
Upcoming Fall Events
Spencer’s Impressive ED Makeover
Dive into Hyperbarics


Upcoming Fall Events
Spencer’s Impressive ED Makeover
Dive into Hyperbarics
USD Builds the Rural Workforce... One Grant at a Time
•
•
•
•
•
•


Sponsored by Children’s Nebraska
When a child is diagnosed with cancer, every moment matters. Children’s Nebraska Hematology/Oncology walks alongside families with expert care, innovative treatments and a team that never gives up hope.
When a child is diagnosed with cancer, every moment matters. Children’s Nebraska Hematology/Oncology walks alongside families with expert care, innovative treatments and a team that never gives up hope.
September is Childhood Cancer Awareness Month, a time to honor children and families facing this difficult journey and to recognize the life-changing impact of early, specialized care. At Children’s Nebraska, we are proud to be a place where families find more than treatment. They find support, compassion and a team that never stops fighting for brighter tomorrows.
When a child is diagnosed with cancer, every moment matters. Children’s Nebraska Hematology/Oncology walks alongside families with expert care, innovative treatments and a team that never gives up hope.
September is Childhood Cancer Awareness Month, a time to honor children and families facing this difficult journey and to recognize the life-changing impact of early, specialized care. At Children’s Nebraska, we are proud to be a place where families find more than treatment. They find support, compassion and a team that never stops fighting for brighter tomorrows.
September is Childhood Cancer Awareness Month, a time to honor children and families facing this difficult journey and to recognize the life-changing impact of early, specialized care. At Children’s Nebraska, we are proud to be a place where families find more than treatment. They find support, compassion and a team that never stops fighting for brighter tomorrows.
When a child is facing cancer or a blood disorder, providers need a partner they can trust. Children’s Nebraska offers the only pediatric-focused program in Nebraska dedicated entirely to hematology and oncology. Our pediatric specialists are nationally recognized, research-driven and deeply experienced in treating everything from the most common to the rarest forms of childhood cancer. Our team brings together oncologists, hematologists, nurses and support staff who understand what kids and families need most.
When a child is facing cancer or a blood disorder, providers need a partner they can trust. Children’s Nebraska offers the only pediatric-focused program in Nebraska dedicated entirely to hematology and oncology. Our pediatric specialists are nationally recognized, research-driven and deeply experienced in treating everything from the most common to the rarest forms of childhood cancer. Our team brings together oncologists, hematologists, nurses and support staff who understand what kids and families need most.
When a child is facing cancer or a blood disorder, providers need a partner they can trust. Children’s Nebraska offers the only pediatric-focused program in Nebraska dedicated entirely to hematology and oncology. Our pediatric specialists are nationally recognized, research-driven and deeply experienced in treating everything from the most common to the rarest forms of childhood cancer. Our team brings together oncologists, hematologists, nurses and support staff who understand what kids and families need most.
the condition can impact many parts of the body, our clinic includes a multidisciplinary team of skilled pediatric providers across many specialties.
As a member of the Children’s Oncology Group, we provide access to advanced clinical trials and the newest therapies. Our Pediatric Infusion Center offers outpatient treatment in a welcoming, kid-friendly space, making visits easier on families. We offer specialized therapies, including chemotherapy, blood transfusions and hydration treatment, all guided by the needs of each individual child.
As a member of the Children’s Oncology Group, we provide access to advanced clinical trials and the newest therapies. Our Pediatric Infusion Center offers outpatient treatment in a welcoming, kid-friendly space, making visits easier on families. We offer specialized therapies, including chemotherapy, blood transfusions and hydration treatment, all guided by the needs of each individual child.
As a member of the Children’s Oncology Group, we provide access to advanced clinical trials and the newest therapies. Our Pediatric Infusion Center offers outpatient treatment in a welcoming, kid-friendly space, making visits easier on families. We offer specialized therapies, including chemotherapy, blood transfusions and hydration treatment, all guided by the needs of each individual child.
This clinic cares for children with hemophilia, Von Willebrand disease, clotting factor deficiencies and other platelet disorders. Families meet with multiple specialists in one visit, reducing the need for additional appointments and providing complete, coordinated care.
From social workers and child life specialists to psychologists and educators, we surround families with a team that supports the whole child physically, emotionally and academically. We provide families with the teams and resources to thrive today and years to come.
From social workers and child life specialists to psychologists and educators, we surround families with a team that supports the whole child physically, emotionally and academically. We provide families with the teams and resources to thrive today and years to come.
From social workers and child life specialists to psychologists and educators, we surround families with a team that supports the whole child physically, emotionally and academically. We provide families with the teams and resources to thrive today and years to come.
We provide specialized follow-up care for childhood cancer and bone marrow transplant survivors. Whether it’s understanding how your child’s cancer treatment affects their future medical care or providing ongoing school support, the Children’s multidisciplinary team at the Survivorship Clinic is here to support your child and your family in the years ahead.
(5437). and ChildrensNebraska.org/Cancer
Children’s offers the only comprehensive Neurofibromatosis (NF) Clinic in the region. NF is a genetic disorder that affects the nervous system and can lead to tumors. Because
Children’s offers the only comprehensive Neurofibromatosis (NF) Clinic in the region. NF is a genetic disorder that affects the nervous system and can lead to tumors. Because
Children’s offers the only comprehensive Neurofibromatosis (NF) Clinic in the region. NF is a genetic disorder that affects the nervous system and can lead to tumors. Because


the condition can impact many parts of the body, our clinic includes a multidisciplinary team of skilled pediatric providers across many specialties.
the condition can impact many parts of the body, our clinic includes a multidisciplinary team of skilled pediatric providers across many specialties.
the condition can impact many parts of the body, our clinic includes a multidisciplinary team of skilled pediatric providers across many specialties.
This clinic cares for children with hemophilia, Von Willebrand disease, clotting factor deficiencies and other platelet disorders. Families meet with multiple specialists in one visit, reducing the need for additional appointments and providing complete, coordinated care.
This clinic cares for children with hemophilia, Von Willebrand disease, clotting factor deficiencies and other platelet disorders. Families meet with multiple specialists in one visit, reducing the need for additional appointments and providing complete, coordinated care.
This clinic cares for children with hemophilia, Von Willebrand disease, clotting factor deficiencies and other platelet disorders. Families meet with multiple specialists in one visit, reducing the need for additional appointments and providing complete, coordinated care.
We provide specialized follow-up care for childhood cancer and bone marrow transplant survivors. Whether it’s understanding how your child’s cancer treatment affects their future medical care or providing ongoing school support, the Children’s multidisciplinary team at the Survivorship Clinic is here to support your child and your family in the years ahead.
We provide specialized follow-up care for childhood cancer and bone marrow transplant survivors. Whether it’s understanding how your child’s cancer treatment affects their future medical care or providing ongoing school support, the Children’s multidisciplinary team at the Survivorship Clinic is here to support your child and your family in the years ahead. To make a referral, call 855.850.KIDS (5437).
To learn more about our specialists and programs, visit ChildrensNebraska.org/Cancer or scan the QR code.
We provide specialized follow-up care for childhood cancer and bone marrow transplant survivors. Whether it’s understanding how your child’s cancer treatment affects their future medical care or providing ongoing school support, the Children’s multidisciplinary team at the Survivorship Clinic is here to support your child and your family in the years ahead.
To make a referral, call 855.850.KIDS (5437).
To learn more about our specialists and programs, visit ChildrensNebraska.org/Cancer or scan the QR code.
To learn more about our specialists and programs, visit ChildrensNebraska.org/Cancer or scan the QR code.

