












New laws and AI are dismantling the barriers to innovative myopia management
Despite the compelling evidence supporting modern technologies for myopia control, widespread resistance to their adoption persists. This reluctance often stems from a mix of financial concerns, limited awareness, misconceptions and practical challenges related to treatment adherence.
Among the most significant challenges is the perceived cost of innovative myopia control options. Many parents are hesitant to invest in solutions like specialty contact lenses or low-dose atropine, while practitioners often regard contact lenses as unsuitable for young children. This cautious approach can lead to a ‘wait and see’ mentality until more robust data is available, causing delays in recommending potentially beneficial interventions due to concerns about efficacy and side effects.
In this issue of COOKIE, we explore innovative strategies for myopia management, highlighting solutions that enhance patient compliance and improve outcomes.
Artificial intelligence (AI) is at the forefront of revolutionizing myopia management. It enables early detection, personalized treatment plans and continuous monitoring of patients. Advanced image analysis tools, such as OCUMETRA and the resources available at CooperVision’s mykidsvision.org and Brien Holden Vision Institute (BHVI) websites, facilitate more accurate diagnoses of myopia severity.
Furthermore, predictive analytics can assess genetic and environmental factors to forecast progression up to age 20, allowing for timely and proactive interventions tailored to individual risk profiles.
Legislative changes, such as the Malaysian Optometry Law, which broadens the scope of optometric practice, have the potential to significantly enhance myopia management. By empowering optometrists to prescribe and monitor a wider range of interventions—including specialty lenses and pharmacological treatments—care becomes more personalized and accessible. This is particularly crucial in underserved regions, where expanded optometric roles can help bridge gaps in eye care and mitigate the long-term risks associated with high myopia.
Additionally, you may want to check out the most recent International Myopia Institute publication, which has recently defined key terms such as myopia correction, myopia control and myopia management. Defining these terms is essential to avoid confusion when communicating with practitioners, researchers, regulators and patients.
As always, we hope you enjoy this issue.

Best,
Dr. Carmen Abesamis-Dichoso OD, MAT, FPCO, FIACLE, FBCLA,

Gamifying Myopia Care
To boost compliance in myopia control, eye care professionals use tech-savvy tools to connect with tech-smart young patients
Zooming In on Gen Z
Dr. Nadia Afkhami shares social media tips on raising myopia control awareness among younger patients
The Myopia Crystal Ball What AI can (and can’t) tell us about the next frontier in myopia detection and management
The Accidental Optometrist
From humble beginnings, Prof. Dr. Bariah Mohd Ali has become a pioneering force in Malaysian optometry


Ortho-K Just Got Smarter
From niche to essential, ortho-K now boasts cutting-edge materials, smarter designs and AI-powered fitting

Are These Myopia's Next Blockbusters?
Researchers are moving beyond traditional methods to explore cutting-edge drug therapies and genetic interventions for myopia control
The DNA of Nearsightedness
New research reveals how family history and specific genetic markers are key to personalized myopia management
Beyond the Blurry Lines
Adapting to ever-changing landscape and ongoing controversies in myopia management
The Bill of Sight
Malaysia’s long-awaited Optometry Bill aims to redefine eye care by elevating professional standards and expanding access





Dr. Carmen Abesamis-Dichoso
Abesamis Eye Care & Contact Lens Center, Manila, Philippines carmen.dichoso@gmail.com

Dr. Kristie Nguyen
Dr. Feenstra and Associates; Dr. Kristie Nguyen PLLC, Florida, USA kristie817@gmail.com

Dr. Monica Chaudhry Learn Beyond Vision New Delhi, India monica.rchaudhry@gmail.com

Dr. Purvi Thomson OCL Vision
London, United Kingdom Purvi@oclvision.com

Dr. Li Lian Foo
Singapore National Eye Centre (SNEC) Singapore drfoolilian@gmail.com

Dr. Maria Sampalis
Sampalis Eyecare Cranston, Rhode Island, USA msampalis@hotmail.com
Society Friends




We are looking for eye care professionals who can contribute articles to COOKIE. Interested? Let's talk! Send us an email at editor@mediamice.com.
To place an advertisement, advertorial, symposium highlight, video, email blast, or other promotion in COOKIE contact sales@mediamice.com
Matt Young CEO & Publisher
Gloria D. Gamat Chief Editor
Mapet Poso Editor
Diana Truong Associate Editor
Maricel Salvador Graphic Designer
Writers
Chow Ee-Tan Elif Uslu
Hazlin Hassan Tan Sher Lynn
Matt Herman Head of Content Strategy
Hannah Nguyen COO
Travis Plage CFO
Ruchi Ranga Society Relations & Conference Manager
International Business Development
Brandon Winkeler
Robert Anderson
Sven Mehlitz
Published by


Streamline Clinical Decisions & Conversions with OCULUS Myopia Management Solutions
The OCULUS Myopia Master® and Pentacam® AXL WAVE support myopia detection, risk assessment, progression projection, and treatment efficacy analysis. Leverage exclusive growth curves and customized reports to support patient education, conversions, and compliance. Fit and evaluate ortho-k lenses while screening corneal health and stability on the Pentacam® AXL WAVE.


boost compliance in myopia control, eye care professionals use tech-savvy tools to connect with tech-smart
by Elif Uslu
Getting kids to follow a myopia treatment plan can feel a bit like herding cats—especially when the treatment isn’t visible or urgent. But in today’s digital age, tech-savvy tools may offer the eye care community new ways to better connect with younger patients, and keep them on track.
In pediatric myopia management, consistency isn’t optional. Whether it’s low-dose atropine, orthokeratology, or specialty spectacle lenses, these therapies rely on daily compliance to be effective. That’s a tall order for kids and teens who may not fully understand the stakes.
And let’s be honest, when you’re 12 years old, putting in eye drops every night isn’t exactly top of the to-do list. Add in busy households, screentime distractions and treatments that might seem boring or “uncool,” and the barriers stack up quickly.
So, how can clinicians help kids—and their parents—stick to the plan? Increasingly, the answer lies in the same place where kids already spend much of their time: digital platforms.
Making myopia personal with games and tech
Turning complex eye conditions into something visual and relatable can make all the difference. That’s why tools like 3D animations and short, engaging videos are gaining traction in clinics and outreach programs alike.
Dr. Li Lian Foo (Singapore) sees this firsthand. “Personalized education tools like 3D animations, videos and interactive content can be very effective in helping children and teens understand their myopia and the importance of sticking to treatment,” she explained. “One approach that’s worked particularly well is community outreach events where we use large 3D models of the eyeball to demonstrate how myopia develops.
Children and parents can physically see how an elongated eyeball affects vision, and this often sparks ‘aha’ moments. Paired with visual aids and short explainer videos, it turns a passive experience into an engaging learning journey.”
Gamification is another powerful ally. By turning compliance into a challenge or reward-based activity, treatment starts to feel like something kids want to do, rather than have to do.
For instance, the MyopiaX app from Dopavision (Berlin, Germany) brings therapy into the digital playground. Used with a virtual reality (VR) headset and Bluetooth controller, this smartphone-based intervention delivers selective ocular light stimulation via immersive gaming, designed specifically to slow myopia progression in children.
VR simulations for empathy and understanding
Virtual reality isn’t just for gaming, it’s changing how we teach and treat myopia. VR tools can give children, teens and their families a first-hand look at what myopia feels like and how it worsens over time. Instead of just describing blurry vision, clinicians can now show it.
Tools like the Myopia Simulator from CooperVision (California, USA) and the MiYOSMART Simulator from HOYA (Tokyo, Japan) allow users to walk through classrooms, playgrounds and sports fields as they would appear with increasing levels of nearsightedness. This firsthand view of myopia’s impact creates a powerful emotional connection to treatment.
Dr. Foo sees promise in this approach. “The idea of using immersive visuals to demonstrate how myopia progresses could be a powerful way to improve understanding—especially for young patients and their parents. By making the invisible effects of myopia more tangible, VR could enhance awareness and potentially drive better treatment compliance.”

