


















Children’s Nebraska, the region’s pediatric health care leader, has been verified as a Level I Pediatric Trauma Center by the American College of Surgeons (ACS), making it the first and only pediatric hospital in Nebraska to earn this distinction.
Level I verification is the highest designation for a trauma care center, recognizing hospitals equipped to provide the most advanced and comprehensive treatment for critically injured children.
“This is the achievement of a moonshot for Children’s Nebraska and for our entire state. Becoming Nebraska’s only Level I Pediatric Trauma Center reflects our unwavering commitment to providing the highest level of care to children and families when every second counts,” said Patrick B. Thomas, MD, MMCi, FACS, trauma medical director. “It’s a powerful testament to our community’s trust and to pediatricians across the region who rely on us to deliver world-class trauma care close to home.”

• 24/7 access to pediatric trauma specialists, including surgeons, emergency physicians, anesthesiologists, neurosurgeons, orthopedic surgeons and critical care teams.
• Child-focused facilities and equipment, designed exclusively for pediatric patients.
• Comprehensive, coordinated care spanning emergency response, surgery, rehabilitation and recovery support.
• Leadership in education, research and injury prevention, advancing pediatric trauma science and sharing best practices statewide.
• Regional collaboration, serving as a referral and resource center for hospitals throughout the region.

This milestone reflects the tireless efforts and collaborative spirit of the entire Children’s team. From physicians, surgeons and nurses to therapists, administrative staff and support services, every individual played a crucial role in achieving this goal.
“This designation was earned through the dedication and expertise of our incredible trauma team – surgeons, nurses, respiratory therapists, emergency physicians, intensivists, interpreter services, rehabilitation specialists, social workers, child life and countless others who work tirelessly behind the scenes to ensure that every child receives coordinated, compassionate and lifesaving care,” said Dr. Thomas. “Their commitment to excellence truly made this possible.”
Children’s Nebraska continues to lead the region in advancing pediatric trauma care, ensuring that children and families have access to the most specialized, lifesaving care right here at home.

Seven providers speak candidly about administrative burden, patient trust, and the tools they need to thrive
■ By Alex Strauss
From navigating misinformation and insurance denials to addressing cost barriers and workforce shortages—here’s what’s on the minds of rural primary care providers as we close out 2025
PAGE 6 | [Sponsored] THE FUTURE IS NOW Rural Health Leaders Chart a Path Forward at Annual Summit
PAGE 14 | RECALLS AND WARNINGS
Risk Management Considerations
■ By Dr. Alan Lembitz
Essential guidance from COPIC on managing FDA recalls and manufacturer warnings, including patient notification protocols and documentation strategies that protect both providers and patients
PAGE 16 | NEWS & NOTES
Avera Foundation sets fundraising record, Sanford Health and Prairie Lakes Healthcare System combine, Monument Health welcomes advanced tendon treatment technology plus dozens more healthcare headlines from across the region
PAGE 19 | USD SCHOOL OF HEALTH SCIENCES SUCCESS SPOTLIGHT: Alex Van Voorhis
PAGE 20 | 2025 THE YEAR IN PICTURES
A visual celebration of the region’s healthcare milestones —from street medicine and clinic-based food pantries to the region’s first GI fellowship, major grants, anniversaries, groundbreakings, remodels, awards, and record-breaking fundraisers across the Upper Midwest
PAGE 22 | BEYOND THE BORDER News from MED’s Multi-State Coverage Area
ello and happy Holiday Season from all of us here at MED ! We’re so grateful for your readership and for the continued support of our digital partners and advertisers who make this publication and our bi-monthly newsletters possible. Enjoy this special year-end edition of MED and we’ll see you next month!
All the best,
—Alex & Steff





Publisher / MED MAGAZINE, LLC
Sioux Falls, South Dakota
Vice President Sales & Marketing
STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Magazine Design / ANGELA CORBO GIER
Client Relationship Manager / BARBIE MUNOZ
Digital Media Director / HYA AMURAO
CONTACT INFORMATION
STEFFANIE LISTON-HOLTROP
VP Sales & Marketing
605-366-1479
Steff@MidwestMedicalEdition.com
ALEX STRAUSS
Editor in Chief
605-759-3295
Alex@ MidwestMedicalEdition.com
WEBSITE
MidwestMedicalEdition.com
MAILING ADDRESS PO Box 90646, Sioux Falls, SD 57109








