The Science of Hope
Dr. Pilar de la Puente’s Mission to Change the Outlook for Women’s Cancers


LIFE IS Bett er WITH A TEAM YOU CAN TRUST
LIFE IS Bett er WITH A TEAM YOU CAN TRUST
We’re on your team to provide your patients with expert orthopedic care you both can count on. Sanford Orthopedics & Sports Medicine has been recognized by the Joint Commission for providing the highest quality of patient-centered, advanced care that goes unmatched in the region.
We’re on your team to provide your patients with expert orthopedic care you both can count on. Sanford Orthopedics & Sports Medicine has been recognized by the Joint Commission for providing the highest quality of patient-centered, advanced care that goes unmatched in the region.
We offer more treatments and more specialties, including:
We offer more treatments and more specialties, including:
• Sports medicine
• Sports medicine
• Total joint replacements and revisions
• Total joint replacements and revisions
• Orthopedic oncology
• Orthopedic oncology
• Wide-awake hand surgery
• Wide-awake hand surgery
• Trauma surgery
• Trauma surgery
• Pediatric surgery
• Pediatric surgery
• Foot and ankle surgery
• Foot and ankle surgery
• Podiatry
• Podiatry
• Concussion care
• Concussion care
• Joint injections
• Joint injections
• Hip arthroscopy and preservation
• Hip arthroscopy and preservation
• Robotic surgery
• Robotic surgery
Connect your patients to a full scope of orthopedic care. Visit sanfordhealth.org to refer a patient.
Connect your patients to a full scope of orthopedic care. Visit sanfordhealth.org to refer a patient.

16, NO. 7 ■ NOVEMBER

The Science of Hope
■ By Alex Strauss
Sanford Researcher Pilar de la Puente, PhD, is revolutionizing women′s cancer research with groundbreaking work on chemoresistance and early detection. Her innovative approach has earned elite NIH recognition, accolades from her hometown in Spain, and even a presence in a comic book!
PAGE 6 | This Month Online
The PT grad who trained with the doctor that saved her limb, Some pics from MED’s recent conference “road trips”, plus how to nominate a MED Cover for 2026
PAGE 12 | Best Practices in Documentation: Caring for Patients Unable to See Mental Health Specialists in a Timely Manner
■ By Dr. Eric Zacharias
At a time when so many people are in need of mental health services, what is the best way to protect yourself when your patient can′t get a timely appointment? The experts at COPIC say proper documentation is key.
PAGE 14 | NEWS & NOTES
The Avera Foundation sets a fundraising record, UnityPoint assumes ownership of MercyOne Siouxland, Sanford Research receives over $8 million from NIH, South Dakota’s first Rural Emergency Hospital, plus more healthcare headlines.
PAGE 19 | USD School of Health Sciences Success Spotlight: Lucas Seehafer, PhD
PAGE 21 | Beyond the Border: News from MED’s Multi-State Coverage Area
A North Dakota physician wins COPIC’s humanitarian award, Nebraska launches Certified Community Behavioral Health Clinics, and Iowa expands mobile training for rural providers
CONTACT INFORMATION
STEFFANIE LISTON-HOLTROP
VP Sales & Marketing
n this issue of MED Magazine, we introduce you to Dr. Pilar de la Puente, the Spanish-born cancer researcher whose infectious enthusiasm for science is matched only by her groundbreaking work. Her recent NIH MERIT grant is just the latest in a long line of accolades helping to put her — and Sanford Research — firmly on the national map.
We've also included important guidance from COPIC on documenting care for patients facing long waits for mental health specialists. And, of course, all the headlines from South Dakota and even some of the surrounding states.
In this season of gratitude, we are so grateful for your continued readership over these last 16 years. If you like receiving this publication in print, please take a moment to renew your subscription before the end of the year. (And if you don't yet receive the print edition, do yourself a favor and subscribe — It's beautiful!) You can do it quickly and easily at MidwestMedicalEdition.com/med-magazine
All the best, —Alex & Steff
Publisher / MED MAGAZINE, LLC
Sioux Falls, South Dakota
Vice President Sales & Marketing
STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Magazine Design / ANGELA CORBO GIER
Client Relationship Manager / BARBIE MUNOZ
Digital Media Director / HYA AMURAO
605-366-1479
Steff@MidwestMedicalEdition.com
ALEX STRAUSS
Editor in Chief
605-759-3295
Alex@ MidwestMedicalEdition.com
WEBSITE
MidwestMedicalEdition.com
MAILING ADDRESS
PO Box 90646, Sioux Falls, SD 57109
10 MARCH Feb 10 APRIL/MAY
10 JUNE May 10
JULY/AUG June 10
SEP/OCT August 10
NOVEMBER Oct 10
DECEMBER Nov 10
NEXT ISSUE
Editorial contributions due November 5 Ads due November 10
Children’s Nebraska Recognized as a Best Children’s Hospital by U.S. News & World Report
Children’s Nebraska Recognized as a Best Children’s Hospital by U.S. News & World Report
Children’s Nebraska Recognized as a Best Children’s Hospital by U.S. News & World Report
U.S. News & World Report has ranked Children’s Nebraska in its 2025-26 Best Children’s Hospitals rankings in the specialties of Pediatric Nephrology, Pediatric Neurology & Neurosurgery and Pediatric Pulmonology & Lung Surgery.
U.S. News & World Report has ranked Children’s Nebraska in its 2025-26 Best Children’s Hospitals rankings in the specialties of Pediatric Nephrology, Pediatric Neurology & Neurosurgery and Pediatric Pulmonology & Lung Surgery.
U.S. News & World Report has ranked Children’s Nebraska in its 2025-26 Best Children’s Hospitals rankings in the specialties of Pediatric Nephrology, Pediatric Neurology & Neurosurgery and Pediatric Pulmonology & Lung Surgery.
The 19th annual Best Children’s Hospitals rankings recognize the top 50 pediatric facilities nationwide in 11 specialties. U.S. News partners with RTI International, a North Carolinabased research and consulting firm, to collect and analyze data from children’s hospitals and pediatric specialists across the country. Methodology factors in clinical outcomes, compliance with established best practices and level and quality of hospital resources directly related to patient care.
The 19th annual Best Children’s Hospitals rankings recognize the top 50 pediatric facilities nationwide in 11 specialties. U.S. News partners with RTI International, a North Carolinabased research and consulting firm, to collect and analyze data from children’s hospitals and pediatric specialists across the country. Methodology factors in clinical outcomes, compliance with established best practices and level and quality of hospital resources directly related to patient care.
The 19th annual Best Children’s Hospitals rankings recognize the top 50 pediatric facilities nationwide in 11 specialties. U.S. News partners with RTI International, a North Carolinabased research and consulting firm, to collect and analyze data from children’s hospitals and pediatric specialists across the country. Methodology factors in clinical outcomes, compliance with established best practices and level and quality of hospital resources directly related to patient care.

