CHIRONIAN



Vice President of Communications and Strategic Initiatives
Jennifer Riekert, M.B.A.
Editor Lori Perrault
Writers
Lenore Carpinelli
Rhea Hirshman
Andrea Kott, M.P.H.
Contributor
Tyler Landis, M.B.A.
Lori Perrault
Melissa F. Pheterson
Kiara Thomas, M.A.
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer
Editorial Board
Salomon Amar, D.D.S., Ph.D.
Amy Ansehl, R.N., D.N.P., FNP-BC
Lenore Carpinelli
Bess J. Chazhur, M.S.
Tetyana Cheairs, M.D., M.S.P.H.
Mill Etienne, M.D. ’02, M.P.H.
Vikas Grover, Ph.D., CCC-SLP
Design Wayne Printing, Inc.
Photography
Edmund F. LaGamma, M.D. ’76
Christopher S. Leonard, Ph.D.
Dana Mordue, Ph.D.
Michelle Novotny, M.A.
Michal L. Schwartzman, Ph.D.
Anitha Srinivasan, M.D., M.P.H.
Dmitry Kalinin, DIA International Group, Inc.
William Taufic Photography
ADMINISTRATION
Alan Kadish, M.D., President
Christopher Pope
John Vecchiolla Photography
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer
Robert W. Amler, M.D., M.B.A., Dean, School of Health Sciences and Practice, Vice President for Government Affairs
Marina K. Holz, Ph.D., M.P.H. ’23, Dean, Graduate School of Biomedical Sciences
Neil W. Schluger, M.D., Dean, School of Medicine
Office of Public Relations
Jennifer Riekert, M.B.A., Vice President of Communications and Strategic Initiatives
Lenore Carpinelli, Director of Strategic Communications, School of Medicine
Lori Perrault, Director of Print and Digital Publications
Madlena R. Pesheva, M.P.H. ’21, Director of Creative Communications and Production
Julio A. Rodriguez-Rentas, M.A., Senior Director of Strategic Communications
Kiara Thomas, M.A., Communications Writer and Content Creator
Please direct all inquiries to:
New York Medical College/Chironian, 40 Sunshine Cottage Road, Valhalla, NY 10595. We authorize the use of any material with attribution to New York Medical College. Chironian is published annually by the Office of Public Relations. We welcome reader feedback. Contact us at (914) 594-4536 or at chironian@nymc.edu.
NEW YORK MEDICAL COLLEGE AFFILIATIONS
Major Clinical Affiliated Sites
Westchester Medical Center Health Network (WMCHealth) Westchester Medical Center
Maria Fareri Children’s Hospital Good Samaritan Hospital
NYC Health + Hospitals/Metropolitan
Clinical Affiliated Sites
Beckley VA Medical Center
Calvary Hospital
Greenwich Hospital
Hoboken University Medical Center
James J. Peters VA Medical Center
Landmark Medical Center
Lenox Hill Hospital
Northern Westchester Hospital
NYC Health + Hospitals/Lincoln
Phelps Hospital Northwell Health
Ambulatory Care Programs
CareMount Medical/Optum Care for the Homeless
ODA Primary Health Care Network
Open Door Family Medical Centers
Refuah Health Center
Health Alliance Hospital
MidHudson Regional Hospital
Richmond University Medical Center
Rome Memorial Hospital
Saint Clare’s Hospital
Saint Joseph’s Medical Center
Saint Michael’s Medical Center
St. Mary’s General Hospital
Terence Cardinal Cooke Health Care Center
VA Hudson Valley Health Care System
Yuma Regional Medical Center
Union Community Health Westchester Institute for Human Development Westmed Medical Group


CONNECT WITH US: www.nymc.edu facebook.com/nymedcollege and facebook.com/nymcalumni
Follow us on Twitter @nymedcollege
Connect with us on LinkedIn @new-york-medical-college
Follow us on Instagram @nymedcollege


New York Medical College is a health sciences college, which awards graduate and professional degrees in the biomedical sciences and clinical and administrative health professions. A health sciences college is a community of scholars, which is assembled for the generation, conservation, and dissemination of knowledge about the causes, prevention, and treatment of human disease and disability. While it is a community of scholars, it is not a real estate development organization nor is it a form of public entertainment insofar as it fields no football, basketball, or baseball teams.
There are some people working in and writing about higher education in the United States who think it is appropriate to refer to the faculty as “employees” and the students as “customers.” I reject both appellations. The faculty are not employees of the College, they ARE the College. It is only through the teaching, clinical care, and research of the faculty that the College fulfills its missions. The students are not customers. They are the future of clinical care and biomedical research who are welcomed as learners and collaborators in the community of scholars. I call to the attention of the alumni and friends of the College some of the important awards received by the faculty and students at the College in the past year. These awards demonstrate the accomplishments of the members of our academic village. We take pride in these external validations of our faculty and students’ accomplishments.
Edward C. Halperin, m.d., m.a. chancellor and chief executive officer
2024 Westchester Magazine’s Healthcare Heroes: Neil W. Schluger, M.D., dean of the School of Medicine
2024 American Society for Biochemistry and Molecular Biology Fellow: Marina K. Holz, Ph.D., M.P.H. ’23, dean of the Graduate School of Biomedical Sciences
American Medical Association 2024 Excellence in Medicine Awards – the Dr. Edmond and Rima Cabbabe Dedication to the Profession Award: Mill Etienne, M.D. ’02, M.P.H., vice chancellor of diversity and inclusion, associate dean of student affairs, and associate professor of neurology and of medicine
Westchester Institute of Human Development President’s Award: Robert W. Amler, M.D., M.B.A., dean of the School of Health Science and Practice and vice president for government affairs 2024 Excellence in Public Health Award from the U.S. Public Health Service Physician Professional Advisory Committee: Medha Reddy, School of Medicine Class of 2024 2023 Children’s Dream Foundation Medical Service Award: Allen J. Dozor, M.D., professor of pediatrics and clinical public health
The OpEd Project’s Public Voices Fellowship, through the Paul and Daisy Soros Fellowships for New Americans: Mill Etienne, M.D. ’02, M.P.H., vice chancellor of diversity and inclusion, associate dean of student affairs, and associate professor of neurology and of medicine
2024 DermMentors Resident of Distinction Award: Seher Banu Farabi Atak, M.D., second-year dermatology resident in the NYMC-sponsored Dermatology Residency Program at NYC Health + Hospitals/Metropolitan 2023 Westchester Magazine’s Healthcare Heroes: Manoj Abraham, M.D., clinical associate professor of otolaryngology
Augustine Moscatello, M.D., M.S., professor of clinical otolaryngology and department chair
Mill Etienne, M.D. ’02, M.P.H., vice chancellor of diversity and inclusion, associate dean of student affairs, and associate professor of neurology and of medicine
Ellen Bloom, M.P.H. ’00 2023 Gold-Headed Cane Award from the American Urological Association: Muhammad Choudhury, M.D., professor and chair of urology
National Board of Medical Examiners 2023 Edithe J. Levit Distinguished Service Award: Tracey Milligan, M.D., FANA, professor and chair of neurology Westfair 2023 Doctors of Distinction: Doctor without Boundaries Award: Fawaz AlMufti, M.D., associate professor of neurology, neurosurgery, and of radiology
Westfair 2023 Doctors of Distinction: Promise of the Future Award: Thomas Gagliardi, School of Medicine Class of 2024
American Neurologic Association 2023 Distinguished Neurology Teacher Award: Tracey Milligan, M.D., FANA, professor and chair of neurology American Medical Association Foundation Physician of Tomorrow Scholarship: Thomas Gagliardi, School of Medicine Class of 2024
American Academy of Neurology Changemaker Award: Mill Etienne, M.D. ’02, M.P.H., vice chancellor of diversity and inclusion, associate dean of student affairs, and associate professor of neurology and of medicine
Mental Health Association of Westchester and the Mental Health Association 2023
Honoree: Leslie Citrome, M.D., M.P.H., clinical professor of psychiatry and behavioral sciences
Microcirculatory Society 2023 Landis Award: Akos Koller, M.D., Ph.D., professor emeritus of physiology
Alpha Omega Alpha Richard L. Byyny 2023 Fellow in Leadership: Kristina H. Petersen, Ph.D., associate professor of biochemistry and molecular biology
Induction as a full member into the American College of Surgeons Academy of Master Surgeon Educators: Kathryn Spanknebel, M.D., FACS, dean of faculty and academic affairs, associate professor of surgery, and vice chancellor for student mental health and wellness
Induction into Sigma Xi, the scientific research honor society: Fawaz Al-Mufti, M.D., associate professor of neurology, neurosurgery, and of radiology
International Association of Top Professionals Global Health Care Leader of the Decade Award: Padmini Murthy, M.D., M.P.H., M.S., FAMWA, FRSPH, professor of public health and director of global health

Members of the School of Medicine (SOM) Class of 2023 celebrated taking their next step in their medical training on Match Day when they gathered in the Willner Lobby of the Medical Education Center to learn where they were matched to medical residency programs through the National Resident Matching Program (NRMP). At precisely noon on March 17, 2023, with the atmosphere rife with anticipation, the students were at last able to tear open their envelopes and learn their match results. The 2023 match had 42,952 applicants who certified a rank
order list (“active applicants”) and 40,375 certified positions.
The Class of 2023 is training in 25 states at 103 different institutions, including several of New York Medical College’s (NYMC) major clinical affiliated sites, Westchester Medical Center and NYC Health + Hospitals/Metropolitan, as well as clinical affiliated sites NYC Health + Hospitals/Lincoln, Greenwich Hospital, Lenox Hill Hospital, and Landmark Medical Center. NYMC medical students also matched at


academic medical centers across the country, including Beth Israel-Deaconess of the Harvard Medical School, Brown, Cleveland Clinic, Mayo Clinic, Mount Sinai, Johns Hopkins, Columbia, Weil Cornell, New York University, Tufts, UCLA, and Yale.
The top career choices for the Class of 2023 were internal medicine, pediatrics, emergency medicine, psychiatry, general surgery, anesthesiology, radiology, obstetrics and gynecology, and neurology. ■

For one decade, the Clinical Skills and Simulation Center (CSSC) has trained more than 4,000 students, physicians, residents, and other allied health professionals who pass through its doors each year. Now, they are preparing for another milestone: a major expansion and renovation to accommodate the need for additional programming, updated facilities/equipment, and added certification programs. Highlights of the renovation were revealed on the evening of September 19, 2023, at the “Past, Present and Future” reception and tour, which also showed appreciation to the generous donors who are making it possible.
The innovative training environment that promotes interprofessional collaboration, teaching, and assessment in an authentic clinical setting is at its peak capacity. “The programming offered by the CSSC creates a bridge between the academic and clinical communities by exposing our learners to hands-on, competency-based learning utilizing standardized patients, high fidelity manikins, realistic task trainers, and point of care ultrasounds,” said Katharine Yamulla, M.A., CHSE, assistant dean of clinical skills education and assessment and director of the CSSC. “This vital expansion and renovation will also allow us to implement new programs that address the unique needs of marginalized communities, including patients with disabilities, to ensure our trainees deliver culturally competent health care. We are so grateful for all of our donors who are making this possible.”
The generous donors include Paul Ostrovsky, M.D. ’78, and Rebecca Ostrovsky; David E. Asprinio, M.D., chair of the Department of Orthopedic Surgery and professor of clinical orthopedic surgery, and Kim Flood, M.D.; Ben Chouake, M.D., a member of the Board of Trustees, and Esther Chouake, M.D.; Lee Pressler, M.D. ’90; Ronald P. Gregoire, M.D. ’74; and the Children’s Dream Foundation. Naming opportunities are still available. Additional information is available by

emailing development@nymc.edu, calling (914) 594-2720, or visiting https:/nymcalumni.org/give.
The 7,200 square-foot expansion and renovation, which commenced in February 2024, and is expected to be complete in September 2024, includes two additional standardized patient exam rooms, an advanced ultrasound laboratory, and specialty training suites to support orthopedic training, cardiopulmonary care, labor and delivery, as well as specialized pediatric care, emergency care, operative simulation, critical care, and advanced procedural competences. The suites will be equipped with sophisticated simulators, such as a birthing simulator and a full-scale anesthesia manikin, laparoscopic simulators, virtual reality training solutions, as well as scrub sinks to promote best practices for infection control. Additionally, a three-bed patient care unit will function as a multi-purpose simulation room and can be configured as a trauma/triage care unit, emergency department, and/ or a post-operative/recovery care unit. Each bed in this unit will be in its own examination bay, equipped with a monitor, headwall, and appropriate examination/resuscitation equipment. ■
The NYMC community rose to the occasion for the sixth annual Days of Giving Campaign in March 2023, and raised $480,000 for student scholarships. The goodwill of 45 ambassadors and 327 gifts from 315 donors hailing from 27 states, along with matching gifts from a generous group of donors will impact the lives of students in the School of Medicine, School of Health Sciences and Practice, and Graduate School of Biomedical Sciences. “This year’s Days of Giving campaign was a tremendous fundraising success with increased participation from faculty, staff, alumni, and students. The unprecedented number of student callers helped solidify our efforts as alumni happily chatted with the medical students and reminisced about their time at NYMC,” said Bess J. Chazhur, M.S., chief development officer and executive director of alumni relations. “We are deeply grateful to all those who participated in this special 48-hour campaign.” ■

The New York Medical College (NYMC) and Touro University (TU) communities gathered for a melancholy observation of Yom Hashoah on May 4, 2023. A moving presentation by Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, the Miriam Popack Chair of Biomedical Ethics and the Holocaust, director of the Hirth and Samowitz Center for Medical Humanities and Holocaust Studies, and provost for biomedical affairs at TU, explored new scientific research that demonstrated that the “Dachau ashes” that were analyzed by NYMC and buried in 2014 were more complex and sinister than previously described.
Dr. Halperin told the story of U.S. soldier and North Carolina repairperson for addressographs, Walter Corsbie, who was given a lump of a rounded cement-like material assumed to be the ashes from a crematorium and was told to keep the object as a souvenir of the Dachau camp. For 30 years, the cement-like object stayed on his nightstand in a tin cigarette case until it was inherited by his son Joseph Corsbie. He tried to donate the object to the U.S. Holocaust Museum, who said that they are unable to accept human remains, and the Dachau Museum, which claimed the object was crematoria concrete tags. Corsbie contacted a friend and ultimately met with Sharon Halperin, M.P.H., director of the North Carolina Holocaust Speakers Bureau, and wife of Dr. Halperin.
Sharon Halperin, brought the cement-like object home, where Dr. Halperin started to examine and take pictures of it and shared it with The Milton Helpern Institute of Forensic Medicine, where they found that there were no bony fragments. However, they did find human proteins inside the specimen using proteomic mass spectrometry.
Once notified, Corsbie wanted the object to be buried in sanctified grounds. With the approval of the rabbis, arrangements were made for a burial ceremony in 2014 with hundreds in attendance, including Holocaust survivors. The Holocaust Speakers Bureau placed a descriptive plaque on the fence of the cemetery and the memorial was unveiled a year later. Students from local schools were given tours by the Halperins, who told them about the “Dachau ashes.”
During the summer of 2022, Dr. Halperin received an email from The Milton Helpern Institute of Forensic Medicine who

revealed that the “Dachau ashes” matched a group of concrete discs in museums in Cape Town, South Africa, and Yad Vashem, Israel. The discs had a hole and numbers stamped on them and matched the circumference of the “Dachau ashes.” The people who donated the objects were told that the round cementlike objects were assumed to be covered with fat and used as artificial soap or a tag for belongings before people entered the gas chambers.
Germany faced a shortage of concrete following the bombing of concrete manufacturing factories. Human bones from the concentration camps were possibly grinded to be used as aggregate, instead of gravel or pebbles, for concrete. There is a strong possibility that people in the concentration camps used the “Dachau ashes” as coat checks or soap to avoid a stampede from entering the gas chambers disguised as showers.
“What you heard is the end results of eugenics in medicine,” said Dr. Halperin. “The fingerprint of medicine is all over those discs because it was geneticists and doctors interpreting mendelian genetics and Charles Darwin to give us this kind of intellectual justification for this.”
Rabbi Moshe D. Krupka, M.S., executive vice president, TU, concluded the event with a prayer with Paul Glasser, vice president for institutional advancement, TU. “Yes, there is evil and racism in this world. There are horrible people who do horrible things, but we will make it better. That is what we stand for and who we are,” said Rabbi Krupka. ■
The Center for Disaster Medicine (CDM) celebrated a significant milestone with a groundbreaking ceremony for its new Simulation and Educational Facility on September 13, 2023. In attendance were esteemed political leaders and distinguished faculty as well as leadership from New York Medical College (NYMC). Their collective pride in the expansion was palpable, as they gathered to mark this momentous occasion.
The Center’s new development will continue NYMC’s globally recognized assets, expertise, and research findings encompassing natural disasters, terrorism, operational, and tactical medicine, and public health preparedness, with competence in the unique needs of children, persons with disabilities, climate change, equity in preparedness, and response, and health care systems preparedness.
“The vast expertise within our Center positions us as the optimal resource to provide this essential training and education across the entire state,” said David S. Markenson, M.D., M.B.A., director and medical director of the CDM.
The New York State Assembly provided $250,000 through a State and Municipal Program Grant and Senator Peter Harckham provided $200,000 in capital funding for the extension of the CDM. Local representatives, Majority Leader Andrea Stewart-Cousins, and Senator Harckham, who represented the Center for multiple years prior to redistricting, gave remarks at the groundbreaking about the impact the Center has had on the community for nearly 20 years.
“Today’s event literally opened the wall into exciting new spaces and opportunities to expand the Center’s impact in preparing resilient communities

across New York State,” said Robert W. Amler, M.D., M.B.A., dean, School of Health Sciences and Practice and vice president for government affairs. ■


Members of the School of Medicine (SOM) Class of 2027 marked a milestone in their medical education as they donned their white coats for the first time during the SOM White Coat Ceremony at the Performing Arts Center at Purchase on July 28, 2023. A long-held tradition at New York Medical College (NYMC), the White Coat Ceremony emphasizes the importance of professionalism and humanism in medicine at the beginning of medical school.
The 219 members of the class processed into the auditorium with their white coats draped over their arms as their families and friends looked on with pride. During the ceremony, several faculty and student speakers spoke of the enormous responsibility they would carry as physicians, symbolized by their white coats, and emphasized the importance of maintaining their humanism throughout their careers.
“These white coats that you will soon receive symbolize the hard work and specialized knowledge that characterize us as physicians. But also remember the values that they represent: the dedication to your patients above all, and the commitment to excellence that is demanded by the path we have chosen,” said Neil W. Schluger, M.D., dean of the SOM.
The keynote address was presented by Muhammad Choudhury, M.D., professor and chair of the Department of Urology. During his address, Dr. Choudhury spoke of the importance of the six standards of resident and fellowship training—medical knowledge patient care, professionalism, interpersonal/ communication skills, practice-based learning, and system-based practice—as adopted by the Accreditation Council for Graduate Education, interspersing his remarks with examples from his own career and inspiring the Class of 2027 as they embarked on their medical school journey. ■
Doctor of Physical Therapy (D.P.T.) students from the Class of 2025 reached a significant milestone in their educational journeys, donning their white coats for the first time at the D.P.T. White Coat Ceremony in John W. Nevins, M.D. ‘44, Auditorium on April 18, 2023. In front of friends, family, faculty, and School of Health Sciences and Practice (SHSP) leadership, the 49 students asserted their commitment to the field of physical therapy as they transition to the clinical side of the curriculum.
Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, addressed the students with proving insight into the “third person in the room” students can expect to encounter when examining a patient in the future.
This person, visible or not, influences what happens between a doctor and patient, and it is important to remain cognizant of outside entities that affect that relationship. Dr. Halperin embraced the students as members of the white coat community. “I am happy to welcome you to that body of women and men in white coats, stretching backward and forward in time, who have committed themselves to the relief of pain, the amelioration of suffering, and to helping people avoid, to the extent possible, premature death.”
Alumni speaker Nicholas Sheehan, D.P.T. ’16, PT, assistant professor of physical therapy, provided his perspective on the evolution that occurs when shifting from coursework to clinical studies. “All of your hard work is no longer just for you.

It is for the patients you will be treating. In our profession, we meet people in their darkest times, and you will be there not only as their physical therapist but as a major foundation to their support system.”
Students were then called on to don their white coats with assistance from D.P.T. faculty members. Proudly wearing their new coats, the students were eager to begin the next chapter of their educational endeavors. ■

F amilies, faculty, and students proudly assembled in the John W. Nevins, M.D. ’44, Auditorium as the Graduate School of Biomedical Sciences (GSBMS) hosted its biennial Lab Coat Ceremony for Ph.D. candidates on September 15, 2023. The ceremony welcomed secondand third-year Ph.D. candidates and new M.D./Ph.D. students who gleefully donned their lab coats, surrounded by their loved ones and mentors who joined in to celebrate this significant moment.
Marina K. Holz, Ph.D., M.P.H. ’23, dean of the GSBMS, professor of cell biology and anatomy, and interim chair of the Department of Biochemistry and Molecular Biology, warmly welcomed the Ph.D. students. “I hope you all can appreciate that science is a long-term endeavor and
the longevity and endurance in science takes a lot of hard work and being excited and asking what’s next,” said Dr. Holz.
The presentation of the lab coats was led by Tetyana Cheairs, M.D., M.S.P.H., assistant dean for Ph.D. programs and assistant professor of pathology, microbiology, and immunology. GSBMS faculty addressed the Ph.D. students, which included entry cohorts from 2023, 2022, and 2021. Each Ph.D. candidate took their turn, donning their white coat with the guidance of their mentors.
After the students donned their white coats, Tara Jarboe, M.S., fifth-year Ph.D. candidate in pathology, microbiology, and immunology, gave the student address and shared her passion in science was solidified when she was faced with a
family member with an aggressive form of pancreatic cancer when she was in the ninth grade. “Every day as you put on your lab coat and prepare yourself to conduct your research, it serves as a reminder to the commitment we make to ourselves and to our field to how we approach our research with passion, but also great care,” said Jarboe.
The ceremony concluded with a keynote address by Marcello Rota, Ph.D., associate professor of physiology, who spoke about his journey in research and encouraged students to continue to ask questions and be curious. The doctoral candidates concluded the ceremony by reciting the Graduate Student Code, affirming their commitment to ethical conduct in their profession. ■
In March 2023, Touro College of Dental Medicine (TCDM) at New York Medical College received approval from the Commission on Dental Accreditation to increase enrollment. The additional 100 seats will increase the number of students in new classes to 210, allowing the school to educate more dentists to address current national shortages. In July 2023, TCDM welcomed the expanded incoming class as the Class of 2027, the eighth graduating class for the school.
In this new program, all students will spend their first two years at TCDM’s Valhalla, New York, campus, where they learn and study biomedical foundation and simulation of dental skills. For the last two years, when students begin their clinical studies, 110 students will continue their studies in New York and
Students from New York Medical College’s (NYMC) Doctor of Physical Therapy (D.P.T.) Class of 2025 hosted the 25th Annual Race for Rehab on October 15, 2023. The 5K race was the most successful to date, as students raised more than $16,000 to support Achilles International, a non-profit organization that provides a community of support for athletes with disabilities.
More than 170 participants, including 35 Achilles athletes, joined the race around NYMC’s Valhalla campus. An awards ceremony capped off the event, announcing the winners in each category, including Achilles athletes, alumni, as
100 students will complete their studies in Albuquerque, New Mexico.
“New Mexico does not have a dental school,” said Ronnie Myers, D.D.S., dean of TCDM. “Creating a dental school clinical educational facility within the state will provide an opportunity to deliver needed dental care to underresourced communities while at the same time open local access to New Mexico students interested in becoming dentists.”
A new clinical facility will be built on the campus of Lovelace Biomedical Research Laboratories, the not-for-profit contract research organization with a rich history of helping pharmaceutical and biotechnology partners. (See story on page 28).
Touro Dental Health will be the first dental school facility in the state of
well as male and female finishers in different age categories.
Daisy Alverez, Peter Calicchia, and Cristina Santamaria from the D.P.T. Class of 2025 had this to say about the successful event: “This year’s event was truly special because of the unprecedented community turnout. Our team was extremely successful in rallying our community together. The race was driven by the inspiration of the Achilles athletes and their continuous commitment

New Mexico. Historically, New Mexico has struggled with representation in dental education and dental resources. In 2021, the population in New Mexico was estimated at 2.1 million and the number of dentists per 100,000 people was 48.44, far below the national average of 60.84 and one of the lowest ratios in the country. With a dental school clinic within the state, it is anticipated that an increased number of graduating students will remain in New Mexico to pursue their career and help to address the problem. ■
to achieving their potential. They gave us a sense of perspective and gratitude, and their positive mindset to continue to live their lives to the fullest despite their disabilities motivates us to do the same daily. The Race for Rehab holds close to our hearts, empowering athletes with physical disabilities and raising funds for those who lack the resources to participate. Through hard work and dedication, we surpassed our goal, raising $16,030, a surreal achievement.” ■

Founded in 2023, the Women’s Institute for Science Entrepreneurship (WISE) at New York Medical College (NYMC) was created to support women innovators in cultivating new scientific concepts and launching new businesses to make an impact in their communities and the world. It also serves as a catalyst for change, inspiring women to pursue STEM education and research. It was established with an $825,000 award sponsored by U.S. Senator for New York Kirsten Gillibrand and appropriated by the U.S. Department of Commerce, and the National Institute of Standards and Technology’s Scientific and Technical Research Services.
WISE brings together interdisciplinary teams of faculty and students at NYMC, Touro University (TU), and BioInc@NYMC to connect students, researchers, faculty, and biotech entrepreneurs on- and off-campus to work collaboratively creating synergy to lead to groundbreaking scientific projects.
“Interventions that create a path for women in science to become business leaders are most effective when introduced early in their educational and professional careers, and this program robustly promotes this goal,” said Marina K. Holz, Ph.D., M.P.H. ’23, dean of NYMC’s Graduate School of Biomedical Sciences (GSBMS), professor of cell biology and anatomy, and interim chair of the Department of Biochemistry and Molecular Biology, who serves as director of WISE.
Over the summer of 2023, WISE hosted a Summer Trainees in Academic Research (STAR) Program, welcoming six students from TU Lander College for Women to participate in a six-to-eight-week program conducting research under the mentorship of NYMC faculty. “The WISE-STAR program provides the initial exposure of future women in biomedical science to basic translational research opportunities during their undergraduate education. It aims to strengthen their continued passion in biomedical careers and further incubate their future scientific entrepreneurship ambitions,” said Austin

M. Guo, Ph.D., assistant professor of pharmacology, program director of GSBMS’ Interdisciplinary Biomedical Science Program, and director of the WISE-STAR Program.
Participants were selected for their strong undergraduate academics and desire for a future health care career. Leah Gutman, who is pursuing a Bachelor of Science degree and expects to graduate in 2025, investigated cancer dormancy in the laboratory of Julie Di Martino, Ph.D., assistant professor of cell biology and anatomy.
“The chance to participate in this program was a remarkable opportunity to see how discoveries in science come about. I learned about the tremendous amount of research, time, and effort that goes into a scientific discovery. In addition, I have a better understanding of tumor cells and will use that as a foundation for further
analysis on this topic,” said Gutman who aspires to go to medical school. “The WISE-STAR program allowed me to gain hands-on experience while developing lab skills. Learning new lab techniques and implementing them into the research process was invigorating.”
Another WISE-STAR participant was Rachel Kasztl, a biology major with the goal of attending graduate school and earning a Ph.D. She worked in the laboratory of Xiu-Min Li, M.D, M.S., professor of pathology, microbiology, and immunology and of otolaryngology, and was mentored by GSBMS students Daniel Kopulos, M.S. candidate; Fariba Ardalani, M.S., Ph.D. candidate; and Ibrahim Musa, Ph.D. ’23, post-doctoral fellow.
Kasztl spent time in the lab learning skills and procedures, running assays, as well as reading scientific papers and literature. “I started an experiment in which I cultured U266 cells with Berberine and then ran an ELISA to determine IgA levels. That experiment is still underway and is just a step in a much larger research question, so there is no title yet,” said Kasztl. “I had experience with PCR, cultured mammalian cells, and related skills in my previous lab internships, but had never run an ELISA. I also wanted to be able to immerse myself in the scientific literature on a topic for which I did not have a background on to improve my scientific literacy skills.”
Kasztl is appreciative of her time at WISE and NYMC. “The Ph.D. and master’s students I worked with were passionate, focused, and incredibly knowledgeable. They were amazing teachers,” she said. “I fine-tuned my abilities to work under the hood and cell culture. These skills are incredibly important in any lab, so I will definitely use these skills in the future.”
WISE is also supporting Master of Science students in the GSBMS with scholarships awarded to students who show dedicated interest in womencentered entrepreneurship in the field of biomedical sciences. ■
The New York Medical College (NYMC) community buzzed with excitement and anticipation as the Class of 2023 celebrated their dedication to medicine, biomedical science, and the health sciences, and looked onward to the journey that lies ahead of them. Behind Sunshine Cottage, families, friends and faculty gathered to commemorate the graduates for their time at the College, on May 22, 23, and 24. With the beaming sun and rich greenery of the NYMC campus, the graduates glowed as they solidified their commitment to their respective professions. The three ceremonies—the


