KIDNEY
The magazine of the National Kidney Federation





A warm welcome to all our readers as we move from Autumn into Winter.
There’s a touch of festivity in this issue along with some stirring patients’ stories and a great variety of articles, which I hope you find stimulating and interesting. Some of the themes we have covered over the year are touched on – David Stiff’s story as donor to his daughter Hattie whose story we published a couple of years ago, James and his thoughts on travelling, and Ali’s story following her journey and her talk at the conference just last month.
Importantly we have an article on the NKF’s visit to Downing Street to raise awareness of kidney disease and to encourage government to raise its status as a health priority. There’s also information about the NKF’s webinar series and other opportunities to get involved. There’s also fascinating insight into the day of a living donor co-ordinator as well as a behind the scenes view of the NKF’s remarkable Helpline.
I hope you are all able to enjoy the festive season with your families and friends - which I know seems a long way off, but it does have a habit of creeping up on us. I got in the mood with my baking for this issue!
Warm wishes,
Annie Taylor Editor
kidneylife@kidney.org.uk
NKF OFFICERS
Chairman – David Coyle
Co Vice Chair – Caryl Bryant
Co Vice Chair – Tarsem Paul
Treasurer – Geoff Downes
Secretary – Brian Child
NKF TEAM
Andrea Brown – Chief Executive
Pete Revell – Head of Marketing & Fundraising
Donna Blizard – Office Manager
Sharney Warren – Communications and Marketing Officer
Fiona Broomhead – Senior Office Administrator
Joe Rutter – Social Media and Website Coordinator
Lucy Vasiliou – Policy and Public Affairs Manager
Heather Mooney – Accounts Administrator
Chris Talbot – Membership Development Lead
Linda Pickering – Helpline Advisor
Stephen Emmerson – Helpline Advisor and Peer
Support Coordinator

For 26 years the NKF’s Helpline has been the UK’s largest provider of kidney-related medical information leaflets, offering over 200 titles written by experts for patients and carers. Stephen Emmerson and Linda Pickering are the team behind the NKF’s Helpline, available to provide help and support to kidney patients and their families every weekday. I caught up with them to find out more about their work.
1 Tell me a bit about your team
I’m Stephen, a twice-transplanted kidney patient who has also been on haemodialysis, and Linda is a former carer for her late husband who had kidney disease. Linda’s perspective is unique and she also has experience as an advocacy officer for kidney patients.
2 How many different leaflets are available for kidney patients and their families/carers?
We have over 200 patient information leaflets covering every aspect of living with kidney disease. We have easy read patient information booklets too. We create information packs for CKD Stage 3, dialysis, pre and post transplant, exercise and diet.
3 How many information leaflets do you send out each year?
Since January we have printed and distributed 35,500 patient information leaflets for hospital renal departments and dialysis units across the UK. We also provide leaflets for Kidney Patient Associations with their own logos on.
The NKF’s early detection campaign has resulted in us contacting Integrated Health Boards and GP practices. We have sent 12,000 leaflets to GP practices. We print all the NKF materials for conferences and adding all this together we’ve printed around 50,000 bits of information this year.
4 How many calls do you receive on an average day?
We usually have 10 to 15 calls a day which come through to the freephone number - 0800 169 0936 which we answer straightaway. We respond to e-mail enquiries and to the live chat facility on our website - www.kidney.org.uk
5 Do the leaflets take up a lot of space or do you print materials as requested?
The Helpline prints on demand in the office so we can usually send orders out the same day.
6 Are leaflets regularly reviewed and updated so that recipients can be sure they are getting the latest information?
Yes, each leaflet is reviewed every three years by nephrologists, renal pharmacists, transplant specialists, dietitians and other professional people who write or review a subject. The NKF has been awarded the PIF TICK – the UK’s only assessed quality mark for health and care information.
7 Which are the most popular leaflets?
The most popular resources are for renal hospitals, the pre and post-transplant leaflets, and dialysis leaflets. For GP practices, the most popular is CKD stage 3 information.
8 What’s the question you get asked most by patients?
The most common question we have at the Helpline is from people who do not understand their CKD stage or what their eGFR means. People are often told they have CKD but do not know anything about it.
9 You have been running the Helpline for 8 years Stephen, and Linda for four years. What do you get out of it?
The most rewarding thing about the Helpline is that you are there on the end of the phone to support patients and carers when they are struggling to find the information they need. People appreciate the fact that they get a human voice straight away. We both get a great deal of satisfaction from helping people.
10 What is the most valuable thing about the Helpline?
How quickly the phone is answered and how reassuring we can be to people.
Our huge library of information is vital as it comes from trusted sources. The Peer Support service is run by the Helpline offering patients and carers a unique opportunity to speak to like-minded people for support with their diagnosis, home therapies options, as well as learn about being a living donor.
11 What are the plans for the future of the Helpline?
We will continue developing our patient information library as well as supplying the renal units with resources for their patients. We will develop our Peer Support service and continue to promote information to GP practices as part of early detection for kidney disease.
The NKF Helpline is funded by charitable donations, industry partners and the National Lottery.


The event provided a unique gathering for people to meet others facing similar challenges, make new friends, and share experiences in a friendly, social setting with a focus on kidney health.
Those attending enjoyed a range of talks and discussions led by healthcare experts and people living with kidney conditions. Highlights from the day included the great array of guest speakers:
• Caryl Bryant, Co-Vice Chair, NKF, who shared her family’s journey supporting her son Ben through Goodpasture syndrome, a rare autoimmune disease and her perspective on ‘making the most of your new kidney’.
• Roger Greenwood, from the Dialysis Society, spoke on improving outcomes for dialysis patients.
• Andy and Stacey Jones, a living donor and transplant recipient gave us their moving story on organ donation.
• Alex Gibbs, a patient speaker, reflected on the highs and lows of dialysis as a young adult.
• Oscar Walton, Kidney Dietitian, offered advice on nutrition and kidney health.
• Dr Lisa Willcocks and Benjamin Stokes explained the importance of regular blood and urine testing and monitoring, and managing chronic kidney disease.
• Kathryn Taylor, Social Worker at Bristol Royal Hospital for Children, presented a talk on psychosocial aspects of kidney care and multi-disciplinary team working.
• Lisa Ancliffe, Clinical Lead Occupational Therapist, explored frailty in kidney disease and strategies for its prevention.
• Dana Holmes and Alison Lawrence, NKF Peer Supporters, shared their journey from diagnosis through to dialysis, home treatment and life on the transplant list.





