


















ByAmyLitterini,PT,DPT
Many of us living in Maine know Lee Goldberg as the co-anchor of the Morning Report on News Center Maine on WCSH 6. He’s a successful journalist, husband, father of eight, lifelong Mainer, realtor, New England sports fan, and loves to grill for his family year-round at “Goldie’s Grill.” But if you ask Lee, as a prostate cancer survivor he also wants to be known for his advocacy for prostate specific antigen (PSA) testing for people at risk for prostate cancer, and about the non-profit organization he co-founded, Prostate Cancer Maine.
In 2024, the American Cancer Society estimates that 299,010 new prostate cancer cases will be diagnosed, and 35,250 deaths will occur. Prostate cancer is the most commonly diagnosed cancer in men nationally, as well as here in Maine. Prostate cancer is the second leading cause of cancer death in the US following lung cancer; but thanks to early detection and advances in treatment, there are 3.3 million prostate cancer survivors alive in the US today.
Since being diagnosed at age 52 in March of 2021, Lee has been on a mission to get the word out about PSA testing, which he credits with saving his life. He thanks his PCP, Dr. Timothy Baum of Intermed, for ordering a PSA unbeknownst to Lee, which was done on an existing vial of his blood being used for other routine lab testing. Much to their surprise, the discovery of his elevated PSA was completely unexpected, and it changed his life. The average age for the diagnosis of prostate cancer is 67, and Lee had no symptoms or family Left: Lee discussing Prostate Cancer Maine on WCSH6

Continuedfrom previous history to indicate he was at higher-than-average risk for developing prostate cancer at his young age. Having not taken a sick day from work in 32 years, his diagnosis came as a shock.
Prostate cancer screening, which includes checking PSA levels in the blood, and often digital rectal exam (DRE) of the prostate, is to be an informed, shared decision made between individuals and their health care providers. An elevated PSA does not necessarily mean a person has prostate cancer, it is a piece in a puzzle that may require close monitoring with repeat PSA’s and/or additional testing such as a prostate tissue biopsy.
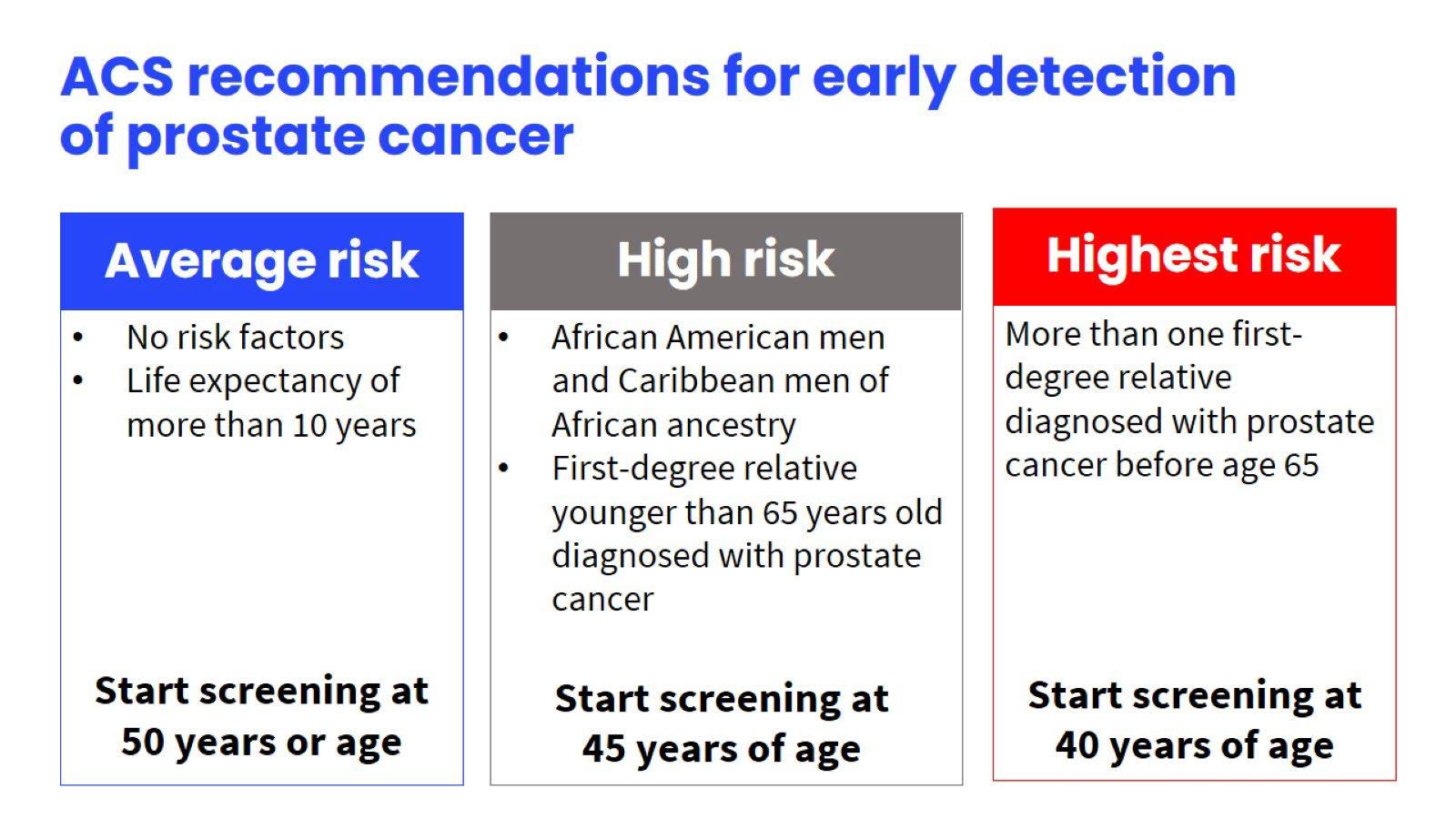
Routine PSA testing is currently not an absolute standard of care for people with prostates in the healthcare system in the United States. There is also no consensus on the recommended age at which to start prostate cancer screening. The American Cancer Society (ACS) advises individuals at average risk start screening at age 50, but for those with greater risk (i.e. family history of prostate cancer, and black ancestry) should begin as early as age 40. The American Urology Association recommends assessing baseline PSA between the ages of 45-50, with those at increased risk at age 40 (to include those with known genetic mutations). However, the most recent guidance from the US Preventative Services Task Force lists prostate screening with a level C recommendation for the strength of the available evidence, which means it should be an individual decision between the patient and their healthcare provider beginning at age 55 and ending at 69. In Lee’s case, had his PCP waited until he turned 55, his cancer would have gone unchecked for an additional three years.