■ By Alex Strauss
USD is building the healthcare workforce of tomorrow with help from more than $6 million in grants. In this month's cover feature, we explore what that money is doing, and how it could help more rural residents access the care they need.
PAGE 5 | [Sponsored]
Pork Delivers Where it Counts: Nutrition, Flavor and Satisfaction to Support Health and Wellness Goals
PAGE 6 | This Month Online
Nominate a MED Cover for 2026, Why SD is a top state for healthcare, upcoming fall events, and other exclusive online content
PAGE 8 | [Sponsored]
Case Study: How Comprehensive Planning Revolutionized Spencer Hospital’s Emergency Department
CMBA Architects' plan for Spencer illustrates the pivotal role of design in efficiency, staff satisfaction, and quality healthcare.
PAGE 14 | [Sponsored]
A Deep Dive into Hyperbaric Oxygen Therapy
■ By Daniel Todd, MD, FACS, of Midwest Hyperbarics
HBOT has long been used to treat wounds, but there's growing evidence that it's also effective for a host of other conditions ranging from hearing loss to post-stroke treatment to longevity.
PAGE 16 | NEWS & NOTES
PAGE 21 | USD School of Health Sciences Success Spotlight: Catherine Bilyeu
PAGE 22 | [Sponsored]
How an OB/GYN is improving clinician experience at Sanford Health
A Sanford doctor is spearheading some innovative solutions to combat burnout and promote wellbeing among her colleagues.
ELCOME to the September/ October issue of MED Magazine, where we’re focusing on one of healthcare′s most pressing challenges: how to build the workforce we desperately need.
In our cover feature, we explore how USD is tackling this head-on with more than $6 million in grants aimed at training the next generation of healthcare professionals. It’s inspiring work that could be a game-changer for rural communities across our region.
Speaking of deep dives, you’ll also discover the fascinating world of hyperbaric oxygen therapy and how it’s expanding beyond wound care to treat everything from hearing loss to stroke recovery. Plus, we take you inside Spencer Hospital's emergency department transformation a perfect example of how thoughtful design can bolster patient care and staff satisfaction.
If you like what you see here, subscribe to our newsletter to stay updated between issues.
All the best, —Alex & Steff
Publisher / MED MAGAZINE, LLC
Sioux Falls, South Dakota
Vice President Sales & Marketing
STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Magazine Design / ANGELA CORBO GIER
Client Relationship Manager / BARBIE MUNOZ
Digital Media Director / HYA AMURAO
CONTACT INFORMATION
STEFFANIE LISTON-HOLTROP
VP Sales & Marketing
605-366-1479
Steff@MidwestMedicalEdition.com
ALEX STRAUSS
Editor in Chief
605-759-3295
Alex@ MidwestMedicalEdition.com
WEBSITE
MidwestMedicalEdition.com
MAILING ADDRESS
PO Box 90646, Sioux Falls, SD 57109
10
JULY/AUG June 10
SEP/OCT August 10
NOVEMBER Oct 10
DECEMBER Nov 10
NEXT ISSUE
Editorial contributions due October 5
Ads due October 10
AS HEALTHCARE PROFESSIONALS, you know this truth well: Patients stick with what tastes good. That’s why pork’s role as a nutrient-dense, flavor-forward protein is gaining momentum in today’s dietary landscape.
Backed by clinical trials and national dietary guidelines, the Taste What Pork Can Do™ campaign highlights how pork delivers where it matters most: nutrition, flavor, and satisfaction.
• Pork tenderloin, sirloin chops, and sirloin roasts meet the American Heart Association Heart-Check standards as heart-healthy choices. In fact, today’s pork is leaner than ever—with 16% less total fat and 27% less saturated fat than 30 years ago.
• Lean pork fits into DASH and Mediterranean diets, supporting healthy blood pressure and cholesterol.,
• High-protein meals with pork improve post-meal blood sugar in adults with prediabetes and do not negatively impact insulin or glucose levels, helping debunk outdated myths about red meat and diabetes.,,
• Pork-based diets have been shown to reduce body fat and enhance physical function—especially in older adults.
• Pork’s high-quality protein boosts satiety, curbs cravings, and supports sustainable weight management.
Fresh pork is naturally low in sodium and provides:
• 22 g of high-quality protein per 3-ounce serving
• Key micronutrients like B6, niacin, thiamin, selenium, and choline
• Bioavailable heme iron and complete amino acids— especially valuable for aging adults and those with higher nutrient needs
And it delivers 110+ natural flavor notes from umami to floral—because nutrition that tastes good is nutrition that lasts. In fact, a recent clinical trial in older adults found pork outperformed other proteins on protein quality, meal enjoyment, and willingness to continue eating it post-study.
“Flavor drives behavior,” says Dr. Kristen Hicks-Roof, Director of Human Nutrition at the National Pork Board. “When food tastes good, people stick with it.”
Healthcare professionals are taking note
• 2,900+ dietitians and medical professionals now engage with the Pork & Partners network
❱ Access the online version of this article to see all of the referenced studies
• 71% of nutrition experts say they plan to recommend pork as part of their guidance LEARN MORE AND ACCESS PATIENT RESOURCES: https://pork.org/porkandpartners/ #TasteWhatPorkCanDo | @tastewhatporkcando
September 11–12 8:00 am – 5:00 pm
Iowa Healthcare Leaders Association (IHLA) Fall Conference
Location: Hilton Garden Inn, West Des Moines, Iowa