Mobile apps are increasingly integral to myopia control. EyeDropAlarm (Aviya LLC, California, USA), for example, helps patients stay consistent with treatment by sending timely reminders to take their prescribed eye drops—ideal for managing routines like low-dose atropine therapy.
Another example is Myopia App (VisionApp Solutions S.L.; Águilas, Spain), which helps protect children’s eyes during screen time. It alerts users when they’re holding a device too close or when screen brightness is too high—two key risk factors for visual strain and myopia progression. With features designed to encourage healthy digital habits, the app supports kids and parents alike to take small, consistent steps toward better eye health. “It is definitely an exciting space with real potential to complement clinical care,” said Dr. Foo. “As we move forward, we are interested in exploring and validating evidence-based platforms that integrate these elements while also promoting healthy screen habits and reinforcing the importance of outdoor time.”
Today’s eye clinics are becoming smarter and more engaging. Touchscreen-enabled portals let patients view their treatment progress, submit questions and manage appointments with ease. Platforms like Compulink Advantage (Compulink Healthcare Solutions; California, USA) and RevolutionEHR (Wisconsin, USA) feature interactive dashboards, progress charts and even short educational modules— designed to make care more transparent and engaging for all ages.
Some practices have added in-office kiosks where young patients can review their progress or watch a fun explainer video while waiting for their appointment. These environments make eye care feel less clinical and more approachable.
“At the Myopia Centre at Singapore National Eye Centre, we utilize digital displays in our clinic waiting areas to deliver bite-sized, childfriendly education on myopia control. These visual tools help empower families with timely and accessible information while they wait for their consultation,” shared Dr. Foo.
“In addition, our online patient portals provide access to follow-up plans and educational resources, reinforcing key messages shared during the visit and supporting better engagement and adherence. That said, there remains untapped potential in leveraging social media and other digital platforms to further engage and educate our patients beyond the clinic setting,” she noted.
Of course, not all tech is created equal—and not all families have equal access. That’s why it’s essential to use digital tools thoughtfully. While they can make a big difference in education and adherence, they shouldn’t become just another source of screen time—or create new concerns around data privacy.
more personalized, immersive and intelligent. We’re talking about smart, AI-powered platforms that tailor interventions to each child’s behavior, or augmented reality tools that turn eye care into an interactive experience right at home.
But here’s the thing, technology isn’t the magic cure. It’s a bridge, a way to meet kids—and their families— where they are. And when done right, it doesn’t just improve compliance; it transforms the entire experience of care. It helps them understand, engage and ultimately, take ownership of their eye health.
The real goal isn’t just better adherence—it’s getting them to care. And that’s a future worth seeing clearly.

Ensuring patient data is protected, limiting unnecessary screen exposure and avoiding over-reliance on technology are all part of the equation. Clinicians also need to keep in mind that not every family has access to app-based or VRenhanced tools—and socioeconomic disparities can be a real barrier. “As with any technology, the benefits must be balanced against potential risks. Excessive screen time remains a concern, especially in younger children, so it’s important that digital tools are used with clear boundaries. Privacy and data security are also critical, particularly when apps collect sensitive health information from minors,” warned Dr. Foo.
Looking ahead, the future of myopia control is poised to be
Dr. Li Lian Foo is a consultant at the Cataract and Comprehensive Ophthalmology Department, Singapore National Eye Centre (SNEC). She graduated with First Class Honors in Chemical Engineering from NUS in 2008 and earned her MD from Duke-NUS in 2012. She became a Fellow of the Royal College of Ophthalmologists in 2016 and attained a Master of Medicine in Ophthalmology and a Graduate Diploma in Family Medicine in 2017. An accomplished researcher and author, Dr. Foo has published nine peer-reviewed papers, presented at international conferences and co-authored two ophthalmology guidebooks. She received the Young Investigator Award at SGH’s Annual Scientific Meeting in 2011. Dr. Foo’s passion for innovation led her to the MIT-Harvard Medical School Healthcare Innovation Bootcamp in 2019, where her team was runner-up in the elevator pitch competition. She also completed the Eureka-Singapore Monsoon School on Translational Medicine. As SNEC’s first Myopia Fellow, Dr. Foo is dedicated to addressing the myopia epidemic through innovative solutions. With a vision to enhance clinical care, she strives to develop novel tools and treatments, bridging gaps in ophthalmology and improving patient outcomes.
drfoolilian@gmail.com