What makes the screening guidelines controversial is the need to balance risks and benefits of screening. For some, there is an emotional toll associated with screening. The risk of false positive results (i.e. a result that indicates a specific condition is present when it is not), and potential complications due to prostate biopsies can also be a concern. When prostate cancer is diagnosed, there is often a perceived sense of urgency to treat it, which can ultimately lead to treatment-related side effects and overtreatment when treatment may not be necessary. For the overwhelming majority of people diagnosed with prostate cancer, their cancer will not be a threat to their life. If caught early, prostate cancer survivors have the option of observation with enhanced screening, or active surveillance (i.e. close monitoring with the plan to treat if the cancer begins to grow).
Dr Stephen Ryan was a critical care team member for Lee as he began his cancer treatment. Thankfully for Lee, since his cancer was caught early, he had treatment options and flexibility in the timing of addressing his cancer. After monitoring his PSA for approximately a year with active surveillance, a period of time which also included the timing of the birth of his eighth child Theo, Lee selected surgery. Had he taken an urgent, knee-jerk reaction to treating the cancer immediately, his son may not have been brought into the world.
Continuedfrom previous
Dr. Ryan shared: "PSA-based prostate cancer screening has prevented many men from developing advanced and incurable prostate cancer. There are downsides to PSA screening, including a possible prostate biopsy or just the anxiety associated with an elevated PSA. A good doctor can have a thoughtful discussion around these risks and I would advocate that every man older than 45 start that discussion with their doctor."
Lee also feels strongly that if your conversations and shared decisions with your primary care provider are not acceptable to you, get a new doctor. If you are eligible for prostate cancer screening, Lee says: “Don’t ask, TELL your primary care provider you want to be screened for prostate cancer.” Feeling heard and supported, as he has through his cancer journey, is critical.
Prostate Cancer Maine has a mission to bring awareness, education and services regarding prostate cancer. They plan to have awareness events coming up throughout the year, with the next event on September 30, 2024, at Dunstan Tap & Table in Scarborough. To stay connected, check out their website at www.prostatecancermaine.org for updated information.
Click below for videos of Lee’s journey:
• NEWS CENTER Maine anchor Lee Goldberg launched prostate nonprofit | newscentermaine.com
• Lee Goldberg: 'How could I possibly have cancer?' | newscentermaine.com



Sarcoma is a rare cancer that can occur in various parts of the body. It grows in connective tissue such as muscles, tendons, bones, cartilage, nerves and blood vessels. With over two million new cancer cases predicted in the US in 2024, the American Cancer Society estimates 13,590 will be diagnosed as soft tissue tumors, and 3,970 will be diagnosed in bones and joints.