Graduate School of Biomedical Sciences (GSBMS) on May 22, the School of Medicine (SOM) on May 23, and the School of Health Sciences and Practice (SHSP) on May 24—conferred 389 degrees to the Class of 2023, including 207 doctor of medicine (M.D.) degrees; 41 doctor of physical therapy (D.P.T.) degrees; 9 doctor of philosophy (Ph.D.) degrees; 76 master of science (M.S.) degrees; 49 master of public health (M.P.H.) degrees; and 7 doctor of public health (Dr.P.H.) degrees.
Students and guests at the GSBMS ceremony welcomed commencement
speaker Jeffrey M. Friedman, M.D., Ph.D., Marilyn M. Simpson Professor, The Rockefeller University investigator at the Howard Hughes Medical Institute and director of the Starr Foundation Center for Human Genetics, who spoke about overcoming obstacles that can be a defining moment. The SOM heard remarks from Machelle H. Allen, M.D., senior vice president and deputy chief medical officer of NYC Health + Hospitals Corporation, who spoke about finding her purpose in medicine. The SHSP’s speaker Ann Kurth, Ph.D., RN, CNM, MPH, FAAN, FACNM, president of the New







York Academy of Medicine (NYAM) and the first epidemiologist to head NYAM in its 175-year history, remarked on the importance of the students entering public health today.
Alan Kadish, M.D., president of Touro University and NYMC, took the stage at the ceremonies with advice for the soonto-be life sciences professionals about work-life balance. “Rather than viewing work and life as two distinct poles, view work as a part of what we are here for,” said Dr. Kadish. “And of course, your need to spend time for yourself, but

through your work in the great profession of being a physician, you use that time to develop yourself personally, but more importantly to give back to society and particularly those members of society who are most in need of it.”
At the conclusion of each ceremony, Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, left the newly minted NYMC alumni with a charge and parting words. “While you have been with us, we have strived to impart both values and knowledge because wisdom occurs at the



confluence of knowledge and values,” said Dr. Halperin. “We confidently send you forth well prepared for the challenges posed by your respective disciplines. As you go forward, I charge you to commit yourselves to the highest professional and ethical standards, to render to all people the dignity that is rightfully theirs, to remember that you are stewards of the connected human family, to be compassionate to those in need, and to remember with pride New York Medical College—as we will proudly remember you.” ■




Kenneth Knapp, Ph.D., assistant professor of public health, was appointed chair of the Department Public Health in the School of Health Sciences and Practice (SHSP), after serving as interim chair since June 2023. He also serves as director of the Center for Long-Term Care in SHSP’s Institute of Public Health and as director of the Dr.P.H. program.
Dr. Knapp has 30 years of teaching experience at the undergraduate, master’s and doctoral levels—with the last 13 years at New York Medical College (NYMC) teaching courses in health economics, social determinants of health, health services research, Stata, and others.
“Dr. Knapp takes the helm of our public health program at an exciting time,” said Robert W. Amler, M.D., M.B.A., dean of the SHSP and vice president for government affairs. “Thanks to his insight and sensitivities to the needs of our master’s and doctoral students, we now offer a spectrum of academic
Dr. Knapp takes the helm of our public health program at an exciting time.
Dr. Amler
options that focus on the career goals and priorities they hold most dear.”
An economist who specializes in gerontology, Dr. Knapp’s scholarship includes co-authoring publications in peer-reviewed journals, including International Psychogeriatrics, Innovation in Aging, Cogent Social Sciences, Journal of Public Health, World Journal of Social Science Research, Journal of Patient Safety, and most recently in Preventing Chronic Disease. A 2021 co-authored article on cognitive decline among family caregivers was published in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report—the first ever by NYMC faculty. Dr. Knapp has also conducted research for AARP’s Public Policy Institute, the Health and Hospital Corporation of New York City, and the New York City Department of Health and Mental Hygiene, Bureau of HIV Prevention and Control. He has also contributed to book chapters on housing and living arrangements of older people.
Dr. Knapp was an original member of the interdisciplinary research team at the International Longevity Center, a nonprofit think-tank led by Pulitzer Prize-winning author and geriatrician Robert N. Butler. He previously served as visiting assistant professor in the Master of Health Administration program at Seton Hall University. He serves as a senior associate for China America Living Arts, a nonprofit organization dedicated to the promotion of traditional and contemporary Chinese and cross-cultural arts through education and research.
Dr. Knapp earned an M.A. from the City College of New York, and a Ph.D. in economics from the Graduate School and University Center, City University of New York. ■

Robert D. Holland, M.D., M.H.A., was appointed as the Catherine and Vladislav P. Hinterbuchner Professor and Chair of the Department of Rehabilitation Medicine at New York Medical College (NYMC) and director of rehabilitation medicine at NYC Health + Hospitals/ Metropolitan, a major clinical affiliate of NYMC. Dr. Holland brings a wealth of invaluable clinical and visionary leadership experience.
“Dr. Holland will bring valuable expertise in rehabilitation medicine to his new role, and I am confident he will be an exemplary clinician, educator, and administrator for students, residents, faculty, and patients,” said Neil W. Schluger, M.D., dean of the School of Medicine and professor of medicine.
With decades of experience, Dr. Holland most recently served as medical director of Mount Sinai’s Amsterdam Nursing Home and Rehabilitation Center in New York City. He also served as the medical
“Dr.
Holland will bring valuable expertise in rehabilitation medicine to his new role, and I am confident he will be an exemplary clinician, educator, and administrator for students, residents, faculty, and patients.
Dr. Schluger
”director of the Consumer Directed Personal Assistance Program of the Rockland County Department of Social Services, in Pomona, New York. Prior to that, he held esteemed positions as chief medical officer of the Dr. Susan Smith McKinney Nursing and Rehabilitation Center in Brooklyn, New York; senior medical director of OrthoNet, LLC, in White Plains, New York; and director of musculoskeletal rehabilitation and attending physician at Helen Hayes Hospital in West Haverstraw, New York. He has also been an attending physician at Westchester Medical Center and Staten Island University Hospital. He previously held an academic appointment as assistant professor of clinical rehabilitation at Columbia University.
In addition to his prolific medical career, Dr. Holland serves as a skilled flight surgeon with the U.S. Air Force Air National Guard, 105th Medical Group. Board-certified in physical medicine and rehabilitation, he also holds a master’s
degree in health care administration from Columbia University in New York. He completed an internship at St. Barnabas Medical Center in New Jersey and a residency in physical medicine and rehabilitation at Boston Medical Center.
The Hinterbuchner Chair was generously gifted in 2017 by the estate of Catherine Hinterbuchner, M.D., who had the distinction of being both the first female chair of the Department of Rehabilitation Medicine at NYMC and the College’s first residency program director in the specialty, as well as Metropolitan’s first chief of rehabilitation medicine. ■
Not all roads lead students directly to New York Medical College. Some are more circuitous than others, making the journey more meaningful.
 BY KIARA R. THOMAS M.A., WITH TYLER J. LANDIS, M.B.A.
BY KIARA R. THOMAS M.A., WITH TYLER J. LANDIS, M.B.A.
Every student at New York Medical College (NYMC) brings a unique story—some fresh from undergrad, others after years in diverse careers. Six NYMC students from the School of Medicine (SOM), School of Health Sciences and Practice (SHSP), and Graduate School of Biomedical Sciences (GSBMS), share the paths that led them to the College, enriching the campus community and their future professions with diverse experiences.


“The end product is this beautiful thing that seems so effortless, but the training is not that at all—it’s structured and regimented,” says Tara Jarboe, M.S. ’19, speaking of ballet. Like many dance professionals, Jarboe, a fifth-year Ph.D. candidate in the GSBMS, began her training early at the age of six, embarking on a path that involved rigorous ballet lessons every day throughout middle school and high school. But when her mother’s cousin was diagnosed with pancreatic cancer and she saw how fast the disease progressed, she knew she wanted a career in cancer research.
Like many young ballet dancers who aspire to have professional careers, Jarboe had to decide whether to pursue ballet after high school or go to college because of the physical strain
Fewer than two percent of the 460,000 National Collegiate Athletic Association student-athletes go pro, and medical school acceptance rates average just five percent. Despite these odds, James Williams, SOM Class of 2025, a former National Football League (NFL) offensive lineman, pursued admission to NYMC’s SOM.
In 2010, Williams inked a free-agent contract with the Tampa Bay Buccaneers after an illustrious playing career during his undergraduate years at Harvard University. One of the nation’s premier linemen, he earned three All-American selections and was a unanimous choice All-Ivy League pick three times. Williams achieved the remarkable feat of starting every game for the Crimson from his sophomore to senior seasons, a rarity in football due to its high injury rate.
The physical toll of the sport manifested in multiple injuries upon Williams’ entry into the NFL. Released by the Buccaneers after one season, he then signed with the Indianapolis Colts. Despite enduring injuries during preseason camp, he
that ballet imposes on the body and the constraints that arise as the body matures. Ultimately, Jarboe went to Wake Forest University in Winston-Salem, North Carolina, as she always planned. She received her Bachelor of Science in chemistry and double minored in biology and dance. After college, she knew it was now or never if she wanted a professional ballet career. For five years, her career blossomed. Jarboe was a dance instructor at the Mill Ballet School in Lambertville, New Jersey, as well as a dancer and assistant rehearsal director at the Roxey Ballet Company. She played leading roles, including the Snow Queen from the Nutcracker, Frida Kahlo, and was also featured on National Geographic’s Instagram account.
As dancing became harder on her body, Jarboe decided to go to NYMC in 2017 for her master’s in microbiology and immunology. After graduating, she became an adjunct professor at
Manhattanville College in 2020 while pursuing her Ph.D. in microbiology and immunology at NYMC. Her dissertation, with the help of her mentors Raj K. Tiwari, Ph.D., professor of pathology, microbiology, and immunology and associate professor of otolaryngology; and Xiu-Min Li, M.D., M.S., professor of pathology, microbiology, and immunology; focuses on how the natural compound berberine is able to remodel fatal anaplastic thyroid cancer properties to make it more amenable to therapy.
“It is so important to me that information is passed onto the future generations so that ideas and education can continue with good integrity,” says Jarboe. “I feel like that with dance, and I also feel like that with teaching science.”
A teacher at heart, Jarboe wants to stay in academia feeding the minds of the next generation and contributing to the world of cancer research.
secured a spot on the Colts’ practice squad the following year. Unfortunately, a Lisfranc injury during preseason hindered his dreams of a prolonged NFL tenure. “That was pretty much career-ending. I could never get my foot back to the way it was before,” he explains.
Transitioning from the NFL to NYMC was not instantaneous for Williams. He worked as a personal trainer and a pre-loader for UPS while obtaining a postbaccalaureate certificate in pre-medicine from the University of Massachusetts Dartmouth.
As an economics major at Harvard, he lacked the necessary prerequisite courses for medical school. To bridge this gap, Williams assisted his mother, Jennifer Smith-Williams, D.D.S., a dentist whose oral surgery practice suffered staffing shortages during the COVID-19 pandemic, balancing fulltime work with MCAT preparation.
Attributing his success in medical school to consistency and unwavering selfbelief, Williams expresses gratitude for guidance from NYMC faculty, including
Mill Etienne, M.D. ‘02, M.P.H., FAAN, FAES, vice chancellor for diversity and inclusion, SOM associate dean for student affairs, and professor of neurology and of medicine.

Williams’ support in medicine runs deep. Besides his mother, his father, Martin J. Williams, M.D., a critical care surgeon, inspired him to earn a medical degree.
Reflecting on his father’s impactful career in under-resourced communities, Williams has an interest in specializing in orthopedic surgery, a field that has intrigued him since he suffered his bonerelated injuries in the NFL.
Looking ahead to his graduation from NYMC and the attainment of the title James Williams, M.D. ’25, he will join the less than six percent of Black doctors in the U.S.—beating the odds once again.

Rommel Torres, M.B.A., Doctor of Physical Therapy (D.P.T.) Class of 2025 in the SHSP, looks forward to graduating and starting his career. Since earning his bachelors in sports management and a minor in business administration from St. John’s University in Queens, New York, Torres dreamed about working as a chief operating officer or vice president of operations at his favorite sports team. He completed internships at the Brooklyn Nets, New York Islanders, as well as college teams, including Hofstra University. “But working in sports was a different animal,” Torres says. He worked 12-hour shifts during game nights and had to be back at the office the next day. He also was in sales, the starting point for many executives, and realized he had a long way to go up the corporate ladder.
When he realized that sales and the structure of the industry was not for him, he changed jobs and worked at Montefiore Medical Center and the Montefiore Health System for five years. He quickly moved up the ranks to project manager, working in different departments to advance his career. He also earned his M.B.A. in management with an advanced certificate in health care management and other certifications to help his career, but he still felt something was missing.
In 2018, Torres suffered a knee injury while doing CrossFit and his physician advised him to see a physical therapist. “I thoroughly enjoyed going to physical therapy, working hard to heal, and then interacting with my therapist,” says Torres, who later asked his physical therapist about a possible career change. “You should absolutely go back to school for PT. Do not even think twice about going. Just go,” his physical therapist advised.
Torres became a physical therapy aide at Westmed Medical Group in Stamford, Connecticut, for two years to meet the volunteer requirement for physical therapy school. While working hands-on with his patients, Torres knew this was the career he was meant to pursue. On his last day, many of his patients teared up, thankful that Torres was there to help them through some of the toughest times of their lives.
Drawn by the cohesive community of the College and holistic approach of the physical therapy curriculum, Torres enrolled at NYMC in 2022. “My journey did come full circle,” says Torres about his journey within the sports industry. “It was a much bigger circle than I wanted it to be, but I am here now.”
At three months old, Coby Fliegelman’s, SOM Class of 2026, mother became concerned when she noticed abnormalities with her son’s hearing when playing and interacting with others. Subsequently, she brought him to be examined by Arnold P. Gold, M.D., professor of clinical neurology and pediatrics at Columbia University and founder of the Arnold P. Gold Foundation, which signature programs include the White Coat Ceremony and the Gold Humanism Honor Society. Diagnosed with bilateral profound sensorineural hearing loss, one-year-old Coby became the youngest child in the United States at the time to receive a cochlear implant in 1999. Given the experimental nature of the surgery, the doctors only implanted on one side. “Without Dr. Gold’s compassion, kindness, and willingness to listen to my parents, I would probably still be living in a silent world,” says Fliegelman.
Going through an additional round of cochlear implantation to receive his second implant at seven years old and interacting with surgeons, audiologists, otolaryngologists, anesthesiologists, and speech therapists, Fliegelman knew what his career path would be. “Medicine speaks to me,” he says. “How I am able to connect with patients and really transform what their future lives may look like is remarkable. I am thankful for my family and the medical team that helped me for all those years. This is just one of the ways I want to give back.”
Always ready to lend a helping hand, Fliegelman offers words of support and encouragement to the parents of newborns and children he mentors who are hearing impaired and struggling with self-esteem and connecting with their peers. He aims to guide others through the hurdles he once faced, offering the same kindness and solace he received during his youth.
Graduating as valedictorian from Touro University’s Lander College of Arts and Sciences, Fliegelman says it was a “no brainer” when he submitted his application to NYMC. “I heard from previous students about how accommodating the NYMC community is and how collegial and warm the faculty at the College are,” he says. “One of the things that I felt was important was being in an environment where I would not feel less than or feel that I would need to bend my back over to get the accommodations that I need for my unique circumstance.” As Fliegelman approaches his clerkships in medical school, the lessons he learned from his medical team, all those years ago, stay with him: to actively listen to his patients and be a humanistic physician.


While providing dental care for children with special needs in India during the COVID-19 pandemic, Anushka Parakh, B.D.S., Speech-Language Pathology (SLP) Class of 2024 in the SHSP, noticed a change with her patients. The disruption in their routines triggered alterations in their diets, with more snacking, lapses in dental visits, heightened dental pain, and mood and behavioral challenges. “When I researched about how I could help the parents manage their child’s behavior better, is when I realized SLP could be something that I could look at as a possible avenue for a career,” recalls Parakh.
Through extensive research, she delved into the realms of feeding therapy and other therapeutic approaches to enhance the well-being of her patients. This exploration ultimately inspired her to specialize in pediatric dysphagia and early intervention, a decision made after nearly two years of practicing as a dentist. “I have spoken to many parents who have children with special medical needs, and they are so concerned about their children’s medical conditions that their oral hygiene and access to therapies sometimes take a backseat, which is understandable,” says Parakh.
Parakh’s fervent dedication in dentistry drove her to volunteer at two non-governmental organizations, where she provided oral hygiene education and dental treatments to children and adults with special needs. She also holds a patent for a toothbrush designed to assist the visually impaired. Moreover, she collaborated with the head of pediatrics at her dental school to publish a book on dental hygiene in Braille, showcasing her commitment to inclusivity in health care. They donated copies of the book to the library of a school in Karnataka, India, to help with the oral hygiene of the children who were visually impaired.
Pursuing her education in the United States, Parakh intentionally embarked on her SLP career at NYMC. “The faculty at the College have been very considerate and eager to teach. I really love that about the school. It is not all about getting work done and getting good grades. The College is very holistic.”
In terms of plans after graduation, Parakh sees herself opening a comprehensive clinic for dentistry and speechlanguage pathology after working alongside her fellow speech-language pathologists in the States. “I have come to appreciate the kind of work SLPs do because they make a difference in every patient’s day-to-day life. I feel very humbled to be able to learn how I can help someone regain the skills they once knew how to do.”
Despite getting her Ph.D. in cognitive science at Columbia University and having a successful career in health care technology, Anita Krishnan, Ph.D., SOM Class of 2024, longed to go to medical school. “It was not that I had not thought about it before” Krishnan recalls. “My father is a surgeon and a humanitarian. As a child, I deeply appreciated the broad reach and tangible impact he had on the communities he served at home and abroad.” The sharp cultural contrast she experienced growing up in a small Southern town as the child of Indian immigrants, however, shaped her interest in how people build knowledge, make decisions, and perceive “truths” in their environments, leading her to study cognitive science. While she gained clarity on her draw to medicine early during her Ph.D., the idea of pivoting to medical school then seemed increasingly farfetched as she advanced in her doctoral scholarship.
It was when Krishnan became sick and required multiple surgeries, that she reevaluated her life priorities and how she derived meaning on a day-to-day basis. “I was not going to live with this regret any longer,” she says. “The more I experienced personal and professional growth, the more compelling, or louder, my calling to medicine became. Prior to my experience as a patient, it seemed a little absurd to leave for school at the height of my professional momentum. I attempted to satisfy the calling in other ways, but there was an undeniable gap that persisted.” Krishnan knew the profound privilege it was to help someone in need, as her doctors did during one of the most vulnerable times in her life and from watching her father devote himself to caring for his patients. “Medicine, for me, is a vehicle for service, but one that is utterly distinct in the way it fuels my curiosities and nurtures my spirit without limits.”

Since childhood, Krishnan has been highly sensitive to the pain of others and developed a passion for trying to mitigate that pain for all beings. She has worked with under-resourced populations in the U.S. and India for years, ranging from providing support to individuals in prisons who are HIV-positive, to supporting young mothers battling substance use, to championing animal welfare causes, among many others. In addition to her personal service endeavors, Krishnan is a director of philanthropy at her husband’s charitable foundation. The foundation helps to amplify the work of organizations serving the under-resourced through funding, agenda-setting, and hands-on work. In this role, Krishnan further solidifies her commitment to the wellbeing of marginalized communities, in particular.
When she stepped on NYMC’s campus, she felt warmth and community. “I was looking into the College and was struck by many of the amazing faculty members. There is genuine camaraderie among the students, which I highly value and can be a rarity in medical schools.” Looking forward to the career she is destined for, Krishnan is ready to start a residency in internal medicine on her path to becoming a critical care physician. She is guided now by the bright light inside of her that has been flickering for years. ■
As one of today’s most prevalent—and most complex—chronic diseases, obesity warrants less stigma and over-simplification, and more empathetic, evidencebased approaches. From genetic detective work to smell-and-taste perception, New York Medical College (NYMC) is modeling best practices for advanced treatment, preventative care, and even novel therapeutics.
BY MELISSA F. PHETERSON

With two-thirds of Americans struggling with excess weight, obesity is more prevalent than ever. Yet surrounding bias and stigma can obstruct proper management and care. In response, six leading obesity treatment and prevention organizations issued a consensus in 2022: Obesity is a highly prevalent chronic disease characterized by excessive fat accumulation or distribution that presents a risk to health and requires lifelong care. Virtually every system in the body is affected by obesity. Major chronic diseases associated with obesity include diabetes, heart disease, and cancer.
“Obesity is a complex medical condition that is not just a matter of willpower, vanity, eating less, or moving more,” says endocrinologist Jamie Mullally, M.D., associate professor of medicine at NYMC and medical director of obesity medicine at Westchester Medical Center. “As one of today’s most prevalent chronic diseases, obesity increases the risk of numerous adverse health outcomes—diabetes, heart disease, even death.”
Obesity is defined as a Body Mass Index (BMI)—the measure of weight relative to height—above 30. Traditionally, health care providers have focused on treating the consequences of obesity, such as high blood pressure and cholesterol. “Doctors would
prescribe medications without regard for side effects—like weight gain,” says Dr. Mullally. Doctors might also ascribe joint pain and other mobility issues to excess weight, without ruling out underlying medical issues like a torn meniscus or herniated disc. Advising those patients to exercise for weight loss creates a vicious cycle. It was only in 2013 that the American Medical Association (AMA) recognized obesity as a chronic disease and should be treated as such.
Dr. Mullally trained with Louis J. Aronne, M.D., an obesity medicine pioneer, who realized the benefits of a nuanced approach, such as exploring alternatives to medications that contributed to weight gain. That “tremendous paradigm shift” inspired Dr. Mullally to become certified in obesity medicine. In her endocrinology practice, about half of the patients have obesity. “Each one has a unique treatment path,” she says. “We discuss their weight history, lifestyle, and health; and I make a point of using language that de-stigmatizes: a person with obesity, severe, or Class III instead of morbid.” She also reassures them up front: obesity is not their fault.

“Discovery is driven by teamwork. I cannot thank NYMC enough for all its resources and support in terms of clinicians, faculty members, and students.
Dr. Schwartzman
”

“Hearing this can be very impactful,” she says. “Other doctors may have dismissed their medical issues as a consequence of their excess weight. Many health care providers, unfortunately, still hold stereotypes that patients with obesity are lazy and lack willpower, despite scientific evidence that weight is under the complex regulation of biological, neuro-hormonal, genetic, and environmental factors. This stigma can cause irreparable harm.”
Maintaining an active lifestyle is key to all weight loss, says Dr. Mullally. Drastically reducing calories by dieting only works in the short term—then backfires. “Our bodies are designed to defend a higher weight,” she explains. “When you are using willpower to restrict eating, your metabolism slows.” The body, perceiving the threat of scarcity, slips into starvation mode, increasing hunger signals and slowing energy expenditure. “So, the physiology of weight loss is working against you.”
The physiology of weight gain also drives the “hunger-obesity paradox,” which physicians and nutritionists observe in those contending with food insecurity. Diane Lindsay-Adler, M.S., RDN, CDN, clinical assistant professor of pediatrics and adjunct assistant professor of public health, is a registered dietitian at Boston Children’s Health Physicians, where she supports children with obesity– some as young as five. In children, obesity is defined as BMI at or above 95th percentile, though Lindsay-Adler prefers to examine body composition: ratio of fat to muscle to water.
Children with obesity may also be malnourished and foodinsecure, she explains, due to their high intake of low-cost, high-calorie food. In addition, “they might have cyclical food restrictions which results in adverse metabolic responses,” prompting the body to hoard calories as it anticipates scarcity. “Food insecurity and obesity are linked in a vicious cycle. Poor dietary intake contributes to obesity and its physiological, physical, and social consequences—from high blood pressure and diabetes to asthma, depression, and social stigma.”
Recent breakthroughs in medications are also changing the landscape of treatment.
“This is an exciting time for the medical management of obesity,” says Dr. Mullally. “There have been huge advances in the field that are game-changing. In our clinical practice, we are seeing patients on these medications achieve more than 16 to 22 percent weight loss.”

Determining the best medications relies on a thorough understanding of each patient’s obesity. “Is the patient eating in response to cravings or food addiction? Then we might try a drug which adjusts dopamine levels and is also used for smoking cessation. If a patient never feels full, one that mimics the gut hormone which slows digestion and signals fullness to the brain could help.” As the Food and Drug Administration approves more weight-loss drugs, Dr. Mullally hopes that insurance companies will broaden coverage for these medications.
Lindsay-Adler also sees promise in new medications, especially for teenagers. “No matter how hard they try, my patients may be working against a genetic predisposition or struggling with food insecurity,” she says.
Medication is just one piece of the puzzle. The big picture involves mindful eating, frequent movement, and general wellness.
“We promote the idea of starting small, like walking five minutes a day or doing five wall-presses,” Dr. Mullally says. “We discuss the importance of awareness: patients weighing themselves, noticing gains or plateaus, logging their food intake. When people start to snack, especially in the evenings, they are often not aware of the calories they are consuming.” She also taps into the network of WMCHealth, referring patients to cardiologists, gastroenterologists, and orthopedists—and lately, sleep specialists. “Sleeping poorly can dysregulate hormones linked to weight gain,” she explains. “Obstructive sleep apnea is under-diagnosed among patients with obesity and can improve with treatment.”
Rather than a target weight or BMI, Dr. Mullally’s goal is for patients to simply regain control of their health. “We know that even five to 10 percent weight loss can improve diabetes and blood sugar levels, cholesterol levels, fat accumulation in the liver, joint pain, and heart health,” she says. “My patients and I discuss their metabolic health,” which involves advisable ranges of blood sugar, blood pressure, waist circumference, cholesterol, and triglycerides. “But we also look at physical condition and quality of life: their ability to remain active by doing the things they want to do.”
Lindsay-Adler also grounds her counsel in patient education, offering guidance on how to plan, shop, and prepare healthy food on a budget. Among children and teenagers in food insecure households, she says, French fries account for the greatest portion of total vegetable intake. “If I can teach families to carve out time for meal prepping, they can grab healthy food from the fridge or freezer instead of grabbing McDonald’s,” she says. “I show them how to use unit pricing, read nutrition labels, buy frozen fruits and veggies. My goal is to empower individuals.”
Lindsay-Adler also works with patients at the Children’s Environmental Health Center of the Hudson Valley, a collaborative enterprise affiliated with NYMC to protect children against toxins, pollutants, and other hazards. As the country’s only center of its kind based out of the Division of Pediatric Pulmonology, it offers Lindsay-Adler access to children with both asthma and obesity, who often have complex medical issues and reduced responses to medications. “Carrying around extra weight makes it harder to breathe.”
Lindsay-Adler’s most recent work, for which she was recognized at the Second Annual Leonard Newman, M.D. ’70, Assistant Professor Research Symposium, assesses the taste and smell sensitivity in children with obesity and asthma. To test existing evidence that children with obesity and children with asthma had decreased perception of taste and smell, she created four groups—including those with asthma, obesity, and both conditions—and gave them smell sticks, taste strips, strips to gauge bitterness sensitivity, and a sino-nasal outcome test to evaluate the condition of the nasal cavity.
Lindsay-Adler then classified patients into three categories: non-tasters, normal tasters, and super-tasters. Although no differences in taste and smell sensitivities were observed among the groups, Lindsay-Adler found that children with obesity—with and without asthma—reported significantly worse nasal blockage, sneezing, and ear pain, as well as higher levels of frustration, restlessness, and irritability than children at healthy weights. Further investigation will explore whether treatment aimed at decreasing sino-nasal symptoms, both physical and emotional, might better address obesity-related conditions.
Lindsay-Adler’s research into the relationship between taste and smell sensitivity in children with obesity and asthma is supported by a grant from the Pediatric Nutrition Practice Group, a dietetic
practice group under the umbrella of the Academy of Nutrition and Dietetics. The data she has collected is now under analysis, in preparation for submission to academic journals.
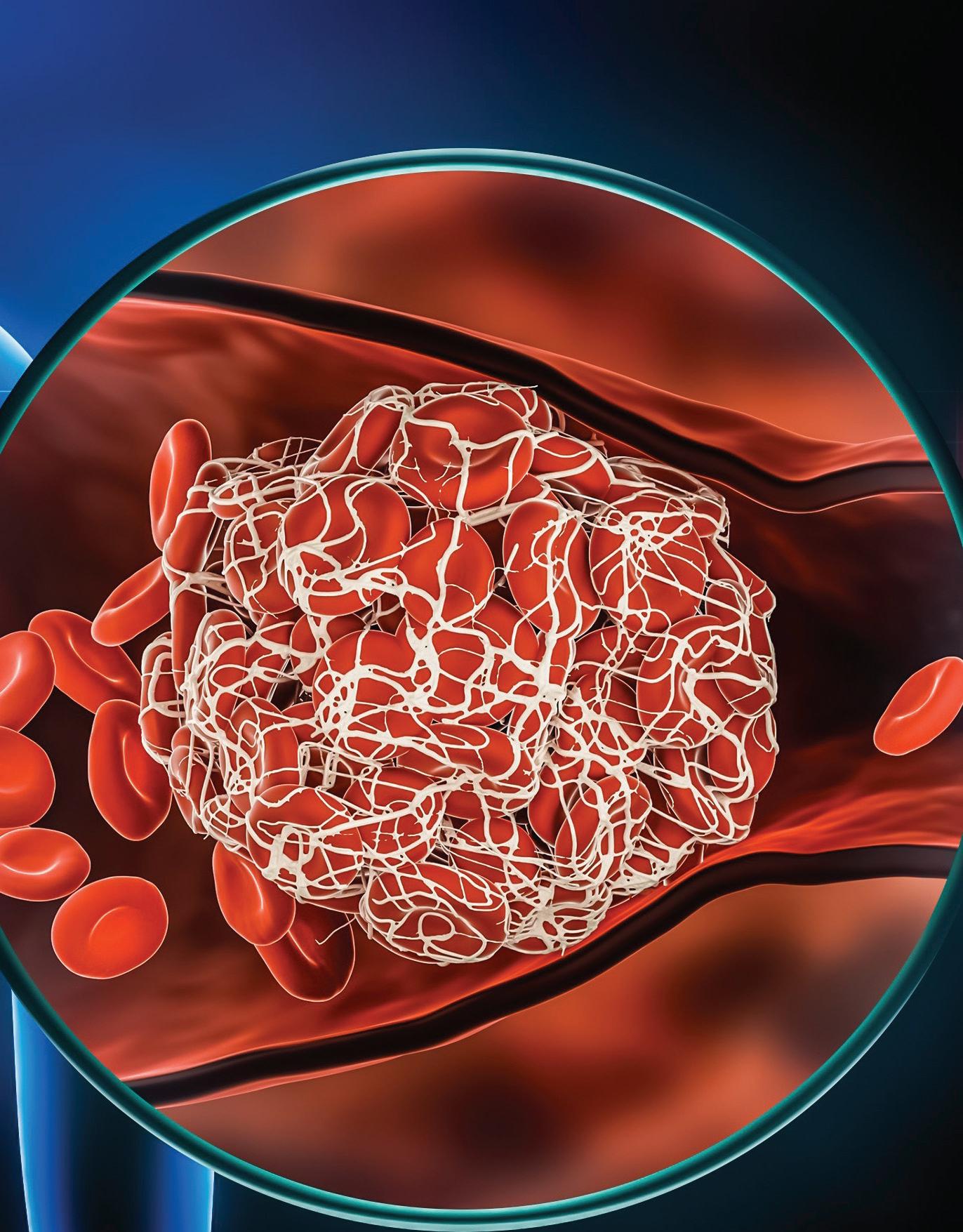
How did NYMC blaze a trail toward a major therapeutic breakthrough for obesity? “It started with scientific curiosity,” says Michal Laniado Schwartzman, Ph.D., professor and chair of pharmacology. Several years ago, her colleague Nader G. Abraham, Ph.D., former professor of medicine and pharmacology, asked Dr. Schwartzman to assist with experiments in mice regarding a signaling molecule—a molecule regulating specific processes or systems in the body—called 20-Hydroxyeicosatetraenoic acid (20HETE). As a pro-inflammatory lipid (fat) mediator, 20-HETE has been observed to damage vascular function and increase blood pressure. When mice are given testosterone, their 20-HETE levels spike.
“In humans, production of 20-HETE increases in response to injury, stroke, or heart attack, as well as in response to diets enriched in fat,” explains Dr. Schwartzman. “We know that obesity sets in motion this chain reaction toward a higher risk of cardiovascular and metabolic disease such as diabetes, hypertension, cardiac failure, and vascular dysfunction. The biological activity of 20-HETE was somehow driving these complications.” But how?
Dr. Schwartzman’s team obtained mice bred to have increased concentrations of 20-HETE in their tissues and blood. She placed these mice on a highfat diet—pellets whose nutritional profile were akin to bacon and doughnuts. As hypothesized, those mice developed higher rates of obesity-related disease. “As BMI rises, 20-HETE goes up,” says Dr. Schwartzman.
To dig deeper, Dr. Schwartzman turned to Victor G. Garcia, Ph.D. ’15, assistant professor of pharmacology, who was then among her graduate students. Dr. Garcia accepted her challenge: pinpoint the cellular target or receptor for 20HETE—that is, the proteins within cells that respond to the signal of 20-HETE and do its bidding. In the summer of 2013, one likely candidate began to emerge: the orphan G protein-coupled receptor GPR75. On October 31, 2013, the research team received independent confirmation that 20-HETE does indeed activate GPR75. “We all gasped: ‘It turns on!’” says Dr. Garcia.
Shortly thereafter, Dr. Schwartzman reached out to Regeneron, the pharmaceutical company in

