CHIRONIAN
LEADING THE CHARGE
FINDING NEW WAYS TO IDENTIFY AND TREAT STRESS


FINDING NEW WAYS TO IDENTIFY AND TREAT STRESS

Vice President of Communications and Strategic Initiatives
Jennifer Riekert, M.B.A.
Editor Lori Perrault
Writers
Lenore Carpinelli
Rhea Hirshman
Andrea Kott, M.P.H.
Contributor
Barbara Moroch
Lori Perrault
Melissa F. Pheterson
Kristin Baird Rattini
Kiara Thomas, M.A. Nicholas Webb, M.S.I.S.
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer
Editorial Board
Salomon Amar, D.D.S., Ph.D.
Doris Bucher, Ph.D.
Lenore Carpinelli
Bess J. Chazhur, M.S.
Tetyana Cheairs, M.D., M.S.P.H.
Mill Etienne, M.D. ’02, M.P.H.
Design
Wayne Printing, Inc.
Photography
Christopher Pope
William Taufic Photography
Alan Kadish, M.D., President
Ben F. Johnson, Ed.D.
Edmund F. LaGamma, M.D. ’76
Joseph F. Morales, D.D.S.
Dana Mordue, Ph.D.
Michelle Novotny, M.A.
Michal L. Schwartzman, Ph.D.
John Vecchiolla Photography
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer and Interim Dean, School of Medicine
Robert W. Amler, M.D., M.B.A., Dean, School of Health Sciences and Practice, Vice President for Government Affairs
Marina K. Holz, Ph.D., M.P.H. ’23, Dean, Graduate School of Biomedical Sciences

Office of Public Relations
Jennifer Riekert, M.B.A., Vice President of Communications and Strategic Initiatives
Lenore Carpinelli, Director of Strategic Communications, School of Medicine
Tyler Landis, M.B.A., Assistant Director of Communications, School of Health Sciences and Practice
Lori Perrault, Director of Print and Digital Publications
Madlena R. Pesheva, M.P.H. ’21, Director of Creative Communications and Production
Julio A. Rodriguez-Rentas, M.A., Senior Director of Strategic Communications
Kiara Thomas, M.A., Communications Writer and Content Creator
Please direct all inquiries to:
New York Medical College/Chironian, 40 Sunshine Cottage Road, Valhalla, NY 10595. We authorize the use of any material with attribution to New York Medical College. Chironian is published annually by the Office of Public Relations. We welcome reader feedback.
Contact us at (914) 594-4536 or at chironian@nymc.edu.
Major Clinical Affiliated Sites
Westchester Medical Center Health Network (WMCHealth)
Westchester Medical Center
Maria Fareri Children’s Hospital
Good Samaritan Hospital
NYC Health + Hospitals/Metropolitan
Clinical Affiliated Sites
Beckley VA Medical Center
Calvary Hospital
Greenwich Hospital
Hoboken University Medical Center
James J. Peters VA Medical Center
Landmark Medical Center
Lenox Hill Hospital
Northern Westchester Hospital
NYC Health + Hospitals/Lincoln
Ambulatory Care Programs
CareMount Medical
Open Door Family Medical Centers
Refuah Health Center
Health Alliance Hospital
MidHudson Regional Hospital
Phelps Hospital Northwell Health
Richmond University Medical Center
Rome Memorial Hospital
Saint Clare’s Hospital
Saint Joseph’s Medical Center
Saint Michael’s Medical Center
St. Mary’s General Hospital
Terence Cardinal Cooke Health Care Center VA Hudson Valley Health Care System
Westchester Institute for Human Development
Westmed Medical Group
CONNECT WITH US: www.nymc.edu

facebook.com/nymedcollege and facebook.com/nymcalumni

Follow us on Twitter @nymedcollege
Connect with us on LinkedIn @new-york-medical-college
Follow us on Instagram @nymedcollege
Touro was recently granted university status by the New York State Board of Regents. The word “university” shares a root with “universe”: the totality of existing things. University is a shortened version of “universitas magistrorum et scholarium” meaning a “community of masters and scholars.” A health science university is uniquely positioned to draw upon the resources of a diverse community of scholars to generate new techniques and new knowledge.
Much has been written and said about interprofessional health professions education and collaboration. Health care is often delivered by teams. Close coordination between physicians, nurses, physical therapists, speech-language pathologists, psychologists, social workers, physician assistants and other disciplines is the norm in modern health care. Within a discipline such as medicine or dentistry, multiple specialists are often involved in the care of a patient and, similarly, close coordination of these specialties is essential.
During the past year, I have treated two patients where I have seen unequivocal evidence of the benefits of interprofessional collaboration, which is characteristic of a university. The first patient was a teenager with rhabdomyosarcoma of the flexor digiti minimi brevis muscle of the hand. Rhabdomyosarcoma is a malignant, and potentially fatal, tumor of striated muscle. The flexor digiti minimi brevis muscle plays an important role in control of the fifth digit. The tumor was palpable beneath the palm. The second patient was a three-year-old with vaginal rhabdomyosarcoma.
To cure rhabdomyosarcoma one needs to treat with chemotherapy and, in general, also obtain local control of the primary tumor with surgery, radiation therapy alone or surgery combined with radiation therapy. In the case of the teenager with the tumor of the hand, extirpative surgery or high dose external beam irradiation would seriously compromise long-term function of the hand. In the case of the young child with rhabdomyosarcoma, the adverse consequences of a radical vaginectomy are obvious. External beam radiation therapy would have a high risk of injury to the bladder, rectum and bony pelvis.
A well-established technique to obtain malignant tumor control with preservation of normal tissue function is the use of a radioactive implant as an alternative to external beam irradiation. This highly localized form of radiation is commonly employed in adults with carcinoma of the cervix or prostate.
But how could I fabricate customized molds of the body part that needed to be irradiated in these children and use these molds as carriers of the tubes which would contain the radioactive seeds? A walk across the New York Medical College (NYMC) campus to visit our partners at the Touro College of Dental Medicine (TCDM) at NYMC solved the problem. TCDM faculty, led by Dr. Alan Jurim, are highly skilled dental mold makers and operators of three-dimensional printers. For both patients, they fabricated customized devices which, in conjunction with a robot, delivered the radiation exactly where it was needed whilst allowing us to shield tissues we did not wish to irradiate.
One of the roles of a professor is to model good behavior. The students at NYMC and the TCDM witnessed the good behavior of interprofessional collaboration amongst the “community of masters and scholars” in the care of these two children. I hope that our students will carry with them the lesson that the silos of individual disciplines must be cast aside for the purpose of maximizing the benefits accrued to an individual patient.
I assure the NYMC community that our faculty will continue to strive to be at the forefront of interprofessional collaboration and education in health care and the biomedical sciences and to serve as role models for our students.
Edward C. Halperin, m.d., m.a. chancellor and chief executive officer



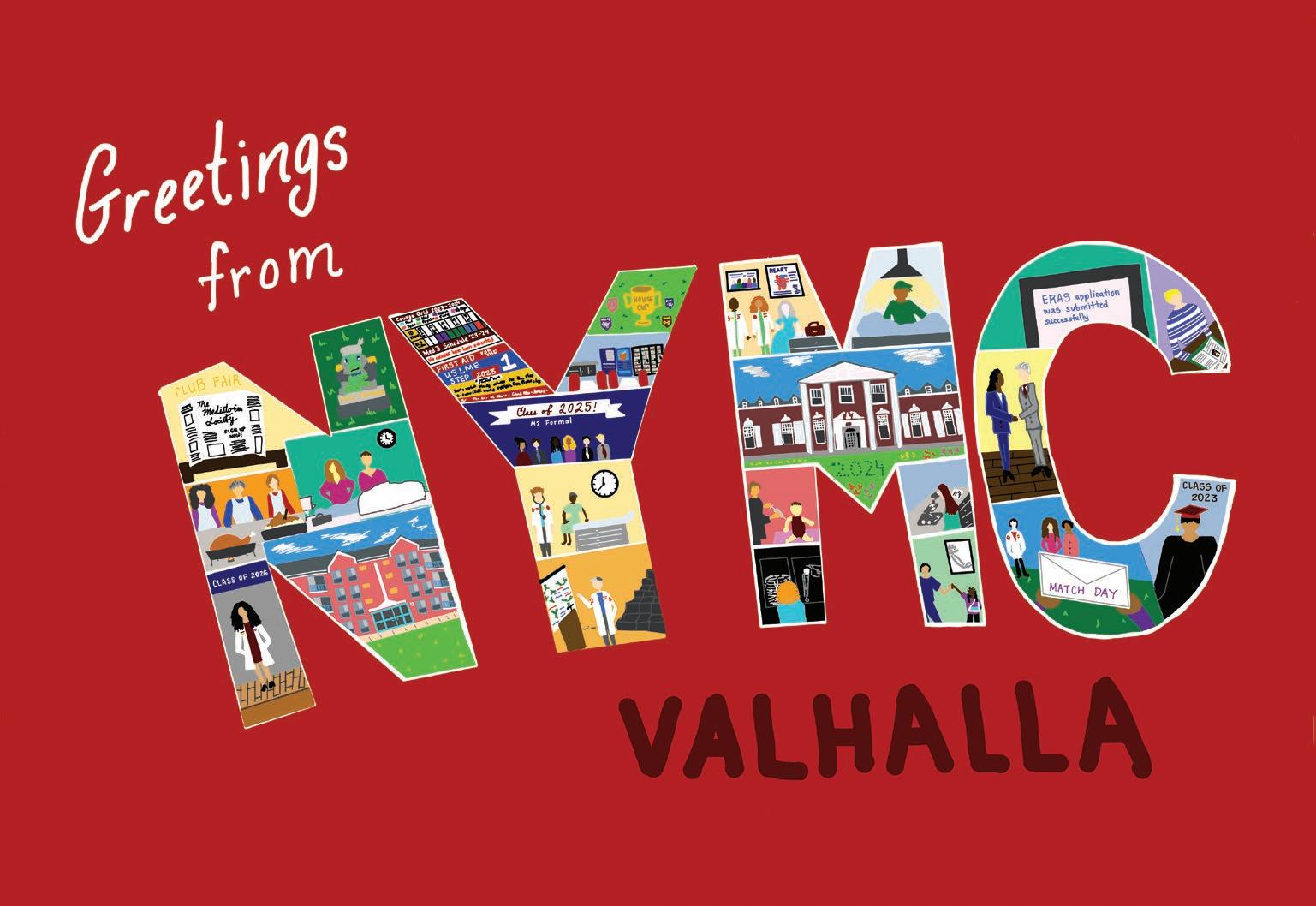
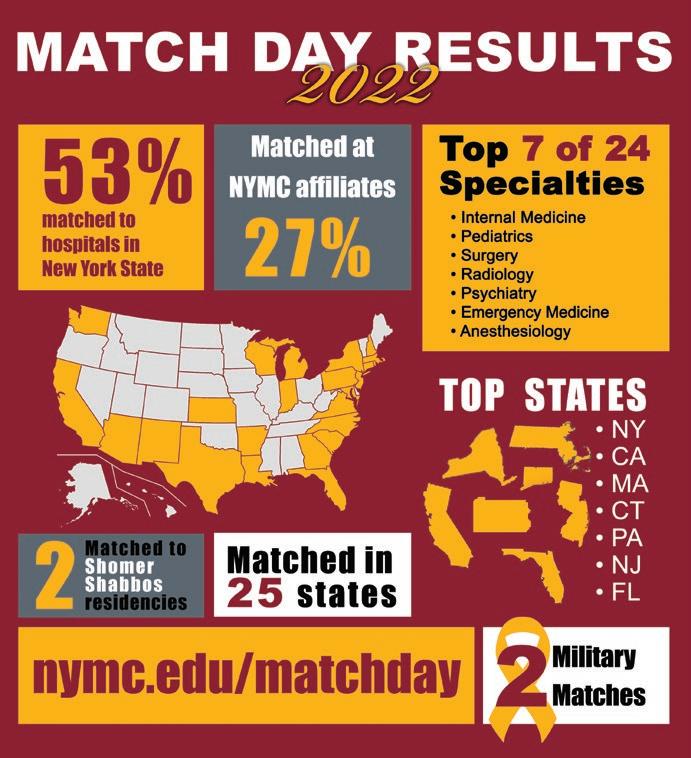
Members of the School of Medicine (SOM) Class of 2022 had the opportunity to celebrate Match Day in person on March 18, 2022—for the first time since the pandemic began—as they gathered in the radiant sunshine outside the Medical Education Center (MEC) to learn where they matched to medical residency programs.
The atmosphere outside the MEC was electric as students anxiously awaited noon when they could at last tear open their envelopes to find out where they will take the next step in their medical education training. When the time to learn their match results came, the atmosphere quickly transformed to one of celebration–with shouts of happiness filling the air.
The SOM Class of 2022 is training in 25 states at 105 different institutions. Some were matched at NYMC’s affiliate hospitals— Westchester Medical Center, NYC Health + Hospitals/Metropolitan, NYC Health + Hospitals/Lincoln, Greenwich Hospital, Lenox Hill Hospital, Richmond University Medical Center and Landmark Medical Center—as well as other academic medical centers across the country, including two hospitals of the Harvard Medical School System (Massachusetts General and Beth Israel-Deaconess), Walter Reed National Military Medical Center, Brown, Dartmouth, Emory, Mount Sinai, Johns Hopkins, Columbia, Weil Cornell, New York University, Tufts, UCLA and Yale.
The top career choices for the Class of 2022 were internal medicine, pediatrics, general surgery, radiology, psychiatry, emergency medicine, anesthesiology, family medicine, obstetrics and gynecology, orthopedic surgery, neurology and urology. ■
The New York Medical College (NYMC) and Touro University (TU) communities came together for a somber and informative observation of Yom Hashoah on April 28, 2022, hosted in conjunction with the Miriam Popack Chair in Bioethics and the Holocaust. The ceremony, which welcomed audiences both in-person and online with more than 560 viewers, featured presentations that explored the impact of the Nuremburg Trials on the evolution of medical ethics through the perspective of experts in law and ethics.
Marie T. Ascher, M.S., M.P.H., the Lillian Hetrick Huber Endowed Director of the Phillip Capozzi, M.D., Library, and Sheldon Rubenfeld, M.D., FACP, clinical professor of medicine at Baylor College of Medicine and executive director of the Center for Medicine after the Holocaust, presented opening remarks. Dr. Rubenfeld called the Nuremberg Trials a watershed event in the history of medical ethics and spoke about the impact of unsung hero John W. Thompson, M.D., a member of the Canadian Air Force, who laid the groundwork for the trials after deeming much of the research done by Nazi physicians as criminal.
A deeper look into the trials and the Nuremberg code was presented by George J. Annas, J.D., M.P.H., William Fairfield Warren Distinguished Professor and director of the Center for Health Law, Ethics and Human Rights at Boston University's Schools of Public Health, Medicine and Law during his presentation, “The Nuremberg Doctors Trials and the Birth of Bioethics.” He described how the code gave rights to human research subjects, and how the dehumanization of victims, in this case, Jewish people, is prevalent when large numbers of people are killed.
John Q. Barrett, J.D., Benjamin N. Cardozo Professor of Law at St. John’s University, provided a different look at the initial Nuremberg trial before

the subsequent “doctors’ trials” and focused on the pivotal role played by Associate Supreme Court Justice Robert H. Jackson as chief prosecutor for the United States in the trials of Nazi physicians, who is credited with being a driving force in the trials.
The psychology behind the Holocaust and how the Nazi physicians thought was broken down by renowned psychiatrist and alumnus Robert J. Lifton, M.D. ’48, author of The Nazi Doctors. Dr. Lifton, who has spoken to Nazi physicians himself for his research, explained how they believed that they were benefitting others by murdering Jews.
Boaz Nagar spoke of the experience of his father, Shalom, who as a prison guard was involved with the execution of Adolf Eichmann, one of the primary orchestrators of the Holocaust. Nagar said that his father stayed strong in his faith despite the execution being deeply traumatic for him and that this instance represented the commitment to justice after the Holocaust.
Rabbi Moshe D. Krupka, M.S., executive vice president, TU, closed the event by recounting the story of Hadassah Bimko Rosensaft, M.D., a Jewish dentist from Poland who saved hundreds of lives in concentration camps, even after her family was killed. “Dr. Bimko was a victim. She reached down deep and found the strength to peel away at the pain, to peel away at the adversity,” Rabbi Krupka said. “Dr. Bimko understood that this is the mission of mankind to help others.” ■
Itwas a milestone occasion as members of the Doctor of Physical Therapy (D.P.T.) Class of 2024 took a symbolic step toward beginning their clinical studies as they donned their white coats for the first time during the White Coat Ceremony on April 12, 2022. Family and friends of the students witnessed their loved ones affirm their commitment to the field of physical therapy.
The D.P.T. cohort processed into the ceremony with their coats in hand and enjoyed a keynote address by alumnus Dominique Torres, P.T., D.P.T. ’15, CBIS, senior physical therapist at Mount Sinai Hospital, who spoke about finding one’s purpose, or one’s “why,” when it comes to physical therapy and embracing a humanist approach to the profession.

Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, also addressed the students telling them that the coat sends a message to others that they can be trusted and that they will follow science in their treatment. “Each of you can decide what thoughts go through your mind when you put on your white coat, but wear it with humility and with pride, do nothing to ever dishonor the message sent by the white coat,” Dr. Halperin said.
The pinnacle of the ceremony followed with the students putting on their white coats with the assistance of faculty before reciting the Pledge for Physical Therapy from the American Physical Therapy Association Education Section 2004, a pledge the D.P.T. Class of 2024 will reaffirm at their commencement. ■

Touro University (TU) celebrated their 50th anniversary with more than 1,000 students, alumni, faculty, friends and supporters from around the world at New York City’s Marriott Marquis on December 4, 2022. Past, present and future merged at this celebration of Touro’s meteoric rise from a small college with 35 students to an academic powerhouse with 19,000 students, 140,000 alumni and 246 undergraduate, graduate and professional programs producing valued leaders in medicine, business, law and more.
Touro’s visionary founder, Dr. Bernard Lander, of blessed memory, built a college from the ground up at age 56 and continued expanding its programs until well into his 90s. His dream of creating a center of higher education that would literally be all things to all people has been realized. Under the skillful leadership of his successor and current President Alan Kadish, M.D., Touro has emerged as an institution imbued with Jewish values and a diverse group of students who enjoy a quality education and meaningful careers in a wide array of fields.
With this historic milestone, the community also celebrated the new TU Campus dedicated to Cross River Bank. The bank’s chief executive officer and founder and member of TU’s Board of Trustees, Gilles Gade, and the bank’s board gifted $5 million for the campus at 3 Times Square, an iconic skyscraper in
midtown Manhattan. The Cross River Campus of TU houses the College of Pharmacy, New York School of Career and Applied Studies, Graduate School of Education, Graduate School of Jewish Studies, Graduate School of Social Work and Graduate School of Technology.
TU has also proudly introduced a new look to their logo. Their iconic initials will now be a locked into a monogram shaped like a shield to represent prestige and excellence in higher education. The emblem will be crowned with an eternal flame as a symbol of the University’s Judaic heritage and the illuminating power of education, a beacon to all those who seek knowledge and the warmth of community.
“Looking at the world today, where 73 percent of college students say they hide their Jewish identity on campus and 50 percent report experiencing antisemitism, Touro’s mission is more important than ever. Students from diverse backgrounds representing all nationalities and ethnicities share ideas, friendship and collaboration…At Touro, we are developing students who will become leaders of tomorrow, the right kind of leaders—those who are dedicated to serving society and understanding and respecting others. Here’s to the next 50 years!” said Dr. Kadish. ■

The keynote speaker, Leonard J. Newman, M.D. ’70, professor and chair of the Department of Pediatrics and associate professor of family and community medicine, spoke about the importance of compassion when seeing patients, and the three “A’s” of being a physician— affability, availability and ability, which can be challenged by external factors.
The White Coat Ceremony for the New York Medical College (NYMC) School of Medicine (SOM) Class of 2026 on July 29, 2022, capped off an eventful Transition to Medical School Week for more than 210 incoming medical students. The ceremony marks the first time that students don their white coats before beginning their medical education. Students filed into the elegant Palace Theater in Stamford, Connecticut, along with NYMC and Touro University (TU) leadership and faculty to put on their white coats with the help of faculty
investors in front of an audience of more than 1,300 guests.
“You are beginning a journey that will achieve many milestones, meeting lifetime mentors, friends and colleagues, and pursuing academics to become a physician. Receiving your white coat in the presence of your family, friends and school, is a big honor and a day you will forever remember,” said Deepika Dhawan, SOM Class of 2023, who spoke to the students as a member of the Gold Humanism Honor Society.
Lovelace Research Institute in Albuquerque, New Mexico, has joined Touro University (TU) and New York Medical College (NYMC). Founded in 1947, Lovelace is one of the oldest notfor-profit biomedical research institutes in the country. The Institute is noted for excellence in respiratory disease, neuroscience research, toxicology, drug development experience and in protecting the nation against chemical, biological and nuclear threats.
“Touro is thrilled that Lovelace is joining our university. This affiliation will significantly impact our research capability and expand our capacity to make a difference in the health and lives of Americans. Together with Lovelace, Touro will be able to bring in-depth understanding of potential

health risks and optimize the efficacy of pharmaceuticals,” said Alan Kadish, M.D., president of TU and NYMC.
“We also plan to leverage the Lovelace clinical trial infrastructure, to run a Touro/NYMC centralized clinical trials research office. Our NYMC faculty will serve as M.D. advisors for Lovelace clinical trial research and provide basic science support in infectious disease,” continued Dr. Kadish.
Lovelace has three campuses in Albuquerque comprising more than 375,000 square feet of research lab space and receives more than $70 million per year in grants and contracts. The Institute has published thousands of research papers and employs 400 physicians, scientists and researchers.
“As you care for patients you must be sensitive to their emotional and social needs,” Dr. Newman said. “You will certainly have the ability to be an outstanding physician, but you need to ensure that the care you deliver will meet the needs of your patients from the point of view of your affability and availability.”
Proudly wearing their new white coats, the future physicians recited the Class of 2026 Medical Student Oath that was carefully and thoughtfully crafted by the students who pledged to “acknowledge that the white coat signifies a sacred and implicit trust…and strive daily to earn and to honor that trust.” ■
“We are looking forward to collaborating with Touro on research projects increasingly over time,” said Robert Rubin, Ph.D., president and chief executive officer at Lovelace Research Institute. “This new affiliation will provide long-term stability, new opportunities to expand our mission as we join an academic medical center. The leadership is excited at this new opportunity to advance our mission to improve public health.” ■
The School of Medicine (SOM) Class of 2026 will be the first class to experience the new medical education curriculum launched in 2022. The new curriculum, which was developed by a broad representation of administration, faculty and students, integrates basic science and clinical course content during the first 18 months of medical education, while also allowing students to enter clerkships much earlier in their education.
“In the old curriculum, the discipline-based courses, such as histology, anatomy, pathophysiology and pharmacology, were taught separately. Now we have completely integrated those courses so they no longer exist in isolation,” said Pamela Ludmer, M.D., M.S., associate dean for curriculum integration. “The first new course, Fundamental Processes of Life, incorporates the basic foundational principles from some of these different disciplines, as well as biochemistry, ethics and patient care. This is extremely important because as physicians, we do not think of pharmacology, anatomy and histology, for example, separately from patient care. We look at the patient as a whole person and think of everything as being connected. We want to teach our medical students how to integrate this knowledge together from the start.”
Later in the first year of the new curriculum, students take an introduction to systems course, which bridges the content from the fundamental processes course, introduces concepts that will be applied throughout the remaining courses and further integrates basic science with patient care and health systems science principles.

“The focus is to create courses that are not siloed but are integrated organ systems-based, including brain and behavior, cardiorespiratory, renal/ reproductive/endocrine and gastroenterology/dermatology/ rheumatology,” said Dr. Ludmer. “Another important area of focus is health system science, in which we teach students concepts that allow them to function in a very complex health care system—patient safety, quality improvement, high value care, leadership and teamwork. And this is something we have been incorporating not just into this new curriculum but for all our classes of students.”
In addition, as part of the new curriculum, students will also enter clerkships three months earlier—in April of their second year of medical education— allowing them more time to solidify their clinical skills, complete scholarly projects and prepare for residency. ■

New York Medical College (NYMC) and Union Community Health Center (UNION) in the Bronx, New York, have partnered to establish a clinical and allied health profession training program at UNION to provide students with clinical and public health policy experience during required and elective rotations in the fields of medicine, public health, physical therapy and speech-language pathology. The collaboration with one of the largest Federally Qualified Health Centers in New York State will also have additional opportunities for biomedical, clinical, translational and public health research activities.
The academic affiliation agreement will enhance the training and education of future primary care providers and health professionals and address workforce shortages and challenges faced by underresourced communities by providing culturally competent training venues for the development of a culturally competent workforce. The agreement also covers fostering research opportunities regarding health care policy, biomedical science, financial, legal/regulatory and social elements pertaining to these communities.
“NYMC and UNION share common culture and values centered on providing high quality, accessible medical care and education to everyone, with a specific focus on underresourced communities,” said Salomon Amar, D.D.S., Ph.D., vice president for research at NYMC and senior vice president for research affairs at Touro University. “Founded on common goals and interests, the affiliation will be beneficial to patients, students, health care providers and community members in the Bronx, and in the promotion of translational and interdisciplinary research.” ■
The New York Medical College (NYMC) Master of Science Clinical Laboratory Sciences (CLS) program in the Graduate School of Biomedical Sciences was granted accreditation for five years by the National Accrediting Agency for Clinical Laboratory Sciences (NAACLS). The accreditation, awarded to the program for the first time, gives the program national recognition and affirms the program’s high academic standards.
The CLS program, which began in 2019, provides a unique health care opportunity, training students for a professional career in medical and pharmaceutical laboratories, performing diagnostic laboratory tests to help monitor treatments and uncover new disease states. Completion of the CLS program at NYMC qualifies the student to take the New York State Exam for Clinical Laboratory Science licensure, upon graduation, a requirement of the New York State Education Department to work in a hospital laboratory.

“I am delighted that our CLS program is recognized by this national accrediting agency because it underscores the quality of our program. This milestone would not have been possible without the hard work of the faculty and staff of this master’s program, who provide support and mentorship to our students,” said Carol Carbonaro Ph.D., SM, MLSCM, CLS program director and clinical associate professor of pathology.
The excellent news comes just three years after the program welcomed its first class of students and one year after the program saw its first graduates in 2021.
NAACLS accreditation assures current students, graduates and future applicants that NYMC has developed a program which meets established national education standards in clinical laboratory science. ■

GraduateMedical Education (GME) at New York Medical College (NYMC) has enjoyed another successful year, under the new leadership of Jennifer Salcedo, M.D., M.P.H., M.P.P., FACOG, who joined NYMC as the designated institutional official and associate dean for graduate medical education, in August 2022. Dr. Salcedo previously served as associate professor and residency program director in the Department of Obstetrics and Gynecology at the University of Texas Rio Grande Valley (UTRGV). While at UTRGV, she collaborated with colleagues to develop the new residency program and started an innovative border health track to address community needs in women’s health.
The Accreditation Council for Graduate Medical Education (ACGME) has again granted continued accreditation to the NYMC School of Medicine (SOM) as the sponsoring institution for medical residency programs overseen by the school. The ACGME’s Institutional Review Committee said the SOM demonstrated substantial compliance with the ACGME's institutional requirements and approved the annual review with commendation.
One of the strengths of NYMC medical training is the College’s extensive network of affiliated hospitals and clinical sites that encompasses more than 25 affiliates, across four states—New York, New Jersey, Connecticut and Rhode Island. Most recently, NYMC signed an academic affiliation agreement with New Jersey hospitals St. Mary’s General Hospital in Passaic and Saint Clare’s Hospitals in Denville and Dover to sponsor residency programs in internal medicine and psychiatry at the hospitals, which are members of the Prime Healthcare System.
Prime Healthcare sought out NYMC for this affiliation after witnessing the exceptional quality of NYMC’s undergraduate medical education program and graduate residency and fellowship programs through NYMC’s affiliation with Saint Michael’s Medical Center in Newark, New Jersey, and Landmark Medical Center in Woonsocket, Rhode Island, which are also members of Prime Healthcare.
GME also continues to expand its programs at existing affiliate sites, with the introduction of an NYMC-sponsored fellowship program in endocrinology, metabolism and diabetes at NYC Health + Hospitals/Metropolitan (MET) in New York City.
After a nationwide search, Leslie Halpern, D.D.S., M.D. ’93, Ph.D., M.P.H., has joined NYMC as program director of the NYMC-sponsored Oral and Maxillofacial Surgery Residency Program at MET. Dr. Halpern will also serve as section chief of oral and maxillofacial Surgery at MET and as an attending clinician/educator at Westchester Medical Center. Holding multiple master’s and doctoral degrees, Dr. Halpern brings a unique and robust formal educational background to her new roles, including a D.D.S. from New York University, an M.D. from NYMC and an M.P.H. from Harvard University. ■
The School of Health Sciences and Practice (SHSP) opened the Spring 2023 semester with a new Master of Public Health (M.P.H.) Generalist Program. The generalist program, which involves less time and cost, enables students to customize their education according to their interests and needs, while gaining a broad grounding in public health and expert knowledge in the core competency areas.
The 42-credit M.P.H. Generalist Program allows up to 18 to 21 elective credits, which in some cases may also fulfill the requirements for an advanced certificate. In addition, the cost may be covered by financial aid, sparing or reducing out-ofpocket expenses. The program is accredited by the Council on Education for Public Health. Courses are offered on campus, online or in hybrid fashion to accommodate student schedules and needs.
“The benefit of the M.P.H. Generalist Program is it gives students a broad range of knowledge in public health with the flexibility to focus on a specific discipline if they choose to do so,” said Kenneth A. Knapp, Ph.D., assistant professor and interim vice chair of the Department of Public Health, director of the Dr.P.H. program, and director of the Center for Long-Term Care. “The trend for M.P.H. generalists is definitely on the uptick and New York Medical College is on the forefront of keeping up with the ever-changing world of public health.”
“It is an exciting, yet challenging time, to be in the field of public health. Our M.P.H. Generalist Program is designed to prepare students to meet those challenges and become skilled practitioners equipped to address the health needs of populations,” said Michelle Novotny, M.A., associate dean for admissions and enrollment management, SHSP.
The M.P.H. Generalist Program is available to medical students who wish to earn a dual M.D./M.P.H. degree. “Knowledge of public health issues is important for physicians to better care for their patients. The M.P.H. Gen will give them that knowledge to address issues beyond medical care,” said Dr. Knapp.
“An M.P.H. degree is a major step for a serious student of public health science, practice, policy or administration,” said Robert W. Amler, M.D., M.B.A., dean of the SHSP and vice president for government affairs. “Our new M.P.H. Generalist Program is designed to make that step a bit lighter and more directly focused on each student’s desired career path.” ■



New York Medical College (NYMC) formed a new academic affiliation with New Jersey hospitals, St. Mary’s General Hospital in Passaic and Saint Clare’s Hospitals in Denville and Dover, which designates the hospitals as primary clinical sites for the education of NYMC residents. The NYMC sponsorship includes residency programs in internal medicine and psychiatry and further enhances NYMC’s extensive network of affiliated hospitals and clinical sites that encompasses more than 25 affiliates, across four states—New York, New Jersey, Connecticut and Rhode Island.
“At NYMC, we are proud to expand residency training to high-quality sites, such as St. Mary’s General Hospital and Saint Clare’s Hospitals, where residents and program faculty strive to serve their communities,” said Jennifer Salcedo, M.D., M.P.H., M.P.P., FACOG, associate dean for graduate medical education, designated institutional official and associate
professor of obstetrics and gynecology at NYMC. “Working with the leadership and clinicians of these hospitals expands opportunities for collaboration between our NYMC-sponsored programs for the benefit of learners and patients in our evolving health care system.”
The hospitals are members of the Prime Healthcare System and have been trusted providers of health care for more than 125 years. St. Mary’s is a nationally recognized 293-bed acute-care hospital that specializes in cardiovascular services, a comprehensive program for cancer care, both inpatient and outpatient behavioral health services and is a center of excellence for maternal-child health. Saint Clare’s Health is nationally recognized in advanced cardiac care, a certified primary stroke center, Morris County’s first accredited Comprehensive Center for Bariatric Surgery, as well as offers the most comprehensive behavioral health services in Northern New Jersey. ■
Cheers filled the tent behind Sunshine Cottage on May 24, 25 and 26, as members of the Class of 2022 shared in the celebration of the culmination of their time at New York Medical College (NYMC), as the pomp and circumstance of commencement returned to an in-person setting for the first time since the beginning of the COVID-19 pandemic. Separate ceremonies took place in order to be able to accommodate nearly 1,900 guests who took in the lush green space and beauty of the Valhalla campus which was in full bloom.
The three ceremonies—the School of Health Sciences and Practice (SHSP) and Graduate School of Biomedical Sciences (GSBMS), then known as the Graduate School of Basic Medical Sciences on May 24, the Touro College of Dental Medicine on May 25, and the School

of Medicine (SOM) on May 26—conferred 594 degrees to the Class of 2022, including 218 doctor of medicine (M.D.) degrees, 42 doctor of physical therapy (D.P.T.) degrees, four doctor of philosophy (Ph.D.) degrees, 120 master of science (M.S.) degrees, 103 master of public health (M.P.H.) degrees, two doctor of public health (Dr.P.H.) degrees and 105 doctor of dental surgery (D.D.S.) degrees.