ON AN OVERCAST DAY IN Sioux Falls, some of the most influential voices from across the country came together, full of energy and optimism, to explore solutions to the most complex issues facing rural health care today at the fourth annual Summit on the Future of Rural Health Care.
“The future of rural health care depends on more than just identifying our challenges. It requires us coming together and learning from each other and building solutions together,” said Bill Gassen, Sanford Health president and CEO.
The day kicked off with a fireside chat with American Hospital Association President and CEO Rick Pollack, who spoke about the importance of
advocacy and partnership to solve challenges facing the field related to access and affordability. He also emphasized the power of telling the hospital story to strengthen trust and advance policy priorities.
“When you look at all the polling about trust, doctors, pharmacists, nurses…they have so much credibility,” Pollack said.“It’s hard to break through, which is why we have to constantly work and make sure that we tell that positive story and give people the opportunity to visit our facilities and see what we do and see the heroic work of our caregivers.”
Public policy was top of mind for many in attendance, with state and federal officials delivering remarks, including CMS Administrator Mehmet Oz, M.D., Gov. Larry Rhoden of South Dakota and Gov. Tim Walz of Minnesota.
Dr. Oz urged leaders to “find the best ideas”
for a $50 billion Rural Health Transformation Program, adding the potential for far-reaching impact.
“The lessons that we learn by improving rural care, many times are translatable to urban areas as well,” said Dr. Oz.
Other topics included the promise of AI, leadership principles, improving the patient experience and making health care more affordable. American Medical Association President Bobby Mukkamala, M.D., spoke about his recent journey after being diagnosed with a brain tumor, and how that has influenced him as a leader and physician.
“To then become a patient, I think just makes you more informed about the system,” said Dr. Mukkamala. “When I tell them about my story, in navigating the health care system…that’s an amazing experience that helps to inform decisions. So ground-level experience, but 10,000-footlevel decision making. When one intersects with the other that closely, I think it makes for better decisions.”
Shifting landscapes and questions about funding can be difficult to navigate, but leaders in states ranging from New Mexico to New Hampshire were unified and optimistic at the end of the day.
“35% of the hospitals in the country are rural hospitals, and 25% of the people receive care at those facilities. So, we’re a big part of the American ecosystem,” said Joanne Conroy, M.D., president and CEO at Dartmouth Health. “We have to be vocal at any number of levels about how we need to transform rural health care in the U.S.”
In the end, leaders moved the conversation forward, with Gassen summing up the sentiment of many of this year’s attendees in his closing remarks.
“I’m going to leave this place as I did coming in, but even a little bit more optimistic. I am very bullish about the future of rural health care,” Gassen said. “I hope that you leave here feeling energized about our collective ability to lead and to actually transform real change. Thank you again for what you do each and every day for the patients who you serve.” ❖
Telling the Hospital Story: The Power of Advocacy and Partnership
Rick Pollack, MPA, president and CEO, American Hospital Association
Bill Gassen, JD, president and CEO, Sanford Health (moderator)
From Disruption to Action: Leveraging Data and Innovation to Transform Patient Care
Nworah Ayogu, MD, MBA, partner, Thrive Capital
Emily Barey, MSN, chief nurse evangelist, Epic
Ateev Mehrota, MD, MPH, professor and chair, Brown University School of Public Health
Dave Newman, MD, chief medical officer of virtual care, Sanford Health (moderator)
Bridging Clinical Research and Patient Care through AI and Technology
Seema Verma, MPH, executive vice president and general manager, Oracle Health and Life Sciences
Alexis Kayser, healthcare editor, Newsweek (moderator)
When the Doctor Becomes the Patient: Reflections on Purpose, Leadership and the Future of Health Care
Bobby Mukkamala, MD, president, American Medical Association
Heather Spies, MD, MBA, FACOG, physician director of clinician experience and well-being, Sanford Health (moderator)
Embracing the Future: Leading Change and Advancing New Possibilities
Joanne Conroy, MD, president and CEO, Dartmouth Health
Bill Gassen, JD, president and CEO, Sanford Health
Andrea Walsh, JD, president and CEO, HealthPartners
Erik Wexler, MBA, president and CEO, Providence
Alexis Kayser, healthcare editor, Newsweek (moderator)
Thriving in a Dynamic Landscape: How Provider-Aligned Plans Drive Value and Keep Patients at the Center
Tony Hernandez, MHA, president, Presbyterian Health Plan
Dan Liljenquist, JD, chief strategy officer, Intermountain Health
Molly Smith, group vice president for public policy analysis and development, American Hospital Association
Tommy Ibrahim, MD, MBA, MHA, executive vice president and CEO, Sanford Health Plan (moderator)
Building a Culture of Innovation and Trust
Aneesh Chopra, chief strategy officer, Arcadia
Mario Schlosser, co-founder and chief technology officer, Oscar Health
John Doerr, MS, MBA, chair, Kleiner Perkins (moderator)
To listen to these discussions and more, you can view the summit in its entirety or select individual segments at https://vimeo.com/1127951127.
By Alex Strauss

At the end of each year, we invite a group of healthcare professionals in our region to share their insights on what’s working —and what could be working better—in their practices. This year, we posed two questions to seven primary care providers from across South Dakota, Southwest Minnesota, and Northwest Iowa. From the high cost of care to countering misinformation to preparing for AI, their answers provide a fascinating glimpse into life in rural primary care today.

The biggest challenge I’ve faced is navigating the increasing misinformation and misleading health information that patients encounter. Since COVID-19, there’s been growing mistrust of our medical system. Patients often arrive with conflicting information from various sources, and sorting through these misconceptions in the exam room takes considerable energy and time away from other aspects of care.
Sorting through the “noise” of companies selling a quick fix for complex medical issues or social media accounts providing baseless medical advice has become a larger part of my practice. I practice evidence-based medicine and take my oath to “do no harm” seriously, as do my colleagues. Building relationships and maintaining trust has become as essential as clinical expertise in providing effective primary care and help patients make the best decisions for themselves and their health.
MONUMENT HEALTH SPEARFISH CLINIC SPEARFISH, SD
What was the biggest challenge you faced as a primary care provider in 2025?

