical settings, and many were related to their current medical distrust. “We don’t trust the system, because it can’t be trusted. Health care should come first, but it’s become a business,” one person told us. Another said, “Trust was broken long ago in the African American community when it comes to medical research. People should be informed before they agree to participate, but the health care system hasn’t done enough to ease our concerns.” We shared the findings with hospital leadership, clinicians, other researchers, and the very people we listened to.
Based on comments like these, the challenges for repairing confidence in the medical system loomed large. A key finding from the Forward Movement Project was the importance of reciprocal trust-building between communities and institutions. Participants stressed that trust must be earned through transparency, accountability, and collaboration, with institutions showing a willingness to listen, learn, and adapt their practices based on community input.
continued on next page
continued
From Distrust to Confidence: Can Science and Health Care Gain What’s Missing? continued from page 29
So, about a year later, we returned to the same neighborhoods for the second phase of the research, bringing clinicians with us so that they could talk directly with community members and answer questions raised about the health care system. This was what we called a “user-generated” intervention, which consisted of participant-driven dialogues with oncology clinicians and support professionals. This was a rare opportunity for conversations between community members and health care professionals and researchers, allowing participants to discuss their questions about care, and to initiate important discussions. Findings from this second phase of the project were positive and indicated that this activity helped people learn new things about science and medicine and would help them during future medical encounters, and over half reported more willingness to join a clinical trial than before the intervention. This kind of open communication is a crucial first step toward building trust.
The Forward Movement Project also highlighted the importance of representation in reducing distrust. Community participants noted that racial or ethnic matching with clinicians improves culturally competent communication and empathetic care. Other research supports increasing the number of scientists and health care professionals from underrepresented backgrounds to create a workforce that better reflects the communities it serves.
Trust is a fragile, underappreciated psychological construct that must be earned and is difficult to repair once broken. In that way, institutional distrust is not unlike repeated betrayals in personal relationships, but on a much larger and intergenerational scale.
It’s up to those with power and authority to take concrete actions for improvement so biomedical institutions and health care systems hold the primary responsibility for addressing distrust. Here are some ways they could start:
Publicly acknowledge the historical wrongdoings that have contributed to distrust, such as the Tuskegee syphilis study and forced sterilizations. This includes issuing apologies, acknowledging ongoing harm, and outlining the tangible steps to ensure that these violations never happen again.
Recruit and retain well-qualified individuals from underrepresented backgrounds at all levels – from students to leadership positions. Reflecting the diversity of the populations served is important, as is ensuring that these persons are committed to the intentional and long-term efforts needed to
make progress on building trust.
Implement continual and comprehensive training on factors known to influence trust and distrust, such as cultural competency, bias, and practices and policies that foster and maintain inequities.
Invest in long-term partnerships with communities, not just when there is a need for research participants or representatives to serve on patient advocacy boards without decision-making authority. The exchange of knowledge is critical, and community members can offer informed views on health care policy, research agendas, and institutional priorities.
Move beyond traditional metrics of success such as patient satisfaction surveys, and instead work with communities to define what successful relationships and outcomes look like, which might include measures of trust, community empowerment, and perceived respect. This also involves engaging in health education, supporting local health initiatives, and contributing to overall community well-being.
Demonstrate a genuine desire to build and maintain trusting relationships. This will require efforts to strengthen oversight and accountability, such as independent panels consisting of scientists, clinicians, and community voices; community-identified and wellresourced public health initiatives; regular equity-focused audits of policies, treatment, and health outcomes, research enrollment and patient demographics; and corrective actions when disparities are identified.
Reducing distrust that has built up over a long time is far from simple. However, science and health care institutions can choose to take proactive, transparent, and sustained steps toward rebuilding trust. Equally important, they should raise awareness at local, state, and national levels about their efforts to prioritize the best interests of all communities for a more equitable future. •
About the Author: Monica Webb Hooper is a clinical psychologist and deputy director of the National Institute on Minority Health and Health Disparities at the National Institutes of Health. This document is a reprint granted permission by The Pew Charitable Trusts and is provided for informational purposes only. The original copyright holder retains all rights to the content. Please refer to the original source From Distrust to Confidence: Can Science and Health Care Gain What’s Missing? | The Pew Charitable Trusts for the most up-to-date information and any necessary permissions for further reproduction or distribution.












Saturday, April 26, 2025
8:00 AM - 12:30 PM
Thomas Jefferson University, Bluemle Life Sciences Building, Rooms 105 and 107 233 S. 10th Street, Philadelphia, PA 19107
Program Director : David A. Sass, MD FACP FACG AGAF FAASLD
Rorer Professor of Medicine, Division of Gastroenterology and Hepatology, Sidney Kimmel Medical College at Thomas Jefferson University, Medical Director, Liver Transplantation, Thomas Jefferson University Hospital













At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.