Everyone attending was able to explore the exhibition hall, meeting and chatting with a variety of organisations and charities including; Rapidcare, Independence Products, Vifor Pharma, Mesogeios, Book Dialysis and Lister Area Kidney Patients’ Association
The weekend was a celebration of the wonderful renal community, and was kindly sponsored by CSL Vifor and Novartis
NKF Chief Executive, Andrea Brown, commented, “A big thank you to all our attendees, guest speakers, exhibitors, and sponsors. I hope each person left the event feeling informed and empowered by the many kidney support networks available. Thank you to everyone who joined us and made the Annual Event such a great success. We look forward to welcoming you all again in 2026.”

































I had attended the NKF Annual Event last year and really enjoyed the event, therefore it was no question I wanted to come back this year. It was great to meet other people from the kidney community.
It was great to meet new people and the event was very informative.



It appealed to me as I wanted to see what others had say to about coping with their kidney condition.
My wife lost all kidney function unexpectedly in October 2024, we are trying to understand the longer term reality of living with kidney failure and the conference was a good way of learning quickly.
Lucy Vasiliou, NKF Policy and Public Affairs Manager, provides an update on policy developments.
“I would like to start by saying a huge thank you to everyone in our kidney community who has supported and signed the open letter to the Prime Minister calling for a national strategy on kidney disease. This has marked the start of our joint campaign with the UK Kidney Association, Kidney Research UK, Kidney Care UK and the PKD charity asking the government about the 7 Million Lives at Risk ‘What’s the plan?'"
Your voices - patients, families, clinicians and supporters - have made this moment possible. Together, we’re showing that when the kidney community speaks with one voice, we can be heard at the very heart of government.
The open letter closed to signatures earlier this month and we are pleased to report that over 13,000 added their name in support of the call to action. Because of your incredible support enabling us to reach over 10,000 signatures this means that the government has to provide a response and we will share this with you, along with any further actions, as soon as we can. On the 22nd October, representatives from the NKF, UK Kidney Association, Kidney Research UK, Kidney Care UK and PKD charity came together to hand the open letter in at 10 Downing Street.


Later that day, we also held the All-Party Parliamentary Kidney Group (APPKG) meeting in Westminster which was a great opportunity to talk about the open letter, share patient stories and discuss what needs to change with MPs who can support us in striving for that change.
We heard from patients from across the charities and our very own NKF Executive Committee Member, Asif, shared his story of living with kidney disease, receiving a transplant and the impact it has had on his life.
Asif said: “I was diagnosed with kidney disease too late. If I’d known earlier, I could’ve made choices to live better. Millions are still being diagnosed late. It’s time to treat kidney disease as a priority. Early detection doesn’t just save lives; it transforms them and eases pressure on our health services.”
Speaking at the meeting, Dr Katie Vinen (Consultant Nephrologist at King’s College Hospital and President of the UK Kidney Association) and Professor Smeeta Sinha, National Clinical Director of Renal Medicine shared the clinician’s perspective on why kidney disease should be prioritised, standing united with patients on the call to action.
Katie shared her thoughts; “As the professional voice of the UK’s kidney healthcare community, we see first-hand the pressures on kidney services and the consequences of continued under-prioritisation. Kidney disease is a growing health challenge that intersects with many other long-term conditions, yet it remains largely absent from national strategic planning. We have repeatedly called for a clear national approach to support consistent, high-quality care. This letter reflects the strength of feeling across the kidney community: change is urgently needed, and our members stand ready to help deliver it.”


As you know kidney disease affects around 7.2 million people in the UK – that’s more than one in ten of us –and the numbers are rising. Yet kidney disease was left out of the government’s 10-Year Health Plan, despite being a major cause of illness and a key risk factor for heart disease.
Every day, we hear from patients who face the reality of living with kidney disease – from the anxiety and worry of just being diagnosed, to the challenges of hours spent on dialysis each week and the difficulty of finding and waiting for a suitable transplant. These treatments save lives, but they take a huge toll on people’s physical and emotional wellbeing.
We know that early diagnosis and prevention can make a life-changing difference. That’s why we’re calling for kidney disease to be recognised as a national priority and more awareness to be raised on the importance of kidney health. We are also calling for priorities on home dialysis, organ donation and transplantation and support for everyone affected.

The NKF is proud to be run by patients, for patients and we believe that kidney patients and families deserve to be prioritised by the government and a national strategy on kidney disease would ensure patients experience the right care, at the right time. We will continue to make sure we are advocating for the changes that patients want and need to improve access to treatment and ultimately their lives.
Andrea Brown – Chief Executive NKF.
The NKF is proud to represent the voices of kidney patients through every level, whether that is through the Kidney Patients Associations, Regional Network groups or Parliament, we believe strongly that patient voices must always be heard.
By continuing our work with the All-Party Parliamentary Kidney Group, we’ll make sure patient voices are front and centre in conversations about the future of kidney care.
We’ll continue to campaign for:
• Better awareness and education about kidney health
• Earlier diagnosis and access to the latest treatments
• Improved dialysis and transplant services
At the NKF, everything we do starts with patients. Whether it’s through our Helpline, Kidney Patient Associations, or our national campaigns, we’re here to make sure you are heard, supported, and never alone.
You’ve already made an incredible difference by standing with us in signing the open letter. Please keep spreading the word – share your story, write to your MP, or get involved with your local Kidney Patient Association.
Together, we can show the government that kidney disease can’t be ignored any longer. With your help, we’ll keep fighting for better care, better lives, and a better future for everyone affected by kidney disease.