PRIMARY
Challenges are nothing new to providing primary care in rural areas. Being able to provide cost effective care to our patients is a daily challenge, whether it be pre-authorizing medications or diagnostic tests, accessing specialized treatments, trying to help patients understand how putting off care is more costly, or making sure that patients can follow through with recommendations with limited financial resources.
This additional financial strain on patients adds to provider workloads and takes a lot of time. I try to balance my treatment recommendations with where the patient is at, medically and financially, when they share that finances are a struggle. That is the best way I have found to treat the whole person in family medicine. Helping patients remove barriers to care where I can, is something that I take a lot of pride in.
LANDMANN JUNGMAN MEMORIAL HOSPITAL AVERA SCOTLAND, SD
| FAMILY
One of the biggest challenges I faced as a primary care provider this last year has been difficulty with insurance coverage. Whether it is a simple denial for a medication that is considered first or second line, or a denial because I am not a specialist, it is a hindrance to providing patient care.
The other great challenge of the last year has been the increasing mistrust of science and medicine and large amounts of misinformation. This frequently plays out in the exam room and makes patients fearful of evidence-based medicine which puts their health at risk despite them believing the opposite. It is possible to combat this with education and empathy, but it is often difficult to overcome that fear which makes treating patients more complicated and occasionally less successful.
In primary care, the goal is always to prevent disease before it occurs, but this is becoming more difficult as people are reluctant to trust modern science and medicine.


The biggest challenge I have faced as a primary care provider in 2025 is juggling administrative burden, insurance denials and coordination of care for patients. Our clinic serves a diverse population including patients who speak a language other than English as their primary language. This can make it difficult to evaluate health literacy and requires more follow-through to ensure patients are understanding their diagnoses, plans of care, and appropriate follow up needs.
SANFORD WORTHINGTON CLINIC, WORTHINGTON, MN

The biggest challenge that I faced over this year has been navigating ways to provide care for those who are unable or hesitant to receive care. This includes both disadvantaged groups who are fearful of costs without social safety nets, or fearful of deportations, pandemic and the constantly changing vaccination
Especially in a rural community where there are changes can have large effects. This then affects the full spectrum of people in the community who needtaged, the resources for all must be readjusted. It isn’t like we stop providing care just because someone can’t afford it — we all just suffer slightly more, together.
ability to provide these services is lessened, and the global cost on the healthcare system is increased.
The biggest challenge I faced as a primary care provider in 2025 was navigating the impact of a shrinking workforce. With primary care providers making up less than five percent of the overall healthcare workforce, the demand for services far exceeded the available supply. This shortage often meant working extended hours and managing a growing number of complex cases with limited resources. The lack of adequate funding from Medicare and Medicaid only intensified the issue, particularly in rural and low-income areas where access to care was already limited. I often witnessed how delayed or insufficient access to care contributed to worsening chronic conditions such as diabetes and heart disease. Balancing the desire to provide high-quality, patient-centered care with the reality of systemic limitations was both the most challenging and the most defining aspect of my experience as a provider in 2025.


Healthcare professionals have and will continue to face various challenges over time, but my biggest challenge this past year has been the general public’s mistrust of modern medicine. The vast wealth of information on the internet is wonderful, yet dangerous when used incorrectly. I imagine that this issue will only continue to worsen with further technological advances and the rise of AI.
One of my mottos the past few years has been that, what is natural does not always mean safe or best. It is ironic that Science built these powerful tools and also has led so many to distrust Science.
On the other hand, this is another instance that portrays the continued need for human hands in the art of medicine. As a primary care provider, one of my goals is to continue to build the relationships with my patients that will overcome the influences of “Dr. Google”.

QUESTION
TWO
What’s on your wish list of things that would make your job easier or more effective in 2026?

I could be more effective if I had less . . . paperwork and documentation requirements. ”
I’m optimistic about artificial intelligence continuing to transform primary care practice. Over the past year, AI has drastically improved my efficiency, particularly with documentation and patient notes. This technology allows me to spend more time on what truly matters—connecting with patients and addressing their health concerns. Looking ahead to 2026, I’m eager to see AI further minimize medical errors and enhance clinical efficiency. The potential for AI to support diagnostic accuracy, flag medication interactions, and streamline administrative tasks could be transformative for both patient safety and provider sustainability in primary care.
Although I’m generally pretty content with my job, there are a few things that would make it easier. Electronic Medical Records (EMR) have their benefits but I am looking forward to moving to a more user friendly EMR with AI that can be used safely and effectively to help speed up clinical documentation. That would mean less time after “normal” working hours spent on the computer, which would be great.
I would feel like a more effective provider if I could have all patients be receptive to preventative care. Preventative care is so important and seems to be undervalued by a lot of people. As a provider, I know the importance of preventative care and how much more effective I could be if we could convince everyone the importance of prevention.
The last thing on my wish list would be to have power exam tables in all the clinic rooms, so it would be easier to get patients on and off the tables, especially geriatric patients. Who knows, maybe Santa will read this and we will get a special delivery!
SCOTLAND, SD
My wish list would include a decrease in the number of prior authorizations required for treatment plans that are considered standard of care. This red tape often creates more work and spends more healthcare dollars than the treatment requested in the first place as we try ineffective approaches first despite knowing these will likely fail.
The decrease of that red tape would make clinic workflow significantly smoother and less frustrating for the entire healthcare team. We must be efficient with our time in clinic and arguing with insurance companies to provide our patients with the care they need and deserve can be quite disheartening.