September 19 8:00 am – 4:00 pm
CNOS Occupational Medicine Symposium
Location: Holiday Inn Express, Dakota Dunes, SD
September 24–26 8:00 am – 5:00 pm
99th Annual SDAHO Convention
Location: Sioux Falls, SD
October 3 8:00 am – 4:30 pm
Avera Cancer Institute
Oncology Symposium
Location: The District Sioux Falls
October 7–8
9:00 am (Tues) – 12:00 pm (Wed)
Iowa Hospital Association
96th Annual Meeting
Location: Community Choice Credit Union Convention Center, Des Moines, IA
October 17 8:00 am – 4:00 pm
CNOS Orthopaedic
Sports Medicine Symposium
Location: Holiday Inn Express, Dakota Dunes, SD
October 22 9:00 am – 4:00 pm
Denials to Dollars Workshop [IHLA]
Location: Hilton Garden Inn West Des Moines
October 23 7:30 am – 4:00 pm
IHLA Panel of Payers
Location: Hilton Garden Inn West Des Moines
SEE THE WEBSITE for more upcoming live and virtual events and learning opportunities (and submit your own)
The USD Sanford School of Medicine announced last month that it would move the first 18 months of its Doctor of Medicine program from Vermillion to Sioux Falls starting in the summer of 2027.
USD shared the news at a joint press conference alongside the State of South Dakota, the City of Sioux Falls, the South Dakota Board of Regents and representatives from South Dakota’s major health care systems on Thursday, Aug. 14, 2025. This decision comes after the school celebrated 50 years of offering the MD in 2024.
USD’s medical education is currently split between locations, with the first 18 months of the medical program taking place on USD’s main campus in Vermillion. Consolidating the first 18 months of medical education in Sioux Falls will enhance students’ pre-clinical education by giving them more opportunities to work with and learn from clinical faculty.
VISIT OUR WEBSITE TO READ THE FULL ANNOUNCEMENT AND WATCH USD’S VIDEO ON THE IMPACT OF THE CHANGE
With the average American spending nearly $14,600 per year on personal health care, the personal-finance website WalletHub recently released its report on 2025’s Best & Worst States for Health Care.
In order to determine where Americans receive the highest-quality services at the best prices, WalletHub compared the 50 states and the District of Columbia across 44 key measures of health care cost, accessibility and outcome. The data set ranges from the average monthly insurance premium to physicians per capita to the share of insured population.
Health Care in South Dakota (1=Best, 25=Avg)
✦ Overall Rank: 10th
✦ 9th Hospital Beds per Capita
✦ 21st Cost of Medical Visit
✦ 11th % of At-Risk Adults with No Routine Doctor Visit in Past Two Years
✦ 7th % of Adults with No Dental Visit in Past Year
✦ 18th % of Medical Residents
Retained
SEE OUR WEBSITE for a link to the full report and expert commentary.
Five hospitals in South Dakota are among the 4,800 nationwide recognized by the American Heart Association for consistently following up-to-date, research-based guidelines to ensure all patients have access to lifesaving heart and stroke care. Find out who they are on the website.


Dr. Melissa “Mo” Dittberner will be a featured speaker at SDAHO’s Annual Convention, taking place September 24-26, 2025, at the Sioux Falls Convention Center. Dr. Dittberner will share her lived experience as a person in long-term recovery, tracing her journey from addiction to advocacy. Get all the details about the SDAHO Convention on our website.

There is more to being found by parents searching online for healthcare for their children than just having an attractive website. The same principles apply to other types of providers, as well. The experts at Blend Interactive break it down in this exclusive online article.
Have you ever looked at a MED Magazine cover and thought, “They should do a feature on [fill in name of South Dakota area medical professional(s) doing something noteworthy.]”, we have good news! MED is once-again accepting nominations for our Cover Features in 2026. We give preference to institutions and individuals who are innovating in some way to advance healthcare in the region. Please submit your nomination via email to Info@MidwestMedicalEdition.com. Include the name of the person or people you are nominating, how to contact them, and up to 400 words on why you think MED subscribers should know about them. [ NOTE: MED cover articles are not paid features]












Scan the QR code on this page or visit MidwestMedicalEdition.com TO JOIN THE VIP LIST.

THE DESIGN OF HEALTHCARE FACILITIES plays a pivotal role in operational efficiency, staff satisfaction, and, most importantly, the quality of patient care. At CMBA Architects, we’re driven to design environments that foster healing for patients and deliver supportive spaces for staff. By designing with a people-first approach, we stay at the cutting edge of healthcare design and can give back to the people and communities we serve.
One of the ways we’re working to revolutionize healthcare design is by assisting our clients with master planning, where our team maps out flexible, long-term plans that consider technological advances, evolving industry trends, and shifting demographics. A comprehensive master plan keeps healthcare facilities agile, allowing them to respond effectively to immediate needs while strategically planning for future changes.
Spencer Hospital’s emergency department, located in Spencer, Iowa, collaborated with CMBA Architects on redeveloping its master plan. CMBA worked with Spencer Hospital to develop a plan that not only improved departmental needs and patient privacy but also enhanced the emergency department’s operational efficiency and accessibility.
An emergency department isn’t very helpful if you can’t find it when you’re in an emergency. The department sat opposite a well-traveled street and was difficult to spot. Spencer Hospital needed its emergency department to be centrally located, visible, and accessible to all.
What happens at the emergency department, stays at the emergency department. The department needed to improve privacy for its patients for the sake of both the provider and the patient.
Saving lives is risky business –safety must always come first. To

care for their community, an emergency department must care for its staff. The department needed to build safety features into its strategy to minimize risk for its staff.
The first thing CMBA looked to solve was the location of the emergency department. It needed to be in a more visible, centrally located, and accessible spot. The master plan moved the department to the opposite side and integrated striking signage, helping wayfinding and positioning the department for all to see.
Once the location was decided on, integrating design that prioritized patient and staff privacy was the next focus. CMBA integrated an on- and off-stage design for patients and staff to streamline care and allow what should be private to remain private. Providers have a designated section in the middle unseen by the patient, keeping the experience private and streamlined. Rooms have a door for the patient and the provider to avoid patients entering this designated section. This also cuts down on reaction times, as providers can easily react when a
situation arises. In addition to this style of layout, a triage room was added to assess patients as they come in and filter the appropriate care quickly, further enhancing the quality of patient care and efficiency of the department.
Lastly, CMBA integrated features into the design to prevent situations from escalating and provide a safety net for providers. Two behavioral holding rooms with retractable doors, hiding all potentially dangerous equipment, were included in the plan. These rooms serve as backups and help provide a safe spot for providers to take care of those who may be at risk.
Supporting healthcare providers is key to providing great care. By creating a master plan that meets a healthcare facility’s goals, like Spencer Hospital’s goal of improving departmental needs, patient privacy, efficiency, andquality of patient care, CMBA Architects is helping create better access to care in communities across the Midwest.
Spencer Hospital’s new Emergency department, which opened in August, marks the first major milestone is bringing its new master plan to life
With offices throughout Iowa, Nebraska, and South Dakota, CMBA is committed to partnering with hospitals and health systems to shape environments that support the future of healthcare.
Our mission is to create healing environments that prioritize safety, comfort, and well-being by supporting patients, empowering staff, engaging communities and inspiring innovation through creativity and compassion. ❖



