

CHIRONIAN
CHIRONIAN
Vice President of Communications and Strategic Initiatives
Jennifer Riekert, M.B.A.
Editor Assistant Editor
Lori Perrault Kiara Thomas, M.A.
Writers
Lenore Carpinelli
Cara Gileau
Rhea Hirshman
Andrea Kahn
Contributor
Barbara Moroch
Lori Perrault
Melissa F. Pheterson
Kristin Baird Rattini
Kiara Thomas, M.A.
Nicholas Webb, M.S.I.S.
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer
Editorial Board
Salomon Amar, D.D.S., Ph.D.
Amy Ansehl, R.N., D.N.P., FNP-BC Bernadette Bauer
Lenore Carpinelli
Tetyana Cheairs, M.D., M.S.P.H.
Mill Etienne, M.D. ’02, M.P.H.
Vikas Grover, Ph.D., CCC-SLP
Design Wayne Printing, Inc.
Photography
Edmund F. LaGamma, M.D. ’76
Christopher S. Leonard, Ph.D.
Dana Mordue, Ph.D.
Michelle Novotny, M.A.
Michal L. Schwartzman, Ph.D.
Anitha Srinivasan, M.D., M.P.H.
Dmitry Kalinin, DIA International Group, Inc.
Christopher Pope
William Taufic Photography
ADMINISTRATION
Alan Kadish, M.D., President
John Vecchiolla Photography
Joe Vericker, Photo Bureau
Edward C. Halperin, M.D., M.A., Chancellor and Chief Executive Officer
Robert W. Amler, M.D., M.B.A., Dean, School of Health Sciences and Practice, Vice President for Government Affairs
Marina K. Holz, Ph.D., M.P.H. ’23, Dr.P.H. ’24, Dean, Graduate School of Biomedical Sciences
Neil W. Schluger, M.D., Dean, School of Medicine
Office of Public Relations
Jennifer Riekert, M.B.A., Vice President of Communications and Strategic Initiatives
Lenore Carpinelli, Director of Strategic Communications, School of Medicine
Katie Coates, Director of Creative Communications and Production
Cara Gileau, Communications Specialist
Lori Perrault, Director of Print and Digital Publications
Faye Seltzer, Administrator
Kiara Thomas, M.A., Communications Writer and Content Creator
Alina Zhurbenko, M.A., Communications Coordinator
Please direct all inquiries to:
New York Medical College/Chironian, 40 Sunshine Cottage Road, Valhalla, NY 10595. We authorize the use of any material with attribution to New York Medical College. Chironian is published annually by the Office of Public Relations. We welcome reader feedback.
Contact us at (914) 594-4536 or at chironian@nymc.edu.
NEW YORK MEDICAL COLLEGE AFFILIATIONS
Major Clinical Affiliated Sites
Westchester Medical Center Health Network (WMCHealth)
Westchester Medical Center
Maria Fareri Children’s Hospital
Good Samaritan Hospital
NYC Health + Hospitals/Metropolitan
Clinical Affiliated Sites
Beckley VA Medical Center
Calvary Hospital
Greenwich Hospital
Hoboken University Medical Center
James J. Peters VA Medical Center
Landmark Medical Center
Lenox Hill Hospital
Mount Sinai Medical Center, Miami Beach
Northern Westchester Hospital
NYC Health + Hospitals/Lincoln
Ambulatory Care Programs
Care for the Homeless
ODA Primary Health Care Network
Open Door Family Medical Centers
Optum Refuah Health Center
Health Alliance Hospital MidHudson Regional Hospital



Phelps Hospital Northwell Health
Richmond University Medical Center
Rome Memorial Hospital
Saint Clare’s Hospital
Saint Joseph’s Medical Center
Saint Michael’s Medical Center
St. Mary’s General Hospital
Terence Cardinal Cooke Health Care Center
VA Hudson Valley Health Care System
Yuma Regional Medical Center
Summit Health Union Community Health Westchester Institute for Human Development
CONNECT WITH US: www.nymc.edu facebook.com/nymedcollege and facebook.com/nymcalumni



Twitter @nymedcollege
LinkedIn @new-york-medical-college
Instagram @nymedcollege

Message from the Chancellor
The First Responsibility of a Schoolteacher

Many university campuses in the United States, over the past two years, have been roiled by political demonstrations, tent cities, posters, and graffiti. This behavior has spilled over into commencement exercises, which have been disrupted by shouting, chanting, signs, and walkouts. During this period, however, the campus of New York Medical College (NYMC) has been orderly, and our commencement exercises have been dignified and professional. I want to share some thoughts with the alumni and friends of the College regarding how NYMC maintains a safe, professional, respectful, and collegial campus atmosphere.
My mother was an eighth-grade English teacher. She always taught me that “many people say that the first responsibility of a teacher is to understand that if their student hasn’t learned, then the teacher hasn’t taught. That is incorrect. The first responsibility of a teacher is to establish and maintain a safe learning environment. Students must feel physically safe. Classrooms and school buildings must be in good repair. Students must feel emotionally safe. They must not be distracted from their studies by anxiety. Only if these conditions of physical and emotional safety prevail can education take place.”
I believe that my responsibility as chancellor and chief executive officer of NYMC is to be a good schoolteacher and, foremost, to maintain a safe learning environment for our students. I recognize that some people think that the First Amendment to the U.S Constitution guarantees the right of citizens to free speech and that this right means that anyone can say whatever they want, wherever they want. I think that such a point-of-view is neither correct law nor sound academic management.
I can play “cops and robbers” with my grandchildren in the living room. My free speech rights include my right to say, “This is a stick-up,” during the game. If, however, I say, “This is a stick-up,” to the bank teller at my local bank, my free speech rights are subordinate to the bank teller’s and the bank’s rights not to be placed in fear of their life and property. My behavior in the bank would be illegal. I may think I have the right to free speech to plagiarize someone else’s work in my writing, but if I do that in a term paper for a class at NYMC, I am going to suffer the consequences. If a medical student or house officer writes or says that they are going to intentionally mistreat a patient because of their race, religion, gender identity, or political views, they are going to promptly find themselves standing before a professionalism committee and licensure authorities to explain themselves — and claiming a “right to free speech” is not going to gain any sympathy.
On NYMC’s campus we have written policies on unprofessional behavior on social media. We have clear directives for professional behavior in the classrooms, the laboratories, on the wards, and at commencement. This has led me to say, more than once in the last two years, “The First Amendment of the Constitution and the policies of this College both are pertinent to the governance of behavior on this campus, and both will be enforced.”
I believe that the reason NYMC’s campus has been orderly and calm, in comparison to many other campuses, is that we admit and educate mature students who understand that their priority is to serve the sick, promote the common good, and generate new knowledge through research. I believe that the fact that we are a College under religious auspices contributes to a positive and constructive campus environment. I also think that our articulation of our policies has helped. Ultimately, I assure the alumni and friends of this College that the administration is committed to a welcoming campus for those who came to this College to engage in the generation, conservation, and dissemination of knowledge about the causes, prevention, and treatment of human disease and disability. We believe in upholding standards of professional behavior which are conducive to achieving the goal of a safe learning environment and meeting that goal was what my mother taught me was my first priority.

Edward C. Halperin, m.d., m.a. chancellor and chief executive officer
NEWS Briefs
NYMC Administers First Novel Inhaled mRNA Therapy for Cystic Fibrosis in the U.S.
In December 2024, New York Medical College (NYMC), in collaboration with ReCode Therapeutics, a clinical-stage genetic medicines company, administered the first U.S. dose of RCT2100 — a novel investigational inhaled messenger RNA (mRNA) therapy for people with cystic fibrosis (CF). The clinical trial, which will assess the safety and tolerability of RCT2100, will provide new hope for people who do not respond to existing cystic fibrosis transmembrane conductance regulator (CFTR) modulator treatments. While there are currently 13 clinical trial sites for RCT2100 throughout the country, this was the first dose to be successfully administered in the U.S.
“This milestone represents a pivotal moment for the CF community and reflects our ongoing commitment to advancing care for patients with CF,” said Allen J. Dozor, M.D., professor of pediatrics and chief of the Division of Pulmonology, Allergy, and Sleep Medicine at NYMC and president of Boston Children’s Health Physicians, who personally administered the dose. “We are proud to play a leading role in this important study and are hopeful that RCT2100 will provide a meaningful new option for those living with this challenging disease.”
Additional doses followed by 24-hour observation periods are a crucial part of the clinical trial protocol, carefully designed to monitor how the therapy interacts with the body. Once the second dose was well-tolerated, the patient received repeated doses every two to three days for a few weeks, with the hopes that there continues to be a positive response to the therapy.

“Living with CF has been a long and interesting journey,” said Nicholas Brandner, the clinical trial patient. “I am grateful for my medical team in getting me the proper care and providing me with the opportunity to take part in trial medications like RCT-2100. My body took time to adjust, but I am hopeful that 2025 will bring success in advancements in gene therapy for CF. I can’t wait.”
CF is caused by mutations in the CFTR gene, which affects approximately 105,000 people worldwide. While CFTR modulators offer hope for 90 percent of the CF community, many patients still face barriers. Many will not be able to take the medication due to side effects, lack of response, or other reasons. About 10 percent of the CF community has genetic mutations that prevent them from benefiting from these therapeutics.
RCT2100 is an investigational inhaled therapy for CF based on mRNA. Unlike current treatments, which correct or enhance faulty CFTR proteins, RCT2100 is designed to deliver CFTR mRNA directly to lung cells, instructing them to produce new, fully functional CFTR proteins. This approach aims to address the underlying cause of CF, potentially improving proper protein function in the lungs rather than just managing symptoms.
In March 2025, the U.S. Food and Drug Administration granted Orphan Drug Designation for RCT2100 and the clinical trial is in the process of working with a second patient. ■

Liaison Committee on Medical Education Reaffirms NYMC Accreditation for Maximum Term of Eight Years
After a long and rigorous process, the Liaison Committee on Medical Education (LCME) reaffirmed the School of Medicine’s (SOM) accreditation for the maximum eight-year period through 2032.
The LCME is officially recognized by the U.S. Department of Education to accredit medical schools in the United States and Canada and has joint oversight by the Association of American Medical Colleges and the American Medical Association. For U.S. medical education programs, accreditation by the LCME establishes eligibility for selected federal grants and programs, eligibility of U.S. students in M.D.-granting schools to take the United States Medical Licensing Examination, and eligibility for residency programs accredited by the Accreditation Council for Graduate Medical Education.
The accreditation process included a thorough selfstudy of all functions of the SOM from admissions policies and practices to research resources and opportunities to ensure the SOM met the LCME’s specific 12 standards, as well as a visit to campus by an LCME Site Survey Team in April 2024, to meet with administrators, faculty, staff, and students about all aspects of the medical school program, resources, and facilities.
The team effort was led by Pamela Ludmer, M.D., M.M.E.L., dean for undergraduate medical education, who served as faculty lead for the SOM accreditation, with invaluable input from the members of the LCME Self-Study Task Force, EQUIP Team, Self-Study Executive Committee, and five working groups focused on educational program, educational resources, faculty affairs, governance, and medical students and comprised of faculty, students, and administrators.
“The teamwork, camaraderie, and collegiality that was demonstrated over the last two years by all those who worked diligently towards this LCME reaccreditation was truly admirable,” said Neil W. Schluger, M.D., dean of the SOM. “Throughout this process we have adopted and engaged in a culture of continuous quality improvement, and that will continue. We are committed to a process of review that strives to provide the highest quality education through the most effective means for our students.” ■
School of Medicine Expands Academic Affiliations
The New York Medical College (NYMC) School of Medicine (SOM) has expanded its academic affiliation footprint with two new affiliations: Mount Sinai Medical Center (MSMC) in Miami Beach, Florida, and Yuma Regional Medical Center (YRMC) in Yuma, Arizona. The partnerships further enhance NYMC’s extensive network of affiliated hospitals and clinical sites that encompasses more than 30 affiliates, now across seven states—New York, New Jersey, Connecticut, Rhode Island, West Virginia, Florida, and Arizona.
The affiliation agreement with MSMC establishes clerkship rotations for medical students in internal medicine, obstetrics and gynecology, psychiatry, and surgery, as well as electives in emergency medicine, anesthesiology, and urology. Named one of America’s 100 Best Hospitals™ by Healthgrades™ for 2024, MSMC operates across 13 locations, including three emergency centers, and is the largest private, independent, not-forprofit teaching hospital in Florida.
“We are excited to welcome MSMC to NYMC’s robust network of clinical affiliates. Mount Sinai is renowned for its exceptional patient care and the expertise of its physicians. I am confident that our students will greatly benefit from the
outstanding educational opportunities available to them there, which will significantly enhance their clinical skills,” said Neil W. Schluger, M.D., dean of the SOM.
“Educating the next generation of expert physicians for our community has been at the core of Mount Sinai’s mission for 75 years,” said Gino R. Santorio, president and chief executive officer of MSMC. “Our newest affiliation with NYMC enhances our ability to continue to attract top medical minds, fostering an environment where emerging doctors are mentored by expert faculty. This steadfast commitment to continuous learning fuels medical advancements, which results in enhanced quality care and better patient outcomes.”
The agreement with YRMC establishes clerkship rotations for medical students in internal medicine, pediatrics, family medicine, and surgery and electives in orthopedics, adult cardiology, and hematology/oncology. YRMC, a hospital boasting more than 400 beds spread across 28 care locations, offers a wide range of medical services to more than 600,000 patients annually in a predominantly rural area in southwestern Arizona.
“At NYMC, we are proud of the network of affiliates that offers our students an array

of outstanding educational opportunities to enhance their clinical skills,” said Dr. Schluger. “We look forward to a collaboration with the leadership and clinicians at Yuma Regional Medical Center that will be mutually beneficial for years to come.”
“This partnership sets forth a new direction in the advancement of rural medicine,” said Robert Trenschel, D.O., M.P.H., president and chief executive officer, of YRMC. “Yuma Regional Medical Center is located in the southwest corner of Arizona, bordering California to the west and Mexico to the south. Our unique geographic location serves as a pillar for diverse learning and a unique set of pathology. Our commitment to building a healthier tomorrow is modeled in the collaboration of our two organizations.” ■

Touro University Expands Footprint with Acquisition of New York
College of Podiatric Medicine
The New York College of Podiatric Medicine (NYCPM) is now officially part of Touro University (TU) and New York Medical College (NYMC). Founded in 1911, NYCPM was the nation’s first medical college devoted to educating and training doctors of podiatric medicine and combines outstanding classroom instruction with clinical training in one of the world’s largest foot care clinics.
Located in East Harlem, New York, NYCPM offers a four-year program consisting of two years of pre-clinical and two years of clinical sciences, as well as graduate medical education and continuing medical education. Twenty percent of practicing podiatrists in the country have graduated from NYCPM.
“As health care moves towards a team-based approach, podiatrists will become increasingly important. Touro health care educational systems and their clinical health care delivery systems will integrate NYCPM in a way that improves patient care and transforms the experience for students and faculty,” said Michael Trepal, D.P.M., FACFAS, dean and vice president of academic affairs at NYCPM and assistant professor of surgery at NYMC.
“Touro is known for its ability and willingness to innovate rapidly, and we are adept at finding the best educational techniques and solutions to meet the needs we identify. Some of the best job opportunities currently exist in the health care field, and our goal is to offer an array of choices and prime our students for success. Educating approximately 7,700 students annually in the health sciences, Touro is quickly becoming one of the largest health care educational systems in the U.S. Adding podiatric medicine to our existing network of medical and health science schools and programs will serve to augment and strengthen our academic offerings,” said Alan Kadish, M.D., president of TU and NYMC. ■


Touro College of Dental Medicine Breaks Ground on New Mexico’s First Undergraduate Dental Clinical Training Facility
Touro College of Dental Medicine
(TCDM) broke ground on a clinical facility in Albuquerque, New Mexico, on the campus of Lovelace Biomedical Research Institute, a member of Touro University, in September 2024. Touro Dental Health New Mexico is TCDM’s clinical training facility that will provide 200 TCDM students a new dental practice location.
“Touro University (TU) is committed to delivering quality education as well as integrity, inclusivity, and respect for all members of our new Touro community in New Mexico,” said Alan Kadish, M.D., president of TU and New York Medical College. “We provide diverse, innovative, and engaging course offerings that nurture personal growth and intellectual inquiry in superior academic programs.”
Students at TCDM spend their first two years in the classroom studying basic biological sciences, and the last two years seeing patients in the clinics. Moving forward, 100 students from each TCDM class of 200 will complete their classroom training on TCDM’s Valhalla campus before spending their final two years treating patients from the Albuquerque community in the new clinical facility.
“TCDM is thrilled to expand to New Mexico and create the first ultramodern, world-class dental clinical training facility in the state. Our mission is to improve oral health care and graduate outstanding dental professionals who deliver excellent health care service to diverse communities,” said Ronnie Myers, D.D.S., TCDM dean. “With the first pre-doctoral dental student clinical educational facility in New Mexico, we
will provide an opportunity to deliver much needed low-cost oral health care to under-resourced communities while at the same time expanding local access to New Mexico students interested in becoming dentists.”
New Mexico falls behind the nation in the average number of oral health care professionals available to serve its residents. Recent studies reveal that the number of dentists per 100,000 people in New Mexico is only 48.4, below the national average of 60.84.
“We anticipate that there will be a significant number of graduates who remain in New Mexico to pursue their dental careers filling this void, adding to our incentive to build the new facility and clinic in the land of enchantment,” said Dr. Myers.
New Mexico’s first pre-doctoral dental school clinical training facility will encompass more than 70,000 square feet of educational and clinical space and house more than 100 dental units, including units to provide specialty care in oral surgery, orthodontics, endodontics, and pediatric dentistry. The new facility will deliver necessary dental care to those in need, while also providing local access to New Mexico students interested in becoming dentists.
TCDM’s faculty of general dentists and highly skilled specialists including periodontists, prosthodontists, endodontists, orthodontists, oral surgeons, dental anesthesiologists, and radiologists enables the school to provide a full range of dental care under one roof, while providing students with hands-on exposure to and training in all dental disciplines. ■
NEWS Briefs
Joel Kupersmith, M.D. ’64, Presents Inaugural Endowed Lecture on Virtual Care and Health Ethics

Alumnus Joel Kupersmith, M.D. ’64, professor emeritus of medicine at Georgetown University Medical Center, returned to campus to deliver the inaugural Drs. Joel and Judith R.F. Kupersmith Endowed Lectureship in Health Policy and Ethics. He presented the lecture, “Virtual Care and the Future of Medicine,” exploring the evolution, uses, economics, outcomes, and ethical challenges of virtual care, telehealth, and remote patient monitoring, which have become integral to American medicine, particularly since the COVID-19 pandemic. A question-and-answer session hosted by Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, followed. The event was made possible by the generous endowment of Dr. Kupersmith and Judith Friedman Kupersmith, M.D. ’69. The lecture series aims to provide valuable insights into pressing topics in health ethics and policy. Dr. Kupersmith is former dean and vice president for clinical affairs at Texas Tech University Health Sciences Center and served as chief research and development officer in the Department of Veterans Affairs (VA), where he initiated the Million Veteran Program genomics mega-database, a Central Institutional Review Board, new clinical research methods, and improvements in the VA’s research infrastructure. ■
NYMC Receives Bequest for Long-term COVID-19 Research
NewYork Medical College (NYMC) is the beneficiary of a $150,000 donation bequeathed by Joel P. Margolis, OBM, who passed away on March 15, 2024, at the age of 79.
Mr. Margolis was an auditor for the New York State Legislative Commission of Expenditure Review prior to his retirement.
The donation is to support researchers with promising approaches to curing or alleviating long-term COVID-19 or similar viral illnesses. Long-term COVID refers to a range of health problems that persist or develop after an initial

COVID-19 infection with long-term symptoms. In some patients, the disease is debilitating. There is no single test to diagnose long-term COVID and it is a serious public health concern.
Mr. Margolis held a deep appreciation for both Touro University and NYMC. He was especially grateful for the medical referrals he received from Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, which he valued greatly. ■
NYMC.edu Gets a Makeover
The NYMC.edu website has a fresh, modern look and improved functionality to enhance the College’s online presence. The development of the new site was a monumental collaborative effort, spearheaded by the Office of Public Relations and the Touro University Department of Online Services. Together with the dedicated input from administration, faculty, students, and staff across all three schools, the new website creates a digital experience that truly reflects the spirit and excellence of New York Medical College (NYMC).
The redesigned website offers several key improvements including streamlined navigation for a simpler, more intuitive browsing experience and enhanced content with a particular focus on engaging prospective students and the general public. The fresh aesthetic aligns with NYMC’s branding while showcasing our integral role within the Touro University system. The new look is professional, modern, and a true reflection of our commitment to excellence. ■

The Clinical Skills and Simulation Center (CSSC) at New York Medical College (NYMC) is undergoing a major renovation and expansion, with completion expected in summer 2025. Once finished, the updated facility will total 27,000 square feet of advanced, hospital-grade training space designed to better prepare students and health care professionals for real-world clinical settings.
The CSSC, which serves more than 5,000 learners annually, plays an essential role of hands-on education for NYMC’s medical, dental, and physical therapy students, as well as residents, faculty, and various health care providers. The renovations, which started November 2024, will add seven new medical suites, upgrade classrooms and labs, and increase the number of standardized patient exam rooms to 22—including six
NYMC’s Clinical Skills and Simulation Center Expands to Advance Health Care Training
fully accessible rooms to support training in inclusive and culturally competent care with manikins of diverse skin tones, electronic beds, Hoyer lifts, and large doors to accommodate wheelchairs.
New features include an ultrasound and procedural skills classroom, a threebed inpatient ward, labor and delivery suite located next to a pediatric room to simulate seamless care transitions, an orthopedic suite equipped for robotic surgical simulation, interconnected critical care and operative simulation suites, and surgical and procedural skills lab that features high-tech stations and interactive monitors for hands-on learning and tutorials. These enhancements are designed to mirror the environments where students will eventually practice, using high-fidelity manikins, smart technology, and real-time performance feedback to support skills development.
“The renovation is still underway, but every step brings us closer to a center that reflects the future of simulation education,” says Katharine Yamulla,
M.H.E.A., CHSE, director of the CSSC and assistant dean for clinical skills education and assessment, who is overseeing the development. “We are creating a space where students actively observe, engage, practice, and learn in environments that mirror the real-world settings they aspire to be in.”
The newly expanded CSSC will also further elevate interprofessional education by creating collaborative learning experiences for students across multiple disciplines—between the School of Medicine, School of Health Sciences and Practice, and Touro College of Dental Medicine. By supporting teamwork and cross-disciplinary communication in realistic clinical scenarios, the Center will prepare students for the collaborative nature of modern health care. With its advanced technology and immersive training environments, the CSSC is set to position NYMC as a regional leader in clinical simulation, offering a cutting-edge hub that champions innovation, empathy, and excellence in health care education. ■
Clinical Trials Unit Meets the Needs of the Most Complex Trials
The New York Medical College (NYMC)
Clinical Trials Unit (CTU) is the Hudson Valley’s only outpatient clinical trials facility. Located on the third floor of 19 Skyline Drive, the CTU was designed to help promote biomedical and translational research, clinical science, public health research, and innovation. The dedicated research suite comprises more than 1,520 square feet complete with private exam and triage rooms, waiting areas, nurse’s station, laboratory and refrigeration equipment, infusion pumps, cardiac monitors, phlebotomy supplies, adult and pediatric crash carts, computer equipment, restrooms, and secure storage facilities.
The CTU is staffed with a clinical research nurse and research coordinator who are available to assist with every stage of clinical research, from planning and study design to logistics and equipment provisioning, and works in

tandem with investigators to ensure clinical and translational trials are conducted with precision and efficiency.
The CTU is directed by Salomon Amar, D.D.S., Ph.D., vice president for research and professor of pharmacology and of pathology, microbiology, and immunology, at NYMC, and senior vice president for research affairs at Touro University, with support from the NYMC Office of Research Administration and Institutional Review Board, allowing
seamless access to the full complement of expertise and institutional resources.
“The CTU demonstrates NYMC’s commitment to advancing biomedical research,” said Dr. Amar. “Our clients will find the NYMC CTU dedicated space for outpatient research easier to navigate than a large hospital. We welcome a variety of audiences from faculty to private investigators to research participants and volunteers, as well as student interns and potential study sponsors.”
Beyond its robust infrastructure, the CTU offers the use of the NYMC Data Management Core, established to assist biomedical and clinical researchers in designing and executing their studies and access to REDCap Cloud, a web-based application for building and managing surveys and databases online for clinical and translational research. ■




Match Day Marks Another Milestone for Class of 2024
The
Ides of March was far from a time of misfortune for the School of Medicine (SOM) Class of 2024 as they celebrated taking the next step in their medical training on Match Day. Gathered outside the Medical Education Center, at precisely noon, they were at last able to tear open the envelopes that held the key to their futures and learn where they were matched to medical residency programs, as family and friends proudly looked on. The 2024 match included 50,413 applicants total, 44,853 applicants who certified a rank order list (“active applicants”), and 41,503 certified positions in 6,395 residency training programs.
The Class of 2024 is training in 18 states and the District of Columbia at 77 different institutions, including at NYMC major clinical affiliates Westchester Medical Center and NYC Health + Hospitals/Metropolitan, as well as local clinical affiliates NYC Health + Hospitals/Lincoln, Lenox Hill Hospital, Northern Westchester Hospital, and Greenwich Hospital. They are also continuing their medical training at other major top tier, research-intensive, academic medical centers across the country, including

Beth Israel-Deaconess, Brigham and Women’s Hospital, and Massachusetts General of the Harvard Medical School, Brown, Dartmouth, Mount Sinai, Johns Hopkins, Columbia, Weil Cornell, New York University, and Yale.
The top career choices for the Class of 2024 were internal medicine, emergency medicine, anesthesiology, general surgery, psychiatry, radiology, pediatrics, obstetrics and gynecology, and neurology.
“Now it’s real—you’re all going to be doctors, and you’re all going to train at terrific places,” said Neil W. Schluger, M.D., SOM dean and professor of medicine. “Congratulations to all of you. We’ll watch you with pride and excitement for what you will accomplish in your careers.”
“As we approach the moment to find out where you will all be going, remember that no matter what is in that envelope it marks the crowning achievement of all you have accomplished and all you have worked for,” said Susan Rachlin, M.D., senior associate dean for student affairs. “Any program will make you the specialist of your choice, so please relish and treasure this moment.” ■




School of Medicine Class of 2028 Marks Start of Medical School Journey
Members of the School of Medicine (SOM) Class of 2028 marked their first significant moment as medical students at New York Medical College (NYMC) during the annual White Coat Ceremony on July 24, 2024. Taking place on the beautiful grounds of Caramoor Center for the Music and the Arts in Katonah, New York, the ceremony is an annual tradition for SOM firstyear students during which they don their white coats for the first time and pledge an oath they developed as a class to emphasize the professional and humanistic qualities of a physician they consider most important.
Throughout the ceremony, members of the NYMC community offered their advice to the 219 first-year medical students as they embarked on their medical school journey. As they prepared to don their white coats, students were reminded of
the profound responsibility they were undertaking. “If you see a patient in the emergency room, the ICU, the operating room, or at the bedside, all you should see is a human being—regardless of where that person was born, what languages he or she speaks, who they love, who they pray to, if they pray, whatever they feel about the politics of the day, if they’re a Yankees fan or a Mets fan—and you should treat all your patients as no more and no less than that—a human being worthy of respect, dignity, and the highest possible standard of medical care,” said Neil W. Schluger, M.D., SOM dean and professor of medicine.
Keynote speaker, David Asprinio, M.D., professor and chair of the Department of Orthopedic Surgery, addressed the SOM’s newest aspiring physicians directly, offering his sage advice. In his remarks, he reminded them of the humility

essential to their future profession. “Certainly, your accomplishments will be recognized by many, and you will be held in high esteem,” he said. “I hope however that you allow others to be impressed and to recognize your accomplishments and do not become too impressed by yourselves. You are training to do a job. It is an important job that comes with great responsibility; however, others have different jobs that also have great responsibility… What I believe will separate you from your peers who have pursued other careers is the selfless manner in which you will approach each and every patient interaction.”
The Class of 2028 left inspired and united, ready to begin their journey with a commitment to compassionate care and the values they pledged to uphold. ■

Briefs
Classes of 2024 and 2025 SLP Students Shine Bright at the White Coat Ceremony
Ina momentous occasion that marked a significant step in their educational journey, speech-language pathology (SLP) students from the Classes of 2024 and 2025 donned their white coats for the first time. The White Coat Ceremony took place in the John W. Nevins, M.D. ’44 Auditorium on April 1, 2024, where the ambiance was charged with jubilation and a sense of accomplishment.
The event, attended by an enthusiastic audience comprising of family, friends, esteemed faculty members, and distinguished leaders, was a testament to the dedication and commitment of the 38 students from the Class of 2024 and 32 students from the Class of 2025 to the field of SLP. With this symbolic gesture, they signified their transition into the clinical phase of their curriculum and the exciting commencement of their budding careers.
The proceedings began with a heartfelt message delivered by Vikas Grover, Ph.D., CCCSLP, chair of the Department of Rehabilitation Sciences and chief and professor in the Division of Speech-Language Pathology, who also shared encouraging sentiments with the students, echoing pride, achievement, and responsibility. “We tend to
think of speech as something of our mouths,” he said. “We forget that speech has an origin and connection to our hearts and brains. The ceremony is a reminder of how complete your learning is and your willingness to come into your journey of service to others.”
The spotlight turned to the invited speaker, Izel Obermeyer, M.S., OTR/L, ATP, FAOTA, chief clinical officer of the Westchester Institute for Human Development, who inspired students to use their education and personal experiences to shape the speech-language pathologists they want to be in their careers, and to make the most of their careers. Alumnus speaker Andrew Keltz, M.S. ’20, CCC-SLP, encouraged students to offer kindness and compassion to their patients no matter of their circumstance.
With bated breath and hearts brimming with pride, the students were called to the front of the auditorium to ceremoniously don their white coats with the assistance of their dedicated SLP faculty members. Adorned in their emblematic attire, the students stood tall and recited the Pledge for Speech-Language Pathology with unwavering commitment. ■



D.P.T. Class of 2026 Celebrates the Start of Clinicals with the White Coat Ceremony
The Doctor of Physical Therapy (D.P.T.) Class of 2026 celebrated a pivotal moment in their academic journey during the White Coat Ceremony in the John W. Nevins, M.D. ’44 Auditorium on April 15, 2024. Among an audience comprised of family, friends, faculty, and leadership, students embraced their commitment to the field of physical therapy as they marked the transition to the clinical phase of their education.
Students gathered for photographs and buzzed with conversations, clutching their pristine white coats, as they looked forward to their next two years of clinicals. Janet P. Dolot, M.S., D.P.T., Dr.P.H. ’14, PT, OCS, associate professor, program director, and chief of the Division of Physical Therapy, set the tone by introducing Rabbi Baruch Fogel, M.A., campus rabbi of Touro University, for the invocation, followed by inspiring words for the students as they take this next leap in their educational journey. “Donning the white coat serves to remind wearers of their professional duty to practice with honor, caring, and a patient-centered approach,” she said.