by Ali Lawrence

Ali describes in this honest account, her journey with kidney disease over the years and what it means to her to be a Peer Supporter for the NKF
Kidney disease came storming into my life in 1998, I was 26. Everyone has their own story of how they were diagnosed and for me it was through a routine medical check. I was prescribed blood pressure medication, told to keep to a low salt diet and that was that. Me and my husband, Phil moved to South Africa later that year and began a new adventure, but otherwise life continued as normal and did for the next two decades.
Then in 2019 my kidney function plummeted, and during a kidney appointment the heady topics of transplant and dialysis came up; things I knew were coming but had hoped I could magically avoid. I met with the transplant team to be worked up and by January 2020 I was active on the list.
During this time, I was having to decide, ‘what dialysis should I do?’ Dialysis is cr*p, but for me it was about finding the dialysis that was the least cr*p for me. I wanted to dialyse at home as my independence is really important to me and meant I could continue running my business. I feel very lucky that home dialysis was an option for me.
Originally, I'd planned to do home Haemodialysis but during a scan to assess me for a fistula, the surgeon asked me “have you ever considered Peritoneal Dialysis (PD)?” They told Phil and me that I’d be a good fit for PD and took the time to go over the positives and negatives so we could see the full picture. The two of us spent the weekend talking about it and I decided to go for it. I chose Automated Peritoneal Dialysis (APD) which is done overnight on a machine.
After this, everything seemed to move at warp speed and within a few weeks I was sitting on my bed with my PD catheter in my belly, me and Phil had done our training and I was about to do my first session on my machine. It was Saturday 14th March 2020, not long before the lockdown. I'm not going to lie, I sat on my bed that night and sobbed. Dialysis wasn’t easy to start with but over the next few weeks - with Phil’s help - I slowly began to get used to it. I named my machine ‘Bob’ after a character
from Blackadder and felt proud to be able to retain some independence and keep myself alive and well. Plus we could take ‘Bob’ with us on weekend breaks.
Then in 2021 I had to switch to Continuous Ambulatory Peritoneal Dialysis (CAPD). This was probably one of the biggest challenges I’d faced so far - especially mentally. Physically, I struggled to adapt to carrying the fluid in my belly all day but the emotional challenge was much tougher. I hated having to stop my life to do my exchanges. Luckily my Trust has a renal counsellor and I reached out to them for help. I’m so glad that I did as Carole - my counsellor - really got me and by extension Phil through this. With her help I learnt I could do activities during my exchanges to make the best of the time. And after a bit of trial and error I settled on yoga and quickly saw an improvement in how I was feeling mentally and physically.
Unfortunately, later that year I was twice admitted to hospital with peritonitis and on the second occasion had to lose my PD catheter. Once my head had finished spinning, I decided I wanted to do home HD and while I waited for my training I did self-care in my unit. This made such a difference and it was wonderful to take back some control of my health and feel a bit more like me again. By September 2022 I’d finished my training and was back to dialysing at home, this time it was HD on my NxStage machine ‘Nelly’.
While this was going on we were still waiting for ‘the call’ to say there might be a kidney for me. In August 2022 me and Phil were matched in the Living Kidney Sharing Scheme but sadly it didn’t go ahead. Then in November, we got our first call and excitedly headed for the hospital. Unfortunately, the kidney wasn’t viable. We had never seen that coming and I remember grieving for the new life that had been offered and then so abruptly taken away.
We got our next call in December, and sadly again the kidney wasn’t viable. We headed home, but this time we felt strangely upbeat having had two offers within a month.


2023 arrived and on 4th January we got another call. We headed off to the hospital expecting to be home again that night but just after midnight I received my longed-for kidney transplant.
It took a few days for my kidney to wake up but I’ll never forget being told that the kidney was working. My recovery since then has been up and down but thanks to my donor and her family my life has changed so much. It’s wonderful to be able to do the things that make my life worth living. I love film and performing and I’ve returned to volunteering at my local community cinema and hope to be back on stage again soon. Sorry! One of the biggest landmarks for us since my transplant is being able to travel abroad again, and last year we finally did it. We had an amazing adventure and really made up for all the lost time.
Something else which my transplant has given me is the ability to be an even more active advocate for kidney health, especially championing home dialysis, peer support and organ donation. And in the years while I was on dialysis and through the uncertainty of waiting for a transplant, being able to talk to someone who really understood helped keep me alive as much as the dialysis.


So, when in 2021 I heard that the NKF was launching a Home Dialysis Peer Support Service and looking for volunteers I jumped at the chance to sign up. I loved the idea that my experience of home dialysis would be able to help fellow patients and their families. And now since the service was expanded, I’ve also been able to use my experience of in-centre HD and transplant to support lots of people through one of the most life-changing times in their lives.
In October I was honoured to - nervously - stand alongside my fellow Peer Supporter – Dana Holmes –at the NKF Annual Event and talk about my experience of home dialysis and what the NKF Peer Support Service means to me.
Being a Peer Supporter is one of the best things I’ve ever done and I feel really privileged to have been able to help fellow patients and their families over the last four years and look forward to doing that for a long time to come

As part of our speaker sessions at this year’s Annual Event, we heard from Dr. Lisa Willcocks, a Consultant Nephrologist at Cambridge University Hospitals NHS Foundation Trust, and patient representative Benjamin Stokes who shared some practical and personal thoughts around managing the numbers which matter most in IgA nephropathy.
Dr. Willcocks opened the session by highlighting the important role of regular blood and urine testing in renal diseases, outlining the three key numbers that everyone living with chronic kidney disease or IgA nephropathy should know about: proteinuria, estimated Glomerular Filtration Rate (eGFR), and blood pressure. “Understanding and keeping an eye on these key numbers can help you better understand your kidney function and work with your healthcare team to decide how best to keep your kidneys working as well as possible, for as long as possible,” she explained.
Proteinuria, or excess protein in the urine, is a sign of kidney damage and inflammation.1 It can be measured in several ways, including urine dipsticks and protein-to-creatinine ratios.1 eGFR, or creatinine, which is used to calculate eGFR, is measured through a blood test and reflects overall kidney function, while blood pressure monitoring is essential, as high blood pressure can accelerate kidney damage. 2,3 As well as explaining the numbers and their importance, Dr. Willcocks emphasised how regular monitoring of them can give a clearer picture of what’s happening with someone’s kidneys and urged people who are unsure or worried to ask questions with their healthcare team.
The session then shifted to a Q&A, where Benjamin Stokes shared his personal journey with IgA nephropathy following a diagnosis in 2012. “When I was first diagnosed I was working as a personal trainer and I didn’t even consider that I might have kidney disease, let alone a particular type of rare kidney disease, but it soon became clear that this condition was going to be with me forever,” he recalled. “Quite quickly I began to think, ‘well what can I do about this’. I wanted to take control of anything and everything I could to try and prolong the quality of life that I had.” Through asking questions and self-learning, Benjamin moved from feeling anxious and isolated to becoming aware and informed. He described how, by understanding what he could and couldn’t control, he began to take charge of the things he could, to ensure his test results showed the most accurate representation of what was going on with his kidneys.
Benjamin highlighted the importance of building habits around kidney health. He learned to ask his healthcare team about his results and what they meant for his condition. He also began to manage variables within his control - like hydration, exercise, and diet - before tests. “I wanted to ensure medical decisions were based on the most accurate information possible, and I soon realised there were things that would impact my results. For example, if I had done a workout the day before my tests, my results could really fluctuate, so I tried maintaining consistency where I could,” he said.
He encouraged others who might be in a similar position to do the same: ask questions and ensure you understand these numbers as much as possible. He also recommended using reliable, trusted resources like the ‘Tracking Your Numbers’ booklet developed as part of the ‘Navigate Your Numbers in IgA nephropathy’ campaign, as well as the wider NKF support network.
“Especially as a young person, it can be difficult to talk about feeling anxious and scared about the future, so just ask questions and there is more information out there now. Don’t put pressure on yourself as a patient, but I couldn’t encourage you more to seek information to empower yourself with knowledge,” Benjamin concluded.
By demystifying the numbers and encouraging open dialogue with healthcare teams, Dr. Willcocks and Benjamin Stokes demonstrated that knowledge truly is power when it comes to living well with IgA nephropathy.
Navigate Your Numbers in IgA nephropathy (IgAN) is a disease awareness campaign initiated and funded by CSL Vifor with input from the National Kidney Federation and people living with and treating IgA nephropathy.