Students and guests at the SHSP and GSBMS ceremony had the opportunity to hear from commencement speaker Sherlita Amler, M.D, M.S, R.N., Ed.S., C.E.M., Commissioner of Health in Westchester County, adjunct professor of public health, clinical associate professor of pediatrics, and senior fellow in the Center for Disaster Medicine.




Dr. Amler spoke from her more than four decades of experience as a public health professional, including the last two amidst the COVID-19 pandemic. “The future health of our people will depend in part on you and your professional colleagues. Some of you will go on to develop new procedures, treatments and preventive strategies,” Dr. Amler said. “Never in our shared history has the work you have prepared for been more vital. My fondest wish for you is that you find professional and personal fulfillment using the tools you have acquired here, while making this world a healthier place.”
The SOM welcomed commencement speaker, award-winning scientist and executive, Albert Bourla, D.V.M., Ph.D., chair and chief executive officer of Pfizer. Dr. Bourla has received various accolades for his work leading Pfizer,









especially during the COVID-19 pandemic. Dr. Bourla spoke about the monumental task of developing an effective vaccine in a time span that would shatter previous records, and how it took an ambitious mindset to achieve it.
“At Pfizer, we referred to the development of our COVID-19 vaccine as a moonshot–a term shorthand for reaching big, for pursuing aspirational and difficult ventures. Today I challenge you to pursue your own moonshot. To ask yourself how you can achieve something no one else has done before,” Dr. Bourla said. “I encourage each one of you to aim high, higher than you can ever imagine. If at first you miss, do not lower the target. Keep aiming high because when you hit, the reward will be great; for you and for the people that are dependent on you.” ■
Steven Lansman, M.D., Ph.D., has been appointed chair of the School of Medicine (SOM) Department of Surgery at New York Medical College (NYMC) and director of the Department of Surgery at Westchester Medical Center (WMC), effective February 1, 2023. He served as interim surgery chair and director since November 2021. Dr. Lansman joined the faculty of NYMC as professor of surgery and the clinical staff of WMC as chief of the Section of Cardiothoracic Surgery in 2005.
“I have tremendously enjoyed working with the faculty, fellows, residents and students in the Department of Surgery as interim chair over the year. It is an incredible honor and the highlight of my career to serve as chair for this distinguished group,” said Dr. Lansman.
Dr. Lansman was instrumental in building WMC’s cardiac transplant program and introducing the use of extracorporeal membrane oxygenation (ECMO), among other health care therapy
advances at WMC. He also oversaw the addition of a hybrid operating room at WMC and the related expansion of minimally invasive and catheter-based approaches to aortic valve replacement and mitral valve repairs.

With more than 150 peer-reviewed publications and author of 13 book chapters, Dr. Lansman is a valued mentor to junior faculty, residents and students at NYMC.
Previously, Dr. Lansman was on the medical staff of Mount Sinai Medical Center in New York City, where he started the hospital’s heart transplant program and performed the first cardiac transplant at Mount Sinai in 1986. He also directed Mount Sinai’s Mechanical Assist and Heart and Lung Transplant Program. Before joining Mount Sinai Medical Center, Dr. Lansman served as interim chief of cardiothoracic surgery for SUNY Brooklyn, the Brooklyn VA Hospital and Kings County Hospital.
Since 1988, he has organized and directed the Aortic Symposium Series, an internationally recognized forum for aortic surgery that draws more than 1,000 participants. From 2001 to 2002, Dr. Lansman served as president of the New York Society of Thoracic Surgery.
Dr. Lansman received his M.D. and Ph.D. in biophysics from the State University of New York (SUNY) Downstate Health Science Center. He also completed a general surgery residency at Montefiore Medical Center and a fellowship in cardiothoracic surgery at SUNY Downstate. ■
“
It is an incredible honor and the highlight of my career to serve as chair for this distinguished group. Dr. Lansman
The School of Health Sciences and Practice (SHSP) announced the creation of the Department of Rehabilitation Sciences, which comprises the Division of Physical Therapy (PT) and Division of Speech-Language Pathology (SLP). The new department will be led by Sambit Mohapatra, Ph.D., P.T., chair and professor (nominated) of the Department of Rehabilitation Sciences, who will begin on July 1, 2023. He joins New York Medical College (NYMC) from the Department of Rehabilitation and Movement Science in the University of Vermont’s College of Nursing and Health Sciences, where he is a tenured associate professor and program director of the Doctor of Physical Therapy program.
“The new Department of Rehabilitation Sciences will expand students’ interdisciplinary opportunities to learn evidence-based modalities to help injured, ill and recovering patients develop or regain mobility, motor and language

functions to achieve optimal health,” said Robert W. Amler, M.D., M.B.A., dean of the SHSP and vice president for government affairs.
Janet Dolot, P.T., D.P.T., Dr.P.H. ’14, has been named chief and associate professor in the Division of Physical Therapy in the Department of Rehabilitation Sciences. Vikas Grover, Ph.D., CCC-SLP, has been named chief and associate professor in the Division of SpeechLanguage Pathology in the Department of Rehabilitation Sciences.
Dr. Mohapatra earned his Ph.D. in rehabilitation sciences and neurosciences from the University of Illinois, Chicago. He held a faculty position at the University of Montana in the Department of PT and also served as a postdoctoral fellow at Georgetown University’s MedStar Health Research Institute in Washington, D.C. Dr. Mohapatra has a strong research and publication/presentation record
and a solid background in clinical settings as a licensed physical therapist. His research focuses upon individuals with neurocognitive brain disorders that impact balance. Recently, this research has included individuals with long COVID-19 who are experiencing balance-related issues. He is active in the American Physical Therapy Association among other organizations and has served as a grant reviewer for the National Institute on Disability, Independent Living, and Rehabilitation Research for a number of years.
“Realignment of our existing programs in physical therapy and speech-language pathology in a unified Department of Rehabilitation Sciences affords our faculty greater flexibility in sharing expertise across disciplines to pursue their professional goals in research, teaching and service,” Dr. Amler said. ■
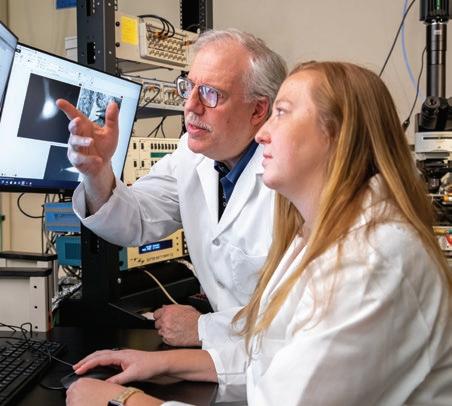
Each year, influenza takes on a different shape. In response, so does the vaccine that protects the world’s population against this highly contagious respiratory virus. It takes methodical testing, meticulous genetics and many cartons of chicken eggs to nurture traces of isolated human samples into the strains that form the basis for the world’s annual flu vaccine supply. And it happens each year in a laboratory at New York Medical College (NYMC).
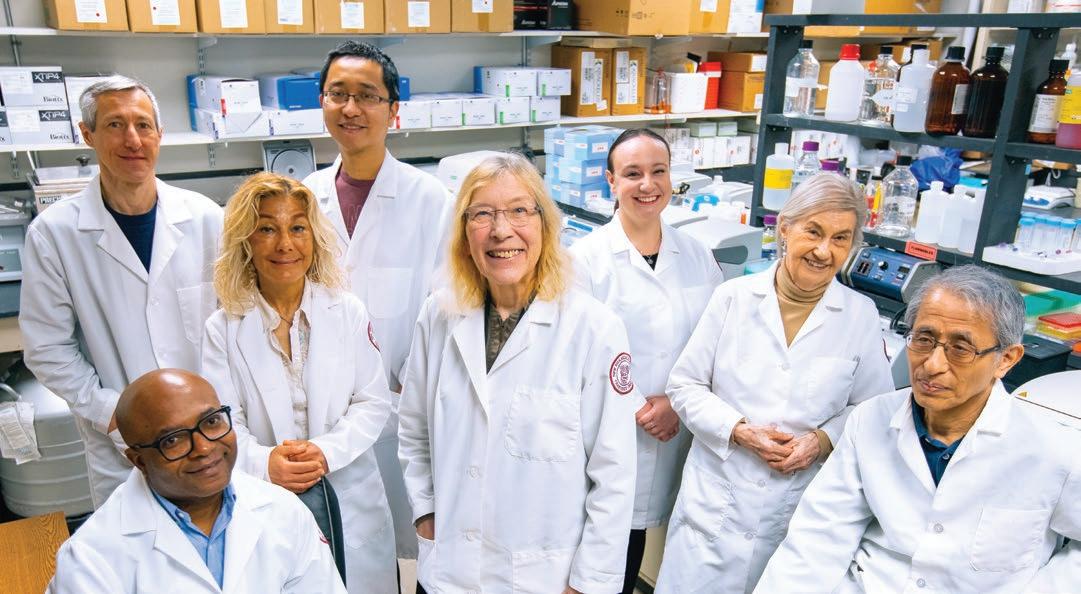
At the helm is Doris J. Bucher, Ph.D., associate professor of pathology, microbiology and immunology. She has spent her career coaxing flu strains into candidates for global production, even as the virus stubbornly mutates. The recent memory of lockdown and other drastic measures to control a deadly outbreak of infectious disease only underscores her critical role in staying ahead of each year’s virus, saving possibly millions of lives each year.

For twenty years, government agencies and global vaccine taskforces have supported Dr. Bucher, whose team takes traces of each year’s infection and engineers them into robust vaccines.
Dr. Bucher has a well-deserved reputation for her “green thumb” in the lab, turning flu virus into seed stock—a form that grows rapidly in embryonated chicken eggs, so that drug manufacturers can make hundreds of millions of vaccine doses.
Dr. Bucher and her team of immunologists, virologists and other researchers have two decades of experience at NYMC cultivating strains. For 20 years, they have received approximately $1 million each year in grants from various government and global agencies—most significantly, the International Federation of Pharmaceutical Manufacturers and Associations’ Vaccine Taskforce, which has supplied continuous funding since 2004. Federal agencies, including the Biomedical Advanced Research and Development Authority and the National Institutes of Health, have also provided grants and contracts. The Centers for Disease Control and Prevention (CDC) remains an active partner, tapping into the resources of NYMC to keep the flu at bay.
Each year’s vaccine must capture the three or four strains predicted to, most likely, emerge during the subsequent flu season. The lab’s time-tested ingredient for stimulating growth, says Dr. Bucher, is a “very old virus that has been growing since 1934,” called PR/8. Like a sourdough starter for bakers, this virus that was isolated 88 years ago—when the flu epidemic of 1918 was a fairly recent memory—reliably activates each new flu vaccine in the reassortment process. “In the first cycle, we inject a diluted version of the PR/8 virus and this year’s virus into the same egg. Then we allow them to multiply, replicate and swap genes.” The virus reproduces itself in the cells that line the pointed end of the egg, where the protein-rich egg white is concentrated. The team repeats the process through several twoday cycles to sort and purify the hybrid strains that best thrive into one uniform seed stock. Candidates must have the right mix of surface antigens, triggering the proper defense from the immune system. Just as critically, they must have strong growth

properties to support mass production of doses. Once these strains have been purified, they are treated with formaldehyde. Now inactivated, but still effective, they can be manufactured into the annual vaccine. “My team is skilled at pulling out the strains that are successful,” says Dr. Bucher. “This is what we do, each and every year.”

Dr. Bucher grew up in Pennsylvania, on a dairy farm that had belonged to her family since the 1800s. Her parents encouraged her to attend college. “As a good farm girl,” she jokes, her field of study at Penn State was nutrition. Her mentor, Ruth Pike, Ph.D., suggested she continue her education at the University of California, Berkeley. “Biochem was hot at the time,” she recalls. After receiving her Ph.D. from U.C. Berkeley and completing a post-doc at UCLA, she began to hone in on influenza. In 1969, she was recruited to join the lab of Edwin D. Kilbourne, M.D., the late professor emeritus of microbiology and immunology, at Mount Sinai School of Medicine. Just before plunging into flu research, she fell terribly ill—with influenza. “It was the sickest I have ever been in my life; and it pushed me over the edge,” she recalls. Having recovered, she vowed to commit her career to fighting this important virus.
The partnership between Dr. Kilbourne and Dr. Bucher was an achievement for public health. It was Dr. Kilbourne, often called the “father of the flu,” who developed the first
genetically engineered vaccine, that devised the high-yield reassortants for Type A strains, which provide two of the flu’s four subtypes. To advance his efforts, Dr. Kilbourne was able to tap into Dr. Bucher’s expertise in developing vaccines with purified proteins.

In 1987, Dr. Bucher joined NYMC’s Department of Microbiology and Immunology. Five years later, she convinced Dr. Kilbourne to join her at NYMC—along with his lab supervisor, Barbara Pokorny. Before Dr. Kilbourne retired in 2002, Dr. Bucher led efforts to extend the high-yield reassortant system to Type B strains of the virus, which would strengthen the efficacy of vaccines. The names of all seed strains produced under Dr. Bucher’s supervision begin with NYMC, honoring their lab of origin.
The following year’s vaccine had an even stronger connection to NYMC. Strains of the infection are named for the places they are first isolated—Hong Kong, California, etc. So, when the CDC sent Dr. Bucher a new strain called NY/55, she wondered where it had originated. The answer: just across the parking lot. That sample had been isolated by Syed H. Abid, Ph.D., former adjunct assistant professor of microbiology and immunology. Given the 30,000 influenza isolates made in the U.S., the odds for such proximity were long. “To think: We could have walked across the parking lot to exchange materials, but we had to go through the CDC.”
My team is skilled at pulling out the strains that are successful. This is what we do, each and every year. Dr. Bucher ”
“
In 2009, amid growing concerns over a new variety of swine flu, the CDC sent a sample of H1N1, a novel Type A strain, to Dr. Bucher’s lab. A New York Times article that May, highlighting her contributions, described the parcel that arrived at her desk: “a vial containing millions of swine flu viruses in a milliliter of fluid…packed with dry ice in a plastic foam box inside a cardboard carton.” Her team worked feverishly to grow the seed stock in 23 days, allowing for the preparation of some 500 million doses of vaccine. Due to their rapid response, a crisis was averted. But as the chaos subsided, and her fatigued lab recovered, Dr. Bucher’s heightened anticipation of a pandemic caused by a new infection would prove correct.

The seasonal incidence of flu varies based on the severity of the flu season. On the CDC website, there are three seasons since 2010 ranked as “high” or “moderate/high” severity: 2014-2015, 2017-2018 and 2019-2020. The data entry for 2020-2021 was blank, with a footnote: the season could not be assessed, due to the “uncharacteristically low level” of influenza that season. But the next year, in 2022, rates climbed back up and health officials caution that severity might spike again.

“During COVID-19, we did not want to abandon the flu. It quieted down for two or three years, but we knew it would come back.” While the COVID-19 vaccines relied on the use of messenger RNA, Dr. Bucher stands by the time-tested method of growing the vaccine in eggs. She recently told Healthline that
mRNA vaccines need to be stored at ultracold temperatures, making logistics for distribution more complicated.
“There is still a need for a flu vaccine,” she stresses. “We still focus on high-yield reassortant strains. They are proven to work. As long as they are still useful, we will keep making them.”
Fighting infectious disease by empowering each patient places Dr. Bucher at the crossroads of clinical medicine and public health. “I am lucky to have the best of both worlds: fundamental research with clinical importance,” she says.

Her position at NYMC gives her access to both worlds. “We have a skilled cadre of grad students and post-docs, with the collaboration that thrives between lab research and clinical medicine,” says Dr. Bucher.
When she is not growing vaccines, Dr. Bucher recharges with walks in Central Park and attends programs at Manhattan’s 92nd Street Y. One of her four daughters has written for the medical drama The Good Doctor, which features a surgeon who has autism and can register the tiniest of details and changes. “She gets some of her ideas from my experience,” Dr. Bucher says.
Recently, Dr. Bucher, a grandmother of three, visited a drug store off-campus for the version of the flu vaccine suggested for those over 65. She mentioned to the person administering the injection that she was among those who helped produce the shot. “But,” she sighs, “I am not sure they believed me.” ■
From modular layouts to shared resources, the new laboratories in the Basic Sciences Building offer both focused workspace and collaborative energy to enhance biomedical research at New York Medical College.
 BY MELISSA F. PHETERSON
BY MELISSA F. PHETERSON
Designing the perfect research lab holds tremendous appeal in academia. With a wish list of upgrades that include tables designed to withstand vibrations, a shared enclave of protective fume hoods, research friendly floorplans, enhanced lighting and modular furniture to design custom layouts, specifically tailored to each lab’s investigations. The ideal layout would also boast an open floorplan that dispenses with cloistered silos to help facilitate collaboration among researchers.
With this ideal research environment in mind, the laboratory renovation project to the Basic Sciences Building (BSB) at New York Medical College (NYMC) was propelled by a matching grant from New York State’s higher education capital (HECap funding). The renovations have transformed the space to become not only innovative, but collaborative by design to enrich and diversify biomedical research. Enhancements include the construction of 17,000 square feet of multidisciplinary research space,
accommodating up to 12 research teams; 3,000 square feet of shared core instrumentation space; and installation of flexible casework systems and bestin-class equipment, such as biosafety cabinets, autoclaves and fume hoods.
“When applicants evaluate whether to take a position here, the first thing they ask is to see the lab,” says Salomon Amar, D.D.S., Ph.D., vice president for research and professor of pharmacology and of pathology, microbiology and immunology at NYMC and senior vice president for
research affairs at Touro University, who oversaw the renovation from its start in 2019. “Because the lab is where researchers spend most of their time, they need to ensure its infrastructure is conducive to research. Through the improved laboratory space, we are better positioned to attract promising scientists, professors, post-docs and students to pursue their own research and support our existing investigations. This beautiful space will bear fruit, in terms of what we can produce within.”

“The new construction and renovations of the BSB adhere to the newest best practices in lab design, including modular benches and open layout,” says Marina K. Holz, Ph.D., M.P.H. ’23, dean of the Graduate School of Biomedical Sciences, professor of cell biology and anatomy, and interim chair of the Department of Biochemistry and Molecular Biology. “Our new BSB facilities are a testament to the commitment of our administration to enhance and strengthen our research capacity.”
In the new, highly flexible paradigm, shared access cores with open bench zones provide space for performing
biomedical research. Results and data are then analyzed in dry computation space located within a designated office zone, in order to maximize both space and HVAC efficiencies. The “open lab bay” layout allows for relocation of bench and workstation positions, encouraging research teams to evolve, grow and even welcome visiting collaborators.
“The open concept inherently encourages higher levels of cooperation among researchers as they move through the workplace,” says Ron Matten, M.P.A., associate vice president of facilities management and capital planning, on updating the 50-year-old facility. “Our design also adheres to best practices in sustainability, cutting redundant spaces to optimize energy efficiency.”
The laboratory renovations reflect the mission and core values of the College and advance several key priorities in the College’s strategic plan for 20212026 including promoting biomedical research and innovation to improve public health, educating biomedical professionals to prepare them for careers as medical professionals, researchers,
innovators and leaders, and providing a campus environment that inspires innovative teaching, effective learning and exceptional research.
“With these renovations that bring our labs to the forefront of innovation, we support and advance key aspects of the College’s new strategic plan to establish our position as a leading health sciences institution,” says Dr. Amar.
“The innovations are also designed to attract pharmaceutical and biomedical researchers across the region, who can pursue their research in our updated space,” he adds. “This new hybrid paradigm, merging academic and commercial spheres under the same roof, aligns with our strategic initiatives to build sustainable and competitive research, curate areas of research excellence and partnerships and enhance our focus on community outreach.”
Reaching beyond its footprint, the renovated BSB aims to nurture a culture of collaboration throughout campus, from the newest students to the most seasoned investigators.
“The renovation was designed to foster ties among departments, attract new talent and help our clinical faculty engage in translational science—bringing lab findings to patient bedsides at our hospital affiliates,” says Padraic B. Reynolds, M.P.H. ’14, associate dean for academic administration at the School of Medicine. “These collaborations will build on our strengths of seeking treatment strategies for COVID-19, cancer and other infectious diseases, cardiovascular and metabolic disease, as well as other public health challenges. Our biomedical science students will be able to participate
in research with a greater sense of teamwork, which is critical to success in their careers.”
Laboratory renovations were conducted in consultation with department chairs and deans, as well as many stakeholders at the College. Early this year, individual faculty and chairs met with renovation teams to go over final details of the new space. Among the first to move in was Christopher S. Leonard, Ph.D., interim chair of the Department of Physiology and professor of physiology. His verdict: “It is the best lab I have ever had. It has opened new vistas
of research that we have never been able to pursue.”
Dr. Leonard saw immediate potential in the modular, adjustable configurations for lab equipment and furniture. “There are places we need traditional wet lab benches for solutions,” he explains, “but much of our work involves specialized high-sensitivity electronic measurement of nerve cells, which requires different tables to block vibration.”
More expansive facilities allow Dr. Leonard’s team to conduct essential research, such as observation of cardiac


activity. It also creates an inviting space to consult with experts in neuroscience, cardiology and respiratory physiology— just some of the fields linked with physiology. And he values the efficiency of shared resources, close at hand.
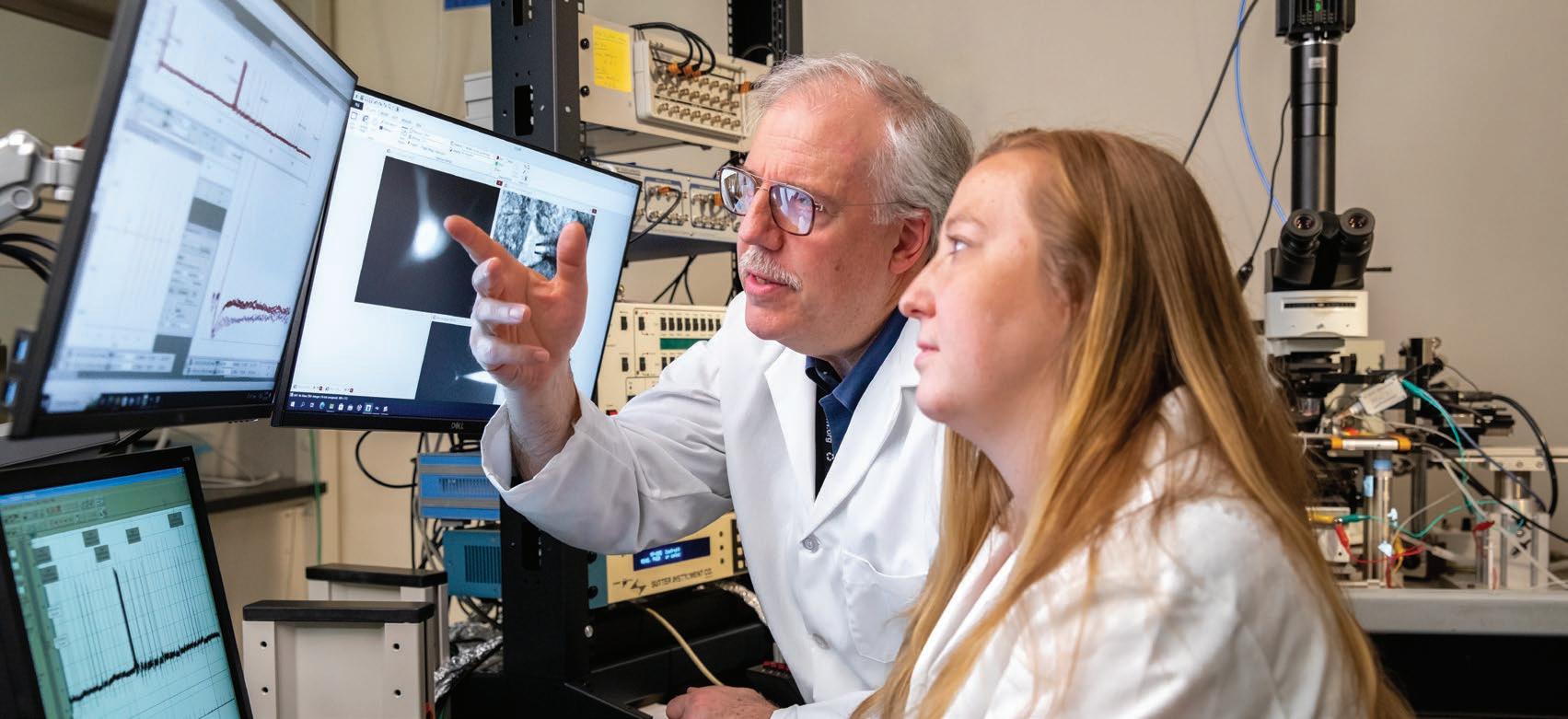
“The space consolidates a number of operations that were distributed across campus,” he says.
“Top on my list was to have a ‘functional lab space,’ and you may wonder what I mean by that,” says Chioma M. Okeoma, Ph.D., professor and vice chair of research in the Department of Pathology, Microbiology and Immunology. She
clarifies: “At a former institution, my lab spaces were on two different floors and three separate places, making it difficult to coordinate experiments. This lab allows my team and other members of the research community—faculty, staff, students postdocs, residents—to access resources and help us function optimally.”
Despite the challenging timeline of the project, its most looming obstacle—the COVID-19 pandemic—may have given way to its greatest strength. “We are appreciative of the team for the work to keep the project’s momentum alive,” says Dr. Leonard. “As we emerge from
the pandemic, the prospect of renovated laboratory space motivates people to return, safely, to a shared space. It is good for espirit de corps; and it restores the creative collaboration that is essential to research.” ■

 BY ANDREA KOTT, M.P.H.,
KIARA THOMAS, M.A.
BY ANDREA KOTT, M.P.H.,
KIARA THOMAS, M.A.
A2022 survey by the American Psychological Association in Stress in America, cited a “barrage” of external, long-term stressors—inflation, violence and crime, political divisiveness and racial discord—for their impact on adults’ physical and emotional health, including headaches, fatigue, anxiety and depression. Such stress can temporarily derail anyone, although most people eventually push through. For those who do not or those who need help finding ways to quell their tensions and anxieties, New York Medical College (NYMC) is addressing the perils of stress through research and clinical perspectives, on campus and across the globe.

Esther L. Sabban, Ph.D., professor of biochemistry and molecular biology and the newly appointed Sidney E. Frank Distinguished Professor of Psychiatry and Behavioral Sciences, has spent the better part of her 40-year career studying the molecular underpinnings of susceptibility and resilience to stress, particularly post traumatic stress disorder (PTSD). Now, with the support of the Sidney E. Frank Distinguished Professorship of Psychiatry and Behavioral Sciences’ $5 million endowment, she hopes to translate her findings from animal studies into tools that can help people.
Ideally, such tools would allow clinicians to identify individuals who are resilient or susceptible to PTSD and inform the development of pharmaceutical interventions to prevent or treat its resulting cascade of harmful health effects. “Our research aims to not only increase resilience and alleviate symptoms of traumatic stress but also lead to clinical interventions that can reduce the long-term consequences of severe stress,” Dr. Sabban says.
PTSD is a debilitating psychiatric illness that can result from exposure to acute trauma, like an automobile accident, natural disaster, war or other lifethreatening events. It may also result from chronic, untreated stress. Among its many symptoms are flashbacks, increased reactivity to loud sounds, avoidance of things that could repeat trauma, depression and anxiety. It can lead to numerous physical and psychological ailments, including hypertension, cardiovascular disease, sleep trouble, sexual dysfunction and substance abuse—and it is prevalent. The statistics on PTSD are staggering. According to the U.S. Department of Veterans Affairs/ National Center for PTSD:
• Approximately eight out of every 100 people will have PTSD at some point in their life, with prevalence in military personnel who served in Iraq and Afghanistan around 20 percent.
• In any given year, approximately 12 million adults experience PTSD.
• Women are twice as likely as men to develop PTSD.
Some stress is valuable, Dr. Sabban acknowledges. “It can concentrate your mind and keep you from doing things that are particularly foolish,” she says. “Stress can also engrave negative experiences or situations into the memory, which helps us to avoid repeating them.”