To learn more about sarcoma, access the Sarcoma Foundation of America and for sarcoma awareness access the American Association for Cancer Research. To hear from a young adult sarcoma cancer survivor, click the box to the right to meet Alexis Browning.


The American Cancer Society National Cancer Information Center has trained Cancer Information Specialists available 24/7 to provide answers and support by phone at 1-800-227-2345, Live Chat or Video Chat.
The American Cancer Society’s estimates for prostate cancer in the United States for 2024 are:
• About 299,010 new cases of prostate cancer
• About 35,250 deaths from prostate cancer About Prostate Cancer | American Cancer Society


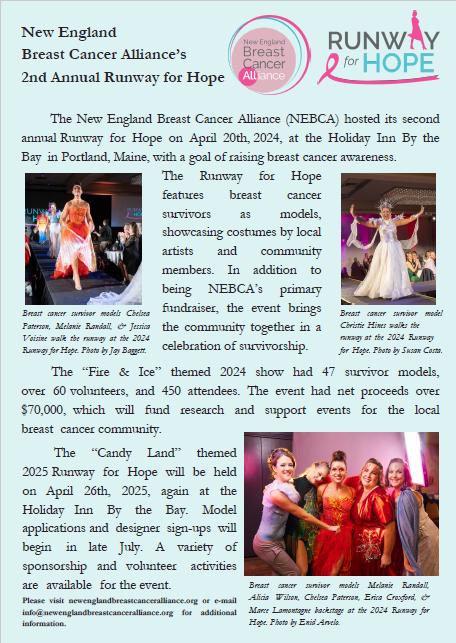
By Marisa Dolan Paraschak, Founder & President, New England Breast Cancer Alliance
By Amy Litterini, PT, DPT, Program Manger of Survivorship

Recently updated guidance from the US Preventative Services Task Force (USPSTF) has lowered the recommended age for all women to begin breast cancer screening to 40. Prior to 2024, the USPSTF previously recommended screening begin between the ages of 40-50 as an individual decision with their clinician on when to start.
The summary of the new recommendations is in the table below. The grade B refers to the available evidence as providing a moderate net benefit. The recommendations are for persons assigned female at birth. The evidence grade of I, is insufficient to recommend routine screening for women age 75 or older, or for supplemental screening (i.e. breast ultrasound or MRI) for women with dense breasts.

Other national organizations, including the American College of Radiology and the American Cancer Society, recommend starting mammograms at age 40 or 45 annually rather than biennial (i.e. every other year) per the USPSTF.
These recommendations do not apply to breast cancer survivors, or those at very high risk of breast cancer due to genetic mutations. The recommendations also do not apply to women who had high-dose radiation therapy to the chest when they were young, or to women who’ve had a lesion on previous biopsies.
Please talk to your health care provider about your individual risk factors to determine the recommended screening schedule for you.