Alumnus keynote speaker Jonathan Filipe, D.P.T. ’16, head athletic trainer of the Brooklyn Nets and sports and orthopedic clinical specialist, delivered an empowering message, highlighting the inevitable challenges ahead while emphasizing the profound impact they will have on countless individuals throughout their careers. “These next two years, you will find many shortcomings because every profession has them,” he said. “Do not fall into the trap of letting those shortcomings override the importance and impact you’ll have on thousands of people throughout your career.”
The highlight of the ceremony came as students were called forward to don their white coats, symbolizing their transition into the clinical realm. With assistance from D.P.T. faculty members, they proudly adorned their new attire before reciting the Pledge for Physical Therapy from the American Physical Therapy Association Education Section 2004, reaffirming their dedication to their chosen profession. ■

NEWS Briefs
NYMC Reflects on the Legacy of Medicine During the Holocaust for Yom Hashoah
The New York Medical College (NYMC) and Touro University (TU) communities gathered for a solemn and insightful observation of Yom Hashoah on May 3, 2024. Hedy Wald, Ph.D., adjunct assistant professor of clinical biomedical humanities and ethics, NYMC, and clinical professor of family medicine, Alpert Medical School of Brown University; and commissioner, Lancet Commission on Medicine, Nazism, and the Holocaust, presented her keynote lecture on the legacy of medicine during the Holocaust and its contemporary relevance, shedding light on the lessons to be learned.
Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, delivered remarks honoring Esther Lederman, a Holocaust survivor. Lederman and her family sought refuge in the village of Chmielnik during the Nazi occupation. Her mother and sister were captured and killed in Treblinka. Lederman was hidden for nearly two years by the Zal family, who are recognized as righteous Christians in both the U.S. Holocaust Museum and in Yad Vashem. She was liberated by the Red Army but fled post-war pogroms to the American occupation zone in Germany. Lederman lectured about her experiences at colleges, schools, military bases, and civic organizations.
Dr. Halperin's voice resonated with conviction as he recounted Lederman's story, underscoring the profound importance of bearing witness to the past. “Silence in the face of evil, only advantages the victims,” he said. “It never advantages the oppressors. NYMC convenes today’s program, in part, to convey the message

that health care professionals need to be cognizant of the dangers of language and capable of responding.”
Building upon this imperative, Dr. Wald, daughter of a Holocaust survivor, shared her research on integrating Holocaust awareness into medicine, emphasizing its benefits for medical education and practice. She delved into the historical context of eugenics during the Holocaust, highlighting the involvement of physicians in ethnic and racial cleansing, targeting Jews and people with disabilities.
Dr. Wald emphasized the purpose of teaching medical students the atrocities committed during the Holocaust, particularly focusing on the involvement of medical professionals and institutions in unethical human experimentation, sterilization programs, and euthanasia
to produce the future culturally aware physicians. Every year, she takes 20 medical students to the AuschwitzBirkenau concentration camp to teach them about the influence of medicine in context of the Holocaust. The students consider the unethical tragedies and their role in shaping the health care system as empathetic professionals.
Rabbi Moshe D. Krupka, M.S., executive vice president, TU, closed the event with a prayer alongside Rabbi Baruch Fogel, M.A., campus rabbi of TU. “The purpose of these programs is not to merely weep, but to instill through education, emotional grit, and commitment to a better day,” said Rabbi Krupka. “That Tikvah, that hope, for all people, for peace, for tranquility, for understanding and value of life and true ethics.” ■
NYMC WELCOMES
New Department Chairs

New York Medical College (NYMC) and Westchester Medical Center (WMC) jointly announced the appointment of Erika Berman Rosenzweig, M.D., as chair of the Department of Pediatrics in the School of Medicine (SOM) and director of the Department of Pediatrics at WMC. Dr. Rosenzweig also assumed the role of the William Russell McCurdy Physician-inChief at Maria Fareri Children’s Hospital.
“We are delighted to welcome Dr. Rosenzweig to NYMC as the chair of the Department of Pediatrics,” said Neil W. Schluger, M.D., dean of the SOM. “Dr. Rosenzweig is an internationally prominent physician in her field, with a reputation as an outstanding clinician, teacher, and researcher. We are confident that her visionary leadership will further enhance the tradition of excellence in pediatrics at NYMC, WMC, and Maria Fareri Children’s Hospital over many years.”
Dr. Rosenzweig is a world-renowned expert in the field of pulmonary
Erika Berman Rosenzweig, M.D. Chair of the Department of Pediatrics
“Dr. Rosenzweig is an internationally prominent physician in her field, with a reputation as an outstanding clinician, teacher, and researcher. We are confident that her visionary leadership will further enhance the tradition of excellence in pediatrics at NYMC, WMC, and Maria Fareri Children’s Hospital over many years.
hypertension and serves in leadership capacities for the Pulmonary Hypertension Association and for the Pediatric Pulmonary Hypertension Network of North America. She has authored and co-authored more than 250 scientific publications and has been editor-in-chief of the journal Advances in Pulmonary Hypertension. Notably, she has led more than 50 clinical trials developing novel therapeutic approaches for the treatment of pulmonary hypertension, a life-threatening condition that plagues both children and adults.
Board-certified in pediatric cardiology and adult congenital heart disease, Dr. Rosenzweig received her medical degree from Mount Sinai School of Medicine and completed her residency in pediatrics and fellowship in pediatric cardiology, with special training in pulmonary hypertension at Columbia University Medical Center/New York-Presbyterian Hospital. Over her distinguished 24year tenure as a faculty member at
”Dr. Schluger
Columbia, Dr. Rosenzweig rose to the position of professor and vice chair for clinical and translational research in the Department of Pediatrics and director of the Adult and Pediatric Pulmonary Hypertension Comprehensive Care Center. She continues to actively care for patients with pulmonary hypertension referred to her from around the world.
Dr. Rosenzweig succeeds Leonard Newman, M.D. '70, as chair of the NYMC Department of Pediatrics, and Michael Gewitz, M.D., as director of the Westchester Medical Center Department of Pediatrics and the William Russell McCurdy Physician-in-Chief of Maria Fareri Children’s Hospital. For more than four decades, Drs. Newman and Gewitz each served in various leadership roles at NYMC, WMC, and Maria Fareri Children’s Hospital, advocating for the advancement of children’s health care locally and nationally. ■
NYMC WELCOMES New Department Chairs

Vikas Grover, Ph.D., CCC-SLP, associate professor of speechlanguage pathology, was appointed chair of the Department of Rehabilitation Sciences in the School of Health Sciences and Practice (SHSP). He also serves as chief of the Division of Speech-Language Pathology (SLP), in addition to academic program director of SLP and director of speech perception and production lab at New York Medical College (NYMC) and clinical educator at Boston Children’s Health Physicians.
The restructured Department of Rehabilitation Sciences combines the Divisions of Physical Therapy and SLP to foster a robust interdisciplinary environment. This reorganization offers students enriched, cross-functional learning experiences while allowing faculty to share expertise across disciplines, expanding opportunities for collaborative research, innovative teaching approaches, and community service initiatives.
With an impressive career that blends research, clinical expertise, and academic
Vikas Grover, Ph.D., CCC-SLP Chair of the Department of Rehabilitation Sciences
“Dr. Grover has shown exceptional capabilities in leadership and innovative strategies to improve program effectiveness. He has an interprofessional outlook that will make him effective in leading our degree programs in therapeutic specialties.
”Dr. Amler
leadership, Dr. Grover, who joined NYMC in 2018, brings a transformative vision to the department. He is a certified member of the American Speech-LanguageHearing Association and has a wealth of experience working with multicultural and linguistically diverse populations.
Dr. Grover's clinical background includes extensive work with children in early intervention, providing services from birth to three-year-old children with speechlanguage delays, autism spectrum disorder, and feeding and swallowing issues.
He is dedicated to training both multicultural and multilingual parents and professionals in early intervention. Dr. Grover is particularly interested in the challenges faced by multilingual speakers in perceiving and producing sounds that are non-native to them. His research focuses on how native Hindi speakers of English perceive and produce the /v/ and /w/ sounds.
In addition to his clinical work, Dr. Grover's research focuses on speech production and speech perception. His
dual roles as a clinician and educator underscore his commitment to advancing the field of SLP and ensuring that individuals with communication disorders receive the best possible care and support.
Dr. Grover earned his B.Sc. in speech, language and hearing from Mangalore University, M.A. and M.Phil. in linguistics from Delhi University, and M.Phil. and Ph.D. in speech-language-hearing sciences, from the City University of New York Graduate Center. In 2021, he was elected as a faculty member into the NYMC chapter of the Alpha Eta Society, the national honor society for allied health professionals. Westchester Magazine named Dr. Grover a 2025 Healthcare Hero.
“Dr. Grover has shown exceptional capabilities in leadership and innovative strategies to improve program effectiveness,” said Robert W. Amler, M.D., M.B.A., dean of the SHSP and vice president for government affairs. “He has an interprofessional outlook that will make him effective in leading our degree programs in therapeutic specialties.” ■

John Phillips, M.D., FACS, was appointed chair of the Department of Urology in the School of Medicine (SOM), while also assuming the role of director of the Department of Urology at Westchester Medical Center (WMC).
A national leader in robotic surgery, residency training, and the basic science of urologic diseases, Dr. Phillips joined WMC as section chief of Urologic Oncology and Robotic and Laparoscopic Surgery and the New York Medical College (NYMC) faculty in 2007. In addition to his continued role as section chief, he currently serves as program director for the WMC Residency Training Program in Urology as well as professor of urology and executive vice chair of the NYMC Department of Urology.
An expert in kidney cancer and minimally invasive kidney-preserving surgery for small renal masses, Dr. Phillips has performed more than 2,000 Da Vinci robotic surgeries and is a pioneer
John Phillips, M.D., FACS Chair of the Department of Urology
“Dr. Phillips’ extraordinary expertise in robotic surgery and dedication to advancing urologic care, combined with his commitment to enriching the educational experience for our medical students, ensures that the next generation of physicians will benefit from his leadership and innovation.
Dr. Schluger
”in MRI-based fusion prostate biopsy, which has markedly lowered infectious complication rates of prostate biopsies.
With a strong background in neo-bladder reconstruction after bladder removal (cystectomy), Dr. Phillips has performed total intracorporeal neobladder surgeries since 2015. In 2020, Dr. Phillip’s lab was selected as a three-year award recipient in the Empire State Clinical Research Training Program, which has led to the pre-clinical evaluation of nanoparticle therapy in bladder cancer.
Dr. Phillips has been widely published and presented on a range of urological topics. He is the founder and editorin-chief of the International Journal of Urologic History, a past member of the Leadership Class of the American Urological Association, and a past president of the New York State Urologic Society. In 2024, he began a three-year term as the historian of the American Urologic Association.
“We are thrilled to welcome Dr. John Phillips to his new role as chair of the Department of Urology at NYMC,” said Neil W. Schluger, M.D., dean of the SOM. “Dr. Phillips’ extraordinary expertise in robotic surgery and dedication to advancing urologic care, combined with his commitment to enriching the educational experience for our medical students, ensures that the next generation of physicians will benefit from his leadership and innovation.”
Board-certified in urology, Dr. Phillips received his medical degree from Yale University School of Medicine. He completed a residency in general surgery and urology at Yale-New Haven Hospital and a fellowship in urologic oncology at the National Cancer Institute of the National Institutes of Health.
Dr. Phillips succeeds Muhammad Choudhury, M.D., who led the Department at NYMC since 2001 and the Division of Urology at WMC since 1989. ■
COMMENCEMENT
NYMC Honors the Class of 2024
TheNew York Medical College (NYMC) community buzzed with excitement as the Class of 2024 marked their achievements in medicine, biomedical science, and the health sciences. Leadership, faculty, and loved ones gathered to honor the graduates as members of the Class of 2024 reveled in their accomplishments and looked forward with enthusiasm to the adventures that await them. The graduates radiated pride as they affirmed their dedication to their chosen professions. The ceremonies— the School of Health Sciences and Practice (SHSP) and School of Medicine (SOM) on May 21 at The Performing Arts Center at SUNY Purchase College and the Graduate School of Biomedical Sciences (GSBMS) on May 23 on the NYMC campus— conferred 193 doctor of medicine (M.D.) degrees; 46 doctor of physical therapy (D.P.T.) degrees; five doctor of philosophy (Ph.D.) degrees; 78 master of science (M.S.) degrees; 42 master of public health (M.P.H.) degrees; and seven doctor of public health (Dr.P.H.) degrees.
Graduates soaked in the advice of commencement guest speakers. SHSP commencement speaker James V. McDonald, M.D., M.P.H., health commissioner for the New York State Department of Health, spoke to the graduates about finding and maintaining joy in their careers. “As you graduate today, whether you’re helping people walk and talk, whether you’re helping people prevent problems, whether you’re finding data that shows us where we’re going, I hope you recognize the power of passion that is yours to find,” said Dr. McDonald.
School of Medicine


The SOM commencement speaker and honorary degree recipient, Steven L. Kanter, M.D., executive director of the Alliance of Academic Health Centers International and special advisor to the president and chief executive officer of the Association of American Medical Colleges and executive director of Alliance of Academic Health Centers International, remarked about the advent of the new phase of the new physicians’ lives. “Always remember that providing health care is only one aspect of being a physician,” said Dr. Kanter. “As physicians, we are healers, helpers, carers, advocates for the sick, and advocates for the help of all. And we do this as we strive to be ever wiser scientists and humanists.”
GSBMS commencement speaker Brooke Grindlinger, Ph.D., renowned microbiologist and chief scientific officer at The New York Academy of Sciences, spoke about the ability of the graduates to emphasize real-world impact with their new degrees in biomedical sciences. “Your unique experiences and viewpoints are unmatched,” said Dr. Grindlinger. “So, embrace boldness in your ideas, cultivate a strong viewpoint, seize control of your professional journey, and fearlessly stand out.”
Former dean of the SOM, Jerry L. Nadler, M.D., MACP, FAHA, FACE, adjunct professor of pharmacology, was awarded an honorary degree. ■



School of Health Sciences and Practice



Graduate School of Biomedical Sciences







Running for a Cause
NYMC students go the distance at the 2024 TCS New York City Marathon while others volunteer on the sidelines

BY KIARA THOMAS, M.A.
Six students from New York Medical College (NYMC) took their marks at the iconic TCS New York City (NYC) Marathon on November 3, 2024. While they conquered the 26.2-mile course across the five boroughs, raising more than $20,000 for charity, dozens of their fellow classmates volunteered their services to provide aid behind the scenes. It was a giving and learning opportunity for all.
RYAN MOHEBPOUR, SOM CLASS OF 2028

This was the second NYC Marathon Ryan Mohebpour, School of Medicine (SOM) Class of 2028, completed. He ran in support of Strive for Stride, a nonprofit with 400 runners from 27 countries that supports immigrant, BIPOC, and low-income runners. While navigating the demands of his first semester at NYMC, Mohebpour remained steadfast in his deep commitment to both his medical career and his running goals.
“The NYC Marathon is a race known world-wide,” says Mohebpour, who raised more than $4,000 for Strive for Stride and finished the marathon in four hours and seven seconds.
“Many talented runners want to participate, but fundraising and getting to the race can be some of the most challenging aspects. I thought it would be great to be a part of an organization that gives people that chance.”
Aligning with an organization’s mission was crucial when deciding which team to run for, explains Mohebpour, who ran for Fred’s Team for the Memorial Sloan Kettering Cancer Center the previous year.
“I watched the NYC Marathon when I first moved to Manhattan from Florida, and I was so inspired—not just because of the sheer distance people were running, which seemed almost impossible when you see it on the map, but by the people themselves,” says Mohebpour. “Everyone had their own personal reason for being there and shared emotional moments with family. I wanted to share that experience and be part of
something bigger than myself. I wanted to challenge myself in a way I hadn’t before.”
Mohebpour views running in the marathon as more than just an accomplishment to boast about; it’s an opportunity to make a difference in the lives of people around the world. Just like medicine, by aligning his running with causes he deeply cares about, he uses his passion to support and uplift others, demonstrating that the impact of his efforts extends far beyond the finish line.
JOSHUA GARELIK, SOM CLASS OF 2027

Joshua Garelik, SOM Class of 2027, entered his second year of medical school balancing the demands of academics and training for his first-ever NYC Marathon. He incorporated interval and strength training into his busy schedule, with a goal of running at least 20 miles a week, which led him to finish the marathon in four hours and 35 seconds.
Garelik teamed up with Margot Richards, SOM Class of 2027, to run for the New York Road Runners Team for Climate. The nonprofit, which aims to build healthier lives and stronger communities through running, partnered with Anew Climate, a global leader in climate solutions, to use the funds raised to purchase carbon credits supporting two improved forest management projects. He raised more than $3,000 to support their mission.
An active member of the College’s Environmental Health Interest Group, Garelik started running three years ago, adding the hobby to his weight training regimen to stay in shape, but he hated it. He opted to bike, play basketball, or surf. After graduating from college, he and his friends decided to run a half marathon, which motivated him to start running consistently.
“I had a great time and have been hooked ever since,” Garelik, who has run two half marathons, says. “I noticed improvements in my energy levels throughout the day. I feel great after a run, especially after a challenging one. Then, one day, I thought, I should run in the NYC Marathon. When else in my life am I going to be in New York running with more than 50,000 people at the same time?”
Interested in health, fitness, and medicine, Garelik had the unique opportunity to enroll in an advanced gross anatomy class in high school, an experience that solidified his decision to pursue a career in medicine. “Medicine seemed like the perfect career path where I could be presented with challenges and, hopefully, come up with solutions—or at the very least, contribute to making things better,” he says.
As Garelik reflects on his journey from casual runner to marathon runner, he recognizes the parallels between his passion for medicine and his commitment to running. Both require discipline, perseverance, and a desire to improve lives—whether it’s his own through fitness or others through medical care.

MARGOT RICHARDS, SOM CLASS OF 2027
Margot Richards, SOM Class of 2027, successfully conquered the full 26.2 miles of the NYC Marathon. She rose to the challenge of a lifetime on the route to becoming a physician.
“It is really easy, as a medical student, to get sucked into school and only focus on your studies,” says Richards. “But I prioritize having balance and pursuing other interests.”
Richards finished the marathon in four hours, 49 minutes, and four seconds, also running for the New York Road Runners Team for Climate alongside team member Joshua Garelik, SOM Class of 2027, and raising more than $3,000.
“As physicians, we want to make the world a better place and implement changes that help people,” says Richards, who grew up composting and bringing recyclable bags to the grocery store. “I thought, ‘What better way than to leave the Earth in a better state than we found it in than running with Team for Climate?’”
Richards’ journey to the marathon was shaped by her experiences in high school. Richards was a 100-meter runner and intended to continue running in college. However, hip surgery during her junior year derailed her plans. A yearlong recovery led her to focus her sights on enrolling in 5Ks and 10Ks, with encouragement from her surgeon. This experience, coupled with her years volunteering on a suicide hotline, inspired her to enroll in medical school.
"For me, being there for people during their worst moments and helping them through it has always been incredibly rewarding,” she says. “In medicine, you have the power not only to support them but also to help them recover."
Running the marathon marked a new chapter in Richards’ journey, pushing her beyond her previous limits, much like the challenges she faces in medical school.
“I never thought I would be able to run a marathon,” she says. “Having this new challenge for myself was really exhilarating.”
AMBER ZHAO, SOM CLASS OF 2027
For three and a half years, Amber Zhao, SOM Class of 2027, volunteered as a crisis counselor and legal advocate for Crime Victims Treatment Center (CVTC), ensuring sexual assault and domestic violence victims in the emergency room were taken care of and helping them navigate the hospital system. Zhao's unwavering commitment to advocating for these individuals led her to run in her first NYC Marathon to support the organization, raising more than $3,500 for CVTC and finishing in five hours, 22 minutes, and 31 seconds.

“It is impossible to live in New York and not want to run the marathon,” says Zhao. “Being here for six years, there’s no way this idea wouldn’t have popped in my head.”
Hailing from St. Paul, Minnesota, Zhao admired the more than 50,000 runners who weaved through the five boroughs for various charities each year. The idea of participating in this iconic event lingered in her mind, but it wasn’t until she attended NYMC that she decided the time was right to check this goal off her bucket list.
Her path to the marathon, however, was not without its challenges. Zhao had initially planned to participate in the race in 2020, but the onset of the COVID-19 pandemic derailed those plans. Years later, she found herself hitting the ground running for a cause she passionately supports.
“I appreciate the work that CVTC does,” says Zhao. “This is a cause I always cared about. My experience as a counselor taught me how to look for ways to improve the patient experience and solidified my desire to go to medical school,” she says, determined to continue making a meaningful impact.
LAUREN KANN, SOM CLASS OF 2027

When Lauren Kann, SOM Class of 2027, heads out for a run, she navigates trails between towering hemlocks and slender birches. For the NYC Marathon, she put her foot to the pavement for four hours, 43 minutes and 53 seconds, surrounded by skyscrapers, bridges, and tens of thousands of people.
Running is not new for Kann, who completed three half marathons as a teen. She ran the Miami half marathon for Yachad, an international organization supporting Jewish people with disabilities, with her father and her sister Rebecca Kann, SOM Class of 2026. An avid hiker, she transitioned to running trails, running up to 15 miles during her college years, waving to cows and horses, traversing gorges.
Encouraged by a friend, Kann finally decided to turn her longheld dream into reality by running in the NYC Marathon, but she only had nine weeks to train. She ran to support Team Blue Card, an organization that assists Holocaust survivors through financial assistance for essentials like rent, food, medical expenses, and home improvements to help survivors stay independent in their homes. The name of the organization derives from the blue paper cards issued to Jewish donors who raised funds for people who had lost their jobs to the growing antisemitism before World War II.
“I have been involved in various initiatives related to Holocaust survivors, including volunteer work and fundraising, largely due to my experiences at a Jewish school,” says Kann, who raised more than $3,000 for Team Blue Card. Two of her late grandparents were Holocaust survivors and Kann grew up hearing their stories of heartbreak and heroism. Team Blue Card’s cause felt especially important to her.
To train for the marathon, Kann ran trails, even spotting a black bear on one of her trips. Her love of nature and the outdoors influenced her decision to study medicine using the perspective of “One Health,” which recognizes the intersection of human, animal and environmental health, an approach she hopes to apply in a career in disaster medicine.
SAMANTHA FEA, D.P.T. CLASS OF 2027

“I signed up for a half marathon spontaneously and that was it,” says Samantha Fea, Doctor of Physical Therapy (D.P.T.) Class of 2027. “It was all over from there.”
Fea has completed four half marathons and two NYC Marathons in two years. Compared to her other life-long interest in dance, she has found running to be a completely different yet equally fulfilling way to challenge herself and push her physical and mental limits.
“For the last three miles of the marathon I question myself, ‘Why do I do this to myself? I’m never running again,’” says Fea. “But when I finish, the energy and feeling of accomplishing something that big is something I can’t describe. I’ve never felt that way in my years of dance.”
For the second year, Fea supported Team for Kids at the NYC Marathon. She raised more than $3,000 for the organization, which is committed to fundraising for New York Road Runners youth and community programs dedicated to fitness and running. Deeply understanding and appreciating how fitness played into her own personal growth, Fea felt a strong connection to their mission.
For years, Fea’s fitness was dance. She didn’t step foot into a gym until after college. She worked as an aid and fitness coach at a physical therapy and fitness center, fulfilling her hours for her nursing school requirement. Fea enjoyed her work so deeply that she stayed for two years before shifting her career goals and applying to the NYMC School of Health Sciences and Practice D.P.T. program.
For 16 weeks, Fea allotted time in between her classes and studies to train in the five boroughs. She accomplished her goal of finishing just under four hours at three hours, 59 minutes and 42 seconds. “New York’s marathon is a tough course. It’s one of the hardest. Seeing that I finished under four hours, when I finished at four hours and 12 minutes the previous year felt amazing.”
Through running, Fea has discovered the transformative power of movement, not only in her own life but also in the lives of others. As a physical therapy student, she channels this devotion into helping others recover, grow stronger, and overcome their own challenges.

STUDENTS JOIN FORCES TO SUPPORT MARATHON RUNNERS
As more than 50,000 marathon runners from around the world tackled the 26.2 miles of the TCS NYC Marathon, many found support from dozens of NYMC students, part of Touro University’s Team Touro volunteers, from different disciplines volunteering as medical aid, helping them along every step of the way.
“I worked with high-level athletes in their unexpected time of need for what should be the best day of their lives,” says Jeff Duro, D.P.T. ’25. “I was one of the first people these athletes saw after crossing the finish line, seeing them before their families and friends. I was able to share that moment with them. It put into perspective for me that this moment could taint their view of what they just accomplished, but I had the opportunity to treat their injury and remind them that they just completed one of the greatest feats of their lives.”
Students gained hands-on experience in a fast-paced and high-energy non-traditional clinical setting. They practiced critical skills, including patient triage, quick decision-making, and compassionate care under pressure, all while supporting runners through one of the most challenging achievements of their lives. For these students, well-equipped with their learning at NYMC, it was a chance to grow as future physicians and physical therapists, strengthening qualities of resilience, empathy, and adaptability.
“I saw a few cases of heat exhaustion and even a couple of runners who experienced dizziness and mild disorientation, which we don’t typically see in a clinic,” recalled Kennedy Tran, D.P.T. ’25, who says the marathon helped improve his triaging skills. “The unpredictable nature of outdoor, high-endurance events brought unique challenges to patient care.”
The medical volunteers were stationed in medical tents throughout the marathon’s route for up to 12 hours aiding runners who experienced common injuries, like dehydration, muscle cramps, and exhaustion. CPR-trained volunteers attended orientation two weeks before the marathon to prepare for their roles. On race day, they assisted in taking medical histories,

tracking runners, and supporting the medical teams, which included attending physicians, resident physicians, physical therapists, nurses, and other health care professionals. Students in physical therapy also provided massages and guided stretching to help runners recover.
“Every single person in a medical tent has a breadth of knowledge and years of experience behind their back that differ from yours and from the person next to you, and now you are united to take care of a patient,” says Dana Ross, a student in the Accelerated Master’s Program in the Graduate School of Biomedical Sciences. “You have most likely just met yet are driven by the same goal and love for health care. I find this aspect of these events to be beautiful.”
“Observing how each role approached the same cases with their specific skill sets gave me a new appreciation for the strengths each discipline brings to patient care,” says Steven Shifren, D.P.T. ’25. “The collaborative environment showed me how diverse expertise converges to create effective treatment in dynamic situations.”
Students studying in various health care disciplines developed a greater respect for and admiration of each other's expertise and dedication.
“I also was very impressed and appreciative of the physical therapists who volunteered at the event. From a strictly ‘medicine’ standpoint, the treatment for cramping felt quite limited when compared to the specific massages and stretches the expert physical therapy volunteers were able to provide,” says Alex Park, SOM Class of 2026, whose father, Chong H. Park, M.D. '96, graduated from NYMC. “I also think it is important for everyone to have some physical therapy knowledge to help prevent and recover from injuries.”
For many NYMC students, this experience sparked a newfound interest in sports medicine. For others, the marathon reaffirmed their dedication to their chosen fields, already eager to volunteer again next year and be part of a life-changing day for runners. ■
TWENTY YEARS OF REVOLUTIONIZING Emergency Preparedness
The Center for Disaster Medicine is on the front lines of training, research, and response initiatives in disaster preparedness, emergency medicine, and public health resilience.