It is traumatic or untreated chronic stress that can morph into PTSD. Dr. Sabban notes that PTSD sufferers are twice as likely as demographically matched controls to attempt suicide. “PTSD is the most severe outcome of trauma. It is also the most intriguing because it can last for years, as it has in Vietnam War veterans. People with PTSD are crying out for help. It can severely impair all aspects of their life,” she says.
After earning bachelor’s and master’s degrees in biochemistry with honors from Hebrew University in Jerusalem, Israel, Dr. Sabban received her Ph.D. in biochemistry from New York University. There, as a research assistant professor in the Departments of Cell Biology and Psychiatry, she began studying the enzymes that synthesize catecholamines, the neurohormones that trigger the body's “fight-or-flight” stress response. “I became interested in the body’s stress response when I was studying the neurotransmitters epinephrine, norepinephrine and dopamine—the main types of catecholamines—which the body releases in response to emotional or physical stress,” she says. In 1983, she joined the NYMC faculty as an assistant professor, the first woman in the Department of Biochemistry and Molecular Biology, where she has been a full professor since 1991. She has published nearly 200 peer-reviewed publications and her laboratory has received funding from the National Institutes of Health, Department of Defense, American Heart Association and the Office of Naval Research.

Dr. Sabban’s work features the use of the single, prolonged stress, animal PTSD model, which has detected higher levels of norepinephrine in PTSD-susceptible rats than in controls and resilient rats. She has used this model to prove that the intranasal delivery of neuropeptide Y or melanocortin 4 receptor antagonists to the brain prevents the development of many PTSD-associated impairments. If successful in humans, it would reduce much anguish, suffering and loss of life and provide massive financial savings for society.
Most recently, she began looking into the impact of the intestinal microbiome and has shown an association between pre-existing inflammation and higher susceptibility to PTSD. After exposing rats to a single episode of traumatic stress, Dr. Sabban found that only 50 percent developed signs of PTSD, including depression, anxiety and impaired social interaction. “We looked to see what distinguished them from rats who did not develop PTSD and what predicted stress, and we found a difference in their microbiome,” she says. “Those who were more susceptible to stress had more pro-inflammatory bacteria in their gut.”
PTSD-susceptible rats (or in the case of Dr. Sabban’s research, SPS-susceptible, for single prolonged stress, which is the animal model for PTSD) also exhibited lower levels of cecal acetate, a gut microbiota-derived short chain fatty acid, according to Arax
Tanelian, a doctoral student in Dr. Sabban’s lab. “Cecal acetate levels in the rats correlated inversely and significantly with anxiety,” Tanelian says, “Rats with a higher level of cecal acetate were less susceptible to stress-induced anxiety.”
Dr. Sabban and her team also found that anxiety-prone female rats had lower levels of the bacteria lachnospiracea in their gut than anxiety resilient female rats, while in males, lachnospiracea correlated positively with anxiety. “If you can modify the microbiome or products of the microbiome, then you have a noninvasive way of altering neuropsychiatric symptoms,” she says.
Many colleagues, like Stephen J. Ferrando, M.D., the Edith Har-Esh, M.D., Professor and Chair of the Department of Psychiatry and Behavioral Sciences and director of psychiatry at WMCHealth/Westchester Medical Center, express gratitude and admiration for Dr. Sabban’s work. “Her work has clearly informed the biological mechanism behind the development of traumatic stress,” Dr. Ferrando says. “Her development of the animal model and behavioral paradigm are important to test new treatments. Her work has informed our basic understanding and led to the potential to bring treatment trials,” he says.
Dr. Ferrando, who is researching the acute and long-term psychiatric effects of Long COVID-19, is currently partnering with Dr. Sabban in developing inflammatory biomarkers to predict which patients will develop depression, anxiety, brain fog or other cognitive symptoms of PTSD. “We have teamed up with Dr. Sabban for help in designing the biomarker analysis component,” Dr. Ferrando says, noting that 25 to 27 percent of patients with Long COVID-19 meet the criteria for PTSD. The pair also plan to corroborate a treatment study of PTSD using intranasal neuropeptide Y. “We’re looking to eventually develop this into a treatment for humans with PTSD, which would make it a true translational study, translating bench research findings from animal studies into actual human treatment,” he says.
Dr. Sabban’s broadening body of research could have profound implications for students who commonly suffer stress overload, says Robin Hershkowitz, LCSW-R, director of the Office of Student Mental Health and Wellness and assistant professor of psychiatry at NYMC. “Stress is not a personal weakness, but in these environments, people often feel like it is,” Hershkowitz says.
By categorizing different types of stress, exploring its longterm negative impact and ways of screening for, preventing and treating it, it is important to raise critical awareness about the importance of recognizing warning signs. “We have so much more awareness and understanding of what PTSD looks like, which allows us to identify the condition earlier, reduce the stigma surrounding it and eliminate barriers to treatment,” Hershkowitz says. “If we can understand why one person reacts one way and others in different ways, it gives us more information on how to help them.”
NYMC puts this awareness into practice with platforms for students to initiate anonymous dialogues with mental health providers after they have completed a mental health screening. “One cannot dialogue with us without completing the screening but can complete the screening and choose not to respond to our outreach for dialogue,” Hershkowitz says. Additionally, students can access this survey, which begins with an anonymous interaction and assesses their mental health needs. “Ninety-five percent of students who complete the survey end up coming in for an appointment,” Hershkowitz says.
In addition to a team of licensed clinical social workers in the Office of Student Mental Health and Wellness who provide free and confidential support, including psychological counseling, coaching, advocacy, psychiatric evaluation, consultation, psycho-educational events, workshops, support groups and wellness programs, all students in the NYMC School of Medicine (SOM), School of Health Sciences and Practice (SHSP), and Graduate School of Biomedical Sciences and Touro College of Dental Medicine students have 24/7 access to Teledoc. Students can book appointments with board-certified psychiatrists, licensed psychologists and therapists who provide evaluations, medication and management via telephone, video or mobile app.

A recent SOM intersession on career planning and wellness was a three-day mini course in January 2023, that featured a series of small group sessions to provide students with important foundational knowledge and skills to help them contemplate their future while improving their awareness of wellness to help through medical school.
A respite from studies, the wide range of wellness-based activities offered covered the seven dimensions of wellness— physical, emotional, academic, social, spiritual, environmental and financial. Seeking to assuage some of the stressors of medical school, sessions were offered by the Office of Academic Support Services on study techniques; the Office of Student Mental Health and Wellness on managing anxiety and responding to situations more effectively; and the Office of Financial Aid on budgeting student finances.
“
”
Our research aims to not only increase resilience and alleviate symptoms of traumatic stress but also lead to clinical interventions that can reduce the long-term consequences of severe stress. Dr. Sabban
Stress and trauma know no boundaries so Patricia L. Gerbarg, M.D., clinical assistant professor of psychiatry and behavioral sciences, teaches thousands of people around the world how to cope during war and other mass disasters.
Dr. Gerbarg and her husband, Richard P. Brown, M.D., associate professor in clinical psychiatry at Columbia University College of Physicians and Surgeons and former faculty member at NYMC, began their mind-body trauma-relief programs more than 20 years ago in the United States after the terrorist attacks on September 11, 2001. They are the co-founders of the Breath-BodyMind Foundation. When they first learned about the COVID-19 pandemic in January 2020, they anticipated that in-person courses would no longer be safe. They began strategizing a way to provide the program in an online format, while also teaching effectively. They rolled out the first online program six months later.
PTSD in adults and children, resulting in anxiety, panic attacks, nightmares, physical and mental exhaustion, headaches and stomach ailments. The breath-centered mind-body-relief program uses simple and easy to teach techniques to provide rapid relief during times of distress for children and adults. Graduates of the courses have used practices, such as slow breathing, gentle movements and imagery exercises to help children who are taught in schools and in bomb shelters.
“Triggers for stress and trauma are happening everywhere all the time,” says Dr. Gerbarg. “Adults are very concerned about the effects this war will have on the children in Ukraine, who must live with these traumas, the loss of family members, being displaced, being in refugee camps and more.”
Dr. Gerbarg offers seminars on integrating their mindbody practices into psychotherapy, while Dr. Brown teaches advanced techniques for people who may need specialized instruction, for example, military personnel or those with serious physical injuries.

Two weeks after Russia launched the full-scale invasion of Ukraine on February 24, 2022, Dr. Gerbarg and Dr. Brown offered their first online mind-body trauma relief program with translation for people in the war-stricken country. Psychologists, veterans, schoolteachers, emergency services professionals and refugees registered for their free courses to help themselves and the Ukrainian community survive the stress and trauma that come from war and losing loved ones. The courses have drawn anywhere from a few dozen to 700 students each and thousands have learned from their trauma relief teachings. More than 250 Ukrainians, mostly mental health professionals, went on to become certified Breath-Body-Mind trauma relief teachers.
The stressful conditions Ukrainians are under, whether they are on the front lines or refugees, can cause a high incidence of
During the teacher training sessions, attendees are taught how to teach the practices in-person or online and how to adapt the practices for people who may have physical conditions, respiratory problems or emotional disorders. They are also taught how to adapt the teaching methods for different cultures and steps to take if someone should have a negative reaction.
Trauma techniques were tailored for Ukrainians and practices had to be softened and slowed down because many people were physically sensitive due to the bombings, and they could be triggered by loud sounds or vibrations. Also, imagery exercises for children were changed, for example, from a clear blue sky, which could be associated with bombs falling, to a quiet secret garden of their own.
Feedback has been positive. Dr. Gerbarg remarks, “Some of the people I have trained said this is the first time in months that they stopped shaking or this is the first time they’ve been able to hear a siren go off and not have a panic attack.”
Triggers for stress and trauma are happening everywhere all the time.
Dr. Gerbarg
Ukrainian psychologists and psychiatrists told Dr. Gerbarg that while they were busy taking care of as many people as they could, they were also spending nights and weekends studying trauma courses. Many of them were struggling with their own depression and exhaustion, while trying to take care of their patients. Professionals found the Breath-Body-Mind Foundation courses helpful in several ways. They reported that the breath practices calmed them, restored their ability to sleep, relieved their depression, increased energy, rid their headaches and made it possible for them to feel normal again.
“They told us that our teachings were different because we treated them with respect and acknowledged that they know a lot too,” Dr. Gerbarg says. “Also, we taught them how to take care of themselves. You have to be in the right psychophysiological state in order to be able to convey these practices effectively and help other people.”
In addition to underscoring the importance of spotting signs of PTSD, Dr. Sabban’s work underscores the need for better treatment. “An estimated one in 13 people will develop PTSD at some point in their lives, so finding treatment or ways to prevent it is important for all of us,” Tanelian says. “Most studies of PTSD are performed on males and the majority of treatments are based on males’ responses,” Tanelian says. Since women have a higher risk than men of developing PTSD, finding sexspecific treatments is essential. “What is true for one sex is not necessarily true for the other,” she adds.

What is true is that stress, which contributes to more than twothirds of illnesses that physicians treat, including cardiovascular disease, hypertension and depression, takes a sizeable toll on public health, says Chia-Ching Chen, Ed.D., M.A., M.S., CHES, professor of public health and director of the health education certificate program in the SHSP. “PTSD can be considered a social determinant of health which, according to some studies, connects the experience of traumatic events with physical health outcomes,” Dr. Chen says. “Identifying clinical and research opportunities to impact the pathways between social determinants and health is critical in public health,” she says.
Eliminating sources of stress would be ideal, yet virtually impossible. So, until that time, NYMC remains committed to providing tools to keep stress at bay and make PTSD a predictable and treatable disease in the future. ■
At 60 years, the Graduate School of Biomedical Sciences at New York Medical College embraces its growth “beyond basic” to inaugurate its next chapter with a new name.
With its academic rigor, lifesaving potential and fundamental role in population health, there’s nothing “basic” about how the discipline of medical sciences has evolved. So as the graduate school of New York Medical College (NYMC) celebrates its “diamond anniversary” 60th year, the bright new facets of its identity shine within a new name. At the start of this 2022-2023 academic year, the Graduate School of Basic Medical Sciences became the Graduate School of Biomedical Sciences (GSBMS), in a name change approved by the College’s Board of Trustees. The new title provides a more accurate representation of a student body engaged in the academic and research activities that drive today’s biomedical research and funding, guided by values of excellence, intellectual curiosity and diversity and inclusion.
“The name change from ‘Basic’ to ‘Biomedical’ captures the graduate school’s vision of interdisciplinary science, collaboration and academic research at the crossroads of science and medicine,” says Marina K. Holz, Ph.D., M.P.H. ’23, who took the helm as the dean of GSBMS in 2018, and is also professor of cell biology and anatomy, interim chair of the Department of Biochemistry and Molecular Biology,

director of the Integrated Ph.D. Program and director of the Women’s Institute for Science Entrepreneurship (WISE). “The new title also more accurately expresses our identities. Our students, faculty and researchers are indeed biomedical scientists whose work spans the disciplines related to human health and disease. As a relatively young school, we have already accomplished a great deal. We maintain a unique identity in Westchester County by providing quality graduate biomedical education in a tightknit community that creates a supportive environment. We excel in that mission.”
The name change also highlights the synergies between GSBMS and the School of Medicine (SOM). “The term ‘biomedical’ reflects integration of basic medical sciences, which investigate foundations of health and disease, with applied sciences that study practical applications to diagnose conditions, treat disorders and promote health,” says Tetyana Cheairs, M.D., M.S.P.H., assistant dean for Ph.D. programs and assistant professor of pathology, microbiology and immunology. “This translational research is a key asset of NYMC and the name change helps us reflect that as we move forward. In addition to our ties with the SOM, our proximity to Bioinc@NYMC, our biotechnology incubator, and companies
The name change from ‘Basic’ to ‘Biomedical’ captures the graduate school’s vision of interdisciplinary science, collaboration and academic research at the crossroads of science and medicine.
Dr. Holz
like Regeneron Pharmaceuticals present further opportunities for collaboration. Our curriculum is designed to foster the interdisciplinary, groundbreaking research captured in the term biomedical.”
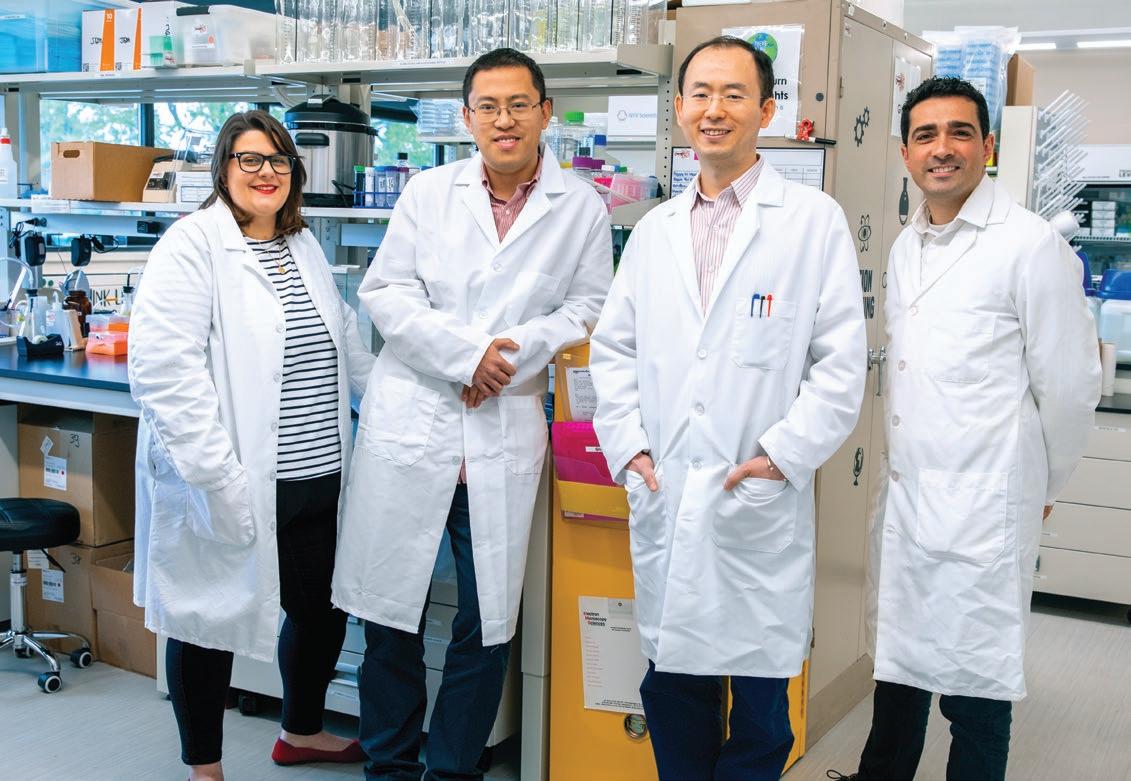
Recent faculty hires also broaden opportunities for biomedical research. “Our boost in hiring has brought faculty with fresh ideas, insight and resources,” says Dr. Cheairs. “Their initiatives are valuable assets not just to the graduate school, but to the entire College.”
In keeping with its focus on diversity and inclusivity, GSBMS has removed long-entrenched barriers, financial and otherwise, that might discourage applicants to graduate school. When Dr. Holz joined as dean, she led the initiative to waive the requirement of Graduate Record Examinations (GRE) for admission to the Ph.D. and two-year M.S. programs.
“The majority of students we serve are local and come from surrounding communities. Many are ‘first-generation’ scholars and often come from nontraditional professional backgrounds,” says Dr. Holz. “This diversity is an asset to our school. In fact, we noticed that removing the GRE requirement increased the number of and enhanced the quality of applicants.”
Dr. Cheairs agrees, calling the decision beneficial. “The GRE is attached to a bias toward someone who has the time and resources to prepare for, and if needed, retake, this test,” she explains. “Our approach to reviewing applicants is more holistic. We conduct interviews with applicants to the Ph.D. program so they can discuss their academic accomplishments and research experience, share their passions and convey how well-versed they are. We look at the big picture of their academic records and professional focus. That holistic approach gives us a much better picture of the applicant’s potential in biomedical science than a score on the test.”
Dr. Cheairs points out NYMC’s proud history of inclusivity and community. “We have carried this legacy into the present very well,” she says. “The diversity of our students and their professional backgrounds are a huge advantage for us. They bring connections and perspectives that strengthen our networks within business, industry and government. This elevates the status of our graduate school, promoting our strengths to a much broader community.”
Supportive guidance for professional development is a keystone of the
The diversity of our students and their professional backgrounds are a huge advantage for us. They bring connections and perspectives that strengthen our networks within business, industry and government. This elevates the status of our graduate school, promoting our strengths to a much broader community.
Dr. Cheairs
GSBMS’ new identity. “Our graduate program is far more than just academic and research fundamentals,” says Dr. Cheairs. “We offer many professional development opportunities to the graduate students throughout our curriculum. The intimate size of our school allows close collaboration among students with faculty, advisors and investigators. In hindsight, students realize we give them more than just assignments to complete. We give them ways to apply their knowledge, enhance their core competencies and hone their research and presentation skills.”
In 2018, GSBMS launched the Master of Science (M.S.) in Clinical Laboratory Sciences (CLS) program. This two-year program allows students to qualify for the national certifying examination for clinical laboratory technologists after their first year and to start working as licensed laboratory technologists in New York State and nationwide, while completing their literature review during their second year. Training for CLS encompasses chemistry, toxicology, hematology, urinalysis, diagnostic immunology and other critical skills for medical, industrial and pharmaceutical laboratories. This year, the CLS Program received full accreditation from the National Accrediting Agency for Clinical Laboratory Science (NAACLS). “This program is unique in providing a defined path for our career-minded students into

a critically important and rewarding profession,” says Dr. Holz.
Two events of the last few years have riveted attention upon this intersection of science and medicine, says Dr. Holz. First, the spread of COVID-19 made clear the importance of laboratory scientists in testing, tracing and developing vaccines against the virus to curb the pandemic. Second was the sobering legal actions and lawsuits against Theranos, in which the misrepresented accuracy of blood analysis technology had severe consequences for both investors’ and patients’ health. One of the whistleblowers who brought the scandal to light was trained in CLS. “Theranos made people realize that our entire health system depends on lab technicians performing their work accurately and ethically,” says Dr. Holz.
GSBMS also provides a springboard for students to enter medical school with firsthand experience through immersion. Under an agreement between the GSBMS and the SOM, students in the Interdisciplinary Biomedical Sciences (iBMS) Accelerated Master's Program (AMP) or applicants who have completed this program, are admitted to SOM if they meet certain academic performance benchmarks. In this one-year, postbaccalaureate pre-medical program,
students enroll in many of the same classes as first-year medical students.
“The AMP program is an incredible opportunity for academic enhancement,” says Dr. Holz. “Students receive a thorough grounding in biomedical sciences, while also sitting alongside medical students, to discover medical school for themselves. At the end of the program, they are very well-equipped to continue on to medical school. This linkage agreement removes yet another barrier for students, affirming our commitment to advancing these students in their journey to medical school. We want to remove some of that uncertainty while supporting their success.”
Naveena Chittineedi, SOM Class of 2024, is among those who completed the AMP to transition into SOM.
“This program is one of the keys to my success as a medical student,” says Chittineedi, who emigrated from South India to Jamaica, Queens, with her mother and two siblings in 2007. “I knew from a young age I wanted to be a doctor. I also knew there would be significant barriers to getting there. In my family, no one has gone to medical school or even graduate school. After college, I realized I needed to enhance my application for medical school. I knew I wanted to stay in New York to lean on my family support system. GSBMS appealed to me because of its intimate class size, faculty-to-student
ratio and closeness to home.” When Chittineedi discovered the program would expose her to lectures, group discussions and labs with first-year medical students, she says, “I was floored.”
“We took the same classes, got to know the same professors and joined the same clubs. That immersion into the student body really gave me a taste of what being a first-year medical student was like, even as I built my application for medical school. The rigor prepared me for success when I matriculated.” Chittineedi credits her advisor, Brian B. Ratliff, Ph.D., associate professor of physiology and of medicine, director of the AMP and codirector of the Medical Physiology Course, with reaching out frequently to evaluate performance, prepare for interviews and offer guidance to medical school admission. “From exams to interviews, he was there for every single milestone. I also want to give credit to Dr. Libor Velisek, [M.D., Ph.D., professor of cell biology and anatomy, pediatrics and of neurology, SOM assistant dean for basic medical sciences and director of the M.D./ Ph.D. program,] and Dr. Jana Veliskova, [M.D., Ph.D., professor of cell biology and anatomy, obstetrics and gynecology and of neurology,] who prepared me for my interviews and checked in with me throughout the process. Because I didn’t have family or friends to guide me, it was essential to have these faculty mentors.”
Keenly aware of social justice and health equity, Chittineedi hopes to practice in medically underresourced communities, such as the one where she grew up. The College’s network of clinical affiliations gave her the opportunity to serve as a patient care associate and certified rape crisis counselor, building skills in advocacy. She now serves as the executive director of the NYMC Center for Human Rights, a student-run clinic providing forensic medical evaluations to asylum seekers and human trafficking victims.
GSBMS also offers a one-year accelerated master’s linkage program for admission into the Touro College of Dental Medicine (TCDM) at NYMC. Its hybrid curriculum is designed to introduce students to a dental school atmosphere, receive a grounding in dental science and enroll in graduate-level biomedical courses that enhance skills in both learning and critical thinking.
Sydney Spal, D.D.S. ’22, completed the linkage program to gain an edge in dental school at Touro. “I took each science class alongside students pursuing their Ph.D. and master’s degrees in the GSBMS,” says Dr. Spal. “Studying that material with the same instructors helped refresh my background knowledge. The peer study sessions were intense because the candidates were very bright. I watched them review the material on the whiteboard in the library.” This served
her well in dental school: “There, it was me standing at the whiteboard, teaching everybody else as I had seen the graduate students do. That experience reinforced my learning.”

Under the guidance of Kenneth M. Lerea, Ph.D., assistant dean for master’s programs, professor of cell biology and anatomy, and course director for histology and cell biology, Dr. Spal completed a literature review of the effects of squamous cell carcinoma in the oral cavity among smokers, translating material covered in her graduate courses into applications for dental patient care. Dr. Spal is now completing her dental residency at St. Francis Hospital Dental Center in Hartford, Connecticut
With the momentum of its new name, the GSBMS is poised for a leadership role in its next chapter. “We want to continue improving by staying attuned to our students’ needs in a changing world,” says Dr. Holz. “Our charge is to provide the education they need for the career opportunities they seek. Recruiting faculty, removing obstacles, establishing programs and creating pathways to success are all centered on benefiting our students. They will always be our priority.” ■
Abdelfattah El Ouaamari, Ph.D.
Associate Professor of Cell Biology and Anatomy and of Pharmacology

Dr. El Ouaamari studies the role of inter-organ communications in glucose metabolism with an emphasis on the identification of molecular and cellular mechanisms promoting regeneration and function of islet insulin-producing β cells. He has made novel discoveries on the roles of autonomic innervation of the pancreas. His research brings strong basic science with high translational potential. He most recently served as assistant professor in the Department of Medicine, Division of Endocrinology, Metabolism and Nutrition at Rutgers Robert Wood Johnson Medical School.
Malik Bisserier, Ph.D.

Assistant Professor of Cell Biology and Anatomy and of Physiology
Dr. Bisserier’s interests include further investigating the transcriptional and epigenetic alterations in pulmonary arterial hypertension with the ultimate goal to develop new therapeutic strategies for prevention and treatment. He is also a member of the American Thoracic Society, American Heart Association, International Society of Heart Research and the Pulmonary Vascular Research Institute, and he currently serves as guest editor of several journals. Dr. Bisserier was awarded several prestigious recognitions, including the Cournand and Comroe Early Career Investigator Award from the American Heart Association. He joins NYMC from the Cardiovascular Research Institute at the Icahn School of Medicine at Mount Sinai in New York City.
Julie DiMartino, Ph.D.
Assistant Professor of Cell Biology and Anatomy
Dr. DiMartino focuses her research on dormancy escape and cancer metastasis using a combination of in-vivo models and imaging technics. She was awarded an Early Career Investigator Award from the METAvivor foundation and the 2022 Rupert Timpl award from the International Society for Matrix Biology. She has published more than 20 academic papers, in respected peer-reviewed journals, including Journal of Cell Biology, Cancer Discovery, Nature, Nature Cancer and Cell. Prior to joining NYMC, she was at the Icahn School of Medicine at Mount Sinai Hospital, New York, where she focused on the role of the extracellular matrix in cancer dormancy.
Shuai Gao, Ph.D.Assistant Professor of Cell Biology and Anatomy and of Biochemistry and Molecular Biology

Dr. Gao’s research interest is interrogating the interplay between transcription factors (e.g., AR, FOXA) and epigenetic modulators (e.g., histone demethylases) in driving drug resistance in prostate cancer. Dr. Gao is a recipient of the Department of Defense Idea Development Award-New Investigator Option and has also received multiple national training awards. He has been studying dysregulated gene transcription in the progression of prostate cancer for 14 years and has 23 peerreviewed publications. He was a research assistant professor at the University of Massachusetts Boston prior to joining NYMC.
Jian Li, Ph.D.
 Assistant Professor of Cell Biology and Anatomy
Assistant Professor of Cell Biology and Anatomy
Dr. Li’s lab combines genetics, genomics and cellular biological approaches to understand protein homeostasis and stress response in reproduction, aging and cancer. His research has received multiple grant awards, including postdoctoral fellowships from National Ataxia Foundation, BrightFocus Foundation for Alzheimer’s Disease Research and Maximizing Investigators' Research Award (MIRA) from the National Institutes of Health. He comes to NYMC from the faculty of the Oklahoma Medical Research Foundation.
If the eyes are windows to the soul, then the cornea is the window to the eyes. Yet when the cornea is cloudy, it is like looking through dirty glass and not being able to see clearly. It occurs rarely, especially in children, which makes Gerald W. Zaidman, M.D., professor of clinical ophthalmology and vice chair of the Department of Ophthalmology, who specializes in pediatric corneal transplant surgery, one of the most sought-after ophthalmological surgeons in the world.
Dr. Zaidman is one of just 40 pediatric corneal transplant surgeons in the United States. “Children are the least common
group of patients who need transplants,” he said, noting that of the 50,000 corneal transplants in the U.S. each year, approximately 500 occur in patients younger than age six. In his four decades of practice, he has performed close to 4,200 corneal transplants, including 500 on children. “I probably do 80 transplants every year on adults and maybe six or eight a year on children,” he says. “Very few people do anywhere close to that number of children.”
The most common reasons for corneal surgery in adults include Fuchs dystrophy, a disease that causes the
cornea to swell; keratoconus, in which the cornea changes shape; genetic conditions like corneal dystrophy; glaucoma; or an infection from a contact lens, scarring or some other trauma.
In children, most corneal transplants aim to correct birth defects. “Corneal transplant surgery in any child born with a cloudy cornea is unique,” Dr. Zaidman says. The surgical specialty exists in so few countries that patients from around the world come to see him. “If a child is born with an abnormal cornea, then they should be examined as soon as possible,” he says.

Dr. Zaidman has a global reputation and is one of 40 pediatric corneal transplant surgeons in the nation.
His global reputation gives no hint that Dr. Zaidman never planned on a career in medicine. “I loved science in college and thought I would do basic science,” says Dr. Zaidman, who earned his bachelor’s degree in 1972 at the City University of New York’s Queens College, and his medical degree three years later from the Albert Einstein College of Medicine. But what really interested the warm, chatty ophthalmologist was people—children especially. “When I told my advisor I was interested in people and science, she said, ‘Have you ever considered medicine?’ It was the best advice anybody ever gave me.”