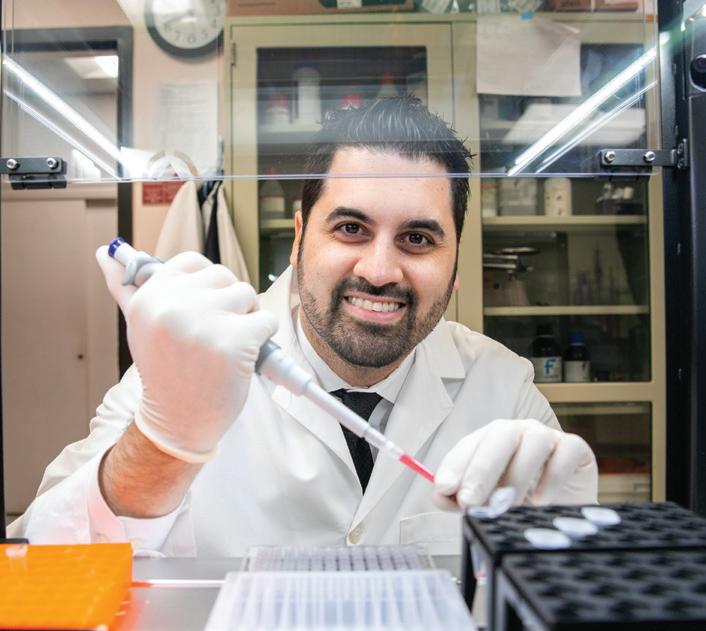
Tarrytown, New York, that frequently collaborates with NYMC. Through their VelociGene technology, Regeneron generated a colony of mice lacking GPR75 globally. The mice arrived at Dr. Schwartzman’s lab and received the same high-fat pellets as their sole source of nutrition. “Typically, a mouse on a high-fat diet will double or even triple in size,” says Dr. Garcia. But with the 20HETE signals muted from the GPR75 deficiency, these mice gained 44 percent less weight than mice consuming the same diet. The gene deficiency also offered protection from inflammation, insulin resistance, high blood pressure, and diabetes. The link between GPR75 and obesity sharpened into focus.
In 2021, Dr. Schwartzman received an urgent call from the CEO of Regeneron, who had results from a genetic sequencing of 640,000 subjects from the United States Europe and South America, conducted by Regeneron’s Genetics Center LLC. One in 3,000 of them had a “protective loss-of-function” mutation, meaning one inactive copy of the two GPR75 alleles they had received (one from each parent). These individuals had lower rates of diabetes, lower BMI, and better cardiovascular outcome—with strong parallels to the GPR75-deficient mice. All told, they had a 54 percent lower risk of obesity than those without the mutation.
An explosion of scientific interest in this “anti-obesity gene” followed the team’s published findings. In October, Dr. Schwartzman received a $2,268,684 four-year grant from the National Heart, Lung, and Blood Institute, with Dr. Garcia serving as a co-investigator, to more fully grasp the mechanisms linking GPR75 to obesity-driven metabolic and cardiovascular complications.
“For example, inflammation tends to be the villain of obesity— the bad actor who puts every system in the body on alert. We have noted that the activation of GPR75 by 20-HETE creates a major blockage of insulin action, which leads to more glucose (sugar) in the blood. We are also tracking the pathways by which inflammatory cells begin to infiltrate blood vessels.”
Additional grants awarded to Dr. Garcia including the Sinsheimer Foundation Award and an National Institutes of Health RO3 award provide additional funding to support investigation into the role of GPR75 in the pathogenesis of cardiometabolic diseases.

Guided by their findings, she and Dr. Garcia are dedicating their lab resources, including the students they mentor, to develop a GPR75 blocker known as AAA that might prevent and even reverse obesity. “Working on a drug with so much therapeutic potential is not just exciting,” says Dr. Garcia. “It is life changing.”
Dr. Schwartzman credits student involvement as key to her lab’s success. “Discovery is driven by teamwork. I cannot thank NYMC enough for all its resources and support in terms of clinicians, faculty members, and students.”
In October, Danielle Diegisser, a Ph.D. student in the Graduate School of Biomedical Sciences (GSBMS), presented her contribution to research of the GPR75 blocker, AAA, at an international conference on signaling molecules—receiving two of four awards given to NYMC students. The other two awards went to Alexandra Wolf, a Ph.D. student in the GSBMS, for her work exploring the impact of GPR75 on obesity-driven liver disease and hypertension.
“My professors and mentors at NYMC have greatly expanded my foundational knowledge for research,” Diegisser says. “Working with them has been rewarding and inspiring. I cannot wait to continue this journey with the colleagues I’ve met along the way.”
During the 2023–2024 academic year, Dr. Mullally introduced an overview of obesity medicine while teaching a physiology course, making NYMC among the first medical schools to cover the specialty. She has worked with students in the Culinary Medicine Interest Group, which promotes skills to develop nutrition-integrated care. “I am excited to offer opportunities for NYMCs students as we grow our practice—and work toward creating a state-of-the-art endocrine disease and metabolic center.” In the future, she sees promise in precision medicine based on genetic sequencing, similar to the Regeneron findings.
“With 60 to 70 percent of the population of U.S. overweight or having obesity,” says Dr. Mullally, “we are finally giving the condition its due attention; developing treatment that shows proven, promising results; and training tomorrow’s doctors for this critical specialty.” ■

Neil W. Schluger, M.D., Teaches Students to Put their Patients First with a Focus on Medicine, Public Health, Science, and Policy
Dr. Schluger’s encounters with three global health crises have significantly influenced both his approach to medical practice and his methods of education.BY ANDREA KOTT, M.P.H.
“Iwant students to think expansively about what a career in medicine means, and what it could be,”
Neil W. Schluger, M.D., dean of the School of Medicine (SOM), says with infectious zeal. “Even if they come here with an idea of what they think they want to do, I want them at some point to think about the kind of medical career they never thought of before, a career that is lasting and sustainable and could lead to something bigger.”
Dr. Schluger, who became dean in August 2023, after an international search by a committee led by Alan Kadish, M.D., president of New York Medical College and Touro University, and Kelly A. Hutcheson, M.D., M.B.A., professor and chair of the Department of Ophthalmology, speaks from personal experience. The internationally recognized pulmonologist, researcher, and educator entered medicine never anticipating the distinguished career he would enjoy. His career has taken him to some of the world’s most medically underresourced countries to care for patients, develop programs, and teach fellow physicians, and it has evolved, in part, from his willingness to think outside the box as he explored the various ways—as a clinician, lab scientist, and public health advocate—that he could put his medical degree to work. “I do not want students to come here thinking of medicine as a vocation, or that all they need is to learn vocabulary and how to manipulate instruments,” he says with a warm smile. “I want them to think about what it means, in the fullest sense of the word, to be a physician.”

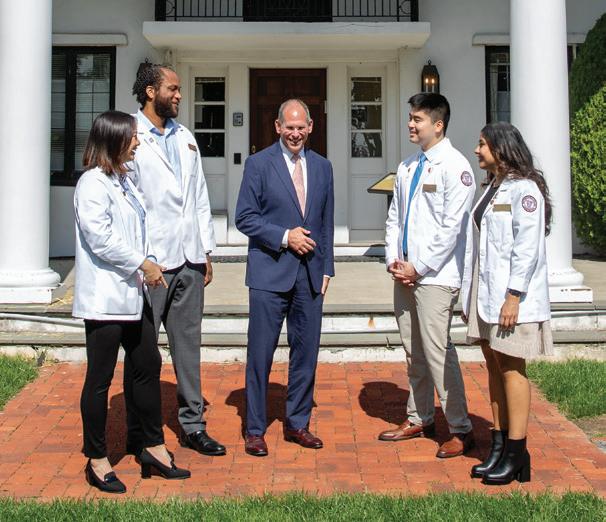

Dr. Schluger is reflective and disarmingly candid. Born in Brooklyn and raised in Queens, New York, he earned his bachelor’s degree in biology from Harvard College in 1981 and his medical degree from the University of Pennsylvania four years later. Asked about his professional trajectory, he offers with neither hesitation nor apology that he never made a conscious decision to become a doctor. Rather, he followed the footsteps of his father. His brother also became a physician, as did his wife, her brother, and her father. Three of his four children would also follow in the footsteps of their parents and become physicians.
He notes that his career in medicine began taking shape three months before he even started medical school, when a report appeared in Morbidity and Mortality Weekly Report about five men in Los Angeles who had a mysterious infection that would later be recognized as AIDS. “When I came to New York to train at St. Luke’s Hospital in 1985, it seemed like everybody who was coming in for treatment had AIDS,” he recalls. “Amidst fear and uncertainty, nobody was sure what to do, but people realized there would be a lot more than medicine involved in dealing with the epidemic.”
Dr. Schluger completed a threeyear fellowship in pulmonary and critical care medicine at the New York Hospital-Cornell Medical Center in 1992. He then joined the faculty at New York University School of Medicine and worked clinically at Bellevue Hospital, on the famed Bellevue Chest Service at the height of widespread tuberculosis (TB) in New York.
As AIDS devastated New York City and the world, the TB epidemic was also gaining steam. The effectiveness of the preferred treatment, Directly Observed Therapy (DOT), depended on clinicians being able to closely monitor patients to ensure that they took all their medications at the prescribed times. But, while directing the DOT program at Bellevue, Dr. Schluger realized that TB patients almost always had numerous coexisting morbidities and other life
complications that prevented them from complying with their therapeutic regimens. Language barriers alone hindered efforts to effectively convey the importance of following the DOT protocol with patients who came from 39 countries and spoke 13 distinct languages. In addition, poverty, homelessness and/ or substance use disorders frequently prevented patients from adhering to their TB treatment. “My colleagues and I would talk about their lack of housing or their alcohol abuse and how we could help to get them back and forth to the clinic so they could take their medication,” Dr. Schluger recounts. Gradually, he began to consider that taking TB medicines might not have been the most important thing for these patients, compared to finding a place to sleep or food to eat. “That is when I realized that when it comes to medicine, nothing occurs in a vacuum.”
During his fellowship at Cornell, Dr. Schluger spent considerable time training as a scientist in renowned basic science laboratories at Rockefeller University and the National Institutes of Health. In Rockefeller University’s Laboratory of Medical Biochemistry and in the pulmonary branch of the National Heart, Lung, and Blood Institute, Dr. Schluger encountered his newfound appreciation for science, something he hopes all medical students will experience. “If you do not think science is great, then think about the drugs that have been developed for HIV,” he says fervently. “I grew up at a time when we watched people die from this untreatable disease, and now patients are surviving on one pill a day,” he exclaims. “Because amazing science was done, there are now drugs that might make it possible for people with cystic fibrosis to lead normal lives. And hepatitis C is now curable too,” he adds.
In the ensuing years, he accepted a series of prestigious academic and clinical appointments, including as chief of the Division of Pulmonary, Allergy and Critical Care Medicine at Columbia University Irving Medical Center, where he was also professor of medicine, epidemiology, and environmental health sciences. He was also director of the Population and Global Health Track

Students come to medical school for all the right reasons, idealistic, and ambitious,” he says. “Our goal is to keep their excitement going by exposing them to clinical medicine as well as basic science, public health, and health policy, and to give them opportunities to interact with people so they can see all sorts of varying careers in medicine.”
Dr. Schluger“ ”for the Scholarly Projects Program at the Vagelos College of Physicians and Surgeons at Columbia University, and co-director of the educational program in global and population health at the school. In 2020, following his 22 years on the faculty at Columbia, he became the Barbara and William Rosenthal Professor and Chair of the Department of Medicine at New York Medical College and director of the Department of Medicine at Westchester Medical Center.
Dr. Schluger spent a great deal of his research career with the Tuberculosis Trials Consortium, an international collaboration sponsored by the U.S. Centers for Disease Control and Prevention, which he chaired from 2000 to 2016. He also taught internationally, including in India, Thailand, Zimbabwe, and Israel.
All of this led to his greatest achievement in global health: the co-founding, in 2013, of the East Africa Training Initiative (EATI), a two-year fellowship training program in pulmonary and critical care medicine and the first program of its kind in Ethiopia and the broader East African region.
With funding from the Swiss Lung Foundation and Vital Strategies, a nonprofit global public health organization that designs solutions to pressing health problems, Dr. Schluger and a team of physicians and public health officials
developed the curriculum based on the standards of the Accreditation Council for Graduate Medical Education to train pulmonary critical care fellows. Their goal was to develop a sustainable program with an all-volunteer faculty that would remain onsite in Ethiopia until they could train a sufficient number of Ethiopian physicians.
Before the program’s launch, the country had only one pulmonologist for its 110 million people. More than a decade after its founding, the program has trained the first generation of pulmonary physicians in the country and established an academically oriented pulmonary division at Ethiopia’s leading public hospital. To date, it has graduated 25 specialists, including two pediatric pulmonologists and two physicians from Rwanda and Tanzania, who have assumed leadership roles at hospitals across East Africa. At Black Lion (Tikur Anbessa) Hospital, Ethiopia’s largest public hospital and its main teaching and referral center, patients can now access advanced pulmonary services, including bronchoscopy and pulmonary function testing. The hospital’s chest clinic sees more than 500 patients monthly, while medical ICU capacity has grown substantially, and critical care ultrasound is widely used. “Ethiopia is one of the poorest countries in the world and there was nothing we

could do to change that, but the impact of the program has been magnified in many ways,” Dr. Schluger says.
By increasing the country’s capacity to train pulmonary health providers, the EATI program has dramatically increased accessibility to pulmonary health care, which has improved health equity. This sequence of improvement, starting with program development, which fueled education and training, and led to increased service delivery, health care access, and better patient outcomes, is what Dr. Schluger means when he refers to physicians “creating something lasting and sustainable that could lead to something bigger.” It is the kind of experience that has made his career so fulfilling, and that he wishes for all the College’s medical students.
“I want students to be exposed to great clinicians at the bedside and in the operating room. I want them to work in laboratories and communities. I want
them to learn to use not just their skills but also their compassion to make patients better.
Dr. Schluger
”“Students come to medical school for all the right reasons, idealistic, and ambitious,” he says. “Our goal is to keep their excitement going by exposing them to clinical medicine as well as basic science, public health, and health policy, and to give them opportunities to interact with people so they can see all sorts of varying careers in medicine.”
Dr. Schluger’s career, which exemplifies such variety, has earned him numerous accolades, including, most recently, recognition as a Crain’s New York Business 2023 Notable Health Care Leader and Westchester Magazine’s 2024 Health Care Hero. He has authored more than 200 articles, chapters, and books, which have appeared in The New England Journal of Medicine (NEJM), The Journal of the American Medical Association, The Lancet, and The Lancet Respiratory
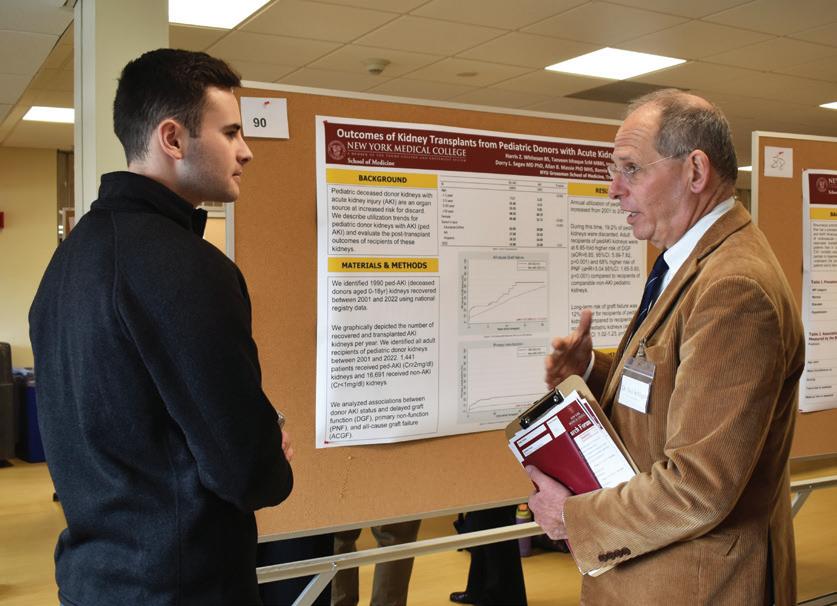
Medicine, among other leading journals. He is an associate editor of The American Journal of Respiratory and Critical Medicine, and a past president of the American Lung Association of New York. He also has written and edited several editions of The Tobacco Atlas, the definitive work describing the extent and consequences of the global epidemic of tobacco use, published by the American Cancer Society and Vital Strategies, where he serves as both a trustee and senior advisor for science.
During the COVID-19 pandemic, Dr. Schluger became an important voice as the lead author of the May 7, 2020, NEJM article, “Observational Study of Hydroxychloroquine in Hospitalized Patients with COVID-19,” which, using data from an observational trial of 1,400 patients who took hydroxychloroquine,


debunked claims about the drug’s ability to beat the virus.
In his office, gazing at a display of photographs that he has taken during his decades of global health work, Dr. Schluger ponders the term “global health,” which has encompassed so much of his career. He offers a thoughtful explanation, emphasizing that global health entails more than traveling around the world to see patients. “Global health is about justice, and justice means everyone is treated the same,” he asserts. “Everyone in the world deserves the right to live in a healthy environment with equal access to high quality care.”
With steady emphasis, he notes that the practice of global health must involve reciprocity among participants who share the knowledge, skills, and experience needed to create not only a more sustainable health care system but also more effective patient care. “Whatever we do is a two-way street,” Dr. Schluger says. “The places where we send our students should benefit as much from the work they do as our students benefit from being there.”
Describing his long-term dedication to global health is one way that he hopes to motivate and guide students toward medical careers that unfold in unexpected and wonderful ways. Another is the

weekly discussion group, “Reflections on Medicine,” that he hosts for students who want to learn about and share their own perspectives on medicine. He uses these discussions to impart his own experiences and suggestions, not to mention wisdom, which he is happy to share.
“All human beings care about the same thing: health and safety for themselves and their families,” he says. “But there is so much that goes on culturally, socially, and economically that has an impact on people’s health. Although medicine is at the heart of what physicians do—what we do is important—it is far from the only thing that’s necessary for people to be healthy.”
What it takes to be healthy, in Dr. Schluger’s view, is as multidimensional as what it means to be a physician. “As physicians, we go to work every day to make people’s lives better in some way, and it is a privilege to be able to do that,” he says. “We have status and respect and make generous incomes. Yet, there is an unwritten social contract that we get this status only as long as people think we are working in their best interests. Because, when it comes to medicine,” he says, “the most important person is the patient.”
To care for patients most effectively, a doctor must understand the circumstances of their lives. This, Dr.
Schluger explains, is why he is working hard to raise students’ awareness of the relationship between medicine and public health, as well as science and policy. “I want students to be exposed to great clinicians at the bedside and in the operating room. I want them to work in laboratories and communities. I want them to learn to use not just their skills but also their compassion to make patients better,” he says.
Medical students appreciate Dr. Schluger’s vision. “Dr. Schluger is a true advocate for students and a tremendous asset to the NYMC community. Not long after his appointment as dean, he readily met with members of the SOM Student Senate to partner on goals for the year and to offer his support of our efforts. He has also prioritized his time to offer invaluable advice regarding residency applications to our class,” says Katherine Lo, SOM Class of 2024 and president of the SOM Student Senate. “He is truly committed to the success of our students and institution, and we are grateful to have him as our dean.”
If Dr. Schluger can help students carve out meaningful medical careers by conveying his vision, then he will have achieved the bulk of what he set out to do when he assumed the position of dean. “I chose to become dean of the School of Medicine because I knew it was a unique opportunity to make an impact on somebody’s career.” ■
New York Medical College’s newest partner in health research and clinical innovation may be 2,000 miles away, but its contours perfectly map onto campus capabilities—shortening the distance from bench-to-bedside. In just two years of collaboration, the Lovelace Biomedical Research Institute and NYMC have already forged powerful ties, pilot projects, and paradigm shifts in collaborative impact.
 BY MELISSA F. PHETERSON
BY MELISSA F. PHETERSON
The city of Albuquerque, New Mexico, may evoke images of the Rio Grande, mountain ranges, and historic adobe buildings. But in this emerging hub of technology in the Southwest, one longstanding point of pride is Lovelace Biomedical Research Institute, a 75-year-old institution with three sprawling campuses, cutting-edge laboratory space, and more than 400 experts pursuing clinical and pharmaceutical breakthroughs.
In November 2019, Salomon Amar, D.D.S., Ph.D., vice president for research, senior vice president for research affairs at Touro University (TU), visited Albuquerque to explore an affiliation between Lovelace, TU and New York Medical College (NYMC), fulfilling a charge from Alan Kadish, M.D., president of TU and NYMC. Lovelace, a not-for-profit organization with a robust basic science infrastructure, is noted for its drugdevelopment laboratories and excellence in respiratory disease, neuroscience research, and toxicology. Its powerful medical imaging capabilities and high-level data analysis can identify
biomarkers—trace amounts of disease, infection, and injury— that guide new approaches to gene and cell therapy. In turn, NYMC has renowned academic specialists, interdisciplinary physicians, troves of patient data, and protocol for clinical trials to breathe viability into Lovelace’s lab work.
The missions of both institutions, their leadership realized, could be enhanced and advanced by working together, fusing their areas of expertise to expedite the process of translational science, which ushers laboratory findings into real-world applications. From a scientific perspective, specialists at each organization could pool their expertise into a collective inquiry, bridging gaps, and sharing resources. And from a practical perspective, the act of diversifying partners, much like diversifying portfolios, often leads to financial growth—in this case, from federal grants and commercial investments.
“This affiliation between Touro and Lovelace will significantly impact our research capability and expand our capacity

Lovelace’s three campuses in Albuquerque comprise more than 375,000 square feet of research lab space and receive more than $70 million per year in grants and contracts. The Institute has published thousands of research papers and employs 400 physicians, scientists, and researchers.
This affiliation between Touro and Lovelace will significantly impact our research capability and expand our capacity to make a difference in the health and lives of Americans. Together with Lovelace, Touro will be able to bring in-depth understanding of potential health risks and optimize the efficacy of pharmaceuticals.
Dr. Kadish
Dr. Amar, who is also a professor of pharmacology and of pathology, microbiology and immunology at NYMC, and professor of dental medicine at the Touro College of Dental Medicine (TCDM), helped select and recruit the five Lovelace Research Fellows on the NYMC faculty, who remain at the vanguard of collaboration. “Our Lovelace Research Fellows help integrate Lovelace’s research into the fabric and framework of Touro,” he says. “They provide Lovelace with academic expertise, patient populations, and guidance on how to apply its findings to clinical care and public health. In turn, Lovelace provides the research infrastructure that is so valuable. From this, we create ground that is extremely fertile for partnership and innovation.”
To stimulate collaboration and encourage the joint endeavors that bolster federal funding, Dr. Amar and Robert W. Rubin, Ph.D., chief executive officer at Lovelace, have developed an internal program of awarding pilot funds for joint projects, with an expedited process of review and decision. In the future, Touro and NYMC aim to operate a centralized clinical trials research office built on Lovelace’s research infrastructure. In addition, the partnership will broaden opportunities for students at NYMC and TCDM in graduate biomedical science, medical, and dental
to make a difference in the health and lives of Americans. Together with Lovelace, Touro will be able to bring in-depth understanding of potential health risks and optimize the efficacy of pharmaceuticals,” said Dr. Kadish.
The COVID-19 pandemic affirmed that it was possible to collaborate while 2,000 miles apart and leadership from both institutions continued discussions, resuming in-person visits once travel restrictions lifted. The affiliation between Lovelace and Touro/NYMC was officially announced in 2022, unleashing a surge of collaboration in the spheres of science, research, academics, and patient care.
“This affiliation is a monumental achievement, because it leverages the expertise and resources of each institution to pursue new opportunities and new heights together,” says Dr. Amar. “The notion of the ‘whole being greater than the sum of its parts’ applies perfectly as this collaboration unfolds.”