THE SAME VAST RURAL LANDSCAPES that many South Dakotans find so beautiful can also make it enormously challenging to deliver health care here. Many rural communities are separated by hours of driving and there are never enough healthcare professionals to serve them.
That’s why the University of South Dakota School of Health Sciences is taking a bold, strategic approach to help meet South Dakota’s healthcare workforce needs. Through four major federal grants totaling over $6 million, USD is not just training the next generation of healthcare providers—it’s reshaping how they think about rural practice.
These grants represent a huge investment in South Dakota’s healthcare future: a $1.05 million HRSA grant focused on rural nursing workforce development, a $3 million Department of Labor nursing expansion program, a $1.1 million HRSA telehealth training initiative, and a $1.06 million COMPASS grant targeting mental health professional shortages.
Together, these programs are creating new pathways for students to discover what’s rewarding about rural healthcare while building systems that will support them for the long haul.
For Dalton Bremer, who grew up in the small northwestern Iowa town of Ocheyedan, the HRSA grant’s rural immersion program was a gamechanger. Through the grant, he spent ten shifts over three weeks at Freeman Medical Center in Freeman, South Dakota. The experience completely changed how he thought about rural nursing.
“It’s not that nursing is drastically different in a small hospital,” Bremer explains. “It’s just that you are the only one there—there’s no IV team, there’s no wound care team. You are practicing the full depth of all of your skills.”
Anne Pithan, Chair of USD’s Department of Nursing, says this is exactly the point. “It has allowed us to immerse these students in rural communities and hospitals to really expose them to rural medicine and rural nursing care so that they can develop a love and passion for it.”
The three-year, $1.05 million grant, which started in 2022, places students in rural healthcare settings all across South Dakota—places like Hot Springs, Pine Ridge, Vermillion, Tyndall, Viborg, Sturgis, Mitchell, Canton, Freeman, and Chamberlain. The program picks up the
BY ALEX STRAUSS
tab for students’ lodging, meals, and travel, which removes the financial barriers that might otherwise keep students from participating.
For Bremer, the experience built confidence that extended far beyond his three weeks in Freeman. “It really pushed me to grow in my skills. After I did those ten shifts, I felt much more confident practicing those skills in the next year of nursing school. I really felt more like a nurse than a student.”
Now working at Avera McKennan Hospital in Sioux Falls, Bremer’s longterm goal remains unchanged: returning to rural practice in his home town. “There are so many different avenues to make an impact on those communities that you serve. For me, it’s a way of giving back to the place that raised me.”


While the HRSA grant immerses individual students in rural practice, USD’s $3 million Department of Labor grant supports a broader, two-pronged approach to address the nursing shortage. The first prong includes targeted recruitment and education in collaboration with workforce development and practice partners. The second is about facilitating collaborations to improve nursing workforce pipelines in the future. The exceptionally competitive five-year grant runs through May 2028.
One ambitious goal with this grant
funding is to credential 128 nurses with bachelor’s and master’s degrees for employment in South Dakota. At the halfway point, the program has already credentialed 63 new nurses—putting it on track to meet its targets.
The grant has also allowed for the creation of the South Dakota Nursing Network (SDNN), of which Pithan is now the leader. “The South Dakota Nursing Network is an entirely volunteer organization including educators, bedside nurses, leadership, and representatives of regulatory bodies—all committed to making nursing excellent in the state of South Dakota,” says Pithan.
The DOL grant led to the creation of four distinct action teams that address different aspects of workforce development: recruiting diverse nursing candidates, improving training for high-demand specialties like mental health nursing, expanding preceptor programs, and reviewing practice policies, environments for nurses, and employment standards. This team also hosts an annual SDNN nursing summit—this year scheduled for October 21st in Sioux Falls.
What makes the South Dakota approach unique, according to Pithan, is the genuine spirit of cooperation that defines the state’s nursing community. “The specialness of South Dakota is that people care so much about the nursing profession. There’s much more camaraderie here. You don't see that as much in other states.”
This collaborative approach extends to the practical impact of the grant. “Sometimes it’s just that little bit of extra help that can really bring people into the profession,” says Pithan, referring to the financial support and pathway programs that have already brought more than 60 new nurses into South Dakota’s workforce.
Recognizing that not every community can support on-site specialists, USD’s $1.1 million HRSA telehealth grant is preparing students to deliver care through innovative technology platforms. The three-year initiative brings together the School of Health Sciences, the Sanford School of Medicine, the Department of Communication Sciences & Disorders, and the Department of Psychology in an interprofessional approach to telehealth education.
“Introducing telehealth early in their education provides students with a solid foundation in utilizing this technology to deliver healthcare services,” explains Ranelle Nissen, Associate Dean of Academics in the School of Health Sciences.
COMPASS grant (Clinical Opportunities for Mobilizing Professionals in Assisting South Dakota’s Service gaps) specifically targets the behavioral health needs of children, adolescents, and young adults aged 16-25.
Led by Kelly Bass, Chair of USD’s Department of Social Work, the two-year program provides stipends to Master of Social Work students who complete 250-hour clinical placements with community mental health agencies, the state psychiatric hospital, or clinics serving other underserved areas. The program also pays for clinical supervisors’ training time and provides free continuing education units for participating social workers.



The program uses a hub-and-spoke model, with USD serving as the hub and rural clinical sites across the state functioning as spokes. This design allows students to gain hands-on experience with telehealth technology while rural communities benefit from expanded access to specialized services.
“Students gain practical hands-on experience with telehealth equipment, enhancing their proficiency and confidence in this essential aspect of healthcare,” says Nissen. The goal extends beyond individual student training to create a regional telehealth consortium that will facilitate resource sharing and collaboration among healthcare partners throughout South Dakota.
The newest addition to USD’s grant portfolio addresses one of healthcare’s most pressing challenges: the shortage of mental health professionals. The $1.06 million
The partnership with the South Dakota Department of Social Services Behavioral Health Program and the Human Services Center creates direct pathways from education to employment, addressing the reality that all of South Dakota faces mental health professional shortages, with particularly problematic declines in children’s and youth mental health.
Together, these four grants represent more than individual program successes—they demonstrate USD’s comprehensive understanding of rural healthcare workforce challenges and its commitment to sustainable solutions. By addressing nursing, telehealth, and mental health simultaneously, the university is creating an interconnected system that supports both providers and communities.
And the impact extends beyond the immediate grant periods. Students like Dalton Bremer carry their rural immersion experiences into their careers, while the South Dakota Nursing Network builds lasting infrastructure for collaboration and support. The telehealth training prepares graduates for the realities of modern healthcare delivery, and the COMPASS program addresses critical mental health needs that affect every community.
As these programs continue to evolve and expand, they’re not just filling workforce gaps—they’re fostering a new generation of healthcare providers who understand the unique rewards and challenges of rural practice. In a state where geography often determines access to care, USD’s grant-funded initiatives are helping ensure that quality healthcare can reach even the most remote communities. ❖



BY DANIEL TODD, MD, FACS OF MIDWEST HYPERBARICS

As an otolaryngologist, I have been using Hyperbaric Oxygen Therapy (HBOT) for the past 30 years, primarily in the treatment of patients with head and neck cancer. But the advent of small and powerful oxygen generators and compressors has paved the way in recent years for the development of powerful HBOT chambers for home use.
My renewed interest in the many other applications for HBOT started after my wife was asked to help a friend get in and out of her home chamber. The friend had experienced remarkable results with low-pressure HBOT treatments at home for her ulcerative colitis.
After my wife tried the chamber herself and had positive results for her fibromyalgia and neuropathies, she informed me that we were buying one. Before you knew it, we had a constant stream of friends and family coming through our home “clinic” to treat various issues with HBOT.
At the same time, my stepdaughter, Jada Hieb, was just finishing her DNP training. With such clear demand for HBOT and a new professional in the family to work with, it seemed like the perfect time to open our outpatient facility, Midwest Hyperbarics, in Sioux Falls. Jada, who has a background in cardiology, has an overall understanding of both the medical and business side of HBOT that has been invaluable in our clinic.
Because many patients are claustrophic in monoplace chambers, we also invested in a three-seat walk-in chamber. All multiplace walk-in chambers are compressed with medical grade room air while the patient breathes 100% oxygen through a mask or hood, nearly eliminating the risk of fire or other types of accidents that have been reported in some other facilities. We have also reconfigured our monoplace medical grade chambers to operate this way because of the safety benefits.