BY ANDREA KAHN
The moments before catastrophe strikes—a school hallway erupting in gunfire, the first frantic response to an unfolding terror attack, or the winds rising with the fury of a hurricane—mark a fragile threshold between survival and tragedy. For decades, disaster readiness in the United States has stumbled at that threshold, unprepared to meet the moment.
The aftermath of 9/11 made this failure impossible to ignore. America’s disaster preparedness systems were fragmented, reactive, and designed for the mythical “average” adult, leaving vulnerable populations—children, the elderly, and people with disabilities—at significantly higher risk.
It was this glaring reality that spurred the creation of the Center for Disaster Medicine (CDM) in 2005. Founded by Robert W. Amler, M.D., M.B.A., dean
of the School of Health Sciences and Practice (SHSP) and vice president for government affairs at New York Medical College (NYMC) and a former senior official with the U.S. Department of Health and Human Services, and David S. Markenson, M.D., M.B.A., Dr.P.H.’25, a pediatrician and global expert in emergency preparedness, the Center had an ambitious mission: to revolutionize disaster preparedness by making it proactive, inclusive, and built for the realities of an unpredictable world.
“It’s not a matter of ‘if,’ but ‘when,’” says Dr. Markenson, director and medical director of the CDM, senior associate dean of research, SHSP, and professor at the Institute of Public Health. “Our goal has always been to stay ahead of future crises, fill in the gaps, and build a system that is ready for anything—big or small—and works for everyone. Too often, plans focus
on the last disaster instead of preparing for the next one and leave out whole segments of people.”
The first civilian resource of its kind in the nation, the CDM has evolved into a national leader. Its multidisciplinary team has redefined readiness through cutting-edge simulations, research, and community-focused training. In 2024 alone, more than 1,000 first responders, health care workers, and educators completed in-person training, while countless others benefited from its programs nationwide.
THE HUDSON VALLEY: A MICROCOSM OF RISK
Situated at NYMC in Valhalla, New York, the CDM operates in the Hudson Valley, a region whose diverse geography makes it an ideal testing ground for inclusive and scalable disaster preparedness.
With NYMC’s public health expertise, cutting-edge facilities, and extensive partnerships, the CDM was wellpositioned from the start.
Indeed, the Hudson Valley’s unique landscape reflects the complexities of national disaster readiness. Urban hubs like Yonkers border stretches of rural farmland, while the Hudson River and aging infrastructure introduce constant risks. Winter storms cause power outages, industrial corridors face chemical spill threats, and flooding remains a perennial hazard. “The Hudson Valley is a microcosm of the challenges we face nationally,” says Dr. Markenson. “If we can solve problems here, we can scale those solutions anywhere.”
The CDM has turned its attention to emerging crises like extreme heat driven by climate change, developing strategies to protect the Hudson Valley’s most at-risk residents, including the elderly and lowincome communities—an approach that underscores the ever-growing urgency of disaster preparedness.
BRIDGING THE DIVIDE BETWEEN CARE AND CHAOS
For years, police, fire, and EMS have operated independently, with little overlap in their defined professional roles—leaving critical gaps when largescale emergencies strike. While both police and fire recruits receive basic emergency medical training, that training is rarely revisited, and often falls short in preparing them for the unpredictable realities of the field.
“ ”
The Hudson Valley is a microcosm of the challenges we face nationally. If we can solve problems here, we can scale those solutions anywhere.
Dr. Markenson
Tackling this shortfall head on, the CDM created the Division of Operational and Tactical Medicine and developed their Tactical Emergency Casualty Care-Rescue Task Force program. Designed for high-risk scenarios like mass shootings and terrorist attacks, the program has trained hundreds of first responders and even civilians to provide life-saving care and tactical response in the crucial moments which can make the difference between life and death.
“Every second matters in an emergency,” says CDM Assistant Director Tai M. Lee Jr., MEP, NRP, CIC/RF, TP-C, a paramedic and retired NYPD officer. “Knowing how to stop a bleed or open an airway can completely change the outcome for someone in crisis. It is about giving people the tools to act.”
TRAINING FOR THE CHAOS OF REALITY
In the shadowy haze of a smoke-filled training room, strobe lights flash erratically, sirens blare at ear-splitting volume, and manikins lie scattered on the ground, some with mock injuries so realistic they make first-time trainees pause. This is not chaos—it is preparation, meticulously designed by Lee, who leads
responder trainings at the CDM. “We create environments that replicate reallife chaos—dark, noisy, overwhelming,” he says. “It is about forcing people to get comfortable being uncomfortable because that is what saves lives in the field.”
Historically, disaster training was passive and predictable—limited to classroom lectures that rarely addressed the chaotic realities of emergencies. Trainees learned theory, but practical, immersive simulations that mirrored real-world conditions were virtually nonexistent.
The CDM revolutionized disaster training. Under Dr. Markenson’s leadership, the Center pioneered immersive, scenariobased programs that drop participants into high-stakes crisis simulations, preparing them to think fast and act decisively.
"‘Crawl, walk, run,’ is our training method,” Lee explains. “If we just threw people into an ultra-complex scenario, they would surely fail. And when we first start, people freeze. But by the end of the training, they have practiced the skills so much that they just do it—they are assessing the scene, stabilizing victims, and working as a team.” That repetition is what sets CDM’s training apart, turning knowledge into instinct.
Teddy Druckman, a lieutenant with the Larchmont Volunteer Ambulance Corps who has completed multiple CDM training courses, puts it simply: “Their training is unlike anything else. You are not just learning in a classroom; you are in the thick of it, applying skills over and over until it becomes second nature.”

And, he adds, programs build cooperation among responders. “When you train together, you understand each other’s roles and trust each other in ways that would not happen otherwise. It is no longer about who is in charge; it is about getting the job done and saving lives.”
The CDM is not only a world-class training center but a leader in innovative research. In 2018, New York State named the facility a Center of Excellence in Precision Medicine and Responses to Bioterrorism and Disasters. This designation has supported research on topics like how climate change increases disaster risks and how to strengthen hospitals during pandemics. CDM staff mentor students at NYMC, Touro University, and institutions worldwide in disaster, tactical, EMS, and pediatric emergency medicine research.
One current project integrates Full Dive Virtual Reality with emerging immersive medical technologies developed by the Center, advancing education and drills with ultra-realistic simulations. “Mass casualty events, public health emergencies, and disasters are evolving, and so are the solutions,” says Lee. “Our job is to stay ahead of the curve.”
EMPOWERING HOSPITALS AND HEALTHCARE WORKERS
The CDM trains healthcare workers, allied health professionals, and students in mass casualty triage and preparedness, both on-site and in real-world hospital settings. Its programs stand out not just for their content but for their immersive approach—using trained actors with realistic injuries, high-tech manikins that speak and respond, and hands-on simulations that mirror real-life crises. These exercises help participants refine their triage skills, assess emergency protocols, and integrate facility management plans under pressure.
“ ”
When people are trained, they respond with confidence, not panic, and that saves lives. Preparedness is not just for big disasters—small emergencies—like a shop-class injury or a power outage—demand preparedness. It is always key.
Dr. Markenson
training capacity and allowing multiple programs to run simultaneously. Funded through a combination of state and federal grants, the new classrooms—each designed for 20 to 30 participants— will provide critical breakout space for specialized training, including Homeland Security courses.
While the CDM has long been a leader in hands-on simulation training, the new Center elevates that training to a whole new level, replicating the urgency of realworld emergencies with unprecedented realism. Inside, high-fidelity manikins breathe, bleed, and react like actual patients, while a hidden control room allows instructors to manipulate conditions on the fly—altering vitals, introducing sudden complications, and forcing trainees to make split-second decisions. An integrated AV system records every moment, allowing for detailed playback and analysis. By reviewing their responses after performing under pressure, first responders and medical personnel can refine their skills in high-stakes, life-or-death scenarios.
“This expansion is about more than just adding space—it is about expanding possibilities,” Lee says. “With these new classrooms and simulation capabilities, we can train more people and adapt to the evolving challenges first responders face. It is an investment in the future of disaster preparedness.”
SAVING LIVES IN REAL TIME
EXPANDING TRAINING FOR A CHANGING WORLD
As the CDM expands its role in training and preparedness, it is also undergoing a physical transformation.
In spring of 2025, a state-of-theart simulation center and two new classrooms opened, doubling the Center’s
On a cold Tuesday afternoon in December 2024, Robert Kick, a cardiothoracic nurse and veteran volunteer firefighter and EMT, responded to an emergency call: a motorcycle accident on a city road in Rockland County. Arriving at the chaotic scene, Kick immediately assessed the victim—severe injuries to the chest, a broken pelvis and legs, and a motorcycle still running in the background. But one critical detail stood out.
Blood was gushing from the man's groin—sign of an arterial bleed. “I could see it from a distance,” Kick recalls. With arterial bleeding, a person can bleed out in three minutes. It had already taken him one and a half minutes to reach the scene. A standard assessment could have taken another minute or two—time the victim did not have.
Instead, instinct and training took over. Just weeks earlier, Kick had completed the trauma response course taught by Lee, which emphasized rapid assessment and bleeding control. The repetition drilled into him during training made the difference. He immediately applied pressure to the exact spot needed to stop the bleed, blocking out the surrounding chaos.
“The speed and confidence in which I reacted would not have happened if I had not taken Tai’s course,” Kick says. “Even with everything going on—the screaming, the wreckage, the bike’s engine idling in the chaos—I had tunnel vision. I saw the bleed and stopped it.”
Without that split-second response, the outcome could have been very different.
PROTECTING THE MOST VULNERABLE
Since its inception, children have played a key role in the CDM’s mission. “Children make up 25 percent of the population, yet they are often left out of preparedness plans,” says Dr. Markenson. “If parents do not believe their children are safe, they will not comply with emergency orders, and the whole plan falls apart.”
Every day, schools face emergencies— some that make headlines, some that do not. Those on the scene—teachers, principals, custodians, security guards— often face split-second, high-impact decisions. In those circumstances, preparedness can make the difference between life and death.

“There is not a month that goes by that a New York school does not face a crisis,” says Dr. Markenson. “When people are trained, they respond with confidence, not panic, and that saves lives. Preparedness is not just for big disasters—small emergencies—like a shop-class injury or a power outage—demand preparedness. It is always key.”
TRANSFORMING SCHOOL PREPAREDNESS IN YONKERS
During the 2023–24 school year, the CDM partnered with Yonkers Public Schools in a pioneering pilot program, training nearly 4,000 educators, administrators, and staff across 29 schools. From mass shootings and opioid overdoses to fires, floods, terrorist threats, and mental health emergencies, these customized programs and educational experiences equipped staff, parents, and community members with the tools to respond quickly and effectively to a broad range of crises. “This is not just theory,” says Emily Kaplan, Dr.P.H. ’21, and M.P.A., EMTP, assistant director of the CDM and assistant professor of public health in the SHSP. “We make sure participants leave with practical skills they can use in any emergency.”
When developing large-scale emergency drills and educational programs, Dr. Kaplan guides participants through simulations using their school's floor plans—much like a strategic board game—helping them map out evacuation routes, gathering points, and locations of essential supplies. As a result, one Yonkers school relocated its Narcan supply to ensure faster access during a
potential opioid crisis. “It is all about matching training and filling gaps with actual experience,” she says.
These trainings do not just prepare individual schools—they equip educators to train others through train the trainer programs in courses such as CPR, first aid, bleeding, and opioid emergencies, spreading a culture of preparedness throughout the district and assuring continuity of this knowledge and education. As more schools recognize the need for proactive emergency planning, demand for CDM’s training continues to grow. By 2025, dozens of schools are already on the waiting list, eager to implement these life-saving programs in their own communities.
When Saunders Trades and Technical High School, which has more than 1,000 students, partnered with the CDM, Principal Jeremy Rynders saw it as a crucial opportunity. “With culinary and carpentry programs—and teenagers— accidents can happen,” he says. “And we could not have funded this on our own.”
The CDM staff went beyond training teachers in “Stop the Bleed,” CPR, and basic first aid—they certified them to train students. “It was game-changing,” says Rynders. “Now, if something happens, we will have 25 students who know exactly what to do, not just the teacher.”
Chef Titus Thompson Okumodi, a culinary instructor at Saunders for nearly 30 years, is well aware of the risks that come with the kitchen—from knife mishaps to fires. “My job is not just to teach cooking; it is to make sure my

students know how to protect themselves and save lives,” he says. “These handson certifications do not just make them safer—they give them an edge in the industry, setting them up for success in the real world."
THE ROAD AHEAD
The CDM’s transformative work over the past 20 years can be traced back to the principles it established in its earliest days. Today, it stands as a national leader, addressing the full spectrum of disaster readiness with the same urgency and clarity that shaped its founding mission, redefining preparedness as inclusive, proactive, and rooted in real-world challenges.
As the CDM enters its third decade, its focus remains clear: to prepare communities for the crises of tomorrow. Whether training schools to manage emerging threats, expanding partnerships in under-resourced areas, or integrating new technologies into disaster response, the CDM continues to evolve with the changing landscape.
“What we started 20 years ago has become a model for emergency preparedness for mass casualty events, public health emergencies and disasters and has set the standard for research and education in disaster, operational, tactical, EMS and emergency medicine,” Dr. Markenson says. “And the need for this work is more urgent than ever.” ■

Cairo,
M.D.,
Engineers Hope to Cure Childhood Cancer
Mitchell
Mitchell Cairo, M.D.’s relentless pursuit of a cancer-free future for children inspires his prolific research, empathic patient care, and courageous clinical trials. While proud of the staggering progress in his field, this physicianscientist remains focused on breakthroughs to yield even better results.

BY MELISSA PHETERSON
When Mitchell Cairo, M.D., began his formal education, he had no idea that he would pursue medicine or research, let alone become a world-renowned physician-scientist with the staggeringly ambitious goal of curing childhood cancer.
Dr. Cairo, professor of pediatrics, medicine, pathology, microbiology, and immunology, and cell biology and anatomy, and vice chair of the Department of Pediatrics at New York Medical College (NYMC), has produced nearly 500 peer-reviewed publications, delivered more than 1,300 national and international presentations, and received numerous multi-million-dollar grants. But he entered the University of Wisconsin with modest ambitions.
“I grew up in a poor, working-class environment,” he says. “Neither of my parents went to college, nor did we know anyone in medicine.”
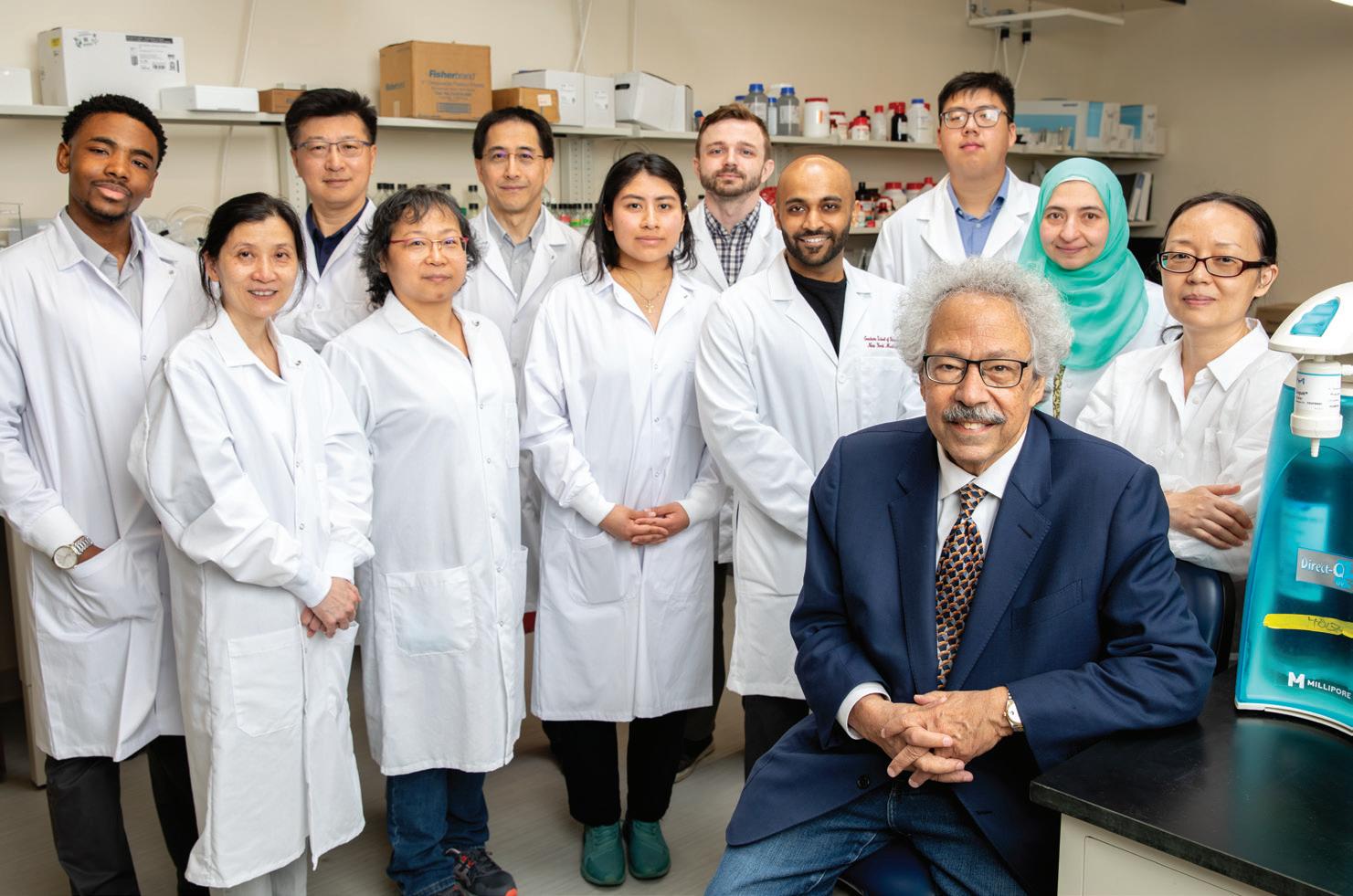


During medical school, Dr. Cairo’s pediatric clinical clerkship introduced him to young patients with blood and cancer disorders. “These are patients, and families, with whom I kept lifelong relationships,” he says. He also appreciated the science-driven, tangible outcomes of hematology and oncology. “I wanted to get into a field where I could make a difference. Instead of simply managing a chronic condition, I wanted the ability to diagnose a patient and prescribe a therapy that could treat and cure what might have been a lethal disease.”
In the late 1980s and early 1990s, Dr. Cairo saw vast room for improvement in treatment, which at the time involved “nitrogen mustard and other noxious therapies”—aggressive approaches that destroyed healthy cells and tissue along with cancerous ones.
“Those were the tools in our toolbox, at the time,” he says. “However, I began to realize that while these treatments work well, they have a lot of unpleasant side effects, both during treatment and, more importantly, later in life,” he says. The long-term effects of beating cancer were often as miserable as the cancer itself.
Leveraging his interest in science, he yearned to probe deeper: to investigate the mechanisms driving the cancer, understand why certain patients respond to treatments and others do not, and design a methodical approach to target rogue cells while sparing healthy tissue. One early triumph was a clinical trial for

Rituxan, a targeted immunotherapy that both attacked specific cells while rallying the patient’s own immune response. That proof of concept paved the road to cellular therapy, then regenerative cell therapy, and now gene therapy. “Each iteration advances the same theme of how we can leverage a patient’s own cells, or universal donor cells, and result in a curative effect that will have the least amount of acute or long-term harm,” Dr. Cairo says.
CLINICAL TRIALS OF COURAGE
Bold new approaches to cancer treatment rely upon rigorous clinical trials, some of which recruit young patients who need a miracle. “Developing ‘first in adult, first in child, first in baby’ trials is a point of pride in my career,” says Dr. Cairo, who supervises studies at medical sites across the United States, supported by grants from such agencies as the National Cancer Institute and Department of Defense. His passion for translational research, the bridge between laboratory-based inquiry and bedside clinical care, grounds his professional identity.
“I have believed in translational research since my first day of medical school,” says Dr. Cairo. “I believe that taking to the bedside a breakthrough in the lab or learning something at the bedside to bring back to the bench, is the ultimate goal in being a physician-scientist.”
The drawback, he acknowledges, “is that I am competing with people who are focused on research with no clinical responsibilities or who are treating patients


without research obligations.” But he remains committed to both, and the synergies they spark. “At the end of the day, I believe translational research is the fastest way to integrate breakthroughs into patient care and to accelerate cures. Since I made the decision to become a physicianscientist, I have not looked back.”
Dr. Cairo’s moral compass in treating his patients points to just one question: “If this were my own child, what would I want done?” He allows that while experimental treatments carry uncertainty, the results may answer a family’s most urgent prayers: to find the definitive cure for a chronic condition.
Hanif Mouehla is one such success story. In 2013, Mouehla was admitted to the pediatric intensive care unit at Maria Fareri Children’s Hospital at Westchester Medical Center (WMC), where Dr. Cairo directs the Children and Adolescent Cancer and Blood Diseases Center. The eight-year-old was suffering from acute chest syndrome, with lung damage related to acute sickle-cell anemia. “Every time I went to the doctor,” says Mouehla, “the future looked bleak.”
Historically, patients with sickle-cell anemia had to rely on receiving healthy cells from bone marrow, donated by siblings, to replace their damaged sickle-shaped ones. But only 15 percent of patients’ siblings have genetically compatible or matching tissue, ruling out this option for most—including Mouehla, whose older brothers (a set of twins) were not a genetic match. Attempts to recruit
cells from unrelated donors in a national registry were not successful. Then, Dr. Cairo began to consider another idea: taking marrow cells from a parent donor, or a genetic half-match, and engineering the cells for total compatibility and increased resilience.
In 2014, with Mouehla in an induced coma, Dr. Cairo approached his mother Musa and explained the study he was piloting at WMC. If she donated her bone marrow, he explained, those cells could be genetically enriched to target and destroy the sickle cells that were making her son ill. Mouehla’s mother could give him life— for the second time. She had her bone marrow extracted that summer. Then, in a new procedure called a haploidentical allogeneic stem cell transplant, Musa’s cells were enriched in the Cellular and Tissue Engineering Laboratory (CTEL), an expansive facility within the Children and Adolescent Cancer and Blood Disease Center at WMC. The proprietary method developed by Dr. Cairo’s team deleted potentially dangerous T-cells while enriching the “progenitor cells” that could rally in Mouehla’s body.
“Dr. Cairo has transformed my life tremendously,” says Mouehla, now a student at Harvard University. Although he was too sick to recall their first meeting, “I do remember my mom telling me how much she trusted him. He was focused on his work, but also knew when to be lighthearted and how to lift my spirits.”
In 2024, during a summer research internship in Dr. Cairo’s lab, the former
Developing ‘first in adult, first in child, first in baby’ trials is a point of pride in my career Dr. Cairo “
”
patient analyzed data from patients who had received a haploidentical allogeneic stem cell transplant—the same treatment he had helped to pioneer. He also published the article “Fertility and Sexual Development Outcomes in Pubertal and Post-Pubertal Children and Young Adults after Myeloablative Conditioning (MAC) and Familial Haploidentical T-Cell Depleted Allogeneic Stem-Cell Transplantation” in the American Society of Hematology digital journal, sharing authorship with Dr. Cairo and his colleagues. The abstract was selected by the American Society of Pediatric Hematology and Oncology for presentation at the annual Pediatric Transplantation Cellular Therapy Consortium in Louisville, Kentucky, in May 2025.


“His top priority, from day one, was to save me,” says Mouehla. “It is my dream to follow in his footsteps.”
FINDING VALUE IN HIS “VILLAGE”
“Mentorship has been part of my mantra since the beginning,” says Dr. Cairo, noting that he has trained 26 students at NYMC in his laboratory, and nearly as many junior faculty. “It requires a village, particularly in the field I am in. I am so grateful to have a local, national, and global village. The high point of my career has been to pay it forward, allowing the next generation to populate this field and continue the tradition of translational research.”
This philosophy accords with Dr. Cairo’s conviction that one’s success builds from connections with others. “The key is to surround yourself with extremely bright people and support them.” He has known several of his colleagues for more than 20 years—and two for 45 years.
Yanling Liao, Ph.D., associate professor of pediatrics at NYMC, has worked with Dr. Cairo since 2008 on cord blood stem cell research and transplantation.
“Dr. Cairo has inspired me in multiple ways,” says Dr. Liao. “He has shown me how fulfilling it is to conduct novel research that makes a difference in the lives of patients and their families. He is constantly thinking of innovative ways to enhance research and strives to implement these findings into practice.”
As a mentor and friend, she says, “Dr. Cairo has provided me with full support to explore various research ideas and develop my career path. He has recently led me to the field of immunotherapy, as this is a game changer in treatment of cancer and inflammatory disease.”
Dr. Liao applies immunotherapy research to epidermolysis bullosa (EB), a rare genetic disease that causes fragile and blistered skin.
“Seeing the deep appreciation from Dr. Cairo’s patients and their families has always given me goosebumps,” she says. “When I first meet patients with EB, seeing them layered in bandages and struggling with everyday tasks that most of us take for granted, I am motivated by Dr. Cairo to be an advocate for raising awareness. His example has also strengthened my commitment to do research that could improve the quality of their lives.”
FROM “FIVE PATIENTS, FOUR FUNERALS” TO BRINK OF CURE
Even on the most taxing days, Dr. Cairo draws resolve from looking back on the strides made in his field. “To put it in perspective, when I started practicing in the early 1980s, only 20 percent of children with cancer survived,” says Dr. Cairo. “For every five patients I diagnosed, I attended four funerals. Today, the cure rate is rapidly approaching 85 percent. We have had a great renaissance over the last 50 years, and we are on the brink of developing therapy that’s even more well-tolerated.”


The next challenge is breaking the code for cancers that remain stubbornly resistant to immunotherapy: brain stem tumors, advanced pancreatic cancer, and glioblastoma. “Eventually, we will refine our existing tools to determine the key resistant factors and develop ways to circumvent their mechanisms,” he says. “I believe we will get there. I also believe we will reach our goal of eliminating chemotherapy and radiation in my lifetime.”
KILLER CELLS AS CANCER ASSASSINS
Dr. Cairo is now working with Dr. Liao and other colleagues on several grantsupported initiatives that harness the latest technology in immunotherapy and cellular regeneration.
• A National Cancer Institute grant, part of the Cancer MoonshotSM research initiative, identifies mechanisms of resistance to antibody-based and cell-based immunology in pediatric solid tumors.
• A U.S. Food and Drug Administration grant treats babies with severe congenital cytomegalovirus (CMV) infection, acquired from mothers during pregnancy. Left untreated, babies with CMV risk developing cerebral palsy and intellectual disabilities. This intervention uses the mother’s “memory” CMV T-cells, trained to destroy the CMV she was exposed to. “In the CTEL, we isolate and enrich these T-cells from the mother, and then give them to the baby after birth, via
infusion. We have already treated two babies successfully,” says Dr. Cairo.
• A Department of Defense (DOD) grant supports a new cancer treatment strategy using targeted chimeric antigen receptor (CAR) technology, which deploys killer cells (“K cells”) to seek and destroy acute myeloid leukemia cells. Another DOD grant helps develop antibody-based treatment in patients with acute lymphoblastic lymphoma.
In his downtime, Dr. Cairo may slip on gym shorts and sneakers to play a round of basketball for the Pediatric Cancer Research Foundation, which he founded in 1982 and has raised more than $46 million to date. But as an avid Deadhead, he’s just as likely to don tie-dyed shirts with dancing bears. “I became a Grateful Dead fan in 1969, and have enjoyed too
many concerts to recall,” he says. He continues to support their current lineup, Dead & Company, attending eight shows last year alone.
His family remains his foundation. “My wife and I have been together for more than 52 years, and I could never have accomplished what I have done without her total support in every area,” he says. His two sons, daughter-in-law, and toddler grandson also affirm his resolve to strengthen families by saving lives.
Dr. Liao recalls the day Dr. Cairo read her an email from a former patient, his voice shaking with emotion. “The patient expressed profound gratitude, thanking him for giving him the chance to live and have a family.” Through tears, Dr. Cairo told her: “This is why I do what I do.” ■
“ ”
I believe that taking to the bedside a breakthrough in the lab or learning something at the bedside to bring back to the bench, is the ultimate goal in being a physician-scientist. Dr. Cairo


BY NICHOLAS WEBB, M.S.I.S.
The year 2025 marks two milestone anniversaries: the 165th anniversary of New York Medical College (NYMC), and the 150 th anniversary of NYC Health + Hospitals/Metropolitan. These two institutions have been affiliated since the founding of Metropolitan in 1875, making the affiliation between NYMC and Metropolitan the longest affiliation between a medical school and a municipal public hospital in American medicine.
The roots of NYMC began in 1860, when the New York State Legislature granted a charter to “The Homeopathic Medical College of the State of New York, in New York City.” The College was established by a group of physicians and philanthropists led by poet and editor William Cullen Bryant, who chaired the College’s Board of Trustees from 1862 to 1872, and surgeon Jacob Beakley, A.M., M.D., the founding dean.
Homeopathy, a system of medicine established by German physician Samuel Hahnemann, M.D., was considered a legitimate rival to mainstream
allopathic medicine during the midnineteenth century. Physicians educated in traditional medical schools were taught to cure disease by balancing their patient’s humors through aggressive bloodletting and purging. While the theory underlying homeopathy is now known to be unscientific, its therapeutic regimen of herbal remedies in small doses often led to superior clinical outcomes than traditional practice. By 1860, the new medical doctrine had made many prominent converts among New York City physicians who had received their M.D.s from the city’s allopathic medical schools.
CELEBRATING NYMC AND METROPOLITAN HOSPITAL: 165 Years of Education and 150 Years of Care
The Historic Affiliation and Tradition of Excellence Hits its Sesquicentennial

THE FOUNDING OF MET
New York City’s municipal hospital system, however, was closed to homeopaths. Faculty from the city’s allopathic medical schools could receive staff appointments and teach students at Bellevue and the other city hospitals. Homeopathic physicians, whose patients included many of the city’s most prominent citizens, could not. In spring 1875, a group of homeopaths, comprising mostly of NYMC faculty, petitioned the city government to open a homeopathic municipal hospital. In September of that year, the Ward’s Island Homeopathic
Hospital, predecessor of the modern Metropolitan Hospital, opened to patients.
Not long after the opening of the hospital, medicine changed dramatically. The scientific and clinical advances of the 1880s, including the germ theory of disease and the widespread adoption of antiseptic surgery, laid the groundwork for modern medicine as we know it today. On the staff of the Ward’s Island Homeopathic Hospital and the faculty of what was then known as the New York Homeopathic Medical College, fierce battles were fought between adherents of traditional homeopathy and physicians
who wanted to adopt and teach the new scientific medicine. Longtime medical board chair Egbert Guernsey, M.D., and secretary Alfred K. Hills, M.D., successfully resisted an attempt by their professional rivals to have the New York City mayor dismiss the medical board and replace them with orthodox homeopaths. Dr. Hills soon became the first homeopathic M.D. to be named a fellow of the New York Academy of Medicine, which had been founded in 1847 for the explicit purpose of defending allopathic medicine against homeopathy.
RELOCATION AND EVOLUTION
In 1894, the hospital relocated to Roosevelt Island. Its new facilities had previously been the home of the New York City Lunatic Asylum, which had been shut down by the city when investigative reporter Nellie Bly, published a widely circulated expose of its inhumane practices. During the move to Roosevelt Island the word “homeopathic” was dropped from the hospital’s name and it was renamed the Metropolitan Hospital. It has been known by variations of this name ever since.
Teaching at NYMC also kept pace with developments in scientific medicine. By the 1890s the College had established a basic science faculty whose members held Ph.D.s rather than M.D.s. The firstyear Class of 1894 was the first cohort of students to follow a mandatory four-year curriculum with two years of laboratory work and two years of clinical rotations. Along with the Flower Hospital, which was the College’s teaching hospital in Manhattan, Metropolitan became the primary location of NYMC’s clinical clerkships. Alumni of the College often joined the house staff at Metropolitan as interns after receiving their M.D. degrees. Some of them spent their careers at Metropolitan, rising to become attending staff and department chairs.
By World War I, Metropolitan had become one of the biggest municipal hospitals in New York City. The fresh air of Roosevelt Island made Metropolitan the ideal home of the city’s municipal ward for tuberculosis patients. For many years, the hospital had the largest tuberculosis ward in the United States. In the 1920s, the last vestiges of homeopathy were dropped from the College’s teaching curriculum and from clinical practice at Metropolitan. The association between the two institutions continued, however. In 1929, New York City replaced the ad hoc governance structures of the rapidly growing municipal hospital system with a centralized Department of Hospitals, the predecessor of the modern Health + Hospitals Corporation. During this change, city officials assured the trustees of the College that the close association between the College and Metropolitan would remain unbroken.