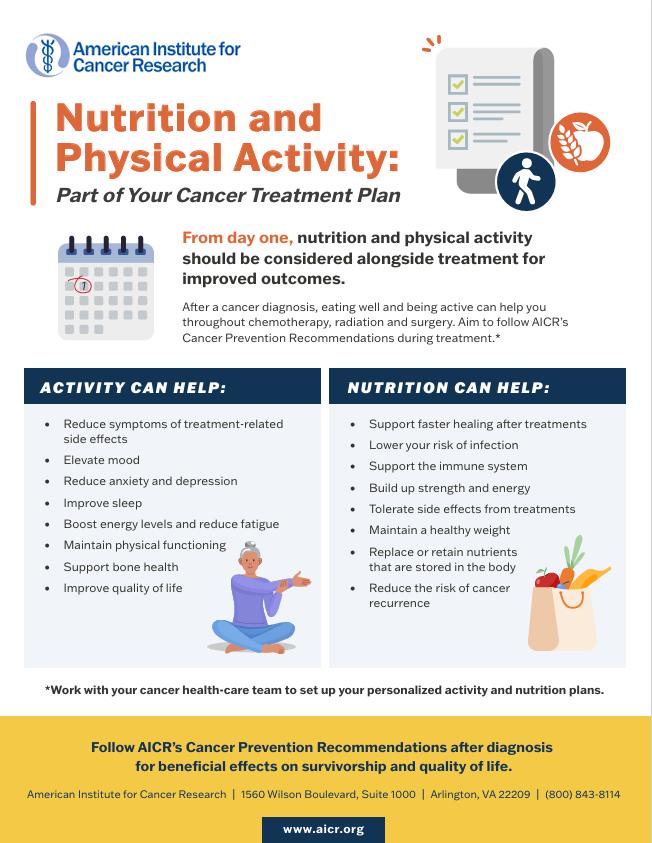
By Ashley Lazarz, R.D., L.D
Each year, billions of dollars are spent on useless and in some cases harmful nutrition advise. When it comes to cancer, it’s not uncommon for well-meaning patients, family members and friends to seek advice found online in hopes of helping themselves or a loved one. So, how does one decide what nutrition information is safe and what is too good to be true? Our best option is to have a plan for looking at information before it confronts us because all of us can be fooled some of the time. Consider these points to determine what makes sense and what does not.
1. Does the advice or product promise a quick fix?
Complicated medical problems such as cancer seldom have a quick, effortless, or simple solution. 2. Does it sound too good to be true?
Be careful when a product is advertised as a “cure” for a serious disease such as cancer. Delaying medical treatment could have serious consequences. There are no known “nutrition cures” for cancer.
3. Are recommendations based on a single study?
One study may not prove anything, but several studies in which evidence accumulates bit by bit can uncover the truth.
4. Is a product being sold as the solution to the problem? Keep in mind that the seller may be more interested in your money than your health. Sellers can be very convincing, and many of them are true believers in what they are selling.
5. Does the advice refer to studies reported in nonscientific sources?
Publications in a peer-reviewed journal are a good indication that an expert panel has reviewed the claims. Testimonials and case studies do not prove the usefulness or safety of any product.
Each Yes answer is a red flag that you could be looking at misleading information. So, how can you recognize sound nutrition information vs. a gimmick? Health care providers use scientific studies to make recommendations. You can always ask your health care provider if you are unsure about a medical treatment you read about online. When it comes to nutrition, ask your oncology dietitian. Although there are some things we do not know about nutrition and cancer, there are many things we do know. Dietitians rely on the Academy of Nutrition and Dietetics and other major cancer research centers to evaluate the latest nutrition recommendations. Here are some tips for evaluating nutrition literature.
1. How many studies have produced these results?
One study may not prove anything, but several studies can provide a base for changing health habits. 2. Did the study include a control or comparison group?
A study without a control or comparison group is unsound. Having a basis for comparison is important.
3. How long was the study and how many subjects were included in it? Continued next
Continued from previous
The fewer the number of subjects and the shorter the time, the greater the chance that the findings don’t tell the whole story. If the age and sex of the subjects are different from you, the results may not apply to you.
Uncertainty and anxiety often go hand and hand with a cancer diagnosis. Concerns about conventional treatments and their side effects cause some patients to seek alternative therapies even if the alternatives are not medically proven. A diet that promises to change the body’s pH so cancer cells can’t survive would certainly be appealing, but there is no diet that cures cancer. Conventional treatment therapies recommended by your medical oncologist, radiation oncologist and surgical oncologist will give you the best outcome when it comes to treating your cancer. Misinformation about nutrition and product scams can be harmful to cancer patients in several ways.
Here are some harmful results:
1. Failure the seek needed medical care
Early and timely diagnosis and treatment of cancer can be lifesaving.
2. Undesirable nutrient-drug interactions