During medical school, Dr. Zaidman discovered he loved pediatrics. By specializing in ophthalmological surgery, he could care not only for children but also for adults, while treating all types of diseases. And ophthalmology allows for continued patient care. “Patients can be with you for 30 years,” he says.
Recently, Dr. Zaidman performed a second corneal transplant in an eightyear-old Israeli boy who was born with a cloudy, opaque left cornea. “I did his first corneal transplant in 2015 when he was about four or five months of age,” he says. He stayed in close touch with the boy’s family, as he does with all his patients, and learned that the first transplant had failed. After unsuccessful treatment in Israel, the family decided to return to the United States to see Dr. Zaidman. Their seven-week stay included another

transplant surgery and multiple follow-up visits. After the surgery, the young boy exclaimed, “I can see 1,000 times better now!” Dr. Zaidman explains, “Well, he does see things out of that eye that he could not see before the surgery, but 1,000 times is very nice and generous. Now, he is doing very well.”
Following pediatric patients closely is critical because they cannot monitor or effectively communicate problems after surgery. “Corneal transplant surgery in any child is unique and never the same as taking care of a transplant in an adult,” Dr. Zaidman says. “You can ask adults to make sure they can see out of their eye as it heals but you cannot expect a fivemonth-old to do that.”
This explains the lower success rate of pediatric corneal transplant surgeries— 70 to 85 percent—versus 90 percent or more for adults, and why he insists on seeing his pediatric patients twice weekly for four months. “A baby may get used to using one good eye and not realize that they have a second eye that is not healthy,” he says. “I have to educate parents how to monitor the eye that is having problems. I teach them to buy a pocket flashlight and how to look at their child’s eye. If their cornea is clear, then their pupil should be easily visible.”
Pediatric corneal transplant surgery has come a long way since the days when an ophthalmologist sewed shut the eyes of an infant for lack of knowing how to treat cloudy corneas. When, as a


fellow, Dr. Zaidman first transplanted a baby’s corneas, he recognized the need for greater education and information sharing among doctors treating corneal disease. Thus, he founded and directs the Pediatric Keratoplasty Association (PKA), a worldwide organization that encourages doctors to share information and treatment methods on children and infants with corneal diseases. “It is a way of furthering knowledge and educating parents so they know that we can do something to help their children see.”
Founding the PKA has been one of his greatest achievements, along with maintaining ongoing relationships with his patients and their families. “Some kids I operated on are now in their twenties,” he says, referring to a woman whose cornea he transplanted during her infancy. “Now she is going to medical school,” he boasts. His satisfaction is profound, so much so, that he has no plans to retire any time soon. “I am having too much fun.” ■
Corneal transplant surgery in any child is unique and never the same as taking care of a transplant in an adult. You can ask adults to make sure they can see out of their eye as it heals but you cannot expect a fivemonth-old to do that.
Dr. Zaidman
Just eight New York Medical College (NYMC) alumni are in the esteemed circle of holding a triumvirate of degrees, one from each school, the School of Medicine, Graduate School of Biomedical Sciences and the School of Health Sciences and Practice. Chironian met up with three of them: Karen Clarke, M.S. ’93, M.P.H. ’94, M.D. ’96; Rajeer Vibhaker, Ph.D. ’99, M.P.H. ’99, M.D. ’99; and Cara Taubman, M.S. ’05, M.P.H. ’10, M.D. ’10. Though they grew up in different parts of the world and have different specialties and research interests, they all knew they wanted to become physicians in early childhood. What they didn’t know was how NYMC would open a world of possibilities to them and make those childhood dreams reality.
Dr. Clarke is a hospitalist at Emory University Hospital in Atlanta, Georgia, as well as an associate professor of medicine at Emory University School of Medicine. As a hospitalist, she is the lead physician for hospitalized patients with a range of acute and chronic conditions, spanning from young adults to the elderly.
microbiology and immunology, an M.P.H. in environmental health and her M.D. She completed her internal medicine internship and residency at the University of Texas Health Sciences Center at San Antonio, worked in emergency care in several Texas hospitals, served as a house physician in upstate New York, and then as a hospitalist in Texas and Arizona before arriving at Emory in 2008.
“My plan in medical school was to focus more on research,” she says. “Thirty years ago, I was sure that I would be running a research lab as my career progressed— maybe even inventing new medicines. My interest was always in helping sick people get better.” Dr. Clarke has published papers addressing topics such as COVID -19 and catheter-associated urinary tract infections. Some of her publications also focused on quality improvement issues such as the appropriate use of diagnostic tests and medications (specifically proton pump inhibitors) in hospitalized patients.
For Dr. Clarke, there is no contradiction between science and faith. “Every morning,” she says, “I start with a prayer that all my patients will have good outcomes.”
In her earlier years, Dr. Clarke pictured herself in a career oriented more towards research than clinical medicine. Growing up in the Bahamas, she was a selfdescribed science nerd whose favorite school subjects were biology, chemistry and physics. “By the time I was eight or nine, I was thinking that I wanted to be a doctor,” she recalls. “I was encouraged by teachers and incredibly supportive parents. They expected me and my sisters to do well and made many sacrifices for us,” she notes. She went to the best schools available in the Bahamas then to high school in England.
At Nebraska Wesleyan University, she majored in chemistry and then arrived at NYMC where she earned an M.S. in
Although she maintains these and other research interests, Dr. Clarke’s career trajectory shifted and, for more than 20 years, she has devoted herself primarily to hands-on patient care.

Dr. Clarke typically sees 12 to 18 patients daily, some of whom have been sent from other facilities to Emory because of its status as a tertiary care hospital. She takes particular satisfaction in attending to the smallest details and finding accurate diagnoses—something she emphasizes when teaching physician assistant students who round with her.
We should never move forward without a clear vision,” she says. “Every test and every procedure we order, every
medication we administer—there has to be a solid rationale for why something should or should not be done based on the specific needs of that patient.”
For relaxation, Dr. Clarke listens to music. “A little of everything,” she says, “but especially reggae and tunes of the 80s and 90s.” She loves to travel, having been to Central America, the Caribbean, many countries in western Europe and a good portion of the U.S.
Although Dr. Clarke’s professional life took a turn she did not quite expect, she knows she is in the right place. “I give every patient a hundred percent,” she says, “and I work extremely hard to keep learning from all of them. God carries me every day through every decision I make about caring for my patients. I feel blessed.”
my clinical work is taking care of the families who are navigating unfamiliar territory and often have to make difficult decisions.”
He began his academic journey at Macalester College in St. Paul, Minnesota, where he majored in chemistry and biology. Applying to medical schools was a challenge; at that time, he was still on a foreign student visa. But NYMC allowed foreign students to apply and accepted him. Although he had done some research in college, Dr. Vibhakar did not initially see research as his focus. However, during his first year, he was assigned to shadow Joseph M. Wu, Ph.D., professor of biochemistry and molecular biology. “He was an amazing teacher who got me excited about his work understanding how DNA binds to proteins.” Subsequently, he was accepted into the M.D./Ph.D. program specializing in pathology, where he realized that he could also fit in the classes needed for the M.P.H. specializing in epidemiology and pursued that degree as well, doing research in a cancer biology lab.
He completed his residency in pediatrics and a fellowship in pediatric oncology at the University of Iowa. In 2014, he joined the University of Colorado School of Medicine where he is currently professor of pediatrics, program leader for the Pediatric Neuro-Oncology Program and a faculty member in the Department of Neurosurgery, Department of Cell and Developmental Biology and Cancer Biology Program.
Dr. Vibhakar pictured himself as a family doctor from the time he was a young boy in Moshi, Tanzania, making home visits with his family physician father. “I watched him interact with everyone from babies to grandmas,” he says, “and I knew that was what I wanted to do.”
Now, as a physician-scientist specializing in pediatric oncology—specifically childhood brain tumors—Dr. Vibhakar still cares for families but not as he originally envisioned. “Yes, I am a medical doctor,” he says. “I check lab reports and prescribe treatments. But
Dr. Vibhakar spends about two-thirds of his time in the lab and the remainder caring for children with brain tumors and young adults whose tumors were diagnosed earlier in childhood. He explains that pediatric brain tumors are different from those found in adults. “A pediatric tumor occurs because of dysregulation during development,” he says. “Cells replicating in a particular location that should go quiescent do not do so at the right time; they keep multiplying and develop into tumors.”
His lab studies what happens when that development goes awry. “Why the development goes wrong is almost impossible to answer at this point,” he
notes. “But if we can figure out what happens when development goes wrong, we can make progress.” Dr. Vibhakar’s lab researches the basic mechanisms of how DNA is packaged and the pathways and mechanisms that cancer cells depend on that, if better understood, could be targeted for therapy.
As a clinician, Dr. Vibhakar notes that survival rates for some kinds of pediatric brain tumors have increased significantly in the past 20 years. “But there are others on which we have made no progress. So, for some patients, I am able to offer therapies and hope; for others, the conversation has to be about quality of life and end-of-life care,” he says. When he teaches, he emphasizes two skills. “First, I want them to be able to think through the problem,” he says. “My residents sometimes get upset because I will not let them just report lab results. Until you tell me why that number does or does not matter for the patient, I do not want to hear what the number is.”

The second lesson is how to listen to family members. “Sometimes parents will tell the doctors what they think we want to hear or will describe something as normal because they have become accustomed to it. Do not listen only to the words. Watch faces, gestures and tones of voices. And really listen to the children themselves. Often, they will be the ones to tell us what is really going on,” he explains.
About his career, Dr. Vibhakar says, “I love what I do. As a physician-scientist, you get calls from the clinic while you are in the lab, and you will have the lab paperwork awaiting you after your clinic time. But if you really want to make a difference, being a physician-scientist is the way to go. Even with the amount of work, I would not want to do anything else.”
Exposed to medicine at an early age by her mother and godmother, both nurses, Dr. Taubman found her calling when she spent a high school summer volunteering in the Emergency Department at New York’s St. Luke’s Hospital. “That summer solidified for me that I wanted to be a doctor,” she says.
After obtaining a B.S. in microbiology at the University of Rochester, she came to NYMC to study biochemistry. The following year, she worked with autistic children in Brooklyn while applying to medical school and then entered NYMC’s M.D./M.P.H. program.
Her summer at St. Luke’s sparked her interest in emergency medicine. However, once in medical school, Taubman told herself that she was not automatically going to focus on that field. “But, as I went through my rotations,” she says, “the problem turned out to be that I liked a little bit of everything.” So, she returned to her first love—which, she points out, does have “a bit of everything”—and went on to complete a residency in emergency medicine at Jacobi and Montefiore Medical Centers.
Since 2017, Dr. Taubman has been assistant director of the Emergency Department at New York’s Harlem Hospital, caring for fellow New Yorkers and sharing responsibility for the department’s day-to-day operations.

Her path to her current position took her through Ghana, Rwanda and South Sudan as part of Columbia University’s fellowship program in global emergency medicine. For much of the two-year program, Dr. Taubman worked with Doctors Without Borders, known internationally by its French name— Médecins Sans Frontières or MSF. She developed a mass casualty plan for a hospital in Ghana, helped the Rwandan government develop and administer an assessment of acute care capacity in the country’s hospitals, taught emergency medicine and provided direct patient care in refugee and internally displaced persons camps in South Sudan.
When her fellowship was completed, Dr. Taubman knew she wanted to go back into the city hospital system. “I have always been a proud New Yorker,” she says, “and who takes care of New York? The public hospitals.”
Her experience in global emergency medicine turned out to be excellent preparation for her other role at Harlem Hospital—clinical director of emergency management—particularly when the COVID -19 pandemic took hold in New York City. Overseas, she dealt with sudden influxes of patients because of mass casualties or the rapid spread of infectious agents, where there was a tremendous amount of need, and where medical
personnel had to constantly re-direct resources to help the largest number of people who needed extra care.
“That was what we faced in New York in the spring of 2020. It was a difficult and surreal time, but I was able to help my colleagues who had never been in a parallel situation,” says Dr. Taubman. “I am proud of how we handled the spring of 2020. I do not think anyone could have been prepared for what happened. But, if I had to do it again, the people at Harlem Hospital are the ones I would want to work with .”
When she is not working. Dr. Taubman loves to travel, read especially nonfiction, and explore the Big Apple. She will tell you that, despite what we see on television, life in the ER is not filled with glamour and non-stop excitement. But she loves her work and points out that, as an emergency medicine physician, she feels privileged to be able to treat anyone who needs care without regard to insurance status.
“I have the greatest job in the world,” she says. “I get to care for people who may be in their worst moments and tell them they are going to be okay. I do not always get to fix them right then—sometimes my colleagues will do that. But I get to reassure them: We are here and we will help you.” ■
Fawaz Al-Mufti, M.D., was one year out of medical school, without a chosen specialty, when war thrust him into emergency medicine. It was 2003 and senior staff at the Nahrain Teaching Hospital in Baghdad, Iraq, where Dr. Al-Mufti had just finished a transitional residency—including six months of surgical training—were fleeing, leaving him and junior colleagues to treat the surge of civilian casualties.
Two years later, Dr. Al-Mufti was delivering urgent care to people in conflict zones around the world for Doctors Without Borders/Médecins Sans Frontières (MSF). Despite all this experience, he would have to repeat his residency to practice emergency medicine in the United States. Instead, he chose not one but three new specialties, becoming a triple, boardcertified neurologist, neurointensivist and neuroendovascular surgeon. “War makes life feel so unpredictable—too short to waste doing the same thing again,” Dr. Al-Mufti says. “I am who I am today because I did not choose the easier path but rather the road less traveled. Instead of considering adversity a problem, I saw it as an opportunity to overcome something to better myself.”
Surviving war informed Dr. Al-Mufti’s remarkable professional evolution, but his tenacity—which propelled him to become associate professor of neurology, neurosurgery and of radiology, as well as assistant dean for graduate medical education research, in addition to being the director of the neurocritical care unit at Westchester Medical Center (WMC)— began much earlier.
Born in Iraq to an economist mother and engineer/architect father, Dr. AlMufti grew up traveling the world with
his family. From an early age, he spoke English, Arabic, Kurdish, Greek and French, and found acceptance among the Sunnis, Shiites and Kurds in his family. “My multicultural upbringing and the multi-ethnicities in my own family shaped who I was and wanted to become— someone who could accept and help others,” he says.
Although painting was his first love, his concern over Iraq’s civil strife, its suppression of human rights and civilians’ suffering drove him toward medicine. “It always struck me to see people disfigured from war,” he says. “I thought, ‘Had this person received the proper care, maybe they would not be disfigured.’ I wanted to create beauty on paper, but I decided to create art through medicine.”
He recalls his early, by-the-bootstraps training, when trucks dropped off 50 to 100 patients at the hospital daily, and he and fellow medical staff had to triage. “One of us would open a textbook and read out loud what to do to save someone’s life,” he says. Yet, he wanted to do more. For the next five years, he helped MSF deliver urgent health care to underresourced communities in conflict zones around the world. “MSF goes where nobody goes,” he says. “There are no hospitals, no roads, just mud houses. I decided to dedicate my career to helping these people.”
Upon moving to the U.S. in 2009, with his wife and six-month-old daughter, he learned that he would have to repeat his residency to practice emergency medicine, so he decided to change specialties. “I chose neurology because I wanted to learn more about the brain,” he says. “I love the adrenalin rush of acute care. Following
my neurology training, neuro-critical care seemed like the perfect marriage between neurology and emergency medicine.”
In addition to treating cerebral aneurysms, cranial and spinal arteriovenous malformations, acute stroke, as well as intracerebral hemorrhage, Dr. Al-Mufti instructs medical students, residents and fellows. He conducts his own research into subarachnoid hemorrhage and acute ischemic stroke. He also developed WMC’s neurocritical and neuroendovascular protocols, featuring a training curriculum for neurocritical care nursing and neuroendovascular “boot camp” for neurology and neurosurgery residents, fellows, nurses and technologists.

Having survived multiple wars and engaged in two careers, Dr. Al-Mufti now lives with his wife, a pediatric neurologist, and their four children. “I am most thankful for every day I spend with my family and their endless support. They are my muse, my rock and the compass that guides me.”
To all of this, he credits his triumph over adversity. “You have two options,” he says. “You either curl up in a fetal position to protect yourself, or stand up strong, weather the storm and emerge on the other side.” ■
I am who I am today because I did not choose the easier path but rather the road less traveled. Instead of considering adversity a problem, I saw it as an opportunity to overcome something and better myself.
When Stefanie Blanco, M.S. ’10, started the position of assistant professor in New York Medical College’s Speech-Language Pathology (SLP) program in August 2022, she felt like her career path was coming full circle. She had not only earned her master’s degree in SLP at NYMC but found her passion—the specialty of Augmentative and Alternative Communication (AAC)—under the mentorship of Kathleen Franklin, Ph.D., CCC-SLP, associate professor of speechlanguage pathology.

After 12 years of clinical experience, Professor Blanco will share her passion and skills with the next generation of speech-language pathologists at NYMC.
AAC provides a set of tools and strategies that an individual can use to solve communication challenges by augmenting or providing an alternative to natural speech. Those tools can run the gamut from low tech to high tech, for example American Sign Language to simple communication books that can be quickly assembled to help brain injured patients in the hospital to highly customizable computer and tablet communication apps for those with a variety of access needs.
“In my 12 years in practice, not only has there been this amazing trajectory of advancement of technology that can assist individuals but there has been more evidence-based research to show us which treatment methods are actually working,” Professor Blanco says. “That combination is enabling us to provide more effective outcomes for patients.”
A prime example of this is the prioritization of core vocabulary. Out of the thousands of words that people use, approximately 350 to 400 of them are used 80 percent of the time. “Research has shown that if we give patients access
to those core vocabulary sooner and faster, it can provide them with improved communicative control within their environment,” Professor Blanco says. “So, many of the available communication apps are now programmed to include and prioritize core vocabulary.”
In Professor Blanco’s AAC class—one of five she is teaching—students learn how to properly identify which alternative mode of communication would work best for a variety of patients in different scenarios, do hands-on training to develop their own fluency with the various devices and then learn how to teach those methods to not only the patient, but to their family members as well, which is crucial to a successful outcome. “We know from research that if you do not properly train a patient’s circle of caregivers, it can lead to device abandonment,” she says.
Three of Professor Blanco’s other classes work in tandem. Foundations of Speech, Language and Cognition teaches first-year SLP students the typical developmental path of communication. Language Disorders then trains the students to identify where the breakdown in that process may occur. Speech Sound Disorders helps students examine the causes and treatment of a variety of articulatory and phonological disorders that can affect someone’s ability to communicate effectively.
“For adults, when there is an acquired injury like a stroke and they lose the ability to communicate, it can be devastating,” Professor Blanco says. “My job is to be able to bridge that gap for them
and improve communication and quality of life in this new and unsettling time.”
Professor Blanco has found it especially rewarding to work with pediatric patients, particularly during her decade-plus at Blythedale Children’s Hospital, an independent specialty children's hospital in Valhalla, New York, dedicated to the diagnosis, care and rehabilitation of children with complex medical and rehabilitative needs. “I have countless stories of being there for the first time a child says for example, ‘I love you’ to their mother or ‘Hello’ to their father,’” Professor Blanco says. “It is those moments that keep me so inspired every day.”
She is excited to share those experiences with her NYMC students. “I look forward to taking what I have learned in the clinical world and giving it back to the next generation of SLPs,” Professor Blanco says. “They are the future of the profession.” ■
I look forward to taking what I have learned in the clinical world and giving it back to the next generation of SLPs. They are the future of the profession.
Chioma M. Okeoma, Ph.D., believes that great advances in science all start with collaboration. In her new role as professor and vice chair of research in the Department of Pathology, Microbiology and Immunology, the award-winning interdisciplinary scientist is excited to forge new partnerships among her New York Medical College (NYMC) colleagues to bolster the College’s research portfolio and inspire the next generation of research scientists.
“I have great expertise and skills in certain areas, but there are other things I cannot do,” Dr. Okeoma says. “You move research forward through collaboration, by sharing knowledge and resources and working together.”
Dr. Okeoma’s vast expertise in innovative research focuses on understanding the biology and functions of extracellular particles, including extracellular vesicles
She was inspired to pursue virology and immunology by the health disparities she witnessed while growing up in Biafra in southeastern Nigeria, where malaria is widespread and resources are scarce. “For me, my motivation has always been, ‘How do I help people? How do you solve a problem so that you can help not just your people, but everyone? What will be your contribution to science and medicine in terms of health?’” Dr. Okeoma says. Her career path has taken her to New Zealand and the University of Pennsylvania for training and to academic posts at the University of Iowa and, most recently, the Department of Pharmacology at Stony Brook University Renaissance School of Medicine. While Dr. Okeoma has seen an increase in measures to increase diversity within medical research, “diversity without inclusion is a problem,” she says. “If you don’t have
the NYMC campus but across Touro University. For example, she is helping establish an EV program at Touro’s newest affiliate, the Lovelace Biomedical Research Institute in New Mexico.
(EVs) and extracellular condensates (ECs). These particles are released from all cells in the body and play a vital role in intercellular communication. She studies how EVs and ECs are involved in immune regulation and host responses to viral infections such as HIV, as well as drug abuse and cancer.
Among her breakthroughs, Dr. Okeoma discovered that elevated levels of the protein BST-2 is linked to poor survival in patients with invasive breast cancer. Recently she secured more than $1 million in grants from the National Institutes of Health for her ongoing HIV research. Dr. Okeoma is examining how THC—the active element in marijuana— affects EV function and composition in patients with HIV and could potentially dampen inflammation that can lead to subsequent neurological dysfunction.

the power to make things right, then you find a place where your contributions can make a difference.”
Dr. Okeoma has found that place at NYMC. “I feel that people really listen and want to make changes,” she says. She considers her mandate as vice chair of research is “to do everything in my power to grow our research portfolio.” With the collaboration of the Humayun K. Islam, M.D., Ph.D., clinical professor and chair of the Department of Pathology, Microbiology and Immunology, Dr. Okeoma has already started eliminating red tape and streamlining the procurement system to enable labs to operate more efficiently. She is mentoring the postdocs in her lab, so that they, too, can inspire their own students someday. Dr. Okeoma is advising junior faculty on their research efforts not only on
Dr. Okeoma has found she is just as likely to be asked for help on grant applications and research methods as for non-academic life lessons. “I am a minority, a woman and a mother of four who happens to be in the academia. I am always asked, “How do you do this?’” she says. “It is an honor for me to be able to share how I have navigated my career. That is also mentorship.” ■
If you don’t have the power to make things right, then you find a place where your contributions can make a difference.
Chironian met up with Anthony M. Sozzo, M.A., M.S.Ed., associate dean for student affairs and director of student financial planning and student activities, to learn more about how scholarships aid in the future of aspiring physicians, researchers, physical therapists, speechlanguage pathologists and public health professionals. Sozzo is well-known among students for his wealth of knowledge on everything financial aid, having worked with thousands of students in the School of Medicine, School of Health Sciences and Practice and Graduate School of Biomedical
HOW IMPORTANT IS SCHOLARSHIP FUNDING TO NYMC’S RECRUITMENT EFFORTS?

There is a lot of competition for the best and brightest students. We are fortunate the College has afforded us resources that the Offices of Admissions are using to recruit students from diverse backgrounds. We want to level the playing field and give, as many students as possible, a chance by providing funding for their education.
I always say students do not have to leave school because of money. Scholarships will get students here and allow them to borrow less money in the future. Students will not feel as nervous or emotionally upset about having debt when they have a scholarship. Part of what we do for students who do have to borrow is make sure they are well equipped with the knowledge of how to manage their finances and loan portfolio once they graduate.
HOW DOES OUR SCHOLARSHIP PROCESS HELP ENCOURAGE DIVERSITY OF OUR MEDICAL SCHOOL APPLICANTS?
The School of Medicine Office of Admissions awards scholarships. They holistically review the students for scholarships addressing diversity and needs, and it works extremely well. We have one of the highest percentages of underrepresented students for U.S. medical schools, approximately 20 percent, which is remarkable. It is always good, especially if you are from a low-income background, to have some help reducing the amount of loans you may still have to borrow.
We have a zero percent default rate right now, looking back at the last three years. Before the COVID-19 pandemic, we were averaging 0.82 percent default rate for all three schools over a 10-year period. As a donor and taxpayer, when you give money to a scholarship campaign, you are getting it back many times over. It is really a great investment for the donor as well as a great investment for this country.
Sciences for four decades. He served as the graduate/ professional caucus chair of the National Association of Student Financial Aid Administrators (NASFAA), a national nonprofit organization that represents more than 22,000 financial aid professionals and thousands of colleges, universities and career schools and is decorated in achievements for his dedication to financial aid support for students and alumni. He was honored with the NASFAA 2019 Meritorious Achievement Award and was named the NASFAA 2013 Most Valuable Professional. From the impact scholarship has on the diversity of our student body to the multitude of resources available to tackle debt head on, Sozzo and the Office of Student Financial Planning are supportive of applicants, students and alumni when it comes to financial planning for higher education.
Scholarship funding is applied to tuition and helps to reduce the cost of attendance. Should a student need to borrow loans, the scholarship will reduce the amount they will borrow at NYMC. For example, a $15,000 renewable scholarship equates to a $60,000 saving over a fouryear period.
Since 2018, alumni and friends have donated nearly $6.5 million for scholarships, a third of which comes from Days of Giving, our annual twoday scholarship fundraising campaign. During this two-day campaign each, all gifts for scholarships are matched by a group of generous donors. The Founder’s Dinner also raises much needed funds each year, a portion of which goes towards scholarship.
WHAT IS THE TOTAL AMOUNT IN THE SCHOLARSHIP POOL?
The scholarship pool is in the $6,500,000 range this year and approximately 40 percent of students are receiving scholarships or grants.
HOW HAVE YOU SEEN SCHOLARSHIPS HELP NYMC STUDENTS?
A simple letter that states you received a scholarship is welcoming and shows that you are important to NYMC. It also relieves stress. That letter brings students to our campus, who will become graduates who will have a positive impact on the world. They will give back to their community because of the graciousness of the donors who allowed them to receive a scholarship and they pay it forward by being donors who help support the education of our future graduates. Scholarships create a culture of giving and I could not be prouder of being part of that culture at New York Medical College. ■
More than 130 members of the New York Medical College (NYMC) community gathered for an enjoyable day on the course at the annual golf tournament at Saint Andrew's Golf Club, in Hastings-On-Hudson, New York, on June 27, 2022. The tournament honored David E. Asprinio, M.D., chair and professor of clinical orthopedic surgery for years of support and dedication to the College while raising more than $185,000 for student scholarships and the expansion of the Clinical Skills and Simulation Center.



After hitting the links, a reception followed to celebrate Dr. Asprinio for his dedication and commitment to patients and their families. With 22 years of experience as an orthopaedic trauma surgeon and orthopaedic spine surgeon, Dr. Asprinio has served as department chair and program director of clinical orthopaedic surgery for 16 years. Dr. Asprinio also serves as co-director of the orthopaedic trauma fellowship shared between the Hospital for Special Surgery and Westchester Medical Center.
“We join in celebrating an exceptional and thoughtful clinician, a gentleman, a loyal supporter of the College, a father, son and a husband; and my doctor,” said Edward C. Halperin, M.D., M.A., chancellor and chief executive officer.
“The camaraderie among colleagues, friends and family was a testament to the NYMC community,” said Martin Katzenstein, M.D. ’78, associate professor of pediatrics and chair of the Board of Advisors at NYMC, who chaired the event. ■

After a two-year hiatus due to the COVID-19 pandemic, the School of Medicine (SOM) reunion was back in person on November 5 and 6, 2022. Alumni celebrating five-year graduation anniversaries and 50th anniversary honorees from the 2020, 2021 and 2022 cohorts, enjoyed an evening of dining and dancing followed by a brunch and campus tour the next day.


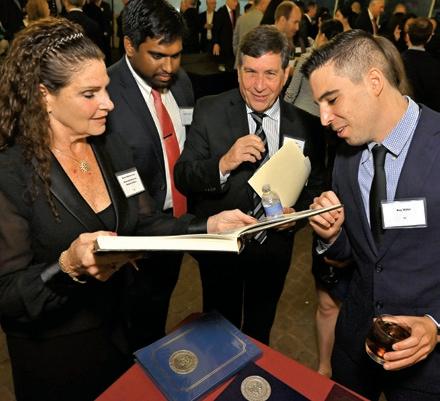




More than 165 alumni from class years ending in zero, one, two, five, six and seven, along with current students, faculty and administration, enjoyed an evening banquet at the Westchester Marriott in Tarrytown, New York.
Anthony Sozzo, M.A., M.S.Ed., associate dean for student affairs and director of student financial planning and student activities, served as the emcee.
The a cappella music of the Arrhythmias entertained the guests, who included
Jason D. Buchwald, M.D. ’97, who founded the Arrhythmias when he was in medical school. Speakers of the evening included Mill Etienne, M.D. ’02, M.P.H., vice chancellor for diversity and inclusion and associate dean for student affairs, and associate professor of neurology and of medicine, who was celebrating his twentieth anniversary from graduating from medical school and Rajkumar Pammal, SOM Class of 2023 and president of the SOM Student Senate.
Among the guests was Gerald D. Holzwasser, M.D. ’56. Dr. Holzwasser is 91 years old and is a full-time radiologist at Strong Memorial Hospital in Rochester, New York. There were also three generations of the Cooper Family in attendance: Harvey E. Cooper, M.D. '60, Jonathan D. Cooper, M.D. '87 and Jaimee Cooper, SOM Class of 2024.
The following day, alumni enjoyed a
brunch on campus at 19 Skyline Drive and had the opportunity to interact with current students in a panel discussion. Students shared their experiences in medical school and what New York Medical College means to them.
Alumni were inspired and shared their experiences as well, including Eric G. Levy, M.D. ’97, a solo practice family practitioner in Santa Maria, California, who recently endowed a scholarship for students.
Alumni wrapped up the weekend with a tour of campus and the Clinical Skills and Simulation Center and a wealth of memories. ■




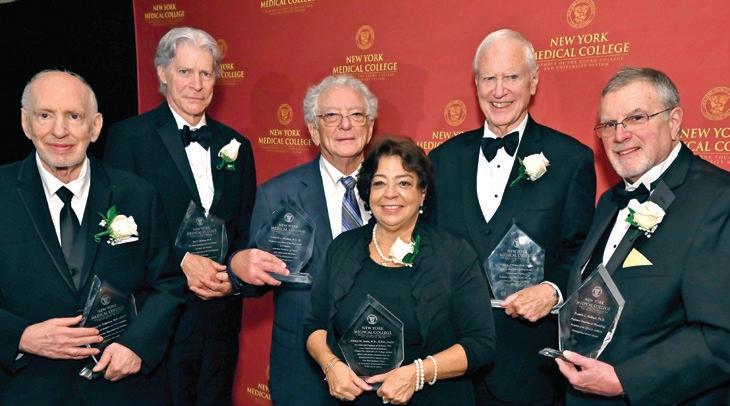
The evening of October 26, 2022, was a special one as guests gathered for the annual Founder’s Dinner at Marina Del Ray in the Bronx. More than 385 academic, health care, business and community leaders came together to celebrate New York Medical College’s (NYMC) proud history and promising future and to honor distinguished faculty and alumni leaders for their impactful and transformative achievements.
Gladys M. Ayala, M.D., M.P.H., F.A.C.P., former vice chancellor for College-wide student affairs, and senior associate dean for School of Medicine student affairs, NYMC and now dean and professor of medicine, NYU Long Island School of Medicine; William H. Frishman, M.D., MACP, professor of medicine and pharmacology and chair emeritus of the Department of Medicine; Leonard J. Newman, M.D. ’70, professor and chair of the Department of Pediatrics and associate professor of family and community medicine; James J. O'Brien, Ph.D., M.A., vice dean emeritus, School of Health Sciences and Practice (SHSP) and professor emeritus of public health; and Ben C. Watson, Ph.D., vice dean emeritus, SHSP and professor emeritus of speech-language pathology, were recipients of the Distinguished Service and Leadership Awards. The evening also honored Francis L. Belloni, Ph.D., professor emeritus of physiology, with the Alfred B. DelBello Distinguished Service Award.
The event was emceed by Vilma E. Bordonaro, M.B.A., chief of staff, NYMC, and Michael Crupain, M.D. ’06, M.P.H., senior vice president of clinical operations, Sharecare.
The presenting gold sponsors of the 2022 Founder’s Dinner were the NYMC Board of Advisors and Boston Children’s Health Physicians. Silver sponsors were William H. Frishman, M.D., MACP, and Westchester Medical Center and Bronze sponsors were Mr. and Mrs. Ben Chouake; Andrew and Sarah Levy; Dr. Meryl and Mr. Joseph Mark; Dr. and Mrs. Lawrence F. Neshiwat; Reva and Martin Oliner; Pavarini Construction Company Inc.; Ronald and Peggy Poe; Alan Rosenthal, D.M.D.; and Webster Bank. ■
Grateful for the opportunity afforded by New York Medical College, Phillip Capozzi, M.D. ’96, pays it forward with a legacy gift that will support future generations of health science professionals and researchers in the form of the Phillip Capozzi, M.D., Library.
BY KRISTIN BAIRD RATTINIIt was a grand occasion on May 20, 2022, for the New York Medical College (NYMC) and Touro University (TU) community, when the Health Sciences Library was officially renamed the Phillip Capozzi, M.D., Library, after Phillip Capozzi, M.D. ’96. Dr. Capozzi’s legacy gift to NYMC will enable the library to continue its tradition of being a dedicated communal learning space.
“We honor an alum today, who has lived the best of values, who has practiced as a highly successful physician, has
1885
mentored students and who has been generous not just to us, but to other institutions,” Alan Kadish, M.D., president of NYMC and TU said. “This is a very important moment in the history of the College.”
At the ribbon-cutting ceremony, Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, spoke of the vital role that libraries play at educational institutions as repositories of information for all to learn. “Many things have changed, but Dr. Capozzi’s

The students of the Class of 1885 vote unanimously to establish a medical library at the College and begin raising funds and purchasing books.
Eugene H. Porter, M.D. 1885, elected by his fellow students to lead the Library Committee, went on to serve as New York State Commissioner of Health from 1905 to 1913.
1890
gift will assure us that three things remain the same, with the first being that the tripartite mission of a university is the generation, conservation and dissemination of knowledge—and libraries are the lynchpin of the conservation of knowledge,” Dr. Halperin said.
“What has not changed but has been amplified is the ethos of the library— the library is dedicated to providing the information needed by its learners, educators, researchers and practitioners.
As part of the College's move to a new campus at the Flower Hospital on York Avenue and 63rd Street, the Library acquires a dedicated reading room.
1921
The College hires its first professional librarian, Frances Holly, to supervise the operations of the library.
1925
The Library becomes known as the Prentiss Library in honor of a donation from Jennie B. Prentiss, M.D., the first female physician to practice in Steubenville, Ohio, and longtime colleague of Claude A. Burrett, Ph.B., M.D., FACS, who had previously been dean of a medical college in Ohio and served as NYMC dean from 1925 to 1939 and president from 1939 to 1941.
More than ever the library is also a place where shared tools, technology and resources can be explored and used,” said Marie T. Ascher, M.S., M.P.H., the Lillian Hetrick Huber Endowed Director of the Phillip Capozzi, M.D., Library. “What we are offered today is an opportunity to both continue and enhance the services, the resources, the space and the staff of the library. We will make you, and do your name, proud.”