UK-NP-2500242 October 2025
1 Pitcher D, Barratt J, et al. Future Rare Diseases. 2025;1
2 Kidney Research UK. Understanding test results. 2025. Available at: https://www.kidneyresearchuk.org/kidney-health-information/living-withkidney-disease/how-can-i-help-myself/understanding-test-results/ Last accessed October 2025.
3 National Kidney Federation. IgA Nephropathy. 2025. Available at: https:// www.kidney.org. uk/iga-nephropathy Last accessed October 2025.


The National Unified Renal Translational Research Enterprise project (NURTuRE) was set up in the UK in 2019 to help people with chronic kidney disease (CKD) and another kidney condition called idiopathic nephrotic syndrome (INS).
The idea of the project is to collect samples (blood, urine, tissue) and health data from patients to create a 'biobank' (a large collection of biological material) which researchers can use to study kidney disease.
Why this project matters for people with kidney disease
• CKD affects about 10% of adults and can lead to serious problems such as heart attack, stroke, or end-stage kidney disease (ESKD).
• But not everyone with CKD develops these severe outcomes – some progress faster than others.
• One aim of NURTuRE is to help predict who is at higher risk and who is at lower risk, so doctors can direct care and monitoring more accurately.
• It will also help develop new treatments faster, since the research will have access to many samples and data all in one place.
How it works
• The biobank recruited over 3,000 patients with CKD already, and over 500 with INS.
• For each participating patient, samples are collected: more than 90 blood/plasma/serum samples plus 30+ urine samples.
• Patients also have follow-up visits (for example, one more visit a year later) and then long-term follow-up (for many years) using routine clinical data (so fewer extra hospital visits just for the study).
• The biobank uses linked data from the UK Renal Registry and the National Registry of Rare Kidney Diseases (RADAR) to connect the samples with patients’ health records.
What this could do for you (as a kidney patient)
If you have CKD or INS, this kind of research might mean that in future:
• Doctors can better tell how fast your disease might progress — so you might get more tailored care (for example, more monitoring if you’re high-risk, or fewer visits if you’re low-risk).
• New treatments might become available sooner because researchers have better tools and samples to test ideas.
• Less burden for you: since data/samples are collected within usual care frameworks, you might not need lots of extra hospital visits just for research.
Things to know / things they emphasise
• The biobank is a collaboration: Universities, charities (such as Kidney Research UK) and several pharmaceutical companies all working together.
• The biobank is not just for one study — it’s built so many future research projects can use the resource.
• From around 2020, the samples have been made available to external researchers (not just the partners) under governed access.
• The combined system is both a registry and biobank, meaning health data plus physical biological samples in one linked resource.
• Having lots of samples and data means better quality research leading to better understanding of kidney disease.
• Being better able to predict risk means care could become more personalised e.g. 'this patient needs more monitoring', or 'this patient is stable so requires fewer visits'.
• New treatments might be developed faster and more cost-effectively.
• For patients: less extra burden, since research is integrated with usual care.
• This doesn’t mean a new treatment is already available tomorrow - research takes time.
• Even though the biobank aims to help many types of kidney disease, results may take years to translate into everyday care.
• Participation in research may still involve some extra steps, (for example for consent or sample collection) though the project attempts to minimise extra hospital visits.
Find out more at nurturebiobank.org

Nearing fifty, I never thought I’d make it this far.
Life has never followed a straight path
I’ve had several partners and lovers, loyal pets, and a few unforgettable years away at university. Nearing forty, I finally left my childhood home – carrying with me a lifetime of memories and more than a few medical records.
My journey has been far from 'normal' – three kidney transplants, years on peritoneal and haemodialysis, and more hospital admissions, operations, and needles than I can count. I’ve also faced cancer, meningitis, a heart attack, and the loss of my brother – when I was the one everyone expected to go first.
Yet through it all, there have been good times – moments of joy, connection, and freedom.
Freedom to Travel – and its Frustrations
Thanks to the Freedom dialysis booking service, I’ve managed to travel abroad while on treatment – to Rhodes, Madeira, and even the holiday unit at Southbourne-by-the-Sea. I’ve also enjoyed short breaks during transplant years, though those memories grow hazy now.
But in 2025, travelling on dialysis within the UK has become increasingly difficult.
On my most recent trip to London, the dialysis unit changed my treatment days at the last minute. Suddenly I was scrambling to rearrange trains and hotels – at a £250 personal cost. I could afford it, but many couldn’t. For some, that experience alone would be enough to stop travelling entirely.
For me, it raises the question: is it even worth trying anymore?