For example, studies have found that anticancer drugs may be less effective in patients who took St. John’s wort while receiving anticancer drugs.
3. Failure to continue essential treatment
Deciding to take vitamin supplements in place of continuing cancer treatment. 4. Economic loss
Spending money on reported remedies and cures that do not work when money could have been spent on healthful foods.
Many reliable sources of information are available to you. These include scientific and professional associations, government agencies, nutrition departments at accredited colleges and universities and the dietitian at your cancer center. Check out the list below if want to know more about nutrition and cancer.
• American Cancer Society (ACS): www.cancer.org
• American Institute for Cancer Research (AICR): www.aicr.org
• National Cancer Institute (NCI): www.cancer.gov
• Oncology Nutrition Dietetic Practice Group: www.oncologynutrition.org
• Memorial Sloan Kettering Cancer Center, “About Herbs, Botanicals, & Other Products”: www.mskcc.org/cancercare/diagnosis-treatment/symptiom-management/integrative-medicine/herbs
• Natural Medicines: https://naturalmedicines.therapeuticresearch.com
• National Institute of Health, Office of Dietary Supplements: https://ods.od.nih.gov
• Content adapted from: https://www.ndsu.edu/agriculture/extension/publications/finding-truth-i-reliable-nutrition-andhealth-information
By Amy Litterini, PT, DPT
A recent study published in the International Journal of Epidemiology took a closer look at the benefits of resistance training, or strength training, by older adults. The study, entitled: “Weight training and risk of all-cause, cardiovascular disease and cancer mortality among older adults,” was led by researchers from both Australia and the US.

Self-reported weight training was examined in 216,339 Americans (mean age 69.9 years; 58% men, 42% women) in the years 2004 and 2005, with long-term followup to 2019. The researchers examined associations between weight training and mortality (i.e. death).
The study results demonstrated that any amount of weight training, when compared to none, was associated with lower risk of death from all-causes as well as death from cancer. Women had a larger risk reduction benefit than men, but both had reduced risk. The greatest mortality risk reduction was observed for individuals who performed both weight training and aerobic (cardiovascular) exercises.
If you’ve considered starting an exercise program, there’s no time like the present. Please discuss your medical history with one of your providers for the best way to get started. An evaluation with a rehab professional, such as a physical therapist or exercise physiologist, may help first if you have any barriers to exercise from cancer treatment, or other conditions like arthritis, heart disease, or diabetes. If you have few or no barriers but have not exercised before, or have not in a long time, seek out a certified exercise professional for a supervised program with that can be tailored to your individual needs and fitness level.

BySummerKnight,RN,GUNurse Navigator
Maine Medical Partners Urology has a relationship with the Maine Coalition to Fight Prostate Cancer. This program is run by volunteer prostate cancer survivors. They have an excellent resource called One 2 One Confidential, which is a hotline people can call to get connected with a prostate cancer survivor to

discuss their experiences. Patients or their families can call 1-855-552-7200 ext. 801 to connect with One 2 One. They have many support groups all over the state, which are very successful. They also have important information regarding prostate cancer, and several resources like transportation support, and lodging tips and assistance. The website for Maine Coalition to Fight Prostate Cancer is: https://mcfpc.org/.
For more than 25 years, ZERO Prostate Cancer has helped people and families impacted by prostate cancer. ZERO is the primary destination for all impacted by the disease to convene, get support and education, and come together as one united voice to create a better future for the prostate cancer community.



3rd Tuesday every other month
5:30 - 6:30 pm
100 Campus Drive
Scarborough,ME Conference Rooms
1&2 behind the cafe
Email: nnengland@bcan.org
Please join us for our Bladder Cancer support group. If you are a patient, survivor, caregiver, family member… all are welcome!
September 17th, 2024
November 19th, 2024
January 21st, 2025
March 18th, 2025
May 20th, 2025
July 15th, 2025
September15th, 2025
Join Zoom Meeting
https://us02web.zoom.us/j/86063821211? pwd=MDVuTThkNStsUVpHTU9PK0JCWXVpdz09 Meeting ID: 860 6382 1211 Passcode: 028474

Cancer and Careers’ Balancing Work & Cancer Webinar Series offers sessions related to the challenges of balancing work and cancer. All webinars are free to attend. The 2024 line-up includes topics critical to patients, survivors, and their care teams. Whether you’re looking for guidance on job search, help with setting boundaries or developing your communication skills, next year’s program has you covered on those and more. We hope you will join us for one, or all, of the topics!