education, as Lovelace researchers join the faculty and students complete rotations at Lovelace and its surrounding community.
In an early instance of collaboration, Dr. Amar and Ted Barrett, Ph.D., senior director of pharmacology at Lovelace, executed a pilot study on an intranasally delivered COVID-19 vaccine, tapping into Lovelace’s expertise in nanoparticles and aerosol technology for what Dr. Amar calls a “proof of concept.” Further testing on the efficacy of intranasal vaccines against respiratory infections, like influenza and RSV, will rely on cooperative efforts from both organizations. “So far, we have promising data,” says Dr. Amar. “Once it is conclusive, we will go to the FDA and embark on the process of developing a clinical trial.”
“We have many mutual interests and similarities, but enough difference for us to see the value in collaboration,” says Lovelace Fellow Tracey A. Milligan, M.D., M.S., FAAN, FAES, FANA, professor and chair of neurology at NYMC and director of neurology at Westchester Medical Center (WMC). To complement her research into traumatic brain injury (TBI), she points to Lovelace’s research MRI facilities managed by experts in neuroscience. “They have outstanding resources for basic science, which complement our focus on clinical research,” she says. “It is a great opportunity for us to perform translational science,” meaning science that turns research into treatments and interventions that improve patient health. “WMC is a Level 1 trauma center, the highest level of critical care,” she says, citing plans in the future for a center for concussions and mild TBI. “In treating patients who have sustained concussions, we are looking for the biomarkers— substances in blood that indicate TBI—to help us understand more about their future risks.” That is where Lovelace’s basic science shines. “Their animal models are a reliable way to replicate the disease process and perform blood tests for biomarkers, so we can glean insight into treating our patients.” She sees great potential for developing research studies and clinical programs with Lovelace. “I grew up in Albuquerque; in
fact, my father used to work at Lovelace. It is thrilling to have Touro invest in this collaboration.”
“There are so many resources for infectious disease at Lovelace, and so many opportunities for collaboration,” says Chandra Shekhar Bakshi, DVM, Ph.D., professor of pathology, microbiology and immunology.
Dr. Bakshi, a Lovelace fellow who contributed to the intranasal vaccine study led by Dr. Amar and Dr. Barrett, sees promise for his research in Lovelace’s tightly regulated animal Biosafety Level 3 (BSL-3) facility for highly virulent organisms, in addition to its capacity to aerosolize pathogens. “Inserting droplets inside the nose is an artificial way of infecting a subject,” he explains. “In the natural world, we inhale those organisms. Lovelace’s ability to aerosolize pathogens mimics the natural infection process, which makes this approach ideal from a research standpoint.”
“
The facilities at Lovelace are spectacular, but it was the people that impressed me the most.
Another asset for research is collaboration itself. “No impactful research can be done in isolation, because not all resources exist under one roof,” he explains. “This is the era of superspecialization in a very narrow area of research. For that reason, pulling together a strong team of colleagues optimizes our chances for grant funding. As we visit Lovelace and their researchers visit us, I am seeing real integration unfold as we brainstorm and exchange scientific ideas.”
”
Dr. Dozor
Paul M. Arnaboldi, Ph.D., Lovelace fellow and assistant professor of pathology, microbiology and immunology, is gleaning data from Lovelace’s aerosol models for his research into intranasal vaccination against infectious disease an idea that originated from extensive scientific discussion involving Dr. Kadish. “Lovelace has a strong history in respiratory research that strongly aligns with my own investigations,” he says. “Mucosal surfaces are the primary entry point for most pathogens, the site where you want the greatest protection, and potentially the method to promote the most immunity.”
Dr. Arnaboldi’s project with Lovelace focuses on human adenovirus (HAdV) respiratory infections, which remain among the most prevalent causes of acute disease requiring hospitalization in children and occasionally adults. The complication is that adenovirus has many different strains; and existing vaccines are restricted to military use.
Dr. Arnaboldi collaborates with Alison A. McCormick, Ph.D., (former assistant professor of pharmaceutical sciences at Touro University California, now at UC Davis), a fellow expert in vaccine development, and Adriana Kajon, Ph.D., a senior scientist at Lovelace and expert in adenovirus research. “We have developed a nice rhythm together,” he says. Dr. McCormick oversees the production of vaccines with peptide-protein conjugates, a molecular structure that has been shown to enhance vaccine absorption and recognition by the immune system. At Lovelace, Dr. Kajon helms the testing of mice’s blood samples for virus-neutralizing activity, using the facility’s high-level data analysis. At NYMC, Dr. Arnaboldi evaluates the intensity of the immune response in mice. Their shared goal is to generate an intranasal vaccine with broad protection; develop

preliminary data to support an National Institutes of Health (NIH)-funded research program; and design antibodies that offer robust adenovirus protection for transplant recipients, cancer patients, and others with compromised immunity.
“Each of us has a strong track record in obtaining NIH funding, and that should increase exponentially when working together,” he says.
The research of Lovelace Fellow Chioma M. Okeoma, Ph.D., professor and vice chair of research in the Department of Pathology, Microbiology and Immunology, depends on catching a better glimpse of extremely tiny particles: the extracellular vesicles (EVs) released by cells. EVs carry “cargo” that yields clues about disease detection, progression, and response to treatment. “When I was recruited as a Lovelace Fellow, I thought it was a great opportunity to expand and grow recognition for EVs, which represents the largest-growing area in NIH funding,” she says. At Lovelace, she met like-minded colleagues like
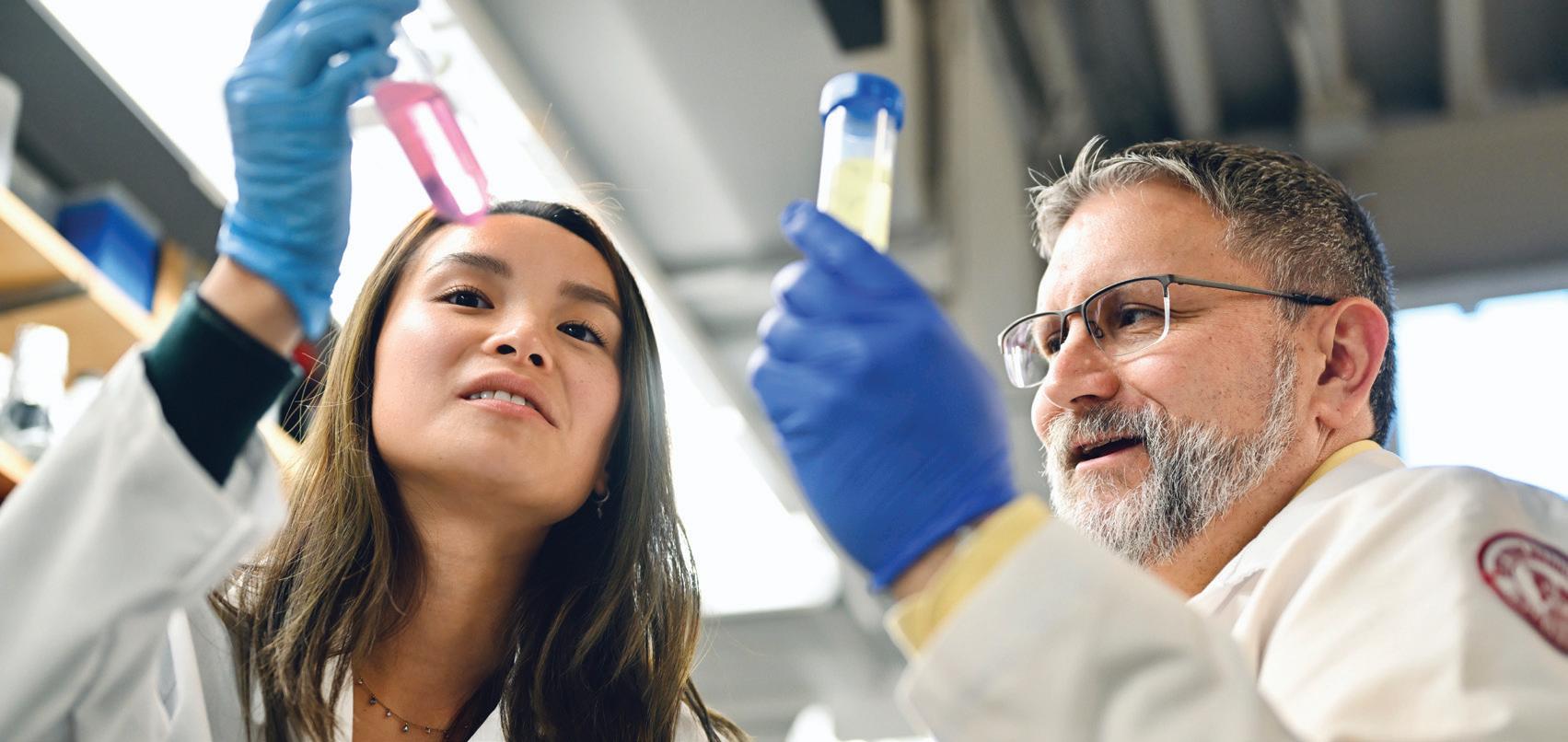


Dr. Kajon, whose focus on adenovirus can draw strength from insight into EVs. Dr. Kajon’s lab investigates how adenovirus utilizes EVs to promote pathogenesis, or disease development. Her team sends samples of inactivated EVs from adenovirusinfected cells via FedEx to Dr. Okeoma’s lab for physical assessment. Working together in biweekly virtual meetings, they have pieced together clues that EVs from cells infected with adenovirus may help spread the infection.
“Typically, the adenovirus virus kills the cell upon leaving it. But we are discovering that with the help of EVs, adenoviruses can move among cells without killing them.” To investigate further, Dr. Okeoma and Dr. Kajon are applying for grants. “By publicizing our findings, we hope to show to the world that we are successfully working together and hopefully our collaboration will lead to new insights into adenovirus pathogenesis.”
Another of Dr. Okeoma’s collaborations involves Lovelace’s access to transmission electron microscopy at the University of New Mexico that can capture detailed images of EVs from postmortem brain tissues. “We are determining whether we can use EVs from post-mortem brain tissues as biomarkers among HIV patients who died of drug overdose,” Dr. Okeoma explains. “If we generate a map of their brain, is the circuitry different than HIV patients without drug addiction—and can EVs tell us that?”
“The facilities at Lovelace are spectacular, but it was the people that impressed me the most,” recalls Lovelace Fellow Allen J. Dozor, M.D., professor of pediatrics and clinical public health, director of the Children’s Environmental Health Center of the Hudson Valley, associate physician-in-chief at Maria Fareri Children’s Hospital at WMC, and president of Boston Children’s Health Physicians. “They all are clearly top-ranked, excellent, and thoughtful scientists dedicated to performing high quality research.” As a pulmonologist, he values the legacy of William

Randolph Lovelace II, the institution’s founder. “He and the center made major contributions to our understanding of how aerosols penetrate the airways and lungs.”
Dr. Dozor is a clinical researcher with almost four decades of experience, which includes overseeing clinical trials across multiple centers. “I immediately appreciated the potential of combining the powerhouse basic scientists at Lovelace with the physician-scientists here at NYMC,” he says. “As a Lovelace Research Fellow, my major goal has been to build relationships between these groups. We bring to the table superb clinical faculty, with large patient databases to draw on for clinical trials. Their Ph.D.s bring the ability to develop the preclinical science required to bring a new therapeutic to FDA approval.” The basic concept, he adds, is simple: “Work with the scientists at Lovelace to take their basic science research and translate their discoveries into clinical trials,” with the aim of bringing a new drug to market. In the area of pulmonary disease, this might involve studies into lung function, respiratory mechanics, and sampling or sequencing patient genetics, all of which are strengths of Lovelace.
As partnerships further develop, students at NYMC will have a chance to travel to Lovelace for investigations and perhaps clinical rotations. In particular, TU plans to offer a summer program for students; and TCDM will offer dental training to students who matriculated in Valhalla. “Dr. Kadish elected as an administrative move to create an extension of our dental school in Albuquerque,” says Dr. Amar, explaining that New Mexico’s lack of dental schools creates “a segment of its population in critical need of dental services.” Once this program launches, NYMC will develop other initiatives with lodging, kosher food service, and opportunities for research, and mentorship.
The endeavors of the research scholars and their partners will open the way toward experiences for our faculty and students at Lovelace, and opportunities for Lovelace researchers to share their knowledge at NYMC.
Dr. Amar
“The endeavors of the research scholars and their partners will open the way toward experiences for our faculty and students at Lovelace, and opportunities for Lovelace researchers to share their knowledge at NYMC,” says Dr. Amar. “I look forward to witnessing the fruitful collaboration that elicits financial support. By working together, we will both remain at the forefront of biomedical research and public health.” ■
“Lung cancer, chronic obstructive pulmonary disease, and asthma are quite common, and pharmaceutical companies are enthusiastic about the potential for new drugs,” he explains. “One of my major missions has been to increase and support clinical research in the Department of Pediatrics, and I am very pleased with the significant increase in research during my tenure,” he adds. “Having Lovelace as a partner can expedite the complex, tightly regulated journey toward the clinical trials that spearhead innovation.”
 BY ANDREA KOTT, M.P.H.
BY ANDREA KOTT, M.P.H.
Qualifying for medical school once depended solely on high academic achievement. But during the past decade, admissions committees, like the New York Medical College (NYMC) School of Medicine’s (SOM), have recognized the importance of acquiring more comprehensive information about the character of potential students— and future physicians—than school transcripts alone can provide. Years before the U.S. Supreme Court ruled to outlaw affirmative action, the SOM had been expanding its approach to screening and evaluating candidates, determined to maintain its commitment to diversity and inclusion and has expanded it even further since the decision.

Featured in this expanded approach to screening and evaluation is the Multiple Mini-Interview (MMI) which is designed to assess candidates’ communication and problem-solving skills, ethical scaffolding and preparedness, and other personal traits that the SOM deems essential to becoming an effective and compassionate physician.
The Office of Admissions began using the MMI more than a decade ago, in 2012. Since the COVID-19 pandemic, it has been implementing the tool through a computer-based platform. Thus, instead of walking from room to room to meet with individual interviewers, candidates move virtually, explains Karen Murray, M.D. ’99, dean for admissions for the SOM, and assistant professor of obstetrics and gynecology. “Other than flipping to a virtual platform, the MMI process is still the same,” Dr. Murray says. “The things we are looking for in applicants are exactly the same, we
Dr. Murray ” “
It is a more holistic way of analyzing applicants than having just one interviewer relying on undergraduate grades and an MCAT score.

are using similar scenarios, it is run the same way, and interviewers come from all walks of life,” she adds.
The MMI requires each applicant to interview with eight different individuals, all volunteers from the broader NYMC community, including SOM faculty and staff members, alumni, students, allied health professionals, hospital staff, community members, and patients. These volunteers do not sit on the admissions committee, although they do receive training from the Office of Admissions. “The admissions committee and the MMI team are two separate groups of people,” Dr. Murray says.
The process begins by giving each candidate two minutes to read a scenario that is posted on the door of a virtual interview room. Then a signal sounds, and the candidate enters the room with an interviewer and engages in a focused, six-minute discussion about the scenario. Interviewers rely on this process to evaluate candidates’ life experiences and accomplishments, communication skills, aptitude for understanding medical scenarios, and overall presentation. After six minutes, an automated voice prompts them to change rooms, where they will discuss a new scenario with a different interviewer. Unlike admissions committee members, interviewers do not view candidates’ interview results or applications. “They just assess each candidate according to the six minutes they each have,” Dr. Murray says.

She considers the composite MMI score an essential component of each candidate’s well-rounded application, which also
includes GPA, MCAT scores, a personal statement, letters of recommendation, and a compilation of research, employment, community service, and other volunteer experiences. “It is a more holistic way of analyzing applicants than having just one interviewer relying on undergraduate grades and an MCAT score,” she says. Most importantly, the MMI helps to mitigate interviewers’ unconscious bias because it gives candidates multiple opportunities to demonstrate their skills, she adds.
For instance, an applicant might have average scores but exceptional life or work experiences and tremendous compassion, which are the kind of qualities that patients seek in physicians. On the other hand, an applicant might have an excellent academic record but an impersonal or arrogant manner, qualities that do not promote good doctor-patient relationships or the SOM’s values or mission. “Just because you score well does not mean you have the attributes of a good doctor,” Dr. Murray says. “The MMI gives you an idea of who each applicant is and gives them the opportunity to showcase who they are and talk about what kind of medicine they want to do, and where they see themselves in the next five or 15 years. It is a wonderful process, and it works,” she says.
Dr. Murray joined the SOM faculty in 2003 as an interviewer in the school’s then oneon-one interview process. Since taking the helm of the admissions office in 2018, her many goals have included making the admissions process more equitable for all applicants. The first step to do this effectively required diversifying the admissions committee which, at the time,
had only two members from demographic groups underrepresented in medicine (URMs) and few women. “One of the first things I noticed when I came to the admissions committee was that lack of representation, which means that if you are a woman or URM, your voice is not heard,” she says. In addition to requiring yearly anti-bias and anti-racism training for everyone, Dr. Murray launched an effort to recruit men and women of color, increasing diversity on the committee by some 25 percent.
“It is important to have the admissions committee understand the strengths
of diversity and why a medical school exists,” says Mill Etienne, M.D. ’02, M.P.H., vice chancellor of diversity and inclusion, associate dean of the SOM student affairs, and associate professor of neurology and of medicine. “We are here to improve the health of our communities and doing so requires that we have a plan to recruit future doctors who reflect the demographics of the communities they will serve,” he adds.
Dr. Murray also felt the importance of increasing the number of female members, who comprise more than half of the admissions committee today. She


is dedicating the same effort toward encouraging female medical school applicants. “When I started medical school in the early 1990s, women in white uniforms were still assumed to be nurses, since doctors traditionally had been male,” she says. “NYMC was one of the first medical schools to admit a Black woman,” she says. Indeed, more women are entering medicine than ever before, as demonstrated by last year’s class, which was 55 percent female, she says. “NYMC has always led the trends.”
In the years since Dr. Murray arrived, the SOM has doubled its number of underrepresented minorities from eight to 16 percent. In addition, the number of applicants of Korean, Chinese, East Indian, or Vietnamese descent has increased, as has the number of Jewish applicants. “We have a lot more Jewish applicants, because the school is now under the auspices of Touro University, which observes all the Jewish holidays, removing a previous challenge to observant Jewish students,” she says. “Our commitment to diversity and inclusion encompasses our accommodation for Jewish observance and culture,” says Dr. Etienne.
Yet, despite significant advances in the SOM’s URM enrollment, which has exceeded 20 percent in recent years, there have been some declines. For example, last year’s URM enrollment was only 18 percent, a dip that Dr. Murray attributes to “a lot of moving parts in the world.”
Among these moving parts is the cost of medical school tuition. Tuition at NYMC is typical of private medical schools in the U.S. but students often choose a school based on the amount of financial aid they are offered. “We accept a lot of qualified applicants, but it is difficult to hold onto them,” she explains. “We try to offer as many scholarships as we can but it is hard to compete with other schools that have more money than we do. We have had students to whom we would give a half tuition scholarship and they would come back asking for more, saying that another institution had given them a full ride, and they end up going elsewhere,” she says.
Also challenging the SOM’s efforts to increase or at least maintain URM enrollment is the recent U.S. Supreme Court ruling ending affirmative action. “That is another challenge that has gotten thrown at us this year,” Dr. Murray says. “We can no longer screen by ethnicity or race.” As a result, the school must screen according to other parameters. “As we screen for diversity, we have to make sure we come up with ways to help students come to school and support them while they’re here,” she says.
The good news is that SOM is finding other ways to welcome racially, ethnically, and socioeconomically diverse students. One way includes identifying those who qualify for the MCAT fee assessment program; represent the first generation in their family to apply to medical school; or,
fit the Association of American Medical College’s definition of ‘socioeconomically disadvantaged,’ she says.
Another way in which Dr. Murray is working to increase diversity is by collaborating closely with the Student National Medical Association to encourage undergraduate college students of color to consider medical school by inviting them to attend medical school for a day. “College students of color need to see medical students who look like them,” she says. She is also backing the SOM’s efforts to provide steady student support in the form of mental health and wellness, and academic support services. “We also have a robust pre-matriculation program through which we get students well

acclimated in the campus environment so they can have a greater sense of belonging. This has had a positive impact on academic outcomes for our students,” says Dr. Etienne.
In the years to come, maintaining its commitment to racial and ethnic, gender as well as socioeconomic diversity will likely be an ongoing challenge for the SOM. “Despite these challenges, we must not give up on our goal of doing all we can to make our communities healthier,” says Dr. Etienne. “We must make eliminating health disparities in the U.S. our next moonshot. NYMC is well positioned to lead the way in that endeavor.”
For an institution that takes credit for more than its share of firsts among medical schools, Dr. Murray says, “Nothing is impossible.” ■
The SOM Office of Admissions seeks volunteers to serve as interviewers for the Multiple Mini-Interview. Volunteers include faculty, staff, alumni, medical students and residents, nurses and other allied health professionals, public health experts, social workers, legal professionals, education experts, patient advocates, former patients, leaders of community organizations, as well as community members at large. The interview season runs from mid-September through March, with interviews taking place Mondays, Tuesdays, and Thursdays. Interviews take place on the Valhalla campus or virtually. Interviewers are asked to sign up to interview one afternoon per month and training is provided.
For additional information, please visit www.nymc.edu/mmi or call (914) 594-4507.
 BY ANDREA KOTT, M.P.H.
BY ANDREA KOTT, M.P.H.
Having survived kidnapping, assault, and torture by a gang— who partially severed three of Jane’s fingers—Jane* made it to the United States and applied for asylum. Like all asylum seekers, Jane had to apply for asylum within one year of arriving in the U.S. The process involved interviews and court hearings at which Jane had to demonstrate a credible fear of persecution based on race, religion, nationality, political opinion, or belonging to a particular social group. Detailed testimony about any physical, psychological, or sexual abuse, or threats
experienced in Jane’s home country or while journeying to the U.S. is required. The procedure takes a careful medical and psychological evaluation to elicit such traumatic testimony. That is where New York Medical College’s (NYMC) Center for Human Rights (CHR) comes in.
Founded in 2017, CHR is a student-run clinic that provides pro-bono forensic medical and psychological evaluations to asylum seekers, including sex- and
labor-trafficked victims, in Westchester County, New York. These evaluations are critical to their applications for asylum or legal protective status in the U.S. Ninety-four percent of asylum seekers’ applications that include a medical evaluation receive approval, compared to 37.5 percent that do not. Yet, human rights organizations, overwhelmed by unprecedented numbers of migrants seeking asylum cannot meet the demand for needed medical evaluations, making CHR’s work more crucial than ever. In January 2019, the U.S. had a backlog of 325,277 asylum cases.
As of May 2023, persecution, conflict, violence, or human rights violations forced 110 million people worldwide to flee their home countries. Of these, more than 1.1 million are seeking asylum in the United States. Jane* is one such individual.

To produce these evaluations and the affidavits that asylum seekers need to present in court, CHR works closely with local human rights organizations, such as My Sister’s Place, Neighbor’s Link, and Physicians for Human Rights. It also relies on a cadre of generous volunteer clinicians—physicians, social workers, nurses, and physician assistants—who conduct the evaluation interviews. But it is NYMC’s student volunteers who drive the organization by overseeing all its efforts, including advocacy and research, to meet the medical and social needs of individuals who have suffered human rights abuses.
“NYMC values and prides itself on cultivating students who can assimilate and process a vast amount of clinical information, and who are also committed to serving individual patients and the good of society,” says Rebecca A. McAteer Martin, M.D., ’08, associate professor of family and community medicine and CHR’s faculty advisor. “A number of students at CHR are immigrants themselves or have come over as asylees, which makes this work particularly meaningful to them.”


One such student is Rahim Hirani, an M.D./Ph.D. candidate and one of CHR’s executive directors. Born and raised in Pakistan, Hirani witnessed family and friends endure the trials of pursuing safety in the U.S. “I have seen how mentally and financially draining seeking asylum can be, so this work feels very personal to me,” Hirani says. “For this reason, I want to make sure that I can contribute whatever I can,” he says.
Hirani partners with co-executive director Kavya Tangella, School of Medicine (SOM) Class of 2026, to make sure that the clinic runs smoothly. This entails shepherding attorneys’ requests for client information to CHR’s co-directors of clinical operations, Jacob Fiedler, SOM Class of 2026, and Helen Ng, SOM Class of 2026. Fiedler and Ng pass along these requests to one of CHR’s four case managers, Yael Weitzner, Emily Zhang, Francesca Ricciardi, or Talia Saal, all from the SOM Class of 2026, who then try to find clinician volunteers to conduct the necessary evaluations. Psychiatric evaluations take place remotely, while physical evaluations take place on campus.
NYMC values and prides itself on cultivating students who can assimilate and process a vast amount of clinical information, and who are also committed to serving individual patients and the good of society. Dr. Martin ” “

Once a case manager identifies an evaluator, they schedule the evaluation, according to when they, the client, clinician, client’s attorney, an interpreter, and two student volunteers can attend. Although only clinicians speak directly with clients, other attendees may quietly observe, while the student volunteers take notes of the interview, transcribe them, write up the evaluation, and draft the affidavit. “Case managers make sure that evaluations contain all the information that an affidavit and immigration judge would need about the trauma that a client has endured, why they should receive asylum, and why returning them to their country would endanger their life,” Hirani explains.
After drafting both the interview notes and affidavit, students send them to the clinician evaluator for comments and corrections. The clinician then has the documents notarized and the case manager delivers them to the client’s attorney. “Without student volunteers, it would be difficult for clinicians to do evaluations because of the time it takes to transcribe them and write the affidavits,” Tangella says.
The work is time- and labor-intensive, which explains CHR’s shortage of evaluators. In 2021, the organization had only two clinician evaluators. Now it has seven or eight, which is still too few, Hirani says. “We do not have enough evaluators for the number of requests we receive, so unfortunately, we have to turn people away,” he says.
Of the 40 interview requests that CHR received from April through September 2023, 20 were accepted and successfully evaluated. “We are receiving more and more requests but have been able to handle only 50 percent of them because we do not have enough clinicians,” Hirani says. “In the last month alone, we received 11 or 12 requests, which reflects the unprecedented number of refugees in New York City,” he adds.
Dr. Martin, who is a full-time palliative medicine consultant at Westchester Medical Center and faculty advisor for several other on-campus programs, finds time every few months to conduct one asylum interview for CHR. “Each interview takes upwards of three or four hours with a translator,” she says. “The stories themselves are often difficult to hear, and there are times when clients re-experience trauma, so you have to be so careful when you do these interviews,” she says.