As much as we despise computers sometimes, AI may eventually be a saving grace. ”

I believe having more in-clinic support such as pharmacists embedded in the clinic would be beneficial. Also, expanding our current number of in-person interpreters to deliver care more effectively to our diverse population. I could also be more effective if I had less administrative burden of paperwork and documentation requirements.
The biggest thing that I would wish for would be consistency. Regardless of what or how many resources are available, even just knowing that information would allow for more effective planning and allocation. I want to be able to care for my patients and be able to provide the same care week after week and not have to worry about whether the resources I provided last week will still be available this week. People should be able to walk into a doctor’s office and have a reasonable expectation of what will happen and what care can be provided.
My wish list includes increased funding for Medicaid and Medicare, which can profoundly affect the lives of individuals in rural and low-income communities by expanding access to preventive services and chronic disease management. When financial and logistical barriers are reduced, individuals are more likely to seek timely medical care, attend scheduled appointments, and access specialized services. These improvements not only enhance individual well-being but also contribute to broader public health goals, including the reduction of health disparities and the promotion of equitable health outcomes.
Gone are the days when a health care provider could just treat the patient. I doubt that anyone’s dream job when they chose healthcare was to spend the majority of their days facing a computer screen or fighting insurance companies, but this is the world we now endure.
My wish list of things that would improve my work largely revolve around things that would diminish administrative burden. Similarly to how we review a patient’s medication list, EHR systems should constantly be reviewed to reduce the redundancy in computer “clicks” and streamline processes.



As much as we despise computers sometimes, AI may eventually be a saving grace. As I frequently tell my patients who are caregivers, you cannot take care of someone else if you do not take care of yourself first. Hopefully we can move towards a future that reduces our time with computers and increases our time with patients and family.
BY ALAN LEMBITZ, MD
FROM TIME TO TIME , the FDA, manufacturers, and other agencies issue recalls or serious warnings about devices, drugs, instruments and other healthcare-related products. When one of these notices impacts your medical practice, it is important to follow a comprehensive process and document all the steps you have undertaken to avoid potential liability and to maintain care for patients. Facilities, physicians, advanced practice providers, pharmacists and other healthcare professionals may all become involved in such warnings and recalls. Depending upon the situation, medical providers may want to seek legal counsel to clarify their duties and responsibilities. The following are some general guidelines and key considerations:

Be aware that the manufacturers and pharmaceutical companies often put the responsibility for patient notification and counseling on the licensed healthcare providers. For example, typical language in recalls or warnings may read as follows: “[Manufacturer’s name] will not communicate with patients directly about this issue. If patients have been impacted as part of this issue, healthcare providers have the responsibility to inform patients and/or update a patient’s care pathway.”
Always start with the most recent and accurate information from the agency and/or manufacturer. In general, the warnings and recalls describe the risks, benefits, and potential actions.
Recall and warning notices frequently contain the following types of actions, and you should be aware of these specifics for a given patient and a given biologic, drug, device, or other healthcare-related product:
• The recommended treatment or action for users to minimize risks or impact of the affected product to their patients.
• Actions to be taken such as correction or removal of the device.
• Necessary monitoring or additional steps for follow up with patients.
• Any available alternatives.
Follow the manufacturer’s recommended action steps exactly, document those steps, and in the event that you cannot, document why you can’t . For individual patient encounters, your actions should also be documented in their personal medical record. In the case of patient non-compliance with your recommendations, document their informed refusal.
Use your patient lists, EHR, and other resources to try to identify all of your affected patients. This applies most importantly to when you were the prescriber, used the device, or implanted the materials into your patient. If the recall is a general over-the-counter medication or one that you did not prescribe, the extent to which you identify, notify, and counsel is likely reduced.
If you are unable to reach affected patients, try at least two attempts, and ideally use multiple modes such as phone, emails, etc. In serious recalls, it may be necessary to send a “return receipt requested” letter and keep a copy.
Some warnings and recalls may result in high volumes of patient calls, therefore, you should direct inquiries (as best as possible) to an informed respondent in your office or facility who can provide the guidance and who understands when scheduling appointments with the providers is necessary. It might be advisable for your “designated informed respondent” to have a script available. While the recalls and warnings are generally written at the provider level of

❱ If you aren’t signed up for FDA alerts, you can find the direct link on our website.
understanding, many consider sending the patients the exact verbiage from the manufacturer. Document each and every phone call with patients.
One of the most complicated issues is the financial responsibility for all the above actions. In some instances, the necessary follow-up visits, procedures, and therapy are paid by the patient or their insurer, and patients may need to make claims against the manufacturer for reimbursement. In other instances, the manufacturer will describe the process by which they will assist patients and their insurance payers to reduce costs and any financial burden from the recalls or serious warnings.
Lastly, in the event of legal action against the manufacturer or entity responsible for the harm, it is important that the facilities, licensed providers, pharmacists and other healthcare professionals follow all of the above steps to avoid being also named. In general, the legal actions are against the manufacturer and not the healthcare professionals and facilities, however, each case (individual or class action) is very fact-based. ❖
The information provided herein does not, and is not intended to constitute legal, medical, or other professional advice; instead, this information is for general informational purposes only.