During the Great Depression and World War II, both the College and Metropolitan continued to expand and modernize. The tuberculosis ward at Metropolitan was rendered obsolete by the discovery of antibiotics, and in 1955 the hospital relocated from Roosevelt Island to its current location on 98th Street in East Harlem, bringing it even closer to NYMC, which was then located at Flower-Fifth Avenue Hospital on 106th Street.
In the second half of the 20 th century, NYMC was particularly distinguished by its psychiatry faculty, led from 1960 to 1988 by psychiatrist and social activist Alfred M. Freedman, M.D. At Metropolitan, the creation of an inpatient psychiatric wing in 1961 was the beginning of a significant history as a center of mental health care for one of the city’s most underserved communities. In the 1960s, Metropolitan’s psychiatry facilities became the first designated Community Mental Health Center in New York State. Under the leadership of Phyllis Harrison-Ross, M.D., longtime chair of the hospital’s Department of Psychiatry, Metropolitan pioneered the development of culturally competent psychiatric care to serve its diverse community of Black and Hispanic patients in East Harlem.
THE NYMC-MET AFFILIATION ENDURES
The relocation of NYMC to Westchester County in 1972 did not interrupt the affiliation of the two storied institutions. The New York City fiscal crisis of the 1970s was a challenging time for the municipal hospital system, and many hospitals serving under-resourced communities in upper Manhattan and the Bronx were shut down due to budget cuts. At Metropolitan, however, a unique coalition of faculty, house staff, and East Harlem community members united to keep the hospital open during these troubled years.
Although medicine has evolved dramatically since the founding of Ward’s Island Homeopathic Hospital, the commitment of Metropolitan Hospital’s staff and NYMC’s faculty and students to medical excellence remains steadfast. Today, as a part of Touro University, NYMC remains a center of excellence in medical education for New York City and its surrounding communities, and Metropolitan Hospital remains an important center of care for the population of upper Manhattan. Their historic affiliation continues to play a vital role in shaping the future of healthcare. ■
BUILDING A LEGACY IN SURGERY AT METROPOLITAN: Marc
K. Wallack, M.D., and the General Surgery Residency
Training Program
The relationship between New York Medical College (NYMC) and NYC Health + Hospitals/Metropolitan entered a new era in 2012 with the launch of the NYMC at Metropolitan Hospital Center (MHC) General Surgery Residency Training Program, the first new general surgery residency to be established in New York City in more than 50 years.
Under the leadership of Marc K. Wallack, M.D., chair of surgery at Metropolitan and professor of surgery at NYMC, the residency training program has grown from humble beginnings to become a desirable residency program that attracts motivated residents from throughout the United States and internationally. In a rare feat, the College-sponsored graduate medical education program in general surgery was approved by the Accreditation Council for Graduate Medical Education based on its very first application with no revisions necessary and was accredited with commendation.
Dr. Wallack’s first order of business was to recruit a teaching faculty. Drawing on the network he had built as chair of surgery at St. Vincent’s Catholic Medical Centers, he recruited a staff of full- and part-time faculty to Metropolitan. To provide a complete course of surgical training to residents, he brokered agreements for specialty training with other Manhattan hospitals.
“New York,” he explains, “has become my campus.”

together to develop an academic program,” Dr. Wallack explains. “If we did not have students, it would not be the same.” For many NYMC students, a rotation at Metropolitan is their first experience of clinical surgery, and the program works closely with clerkship students to get feedback on resident teaching. Many NYMC graduates apply to the residency program after completing their M.D. degrees, and some have gone on to become full-time faculty. “It has been an honor,” says Dr. Wallack, “to do this with New York Medical College.”
“
” You need students and residents together to develop an academic program. It has been an honor, to do this with New York Medical College. Dr. Wallack
The affiliation between Metropolitan and Memorial Sloan Kettering Cancer Center was a particularly important step for the program, by providing Metropolitan residents the opportunity for both clinical training and laboratory research experience in cutting-edge surgical oncology.
Metropolitan’s status as a New York City municipal hospital attracts talented residents. “You need students and residents
In 2024, Dr. Wallack was accepted into membership in the American College of Surgeons Academy of Master Surgeon Educators® for his leadership role in advancing the science and practice of education across all surgical specialties, promoting the highest achievements in the lifetime of surgeons. Individuals are selected following a stringent peer-review process and those selected have consistently demonstrated the highest levels of leadership and excellence in surgical education. Dr. Wallack’s long distinguished career as a surgical educator and researcher has also earned him numerous grants from the National Institutes of Health, and induction into the prestigious Robert Goldstein Society, an honor reserved for faculty who have been honored with NYMC Excellence in Teaching Awards for more than ten years. He served as the principal investigator of the first randomized double-blind multiinstitutional FDA-approved melanoma vaccine trial in the world developed and funded by the National Cancer Institute and served for more than 30 years as a board member of the Association of Program Directors in Surgery, including a term as president. ■
A Gift That Shapes the Future of Medicine
NYMC Dedicates The Norman E. Alexander Family M Foundation Medical Education Center Plaza

BY KIARA THOMAS, M.A.
The Medical Education Center Plaza at New York Medical College (NYMC) has officially been named The Norman E. Alexander Family M Foundation Medical Education Center Plaza following the foundation’s $3 million endowment to fund scholarships for medical students pursuing internal medicine. NYMC community members gathered on March 19, 2025, for the dedication ceremony, where Mark Alexander, M.D. '77, an NYMC alumnus and president of the foundation, dedicated the plaza to his late father, Norman E. Alexander, a distinguished businessman, philanthropist and former president of the NYMC Board of Trustees.
“ ” Occasionally, one encounters someone who truly exemplifies the idea that personal success comes with a responsibility to others, society, and the organizations that shaped them. Dr. Kadish
“My late father had a lifelong ferocious appetite for knowledge and education, and not just in business at which he excelled, but almost in any subject that even serendipitously came within a whisper of his attention,” said Dr. Alexander. “He was driven to understand it and then push the needle forward for the betterment of all.”
Starting next year, The Norman E. Alexander Family M Foundation Scholarship will be awarded to graduating medical students with financial need and strong academic standing who have matched in general internal medicine and demonstrate a sincere commitment to pursuing primary care/internal medicine. The scholarship aims to make primary care more accessible by reducing financial barriers for medical students.
“Occasionally, one encounters someone who truly exemplifies the idea that personal success comes with a responsibility to others, society, and the organizations that shaped them,” said Alan Kadish, M.D., president of NYMC and Touro University.
“Few exemplify this better than Dr. Alexander. When I first met him, he spoke eloquently about how a series of what he called 'accidents,' but I’d call talent, put him in a position to give back. In recent years, he has generously donated to organizations that advance scientific research, serve society, and help others. In that spirit, he has made an extraordinary gift to NYMC to support scholarships for students pursuing internal medicine, which he considers a great human calling.”

Since 2001, the plaza has been a cherished gathering place for numerous College events and celebrations. It has served as a vibrant backdrop for the annual Match Day celebration, where medical students excitedly receive their residency match results, marking the next step in their medical careers. The plaza comes alive with joy as confetti cannons and balloons fill the air, symbolizing this significant milestone. Now, it will stand as a tribute to Alexander, a graduate of Columbia University and Columbia Law School, who built a 70-year career in business, including serving as the executive chair of Sequa Corporation, a $2 billion conglomerate he led for nearly 50 years.
Addressing Dr. Alexander, Edward C. Halperin, M.D., M.A., chancellor and chief executive officer of NYMC, said, “Dr. Alexander, the most important thing we do at NYMC is to welcome young people to the community of scholars for the generation and dissemination and conservation of knowledge about the causes of prevention of human disease and disability. The most important thing we do is try to make medical care better for our grandchildren than it is for us. The most important thing we do is try to predict the future of medicine by inventing it ourselves. We are very grateful for the gift.”
A staunch supporter of academic, Jewish, and other philanthropic causes, Alexander served as a member of the Board of Visitors of Columbia Law School and of the Board of Columbia/Barnard Hillel, where his commitment to the Jewish community led to the
establishment of the Alexander Program Center for Jewish Life. In recognition of his exceptional service, Alexander was awarded Columbia University’s John Jay Award in 1985.
A lifelong advocate for Jewish culture, he was a patron and trustee of The Jewish Museum, as well as a governor and vice president of the American Jewish Committee. He was a longstanding member of the publication committee of Commentary Magazine, a founding member of the board of The Jewish Week, and a major supporter of UJA-Federation, Temple Kol Ami in White Plains, New York, and supporter of the Jewish Publication Society.
Alexander was a founding board member of the Albert Einstein Medical College and played a significant role in the health care sector, serving on the boards of Bronx Lebanon Hospital and as president of the NYMC Board of Trustees from 1976 to 1979. His legacy in business and philanthropy leaves an indelible mark on the institutions and communities he supported throughout his life.
Influenced by his father’s leadership and service, Dr. Alexander, a physician with a successful career spanning medicine, business, and philanthropy, has been an active supporter of the Weizmann Institute of Science and numerous other causes, particularly in the sciences and the arts. After graduating NYMC, Dr. Alexander completed his internal medicine training at Brown University before embarking on a professional career that included private practice and serving as vice president and medical director for Metropolitan Life Insurance Company.
With the establishment of The Norman E. Alexander Family M Foundation Scholarship, Dr. Alexander ensures that future generations of medical students will be supported to enter the field of internal medicine and become leaders in the field. The plaza’s renaming serves as a lasting tribute to his father’s values of leadership and learning, reinforcing the College’s mission to train compassionate, skilled physicians who will carry forward the legacy of service and excellence exemplified by the Alexander family. ■


A Legacy of Giving: Endowed Scholarships at NYMC
BY BARBARA MOROCH
In the realm of higher education, endowed scholarships play a pivotal role in shaping the lives of students, particularly within the health sciences fields. By fostering a culture of support and commitment, endowed scholarships serve as a bridge to opportunity, easing the financial burdens associated with higher education.
Endowed scholarships represent a long-term commitment to making higher education in the health sciences accessible. “Endowed scholarships ease the financial burden for many colleges and universities and are often a factor when students are considering further studies,” says Anthony M. Sozzo, M.A.,
M.S.Ed., associate dean for student affairs and director of student financial planning and student activities. This commitment not only supports currently enrolled students but also ensures that future students have the opportunity to pursue a health sciences education. He has witnessed the impact of the scholarships firsthand as he has counseled multiple generations of students during his more than 40 years at New York Medical College (NYMC). “It is always rewarding for me to see the gratitude and appreciation of the students who are the recipients of the scholarships,” says Sozzo. “They feel a connection to the donor and experience quite a sense of relief that their debt will be lessened,” says Sozzo.
At NYMC, endowed scholarships contribute significantly to the institution's efforts to reduce student debt. Each year, NYMC awards more than $10.3 million in scholarship funds to students exhibiting both academic promise and financial need. This initiative helps deserving students manage their educational costs and focus on their academic journeys, aligning with NYMC's goal of fostering a lasting legacy of educational support.
Those interested in establishing an endowed scholarship at NYMC can follow a structured process working with the Office of Development and Alumni Relations. The minimum donation required to establish a fund is $25,000,
Honoring Alumni, Inspiring Future Generations, and Advancing Education and Research Through Endowed Giving

and the parameters for scholarships can be tailored to reflect the donor's values.
To ensure that scholarship criteria align with donor values, NYMC actively engages in communication with potential donors. By tailoring scholarships to specific fields of study or demographics, NYMC ensures that the donor's vision is respected and upheld.
ENGAGING DONORS AND ALUMNI
NYMC fosters engagement between donors and scholarship recipients through various events. “We actively engage our alumni throughout the year by hosting special events such
as our annual Golf Outing, Founder’s Dinner, and Homecoming,” says Bernadette Bauer, manager of alumni engagement. These opportunities not only allow alumni to reconnect but also enable them to meet current scholarship recipients, strengthening the bond between past and present members of the NYMC community.
For those considering establishing an endowed scholarship, Sozzo has one important piece of advice: “Think about the impact you want to make and what it would have meant to you if given that opportunity when you were a student.” By focusing on the potential impact on others, donors can better envision their
contributions and the positive change they can create through their generosity.
“Endowed scholarships are a lifeline for students in the health professions. They not only ease the burden of education costs but also fuel the next generation of compassionate caregivers, innovative researchers, and public health leaders who will shape the future,” says Sozzo.
A LASTING TRIBUTE:
THE AVINASH
In 2023, the Agarwal family established the Avinash Agarwal, M.D., Scholarship Fund at NYMC to honor the legacy of Avinash Agarwal, M.D. ’99, a dedicated transplant surgeon and researcher. Dr. Avinash Agarwal’s contributions to transplant surgery and his commitment to improving patient outcomes continue to inspire those who knew him, and this scholarship reflects his family’s deep ties to NYMC.
Dr. Avinash Agarwal’s connection to NYMC began in the mid-1970s, when his father, Nanakram Agarwal, M.D, arrived in New York to start a surgery residency sponsored by NYMC. “NYMC has been the foundation of our medical careers,” says Ritu Agarwal, M.D., Avinash’s sister, reflecting on how the school helped her family navigate their new life in the U.S. Growing up, she and Dr. Avinash Agarwal developed their early interest in science. Dr. Avinash Agarwal’s research in cartilage regeneration, under Stuart A. Newman, Ph.D., professor of cell biology and anatomy and of medicine, sparked his passion for medical research and led to his future as a transplant surgeon. “His pride in being an alum inspired us to create this scholarship,” Dr. Ritu Agarwal shares.
She remembers how her brother always strove for excellence. “He expected the best from those around him,” she
AGARWAL,
M.D. ’99, SCHOLARSHIP FUND
says. His dedication to his patients was matched by his pursuit of groundbreaking research that improved transplant outcomes, reduced immunosuppression effects, and enhanced organ preservation. “He led national efforts to raise awareness about organ donation and transplantation,” she reflects. Throughout his career, Dr. Avinash Agarwal saved 793 lives by recovering more than 800 organs.
Through the scholarship fund, the Agarwal family aims to inspire future medical students to pursue research and innovation. “Research fosters independent thinking and better patient outcomes,” Dr. Nanakram Agarwal explains. They envision the fund supporting students who will contribute to advancements in medicine, just as Dr. Avinash Agarwal did.
The scholarship will provide NYMC students with opportunities to engage in basic science research, build selfconfidence, and prepare for careers in medicine and academia. “We hope to see students who are passionate about solving complex health care problems,” Dr. Nanakram Agarwal adds.
One of the most rewarding moments for Dr. Nanakram Agarwal was watching the first scholarship recipient, Rebecca Kann, SOM Class of 2026, present her research at an international meeting in Vienna.

“It was an incredibly proud moment,” he says. “We hope this scholarship inspires young medical students to pursue their passion for research.”
“I am extremely grateful to be the inaugural recipient of the Avinash Agarwal, M.D., ’99 Scholarship. This generous support allowed me to present my research, “The Role of Interleukin-1 Driven Inflammation in Recessive Dystrophic Epidermolysis Bullosa,” at the Inflammatory Skin Disease Summit in Vienna, Austria, in November 2023,” says Kann. “Sharing my work at an international conference was an invaluable opportunity to engage with experts in the field, gain new insights, and further my passion for dermatologic research. I deeply appreciate this award’s role in advancing my academic and professional growth.”
Ultimately, the scholarship aims to foster a new generation of researchers and physicians who embody the qualities that defined Dr. Avinash Agarwal’s legacy: excellence, empathy, and a commitment to improving patient care. Through this fund, his impact will continue to resonate for years to come.


HONORING A LEGACY: THE WILSON YOUNG, M.D., PH.D., ENDOWED SCHOLARSHIP FUND
In memory of Wilson Young, M.D. ’07, Ph.D. ’07, M.S. ’99, who passed away in 2022 at the age of 49, his family established the Wilson Young, M.D., Ph.D., Endowed Scholarship Fund at NYMC to honor his impact on medicine and research. Originally from Harlem and raised in Scarsdale, New York, Dr. Young was a dedicated physician and researcher, earning his master’s, medical degree, and doctorate in pharmacology from NYMC. His commitment to the intersection of medical practice and science inspired this scholarship, aimed at preserving his legacy at NYMC.
“Wilson taught us all the importance of asking questions and to continue to be engaged in learning,” said Bonnie Young, Dr. Young’s wife. “He taught his children and me that we could do anything if we worked hard.” His dedication to his patients and his role as a mentor left a lasting impression on many, including their young children, Emma and Theodore. Young recalls, “He treated patients until he physically couldn’t.”
The scholarship seeks to support aspiring medical students who embody the values Dr. Young held dear: dedication, innovation, and a passion for clinical research. Young hopes that recipients will carry forward his legacy.
For Young, creating this scholarship is a way to ensure that Dr. Young’s contributions to science and humanity are remembered. She expresses, “It gives me peace knowing that his children will know how much impact he had on his community during his lifetime and after he passed away.” Through this enduring tribute, she hopes future students will help others live healthier lives, saying, “...one day, maybe a father or a mother will be able to see their children grow up... where at one time, it would not have thought to be possible otherwise.” Dr. Young’s spirit will continue to inspire new generations of health professionals, ensuring that his legacy lives on. ■

Creating an Endowed Scholarship at NYMC
To establish an endowed scholarship at NYMC, please contact the Office of Development and Alumni Relations at development@nymc.edu or call (914) 594-2720 to discuss your interest.
Your one-time donation will be invested to generate ongoing funds for future scholarship awards, and you can specify criteria for selecting recipients based on factors like academic merit, financial need, or specific areas of study.
FACULTY SPOTLIGHT
SRIHARI
S.
NAIDU, M.D., FACP, FACC, FAHA, FSCAI,
Pushing the Boundaries in Treating Cardiovascular Disease
BY KIARA THOMAS, M.A.
“To be a true expert, one must master not only the practice, but also the art of teaching and publishing on a subject,” says Srihari S. Naidu, M.D., FACP, FACC, FAHA, FSCAI, professor of medicine and renowned interventional cardiologist. He does all three and has cultivated his expertise in hypertrophic cardiomyopathy (HCM) and cardiogenic shock for decades, garnering worldwide recognition for his part in advancing the clinical practice and understanding of these complex diseases.
Dr. Naidu’s interest in these conditions stems from their complexity and prevalence. HCM is one of the most common inherited cardiovascular disorders, where pumping blood from the heart is difficult due to a thickened heart muscle. The disease, which can cause sudden cardiac arrest in athletes and increases the risk of heart failure as patients age, affects one in 500 people in the United States, with a large percentage of people undiagnosed or diagnosed in middle age, according to the American Heart Association. Similarly, cardiogenic shock, the most severe type of heart failure when the heart is unable to deliver sufficient blood and oxygen to the body, poses a life-threatening challenge. Fifteen years ago, there was not much interest in the diseases, but now they are among the most important topics in the field. Early in Dr. Naidu’s career, he became trained in a rare procedure called alcohol septal ablation to treat HCM and started getting patient referrals from other physicians and health care networks. Since 2014, each year he teaches the procedure to other physicians from around the world at his in-person proctoring course at Corewell Health William Beaumont University Hospital in Michigan. Dr. Naidu serves as the system director of the Cardiac Catheterization Laboratories and director of one of the largest HCM programs in the nation at Westchester Medical Center, with more than 2,500 patients. “Over the years, I have become good at seeing where the field of cardiology is going and preparing myself,” he says. “By doing that, you are ahead of the curve.”
Following in his parents’ footsteps, Dr. Naidu witnessed their dedication to their patients and believes it to be the cornerstone of his clinical practice. His late mother Saraswathi Naidu, M.D., was a nephrologist and his late father Sriram Naidu, M.D., former assistant professor of medicine at New York Medical College, headed the first cardiac catheterization lab at Flower Fifth Avenue Hospital, and was among the first cardiologists to perform cardiac catheterizations on a large scale in the 1970s. Seeing the impact his father had on his patients, colleagues and the field of cardiology, Dr. Naidu continuously finds ways to push the boundaries of what is possible.
In 2019, Dr. Naidu chaired a team of 15 cardiologists from the Society for Cardiovascular Angiography and Interventions (SCAI), who created and published a consensus statement on a universal classification of cardiogenic shock with an updated statement in 2022. The 2019 publication was endorsed by the American College of Cardiology, American Heart Association, Society of Critical Care Medicine, and Society of Thoracic Surgeons, with the American College of Emergency Physicians, European Society of Cardiology and the International Society for Heart and Lung Transplantation signing on in 2022. The change was well-received by physicians around the world who adapted the definition rapidly and now have a universal language to communicate about the disease and the treatment of it.
“If you do one thing, such as publish one publication, you can change the entire world and move the survival rate from 50 percent to 70 or 80 percent, which affects the lives of millions of people,” says Dr. Naidu. “You can make big differences when you do small things at a big level.”
Dr. Naidu worked with the American College of Cardiology, the Cardiovascular Research Foundation, and SCAI to found the Emerging Leader Mentorship Program in 2011, which recruits top interventional cardiologists into the national societies for leadership roles early in their careers.

A decade later, these individuals have gone on to lead the field and push the boundaries of cardiovascular care globally.
President of SCAI and founding board member of the Hypertrophic Cardiomyopathy Medical Society, Dr. Naidu also uses his platform on X, formerly Twitter, to raise awareness, advocate for patient care and answer questions of his more than 12,000 followers. In 2024, he published a children’s book with Lindsay Davis, former Miss Ohio 2011 and eponym of “Lindsay’s Law,” who is living with HCM, titled Lindsay’s Big Heart, to educate on HCM and sudden cardiac arrest prevention in children. Dr. Naidu’s commitment to raising awareness and educating others reflects his broader vision for making a lasting impact in cardiology.
“It took me a while to realize I could be a leader, more than just a doctor,” says Dr. Naidu. “I went from wanting to be a doctor to a good doctor to a cardiologist and finally to a cardiologist using whatever platform and ideas I may have to really push the envelope. I am at the stage of my life where I am always looking to do more to move the field of cardiology forward and help the next generation do the same. Indeed, there is a circle of life even within academia, and it is nice to feel like I am doing my part.” ■
AINSLEY ROSSI,
D.P.T., PT, OCS,
Shares Her Global Path in Physical Therapy
BY CARA GILEAU
Hailing from Australia, Ainsley Rossi, D.P.T., PT, OCS, assistant professor of physical therapy in the School of Health Sciences and Practice, started her academic journey at the University of Queensland, where she studied physical therapy, and loved the idea of helping people move better, feel better, and live better. After graduating, she moved to the United Kingdom, where she spent five years as a physical therapist. During this time, Dr. Rossi traveled every few months and enjoyed taking her work to different parts of the world, while also taking additional courses to strengthen her skillset. It was during this time that she began to specialize in orthopedic physical therapy, before moving to the United States.
After relocating, Dr. Rossi considered whether to explore an entirely new career, as she needed to pass the necessary board exams to become licensed in the U.S. As much as she liked the idea of starting over and focusing on a completely new path, she stayed loyal to the field of physical therapy and enjoyed witnessing the transformative progress in her patients’ health, which made it all worthwhile.
Dr. Rossi took an interest in shadowing professors at The State University of New York University at Buffalo while volunteering in a clinical setting, a step that eventually led her to her decision to enter academia. She became an American Physical Therapy Association-credentialed instructor and relished combining her love of physical therapy with the rewarding experience of educating the next generation in her first academic role. Dr. Rossi’s journey as an educator took her to Atlanta, Georgia, teaching at Emory University. While still practicing parttime, she also took on the role of clinical instructor, finding fulfillment in helping students learn and grow through handson experiences.
Dr. Rossi’s next stop was back to the northeast, teaching at Quinnipiac University in Hamden, Connecticut, for nearly five years before starting her role in August 2024, at New York Medical College (NYMC). “It has been a journey, but it has been fun,” she says. “Each move has had that moment where I was able to stop, look around, and be intentional about where I go next.” Dr. Rossi enjoys teaching the foundational courses in physical therapy at NYMC, as well as orthopedics. She is deeply invested in understanding how students internalize and apply the knowledge they gain— particularly those who have engaged in clinical experiences. With a renewed focus on psychomotor skill development in physical therapy education, she aims to become a more well-rounded professor. Rather than immersing herself solely in teaching and clinical work, she is choosing to preserve space for scholarship and professional growth.
Dr. Rossi’s time at NYMC has been incredibly rewarding, and she is taking time to enjoy the transition as she builds relationships with the faculty and students. “I love the students. They are phenomenal,” she says. “They come from all over and have such a great sense of the world. I think I learn more from them than they learn from me.” But the learning doesn’t stop with her students. Dr. Rossi also finds mentorship and motivation among her colleagues. “Everyone is extremely kind,” she says. “It is uplifting to be part of an institution with such a positive atmosphere. I can see how that positive energy flows directly into the classroom.”
When asked what advice she would offer to new faculty members, Dr. Rossi highlights the importance of listening and learning. Dr. Rossi believes new faculty can learn a great deal by taking time to observe and understand the interpersonal

rhythms of their department. Although every individual brings unique talents, understanding the flow and function of the existing team is essential for building strong, collaborative relationships.
Looking ahead, Dr. Rossi is particularly excited about the new curriculum in the Division of Physical Therapy. The opportunity to help influence its development in thoughtful and purposeful ways is one she welcomes. Beyond curriculum development, she also plans on returning to research and focusing on interprofessional education. She will commence coursework for her Doctor of Education degree this summer, with plans to further pursue the many opportunities for developing interprofessional educational experiences available at NYMC.
Whether it is taking a new step in her own life or helping patients take theirs, Dr. Rossi is excited for what’s to come. ■
FACULTY SPOTLIGHT
CHRISTOPHER WHITEHURST,
PH.D.,
Cracking the Code of EBV
BY RHEA HIRSHMAN
The Epstein-Barr virus (EBV) is ubiquitous. A human tumor virus of the Herpesviridae family, EBV infects more than 90 percent of the world's population. While generally asymptomatic, it can have serious consequences if reactivated—a challenge that Christopher Whitehurst, Ph.D., assistant professor of pathology, microbiology, and immunology, as well as biochemistry and molecular biology, is addressing through his research.
Usually acquired in childhood through normal interactions including playing with friends, kissing a parent, EBV, one of nine known human herpes viruses, may present as a slight cold or EBV acquired in adolescence can cause infectious mononucleosis.
Once acquired, EBV remains latent in the body for a lifetime, never completely cleared by the immune system. Most people never know they carry it and there is currently no effective treatment for it. However, if it is reactivated by factors such as prolonged stress, hormonal changes, or other infections, it can become the driving factor for a variety of cancers — including Hodgkin’s lymphoma, Burkitt’s lymphoma and nasopharyngeal (head and neck) carcinoma. Linkages have been found between EBV and multiple sclerosis, and those who have or have had malaria are even more likely to develop lymphoma from EBV. EBV is also implicated in posttransplant lymphoproliferative disorders –cancers of the lymphatic system.
“Transplants require immune suppression,” explains Dr. Whitehurst, “and this suppression can allow the Epstein-Barr virus to reactivate and cause problems.”
A member of the New York Medical College (NYMC) faculty since 2021, Dr. Whitehurst currently focuses his research on EBV. More specifically, his lab has been working with an enzyme called BPLF1, one of about 90 proteins that the virus encodes for. “If you knock out, or inactivate, this protein, you reduce EBV infectivity by approximately 90 percent,” he says. “Also, inactivating BPLF1 impedes the capacity of
cells to morph into cancer cells, decreasing the risk of developing malignancies.”
Dr. Whitehurst, who received his undergraduate degree in biochemistry from Clemson University, his master’s in chemistry from the University of Wisconsin, and his Ph.D. in biochemistry from North Carolina State University, first encountered BPLF1 during his postdoctoral fellowship at the University of North Carolina (UNC) at Chapel Hill. “BPLF1 and its relationship to the EpsteinBarr virus were just being discovered when I was interviewing at UNC,” he says, “and I was intrigued.” Instead of the project he originally applied for, he was able to turn his attention to BPLF1, moving into positions at UNC as research associate and then research assistant professor.
Now, supported by a grant from the National Institute of Allergy and Infectious Diseases, Dr. Whitehurst’s lab is testing the efficacy of thousands of commercially available compounds that might have the potential to inhibit BPLF1, thereby reducing EBV replication. Downstream, they will test the most promising substances for toxicity in animal models. The eventual goal is the development of therapeutics to target the full range of EBV-triggered diseases.
Dr. Whitehurst teaches in both the School of Medicine and in the Graduate School of Biomedical Sciences, lecturing primarily on microbiology, biochemistry, and virology (particularly the herpes viruses). But, he says, his favorite place to teach is in his own lab. “I especially love teaching lab techniques and then watching my students figuring out how to run with those techniques on their own.”
Along with many of his colleagues, Dr. Whitehurst also welcomes into his lab local high school students, who have access to internships and other research opportunities offered throughout New York State. Last year, under his mentorship, a high school student conducted a study of the increased incidence of EBV reactivation in COVID-19
patients and published the results, as first author, in the journal Virus Research . “These students do amazing work,” Dr. Whitehurst says. “I love when they let me know about how they did in science fairs, or which college they will be attending, or how their research is going. I hope I have given them many of the tools they need to continue their own scientific journeys.
Collaborating with his colleague Paul M. Arnaboldi, Ph.D., assistant professor of pathology, microbiology and immunology, Dr. Whitehurst is also looking at potential connections between EBV and Lyme disease. “Many people with persistent Lyme disease have symptoms similar to those in someone with mono,” he says, “so we are looking at whether reactivated EBV might be involved.” He is also collaborating with Xiu-Min Li, M.D., M.S., M.P.H. ’24, professor of pathology, microbiology and immunology, and of otolaryngology, who helped develop a nanoparticle that allows for more efficient medication delivery, in an exploration of the nanoparticle’s potential for eventual treatment of EBV.
“The more I learn, the more I realize there is to learn,” Dr. Whitehurst says. “With enthusiastic students and generous and accessible colleagues here at the college, I look forward to continuing and expanding on my research.” ■
ALUMNI Lighting the Way at NYMC
At New York Medical College (NYMC), the journey from student to faculty member is a testament to the enduring bond between the institution and its graduates. Many of our esteemed faculty members once walked these same halls as students, before returning to share their knowledge, expertise,