Dialysis Away From Base – Not a 'Holiday'
“Attending my brother’s funeral is not a holiday. To call it one feels insulting.”
There’s often confusion between DAFB and “holiday dialysis.” Many units refer to “holiday bloods,” but not every trip is a holiday.
For some of us, travelling for dialysis means visiting ageing parents, attending family funerals, or fulfilling volunteer commitments – essential life events that keep us connected and human.
When my brother passed away, I couldn’t secure dialysis locally. I managed only by hiring private transport at short notice – another £450 expense. Situations like that shouldn’t happen. No one should have to choose between family and treatment.
Patients without access to portable home machines like NxStage, MyDial, or Quanta, and without personal transport, face real restrictions. For many, it feels like being trapped in your own town – unable to visit loved ones or take part in normal life.
Some exciting innovations are happening – smaller 10kg portable machines are currently in clinical trials in the Netherlands. These could eventually be used for both haemodialysis and PD. (I’ll be writing a separate article about that for KCUK.)
It’s amazing to think that Wilhelm Kolff, the Dutch inventor of the dialysis machine, built a 5kg 'portable' model decades ago. Yet even now, most machines remain bulky, heavy, and dependent on large quantities of dialysate. Technology has shrunk everything from mobile phones to supercomputers – except dialysis.

If we’re serious about improving quality of life for kidney patients, we must integrate dialysis access into new housing developments and transport planning.
Imagine if new GP surgeries automatically included small dialysis units. Imagine if local councils worked with housing associations – like Habinteg Housing, The Bournville Village Trust, Transport for All, and Transport for New Homes – alongside kidney charities like NKF and Kidney Care UK, to plan truly inclusive communities.
Transport remains one of the biggest barriers. With the cost of living so high, many of us can’t afford £25 taxi rides to clinic. While patient transport services exist, they are often unreliable, uncomfortable, and demeaning. We deserve better – safe, timely, and dignified transport to treatment.
“We can’t keep calling it ‘accessible’ if it only works for people with cars.”
Hope and Momentum
I applaud everyone involved in the NKF’s Home Dialysis Campaign. It’s a huge step forward.
There’s a proverb I love: “The best time to plant a tree was 30 years ago. The second-best time is now.”
We have a lot of catching up to do – but with collaboration, technology, and patient voices, I truly believe progress is coming.
James Warham has lived with kidney disease since the age of five, beginning treatment at Great Ormond Street Hospital. He has campaigned with his mother against hospital school closures, helped establish the early Young NKF, and continues to support kidney patient groups including the Midlands Kidney Forum and the Centre for Sustainable Healthcare.
James lives in Telford, West Midlands with his partner, continues home haemodialysis, and somehow still finds time for yoga, green causes, and the Men Walking & Talking support group.
The best time to plant a tree was 30 years ago. The second-best time is now.
As the NHS embarks on its ambitious 10-Year Health Plan, the National Kidney Federation (NKF) has been working tirelessly to ensure kidney patients' voices are heard and their needs prioritised. Our recent advocacy efforts have focused on several critical areas that will shape the future of kidney care in the UK.
Four years ago, the National Kidney Federation (NKF) launched its webinar series, designed to inform, educate, and empower kidney patients and their families. Held on Wednesdays at 5pm, the webinars take place approximately six times a year and cover a wide range of topics relevant to living with kidney disease. They can be viewed shortly after they have been delivered and are available for anyone to view.
Each session features expert presenters, including healthcare professionals and patient speakers who share their insights and lived experiences. Over the years, subjects have included Keeping Active, Healthy Eating, Benefits Advice, Pharmacy and Medication Delivery, and even discussions around Sexual Relationships - all aimed at providing practical advice and emotional support to those living with kidney disease.
All webinars are recorded and available on the NKF YouTube channel, where they continue to reach and inspire audiences in the UK and beyond. The series has proven incredibly popular - with one webinar alone receiving over 399,000 views.
Healthy Eating with Diabetes & Kidney Disease
- the most recent webinar, held this month
View it here at www.kidney.org.
uk/Event/nkf-webinar-series
Hosted by Yuko Ishida, BSc (Hons), MSc RD, Specialist Diabetes

Dietitian Greater Glasgow and Clyde NHS, Yuko is the creator of renal dietary videos that help patients with good food choices. Yuko is joined by Hattie Stiff, NKF Ambassador to discuss her experience of a renal diet. The webinar focuses on both diabetic and kidney patients aiming to help them improve their understanding of the best diet for managing their conditions.

You can find the full collection here: www.kidney.org.uk/Event/nkf-webinar-series
Previous webinar topics have included:
• COVID-19 & kidney disease
• Travel & Dialysis
• Ageing Well with Kidney Disease
• Navigating Menopause
• Itching and Skin Care with Kidney Disease
• Fatigue Management
• Sexual Relationships in Kidney Failure
• Foot Care
• Matching for Transplant – A Guide to Compatibility and Blood Tests
• How a Kidney Patient Association (KPA) Can Support You
• Patients Know Best App
• Healthy Eating with Diabetes and Kidney Disease
• Insight into Renal Pharmacy
• Benefits for Kidney Patients
• NBTA – Opt-Out in England: Two Years On
• Patient Choice and Vascular Access
• Keeping Active with Kidney Disease
• 'Help – I Need Somebody' Webinar
• Healthy Eating for Your Kidneys
• Organ Donation: One Year On
The National Kidney Federation (NKF) is partnering with Curovia Healthcare in an exciting new project to create a series of short, animated videos to help people understand more about chronic kidney disease (CKD) and treatment options, including dialysis.
These videos are being created completely free of charge by Curovia, to benefit all kidney patients and their families.
Before the videos are made, we want to listen to your experiences.


And so we’re holding online focus groups with patients and family members to explore:
• What was hardest to understand when you first learned about kidney disease?
• What do you wish you had known earlier?
• What would make information clearer or more helpful – especially for people who speak English as a second language?
You don’t need any special skills to join the focus groups, just your experience and your voice. Everything you share will help make kidney information easier and more accessible for everyone to understand.
If you would like to join a focus group or find out more, please contact – Kate Pym at info@curovia.co.uk
Together we can make a real difference for kidney patients and their loved ones.