The annual Best Children’s Hospitals rankings are designed to assist patient families and their providers in making informed decisions about where to receive care while recognizing hospitals that excel in specialized treatment.
The annual Best Children’s Hospitals rankings are designed to assist patient families and their providers in making informed decisions about where to receive care while recognizing hospitals that excel in specialized treatment.
The annual Best Children’s Hospitals rankings are designed to assist patient families and their providers in making informed decisions about where to receive care while recognizing hospitals that excel in specialized treatment.
Leading Pediatric Nephrology Care
Leading Pediatric Nephrology Care
Leading Pediatric Nephrology Care
Children’s offers the region’s only advanced pediatric program for children with kidney conditions. Our board-certified pediatric nephrologists have advanced training in managing both mild and severe kidney diseases. Led by division chief Melissa Muff-Luett, MD, Children’s treats all forms of kidney disease and houses the state’s only pediatric dialysis center, providing services and technologies specifically designed for children. Our compassionate team collaborates with providers across specialties to create personalized care plans and partners with patient families to guide lifestyle changes, helping children grow and thrive at every stage of care.
Children’s offers the region’s only advanced pediatric program for children with kidney conditions. Our board-certified pediatric nephrologists have advanced training in managing both mild and severe kidney diseases. Led by division chief Melissa Muff-Luett, MD, Children’s treats all forms of kidney disease and houses the state’s only pediatric dialysis center, providing services and technologies specifically designed for children. Our compassionate team collaborates with providers across specialties to create personalized care plans and partners with patient families to guide lifestyle changes, helping children grow and thrive at every stage of care.
Children’s offers the region’s only advanced pediatric program for children with kidney conditions. Our board-certified pediatric nephrologists have advanced training in managing both mild and severe kidney diseases. Led by division chief Melissa Muff-Luett, MD, Children’s treats all forms of kidney disease and houses the state’s only pediatric dialysis center, providing services and technologies specifically designed for children. Our compassionate team collaborates with providers across specialties to create personalized care plans and partners with patient families to guide lifestyle changes, helping children grow and thrive at every stage of care.
Exceptional Care in Pediatric Neurosciences
Exceptional Care in Pediatric Neurosciences
Exceptional Care in Pediatric Neurosciences
Children’s Neurosciences brings together experts in pediatric neurology and neurosurgery to provide the highest-quality care to children with conditions of the brain, spinal cord, nerves or muscles. Our team uses advanced diagnostic tools for precise evaluations and the latest minimally invasive surgical techniques so patients can heal faster. Children’s
Children’s Neurosciences brings together experts in pediatric neurology and neurosurgery to provide the highest-quality care to children with conditions of the brain, spinal cord, nerves or muscles. Our team uses advanced diagnostic tools for precise evaluations and the latest minimally invasive surgical techniques so patients can heal faster. Children’s
Children’s Neurosciences brings together experts in pediatric neurology and neurosurgery to provide the highest-quality care to children with conditions of the brain, spinal cord, nerves or muscles. Our team uses advanced diagnostic tools for precise evaluations and the latest minimally invasive surgical techniques so patients can heal faster. Children’s

is designated as a Level 4 Pediatric Epilepsy Center by the National Association of Epilepsy Centers and has the only EEG lab in the state accredited by ABRET Neurodiagnostic Credentialing and Accreditation. The Pediatric Neurology program is led by division chief Sookyong Koh, MD, PhD, and the Pediatric Neurosurgery program is headed by division chief Arnett Klugh III, MD, in a unified Pediatric Neurosciences department.
is designated as a Level 4 Pediatric Epilepsy Center by the National Association of Epilepsy Centers and has the only EEG lab in the state accredited by ABRET Neurodiagnostic Credentialing and Accreditation. The Pediatric Neurology program is led by division chief Sookyong Koh, MD, PhD, and the Pediatric Neurosurgery program is headed by division chief Arnett Klugh III, MD, in a unified Pediatric Neurosciences department.
is designated as a Level 4 Pediatric Epilepsy Center by the National Association of Epilepsy Centers and has the only EEG lab in the state accredited by ABRET Neurodiagnostic Credentialing and Accreditation. The Pediatric Neurology program is led by division chief Sookyong Koh, MD, PhD, and the Pediatric Neurosurgery program is headed by division chief Arnett Klugh III, MD, in a unified Pediatric Neurosciences department.
Excellence in Pediatric Pulmonary Medicine
Excellence in Pediatric Pulmonary Medicine
Excellence in Pediatric Pulmonary Medicine
Led by division chief Casey Burg, MD, Children’s offers the region’s largest and most comprehensive multispecialty program for diagnosing, managing and treating childhood pulmonary disorders. Our specialists take a highly collaborative approach, combining expertise from Children’s Allergy, Asthma and Immunology, Pulmonology & Sleep Medicine to address breathing concerns, while also working with providers across Children’s more than 50 pediatric specialties to provide the full spectrum of care. Children’s is home to the state’s only pediatric programs accredited by the Cystic Fibrosis Foundation and the Pulmonary Hypertension Association, providing the most advanced care for children with these complex conditions. Children’s also houses the region’s only pediatric sleep lab accredited by the American Academy of Sleep Medicine, providing advanced diagnostic testing for more than 10 years.
Led by division chief Casey Burg, MD, Children’s offers the region’s largest and most comprehensive multispecialty program for diagnosing, managing and treating childhood pulmonary disorders. Our specialists take a highly collaborative approach, combining expertise from Children’s Allergy, Asthma and Immunology, Pulmonology & Sleep Medicine to address breathing concerns, while also working with providers across Children’s more than 50 pediatric specialties to provide the full spectrum of care. Children’s is home to the state’s only pediatric programs accredited by the Cystic Fibrosis Foundation and the Pulmonary Hypertension Association, providing the most advanced care for children with these complex conditions. Children’s also houses the region’s only pediatric sleep lab accredited by the American Academy of Sleep Medicine, providing advanced diagnostic testing for more than 10 years. Visit ChildrensNebraska.org/Providers or scan the QR code to learn more
Visit ChildrensNebraska.org/Providers or scan the QR code to learn more about our specialties and how to make a referral.
Led by division chief Casey Burg, MD, Children’s offers the region’s largest and most comprehensive multispecialty program for diagnosing, managing and treating childhood pulmonary disorders. Our specialists take a highly collaborative approach, combining expertise from Children’s Allergy, Asthma and Immunology, Pulmonology & Sleep Medicine to address breathing concerns, while also working with providers across Children’s more than 50 pediatric specialties to provide the full spectrum of care. Children’s is home to the state’s only pediatric programs accredited by the Cystic Fibrosis Foundation and the Pulmonary Hypertension Association, providing the most advanced care for children with these complex conditions. Children’s also houses the region’s only pediatric sleep lab accredited by the American Academy of Sleep Medicine, providing advanced diagnostic testing for more than 10 years. Visit ChildrensNebraska.org/Providers or scan the QR code to learn more about our specialties and how to make a referral.
THIS MONTH ONLINE
Exclusive Online Articles
Risk factors for cardiovascular disease negatively impact health during and after pregnancy
Driven by increases in health risk factors, cardiovascular-related complications during pregnancy are on the rise in the U.S., even among people with no previous heart disease, according to a new study in the Circulation journal.
SEE HIGHLIGHTS OF THE NEW RESEARCH ON THE WEBSITE.
How RTLS Technology is Enhancing Healthcare Safety and Efficiency
RTLS technology functions as a kind of “indoor GPS” system for healthcare facilities, enabling real-time locating of equipment, staff, and patients. But the Midmark CareFlow RTLS solution, integrated through Jeron’s nurse call systems (from DTB Systems), offers something particularly valuable: immediate safety support for healthcare workers through wearable emergency alert buttons.
FIND OUT EXACTLY HOW IT WORKS IN THIS EXCLUSIVE ONLINE ARTICLE.