Martin Katzenstein, M.D. ’78
and experience with the next generation. These alumni, having experienced firsthand the transformative power of an NYMC education, are now shaping the future of health care by mentoring and inspiring new waves of medical professionals and researchers. ■
Chair of NYMC Board of Advisors, Assistant Dean for Clinical Affiliations, and Associate Professor of Pediatrics
As a prospective medical student, I was drawn to Flower Fifth Avenue Hospital, NYMC’s primary teaching hospital, now known as Terrance Cardinal Cooke Health Care Center, because of its well-respected reputation for its clerkship program. The clinical departments, particularly obstetrics and psychiatry, and their respective professors were nationally renowned. Today, the hospital continues to serve as a clinical site and hospital affiliate of the NYMC School of Medicine.
After my pediatric training from NewYork-Presbyterian Hospital/ Weill Cornell Medical Center, I had the opportunity to be part of the newly established Westchester Medical Center (WMC) and to be part of a team with the late Edward Wasserman, M.D.,
Victor G. Garcia, Ph.D. ’15
Associate Professor of Pharmacology
As a master’s student at the University of Medicine and Dentistry of New Jersey, I became deeply interested in stem cell biology and pharmacology. This passion led me to NYMC’s Integrated Ph.D. Program, which was particularly exciting because it allows students to participate in several lab rotations, providing valuable insight and perspective into different fields and labs they may want to pursue. The rotations deepened my interest in science, and I had the immense honor of ultimately joining the Department of Pharmacology for my Ph.D. training.
During my Ph.D. training, I had the incredible opportunity to identify the receptor for the proinflammatory lipid 20HETE, known as GPR75, with Michal L. Schwartzman, Ph.D.,
Nkem Chukwueme, M.D., M.P.H., Dr.P.H. ’23
Adjunct Assistant Professor of Public Health
My passion for success, desire for a flexible program, and admiration for the work of NYMC and its affiliations on tuberculosis research in the past led me to NYMC. I was also drawn by conversations I had with the faculty chair during my interview, who suggested potential opportunities for hands-on experience in research and teaching assistance, which are both indications of a supportive community and faculty. The rigorous training I received, combined with a supportive environment, helped me redefine my leadership skills and chart new opportunities for career growth and mentorship support within a large community.
Returning to NYMC as a professor was unexpected, unplanned, and spontaneously recommended by the dissertation team after
professor emeritus of pediatrics and former chair of pediatrics; the late Harry Dweck, M.D., former professor of pediatrics and director of neonatology at WMC; and Leonard J. Newman, M.D. ’70, former chair of the Department of Pediatrics. I was honored to care for newborns under their tutelage. In medical school, we were taught to be passionate about our patients as well as our community. I was influenced to give back to the medical school that educated me, which guided me to establish, along with Alan Kadish, M.D., NYMC and Touro University president, the NYMC Board of Advisors, which has helped finance many medical school academic activities and launch the annual Golf Tournament at Saint Andrew’s Golf Course.
professor of pharmacology and medicine, associate professor of ophthalmology, chair of pharmacology and the Alumni Endowed Chair in Biomedical Sciences. This discovery single-handedly changed my career. Currently, GPR75 is recognized as a key target in various diseases, including obesity, diabetes, cardiovascular conditions, and liver disease. Major pharmaceutical companies around the world are now interested in GPR75, as targeting it holds immense therapeutic potential. With this breakthrough, it felt right to leave my postdoctoral training at Yale University and return to NYMC to further explore and expand on this story. Returning to NYMC has also allowed me to give back in many ways, offering research opportunities to students from various backgrounds and academic levels.
my dissertation defense. I was compelled enough and graciously rewarded by a team that have become a part of my success story. The opportunity to mentor and inspire the next generation of Dr.P.H. students is incredibly rewarding. From my professors, I learned how to be fun while communicating and impacting knowledge. I have learned that a supportive faculty is more likely to succeed and get the best out of students. I have also learned the incredible ability to be tolerant of the different capacities and experience levels that students have to offer, which serves as opportunity for me to exchange knowledge and experiences. These are all lessons I am passing on to my students.
ALUMNI and DONOR Events




Kenneth Theobalds Honored at NYMC’s Annual Golf Tournament
Sunshine and clear skies made for a perfect day at the fourth annual New York Medical College (NYMC) Golf Outing and Reception, sponsored by the NYMC Board of Advisors at the Saint Andrew's Golf Club in Hastings-on-Hudson, New York. On June 17, 2024, the event honoring Kenneth Theobalds, a member of the NYMC Board of Trustees and president and managing partner of RiverRun Partners LLC, was the most successful to date, raising more than $200,000 with 130 golfers taking to the course, reveling in the pleasant weather as they tested their skills in a putting and hole-in-one contest.
“Our annual golf tournament turned out to be a beautiful day of competition, celebration and community-building, and for that we are grateful,” said Edward C. Halperin, M.D., M.A., chancellor and chief executive officer. “The funds raised will go a long way toward shaping the next generation of skilled, empathetic and dynamic health care professionals and researchers who come through this campus.”
The evening reception, which brought together more than 175 attendees, celebrated Theobalds for his contributions to the College and the greater Westchester community, along with his work to promote fairness and equity in financial services.
“It’s a pleasure to play at this outing in support of NYMC,” said Theobalds. “I

want to thank the trustees, faculty, and sponsors who supported this event focused on education, the future, and lessening the financial burden on our students.”
Theobald’s community service and corporate philanthropy has gained him wide recognition from the United States Congress, New York State Senate, Westchester County Legislature, National Association for the Advancement of Colored People, African American Men of Westchester, American Red Cross, Mount Vernon Hospital, Guiding Eyes for the Blind, American Diabetes Association, Arts Westchester, the College of Westchester, and many other organizations. ■


NYMC Celebrates Visionary Public Health Leaders at
TAnnual Founder’s Dinner
he scenic Surf Club on the Sound in New Rochelle, New York, set the stage for an unforgettable evening at the Founder’s Dinner on September 26, 2024. The annual fundraising event brought together more than 450 academic, health care, business and community stakeholders to celebrate New York Medical College’s (NYMC) outstanding leaders and their impressive achievements.
The evening honored Robert W. Amler, M.D., M.M.S., M.B.A., FAAP, FACPM, vice president for government affairs, dean of the School of Health Sciences and Practice, and professor of public health, pediatrics, and of environmental health sciences; and Sherlita Amler, M.D., M.S., Ed.S., RN, FAAP, CEM, commissioner of health for Westchester County, clinical associate professor of pediatrics, adjunct professor of public health, and senior fellow in the Center for Disaster Medicine, who received the William Cullen Bryant Award, the most prestigious honor awarded by the College. The award was established to recognize those remarkable individuals who, in the tradition of the


College’s founder, William Cullen Bryant, demonstrate seminal leadership in health care, science, education, business or the arts.
Edward Chew, M.D. ’03, FACEP, chief executive officer for Physician Affiliate Group of New York, chief of emergency medicine and deputy chief medical officer of Harlem Hospital, assistant clinical professor of emergency medicine, Columbia University Vagelos College of Physicians and Surgeons, a member of NYMC Board of Advisors and honorary surgeon for the New York Police Department, received the Jackson E. Spears Community Service Award, which recognizes individuals and organizations that have demonstrated exceptional commitment to serving their communities. He is the first NYMC alumnus to be awarded this prestigious honor.
The event raised more than $400,000 to benefit NYMC students through scholarships and important initiatives, and further NYMC’s mission to educate the next generation of physicians and health care providers, and support life-saving biomedical research.





THE 2024 SPONSORS INCLUDED: Presenting: Regeneron
Premier: Tamar and Avi Retter, M.D.
Gold: Robert W. Amler, M.D., M.B.A., and Sherlita Amler, M.D., Edward Chew, M.D. ’03, NYMC Board of Advisors, and Westchester Medical Center
Silver: Boston Children’s Health Physicians and Saint Joseph’s Medical Center
Bronze: Sarah and Andrew Levy, Dr. Meryl Mark and Mr. Joseph Mark, Ronald and Peggy Poe, PAGNY, Stifel, Nicolaus & Company, Phelps Hospital
Northwell Health, and Webster Bank
Dessert: KPMG, CFI Office, DIGroup, Ellen and Mitchell Cairo, M.D., and Pavarini Construction Company
Music: ABM Janitorial Services
Flowers: Ben Chouake, M.D. ■
BOARD OF TRUSTEES
Joseph D. Mark, Chair
Joseph Schwartz, M.D., Vice Chair
Alan Kadish, M.D.
Robert Alter, M.D.
Gary Barnett
Howard Baruch, M.D.
Benjamin Chouake, M.D.
Rabbi Menachem Genack
Gary Gettenberg, M.D. ’83
Munr Kazmir, M.D.
Moshe Lichtenstein
Rubén A. Medina, M.B.A., M.P.H.
Lawrence F. Neshiwat, M.D.
BOARD OF ADVISORS
Martin S. Katzenstein, M.D. ’78, Chair
Mykola Alyskewycz, M.D. ’92
Christel Bauer, M.D.
Sabra Brock, Ph.D.
Diana Bryk, M.D.
William J. Camera, C.P.A.
Edward Chew, M.D. ’03
Steven H. Cho, D.D.S.
Eric I. Choe, M.D. ’88
Raymond A. Conta, J.D.
Noreen Ferrante, M.D. ’84
Kathleen Case Finzel, M.D. ’87
Isaac Galandauer, M.D. ’02
Moshe E. Hirth, M.D. ’88
Moira T. Imperial
Howard Jonas
Russell Kamer, M.D.
Martin D. Keltz, M.D.
Baoqing Li, M.D. ’05
Norman L. Maron, M.D. ’70
Stephen Nicholas, M.D. ’86
Martin Oliner, Esq.
Eliot Peyser
Ronald F. Poe
Joseph Popack
Ammir Rabadi, M.D.
Avi Retter, M.D.
Stephen Rosenberg
Alan B. Rosenthal, D.M.D.
Henry Saphier, M.D. ’61
Kenneth R. Theobalds
ALUMNI PROFILE
Deena Casiero, M.D. ’06 Advancing the Game of College Sports Medicine
BY KIARA THOMAS, M.A..
Leonard J. Newman, M.D. ’70
Rebecca B. Newman, M.D. ’05
Paul Ostrovsky, M.D. ’78
Michael Paris
Chong H. Park, M.D. ’96
Lawrence Rein
Anne Negrin Reis, M.D. ’02
Richard Rohr, M.D. ’80
Bruce Schanzer
Jonathan Sheindlin, M.D. ’93
Tamy Skaist
William Smith
Susan N. Tierman, M.D. ’79
Steven Topfer, D.O.
Rajesh Verma, M.D. ’93
Anthony Viceroy, M.B.A., CPA
Vincent J. Vigorita, M.D. ’76
Patricia White, M.D.
John M. Zimmerman, M.D. ’78

Sports medicine was the field Deena Casiero, M.D. ’06, knew she wanted to pursue after experiencing ACL tears in high school and college, although she thought it would be in athletic training. While at Springfield College in Massachusetts, she pursued a bachelor's degree in athletic training with a minor in sports psychology, drawing on her experience as a basketball and softball player. It was during her senior year that Dr. Casiero's career aspirations evolved.
“Around my junior year of college, I felt frustrated that I always had to defer to doctors for X-rays, MRIs, or lab results,” says Dr. Casiero, National Collegiate Athletic Association (NCAA) chief medical officer and senior vice president of the Sport Science Institute. “I wanted to take that next step, diagnosing and treating athletes, and coming up with treatment plans.” This realization led her to consider medical school, setting her on the path to becoming a physician.
She spent the next two years earning a post baccalaureate degree and sitting for the MCAT. She chose New York Medical College (NYMC) for its many diverse clinical opportunities. Her athletic training background proved invaluable in medical school, giving her a strong foundation and smooth transition. She had already taken high-level anatomy and physiology classes and had experience in interviewing patients, obtaining a medical history, and performing a physical exam.
“During my fourth year at NYMC, I completed electives in New York City with a physician who served as team physician for the USA Women's Sevens rugby team,” recalls Dr. Casiero. “That rotation allowed me to make connections that profoundly shaped my career. The experience I gained working with the team continued throughout my residency. None of this would have been possible without NYMC."
Before joining the NCAA, Dr. Casiero built an extensive career in elite sports medicine. She served as assistant team physician for the New York Islanders and medical director at Hofstra University. At the U.S. Open Tennis Championships, she took on dual roles as tournament physician and director of player medical services. Her path then led to the University of Connecticut for nine years, where she initially served as director of sports medicine and head team physician before being promoted to senior associate athletic director for sports medicine, while continuing her role as head team physician.
During the COVID-19 pandemic, Dr. Caserio became involved in task forces and advisory groups across colleges and universities, where team physicians devised plans to keep their athletes safe. In 2021, she became a member of the NCAA Committee on Competitive Safeguards and Medical Aspects

of Sports, where she served as vice chair before accepting the position as NCAA chief medical officer. She is also a member of the American College of Sports Medicine and the American Medical Society for Sports Medicine.
“The two and a half years that I was on the NCAA Committee on Competitive Safeguards and Medical Aspects of Sports were probably some of the most professionally satisfying moments of my career. The committee was incredibly passionate, dedicated, thoughtful, and intentional as they deliberate issues about student athlete health, safety, and performance. While I was on that committee, the chief medical officer at the time, announced that he was retiring, and that was the first time that I started to think about a different career path.”
As the NCAA's chief medical officer, Dr. Casiero leads initiatives to enhance student athlete care across member institutions. Her team collaborates closely with these institutions, providing guidance and education on health, safety, and performance. In her role as senior vice president of the Sport Science Institute, she directs all operational and management aspects of the department. As a key member of the senior leadership team, Dr. Casiero advises the NCAA president and executive staff on critical health and safety matters affecting collegiate athletes nationwide while providing strategic guidance to member institutions on medical policies and best practices.
“Being a woman in this role, I hope my story inspires young women in every field, particularly medicine,” says Dr. Casiero. “We often become our own harshest critics, but I want them to know that with determination, any goal is achievable. My message is simple: believe in yourself as much as others believe in you and never be afraid to reach for the stars.” ■
MILESTONES Alumni Achievements
STAY IN TOUCH
We would love to share your most recent news and accomplishments in the next issue of the Chironian. If you have any recent professional accomplishments or developments, published a book, or have any family news to share, please let us know.
Submit your updates online: www.nymc.edu/alumni
The 20s

Marina K. Holz, Ph.D., M.P.H. ’23, Dr.P.H. ’24, dean of the Graduate School of Biomedical Sciences, professor of cell biology and anatomy, and interim chair of biochemistry and molecular biology at NYMC, was named an American Society for Biochemistry and Molecular Biology 2024 fellow and was appointed to serve on the American Association of Medical College’s Group on Women in Medicine and Science Steering Committee for a threeyear term.

Jessie Moore, M.P.H. ’10, Dr.P.H. ’23, CHES, adjunct professor of public health in the School of Health Sciences and Practice at NYMC, was appointed director of public health for Sullivan County in New York.
Mina M. Belfert, D.P.T. ’21, and Frank J. D’Arrigo, D.P.T. ’20, were engaged in April 2024. They returned to the NYMC campus to have their engagement photos taken.

Mail them to:
Office of Development and Alumni Relations New York Medical College 40 Sunshine Cottage Road Valhalla, NY 10595
The 10s
Samantha Castella, D.P.T. ’19, published a children’s book, Minty’s Scoop on School. “As a mom and pediatric PT, I’m passionate about helping kids grow with confidence, which is why this story is so close to my heart. Minty is a mint chocolate chip ice cream cone who’s nervous about her first day of school and afraid she won’t fit in, until she discovers that being unique is what makes her so special,” she writes.
Deepkumar G. Patel, D.D.S., M.P.H. ’19, was recently commissioned as Captain of the dental corps of the Vermont Army National Guard.
Tina Fickeria, M.P.H. ’18, and Kevin Buelta were engaged in the spring of 2024, and have a wedding scheduled in 2025.


Raymond A. Pashun, M.D. ’14, is beginning a new position as assistant professor at the University of Michigan in 2025. “I will be primarily practicing as a critical care cardiologist. My wife, Mary, and goldendoodle, Chewie, are very excited for our move,” he says.

Alexandra J. Normington, M.P.H. ’14, has been named chief communications and marketing officer for Cook County Health in Chicago, one of the leading public health care systems in the country, serving more than 600,000 individuals each year through its hospitals, including Chicago’s preeminent Level 1 trauma center, community health centers, correctional health services at the Cook County Jail, Medicaid managed care plan CountyCare, and Cook County Department of Public Health. She also serves as chair of the Board of Directors for Pillars Community Health, a federally qualified health center that provides comprehensive primary, dental and mental health care, as well as domestic violence and sexual assault services, and education in Chicago’s western suburbs.

Akshat Jain M.D., (GME ’11), M.P.H., is thrilled to announce the City of Redlands in California has officially declared September, “Sickle Cell Awareness Month.” He expresses a heartfelt thank you to Mayor Eddie Tejeda, and the City Council, for recognizing the importance of public policy in healthcare and the positive impact it can have on patients, communities, and stakeholders. In 2023, Dr. Jain received several recognitions for his work in California, a legislative milestone that represents hope for all individuals impacted by sickle cell disease.
Ijeoma Opara, Ph.D., M.P.H. ’11, M.S.W., was one of 400 recipients of the Presidential Early Career Award for Scientists and Engineers honored by former President Joe Biden. She was recognized for her work in science outreach and prevention research, focusing on empowering urban youth.


Tariq Z. Rajnarine, M.D. ’11, is medical director of Good Shepherd’s Brain Injury Program at the Good Shepherd Rehabilitation Hospital in Center Valley, Pennsylvania. Prior to joining Good Shepherd, Dr. Rajnarine served as an attending physician in both the stroke and spinal cord injury rehabilitation programs at Jefferson Moss-Magee Rehabilitation in Philadelphia, where he co-established and was the clinical director of Klein Family Parkinson’s Rehabilitation Center. He is board-certified by the American Board of Physical Medicine and Rehabilitation. (Photo Credit: Good Shepherd Rehabilitation)
The 00s
Jessica L. Baliski, M.S. ’09, was voted best in speech therapy in the medical/medicine category of the Best of 2024 Washington Township, New Jersey listing.
Carol Russell, D.O., (GME ’06), was appointed associate chair of obstetrics and gynecology at Northwell Health Staten Island University Hospital. She was instrumental in bringing forward groundbreaking advancements in maternal and newborn care, as the hospital opened a standalone women and newborn center and was featured in Industry Magazine, discussing her role in the processes and future of this enhanced service facility.
Giles Willis Jr. D.D.S. (GME ’04), was a recipient of singer and talk-show host Kelly Clarkson’s annual “Christmas surprises” of $100,000, which he is using to establish a much-needed dental clinic near his Arkansas hometown, which has been without one for two decades.

After many years in community hospital practice, Isabel C. Legarda, M.D. ’02, joined the anesthesia faculty at Massachusetts General Hospital parttime. For several years, she provided ketamine infusion treatment for major depression. After retiring from that in 2020, she completed a master’s degree in bioethics at Harvard Medical School and teaches clinical ethics for first-year students from time to time. Once both her children were grown and out of the nest, she went back to her roots as a literature major and starting writing again. She published several poems and short stories in various literary magazines and a book of poetry, Beyond the Galleons , about Philippine colonial history and diasporic experience. “NYMC prepared me well to live my best life. I’m so grateful,” she writes.
Baturu Mboge, M.P.A., M.P.H. ’15, Dr.P.H. ’17
Plants the Seeds of Change as a Global Health Leader
BY KIARA THOMAS, M.A..
Baturu Mboge, M.P.A., M.P.H. ’15, Dr.P.H. ’17, vice president for learning and development at Advance Care Alliance of New York (ACANY) and LIFEPlan CCO, has dedicated his career to advancing public health and supporting marginalized communities, bridging gaps from the vibrant landscapes of The Gambia to the bustling streets of New York City.
A Gambian by birth and upbringing, Dr. Mboge grew up in a rural community where he witnessed severe disparities in resources and opportunities for women, people in rural areas, and people with disabilities. These early experiences fueled his commitment to social justice. He began his career in education, working as a teacher in junior secondary schools and later for a nonprofit supporting rural Gambian women engaged in agriculture.
“I worked very closely with civil society organizations, youth, women, and faith-based organizations on human rights, poverty, and other forms of deprivation in African communities,” says Dr. Mboge. “With these experiences, I was able to link to social and economic determinants of health during my studies at New York Medical College (NYMC).”
Dr. Mboge’s academic and professional journey is a testament to his dedication to development and social justice. He earned his bachelor's in development studies with a minor in sociology at the University of The Gambia, and a diploma in management studies and information technology at the Management Development Institute in 2005. Concurrently, he also worked as a development trainer with the West African Rural Development Centre, conducting training in rural Gambia and Ghana on participatory development; with the Child Fund International in The Gambia as a program site coordinator for community development initiatives; joined the African Center for Democracy and Human Rights Studies as a program assistant; and served as the co-chair of the Global Call to Action Against Poverty in The Gambia.
A hunger for more knowledge and influenced by his background in human rights, Dr. Mboge traveled 4,000 miles to the United States in 2006, leaving his successful career to pursue a master’s degree in public administration with a focus on emergency management at the City of New York’s John Jay College of Criminal Justice. “Growing up in Africa, I witnessed the challenges posed by disasters," he says. "I focused on emergency management to help communities in need with disaster preparedness, mitigation, recovery, and response."

A graduate during the Great Recession and uncertain of his future, Dr. Mboge was all but discouraged to pursue his passions when he graduated in 2009. He became a livein caregiver, providing care to people with intellectual and developmental disabilities.
“Being a caregiver was one of the best highlights of my career,” he says. “I cannot describe the feeling you get when the people you support look at you and say, ‘Thank you for helping me.’ The families have been incredible and make you feel at home.”
One of those he cared for worked at the Westchester Institute for Human Development (WIHD), an affiliate of NYMC, which eventually led Dr. Mboge to a position there as a Medicaid service coordinator. Learning about WIHD’s affiliation with NYMC, he pursued an M.P.H. and later a Dr.P.H., deepening his expertise in public health policy, while continuing his work with WIHD.
In July 2018, Dr. Mboge joined ACANY as a senior director of care management. Now, as the vice president for learning and development for ACANY and LIFEPlan CCO, he provides comprehensive training to 1,600 employees, building partnerships within the learning community, and leading the development of workforce programs for intellectual and developmental disabilities.
Reflecting on the impact of his career, he shares, “My greatest achievement has been building trust and meaningful relationships. We all have the capacity to build better communities, and people will remember you for the impact you make in their lives.” ■
The 90s
Scott T. LeRoy, M.P.H., M.S. ’97, is pleased to share, “My 14-year-old daughter, Payton Leroy, was selected to attend the Congress of Future Medical Leaders in June 2025. She has maintained a 4.0 average for several years and is crushing it in her first year of high school at North Caroline High School. She loves science, engineering, and math and she is also a ranked player in the USTA in tennis, with hopes of making the high school team.”

Barbara A. Kennedy McNabb, M.P.H. ’96, L.M.S.W., writes, “I went from Greenwich, Connecticut, to Midland, Texas, the oil patch. We call it ‘Beaupre’ for ‘Beautiful fields’ — oil fields, that is. It was not a straight line that I traversed, nor a level one; it was both divine and magical. My latest project is my book, The White House: How Opioids Took Over a Small Town. Community work has never been more challenging and for most of what ails, the cure is prevention. Avoidance means to stand away, not near, a vector or walk around a toxic site protected.”
James L. Januzzi Jr., M.D. ’94, was awarded the American College of Cardiology Distinguished Clinical Researcher Award and was named the C. Michael Gibson Chair in Medicine at the Baim Institute for Clinical Research. He continues to serve as the Adolph Hutter Professor of Medicine at Harvard Medical School and staff cardiologist at Massachusetts General Hospital and is in his 20th season as a team physician for the Boston Red Sox.
Commander Kenneth Wells, M.D. ’94, is following in the footsteps of his classmate Michael Moellenhoff, M.D. ’94, practicing in New Zealand for one year, working in a small community health clinic in Levin, located on the southern part of the North Island. “It is interesting to see the differences in the medical systems, a bit of change from Newport, Rhode Island. If any NYMC classmates are passing through, do reach out,” he writes.
The 80s
Thomas, A. Sharon, D.N.P., M.P.H. ’88, published a book, The Disease of Politics and the Politics of Disease: The COVID -19 Origin, Aftermath, and Future.
Philip R. Cohen, M.D. ’83, has focused his attention on forensic dermatology with papers on identifying human trafficking victims in the journal Cureus in November 2023 and the cutaneous manifestations of drug reactions that can mimic traumatic injuries also in Cureus in October 2023. In addition, with co-authors, he has developed a colorimetric scale for skin color to be used for forensic evaluations, which was published in Cureus in November 2023. He and his wife share their home with three basenjis.
Adelaide G. Nardone, M.D. ’83, is proud to announce she published a book, One Million Vaginas, a memoir of her journey as an orphan girl who fulfilled her dream to become an obstetrician and gynecologist.
Jay D. Tartell, M.D. ’82, wrote a book, Evolution of the Brown Bess Musket, Early British Infantry Flintlocks in Context, a holistic monarch-by-monarch journey exploring and summarizing how early military flintlocks arms and tactics inter-relate with events in British and Colonial American history.

Charles E. Dorfman, M.D. Fifth Pathway ’80, has retired after 40 years of practice.
David J. Glass, M.D. ’85, vice president of research, aging/age-related disorders and director of the postdoctoral fellow program at Regeneron Pharmaceuticals, was inducted into the U.S. National Academy of Sciences in recognition of his exceptional contributions to the understanding of the control of skeletal muscle homeostasis.
The 70s
Alice Jones, M.D. ’78, reports in the fall of 2025, Unbound Edition will publish her memoir, a blend of prose and poetry focused on moments in her life as a physician and psychoanalyst, and on the losses and joys that time brings.
John T. Repke, M.D. ’78, reports the fifth annual John T. Repke, M.D., FACOG, Endowed Lecture in Maternal-Fetal Medicine took place at Penn State College of Medicine on October 30, 2024. The lecture, “Environmental Exposures During Pregnancy” was presented by Eva K. Pressman, M.D., the Henry A. Thiede Professor and Chair of Obstetrics and Gynecology at The University of Rochester School of Medicine and Dentistry. Dr. Repke, who was chair of the Penn State Department of Obstetrics and Gynecology from 2002-2017, was the recipient of the 1999 NYMC Alumni Medal of Honor. He and his wife, Jaque, reside in Palmyra, Pennsylvania.
Sanford F. White, M.D. ’78, recently retired and moved to Massachusetts.

Steven M. Fruchtman, M.D. ’77, writes, “I did it. I hung up the license and retired. I suspect I joined many other retirees from the Class of 1977. I want to thank NYMC for opening the door to an exciting career in academic medicine as a hematologist oncologist, followed by a drug development career as a CMO and CEO of publicly and privately held companies. It has been a tremendous educational journey leading to advances in clinical medicine and health authority approvals for transformative experimental drugs, some of which were influential in prolonging life and the quality of life. I could never have imagined the career I had surrounded by my great kids and their paths in healthcare and thus caring for others. I have had many great mentors along the way, and I want to thank them. My journey into hematologyoncology was initiated as a student at NYMC by Drs. Sheldon Rothenberg and Maria DaCosta. They were two great teachers who continued to offer me their advice at many points along the path. The best thing is to remain friends with many of my NYMC classmates, whom I have cherished for over 40 years. You know who you are. All the best.”
Stephen G. Marcus, M.D. ’76, is the CEO of Cantex Pharmaceuticals, a company developing azeliragon, an oral inhibitor of the receptor for advanced glycation end products (“RAGE”). Cantex has ongoing phase 2 clinical trials in top U.S. medical centers in glioblastoma, brain metastasis, metastatic pancreatic cancer, and breast cancer, and a phase 3 clinical trial in hospitalized patients with pneumonia. Azeliragon recently obtained FDA orphan designations for brain metastasis from breast cancer, glioblastoma, and pancreatic cancer.
Martin A. Schwartz, M.D. ’75, retired last year, toured Scotland, and attended the national mystery fans convention, Bouchercon. “I finally had the time to attend a relative’s wedding; I’m trying hard to learn how to sleep late,” he writes.
Neil S. Silber, M.D. ’75, writes, “I retired after 36 wonderful years of solo practice without ever having participated with the managed care model. I am living year-round in sunny Florida and enjoyed seeing my NYMC classmates at our 50-year homecoming celebration.”