Based on our positive experience with home chambers, we also elected to sell hardshell monoplace chambers for home use. At a maximum of 2 ATA (Atmospheres Absolute), these chambers hit the “sweet spot” of both efficacy and safety and are ideal for people with chronic conditions who want ongoing therapy at home.
After using HBOT for several patients with Sudden Sensorineural Hearing Loss, I am making it my personal mission to raise awareness of how early diagnosis and treatment can be a game changer in this condition.
Many insurance plans cover HBOT for this application, which is recommended along with early steroids by the American Academy of Otolaryngology. At Midwest Hyperbarics, our onsite microscope allows us to place topical steroids in the middle ear, when indicated, as well as to perform myringotomies or place tubes, when necessary.
HBOT therapy really shines in acute neurologic injury such as concussion. Just a few treatments and the post concussive symptoms disappear. We assume that this works much the same way for concussion as it does for early hearing loss. Post stroke patients with idiopathic cranial neuropathies such as facial paralysis will certainly see benefit, as well.
I have personally seen the benefits of HBOT in facilitating recovery after surgery or trauma. A colleague underwent two total knee replacements at two different times, one with post-operative HBOT and one without. Although it is anecdotal, my colleague recovered in a fraction of the time with the HBOT. HBOT literally squeezes the edema of the affected area with each session and oxygenates the inflamed operative site. Professional athletes use this

Netflix “Don’t Die” personality Bryan Johnson finally got around to purchasing a home HBOT chamber and found the benefits outperformed everything else he had tried. He shares his results in a YouTube video entitled “This machine made me younger”.
Wound care seems to be the predominant indication for HBOT. Poor circulation, often due to diabetes, radiation, or just bad luck, can lead to very poor wound healing. Working with vascular surgeons and/or podiatrists to avoid the next amputation can be both challenging and rewarding. Our newest DNP, Jessica Freudenthal, has a passion for wound care and has helped start a wound care center in the past. We are looking forward to having her help us develop this area of our practice. ❖


For more information on home HBOT chambers available through Midwest ENT: Midwesthyperbarics.com/sales
For a complete referral guide with a list of insurance indications for HBOT: Midwesthyperbarics.com /referral guide
The fascinating physiology of pressure can be illustrated by the paper “Life without blood” [Boerema, 1960] where researchers replaced the red blood cells with serum in piglets, which then lived with a hemoglobin of zero in a 3 ATA chamber with no morbidity. The pressure bypasses the need for red blood cells to carry the oxygen, because it compresses it directly into the serum and tissues. This is what allows us to oxygenate and heal tissue that is not getting a good blood supply. Which basically describes nearly every injury known to man.

Monument Health Foundation’s fourth Golden Guitars Gala raised a record $500,000 for Children’s Miracle Network in June, setting a Foundation record for the largest amount raised at a single event. During the gala’s live auction, the top-selling guitar signed by Journey auctioned for an impressive $30,000. The event has featured 19 celebrity guitars plus two surprise guitars from Whiskey Meyers and Music Row Live artists. More than 250 attendees participated in the fundraiser, which supports children receiving care at Monument Health hospitals in the Black Hills region.
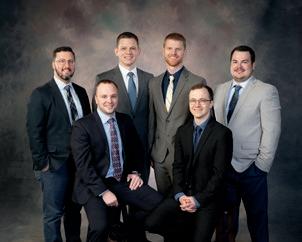
Six new physicians have graduated from Monument Health’s Family Medicine Residency Program. Two will stay on as faculty, three will join Monument Health clinics, and one is entering a sports medicine fellowship. The three-year residency program focuses on family medicine with an emphasis on rural healthcare

Monument Health’s Bhaskar Purushottam has co-authored a research paper in the Journal of Endovascular Therapy on profunda femoral artery retrograde puncture techniques for complex blocked blood vessels in lower extremities. The study represents the largest series published using this technique for Ilio-Femoral Chronic Total Occlusions in patients with Peripheral Arterial Disease. Purushottam was the only United States-based physician contributing to the research paper.

provides an automated blood pressure cuff and educational materials for adults to check their blood pressure and learn about cardiovascular health. The initiative addresses the fact that nearly half of Americans have high blood pressure, with many unaware of their condition due to lack of symptoms.
Monument Health Rapid City Hospital has received the American Heart Association’s Get With The Guidelines-Stroke Gold Plus quality achievement award along with the Target: Stroke Honor Roll and the Target: Type 2 Diabetes Honor Roll awards. The recognition acknowledges the hospital’s commitment to ensuring that all stroke patients receive appropriate treatment according to research-based guidelines. These awards also mean they adhere to specific criteria that reduce time between patient arrival and treatment with thrombolytic therapy.
Sanford Health will run its fourth annual Summit on the Future of Rural Healthcare on October 14th at the Sanford Barn in Sioux Falls. The theme “Advancing access, quality and sustainability” will feature conversations with health system CEOs and industry experts. Confirmed speakers include Bill Gassen, Rick Pollack from the American Hospital Association, and CEOs from Dartmouth Health, HealthPartners and Providence. The event will also be available to livestream.


Becker’s Hospital Review has named Sanford Health’s Brad Reimer to its 2025 list of hospital and health system CIOs to know. At the same time it has also named Sanford Luverne and Rock Rapids CEO Tammy Loosbrock to its 2025 community hospital CEOs to know list for the third consecutive year. As senior vice president and chief information officer, Reimer oversees technology systems, patient-critical applications, business solutions, infrastructure and information security. Loosbrock oversees hospitals serving residents in surrounding rural areas including clinics in Adrian and Edgerton, Minnesota.
Sanford Imagenetics and the Department of Veterans Affairs have reached 100,000 pharmacogenomics tests through the Pharmacogenomics testing for Veterans (PHASER) program. The program helps clinicians understand medication interactions with patients’ genetic makeup. Approximately 90 percent of people have gene changes that can affect how they respond to medication.. Free tests are available through 2025 for patients with eligible military status.

The American Hospital Association has named Sanford Health CEO Bill Gassen as Chair-elect Designate, positioning him to become the 2027 Chair of the national organization representing America’s hospitals and health systems. Since 2020, Gassen has helped transform rural healthcare at Sanford Health, which serves over two million patients across the upper Midwest. He has previously served in executive roles including chief administrative officer, corporate counsel, and chief human resources officer.

Sanford Health’s David Newman was part of a panel discussion on AI applications in healthcare at the American Hospital Association Leadership Summit in Nashville in July. The panel, titled “Cutting-edge AI Transforming the Patient and Clinician Experience,” examined real-world AI applications in diagnostics, risk assessment and workflow optimization. Newman serves as vice president and chief medical officer for virtual care at Sanford.