Alan Lembitz, MD, is COPIC’s VP of Patient Safety and Risk Management

Avera Heart Hospital in Sioux Falls recently broke ground on a $21.5 million, 35,000-square-foot addition on the north side of the hospital facing Interstate 229. The three-story expansion will house advanced diagnostic imaging services including cardiac PET CT, SPECT scan with CZT technology, three nuclear stress rooms, and 15 echo/vascular sonography rooms. The garden level will accommodate cardiac MRI and additional CT equipment. Construction supports the hospital’s growing team of 22 cardiologists and expanding market share. Leaders plan to occupy the addition next winter.
Avera has been recognized by Becker’s Hospital Review as one of 100 hospitals offering exceptional orthopedic programs for 2025. Since 2016, Avera has built an orthopedic network of 56 physicians and 49 advanced practice providers delivering care across eight clinics and 40 outreach locations. Services include joint replacement, sports medicine, pediatric orthopedics, spine care and hand and foot surgery. The program incorporates robotic-assisted joint replacement, 3D-printed custom implants and regenerative medicine therapies.

Avera Pierre Clinic is the most recent location for a food pantry that provides emergency food supplies to patients experiencing food insecurity. Patients with clinic appointments will be screened, and those who need food will receive a three- to five-day supply along with information on other community food resources. In South Dakota, nearly 115,000 people are food insecure, representing 12.4% of the population. The pantry is funded through donations and a federal HRSA grant and was created in partnership with Avera Operations, Avera Research Institute and Feeding South Dakota.
Avera is partnering with Emily’s Hope to provide free naloxone at numerous Avera sites across South Dakota. Naloxone reverses opioid effects and can save lives during overdoses by helping individuals wake up and breathe properly. The nasal spray requires no needles and causes no harm if administered to someone not experiencing an overdose. Emily’s Hope, a Sioux Falls nonprofit, has distributed more than 22,000 doses statewide. Distribution boxes are being installed at Avera locations in Sioux Falls and Yankton

Several Avera facilities have committed to be part of Mission: Lifeline Stroke, a statewide American Heart Association initiative to strengthen stroke care across South Dakota. The program connects hospitals, emergency medical services, first responders, rehabilitation facilities and regulatory agencies into an integrated system that uses evidencebased guidelines for timely stroke treatment. The initiative addresses gaps in care delivery for both rural and urban hospitals, ensuring all stroke patients have optimal chances for survival and recovery.

Michael Pietila, MD, FCCP, FACP, a board-certified pulmonologist and critical care physician with Yankton Medical Clinic, has been honored with the Top Physician of the Year Award from Avera Home Medical Equipment for the third consecutive year. Among 1,800 physicians including 1,200 Avera physicians and 600 independent physicians, Dr. Pietila achieved the highest performance across AHME’s key quality indicators. The pulmonology team at Yankton Medical Clinic includes Linda Reese, PA-C, and two registered respiratory therapists, offering comprehensive pulmonary function testing, imaging and sleep medicine services.

Amanda Sedlacek, DO, FACOI, MSA, with Yankton Medical Clinic has earned the designation Fellow of the American Academy of Hospice and Palliative Medicine, the highest honor bestowed upon members. Dr. Sedlacek is an Internal Medicine/Palliative Care Physician serving the Southeast South Dakota and Northeast Nebraska region through telehealth and in-office visits. She will receive the designation at the Annual Assembly of Hospice and Palliative Care in San Diego on March 7, 2026. She is the second AAHPM fellow in South Dakota.


Yankton Medical Clinic recently added Ophthalmology and Optometry to its specialty services. Dr. Trevor Kindle, Ophthalmologist, and Dr. Luke Rockne, Optometrist, will begin seeing patients in the new year, offering routine eye exams, glasses and contact lens prescriptions, diagnosis and treatment of eye diseases, and advanced medical and surgical eye care including glaucoma and cataract treatment. Both physicians were raised in Yankton and are committed to providing comprehensive vision care locally, eliminating the need for patients to travel to larger cities for advanced eye care services.
Patients in the Black Hills region now have access to minimally invasive treatment for chronic tendon pain through Primary Care Sports Medicine Physician Hollan Harper, DO. Dr. Harper is using the FDA-cleared Tenex 2nd Generation technology to treat tendon conditions affecting the shoulder, hip, elbow and other areas. The outpatient procedure requires only local anesthesia and no stitches, with most patients returning to normal activities within six to twelve weeks. The treatment addresses conditions including tennis elbow, jumper’s knee, plantar fasciitis and rotator cuff issues.