Wednesday, July 10th, 1 PM ET/10 AM PT
Communicating Effectively: Part 1
Wednesday, August 7th, 6 PM ET/3 PM PT
Communicating Effectively: Part 2
Wednesday, September 11th, 6 PM ET/3 PM PT
Wednesday, October 9th, 6 PM ET/3 PM PT
Wednesday, November 6th, 6 PM ET/3 PM PT
Wednesday, December 4th, 1 PM ET/10 AM PT





By KatieSharp,MD,FalmouthIntegrativeMedicine
Did you know that up to 60% of foods in the grocery store contain added sugar?1 Manufactures add sugar to products to make them more palatable and extend shelf life. It is present in foods you may not think about such as yogurts, beverages, salad dressing, pickles, granola bars, cereals, soups, bread, ketchup and condiments.
Americans take in an average of more than 17 teaspoons of sugar (about 290 calories) a day from added sugars, often in sweetened beverages, far more than recommended.2 Be aware that added sugar is not an essential nutrient so there is no recommendation to have it in your diet. However, there is a recommendation from the Dietary Guidelines for Americans to limit added sugars to less than 10% of your total daily calories, for example, a 2,000 calorie diet has no more than 200 calories in added sugar or about 12 teaspoons.3 For children younger than 2 years old there is the recommendation that they should not be fed food or beverages with added sugar at all.3 The more you can limit added sugar the better as there is a link to the most common diseases in the US such as diabetes, heart disease and obesity. The goal is not to eliminate all sugars. Sugar comes naturally in carbohydrates such as fruits and vegetables which aids in prevention and management of chronic disease such as diabetes or high blood pressure.2 There are beneficial nutrients in fruits and vegetables that help blunt blood sugar spikes such as fiber, and antioxidants, essential vitamins and minerals for health.
The Most Common Added Sugars2:
sugar
Fruit juice concentrates
High-fructose corn syrup Syrup sugar molecules ending in "ose" (dextrose, fructose, glucose, lactose, maltose, sucrose).
For a quick exercise, take a look at the nutrition label on the common foods you have at home such as yogurts, ketchup, pickles or granola bars. You may be surprised at the amount and percentage of added sugar!
Resources for more information on added sugar:












1. New York Times: You’d be Surprised at How Many Foods Contain Added Sugar. https://www.nytimes.com/2016/05/22/upshot/itisnt easy to figure out which foods containsugar.html#:~:text=A%20team%20of%20researchers%20at%20the%20University%20of,in%20the%20store%2C%2068%20percent%20ha d%20added%20sugar.























2. Harvard Health: Added Sugar: Where is it hiding?. https://www.health.harvard.edu/staying healthy/added sugar where hiding 3. Centers for Disease Control and Prevention: Get the Facts: Added Sugars. https://www.cdc.gov/nutrition/data statistics/addedsugars.html

Session
Dates


FREE! Classes meet the 1st Thursday of the month from 3 to 4 pm

Aug 1 How to Create a Healthy Lunch- Learn how to create a balanced breakfast, quality and quantity lunch prep for the week, fiber
Sept 5 How to Create a Healthy Dinner- Learn how to create a balanced dinner using the Harvard plate, dinner prep for the week, quality and quantity , fiber
Oct 3 How to Create Healthy Snacks- Snacking portions and recommendations, how to read a nutrition label, creating snacks for on-the-go with quality and quantity, fiber
Nov 7
How to Create a Healthy Dessert- Take care of your “Sweet Tooth” with recipes that are low in sugar and high in fiber, learning how to replace fats and sugars in baking, fiber
Dec No Class




Courtesy of The High Protein Cookbook for Muscle Health During Cancer Treatment from researchers at the University of Alberta. Access HERE. Wilson HA, Armet AM, and Prado CM. 2022. The High Protein Cookbook for Muscle During Cancer Treatment http://openeducationalberta.ca / proteincookbookforcancer
Lauren Ciszak, a Preventive Medicine fellow at MaineHealth, has partnered with culinary medicine app: The Pursuit App, a culinary medicine platform for patients. Brought to you by Rewire Health, this evidence-based platform with personalized recipes that translate nutrition recommendations, food safety, and culinary skills into delicious and accessible meals. The mobile application is adaptable to meet individual health needs, cultural considerations, preferences, and equipment availability. This pilot is being offered free of charge to all MaineHealth programs. Please discuss any specific dietary restrictions you may have with your provider and/or a registered clinical dietitian before using.




Pursuit is an app that helps you learn valuable cooking skills to make meals that taste good, and are good for you.
Through our partnership the app is available for free to you.





Recipes include easy - to - follow video content for preparing ingredients.
Recipes are personalized just for you, allowing you to have an easier experience cooking foods that you enjoy.
Recipes can be tailored to ingredients you like or already have at home.

App Store & Google Play
(Open on a phone)





Ingredient swap - outs
Recipes can be tailored to ingredients you like or already have at home
Recipes meet you where you are, and are catered to all skill levels. You will get to practice valuable cooking skills just by making meals!