Jon Pociask has been named chief operating officer for Sanford Health Sioux Falls Region South Network, overseeing operations for clinics and medical centers in South Dakota, northwest Iowa and southwest Minnesota. Pociask previously served as vice president of operations for primary care and behavioral health services, starting his Sanford career in 2005.
Four Good Samaritan locations have received 2025 Silver Achievement in Quality awards from the American Health Care Association and National Center for Assisted Living. The award recipients include facilities in Albion, Nebraska; Howard Lake, Minnesota; Fargo, North Dakota; and Pipestone, Minnesota. The recognition represents the second of three progressive levels in the National Quality Award Program, with data showing Silver and Gold recipients outperforming national averages.
Sanford USD Medical Center has received the American College of Cardiology’s NCDR Chest Pain-MI Registry Platinum Performance Achievement Award for 2025, joining only 323 hospitals nationwide with this recognition. The award acknowledges sustained achievement over two consecutive years and performance at the highest level for specific measures.
Military Friendly Brands has ranked Sanford Health No. 3 in the Government & Non-Profit category on its annual list of organizations that provide opportunities for veterans and military spouses. Sanford was the top-ranked healthcare system on the list. Among the benefits Sanford offers are differential pay during deployment, continuation of benefits, automatic screening interviews for veteran applicants, and $5,000 scholarships for military and veteran employees pursuing education.

Sanford Health’s Nurse Residency Program has received Full Accreditation with Distinction from the American Nurses Credentialing Center Practice Transition Accreditation Program, maintaining recognition it first received in 2021. The program is among 297 accredited programs worldwide and the first and only one in North Dakota to receive accreditation with distinction. The evidence-based program supports new nurses with less than 12 months of experience transitioning from student to professional registered nurse.
Sanford Medical Education and USD Sanford School of Medicine have received accreditation to launch South Dakota’s first emergency medicine residency program. The three-year program will accept six residents annually beginning July 2026. Residents will complete 25 months of core EM training, including time at Sanford’s new 12-bed pediatric Emergency Department, opening in 2026, as well as rotations in ICU, obstetrics, surgery and other specialties.
Creekside Medical Clinic, an independent physician-owned group in Rapid City, has agreed to join Sanford Health effective September 1. practice includes four family medicine physicians and two advanced practice providers serving western South Dakota for over 25 years. The clinic will continue operating at its current location on Jackson Boulevard with no disruption to patient care, offering comprehensive outpatient medical care and preventive health services.


Foundation Park, a 330,000-square-foot facility that consolidates multiple departments including centralized pharmacy services, supply chain distribution, biomedical engineering, and home medical equipment operations. The center serves as central distribution for medical supplies across Avera’s network of hospitals, clinics and long-term care centers in 100 communities. Enhanced automation includes conveyor belts and dispensing robots to improve efficiency and allow pharmacists more time for direct patient care.
Avera McKennan Hospital & University Health Center has received the Get With The Guidelines Heart Failure Silver Plus award from the American Heart Association, along with Target: Heart Failure Optimal and Target: Type 2 Diabetes Honor Roll recognition. The quality achievement award recognizes hospitals demonstrating commitment to treating patients according to evidence-based guidelines, aiming to increase healthy days at home and reduce hospital readmissions for heart failure patients.
on the American Registry of Radiologic Technologists certification exam for its 2025 Radiologic Technology program graduates for a fifth consecutive year. All 17 graduates passed the national certification exam on their first attempt. The ARRT certification represents a national standard for medical imaging professionals, and the 100% pass rate demonstrates the college’s commitment to academic excellence.
UnityPoint Health St. Luke’s has received the American College of Cardiology’s NCDR Chest Pain-MI Registry Silver Performance Achievement Award for 2025, marking the eighth year in the last 10 years the hospital has received this recognition. The award acknowledges sustained achievement in the registry and performance with distinction in specific measures. St. Luke’s is one of nine UnityPoint Health hospitals receiving performance achievement awards from the American College of Cardiology.
that ran from June 9 to July 6. Ten Siouxland locations participated in the fundraising by asking associates, customers and members to support children’s healthcare. The funds help pay for medical equipment, research, therapy programs and charitable care at UnityPoint Health St. Luke’s for children in the region.

Brenda Nyatanga, MD, is joining the cardiology team at UnityPoint Health–St. Luke’s in Sioux City. Dr. Nyatanga treats a variety of patients with conditions such as high blood pressure, high cholesterol, coronary artery disease and arrhythmias, as well as those focused on preventive care due to family history or lifestyle risks. Her approach is known to be meticulous and empathetic, fostering strong provider–patient relationships built on trust and collaboration. Dr. Nyatanga will offer services at two locations in Sioux City.

Spencer Hospital in Spencer, Iowa opened its new Emergency Department in mid-August. The new facility, visible from Grand Avenue, will improve accessibility for patients and families during urgent medical situations. Access to the Emergency Department is located on East 11th Street off Grand Avenue. The new ED represents a major investment in the health of the community, combining advanced design with the same trusted, patient-cen tered care Spencer Hospital is known for.

Yankton Medical Clinic’s Scott Weber has received the Edward J. Batt Memorial Teaching Award from the USD Sanford School of Medicine Department of Family Medicine. The award recognizes physicians with at least three years of appointment who demonstrate outstanding commitment to medical education, actively teach in clerkships, and receive high evaluations from students and faculty. Weber serves as Clinical Professor at the Sanford School of Medicine while maintaining a full-time family and sports medicine practice.


Joseph Elliott, a boardcertified interven -
tional cardiologist, has joined the team of heart specialists at Prairie Lakes Healthcare System. Dr. Elliott grew up in Ohio and earner his MD from Ross University School of Medicine in Dominica. He completed his internal medicine residency at the Canton Medical Education Foundation/Aultman Hospital NEOMED Program in Canton, Ohio, where he also completed fellowship training in cardiovascular disease and interventional cardiology. He joins physicians Ravi Kalaga, Jacklyn Karli, Travis Erickson, and Kahley Meyer in the Prairie Lakes Cardiology Clinic and Cardiac Catheterization Lab.
Healthcare System’s 28th Annual Hospital Hill Run in June. The event featured 5K run and walk events, a one-mile kids run, and a one-mile walk for all ages. Proceeds from the event support the Prairie Lakes Caring Club House, a not-for-profit, community-based project of the Prairie Lakes Healthcare Foundation, with support from PLHS. The Caring Club House provides lodging for out-of-town patients, families, and caregivers receiving services through Prairie Lakes services.

PLHS nephrologist Tina Melanson won the 2025 Volunteerism Award from the South Dakota Chapter of the American College of Dr. Melanson, who has served patients at Prairie Lakes for the past 14 years, co-founded the Lake Area Kidney Endowment in 2015, which has donated nearly $171,000 to local patients with chronic kidney disease. The funds help pay for transportation, medication costs, and other essential resources. The organization assists individuals in northeast South Dakota and western Minnesota, keeping support local and addressing immediate patient needs.

Prairie Lakes Healthcare System has moved its Podiatry Clinic to the second floor of the Prairie Lakes Specialty Clinic, joining other specialty services under one roof. The relocation from Prairie Lakes Brown Clinic-Main offers patients a more centralized and convenient experience. Laurie Fieber, Vice President of Service Line Operations, will allow for more seamless, collaborative care.
Orthopedic Institute (OI) has opened an outreach clinic in Luverne, Minnesota. The expansion offers Luverne residents easier access to specialized orthopedic services without the need for long-distance travel. Located within Freedom Family Clinic on West Gabrielson Road, the new OI clinic will provide diagnosis and treatment of musculoskeletal conditions with a focus on hip, knee, foot and ankle, shoulder, elbow, and other sports-related injuries. When surgery or advanced diagnostic imaging is required, patients will be seamlessly referred to Orthopedic Institute’s main clinic in Tea, South Dakota.