Following the interview, she often conducts additional research to support her findings. “Sometimes a judge will say there are discrepancies or gaps in a report, and so I will include evidence in the literature that demonstrates the impact of post-traumatic stress syndrome on memory,” she says. Then, she will edit the final eight to twelve-page report, which includes her diagnostic assessment and treatment recommendations.
All CHR’s volunteers, including clinicians, must complete an online training, which includes an overview of the immigration and asylum systems in the U.S. and a template for interviewing asylum seekers. Even though most evaluations are psychological, any clinician with a health care certification, primary care training or skills in interview-based care can perform them since a template supplies all the questions. “The training consists of a few online modules and takes no more than a couple of hours,” Tangella says. “Clinicians do not need to make a major commitment or have any prior related experience. They can do interviews whenever they have availability, whether that is once every month or once every year. It just takes being interested,” she adds.
Providing medical and psychological evaluations is only part of what CHR does. The organization also has an advocacy team that educates clients about local resources to help them find
employment, learn English, or cope with difficult issues like domestic violence. In collaboration with local organizations, community health centers, and clinical care networks, the advocacy team plans community events addressing human rights issues. “We also have a journal club for students as a forum to talk about issues relating to asylum seekers, like gang violence and other topics,” Tangella says. “Having the space to discuss these topics is important for us as future physicians,” she notes.
CHR also has a newly formed research team that is hoping to explore the impact of student-run asylum clinics on clients and students, and effective approaches to treating victims of human rights abuses. The Center also has a recruitment team that tries to engage clinicians by educating them about its mission, work, and the impact they can make.
Dr. Martin, who has dedicated her career to treating suffering patients like Jane, who she interviewed, says that volunteering for CHR is her duty as a physician. “The people who CHR serves are so vulnerable, and medical schools are obligated to consider vulnerable populations, including asylees and human trafficking victims,” she says. “If we as clinicians do not do it, then who does? If we do not advocate for and model this work for students, then who will? It will increasingly become an underserved need. It already is.”
She urges clinicians to give CHR whatever time they can spare. “If you have administrative time, then take one afternoon every three months to do an evaluation. If you are in private practice, then try to block out one afternoon every quarter to provide pro-bono care and get buy-in from your practice that this is valuable work. If every clinician in the U.S. gave half a day a week, a tithe of their time, we would not have a problem with medically underserved populations.”
At the time of this writing, neither Dr. Martin nor CHR know how Jane’s asylum case turned out. “Even though having a medical evaluation increases clients’ chances of being granted asylum by 70 to 80 percent, these cases can take up to 10 years to settle, and we may never know what happens to the individuals,” Tangella says. It is a scary unknown but one that strengthens the resolve of CHR’s volunteers to continue their work. “Whatever field I go into I want to do this work,” Hirani says. “We can actually make a difference in people’s lives while we are in medical school, which is the most meaningful thing we can do,” adds Tangella. ■
For additional information or to learn how to volunteer with the NYMC CHR, please visit www.nymcchr.org.
* Name has been changed to Jane to protect the individual’s identity.
“We need to create a world where children are supported, so they can achieve their fullest potential.” These words resonate with parents, educators, and child advocates alike, and they come from someone who embodies all three.
Shetal Shah, M.D., professor of pediatrics in the Division of Neonatology, cares for some of Westchester’s most vulnerable newborns and considers it his responsibility to prioritize the needs of children in every way possible. “We should make sure that the unique needs of children come first, and everything is built around them,” Dr. Shah asserts. “Unfortunately, that is not how systems are designed.”
Confronting such systems, namely Medicaid, and the state and federal legislatures that fund it, is a big part of what drives this neonatologist and father of two. That is partly because 70 to 80 percent of the children he cares for at Maria Fareri Children’s Hospital rely on the public health insurance program. “Advocating for better health policies is a natural extension of what I do in the Neonatal Intensive Care Unit (NICU),” Dr. Shah says. “We work hard to get these infants home and then cannot get them medicine because they are uninsured? That should never occur, and I can help prevent it.”
Born into a family of physicians, Dr. Shah always knew that he would become one too. He earned his undergraduate degree magna cum laude from Princeton University and his medical degree from Cornell University Medical College with honors. He completed his pediatrics residency at Duke University and his neonatology fellowship at New York University.
Neonatology fascinates him. “It is the most successful field of medicine ever created,” Dr. Shah exclaims. “We are actively resuscitating babies born at 22 weeks, which was once inconceivable. From a medical standpoint, it rivals any achievement in medicine, except for vaccination.”
He calls the NICU a “magical place,” where he not only cares for premature
infants but also educates parents about public health interventions, such as vaccinations for flu and COVID-19, and quitting smoking. “The only way to protect children is to surround them with a ‘cocoon of immunity’ by making sure no one around them smokes and everyone is vaccinated,” Dr. Shah says.
His idea of immunizing parents in the NICU led to two New York State public health laws—the Newborn Neonatal Influenza Protection Act of 2009 and the Neonatal Pertussis Prevention Act of 2012. It also earned Dr. Shah a national citation of merit from the American Academy of Pediatrics (AAP), and a proclamation from the New York State Assembly. He performs most of his advocacy work on behalf of the AAP, where he sits on the NeonatalPerinatal Medicine Executive Committee. Much of this current work entails pushing for continuous Medicaid funding to spare families the eligibility losses that disrupt coverage and care. Dr. Shah has been honored by the United States Congress for his work supporting and preventing the repeal of the 2010 Affordable Care Act, and his backing of federal programs that benefit babies, such as the Supplemental Nutrition Program for Women, Infants and Children, otherwise known as WIC, as well as improved national vaccination policies. However, his advocacy is about more than getting bills passed. It is about advancing all efforts that are in children’s best interest and fighting those that are not. Dr. Shah played a major role—along with Boriana Parvez, M.D., clinical professor of pediatrics at New York Medical College (NYMC) and medical director of the Liquid Gold Donor Milk Program at Maria Fareri Children's Hospital's Regional NICU; Edmund F. La Gamma, M.D. ’76, professor of pediatrics and of biochemistry and molecular biology at NYMC, chief of the Division of Newborn Medicine, and director of the Regional Neonatal Center of Maria Fareri Children’s Hospital; and Heather L. Brumberg, M.D., M.P.H., professor of pediatrics and clinical public health

at NYMC, director of neonatal public health programs, associate director of the Regional Perinatal Center, and medical director of the Lower Hudson Valley Perinatal Network at Maria Fareri Children's Hospital—in the creation and passage of legislation that secured Medicaid coverage of donor milk for high-risk neonatal infants.
Those efforts led to the creation of a legislative toolkit, widely promoted by the AAP Neonatal Section, which led to Medicaid coverage for donor milk in Ohio, Washington, Georgia, and Maine.
He has also worked to block efforts to weaken Public Health Law 2164, which requires all public, private, and parochial school students in New York State to be vaccinated for diphtheria, tetanus, pertussis, measles, mumps, rubella, poliomyelitis, hepatitis B, varicella, and meningococcal disease.
By educating parents as well as policymakers, this widely published 2010 Fulbright Scholar is doing all he can to ensure that children come first in health care decision-making. “Children make up 20 percent of our population, 100 percent of our future, but zero percent of the electorate. If we do not put them first, how can we expect others to?” ■
With a passion and commitment to helping rehabilitate the smallest patients, Victor Santamaria, Ph.D., PT, assistant professor of physical therapy in the Department of Rehabilitation Sciences, joined New York Medical College (NYMC) in 2022. It is a role he stepped into with purpose and dedication, the very same approaches that have served him well throughout his career, helping to make transformative strides in the field of pediatric physical therapy.
Dr. Santamaria developed the pediatric and research curricula with a unique touch, aiming to equip students not just with clinical knowledge, but also with a deep understanding of evidence-based practices. "I want my students to learn a child- and family-centered approach," he says. “This is the best way to apply clinical knowledge to address diseaserelated physical impairments, functional limitations, and participation restrictions so that we, as physical therapists, can have a meaningful impact on the child and family’s life.”
Pediatric physical therapy, he explains, is fundamentally different from its adult counterpart. A child's motivations and approach to therapy are unique, requiring an engaging and game-oriented process. Assessments and treatments must be childfriendly and enjoyable, he emphasizes.
Dr. Santamaria’s journey into pediatric physical therapy is not just a career choice; it is a calling rooted in a deepseated interest in pediatric pathology. His specialization in pediatric neuromotor conditions has become a testament to his love for working with infants and children. “I have always been fascinated with the brain sciences…how the brain develops, learns, and recovers from injuries. It is
admirable to see how happy, resilient, and dedicated children who live with disabilities can be,” Dr. Santamaria notes.
As pediatric physical therapy evolves, he sees a shift from traditional, hands-on therapies to more active and self-initiated interventions—where motor learning and control principles play a central role in pediatric neurorehabilitation. Dr. Santamaria is developing new clinical tools and motor interventions for children with cerebral palsy who live with severe movement disorders and are wheelchairusers. “By combining robotics with intensive motor therapy based on goaloriented postural and reaching abilities, we are able to improve the functionality of these children at many levels,” he says.
A native of Málaga, Spain, Dr. Santamaria now lives in New York along with his wife, Jaya Rachwani, and their two children. Rachwani shares his passion for pediatric physical therapy. They often collaborate on research studies together. Amidst his academic pursuits, he cherishes his annual reunions with relatives back in Spain and finds joy in good old-fashioned family time.
Extending his gratitude to his colleagues at NYMC for welcoming him as part of the team, Dr. Santamaria adds, “I am grateful for all the support I received in the process of assembling a motion analysis laboratory, which will be invaluable in the study and treatment of mobility-limiting conditions.”
Dr. Santamaria’s story is a beacon of inspiration for his students, the children he treats, and their families. His impact goes beyond the confines of a classroom, reaching into the hearts of those touched by his dedication to the well - being of children. ■

By the time Abdelfattah El Ouaamari, Ph.D., associate professor of cell biology and anatomy and of pharmacology, was in high school in his native country of Morocco, he was completely enthralled with science— especially the life sciences. After two years at a local college, he pursued his science education in France, where he obtained a B.A. in biochemistry, an M.S. in life and health sciences, and a Ph.D. in molecular and cellular biology at the University of Nice Sophia-Antipolis.
As a graduate student, he studied diabetes, and a post-doctoral fellowship at the Joslin Diabetes Center in Boston brought him to the United States. Dr. El Ouaamari remained at Joslin as a research associate while also being appointed as an instructor of medicine at Harvard Medical School. He then spent five years as an assistant professor of medicine at Rutgers University before coming to New York Medical College (NYMC) in 2022.
Since his graduate school days, Dr. El Ouaamari’s research has focused on diabetes and insulin resistance, with a concentration on the insulin-producing pancreatic beta cells. When the body converts food into dietary sugars, insulin instructs the cells to take in that sugar and convert it into energy. In type 1 diabetes, the body’s immune system attacks and destroys the insulin-producing cells. Whereas in type 2 diabetes the cells don’t take in enough sugar; the pancreas produces more insulin but eventually cannot make enough insulin to keep blood sugar levels in a healthy range and avoid the damage caused by excess sugar in the bloodstream.
While his Ph.D. dissertation focused on the beta cells as independent entities, Dr. El Ouaamari’s post-graduate work began to explore ‘organ crosstalk’—the ways organ systems interact with the pancreatic
cells to keep blood sugar stable. For the past several years, his lab has been studying how the peripheral nervous system—neurons that branch off from the spinal cord and the vagus nerve extend to all parts of the body—interacts with and controls the activity of the insulinproducing beta cells. “We know also that long-distance organs communicate with the pancreas to modulate the regeneration, survival, and function of insulin-producing beta cells,” Dr. El Ouaamari says. “The questions we are asking now are about the nature and the identity of the molecules mediating this inter-organ metabolic communication, and the mechanisms by which the nervous system senses the molecules. The answers will eventually help us design new therapies for diabetes.”
Most recently, he has shifted to researching the related area of obesity, which has increased dramatically in the U.S. over the past 50 years. “The calories in/calories out model explains some instances of obesity,” Dr. El Ouaamari says, “but there is much more to the story.” He points to the increased availability of cheap, high-carbohydrate foods and the ubiquity of added sugar in the food supply. The body’s physiological response to that sugar overload— increased insulin production—creates what he calls a “hormonal milieu in favor of developing obesity” in many people. A deeper understanding of this process could generate new therapeutic interventions for obesity.
“There is nothing more satisfying than quenching your curiosity,” Dr. El Ouaamari says, “and connecting with others who are as intrigued by the questions as you are. I have generous and accessible colleagues here at NYMC and look forward to asking and eventually answering many more questions.” ■

Torrential thunderstorms could not dampen the spirit at the NYMC golf outing and reception on June 26, 2023. While play was suspended for a time due to the weather, 85 golfers hit the links and tested their skills in a putting contest and a closest to the pin contest at Saint Andrew’s Golf Course in Hastings-on-Hudson, New York. An evening reception honored Steven Lansman, M.D., Ph.D., professor and chair of the Department of Surgery, and Rubén A. Medina, M.B.A., M.P.H., founder of RC Solutions, Inc. and member of the NYMC Board of Trustees. The third annual golf outing raised $158,000 and was chaired by Martin Katzenstein, M.D. ’78, assistant dean for clinical affiliations, associate professor of pediatrics, and chair of the Board of Advisors, and was sponsored by the Board of Advisors. “It was wonderful to see the NYMC community come out for the golf tournament and support student scholarships. We are most grateful to all the sponsors and supporters,” said Bess J. Chazhur, M.S., chief development officer and executive director of alumni relations. ■







Nostalgia and laughter filled the air as alumni from across the years reunited for a celebration of shared memories and enduring connections on November 4 and 5, 2023. The Alumni Reunion this year was the first-time graduates from the School of Medicine, Graduate School of Biomedical Sciences, and School of Health Sciences and Practice were welcomed back to New York Medical College (NYMC) to reminisce and share their successes.
More than 70 guests attended the reunion weekend from the class years ending in three and eight, with special recognition of the 50th and 25th anniversary class years, 1973 and 1998 respectively. Current students, faculty, and administration were also in attendance to celebrate at the reunion dinner dance and jubilarian awards ceremony at the Sleepy Hollow Hotel in Tarrytown, New York.
The weekend of festivities concluded with a brunch on-campus at 19 Skyline Drive, a studentled panel discussion featuring second- and fourthyear medical students, and an exclusive tour of the Clinical Skills and Simulation Center. ■










Theannual Founder’s Dinner was a night to remember at Marina Del Rey in Throgs Neck, New York, on October 25, 2023. The annual fundraising event brought together more than 300 academic, health care, business, and community stakeholders to commemorate New York Medical College’s (NYMC) rich legacy and bright prospects, while also paying tribute to two distinguished leaders for their impactful and transformative accomplishments.
The evening honored Matthew A. Pravetz, O.F.M., Ph.D. ’88, professor emeritus of cell biology and anatomy, and Alan B. Rosenthal, D.M.D., adjunct assistant clinical professor of dental medicine and member of the Board of Trustees at NYMC, and assistant dean of community outreach and global health at Touro College of Dental Medicine, with Distinguished Service Leadership Awards.
The Founder’s Dinner raised $350,000 for scholarships and essential initiatives that advance the College’s commitment to educating future physicians, public health leaders and support life -saving biomedical research.

The 2023 sponsors included: Presenting: Regeneron
Gold: NYMC Board of Advisors, Martin Katzenstein, M.D. ’78, Pavarini Construction Company, Avi Retter, M.D., and Margaret Retter Esq., and Westchester Medical Center
Silver: Boston Children’s Health Physicians and Alan Rosenthal D.M.D.
Bronze: California Bank and Trust, Dee DelBello, Andrew and Sarah Levy, Dr. Meryl and Mr. Joseph Mark, Piazza Brothers, Ronald and Peggy Poe, and Webster Bank
Flowers: Lee Pressler, M.D. ’90, Walter Lewis, M.D. ’91, and Christel Bauer, M.D., NYMC Board of Advisors
Dessert: Garfunkel Wild, P.C., KPMG, and North80 ■








Joseph D. Mark, Chair
Joseph Schwartz, M.D., Vice Chair
Alan Kadish, M.D.
Robert Alter, M.D.
Gary Barnett
Howard Baruch, M.D.
Benjamin Chouake, M.D.
Dee DelBello
Rabbi Menachem Genack
Gary Gettenberg, M.D. ’83
Munir Kazmir, M.D.
Moshe Lichtenstein
Rubén A. Medina, M.B.A., M.P.H.
Lawrence F. Neshiwat, M.D.
Martin S. Katzenstein, M.D. ’78, Chair
Christel Bauer, M.D.
Sabra Brock, Ph.D.
William J. Camera, C.P.A.
Edward Chew, M.D. ’03
Steven H. Cho, D.D.S.
Eric I. Choe, M.D. ’88
Raymond A. Conta, J.D.
Noreen Ferrante, M.D. ’84
Kathleen Case Finzel, M.D. ’87
Moshe E. Hirth, M.D. ’88
Moira T. Imperial
Howard Jonas
Russell Kamer, M.D.
Martin D Keltz, M.D.
Norman L. Maron, M.D. ’70
Leonard J. Newman, M.D. ’70
Rebecca B. Newman, M.D. ’05
Stephen Nicholas, M.D. ’86
Martin Oliner, Esq.
Eliot Peyser
Ronald F. Poe
Joseph Popack
Ammir Rabadi, M.D.
Avi Retter, M.D.
Stephen Rosenberg
Alan B. Rosenthal, D.M.D.
Henry Saphier, M.D. ’61
Rabi R. Sinha, M.D.
Kenneth R. Theobalds
Paul Ostrovsky, M.D. ’78
Michael D. Paris, M.D. ’67
Chong H. Park, M.D. ’96
Lawrence Rein
Anne Negrin Reis, M.D. ’02
Richard Rohr, M.D.
Bruce Schanzer
Jonathan Schedilin, M.D.
Tammy Skaist
William Smith
Susan N. Tierman, M.D. ’79
Steven Topfer, D.O.
Rajesh Verma, M.D. ’93
Anthony Viceroy
Vincent J. Vigorita, M.D. ’76
Patricia White, M.D.
John M. Zimmerman, M.D. ’78


Ashanda M. Saint Jean, M.D. ’98, clinical associate professor of obstetrics and gynecology at New York Medical College (NYMC), is one of six children born into a family who embodies a strong work ethic and giving back. Her mother, who was a phlebotomist and aspired to be a nurse, unfortunately was unable to complete her schooling after having children. Dr. Saint Jean, and her oldest brother, both of whom pursued careers in medicine, have continued their mother’s legacy by achieving professional success in their respective fields, while helping others.
Dr. Saint Jean’s medical education started at the Sophie Davis School of Biomedical Education Program at CUNY. The program was initially created to produce Black and Hispanic physicians to work in medically under-resourced areas in New York State. Students obtained a B.S. and M.D. degree in seven years with the stipulation of working as a primary care physician in a medically under-resourced area.
Dr. Saint Jean completed her first five years at City College and was matched at NYMC, one of the seven participating medical schools at the time. She completed an internship and residency in obstetrics and gynecology at Danbury Hospital in Danbury, Connecticut.
“I always give gratitude to my teachers, my attendings, my professors, and NYMC because they all made my pathway in residency quite easy. NYMC truly is number one,” she says. “They have esteemed clinicians who light a flame in their students. They really nourish it, so that it can grow.”
It was on her last day of rotations at NYC Health + Hospitals/Metropolitan when Dr. Saint Jean was overcome with emotion and knew she wanted to become an OB/GYN. She loved childbirth and serving her patients. She was confident that she was going to pursue this career path. “I can proudly say that for 25 years, I’ve had the esteemed pleasure of being a part of the best day of someone’s life.”
Today, Dr. Saint Jean finds herself as chair and associate physician at Health Alliance Hospital in Kingson, New York, which is part of the WMCHealth Network and a clinical affiliate of NYMC, teaching alongside her former professors, like Jonathan Mays, M.D., clinical associate professor of obstetrics and gynecology, and Yvonne Thornton, M.D., M.P.H., professor emeritus of obstetrics and gynecology. “I think one of my own full circle moments is now being back at NYMC and being a part of the students’ lives. I wanted to come back to teach medical students because the only way you can make things better for the next generation of people is rooted in the education of our future clinicians.”
Dr. Saint Jean was instrumental in the start of WMCHealth Network’s Center to Advance Women’s Health Equity, which aims to reduce cesarean delivery rates associated with health complications, enhance access to mental health, and provide comprehensive prenatal care. The Center is available to all women, particularly those at the highest risk for pregnancy complications. “Pregnancy and motherhood are journeys that should be surrounded by joy, love, laughter, and excitement. And that’s not what’s happening,” she says. “We are going to bend the curve towards humanity and put patient-centered care first. We are also going to develop strategies that address the whole biopsychological and social picture of a patient and evaluate how that plays into one’s journey.” Dr. Saint Jean is also one of the only physicians appointed to the Maternal Mortality Review Committee for both New York City and New York State.
Students continue to be surprised when they find out that 25 years ago their professor was once an NYMC student practicing sutures and phlebotomy, just like them. Dr. Saint Jean uses the same advice from her professors and experiences to shape how she teaches her students. “I always tell my students that the way I became the best provider was when I was a patient,” she says. “I want them to deliver health care with humility and not to get that lost in the science of it all.” ■
We would love to share your most recent news and accomplishments in the next issue of the Chironian. If you have any recent professional accomplishments or developments, published a book, or have any family news to share, please let us know. Submit your updates online: www.nymc.edu/alumni
Mail them to:
Office of Development and Alumni Relations New York Medical College 40 Sunshine Cottage Road Valhalla, NY 10595

Oluyemisi Ariyibi, M.B.B.S., M.P.H. ’16, was elected fellow of the American College of Physicians.
Padraic Reynolds, M.P.H. ’14, is now in his 15th year at NYMC, currently as associate dean of academic administration for the School of Medicine. He recently completed a two-year term as chair of the Association of American Medical Colleges Data and Benchmarking Committee of the Group on Business Affairs.

Rollin G. Medcalf, M.D., PreInternship Program ’10, is an assistant teaching professor of medical studies at Arizona State University in the College of Health Solutions and an adjunct professor at Thomas Jefferson University, where he teaches anatomy and physiology. Recently he became the concertmaster of the Sierra Vista Symphony Orchestra.
Carolyn Wilson, M.P.H. ’10, a senior health program coordinator at Ledge Light Health District, was awarded the 2023 Prevention Professional of the Year Award from the Connecticut Association of Prevention Professionals. She coordinates the Groton Alliance for Substance use Prevention (GASP) and provides academic detailing on opioid safety to prescribers and pharmacists in Eastern Connecticut.
Rebecca A. McAteer Martin, M.D., ’08, clinical associate professor of family and community medicine and advisory dean in the School of Medicine at NYMC, and palliative medicine consultant at Westchester Medical Center, published a memoir, Though the Darkness: Medicine, Missions, and Meeting God in Nepal, sharing the realities of illness, death, poverty, and loss while serving as a volunteer physician from 2013 to 2015 at Tansen Mission Hospital located in the Annapurna Himalayan foothills of western Nepal, including her experience of enduring Nepal’s devastating 7.8 earthquake outside of Kathmandu in 2015 and the aftermath. Dr. Martin led a book discussion for the NYMC community in January 2024.

Michael Crupain, M.D. ’06, M.P.H., released a new book, The Power Five: Essential Foods For Optimum Health, published by National Geographic Books. In his latest work, Dr. Crupain’s third book and second cookbook, he empowers readers to focus on eating more of the foods associated with a longer healthier life rather than worrying about what not to eat. He incorporates the five essential foods for living longer, including fruits and vegetables, beans, whole grains, seafood, and nuts and seeds, into more than 80 recipes. These recipes are designed to maximize taste, texture, and flavor, championing the idea that eating and living healthier no longer feels like a chore. “Each chapter delves into the science and nutritional information in a playful, at times humorous way, making it easy to digest why each of these foods is essential and powerful. The subsequent recipes are weeknight accessible and sophisticated,” he says.

Eugene C. Jacquescoley, M.P.H. ’05, recently applied to the Certification Board of Infection Control and Epidemiology and Harvard’s Kennedy School for Government Performance Lab. His band, Jacquescoley, has performance dates in Rio de Janeiro, Brazil, Abu Dhabi, and Montreal in 2024 and Madison Square Garden in New York City, and Detroit in 2025.


Kevin R. Cummings, M.P.S., M.P.H. ’00, is happily retired and enjoys traveling with his wife, Rose, and spending time with their three grandchildren.
Shahrad Aynehchi, M.D. ’98, is the managing partner at Unio West Coast Urology in Los Angeles. “I am married with two children, a budgie and a mortgage,” he writes.
Rod Tanchanco, M.D., GME ’96, launched a podcast in March 2024, MediSagas: Tales in Medicine, featuring stories from the history of medicine in a compelling narrative format. “If there are medical history buffs who enjoy researching a good story, writing, playing with technology, and would like to join this venture, reach out to me,” he writes. He is also the author of First Patients: The Incredible Stories of Pioneer Patients.

Maja L. Lundborg-Gray, M.D. ’95, received Samaritan Medical Center’s Lifetime Achievement Award in March 2023, in recognition of her 25year commitment to the community as a lead emergency medicine physician and public health advocate. Her husband, Daniel Gray, M.D. ’91, and father, Carl Lundborg, M.D. ’67, were in attendance along with her mother, Karen. “My parents and my husband have been my strongest supporters in life and in my career. I am so very grateful for them. I am also grateful to New York Medical College for providing me with a strong foundation in medical education and research opportunities,” she writes.
James L. Januzzi Jr., M.D. ’94, is currently the Adolph Hutter Professor of Medicine at Harvard Medical School, a cardiologist at Massachusetts General Hospital, and director of Heart Failure and Biomarker Clinical Trials at the Baim Institute for Clinical Research. He is in his 19th season as a team physician for the Boston Red Sox. “I’m enjoying life as a clinical trialist and clinician seeing patients with cardiovascular disease, and now that we’re empty nesters, Roberta and I are having more and more fun,” he writes.

Jamel Y. Patterson M.D., GME ’92, M.S., M.P.H., is president of the Ageno Foundation International, Inc., a charitable organization serving the indigent globally by providing access to clean water, education, economic empowerment, health care, and nutrition. To date they have drilled 13 boreholes for clean water, in Uganda, Kenya, Malawi, Dominican Republic, Congo, and India. A book about the Ageno Foundation is currently underway.
Peter E. Bentivegna M.D. ’85, FACS, completed a two-year appointment as president of the New England Hand Society and presided over the 50 th Anniversary Meeting in Sturbridge, Massachusetts. It is the largest regional society and a great source for grassroots academia and future national leadership in the field.

Reputations are built not only through hard work, but through effective communication. Dawn French, M.P.H. ’15, senior vice president for marketing, communication and community relations at White Plains Hospital in White Plains, New York, has made it her mission to strengthen the hospital’s reputation through underscoring its commitment to the community’s well-being, and advancing its strategic vision to propel the hospital into the future.
“It was a bit accidental that I ended up in health care,” says French. “Now I cannot imagine doing anything else.” Two decades ago, immersed in a successful career in broadcast news, the married mother of three decided to step away temporarily to raise her family. That set the stage for a leap into the world of health care. “When it came time to return to the workforce, I applied for a job at White Plains Hospital,” she continued. “I saw the opportunity to leverage my skill-set and be able to make an impact in an incredibly meaningful field.”
New York Medical College laid the foundation for French’s health care career, where she earned a Master of Public Health in health policy and management in 2015. She remembers one particular class, led by Denise C. Tahara, M.B.A., Ph.D., former associate professor of public health, which exposed her to the many aspects of health care management. “There was a lot of project-based work,” recalls French, “which gave us real-life examples through case studies, and we were encouraged
to develop innovative solutions.” A project promoting immunizations in the undocumented population broadened her understanding of health care barriers and earned her capstone group an award for their work.
As the health care landscape evolves, French remains at the forefront of change, helping to steer White Plains Hospital through challenges, most notably during the COVID-19 pandemic, and embracing trends that shape the future of health care. With a focus on accessibility, the hospital’s network now spans 31 locations, and has continue to bring more advanced programs and services to the region, ensuring that quality care is never far away for patients.
“Health care is constantly evolving as new technologies and treatments are discovered and patient populations grow and change, which is why collaboration among doctors, nurses, and support staff is key,” explains French. For the community, she and her team aim to build on the reputation of White Plains Hospital. “A big part of my team’s role is education around prevention and staying healthy. We want to keep people out of the hospital, but of course, when you are sick you want the best care and I feel very proud of the high-quality care we provide to the community.”
French’s journey from broadcast journalism to health care administration is not just a career shift; it is a testament to the transformative power of embracing unexpected paths, taking on new challenges, and finding fulfillment. “Health care is such a gratifying profession—every day you are doing work that impacts someone’s life. It is an incredibly rewarding career.” ■

Joseph Cervia, M.D. ’84, M.B.A., was appointed to the American Board of Pediatrics, Subboard of Pediatric Infectious Diseases, effective January 1, 2024. He also continues to serve as pediatric infectious diseases society liaison on the Board of the HIV Medical Association.
Philip R. Cohen, M.D. ’83, published a report on “Fist sign-associated post ambulatory swollen hands” in JAAD Case Reports. This relatively common, yet rarely described condition, also known as POTASH, has only been reported three times before in medical literature; two of these reports were also published by Dr. Cohen. His report focused on POTASH in individuals who participate in walking, hiking, and running. In addition, he has provided the first description of a previously unrecognized variant of skin cancer and his paper on basal cell carcinoma in situ was published in Cureus in September 2022.
Daryl R. Altman, M.D. ’82, joined Allergy, Asthma, and Sinus Center of Long Island, with offices in Queens, Nassau, and Suffolk Counties, New York.

Matthew J. Arduino, M.S. ’81, Dr.P.H., received a joint award for contributions to the field of infection prevention and epidemiology from the Association of Practitioners for Infection Control and Epidemiology (APIC) and the Society for Healthcare Epidemiology of America (SHEA). He was recognized at the SHEA Spring Conference in Seattle, Washington, in April 2023, and the 2023 Annual APIC Conference in Orlando, Florida, in June, where he presented “Wading Through Water: Microbes, Endotoxin, and More than 30 years at CDC.” He is currently the senior advisor for hygiene and infection prevention, in the Healthcare Systems Strengthening, Resiliency Training Branch, Division of Healthcare Quality Promotion, Centers for Disease Control and Prevention, in Atlanta, Georgia.
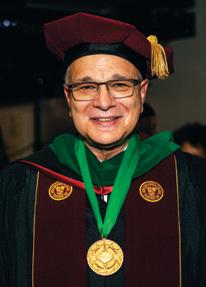
After spending the last seven years working for the government overseas in both Baghdad and the Marshall Islands, Christopher J. Kaczmarski, M.D. ’80, is now officially retired. “I look forward to many well-deserved pleasures I can enjoy now in my abundant free time,” he says.
Nedra J. Rosen (formerly Braverman), M.D. ’80, retired from the practice of medicine. “I look back with pride at the practice I created and the relationships I established with so many patients... as well as the rewards, challenges, and stress of practicing this most honored profession,” she writes. “I look forward with both apprehension and enthusiasm to whatever the next chapter may bring. My husband and I are enjoying our expanding family as our daughter is getting married and our sons have given us four grandchildren to love.”
Steven Fruchtman, M.D. ’77, is the president and CEO of a publicly traded company, Onconova Therapeutics, that has two drugs in development: rigosertib and narazaciclib. Rigosertib down-regulates the PLK-1 pathway, which drives the squamous cell carcinomas (SCC) that are the primary cause of death in young adults who have recessive dystrophic epidermolysis bullosa (RDEB), a congenital disease of type VII collagen which binds skin cells in place. There are no FDA-approved drugs for SCCs that complicate RDEB, and complete cutaneous responses with rigosertib have been reported at major medical meetings. Narazaciclib is a differentiated CDK4/6 inhibitor that potently targets additional tyrosine kinases important in tumor surveillance by the host’s immune system. They will be studying narazaciclib in endometrial cancer, the most common cancer of the female reproductive tract, with plans to study refractory HR+ HER2—metastatic breast cancer as well. “I thank NYMC for the opportunity to do my life’s work and care for those with unmet medical needs,” he writes.