Dr. Nadia Afkhami shares social media tips on raising myopia control awareness among younger patients
by Tan Sher Lynn
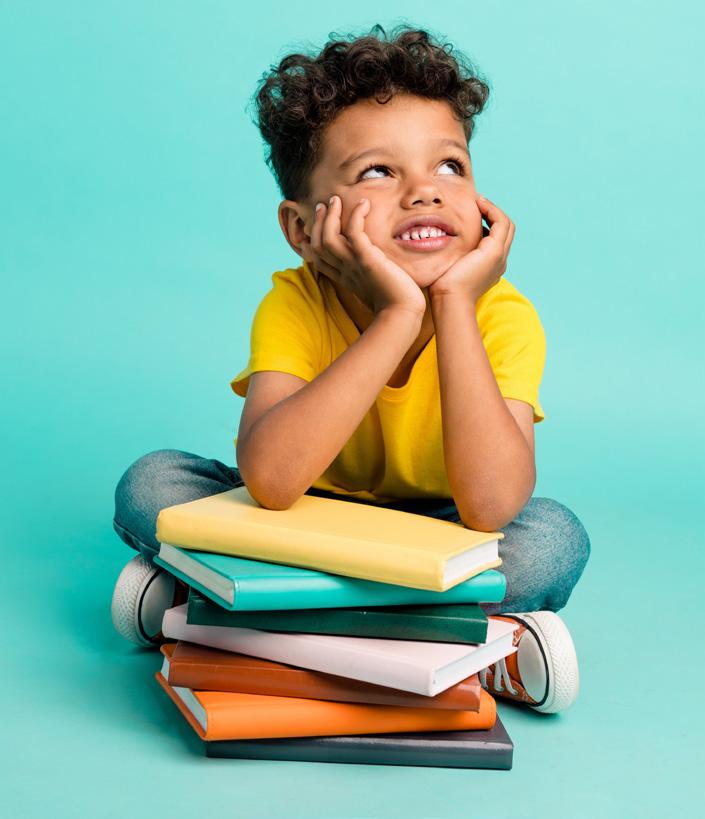
To connect with tech-savvy Gen Z and Millennials, optometrists are now leveraging a generation-specific social media strategy, proving it's as vital as advanced tech for promoting myopia awareness and control.
In today’s digital-first world, the old playbook of patient outreach— print flyers, word-of-mouth or the occasional Facebook post—no longer cuts it, especially when trying to connect with Gen Z and Millennials.
For optometric practices looking to stay relevant and trusted by younger patients, a thoughtful, generationspecific social media strategy is becoming just as vital as the latest diagnostic technology, especially when it comes to promoting myopia awareness and control.
Dr. Nadia Afkhami, an IranianAmerican optometrist with a passion for modern patient engagement— and an Instagram following of 24.4K—knows this better than most. From styling frames on Instagram to busting myopia myths on TikTok, she’s seen firsthand how the right online presence can transform a practice’s reach and patients’ trust.
1
Dr. Afkhami stressed that it’s crucial for optometrists to understand how different generations consume online, as each generation engages with content differently.
“Gen Z tends to favor short, authentic and fast-paced content, while millennials still appreciate aesthetics and value-driven messaging,” she explained. “If we’re not meeting patients where they are—in both platform and tone—we risk being tuned out. Understanding their habits allows us to be intentional, whether that means using trending audio on TikTok or crafting informative carousels on Instagram.”
Simply put, generic posts won’t break through the noise. To resonate, optometrists must tailor content to each audience’s preferences, and deliver it where they’re already scrolling.
2
So, where should a practice focus its efforts to reach patients who may be at risk for myopia or already experiencing it? For Dr. Afkhami, two channels top the list for reaching Gen Z and Millennials.
“Instagram and TikTok are the top contenders. Instagram is still huge for visual appeal, especially for eyewear styling, behind-the-scenes reels and educational posts,” she said. “TikTok, on the other hand, offers incredible reach and relatability. It’s the best place to show personality, debunk myopia myths and build a connection with younger audiences who don’t necessarily respond to traditional marketing.”
The key is to lean into each platform’s strengths. Instagram’s polished, curated aesthetic is ideal for showcasing myopia control solutions like specialty lenses or orthokeratology. Meanwhile, TikTok’s casual, snappy style is perfect for playful challenges, myth-busting and authentic snippets from daily practice life.
3
One reason social media works so well for optometrists is its power to make eyewear and eye health feel personal and approachable.
“People want to see themselves in what you’re offering—literally,” Dr. Afkhami commented. “When they see diverse face styling frames or using blue-light lenses during screen time, it’s not just a product, it’s a lifestyle match. Visual storytelling bridges the gap between clinical and relatable. It also helps demystify what an eye exam or myopia control treatment looks like, which makes care feel more approachable.”
From photo carousels to short videos, the goal is to highlight real people and real experiences. This breaks down barriers, reduces patient anxiety and makes booking that first appointment feel less intimidating.
For practices ready to take things a step further, live streaming offers huge potential — if done right. Whether it’s a frame styling session, a behind-the-scenes look at lens fitting, or a Q&A with a doctor explaining how myopia develops or demonstrating new myopia control contact lenses, a live session helps humanize your practice and builds trust faster than static posts alone.
“Keep it short, interactive and welllit,” Dr. Afkhami advised. “Promote the live ahead of time, and always have a second person monitoring the comments so you can respond in real time. Use real patients or staff to model frames—it makes it more genuine. And always end with a clear call-to-action, like a limitedtime discount or link to book an appointment.”
Meanwhile, demonstrations play a powerful role in educating patients about their options. “Quick, hands-on videos, like dropping different lenses to show durability or demonstrating how photochromic lenses react to light, are super effective,” Dr. Afkhami said. “They’re satisfying to watch and turn complex info into something tangible. When patients see the difference, they’re more likely to value the upgrade and follow through with a purchase.”
One of the simplest ways to boost engagement is to tap into people’s love of a fun challenge, especially on TikTok or Instagram.
“Keep it simple and fun. Challenges like ‘#FramesOfTheDay’ or ‘Tag a friend who needs glasses’ are lowbarrier but high-engagement,” said Dr. Afkhami. “Always include an incentive, like a free pair of bluelight lenses or a gift card. And don’t forget to clearly state the rules and timeframe to keep it professional and fair. Bonus tip: feature the winner on your page—it builds credibility and community.”
genuine buzz that translates into new bookings or sales.
Nevertheless, with social media’s reach comes responsibility, especially when real patients or influencers are involved. It’s crucial for practices to responsibly use patient stories, staff modeling or influencer partnerships while maintaining professionalism and compliance with privacy standards.
“Consent is everything,” Dr. Afkhami stressed. “We always use written release forms for any patient-related content, even if it’s just a testimonial. Staff modeling is a great alternative as it keeps things real while being low-risk. With influencers, it’s important to choose partners whose brand aligns with your values. The messaging should feel authentic and always be reviewed to ensure compliance with the Health Insurance Portability and Accountability Act (HIPAA) and professional boundaries.”

Dr. Afkhami shared that her company once ran a “Frame Face-Off” on Instagram Stories where followers voted on their favorite styles. “Not only did we sell out of the winning frame within two weeks, but we also had a 20% bump in styling appointments just from people who wanted to try them on. It was fun, interactive and created real momentum both online and in-office,” she said.
In the age of scrolls, swipes and Stories, Dr. Afkhami’s advice is clear: Optometrists who show up online— intentionally, authentically and consistently—won’t just stay relevant. They’ll thrive.