Lisa Aguilar, RRT, RPFT, is the recipient of Monument Health’s 2024 PHIL Award. The PHIL Award is the only nationally recognized hospital-based recognition program honoring outstanding respiratory therapists. Aguilar has been with Monument Health since 2005. She became a Registered Respiratory Therapist in 2013 and earned her RPFT credential in 2022. She works in the outpatient setting performing pulmonary function tests and treatments while facilitating the Pulmonary Rehabilitation Program. Winners of the PHIL Award are nominated by patients, family members and other caregivers.
Monument Health came to the rescue recently to help keep the North Hills Cinema in Spearfish open after it was announced that the theater would close. The health system agreed to purchase the building and lease the space back to a pair of local businessmen who will run the theater. The property is adjacent to the Spearfish Hospital campus and was acquired as part of Monument Health’s long-term strategic planning. Monument Health will not be involved in daily cinema operations. The partnership preserves a community gathering place while supporting the health system’s expansion needs.

James Johnston, DPM, podiatrist at Sanford Aberdeen Clinic, has been named the 2025 Sanford Clinic Physician of the Year. The award, established in 2006, recognizes physicians who consistently demonstrate exceptional work promoting a positive environment. Dr. Johnston graduated from California School of Podiatric Medicine at Samuel Merritt University and completed his residency at UCSF San Francisco VA Medical Center. He is board certified in foot surgery and reconstructive rearfoot and ankle surgery by the American Board of Foot and Ankle Surgery.

two organizations have combined. The partnership includes financial investments in the Watertown community. Prairie Lakes will eventually transition to the Sanford Health name and brand while preserving and expanding health services across the communities it currently serves. Patients will continue seeing their current providers with no disruptions in care and John Allen, Prairie Lakes president and CEO, will continue leading the organization.
Stellenbosch University and Tygerberg Academic Hospital in Cape Town, South Africa, and the University of Otago, Dunedin School of Medicine in New Zealand, have joined the Sanford Children’s Genomic Medicine Consortium. The consortium comprises 12 leading domestic and international children’s hospitals, university medical centers and research universities working to transform pediatric health care through genetics and genomics. The group applies collaborative research, advocates for pediatric precision medicine in public policy and sponsors joint educational initiatives for common, rare and undiagnosed childhood conditions.

Good Samaritan president and CEO Nate Schema has been elected Vice Chair of the American Health Care Association’s Board of Governors. AHCA is the nation’s largest association representing long-term and post-acute care communities. Schema has served on the Board since 2022, most recently as Executive Liaison. He is the Board’s not-for-profit representative and chaired the association’s not-for-profit council from 2022-2025. The Board held elections for 2025/2026 terms at the Annual AHCA/NCAL Convention & Expo.
Black Hills Plastic Surgery in Rapid City is joining Sanford Health as part of the Black Hills region. The partnership is expected to be finalized by the end of the year. The practice’s team includes two board-certified physicians, one advanced practice provider, and six employees, all of whom are anticipated to join Sanford Health. The practice will stay at its current location. Black Hills Plastic Surgery is the latest independent physician group in western South Dakota to join Sanford Health. Creekside Medical Clinic joined Sanford in August and Black Hills Orthopedic and Spine Center (BHOSC), Black Hills Surgical Hospital (BHSH), Black Hills Urgent Care, and Black Hills Surgery Center of Wyoming became a part of Sanford Health last November.


TODD SCHAFFER MARTHA LECLERC Two Sanford Health leaders were featured panelists at the annual Becker’s CEO + CFO Roundtable in Chicago in early November. Todd Schaffer, MD, PharmD, MSS, FAAFP, president and CEO of Sanford Bismarck, joined a keynote panel entitled “The Next 5 Years of Healthcare: Bold Ideas and Big Risks Ahead.” Martha Leclerc, vice president of corporate contracting for Sanford Health, participated in a panel on “The Intersection of Economics and Politics: Key Issues for Today’s Healthcare Leaders.” The event brings together CEOs, CFOs and physician leaders from top hospitals nationwide.

Two University of South Dakota audiology faculty members, Lindsey Jorgensen, Ph.D., Au.D., and Jessica Messersmith, Ph.D., have been named Distinguished Fellows of the American Academy of Audiology. Jorgensen is chair and professor in the Department of Communication Sciences & Disorders. Messersmith serves as interim dean of the School of Health Sciences and professor in the department. This inaugural recognition honors audiologists whose work has advanced the profession, reflecting the leadership and vision of AAA founder James Jerger, Ph.D.
The University of South Dakota Department of Dental Hygiene received a state-of-the-art PerioView endoscope through funding from the Delta Dental of South Dakota Foundation and PerioView.
The specialized dental camera allows visualization inside periodontal pockets to diagnose and treat gum disease. Students will gain hands-on experience using ultrasonic instruments in challenging areas including root concavities, furcations and deep pockets. The tool will be integrated into Periodontology I and II courses, helping students more accurately classify and treat gum disease for improved patient care.
Alex Van Voorhis, MSW, CSW Degree: Master of Social Work
Current Position:
Program Supervisor, Center for the Prevention of Child Maltreatment, University of South Dakota