The library continues to be the premier space on campus for students to study and self-direct their learning, while also providing a suite of curated, primarily electronic information sources available to all NYMC constituents. With new areas of emphasis including an expanding focus on data management and curation, and expert collaboration with highly trained health sciences librarians in research and teaching, an effective, quality library comes with expenses. Dr. Capozzi's gift will allow the library to both maintain and enhance its position as a vital center of knowledge
development and management, training and learning at the College.
Dr. Capozzi, who has a 25-year career in anesthesiology, had long planned to give back to NYMC in a big way. His untraditional story of how he became an anesthesiologist after graduating at NYMC at 43-years-old is one that inspires many.

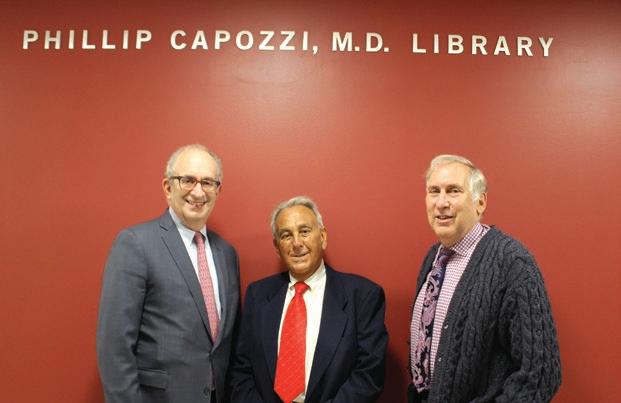
After earning a pre-med degree and graduating near the top of his class at Syracuse University, he was not admitted into medical school. He was crushed. He had dreamed of becoming a physician for years. For the next 16 years he decided to pursue other paths. Dr. Capozzi helped operate his family’s business in upstate New York managing entertainment for a golf course and banquet room and developed a thriving real estate practice. But all the while his desire to practice medicine never waned.
So, in 1990, when a urologist friend and his wife encouraged the 38-yearold Capozzi to apply again for medical school for the following school year, his
1956
The Library moves to a larger space at FlowerFifth and becomes known as the Lillian Morgan Hetrick Library in honor of a donation by the wife of J.A.W. Hetrick Jr., M.D., 1918, who served as acting dean from 1941-1942, dean from 1942-1953, and president from 1953-1957.
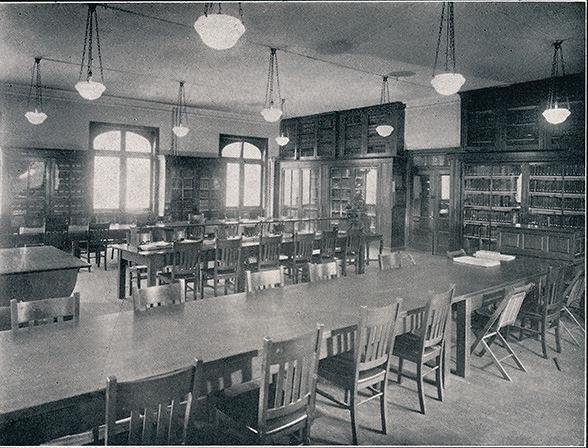
first reaction was of disbelief. “I told them they were crazy,” Dr. Capozzi says with a laugh. “Then I thought, ‘Why not look into it?’”
He did. Applying to medical school is a grueling process, especially when you are a working professional who has not cracked open a textbook in nearly two decades. He spent five arduous months preparing for the MCAT.
“I’d go into my real estate office early in the morning, and then spent from 9 a.m. to 3 p.m. five days a week at the Kaplan Course office,” he recalls. “After my first day, I walked out and said, ‘I can’t do this.’ But I went back the next day and took on the challenge head on. I really wanted to succeed.” He did: He earned a higher score on the MCAT than when he had first taken it.
“I only applied to a few schools because I really did not think I would get in,” he says. “This was back in the old days, when many schools did not take applicants over 30 years old. When I
was invited for an interview at NYMC, I was completely shocked.”
When he arrived for his interview, Dr. Capozzi instantly felt welcomed on campus. “For some reason, the dean and faculty seemed to take an immediate liking to me,” he says. “They liked the idea that I had lived my life and that I knew exactly what I wanted to do.
“They did not have to accept me. There were 5,000 other applicants for 150 positions. But they did. It felt like it was meant to be,” he recalled.
Dr. Capozzi was not the only non-traditional medical student in the entering class. One of his “atypical applicant” peers had worked at a gas station; another was a podiatrist. “The three of us were probably closer in age to the other students’ parents than we were to them,” he says. He was realistic about the unique challenges of being an older student. “It was not easy going back to school,” he says. “But the faculty were so supportive and they made suggestions for how to study and approach the whole program.”
He took a long practical view of his prospective medical career. “I knew I was too old to attempt a surgical residency, due to the physical demands and the fine motor skills required,” he says. “I realized that anesthesiology was perfect for me. It was a specialty I could pursue for many years, even with my later start.”
Against the odds, Dr. Capozzi graduated from NYMC in 1996 at age 43. He returned home to the Syracuse area to practice medicine near his aging parents. He performed general anesthesia for several years in a community hospital. “You handle all kinds of cases in that setting, from orthopedics to gynecology,” he says.
He then accepted an opportunity to work at an endoscopy center, with which he was affiliated for 15 years. Along the way, he has taken the time to indulge his passion for travel, stamping his passport in places ranging from Singapore to Rio de Janeiro, the Amalfi Coast to Dubai.
Dr. Capozzi felt overwhelming gratitude that NYMC had taken a big chance on such a nontraditional student. Now, after a thriving career in anesthesiology, Dr. Capozzi is repaying his gratitude to his alma mater by aiding future generations of health professionals in their studies.
“I was given a second chance at life. The faculty and administration wanted me to succeed,” Dr. Capozzi says. “I made a commitment 30 years ago that if I did succeed, I would make provisions to benefit this medical school. I am here today to fulfill that commitment.” ■
1972
When the College moves to Westchester County, the Hetrick Library merges with the library of the Westchester Academy of Medicine and relocates to its present space in the Basic Sciences Building on the Valhalla campus, becoming known as the Westchester Medical Center Library.
1985
The Library changes its name to the Medical Sciences Library, New York Medical College.
2006
A bequest from the estate of Lillian Hetrick Huber, the daughter of Lillian Morgan Hetrick and Dean J.A.W. Hetrick, establishes a permanent endowed directorship at the Library. The endowment ceremony includes remarks by Mrs. Huber's son Jeffrey B. Chick, M.D. ’75, a member of the fourth generation of the Hetrick family to be associated with the College.

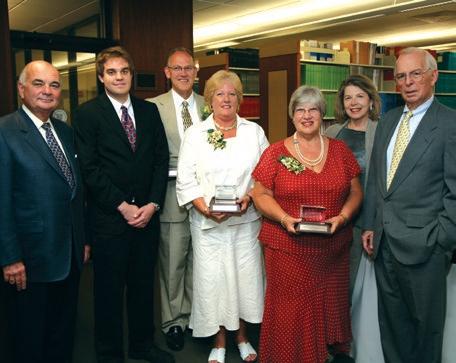
1995
The Library publishes the first edition of its annual Faculty Bibliography.
1996
The Library retires the physical card catalog and offers a computerized online catalog.
2004
The Library is renamed the Health Sciences Library to better reflect the services it provides to all three schools at New York Medical College.
2022
To honor a donation by an alumnus from the Class of 1996, the Library is renamed the Phillip Capozzi, M.D., Library


The two-day campaign on March 29 and 30, 2022, raised money for scholarships so students in the Graduate School of Biomedical Sciences (GSBMS), the School of Health Sciences and Practice (SHSP) and the School of Medicine (SOM), can pursue their education based on their passion and not economic background.
THANK YOU TO ALL OF OUR DONORS.
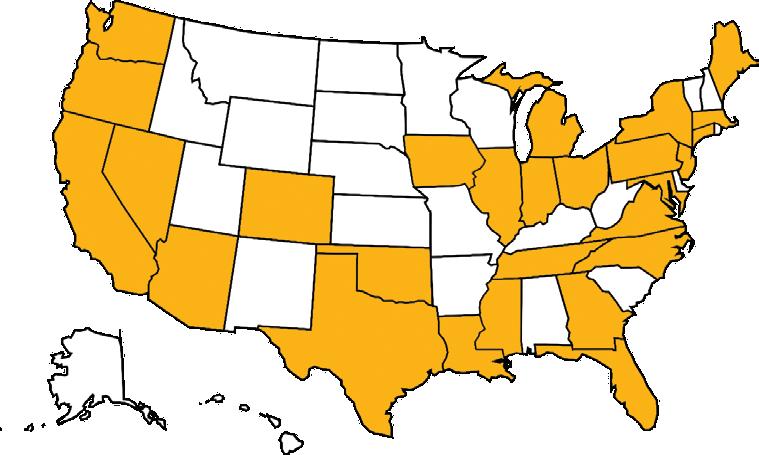
Being afforded a scholarship was a major investment in my future and has made me feel as though NYMC really was the place for me to continue my education. So many doors have opened for me, including the opportunity to pursue a Doctor of Physical Therapy (D.P.T.)/Master of Public Health (M.P.H.) dual degree and I know many more opportunities will arise. I am excited to finally enter society as a health professional and do my part. Thank you for your contributions.”
DOMINIQUE ELLIS, D.P.T. Class of 2022 and M.P.H. Class of 2024, SHSP

“As a soon-to-be physician, I aim to help underresourced patient populations like those in the community I grew up, and I am extremely thankful for all the selfless donors who have contributed to my journey.”
DAYENNY DE JESUS, M.D. candidate, Class of 2022, SOM
“My financial award provided peace of mind. It helped me veer focus back on my schoolwork and away from the fear of accruing debt or of working long hours to the detriment of my grades.”
RANIA HATAB, M.S. candidate in Clinical Laboratory Sciences Candidate, GSBMS

“With financial assistance, an education like the one offered at NYMC can become more accessible to students of varying backgrounds.”
SARI KOPPEL, Master of Science, Speech-Language Pathology (SLP) Class of 2023, SHSP


Institutional knowledge is invaluable when you are plotting the course for a medical school’s future. Two NYMC alumni are each bringing decades of in-house experience and leadership to their new roles as dean of their respective medical schools.
BY KRISTIN BAIRD RATTINI Jeffrey Boscamp, M.D. ’81 Dean of Hackensack Meridian School of MedicineIt is a thrill to build a program from the ground up and Jeffrey Boscamp, M.D. ’81, has done just that at Hackensack Meridian Health. Over his 36 years there, Dr. Boscamp founded the Section of Pediatric Infectious Diseases and the Steven Bader Immunological Institute at Hackensack University Medical Center. As the endowed chair of pediatrics, he helped design, staff and open the Joseph M. Sanzari Children's Hospital, which has since grown from 25 pediatricians to nearly 300 and was the first children’s hospital in New Jersey to be nationally ranked in U.S. News and World Report
And he was part of the leadership team who made their vision of an innovative approach to health education—rather than health care education—a reality with the opening of Hackensack Meridian School of Medicine, which admitted its first class of students in 2018 and earned full accreditation from the Liaison Committee on Medical Education in February 2023.

“It was such an incredible opportunity to design a new curriculum from scratch,” he says. Dr. Boscamp is especially proud of the medical school’s human dimension program, which pairs students with a local family at the beginning of their three-year curriculum. The student visits the family regularly and helps them navigate the health system. “We wanted to have students live and breathe the social determinants of health, which is a big focus that underlies our education,” he says. “Because health is 90 percent of how a person lives versus the 10 percent that is health care.”
As a medical student, a unique opportunity at New York Medical College led Dr. Boscamp to his specialty of infectious diseases. A team from the Centers for Disease Control and Prevention visited the school to discuss their investigation of the 1976 outbreak in Philadelphia of what became known as Legionnaires’ disease. “I thought, ‘This is the best detective work ever,’” Dr. Boscamp recalls. “Every day is a new case, a new challenge to solve when you are in an infectious disease practice; everybody sends you the cases they cannot figure out.”
His passion for teaching and academics was sparked soon afterward and remains a driving force for his work. As Hackensack’s cochief academic officer and senior vice president of medical school development and integration, he focused on linking undergraduate and graduate medical education, to allow a seamless transition for students to secure their residency within Hackensack Health System by the start of their third year. “People are starting to realize that continuum of education is crucial,” he says.
As dean, his goal is to create an urban scholars program, which would underwrite students’ medical school education in exchange for performing primary care in an urban setting. He is also looking forward to establishing a global health curriculum that students can complete in their specialized fourth year. The program will honor his late predecessor, founding dean Bonita Stanton, M.D., who was a celebrated expert in that field.
“I have built up such a network of goodwill over my years here at Hackensack,” says Dr. Boscamp. “We have tremendous support for the medical school, and as dean I will be able to call on the vast resources of our health network to make us even better.”

Being a good
make
But throughout his 20 years at Oregon Health & Sciences University (OHSU), David Jacoby, M.D. ’80, has demonstrated his exceptional skill and leadership in all three realms.
a
His lab is run jointly with his wife, Allison Fryer, Ph.D., who has also been NIH-funded for more than 30 years, as well as two more junior faculty, each with their own NIH funding. He has trained 21 students and fellows and has won multiple teaching awards for his efforts.
After 13 years at Johns Hopkins, Dr. Jacoby was hired at OHSU in 2003 as chief of pulmonary and critical care and led the expansion of that division in patient care, education and research. Under his leadership, the division developed a pulmonary hypertension program and sleep program and expanded the adult cystic fibrosis program. He is still an attending in the Medical Intensive Care Unit as a pulmonologist and an intensivist. “I was drawn to pulmonology by the critical care aspects of it,” he says. “It is a nice combination of cerebral and hands-on activities in a pressured environment.”
Dr. Jacoby expanded the Pulmonary and Critical Care Fellowship Program by securing a National Institutes of Health (NIH) T32 training grant in 2008, which has since been renewed twice. He became director of the OHSU M.D./Ph.D. program in 2008, training the next generation of physician-scientists to advance medicine from the bench to the bedside. He developed a second NIH T32 Medical Scientist Training Program grant. which was recently renewed with a perfect score at study section, he notes proudly.
Dr. Jacoby himself has been continuously funded by the NIH since 1990.
“At different times in my career, different aspects of research have been the most rewarding,” he says. “Early on, you want to make a contribution that leads to a different way of thinking about disease. Then, you just want to understand things. At this point in my career, what is most rewarding in my lab and the M.D./Ph.D. and fellowship programs, is the opportunity to train young scientists. You may not realize the progress you are making at the time, but then you see someone who was in your lab who is now a full professor, setting up their own lab, taking on leadership positions and being highly successful. That is extremely rewarding.”
Dr. Jacoby became interim chair of the Department of Medicine in 2017 and permanent chair in 2018. He is professor of medicine and chemical physiology and biochemistry in the OHSU School of Medicine and served as interim dean of the school from October 2021 until his appointment as permanent dean in December 2022.
As dean, his top priority is recruitment. He inherited seven interim department chairs and is in the process of filling those positions. He is also eager to channel more resources across the school’s institutes and departments. “I have had tremendous support from the faculty and chairs,” he says. “I have known most of these people for the better part of 20 years now, and the unconditional support I have received makes being the dean so rewarding.” ■
clinician does not automatically
you
strong scientist or good teacher.

Joseph D. Mark, Chair
Joseph Schwartz, M.D., Vice Chair
Alan Kadish, M.D.
Robert Alter, M.D.
Gary Barnett
Howard Baruch, M.D.
Benjamin Chouake, M.D.
Dee DelBello
Rabbi Menachem Genack
Gary Gettenberg, M.D. ’83
Munir Kazmir, M.D.
Moshe Lichtenstein
Lawrence F. Neshiwat, M.D.
Martin S. Katzenstein, M.D. ’78, Chair
Christel Bauer, M.D.
Sabra Brock, Ph.D.
William J. Camera, C.P.A.
Edward Chew, M.D. ’03
Steven H. Cho, D.D.S.
Eric I. Choe, M.D. ’88
Raymond A. Conta, J.D.
Noreen Ferrante, M.D. ’84
Kathleen Case Finzel, M.D. ’87
Moshe E. Hirth, M.D. ’88
Moira T. Imperial
Howard Jonas
Russell S. Kramer, M.D.
Martin D Keltz, M.D.
Norman L. Maron, M.D. ’70
Beth McErlean-Pierce
Monica Y. Michell, M.D. ’82
Stephen Nicholas, M.D. ’86
Martin Oliner, Esq.
Eliot Peyser
Ronald F. Poe
Joseph Popack
Avi Retter, M.D.
Stephen Rosenberg
Alan B. Rosenthal, D.M.D.
Henry Saphier, M.D. ’61
Rabi R. Sinha, M.D.
Kenneth R. Theobalds
While medical students learn the science of medicine, Sriram Shamasunder, M.D. ’05, is showing how to combine that knowledge with a patient-first perspective that contextualizes techniques to better serve communities traditionally marginalized from mainstream health care systems.
Leonard J. Newman, M.D. ’70
Rebecca B. Newman, M.D. ’05
Paul Ostrovsky, M.D. ’78
Michael D. Paris, M.D. ’67
Chong H. Park, M.D. ’96
Lawrence Rein
Anne Negrin Reis, M.D. ’02
Bruce Schanzer
William Smith
Susan N. Tierman, M.D. ’79
Steven Topfer, D.O.
Rajesh Verma, M.D. ’93
Anthony Viceroy
Vincent J. Vigorita, M.D. ’76
Patricia White, M.D.
John M. Zimmerman, M.D. ’78
As co-founder of the HEAL (Health, Equity, Action, and Leadership) Initiative, Dr. Shamasunder has built a fellowship program that pairs American-trained health professionals with clinicians, hospitals and NGOs that deliver holistic, equity-based health programs to marginalized communities in the United States, including the Navajo Nation, and internationally. In doing so, HEAL trains frontline providers— half of whom are Native American or from impoverished countries outside the U.S.—to learn the unique circumstances facing each community and adapt their medical practices to be impactful and responsive to community needs.
“Clinical skills are not enough,” says Dr. Shamasunder, associate professor of medicine at the University of California, San Francisco. “If you are not spending enough time with your patients, do not understand the historical context of their environment, or recognize power as a social determinant of health, then you will ask the wrong questions,” he says. “Only by asking the right questions can providers mine the information they need to give care that is individually, culturally and medically appropriate.”
HEAL fellows are not required to stay in the communities after their two-year commitment is over, but many do. This is perhaps surprising given that medical professionals are incentivized to work toward careers at prestigious institutions but speaks to the power of making an intimate and meaningful difference in many people's lives. To date, HEAL has provided medical care for over two million people in underresourced communities across the world and graduated hundreds of Fellows.
The HEAL Initiative in part grows from Dr. Shamasunder’s unique background. Born to immigrant parents from India, he grew up the frequent target of racial slurs in the predominately white, working class, southern California desert town of Lancaster. After the terrorist attacks of 9/11, he felt unwelcome as a bearded, brown-skinned man in America. “I extended that feeling to patients who are consistently othered,” he says. But it was his friendships with fellow poet
and civil rights activist June Jordan, and Partners in Health founder, Paul Farmer, M.D., Ph.D., who helped him view health as social justice.
He met both at the University of California, Berkeley, where he earned his bachelor’s degree in molecular cell biology in 2001. Jordan taught “Poetry for the People,” which married poetry and social activism. Dr. Farmer gave a lecture about caring for people in Haiti, where Dr. Shamasunder planned to work after residency.
Dr. Farmer persuaded him to work in rural Burundi instead. “He made me feel as if I were making the only career decision that made sense—choosing what he called ‘pragmatic solidarity’ alongside the poor,” Dr. Shamasunder wrote in a tribute to his mentor, who died in 2022. Dr. Farmer insisted that physicians identify barriers that prevent patients from receiving care. “Paul reminded us that patients try to seek treatment but are handcuffed by user fees they cannot afford and discouraged by facilities with unavailable, underpaid staff and little equipment,” he wrote.
Meanwhile, Jordan, who was African American and battling breast cancer, was proof that economic privilege does not guarantee health care justice. “June sometimes felt talked down to by her medical team, she felt erased by the health system,” he told a Berkeley TEDx audience in 2016. “At the end of her life, her brilliant career and financial security were not enough to shield her from the challenges most Black women with breast cancer face,” he said. Her needless suffering, and that of people in Burundi, made him realize that preventable deaths begin where power and narrative end, meaning we care about the lives that we know intimately. The realization made him ask, “What does it mean to be a committed doctor in this unequal world?” ■
Office of Development and Alumni Relations
New York Medical College
We would love to share your most recent news and accomplishments in the next issue of the Chironian. If you have any recent professional accomplishments or developments, published a book, or have any family news to share, please let us know. Submit your updates to www.nymc.edu/alumni or mail them to:
40 Sunshine Cottage Road Valhalla, NY 10595
Jermoh Kamara, M.P.H. ’18, was elected to the Worcester School Committee in 2021. She serves in a minority-majority school district that educates more than 24,000 students.

Maraheb AlQallaf, M.D. ’15, CCC-SLP, is a team leader speechlanguage pathologist (SLP) in one of the leading rehabilitation hospitals in Kuwait. She has been training SLP student clinicians from Kuwait University and the University of Alberta Faculty of Rehabilitation Medicine (FRM), Edmonton, Canada, where she was appointed affiliated clinical educator by FRM's Collaborative for Scholarship in Clinical Education for providing extraordinary contribution to the education of their students. In December 2021, she was named the best therapist in Kuwait by local media and is currently pursuing her

Bilingual Extension Certificate at Teachers College, Columbia University. She was also a member of the Leadership Development Program 2022 at the American Speech-Language-Hearing Association.
Akshat Jain M.D. (GME ’11), M.P.H., is director of the Pediatric Sickle Cell Center at Loma Linda University Children’s Hospital, which was recently awarded network affiliation with a national consortium. The Center is one of less than 30 such centers in the United States with a unified mission to improve the care of individuals with sickle cell disease and recognized by the California State Senate.


Gail L. Clifford, M.D. '91, launched a podcast, Single Mom M.D., to support single mother physicians with true work-life balance. It can be found on Apple Podcasts and Spotify.
Marc Denton Stam, M.D. ’88, is director of cardiothoracic and vascular surgery at Baptist Hospital in Fort Smith, Arkansas.
Leona D. Borchert, M.D. ’87, FAAN, is senior medical director in clinical development neurology at Vaxxinity, Inc., a small biopharmaceutical company developing immunotherapeutic vaccines to deliver and democratize health care to middle- and low-income countries. She is the medical director for clinical Phase 1/2 trials using vaccines to investigate the prevention of Alzheimer's and Parkinson's disease.
Peter E. Bentivegna, M.D. ’85 FACS, was elected president of the New England Hand Society and presided over the 50th Anniversary Meeting of the Society in Sturbridge, Massachusetts. He continues to participate with the American Society of Surgery of the Hand (ASSH), Lend a Hand Program, which teaches upper extremity anatomy at Tufts University School of Medicine and to the ASSH Membership Committee.

Philip R. Cohen, M.D. ’83, has decided to focus his interests on psychodermatology. His papers on skin biters (dermatodaxia), nailassociated body-focused repetitive behaviors, such as habit-tic nail deformity, onychophagia and onychotillomania, and delusional infestations were published in Cureus in February, March, and June 2022, respectively. In May 2022, he co-authored the first paper on artificial nail-associated onychotillomania (ANASON) published in Cureus
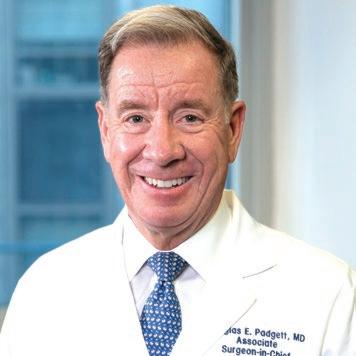
Douglas E. Padgett, M.D. ’82, was appointed surgeon-in-chief and medical director of the Hospital for Special Surgery, a 160-yearold academic medical system specialized in musculoskeletal health. He is a world-renowned orthopedic surgeon, educator and researcher, focused on clinical outcomes, biomaterials and the role of enabling technologies in joint reconstruction.
William C. Reha, M.D. ’81, M.B.A.,
When New York City was the epicenter of the COVID-19 outbreak in the United States in March of 2020, an emergency order from New York State mandated all hospitals in the state to increase capacity by 50 percent to accommodate the expected surge in COVID-19 cases.
The need to create additional space was especially urgent for Montefiore Health System, the largest health system in the Bronx, which at the time was the borough with the highest per capita hospitalizations and deaths from COVID-19 in New York City. Leading the efforts was Jared Shapiro, M.P.H. ’08, associate vice president of environmental health and safety (EHS) at Montefiore, who also serves as adjunct assistant professor in the School of Health Sciences and Practice where he is pursuing his Dr.P.H. degree.
“As a member of Montefiore’s health system Incident Command Staff overseeing our COVID-19 response, I worked with hospital leadership to identify non-traditional locations that could be converted to clinical space, such as conference rooms and cafeterias. Once the locations were chosen at each one of our campuses, work quickly began to make the transformations,” says Shapiro who provides strategic direction and oversight for Montefiore’s 10 hospitals, Albert Einstein College of Medicine, a school of nursing and 350 offsite locations of the health system.
Donald E. Sawyer, M.D. ’70, married Rebecca Laskin in Jackson, Mississippi, on November 5, 2022. His wife, Anne, passed away in April 2020, after a long battle with Alzheimer's disease.
Marvin Ginsburg, M.D. ’64, published his third book on Amazon, Much Ado About Somethings: Poetry of Life. All proceeds go to St. Jude Children's
Those transformations were a truly collaborative effort involving personnel from Montefiore’s EHS department, hospital administration, engineering, physicians and nurses, supply chain services, design and construction and security. For these non-traditional spaces to be brought up to code to serve as clinical spaces, a series of changes had to be made including the installation of flooring, head walls, IT equipment, electrical wires, equipment for medical gasses and suction and water outlets. “The biggest challenge was getting the proper oxygen wall outlets,” says Shapiro. “Due to the nationwide outbreak, the demand for oxygen outlets was enormous as hospitals scrambled to expand their capacity. We sent drivers to our various vendors’ warehouses across New York and New Jersey to ensure we got these vital resources.”
The quick work and team effort paid off. Converting nonclinical spaces to patient care spaces was accomplished quickly and successfully. Montefiore’s Emergency Operations Center received its first COVID-19 patient on March 11,
2020. The unit was open for 18 days and accommodated 170 patients. “While several of those patients went on to a higher level of care,” reports Shapiro, “there were no respiratory or cardiac arrests or deaths on the unit.” This was a point of pride shared by all at Montefiore.
Advancing research and promoting health and well-being are tenets that New York Medical College (NYMC) and Montefiore Health System have in common. The two often partner to better serve the health needs of the diverse local population. Montefiore works with the Center for Disaster Medicine at NYMC, which conducts interdisciplinary research, training, technical assistance, as well as educational activities related to emergency preparedness for disasters, terrorism and public health emergencies. “It is a strategic partnership geared toward better serving people in our communities, which is what it is all about,” explains Shapiro.
NYMC has figured prominently in Shapiro’s life, where he received a Master of Public Health in 2008. Looking back at his long affiliation, he says, “The school has provided me with so much as a student that I love to give back in the form of teaching. I really enjoy meeting students who are passionate about all aspects of public health—working with them, reading their papers and listening to what motivates them.”
Equally rewarding is his work at Montefiore. “It allows me to be a part of the work that ensures our staff is equipped to provide the best possible care to our communities and provides a topnotch education for our future physicians and researchers.”