Easy to follow instructions
Choose your language
Click on an individual ingredient to learn more about it or use the get help button for help with a cooking skill The Pursuit app supports multiple languages, with more launching soon!


Search and save recipes based on meal type, cooking method, time to prepare, and ingredients



Welcomedby MaineHealth Cancer Care

MaineHealth Cancer Care would like to extend a warm welcome to medical oncologist Dr. Christopher Tretter. Dr Tretter comes to us from the Lahey Hospital and Medical Center in Burlington, MA, where he was a senior attending medical oncologist in the Department of Hematology and Oncology. There, he was responsible for the outpatient care of genitourinary malignancies, melanoma and sarcoma, and inpatient care of oncology patients. At Lahey, he also coordinated and led the multidisciplinary Genitourinary oncology programs. His research interests include investigating therapies for genitourinary malignancies and melanoma.
Dr. Tretter is board certified in both internal medicine as well as medical oncology. He graduated from McGill University in Montreal, Quebec, Canada. He completed his internship and residency in internal medicine at the Royal Victoria Hospital in Montreal, QC, and a clinical fellowship in oncology and hematology at Dartmouth Hitchcock Medical Center, Norris Cotton Cancer Center in Lebanon, NH. He has taught as an assistant professor of medicine for Tufts University School of Medicine, The Lahey Clinic, and Dartmouth Medical School. We’re delighted to have Dr. Tretter bring his impressive expertise to our care team! He is currently accepting new patients at our South Portland office on Western Ave.



Cancer Centers across the network shared fruit and baked goods with survivors in celebration of Cancer Survivors Month. Shown above are teams from MaineHealth Cancer Care at Mid Coast in Brunswick (left) and MaineHealth Cancer Care in Sanford (right). Also participating were the clinics at 100 Campus Drive in Scarborough and Western Ave in South Portland. On the Vine in Scarborough created the specially designed cupcakes to represent awareness for the different types of cancer. Thanks goes to Valerie and her bakery team!



By Amy Litterini, PT, DPT
A group of care team members came together to design and create a mural flowing across the central windows of 100 Campus Drive to illustrate the colorful ribbons representing cancer awareness for Cancer Survivors Month in June. They added inspirational words of encouragement for both survivors and the LGBTQ+ community.





By Ashley Stevenson BSN, RN, MaineHealth Manager of Oncology & Infusion, Care Management
Jillian Savage, AGNP-C, is a certified nurse practitioner who has been working in oncology since 2005, first as an oncology nurse and for the last seven years as an nurse practitioner. She has been with MaineGeneral for her career and within the last three years has assisted in developing the advanced practice provider-led satellite clinic at Franklin Memorial Hospital (FMH). Professionally, she has also led the survivorship initiative at the Harold Alfond Center for Cancer Care and looks forward to bringing a survivorship program to FMH.

Outside of work, Jillian and her husband are busy with their three children and all their activities. They love to travel and spend time with family and friends. Having grown up in central Maine, she loves the mountains and the beaches equally.
For more information on the survivorship program for patients at Franklin Memorial Hospital, please discuss with your oncology provider.
Thirteen years after he and his late wife Michele Joly joined a new volunteer council to provide feedback about care for patients at the Harold Alfond Center for Cancer Care (HACCC), Steve Helme remains firmly committed to the group.
So much so that the former Smithfield resident now travels monthly from his home in Moultonborough, NH to attend meetings of the HACCC Patient & Family Advisory Council (PFAC). “We enjoy helping to make the care for patients, their caregivers and family members the best it can be. It’s a privilege to be involved,” he said.
Unlike fellow members who are cancer survivors or receiving treatment, Helme’s perspective is that of a caregiver of a loved one with cancer. Michele, a long-time nurse and administrative director at MaineGeneral, was receiving cancer treatment when the couple were asked to join the council by now MaineGeneral Administrative Director of Oncology Services Debbie Bowden.
He has seen the PFAC evolve as its members have discussed and addressed a wide variety of patientrelated issues.
“We’ve taken on anything that’s stood in the way of really good patient care or had the potential to do that,” he said. “The cancer center employees seem to count on us to help them make some decisions, which is pretty satisfying.”
Helme is not the only member who feels passionately about being on the council. Current Chair Jenn Kelly has been on it for more than three years. She brings several perspectives to discussions at meetings: caregiver for her late parents who had cancer, former cancer patient and survivor.
“Being on the council is a pretty big deal because I’m asked to play a role that’s polar opposite of the one I had as a patient,” Kelly said. “The council is extraordinarily important because we’re the voice of patients and caretakers.”
“We’re a link to those who can make the needed changes or improvements. We could be walking into the building and hear someone talking about an issue like parking, for example. We take that to heart and discuss those things at meetings, which then are relayed to the cancer center staff to address,” she added. “I wish every cancer center had a council like ours.”
Jay McLeod, who has served for four years, is the only member actively receiving treatment at the HACCC, which he has done for nearly six years.
“At first, I wondered what I was doing on the council because I’d never served on a board before,” McLeod said, “but I soon learned they wanted personal opinions of what you see and experience at the center – pros and cons.”
“Being on the council makes you feel like you’re doing good work, and I’ve noticed that once the council approves something, it’s adopted pretty quickly,” he added. “For me, it was good to get back into a role where I felt I was contributing. I feel honored to be on the panel.”
Continued next