Joel Nelson has been named interim Vice President of Finance and Chief Financial Officer at Huron Regional Medical Center and Janna Rose has been promoted to Director of Revenue Integrity. Nelson has been with HRMC for 32 years and previously served as controller and head of the Fiscal Services department. Janna Rose led Materials Management operations for over 17 years.
Levi Kary is the new director of Human Resources at HRMC, transitioning from his role as HRMC Foundation Executive Director. Mati Felderman has combined marketing and communications responsibilities with Foundation leadership and is now Executive Director of Community Engagement and the HRMC Foundation. The changes align individuals with organizational goals while ensuring continued advancement of the hospital’s mission and the work of the Foundation.
Brookings Health System has appointed Megan Sinner as its new ambulance director and Lora Nelson as director of surgical services. Sinner, a nationally registered paramedic with 16 years of emergency medical services experience, oversees pre-hospital advanced and basic life support services. Nelson brings 29 years of nursing experience and 14 years of clinical leadership to oversee perioperative staff in outpatient surgery, preoperative units, operating rooms, and sterile processing.

Tammy Hatting is the new CEO of the South Dakota State Medical Association. Hatting succeeded Barb Smith who retired after 25 years with the organization. Hatting has served as chief operating officer for the South Dakota Association of Healthcare Organizations for seven years, with responsibilities including government relations, lobbying, emergency preparedness, and policy development. Hatting holds a master’s degree in public administration and a bachelor’s degree in healthcare administration from Bellevue University, as well as an associate degree in financial management from the American College of Business in Des Moines. Her healthcare experience includes working at critical access hospitals, patient access management, EMR initiatives, and telemedicine advocacy.
LifeScape held a new fundraising event in June called “Small Shops, Big Impact”. The event was designed to support both LifeScape’s mission and local small businesses. The eight local businesses that participated in this year’s event all had some personal or professional connection with LifeScape and included Makers Exchange, Apricot Lane Boutique, Mulberry Market, Josiah’s Coffeehouse & Café, Say Anything Jewelry, Zandbroz Variety, MK Threads, and Remedy Brewing Company. Participants paid $25 to register ($40 for two shoppers shopping together) and received tote bags, Bingo cards, route maps.
Catherine Bilyeu, PT, DPT, PhD
Degree: Doctor of Physical Therapy, PhD in Health Sciences
Current Position: Associate Director of Clinical Education Assistant Professor, University of Colorado Anschutz Medical Campus

For Catherine Bilyeu, the USD School of Health Sciences made the path from practicing physical therapist in Canada to academic leader in Colorado considerably smoother than it might otherwise have been. Bilyeu says USD recognized her unique journey from the beginning and helped her fill educational gaps at every stage of her career.
Bilyeu grew up in Canada where she earned her original PT degree and built a successful clinical practice. But a few years into her career, she found herself at a crossroads: “I got to a certain point where all PT programs in the US had transitioned to a clinical doctorate and I just had a bachelor’s degree,” she says.
When she decided to pursue a clinical doctorate, USD had protocols in place that made it especially attractive to a foreign-trained graduate. “A lot of other programs wouldn’t recognize that my education had already been credentialed, but USD did,” she says.
USD’s DPT program proved to be exactly what Bilyeu needed. It gave her the tools to not only critically assess research literature but also get started producing her own. “It really filled the gaps that I had in my education to allow me to practice at a higher level,” she says.
Later, when Bilyeu transitioned to education full-time, she returned to USD to hone her skills. “I had such a great experience in my clinical doctorate that I decided to pursue my PhD in Health Sciences at USD,” she says. “The program allowed me to fill the leadership and research gaps and enhance my knowledge around teaching and learning.”
Today, Bilyeu is using the knowledge she gained to do research on faculty development and competency frameworks for clinical instructors. “I really can’t speak highly enough of the USD programs,” she says. “It has dramatically changed my depth of knowledge around health professions education.”
This SUCCESS SPOTLIGHT brought to you by
❱ Intrigued by something you’ve read here? Want to go deeper? Read the full versions of these and other recent news items on our website.