Alan S. Sacerdote, M.D. ’74, an endocrinologist specializing in diabetes and metabolism, was a guest on the Decoding Healthcare Research podcast hosted by Efrain Riveros Perez M.D., in March 2024, discussing vitamin D, insulin resistance, and Type 2 diabetes.
ALUMNI PROFILE
Odaelys Pollard, Ph.D. ’15 Champions STEM and Empowers Future Scientists
BY KRISTIN BAIRD RATTINI
The first step is the most important in any journey. Throughout her impactful career in academia, Odaelys Pollard, Ph.D. ’15, has empowered thousands of high school students as a mentor in the New York State Department of Education Science and Technology Entry Program (STEP) and similar programs aimed at increasing the number of historically underrepresented and economically disadvantaged students prepare for college, and to improve their participation rate in STEM related careers.
Dr. Pollard understands first-hand the challenges that these students often face. A native of the U.S. Virgin Islands and first-generation college student, she struggled with culture shock when she first came to New York in 2007 for postbaccalaureate studies in microbiology and immunology at the University of Rochester School of Medicine and Dentistry. “There were not many faces that looked like mine,” says Dr. Pollard. “The thing that kept me going was finding a group of friends from the Caribbean with similar backgrounds.”
Finding and building support networks would become an enduring throughline for Dr. Pollard both personally and professionally. She co-founded the Black Graduate Student Association at New York Medical College (NYMC) during her Ph.D. studies to foster a sense of community for students navigating similar challenges. She discovered her passion for empowering underrepresented students in STEM upon launching a research program centered on marginalized groups as part of the NYMC’s STEP offering. When the official STEP ended at NYMC, Dr. Pollard and a colleague took it upon themselves to develop a NYMC Summer Research Program that allowed high school students from underrepresented backgrounds to be actively involved in research projects at the College, matching applicants with faculty sponsors and offering their own mentorship. “It has been rewarding to see high school students apply to and get accepted into college science programs.,” she says. “I realized that guiding students into the world of science is what I am destined to do.”
She credits her mentor Dana Mordue, Ph.D., vice chancellor for accreditation and student support and associate professor of pathology, microbiology, and immunology, for nurturing her passion and encouraging her to dedicate herself to this cause. “I am grateful for Dr. Mordue for supporting me,” Dr. Pollard says. “I appreciated that she was mindful of the path I wanted to follow and was supportive of that.”
Her dedication to expanding STEM opportunities continued at Albany Medical College, where she led its STEP before joining The Rockefeller University in 2016 as its science education

program and training manager. She managed six STEM programs ranging from one-day field trips to week-long camps to semester-long research projects and reaching more than 3,000 students. “We wanted to create as many access points as possible, because different opportunities resonate with different students,” she says.
She also taught a research experience course at Hunter College, designed to open students’ eyes to the numerous career paths in science. “The purpose of the course was to introduce students to other career options that they might not have considered and how to navigate those paths,” she explains.
Today, in Dr. Pollard’s current role as director of research for the Borough of Manhattan Community College (BMCC), she is excited to provide STEM opportunities for college students from various countries and diverse backgrounds. By securing new funding, she has doubled the number of research programs and student researchers. She is especially proud of the grants that provide research funds for up to 15 international students and that bolsters mentor training for faculty. Participation in MBCC’s STEP also doubled in the past year.
Through her unwavering commitment to mentorship, advocacy, and expanding STEM access, Dr. Pollard is not only shaping the next generation of scientists—she is transforming lives, one student at a time.
“The enthusiasm of the students has been great,” Dr. Pollard says. Several BMCC students have earned awards at national conferences, often competing against other students from four-year institutions. “I like helping students realize, ‘You belong here. Your work is meaningful,’” she says. “It has been so fulfilling to see our students succeed.” ■

The 60s
Kenneth P. Carlson, M.D. ’73, reports he is happy residing in Porto, Portugal, after 40 years in pediatrics in private practice working for the Department of Health.
Anthony P. Chatowsky, M.D. ’62, a retired psychiatrist who was called Dr. C by his patients and coworkers, shares that the second edition of his book, The Prayer, was published by Stillwater River Publications in 2024. The book offers a pause to study, reflect, and listen to the words of the Lord’s Prayer.
Richard J. Macchia, M.D. ’69, completed his 50th year in the practice of urology in June 2024. Since 2009, he has been on the staff at Cleveland Clinic Florida – Weston.

Michael E. Platt, M.D. ’69, published a book, Adrenaline Dominance. He explains, “Excess adrenaline is virtually unrecognized as the main cause of anxiety, insomnia, and ADHD. It is the cause of colic in babies, bedwetting in children, PMDD, IBS, road rage, RLS, and many other conditions. It may be an important reason for weight gain, causing fat to be deposited while people are sleeping. The book explains how the body releases adrenaline to raise sugar levels for the brain (gluconeogenesis) since the brain requires both sugar and ketones to function. Adrenaline peaks at 2:30 a.m., which is when the brain runs out of fuel. This excess adrenaline causes the release of cortisol, which also raises sugar levels. The book also explains why adrenal fatigue is misdiagnosed if using saliva tests and how to reduce adrenaline, very often within 24 hours.”
Arthur A. Topilow, M.D. ’67, and Judy Fiedler Topilow, M.D. ’67, write, “We are still holding up the New Jersey Shore. Arthur is still a pianist, although a far cry from the medical student lounge at NYMC. Fully retired from practice with Atlantic Hematology Oncology, he has a pre-medical student research program writing posters and medical journal articles at Jersey Shore Medical Center. He enjoys playing jazz concerts in public, racing his sailboat, and exploring and writing about jungles in South America. Judy is fully retired from her pediatric practice and co-directing an MDA-sponsored neuromuscular clinic for 35 years. However, she keeps up her continuing medical education and New Jersey medical license. She is also a fine mahjong player.” They have also recently been in touch with Israel-based classmate Stephen Berger, M.D. ’67, who continues to publish e-books on infectious diseases.
Robert A. Harwood, M.D. ’62, has been fully retired for 10 years and in moderately good health. He’s living in Scottsdale, Arizona, and would love to hear from any nearby classmates.
Michael Schlossberg, M.D. ’62, has been retired for 22 years. “I still pursue my love of master drawings and sculptures. Art collecting has been an adventure and joy. I have donated and loaned objects from my collection to multiple museums worldwide. Traveling has been more difficult, so my wife of close to 50 years and I spend time close to home. Of course, we enjoy our children and grandchildren and look forward to their visits,” he writes.
Harvey E. Cooper, M.D. ’60, has been retired for four years. His granddaughter, Jaimee Cooper, M.D. ’25, graduated from the School of Medicine in May 2025, making her the third generation in the Cooper family to be NYMC alumni. Her father is Jonathan D. Cooper, M.D. ’87.
The 50s
Stephen N. Rous, M.D. ’56, and his wife, Margot, celebrated their 58th anniversary and are both retired from any gainful employment. He shares, “We both dispense pharmaceutical drugs from the local Air Force Base Pharmacy, and we travel as much as we can. We spent a week in the south of France renting the same apartment that we have rented for more than 22 years. Our children and grandchildren are well, thriving and living near us; hence the reason that we now live down here in Virginia and not in New England, where we had lived for more than 30 years and still prefer to our present locale. Most of our days are spent shopping at the local commissary or seeing a variety of doctors and/or dentists. We have very few friends from high school and/or college still among the living but that is the way it goes, I guess, with aging!”
IN MEMORIAM Alumni
Karen R. Brass, M.S. ’04, died on February 19, 2024.
Brian T. Di Stante, M.D. (GME ’02), died on April 9, 2024. He was 54.
Ray T. Whitt, M.D. (GME ’99), died on July 21, 2024. He was 67.
Anthony E. Okoh, M.D. ’97, died on October 27, 2023. He was 67.
J. W. Thomas, M.D. (GME ’91), died on May 1, 2024. He was 60.
Joseph A. Panicali, M.D. ’87, died on October 12, 2024.
Diedre L. McSweeney, M.D. ’86, died on May 2, 2024.
Bonnie L. Robinson, M.D. (GME ’86), died on February 12, 2024.
James D. Woodburn, III, M.D. ’82, died on July 15, 2024. He was 68.
Karlene M. Chin, M.D. ’81, died on May 6, 2024.
John J. Gadomski, M.D. Fifth Pathway ’79, died on December 1, 2023. He was 77.
Marshall D. Kramer, M.D. ’76, died on August 11, 2024. He was 78.
David A. Siegel, M.D. ’76, died on June 28, 2024.
Raghavaiah Kanakamedala, M.D. (GME ’75), died on June 4, 2024.
William Etra, M.D. ’69, died on January 22, 2024. He was 79.
Robert J. Carey, M.D. ’68, died on April 1, 2024. He was 80.
M. Kevin O’Connor, M.D. ’68, died on June 3, 2024.
Peter H. Livingston, M.D. ’65, died on November 18, 2024.
Peter N. Bogdan, M.D. ’64, died on September 14, 2024. He was 85.
William Glatt, M.D. ’64, died on January 20, 2024. He was 85.
Louis H. Lefkowitz, M.D. ’64, died on July 9, 2023. He was 85.
John J. Kearney, M.D. ’63, died on February 27, 2024. He was 86.
Jerome L. Luskin, M.D. (GME ’63), died on May 8, 2024. He was 93.
Joseph F. Hollinger, M.D. ’62, died on February 15, 2024. He was 89.
William M. McCall, M.D. ’62, died on September 13, 2024.
John E. Hoye, M.D. ’61, died on July 21, 2024.
Robert E. Fabricant, M.D. ’60, died on March 22, 2024. He was 88.
John H. Derry, M.D. ’60, died on April 12, 2024. He was 89.
Gerald O. Jensen, M.D. ’57, died on July 18, 2024. He was 97.
James D. Woodburn, II, M.D. ’56, died on February 28, 2024.
Bruce M. Burtan, M.D. ’54, died on May 28, 2024.
Frederick MacDowell, M.D. ’53, died on June 9, 2024. He was 95.
NEW YORK MEDICAL COLLEGE REMEMBERS
Chitti R. Moorthy, M.D., Professor of Clinical Radiation Medicine and Former Chair of the Department of Radiation Medicine

(1949 – 2024)
Kind-hearted compassionate physician, talented artist and philanthropist, Chitti R. Moorthy, M.D., professor of clinical radiation medicine and former chair of
the Department of Radiation Medicine, died on June 17, 2024, at the age of 75. A distinguished researcher and technical innovator in the area of radiation oncology, Dr. Moorthy specialized in low-dose rate and high-dose rate brachytherapy, a form of radiotherapy, and therapies used to treat localized prostate cancer and cancers of the head and neck.
Dr. Moorthy, who joined the College in 1982, became chair of the Department of Radiation Medicine in 2008, a position he held until 2021, when he was honored at the annual NYMC Founder’s Dinner. During his tenure, he developed clinical programs including radiosurgery; total body irradiation and brachytherapy; educational programs for medical students, residents, and fellows; and residency training for overseas health care professionals.
Faculty
Arthur J.L. Cooper, Ph.D., D.Sc., professor emeritus of biochemistry and molecular biology, died on May 30, 2024. He was 78.
Chitti R. Moorthy, M.D., professor of radiation medicine and former chair of the Department of Radiation Medicine, died on June 17, 2024. He was 75.
Charles S. Pavia, Ph.D., adjunct associate professor of medicine, died on June 25, 2024. He was 73.
Ray T. Whitt, M.D. (GME ’99), assistant professor of obstetrics and gynecology, died on July 21, 2024. He was 67.
He also served as the acting chair of the Department of Radiology from 2003 to 2009. His numerous academic and hospital appointments included director of the residency training program in radiation oncology and director of radiation medicine, radiology and the Shaped Beam Radiosurgery Center at Westchester Medical Center.
Dr. Moorthy received his medical degree from Gandhi Medical College in Hyderabad, India, and completed his residency at Michael Reese Hospital in Chicago, Illinois, followed by a fellowship in brachytherapy at Memorial Sloan-Kettering Cancer Center in New York. He was a member of the New York Academy of Sciences, the American Endocurietherapy Society, the American Society of Therapeutic Radiology and Oncology, the Radiological Society
of North America and the New York Roentgen Society, Section of Radiation Oncology.
He also served in many leadership roles including chair of New York Roentgen Society; secretary of Brachytherapy Oncology Association; director of the Association of the Directors of Radiation Oncology Programs; chief executive officer of a large multispecialty hospital in Chennai, India; and founder and chair of the Translational Research Institute of Molecular Sciences in India. Dr. Moorthy also participated in the Indo-American Cancer Congress, and Cancer Units-Research and Education, among other organizations.
Dr. Moorthy will also be remembered as a scholar in Hindu philosophy, talented artist, painter, writer, poet, and ardent supporter of music and art.
Arthur J.L. Cooper, Ph.D., Professor Emeritus of Biochemistry and Molecular Biology

(1946 – 2024)
Talented researcher and respected mentor, Arthur J.L. Cooper, Ph.D., professor emeritus of biochemistry and molecular biology, died on May 30, 2024, at the age of 78. He was an internationally recognized authority in amino acid chemistry and biochemistry and his general research interest was in the biochemical mechanisms underlying neurological diseases, specializing in the workings of metabolic enzymes.
A gifted researcher, his work earned him extramural grant support, several RO1s and numerous foundation grants. He was widely published in peer-reviewed journals, often as first author. His h-index, a metric that measures a researcher’s productivity and the impact of their publications, was a remarkable 61. He served on several editorial boards including the Journal of Biological Chemistry and Analytical Biochemistry, where he also served as editor-inchief. Dr. Cooper also organized several colloquia and workshops at scientific meetings and presented his work all over the world.
Born in London, England, he received a B.Sc. at London University (Northern Polytechnic), an M.Sc. degree from Imperial College, a Ph.D. in biochemistry at Cornell University Graduate School of Medical Sciences, and an honorary D.Sc. from London University bestowed by Princess Anne. After post-doctoral training at Brandeis University, he returned to Cornell where he held a variety of faculty appointments and was a senior research scientist at Cornell-Burke Medical Research Institute, before joining the NYMC community in 2007.
Dr. Cooper served as adjunct professor of biochemistry in neuroscience at the Feil Family Brain and Mind Research Institute, Weill Cornell Medical College, and was a consultant for the Orentreich Foundation in Cold Spring, New York.
Dr. Cooper was an avid gardener and running enthusiast who ran in the New York City and London marathons, raising money for charities, and in the Harry Chapin Run Against Hunger in Croton-on-Hudson, New York. He was also a regular blood and platelet donor and a volunteer judge at numerous high school science fairs over the years.
Ray T. Whitt, M.D., Assistant Professor of Obstetrics and Gynecology, House Advisory
Dean
and Clerkship Director

(1956 – 2024)
Devoted teacher and trusted advisor, Ray T. Whitt, M.D., assistant professor of obstetrics and gynecology, School of Medicine (SOM) house advisory dean, clerkship director and chair of the SOM Admissions Committee, died on July 21, 2024, at the age of 67. He was admired and respected by students and was a pillar of the NYMC academic community.
As a member of a military family, he traveled around growing up: from Alabama and Texas to Michigan and California, Japan to Canada, and several places in between before settling in Colorado for high school.
Dr. Whitt’s path to becoming a physician was a non-traditional one, first attending art school for graphic design and working at a newspaper and then working as flight attendant for United Airlines. When he was 28, he decided to take on the journey of becoming a doctor, first earning his B.A. from Fordham University, followed by medical school at Albert Einstein College of Medicine, all while still
flying the friendly skies. His dream of becoming a physician came true when he graduated from medical school at age 39.
Dr. Whitt completed his residency in NYMC’s Obstetrics and Gynecology Residency Program at New York Health + Hospitals/ Metropolitan and Westchester Medical Center—the start of his long association with NYMC, spanning three decades.
During his career, he served as site director at Metropolitan, assistant professor of obstetrics and gynecology, co-clerkship director of the obstetrics and gynecology core clerkship, before taking on new roles at NYMC—as house advisory dean, joining NYMC Chancellor and CEO Edward C. Halperin, M.D., M.A., in teaching the first-year history of medicine course, and chairing the SOM Admissions Committee.
Dr. Whitt was the recipient of multiple NYMC Excellence in Teaching Awards, a Leonard Tow Humanism in Medicine Award, and a NYMC Student Senate Citation, and he was an Alpha Omega Alpha faculty inductee. He presented the keynote address at the SOM Class of 2021 Gold Humanism Honor Society Student Clinician Ceremony. In November 2024, members of the NYMC community gathered for a celebration of life of Dr. Whitt, encompassing music, poetry, and reflections by faculty, administrators, students, and members of Dr. Whitt’s family who shared memories and the profound impact that Dr. Whitt had on them and the greater community. To honor Dr. Whitt’s legacy, the Stowe House, of which Dr. Whitt served as house advisory dean, was renamed the Stowe-Whitt House.
New York Medical College launched an online all-inclusive platform that provides direct communication between you, fellow NYMC alumni, current students and faculty.
CONNECT
Find and reconnect with fellow graduates, see what they have been up to, and stay in touch.
GIVE BACK
Volunteer as a mentor to NYMC students. Engage in the exchange of advice, career counseling, and other professional guidance. Post and view available job opportunities.
EXPAND
Leverage your professional network by connecting with peers.
Join and/or create groups to share your expertise, experiences, ask for guidance, and more.
Join today by connecting your LinkedIn account or signing up with your email. Registration is simple, just visit www.NYMCConnect.org.
If you have any questions, please contact: development@nymc.edu (914) 594-2720



1 The SHSP unveiled a state-of-the-art motion analysis laboratory equipped with eight infrared cameras that track the movement of markers placed on subjects, to capture precise data. The facility is designed to enhance the learning experience for physical therapy students by providing a visual understanding of movement, while serving as a resource for patient evaluations.
2 NYMC and Touro College of Dental Medicine celebrated the official opening of the new Skyline Auditorium.
3 Students in the Doctor of Physical Therapy program hosted the annual Race for Rehab as a part of their Community Service Project in October, raising more than $10,000 for Achilles International, a non-profit organization that provides a supportive community for athletes with disabilities.



4 Throughout the year the NYMC community shows its true colors and turns out to show support for health awareness observances: red for heart health, gold for pediatric cancer, orange for physical therapy, pink for breast cancer, purple for epilepsy and blue for autism.



5 Student research is flourishing at NYMC and annual events provide opportunities for students to share their findings with their peers and the greater NYMC community while gaining valuable presentation experience and feedback and hearing from notable keynote speakers: Medical Student Research Forum, SHSP Research and Scholarship Day, presented in partnership with the Delta Omega and Alpha Eta NYMC Chapter Honor Societies, and the Graduate Student Research Forum.






6 NYMC was honored at Saint Joseph’s Medical Center annual ball at Westchester Country Club in Rye, New York. Neil W. Schluger, M.D., dean of the SOM, accepted the award on NYMC’s behalf.
7 For more than one decade, NYMC has hosted the Annual Drs. Gabor and Harriette Kaley Endowed Lecture established through the family of the late Gabor Kaley, Ph.D., to honor his life and legacy as a faculty member of 43 years and chair of the Department of Physiology at NYMC for 37 of those years. He was recognized as the longest sitting chair of a physiology department in the nation when he stepped down in 2007.
8 Members of the NYMC community joined Chancellor and Chief Executive Officer Edward C. Halperin, M.D., M.A., on a behind-thescenes hard hat tour of Ellis Island Hospital.
HONOR ROLL OF DONORS
For the Period from July 1, 2023 through June 30, 2024
Thank you to all of our generous donors whose support is critical to the success of our students, faculty, researchers, and the entire NYMC community.
CHANCELLOR’S CIRCLE
The Chancellor’s Circle honors those who make a significant gift or commitment within a single year. In this Circle, there are four Societies distinguished by the nature and size of contributions to the College.
Sunshine Cottage Society
This society is comprised of donors whose gifts and commitments are $50,000 or more.
Mr. Nicholas F. Brady
Mr. Juan I. Gallardo Sr.
Benjamin H. Homan Jr. Charitable Trust
Dr. Meryl Mark and Mr. Joseph Mark
Meryl and Joseph Mark Family Fund
New York Medical College Board of Advisors
Pediatric Cancer Research Foundation
Joseph and Penina Popack
Lavie and Shterna Popack Family Foundation
Regeneron Pharmaceuticals, Inc.
The Barbara and William Rosenthal Foundation
The Alexandrine and Alexander L. Sinsheimer Fund
The George M. Van Cleave Family Foundation
Sarah Upham Trust
Bryant Society
This society is comprised of donors whose gifts and commitments are $25,000 to $49,999.
David E. Asprinio, M.D.
Atlantic Charitable Foundation
Mr. Gary Barnett
The Children's Dream Foundation
Estate of Karlene Marie Chin
Jonathan B. Gavras, M.D. ’86
Gary S. Gettenberg, M.D. ’83
Baoqing Li, M.D. ’05
Ruben Medina, M.B.A., M.P.H.
Paul D. Ostrovsky, M.D. ’78
The Ostrovsky Family Charitable Fund
Lee B. Pressler, M.D. ’90
Pressler Family Foundation
RC Solutions, Inc.
Avi Retter, M.D.
Richard E. Rohr, M.D. ’80
1860 Society
This society is comprised of donors whose gifts and commitments are $10,000 to $24,999.
Anonymous – 2
Mohan P. Abraham, M.D.
Alpha Omega Alpha Honor Medical Society
Alter Family Charitable Trust
Robert Alter, M.D.
The Stephan Ariyan Foundation Fund
Stephan Ariyan, M.D. ’66
Boston Children’s Health Physicians
California Bank and Trust
Drs. Ben and Esther Chouake
Mrs. Nancy M. Danner
Alan D. Dauer, M.D. ’62
Mrs. Delores DelBello
Distinctive Maintenance Company
Martin D. Keltz, M.D.
Lynn Buckvar-Keltz and Martin Keltz Family Fund
Annette E. Kussmaul, M.D. ’93
The Ernest and Marilyn Kussmaul Charitable Foundation, Inc.
Jinhee Kwak, M.D. ’99
Mr. and Mrs. Andrew Levy
Walter M. Lewis, M.D. ’91 and Christel Bauer, M.D.
Mr. Paul J. Maddon
The Paul J. Maddon Family Fund
Jean M. Cacciabaudo, M.D. ’90 and William A. Maiorino, M.D. ’89
Alan Rosenthal, D.M.D.
Mildred Rothstein Rosenthal Family Foundation
Mary Alice O'Dowd, M.D. ’76
Physician Office Based Surgery, PLLC
Mr. and Mrs. Ronald F. Poe
Barry S. Robbins, M.D. ’73
Salamandra, LLC
Seize the Ribbon
Gigi Thomas, M.D.
Mark T. Thompson, M.D. ’71
Titan Advisors, LLC
Webster Bank
Robert A. Welke Cancer Research Foundation, Inc.
Westfair Communications
Mrs. Bonnie Young
Mr. Norman Young
Flower and Fifth Society
This society is comprised of donors whose gifts and commitments are $2,500 to $9,999.
Anonymous – 4
Alliant Insurance Services, Inc.
American Online Giving Foundation
Robert W. Amler, M.D., M.B.A. and Sherlita Amler, M.D.
Firdose S. Ansari, M.D. ’05
Robert A. Barish, M.D. ’79
Augusta H. Belmonte, M.D.
Berkshire Food Distributors Inc.
Mr. Leslie Bond
Mrs. Joi Butler
Philip C. Caron, M.D. ’86
The Caron Family Fund
Cheng Cheng, M.D.
Edward Chew, M.D. ’03
Eric I. Choe, M.D. ’88


Eric I. Choe, M.D., PLLC
Cinqcare
Costanza Cocilovo, M.D. ’96
Kaushik Das, M.D.
Mr. John Y. Davenport
Mr. Thomas A. DeRosa
Kien An Duong, M.D. ’01
Mr. and Mrs. Franklin L. Earle
Epstein, Becker and Green
Fareri Associates, LP
Feder Cohen Donor Fund
John M. Feder, M.D. ’87
Noreen F. Bedini Ferrante, M.D. ’84
John P. Fezza, M.D. ’92
Kathleen Case Finzel, M.D. ’87
Dr. Patricia White and Mr. Daniel Flatley
The Flatley Charitable Fund
Eric C. Fok, M.D. ’93
Nancy J. Freeman, M.D. ’81
Linda K. Friedman, Ph.D.
Michael H. Gewitz, M.D.
Richard Giovannelli, M.D. ’81
Mrs. Jennifer Amler Goldstein
The Jennifer Amler Goldstein Charitable Fund
Arun Goyal, M.D. ’90
Greenberg Traurig, LLP
Karen Grimmell Charitable Fund
Karen E. Grimmell, M.D. ’61
Anita Grover, M.D. ’78
Bob and Laura Gutman
Henry Schein Dental
Jane J. Hew, M.D. ’93
Virany H. Hillard, M.D.
Richard N. Hirsh, M.D. ’69
The IMA Group Management Co., LLC
Mr. and Mrs. Paul Ingrassia
Neha Patel Iyengar, M.D. ’00
Sumeet A. Kadakia, M.D. ’07
Dr. and Mrs. Alan Kadish
Alan L. Kalischer, M.D. ’77
Alan and Tina Kalischer Charitable Fund
Russell S. Kamer, M.D.
Martin S. Katzenstein, M.D. ’78
Jeffrey Kluger, M.D. ’71
Solomon and Sophie Kluger
KPMG, LLP
Krishnan Charitable Fund
Mr. Manish Krishnan
Ms. Susan Kwon
Legato Capital Management, LLC
Armand F. Leone Jr., M.D. ’82
Norman Levine, Ph.D. and Mrs. Norman Levine
Mr. Moshe Lichtenstein
Ms. Shifra Lichtenstein
The Lu Trust Giving Fund
Jocelyn A. Luongo, M.D. ’06
Peter Ly, M.D. Family Foundation
Peter P. Ly, M.D. ’96
George D. Lyons, M.D. ’92
James F. McGroarty, M.D. ’68
Robert J. McNamee, M.D. ’75
Molina Healthcare
Joseph F. Morales, D.D.S.
Morgan Stanley
John E. Mullen, M.D. ’93
The Mullen Family Fund
Mushroom Wisdom, Inc.
Eric Mustonen, M.D. ’75
Dr. and Mrs. Ronnie Myers
Jerry L. Nadler, M.D., MACP, FAHA, FACE
NYC Health + Hospitals
NextGen
Stephen J. Nicholas, M.D. ’86
Paris International Partners, LLC
Mr. Michael Paris
Chong H. Park, M.D. ’96
James F. Passarelli, M.D. ’89
Pavarini Construction Company, Inc.
Peapack Private Bank
Pediatric Urology Associates, P.C.
Alan E. Peters, M.D. ’79
Physician Affiliate Group of New York
Mitchell Pincus, M.D. ’53
Barbara Pineda, M.D.
Prospect Foundation, INC.
Gowtam Ravipati, M.D.
John T. Repke, M.D. ’78
Beverly L. Richman, M.D. ’64
Michael H. Rosenberg, M.D.
Adam D. Rubin, M.D. ’00
Bijan Safai, M.D., D.Sc.
Sagard Holdings
Hon. Brandon R. Sall
Saraya International, Inc.
Pravinkumar B. Sehgal, M.D., Ph.D.
Mr. Bruce J. Schanzer
George C. Shapiro, M.D. ’88, FACC
Jonathan A. Sheindlin, M.D. ’93
Sanford Sherman, M.D. ’56
Catherine B. Small, M.D. ’77
Stifel Nicolaus & Company, Inc.
David Werdegar, M.D. ’56
WJC CPA PC
Robert M. Yacynych, M.D. ’88
Z&R Painting & Contracting LLC
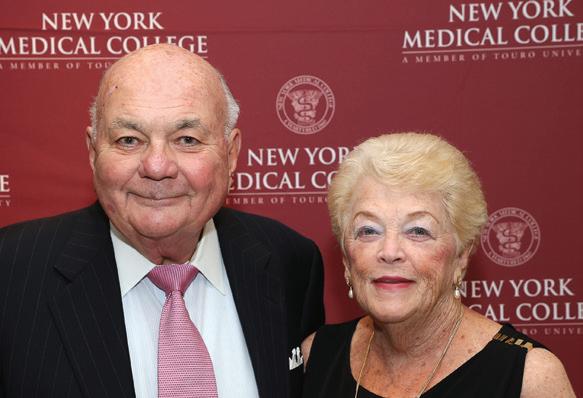
Patrons
$1,000 to $2,499
Anonymous – 7
A.G. Williams Painting
ACA Environmental Services, Inc.
Ann Alexander, M.D. ’78
Michael S. Alexander, M.D. ’78
Gregory L. Almond, M.D., M.S., M.P.H. ’00
Mykola R. Alyskewycz, M.D. ’92
The Antoszyk Family Fund
Andrew N. Antoszyk, M.D. ’83
Ardea Cares Charitable
Mark R. Axelrod, M.D. ’79
Gildy V. Babiera, M.D. ’91
Howard M. Baruch, M.D. Berinstein Giving Fund
Daniel M. Berinstein, M.D. ’93
Alan S. Berkeley, M.D. ’73
Bettina and Spencer Waxman Philanthropic Fund
Nicola Bitetto, M.D. ’64
Peter N. Bogdan, M.D. ’64
Jason S. Bonslaver, M.D. ’06
Brenner Family Charitable Fund
Joel I. Brenner, M.D. ’70
Care Security Systems, Inc.
Catherine G. Caronia, M.D. ’88 and Ronald M. Caronia, M.D. ’88
The Caronia Family Charitable Family
CBIZ Borden Perlman
Christopher T. Channon, M.D. ’76, FACS
Michael T. Charney, M.D. ’66
Qwie T. Chew, M.D. ’65

Frank M. Chieu, M.D. ’71
Roger Chirurgi, M.D.
Elias T. Chua, M.D. ’90
Mr. Gary Cleek
John J. Connolly, Ed.D.
Curi Insurance
Sherry B. Ellis, M.D. ’85
Lauren N. Elliston, M.D. ’08
Jaleh Z. Eslami-Borsody, M.D. ’94
Emalie and John D. Feerick
Burton M. Fink, M.D. ’71
Robert & Brenda Fischbein Donor Advised Fund
Mr. Jeffrey N. Fox
Dr. and Mrs. John A. Fox
Austin T. Fragomen, III, M.D.
Frederick Steinberg M.D. Judith Steinberg
Charitable Fund
William H. Frishman, M.D.
Steven M. Fruchtman, M.D. ’77
Renee Garrick, M.D.
Rabbi Menachem Genack
Jeffrey B. Ginsburg, M.D. ’92
Albert C. Goldberg, M.D. ’63
Mr. Mark Goldstein
Mr. Peter I. Gordon
Harold M. Grafstein, M.D. ’89
Mr. Edmund W. Granski Jr.
Dr. Stuart and Adrienne Green Family Foundation
Stuart A. Green, M.D. ’67
David N. Greenman, D.D.S., M.P.H. ’07
David J. Gross, M.D. P.A.
David J. Gross, M.D. ’84
Edward C. Halperin, M.D., M.A.
The Halperin Family Fund
Gregory P. Harvey, M.D. ’83
James C. Hegarty, M.D. ’62
Naida M. Henriquez, D.M.D.
L. Scott S. Herman, M.D. ’74
Steven H. Horowitz, M.D. ’66
Hudson Cloud Systems
Infectious Diseases Professionals, LLC
Jackson Lewis Foundation
Curtis T. Jones, M.D. ’75
Mr. David Kaminsky
Harvey S. Kaplan, M.D. ’63
Munr Kazmir, M.D.
Mark A. Krich, M.D. ’97
Steven L. Lansman, M.D., Ph.D.
LaRusso Family Charitable Fund
Nicholas F. LaRusso, M.D. ’69
Dr. and Mrs. Zvi Lefkovitz
Christopher S. Leonard, Ph.D.