Continued from previous
Similar to Jenn Kelly, nine-year member Anne Latendresse brings several perspectives to the council –first as a hematology patient treated at the HACCC when it opened in 2007, then, years later, as cancer patient and now survivor. She also lost her father and brother to cancer and her sister is a fellow survivor.
“I was asked to join in 2015 to represent patients with non-cancerous blood disorders, and I’ve been on it ever since,” she said. As someone who was treated at the HACCC from 2007 to 2020, she appreciates the opportunity to help support others.
“The council is a group of good humans who volunteer to help make the process better for everybody –patients, family members and care providers,” she said. “Being on it when I was a patient made the center feel like home and removed the fear of going there for appointments. It’s exciting to see changes being made, in part, because of the perspectives we provide. It’s my way of leaving a legacy and I get choked up when I say that.”
Reflecting on both the PFAC’s origins and what it has become is a source of pride for Debbie Bowden. “I often say to the members, ‘If you don’t think your voices matter, think again,’” she said. “When I go to senior leadership for something, I let them know I brought it to the council for discussion and what their feedback was. They’ve helped me get approval for some things because their words matter in terms of supporting patient care.”
“We’ve also had council representation at our planning meetings for the cancer center expansion project and with other things like the Day of Hope and even the HACCC’s cancer committee,” she added. “As staff, we always want to hear the perspectives of patients and their caregivers. What they continue to offer is extremely important.”

By Diane Madden, MBA, Executive Director Cancer Resource Center of Western Maine
The Cancer Resource Center of Western Maine (CRCWM) held a lovely event for cancer survivors and their families at King's Hill Inn & Barn on Sunday, June 2nd. Over 70 people enjoyed wonderful music from "Just Because", food from Blue Elephant Events & Catering and wonderful mocktails from Sips ‘n Saddles! To learn more about the CRCWM, please click here.





Photocredit:Doug Kolmar










Our Care Teams represented MaineHealth in style at this year’s Pride events, showing others that MaineHealth proudly supports the LGBTQ+ community and that we truly are working together so that all our communities are the healthiest in America!



Clockwise from top L: Survivorship Program Manager Amy Litterini at Pride Portland, top center: the MaineHealth team at start of the Pride Portland parade; top R: center: Alyssa Lewis, Talent Acquisition, right: Rae Egbert, Director of LGBTQ+ Health; center R: Oncology Social Work Navigator Mikala Bousquet with daughter Logan at Pride Brunswick hosting an ACS-CAN table with information.




































Survivorship care is the process of anticipating and addressing immediate, long term, and late-stage effects from a cancer diagnosis and treatment over time. Because survivorship can have as many unique challenges as treatment, the MaineHealth Cancer Care Network (MHCCN) must expand our survivorship program.
You can give comfort to fellow cancer survivors by donating to a special fund dedicated to survivorship programming.
The MHCCN supports life beyond cancer — providing physical, emotional, and practical support for the unique needs of the growing number of cancer survivors.
We hope you will consider joining others by donating to the survivorship fund and help more people live life to the fullest.

Vol. 1, Edition 1 Jan-Mar, 2023


Vol. 1, Edition 2 Apr-June, 2023
Vol.1, Edition 3 July-Sept, 2023


Vol. 1, Edition 4 Oct- Dec, 2023
Vol. 2 Edition 1 Jan- Mar, 2024


Vol. 2 Edition 2 April- June, 2024



We would like to thank our donors and grant funders for their generous support of the MaineHealth Cancer Care Network and the patients and families we serve.