When handled well, these personal touches can build credibility while staying professional and compliant.
Of course, consistency is key, but how can small practices keep up?
@Eyeamdrnadia 4
These bite-sized campaigns not only grow your reach but also create
“Batch content creation is a game changer—set aside one afternoon a month to film or photograph multiple posts,” Dr. Afkhami recommended.
“Use scheduling tools like Later or Canva to automate posting. And assign one staff member (even parttime) to monitor DMs and comments. We’ve found that even a quick emoji response shows patients that you’re engaged—and that trust translates to booked appointments.”
When done well, social media doesn’t just build community, it drives real business.
Dr. Nadia Afkhami , OD, was born in Iran and embarked on a new journey at the age of two, immigrating to the United States with her family. From an early age, her fascination with optometry sparked a passion that would shape her future. Driven by a deep-seated curiosity about vision science and its impact on people's lives, she pursued a career in optometry, aiming to provide exceptional eye care to her community. Outside her professional endeavors, Dr. Afkhami cherishes spending quality time with her friends and family. Whether engaging in leisurely activities or lively conversations, she values these moments dearly. Her free time often revolves around creating cherished memories with loved ones, be it exploring new places, sharing meals, or simply enjoying each other's company. Throughout her journey as an optometrist, Dr. Afkhami has remained dedicated to her patients, ensuring they receive the best possible care. Her commitment to the field extends beyond the clinic, intertwining with a passion for fostering meaningful relationships with those she serves and cherishes. She has been able to connect with others through her social media page on Instagram and with her new collaborative podcast, The Depth Perception.
eyeamdrnadia@gmail.com
From niche to essential, ortho-K now boasts cutting-edge materials, smarter designs and AI-powered fitting by
Hazlin Hassan
Ortho-K has dramatically transformed from a niche intervention into a cornerstone of myopia management. Thanks to high-performance materials, smarter lens designs and intelligent fitting systems, this overnight treatment is now more precise, comfortable and effective than ever before.
Orthokeratology (ortho-K) has gone from fringe to frontline in myopia management—and it’s not slowing down. With today’s cutting-edge materials, optimized lens designs and artificial intelligence (AI)-powered fitting systems, ortho-K has become more precise, more comfortable and more powerful than ever.
Whether you’re a seasoned fitter or just dipping your toes into the overnight lens world, here’s your update on the latest developments shaping the ortho-K landscape.
Spoiler: It's not just about reshaping the cornea anymore; it's about reshaping the way we practice.
1Materials that breathe better
Once upon a time, high-Dk gaspermeable (GP) lenses were a game-changer. Now? They're being turbocharged.
“With the advancement in material developments, we are lucky to have the ability to use the Acuity 200 (fluoroxyfocon A; Acuity Polymers, Inc.; New York, USA), the world’s first ultra-high Dk GP material with a Dk of 200,”1 said Mr. Fakhruddin Shamsheer Barodawala, optometrist and senior lecturer at SEGi University, Malaysia.
Dk refers to the oxygen permeability of the lens material, with higher Dk values indicating better oxygen transmission. GP lenses are often categorized into low Dk (25-50), high Dk (51-99) and hyper Dk (100+). High Dk GP lenses allow better oxygen transmission to the cornea, potentially improving comfort and corneal health.
“They offer superior oxygen permeability, crucial for ocular health. While earlier generations sometimes compromised on durability or wettability, today’s advanced materials have largely overcome these challenges, while maintaining robust structure and excellent on-eye comfort,” said Mr. Fakhruddin.
This level of oxygen flow is essential for overnight lens wearers, helping


reduce hypoxia-related complications while maximizing corneal integrity.
What’s next? Mr. Fakhruddin said he hopes to see “enhanced surface technology for sustained wettability,” which could reduce deposits and elevate patient comfort.
Modern ortho-K designs now embrace toric peripheral curves and optimized back optic zone diameters (BOZD) to better hug diverse corneal shapes.
“A lot of corneas need toric designs to achieve good centration of the lenses. A well-centered lens is essential for better outcomes. Use of these toric designs ensures a better fit for the lenses,” explained Mr. Fakhruddin.
“The ability to fine-tune overall diameter and treatment zones provides greater flexibility in fitting these lenses for the desired purpose.”
Smaller BOZDs (~5 mm) are proving to be more than a minor tweak—they
Photo: Ecaterina Glazcova/Shutterstock.com
can supercharge myopia control.
BOZD refers to the diameter of the central, flatter area of a contact lens.
“In my experience, and with the evidence in the literature, BOZD optimization is highly important in slowing axial elongation in ortho-K, as it directly impacts the amount and profile of peripheral myopic defocus,” said Mr. Fakhruddin.
“A smaller BOZD typically creates a smaller, more concentrated treatment zone on the cornea, inducing a steeper peripheral ‘plus power ring.’ This stronger myopic defocus signal is widely believed to be the primary mechanism by which ortho-K slows eye growth,” he explained.
Studies have shown that lenses with smaller BOZDs can significantly cut axial elongation compared to standard 6mm BOZD designs.2
“Therefore, carefully selecting, and where possible, customizing the BOZD based on factors such as the patient’s pupil size and refractive error is critical in maximizing the myopia control efficacy of ortho-K treatment,” he added.
Manual fitting is fine… until it’s not. Enter cloud-based platforms like Arise (Bausch + Lomb; Ontario, Canada), computer-aided design and computer-aided manufacturing (CAD/CAM), and topographyguided systems, making first-fit success the new standard. The Arise Orthokeratology Lens System leverages AI and cloud computing to create custom lens designs in seconds based on topography data, cutting down chair time and boosting precision.3
“These systems streamline the design process by instantly interpreting topography data and suggesting highly precise, customized lens designs, which would drastically reduce chair time and the need for extensive diagnostic lens sets,” Mr. Fakhruddin noted.

Ortho-K fitting has come a long way in recent years. Updating your approach could unlock faster fittings, better outcomes and even more satisfied patients.
Here’s your cheat sheet:
• Use ultra-high Dk materials.
• Customize lens design: Think toric curves and dialed-in BOZDs.
• Embrace digital fitting tools: Arise, CAD/CAM, topographyguided systems.
• Refine your pediatric approach: comfort, compliance and patience.
• Use AI as a tool, not a crutch— you are still the expert!
The tools are here. The next generation of ortho-K isn’t just smarter, it’s funkier, faster and way more fun to fit.
“They minimize refits and improve patient satisfaction.”
For younger patients or those with astigmatism, topography-guided fitting isn't optional; it’s essential.
“The technology we have today allows for mostly first lens success,” said Dr. Ashley Tucker, director of The Contact Lens Institute of Houston, USA. “Everyone has busy lives, that’s why efficiency is key!”
Ortho-K is a dream for managing childhood myopia, but the real world can get messy. Comfort, compliance and cooperation are the holy trinity of pediatric success.
“When fitting children with ortho-K lenses, initial comfort and adaptation are common hurdles,” Mr. Fakhruddin said. “We manage these with thorough education on expectations and precise insertion and removal techniques.”
still, well, human. Variables like tear film dynamics, patient lifestyle and complex cases mean clinical judgment still trumps code.
“The optometrist’s clinical judgement remains crucial,” he said. “While the benefits of AI in terms of precision, efficiency and customized solutions are undeniable, AI is a highly advanced and intelligent assistant rather than a complete replacement for the practitioner’s expertise.”
“The trend is clearly in that direction, but a final norm of full automation still requires further advancements in AI’s ability to handle the nuanced, subjective aspects of patient care and the diverse range of corneal responses,” he concluded.