Provider Partnerships to Support Deaf and Hard of Hearing Children and Their Families
American Academy of Pediatrics (AAP) Early Hearing Detection and Intervention (EHDI) Provider Education Center (PEC) is hosting a program to help providers better serve deaf and hard-of-hearing children and families.
WE HAVE LINKS TO THE VIRTUAL SESSIONS SPONSORED BY THE SOUTH DAKOTA EARLY HEARING DETECTION AND INTERVENTION (SD EHDI) PROGRAM AT THE USD SCHOOL OF HEALTH SCIENCES ON OUR WEBSITE.
Have you ever looked at a MED Magazine cover and thought, “They should do a feature on [fill in name of South Dakota area medical professional(s) doing something noteworthy.]”, we have good news!
MED is once-again accepting nominations for our Cover Features in 2026. We give preference to institutions and individuals who are innovating in some way to advance healthcare in the region. Please submit your nomination via email to Info@MidwestMedicalEdition.com. Include the name of the person or people you are nominating, how to contact them, and up to 400 words on why you think MED subscribers should know about them.
[ NOTE: MED cover articles are not paid features]
❱ Access the online version of this article to see all of the referenced studies

Institute That Saved Her Limb
W hen Haley Grudzinski was just six weeks old, her family was faced with a difficult choice. Grudzinski had been born with congenital femoral deficiency, or CFD: a condition in which the femur is underdeveloped, leaving her right leg a few inches shorter than her left.
Doctors warned that without intervention, the difference in leg length could be as much as 12 inches. With limited treatment options, the family faced the serious decision to either amputate her leg or search for a specialist willing to pursue treatment.
Grudzinski’s parents, determined to save their daughter’s limb, hunted for a viable solution and discovered Dr. Dror Paley, a renowned Canadian-trained orthopedic surgeon specializing in limb lengthening and deformity correction procedures at the Paley Orthopedic & Spine Institute…
READ THE FULL STORY ABOUT HOW THIS USD GRADUATE ENDED UP IN A CLINICAL ROTATION WITH THE DOCTOR WHO SAVED HER LEG.




ON THE ROAD WITH MED
Once again this fall, MED took its “show” on the road in support of regional healthcare news and marketing. Thanks to everyone who attended one of these events and took the time to say hello. We love meeting you in person!
✦ Iowa Healthcare Leaders Association Fall Convention in Des Moines
✦ South Dakota Association of Healthcare Organizations Annual Convention in Sioux Falls
✦ Iowa Hospital Association Annual Meeting in Des Moines
✦ North Dakota Hospital Association Annual Convention in Fargo
✦ Nebraska Hospital Association Annual Convention in La Vista
MED is always looking for sponsorship opportunities. If you know of a gathering you think we should be a part of, email us at Info@MidwestMedicalEdition.com
STAY IN THE KNOW
MED updates our digital subscribers twice every month with a curated selection of top healthcare industry headlines from around the region. Every MED newsletter features direct links to the articles you’re most interested in. PLUS, get free early access to every digital issue of MED Magazine. Sign up at MidwestMedicalEdition.com/MED-VIP











At IHA in Des Moines with Josh White of Five Nines
At SDAHO in Sioux Falls with Monument Health CEO Paulette Davidson
IHA, Des Monies
At IHLA, Des Moines

The Science of Hope
Dr. Pilar de la Puente’s Mission to Change the Outlook for Women’s Cancers

BY ALEX STRAUSS
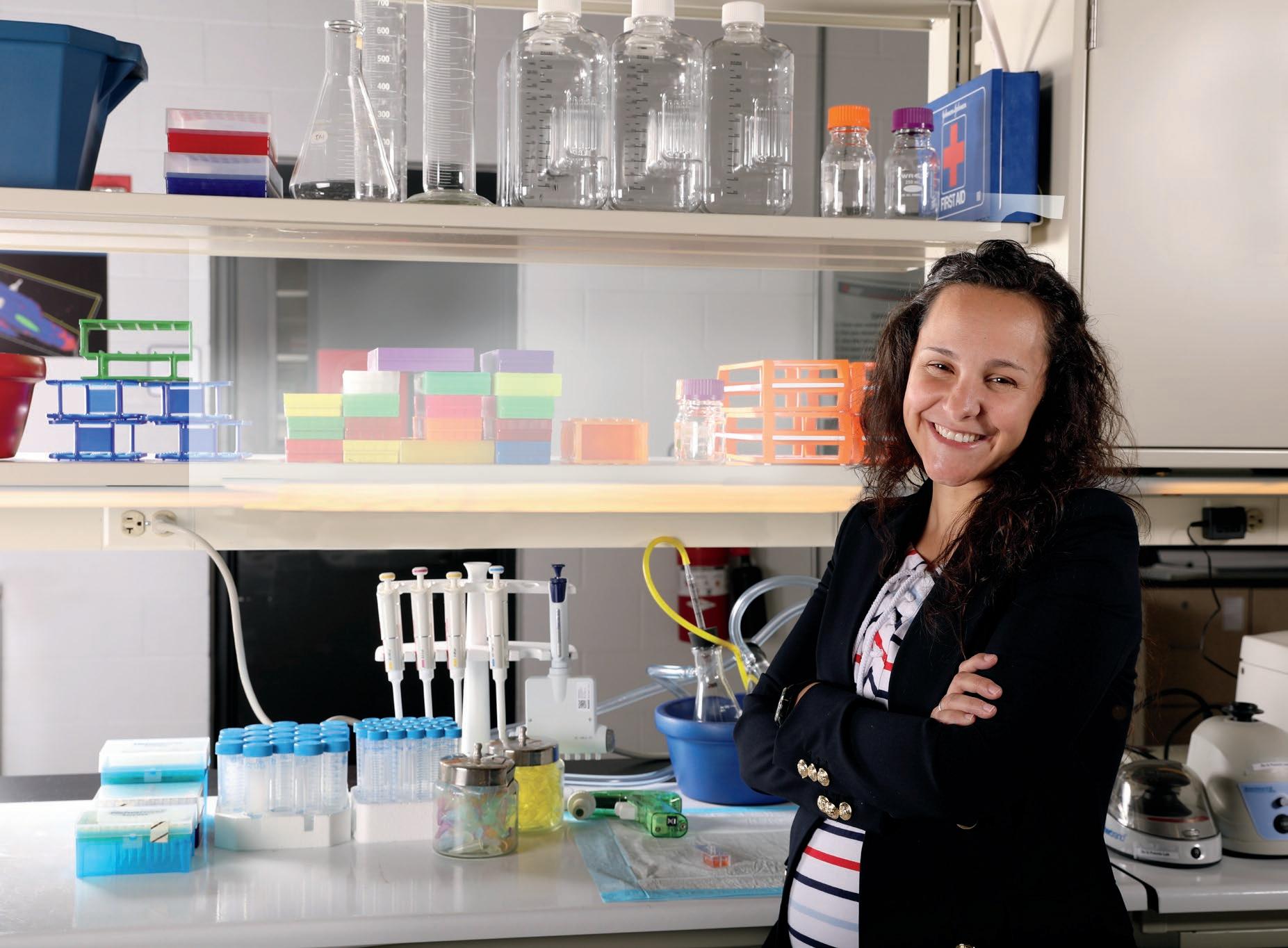
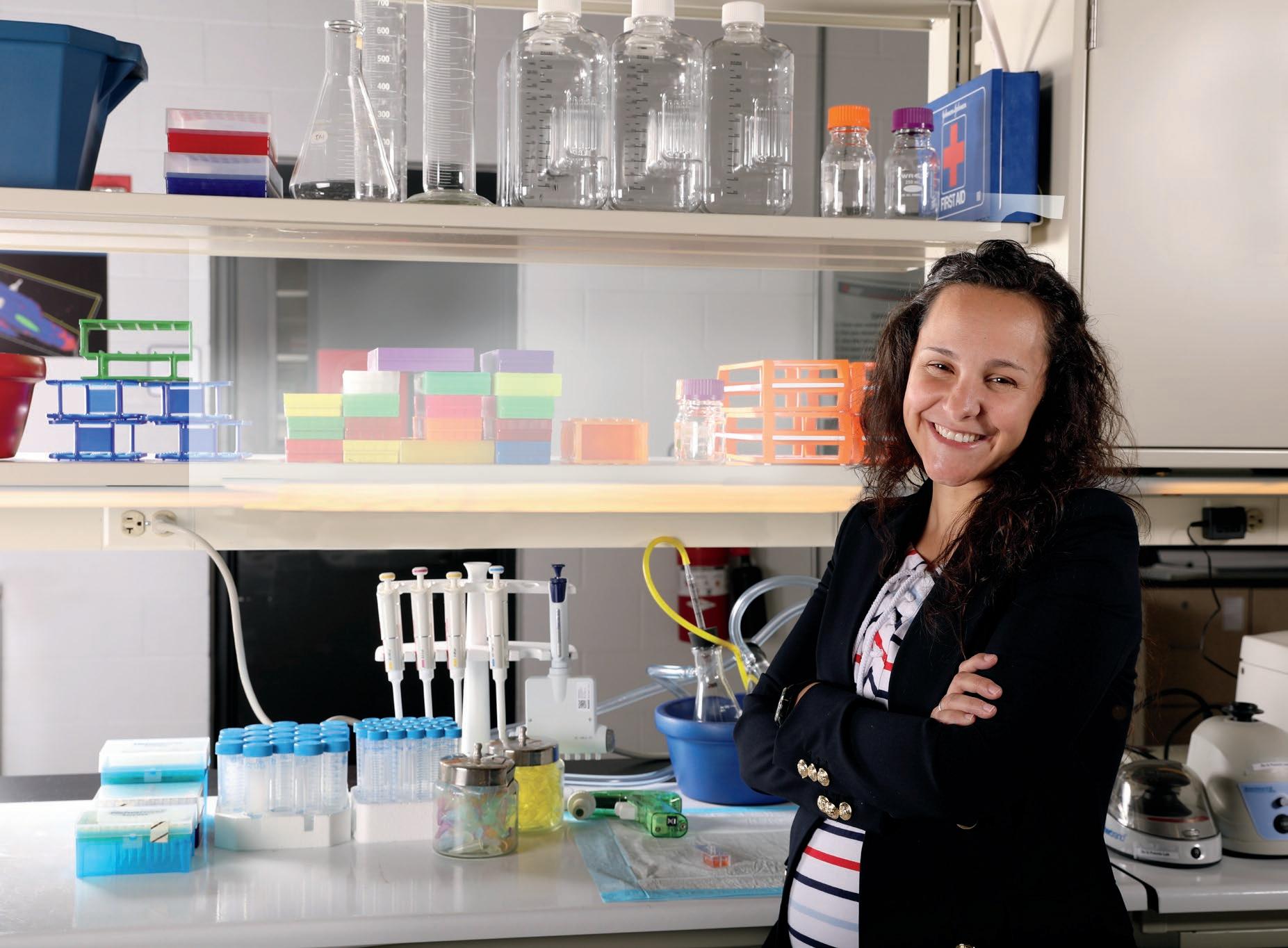
Most people dread Monday mornings. Dr. Pilar de la Puente lives for them.
“I love my job. I am the happiest person,” says the biomedical engineer and principal investigator at Sanford Research. “When it gets to Monday, I am happy to go to work. I am always excited to hear from my lab members. When we have a breakthrough, I dance.”
This infectious enthusiasm isn’t just personality—it’s fuel for one of the most promising cancer research programs in the region. Between juggling three young children and leading a lab focused on some of the most challenging questions in oncology, she brings an energy and commitment that’s reshaping how researchers understand and fight women’s cancers.
That joy has lately had good reason to express itself. This past year, Dr. de la Puente received recognition that puts her—and Sanford Research—squarely on the national map for cancer research.
Taking on Chemoresistance
The latest reason to celebrate is a 7-year MERIT (Method to Extend Research In Time) Award from the National Institutes of Health in support of the de la Puente lab’s work on ovarian cancer.
The grant will provide $2.75 million over the first five years and nearly $4 million over the entire seven. Unlike typical research grants, the R37 cannot even be applied for—researchers must be selected by the NIH, a distinction reserved for the top one to two percent of scientists in their field.
The grant represents not just financial support but validation of an approach that challenges conventional thinking about cancer treatment.
“What we have learned in the lab is that it is very important to understand not only the cancer cells and how they work but also the environment they are in,” explains de la Puente. “What they are sur rounded by is really important, especially in breast and ovarian tumors. If you think about cancer as the seed, the environment around it is like the soil. Chemotherapy affects both the seed and the soil.”
The problem is that while chemotherapy kills cancer cells, it also fundamentally alters the tumor
environment in ways that can make the cancer even more resistant when it returns. Chemotherapy is still the primary treatment for ovarian cancer, but recurrence is common. Dr. de la Puente’s lab is looking for ways to block changes in the tumor environment, allowing chemotherapy to work better and for longer.
From Spain to SD
Dr. de la Puente’s path to cancer research was not a straight one. Born and raised in León, Spain, she was drawn to biology and health, but didn’t want to treat patients.
“I love to build things,” she says. Professors suggested biomedical engineering, which would give her the opportunity to still work in healthcare but with a different “toolkit”. “That was the greatest advice,” says de la Puente.
Dr. de la Puente earned her PhD in Biomedical Engineering and Biological Sciences at the University of Salamanca, then trained as a postdoctoral fellow at Washington University in St. Louis, specializing in cancer tissue engineering, nanomedicine, and translational precision-based drug screenings. When she was first tasked with solving a cancer-related question, something clicked.
“I realized that cancer was so unique and usually doesn’t have the toolkit that biomedical engineering can provide,” she says. “It was challenging but once I got a hold of it, I loved it.”