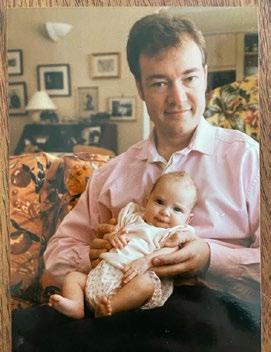
by David Stiff
My daughter Hattie was born with kidney disease in 1997. My wife had been hospitalised with preeclampsia a couple of weeks before she was born and during a routine scan, the medical team discovered that Hattie had a kidney problem. They could not provide a detailed diagnosis without further tests and for the health of both mum and baby, my wife had an emergency Caesarean at 33 weeks.
The first time I saw Hattie the day after the birth, she was separated from mum having a blood test. She was so tiny. The doctor was taking blood from the back of her hand and she was clearly in pain and distressed. It broke my heart and that was the first of many heartbreaking moments on this long journey of ours. The diagnosis came within a day or so. Hattie had severe kidney failure and was very, very unwell.
The local hospital, as good as it was, could not provide the specialist renal care that Hattie needed and a transfer was arranged to Guys in London. My wife was not well enough to leave the hospital and the doctors were so concerned with Hattie’s condition; she was advised to “say goodbye” as we prepared for the transfer by ambulance.
The weeks that followed were a blur, sharing my time between hospitals and trying to understand what was happening to my daughter and my wife. Eventually my wife was transferred to Guys so we could all be in one place. On different floors but in one building. Over the weeks that followed, my wife improved enough that she could spend time with Hattie in the ICU. Hattie was so small and fragile, and everything seemed so raw and painful. After six weeks Hattie’s condition had stabilised enough for us to leave Guys.
The team at Guys had saved her life and she was stable for now. She needed a kidney transplant as soon as she gained enough weight. Ten kilograms was the target. That would be achieved easily within a year for a healthy girl. For Hattie, it would take a lot longer. We just had to keep her going.
Armed with boxes of medication, the skills to insert nasogastric tubes and give injections with hypodermic needles that looked far too large for her tiny arms, we took the long journey home.
I remember the exact spot on the journey home where the chaos of the past two months and the demands of processing overwhelming amounts of information briefly quietened down. I had one thought that overtook everything else, I will do whatever I have to, to help Hattie get better and donating a kidney will be part of that journey. It was never a question of donating; it was just a question of timing.
It took Hattie nearly two and a half years to get to 10kg. That was a long and bumpy road but we got there. The team at Guys explained how the donor scheme worked and the likely timeline. They explained the priority given to children and the advantage of saving my kidney until she needed her next transplant when she was older. Another reality check, she would need a number of transplants throughout her life. That was a tough moment.
We went on the transplant register and after only a few months, we got the call, “we have a kidney, it’s a good match and you need to get to Guys as quickly as possible”. It was as exciting as it was scary. The transplant was a success. Her kidney function went from less than 5% to normal overnight. We had been given the gift of life for our precious daughter from a grieving family who had lost a loved one. Every aspect of that is hard to comprehend.
Overwhelming relief and joy and bewildered awe at the kindness from complete strangers. It’s impossible to describe quite how valuable that brave decision has been to our family. We were and still are, so grateful.
After three weeks in hospital and a further eight weeks where we stayed near the hospital and took Hattie in every day, we came home with a different set of medicines and a different child. That kidney, that gift of life, lasted for 22 years and saw our daughter grow from a toddler to a young lady in her early twenties.
As we had been warned, the kidney started to decline as Hattie was starting university. The rate of decline increased rapidly over the next year or so and I was tested to see if I was a good enough match to donate a kidney. I had never doubted it, but it was a relief to find out I was a good match. Very soon after that, the work up began. I had a series of medical tests to ensure I was healthy, my kidneys were healthy, and one could be extracted easily. The final part of the process was an interview to ensure I fully understood what I was doing and check that I really wanted to go ahead. I did and had done for 22 years.
We were expecting the transplant to happen quite quickly. Hattie would be put on dialysis for a few weeks to boost her strength now that her kidney was failing. The few weeks turned into two and a half years, as we battled through Covid and through Hattie’s


rapidly declining health. Four transplant dates came and went as each was cancelled for a variety of reasons beyond our control. Finally, the day came. Hattie was already in the care of Southmead hospital when I went in on the morning of the transplant. My operation was performed in the morning and Hattie’s in the afternoon. Both successful and for Hattie, life changing. My stay in hospital was brief, and within three days I was out and recovering at home. Hattie stayed longer as her body recovered from the operation.
My recovery was rapid. After a week or so I was able to get around the house pretty well and I even went for a short, very slow walk in a local park. Within a month I felt almost back to normal and after 2 months I slowly started back at work. Four years on, I’m as fit as I’ve ever been, my small scars have long since healed and there is nothing I can’t do that I did before the operation. It’s difficult to imagine that I have only one kidney. For me, I’ve lost nothing. For Hattie, she has gained everything. An almost miraculous gift of life.
I had never doubted my resolve to give Hattie one of my kidneys. I’m so grateful I could. For me the process was straightforward and in the grand scheme of things, it was a small but wonderful detour in my life. My life is richer for the experience and the rewards have been immense. I’m so grateful to the NHS renal teams who have been part of our journey. Their compassion, skill and commitment have quite literally been lifesaving.
Having been through this experience and seen the rewards of kidney donation, I cannot say loudly enough how much I admire anyone who steps forward to help others in this way.
At the National Kidney Federation our vision is clear, we want everyone affected by kidney disease to live their best possible life. That means being equipped with the right knowledge, supported through our services and given a strong voice in the fight for better care.
Since our formation in 1978, gifts left in Wills have played a powerful role in making this vision a reality. These legacies have funded vital support services such as our free Helpline, offering guidance and emotional support and our National Peer Support Service, connecting patients with trained volunteers who can understand and help support their journey.
Over the past five years, legacies have accounted for more than a third of our income. Quite simply, without this generous support, much of our work would not be possible.
In this issue of Kidney Life you will find included a leaflet about how you might contribute to a lasting legacy.
Your gift could help us:
• Expand and strengthen our vital patient services, including our Helpline and Peer Support services.
• Campaign so that kidney patients and families have the care they deserve and the ability to choose the treatment options that works for them, such as home therapies.
• Ensure that kidney disease remains high on the agenda for decision makers, amplifying the patient voice where it matters most.
Together, we can provide patients and their families with the care, support, and choices they deserve. Together, we can Do It For Them. By choosing to leave a gift in your Will, you become part of an extraordinary group of people creating lasting change for future generations of kidney patients.
And to make things simple, our partnership with FreeWills means you can write your own fully comprehensive Will, free of charge. It’s secure, straightforward and enables you to leave a legacy of hope.
To download our free legacy giving pack or to start your free Will today, please visit: www.kidney.org.uk/ legacy-giving


Our legacy giving pack is designed to guide you through the process with clarity and confidence. It includes everything you need to know about leaving a gift in your Will, from understanding the types of legacies, to step by step instructions on how to ensure your wishes are carried out. We know that making a Will can feel complicated and overwhelming, which is why we’ve created a legacy giving pack to give you peace of mind.
A gift in your Will is more than just a donation – it’s a lifeline, a voice and a promise of a better tomorrow.