Clear routines and hygiene-focused training are also key. For younger kids aged five to seven years old, it’s as much about psychology as it is physiology.
“It requires immense patience from both parents and doctors,” Dr. Tucker acknowledged. “The key is to validate the child’s fears and ease them into success.”
Although we are close, we’re not quite at the age of AI-controlled ortho-K autopilots.
“AI-guided fundus imaging and examinations have already been developed and are in clinical settings,” Mr. Fakhruddin noted. “However, a fully-automated system where AI makes all the decisions without significant human oversight isn’t quite the standard yet.”
Why? Because the human eye is
1. Acuity Polymers. The First Ultra Dk GP Lens Material. Available at https://www. acuitypolymers.com/gp-materials/acuity-200. Accessed on July 10, 2025.
2. Yang X, Won L, Xiao K, et al. Therapeutic efficacy of orthokeratology lenses with different back optic zone diameters in myopia control: A systematic review and meta-analysis. Cont Lens Anterior Eye. 2025;48(4):102400.
3. Bausch + Lomb. Bausch + Lomb Launches Arise™ Orthokeratology Lens System in the United States. Available at https://ir.bausch. com/press-releases/bausch-lomb-launchesarisetm-orthokeratology-lens-system-unitedstates. Accessed on July 10, 2025.

Mr. Fakhruddin Shamsheer Barodawala is a senior lecturer at SEGi University, Malaysia, where he primarily teaches contact lenses and is actively involved in anterior eye and contact lens research. Mr. Fakhruddin graduated in Optometry from the Lotus College of Optometry, India. He holds fellowships awarded by the Association of Schools and Colleges of Optometry, India; the International Association of Contact Lens Educators (IACLE); the American Academy of Optometry (AAO) and the British Contact Lens Association (BCLA). He has also been elected a member of the Board of Directors at IACLE, works closely with the BCLA’s Digital Learning Committee, and has been appointed as one of BCLA’s Global Ambassadors. Mr. Fakhruddin is a registered optometrist of the Optometry Confederation of India (OCI) and is a lifetime member of the Indian Optometric Association (IOA) in addition to being a member of IACLE, AAO and BCLA. He is also the founder of Online Optom Learning Series (OOLS), a platform offering webinars and courses for optometry students and practitioners. Since its launch, OOLS has hosted nearly 250 sessions.

www.ools.co.in.
Dr. Ashley Tucker graduated from the University of Florida with a Bachelor of Science degree in Microbiology and Cell Science in 2006, before going on to graduate from the University of Houston College of Optometry in 2010. Dr. Tucker completed a Cornea and Contact Lens Residency at the University of Houston, where she received extensive training and experience in the diagnosis and treatment of corneal diseases and complex contact lens fits. She is a partner at Bellaire Family Eye Care and The Contact Lens Institute of Houston, a private practice in Houston, Texas, where she primarily cares for patients in need of specialty contact lenses and myopia management. She is also a visiting assistant professor at the University of Houston College of Optometry, where she is the course master for the Ophthalmic Optics Laboratory. She regularly provides continuing education on the topics of anterior segment disease, specialty contact lenses, myopia management, and ophthalmic optics. Dr. Tucker is a member of the Speaker’s Bureau for the Specialty Division of Bausch Lomb, a consultant for CooperVision, and a lecturer for the STAPLE (Soft Toric and Presbyopic Lens Experience) program. She also serves as the public education chair for the Scleral Lens Education Society, is a member of the advisory board for the Gas Permeable Lens Institute, serves on the AOA Contact Lens and Cornea Section, and is on the Program Committee for the Global Specialty Lens Symposium. She is also a regular columnist for Contact Lens Spectrum.
ashley.w.tucker@gmail.com







What AI can (and can’t) tell us about the next frontier in myopia detection and management
by Diana Truong

Can AI really see the future? From deep learning models to fundus “fortune-telling,” here’s how artificial intelligence is transforming myopia management into a smarter, sharper and more personalized science.

These days, technology seems to predict just about everything, from your next Netflix obsession to whether you’ll need an umbrella tomorrow. So it was only a matter of time before artificial intelligence (AI) set its sights on the future of our patients’ vision.
Think of it as a high-tech crystal ball: AI and predictive analytics are reshaping the way eye care professionals tackle myopia. What was once a reactive game of catchups is evolving into a smarter, more proactive and highly personalized approach to care.
For some optometrists, hearing the term “artificial intelligence" might trigger visions of robot overlords or mysterious black-box algorithms making clinical calls. But according to Dr. Li Lian Foo, a consultant at Singapore National Eye Centre, it’s time to set the record straight…and maybe lower your heart rate a little.
"One common misconception is that AI will eventually replace the role of optometrists," Dr. Foo explained. "In reality, AI is best seen as an assistive tool that augments, rather than replaces, clinical judgment."
That fear of being replaced isn’t the only misconception she encounters. "Another is that AI is a 'black box' that cannot be trusted or understood. Additionally, some may assume AI is only for high-tech institutions or research settings,” she added. “In truth, scalable AI tools are being integrated into everyday practice, including community and primary eye care, to improve screening, triage and access, especially in underserved areas."
"One common misconception is that AI will eventually replace the role of optometrist."
Still feeling a little wary? You’re not alone. But Dr. Foo offers a helpful reframe: Think of AI as your extra set of eyes. "It can rapidly analyze