Dr. Pilar de la Puente (center) with members of her lab at Sanford Research
A Three-Front War
The chemoresistance work represents just one piece of de la Puente’s comprehensive cancer research. Her lab tackles the disease from three additional interconnected angles, each addressing a critical gap in current cancer care.
SEARCHING FOR BIOMARKERS
Early symptoms of ovarian cancer— bloating, abdominal discomfort, fatigue—mirror common experiences for women in their 50s and 60s, making the disease notoriously difficult to catch in its early stages.
As an American Cancer Society Research Scholar, Dr. de la Puente is working to identify biomarkers that could lead to earlier diagnosis.
“If ovarian cancer is caught in Stage 1, the survival rate is 90 percent,” she says. Finding reliable biomarkers could transform those statistics, catching cancer when it’s most treatable.
TURNING
COLD TUMORS HOT
Immunotherapy has revolutionized care for some cancers, but it largely fails in breast and ovarian cancer.
Dr. de la Puente’s team is working to understand why these tumors are immunologically “cold”—meaning they lack the immune cells needed to respond to immunotherapy. By recreating these cold tumors in the lab, they can test strategies to transform them into “hot” tumors that the immune system can recognize and attack.
UNDERSTANDING METASTASIS
The third front examines one of cancer’s most deadly characteristics: its ability to spread. Using microfluidics technology, de la Puente studies how tumor cells travel through the blood. More intriguingly, her lab is investigating why certain cancer cells seem drawn to specific sites in the body.
“Is there something about the area that is attractive to these cells?,” she asks. Understanding these patterns could reveal new targets for preventing cancer’s spread.
Recognition and Impact
The accolades have been piling up. This fall, Dr. de la Puente received an International Excellence Award from her hometown of León, Spain, recognizing distinguished individuals who have brought honor to their community through outstanding contributions in their professional field. The award, given by the Economist College Association and Fundacion Monteleón, required a quick three-day trip back to Spain.
“I love the award but I love even more the chance to see my family,” she says.
But perhaps more meaningful is what these awards represent for her adopted home. Dr. de la Puente is only the third recipient of an American Cancer Society Research Scholar grant in South Dakota’s history. The NIH MERIT grant further elevates Sanford Research’s profile on the national stage.
“It has happened that I have been able to get great success here in this place that fewer people know about,” she says with a laugh. “I have to explain to my friends where South Dakota is.”
Beyond the research itself, de la Puente is deeply committed to mentoring the next generation of scientists. She serves as chair of the health equity and experience committee at Sanford Research and has taken on an advocacy role for contemporary role models in science.
When she was invited to participate in “Cancer Wars,” a comic book series featuring Hispanic women in cancer research, she jumped at the opportunity. The book has been
distributed in both Spain and the United States, and Dr. de la Puente has conducted virtual calls with schools in multiple countries to discuss it.
“The only woman anyone thinks about in science is Marie Curie,” she says. “But students need to know that there are more contemporary role models.”
Research in
Unexpected Places
There’s a certain irony to Dr. de la Puente’s success in South Dakota. While friends back in Spain may struggle to locate her state on a map, she’s discovered unexpected advantages to conducting cutting-edge research in a rural area.
“Living and working in a more rural environment gives me opportunities to study underrepresented populations,” she explains. “I can get samples from Native Americans, which is not possible in other places. It is a great location for research. We just need to be better known.”
Recent grants and awards for de la Puente’s lab and others are helping. Sanford Research is gaining a reputation in the national cancer research community. The newest grant will allow the de la Puente lab to train more new researchers locally, building capacity for the future.
“We are advancing science. That is what is most important,” she says. “This could mean better opportunities for treatment of women in the future.”
For a researcher who dances when breakthroughs happen, that future can’t come soon enough. Having lost friends and her own mother to cancer, Dr. de la Puente knows better than most the vital importance of the answers she’s seeking.
And every Monday morning, she shows up ready to find them. ❖