While he spends his professional time in New York, Shapiro is a Jersey boy, having grown up in Woodcliff Lake, a small town in Bergen County where he lives with his wife and two young children. He makes it a priority to spend as much time as possible with them outside of work, “ensuring they are happy and, of course, healthy.” ■
for the School of Medicine, Graduate School of Biomedical Sciences and School of Health Sciences and Practice
Celebrating classes ending in ’3 and ’8
Reception and Dinner
Saturday, November 4, 2023
Sleepy Hollow Hotel, Tarrytown, New York

Brunch and Campus Tours
Sunday, November 5, 2023
19 Skyline Drive, Hawthorne, New York

www.nymc.edu/reunion
If you have any questions, please contact the NYMC Office of Development and Alumni Relations at (914) 594-2720 or development@nymc.edu.
Itis a major career decision that many graduate students face: Do you stay in academia or work in industry? Michelle Gaylord, Ph.D. ’12, who earned her degree in microbiology and immunology, knew since her undergraduate days that industry was the right fit for her career in immunology. “I like the hustle and bustle,” she says. “There is a buzz and excitement because you’re always working on something that, if successful, will ultimately touch patients.”
As a principal scientist at Pfizer, Dr. Gaylord experienced that hustle, bustle and buzz on an unprecedented level when the COVID-19 pandemic emerged in early 2020 and the company rapidly mobilized its talent and resources to develop a vaccine against the virus. “Everyone jumped in and asked, ‘What can I do to help?’” she says. “The atmosphere was team-oriented and laser-focused.”
Dr. Gaylord’s talent lies in clinical and diagnostic assay development and validation. When a doctor orders blood tests to screen for a particular disease, such as COVID-19 or Lyme disease, immunoassays can detect and measure the presence of antibodies against that ailment.
She honed her assay skills by focusing on the mechanisms of Lyme disease pathogenesis for her dissertation at New York Medical College (NYMC). Dr. Gaylord worked with samples from Lyme disease patients treated at the Lyme Disease and Diagnostic Center directed by Gary Wormser, M.D., professor of medicine, pathology, microbiology and immunology, and of pharmacology and vice chair of the Department of Medicine.
Dr. Gaylord valued the mentorship of Mary Petzke, Ph.D., assistant dean for medical student research and associate professor of pathology, microbiology and immunology, as well as Ira Schwartz, Ph.D., professor emeritus of microbiology and immunobiology and former chair of the Department of Microbiology and Immunology, in whose lab she worked. “I really admired and respected all the people in that lab,” she says. “I still think about those colleagues to this day.”
After a two-year postdoctoral fellowship at the Icahn School of Medicine at Mount Sinai, she joined Siemens Healthineers as a senior biochemist in laboratory diagnostics and immunoassays. “Siemens developed assays for all sorts of conditions, so I learned an incredible amount during my four years there,” Dr. Gaylord says.
She joined Pfizer as a principal scientist in December 2018, working on high-throughput clinical immunoassays and diagnostics. “Our team would put assays through a series of tests to make sure they were fit for use on a large scale to test samples

from our clinical trials,” Dr. Gaylord explained. “Everything is done with the utmost quality.”
With the right skills, in the right place, at the right time when the COVID-19 pandemic hit, Dr. Gaylord was ready when Pfizer, in collaboration with BioNTech, started developing its mRNA vaccine. She was promoted to senior principal scientist in June 2020. She evaluated novel technologies to improve the efficiency of assay development and was part of the team that validated one of the assays that supported clinical trials of the Pfizer-BioNTech vaccine. When the FDA granted emergency use authorization for the Pfizer-BioNTech COVID-19 vaccine in December 2020, the mood at Pfizer “was joy, absolute joy,” she says. “It made all of the challenges and hard work worth it.”
Dr. Gaylord, now an associate director in the clinical and diagnostic assay development organization at Pfizer, is currently working on serological diagnostics and emerging technology to support vaccines in Pfizer’s pipeline. “I want to continue learning,” she says. “I am lucky to be at Pfizer and be able to work on cutting-edge research.” She led the team that validated a serological diagnostic algorithm to support the Lyme disease vaccine candidate being developed by Pfizer in collaboration with Valneva. Dr. Gaylord says, “It is great to have my experience from NYMC come full circle.” ■
Wilson Young, M.D. ’07, Ph.D. ’07, M.S. ’99, died on November 16, 2022. He was 49.
Robert F. Smith, M.D. ’04, died on January 26, 2022. He was 59.
Avinash Agarwal, M.D. ’99, died on January 19, 2022. He was 47.
Melvin J. Helm Jr., M.D., Fifth Pathway ’96, died on December 18, 2021. He was 55.
Marsha L. Henderson, M.P.H. ’95, died on November 14, 2022. She was 84.
John C. Hordines, M.D. ’93, died on October 10, 2021. He was 54.
Jeffrey R. Bechler, M.D. ’87, died on December 29, 2022. He was 63.
Douglas T. George, M.D. ’84, died on March 3, 2022. He was 68.
Lenore J. Orange, M.D., Fifth Pathway ’84, died on July 30, 2021. She was 80.
Robert S. Abrams, M.D. ’83, died on November 7, 2022. He was 66.
Morris A. Diamant, M.D. ’78, died on February 5, 2022. He was 68.
Gary G. Knackmuhs, M.D. ’76, died on January 14, 2022. He was 71.
Eugene L. Kavanagh, M.D. ’74, died on February 19, 2022. He was 74.
Elliott N. Perla, M.D. ’74, died on June 2, 2022. He was 73.
Jeffrey H. Dobken, M.D. ’73, M.P.H. ’15, died on October 26, 2021. He was 77.
Newton J. Cochran, M.D. ’71, died on October 29, 2021. He was 80.
Paul V. Conescu, M.D. ’69, died on June 11, 2022. He was 78.
Kenneth B. Juechter, M.D. ’68, died on December 6, 2022. He was 90.
Francis A. Manopoli, M.D. ’68, died on July 20, 2021. He was 79.
C. Gene Cayten, M.D. ’67, M.P.H., died on June 23, 2022. He was 81.
Randolph D. Maloney, M.D., F.A.C.S. ’67, died on July 25, 2022. He was 82.
Captain John J. “Jack” Bouvier, M.D. ’66, died on December 13, 2020. He was 81.
Raymond A. Gagnon, M.D. ’66, died on October 11, 2021. He was 81.
N. Noel Testa, M.D. ’66, died on June 29, 2022. He was 81.
Albert L. Saphier, M.D. ’65 died on March 4, 2023. He was 83.
Joel L. Kanter, M.D. ’64, died on April 2, 2022. He was 83.
John J. Healy, M.D. ’63, died on March 5, 2022. He was 85.
Norman A. Lieberman, M.D. ’63, died on January 30, 2022. He was 84.
Martin S. Neff, M.D. ’63, died on December 20, 2022. He was 85.
Joseph Dello Russo, M.D. ’62, died on February 22, 2022. He was 87.
Alan I. Fine, M.D. ’62, died on February 18, 2022. He was 86.
Col. Charles V. Tramont, M.D. ’62, died on November 18, 2021. He was 84.
Barry H. Tischler, M.D. ’61, died on July 15, 2022. He was 86.
John K. Coyle, M.D. ’60, died on February 28, 2022. He was 87.
Richard P. Orphanos, M.D. ’59, died on August 14, 2021. He was 90.
Richard D. Perera, M.D. ’58, died on December 3, 2021. He was 88.
Mark F. Anapoell, M.D. ’57, died on September 27, 2021. He was 89.
William J. Cleary Jr., M.D. ’57, died on September 8, 2021. He was 89.
Richard J. Cobb, M.D. ’57, died on September 28, 2021. He was 90.
Michael L. Daly Jr., M.D. ’57, died on September 15, 2021. He was 91.
Thomas L. March, M.D. ’57, died on October 7, 2021. He was 90.
Ernest J. Steinhilber III, M.D. ’57, died on June 16, 2022. He was 91.
Joseph F. Fennelly, M.D. ’56, died on October 11, 2022. He was 93.
Thomas J. Martin, M.D. ’56, died on June 8, 2022. He was 91.
William F. Varr Jr., M.D. ’56, died on August 5, 2021. He was 91.
Howard N. Christ, II, M.D. ’55, died on December 17, 2021. He was 94.
James J. Finnerty, M.D. ’55, died on February 27, 2022. He was 92.
Paul E. Van Horn, M.D. ’55, died on July 8, 2021. He was 91.
Robert J. Widows, M.D. ’55, died on October 17, 2021. He was 96.
Roderick S. Coler, M.D. ’54, died on January 6, 2023. He was 99.
Jerrold M. Feigenbaum, M.D. ’54, died on January 11, 2022. He was 92.
Grace G. Jorgensen, M.D. ’54, died on July 28, 2022. She was 93.
Julius A. Bosco, M.D. ’53, died on December 31, 2022. She was 93.
Seymour Tobin, M.D. ’52, died on August 4, 2021. He was 95.
Irving Glassman, M.D. ’51, died on February 16, 2023. He was 101.
Aaron M. Schwartz, M.D. ’50, died on December 21, 2022. He was 94.
Arnold I. Turtz, M.D. ’48, died on December 30, 2021. He was 95.
Frank E. Ferro, M.D. ’47, died on October 17, 2021. He was 98.
Beatrice M. Brooks, M.D. ’45, died on September 6, 2022. She was 100.
Delphine Bartosik ,M.D., associate professor of obstetrics and gynecology, died on October 1, 2022. She was 84.
C. Gene Cayten M.D. ’67, M.P.H., clinical professor of surgery, died on June 23, 2022. He was 81.
Sophie Chen, Ph.D., research associate professor of medicine, died on May 8, 2022. She was 79.
Joseph F. Fennelly, M.D. ’56, clinical assistant professor of community and preventive medicine, died on October 11, 2022. He was 93.
Kenneth Bernard Juechter, M.D., clinical associate professor of ophthalmology, died on December 14, 2022. He was 90.
Souheil Kandalaft, M.D., clinical assistant professor of surgery, died on December 31, 2022. He was 90.
Stanley S. Passo, Ph.D., professor of physiology, died on September 14, 2022. He was 82.
Elliott N. Perla, M.D. ’74, professor emeritus of medicine, died on May 26, 2022. He was 73.
Janet Piscitelli, M.D., clinical associate professor of pathology, microbiology and immunology, died on January 24, 2023. She was 61.
Gerard D. Robilotti, M.S., a member of the Board of Trustees from 2007 to 2011, died on May 25, 2022. He was 81. Mr. Robilotti also served on the faculty as distinguished visiting professor in the School of Health Sciences and Practice and as senior associate dean at the College and director of medical education at Danbury Hospital.
Productive in clinical and health services research, Dr. Cayten was a prolific author and served on the editorial boards of several journals. He served as editor-in-chief of Lange Q&A: Surgery, a book for medical students studying for the USMLE Step 2 and the surgery shelf exam, as well as was the co-editor of The Textbook of Penetrating Trauma, a comprehensive and authoritative presentation of only injuries with penetrating mechanisms.
(1941 –
Gifted surgeon and trauma expert, C. Gene Cayten, M.D. ’67, M.P.H., professor of surgery and of community and preventive medicine and senior associate dean at Our Lady of Mercy (OLM) Medical Center, a former affiliate of New York Medical College (NYMC), died on June 23, 2022, at the age of 81.

Dr. Cayten, joined the faculty in 1983 but his ties to NYMC go back 20 years earlier when he entered the School of Medicine in 1963. A junior member of Alpha Omega Alpha, the national medical honor society and recipient of the Cor et Manus award, he went on to complete his surgical residency at the Hospital of the University of Pennsylvania and a research year at Yale University School of Medicine, earning his M.P.H. degree. Dr. Cayten served on the faculty for ten years at the University of Pennsylvania, where he co-founded the Center for the Study of Emergency Health Services which received more than $3 million in grants and contracts during his tenure.
Dr. Cayten served as chief of surgery at OLM in the Bronx, New York, where he especially enjoyed teaching students and residents from around the world. He also made major professional contributions to the development of trauma care systems as director of the Institute for Trauma and Emergency Care at NYMC, as well as program director for the College surgical residency program at Lincoln Hospital in the Bronx, and OLM.
Stanley S. Passo, Ph.D., Professor of Physiology
Dr. Passo proudly served as grand marshal for the 2004 Academic Convocation and in 2005, he was inducted into Alpha Omega Alpha, the national medical honor society. He was a repeat winner of the College chapter of the American Medical Women’s Association’s Gender Equity Award in 2005 and 2011, which recognizes medical school faculty who promote a gender-fair environment by assuring equal opportunity for women and men to study and practice medicine. In 2010, Dr. Passo was honored by the Graduate Student Association with the Honored Faculty Award at the 22nd Annual Graduate Student Research Forum.
A gifted and dedicated teacher and mentor for nearly half a century, Stanley S. Passo, Ph.D., professor of physiology, died on September 14, 2022, at the age of 82. His intellect and infectious smile and laugh won over countless medical, graduate and physical therapy students, as well as medical residents who kept in touch with him long after they completed his physiology course. He joined the NYMC as faculty in 1969 and spent his entire career at the College until his retirement in 2016.
Dr. Passo’s research in pulmonary and cardiovascular physiology and hypertension was motivated by his own father’s struggle with high blood pressure and he relished sharing his knowledge and expertise with students. His gift for teaching earned him the honor of being a distinguished member of the Robert Goldstein Society, an honor reserved for faculty who have been honored with Excellence in Teaching Awards for more than ten years. He was more than qualified for the role, earning teaching awards for more than two decades.
He received his B.S. degree in biology from the City College of New York and his Ph.D. in physiology from the College of Physicians and Surgeons at Columbia University. Dr. Passo completed a post-doctoral fellowship San Francisco Medical Center at the University of California, followed by an additional year of research before returning to his roots in New York.
Elliott N. Perla, M.D. ’74, Professor Emeritus of Medicine and Former Associate Dean for Student Affairs
After graduating from the University of Pennsylvania, he joined the NYMC community as a medical student in 1970. Upon completion of medical school, he completed his residency in internal medicine at Mount Sinai Hospital and a pulmonary fellowship at NYC Health + Hospitals/Metropolitan, where he became chief of the Department of Medicine, associate dean for student affairs, director of the residency program and vice president of the medical board. Dr. Perla also served as chief of the pulmonary disease section of NYC Health + Hospitals/ Lincoln, where he developed and supervised a comprehensive care program for asthma and served as medical director of Terence Cardinal Cooke Health Care Center, where he oversaw the medical administration and coordination of medical education. An active and productive member of the NYMC community, Dr. Perla served as the School of Medicine house advisory dean, a member of the faculty senate and sat on the editorial board of Quill & Scope, the student journal.
Trusted mentor, advisor and confidante to thousands of medical students, Elliott N. Perla, M.D., ’74, professor emeritus of medicine and former associate dean for student affairs, died on May 26, 2022, at the age of 73. His teaching, administrative and clinical responsibilities at NYMC were numerous and he was well respected and admired by students, colleagues and leadership alike.
Dr. Perla was soft-spoken but had a strong voice as an advocate for his students. His teaching efforts were lauded with honors bestowed by graduating residents and teaching excellence awards given by medical students. Graduating classes dedicated multiple yearbooks to him. One student wrote in her nomination for the yearbook dedication, “Dr. Perla has been the most helpful faculty member I have encountered at NYMC. He listens to what you want and need and does everything in his power to make it happen… He always makes you feel like you are a priority to him and does it in a very warm and fatherly way.”
He was instrumental in helping thousands of medical students map out their careers and his “dean’s letters,” or medical student performance evaluations describing the performance of each medical student as part of their residency application process, were legendary. They were even rated among the best letters in the country for quality, content and effectiveness
by a task force from the University of Washington in 1999 according to Association of American Medical Colleges guidelines.
Gerard D. Robilotti, M.S., Former Member of the Board of Trustees
and research activities. He was honored with the Distinguished Service Award for his longstanding dedication to the College at the 2005 Founder’s Dinner.
(1940 – 2022)
Gerard D. Robilotti, M.S., a member of the Board of Trustees from 2007 to 2011, died on May 25, 2022, at the age of 81. He was also distinguished visiting professor in the School of Health Sciences and Practice, senior associate dean at the College and director of medical education for Danbury Hospital. A leader in medical education and hospital administration, Mr. Robilotti was the former president of Danbury Hospital, executive vice president of Danbury Health Systems, Inc. and president of the Danbury Hospital Development Fund. He was influential in strengthening the College’s affiliation with Danbury Hospital, where he enhanced the medical education programs for medical students and residents
Mr. Robilotti was a distinguished lecturer at several institutions, including Western Connecticut State University, Quinnipiac College, University of Connecticut and Yale University. He was a fellow of the Royal Society of Health, the New York Academy of Medicine and the American College of Healthcare Executives and was active in a variety of civic and community organizations, including Boy Scouts of America, Fairfield County Council, Greater Danbury Chamber of Commerce, Western Connecticut State University Foundation and Newtown Savings Bank. He was a member of the Connecticut Hospital Association and served as delegate at the American Hospital Association and regent for Connecticut for the American College of Healthcare Executives. In these roles, he advocated frequently in Hartford and Washington on behalf of the state’s hospitals for sound health and health insurance policies.
Mr. Robilotti was also a Knight Commander of the Grand Order of the Holy Sepulchre.
He graduated from Manhattan College and completed his master’s in hospital administration at Columbia University School of Public Health, followed by a residency in hospital administration at the former Beekman Downtown Hospital.
Wednesday
October
The NYMC Donate Life Club finished the 2021-2022 academic year strong with a record 256 donations. The donations, which all came during a blood shortage in New York, reached approximately 650 patients in area hospitals in a time of great need.




The NYMC community rallied to support the Stand with Ukraine humanitarian drive to aid Ukrainians who were facing a humanitarian crisis from the Russian military invasion of their country. The collection, led by Tetyana Cheairs, M.D., M.S.P.H., assistant dean for Ph.D. programs and assistant professor of pathology, microbiology and immunology, saw more than 2,500 donations of food items, clothes and other products.
The partnership between NYC Health + Hospitals/Metropolitan and NYMC—the longest affiliation between a medical school and municipal hospital in the United States— was celebrated during a Plaque Dedication Ceremony at Met in June 2022. The plaque was restored by Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, and Nicholas Webb, MSIS, archivist and digital preservation librarian, and was originally presented to Metropolitan in 1975 to commemorate the life-saving work of Met staff for three NYPD officers.
5

A distinguished group of women leaders took part in the “Knocking Down Barriers: Women in Healthcare and Academic Leadership” panel discussion at NYMC in March 2022. The event featured three panels and 14 panelists, as leaders from both NYMC and WMCHealth shared their experiences as women in medicine, academia and leadership roles, and the obstacles they faced along the way.

6 The NYMC Health Services staff along with Redab Alnifaidy, SOM Class of 2023, were honored by Westfair’s annual Doctors of Distinction awards. Health services, led by Marisa A. Montecalvo, M.D., director of health services and professor of medicine, won the Team Award, while Ms. Alnifaidy won the Promise for the Future Award.
7 Jonathan V. Pascale, a Ph.D. student was the inaugural recipient of the Melvin H. Amler Prize for Innovation in September. The award is in honor of the late Melvin H. Amler, M.S., D.D.S., a NIH-funded biomedical researcher and practicing dentist whose creativity inspired his students and colleagues for more than six decades.
8 NYMC and TU hosted the Innovation and Entrepreneurship Conference in the Biomedical Space Conference in September 2022. More than 500 guests were in attendance for the conference organized by Salomon Amar, D.D.S., Ph.D., senior vice president for research affairs, TU, vice president for research at NYMC.
9 The Center for Disaster Medicine hosted a two-day course on Operational Medicine for law enforcement in February 2023. Participants included officers from the FBI, Homeland Security and local police departments. Officers were trained in didactic topics in basic tactical medicine, including sensory-impaired environments, direct threat care, indirect threat care and evacuation care. The course combined the fundamentals of basic tactical medicine in austere environments and scenario-based training in tourniquet application, wound packing, airway management and evacuation of victims to reinforce the skills they learned.

10 NYMC faculty members Lori Solomon, M.D. ’99, M.P.H. ’09, Salomon Amar, D.D.S., Ph.D., and Gregory R. Veillette, M.D., were among 12 honored by Westchester Magazine as “2022 Healthcare Heroes.” They were awarded for their dedication to health care in Westchester and beyond at the Ninth Annual Healthcare Heroes luncheon in May 2022.



11 NYMC co-founder and revolutionary, William Cullen Bryant, is back at the College–in oil painting form. The portrait of the long, gray-bearded founding father is hung prominently in the Blanche and Albert Willner, M.D. ’43 Atrium and Lobby in the Medical Education Center, where hundreds of students pass each day and can now be inspired by the man who laid the College’s foundation. Jay D. Tartell, M.D. ’82, gifted the College “Portrait of William Cullen Bryant,” which was painted by Ferdinand Danton Sr., in 1877.
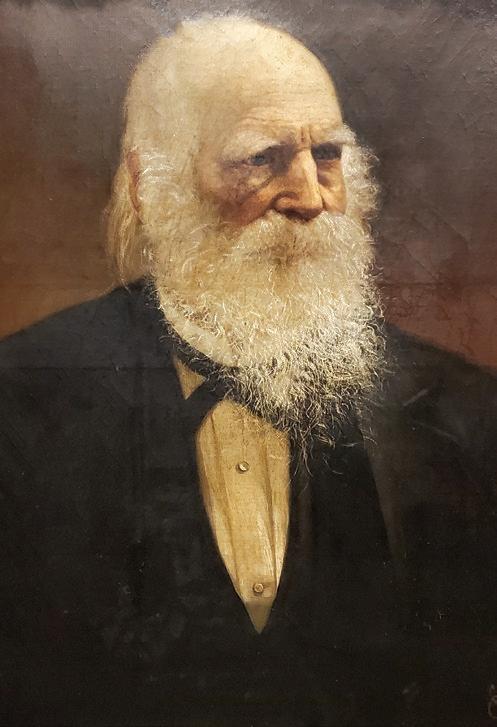
For the Period from July 1, 2021 through June 30, 2022
Thank you to all of our generous donors whose support is critical to the success of our students, faculty, researchers and the entire NYMC community.

The Chancellor’s Circle honors those who make a significant gift or commitment within a single year. In this Circle there are four Societies distinguished by the nature and size of contributions to the College.
This society is comprised of donors whose gifts and commitments are $50,000 or more.
Anonymous – 3
Cantigny Research Foundation, Inc.
Estate of Janice Kiss
Jonathan B. Gavras, M.D. ’86
Benjamin H. Homan Jr. Charitable Trust
Jonas Foundation
Mr. Howard Jonas
Munr Kazmir, M.D.
Annette E. Kussmaul, M.D. ’93
Mrs. Diane L. Levere
Mr. Juanili Lie and Mrs. Stephanie Artati
Ms. Tami Luhby
M.K. Foundation Inc.
Joseph P. Merlino, M.D. ’78, M.P.A.
Dr. and Mrs. Lawrence F. Neshiwat, M.D. ’88
Paul D. Ostrovsky, M.D. ’78
Mr. and Mrs. Vikram S. Pandit
Joseph and Penina Popack
Ammir S. Rabadi, M.D.
Mr. Stephen Rosenberg
Sarah Upham Trust
Anna M. Ward, M.D. ’85
This society is comprised of donors whose gifts and commitments are $25,000 to $49,999.
David E. Asprinio, M.D.
Mr. Gary Barnett and Mrs. Ayala Barnett
Ashoke K. Das, M.D., Ph.D.
Distinctive Maintenance Company
The Sidney E. Frank Foundation
Gary S. Gettenberg, M.D. ’83
Moshe E. Hirth, M.D. ’88
Russell S. Kamer, M.D.
Martin D. Keltz, M.D.
Lavie and Shterna Popack Family Foundation
Dr. Meryl Mark and Mr. Joseph Mark
Mr. Ruben Medina
Ms. Ellen-Jane Moss
New York Medical College Board of Advisors
Mr. and Mrs. Ronald F. Poe
Lee B. Pressler, M.D. ’90
Richard E. Rohr, M.D. ’80
Mr. Andrew Weissman
Westchester Medical Center
This society is comprised of donors whose gifts and commitments are $10,000 to $24,999.
Anonymous – 2
The Benevity Community Impact Fund
Berkowitz Family Giving Account
Frank Berkowitz, M.D. ’83
Boston Children’s Health Physicians
California Bank and Trust
Mr. Charles D. Casarella
The Children’s Dream Foundation
Eric I. Choe, M.D. ’88
Dr. and Mrs. Ben Chouake Confidence Foundation
Alan D. Dauer, M.D. ’62
Mr. Michel David-Weill + Mrs. Delores DelBello
Dira Realty
Estate of William F. Westlin III, Ph.D. ’89, M.S. ’87
Hawk Pointe Golf Club
Mr. and Mrs. Paul Ingrassia
Joan and Sanford I. Weill Medical College and Graduate School
Jinhee Kwak, M.D. ’99
Mr. Martin L. Leibowitz
Mr. Moshe Lichtenstein
Mr. Arthur Luxenberg
Frederick MacDowell Jr., M.D. ’53
Mr. Barry M. Menel
Stephen J. Nicholas, M.D. ’86
NYC Health + Hospitals/Metropolitan Pavarini Construction Company Inc. Physician Affiliate Group of New York
RC Solutions Inc.
Mr. and Mrs. Alan M. Reznik
Barry S. Robbins, M.D. ’73
Mrs. Jill J. Robertson-Li
Alan Rosenthal D.M.D.
Seize the Ribbon
Mr. Jordan E. Slone
Mark T. Thompson, M.D. ’71
Webster Bank
Robert A. Welke Cancer Research Foundation, Inc.
This society is comprised of donors whose gifts and commitments are $2,500 to $9,999.
Anonymous – 1
Mohan P. Abraham, M.D.
ACA Environmental Services, Inc.
Alpha Omega Alpha
Robert Alter, M.D.
Alumni Association of New York Medical College, Inc.
American Century Investments
Robert W. Amler, M.D., M.B.A., and Sherlita Amler, M.D.
Gladys M. Ayala, M.D., M.P.H.
Sudhamani R. Rao, M.D., and Sateesh C. Babu, M.D.
Robert A. Barish, M.D. ’79
Howard M. Baruch, M.D.
Michael J. Bronson, M.D. ’76
Alexander J. Brucker, M.D. ’72
Mrs. Joi Butler
Dr. and Mrs. Mitchell Cairo + Deceased
William J. Camera, C.P.A.
Phillip Capozzi Jr., M.D. ’96
Philip C. Caron, M.D. ’86
Shafi K. Choudhury, M.D., and Muhammad S. Choudhury, M.D.
Elliot Davidoff, M.D. ’71
Deloitte Foundation
Mr. Thomas A. DeRosa
John H. Derry, M.D. ’60
Mr. and Mrs. Franklin L. Earle
Sherry B. Ellis, M.D. ’85
John M. Feder, M.D. ’87
Noreen F. Bedini Ferrante, M.D. ’84
John P. Fezza, M.D. ’92
Kathleen Case Finzel, M.D. ’87
Eric C. Fok, M.D. ’93
Nancy J. Freeman, M.D. ’81
Mark J. Friedman, M.D. ’71
William H. Frishman, M.D.
Garfunkel Wild P.C.
Renee Garrick, M.D.
Harris J. Gelberg, M.D. ’73
Dr. Michael and Mrs. Judy Gewitz
Mrs. Jennifer Amler Goldstein
Arun Goyal, M.D. ’90
Karen E. Grimmell, M.D. ’61
Anita Grover, M.D. ’78
Thomas G. Harrington, M.D. ’91
Col. Paul B. Heller, M.D. ’68
Richard N. Hirsh, M.D. ’69
Mark Hurwitz M.D.
Mario A. Inchiosa Jr., Ph.D.
Mr. Edward J. Jacobson
Sumeet A. Kadakia, M.D. ’07
Dr. and Mrs. Alan Kadish
Martin S. Katzenstein, M.D. ’78
Jamieson D. Kennedy, M.D. ’59
KPMG LLP
Damien B. Lee, M.D. ’97
Dr. and Mrs. Zvi Lefkovitz
Mr. David Lichtenstein
Mr. Darrin Litsky
Jocelyn A. Luongo, M.D. ’06
Peter P. Ly, M.D. ’96
George D. Lyons, M.D. ’92
Hussein M. Matari, M.D.
Ms. Barbara McAdams
Eric L. McLaughlin, M.D. ’01
Mr. Peter R. Milani
Dr. and Mrs. Len Mitchell
Chitti R. Moorthy, M.D.
Tamara Moss, M.D. ’92
Eric Mustonen, M.D. ’75
Dr. and Mrs. Ronnie Myers
Jerry L. Nadler, M.D., MACP, FAHA, FACE NYC Health + Hospitals Corporation
Leonard J. Newman, M.D. ’70 and Randi Newman
Nextgen
Mrs. Ralph A. O’Connell
Reva and Martin Oliner
Mr. Michael Paris
Chong H. Park, M.D. ’96 Physician Office Based Surgery, PLLC
Mitchell Pincus, M.D. ’53
Barbara Pineda, M.D.
Scot C. Remick, M.D. ’82, F.A.C.P.
John T. Repke, M.D. ’78
Avi Retter, M.D.
Daniel Retter, Esq.
Adam D. Rubin, M.D. ’00 Ryco Fundraising LLC
Ms. Laura J. Sagerman
Saint Joseph’s Medical Center
Mr. Bruce J. Schanzer
Neil Schluger, M.D.
Schwab Charitable Fund
Pravinkumar B. Sehgal, M.D., Ph.D.
Jonathan A. Sheindlin, M.D. ’93
Sanford Sherman, M.D. ’56
The Sigmund Foundation
Brij M. Singh Ahluwalia, M.D.
Catherine B. Small, M.D. ’77
Barbara R. Sommer, M.D. ’79, and Alan Fisher, M.D.
Stifel Nicolaus & Company, Inc.
Richard K. Stone, M.D. ’68 +
Mr. Michael Sullivan
The Ernest and Marilyn Kussmaul Charitable Foundation Inc.
The Salon Family Foundation Inc.
Gigi Thomas, M.D.
Touro College of Dental Medicine at NYMC
Nancy N. Tsai, M.D.
United Healthcare Corporation
Sonia A. Velez, M.D., J.D.
Mr. Anthony Viceroy
John L. Vigorita, M.D. Memorial Fund
Vincent J. Vigorita, M.D. ’76
Mrs. Liyong Wei
David Werdegar, M.D. ’56
The Westchester Community Foundation