large volumes of data, highlight subtle changes that might otherwise be missed, or flag high-risk cases earlier,” she explained. “But it doesn't have context, empathy or clinical intuition, which are qualities that only a trained eye care professional brings to patient care."
And if all of this still sounds a bit sci-fi, Dr. Foo gets it. “It's completely natural to feel a little uncertain when new technologies enter clinical practice, especially something as complex as AI," she said. "Rather than taking over, AI serves as a supportive partner. It frees up our time from routine or repetitive tasks so we can focus more on what really matters: connecting with patients, making nuanced decisions and personalizing care."
So, if you’re worried AI is coming for your job, relax. It’s not taking your place. It’s just here to make your job easier, sharper and maybe even a little more fun.
One of AI’s superpowers in the realm of myopia control is spotting trouble before it even knocks.
"Researchers are now leveraging AI and imaging technologies—especially retinal and optical coherence tomography (OCT) images—to uncover subtle structural changes in the eye that may signal early myopia development," said Dr. Foo. "AI algorithms can be trained on large datasets of fundus images to detect patterns like changes in optic disc shape, retinal vessel trajectory or early elongation markers that are difficult for the human eye to quantify consistently."
Here’s where things get especially fascinating: A 2025 study introduced a fresh AI-powered concept called “fundus refraction offset” (FRO), and it just might change the way we think about early myopia detection.1
FRO is an AI-derived metric that measures the gap between what an algorithm thinks the refractive error should be (based on features in the fundus image) and what it actually is.1
To build this tool, researchers trained a deep learning model using over 31,000 fundus images from healthy eyes, teaching it to predict spherical equivalent refraction (SER). When the model was let loose on new, unseen images, it could spot eyes with a fundus that looked more myopic than their actual refractive error suggested.1
"The fundus refraction offset might capture hidden structural changes in the eye that are not yet clinically apparent but are predictive of future myopia progression.”
Even more intriguing? Eyes with a more negative FRO—meaning the fundus looked more myopic than expected—also showed signs like macular thinning and lower choroidal vascularity index. And this was true regardless of their measured SER or axial length. In other words, FRO may help reveal which eyes are structurally more at risk, even when their numbers look deceptively normal.1
"The fundus refraction offset might capture hidden structural changes in the eye that are not yet clinically apparent but are predictive of future myopia progression,” said Dr. Foo. “What is particularly exciting is that this metric could serve as an early warning signal. If the AI detects a fundus pattern that looks more myopic than the current refraction suggests, it could indicate a higher risk of progression in the near future."
This means eye care professionals might soon be able to intervene before refractive error shifts into high gear, giving us a head start in the race against childhood myopia.
The promise and puzzles of genetic data
Imaging isn’t the only place AI is flexing its predictive muscles.
Genetics is the next big frontier in the quest to outsmart myopia.
“Incorporating genetic data into AI models for myopia prediction is a very promising frontier," said Dr. Foo. "We know that myopia is influenced by both genetic and environmental factors, but until recently, clinical practice has focused mostly on lifestyle and refractive trends."
The idea is to combine polygenic risk scores with other data inputs to create a fuller, more personalized risk profile for each child. “This means we could one day identify children who are genetically predisposed to develop high myopia, even before they show clinical signs on refraction or imaging," Dr. Foo explained.
But as with any fortune-telling device, the signals can sometimes get fuzzy. A 2025 review by Liu et al. pointed out that “existing studies have shown that the added value of genetic data in myopia prediction is very limited, and research results are inconsistent.” Some studies reported that genetic risk scores didn’t move the predictive needle much, while others found that they offered an edge over relying on family history alone.2
Still, researchers are far from giving up on the genetic angle. In fact, Ruamviboonsuk et al. recently spotlighted four potential biomarkers (NR1D1, PPP1R18, PG8D2 and PPP1R3D) using machine learning tools. These findings lay the groundwork for future clinical validation and may yet give genetic data a bigger role in shaping personalized prevention strategies.3
AI’s data-driven predictions
AI isn’t just good at spotting early signs of myopia, it’s also becoming a bit of a good fortune teller when it comes to predicting how myopia will progress. A 2024 study, published in Precision Clinical Medicine, developed a multivariate linear regression algorithm that crunched data from more than 612,000 medical records across five independent cohorts.4
Its mission? Predict myopia progression and the risk of developing high myopia. Spoiler alert: it crushed it.
The model achieved an R² value of 0.964 in internal validation and continued to impress across external datasets. For predicting the risk of high myopia, the algorithm clocked in with an area under the curve (AUC) of 0.99—a nearly clairvoyant level of accuracy.4
So what’s behind the magic? Unlike traditional risk assessments that might look at just a few variables (age, current refraction, maybe parental myopia), AI models pull from a much deeper data well.
"By integrating data from multiple sources, such as a child's age, rate of progression, axial length, lifestyle habits, genetic risk and even retinal imaging, AI can identify unique risk profiles and recommend tailored treatment strategies," explained Dr. Foo. "AI can help us match the right intervention to the right patient, at the right time."
The same study also revealed some key clues about who’s at greater risk of high myopia. Kids whose myopia worsened by more than 1.00 D per year hit the high myopia milestone in a median of 3.39 years. Slower progressors had a little more breathing room, about 4.05 years.4
Age of onset matters, too. Children who became myopic between the ages of three to seven reached high myopia in a median of 3.13 years, compared to 4.01 years for those with onset between eight and 18.4
The takeaway? The earlier and faster the progression, the higher the stakes…and the stronger the case for jumping in early with tailored, proactive care.
Among all the breakthroughs AI brings to myopia management, its ability to personalize treatment strategies might be the clearest signal yet that we’re stepping into the future.

Until now, many treatment plans have followed a fairly standardized path, largely based on a child’s age and current refraction. But with AI in the picture, we’re trading in generic protocols for something far more tailored.
“AI has the potential to revolutionize how we approach myopia by moving from a 'one-size-fits-all' model to truly personalized care," said Dr. Foo. "It can help us match the right intervention to the right patient, at the right time. It can also predict who is likely to progress rapidly and may require more intensive follow-up, versus those who are stable and need less frequent visits."
That level of insight means clinicians aren’t just making educated guesses, they’re guided by real-time, datadriven foresight. As Dr. Foo explained, "We are essentially moving toward a feedback loop where AI does not just guide the start of treatment but helps optimize it over time. By continuously analyzing longitudinal data, such as changes in axial length, refraction progression, compliance, side effects and lifestyle factors, AI can help identify which patients are responding well to a particular treatment and which are not."
This kind of ongoing analysis lets clinicians fine-tune treatment decisions, rather than sticking to a rigid plan. "This kind of adaptive learning system is key to realizing precision medicine in myopia management, not just treating the condition, but treating the individual," Dr. Foo noted.
Challenges and considerations
Of course, even the clearest crystal ball might come with a few cracks. As promising as AI is for myopia management, it is not without its blind spots.
"One major concern is bias. If AI models are trained on datasets that lack diversity in ethnicity, geography or socioeconomic background,
the predictions may not generalize well across different populations,” she explained. “This could lead to unequal care or missed risks in underrepresented groups."
Another red flag? Data privacy. As more personal information, like genetic data and high-resolution images, gets pulled into the mix, the stakes get higher.
"As we embrace AI in myopia management, we must remain vigilant about its limitations," cautioned Dr. Foo. "Transparency, proper validation and ethical oversight are essential to building trustworthy AI systems that are safe, equitable and clinically meaningful."
Like any crystal ball from the pages of folklore, AI’s predictive powers in myopia management aren’t flawless. They come with their share of blind spots and a clear need for expert interpretation. But unlike their mythical counterparts, these tools are backed by data, clever algorithms and some serious scientific legwork.
The crystal ball is here. The real question is: Are we ready to look into it?
1. Yii F, MacCormick IJC, Strang N, et al. Fundus refraction offset as an individualized myopia biomarker. JAMA Ophthalmol. 2025:e251513. [Epub ahead of print.]
2. Liu N, Li L, Yu J. Application of artificial intelligence in myopia prevention and control. Pediatr Investig. 2025;9(2):114-124.
3. Ruamviboonsuk V, Lanca C, Grzybowski A. Biomarkers: Promising tools towards diagnosis, prognosis, and treatment of myopia. J Clin Med. 2024;13(22):6754.
4. Li J, Zeng S, Li Z, et al. Accurate prediction of myopia progression and high myopia by machine learning. Precis Clin Med. 2024;7(1):pbae005.