As an undergrad at UND Fargo, Alex Van Voorhis studied music and communications. But, after a half dozen years in sales and marketing, she realized it wasn’t her calling.
“So I started exploring,” she says. “I had always had an interest in working with victims of violence, but I knew I didn’t necessarily want to be a mental health therapist and go down the clinical route.”
Her exploration led her to social work and to Sioux Falls. “I saw that there were so many opportunities within social work to help people through prevention, training and education, grantbased work, policy development, etc.” she says.
When she decided to pursue her master’s degree, the USD School of Health Sciences Master of Social Work program, with its high student pass rate on the state licensing exam and its flexible learning options, stood out.
“I liked that the faculty was here in Sioux Falls but they also had the online degree options,” says Van Voorhis. “So I could still work and attend classes online.”
But the most impactful part of her experience at USD was her internship in the Center for the Prevention of Child Maltreatment, where she is now a program supervisor.
“I just knew, based on the type of work that they did and the team that was here, that this is where I wanted to end up,” she says.
Today, Van Voorhis supervises the delivery of training for prospective foster care parents. The integration between USD’s social work department and the Center for the Prevention of Child Maltreatment made the transition from student to professional seamless.
“Lucky for me, they had a job open when I graduated,” she says. “It was a natural progression to come and take a role here.”
❱ Intrigued by something you’ve read here? Want to go deeper? Read the full versions of these and other recent news items on our website.
This SUCCESS SPOTLIGHT brought to you by







for Digestive Health and launches the Dakotas’ first GI fellowship.
Pictured: Dr. Jeffrey Murray and Dr. Jorge Gilbert
2. USD USD lands nearly $10 million in federal grants to expand telehealth training, launch a biomedical computation collaborative, and combat substance use disorder.
12. DERBY Monument Health Foundation’s inaugural “A Night at the Derby” raises $136,000 for Northern Hills healthcare initiative. 7 3 6 9 10 1 4 8 5 2
3. MERCYONE
The Siouxland Chamber of Commerce celebrates the MercyOne Siouxland Wound Clinic’s expansion
Sioux Falls once again unites for women’s heart health at annual Go Red Event.
Pictured: MED ’s Steffanie Holtrop with stroke coordinator Lucinda Nelson, RN, and Dr Caitlin Hof of Avera Medical Group Neurology
5. PRAIRIE LAKES
Prairie Lakes Healthcare System opens Watertown’s first Baby Café, providing weekly breastfeeding support in the Maternal Child Health family lounge.


6. STREET MEDICINE
Midwest Street Medicine is redefining healthcare access for Sioux Falls’ most vulnerable residents.
Pictured: Shannon Emry, MD
7. MONUMENT
Monument Health’s hip specialists bring university-level surgical expertise to the region.
Pictured: Kenneth Milligan, MD, and Eric Krohn, DO
UnityPoint Health-St. Luke’s completes renovation of its Emergency Department
9. SPENCER Northwest Iowa Bone, Joint and Sports Surgeons, in collaboration with Spencer Hospital, complete their 1,500th knee and hip replacement surgery with the Mako Robotic Arm.
10. JUNE E. NYLEN
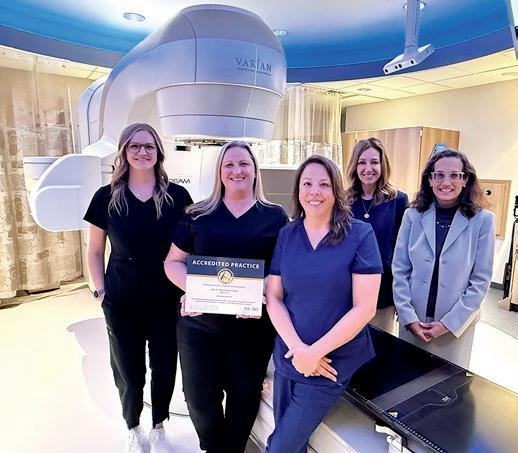
The June E. Nylen Cancer Center becomes the first cancer center in Iowa or Nebraska to receive the APEx accreditation from

Radiation Oncologist Lisa Chaiken, MD, (far right) and JENCC staff.
11. LIFESCAPE
LifeScape opens its fifth adult residential duplex in eastern Sioux Falls.






13. AVERA Avera Health tackles food insecurity at the point of care with its first in-clinic food pantries in Sioux Falls and Parkston.
Pictured: Volunteers Bobbie Ramm and Al Arndt, social worker Laura Nostvik and Avera PR specialist Lydia Slattery.

The Ty Eschenbaum Foundation makes a surprise $100,000 donation to Make-A-Wish South Dakota and Montana on World Wish Day in April. 18 16 19 13 15 17 20
14. RACE The 37th annual Avera Race Against Cancer attracts a record=breaking 7,747 participants and raises a record $765,000 to benefit local cancer patients.