Westchester Radiation Medicine, PC WESTMED Medical Group

Dr. Patricia White and Mr. Daniel Flatley
Mr. Andrew Wiener
William J. Camera & Company
Robert M. Yacynych, M.D. ’88
David H. Young, M.D. ’72
Daniel Zelazny, M.D.
$1,000 to $2,499
Anonymous – 7
Ann Alexander, M.D. ’78
Michael S. Alexander, M.D. ’78
John A. Ambrose, M.D. ’72
Mr. Arthur Amler
Mr. and Mrs. James Amler
Mrs. Peggy Amler
Arthur S. Antler, M.D. ’75
Andrew N. Antoszyk, M.D. ’83
ARC
Gildy V. Babiera, M.D. ’91
Bank of America Corporation
Duncan J. Belcher, M.D. ’91
Dr. and Mrs. Francis L. Belloni
Stephen E. Borkow, M.D. ’63
Niel J. Borrelli, M.D. ’68
Joel I. Brenner, M.D. ’70
Buff City Soap
Howard S. Bush, M.D. ’82
Maria M. Torroella Carney, M.D. ’92
Mark J. Cerbone, M.D. ’84
Michael T. Charney, M.D. ’66
Mr. Bin Chen
Frank M. Chieu, M.D. ’71 and Barbara Chieu
Cigna HealthCare
Costanza Cocilovo, M.D. ’96
John A. Conway, M.D. ’71
Michael B. Corbett, M.D. ’61
Michel-Alexis R. Courtines, M.D. ’98
Elizabeth M. Craven, M.D. ’61 and Wales Craven, M.D. ’63
Michael J. Crupain, M.D. ’06
Ms. Virginia Davenport
Lauren N. Elliston, M.D. ’08
Christopher E. Emond, M.D. ’03
Aynalem Zemedeberhan, M.P.H. ’01 and Mill Etienne, M.D. ’02, M.P.H.
Emalie and John Feerick
Stephen Ferrando, M.D.
Burton M. Fink, M.D. ’71
Linda K. Friedman, Ph.D.
Steven M. Fruchtman, M.D. ’77
Chirag Gandhi M.D.
Rabbi Menachem Genack
Harvey A. Glasser, M.D. ’64
Grace Gorham, M.D. ’74
Stuart A. Green, M.D. ’67
Mr. and Mrs. Hugh Greenberg
David J. Gross, M.D. ’84 and Maria Gross

Edward C. Halperin, M.D., M.A.
Nancy Lee-Hata, M.D. ’02 and Justin T. Hata, M.D. ’02
Hi-Link Technology Group
Hinman Straub, P.C.
Peter Hoffmann, M.D. ’83
Steven H. Horowitz, M.D. ’66
Charlotte L. Tsai, M.D. ’01 and
Danny W. Hsia, M.D. ’01
Daniel Hwang, M.D. ’96
Humayun K. Islam, M.D., Ph.D. ’04
Johnson & Johnson Family of Companies
James W. Justice, M.D. ’58
Drs. Elisa and Steven Kadish
Uchenna P. Kalu, M.D. ’07
Kenigsberg-Blum Donation Fund
John Y. Kim, M.D. ’99
Mr. and Mrs. Sung-Hyun Kim
Jeffrey Kluger, M.D. ’71
Leonard B. Krich, M.D. ’65
Jonathan D. Kunis, M.D. ’82
Steven L. Lansman, M.D., Ph.D.
Mr. Han Lau
Robert F. Lautin, M.D. ’70
Lawless Family Fund
Thang Q. Le, M.D.
Dr. Edward and Renee Lebovics
LeChase Construction
Simon X. Lee, M.D.
Christopher S. Leonard, Ph.D.
Armand F. Leone, Jr., M.D. ’82
Jerry I. Levine, M.D. ’77
Norman Levine, Ph.D.
Mr. and Mrs. Paul H. Lewis
Walter M. Lewis, M.D. ’91
Naixi Li, M.D., Ph.D. ’98 and Xin Quan, M.D. Lion Medical PC
Peter J. Lucas, M.D. ’72
Tyler S. Lucas, M.D.
Vincent A. Lynch, M.D. ’67
Richard J. Macchia, M.D. ’69, F.A.C.S.
Robert F. Mackey, M.D. ’77
William W. MacLaughlin, M.D. ’81
Mr. Paul J. Maddon
Diane J. Madlon-Kay, M.D. ’79 and Richard C. Madlon-Kay, M.D. ’79
Ada M. Marin, M.D. ’83, M.P.H.
Mr. Franicis C. Marino
Norman L. Maron, M.D. ’70
Matthew & Tony General Landscaping, Inc.
William F. McCully Jr., M.D. ’57
Mrs. Judith McGreevy
James F. McGroarty, M.D. ’68
Peter P. McKellar, M.D. ’70
Robert J. McNamee, M.D. ’75
Ms. Caroline Mechanick
Brenda A. Merritt, M.D. ’65
Mr. and Mrs. Gideon Miller
Tracey A. Milligan M.D.
James L. Mills, M.D. ’73
Jeff T. Moise, M.D. ’99
George R. Monahan, M.D. ’57
Simone E. Mordas, M.D. ’91
Karen M. Murray, M.D. ’99
Mushroom Wisdom, Inc.
Aron Neuhaus, M.D. ’71
NYMC Office of Student Affairs
Elaine G. Pacicco, M.D. ’85 and Thomas J. Pacicco, M.D. ’85
Douglas E. Padgett, M.D. ’82
Patricia A. Galvin-Parton, M.D. ’80 and Lance A. Parton, M.D. ’80
James F. Passarelli, M.D. ’89
John T. Pellicone, M.D.
Myles L. Pensak, M.D. ’78
Alan E. Peters, M.D. ’79
Mr. John Piccione
Mrs. Margaret A. Pierce
Stephanie L. Pollack, M.D. ’14
Renaissance Charitable Foundation for Modern Giving

Charles R. Rich, M.D. ’74
Renee Z. Rinaldi, M.D. ’76
Robert & Brenda Fischbein Donor Advised Fund
Kenneth M. Rose, M.D. ’88
Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
Jose H. Santos, M.D. ’82
Theodore J. Schmahai, Ph.D. ’88
Mr. and Mrs. Michael Schwartz
S. Richard Scuderi, M.D. ’61
John H. Seward, M.D. ’61
John P. Sheehy, M.D. ’75
Win Shen, M.D. ’83
David E. Silverstone, M.D. ’73
Michael C. Smith, M.D. ’12
Lori Solomon, M.D. ’99, M.P.H. ’09
Jonathan E. Sonne, M.D. ’98
Anthony M. Sozzo, M.A., M.S.Ed.
Neil Spielsinger, M.D.
Frederick Steinberg, M.D. ’58
Michael S. Stewart, M.D.
Kenneth B. Strumpf, M.D. ’82
Stryker
Yongsook V. Suh, M.D. ’90
Sungja Kim
Synergen Health LLC
Patricia Tager, M.D. ’98
Mariko L. Ishimori, M.D. ’00 and Nicholas Testa, M.D. ’01
TIAA-CREF
Mr. Hiroshi Toyoda
Subhash Virani, M.D. ’95
Susan L. Vogel, M.D. ’76
Mr. Mark Weber
Steven Weinstock, M.D. ’74
Welch Family Charitable Fund
David Wellman, M.D.
Douglas N. Whatmore, M.D. ’77
Philip Wong, M.D. ’96
Mr. Douglas L. York, M.P.H. ’91
Richard J. Zeman, Ph.D.
$250 to $999
Anonymous – 14
LA Plus Technology & Security Solutions
A.J. Indusi Plumbing and Heating, Inc.
Peter J Acker, M.D.
Ms. Basilia Adams
Lori H. Adcock, M.D. ’85
Dr. Chisara Adonai
ADT Security Services
Naomi R. Ham, M.D. ’84 and Elmer
C. Agustin, M.D., M.P.H. ’15
Geraldine L. Ahneman, M.D. ’67
Judith C. Ahronheim, M.D.
Robert Aledort, M.D.
Salomon Amar, D.D.S., Ph.D.
David R. Andrews, M.D. ’78
Mr. Kerrin Antommarchi
Ms. Ingrid C. Armstrong, M.S. ’01
Marie T. Ascher, M.S., M.P.H.
Sanford H. Auerbach, M.D. ’75
Haroutiun C. Avedissian, M.D.
Mark R. Axelrod, M.D. ’79
Deepak Azad, M.D., M.P.H. ’89
Charles J. Bacall, M.D. ’75
Stephanie C. Barnhart, M.D. ’08, M.P.H ’08
Patricia A. Barry, M.D. ’83 and John M. Cosgrove, M.D. ’83, F.A.C.S.
Robert S. Bartolomeo, M.D. ’71
Christine H. Beck, M.D. ’77
William J. Behrje, M.D. ’65
David A. Berkowitz, M.D. ’63
Black Rock
Blackbaud Giving Fund
Robert V. Blake, M.D. ’75
Peter Bloom Jr., M.D. ’04, M.S. ’00
Devon E. Bock, M.D. ’86
Lisa C. Bogdonoff, M.D. ’88
Jason S. Bonslaver, M.D. ’06
Nicholas G. Bonvicino, M.D. ’79
Jeffrey R. Boscamp, M.D. ’81
Michael D. Brandler, M.D. ’98
Tonya M. Brown-Price, M.D. ’90
Jack Bruder, M.D. ’82
Earl A. Bueno, M.D. ’00
Jerome M. Burke, M.D. ’84
Paul D. Burrows, M.D. ’88
Mr. Randal D. Byrd
C. A. Ronan & Co., Inc.
Joseph J. Calandra, M.D. ’82
Joseph A. Camilleri Jr., M.D. ’85
Howard D. Cantwell, M.D. ’65
Care Security Systems, Inc.

Joseph E. Cerbone, M.D. ’82
Christopher T. Channon, M.D. ’76
Burawit B. Charuworn, M.D. ’99
Hee-Joo Cheon-Schingo, M.D. ’92 and Victor A. Schingo, M.D. ’92, F.A.C.S.
William J. Chernack, M.D. ’70
Richard J. Chernick, M.D. ’91
Qwie T. Chew, M.D. ’65
Max Chorowski, M.D. ’75
Christian L. Martos Engineering PLLC
Alfonso P. Ciarlo, M.D. ’65 City Orthopaedics PLLC
Elizabeth M. Clark, M.D. ’85
Alan J. Conrad, M.D. ’81, MMM, CPE, FACHE, FAAPL
Arthur Cooper, M.D.
Martin A. Cooper, M.D. ’63
Ms. and Mr. Anthony Corvini
Mrs. Irene Crasto-Bolin
Dustin Cummings, M.D.
Alton L. Curtis, M.D. ’69
Scott B. Cutler, M.D. ’77
Mr. Larry David
Robert A. Davis, M.D. ’74
John J. Degliuomini, M.D. ’93
Susan Q. DeJoy, M.S. ’94
Depuy Synthes Trauma
M. Sheila Desmond, M.D. ’75
Dominick F. DiFabio, M.D. ’71
Wendy Dolcetti Kaye, M.D. ’77
Bram A. Dolcourt, M.D. ’04
Gary D. Dunn, M.D. ’90
E M Winters Financial Services Inc.
Thomas J. Early, M.D. ’73
Economic Concepts, Inc.
Joseph G. Edelson, M.D. ’78 Edison Ophthalmology Associates LLC
Elsevier
Victor G. Ettinger, M.D. ’67
John C. Evanko, M.D. ’95
Christine M. Fanning, M.D. ’11
Michael J. Feinstein, M.D. ’64
Robert R. Flanagan, M.D. ’75
Susan Fox, M.Ed., M.A., Ph.D.
Dariana Francois, M.D. ’07
Denis J. Frank, M.D. ’71
Martin J. Frank, M.D. ’70 +
Sarise Freiman, M.D. ’76
Mr. Daniel Frenkel
Deborah Fried, M.D. ’83
Richard A. Frieden, M.D. ’84
Bruce I. Friedman, M.D. ’79
The Fuller Foundation
Col. Roger A. Gallup, M.D. ’91
Robert I. Gelb, M.D. ’80
Mr. David George
Matthew J. Geswell, M.D. ’15
Kendra G. Gil, M.D. ’04 and Eric A. Gil, M.D. ’03
Glenn D. Gilmor, M.D. ’86
Jeffrey B. Ginsburg, M.D. ’92
Give Lively Foundation Inc.
Mr. Paul Glasser
Mr. Thomas Gleason
Albert C. Goldberg, M.D. ’63
Barry S. Goldberg, M.D. ’95
David A. Goldenberg, M.D. ’74
Mr. and Mrs. Bert Goldfinger
Laurence D. Goldstein, M.D. ’84
Michael S. Goldstein, M.D. ’72
Paul Goldstein, M.D. ’71
Golf 18
Michael S. Goligorsky, M.D., Ph.D.
Angela E. Gonzalez, M.D. ’94
Virginia A. Gortych-Barnes, M.D. ’87
Jill A. Gradner, M.D. ’94
Patrick V. Graham, M.D. ’77
Adrienne R. Greenlaw, M.D. ’91
David N. Greenman, D.D.S., M.P.H. ’07
Richard H. Greif, M.D. ’75
Martin A. Gross, M.D. ’81
Daniel S. Haddad, M.D. ’83
Adam Hammerman, M.B.A.
Timur Hanan, M.D. ’06
Gregory P. Harvey, M.D. ’83
John J. Healy, M.D. ’63 +
James C. Hegarty, M.D. ’62
Edward R. Heilman, M.D. ’74
Robert Herenstein, M.D., P.C.
Robert M. Herenstein, M.D. ’85
Zhishan Huang, Ph.D. ’05 and Qianxu Guo, M.D., M.S. ’08
John T. Hughes, M.D. ’82
Kelly A. Hutcheson, M.D.
Dr. Lee J. Isabell
Sei Iwai, M.D.
Jason T. Jacobson, M.D.
Mokarram H. Jafri, M.D. ’94
Janus Henderson Investors
Surinder P. Jindal, M.D.
Benjamin F. Johnson, Ed.D.
Sharon Jordan and Edward F. Jordan, M.D. ’72
Frank T. Jordan, M.D. ’71
Lila Kagedan, M.Ed.
Fran E. Kaiser, M.D. ’74
Lawrence S. Kaminsky, M.D. ’78
Kye S. K. Kang, M.D. ’94
Umashankkar Kannan, M.D.
Emily R. Kaplan, D.Ph. ’21
Harvey S. Kaplan, M.D. ’63
Norman R. Kaplan, M.D. ’77
Mr. Seymour Kaplan
Elizabeth M. Kass, M.D. ’88
Kenneth G. Kasses, Ph.D. ’74
Ernest Katz, M.D. ’78
Gurmeen Kaur, M.D.
Garabed O. Kayekjian, M.D. ’94
Kings Harbor Multicare Center Mark Kittleson, Ph.D., MCHES®, FAAHB, FAAHE
Jennifer Koestler, M.D.
Jonathan J. Kramer, M.D. ’83
Mitchell S. Kramer, M.D. ’85
Edward R. Herman, M.D. ’82
L. S. Herman, M.D. ’74
Hilary I. Hertan, M.D. ’82
Robert A. Herzlinger, M.D. ’69
Emile M. Hiesiger, M.D. ’78
Marina K. Holz, Ph.D.
Mr. and Mrs. William B. Hopkins
Rivka S. Horowitz, M.D. ’78, Ph.D.
Stephen K. Hoverman, M.D. ’78
Mr. James A. Kraus
Mark A. Krich, M.D. ’97
Rabbi and Mrs. Moshe D. Krupka, M.S.
Kenneth A. Krutt, M.D. ’84
Ms. Christeena Kurian
Mr. Rocco Labella
Timothy L. Lacy, M.D. ’00
Edmund F. La Gamma, M.D. ’76
Lawrence and Margie Kaminsky Donor Fund

Singh A. Boun, M.D. and Nick Lee, M.D., P.C.

Benjamin Lee, M.D.
Nick H. Lee, M.D. ’95
Louis H. Lefkowitz, M.D. ’64, FACOG, FACS
Peter W. Lementowski, M.D. ’06
Jesse A. Levin, M.D. ’09
Robert H. Leviton, M.D., M.P.H.
John A. Lewis, M.D. ’93
Dr. and Mrs. Lawrence A. Lewis
Jin Li, M.D., Ph.D. ’01 and Gary Guo, M.D., Ph.D.
Leslie LiDonnici, M.D. ’78
Joan P. Liman, M.D. ’83, M.P.H. ’93
Richard L. Lindenbaum, M.D. ’72
Delong Liu, M.D. and Min Xu, M.D.
Mr. John Loike
Charles Lomanto, M.D. ’63
Richard A. Losada, M.D. ’83
Pamela Ludmer, M.D.
Carl B. Lundborg, M.D. ’67
Mr. Brett Lynch
Heather D. Johnson, M.D. ’02 and John P. Magnan, M.D. ’02
Michael J. Majsak, P.T., Ed.D.
Craig W. Markert, M.D. ’73
Alan B. Marks, M.D. ’78
Jon O. Marks, M.D. ’76
Stephen J. Marks, M.D. ’80
William E. Marshall, Ph.D.
Lawrence R. Marwill, M.D. ’63
Maspeth Federal Bank
Jeffrey S. Matican, M.D. ’82
Mr. Ronald Matten
Mr. Roger E. Mayer
Gale Mays
Joseph R. Mazzaglia, M.D. ’71
James T. Mazzara, M.D. ’63
Rebecca A. McAteer, M.D. ’08
Georgeann McGuinness, M.D. ’85
George R. McKendall, M.D. ’84
Camille A. McPherson, M.D. ’03
Barry A. Meisel, M.D. ’70
Jay A. Meisel, M.D. ’93
Martin K. Melman, M.D. ’74
Morton Meltzer, M.D. ’65
John H. Mensher, M.D. ’67
Mercer Health & Benefits LLC
Ms. Deena Merzel
Edward J. Messina, Ph.D. ’73
Bruce A. Miller, M.D. ’67
William Edward Miller, M.D. ’76
Yair Miller, M.D. ’22
Michael A. Miranda, M.D. ’92
Marisa Montecalvo, M.D.
Alan H. Morelli, M.D. ’82
Morgan Stanley
Elliott F. Morse, M.D. ’67
Augustine L. Moscatello, M.D.
Kimberly L. Motta, M.D. ’97
Andrew M. Murphy, M.D. ’78
Ms. Megan Narron
Mohsen Nasir, M.D. ’06
Kathleen G. Nelson, M.D. ’71
Lysa N. Nguyen, M.D. ’01
Tuan T. Nguyen, M.D. ’06
Kelly A. Siano, M.D. ’11
John J. Novello, M.D. ’76
NY Physical Therapy Association Inc.
John D. O’Brien, M.D. ’60
Mr. and Mrs. Chistopher M. Ogorzalek
Yetunde Olowe, M.D.
Omega Environmental Services, Inc.
Guy R. Orangio, M.D. ’79 and Mrs. Patricia Orangio
Geralyn A. U. O’Reilly, M.D. ’94 and Keith J. O’Reilly, M.D. ’94
John C. Park, M.D.
Derek K. Paul, M.D. ’91
Mr. and Mrs. Bruce Pauls
Performance Consultants LLC
Rachel A. Perla, M.D. ’95
Ms. Lori Ann Perrault
John R. Person, M.D. ’73
Joanna C. Pessolano, M.D. ’81
V. Rachel Phillips, M.D. ’79
Mrs. Teletta A. Piper
Joseph W. Placer, M.D. ’64
Jane M. Ponterio, M.D. ’81
John M. Powers, M.D. ’77
Glenn M. Preminger, M.D. ’77
Mr. Eugene S. Putko
Putnam Physical Medicine & Rehabilitation PC

Ms. Nicole M. Raia
Laurence M. Raiford, M.D. ’77
Venkat Ramani, M.D.
Kishore N. Ranade, M.D.
Kathleen R. Reilly Fallon, M.D.
Margaret A. Reilly, Ph.D. ’81, M.S. ’78
Anne Negrin Reis, M.D. ’02
Elisabeth J. Wilder Richards, M.D. ’91
Seth J. Richter, M.D. ’94
Riebling Wealth Strategies LLC
Rodney T. Riedel, M.D. ’01
River Run Partners
James P. Roach, M.D. ’58
Ellen M. Rooney, M.D. ’83
Nancy C. Rose, M.D. ’84 and
G. Marc Jackson, M.D.
William B. Rosenblatt, M.D. ’73
James E. Rosenthal, M.D. ’74
Kathleen M. Rossy, M.D.
Andrew J. Roth, M.D. ’88
Rotundo Plumbing Corp
The Terri & Matty Russo Fund
Stephen D. Ryan, M.D. ’90
Sandra L. Sacks, D.D.S., M.D. ’97 and
Harry G. Sacks, D.D.S., J.D.
Safari Solutions Inc.
Scott R. Saffran, M.D. ’87
Jennifer Taylor Salcman, M.D. ’05
Ms. Lori Sandler
Juan S. Sandoval, M.D.
Sani-Pro Disposal Services, Inc.
Debjeet Sarkar, M.D. ’05
Donald E. Sawyer, M.D. ’70
Mrs. Anne E. Schneider
Dr. Jason and the Honorable Lois Tanzer
Maureen Matturri, M.D. ’66
The David Foundation Inc.
The Pureganic Cafe
Mr. and Mrs. Kenneth Theobalds
Yvonne S. Thornton, M.D.
Raj K. Tiwari, Ph.D.
Christopher A. Tormey, M.D. ’04
Oya Tugal, M.D. ’86
Ms. Rachana Tyagi
Edward S. Valentine, M.D. ’78
Valley National Bank
Scott K. Varland, D.D.S. ’08
Pierre A. Vauthy, M.D. ’72
Henry Velez, M.D. ’76
Robert Schneider, M.D. ’69
Eric H. Schultheis, M.D. ’88
Schultz Eye Clinic
Gerald R. Schultz, M.D. ’63
Jerold Schwartz, M.D. ’56
Michal Schwartzman, Ph.D.
David F. Sciortino, M.D.
William H. Scragg Jr., M.D. ’57 +
Deborah A. Shapiro, M.D. ’89 and
Alan R. Plumer, M.D. ’88
Bruce E. Sherling, M.D. ’73
Tighe P. Shomer, M.D. ’77
Sarah S. Silver, M.D. ’97
Marc Silverman, M.D.
Stacey A. Simons, M.D. ’06
Avtar Singh, M.D.
David L. Smith, M.D. ’61
Ms. Stacy Solow
John C. Somberg, M.D. ’74
Kathryn Spanknebel, M.D.
Specialty Orthopaedics
David J. States, M.D. ’53
David A. Stein, M.D. ’75
Ms. Mary Stein
John T. Stinson, M.D. ’75
Howard L. Sussman, M.D. ’84
Ross H. Taff, M.D. ’74
Marvin B. Tankel, M.D. ’80
Jack H. Vitenson, M.D. ’65
Adrianna Vlachos, M.D. ’86
James A. Walker, M.D. ’61
Joseph P. Walker, M.D. ’74
Marc K. Wallack, M.D.
Thomas G. Webber, M.D. ’73
William R. Weissman, M.D. ’65
Westchester Marriott
Westchester Wine
Milton White, M.D. ’93
Barry R. Witt, M.D. ’84
Raymond F. Wong, M.D.
Richard B. Wu, M.D. ’05
Stephanie M. Wyckoff, M.D. ’97
Dr. Wen Xiong, M.S. ’01
Dr. and Mrs. Vincent J. Yakavonis ’77
Aaron E. Yancoskie, D.D.S.
Zhaohui Yang, M.D.
Gerald W. Zaidman, M.D.
Judith W. Zander, M.D. ’80
Donna A. Zeide, M.D. ’83
Michael Shaochun Zhang, M.D., M.S. ’00
$100 to $249
Anonymous – 20
Faheem A. Abbasi, M.D.
Dianne S. Acuna, M.D. ’92
Barbara S. Akresh, M.D. ’75
Leonard H. Alberts, M.D. ’72
Olivia O. Alegre-Ipanag, M.D.
Norah N. Alruwaili, M.D.
Alan R. Altman, M.D. ’71
Karel R. Amaranth, M.P.H. ’10
Abdel F. Amin, M.D. ’97
Sheba V. Ampalloor, M.D. ’94
Anurag K. Anand, M.D. ’01
Anne R. Mullin, M.D. ’87
Firdose S. Ansari, M.D. ’05
Robert and Amy Ansehl, R.N., D.N.P., FNP-BC

Linda Antillon, M.S. ’05
Matthew J. Arduino, Dr.P.H., M.S. ’81
Ronald L. Arenson, M.D. ’70
Adriane L. Argenio, M.D. ’13
Arise Physical Therapy PLLC
Daniel Z. Aronzon, M.D. ’73
Romain Athus, M.D.
Howard A. Babus, M.D. ’75
Albert J. Bajohr Jr., M.D. ’67
Kenneth S. Bannerman, M.D. ’75
Ms. Nicole Barsamian
Mark A. Bartolozzi, M.D. ’87
Paul G. Battaglia, M.D. ’84
Harold C. Bautista, M.D. ’86
Barbara R. Bellar, M.D., J.D., M.A., M.P.H., M.Div
Cheryl-Lisa R. Bennett, M.D. ’94
George W. Benninger, M.D. ’66
Roseanne C. Berger, M.D. ’77
Basil G. Bernstein, M.D. ’67
Daniel Berson, M.D. ’69
Mrs. Carol Binen
Rima A. Bishar, M.D. ’14
Jeffrey S. Bisker, M.D. ’76
Rajesh Bisnauth, M.D. ’96
Phyllis S. Blacharsh, M.D. ’88
Edward J. Bloch, M.D. ’69
Peter N. Bogdan, M.D. ’64
Ms. Stefania Bonanni
Thomas J. Borelli, Ph.D. ’85
Zakia D. Bowen, M.D.
Mr. and Mrs. Percy R. Bracamonte
Stephen M. Brenner, M.D. ’62
Ronald D. Brooksher, M.D. ’86
David J. Broza, M.D. ’89
Dr. Geny B. Burgos ’90
Liboria Buscemi, M.D. ’96
Felipe C. Cabello, M.D.
Norman A. Cagin, M.D. ’67
Dr. and Mrs. Ronald Caldwell
Michael Campion, M.D. ’82
Maria F. Capparelli, M.D. ’07
Mrs. Tina Cardoza-Izquierdo
Claire J. Carlo, M.D. ’85
Francis X. Carmody, M.D. ’63
Dahlia T. Carr, M.D. ’01
Dana R. Deravin Carr, Dr.P.H. ’13, M.P.H. ’01
Paul F. Carroll, M.D. ’92
James E. Carter, M.D. ’55
Paul S. Carton, M.D. ’63, FACS
Deena Costanza Casiero, M.D. ’06
Carl M. Cassin, M.D. ’59
Joseph P. Castellano, M.D. ’75 and Heather C. McKee, M.D.
Mark Catterall, M.D. ’96
Joseph S. Cervia, M.D. ’84 and Denise L. Blumberg, M.D.
Ms. Ying N. Chan
Paul B. Chaplin, M.D. ’79
A. Roger Chappelka, M.D., FACP, FACOEM
Michael Chavez Chase, M.D. ’72
Anthony P. Chatowsky, M.D. ’62
Ms. Bess Chazhur
Cynthia Chazotte, M.D. ’81
Mr. and Mrs. Henry Chew
Evelyne N. Chiakpo, M.D. ’00
Dr. and Mrs. Joseph Chiaramonte
Neil T. Choplin, M.D. ’76
Ena Chow-Bell, M.D. ’94 and Gregory D. Bell, M.D. ’93
Yun Shin Chun, M.D. ’00
Karen Ann Clarke, M.D. ’96, M.P.H. ’94, M.S. ’93
Bruce M. Cohn, M.P.H. ’09
Dr. and Mrs. Wayne A. Colizza, M.D. ’17
Lionel A. Cone, M.D. ’74
Congregation Adath Jeshrun

Sheila J. Conklin, M.P.H. ’00
Alan F. Cooper, M.P.H. ’91
Marina J. Corines, M.D., ’18
William F. Courter Jr., M.D. ’74
Robert S. Crupi, M.D. ’83
Imelda Cruz-Banting, M.D.
Gerard P. Curran, M.D. ’95
Mr. James Curran
Rachel Cyrlak, M.D. ’81
Arthur S. Cytryn, M.D. ’77
Brian G. Daggett, M.D. ’80
Terrance M. Daino, M.D. ’90
Mr. and Mrs. Peter M. Dale
Christina M. Damo, M.S. ’10
Marc D. Danziger, M.D. ’92
Lorelei S. Davidson, M.D. ’91
Dayton Foundation Depository Inc.
Barry J. Decker, M.D. ’82
Vincent P. DeGennaro, M.D. ’85
Thomas J. Degnan, M.D. ’56
Kevin C. Delahanty, M.D. ’84
Robert V. DeMartini, M.D. ’87
David M. Denmark, M.D. ’05
Katherine A. Dent, M.D. ’77
Vipul Desai, M.D. ’06
Janis DiPietro, M.D. ’79
Earl M. DiPirro, M.D. ’61
Jayne M. Doherty, M.D. ’86
Mr. and Mrs. David Domreis
Floyd J. Donahue, M.D. ’60
Gary R. Donshik, M.D. ’66
Spencer R. Downs, M.D. ’58
William F. Doyle, M.D. ’62
Allen J. Dozor, M.D. ’80
Elizabeth D. Drugge, Ph.D., M.P.H. ’12
Stuart M. DuBoff, M.D. ’69
Elizabeth S. Ehrlich, M.D. ’02
Eli Lilly US and Company
Andrew A. Elimian, M.D.
Benedicta E. Emerhi, M.S. ’02
Letty Emery, M.D.
Jaleh Z. Eslami-Borsody, M.D. ’94
Mr. Finn Estep
Mr. and Mrs. Robert S. Faircloth
Allen Fay, M.D. ’61
Mrs. Barbara Feinstein
Jennifer A. Feldman, M.D. ’07
Dr. and Mrs. William N. Fenney, M.D. ’79
Craig Allen Fenton, M.D. ’68
Robert S. Ferretti, M.D. ’65
Alex E. Fijman, M.D. ’00
Morris C. Finkelstein, M.D. ’85, Ph.D.
Joel G. Fischgrund, M.D. ’78
Felicity G. L. Fishman, M.D. ’06
Martin H. Floch, M.D. ’56
Richard J. Fogler, M.D. ’68
A. P. Fontanetta, M.D. ’73
Dr. and Mrs. Henry E. Fourcade
Steve M. Frank, M.D. ’73
Matthew C. Frankel, M.D. ’78
James T. Friedland M.D.
Dr. and Mrs. Bruce J. Friedman ’76
Steven I. Friedman, M.D. ’76
Mr. Steven J. Friedman
James A. Fugazzi, M.D. ’00
Heidi N. Fusco, M.D. ’08
Francis S. Gagliardi, M.D. ’70
Ian A. Gale, M.D. ’70
Donna M. Gallagher, M.D. ’89
Gary A. Gallo, M.D. ’63
Thresia B. Gambon, M.D. ’94
Veena S. Gangasani, M.D.
Carol A. Garbarino, M.D. ’79
Margaret M. Gennaro, M.D. ’87
Ms. Camille Georgaros
Mina A. Gillers, M.D. ’73 and Bruce J. Gillers, M.D. ’73
Scott A. Glasser, M.D. ’86
William Glatt, M.D. ’64
Edward H. Glenn, M.D. ’64
Ira D. Glick, M.D. ’61
Kenneth H. Goldblatt, M.D. ’72
Bruce Goldfeder, M.D. ’92
Mrs. Rita Gonshorek
Juan P. Gonzalez, M.D. ’94
Ms. Beth Gorin
Michael S. Graham, M.D. ’07
Laurie Grant, M.D. ’83
Henry J. Green, M.D. ’75
Robert D. Green, M.D. ’61
Craig A. Grimes, M.D. ’96
Danielle Breitman Groves, M.D. ’00
Rosemarie Cantor Guercia, M.D. ’50
Bonnie and Paul Heindl
Hal Gutstein, M.D.
Irwin Hametz, M.D. ’73
Robert A. Harwood, M.D. ’62
Edward F. Hassan, M.D. ’84
F. Whiting Hays, M.D. ’60
William A. Healy Jr., M.D. ’61
Craig R. Heim, M.D. ’70
Leo A. Heitlinger, M.D. ’78
Stephen L. Hermele, M.D. ’68
Neil R. Hirsch, M.D. ’73
Robert D. Hirsch, M.D. ’61
Barbara M. Hisler, M.D. ’83
Martin N. Hochberg, M.D. ’63