William C. Reha, M.D. ’81, M.B.A., has been a member of the Board of Trustees of Strayer University since 2007 and has participated in their commencement ceremonies throughout the years including presenting awards and giving the keynote speech in December 2017. He officiated and conferred the degrees during the September 2023 ceremony in Atlanta, Georgia, proudly adorning his NYMC academic attire.
Lloyd P. Haskell, M.D. ’77, works at Johnson & Johnson, and 2024 will mark 20 years there. He is involved in cardiovascular and renal clinical research. He served as the class chair for the 45th reunion in 2022 and encourages everyone in the Class of 1977 to update their contact information with the Office of Development and Alumni Relations.
Stephen G. Marcus, M.D. ’76, is CEO of a Floridabased pharmaceutical company that is conducting phase 2 clinical trials of an oral receptor for advanced glycation end products (RAGE) inhibitor as a treatment of glioblastoma, brain metastasis, pancreatic cancer, and breast cancer. He is the inventor of a treatment of glioblastoma, which was patented in December 2022.
Catherine Dunn, M.D. ’75, is enjoying retirement in Tucson, Arizona, in the winter, and Mazama, Washington, in the summer, and loves spending time with her four grandchildren.
Kenneth P. Carlson, M.D. ’73, retired after 40 years in pediatrics in private practice, professorship and working for the Texas Department of Health. He is living happily in Portugal, a quiet, comfortable, healthy, and safe place. “We get to see our children and grandchildren during extended visits to the United States, but Rachel and I hurry back to our little hideout in Porto,” he writes.
After 18 years of serving as chair of family medicine at Stony Brook’s School of Medicine and family medicine chief of staff at Stony Brook University Hospital, Jeffrey S. Trilling, M.D. ’73, stepped down from his administrative positions and patient care to devote time to writing and teaching at Stony Brook’s Center for Medical Humanities, Compassionate Care and Bioethics. He recently published a book, The Circle of Change, that argues that there is important hidden knowledge to explain patient conflict, impasse, and resistance to plan of care and lifestyle changes beyond technology’s reach that can only be gained through trust and rapport—and asking the right questions. “While physicians are trained to take inventory of the body’s biological systems, practitioners often lack the skill set to ask the right questions to explore personal, family, and cultural systems. And therein lies the pedagogic vacuum to be filled. The book’s purpose is to introduce a systems-based problem-solving approach, as map and compass for harvesting and processing patients’ narratives to uncover meaning and care for the illness,” he says.

Kathleen G. Nelson, M.D. ’71, retired from clinical practice in 2021 and now serves as a voluntary faculty member at Keck School of Medicine. Her career has included serving as a senior associate dean and medical school professor at two medical schools. In her retirement, she works as a leadership coach and consultant (www. AHCcoaching.com).
Michael E. Platt, M.D. ’69, has written several books including Adrenaline Dominance. “As far as I know, it is the only book to discuss the clinical consequences of excess adrenaline: insomnia, anxiety, ADHD, anger and road rage, fibromyalgia, interstitial cystitis, premenstrual dysphoric disorder, colic in babies, bedwetting in children, over-active bladder, irritable bowel syndrome, restless legs syndrome, and much more,” he writes. “I have also written The Miracle of Bio-identical Hormones and a manual, The Platt Protocol for Hormone Balancing.
Paul B. Heller, M.D. ’68, a former full professor at the Medical College of Pennsylvania/Hahneman, writes, “I practiced gynecologic oncology and retired from the U.S. Army as a full colonel where I was chief of gynecologic oncology at Walter Reed Army Medical Center. Upon leaving the Army l relocated to Philadelphia and practiced at Pennsylvania Hospital with a faculty appointment at the University of Pennsylvania. After that I relocated to the Medical College of Pennsylvania and I joined the Jefferson faculty at Abington Hospital in 2019. I am retired since June 2022.“



Whenshe was eight years old, Andrea Love, Ph.D. ’14, absorbed herself in some unusual reading material for a child her age. “I went to the library with my mother one day and checked out The Physician’s Guide to Arthropods of Medical Importance, she says. “It was about disease vectors that can cause all sorts of unpleasant reactions in humans. I walked around reading sections to people and I totally enjoyed making them uncomfortable.”
A child who loved roaming the woods near her Connecticut home and collecting and cataloguing the bugs she found, Dr. Love was encouraged by teachers throughout elementary and high school to explore and experiment. “They encouraged me to be my weird self,” she says. At Norwich Free Academy, she took advanced biology courses, completed independent studies, and graduated knowing that she wanted to study infectious diseases. In the honors college at Stony Brook University, she majored in biology with concentration in biochemistry and cell biology.
When the time came to choose a graduate program, she was intrigued by the Lyme disease research conducted at New York Medical College (NYMC) under the guidance of Ira Schwartz, Ph.D., former chair of the Department of Microbiology and Immunology, now professor emeritus. “I grew up near the epicenter of Lyme disease,” she says, “I thought, ‘This is my niche.’” She immersed herself in researching Lyme—and also confronted the world of Lyme misinformation. “I knew I had a knack for scientific work,” she says, “but I also realized that
I liked educating. I received exceptional training at NYMC, not only in doing and presenting research, but in how to be a good steward of science.”
Deciding that she did not want to stay in academia—“I really did not want to write grants,” she says—Dr. Love became an applications scientist for Revvity, a biotechnology company that develops tools to advance biomedical research in areas including vaccinology, virology, immunology, immunotherapy, cell and gene therapy, and therapeutic protein production. She is now their Northeast North American business director for cell assay and analysis technologies, serving as subject-matter expert for immunology, immuno-oncology, cell and gene therapy, and vaccine-related assays, and she oversees a team that works closely with leaders in academia and industry who use these tools for their research.
But she never abandoned her interest in Lyme disease and in combatting science misinformation. Now, the selfdescribed “lifelong nerd,” who read disease descriptions to anyone who would sit still long enough, has millions of people listening to her—voluntarily. With Jessica Steier, Dr.P.H., PMP, a public health scientist and former undergraduate classmate, Dr. Love launched Unbiased Science—a science communications brand that, since its inception in 2020, has garnered more than 400,000 followers across social media channels and more than one million podcast episode downloads. “When COVID-19 hit,” she says, “we were both aghast at the amount of science and medical misinformation floating around—some of it just confusing but some of it truly dangerous.”
When members of the board of the American Lyme Disease Foundation saw her work with Unbiased Science, they asked last year if she would become the foundation’s new executive director. “Of course, I said, ‘yes.’ What we learn about Lyme disease has implications for so much else in medicine,” Dr. Love says, “including the work of the immune system, the nature of zoonotic diseases, and vaccine technologies. This position gives me another great platform for public and clinical education.” ■

Stephen Berger, M.D. ’67, is retired, but continues to volunteer at Tel Aviv Medical Center in tropical diseases and travel medicine. He has seven grandchildren and is the science director for an online infectious diseases informatics and expert system. To date, he’s published 426 e-books using an engine generated by databases and are all updated yearly. “I will be pleased to forward free copies of two e-books of current interest: Infectious Diseases of Israel, 2023, and COVID-19: Global Status, 2023. These books will be made available to the entire NYMC community, with no need to identify individual recipients and are available at www.gideononline.com/ebooks,” he writes.
Donald E. Doyle, M.D. ’67, writes, “After serving in Vietnam and receiving three medals, I completed an otolaryngology residency. While a resident, I began my career as an inventor. I have 30 U.S. patents, 28 of which are medical/surgical. The best known are the “Doyle Splat Splint” and “Doyle Nasal Packs.” I have had 10 articles published in medical/ surgical journals and I maintain a website, www.doylesurgical.com.”
Melvin L. Schulman, M.D. ’65, shares that his son, Jared E. Schulman, M.D. ‘04, M.P.H. ’04, who died in July 2023, and was chief medical officer and vice president of HackensackMeridian Health, received the National Association of Occupational Health Professional (NAOHP) Founders Award posthumously at the 2023 NAOHP annual conference. The award is a lifetime achievement award recognizing outstanding contributions to the field of occupational health.
Joel Kupersmith, M.D. ’64, is professor of medicine at Georgetown University Medical Center. Last year, he published a book, Supporting Veterans After 20 Years of the All-Volunteer Force and 20 Years of War, with former chief of staff of the United States Army, General George Casey. “I have also been conducting high-level workshops including former VA secretaries on veterans’ issues. I have been interested in veterans’ issues since my eight-year tenure running the VA medical research program nationally. I am also very much involved in teaching and research here at Georgetown,” he writes.
Michael Schlossberg, M.D. ’62, writes, “I’m extremely proud of my son, Richard Schlossberg, M.D., a graduate of the Medical College of Georgia, who was the only Doctor of Medicine named by Georgia Trend to be a Top Doc in Family Practice in the State of Georgia. He is a board-certified Family Practitioner with more than 25 years of experience.”
Robert Harwood, M.D. ’62, has been retired and living in Scottsdale, Arizona, for 10 years. He discovered an interest in art and has developed skill in sculpture and recently had three pieces displayed in a five artist show at the Herberger Theater in Phoenix.
Ira D. Glick, M.D. ’61, reflects on his career in psychiatry: “I have published 218 papers and 50-plus chapters, nine books, most recently Clinical Psychiatry: A Handbook for Medical Students Residents and a textbook on Couples and Family Therapy; and have done model psychopharmacology curricula, one designed for medical students and primary care, and one for psychiatric residents, both going global with wide acceptance in U.S. and Europe. I have also done the first scientific study of mass shooters and the implications for treatment.”
Jared E. Schulman, M.D. ’04, M.P.H. ’04, died in July 2023.
Linda C. DaSilva, M.P.H. ’01, died on March 14, 2023. She was 74.
Marie A. Carlucci, M.P.H. ’97, died on June 11, 2023. She was 70.
Guldeniz Doganay, M.D. (GME ’97), died on September 1, 2022. She was 62.
Anthony E. Okoh, M.D. (GME ’97), died on October 27, 2023. He was 67.
Paul A. Pirundini, M.D. ’91, died on April 6, 2023.
Edward T. McDonough, M.D. ’80, died on September 9, 2023.
William D. Gilson, M.D. ’75, died on June 23, 2023.
Ian R. Jenkins, M.D. ’75, died on March 1, 2023.
Barry Powers, M.D. ’75, died on August 21, 2022.
Salvatore A. Chiaramida, M.D. ’74, died on August 30, 2023. He was 74.
Leonard M. Kagan, M.D. ’73, died on December 12, 2022.
Mark J. Levenson, M.D. ’72, died on February 2, 2024.
Eugene M. Schaufler, M.D. ’72, died on August 3, 2023. He was 77.
Kenneth P. Scheffels, M.D. ’69, died on February 6, 2023.
John J. Stangel, M.D. ’69, died on April 25, 2023. He was 81.
David J. Fischer, M.D. ’68, died in August 2023.
Frank A. Ariosta, M.D. ’67, died on August 9, 2023.
Sheldon D. Kaplan, M.D. ’67, died on May 12, 2023. He was 82.
Morris Cohen, M.D. ’66, died on January 23, 2023.
David J. Gatti, M.D. ’66, died on November 12, 2023. He was 84.
Robert S. Cohen, M.D. ’65, died on June 11, 2023.
Franklin L. DiSpaltro, M.D. ’65, died on May 5, 2023.
Albert L. Saphier, M.D. ’65, died on March 4, 2023.
Harvey Weisslitz, M.D. ’65, died on December 10, 2023. He was 84.
Stephen T. Batthany, M.D. ’64, died on August 26, 2022.
Charles C. Bianco, M.D. ’64, died on October 25, 2022. He was 83.
Pierre Herding, M.D. ’64, died on July 15, 2023.
Louis H. Lefkowitz, M.D. ’64, FACOG, FACS, died on July 9, 2023. He was 85.
Richard J. Rose, M.D. ’64, died on February 26, 2023. He was 83.
Dante L. Catullo, M.D. ’63, died on October 20, 2023. He was 86.
Stephen A. Fisher, M.D. ’63, died on September 29, 2023.
Gerard J. Lawrence, M.D. ’63, died on January 9, 2024. He was 88.
Wayne A. Perkins, M.D. ’63, died on December 1, 2023.
Peter A. Philips, M.D. ’63, died on March 12, 2023. He was 85.
William J. McCann, M.D. ’62, died on February 24, 2023. He was 101.
William E. Deignan, M.D. ’61, died on August 2, 2022. He was 87.
Robert Kirschner, M.D. ’61, died on April 1, 2023. He was 87.
Myron M. Teitelbaum, M.D. ’61, died on February 9, 2023. He was 86.
H. Michael Grant, M.D. ’60, died on March 26, 2023. He was 87.
Frank J. Panettiere, M.D. ’60, died on December 12, 2022.
George W. Seuffert, M.D. ’60, died on December 13, 2023. He was 88.
Carl M. Cassin, M.D. ’59, died on May 20, 2023.
Spencer R. Downs, M.D. ’58, died on March 22, 2023.
John B. Muth, M.D. ’58, died on January 10, 2023. He was 88.
James P. Roach, M.D. ’58, died on March 6, 2023. He was 90.
William F. McCully Jr., M.D. ’57, died on June 30, 2023. He was 91.
William J. Storz, M.D. ’57, died on December 15, 2022. He was 91.
Martin H. Floch, M.D. ’56, died on June 23, 2023. He was 94.
Roderick S. Coler, M.D. ’54, died in January 2023.
Louis G. Gianvito, M.D. ’53, died on January 8, 2024.
Elliott J. Howard, M.D. ’53, died on June 18, 2023.
Burton A. Krumholz, M.D. ’53, died on July 21, 2022. He was 93.
William F. Spence, M.D. ’53, died on August 11, 2023. He was 95.
Irving Glassman, M.D. ’51, died on February 16, 2023. He was 101.
Rose E. Merino, M.D. ’49, died on August 22, 2022. She was 97.
William B. Kantor, M.D. ’48, died on September 30, 2023. He was 98.
Jerrold L. Wheaton, M.D. ’47, died in October 2022. He was 101.
Fredrick Z. Bierman, M.D., senior associate dean and professor of pediatrics, died on February 16, 2024. He was 76.
Janet Piscitelli, M.D., clinical associate professor of pathology, microbiology and immunology, died on January 24, 2023. She was 61.
Brahma Raju Mopidevi, Ph.D., assistant professor of pathology, microbiology and immunology, and director of the Genomics Core Lab, died on February 4, 2024.
Stuart A. Paris, died on December 12, 2022.
Find
Z. Bierman, M.D.,
Senior Associate Dean and Professor of Pediatrics
(1947 – 2024)
Prominent pediatric cardiologist, innovator in pediatric echocardiography, and astute leader in graduate medical education known for his kindness and compassion, Fredrick Z. Bierman, M.D., died on February 16, 2024, at the age of 76. He also served as director of graduate medical education at Westchester Medical Center and practiced at Children’s and Women’s Physicians of Westchester. His career spanned treating the tiniest patients with heart defects as well as caring for their families in times of uncertainty, to training hundreds of residents and cardiac fellows.
Dr. Bierman dedicated his life to the field of pediatric cardiology and will be remembered as a devoted mentor and skilled clinician. He joined New York Medical College in 2011, and in 2012, he was chosen for the honor of serving as mace bearer at the 153rd commencement exercises.
Prior to joining NYMC, he served as chair of the Department of Pediatrics at Cohen Children’s Medical Center, the chief of pediatric cardiology at Schneiders Children’s Hospital, and professor of pediatrics at Albert Einstein College.
Dr. Bierman was regularly recognized as one of the Best
Doctors in America and the Best Doctors in New York. He authored numerous publications, including work on his area of expertise, Kawasaki’s Disease. His pioneering research activity, clinical acumen, teaching excellence and scholarly output earned him a national and international reputation in the field of pediatric cardiology.
Dr. Bierman earned his medical degree, cum laude, from SUNY Downstate College of Medicine and completed his internship and residency at Mount Sinai Medical Center and fellowship in Pediatric Cardiology at Boston Children's Hospital.
New York Medical College (NYMC) and Touro University (TU) rolled out the second volume of the breakthrough journal, Medical Halachah Annual in May 2024, edited by Edward Lebovics, M.D., the Sarah C. Upham Professor of Gastroenterology and interim chair of the Department of Medicine, NYMC. Building on the success of Volume 1, Medical Halachah Annual, Volume 2: Applying Classic Principles to Contemporary Practice, addresses the conundrums posed by new medical technologies and evolving health care challenges. The latest installment comes after the release of last year’s Medical Halachah Annual, Volume 1: The Pandemic and Its Implications, which covered the insights of expert rabbies and physicians who explored the ongoing and ever-changing pandemic and its far- reaching implications through the intersection of halachah, medical ethics, and contemporary medical issues. Volume 3 will be available in 2025.
The inaugural issue of Medical Halachah Annual, published by Touro University/New York Medical College, is simply a triumph. The editors have gathered groundbreaking and thorough articles on eternal and contemporary issues from significant talmidei chachamim, including some who have not previously published extensively in this field. The articles are lively and informative without being superficial. The volume can be read for pleasure and information and should then be kept as an essential reference.
— Rabbi Aryeh Klapper, JewishPress.com
2 Both volumes are available for purchase at




1 Members of the NYMC community joined Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, for a field trip in April 2023, to The Cushing Center at Yale University School of Medicine to view an archival collection of more than 2,200 case studies, which includes human whole brain specimens, tumor specimens, microscopic slides, notes, journal excerpts, and more than 15,000 photographic negatives dating from the late 1800s to 1936.
2 The new Drs. Esther and Ben Chouake Student Commons in the School of Health Sciences and Practice provides a space for students to study or unwind with board games or a game of ping pong and offers grab-and-go food and drinks.
3 The NYMC community celebrated Leonard Newman, M.D. ’70, professor and chair of the Department of Pediatrics, and Michael Gewitz, M.D., professor and vice chair of the Department of Pediatrics, for their decades of service to the College and their impact in the field of pediatrics with the unveiling of their portraits in April 2023.
4 For more than 25 years, the Blanche and Albert Willner Playground in the student housing complex has been a source of enjoyment for children residing on campus. Today, that enjoyment continues, thanks to the hard work and resourcefulness of the student housing maintenance team, who recently refurbished the equipment and play area.

5 Renovations at the Nicholas and Liberta Testa Fitness Center in the student housing complex have significantly enhanced the workout experience. Students can enjoy upgraded equipment and flooring, a new layout, and a fresh coat of paint. Cardiovascular equipment including ellipticals, treadmills, and stationary bicycles, free weights, as well as Nautilus and universal machines are available.





6 NYMC revealed a cutting-edge fitness haven with the recently renovated Dr. Edward F. and Mrs. Anna M. Asprinio Fitness Center in 19 Skyline Drive to enhance the overall well-being of the campus community. The latest state-of-the-art fitness equipment from cardio machines to strength training equipment, includes a new Smith Machine. The fitness center also features a space dedicated to functional training and yoga classes to allow for more versatile and dynamic workout options.
7 In October 2023, the College proudly showcased the new laboratory renovations in the Basic Sciences Building with a ribbon-cutting ceremony and tours. The newly renovated area includes 17,000 square feet of multi-disciplinary research space, 3,000 square feet of shared core instrumentation space, and the installation of flexible casework systems and best-in- class equipment to foster innovation and collaboration.
8 A state-of-the-art golf simulator was installed on campus to provide a realistic and immersive golfing experience with high-definition graphics with multiple virtual golf courses to choose from. The golf simulator was made possible by the generosity of the NYMC Board of Advisors and Martin S. Katzenstein, M.D. ’78, chair of the Board of Advisors, assistant dean for clinical affiliations, and associate professor of pediatrics.
9 Meyer J. Simon, M.D. ’25, was a firstgeneration Jewish immigrant pursuing medicine at NYMC during a time when most United States medical schools imposed an anti-Semitic admissions quota. During the College’s Hannukah celebration in December 2023, the community unveiled Dr. Simon’s portrait and diploma, gifted to the school by his grandson Gary Tannenbaum, M.D., RVT, FACS. It is fittingly on display in the Alumni House.

10 The NYMC community can now enjoy a game of life-sized chess outside the Medical Education Center. The board measures 16 feet by 16 feet while the pieces stand three feet tall, providing an engaging and larger-than-life experience for chess enthusiasts on campus.
11 Yonkers, New York-based artist Biagio “Gino” Civale gifted his abstract mixed media mural from the 1980s, titled, “Strolling Through Tibbetts Park in Yonkers,” to the College for students to appreciate art as they study for their careers in the sciences. The piece is proudly displayed in the NYMC Café for all to enjoy.
For the Period from July 1, 2022 through June 30, 2023
Thank you to all of our generous donors whose support is critical to the success of our students, faculty, researchers, and the entire NYMC community.
The Chancellor’s Circle honors those who make a significant gift or commitment within a single year. In this Circle, there are four Societies distinguished by the nature and size of contributions to the College.
This society is comprised of donors whose gifts and commitments are $50,000 or more.
Anonymous – 1
Estate of Helen MacKay
Estate of Kazuko Nagamatsu
Florida Crystals Corporation
Jonathan B. Gavras, M.D. ’86
Moshe E. Hirth, M.D. ’88
Benjamin H. Homan Jr. Charitable Trust
Mario A. Inchiosa Jr., Ph.D.
Estate of Gerald H. Kass, M.D. ’51
Mr. Ruben Medina
Nikirahul Foundation
New York Medical College Board of Advisors
Pediatric Cancer Research Foundation
Joseph and Penina Popack
Alan Rosenthal, D.M.D.
Mildred Rothstein Rosenthal Family Foundation
Rabi R. Sinha, M.D.
Estate of Vera L. Tedesco
Sarah Upham Trust
This society is comprised of donors whose gifts and commitments are $25,000 to $49,999.
Nanakram Agarwal, M.D.
David E. Asprinio, M.D.
Atlantic Charitable Foundation
Jason Barnett, Esq.
Boston Children's Health Physicians
Breslin Research Foundation
Drs. Ben and Esther Chouake
Alan D. Dauer, M.D. ’62
Estate of Janice Kiss
The Sidney E. Frank Foundation
Gary S. Gettenberg, M.D. ’83
Munr Kazmir, M.D.
Walter M. Lewis, M.D. ’91 and Christel Bauer, M.D.
Dr. Meryl Mark and Mr. Joseph Mark
Reva and Martin Oliner
Paul D. Ostrovsky, M.D. ’78
Mr. and Mrs. Vikram S. Pandit
Chong H. Park, M.D. ’96
Lee B. Pressler, M.D. ’90
Jonathan A. Sheindlin, M.D. ’93
Westchester Medical Center
This society is comprised of donors whose gifts and commitments are $10,000 to $24,999.
Anonymous – 2
The Bloomgarden Family
California Bank and Trust
Mrs. Nancy M. Danner
Mrs. Delores DelBello
William H. Frishman, M.D.
Annette E. Kussmaul, M.D. ’93
Laurel Foundation
Mr. and Mrs. Andrew Levy
Mr. Arthur Luxenberg
Marmor Foundation
Mr. Barry M. Menel
Edward J. Messina, Ph.D. ’73
Dr. and Mrs. Lawrence F. Neshiwat
Pavarini Construction Company, Inc.
Mitchell Pincus, M.D. ’53
Mr. and Mrs. Ronald F. Poe
Avi Retter, M.D.
Barry S. Robbins, M.D. ’73
Seize the Ribbon
Starfish Fund
Mark T. Thompson, M.D. ’71
Vincent J. Vigorita, M.D. ’76
Webster Bank
Weitz & Luxenberg
Westfair Communications
Mr. Norman Young
This society is comprised of donors whose gifts and commitments are $2,500 to $9,999.
Anonymous – 7
ACA Environmental Services, Inc.
Alpha Omega Alpha
Robert Alter, M.D.
Mykola R. Alyskewycz, M.D. ’92
American Online Giving Foundation
Robert W. Amler, M.D., M.B.A. and Sherlita Amler, M.D.
Stephan Ariyan, M.D. ’66
Gladys M. Ayala, M.D., M.P.H.
Robert A. Barish, M.D. ’79
Howard M. Baruch, M.D.
Dr. and Mrs. Francis L. Belloni
Augusta H. Belmonte, M.D.
Frank Berkowitz, M.D. ’83
Dr. Denis A. Bouboulis, M.D. ’86
Dr. and Mrs. Mitchell Cairo
Mr. William J. Camera, CPA
Cantigny Research Foundation, Inc.
Philip C. Caron, M.D. ’86
Steve H. Chang, M.D. ’02
Edward Chew, M.D. ’03


Eric I. Choe, M.D. ’88
CINQCARE
Costanza Cocilovo, M.D. ’96
Cozen O'Connor Foundation, Inc.
Ms. Virginia Davenport
Deloitte Foundation
Mr. Alfred Donnellan
Mr. and Mrs. Franklin L. Earle
Eisner Amper Group
Emalie and John Feerick
Stephen Ferrando, M.D.
Noreen F. Bedini Ferrante, M.D. ’84
John P. Fezza, M.D. ’92
Kathleen Case Finzel, M.D. ’87
Eric C. Fok, M.D. ’93
Nancy J. Freeman, M.D. ’81
Mark J. Friedman, M.D. ’71
Garfunkel Wild, P.C.
Dr. Michael and Mrs. Judy Gewitz
Mrs. Jennifer Amler Goldstein
Arun Goyal, M.D. ’90
Karen E. Grimmell, M.D. ’61
Anita Grover, M.D. ’78
Gregory P. Harvey, M.D. ’83
Col. Paul B. Heller, M.D. ’68
Richard N. Hirsh, M.D. ’69
Hudson MSO, LLC
Mr. and Mrs. Paul Ingrassia
Sumeet A. Kadakia, M.D. ’07
Dr. and Mrs. Alan Kadish
Alan L. Kalischer, M.D. ’77
Martin S. Katzenstein, M.D. ’78
KPMG, LLP
Steven L. Lansman, M.D., Ph.D.
Christopher S. Leonard, Ph.D.
Mrs. Diane L. Levere
Mr. Darrin Litsky
Mr. Juan R. Lopez
Jocelyn A. Luongo, M.D. ’06
Peter P. Ly, M.D. ’96
George D. Lyons, M.D. ’92
Richard J. Macchia, M.D. ’69, FACS
Norman L. Maron, M.D. ’70
James F. McGroarty, M.D. ’68
Catharine Smith Mehl
Molina Healthcare
Ms. Ellen-Jane Moss
Jerry L. Nadler, M.D., MACP, FAHA, FACE
NYC Health + Hospitals
Leonard J. Newman, M.D. ’70 and Randi Newman
NextGen
Mary Alice O'Dowd, M.D. ’76
Paris International Partners, LLC
Mr. Michael Paris
Peapack Private Bank
Alan E. Peters, M.D. ’79
Physician Affiliate Group of New York, P.C. (PAGNY)
Barbara Pineda, M.D.
Ammir S. Rabadi, M.D.
John T. Repke, M.D. ’78
Mr. and Mrs. Stanford Robertson
Richard E. Rohr, M.D. ’80
Adam D. Rubin, M.D. ’00
RV Consulting, LLC
Saint Joseph's Medical Center, Yonkers, NY
Mr. Bruce J. Schanzer
Neil Schluger, M.D.
Pravinkumar B. Sehgal, M.D., Ph.D.
Masaki and Setsuko Shirota
The Sigmund Foundation
Society of Family Planning Research Fund
Barbara R. Sommer, M.D. ’79 and
Alan Fisher, M.D.
Stifel Nicolaus & Company, Inc.
Sundry Donors
Susanne Vasquez Revocable Trust
Jay D. Tartell, M.D. ’82
The Caron Family Fund
Mr. and Mrs. Kenneth Theobalds
Gigi Thomas, M.D.
United Healthcare Corporation
John L. Vigorita, M.D., Memorial Fund
Warsaw ENT
David Werdegar, M.D. ’56
William J. Camera & Company
Robert M. Yacynych, M.D. ’88
Mr. Gerry Yen
Daniel Zelazny, M.D.
Barry M. Zisholtz, M.D. ’83
$1,000 to $2,499
Anonymous – 4
Ann Alexander, M.D. ’78
Michael S. Alexander, M.D. ’78
Mr. and Mrs. James Amler
Firdose S. Ansari, M.D. ’05
Andrew N. Antoszyk, M.D. ’83
Bank of America Corporation
Thomas J. Beggins, M.D. ’84
Mr. Steven Bodine
Arnold J. Brender, M.D. ’81
Joel I. Brenner, M.D. ’70
Howard S. Bush, M.D. ’82
Mrs. Joi Butler
Calvary Fund, Inc.
Dr. and Mrs. Joseph Canterino, D.D.S.
Catherine G. Caronia, M.D. ’88 and
Ronald M. Caronia, M.D. ’88
Carr Business Systems
Christopher T. Channon, M.D. ’76

Charities Aid Foundation of Americas
Michael T. Charney, M.D. ’66
Mr. Bin Chen
Frank M. Chieu, M.D. ’71 and Barbara Chieu
Shafi K. Choudhury, M.D. and Muhammad S. Choudhury, M.D.
Cigna Healthcare
Harvey E. Cooper, M.D. ’60 and Mrs. Lynn Cooper
Ms. Juanita Costa
Gabriel G. Curtis, M.D. ’62 Trust
Elliot Davidoff, M.D. ’71
Kien-An Duong, M.D. ’01
Lauren N. Elliston, M.D. ’08
Mill Etienne, M.D. ’02, M.P.H. and Aynalem Zemedeberhan, M.P.H. ’01
William Etra, M.D. ’69
Faculty Dental Associates, PC
Burton M. Fink, M.D. ’71
The Flatley Charitable Fund
Dr. and Mrs. John A. Fox
Franklin Templeton
Linda K. Friedman, Ph.D.
Steven M. Fruchtman, M.D. ’77

Chirag Gandhi, M.D.
Mr. Tom U. Gardner
Renee Garrick, M.D.
Harvey A. Glasser, M.D. ’64
Mr. Mark Goldstein
Stuart A. Green, M.D. ’67
Mr. and Mrs. Hugh Greenberg
David J. Gross, M.D. ’84 and Maria Gross
Edward C. Halperin, M.D., M.A.
Henry W. Hanff, M.D. ’69
Lloyd P. Haskell, M.D. ’77
Nancy Lee-Hata, M.D. ’02 and Justin T. Hata, M.D. ’02
Hi-Link Technology Group
Hinman Straub, P.C.
Mrs. Beth Hordines
Steven H. Horowitz, M.D. ’66
Albert L. Huber, M.D. ’57
Mark Hurwitz, M.D.
Kelly A. Hutcheson, M.D.
Mr. James E. Inglis
Mariko L. Ishimori, M.D. ’00 and Nicholas Testa, M.D. ’01
Jackson Lewis P.C.
Johnson & Johnson Family of Companies
James W. Justice, M.D. ’58
Drs. Elisa and Steven Kadish
Uchenna P. Kalu, M.D.
Harvey S. Kaplan, M.D. ’63