Jerry I. Levine, M.D. ’77
John A. Lewis, M.D. ’93
Joseph K. Lobl, M.D. ’82
Taylor Lobl Family Fund
Charles Lomanto, M.D. ’63
Mr. Todd S. Lordi
Thomas Lu, M.D. ’96
Peter J. Lucas, M.D. ’72
Vincent A. Lynch, M.D. ’67
The Marcia & Vincent Lynch Charities Fund
Madlon-Kay Charitable Gift Fund
Diane J. Madlon-Kay, M.D. ’79 and Richard C. Madlon-Kay, M.D. ’79
Sabrina Mahboob, M.D.
Ada M. Marin, M.D. ’83, M.P.H.
Mr. Franicis C. Marino
Norman L. Maron, M.D. ’70
Hussein M. Matari, M.D.
James T. Mazzara, M.D. ’63
Peter P. McKellar, M.D. ’70
Ms. Caroline Mechanick
Brenda A. Merritt, M.D. ’65
James L. Mills, M.D. ’73
Mr. David Neiss
Tuan T. Nguyen, M.D. ’06
Optimum Pain Management Center, LLC
Douglas E. Padgett, M.D. ’82
Johanna A. Pallotta, M.D. ’62
Kunjal Patel, M.D.
Mr. Ryan Pearson
Myles L. Pensak, M.D. ’78
Ms. Rebecca Perkins
Joseph W. Placer, M.D. ’64
Alan R. Plumer, M.D. ’88 and Deborah A. Shapiro, M.D. ’89
Dawn Powell, D.D.S.
John M. Powers, M.D. ’77
Ammir S. Rabadi, M.D.
Charles R. Rich, M.D. ’74
Seth J. Richter, M.D. ’94
James J. Rooney, M.D. ’74

Kenneth M. Rose, M.D. ’88
Nancy C. Rose, M.D. ’84 and G. Marc Jackson, M.D.
Andrew J. Roth, M.D. ’88
Mr. Andrew Roussinos
Stephen L. Rubin, M.D. ’70
Rachel Rubinstein, M.D. ’83
Sandra L. Sacks, D.D.S., M.D. ’97 and Harry G. Sacks, D.D.S., J.D.
Sani-Pro Disposal Services, Inc.
Neil Schluger, M.D.
Theodore J. Schmahai, Ph.D. ’88
John H. Seward, M.D. ’61
Win Shen, M.D. ’83
Jeffrey E. Silverstein, M.D. ’91
Mr. William Skolnik
David L. Smith, M.D. ’61
Society of Family Planning Research Fund
Lori Solomon, M.D. ’99, M.P.H. ’09
David J. States Family Charitable Fund
David J. States, M.D. ’53
Frederick Steinberg, M.D. ’58 and Judy Steinberg
Kenneth B. Strumpf, M.D. ’82
Suburban Carting Corporation
Ross H. Taff, M.D. ’74
Dawn M. Terashita Gastelum, M.D. ’99
Ms. Tina Tesch
Mariko L. Ishimori, M.D. ’00 and Nicholas Testa, M.D. ’01
Mr. Hiroshi Toyoda
Nancy N. Tsai, M.D.
US Times Technology Inc.
Sandeepa M. Utpat, M.D.

Scott K. Varland, D.D.S.
John L. Vigorita, M.D., Memorial Fund
Vincent J. Vigorita, M.D. ’76
Susan L. Vogel, M.D. ’76
Ms. Pam Wadav
Brian P. Walker, M.D. ’12
Wayne Printing Incorporated
Mr. Marty Weinberg
Steven Weinstock, M.D. ’74
Douglas N. Whatmore, M.D. ’77
Mr. Gerry Yen
Yen Family Charitable Fund
Daniel Zelazny, M.D.
Richard J. Zeman, Ph.D.
Supporters
$250 to $999
Anonymous – 12
A & C Furia Electric Motors & Pumps, Inc.
A.J. Indusi Plumbing and Heating, Inc.
Faheem A. Abbasi, M.D.
Mr. M. Laniado Abraham
Lori H. Adcock, M.D. ’85
Nanakram Agarwal, M.D.
Elmer C. Agustin, M.D., M.P.H. ’15
and Naomi Ham, M.D. ’84
Robert M. Ahrens, Jr., M.D. ’78
Judith C. Ahronheim, M.D.
Mr. Tom Allnatt
Alan R. Altman, M.D. ’71
Andrew L. Simon, M.D., FACS, PA
The Andrews Family Charitable Fund
David R. Andrews, M.D. ’78
Mr. Kerrin Antommarchi
ARC
Matthew J. Arduino, Dr.P.H., M.S. ’81
Ms. Ingrid C. Armstrong, M.S. ’01 Association of Pathology Chairs, Inc.
Atlantic Westchester, Inc.
Ms. Sybil J. Attardi
Haroutiun C. Avedissian, M.D.
The Awards Center, LLC
Sudhamani R. Rao, M.D. and
Sateesh C. Babu, M.D.
Gerald S. Bahr, M.D. ’72
Albert J. Bajohr, Jr., M.D. ’67
Mahrukh D. Bamji, M.D.
Nicholas G. Baranetsky, M.D. ’74
Stephanie C. Barnhart, M.D. ’08, M.P.H ’08
Patricia A. Barry, M.D. ’83
Robert S. Bartolomeo, M.D. ’71
Paul G. Battaglia, M.D. ’84
Christine H. Beck, M.D. ’77
Richard D. Becker, M.D. ’79
FBO Becker Family Fund
William J. Behrje, M.D. ’65
Barbara R. Bellar, M.D., J.D., M.A., M.P.H., M.Div.
David A. Berkowitz, M.D. ’63
Bernd Allan Strauss
Mrs. Carol Bernot
Basil G. Bernstein, M.D. ’67
Daniel Berson, M.D. ’69
Basil Guralnick Bernstein, M.D. Tzedakah Fund
Richard Besserman, M.D. ’64
Arthur A. Blain, M.B.A., M.D. ’96
Peter Bloom, Jr., M.D. ’04, M.S. ’00
Devon E. Bock, M.D. ’86
Nicholas G. Bonvicino, M.D. ’79
Lisa Borg, M.D. ’80
Denis A. Bouboulis, M.D.
Michael D. Brandler, M.D. ’98
Ms. Julie Brochero
Kevin R. Brown, M.D.
Alexander J. Brucker, M.D. ’72
Jerome M. Burke, M.D. ’84
Andrew S. Burstiner, M.D. ’89
Mr. Terry Burston
Norman A. Cagin, M.D. ’67
Joseph A. Camilleri, Jr., M.D. ’85
Carlos and Gabby’s of Riverdale
Mark Catterall, M.D. ’96
Roy D. Cavalcant, M.D. ’76
CDWFA Trust
Charities Aid Foundation of Americas
Charles Lomanto Revocable Living Trust
Burawit B. Charuworn, M.D. ’99
Hee-Joo Cheon-Schingo, M.D. ’92 and
Victor A. Schingo, M.D. ’92, FACS
William J. Chernack, M.D. ’70
Richard J. Chernick, M.D. ’91
Shafi K. Choudhury, M.D. and Muhammad S. Choudhury, M.D.
Yun Shin Chun, M.D. ’99
Alfonso P. Ciarlo, M.D. ’65
City Heights Pediatrics PC
Alan J. Conrad, M.D. ’81
Martin A. Cooper, M.D. ’63
Ms. and Mr. Anthony Corvini
Mylee W. and Samuel M. Costantini
Michel-Alexis R. Courtines, M.D. ’98
Elizabeth M. Craven, M.D. ’61 and Wales Craven, M.D. ’63
Robert E. Crootof, M.D. ’70 and Mrs. Robert Crootof
Dr. and Mrs. Robert E. Crootof
Charitable Foundation
Michael J. Crupain, M.D. ’06
Mr. James Curran
Alton L. Curtis, M.D. ’69
Christopher Dailey
Terrance M. Daino, M.D. ’90
Mr. Vani Dandolu
David L. Feingold, Inc.
Elliot Davidoff, M.D. ’71
Lorelei S. Davidson, M.D. ’91
Robert A. Davis, M.D. ’74
Dayton Foundation Depository, Inc.
Henry P. Deblasi, M.D. ’55
Lea DeFrancisci-Lis, M.D. ’03
Kevin C. Delahanty, M.D. ’84
Dominick F. DiFabio, M.D. ’71
Anthony A. DiLullo, M.D. ’84
Maj. Beau DiSimone
Bram A. Dolcourt, M.D. ’04
Gary R. Donshik, M.D. ’66
Allen J. Dozor, M.D.
Thomas J. Early, M.D. ’73
Joseph G. Edelson, M.D. ’78
Andrew A. Elimian, M.D.
Elite Caterers of Lawrence
Joseph D. Etlinger, Ph.D.
Victor G. Ettinger, M.D. ’67
Christine M. Fanning, M.D. ’11
David L. Feingold, M.D. ’00
Michael J. Feinstein, M.D. ’64
Virginia E. Feldman, M.D. ’91 and Robert P. Feldman, M.D. ’91
Stephen Ferrando, M.D.
The Film Gallery, LLC
Felicity G. L. Fishman, M.D. ’06
Robert R. Flanagan, M.D. ’75
Mr. Gerard J. Flynn
Arlene A. Forastiere, M.D. ’75
Mr. William Ford
Philip P. Fotanetta, M.D. ’73
John T. Fox, M.D. ’89
Susan Fox, M.Ed., M.A., Ph.D.
Mr. Gregory Francis
Max Pierre Francois, M.D., P.C.
Max P. Francois, M.D. ’88
Frank R. Romano M.D., PC
Denis J. Frank, M.D. ’71
Frieden Family Fund
Richard A. Frieden, M.D. ’84
David and Clair Fung Family Fund
Arthur J. Gallagher Risk Management Services, Inc.
Chirag Gandhi, M.D.
Carol A. Garbarino, M.D. ’79
Margaret M. Gennaro, M.D. ’87
Roshny A. George, M.D.
Mr. Eaten Gettenberg
Kendra G. Gil, M.D. ’04 and Eric A. Gil, M.D. ’03
Steven M. Gitlin, M.D. ’73
Give Lively Foundation, Inc.
Daniel J. Glatt, M.D., M.P.H. ’92
Daniel G. Glicklich, M.D.
Barry S. Goldberg, M.D. ’95
Laurence D. Goldstein, M.D. ’84
Michael S. Goldstein, M.D. ’72
Paul Goldstein, M.D. ’71
Goldstein-Forastiere Family Fund
Michael S. Goligorsky, M.D., Ph.D.
Angela E. Gonzalez, M.D. ’94
Virginia A. Gortych-Barnes, M.D. ’87
Laurie Grant, M.D. ’83
Richard H. Greif, M.D. ’75
Martin A. Gross, M.D. ’81
Mrs. Jill A. Haas
Irwin Hametz, M.D. ’73
Adam Hammerman, M.B.A.
Robert A. Harwood, M.D. ’62
The Hastings Group, LLC
Hearing Loss Association of America
Robert Herenstein, M.D., P.C.
Robert M. Herenstein, M.D. ’85
Edward R. Herman, M.D. ’82
Stephen L. Hermele, M.D. ’68
Lucy S. Hernried, M.D. ’57
Mr. Mitchell Herstic
Hertan Giving Fund
Ms. Sharon Hertan
Robert A. Herzlinger, M.D. ’69
Emile M. Hiesiger, M.D. ’78
Peter Hoffmann, M.D. ’83

David Hong, M.D.
Rivka S. Horowitz, M.D. ’78, Ph.D.
Stephen K. Hoverman, M.D. ’78
Wen-Ray Thomas Hsu, M.D., P.C.
Wen-Ray T. Hsu, M.D.
HUB International Northeast
Magdalen E. Hull, M.D. ’79, M.P.H.
Mark Hurwitz, M.D.
Iron Vault Management
Humayun K. Islam, M.D., Ph.D.
Mokarram H. Jafri, M.D. ’94
Janus Henderson Investors

Jerald W. Katz and Leslie S. Katz
Charitable Fund
Miao Jiang, Ph.D. ’04
Benjamin F. Johnson, Ed.D.
Edward F. Jordan, M.D. ’72 and Mrs. Sharon Jordan
Frank T. Jordan, M.D. ’71
Joseph W. Sorce Funeral Home, Inc.
Ms. Lila Kagedan
Lawrence S. Kaminsky, M.D. ’78
Lawrence and Margie Kaminsky Donor Fund
Emily Kaplan, D.P.H. ’21
Jeffrey M. Kaplan, M.D. ’70
Michael Kaplowitz, M.D.
Elizabeth M. Kass, M.D. ’88
Rabbi and Mrs. David J. Katz, M.D.
Ernest Katz, III, M.D. ’78
Jerald W. Katz, M.D. ’84
Stuart J. Kaufman, M.D. ’77
Kenigsberg-Blum Donation Fund
Jennifer J. Halstead-Kenny, M.D. ’02 and John M. Kenny, M.D. ’01
Kino Construction
Steven D. Klein, M.D. ’98
Susan A. Klein, M.D. ’83
Mr. Eli J. Kleinman
William S. Knight, M.D. ’91
Jonathan J. Kramer, M.D. ’83
Lawrence A. Lewis, M.D. and
Jane Amler Lewis, Ph.D.
George Liakeas, M.D.
Leslie LiDonnici, M.D. ’78
Joan P. Liman, M.D. ’83, M.P.H. ’93
Efrat Z. Lobel-Katz, M.D. ’96
John Loike, Ph.D.
Ms. Taryn Looney
Albert B. Lowenfels, M.D.
Pamela Ludmer, M.D.
Carl B. Lundborg, M.D. ’67
Djoser M. Mack, M.D. ’21
Theresa A. Mack, M.D.
Heather D. Magnan, M.D. ’02 and John P. Magnan, M.D. ’02
Gregory H. Mahairas, M.D. ’59
Catherine C. Labiak-Maher, M.D. ’82
and James O. Maher III, M.D. ’82
John V. Mangieri, M.D. ’63
Manju Agarwal Charitable Fund
Craig W. Markert, M.D. ’73
Alan B. Marks, M.D. ’78
Jon O. Marks, M.D. ’76
Martell Landscaping, Inc.
Tali Reeis Martin, M.D., PC
Mr. Ronald Matten
Gerald J. Matthews, M.D. ’86
Maureen Matturri, M.D. ’66
Mr. Roger E. Mayer

Mitchell S. Kramer, M.D. ’85
Leonard B. Krich, M.D. ’65
Uday M. Kumbar, M.D. ’95
Edmund F. LaGamma, M.D. ’76 and Mrs. LaGamma
Col. and Mrs. Daniel F. Lally
Jeffrey M. Laskoff, M.D., P.A.
Jeffrey M. Laskoff, M.D. ’68
Dr. Edward and Renee Lebovics
Benjamin Y. Lee, M.D. ’02
Sharon R. Lee, M.D. ’89
Christine J. Leehealey, M.D. ’00
Mrs. Patricia S. Lefkowitz
Jesse A. Levin, M.D. ’09
Mrs. Ellen R. Lewis
Joseph R. Mazzaglia, M.D. ’71
McCartin Family Trust
Edward J. McCartin Jr., M.D. ’63
Alan D. McClelland, M.D. ’79
Kevin McDonough, M.D.
Thomas G. McElrath, M.D. ’59
Mrs. Judith McGreevy
Ms. Anastasia McPeak
Camille A. McPherson, M.D. ’03
Barry A. Meisel, M.D. ’70
Merck & Company, Inc., Corporate Giving Program
Keith P. Meslin, M.D. ’99
Bruce A. Miller, M.D. ’67
William Edward Miller, M.D. ’76
Tracey A. Milligan, M.D.
Michael A. Miranda, M.D. ’92
Richard L. Mones, M.D. ’71
James P. Mooney, M.D. ’56
Alan H. Morelli, M.D. ’82
Fernando Moreno, M.D. ’79
Kimberly L. Motta, M.D. ’97
Gary L. Munn, M.D. ’88
Carlos A. Munoz, M.D. ’08
Andrew M. Murphy, M.D. ’78
Karen M. Murray, M.D. ’99
Richard H. Nachtigall, M.D. ’57
Paul F. Nee, M.D. ’94
Mr. George F. Nestler
Aron Neuhaus, M.D. ’71
The Sara and Aron Neuhaus Fund, LLC
Zahid Niazi, M.D.
North Westchester Restorative Center
Mrs. Mary Norton
Stephen A. Obstbaum, M.D. ’67
Mr. Patrick O’Meara
Geralyn A. U. O’Reilly, M.D. ’94 and Keith J. O’Reilly, M.D. ’94
Edward Orff, Ph.D. ’99
George W. O’Rourke Revocable Living Trust
George W. O’Rourke, M.D. ’61
Valerie G. Ostrower, M.D. ’68 and Victor S. Ostrower, M.D. ’65
Kerri L. Palamara McGrath, M.D. ’06
Robert D. Pane, M.D. ’74
Debra M. Parisi, M.D. ’98
John C. Park, M.D.
Rachel A. Perla, M.D. ’95
John R. Person Charitable Trust
John R. Person, M.D. ’73
V. Rachel Phillips, M.D. ’79
PhyCare Solutions, Inc. Piazza, Inc.
Mrs. Teletta A. Piper
Jane M. Ponterio, M.D. ’81
Michael H. Popkin, M.D. ’74
Jodi L. Preminger, M.D. and Glenn M. Preminger, M.D. ’77
Laurence M. Raiford, M.D. ’77
Mr. John Ravitz
Douglas A. Rayner, M.D. ’61
RBT CPAs, LLP
Tali Reeis-Martin, M.D.
Laura M. Reich, M.D.
Margaret A. Reilly Living Trust
Margaret A. Reilly, Ph.D. ’81, M.S. ’78
Reinvent IT LLC
Padraic B. Reynolds, M.P.H. ’14
Riverdale Kosher Market
Frank R. Romano, Jr., M.D. ’76
Steven C. Romero, M.D. ’98
James E. Rosenthal, M.D. ’74
Kathleen M. Rossy, M.D.
Jason E. Roth, M.D. ’98
The Terri & Matty Russo Fund
Patrick Ryan
Ms. Meredith A. Rynkiewicz
Rodrigo L. Sanchez, M.D. ’02 and Mrs. Rodrigo Sanchez
Michael A. Sanford, M.D. ’94
Srivilliputtur G. Santhana Krishnan, M.D.

Debjeet Sarkar, M.D. ’05
Ellen Sawamura, Ph.D.
Donald E. Sawyer, M.D. ’70
Robert Schneider, M.D. ’69
Henry G. Schriever, M.D. ’60
Melvin L. Schulman, M.D. ’65
Schultz Eye Clinic
Gerald R. Schultz, M.D. ’63
Mr. and Mrs. Adolph D. Schulz
Alexandra M. J. Schulz, M.D. ’23
David Schwalb, M.D. ’84
Jerold Schwartz, M.D. ’56
Michal Schwartzman, Ph.D.
David F. Sciortino, M.D. ’78
William J. Semel, M.D. ’63
Russell A. Settipane, M.D. ’84
John P. Sheehy, M.D. ’75
Bruce E. Sherling, M.D. ’73
Neil D. Sherman, M.D. ’98
Tighe P. Shomer, M.D. ’77
Kelly A. Siano, M.D. ’11
Jeff S. Silber, M.D. ’95
Sarah S. Silver, M.D. ’97
Marc Silverman, M.D.
Marc M. Silverman M.D., P.C.
Andrew L. Simon, M.D. ’82
Stacey A. Simons, M.D. ’06
Anthony M. Sozzo, M.A., M.S.Ed.
Kathryn Spanknebel, M.D.
Mr. Franklin M. Steen
David A. Stein, M.D. ’75
John T. Stinson, M.D. ’75
Mr. Lawrence J. Stone
Street Paving, Inc.
Mr. and Mrs. Robert R. Strickland
Mr. Joel Sturm
Viktor P. Sulkowski, M.D. ’71
Deon K. Sutherland, M.D. ’02
Edward T. Swibinski, M.D. ’75
Marvin B. Tankel, M.D. ’80
The Tankel Charitable Fund
Mr. and Mrs. Kenneth Theobalds
Keith S. Tobin, M.D. ’85
Michael J. Trepal, D.P.M.
Mr. Michael A. Tugetman
Ms. Rachana Tyagi
Joel C. Ullman, M.D. ’63
Henry Velez, M.D. ’76
Libor Velisek, M.D., Ph.D.
Joseph S. Vetrano, M.D. ’70
Raissa Villanueva, M.D. ’05
James A. Walker, M.D. ’61
James J. Walsh, M.D. ’80
Thomas G. Webber, M.D. ’73
Mr. Shlomo Weintroub
William R. Weissman, M.D. ’65
Welch Family Charitable Fund
William J. Behrje Living Trust
Barry R. Witt, M.D. ’84
Michael T. Witt, M.D. ’99, M.P.H. ’99
Steven G. Wong, M.D. ’97
Douglas A. Woodburn, M.D. ’83
Richard B. Wu, M.D. ’05
Vincent J. Yakavonis, M.D. ’77
Yakov Consulting, LLC
Aaron E. Yancoskie, D.D.S.
Douglas L. York, M.P.H. ’91
Gerald W. Zaidman, M.D.
Mrs. Karen Zale
Robert W. Zavoski, M.D. ’82
Friends
$100 to $249
Anonymous – 18
Thomas J. Abbamont, M.D. ’85
Ms. Basilia Adams
AdvanceXpo
Barbara S. Akresh, M.D. ’75
Albert and Patricia Bajohr Revocable Trust
Lisa Jan M. Alcaraz, M.D. ’98
Olivia O. Alegre-Ipanag, M.D.
Richard Allen, M.D. ’65
Neelima Alluri, M.D.
Ms. Danielle Aloia
Salomon Amar, D.D.S., Ph.D.
Rudy T. Andriani, M.D. ’81
Leslie S. Anewenah, M.D. ’12
Ramaseshu S. Anne, M.D.
Daniel Z. Aronzon, M.D. ’73
Ms. Margaret Astrologo
Catherine C. Ayoub, D.P.T. ’12, M.P.H. ’13
Mohamed S. Aziz, M.D.
Kenneth S. Bannerman, M.D. ’75
Lori A. Iurato-Barazani, M.D. ’86 and Lance A. Barazani, M.D. ’86
Richard Beerman, M.D. ’80
The Benevity Community Impact Fund
George W. Benninger, M.D. ’66 Bentivegna Family Fund
Mr. Michael Bentivegna
Stewart R. Berliner, M.D. ’88
Michael R. Berman, M.D. ’70
Jeffrey S. Bisker, M.D. ’76
Kenneth S. Blatt, M.D. ’75
Edward J. Bloch, M.D. ’69
Michael S. Bloomstein, M.D. ’73
Lisa C. Bogdonoff, M.D. ’88
Edgar Borrero, M.D. ’81
Ms. Margaret Bradbury
Samuel J. Braitman, M.D. ’72
Ms. Karin Breen
Michael Brody, M.D. ’66
David J. Broza, M.D. ’89
Jack Bruder, M.D. ’82
Mr. Leonard and Mrs. Susie Buchan
Geny B. Burgos, M.D.
Felipe C. Cabello, M.D.
Mrs. Denise F. Cairns
Mr. John Calabrese
Ms. Jolene Calaf
Joseph J. Calandra, M.D. ’82
Dr. and Mrs. Ronald Caldwell
Michael Campion, M.D. ’82
Cardiovascular Innovations
Claire J. Carlo, M.D. ’85
Carlos Omenaca , M.D., FCCP, Vilmed, Inc.
Dana R. Deravin Carr, Dr.P.H. ’13, M.P.H. ’01
The James E. Carter Trust
James E. Carter, M.D. ’55
Paul S. Carton, M.D. ’63, F.A.C.S.
Joseph S. Cervia, M.D. ’84 and Denise L. Blumberg, M.D.
Paul B. Chaplin, M.D. ’79
Charlotte’s Tzedakah Fund
Jonathan Z. Charney, M.D. ’69
Michael Chavez Chase, M.D. ’72
Anthony P. Chatowsky, M.D. ’62
Ms. Bess Chazhur
Cynthia Chazotte, M.D. ’81
Mr. and Mrs. Henry Chew
Joseph Chiaramonte, M.D.
Neil T. Choplin, M.D. ’76
Ena Chow-Bell, M.D. ’94 and Gregory D. Bell, M.D. ’93
Karen Ann Clarke, M.D. ’96, M.P.H. ’94, M.S. ’93
Daniel Clement, M.D.
Lucy A. Civitello, M.D. ’80 and Howard J. Cohen, M.D. ’81
Kenneth Cohn, M.D. ’68
Dr. and Mrs. Wayne A. Colizza, M.D. ’17
Robert D. Collins, M.D. ’59
Roy H. Constantine, M.P.H. ’94, Ph.D.
Matthew S. Coons, M.D. ’86


Mr. Alan F. Cooper, M.P.H. ’91
Harvey E. Cooper, M.D. ’60 and Mrs. Lynn Cooper
William F. Courter Jr., M.D. ’74
Kay L. Cowan, M.D. ’87
Mrs. Irene Crasto-Bolin
Alfred J. Cretella, M.D. ’74
Diana J. Cunningham, M.L.S., M.P.H. ’00
Gerard P. Curran, M.D. ’95
Rachel Cyrlak, M.D. ’81 and Mr. Edward Cusnier
Arthur S. Cytryn, M.D. ’77
Brian G. Daggett, M.D. ’80
Christina M. Damo, M.S. ’10
Greta I. Daun, M.D. ’77
Kenneth J. Davis, M.D. ’62
Robert V. Dawe, M.D. ’75
Maria Audrie A. de Jesus, M.D.
Barry J. Decker, M.D. ’82
Vincent P. DeGennaro, M.D. ’85
Thomas J. Degnan, M.D. ’56
Enzo V. DiGiacomo, M.D. ’65
Jayne M. Doherty, M.D. ’86
Mr. and Mrs. David Domreis
Floyd J. Donahue, M.D. ’60
J. Franklin Donaldson, M.D. ’54
Ellen P. Donshik, M.D. ’68 and Peter C. Donshik, M.D. ’68
James E. Doran, M.D. ’75
Doyle Revocable Trust
Donald E. Doyle, M.D. ’67
William F. Doyle, M.D. ’62
Herbert M. Dreyer, M.D. ’76
Martin B. Duke, M.D. ’63
Michael J. Duran, M.D. ’78
Harsha V. Duvvi, M.D., M.P.H. ’99, FICAE
Steven M. Erlanger, M.D. ’68
Richard M. Evans, M.D. ’84
Mr. and Mrs. Robert S. Faircloth
John Farrelly, D.V.M., M.S. ’10
Allen Fay, M.D. ’61
Lloyd J. Feigenbaum, M.D. ’72
Seymour H. Fein, M.D. ’74
Kalmen A. Feinberg, M.D. ’64
William N. Fenney, M.D. ’79 and Mrs. William Fenney
Craig Allen Fenton, M.D. ’68
Robert S. Ferretti, M.D. ’65
Alex E. Fijman, M.D. ’00
Joel G. Fischgrund, M.D. ’78
William K. Flannery, M.D. ’93
Peter J. Foldes, M.D.
Matthew C. Frankel, M.D. ’78
Mr. and Mrs. John Freund
Bruce J. Friedman, M.D. ’76
Stanley N. Friedman, M.D. ’68
Steven I. Friedman, M.D. ’76
James A. Fugazzi, M.D. ’00
Ian A. Gale, M.D. ’70
Gary A. Gallo, M.D. ’63
Veena S. Gangasani, M.D.
James P. Gardner, M.D. ’78
Jeffrey H. Gelgisser, M.D. ’77
Geny B. Burgos M.D., Inc.
George B. Kurian Fund
Victor Giamos, M.D.
Andrea C. Giardina, M.D. ’66
Scott A. Glasser, M.D. ’86
Edward H. Glenn, M.D. ’64
Ira D. Glick, M.D. ’61
Kenneth H. Goldblatt, M.D. ’72
Eric F. Gould, M.D. ’70
Michael S. Graham, M.D. ’07
James R. Greenbarg, M.D. ’89
Mr. Aryeh Greenberg
Neil T. Greenidge, M.D. ’66
Michelle P. Greenman, M.D. ’19
Jason R. Grossman, M.D. ’10
Ms. Bonnie Gurran-Heindl and Mr. Paul Heindl
Susan D. Ribeiro Guthrie, M.D. ’96
Hal Gutstein, M.D.
Naushaba S. Habib, M.D.
Bruce A. Hagadorn, M.D. ’89
Ms. Stephanie L. Harley
Gehrig L. Harris III, M.D. ’04
Frederick Whiting Hays, M.D. ’60
William A. Healy Jr., M.D. ’61
Craig R. Heim, M.D. ’70
Leo A. Heitlinger, M.D. ’78
Louis I. Heller, M.D. ’81
Paul G. Heyslinger, M.D. ’76
Mark E. Higgins, M.D. ’94
Robert D. Hirsch, M.D. ’61
Barbara M. Hisler, M.D. ’83
Stuart M. Hochron, M.D. ’77
Michael D. Holden, M.D. ’85
Robert C. Holland, M.D. ’84
John S. Hou, M.D. ’97
Scott W. Hoyer, M.D. ’75
Eric L. Hsu, M.D. ’97
JunLing Huang, Ph.D.
John T. Hughes, M.D. ’82
Kelly A. Hutcheson M.D., M.B.A., FAAO
Abebe S. Imiru, M.D.
Edward I. Jacobson, M.D. ’75
Vanessa L. Jeffers, M.D. ’89