Robert C. Holland, M.D. ’84
Ronald Hoogmoed, M.D.
John S. Hou, M.D. ’97
Anna Hsieh, M.D. ’00
Eric L. Hsu, M.D. ’97
Hudson Valley Association of Physicians From India Inc.
Magdalen E. Hull, M.D. ’79, M.P.H.
Cathy J. Jarosz, M.D. ’87
Vanessa L. Jeffers, M.D. ’89
Susan M. Jensen, M.D. ’77
Meena Jhanwar-Uniyal, Ph.D.
Erica C. Jones, M.D. ’92
Mrs. Marie Pinto Jones
Linda F. Lazar, M.D. and
Rande H. Lazar, M.D.
Sheryl L. Leff, M.D. ’85
Stuart D. Lestch, M.D. ’66
Elliot M. Levine, M.D. ’91
Peter D. Levit, M.D. ’76
David C. Lewandowski, M.D. ’15
Boyi Li, M.D.
George Liakeas, M.D.
Mr. and Mrs. Sheon Sang Liao
Harold M. Libatter, M.D. ’80
Michele Libonati, M.S. ’91
Mr. Jonathan Lichter
Robert B. Lim, M.D. ’96
Janet C. Lin-Torre, M.D. ’85
Donna J. Lombardi-Goldfus, M.D. ’93
Milton L. Lorig, M.D. ’77
Ellen Loughran, Ph.D.
Thomas Lu, M.D. ’96
Djoser M. Mack, M.D. ’21
Mr. Robert Madden
Catherine C. Labiak-Maher, M.D. ’82 and James O. Maher, III, M.D. ’82
Andrea G. Maitlin-Katz, M.D. ’88
Mrs. Lynne Maidman Manning
Carl M. Marchetti, M.D. ’60
Richard A. Marcucci, M.D. ’72
Stephen H. Marcus, M.D. ’67
Clifford L. Marshall, M.D. ’77
Marvin A. Roth, M.D., P.A.
Mary Kay Inc.
Harvey G. Masor, M.D. ’65
Samuel D. Kahnowitz, M.D. ’76
Ellen M. Kaplan, M.P.H. ’98
Mrs. Doris Katz
Ms. Susan R. Katz
F. R. Kellogg, M.D. ’74
Jennifer J. Halstead-Kenny, M.D. ’02 and John M. Kenny, M.D. ’01
Mohammed Khan M.D.
Kathleen M. Kicsak-Baumgartner, M.D. ’91
Robert Kirschner, M.D. ’61
William S. Knight, M.D. ’91
Mr. and Mrs. Gary Koellhoffer
Foula C. Kontonicolas, M.D. ’09
Richard S. Kornbluth, M.D. ’75, Ph.D.
Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64
Jonathan S. Kusnitz, M.D. ’84
Roxane E. Lacy, M.D. ’99
Vincent S. LaDelia, M.D. ’82
Hoang M. Lai, M.D. ’03
Laiken Associates Inc.
Michael L. Lapkin, M.D. ’65
Jeffrey M. Laskoff, M.D. ’68
George E. Laubach, M.D. ’63
Massage Envy
Baturu Mboge, M.P.H. ’15
Scot G. McAfee, M.D. ’97
Edward J. McCartin Jr., M.D. ’63
Alan D. McClelland, M.D. ’79
Peter J. McLoughlin, M.D. ’58
Mrs. Rande McMillan
Roxane Lacy, M.D.
Rakesh K. Mehta, M.D.
Keith P. Meslin, M.D. ’99
Steven D. Mills, M.D. ’99
Gudrun E. Mirick Mueller, M.D. ’06
Parvaneh Modaber, M.D. ’62
Mr. Thomas Modero
Gustavo S. Montana
James P. Mooney, M.D. ’56
Dan K. Morhaim, M.D. ’75
Muriel A. Gold Morris, M.D. ’66
Michelle A. Multz, M.D. ’87
Mr. and Mrs. Mitchell A. Mund
James J. Murdocco, M.D. ’65
Kenneth E. Murdock, M.D. ’68
Margaret Mackin Nally, M.D. ’08
Sudha Narasimhan, M.D., M.P.H. ’99
Mrs. Barbara Nash
Martin S. Neff, M.D. ’63
Mario Nelson, M.D.
Mr. George F. Nestler
The Samuel Newman Charitable
Foundation
Mrs. Jane Newman
Dr. Amy N. Nguyen, ’01
Jack D. Norman, M.D. ’63
Sofia Novak, M.D. ’07
Genevieve N. Nwigwe, M.D., G.M.E. ’09
M. Kevin O’Connor, M.D. ’68
Sophia G. O’Donnell, M.D. ’08 and Seth W. O’Donnell, M.D. ’08
Oladapo Odumosu, M.D.
Carlos L. Omenaca, M.D.
Edward Orff, Ph.D. ’99
George W. O’Rourke, M.D. ’61
Mr. and Mrs. Robert P. Osler
Alan J. Ostrowe, M.D. ’66
Otolaryngology Consultants of Memphis

Christopher J. Pappas, Ph.D. ’11, M.S. ’06
Janis A. Pastena, M.D., M.P.H. ’09
Kenneth I. Pataki, M.D. ’70
Mr. and Mrs. Theodore Pavlovitch
Stephanie M. Peduto, M.D. ’92
Fern L. Perlman, M.D. ’75
Lee J. Phillips, M.D. ’85
Harold B. Pinkofsky, M.D. ’89
Dahlia M. Plummer-Barksdale, M.D.
Pneuma Foundation
Jay H. Polokoff, M.D. ’82
Mrs. Marianne C. Portway
Bernard J. Powers, M.D. ’76
Radian Group Inc.
Barry Raff, M.D. ’77, FACC
Alfred B. Randall, M.D. ’70
Douglas A. Rayner, M.D. ’61
Harvey A. Reback, M.D. ’61
Regintex Insurance Brokerage
Harold Reikes, M.D. ’57
Padraic B. Reynolds, M.P.H. ’14
Beverly L. Richman, M.D. ’64
Robert J. Rienzo, M.D. ’75
James E. Rogers, M.D. ’77
Reuben D. Rohn, M.D. ’71
Nancy Roistacher, M.D. ’75
Mr. and Mrs. Claude Rollin
Diane P. Romsaitong, M.D. ’95 and Panus Romsaitong, M.D. ’94
James J. Rooney, M.D. ’74
Eric R. Rosenberg, M.D. ’75
Howard D. Rosenberg, M.D. ’76
Stuart A. Rosenthal, M.D. ’62
Jason E. Roth, M.D. ’98
Malcolm Z. Roth, M.D. ’82
Marvin A. Roth, M.D. ’62
Ronald R. Roth, M.D. ’73
Mrs. Lisa Rubenfield
William Rymer, M.D. ’72
Tabassum Saba, M.D., M.S. ’94
Naghmeh Salamat Saberi, M.D. ’98
Jerome E. Sag, M.D. ’72
Nicholas G. Sakellariou, M.D. ’94
Michael A. Sanford, M.D. ’94
Robert S. Sanford, M.D. ’64
Srivilliputtur G. Santhana Krishnan, M.D.
Albert K. Sassoon, M.D. ’81, M.P.H.
Mr. Brian J. Savarese
Amit Saxena, M.D. ’06
Umer Sayeed Sayeed-Shah, M.D. ’96
James T. Sayre, M.D. ’75
Meri Schachter, M.D. ’69
Neil R. Scheier, M.D. ’85
Janet A. Schneller, M.D. ’79
Michael B. Schoenwald, M.D. ’69
Melvin L. Schulman, M.D. ’65
Richard D. Schultz, M.D. ’88
David Schwalb, M.D. ’84
Jonathan Schwartz, M.D. ’64
Barry J. Sell, M.D. ’71
Denise B. Sepe, M.D. ’83 and Carl J. Koenigsmann, M.D. ’84
Kerian V. Service, M.D. ’08
Russell A. Settipane, M.D. ’84
Mrs. Susan Shimer
Jeff S. Silber, M.D. ’95
Deren M. Sinkowitz, M.D. ’83
Adam C. Sischy, M.D. ’07
Victor S. Sloan, M.D. ’89 and Sandra Gong
John E. Smith Jr., M.D.
Brian K. Solow, M.D. ’82
Faye E. Spector, M.D. ’79
Carl L. Speizer, M.D. ’83
Lawrence M. Spergel, M.D. ’71
Peter H. Stein, M.D. ’09
Mr. Mark Steinberger
Marc A. Stiefel, M.D. ’01
James V. Stillerman, M.D. ’77
Mr. and Mrs. David A. Stutzman
Viktor P. Sulkowski, M.D. ’71
Mark H. Swartz, M.D.
Edward T. Swibinski, M.D. ’75
Ms. Lois Swisher
Lindsay S. Tan, M.D. ’82
Nancy S. Tarlin, M.D. ’86
Lucille P. Taverna, M.D. ’71
Jennifer R. Thulin, M.D. ’79
Paul C. Thur, M.D. ’99
George P. Tilley, M.D. ’59
Janet M. Tobin, M.D. ’88
Keith S. Tobin, M.D. ’85
Mark Tomback, M.D. ’78
James P. Tracey, M.D. ’89
John S. Train, M.D. ’67
Jonathan J. Trambert, M.D. ’77
Jeffrey S. Trilling, M.D. ’73
Kelly Troiano, M.D.
Derin Tugal-Racyznski, M.D. ’10
Joseph A. Tyburczy Jr., M.D. ’73
Joel C. Ullman, M.D. ’63
John N. Van Dam, M.D. ’72
Lisa T. Vasak, M.D. ’92
Joseph A. Veneziano, M.D. ’67
Joseph F. Voli, M.D. ’92
Mr. Jerry Volk
Col. James W. Voskovitch, M.D. ’59
VSP Vision Care
James M. Wallquist, M.D. ’66
Laura R. Walters, M.P.H. ’13
Xing J. Wang, M.D.
Yan Wang, M.D.
Daniel E. Wapner, M.D. ’82
Watchung Pediatrics
Mr. Markus Weidner
Charles L. Weinberg, M.D. ’65
Mr. and Mrs. Jay M. Weinstein
Lora Weiselberg, M.D. ’75
Comd. Kenneth Wells, M.D. ’94
Princess Wells, D.P.T. ’10
Graham F. Whitfield, M.D. ’76, Ph.D.
Geoffrey R. Wickwire, M.D. ’73
Aimi Y. Will, M.D. ’98
Gregory T. Williams, M.D. ’86
Jeanette E. Williams, M.P.H. ’05
Felix Wimpfheimer, M.D. ’45 +
Mr. George Wimpfheimer
Wine Country Occupational Medicine
Yakov Consulting LLC
Hyun J. Yoo, M.D.
Corey C. Young, M.D. ’06
Shelley A. Zara, M.D. ’73 and Harvey D. Zara, M.D. ’73
Robert C. Zeller, M.D. ’71
Robert C. Zoller, M.D. ’77
With a proud history of humanism and inclusivity, NYMC has been educating exceptional health care leaders for more than 160 years. Your contributions allow us to provide scholarships for our extraordinary students, recruit and retain the best faculty, conduct cutting-edge research, invest in technology and maintain state-of-the-art instructional and learning facilities.
We encourage you to explore nymc.edu/give for more information.


Areas where you can make a difference:
• Annual Fund
• Contribute to an existing student scholarship, research, or academic fund
• Establish an endowment fund
• Make a planned gift
• Participate in the annual Founder’s Dinner
• Host a fundraising/ cultivation event
your area
The Legacy Society of New York Medical College recognizes donors who have made provisions for the College in their wills or through other planned gifts as well as those donors whose estate has made a gift to the College.

These members have named New York Medical College as a beneficiary in their estate plans/wills as of February 9, 2023:
Anonymous – 5
Michael S. Alexander, M.D. ’78
Ralph Almeleh, M.D. ’76
Doris Bate, M.D. ’50
Augusta H. Belmonte, M.D.
Barbara Bitsko
Phillip Capozzi Jr., M.D. ’96
James E. Carter, M.D. ’55
Neil T. Choplin, M.D. ’76
Morris A. Diamant, M.D. ’78 +
Emalie and John D. Feerick
Dr. and Mrs. Denis J. Frank ’61
Mark J. Friedman, M.D. ’71
Howard D. Harrison, M.D. ’61
Selma Henig
John F. Hoell, M.D. ’60+
Peter M. Holland, M.D. ’69
Maureen Kennedy, Dr.P.H. ’11, M.S. ’03
Mrs. Mary M. Kogut
Bradley S. and Ruth Friedman Kuhn
Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64
Annette E. Kussmaul, M.D. ’93
Mrs. Diane L. Levere
Carl M. Marchetti, M.D. ’60
Joseph P. Merlino, M.D. ’78, M.P.A.
Mark S. Noveck, M.D. ’80
Lee J. Phillips, M.D. ’85
Kenneth M. Rose, M.D. ’88
Neil R. Scheier, M.D. ’85
John H. Seward, M.D. ’61
Neil S. Silber, M.D. ’75
Theresa A. Smith, M.D. ’56
John T. Stinson, M.D. ’75
Rev. Ruth H. Strang, M.D. ’49 +
Richard K. Stone, M.D. ’68 +
Anna M. Ward, M.D. ’85
Since 1987, the College has received more than $23.5 million in contributions from the estates of these individuals:
Alma Allen
Anne T. Barbieri
Herbert and Sylvia Berger
Marcelle B. Bernard, M.D. ’44 and Edmund D. Marinucci, M.D. ’44
Barbara Bess
Charles E. Birch, M.D. 1891
Alice H. Burgoyne
Michael Caruso
Nathan W. Chaikin, M.D. and Mrs. Frances Chaikin
Herrlich Ciatto
Mary E. Clarke
William P. Coats, M.D. ’53
Wendy E. Cohen, M.D. ’70
Brian J Collins, M.D. ’61
Sidney L. Cramer, M.D. ’41
Mabelle A. Cremer, M.D. ’53 and Martin E. Silverstein, M.D. ’48
Lewis A. Dalburg, Jr., M.D. ’58
R. Margarita De Santis, M.D. ’59
Margot Ammann Durrer, M.D. ’49
Earl H. Eaton, Jr., M.D. ’44
Walter G. Elliott, M.D. ’51 and Mrs. Shirley Elliott
Ethel Esther Sandler
Eva Feld
Miguel Figueroa, M.D. ’48 and Mrs. Lillian Figueroa
Walter E. Fleischmann
Robert W. Fredrickson, M.D. ’51
COL Saul Fromkes
Francis J. Geary, M.D. ’64
Arthur Ginsburg, M.D. ’58
Gerhard J. Haas, Ph.D.
Seymour Halpern, M.D.
Edith Har-esh, M.D.
Adriel and Evelyn H. Harris
Catherine N. Hinterbuchner, M.D.
Arno R. Hohn, M.D. ’56
Dora May Holmes
Constance Ives Foster
Gerald H. Kass, M.D. ’51
Paul Kay, M.D. ’44
William J. Kelley, M.D.
Joseph B. Kiel, M.D. ’31
Janice Kiss
Solomon D. Klotz, M.D. ’37 and Mrs. Harriett Klotz
Henry V. Kogut, M.D. ’43
Salvatore LaCorte, M.D. ’30
Guy Lepore
Anna Lowin
Maurice L. Malins
David K. Marcus, M.D. ’32
Charles D. McCullough, M.D. ’58
Frederick R. Meeks, M.D. 1907
Matthew S. Mickiewicz, M.D. ’41 and Mrs. Helen Mickiewicz
Laura G. Morgan, M.D. ’49
Ellen J. Nolde
James F. X. O’Rourke, M.D.
Richard A. Perry, M.D. ’60
Eileen H. Pike, Ph.D.
Andrew S. Ranier, M.D. ’46
John Louis Rie Jr.
Mrs. Elaine Rosenberg
William S. Rosenthal, M.D.
Harvey Rosner, M.D. ’63
Mark S. Rothenberg, M.D. ’30
William D. Ryan, M.D. ’53 and Mrs. Kathryn X. Ryan
Tamiko Sato, M.D.
Ruth Saunders
Elaine L. Schulman, M.D. ’65
Louis N. Scotti, M.D. ’58
Louise O. Smith
Roy Gene Smith, M.D. ’61
Sander V. Smith, M.D. ’35 and Mrs. Helen W. Smith
Vincent E. Smith, M.D. ’61
Dr. Sidney Stahler, M.D.
Samuel Steinholtz, M.D. ’28
Rev. Ruth H. Strang, M.D. ’49
Dorothy S. Stengel
Theodore R. Struhl, M.D. ’42 and Mrs. Ruth Struhl
Hiroshi J. Tazaki, M.D., Ph.D.
Ciro S. Tarta, M.D. ’43
Roscoe W. Teahan, M.D. 1917
Joseph F. Tedesco, M.D. ’37 and Mrs. Vera L. Tedesco
Solomon Till, M.D. ’25 and Mrs. Elizabeth Till
Ruth E. Trager
Gertrude Tromp
Roy C. Upham, M.D. 1901 and Sarah Upham
William F. Westlin III, Ph.D. ’89, M.S. ’87
S.R. Wiener
Robert M. Wittenberg, M.D. 1919
Percy C. Zanger, M.D. ’49
Morris Zeichner, M.D. ’33
In honor of Robin Altman-Prish, M.D.
Mrs. Kathy and Arlen Goldberg
In memory of David H. Amler, M.D.
Mr. Arthur Amler
Mrs. Peggy Amler
Robert W. Amler, M.D., M.B.A., and Sherlita Amler, M.D.
Dr. and Mrs. Lawrence A. Lewis, M.D.
Ms. Caroline Mechanick
Ms. Megan Narron
Mrs. Lisa Rubenfield
The Salon Family Foundation Inc.
Neil Spielsinger, M.D.
In memory of Melvin Amler, D.D.S.
Mr. Arthur Amler
Mr. and Mrs. James Amler
Mrs. Peggy Amler
Robert W. Amler, M.D., M.B.A. and Sherlita Amler, M.D.
Mrs. Jennifer Amler Goldstein
Bill Goodell, M.D. and Mrs. Melanie Goodell
Mr. Tom Lambert
Mr. Brett Lynch
Mrs. Rande McMillan
Ms. Caroline Mechanick
Renaissance Charitable Foundation for Modern Giving

Mr. and Mrs. Claude A. Rollin
Mrs. Susan Shimer
In memory of Nicholas Antoszyk, M.D. ’48 and Mrs. Corinne Antoszyk
Dr. and Mrs. Andrew Antosyk
In celebration of Ms. Lindsay Barad
Lydia H. Barad, M.P.H. ’09
In memory of Maurice and Etta Bellin
Howard T. Bellin, M.D. ’62
In memory of Julius Berger, M.D. ’37
Roseanne C. Berger, M.D. ’77
In memory of Robert Bernot, M.D.
Mrs. Carol Bernot
In memory of Libby Bogel
Andrew M. Murphy, M.D. ’78
In honor of Derek Borsody
Dr. Karl J. Borsody and Dr. Jaleh Eslami - Borsody
Dayton Foundation Depository, Inc.

In memory of William and Marie Brown
Tonya M. Brown-Price, M.D. ’90
In memory of Edward T. Butler, M.D. ’87
Mrs. Joi Butler
In honor of Penelope and Scarlett Chew
Qwie T. Chew, M.D. ’65
In honor of Eric I. Choe, M.D. ’88
The David Foundation Inc.
Mr. Larry David
In memory Annette Choolfaian, R.N., M.P.A.
Ms. Nicole Barsamian
Dana R. Deravin Carr, Dr.P.H. ’13, M.P.H. ’01
David N. Greenman, D.D.S., M.P.H. ’07
In memory of Richard James Davis
Robert A. Davis, M.D. ’74
In honor of Delores DelBello
Nora Bergasa, M.D.
In honor of John Derry, M.D. ’60
Ms. Lois G. Schiappa
In honor of Janet P. Dolot, P.T., D.P.T., Dr.P.H. ’14, OCS
Edward C. Halperin, M.D., M.A.
In memory of HaRav Avraham dov ben
Aharon A”H
Ms. Deena Merzel
In memory of Joseph Dursi, M.D. ’59
Ms. Tara Alfano
Mrs. Mary Graham
Mrs. Carol Binen
In honor of Tom Floyd
Bruce Goldfeder, M.D. ’92
In memory of Donald Gemson, M.D. ’78
Anita Grover, M.D. ’78
In memory of Mina Geller, M.D. ’73

Bruce J. Gillers, M.D. ’73
In celebration of Ruby Gilmor
Glenn D. Gilmor, M.D. ’86
In honor of Lia Grasso
Nora Bergasa, M.D.
In memory of Mary Graziano
Mrs. Mary Flanagan-Kundle
In memory of Mr. Robert Greenberger
Steven H. Horowitz, M.D. ’66
In memory of J. Leonard Greif, M.D. ’39
Richard H. Greif, M.D. ’75
In memory of Eugene M. Grossman, M.D.
V. Rachel Phillips, M.D. ’79
In memory of Jimmy Gurran
Ms. Bonnie Gurran-Heindl
In honor of Edward C. Halperin, M.D., M.A.
Dr. and Mrs. Ronnie Myers
In memory Lee Healy
John J. Healy, M.D. ’63
In memory of Dr. and Mrs. Abraham Heller
Col. Paul B. Heller, M.D. ’68
In memory of John Hordines, M.D. ’93
Susan M. Jensen, M.D. ’77
In memory of Arthur Karmen, M.D.
Renee Garrick, M.D.
Mrs. Marie Pinto Jones
In honor of Susan Klein
Mohammed Khan, M.D.
In memory of Howard J. Kline, M.D. ’58
James W. Justice, M.D. ’58
Kline/Sawamura Family Trust
Ellen Sawamura, Ph.D.
In celebration of Zachary Kluger
Jeffrey Kluger, M.D. ’71
In memory of Priscilla LaBabera
Robert V. Blake, M.D. ’75
In memory of William Lamp
Laura R. Walters, M.P.H. ’13
In memory of David Lazovitz, M.D. ’71
Alan R. Green, M.D. ’71
In memory of Ms. Florence Lewis
Walter M. Lewis, M.D. ’91
In memory of John J. Lynch, M.D. ’58
Ellen Loughran, Ph.D.
In memory of Howard and Leah Matican
Jeffrey S. Matican, M.D. ’82
In memory of Eileen Brett McCully
William F. McCully Jr., M.D. ’57
In celebration of Kathryn McGoldrick
Dariana Francois, M.D. ’07
In memory of Concetta “Tina” Messina
Edward J. Messina, Ph.D. ’73
In celebration of Yair Miller’s graduation
Mr. Gideon and Mrs. Nava Miller
In memory of G. C. Mitra
Debjeet Sarkar, M.D. ’05
In memory of Robert Nadelman, M.D.
Marisa Montecalvo, M.D.
In memory of Dao Nguyen
Thang Q. Le, M.D.
In memory of Robert W. Niehaus, M.D. ’50
Ms. Lois Swisher
In honor of Kurt Nystrom
Karel R. Amaranth, M.P.H. ’10
In memory of Ralph A. O’Connell, M.D.
Judith C. Ahronheim, M.D.
Ms. Lori Ann Perrault
In celebration of Drs. Seth and Sophia O’Donnell
Sophia G. O’Donnell, M.D. ’08
In memory of Donald Orlic, Ph.D.
Damien B. Lee, M.D. ’97
In honor of Brian Olser, M.D. ’18
Mr. and Mrs. Robert P. Osler
In memory of Frank Paret
Robert W. Paret, M.D. ’59
In memory of Albert A. Pineda, M.D. ’63
Barbara Pineda, M.D.
In memory of Mitchell Pollack, M.D. ’77
Stephanie L. Pollack, M.D. ’14
In honor of Concetta Rinaldi
Renee Z. Rinaldi, M.D. ’76
In memory of Bill Roe
Matthew C. Frankel, M.D. ’78
In memory of Mrs. Shirley Rosenblatt
Donna A. Zeide, M.D. ’83
In memory of Sy and Rena Roth
Ronald R. Roth, M.D. ’73
In memory of James Rubenstein M.D. ’78
Edward S. Valentine, M.D. ’78
In memory of Samuel H. Rubin, M.D.
Adam D. Rubin, M.D. ’00
In honor of Margot S. Rubinstein, M.D. ’83 and Andrew S. Gutterman, M.D. ’83
Deborah Fried, M.D. ’83
In honor of Mr. Matthew Russo
Laurence M. Raiford, M.D. ’77
The Terri and Matty Russo Fund
In honor of Dr. Saul and Mrs. Evelyn Sacks, and David Paion Sr.
Harry G. Sacks, D.D.S., J.D.
In honor of Henry Saphier, M.D. ’61
The Benevity Community Impact Fund
Thomas Gleason
In honor of John A. Savino, M.D. Umer Sayeed Sayeed-Shah, M.D. ’96
In memory of Ms. Anne Sawyer
Donald E. Sawyer, M.D. ’70
In memory of Seymour Schlussell, M.D. ’51 Jack D. Norman, M.D. ’63
In memory of Mr. Edward Severs
Adrienne R. Greenlaw, M.D. ’91
In memory of Ms. Helene Silvers
John T. Pellicone, M.D.
In honor of Brij Singh Ahluwalia, M.D. Venkat Ramani, M.D.
In celebration of Anthony M. Sozzo, M.A., M.S. Ed.
Helen Badoyannis, Ph.D. ’91
In memory of Francis Spear, M.D. Harvey A. Glasser, M.D. ’64

In memory of Dr. Joseph and Mrs. Jeanne
Salvola
Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
In memory of Richard Stone, M.D. ’68
Steve M. Frank, M.D. ’73
Freddy Arce, M.D.
Ms. Courtney Boniface
Mrs. Tina Cardoza-Izquierdo
In memory of Seymour Tobin, M.D. ’52
Keith S. Tobin, M.D. ’85
In honor of Marco J. Tomassi, M.D. ’03 and Michelle P. Tomassi, M.D. ’05
Mrs. Patricia M. Tomassi
In honor of Dominic O. Vachon, M.Div., Ph.D.
James P. Roach, M.D. ’58
In honor of Ray Whitt, M.D.
Morris C. Finkelstein, M.D. ’85, Ph.D.
In memory of Felix Wimpfheiner, M.D. ’45
Mr. George Wimpfheimer
In celebration of Reinhard Zachrau
Yun Shin Chun, M.D. ’00
Justin M. Segraves, M.D. ’14
We have made every effort possible to provide a full and accurate list of donors to NYMC from July 1, 2021 through June 30, 2022. If we have omitted or improperly listed your name, please accept our apologies. If you detect an error, please contact our Office of Development and Alumni Relations at (914) 594-2720 or email us at development@ nymc.edu, so we may correct our records.
The Office of Development and Alumni Relations is pleased to announce the addition of Bernadette Bauer, manager of alumni engagement. Bauer has extensive experience working in alumni relations, planning events and facilitating local and nationwide functions for regional alumni chapters and college fundraisers. In her new role, she is responsible for creating opportunities and events for NYMC alumni to stay connected. Join us in welcoming Bauer to the NYMC community and get to know more about her vision for her new role.

The Office of Development and Alumni Relations is the go-to hub for networking with the NYMC community after graduation. We want to bridge life after college to provide people with the opportunity to stay engaged with NYMC. We also create a culture of philanthropy to support NYMC’s mission to educate the next generation of physicians, researchers and public health professionals. May it be through reunions, regional events or on-campus and virtual offerings, we want to create a welcoming environment for alumni because you are only in school for a handful years, but you are an NYMC alum for life.
I genuinely enjoy making connections while fielding alumni inquiries, especially when it involves the historical side of things. My background is in history and anytime I can learn a little fact here or there and get an incredible story through the historical lens of the College with the aim of inviting alumni to engage is always such a heart touching experience. I recently received an email from a woman who was looking for information about her grandfather who graduated in 1919.
Nicholas Webb [MSIS, archivist and digital preservation librarian at NYMC] was able to find a tremendous amount of information in less than 30 minutes. He put forth a beautiful narrative that was incredible to share with this woman, who was trying to figure out her family history for so long. She finally found that missing puzzle piece by engaging with us. It is an honor to be able to usher in that type of support when receiving general inquiries. You never know what to expect when you pick up that phone or read an email.

Alumni can show support by reaching out if they are interested in serving as a committee representative for their class reunion. You can also stay engaged with us by hosting a get together at your home or local venue in your area. We recently had an event in New Jersey with an alumna at her home. She invited several alumni, as well as current students. We always love to have that type of engagement between current students and alumni. That helps show solid support for current NYMC students. It also provides a layer of mentorship and networking opportunities. Alumni can also purchase a medical kit that includes a stethoscope, aneroid, reflex hammer and macro view diagnostic set for an incoming medical student, volunteer to serve as interviewers for the School of Medicine Office of
Admissions, support student scholarships during Days of Giving, attend our annual Founder’s Dinner or hit the links at the NYMC golf outing. It is interesting to keep abreast of your classmates’ news and accomplishments, so I encourage alumni to submit their class notes online which are published in Chironian
HOW CAN ALUMNI CONNECT WITH THE SCHOOL AND OTHER ALUMNI AFTER GRADUATION?
NYMCConnect.org is a great platform to stay up to date with the College. It is a terrific hub to engage with fellow alumni. We have an active comment board for sharing news and alumni can reach out with general questions or find out who is in the area to meet up with. Alumni can also connect through our various NYMC social media platforms including LinkedIn, Facebook, Instagram and Twitter.
HOW CAN I BE NOTIFIED OF UPCOMING ALUMNI EVENTS AND NYMC NEWS?
You can always view our website at nymc.edu/alumni or NYMCConnect.org and our Facebook page at New York Medical College Alumni and Friends. Be sure to check your email for the alumni e-newsletter Alumni Connections with all the latest news on each school. If you have any questions, you can also give us a call at (914) 594-2720 or email us at development@nymc.edu. ■