Sungja Kim
Mr. and Mrs. Sung-Hyun Kim
David F. Kosnick, M.D. ’73
Mark A. Krich, M.D. ’97
Edmund F. Lagamma, M.D. ’76
Col. and Mrs. Daniel F. Lally
Rebbecca Lambert
Nicholas F. LaRusso, M.D. ’69
Robert F. Lautin, M.D. ’70
Lawless Family Fund
Dr. and Mrs. Zvi Lefkovitz
Jerry I. Levine, M.D. ’77
Norman Levine, Ph.D.
Debra A. Levinsky, M.D. ’76
Joseph K. Lobl, M.D. ’82


Peter J. Lucas, M.D. ’72
George W. Lutz, M.D. ’61
William W. MacLaughlin, M.D. ’81
Janet A. Madigan, M.D. ’77
Diane J. Madlon-Kay, M.D. ’79 and Richard C. Madlon-Kay, M.D. ’79
James O. Maher III, M.D. ’82
Ada M. Marin, M.D. ’83, M.P.H.
The Marino Organization, Inc.
Mr. Francis C. Marino
Ms. Rosemary A. Martino
Hussein M. Matari, M.D.
Peter P. McKellar, M.D. ’70
Robert J. McNamee, M.D. ’75
Brenda A. Merritt, M.D. ’65
James L. Mills, M.D. ’73
Simone E. Mordas, M.D. ’91
Tamara Moss, M.D. ’92
Eric Mustonen, M.D. ’75
Dr. and Mrs. Ronnie Myers
NYMC Office of Student Affairs
James J. O'Brien, Ph.D.
Mr. Timothy G. O'Connor
Mr. Mark G. Oschmann
Douglas E. Padgett, M.D. ’82
Johanna A. Pallotta, M.D. ’62
Betty A. Cervenak Panariello, M.D. ’78 and Anthony L. Panariello, M.D. ’75
Patricia A. Galvin-Parton, M.D. ’80 and Lance A. Parton, M.D. ’80
James F. Passarelli, M.D. ’89
Myles L. Pensak, M.D. ’78
Joseph W. Placer, M.D. ’64

Charles R. Rich, M.D. ’74
Meaghan S. Roche, M.D. ’14
Michael H. Rosenberg, M.D.
Rachel Rubinstein, M.D. ’83
Sandra L. Sacks, D.D.S., M.D. ’97 and Harry G. Sacks, D.D.S., J.D.
Mr. William Saich
Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
Theodore J. Schmahai, Ph.D. ’88
John H. Seward, M.D. ’61
Deborah A. Shapiro, M.D. ’89 and Alan R. Plumer, M.D. ’88
Win Shen, M.D. ’83
Sanford Sherman, M.D. ’56
Marc Silverman, M.D.
Jeffrey E. Silverstein, M.D. ’91
Smiles From Joey, Inc.
Lori Solomon, M.D. ’99, M.P.H. ’09
Jonathan E. Sonne, M.D. ’98
Joseph F. Stein Family Foundation, Inc.
Frederick Steinberg, M.D. ’58
Michael S. Stewart M.D.
Kenneth B. Strumpf, M.D. ’82
Stryker
Ross H. Taff, M.D. ’74
Marvin B. Tankel, M.D. ’80
The James E. Inglis & Patricia M. Burns Fund
The Parkside Group, LLC
The Salon Family Foundation, Inc.
This Close for Cancer Research, Inc.
TIAA-CREF
Nancy N. Tsai, M.D.
Scott K. Varland, D.D.S.
Angela R. Verardo, M.D. ’12
Susan L. Vogel, M.D. ’76
Steven Weinstock, M.D. ’74
Scott S. Weiss, M.D. ’88
Welch Family Charitable Fund
Douglas N. Whatmore, M.D. ’77
Dr. Patricia White and Mr. Daniel Flatley
Mr. Ning Yao
Richard J. Zeman, Ph.D.
$250 to $999
Anonymous – 14
A.J. Indusi Plumbing and Heating, Inc.
Syed A. Abbas, M.D.
Mr. M. Laniado Abraham
Ms. Lucille P. Accetta, M.P.H. ’04
Peter J. Acker, M.D.
Lori H. Adcock, M.D. ’85 Adelaidegray, LLC
Robert M. Ahrens Jr., M.D. ’78
Judith C. Ahronheim, M.D.
Mr. Lee M. Allen II
Dananski Allonce
Gregory L. Almond, M.D., M.P.H. ’00, M.S. ’00
Salomon Amar, D.D.S., Ph.D.
Ms. Karel R. Amaranth, M.P.H. ’10
Mrs. Peggy Amler
David R. Andrews, M.D. ’78
Joseph J. Angella, M.D. ’64
Robert and Amy Ansehl
Mr. Kerrin Antommarchi
APTA New York, Inc.
ARC Document Solutions
Matthew J. Arduino, Dr.P.H., M.S. ’81
Ms. Ingrid C. Armstrong, M.S. ’01
Marie T. Ascher, M.S., M.P.H.
Mark R. Axelrod, M.D. ’79
Masoud M. Azizad, M.D. ’99
Gildy V. Babiera, M.D. ’91
Charles J. Bacall, M.D. ’75
Mahrukh D. Bamji, M.D.
Kenneth S. Bannerman, M.D. ’75
Stephanie C. Barnhart, M.D. ’08, M.P.H ’08
Patricia A. Barry, M.D. ’83 and John M. Cosgrove, M.D. ’83, FACS
Robert S. Bartolomeo, M.D. ’71
Basil Guralnick Berstein, M.D., Tzedakah Fund
Christine H. Beck, M.D. ’77
Richard D. Becker, M.D. ’79
Richard H. Becker, M.D. ’79
William J. Behrje, M.D. ’65
Barbara R. Bellar, M.D., J.D., M.A., M.P.H., M.Div.
The Benevity Community Impact Fund
Stewart R. Berliner, M.D. ’88
Mrs. Carol Bernot
Basil G. Bernstein, M.D. ’67
Richard Besserman, M.D. ’64
Peter Bloom Jr., M.D. ’04, M.S. ’00
Devon E. Bock, M.D. ’86
Peter N. Bogdan, M.D. ’64
Lisa C. Bogdonoff, M.D. ’88
Jason S. Bonslaver, M.D. ’06
Michael D. Brandler, M.D. ’98
Brown & Weinraub, PLLC
Tonya M. Brown-Price, M.D. ’90
Alexander J. Brucker, M.D. ’72
Jack Bruder, M.D. ’82
Jerome M. Burke, M.D. ’84
Felipe C. Cabello, M.D.
Joseph J. Calandra, M.D. ’82
Joseph A. Camilleri Jr., M.D. ’85
Howard D. Cantwell, M.D. ’65
Maria F. Capparelli, M.D. ’07
Care Security Systems, Inc.
Dr. and Mrs. Stephen F. Carolan ’84
Mark Catterall, M.D. ’96
CDWFA Trust
Joseph E. Cerbone, M.D. ’82
Ms. Renee Chan
Burawit B. Charuworn, M.D. ’99
Hee-Joo Cheon-Schingo, M.D. ’92
and Victor A. Schingo, M.D. ’92, FACS
Richard J. Chernick, M.D. ’91
Mr. and Mrs. Henry Chew
Qwie T. Chew, M.D. ’65
Alvin J. Chisolm, M.D. ’68
Alfonso P. Ciarlo, M.D. ’65
City Orthopaedics, PLLC
Lisa A. Clancy-Vieira, M.D. ’87
Anthony A. Clemendor, M.D.
Kenneth Cohn, M.D. ’68
John J. Connolly, Ed.D.
Mr. Raymond A. Conta, J.D.
Jonathan D. Cooper, M.D. ’87
Martin A. Cooper, M.D. ’63
Ms. and Mr. Anthony Corvini
Michel-Alexis R. Courtines, M.D. ’98
Dr. and Mrs. Robert E. Crootof ’70
Mr. James Curran
Terrance M. Daino, M.D. ’90
Mr. Jeffrey Dankberg
Lorelei S. Davidson, M.D. ’91
Robert A. Davis, M.D. ’74
Henry C. DeBlasi, M.D. ’89
Henry P. Deblasi, M.D. ’55
Kevin C. Delahanty, M.D. ’84
Maria Salome R. Desquitado-Tabora, M.D.
Bram A. Dolcourt, M.D. ’04
Janet P. Dolot, M.S., D.P.T., P.T., Dr. P.H. ’14
Gary R. Donshik, M.D. ’66
James E. Doran, M.D. ’75
Allen J. Dozor, M.D.
E M Winters Financial Services, Inc.
Thomas J. Early, M.D. ’73
Joseph G. Edelson, M.D. ’78
Daniel Elefant M.D. ’17
Andrew A. Elimian, M.D.
Christopher E. Emond, M.D. ’03
Jaleh Z. Eslami-Borsody, M.D. ’94
Victor G. Ettinger, M.D. ’67
John C. Evanko, M.D. ’95
Christine M. Fanning, M.D. ’11
Edward Farkas, D.D.S.
Theodore S. Feinson, M.D. ’78
Michael J. Feinstein, M.D. ’64
Dr. and Mrs. William N. Fenney, M.D. ’79
Frederick S. Fensterer, M.D. ’70
Craig Allen Fenton, M.D. ’68
Ilona W. Figura, M.D. ’83
Douglas G. Finn, M.D. ’75
Robert R. Flanagan, M.D. ’75
Ms. May T. Flowers
Mr. Edward J. Flynn
Arlene A. Forastiere, M.D. ’75
Susan Fox, M.Ed., M.A., Ph.D.
Ms. Teri Frangie
Denis J. Frank, M.D. ’71
Beth R. Freedman, M.D. ’06
Sarise Freiman, M.D. ’76
Deborah Fried, M.D. ’83
Paul D. Fuchs, M.D. ’51
The Fuller Foundation
Col. Roger A. Gallup, M.D. ’91
Robert I. Gelb, M.D. ’80
Mr. David George
Laurence D. Goldstein, M.D. ’84
Paul Goldstein, M.D. ’71
Juan P. Gonzalez, M.D. ’94
Jill A. Gradner, M.D. ’94
David N. Greenman, D.D.S., M.P.H. ’07
Richard H. Greif, M.D. ’75
Martin A. Gross, M.D. ’81
Thomas R. Gruffi, M.D. ’13
Bonnie and Paul Heindl
Mrs. Jill A. Haas
Naomi R. Ham, M.D. ’84 and Elmer C. Agustin, M.D., M.P.H. ’15
Irwin Hametz, M.D. ’73
Adam Hammerman, M.B.A., CNE
Timur Hanan, M.D.
Kathleen A. Heffernan, M.D. ’81
Edward R. Heilman, M.D. ’74
Naida M. Henriquez, D.M.D.
Edward R. Herman, M.D. ’82
L. S. Herman, M.D. ’74
Stephen L. Hermele, M.D. ’68
Robert A. Herzlinger, M.D. ’69
Mark E. Higgins, M.D. ’94
Robert D. Hirsch, M.D. ’61
Peter Hoffmann, M.D. ’83
Marina K. Holz, Ph.D., M.P.H. ’23
Rivka S. Horowitz, M.D. ’78, Ph.D.
Stephen K. Hoverman, M.D. ’78
David C. Huang, M.D. ’75
Mr. Darren Hugo
Magdalen E. Hull, M.D. ’79, M.P.H.
Pamela S. Ingber, M.D. ’76

Kendra G. Gil, M.D. ’04 and Eric A. Gil, M.D. ’03
Mina A. Gillers, M.D. ’73 and Bruce J. Gillers, M.D. ’73
Glenn D. Gilmor, M.D. ’86
Jeffrey B. Ginsburg, M.D. ’92
Give Lively Foundation, Inc.
Daniel J. Glatt, M.D., M.P.H. ’92
Albert C. Goldberg, M.D. ’63
Barry S. Goldberg, M.D. ’95
David A. Goldenberg, M.D. ’74
Mr. Gary W. Goldstein

Lee J. Isabell, M.D.
Humayun K. Islam, M.D., Ph.D.
Mokarram H. Jafri, M.D. ’94
Ms. Andrea B. Jeffries
Mrs. Nancy J. Jessen
Miao Jiang, Ph.D. ’04
Benjamin F. Johnson, Ed.D.
Heather D. Johnson, M.D. ’02 and John P. Magnan, M.D. ’02
Alice A. Jones, M.D. ’78
Curtis T. Jones, M.D. ’75
E. Ladd Jones III, M.D.
Sharon Jordan and Edward F. Jordan, M.D. ’72
Peter J. Joson, M.D. ’98
Mr. Adam Juechter
Mrs. Kay Juechter
Jae H. Jung, M.D. ’03
Ms. Lila Kagedan
Lawrence S. Kaminsky, M.D. ’78
Ms. Ellen M. Kaplan, M.P.H. ’98
Mr. Seymour Kaplan
Elizabeth M. Kass, M.D. ’88
Kenneth G. Kasses, Ph.D. ’74
David J. Katz, D.D.S.
Jerald W. Katz, M.D. ’84
Jennifer J. Halstead-Kenny, M.D. ’02 and John M. Kenny, M.D. ’01
Roberta D. Sengelmann-Keshen, M.D. ’93 and Tamir H. Keshen, M.D. ’93
John G. Ketterer Jr., M.D. ’61
Dr. and Mrs. Jordan Kirsch
Evan M. Klass, M.D. ’76
Steven D. Klein, M.D. ’98
William S. Knight, M.D. ’91
Dr. Ann Susan Kober Werner
Jennifer Koestler, M.D.
Steven E. Kong, M.D. ’11
Mitchell S. Kramer, M.D. ’85
Leonard B. Krich, M.D. ’65
Stewart Krug, M.D. ’72
Jin Li, M.D., Ph.D. ’01 and Gary Guo, M.D., Ph.D.
Mr. and Mrs. Sheon Sang Liao
Leslie LiDonnici, M.D. ’78
Scott M. Lieberman, M.D. ’87
Joan P. Liman, M.D. ’83, M.P.H. ’93
Charles Lomanto, M.D. ’63
Ms. Taryn Looney
Linda C. Leedie-Lowe, M.D. ’82 and Robert N. Lowe, M.D. ’82
Tyler S. Lucas, M.D.
Pamela Ludmer, M.D.
Carl B. Lundborg, M.D. ’67
Maja L. Lundborg-Gray, M.D. ’95
and Daniel S. Gray, M.D. ’91
Robert F. Mackey, M.D. ’77
Gregory H. Mahairas, M.D. ’59
Bella Mikhailova Malits, M.D. ’90
Marc M. Silverman, M.D., P.C.
Craig W. Markert, M.D. ’73
Alan B. Marks, M.D. ’78
Jon O. Marks, M.D. ’76
William E. Marshall, Ph.D.
Mr. Michael J. Martin
Maspeth Federal Bank
Mr. Ronald Matten
Matthew & Tony General
Landscaping, Inc.
Maureen Matturri, M.D. ’66

Mr. Rocco Labella
Lakeside Dermatologh, LLC
Michael L. Lapkin, M.D. ’65
Ms. Hattie W. Law
Mark J. Leber, M.D. ’76
Dr. Edward and Renee Lebovics
Benjamin Lee M.D.
Louis H. Lefkowitz, M.D. ’64, FACOG, FACS
Armand F. Leone Jr., M.D. ’82
Jesse A. Levin, M.D. ’09
Ellen R. Lewis
John A. Lewis, M.D. ’93
Baoqing Li, M.D. ’05
James T. Mazzara, M.D. ’63
James K. McAleer, M.D. ’63
Rebecca A. McAteer Martin, M.D. ’08
Edward J. McCartin Jr., M.D. ’63
McElrath Family TRT
Thomas G. McElrath, M.D. ’59
Mrs. Judith McGreevy
Ms. Karen McKercher
Ms. Anastasia McPeak
Ms. Leah McPhee
Camille A. McPherson, M.D. ’03
Melman Family Fund
Martin K. Melman, M.D. ’74
John H. Mensher, M.D. ’67
Bruce A. Miller, M.D. ’67
Mr. Gregory C. Miller
William Edward Miller, M.D. ’76
Tracey A. Milligan, M.D.
Steven D. Mills, M.D. ’99
Helen M. Higgins Minetti, M.D. ’70
Michael A. Miranda, M.D. ’92
Jamil Mohsin, M.D.
Marisa Montecalvo, M.D.
Alan H. Morelli, M.D. ’82
Fernando Moreno, M.D. ’79
Augustine L. Moscatello, M.D.
Kimberly L. Motta, M.D. ’97
Richard E. Murphy Jr., M.D. ’61
Karen M. Murray, M.D. ’99
Naida Henriquez, D.M.D., P.C.
Margaret Mackin Nally, M.D. ’08
Barry E. Nash, M.D. ’65
Mr. George F. Nestler
Aron Neuhaus, M.D. ’71
Amy N. Nguyen, M.D.
Kelly A. Siano, M.D. ’11
Mrs. Mary Norton
Richard E. Nussbaum, M.D. ’80
Stephen A. Obstbaum, M.D. ’67
Guy R. Orangio, M.D. ’79 and Mrs. Patricia Orangio
Edward Orff, Ph.D. ’99
Ms. Lynne Oxboel
Debra M. Parisi, M.D. ’98
Thomas R. Patnaude, M.D. ’74
Derek K. Paul, M.D. ’91
Mr. and Mrs. Bruce Pauls
Rachel A. Perla, M.D. ’95
Elizabeth G. Perry, M.D. ’62
John R. Person Charitable Trust
John R. Person, M.D. ’73
Joanna C. Pessolano, M.D. ’81
Mary M. Petzke, Ph.D.
V. Rachel Phillips, M.D. ’79
Mr. and Mrs. Charles Phipps
Mr. John Piccione
William J. Pickering, M.D. ’71
Mrs. Teletta A. Piper
Francis J. Pizzi, M.D. ’69
Jane M. Ponterio, M.D. ’81
Ms. Ingrid A. Porter, M.P.H. ’00
John M. Powers, M.D. ’77
Glenn M. Preminger, M.D. ’77
Joseph P. Rafferty Jr., M.D. ’87
Laurence M. Raiford, M.D. ’77
Sudhamani R. Rao, M.D. and
Sateesh C. Babu, M.D.
Jyoti Rau, M.D. ’02, Ph.D.
RBT CPAs, LLP
Regintex Insurance Brokerage
Laura M. Reich, M.D.
Margaret A. Reilly Living Trust
Margaret A. Reilly, Ph.D. ’81, M.S. ’78
Mr. Lawrence Rein
Anne Negrin Reis, M.D. ’02
Mr. Padraic B. Reynolds, M.P.H. ’14
Seth J. Richter, M.D. ’94
River Run Partners
Michael J. Rogers, M.D. ’82
Ana Rojas, M.D. ’95
James J. Rooney, M.D. ’74
Nancy C. Rose, M.D. ’84 and G. Marc Jackson, M.D.
Ms. Pearl Rosenbaum
Katha Rossein, M.D. ’78 and Ronald M. Razzore, M.D. ’78

Kathleen M. Rossy, M.D. Rotundo Plumbing Corp
Philip S. Rubin, M.D. ’87
The Terri & Matty Russo Fund
Esther L. Sabban, Ph.D.
Marc R. Salzberg, M.D. ’76
Srivilliputtur G. Santhana Krishnan, M.D.
Debjeet Sarkar, M.D. ’05
Ellen Sawamura, Ph.D.
Donald E. Sawyer, M.D. ’70
Amit Saxena, M.D. ’06
Steven D. Schaefer, M.D.
Mrs. Anne E. Schneider
Robert Schneider, M.D. ’69
Jeffrey A. Schor, M.D. ’91, M.P.H., M.B.A.
Henry G. Schriever, M.D. ’60
Eric H. Schultheis, M.D. ’88
Schultz Eye Clinic
Gerald R. Schultz, M.D. ’63
Holly A. Schwartz, M.D. ’91
Jerold Schwartz, M.D. ’56
Martin A. Schwartz, M.D. ’75
David F. Sciortino, M.D. ’78
John P. Sheehy, M.D. ’75
Bruce E. Sherling, M.D. ’73
Tighe P. Shomer, M.D. ’77
Suzanne M. Shroba, M.D. ’91, M.S. ’89

Stacey A. Simons, M.D. ’06
David L. Smith, M.D. ’61
Michael C. Smith, M.D. ’12
Edward L. Snyder, M.D. ’73
John C. Somberg, M.D. ’74
Mr. Anthony M. Sozzo, M.A., M.S.Ed.
Kathryn Spanknebel, M.D.
Lawrence M. Spergel, M.D. ’71
Carl P. Stamm, M.D. ’80, M.S. ’76
David J. States, M.D. ’53
Mr. Franklin M. Steen
David A. Stein, M.D. ’75
John T. Stinson, M.D. ’75
Mr. Joel Sturm
Viktor P. Sulkowski, M.D. ’71
Mark H. Swartz, M.D.
Mr. Jian-Zhen Tan, M.S. ’97
Dr. Jason and the Honorable
Lois Tanzer
The Film Gallery, LLC
The IMA Group
The Sara and Aron Neuhaus Fund
Tonya Brown-Price Living Trust
Christopher A. Tormey, M.D. ’04
Michael J. Trepal, D.P.M.
Chi H. Truong, M.D. ’92
Shiu-Lin Tsai, M.D. ’91
Mr. Michael A. Tugetman
Joel C. Ullman, M.D. ’63
Edward S. Valentine, M.D. ’78
Mr. Hendrick Vandamme
Henry Velez, M.D. ’76
Joseph S. Vetrano, M.D. ’70
Raissa Villanueva, M.D. ’05
James A. Walker, M.D. ’61
William J. Walsh Jr., M.D. ’64
Anna M. Ward, M.D. ’85
Thomas G. Webber, M.D. ’73
William R. Weissman, M.D. ’65
William J. Behrje Living Trust
Barry R. Witt, M.D. ’84
Dr. Norbert S. Wolloch
Philip Wong, M.D. ’96
Douglas A. Woodburn, M.D. ’83
Richard B. Wu, M.D. ’05
Stephanie M. Wyckoff, M.D. ’97
Dr. Wen Xiong, M.S. ’01
Dr. and Mrs. Vincent J. Yakavonis M.D. ’77
Charles S. Yanofsky, M.D. ’77
Sau Yan Yee, M.D. ’92
Mr. Douglas L. York, M.P.H. ’91
Yusif Medical Services, LLC
Mahrouf M. Yusif, M.D.
Gerald W. Zaidman, M.D.
Donna A. Zeide, M.D.
$100 to $249
Anonymous – 20
Faheem A. Abbasi, M.D
Ms. Basilia Adams
Barbara S. Akresh, M.D. ’75
Leonard H. Alberts, M.D. ’72
Richard Allen, M.D. ’65
Ms. Danielle Aloia
Dr. Fons A. Amaye-Obu, M.P.H. ’10
Rudy T. Andriani, M.D. ’81
Carlos A. Arias, M.D. ’14
Arnold N. Benson, M.D. Trust
Bruce Ascher
Ms. Margaret Astrologo
Howard A. Babus, M.D. ’75
Gerald S. Bahr, M.D. ’72
Imran Baig, M.D. ’01
Albert J. Bajohr Jr., M.D. ’67
Nicholas G. Baranetsky, M.D. ’74
Susan Bard M.D.
Karl J. Barsody, M.D.
Paul G. Battaglia, M.D. ’84
Ulrich Batzdorf, M.D. ’55
Richard Beerman, M.D. ’80
Arnold N. Benson, M.D. ’58
David A. Berkowitz, M.D. ’63
Daniel Berson, M.D. ’69
Martin J. Birkhofer, M.D. ’83
Rima A. Bishar, M.D. ’14
Jeffrey S. Bisker, M.D. ’76
Kenneth S. Blatt, M.D. ’75
Edward J. Bloch, M.D. ’69
Mr. Stephen Boatti
Ms. Stefania Bonanni
Nicholas G. Bonvicino, M.D. ’79
William C. Brender, M.D. ’76
Mr. Frederick Brittain
Denton C. Brosius, Ph.D.
David J. Broza, M.D. ’89
Buchan Family Trust
Mr. Leonard and Mrs. Susie Buchan
Jason D. Buchwald, M.D. ’97
Earl A. Bueno, M.D. ’00
Josue J. Burgueno, M.D. ’18
Norman A. Cagin, M.D. ’67
Mr. Raymond Cajulis
Dr. and Mrs. Ronald Caldwell
Michael Campion, M.D. ’82
Joseph R. Carbone, M.D. ’83
Claire J. Carlo, M.D. ’85
Mr. Thomas Carmichael
Dana R. Deravin Carr, Dr.P.H. ’13,
M.P.H. ’01
The James E. Carter Trust

James E. Carter, M.D. ’55
Paul S. Carton, M.D. ’63, FACS
Carl M. Cassin, M.D. ’59 +
Mrs. Lisa J. Cedergren, M.P.H. ’15
Joseph S. Cervia, M.D. ’84 and Denise L. Blumberg, M.D.
Paul B. Chaplin, M.D. ’79
A. Roger Chappelka, M.D. ’57
Michael Chavez Chase, M.D. ’72
Anthony P. Chatowsky, M.D. ’62
Ms. Bess Chazhur
Cynthia Chazotte, M.D. ’81
Roger Chirurgi, M.D.
Ena Chow-Bell, M.D. ’94 and Gregory D. Bell, M.D. ’93
Yun Shin Chun, M.D. ’00
Elizabeth M. Clark, M.D. ’85
Karen Ann Clarke, M.D. ’96, M.P.H. ’94, M.S. ’93
Dr. and Mrs. Wayne A. Colizza, M.D. ’17
Sean Connolly
Alan J. Conrad, M.D. ’81
Dr. Annette and AJ Contento
Seymour M. Cooper, M.D. ’72
Cornwall Neurology PLLC
Imelda Cruz-Banting, M.D.
Rachel Cyrlak, M.D. ’81 and Mr. Edward A. Cusnier
Arthur S. Cytryn, M.D. ’77
Brian G. Daggett, M.D. ’80
Edward G. Dainesi, M.D. ’89
Mrs. Christina M. Damo, M.S. ’10
Ms. Regina Damon
Trung Q. Dang, M.D. ’00
Ms. Inger G. Danner
Marc D. Danziger, M.D. ’92
Kenneth J. Davis, M.D. ’62
Dayton Foundation Depository, Inc.
Timothy B. Deering, M.D. ’72
Ms. Susan Q. DeJoy, M.S. ’94
David M. Denmark, M.D. ’05
Department of Dental Medicine
Vipul Desai, M.D.
Janis DiPietro, M.D. ’79
Mr. and Mrs. David Domreis