Right now, eye care professionals are at a crossroads. We can approach AI with arms crossed, wary of its imperfections and potential pitfalls. Or, we can see it for what it really is: a powerful, data-driven ally in our fight against the global rise of myopia. Not a magic solution, but a high-tech crystal ball offering early clues and sharper insights into our patients’ visual futures.
The smartest way forward? A bit of both. Use AI for what it does best—analyzing, predicting, flagging risk—and pair it with what only humans can bring to the table: clinical judgment, compassion and ethical decision-making. Together, this combo could move myopia care from reactive firefighting to truly proactive, personalized prevention, saving millions from the long-term consequences of high myopia.

Dr. Li Lian Foo is a consultant at the Cataract and Comprehensive Ophthalmology Department, Singapore National Eye Centre (SNEC). She graduated with First Class Honors in Chemical Engineering from NUS in 2008 and earned her MD from Duke-NUS in 2012. She became a Fellow of the Royal College of Ophthalmologists in 2016 and attained a Master of Medicine in Ophthalmology and a Graduate Diploma in Family Medicine in 2017. An accomplished researcher and author, Dr. Foo has published nine peer-reviewed papers, presented at international conferences and co-authored two ophthalmology guidebooks. She received the Young Investigator Award at SGH’s Annual Scientific Meeting in 2011. Dr. Foo’s passion for innovation led her to the MIT-Harvard Medical School Healthcare Innovation Bootcamp in 2019, where her team was runner-up in the elevator pitch competition. She also completed the Eureka-Singapore Monsoon School on Translational Medicine. As SNEC’s first Myopia Fellow, Dr. Foo is dedicated to addressing the myopia epidemic through innovative solutions. With a vision to enhance clinical care, she strives to develop novel tools and treatments, bridging gaps in ophthalmology and improving patient outcomes.
drfoolilian@gmail.com

Dr. Bariah Mohd Ali
What began as an unexpected university placement blossomed into a lifelong passion for Prof. Dr. Bariah Mohd Ali. Today, she is a respected academic and pioneering practitioner, tirelessly shaping the future of optometry in Malaysia through her leadership in education, research and policy.
In the quiet town of Ipoh, Perak, a young girl was raised by a single mother, a schoolteacher. Her father, a railway clerk, passed away when she was just five. But from those early days of loss and resilience, Prof. Dr. Bariah Mohd Ali’s path was already being carved—a path that would one day help shape the future of optometry in Malaysia.
Today, Prof. Bariah is a respected academic and practitioner, known not only for her expertise in optometry and vision science, but also for her leadership in education, clinical innovation and public health advocacy. She currently serves as a professor at Universiti Kebangsaan Malaysia (UKM) and president of the Malaysian Academy of Optometry (PAOM), where she continues to push boundaries in vision care and policy.


“I never imagined I would be in this field,” Prof. Bariah recalled candidly. “I initially wanted to study law, but science students weren’t allowed to switch to arts programs at public universities back then.”
With medicine and engineering off the table for various reasons, she accepted a place in UKM’s newly introduced Optometry program—a decision that, at the time, was made without fully understanding what the field entailed.
“I only knew it was offered under the Faculty of Medicine, so I thought it might have something to do with healthcare,” she laughed.
But what began as a reluctant acceptance quickly blossomed into a meaningful and life-long passion and career. Looking back, she now sees it as a blessing. “I never looked back after that. UKM was the first university in Malaysia to offer an optometry degree, and I was fortunate to be part of that pioneering group.”
Upon completing her degree in 1991, Prof. Bariah worked briefly in private practice before returning to UKM as a tutor in the Optometry Unit. By 1992, the Optometry Department was officially formed under the Faculty of Allied Health Sciences, and she has remained there ever since.
Her journey in academia took a major leap forward when she pursued her Ph.D. at the University of New South Wales (UNSW) in Sydney, Australia, on a scholarship from the Public Service Department (JPA). At that time, she was already a young mother to two young boys.
“Balancing motherhood, marriage and research in a foreign country wasn’t easy,” she recalled. “But the experience helped shape my character, broadened my understanding of optometry and gave me the tools I needed to contribute meaningfully when I returned.”

Prof. Bariah’s core areas of expertise—specialty contact lenses and myopia control—are driven by clinical demand. In the early days of her career, she began receiving referrals from across the country for complex corneal conditions, such as keratoconus, post-graft irregularities and high astigmatism. At the time, Malaysia lacked advanced designs and diagnostic tools for such cases.
“Managing those cases became a passion of mine. I was fortunate to have a mentor who encouraged me to explore and innovate in that space,” she said, referring to Prof. Emeritus Dr. Norhani Mohidin, her supervisor, early in her career.
In the early 2000s, she undertook clinical attachments in India, Hong Kong and Australia to improve her knowledge in specialty lens fitting. By 2004, she introduced orthokeratology (ortho-K) lenses to the clinic at UKM and later spearheaded research in this area. This service has since grown into a referral and training center for both undergraduate and postgraduate students.
Over the years, Prof. Bariah has received numerous honors that affirm her global standing. These include her appointment as a Fellow of the British Contact Lens Association, American Academy of Optometry and Malaysian Academy of Optometry. In 2020, she received the prestigious IACLE Contact Lens Educator Award for the Asia Pacific region.
This year, her contributions were formally recognized with the Darjah Setia Negeri Sembilan (DNS) medal, awarded by His Royal Highness Yang di-Pertuan Besar Negeri Sembilan.
With a teacher for a mother and a natural love for mentorship, it’s no surprise that teaching became a central part of Prof. Bariah’s calling. “Education is in my blood,” she shared proudly. “That’s why I left private practice to pursue academia.”