Best Practices in Documentation
Caring for Patients Unable to See Mental Health Specialists in a Timely Manner
BY DR. ERIC ZACHARIAS
CASE STUDY
As part of routine health maintenance screening at their PCP’s office, a patient completed a Patient Health Questionnaire, PHQ-9, a validated tool for depression screening. The PCP interpreted the PHQ-9 results to be consistent with severe depression.Over the course of the visit, the PCP completed a relatively detailed review of systems and discussion in the mental health realm and learned that, although not actively suicidal, the patient had significant suicidal ideation in the past. The rest of the ROS and exam were unrevealing.
In addition to ordering lab tests, the PDP made a referral to both a psychiatrist and a therapist. The next day, the patient called the PCP and stated the earliest that any of the five psychiatrist offices could get him in was eight weeks and the earliest a therapist could start working with him was in five weeks. The patient noted he was very frustrated with the long delay and asked if the PCP could start treatment immediately because the depression was having substantial impacts on his sleep, work performance, and relationships, and he was worried about becoming actively suicidal.
The PCP was comfortable managing mild to moderate depression without a psychiatrist’s assistance, but was concerned that major depression with a history of suicidal ideation was too risky to manage without a psychiatrist’s help and that she would be held responsible if any adverse outcome occurred prior to the patient seeing a psychiatrist.

Dr. Eric Zacharias COPIC’s Chief Medical Officer.
For a more detailed explanation of each of the points above, see the extended version of this article on our website.
ANALYSIS AND GUIDANCE
There is a nationwide shortage of mental health providers and often long delays from the time of referral to the time of available consultation. As a consequence, many PCPs and other providers are trying to help these patients that they would typically expect a psychiatrist to be managing and monitoring with medications. Simultaneously, the providers do not want to inadvertently expose themselves to allegations of negligence in the event of adverse outcomes.
Fortunately, best practices for these scenarios are relatively straightforward. As with all patient care conversations, shared decision making should be appropriately documented. This serves to reduce risk of allegations that a provider is “practicing outside of their usual scope” or “should have referred to a specialist.” Of course, no actions can guarantee against lawsuit risk, but the following ideas are helpful and important considerations:
• Care notes should be completed contemporaneously to the patient visit.
• Documentation should clearly state that your judgment was that a referral was indicated and that you made the referral.
• If an AI tool or a scribe is used for documentation of the encounter, you should read the note to ensure that it accurately reflects your awareness of the importance of the diagnosis and efforts at referral.
• Planning regular follow ups with the patient while waiting for the consultation and documenting this is helpful.
• Suicide is an impulsive act and even an experienced psychiatrist has difficulty in predicting if/or when a patient will become suicidal.
The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a printable safety plan template that includes references to the 988 system and links to helpful information for family members. Find it at samhsa.gov/sites/default/files/988-safety-plan.pdf ❖
The information provided herein does not, and is not intended to constitute legal, medical, or other professional advice; instead, this information is for general informational purposes only.

Your Patients’ Best Care
Orthopedic Institute is ready when you need a partner in care for any orthopedic injury or condition a patient may face. We prioritize collaborative relationships with our healthcare partners, all in the best interest of your patients’ long-term care and recovery.
Whether you’ve previously referred to us or not, we want to build a relationship with you, and become a trusted resource for the care your patients need — when they need it.

•
•
News & Notes
AVERA

MICHELLE NEUHARTH
Freeman Regional Health Services has appointed Michelle Neuharth as System Director of Nursing. Neuharth will oversee nursing across the hospital, nursing home, assisted living, and independent living facilities. Neuharth began her nursing career in 2010 after receiving her Associate of Arts in Nursing from Dakota Wesleyan University and has served at FRHS since 2013 in various roles including Community Health, Cardiac Rehab, Emergency Preparedness, and Hospital Director of Nursing. She received her Bachelor of Science in Nursing from South Dakota State University in 2022 and completed the SDAHO Nursing Leadership Program in 2024.

fundraising record in fiscal year 2025, raising more than $59.7 million with support from 21,038 donors, the highest amount in the foundation’s history. total includes 4,296 first-time donors. Current philanthropy projects include Tomorrow’s Promise, a $50 million campaign for women’s healthcare services, the Caring for Life fund support ing programs across the Avera footprint, and Light the Way addressing behavioral health needs. The foundation has received the High Performer distinction from the Association of Healthcare Philanthropy for six consecutive years.

Upper Midwest. The system originated when Benedictine and Presentation Sisters formed a co-sponsorship model, officially establishing Avera on September 1, 2000. The organization has grown from 127 locations in 46 communities to 315 locations in 100 communities, employing 22,600 staff members and serving one million people. Avera operates as a fully integrated continuum of care including hospitals, clinics, long-term care centers, and retirement communities.
Avera Health has been named to Forbes’ list of America’s Best-In-State Employers 2025 for South Dakota. The recognition is based on an independent survey of over 160,000 U.S. employees working for companies employing at least 500 people. More than two million employer evaluations were considered. The final score is based on personal responses from employees as well as public evaluations from friends, family members, and industry colleagues.
Avera and Yankton Medical Clinic have announced a professional services agreement effective January 1, 2026. The announcement describes the agreements as a strategic collaboration to enhance healthcare access and strengthen physician recruitment. The PSA allows YMC to remain an independent medical practice while building increased collaboration with Avera. Goals include high-quality care delivery, physician recruitment, use of the same electronic medical record, and streamlined access to outpatient hospital services. The agreement was modeled after the partnership between Avera and North Central Heart that operates the Avera Heart Hospital in Sioux Falls

MONUMENT

categories including Caring Spirit awards, Mission Awards, Safety Awards, and Excellence Awards. Winners were recognized in the areas of compassion, hospitality, stewardship, patient safety, and quality care delivery. The event has been held every other year since 2002. enhanced Medicare payments.