J. Franklin Donaldson, M.D. ’54
Ellen P. Donshik, M.D. ’68 and
Peter C. Donshik, M.D. ’68
Shideh Doroudi, M.D.
Doyle Revocable Trust
Donald E. Doyle, M.D. ’67
Husni W. Dweik , M.D.
Mr. James A. Dye
Jennifer L. Edwards, M.D. ’91
Eli Lilly U.S. Matching Gift Program
Mr. and Mrs. Robert S. Faircloth
Faith House Adult Family Home, LLC
Ms. Meghan Fashjian
Kalmen A. Feinberg, M.D. ’64
Ms. Susan Ferrand, M.P.H. ’99
Alex E. Fijman, M.D. ’00
Joel G. Fischgrund, M.D. ’78
Felicity G. L. Fishman, M.D. ’06
Alan M. Fixelle, M.D. ’80
Mr. Robert Fogel
A. P. Fontanetta, M.D. ’73
Bruce I. Friedman, M.D. ’79
Bruce J. Friedman, M.D. ’76
Richard J. Friedman, M.D. ’74
Stanley N. Friedman, M.D. ’68
Mr. Steven J. Friedman
Ms. Josselyn Galdamez ’19
Ian A. Gale, M.D. ’70
Gary A. Gallo, M.D. ’63
Carol A. Garbarino, M.D. ’79
Michael R. Gatto, M.D. ’76
Ronald D. Gellis, M.D. ’77
Margaret M. Gennaro, M.D. ’87
Mr. Guillermo J. Gil
Scott A. Glasser, M.D. ’86
William Glatt, M.D. ’64
Edward H. Glenn, M.D. ’64
Ira D. Glick, M.D. ’61
Kenneth H. Goldblatt, M.D. ’72
Mrs. Rita Gonshorek
Ms. Beth Gorin
Michael S. Graham, M.D. ’07
Frederic W. Grannis, M.D. ’69
Henry J. Green, M.D. ’75
Stephan M. Greenberg, M.D. ’66
Jason R. Grossman, M.D. ’10
Mrs. Janet Guggenheim
Susan D. Ribeiro Guthrie, M.D. ’96
Robert A. Harwood, M.D. ’62
F. Whiting Hays, M.D. ’60
William A. Healy Jr., M.D. ’61
Craig R. Heim, M.D. ’70
Leo A. Heitlinger, M.D. ’78
Louis I. Heller, M.D. ’81
Robert M. Herenstein, M.D. ’85
Jane J. Hew, M.D. ’93
Barbara M. Hisler, M.D. ’83
Martin N. Hochberg, M.D. ’63
Robert C. Holland, M.D. ’84
John S. Hou, M.D. ’97
Scott W. Hoyer, M.D. ’75
Eric L. Hsu, M.D. ’97
John T. Hughes, M.D. ’82
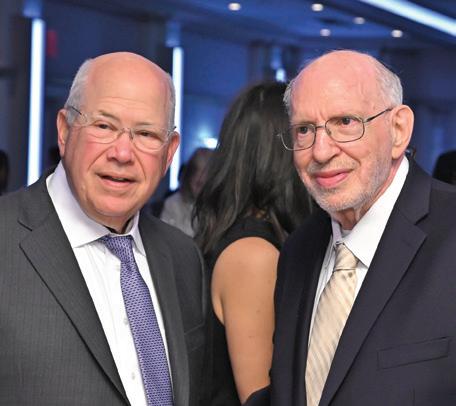
Peter W. Hughes, M.D. ’72
Patrick M. Hutton, M.D. ’74
Parvin Modaber Jacobs, M.D. ’55
Edward I. Jacobson, M.D. ’75
Gregory T. Jarrin, M.D. ’89
Jean A. Krag Trust
Vanessa L. Jeffers, M.D. ’89
Susan M. Jensen, M.D. ’77
John M. Jessup, M.D. ’72
Meena Jhanwar-Uniyal, Ph.D.
John Franklin Donaldson
Erica C. Jones, M.D. ’92
Joshua M. Junge, M.D. ’18
Samuel D. Kahnowitz, M.D. ’76
Elizabeth M. Peters-Kaiser, M.D. ’91 and Richard C. Kaiser, M.D. ’91
Ronald Kanner, M.D.
Emily R. Kaplan, D.P.H. ’21
Jeffrey M. Kaplan, M.D. ’70
Mr. Sean Kass
Mrs. Doris Katz
Ms. Susan R. Katz
Stephen Z. Kaufman, M.D. ’65
Ashutosh Kaul, M.D.
Mohammed-Abdul Khan, M.D. ’00
Kathleen M. Kicsak-Baumgartner, M.D. ’91
Susan A. Klein, M.D. ’83
Richard S. Kornbluth, M.D. ’75, Ph.D.
Jean A. Krag, M.D. ’54
Jonathan J. Kramer, M.D. ’83
Howard R. Krauss, M.D. ’77
Jo R. Kremer, M.D. ’73
Christopher J. Kruger, M.D. ’86
Jeffrey M. Krupen, M.D. ’82
Kenneth A. Krutt, M.D. ’84
Jonathan S. Kusnitz, M.D. ’84
Young-Ju Kwon, M.D. ’92
Ignazio G. Lachina, M.D.
Laiken Associates, Inc.
Mr. Rob Lancia
Charles F. Lanzieri, M.D. ’78
Jeffrey M. Laskoff, M.D. ’68
Linda F. Lazar, M.D. and
Rande H. Lazar, M.D.
Sheryl L. Leff, M.D. ’85
Richard S. Lefleur, M.D. ’66
Roy H. Leiboff, M.D. ’75
Solomon L. Lerer, M.D. ’71
Mark Levey, M.D. ’62
Elliot M. Levine, M.D. ’91
Peter D. Levit, M.D. ’76
Lorraine J. Kuhn, Ph.D. ’84 and I. M. Levy, M.D. ’76
David C. Lewandowski, M.D. ’15
Rachel E. Lewis, M.D. ’07
Ms. Zhaohui Li, M.S. ’02
Harold M. Libatter, M.D. ’80
Nancy T. Lin, M.D. ’04
Efrat Z. Lobel-Katz, M.D. ’96
Milton L. Lorig, M.D. ’77
Ellen Loughran, Ph.D.
Thomas Lu, M.D. ’96
Waldo J. Luciano M.D.
Mr. Robert Madden
Andrea G. Maitlin-Katz, M.D. ’88
Wilfredo Maldonado
Faye Maloney, M.D.
Mrs. Lynne Maidman Manning
Stephen H. Marcus, M.D. ’67
David S. Markenson, M.D.
Clifford L. Marshall, M.D. ’77
Lawrence R. Marwill, M.D. ’63
Jeffrey S. Mason, M.D. ’75
Harvey G. Masor, M.D. ’65
Monica McHenry, Ph.D., CCC-SLP
Rakesh K. Mehta, M.D.
Barry A. Meisel, M.D. ’70
Amy J. Meltzer, M.D. ’81
Miriam A. Menzel, M.D. ’85
Harold Mermelstein, M.D. ’75
Keith P. Meslin, M.D. ’99
Samuel I. Miles, M.D. ’74
Mr. Thomas Modero
James P. Mooney, M.D. ’56
Steven M. Moore, M.D. ’99
Mr. Christopher Moroney
Muriel A. Gold Morris, M.D. ’66
Edward N. Moss, M.D. ’76
Michelle A. Multz, M.D. ’87
Mr. and Mrs. Mitchell A. Mund
Gary L. Munn, M.D. ’88
James J. Murdocco, M.D. ’65
Padmini Murthy, M.D., M.P.H., M.S.
Adelaide G. Nardone, M.D. ’83
Ms. Joanne M. Neff
Mark A. Newell, M.D.
The Samuel Newman Charitable Foundation
Mrs. Jane Newman
Lysa N. Nguyen, M.D. ’01
Mr. Eduardo Nievas
Mr. John Nonna
Jack D. Norman, M.D. ’63
Mrs. Michelle Novotny
Myrna K. Keller Nussbaum, M.D. ’82
Genevieve N. Nwigwe, M.D.
Yetunde Olowe M.D.
Carlos L. Omenaca, M.D.
Hector J. Ortiz, M.D. ’82
Mr. and Mrs. Robert P. Osler
Otolaryngology Consultants of Memphis
Kerri L. Palamara, M.D. ’06
Vincent S. Panella, M.D. ’82
David R. Paradis, M.D. ’96
Janis A. Pastena, M.D., M.P.H. ’09
Mr. and Mrs. Theodore Pavlovitch
David R. Payne, M.D.
Edwin J. Pear, M.D. ’53
Performance Consultants, LLC
Fern L. Perlman, M.D. ’75
Nancy Castellucci Peters, M.D. ’93
Richard E. Petrucci, M.D. ’84
Antonio Petruzzo, M.D. ’92
Lee J. Phillips, M.D. ’85
Evan B. Pockriss, M.D. ’92
Robert S. Port, M.D. ’77
Bernard J. Powers, M.D. ’76
Patricia M. Raciti, M.D. ’11
Joseph Ramieri, M.D. ’69
Alfred B. Randall, M.D. ’70
Susan H. Read, M.D. ’15
Harvey A. Reback, M.D. ’61
Lesley Rechter, M.D. ’76
Harold Reikes, M.D. ’57
Mr. Tom Reilly
Charles R. Reina, M.D. ’74
Retina Group of NY
Beverly L. Richman, M.D. ’64
Elizabeth M. Riley, M.D. ’06
Robert M. Sherman MD PA
Merle S. Robinson, M.D.
Mr. Julio A. Rodriguez-Rentas, M.A.
Reuben D. Rohn, M.D. ’71
Nancy Roistacher, M.D. ’75
Ms. Barbara M. Rolle, M.S. ’91
Diane P. Romsaitong, M.D. ’95 and Panus Romsaitong, M.D. ’94
Marcy L. Rosen, M.D. ’08

Stuart A. Rosenthal, M.D. ’62
Jason E. Roth, M.D. ’98
Malcolm Z. Roth, M.D. ’82
Ronald R. Roth, M.D. ’73
Stephen N. Rous, M.D. ’56
Stephen L. Rubin, M.D. ’70
Richard G. Ryan, M.D. ’77
William Rymer, M.D. ’72
Tabassum Saba, M.D., M.S. ’94
Alan S. Sacerdote, M.D. ’74
Nicholas G. Sakellariou, M.D. ’94
Sanford Medical Corporation
Michael A. Sanford, M.D. ’94
Mr. Brian J. Savarese
Umer Sayeed Sayeed-Shah, M.D.
Meri Schachter, M.D. ’69
Neil R. Scheier, M.D. ’85
Mr. Gary Schneider
Janet A. Schneller, M.D. ’79
Michael B. Schoenwald, M.D. ’69
Melvin L. Schulman, M.D. ’65
Richard D. Schultz, M.D. ’88
David Schwalb, M.D. ’84
Ms. Joyce Seebrooks
William J. Semel, M.D. ’63
Denise B. Sepe, M.D. ’83 and Carl J. Koenigsmann, M.D. ’84
Michael A. Sergi, M.D. ’02
Russell A. Settipane, M.D. ’84
Christina T. Wong Sheridan, M.D. ’00
Robert M. Sherman, M.D. ’68
Mr. and Mrs. James A. Siano
Jeff S. Silber, M.D. ’95
Jeffrey J. Silbiger, M.D. ’81
Edward P. Sirois, M.D. ’59
Jennifer N. Sivitz, M.D. ’02
Victor S. Sloan, M.D. ’89 and Sandra Gong
Smithown Primary Medical Care, PC
Brian K. Solow, M.D. ’82
Mrs. Victoria Sommers
Mrs. Tamar R. Stone
Edward T. Swibinski, M.D. ’75
Ms. Lois Swisher
Lindsay S. Tan, M.D. ’82
Catherine M. Tegtmeier, M.P.H. ’10
Robert P. Thiel, M.D. ’84
Paul C. Thur, M.D. ’99
Keith S. Tobin, M.D. ’85
Col. Robert Francis Todaro, M.D., M.P.H. ’80
Tom Carmichael Charitable Fund
Mark Tomback, M.D. ’78
Judith Fiedler Topilow, M.D. ’67 and Arthur A. Topilow, M.D. ’67
James P. Tracey, M.D. ’89
John S. Train, M.D. ’67
Jonathan J. Trambert, M.D. ’77
Jeffrey S. Trilling, M.D. ’73
Alfred J. Trufelli Jr., M.D. ’77
Oya Tugal, M.D.
Ms. Rachana Tyagi
Joseph A. Tyburczy Jr., M.D. ’73
John N. Van Dam, M.D. ’72
Alberto F. Vera M.D.
Jack H. Vitenson, M.D. ’65
Adrianna Vlachos, M.D. ’86
Joseph F. Voli, M.D. ’92
Col. James W. Voskovitch, M.D. ’59
Lynne Voutsinas, M.D. ’83
Xing J. Wang, M.D.
Yan Wang, M.D.
Mr. and Mrs. Louis J. Wassong
Watchung Pediatrics
Charles L. Weinberg, M.D. ’65
Susan J. Freeman, M.D. ’79 and Marvin J. Weingarten, M.D. ’79
Princess Wells, D.P.T. ’10
Ms. Ellen Wengen
Graham F. Whitfield, M.D. ’76, Ph.D.
Aimi Y. Will, M.D. ’98
Gregory T. Williams, M.D. ’86
Mr. George Wimpfheimer
Mrs. Greta Wimpfheimer
David C. Wolf, M.D.
Sharon M. Wollaston, M.D. ’96 and Sean J. Wollaston, M.D. ’96
Yakov Consulting, LLC
Yan Wang Medical, P.C.
YJK Anesthesia, LLC
Hyun J. Yoo, M.D.
Ms. Brittany L. Young, M.P.H. ’15
Mr. Jason Yuen
Peter T. Zacharia, M.D. ’88
Shelley A. Zara, M.D. ’73 and Harvey D. Zara, M.D. ’73
Robert W. Zavoski, M.D. ’82
Robert M. Zbeda, M.D. ’15
Robert C. Zeller, M.D. ’71
Michael Shaochun Zhang, M.D., M.S. ’00
Leonard A. Zimmerman, M.D. ’69
Robert C. Zoller, M.D. ’77
+ Deceased


With a proud history of humanism and inclusivity, NYMC has been educating exceptional health care leaders for more than 160 years. Your contributions allow us to provide scholarships for our extraordinary students, recruit and retain the best faculty, conduct cutting-edge research, invest in technology and maintain state-of-the-art instructional and learning facilities. We encourage you to explore nymc.edu/give for more information.
Areas where you can make a difference:
• Annual Fund
• Contribute to an existing student scholarship, research, or academic fund
• Establish an endowment fund
• Make a planned gift
• Participate in the annual Founder’s Dinner
• Host a fundraising/ cultivation event in your area
• Days of Giving
• Reunion Weekend
• Medical Kit Initiative Support an area that inspires you. Contact the Office of Development and Alumni Relations at development@nymc.edu or call (914) 594-2720.
The Legacy Society of New York Medical College recognizes donors who have made provisions for the College in their wills or through other planned gifts, as well as those donors whose estate has made a gift to the College.
These members have named New York Medical College as a beneficiary in their estate plans/wills as of December 1, 2023:
Anonymous – 5
Michael S. Alexander, M.D. ’78
Ralph Almeleh, M.D. ’76
Michael Auerbach, M.D. ’75
Doris Bate, M.D. ’50
Augusta H. Belmonte, M.D.
Barbara Bitsko
Paul H. Brenner, M.D. ’61
Phillip Capozzi Jr., M.D. ’96
James E. Carter, M.D. ’55
Neil T. Choplin, M.D. ’76
Mrs. Delores DelBello
Emalie and John D. Feerick
Dr. and Mrs. Denis J. Frank ’61
Mark J. Friedman, M.D. ’71
Howard D. Harrison, M.D. ’61
Selma Henig
Steven P. Kahn, M.D. ’67
Maureen Kennedy, Dr.P.H. ’11, M.S. ’03
Mrs. Mary M. Kogut
Bradley S. and Ruth Friedman Kuhn
Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64
Annette E. Kussmaul, M.D. ’93
Mrs. Diane L. Levere
Carl M. Marchetti, M.D. ’60
Mr. Joel Margolis
Joseph P. Merlino, M.D. ’78, M.P.A.
Mark S. Noveck, M.D. ’80
Lee J. Phillips, M.D. ’85
Harvey A. Reback, M.D. ’61
Kenneth M. Rose, M.D. ’88
Neil R. Scheier, M.D. ’85
John H. Seward, M.D. ’61
Neil S. Silber, M.D. ’75
Victor S. Sloan, M.D. ’89
Theresa A. Smith, M.D. ’56
John T. Stinson, M.D. ’75
Patricia C. Villamena, M.D. ’77
Anna M. Ward, M.D. ’85
Steven Weissberg, M.D. ’66
Since 1987, the College has received more than $24.6 million in contributions from the estates of these individuals:
Alma Allen
Anne T. Barbieri
Herbert and Sylvia Berger
Marcelle B. Bernard, M.D. ’44 and Edmund D. Marinucci, M.D. ’44
Barbara Bess
Charles E. Birch, M.D. 1891
Alice H. Burgoyne
Michael Caruso
Nathan W. Chaikin, M.D. and Mrs. Frances Chaikin
Herrlich Ciatto
Mary E. Clarke
William P. Coats, M.D. ’53
Wendy E. Cohen, M.D. ’70
Brian J Collins, M.D. ’61
Sidney L. Cramer, M.D. ’41
Mabelle A. Cremer, M.D. ’53 and Martin E. Silverstein, M.D. ’48
Lewis A. Dalburg Jr., M.D. ’58
R. Margarita De Santis, M.D. ’59
Margot Ammann Durrer, M.D. ’49
Earl H. Eaton Jr., M.D. ’44
Walter G. Elliott, M.D. ’51 and Mrs. Shirley Elliott
Eva Feld
Miguel Figueroa, M.D. ’48 and Mrs. Lillian Figueroa
Walter E. Fleischmann
Robert W. Fredrickson, M.D. ’51
COL Saul Fromkes
Francis J. Geary, M.D. ’64
Arthur Ginsburg, M.D. ’58
Gerhard J. Haas, Ph.D.
Seymour Halpern, M.D.
Edith Har-Esh, M.D.
Adriel and Evelyn H. Harris
Catherine N. Hinterbuchner, M.D.
Arno R. Hohn, M.D. ’56
Dora May Holmes
Constance Ives Foster
Gerald H. Kass, M.D. ’51
Paul Kay, M.D. ’44
William J. Kelley, M.D.
Joseph B. Kiel, M.D. ’31
Janice Kiss
Solomon D. Klotz, M.D. ’37 and Mrs. Harriett Klotz
Henry V. Kogut, M.D. ’43
Salvatore LaCorte, M.D. ’30
Guy Lepore
Anna Lowin
Maurice L. Malins
David K. Marcus, M.D. ’32
Charles D. McCullough, M.D. ’58
Frederick R. Meeks, M.D. 1907
Matthew S. Mickiewicz, M.D. ’41 and Mrs. Helen Mickiewicz
Laura G. Morgan, M.D. ’49

George R. Nagamatsu, M.D. ’34 and Kazuko Nagamatsu
Ellen J. Nolde
James F. X. O'Rourke, M.D.
Richard A. Perry, M.D. ’60
Eileen H. Pike, Ph.D.
Andrew S. Ranier, M.D. ’46
John Louis Rie Jr.
Mrs. Elaine Rosenberg
William S. Rosenthal, M.D.
Harvey Rosner, M.D. ’63
Mark S. Rothenberg, M.D. ’30
William D. Ryan, M.D. ’53 and Mrs. Kathryn X. Ryan
Ethel Esther Sandler
Tamiko Sato, M.D.
Ruth Saunders
Elaine L. Schulman, M.D. ’65
Louis N. Scotti, M.D. ’58
Louise O. Smith
Roy Gene Smith, M.D. ’61
Sander V. Smith, M.D. ’35 and Mrs. Helen W. Smith
Vincent E. Smith, M.D. ’61
Sidney Stahler, M.D.
Samuel Steinholtz, M.D. ’28
Dorothy S. Stengel
Theodore R. Struhl, M.D. ’42 and Mrs. Ruth Struhl
Hiroshi J. Tazaki, M.D., Ph.D.
Ciro S. Tarta, M.D. ’43
Roscoe W. Teahan, M.D. 1917
Joseph F. Tedesco, M.D. ’37 and Mrs. Vera L. Tedesco
Solomon Till, M.D. ’25 and Mrs. Elizabeth Till
Ruth E. Trager
Gertrude Tromp
Roy C. Upham, M.D. 1901 and Sarah Upham
William F. Westlin III, Ph.D. ’89, M.S. ’87
S. R. Wiener
Robert M. Wittenberg, M.D. 1919
Percy C. Zanger, M.D. ’49
Morris Zeichner, M.D. ’33
In memory of Harvey W. Aiges, M.D. ’71
Eric H. Schultheis, M.D. ’88
In honor of Francis L. Belloni, Ph.D.
Mr. Lee M. Allen II
In memory of Neil Borg, M.D.
Lisa Borg, M.D. ’80
In honor of Mr. Derek Borsody
Jaleh Z. Eslami-Borsody, M.D. ’94
In memory of Margaret B. and Giuseppe T. Cervia
Joseph S. Cervia, M.D. ’84
In honor of Mr. and Mrs. Thumnoon
Charuworn
Burawit B. Charuworn, M.D. ’99
In honor of Penelope and Scarlett Chew
Qwie T. Chew, M.D. ’65
In memory of Archie Cohn, M.D. ’27
Kenneth Cohn, M.D. ’68
In memory of Paul V. Conescu, M.D. ’69
Mrs. Lizabeth Conescu
In memory of Mr. Joseph Corey
Stephen L. Rubin, M.D. ’70
In celebration of Gregory Cowan, M.D.
Kay L. Cowan, M.D. ’87
In celebration of Mr. James DeBlasi
Henry C. DeBlasi, M.D. ’89
In memory of J.C. Deng, M.D.
Shiu-Lin Tsai, M.D. ’91
In memory of Joseph F. Dursi, M.D. ’59
Ms. Margaret Astrologo
In memory of Herbert Elias, M.D.
Carl B. Lundborg, M.D. ’67
In honor of Mr. Robert Fogel
Ms. Jill Zucker

In memory of Martin J. Frank, M.D. ’70
Mrs. Robert Crootof and Robert E. Crootof, M.D. ’70
In memory of John U. Gardner, M.D. ’53
Mr. Tom U. Gardner
In memory of Donald H. Gemson, M.D. ’78
Anita Grover, M.D. ’78
In memory of Mina A. Gillers, M.D. ’73
Bruce J. Gillers, M.D. ’73
In honor of William Glatt, M.D. ’64 retirement
Daniel J. Glatt, M.D., M.P.H. ’92
In memory of Mr. Allan Goldberg
David F. Kosnick, M.D. ’73
In memory of Robert Gonshorek, M.D. ’61
Gary R. Donshik, M.D. ’66
Mrs. Rita Gonshorek
Edward L. Snyder, M.D. ’73
In memory of Mrs. Beatrice and Mr. Nathan Gordon
Steven Samuels, M.D. ’74
In memory of Eugene M. Grossman, M.D. V. Rachel Phillips, M.D. ’79
In memory of Rainer V. Guggenheim, M.D. ’58
Mrs. Janet Guggenheim
In memory of Mr. Jimmy Gurran
Ms. Bonnie Gurran-Heindl
In memory of Camille (Joan) Harriott Sr.
Ms. Camille Harriott
In memory of Mary Ellen Hawkins McAteer, M.D. ’75
Rebecca A. McAteer Martin, M.D. ’08
In memory of Bruce H. Heckman, M.D. ’67, M.P.H.
Judith Fiedler Topilow, M.D. ’67 and Arthur A. Topilow, M.D. ’67
In memory of Thomas H. Hintze, Ph.D. ’80, M.S. ’78
Margaret A. Reilly, Ph.D. ’81, M.S. ’78
In memory of Susan Hochman
Sharon M. Wollaston, M.D. ’96 and Sean J. Wollaston, M.D. ’96
In memory of John C. Hordines, M.D. ’93
Mrs. Beth Hordines
In memory of Kenneth B. Juechter, M.D. ’68
Adelaidegray LLC
American Online Giving Foundation
Mr. Steven Bodine
Dr. and Mrs. Joseph Canterino, D.D.S.
Steve H. Chang, M.D. ’02
Ms. Juanita Costa
Daniel Elefant, M.D. ’17
Stephan M. Greenberg, M.D. ’66
Mr. Darren Hugo
Kelly A. Hutcheson, M.D.
Ms. Andrea B. Jeffries
Mrs. Nancy J. Jessen
Mr. Adam Juechter
Mrs. Kay Juechter
Ms. Hattie W. Law
Levinsky Family Fund
James F. McGroarty, M.D. ’68
Mr. Gregory C. Miller
Morgan Stanley
Mr. Christopher Moroney
P. Mesches and M. Crescenzo Living Trust
Mr. and Mrs. Charles Phipps
Ms. Joyce Seebrooks
Peter T. Zacharia, M.D. ’88
In memory of Stephan L. Kamholz, M.D. ’72
Stewart Krug, M.D. ’72
In memory of Mayer S. Kaplan, M.D. ’33
Jeffrey M. Kaplan, M.D. ’70
In memory of Howard J. Kline, M.D. ’58, FACC
James W. Justice, M.D. ’58
Ellen Sawamura, Ph.D.
In celebration of Spencer and Hayley
Kramer's marriage
Mitchell S. Kramer, M.D. ’85
In honor of Steven L. Lansman, M.D., Ph.D.
Neil Schluger, M.D.
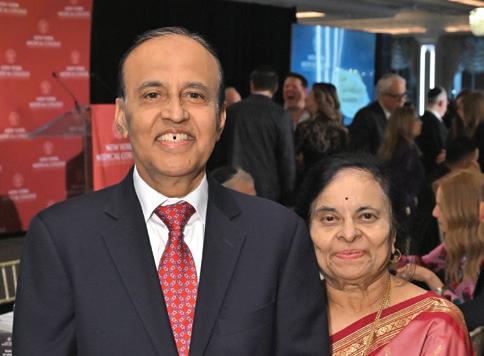
In memory of Shailer Lawton, M.D.
John Franklin Donaldson
In memory of Ms. Florence Lewis
Walter M. Lewis, M.D. ’91 and Christel Bauer, M.D.
In memory of Mr. Paul H. Lewis
Ellen R. Lewis
In celebration of Joshua Li
Baoqing Li, M.D. ’05
In celebration of Joan Liman's (M.D. ’83, M.PH. ’93) zest for life
Ilona W. Figura, M.D. ’83
In memory of John J. Lynch, M.D. ’58
Ellen Loughran, Ph.D.
In memory of Mr. and Mrs. Malumed
Jeffrey Malumed, M.D. ’83

In memory of John M. Marino, M.D. ’59
Gregory H. Mahairas, M.D. ’59
In honor of Jack McClung and Mary Vukman
Martin A. Schwartz, M.D. ’75
In celebration of Mr. Ruben Medina
Eisner Amper Group
Mr. Tom Reilly
In memory of James T. Miglietta, M.D. ’81
Kenneth D. Kushner, M.D. ’81
In memory of Mary Ann Latona Nadler
Jerry L. Nadler, M.D., MACP, FAHA, FACE
In memory of Robert W. Niehaus, M.D. ’50
Ms. Lois Swisher
In celebration of Mr. Yoel Norograd’s graduation in 2023
James N. Shearer, M.D. ’75

In celebration of Brian R. Osler, M.D. ’18
Mr. and Mrs. Robert P. Osler
In honor of Mr. David Pasion Sr.
Sandra L. Sacks, D.D.S., M.D. ’97 and Harry G. Sacks, D.D.S., J.D.
In memory of Albert Pineda, M.D. ’63
Barbara Pineda, M.D.
In memory of Louis G. Raff, M.D. ’24
Ira L. Raff, M.D. ’64
In memory of Mr. Vincent and Mrs. Mildred Reina
Charles R. Reina, M.D. ’74
In memory of Frank Richard Romano Sr., M.D. ’39
Patricia M. Raciti, M.D. ’11
In celebration of Mr. Jaime Roth
Ronald R. Roth, M.D. ’73
In memory of Samuel H. Rubin, M.D.
Adam D. Rubin, M.D. ’00
In honor of Bijan Safai, M.D., D.Sc.
Kathleen M. Rossy, M.D. ’09
In honor of John A. Savino, M.D.
Umer Sayeed Sayeed-Shah M.D. ’96
In memory of Seymour Schlussel, M.D. ’51
Jack D. Norman, M.D. ’63
In memory of Eugene Schwalb, M.D.
David Schwalb, M.D. ’84
In memory of Robert A. Solow, M.D. ’48
Brian K. Solow, M.D. ’82
In honor of Mr. Anthony M. Sozzo
Menasche Krupka, M.D. ’21
In memory of Mrs. Jeanne Stavola and Joseph J. Stavola, M.D. ’87
Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
In honor of Maggie Steele-Tzakos
Ms. Kimberly Tzakos
In memory of Mr. James Stone
Mrs. Tamar R. Stone
In memory of N. Noel Testa, M.D. ’66
Howard D. Cantwell, M.D. ’65
Nicholas Testa, M.D. ’01
In memory of Seymour Tobin, M.D. ’52
Keith S. Tobin, M.D. ’85
In honor of Marco J. Tomassi, M.D. ’03 and Michelle P. Tomassi, M.D. ’05
Mrs. Patricia M. Tomassi
In memory of John L. Vigorita, M.D. ’44
Vincent J. Vigorita, M.D. ’76
In memory of Dr. Felix and Hannah Wassermann
Michael S. Alexander, M.D. ’78
In memory of Paul K. Woolf, M.D.
Christina T. Wong Sheridan, M.D. ’00
In memory of Wilson Young, M.D. ’07, Ph.D. ’07, M.S. ’99
American Online Giving Foundation
Mr. Raymond Cajulis
Ms. Renee Chan
Ms. Meghan Fashjian
Ms. May T. Flowers
Ms. Teri Frangie
Miao Jiang, Ph.D. ’04
Jae H. Jung, M.D. ’03
Ms. Taryn Looney
Sundry Donors
Mrs. Amy Vatanapradt
Ms. Ellen Wengen
Mr. Norman Young
Mr. Jason Yuen
In honor of Joseph and Gila Zelazny
Daniel Zelazny, M.D.

We have made every effort possible to provide a full and accurate list of donors to NYMC from July 1, 2022 through June 30, 2023. If we have omitted or improperly listed your name, please accept our apologies. If you detect an error, please contact our Office of Development and Alumni Relations at (914) 594-2720 or email us at development@nymc.edu, so we may correct our records.




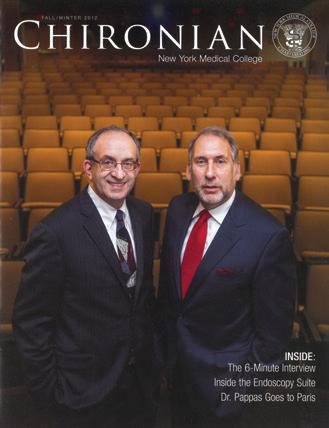

The first issue, published in October of 1884, was edited by students and alumni, and blended a mixture of College news, clinical case reports, and other medical news of interest, as well as original clinical and research articles by faculty and alumni. Its founding editor was Eugene Hoffman Porter, M.D., Class of 1885, (1856 – 1929) who was valedictorian of his class
and went on to serve as the commissioner of the New York State Department of Health from 1905 to 1914. Over the decades, Chironian has metamorphosed, but through its many iterations, it has remained steadfast in serving as a vibrant narrative and documenting the happenings at NYMC, cutting-edge research, faculty profiles, student accomplishments, and alumni news.