“Thanks to the NKF, we know there is support for us at every stage, and we are proud to be a part of this community. By considering leaving a legacy gift to the NKF, you could be helping support families like ours and people like our little Jack, who have kidney issues.”
Maz and Jack
“For me, the NKF has always been and continues to be a meaningful way to channel my energy into supporting kidney patients through advocacy and representation. The NKF works to make life more manageable for kidney patients by providing reliable resources, a freephone Helpline, and dedicated peer support.”
Soumeya Bouacida

“The NKF enriched my life immeasurably the sense that you are making a difference, however small, is very gratifying.”
Ros and Steve
This one’s a bit more complicated with two sets of words to find. You're looking for the words in bold. Good luck!
World Names For Father Christmas
1 From Italy – Babbo Natale
2 From Norway – Julenissen
3 Portugal – Pai Natal
4 UK – Father Christmas
5 Ukraine – Sviatyi Mykolai
6 France – Pere Noel
7 Netherlands – Sinterklaas
8 Germany – Weihnachtsmann
9 Switzerland – Samichlaus
10 Czech Republic – Jezisek
Foods Eaten Across The World At Christmas
1 UK – Mincepie
2 Germany – Stollen
3 Italy – Pandoro
4 Spain – Mariscos
5 Poland – Wigilia
6 Russia – Kutya
7 Mexico – Tamales
8 New Zealand – Pavlova
9 Brazil – Farofa
10 Canada – Tourtiere
If you can find our ‘Elf on the Shelf’, who is hiding somewhere in this magazine and answer the following three questions you could WIN a £25 Amazon voucher to spend on whatever you like.
These are the questions (there’s no right answers!)
1. What do you most like to read about in Kidney Life?
2. What would you like to see more of in the magazine?
3. What page was the Elf on and what was he doing?
Email your reply to kidneylife@kidney.org.uk and a winner will be picked at random.
Good luck, Annie (Editor)


Our 2025 Christmas Draw is here - and the prizes are bigger than ever with a top prize of £1,500 cash and three additional cash prizes - all yours to spend however you wish! Good luck everyone! You can get your raffle tickets online: www.kidney.org.uk/shop/nkf-christmas-draw-2025
Every ticket purchased helps support kidney patients and their families across the UK. Good luck! Thank you for your support!


Send festive cheer and support the NKF at the same time. We’ve got a fantastic selection of Christmas cards, with prices starting from just £3.50 for a pack of 10. But that’s not all. We also have a range of lovely festive goodies - make Christmas meaningful: spread the joy and support the NKF at www.kidney.org.uk/shop
Each year we invite our wonderful supporters to help decorate the NKF Christmas tree – and we’d love you to join in.

On the back page of Kidney Life, you’ll find your NKF Gold Star. Write your festive message or dedication, cut it out, and send it to us – we’ll proudly hang it on our tree for all to see.
If you can include a small donation, it’s greatly appreciated, but not essential. Your message will brighten our tree and lift our spirits. Take part or learn more at www.kidney.org.uk/ christmas-gold-star Let’s make this Christmas shine together!
The NKF is fortunate to have access to charity places in a wide range of running events across the UK. Whether it’s a 10k, half marathon or full marathon, there’s something for everyone – and every step you take will help support kidney patients and their families. If you know someone who would like to take part in any of these fantastic events, we’d love to hear from them!

Runners will receive: • An official NKF running vest • Full support and encouragement from our fundraising team • The knowledge that they are making a real difference for kidney patients across the country • We’ll share your results in Kidney Life
For more details, please contact pete@kidney.org.uk or follow using the QR code.
Well, it was interesting making Christmas goodies in October! But it certainly filled my kitchen with some lovely spicy aromas – especially the cinnamon. These are really nice; tasty and not too naughty. They freeze well too so you can be prepared. Needless to say all 12 had disappeared with a few days. Enjoy! Ed
Dry ingredients
• 6 oz(170g) plain flour
• 1 tsp low-sodium baking powder
• 1 tsp ground cinnamon
• ½ tsp ground nutmeg
• ¼ tsp ground cloves
Wet ingredients
• 4 oz (113g) unsalted butter or soft margarine
• 2 oz (56g) granulated sweetener (Stevia, erythritol, or monk fruit that measures 1:1 with sugar)
• 1 oz (28g) light soft brown sugar (optional for flavour)
• 2 medium eggs
• 1 tsp vanilla extract
1 Soak the fruit
Fruit mix (for soaking)

• 1½ oz (42g) dried cranberries (unsweetened if possible)
• 1½ oz (42g) raisins
• 3 oz (85g) peeled apple, finely chopped and pre-soaked in water (to leach potassium)
• 2 oz (56g)tinned pineapple, chopped and drained (in juice, not syrup)
• 2 fl oz orange or apple juice (no added sugar)
• 1 tbsp lemon juice
Optional Christmasy extras!
• 1 tbsp brandy or rum (optional)
• 1 oz (28g) unsalted chopped almonds or walnuts
Mix cranberries, raisins, apple, pineapple, orange juice, and lemon juice. Cover and soak for 2 hours (or overnight). Drain before using.
2 Preheat oven
Heat to 160°C / 325°F / Gas 3. Line a 12-hole muffin tin with paper cases.
3 Prepare dry ingredients by sifting together the flour, baking powder, cinnamon, nutmeg, and cloves.
4 Cream butter & sweetener
Beat the butter with the sweetener (and brown sugar if using) until light and fluffy. Beat in the eggs one at a time, then stir in vanilla.
5 Combine everything Fold in the soaked fruit and nuts (if using).
Gently fold in the dry ingredients until evenly mixed. Add brandy or rum if desired.
6 Fill cases & bake
Divide the mixture evenly among the 12 paper cases (about two-thirds full). Bake for 25–30 minutes, or until golden and a skewer inserted into the centre comes out clean.
7 Cool & decorate
Cool on a wire rack. When cool, dust lightly with powdered sweetener or decorate with:
• A few fresh cranberries, or
• A small piece of dried fruit and a sprig of mint for a festive look.
• I covered some of the cupcakes with a cream cheese frosting which made them look festive.
• Store the cupcakes in an airtight tin for up to 4 days or freeze for up to 3 months.
• Great for giving as a gift – just wrap individually in parchment or cupcake boxes.
Approximate nutrition per cupcake
(These values will vary slightly by ingredient brand)
• Calories: 150
• Protein: 2.5 g
• Carbohydrate: 18 g
• Sugar: 6 g
• Fat: 7 g
• Sodium: <90 mg
• Potassium: 150 mg
• Phosphorus: <75 mg
by Caroline Basarab-Horwath