Avera has received $1,017,126 from the U.S. Department of Agriculture's Distance Learning and Telemedicine Program to enhance virtual patient care across 28 rural healthcare sites in South Dakota, Minnesota, Nebraska, and Iowa. The three-year Avera RURAL-UP program implements virtual nursing models that enable remote clinical staff to handle patient education, admissions, discharge protocols, and safety surveillance, allowing bedside nurses to focus on direct patient care. Kris Becker, Avera Director of Virtual Health, notes that Avera began grant-funded virtual nursing two years ago at pilot sites in Sioux Falls and Pierre.communication tools.
Monument Health has welcomed Steven Donahue as the first fellowship-trained colorectal surgeon to join the organization and the only practicing colorectal surgeon in Rapid City. Donahue completed his colorectal surgery fellowship at Creighton University in Omaha following his general surgery residency at the University of Nebraska Medical Center and earned his medical degree from the University of South Dakota in Vermillion. He joins Monument Health’s General Surgery group at Rapid City Hospital treating both simple and complex colorectal procedures. Donahue is one of more than 30 new physicians who joined Monument Health between July and October.
Monument Health Rapid City Hospital has been named a High Performing hospital for five procedures and conditions by U.S. News & World Report in its 2025-2026 Best Hospitals rankings. The hospital received recognition for abdominal aortic aneurysm repair, heart attack, pacemaker implantation, pneumonia, and prostate cancer surgery, representing the highest distinction for U.S. News’ Best Hospitals Procedures & Conditions ratings. U.S. News evaluated nearly 5,000 hospitals across 15 specialties and 20 procedures and conditions.
The Avera Sacred Heart Wound Care and Hyperbaric Treatment Center team
Tommaso Cambiaghi, MD, has joined the Monument Health Heart and Vascular Institute as a Cardiothoracic and Vascular Surgeon. Cambiaghi earned his medical degree from Università Vita-Salute San Raffaele in Milan, Italy, where he also earned a Master’s degree in Aortic Surgery. He completed his integrated residency and fellowship in Vascular Surgery at McGovern Medical School at the University of Texas, followed by a fellowship in Cardiothoracic Surgery at Houston Methodist Hospital. Cambiaghi specializes in treating aortic dissection and aneurysms, carotid, coronary and peripheral arterial disease, and heart valve pathology.
Monument Health has purchased the Northern Hills Cinema building in Spearfish and will lease the space to local businessmen Doug Markworth and Norm Fasse, ensuring continued theater operations. The property, adjacent to Spearfish Hospital campus, was acquired as part of Monument Health's long-term strategic planning. When Markworth and Fasse approached the health system about continuing operations, Monument Health recognized an opportunity to support community vitality while meeting regional healthcare expansion needs. Markworth and Fasse officially took over theater operations Monday. Monument Health will not be involved in daily cinema operations.
Monument Health’s pulmonary rehabilitation program has received certification from the American Association of Cardiovascular and Pulmonary Rehabilitation, recognizing the organiza tion’s commitment to improving quality of life for patients.
Program Certification is the only peer-review accreditation process designed to review individual programs for adherence to standards and guidelines developed by AACVPR and related professional societies. The certification is valid for three years.

SANFORD
Monument Health and Dakota Radiology have broken ground on a 12,000-square-foot expansion of their jointly operated healthcare facility at 2929 5th Street in Rapid City. Dakota Radiology and The Imaging Center will add 6,000 square feet on the first floor to house a new MRI unit and PET/CT scanner. Monument Health will use an additional 6,000 square feet on the second floor to expand clinical services. The new imaging technology will reduce patient wait times, eliminate the need for travel to larger cities for specialized diagnostics, and improve the availability of screening for high-risk breast cancer patients.
Sanford Health Foundation raised nearly $1.5 million at this year’s Children’s Gala. The funds will support South Dakota’s first dedicated pediatric emergency department which is being built next to the Sanford Emergency Department in Sioux Falls. The David H. & Christine Billion Pediatric Emergency Department will feature pediatric-specific amenities including a dedicated pediatric CT scanner and kid-friendly colors and murals. Opening in 2026, it will house the state’s only fellowship-trained pediatric emergency specialists, the region’s only pediatric ECMO life support program, and the region’s only accredited Level II pediatric trauma center.
Sanford USD Medical Center has been recognized as one of Money’s Best Hospitals for Bariatric Surgery 2025, the only hospital in South Dakota to make the list. The recognition acknowledges 75 hospitals nationwide for excellence in bariatric care based on exceptional outcomes, patient satisfaction, and safety records.
program offers various options including duodenal switch, Roux-en-Y gastric bypass, sleeve gastrectomy, revisional surgery, and lap band management. The program also provides health coaching, nutritional classes, exercise options, meal replacements, and support groups for patients.
Sanford Health has been named one of America’s Best-In-State Employers 2025 by Forbes in South Dakota, North Dakota, and Wisconsin. Forbes partnered with an independent research firm to survey more than 160,000 employees working for companies with at least 500 people. Sanford Health has 53,000 team members. Survey respondents evaluated workplaces based on criteria including wage parity, work culture, professional advancement paths, and employer action on serious issues. Participants also evaluated previous employers and organizations they knew through friends or family. In 2024, Sanford Health was also honored on Forbes ’ list of Best Employers for Veterans.
Pediatric Emergency Medicine Specialists Mason Ruthford, MD and Donald Ellis, MD, of Sanford Health
U.S. News & World Report’s Best Hospitals for 20252026 has ranked Sanford Medical Center Fargo as the number one hospital in North Dakota and Sanford USD Medical Center as the number one hospital in South Dakota for the fifth consecutive year. Sanford Bismarck Medical Center ranks number two in North Dakota and is nationally ranked in cardiology, heart and vascular surgery. Sanford USD Medical Center received high-performing rankings in gastroenterology and gastroenterology surgery as well as urology. U.S. News evaluated data on nearly 5,000 hospitals in 15 adult specialties and 21 procedures and conditions.
Sanford Health has earned gold recognition in 2025 from the American Medical Association as a Joy in Medicine organization. The program honors health systems that prioritize proven methods to reduce burnout and enhance professional fulfillment. Sanford has lowered its physician burnout rate from 50.3 percent in 2022 to 36.5 percent in 2024, below the 2023 national benchmark of 45.2 percent. This is the third time Sanford has received the recognition and the second time at the gold level.
Sanford Health has announced that Lewis Drug, a pharmacy and retail store chain with 60 locations throughout South Dakota, Iowa, and Minnesota, is joining Sanford Health in a partnership expected to be finalized this fall. The organizations have partnered for more than 25 years, including co-location of 11 Sanford Health clinics with Lewis Drug pharmacies. Lewis Drug will continue to
operate under its current brand but its 188 pharmacists and 1,300 team members will become Sanford Health employees. The leadership team will remain unchanged, with CEO Mark Griffin continuing in a multi-year advisory role.
IKUO MASUHO
Sanford Research has been awarded more than
$8 million from the National Institutes of Health to study ovarian cancer, binge eating disorders, and G proteincoupled receptor signaling. Dr. Leah Irish received $3.2 million to research the link between sleep disturbance and binge eating. Dr. Pilar de la Puente’s lab [see Cover Story] was awarded $2.75 million to study how chemotherapy triggers changes in the tumor environment that may worsen treatment resistance in ovarian
cancer. And Dr. Ikuo Masuho’s lab received $2.1 million to study G protein-coupled receptors to develop pharmacotherapies with minimal side effects and pioneer personalized treatments.
Sanford Health has expanded virtual care services to 27 Good Samaritan skilled nursing and assisted living locations in 14 South Dakota communities as part of its $350 million virtual care initiative. My Care Line virtually connects Good Samaritan caregivers with Sanford Health registered nurses and advanced practice providers during evenings, weekends, and overnights and weekdays and 24 hours on weekends. Half of participating communities have 1,000 residents or fewer, with four lacking a hospital and eight at least an hour from major medical centers.
SIOUXLAND

ROBERT RITZ
MercyOne President and CEO
Robert Ritz will retire on January 2nd, 2026. Ritz joined MercyOne in 2013 as president of Mercy Des Moines Hospital and was appointed CEO of Mercy Health Network in 2017, later rebranded MercyOne. Over the past eight years, Ritz has led MercyOne’s growth to become a comprehensive system providing more than four million patient visits annually with 22,000 employees. In 2022, Ritz led the system through full ownership transfer to Trinity Health and completed acquisition of Genesis Health System, making MercyOne one of Iowa’s largest hospital systems.