Susan M. Jensen, M.D. ’77
John Franklin Donaldson
Erica C. Jones, M.D. ’92
Robert G. Josephberg, M.D.
Samuel D. Kahnowitz, M.D. ’76
Elizabeth M. Peters-Kaiser, M.D. ’91 and Richard C. Kaiser, M.D. ’91
David B. Kaminsky, M.D. ’70
Mr. Seymour Kaplan
Cheryl A. Karcher, M.D. ’92
Kenneth G. Kasses, Ph.D. ’74
Mrs. Doris Katz
Frederic Russell Kellogg, M.D. ’74
Ahmad A. Khan, M.D. ’99
Kathleen M. Kicsak-Baumgartner, M.D. ’91
Adrian W. Klufas, M.D. ’80
Kenneth Knapp, Ph.D.
Carol A. Kovis, M.P.H. ’98
Mr. James A. Kraus
Howard R. Krauss, M.D. ’77
Charles M. Krowicki, M.D.
Christopher J. Kruger, M.D. ’86
Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64
George B. Kurian, M.D.
Eileen M. Kushner, M.D. ’85
Jonathan S. Kusnitz, M.D. ’84
Ignazio G. La China, M.D.
Ignazio G. La China, M,D., PA
Mr. Rob Lancia
Michael L. Lapkin, M.D. ’65
Mr. Eric Lee
Sheryl L. Leff, M.D. ’85
Stuart D. Lestch, M.D. ’66
Mark Levey, M.D. ’62
George A. Levine, M.D., P.A.
George A. Levine, M.D. ’65
Peter D. Levit, M.D. ’76
David C. Lewandowski, M.D. ’15
Boyi Li, M.D. ’21
Harold M. Libatter, M.D. ’80
Janet C. Lin-Torre, M.D. ’85
Delong Liu, M.D. and Min Xu, M.D.
Donna J. Lombardi-Goldfus, M.D. ’93
Milton L. Lorig, M.D. ’77
Ellen Loughran, Ph.D.
Marian Louis, M.D. ’78
Hector F. Lozano, M.D., M.P.H.
Mr. Robert Madden
William S. Maistrellis, M.D. ’63
Mario S. Malonzo, M.D.
Stephen H. Marcus, M.D. ’67
Maurice E. Markewich, M.D. ’70
Marvin A. Roth, M.D., P.A.
Lawrence R. Marwill, M.D. ’63
Lawrence and Louise Marwill
Charitable Fund
Nicole M. Masian, M.D. ’08
Jeffrey S. Mason, M.D. ’75
Harvey G. Masor, M.D. ’65
Frederick H. Mattes, M.D. ’74
Suzanne E. McElligott, M.D. ’03
Monica McHenry, Ph.D., CCC-SLP
George R. McKendall, M.D. ’84
Peter J. McLoughlin, M.D. ’58
Edward J. Messina, Ph.D. ’73
Harold Michlewitz, M.D. ’71
Samuel I. Miles, M.D. ’74
Barry A. Minora, M.D. ’91
Mr. Thomas Modero
Roy Christopher Monsour, M.D.
Jay More, M.D. ’87
Louis J. Morledge, M.D. ’90
Michelle A. Multz, M.D. ’87
Mr. and Mrs. Mitchell A. Mund
James J. Murdocco, M.D. ’65
Padmini Murthy, M.D., M.P.H., M.S.
Adelaide G. Nardone, M.D. ’83
Mrs. Jane Newman
The Samuel Newman Charitable Foundation
Lysa N. Nguyen, M.D. ’01
Efthemia Nicolopoulos, M.D. ’01
Jack D. Norman, M.D. ’63
Sara Noroozkhani, M.D. ’06
Mrs. Michelle Novotny
Mr. and Mrs. Stephen J. O’Connor
M. Kevin O’Connor, M.D. ’68
Anthony O. Ogunjimi, M.P.H. ’90
Peter G. O’Hare III, M.D.
Carlos L. Omenaca, M.D.
O. Opam, M.D.
Brian R. Osler, M.D. ’18
Mr. and Mrs. Robert P. Osler
Alan J. Ostrowe, M.D. ’66
Punit S. Parasher, M.D. ’04
Mr. Thomas A. Parrinello
Gregory K. Paschal, M.S. ’23
Mr. and Mrs. Bruce Pauls
Henry L. Payne, M.D. ’79
Robert A. Peinert, M.D. ’70
Nancy Castellucci Peters, M.D. ’93
Lee J. Phillips, M.D. ’85
Pneuma Foundation
David A. Printz, M.D. ’83
Allen S. Prober, M.D., ’11
J. Michael Purcell, M.D. ’66
Mr. Prabhakar Putheti
Ira L. Raff, M.D. ’64
Mohammed S. Rais, M.D.
Alfred B. Randall, M.D. ’70
Norman A. Ravski, M.D. ’78
Harvey A. Reback Charitable Foundation
Harvey A. Reback, M.D. ’61
Lesley Rechter, M.D. ’76
Regintex Insurance Brokerage
Kathy Reilly Fallon, M.D.
Charles R. Reina, M.D. ’74
Merle S. Robinson, M.D.
Stephen H. Rogers, M.D. ’62
Reuben D. Rohn, M.D. ’71
Nancy Roistacher, M.D. ’75
Howard D. Rosenberg, M.D. ’76
William B. Rosenblatt, M.D. ’73
Stuart A. Rosenthal, M.D. ’62
Malcolm Z. Roth, M.D. ’82
Marvin A. Roth, M.D. ’62
Ronald R. Roth, M.D. ’73
Punyabrata Roy, M.D.
William Rymer, M.D. ’72
Alan S. Sacerdote, M.D. ’74
Jerome E. Sag, M.D. ’72
Nicholas G. Sakellariou, M.D. ’94
Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
Sanford Medical Corporation
Rodrigo L. Sanchez, M.D., PC, Inc.
Roderick M. Santos, M.D. ’93
Mr. Brian J. Savarese
Robert G. Scharffenberg, M.D. ’86 and Mrs. Robert Scharffenberg
Neil R. Scheier, M.D. ’85
Kari R. Schlessinger, M.D.
Michael B. Schoenwald, M.D. ’69
Eric H. Schultheis, M.D. ’88
Schultz Family Giving Fund
Richard D. Schultz, M.D. ’88

Ms. Nina A. Schwab
Martin A. Schwartz, M.D. ’75
Denise B. Sepe, M.D. ’83 and Carl J. Koenigsmann, M.D. ’84
Michael A. Sergi, M.D. ’02
Denise Serrano-Eanelli, Dr.P.H. ’19
Christina T. Wong Sheridan, M.D. ’00
Mr. and Mrs. James A. Siano
Jeffrey J. Silbiger, M.D. ’81
James R. Simcoe, M.D. ’84
Sloan – Gong Family Charitable Fund
Victor S. Sloan, M.D. ’89 and Ms. Sandra Gong
Alessandro Smeraldi, M.D.
Alyson M. Smith, M.D. ’03
Edward L. Snyder, M.D. ’73
Brian K. Solow, M.D. ’82
John C. Somberg, M.D. ’74
Xiaosong Song, M.D.
Faye E. Spector, M.D. ’79
Lawrence M. Spergel, M.D. ’71
Peter H. Stein, M.D. ’09
Leonard Stern, M.D. ’75 and Joan F. Poll, M.D. ’76
James V. Stillerman, M.D. ’77
Mr. Ed Stout
Neil T. Streisfeld, M.D. ’79
James M. Sudimack, M.D.
Mr. I-Hsing Sunm
Michael H. Swirsky, M.D.
Lindsay S. Tan, M.D. ’82
Tanchoco Children and Adolescent Clinic
Imelda T. Tanchoco, M.D.
Dr. Jason and the Honorable Lois Tanzer
Nancy S. Tarlin, M.D. ’86
The Trambert and Shashou Fund
Bruce R. Thompson, M.D. ’80
Col. Robert Francis Todaro, M.D., M.P.H. ’80
Mark Tomback, M.D., P.A.
Mark Tomback, M.D. ’78
John S. Train, M.D. ’67
Jonathan J. Trambert, M.D. ’77
Jeffrey S. Trilling, M.D. ’73
Shiu-Lin Tsai, M.D. ’91
Oya Tugal, M.D.
Salvatore R. Tuzzo, M.D. ’66
Joseph A. Tyburczy Jr., M.D. ’73
John N. Van Dam, M.D. ’72
Jack H. Vitenson, M.D. ’65
Joseph F. Voli, M.D. ’92
Mr. Jerold Volk
Lynne Voutsinas, M.D. ’83
Mrs. Leslie Ann Wade
Daniel J. Waintraub, M.D. ’13
Joseph P. Walker, M.D. ’74
Joseph P. Walker Revocable Trust
James M. Wallquist, M.D. ’66
Shu H. Wang, M.D. ’93
Xing J. Wang, M.D.
Ying Wang, M.D. ’17
Daniel E. Wapner, M.D. ’82
Charles L. Weinberg, M.D. ’65
Lora Weiselberg, M.D. ’75
Mark S. Weiss, M.D. ’78
David Wellman, M.D.
Princess Wells, D.P.T. ’10
Graham F. Whitfield, M.D. ’76, Ph.D.
Carol A. Whyzmuzis, Ph.D., M.S. ’94
Aimi Y. Will, M.D. ’98
Gregory T. Williams, M.D. ’86
Mr. George Wimpfheimer
Ms. Yvette Woods
Xiaochun Zhang Inc
Philip M. Yam, M.D. ’11
Jenny F. Yang, M.D. ’03
Hyun J. Yoo, M.D.
Irini M. Youssef, M.D.
Yusif Medical Services LLC
Mahrouf M. Yusif, M.D.
Shelley A. Zara, M.D. ’73 and Harvey D. Zara, M.D. ’73
Robert M. Zbeda,M.D. ’15
Donna A. Zeide, M.D.
Robert C. Zeller, M.D. ’71
Michael Zhang, M.D., M.S. ’00
Xiaochun Zhang, M.D.
Zoller Giving Fund
Robert C. Zoller, M.D. ’77
WAYS TO GIVE

With a proud history of humanism and respect, NYMC has been educating exceptional health care leaders for more than 160 years. Your contributions allow us to provide scholarships for our extraordinary students, recruit and retain the best faculty, conduct cutting-edge research, invest in technology and maintain state-of-the-art instructional and learning facilities. We encourage you to explore nymc.edu/give for more information.
Areas where you can make a difference:
• Annual Fund
• Contribute to an existing student scholarship, research, or academic fund
• Establish an endowment fund
• Make a planned gift
• Participate in the annual Founder’s Dinner
• Host a fundraising/ cultivation event in your area
• Days of Giving
• Reunion Weekend
• Medical Kit Initiative Support an area that inspires you. Contact the Office of Development and Alumni Relations at development@nymc.edu or call (914) 594-2720.

+ Deceased
Legacy Society
The Legacy Society of New York Medical College recognizes donors who have made provisions for the College in their wills or through other planned gifts, as well as those donors whose estate has made a gift to the College.
These members have named New York Medical College as a beneficiary in their estate plans/wills as of December 1, 2024:
Anonymous – 5
Michael S. Alexander, M.D. ’78
Ralph Almeleh, M.D. ’76
Michael Auerbach, M.D. ’75
Doris Bate, M.D. ’50
Augusta H. Belmonte, M.D.
Barbara Bitsko
Paul H. Brenner, M.D. ’61
Phillip Capozzi Jr., M.D. ’96
James E. Carter, M.D. ’55
Neil T. Choplin, M.D. ’76
Mrs. Delores DelBello
Robert Fabricant, M.D. ’60
Emalie and John D. Feerick
Dr. and Mrs. Denis J. Frank ’61
Mark J. Friedman, M.D. ’71
Howard D. Harrison, M.D. ’61
Col. Paul Heller, M.D. ’68 and Joanne C. Hennessey
Steven P. Kahn, M.D. ’67
Maureen Kennedy, Dr.P.H. ’11, M.S. ’03
Mrs. Mary M. Kogut
Bradley S. and Ruth Friedman Kuhn
Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64
Annette E. Kussmaul, M.D. ’93
Mrs. Diane L. Levere
Carl M. Marchetti, M.D. ’60
Mr. Joel Margolis
Joseph P. Merlino, M.D. ’78, M.P.A.
Mark S. Noveck, M.D. ’80
Lee J. Phillips, M.D. ’85
Harvey A. Reback, M.D. ’61
Kenneth M. Rose, M.D. ’88
Neil R. Scheier, M.D. ’85
John H. Seward, M.D. ’61
Neil S. Silber, M.D. ’75
Victor S. Sloan, M.D. ’89
Theresa A. Smith, M.D. ’56
John T. Stinson, M.D. ’75
Patricia C. Villamena, M.D. ’77
Anna M. Ward, M.D. ’85
Steven Weissberg, M.D. ’66
Eric Weston, M.D. ’71 and Barbara Baccari, Esq.
Since 1987, the College has received more than $24.6 million in contributions from the estates of these individuals:
Alma Allen
Anne T. Barbieri
Herbert and Sylvia Berger
Marcelle B. Bernard, M.D. ’44 and Edmund D. Marinucci, M.D. ’44
Barbara Bess
Charles E. Birch, M.D. 1891
Alice H. Burgoyne
Michael Caruso
Nathan W. Chaikin, M.D. and Mrs. Frances Chaikin
Karlene Marie Chin, M.D. ’80
Herrlich Ciatto
Mary E. Clarke
William P. Coats, M.D. ’53
Wendy E. Cohen, M.D. ’70
Brian J Collins, M.D. ’61
Sidney L. Cramer, M.D. ’41
Mabelle A. Cremer, M.D. ’53 and Martin E. Silverstein, M.D. ’48
Lewis A. Dalburg Jr., M.D. ’58
R. Margarita De Santis, M.D. ’59
Margot Ammann Durrer, M.D. ’49
Earl H. Eaton Jr., M.D. ’44
Walter G. Elliott, M.D. ’51 and Mrs. Shirley Elliott
Eva Feld
Miguel Figueroa, M.D. ’48 and Mrs. Lillian Figueroa
Walter E. Fleischmann
Robert W. Fredrickson, M.D. ’51
Col. Saul Fromkes
Francis J. Geary, M.D. ’64
Arthur Ginsburg, M.D. ’58
Gerhard J. Haas, Ph.D.
Seymour Halpern, M.D.
Edith Har-Esh, M.D.
Adriel and Evelyn H. Harris
Catherine N. Hinterbuchner, M.D.
Arno R. Hohn, M.D. ’56
Dora May Holmes
Constance Ives Foster
Gerald H. Kass, M.D. ’51
Paul Kay, M.D. ’44
William J. Kelley, M.D.
Joseph B. Kiel, M.D. ’31
Janice Kiss
Solomon D. Klotz, M.D. ’37 and Mrs. Harriett Klotz
Henry V. Kogut, M.D. ’43
Salvatore LaCorte, M.D. ’30
Guy Lepore
Anna Lowin
Maurice L. Malins
David K. Marcus, M.D. ’32
Charles D. McCullough, M.D. ’58
Frederick R. Meeks, M.D. 1907
Matthew S. Mickiewicz, M.D. ’41 and Mrs. Helen Mickiewicz

Laura G. Morgan, M.D. ’49
George R. Nagamatsu, M.D. ’34 and Kazuko Nagamatsu
Ellen J. Nolde
James F. X. O'Rourke, M.D.
Richard A. Perry, M.D. ’60
Eileen H. Pike, Ph.D.
Andrew S. Ranier, M.D. ’46
John Louis Rie Jr.
Mrs. Elaine Rosenberg
William S. Rosenthal, M.D.
Harvey Rosner, M.D. ’63
Mark S. Rothenberg, M.D. ’30
William D. Ryan, M.D. ’53 and Mrs. Kathryn X. Ryan
Ethel Esther Sandler
Tamiko Sato, M.D.
Ruth Saunders
Elaine L. Schulman, M.D. ’65
Louis N. Scotti, M.D. ’58
Louise O. Smith
Roy Gene Smith, M.D. ’61
Sander V. Smith, M.D. ’35 and Mrs. Helen W. Smith
Vincent E. Smith, M.D. ’61
Sidney Stahler, M.D.
Samuel Steinholtz, M.D. ’28
Dorothy S. Stengel
Theodore R. Struhl, M.D. ’42 and Mrs. Ruth Struhl
Hiroshi J. Tazaki, M.D., Ph.D.
Ciro S. Tarta, M.D. ’43
Roscoe W. Teahan, M.D. 1917
Joseph F. Tedesco, M.D. ’37 and Mrs. Vera L. Tedesco
Solomon Till, M.D. ’25 and Mrs. Elizabeth Till
Ruth E. Trager
Gertrude Tromp
Roy C. Upham, M.D. 1901 and Sarah Upham
William F. Westlin III, Ph.D. ’89, M.S. ’87
S. R. Wiener
Robert M. Wittenberg, M.D. 1919
Percy C. Zanger, M.D. ’49
Morris Zeichner, M.D. ’33
Tributes and Memorials
In memory of Sumita Adhya, M.D ’06
Victoria L. Mango, M.D. ’06
In memory of Harvey Aiges, M.D. ’71
Eric H. Schultheis, M.D. ’88
In memory of Melvin Amler, D.D.S.
Robert W. Amler, M.D., M.B.A. and Sherlita Amler, M.D.
Mrs. Jennifer Amler Goldstein
Ms. Caroline Mechanick
In memory of Mr. and Mrs. Salvatore Andriani
Rudy T. Andriani, M.D. ’81
In memory of Nicholas Antoszyk, M.D. ’48 and Mrs. Corinne Antoszyk
Dr. and Mrs. Andrew Antoszyk
In memory of Mr. Guillemo and Mrs. Leticia Babiera
Gildy V. Babiera, M.D. ’91
In memory of Dr. and Mrs. Asterio A. Belmonte
Augusta H. Belmonte, M.D.
In memory of Dr. and Mrs. Robert Bernot
Mrs. Carol Bernot
In Memory of Libby Bogel, M.D. ’78
David Andrews, M.D. ’78 and Mrs. David Andrews
Andrew M. Murphy, M.D. ’78
In honor of Mr. and Mrs. John H. Bonslaver
Jason S. Bonslaver, M.D. ’06
In honor of Derek Borsody, M.D.
Karl J. Borsody, M.D. and Jaleh Eslami- Borsody, M.D. ’94
In memory of Mrs. Joan Brodsky
Jules Brodsky, M.P.H. ’90
In celebration of Molly Broe
Lisa Borg, M.D. ’80
In memory of Edward T. Butler, M.D. ’67 Mrs. Joi Butler

In honor of Vince Capanelli, M.D.
Hal Gutstein, M.D.
In memory of Giuseppe and Margaret Cervia
Joseph S. Cervia, M.D. ’84 and Denise L. Blumberg, M.D.
In honor of Penelope and Scarlett Chew
Qwie T. Chew, M.D. ’65
In memory of Tony Cohen, M.D. ’66
Gary R. Donshik, M.D. ’66
In memory of Archie Cohn, M.D. ’27
Kenneth Cohn, M.D. ’68
In memory of Mr. Joseph Corey
Stephen L. Rubin, M.D. ’70
In celebration of Stephen A. Corvini, D.P.T. ’15
Ms. and Mr. Anthony Corvini
In honor of Mr. Maxwell A. Cusnier
Rachel Cyrlak, M.D. ’81
In memory of Richard James Davis
Robert A. Davis, M.D. ’74
In memory of Donald W. Delahanty, M.D. ’51
Kevin C. Delahanty, M.D. ’84
In memory of Ms. Susan M. DiFabio
Dominick F. DiFabio, M.D. ’71
In memory of Ms. Kelly Doyle
Donald E. Doyle, M.D. ’67
In Memory of Joseph F. Dursi, M.D. ’59
Ms. Margaret Astrologo
Adelaide G. Nardone, M.D. ’83
In memory of Martin J. Frank, M.D. ’70
Robert Crootof, M.D. ’70 and Mrs. Robert Crootof
In honor of Sarise Freiman, M.D. ’76
William Edward Miller, M.D. ’76
In honor of Richard A. Frieden, M.D. ’84
Mrs. Miriam Frieden
In Honor of Ann Furtado, M.D.
James M. Sudimack, M.D.
In memory of Donald Gemson, M.D. ’78
Anita Grover, M.D. ’78
In memory of Peter J. George, Esq.
William Cristo, M.D. ’71
In memory of William Glatt M.D. ’62
Daniel J. Glatt, M.D., M.P.H. ’92
In memory of Ziva Goldstein
Michael S. Goldstein, M.D. ’72
In memory of Jack L. Hagadorn, M.D.
Bruce A. Hagadorn, M.D. ’89
In honor of Edward C. Halperin, M.D., M.A.
Kathy Reilly Fallon, M.D.
Bob and Laura Gutman
In memory of Camille J. Harriott
AdvanceXpo
Rigo Harrasme
Ms. Camille Harriott
Mario Harriott
Victoria Harriott
Ms. Lucy Molina
Mr. Carl Pitt
In memory of Sharah Harris
Gehrig L. Harris III, M.D., ’04
In memory of Morris Harwood, M.D.
Robert A. Harwood, M.D. ’62
In honor of Matthew Hau
Eric L. Hsu, M.D. ’97
In memory of Albert Hong, M.D. ’05
Debjeet Sarkar, M.D. ’05
In memory of Mr. and Mrs. Jamadagni
Sandeepa Utpat, M.D.
In memory of Kenneth Juechter, M.D. ’68
Ms. Sybil J. Attardi
Robert G. Josephberg, M.D.
James F. McGroarty, M.D. ’68
In memory of Mayer S. Kaplan, M.D. ’33
Jeffrey M. Kaplan, M.D. ’70
In honor of Saul Kaplan, M.D.
Peter N. Bogdan, M.D. ’64
In memory of Howard J. Kline, M.D. ’58, FACC
Ellen Sawamura, Ph.D.

In memory of Martin L. Lapkin, M.D. ’71
Alan R. Altman, M.D. ’71
In memory of Helen Lau
Eric C. Fok, M.D. ’93
In memory of Louis H. Lefkowitz, M.D. ’64, FACOG, FACS
Mrs. Patricia S. Lefkowitz
In honor of Norman L. Maron, M.D. ’70
Michael R. Berman, M.D. ’70
In memory of Shearwood J. McClelland, M.D.
Rachael M. Sampson, M.D., ’11
In memory of James Miglietta, M.D. ’81
Kenneth D. Kushner, M.D. ’81

In celebration of Racheal Miningham-Monsour
Roy Christopher Monsour, M.D.
In memory of Arthur Mones
Richard L. Mones, M.D. ’71
In honor of Augustine Moscatello, M.D.
Alan S. Berkower, M.D., Ph.D.
In memory of Mary Ann L. Nadler
Jerry L. Nadler, M.D., MACP, FAHA, FACE
In memory of General and Mrs. Shirin Dil Khan Niazi
Zahid Niazi, M.D.
In memory of Ann Norman
Jack D. Norman, M.D. ’63
In memory of Peter A. Philips, M.D. ’63
Ellen P. Donshik, M.D. ’68
In memory of Martin Pine, M.D. ’70
Alfred B. Randall, M.D. ’70

In memory of Albert A. Pineda, M.D. ’63
Barbara Pineda, M.D.
In memory of Frank J. Piper, M.D. ’58
Mrs. Teletta A. Piper
In honor of Louis G. Raff, M.D. ’24
Mrs. Tobi Raff
In honor of Andres Ramirez, M.D.
Ms. Jenny Ramirez
In memory of Adnarayana Satyamanoheri
Ravipati
Gowtam Ravipati, M.D.
In memory of Vincent F. and Mildred Reina
Charles R. Reina, M.D. ’74
In celebration of Margaret Rice
Michael D. Holden, M.D. ’85
In memory of Alice Rickman
Sharon R. Lee, M.D. ’89
In memory of Nicole Rodriquez
Mrs. Denise F. Cairns
In memory of Bill Roe
Matthew C. Frankel, M.D. ’78
In honor of Alan Rosenthal, D.M.D.
Bettina and Spencer Waxman Philanthropic Fund
In memory of Dr. and Mrs. Samuel H. Rubin
Adam D. Rubin, M.D. ’00
In memory of Thelma (Terri) Russo
Laurence Raiford, M.D. ’77
In honor of Carolyn Scharffenberg
Mrs. Robert G. Scharffenberg and Robert G. Scharffenberg, M.D. ’86
In honor Seymor Schlussel, M.D. ’51
Jack D. Norman, M.D. ’63
In memory of Jared E. Schulman, M.D. ’04, M.P.H. ’04
Melvin L. Schulman, M.D. ’65
In memory of Eugene Schwalb, M.D.
David Schwalb, M.D. ’84
In memory of Guy A. Settipane, M.D. ’57
Russell A. Settipane, M.D. ’84
In honor of Mr. and Mrs. Michael Silber
Jeff S. Silber, M.D. ’95
In honor of Christy Strickland, M.D. ’06
Mr. and Mrs. Robert R. Strickland
In honor of Morgan Yale Swirsky, M.D. ’39
Michael H. Swirsky, M.D.
In memory of N. Noel Testa, M.D. ’66
Nicholas Testa, M.D. ’01
In memory of Seymour Tobin, M.D. ’52
Keith S. Tobin, M.D. ’85
In honor of Michelle P. Tomassi, M.D. ’05 and Marco Tomassi, M.D. ’03
Mrs. Patricia M. Tomassi
In celebration of Nora Traub
Mr. and Mrs. Robert S. Faircloth
In honor of Matthew Urban
Sherry B. Ellis, M.D. ’85
In memory of Dr. Felix and Hannah Wassermann
Michael S. Alexander, M.D. ’78
In memory of Kenneth Witt
Barry R. Witt, M.D. ’84
In memory of Ivy Feder-Wohl
John M. Feder, M.D. ’87 and Annette Cohen, M.D.
In memory of Paul K. Woolf, M.D.
Christina T. Wong Sheridan, M.D. ’00
In honor of Mr. Walter and Mrs. Mary Jane Yacynych
Robert M. Yacynych, M.D. ’88
In memory of Wilson Young, M.D. ’07, Ph.D. ’07, M.S. ’99
Ms. Taryn Looney
Ms. Meredith A. Rynkiewicz
Alessandro Smeraldi, M.D.
Alyson M. Smith, M.D. ’03
Mrs. Bonnie Young
Mr. Norman Young
In honor of Reinhard Zachrau, M.D.
Yun Shin Chun, M.D. ’99
In memory of Jeffrey M. Zale, M.D. ’75
Mrs. Karen Zale
In honor of Joseph and Gila Zelazny
Daniel Zelazny, M.D.

We have made every effort possible to provide a full and accurate list of donors to NYMC from July 1, 2023 through June 30, 2024. If we have omitted or improperly listed your name, please accept our apologies. If you detect an error, please contact our Office of Development and Alumni Relations at (914) 594-2720 or email us at development@nymc.edu, so we may correct our records.
Alumni Council
Stay Connected. Grow Your Network. Make an Impact.

NYMC Alumni Council
A Lifelong Community
Under the direction and leadership of the Office of Development and Alumni Relations, the New York Medical College (NYMC) Alumni Council is the official alumni organization that connects you to a lifelong network, career advancement resources, and exclusive opportunities. As a graduate of the School of Medicine, Graduate School of Biomedical Sciences, or School of Health Sciences and Practice, you’re automatically part of this vibrant alumni network.
NYMC Connect
Your Exclusive Online Hub
Stay connected, get inspired, and expand your professional circle with NYMC Connect, our online community.
NETWORK with fellow alumni, faculty, residents, and students.
SHARE personal and professional updates.
ENGAGE in virtual discussions and mentorship opportunities.
ACCESS exclusive job postings and event listings.
Ready to Connect? Get involved now nymcconnect.org
Alumni Events
Bringing NYMC to You
The NYMC Alumni Council hosts on-campus gatherings and nationwide meetups. We bring alumni together in key regions. Don’t miss these chances to reconnect, reminisce, and create new memories.
Alumni Council Meetings
Your Voice Matters
Want to get involved? Attend virtual or inperson Alumni Council meetings. Email us at alumrelations@nymc.edu or call (914) 594-2720 to be added to the invitation list.
Join Us & Shape the Future of NYMC
Your support and participation help us mentor the next generation of health care professionals and keep the NYMC spirit alive. Let’s make a difference—together.



Vincent Yang, School of Medicine Class of 2027, captured the spectacular display of Northern Lights over the New York Medical College campus on October 10, 2024.