I qualified as a nurse in 1998 and began my career as a renal nurse. For the last 20 years, I have had the privilege of leading the Living Donor Programme at Sheffield. Outside of work life is just as full –I have three amazing children, a patient husband and 12 much loved pets. I'm incredibly proud to be part of both my family at home and my extended renal family at work. Here is a day in my life as a Living Donor Coordinator.
6:00am
The morning rush
It’s Wednesday morning, and the alarm goes off far too soon. Wednesdays are always busy with the Living Donor multidisciplinary meeting starting at 7:45am. That means it’s a mad dash to get the children up and ready for school, the dogs walked, and the animals fed. However, by the time I get out of the door, I’m already shifting my mind into work mode.
7:45am
The MDT meeting
I always feel a bit nervous before these meetings, it's crunch time. This is where the team decides if a donor can move forward, needs more tests, or in some cases, has to be declined. I know how much it means to a donor to be accepted. For them, it isn’t just about the tests or surgery – it's about being able to give something priceless to someone they love (or even to someone they’ve never met).
When a donor is accepted, I see the relief, the pride, and often happy tears. It’s a huge moment that makes all the long appointments and waiting worthwhile. And when it's not good news, I feel that too – the disappointment is real, and I always think carefully about how best to support them afterwards. I meet Lisa, the Clinical Practitioner, in the office and we head into the meeting. Sitting in the meeting, I carry their hopes and anxieties with me. Around the table (and sometimes on screen) are surgeons, nephrologists, anaesthetists, and scientists. We run through each donor case in detail –discussing test results, concerns, and next steps. My role is to present each case and make sure the donor’s voice is heard. It’s intense but collaborative and by the end, we have a clear plan for each person. After the meeting I head to the clinic to welcome the ‘one stoppers’ and take them to their first appointment of the day. The one-stop day involves a detailed
kidney function test (measured GFR), assessment by a Consultant Transplant Surgeon and Consultant Nephrologist, ending with the all-important CT scan which completes the core tests required.
9.30am
Check messages
I then head back to the office to look through my emails and messages. There’s always something waiting –blood results to check, clinic lists to organise, or a donor who needs a call back. I like to plan my day, but I’ve learned to expect the unexpected – things can change very quickly!
10.00am
Action MDT
I spend the next hour calling donors to make appointments for donors to come in for their results, give donors updates, or request tests, or excitingly give donors and recipients theatre dates.
11:00am
Nurse Consultation
This morning I have a potential non-directed donor booked for a nurse consultation. They have had their initial tests with Lisa, which included lots of blood tests, including kidney function, liver function virology screening, BP, weight, chest x ray heart tracing. These have been reviewed by our Consultant Nephrologist, and he has cleared them to have their one stop day. Before their one stop day I book a video call with them to discuss the pathway to become a donor, the surgery the recovery, the risks although minimal, and generally get to know them, manage expectations and understand their home and working situation. My job is to guide them through the process, explain all the steps and reassure them that their safety and wellbeing are our absolute priority.
I start by asking my favourite question, ‘Why do you want to donate a kidney?’ This can often be a very emotional response and it is particularly interesting to hear how non-directed donors have reached the decision.
I particularly like this part of the job where I get to know new potential donors and start to form a relationship with them. I start by asking my favourite question, ‘Why do you want to donate a kidney?’ This can often be a very emotional response and it is particularly interesting to hear how non-directed donors have reached the decision.
12:00pm
Service improvement meeting –working lunch
The transplant team meet with our service improvement coach with whom we have worked for many years, improving the living donor and transplant service. We are currently working on donor videos where previous donors and recipients have recorded their journey to share with new donors. We’re also trying to reduce the longstanding issue of patients waiting for their medicines before they can be discharged home. I really enjoy these meetings and as a team we have made many improvements to our service along the way, like our one stop assessment day.
13.00pm
Video call
I have a video call with the donor from last week to check on how they are recovering. It is nice to see them rather than talk over the phone and I can assess their recovery.
13.30pm
Living Donor Clinic
Here I catch up with the one stoppers making sure the day is going well. I coordinate with the clinic making sure the surgeon and nephrologist have the information they need and sit in on the consultations. We have a busy clinic with the one stoppers, results, appointments and post op reviews. It's lovely to see the donor from two weeks ago doing really well. We give good news to a couple of donors, confirming they are suitable to donate and offer theatre dates, followed by having to break the news to a donor that they can't donate. This is the worst bit about my job. It can be devastating to the donor to be declined and we offer support to them.
15.30pm
Meet and greet the donor and recipient
The donor and recipient scheduled for theatre arrive in clinic to be seen by their surgeons, nephrologists and to have final blood tests. I then settle them into the ward, meet their relatives and discuss plans for the next day. It's my job to try and alleviate any last minute concerns the pair may have and reassure relatives.
16:30pm Wrapping Up
The last part of my day is usually paperwork – updating notes, clinic outcomes, documenting conversations; it’s not the most exciting part of the job but it’s essential for keeping everything organised and safe.
17:30pm Heading Home
As I drive home, I think back to the people I’ve spoken with today. Each one is on a journey that will change their life - and someone else’s – forever. It’s a privilege to walk alongside them, to listen, to guide and to be part of something so life-giving.
No two days are ever the same as a Living Donor Coordinator, but every day is centred around supporting people who are considering one of the most generous acts possible: giving the gift of life through kidney donation. Every day reminds me why I love being a Living Donor Co-Ordinator.
If you are considering living donation here are some useful links:
www.organdonation.nhs.uk/livingdonation www.giveakidney.org/ www.donateakidney.co.uk/about-make-yourmark/ www.donateakidney.co.uk/requesting-a-buddy www.nbta-uk.org.uk/living-transplant-initiative