HOLLY SACHAU
Certified Nurse Practitioner
Holly Sachau has joined the team at UnityPoint Clinic General Surgery and Gastroenterology alongside Ben Pottebaum and Ashley Dyhrkopp. Sachau brings over 14 years of experience in medical-surgical nursing and leadership. She says she joined UnityPoint Health because of its focus on collaboration, compassion, and community.
UnityPoint Health assumed ownership of MercyOne Siouxland Medical Center in September, including the hospital and several facilities. The new facility has been renamed UnityPoint Health - St. Luke’s - Downtown. UnityPoint Health and MercyOne team members and providers are continuing to deliver care and conduct business as usual. The transition brings MercyOne employees into the UnityPoint Health organization.
UnityPoint Health - St. Luke’s has received the American Heart Association’s Get With The Guidelines-Stroke Silver Plus Award for ensuring that stroke patients receive appropriate treatment according to nationally recognized, research-based guidelines. Get With The Guidelines is an in-hospital program for improving stroke care by promoting consistent adherence to guidelines, which can minimize long-term effects and prevent death. Program participants qualify by demonstrating commitment to quality care and educating patients to help them manage health and recovery at home.
INDEPENDENTS

KUNDANA NEELAM
Dr. Kundana Neelam has joined the staff at Huron Regional Medical Center. Dr. Neelam is an internal medicine physician. Her presence expands the availability of specifically trained adult medicine physicians in the community. Dr. Neelam recently completed her residency in internal medicine at Roger Williams Medical Center, affiliated with Boston University, in Providence, Rhode Island. She earned her medical degree in Hyderabad, India, before relocating to the United States.

OLIVIA LEPKE
Olivia Lepke, PA-C, is a new member of the General Surgery Clinic staff at Prairie Lakes Healthcare System. Lepke joins Dr. Greg Gerrish, Dr. Kristopher Johnson, and Dr. Jacob Schaeffer. She received her Master of Science in Physician Assistant Studies from the University of South Dakota in Vermillion and completed several clinical rotations in the Watertown area.

JOLYN SACKMANN
DNP Jolyn Sackmann has joined the Prairie Lakes Orthopedics team. Sackmann earned her Doctor of Nursing Practice - Family Nurse Practitioner degree from South Dakota State University in Brookings, where she also completed her Bachelor of Science in Nursing. She has been a Prairie Lakes team member since 2014, serving in the Emergency Services Department, as a House Supervisor, and since 2022 as a nursing instructor at Lake Area Technical College.

The Prairie Lakes Primary Care team has also grown recently. Dr. Alexandra Gauer and Certified Nurse Practitioners Adrienne Bak and Susan Olson are the most recent additions. Gauer joins the Family Medicine team at Prairie Lakes Brown Clinic Northridge while Bak and Olson join providers at Prairie Lakes Brown Clinic Main. Gauer earned her Doctor of Osteopathic Medicine degree from A.T. Still University - Kirksville College of Osteopathic Medicine and completed her family medicine residency at Southern Illinois University School of Medicine. Bak served as a Registered Nurse at Prairie Lakes from 2017 to 2024 before earning her nurse practitioner certification. Olson most recently worked in the emergency department at Children’s Minnesota and Avera Marshall Regional Medical Center.

BECKY KRULL
Becky Krull, a long-time laboratory technician and the Safety & Compliance Officer at The Center for Family Medicine in Sioux Falls is retiring after 48 years of service. Krull joined the Center for Family Medicine as a lab tech in 1977 and became known for her strong work ethic, attention to detail, and compassionate approach to patient care. In later years, Krull transitioned into the role of Safety & Compliance Officer, playing a vital role in ensuring the highest standards of safety and quality across the organization. The Center hosted a retirement celebration in her honor in October.

APRIL WILLMAN
Dr. April Willman of Yankton Medical Clinic has been accepted into Harvard Medical School’s Training to Teach in Medicine program. Willman is a pediatrician and Associate Dean of the Yankton Campus at the University of South Dakota Sanford School of Medicine. The competitive Harvard program is designed for doctoral-level clinician-educators who want to enhance their classroom and clinical teaching skills. Willman will continue serving as Associate Dean and practicing at YMC while she participates in the virtual program through next June.
Yankton Medical Clinic Cardiovascular Laboratory has received a three-year accreditation from the Intersocietal Accreditation Commission (IAC) in Vascular Testing. The accreditation covers Peripheral Venous Testing, Peripheral Arterial Testing, and Extracranial Cerebrovascular Testing. IAC accreditation requires facilities to undergo an intensive application process, including detailed self-evaluation and expert panel review of operational and technical components. The accreditation demonstrates the facility's commitment to quality patient care and compliance with published standards for vascular testing procedures used in early detection of cardiovascular diseases and stroke.

AMANDA SEDLACEK
Dr. Amanda Sedlacek, Internal and Palliative Care Medicine Physician at Yankton Medical Clinic, has had her manuscript “Shared Decision Making in Healthcare: Legal Considerations” accepted for publication in South Dakota Medicine, the official journal of the South Dakota State Medical Association. The manuscript was recognized as timely and significant for the physician community across South Dakota. A dedicated advocate for patient-centered care, Dr. Sedlacek is actively involved in advancing medical education and has participated on national panels and presented at multiple medical conventions.
Midwest Heart and Vascular Associates, an independent cardiovascular practice in Rapid City, has seen more than 350 patients since opening in April according to founder Bhaskar Purushottam. Purushottam is a board-certified Interventional Cardiologist and Vascular Specialist formerly with Monument Health. The new practice launched the first Outpatient Peripheral Catheterization Laboratory in Western South Dakota and neighboring regions and has outreach clinics in Chadron, Nebraska, and Gillette, Wyoming.

DALLIN CHRISTENSEN
Rapid City Medical Center has announced that Dr. Dallin Christensen is now offering Platelet-Rich Plasma injections for patients suffering from loss of smell. Dr. Christensen is the first ENT specialist in the Black Hills region to offer this advanced therapy. Loss of smell, or anosmia, affects thousands of people each year and has become more common following COVID-19 infections. PRP therapy uses a patient’s own platelets, rich in growth and healing factors, to stimulate regeneration of olfactory nerves. This treatment has been shown to improve sense of smell in more than 80 percent of patients.
Lucas Seehafer, DPT, PhD
Degree: Doctor of Physical Therapy
Current Position: Assistant Professor, Exercise Science, Health Communications at Bethany Lutheran College

When you ask Lucas Seehafer, an assistant professor at Bethany Lutheran College in Mankato, Minnesota, what he thinks about his experience at the University of South Dakota School of Health Sciences, his answer is swift and definitive:
“When I think of all the opportunities I’ve ever had in my professional career, they can all be traced back to my time at USD,” Seehafer declares. When you dig a little deeper, it’s easy to see why he is so complimentary of the school where he earned his DPT.
A multi-sport enthusiast from the small town of Winthrop, Minnesota, Seehafer studied exercise science at Bethany Lutheran College with the intent of becoming a physical therapist.
“Originally, I chose USD because I got in,” Seehafer admits. “PT school is very competitive.”
But, once on the campus, Seehafer fell in love with the “small town feel”, the wide range of big-school resources, and the highly engaged professors. It was during his time at USD that Seehafer started a sports blog, which attracted the attention and support of classmates and professors. As the blog grew, Seehafer was tapped to cover Minnesota Timberwolves games with a press pass. Before he knew it, he was writing sports articles for Forbes.
“Eventually, I got connected to a website that is about women’s basketball. That led to creating an injury database that led to my PhD project,” says Seehafer, who just completed a PhD in Kinesiology. He also holds an MA in journalism, which he earned online during the pandemic.
Seehafer even credits his career in academics to a USD faculty member who invited him into his first job as an adjunct professor at Tufts University.
“USD opened all sorts of avenues to me that I didn’t even know existed,” says Seehafer. “I honestly think if I didn’t go to USD, a lot of these opportunities never would have come up.”
This SUCCESS SPOTLIGHT brought to you by
Happenings around the region

ALEX HANNEMANN
Dr. Alex Hannemann joined Urology Specialists in September. Hannemann is from Sioux Falls and earned his Bachelor’s Degree from Augustana University before earning his Medical degree from the University of South Dakota. He completed his urologic residency training at the University of Colorado. Hannemann serves patients in Sioux Falls and provides outreach care in Huron and Dawson, Minnesota.