IF YOU’RE A CLINICIAN, you know how easy it is for stress to pile on.Compassion fatigue, long hours and staff shortages can all negatively affect physical and mental health for medical professionals.
These issues can lead to burnout, and according to the American Medical Association, nearly half of all physicians experienced at least one symptom of burnout in 2023.
For health systems like Sanford Health, addressing burnout head-on is critical to improving the clinician experience and, subsequently, patient care. Heather Spies, MD, is
an OB/GYN and the physician director of clinician experience and well-being at Sanford Health. Through her leadership and collaboration with her peers, Dr. Spies is making strides to improve clinicians’ lives at work and at home.
DR. SPIES’ CAREER AS A PHYSICIAN AND LEADER
From delivering babies and caring for women of all ages to leading internal well-being initiatives, Dr. Spies does a lot to care for others at Sanford Health, and she’s been doing it for a long time.
“I’ve been with Sanford Health
my entire career,” said Dr. Spies. “I’ve worked here for over 18 years, and there have been a lot of changes during that time, but I’ve always felt like I’ve had access to the resources, support and opportunities I need to grow. It’s an incredible place to work for.”
Dr. Spies initially started her practice at Sanford Health in Watertown, South Dakota, and while she’s always loved her job, she’s struggled with managing her well-being in the past.
“Balancing my practice with raising a family was difficult, and to be honest, I didn’t always balance it well,” said Dr. Spies. “One emphasis we have within Sanford Health is that we need to model well-being and look out for each other. We support each other, so it truly feels like we’re a family.”
In 2011, she was invited to join Sanford Health’s Leading the Way program. This gave her the ability to form deeper relationships with her peers and learn from physician and non-physician leaders in the organization.
“I built a community of people around me to check in with and bounce ideas off of,” said Dr. Spies. “We often go through similar experiences when we’re trying to raise a family or balance our personal life with our career, so having a support network was really beneficial for my well-being and growth.”
The Leading the Way program resonated with Dr. Spies and sparked
a desire in her to do more to help her fellow clinicians, which she has done in many different roles since then.
After moving to Sioux Falls, South Dakota, in 2015, Dr. Spies went on to obtain an MBA in organizational leadership. During that time, her colleagues, mentors and leaders at Sanford Health were very supportive, and she was able to continue her full-time clinical practice.
Once she finished her degree, Dr. Spies got to pioneer a new role within Sanford Health — physician director of clinician experience and well-being. This would eventually lead to the formation of groups like the Clinician Well-being Council (CWC) and the Sanford RISES clinician leadership program.
The CWC supports clinicians’ professional and personal lives by prioritizing, advocating for and modeling clinician well-being throughout the organization.
“Working in health care can be stressful no matter where you practice or what your specialty is,” said Dr. Spies. “It’s absolutely essential to us to prioritize clinician experience. If we don’t support our people, they may burn out.”
RISES stands for Reaching Others, Innovating and making an impact, Strategizing to support and sustain the organization, Elevating and empowering others, Serving our colleagues and communities. The program provides Sanford Health’s top clinicians with a chance to grow and embrace their role as a leader. The participants in this program apply with a letter of support from their leaders and are chosen by a selection committee. The goal of the program, like many others, is to build the best culture possible for every clinician at Sanford Health.
“One of the reasons I’m proud
to work at Sanford is that we have very robust clinician assistance programs,” said Dr. Spies. “We support our clinicians. If a clinician would like to seek counseling or coaching for either personal or professional growth, we provide that to them for free.”
Another program Dr. Spies has seen make an impact on the well-being of clinicians is the AMA Joy in Medicine Health System Recognition Program. This program evaluates health systems based on six different categories — assessment, commitment, efficiency of practice environment, teamwork, leadership and support.
“As a part of this program, we as a health system acknowledge and commit to the organizational work that needs to be done to improve well-being in the workplace,” said Dr. Spies. “We are looking for ways to optimize teamwork and efficiency so clinicians have more valuable time with patients rather than administrative tasks. This, coupled with our leadership development initiatives, gives clinicians more joy in their work and makes them feel supported by their leaders.”
Sanford Health received the gold level of recognition from the program in 2023 and continually strives to maintain and improve the initiatives it has in place. Currently, it’s the only system based in the Dakotas to be recognized by the program.
Sometimes the solution for solving physician burnout and other well-being issues comes through technological advances like artificial intelligence. Dr. Spies has seen how it helps employees focus less on daily tasks and more on their patients.
“A lot of primary care physicians are going home and spending two or
three hours a night charting,” said Dr. Spies. “To cut back on this time, we recently introduced an AI tool that uses ambient technology to summarize and input notes into patient charts.”
Cutting back on time spent on patient charts gives physicians the ability to focus on what they enjoy the most — helping patients.
“I think one of the reasons I’ve worked here for so long is that I’ve received support when I needed it,” said Dr. Spies. “I’ve had peers, partners and colleagues step up to encourage me and help me find joy in my work, and it’s what makes Sanford Health so special.”
Sanford Health wants to improve the health of the communities it serves, and that includes the health and well-being of its clinicians, too.
“I love seeing the endless ways Sanford Health has contributed to where we live,” said Dr. Spies. “I have always felt that Sanford attracts people that like to collaborate, communicate and support each other. I have complete trust in the organization because the decisions we make are grounded in our values.”
By investing time and resources into its people, Sanford Health is doing everything it can to improve all aspects of health care.
“Ultimately, it comes down to the patients and giving them the best care we can,” said Dr. Spies. “If we aren’t taking care of ourselves, we can’t be on the top of our game.”
Careers at Sanford Health provide excellent pay, comprehensive benefits, and above all, the opportunity to serve your community. If you’re looking for a rewarding career with plenty of room to grow, start exploring our open positions at sanfordcareers.com today. ❖
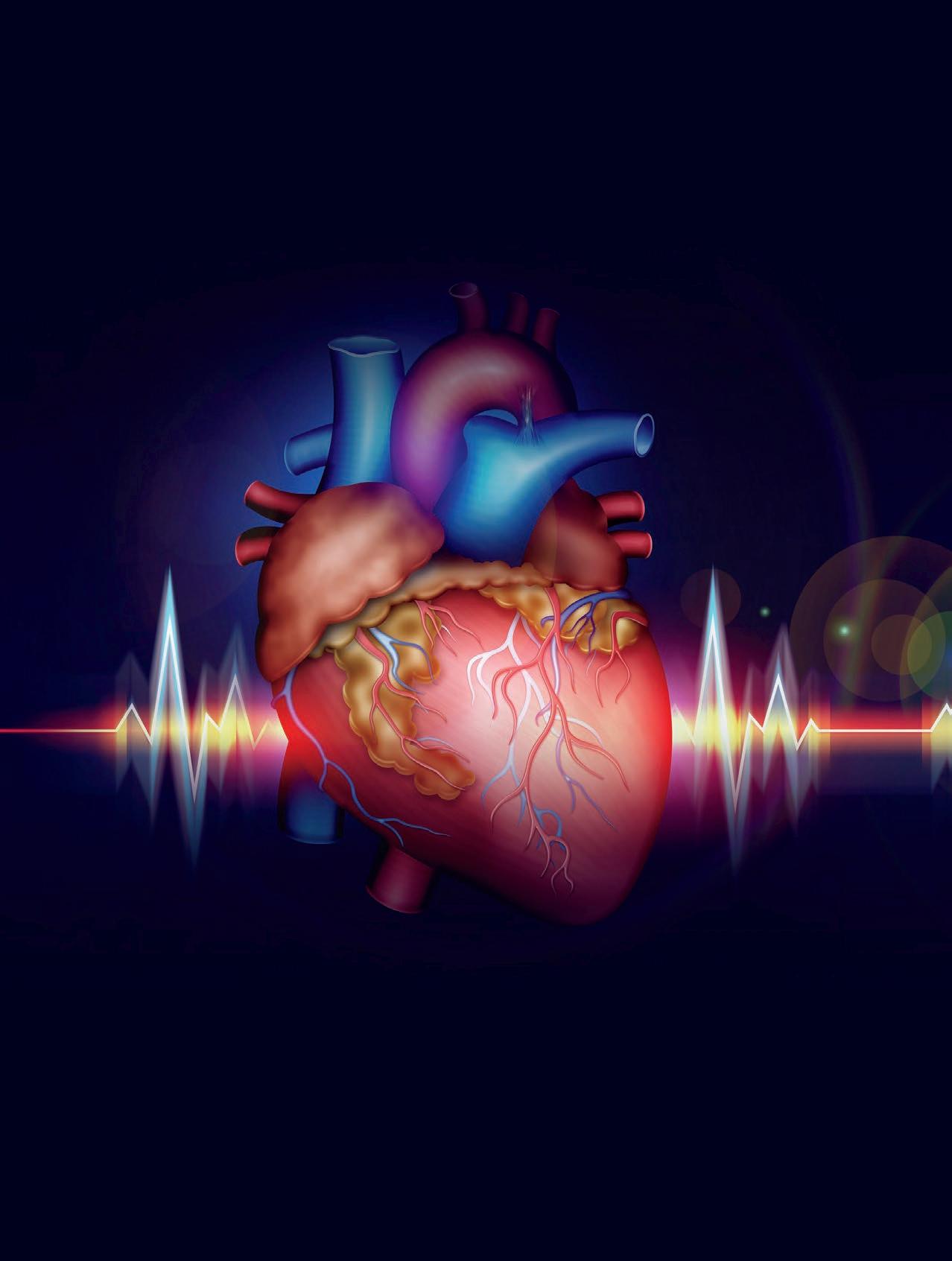
The Monument, Rapid City Oct. 16, 2025 7:30 a.m. – 5 p.m.
Snacks and lunch provided
CME/CE credits available
A day-long symposium offering a practical approach to advances in cardiovascular care and technology, new preventative strategies and the latest wellness information.
For additional information visit: monument.health/cardiovascularsymposium
In-Person and Virtual Options Available