15. MED SCHOOL
The USD Sanford School of Medicine announces that it will move the first 18 months of its Doctor of Medicine program to Sioux Falls in 2027.
Pictured: Dr. Tim Ridgway, dean of the USD Sanford School of Medicine.
16. TEDDY BEARS
Spencer hospital welcomes more than 350 first graders for a Teddy Bear Clinic and hospital tour in March.




17. BROOKINGS
Four nurses at Brookings Health System become the recipients of the hospital’s first DAISY Awards.
18. ANNIVERSARY
Avera celebrates its 25th anniversary as a health system in 2025, marking over 125 years of healthcare services in the Upper Midwest.
Pictured: Signage reveal at Avera Queen of Peace in Mitchell, South Dakota.
19. SANFORD RESEARCH
Sanford Research has been awarded more than $8 million from the NIH to study ovarian cancer, binge eating disorders, and G protein-coupled receptor signaling.
Pictured: Sanford Researcher Pilar de la Puente, PhD 14
20. DONATION
In addition to MED Magazine in South Dakota, MED also curates and shares medical community news with 14,000+ digital subscribers in North Dakota, Nebraska, and Iowa. We periodically print some of the most notable news items from our wider coverage area.

■ Sanford Health Fargo is officially opening its new inpatient oncology unit.
The 6S inpatient oncology unit, located within the Sanford Broadway Medical Center, features 16 private inpatient rooms designated to enhance patient care, comfort and efficiency. The new unit gives Sanford Fargo the capacity needed to care for more solid tumor patients and continue meeting the growing demand for services.
“We are excited to officially open our 6S inpatient oncology unit. Since 2020, patient referrals to radiation and medical oncology have increased by 54%. This unit will allow us to better accommodate the needs of our growing services,” said Susan Jarvis, Sanford Fargo chief operating officer. “This new unit signifies another incredible milestone in our journey toward transforming the Sanford Broadway campus into a modern facility designed to meet the unique needs of our patient population.”
With 6S opening, Sanford Fargo turns toward its next project on 7S, renovating the remaining 12 beds on
the unit to create new, modern patient rooms that can accommodate blood and bone marrow transplant patients. When that renovation is finished in the spring, there will be 40 inpatient oncology beds in total.
The Sanford Roger Maris Cancer Center was recently named to Becker’s Hospital Review’s “Top 100 Hospitals and Health Systems with Great Oncology Programs” for a third consecutive year.
■ The Gastrointestinal department at Iowa Specialty Hospital in both Clarion and Belmond is making GI screening and testing easier and more accurate with two new technologies: the Medtronic GI Genius and the Medtronic PillCam Genius SB.
The new GI Genius technology uses AI to highlight areas in real time that might need a second look, helping doctors locate hard-to-find small or flat polyps that could develop into cancer. While the technology does not replace the experience of a skilled gastroenterologist, research shows it can increase detection by 14%.
Iowa Specialty is one of the first hospitals in Iowa to also offer the Medtronic PillCam. The capsule takes thousands of pictures of the small bowel while traveling through the digestive system and the recording device is so comfortable and convenient that patients can complete the testing while going about a normal day.
“You don’t have to travel to a big hospital to get advanced care,” says Caitlin Larson, GI Leader at Iowa Specialty Hospitals & Clinics. “We are proud to offer it here, close to home, with the personal touch our patients expect and love.”

■ Great Plains Health has been honored with the prestigious 2025 Quest for Excellence Award from the Nebraska Hospital Association (NHA), recognizing the hospital’s outstanding achievements in patient care quality.
A key component of the hospital’s success was implementing a multidisciplinary team approach that includes quality officers, case management, dieticians, coding specialists, care coordination staff, nursing, providers, and IT support. The collaborative effort enabled early identification and intervention for patients at highest risk and helped the hospital achieve a mortality rate of 0.46, well below the national benchmark of 1.
The Quest for Excellence Award is presented annually to one Critical Access Hospital and one Non-Critical Access Hospital. ❖

Behind every one of our 30 + medical specialties, like labor and delivery, primary care, general surgery, and cardiology offered at Prairie Lakes Healthcare System, are over 800 dedicated medical and support professionals committed to ensuring you receive the best care for every stage of your life. 605.882.7000 | prairielakes.com
Pediatrician Rick Kooima, MD A Make-A-Wish Chapter Medical Advisor Avera Medical Group Family Health Center – Dawley Farm 27 years of practice in Sioux Falls
Why do you refer qualifying patients to Make-A-Wish?
A wish granted by Make-A-Wish provides a child with a chronic medical condition the opportunity to focus on something besides their illness. It provides hope and joy during a difficult time for patients and their families. With the entire family involved in the wish, it can frequently draw families closer together during difficult times. The opportunity to participate in a wish often gives kids new energy and strength to fight their illness.”

What would you say to other providers considering referring a child to Make-A-Wish?

When a provider refers a child to Make-A-Wish, they are able to see the joy that comes from the wish. Studies have shown that a wish granted can renew a patient’s hope and help to more effectively fight their illness.”



WHO IS ELIGIBLE TO RECEIVE A WISH?
A child between 2.5 and 18 | Has not received a wish from another wish-granting organization | Has been diagnosed with a progressive, degenerative, or malignant condition that is life-threatening