OTHER
KORY ZIMNEY
University of South Dakota’s Kory Zimney has received a Lucy Blair Service Award from the American Physical Therapy Association . Zimney, professor of physical therapy and associate dean of health sciences at USD, was honored at the APTA Leadership Congress in July in Washington, D.C. His career reflects sustained commitment to the physical therapy profession through multiple leadership roles including APTA-Iowa president, vice president, practice chair, and district director, as well as national roles as APTA House of Delegates representative and Scientific and Practice Affairs Committee member.
Brookings Health System’s Ambulance Director Megan Sinner, Bill Powers, White Volunteer Ambulance Service, and Sheila Monnier, SDEMSA District 1 president
Brookings Health System’s Ambulance service has received the 2024 Career EMS Service of the Year Award for South Dakota Emergency Medical Services Association District 1. White Volunteer Ambulance Service nominated Brookings Health System Ambulance for the award, which recognizes a prehospital care provider predominantly staffed by paid career staff. The team of professional paramedics and EMTs average more than 2,500 calls annually, providing advanced life support services for Brookings and surrounding communities including several nearby towns.

❱ Intrigued by something you’ve read here? Want to go deeper? Read the full versions of these and other recent news items on our website.
Dakota State University and LifeScape have launched a collaborative research project to develop protective clothing for direct care staff working with children with developmental disabilities. The initiative, funded by a $50,000 donation from the LifeScape Foundation, focuses on creating lightweight, discreet garments that protect against injuries from biting, scratching, and pinching during maladaptive behaviors. The project originated with LifeScape Occupational Therapist Arlen Klamm and has been advanced through DSU's AdapT Lab, led by Dr. Justin Blessinger. Ten prototype garments will undergo employee assessment this fall, with additional designs planned for 2026.


Prairie Lakes Healthcare System is one of the first healthcare systems in South Dakota to implement Ion, a robotic-assisted technology for minimally invasive biopsies deep within the lung, not accessible through a traditional bronchoscope. 605.882.7777 |

BEYOND THE BORDER
In addition to MED Magazine in South Dakota, MED also curates and shares medical community news with 14,500+ digital subscribers in North Dakota, Nebraska, and Iowa. We periodically print some of the most notable news items from our wider coverage area.

NORTH DAKOTA
North Dakota Physician Honored for Community Service
BISMARCK, ND —Dr. Julie Blehm, a retired Fargo physician who practiced internal medicine for more than 30 years, won the 2025 COPIC Humanitarian Award at the North Dakota Medical Association’s Annual Meeting. The award recognizes physicians for volunteer medical services and community contributions and includes a $10,000 donation to the recipient’s chosen charity.
Dr. Blehm has been a servant leader for many years and is known for her leadership roles in healthcare and community volunteerism. She has been involved with Special Olympics North Dakota for 20 years and served on the board of directors.
She is also a passionate advocate for mental health and helped establish the North Dakota Professional Health Program, which supports medical professionals with mental illness and substance use disorders. She served on its board from 2014 through 2024.
Dr. Blehm chose the North Dakota Chapter of the American Foundation for Suicide Prevention to receive the COPIC donation.

NEBRASKA
Nebraska Launches Certified Community Behavioral Health Clinics
OMAHA, NE —Governor Jim Pillen joined state health officials to recognize seven organizations as Nebraska’s first Certified Community Behavioral Health Clinics (CCBHCs), a new model designed to expand access to comprehensive behavioral health care.
The inaugural providers—CenterPointe, Community Alliance, Heartland Counseling Services, Heartland Family Services, Lutheran Family Services, South Central Behavioral Services, and The Well—completed a certification program that restructures how they deliver and bill for services.
The CCBHC model offers around-the-clock crisis support, integrated mental health and substance use treatment, specialized care for veterans, peer support, and primary care coordination. The new payment structure reduces administrative barriers and allows providers to better account for the full cost of comprehensive services.
“This new model is a true improvement for the Medicaid system in Nebraska,” said Drew Gonshorowski, Director of the Division of Medicaid and Long-Term Care.
The seven providers have worked with state agencies since April 2024 to meet federal criteria and will begin operating under the CCBHC framework in January 2026, following legislation signed by Governor Pillen in May 2023.
FROM MED ’S MULTI-STATE COVERAGE AREA
Vaccine Champions Award for Lexington Regional Health Center Family Medicine Specialists Clinic
LEXINGTON, NE —Lexington Regional Health Center’s Family Medicine Specialists Clinic has been awarded the prestigious Vaccine Champions Award for the period of July 1, 2024 through June 30, 2025, recognizing its outstanding commitment to vaccine stewardship and inventory excellence.
This award, presented by the Nebraska Immunization Program, celebrates clinics that exemplify the highest standards in vaccine management. The Family Medicine Specialists Clinic achieved zero waste and zero expired vaccine returns for both routine and seasonal vaccines during the award period—an achievement that sets the gold standard for immunization practices across the state.
“We are incredibly proud of our team for their dedication to ensuring every dose counts,” said Dr. Francisca Carlson, Chief Medical Officer.
D r. Blehm with the physician colleague who nominated her, Dr. Misty Anderson, of Valley City

IOWA
Wellmark Foundation Invests in Mobile Training for Rural Health Care Providers
DES MOINES, IA —The Wellmark Foundation has committed $5.3 million to expand the University of Iowa College of Nursing’s Simulation in Motion-Iowa (SIM-IA) program, bringing hands-on medical training directly to rural communities.
SIM-IA uses mobile simulation technology to train first responders and healthcare professionals on-site, eliminating travel barriers and costs. The investment will ensure 86 Iowa counties receive free training at least twice yearly, with one session dedicated to maternal health care.
The timing is critical. More than half of Iowa’s counties lack obstetric services, and many emergency responders have limited access to clinical education. Training scenarios cover high-risk obstetrics, trauma care, cardiac arrest, and other emergencies rural teams commonly face.
“Where you live should not determine the quality of care you receive,” said Laura Jackson, executive vice president at Wellmark. The program aims to build confidence among rural care teams, helping them respond more effectively to medical emergencies.
With one in three Iowans living in rural areas, the expansion addresses significant gaps in health care access and provider training across the state.
Expanding Cancer Care for Iowans
DES MOINES, IA—The Iowa Clinic and MercyOne have announced a partnership designed to expand access to cancer care in central Iowa.
Earlier this year, TIC welcomed three board-certified hematology oncology physicians, significantly expanding its medical oncology capabilities. These physicians started seeing patients at MercyOne Richard Deming Cancer Center in September. They will also provide inpatient consultations for MercyOne.
Additionally, The Iowa Clinic will utilize radiation oncology space, staff, and equipment at MercyOne Clive Richard Deming Cancer Center–Radiation Oncology.
❱ Interested in more news from MED ’s wider coverage area? Select your preferred regional newsletters on our website.


Monument Health welcomes
TOMMASO CAMBIAGHI, M.D.
to the Cardiothoracic and Vascular Surgery team at the Heart and Vascular Institute.

When seconds count, trust the only award winning Cardiothoracic and Vascular Surgeons in the region.



CHARAN MUNGARA, M.D.
TOMMASO CAMBIAGHI, M.D.