Prof. Bariah is an advocate for continuous education. Beyond the lecture hall, she believes in elevating the standards of the optometry profession through structured continuing education.
“Technology is changing optometry rapidly. From diagnostic tools to AI-driven treatments, we need to keep up. Continuing education ensures practitioners are competent and confident in managing more complex cases.”
“Optometry is experiencing significant advancements, particularly in technology and treatment methods. These advancements include innovative diagnostic tools, therapeutic approaches and a growing integration of artificial intelligence (AI), which allows optometrists to focus on specific management such as contact lenses, low vision and binocular vision,” she added.
As president of PAOM, she has been instrumental in organizing local and international seminars, advocating for professional development, and recognizing subspecialties within optometry—a critical step toward advancing the field.
“PAOM believes in continuous education to improve the quality of optometry services in the country. We provide a platform for practitioners to share knowledge and experience in managing patients, and we acknowledge practitioners as experts in subspecialty areas in optometry. Our mission is to raise the standard of practice and education in Malaysia to provide high-quality eye care to the public.
“Technology is changing optometry rapidly,” she enthused. “From diagnostic tools to AI-driven treatments, we need to keep up. Continuing education ensures
practitioners are competent and confident in managing more complex cases.”
Among the most promising changes she is championing is the longawaited revision to Malaysia’s Optical Act 1991. The proposed Optometry Bill, expected to be tabled in Parliament in late 2025, will officially recognize optometrists as primary eye care providers.
“This is a monumental shift,” said Prof. Bariah. “It aligns optometry in Malaysia with global standards and addresses challenges like unregulated online sales, inconsistent training and lack of subspecialty recognition.”
She added that professional development is essential for optometrists seeking to advance in their careers, gain new skills and remain competitive in their field.
One major hurdle is the limited career advancement structures for optometrists within government frameworks.
“There are several challenges including supportive structures that recognize and acknowledge the development and ensure relevance. Unlike the medical profession, optometry doesn’t yet have recognized subspecialties. This discourages optometrists from continuing their professional development,” she noted. “But the implementation of the new bill may finally change that.”
As myopia has become a global public health issue due to the drastic increment in its prevalence, especially in young children and teenagers, Prof. Bariah’s work in this area has become more urgent than ever.
glaucoma and maculopathy, which, if left untreated, can lead to blindness. Therefore, controlling its progression isn’t just about clearer vision—it’s about preventing blindness,” she explained.
“High myopia is closely associated with pathological conditions such as

After more than three decades in the field, Prof. Bariah remains as motivated as ever. “I love my work. And that love is what keeps me going.”
She elaborated that there are several tools and practices in myopia control, which include specifically designed myopia control spectacle lenses or contact lenses (such as ortho-K), pharmacological agents or a combination of both optical lenses and eye drops. Her approach combines optical tools—such as specialty lenses and orthokeratology—with behavioral interventions.
And that love has also illuminated a path for many to follow. cc

“Myopia is closely associated with excessive near work, poor lighting and less outdoor activities. Therefore, less time doing near work (such as using gadgets and smartphones) and more outdoor activities can help to slow down myopia progression.
Her clinical research in myopia control is conducted in collaboration with international companies, and she continues to play an active role in trials and protocol development.
When asked what part of her work brings the greatest joy, she answered without hesitation: her students.
“UKM is a public university, and many of our students come from underprivileged families. Watching them graduate and improve their families’ economic situation—that’s the most gratifying part of my job,” she shared.
Her impact is generational—not only helping students build meaningful careers but also ensuring the public receives the highest standard of eye care.
“I am also grateful that I am involved in the training of optometrists in Malaysia so that the public receive the best eye care services,” she added.

Dr.
Ali is a professor in Optometry and Vision Science at the National University of Malaysia and president of the Malaysian Academy of Optometry. She received her Bachelor’s degree in Optometry from the National University of Malaysia and her Ph.D. from The University of New South Wales, Australia. She was fundamental in the development of a specialty contact lens clinic, which now acts as a referral and training clinic for postgraduate and undergraduate students. She is actively involved in research, with interests in specialty contact lenses and myopia control and has published and presented her research findings locally and internationally. In recognition of her expertise in the area of contact lenses, she was admitted as a Fellow by the Association of Malaysian Optometrist (FAMO) in 2008, British Contact Lens Association (FBCLA) in 2012, Malaysia Academy of Optometry (FAOM) in 2019, and is the recipient of the prestigious IACLE Contact Lens Educator Award for the Asia Pacific region in 2020. Prof. Dr. Bariah is a strong advocate for continuous professional development in the optometry profession. She was elected as a council member in the Malaysian Optical Council (MOC) from 2020-2022 and was instrumental in the development of Malaysian Academy of Optometry (PAOM) in 2018. She is currently the president of PAOM and is actively involved in planning, organizing and delivering seminars for local and international optometrists. In recognition of her leadership contributions to the optometry profession, she was elected as a Fellow by the American Academy of Optometry (FAAO) in 2019.
bariah@ukm.edu.my
Photo: Stokkete/Shutterstock.com
Researchers are moving beyond traditional methods to explore cutting-edge drug therapies and genetic interventions for myopia control
by Hazlin Hassan
For years, low-dose atropine has been the go-to in your pharmacological toolkit. But the war on myopia isn’t just about lenses and nightly drops anymore. It’s getting chemical. Maybe even genetic. But which of these latest developments will fizzle and flame out, and which ones are set to redefine myopia control?
From pre-onset atropine dosing to sustained-release ocular inserts and microneedle patches, researchers are cooking up strategies that go far beyond the traditional playbook.
Some are already making quiet debuts in clinics; others are still setting conference halls abuzz. Either way, myopia control is entering its most experimental and potentially game-changing era yet.
Welcome to the next generation of drug therapies: some familiar, some experimental and some sounding like they were lifted straight off a sci-fi script. Here's our rundown of the latest and most intriguing developments in pharmacological myopia control.
Atropine has long been the star player in the pharmacologic lineup for myopia control. But its low-dose variants, especially 0.01%, have stirred debate.
“Studies in Asia generally reported a meaningful slowing of myopia progression and eye growth with 0.01% atropine,” said Dr. Jeffrey Walline, associate dean at The Ohio State University College of Optometry. “But recent studies outside of Asia have had much less consistent results with the same concentration.”
This has led to recommendations to start myopic children at one drop of 0.05% in each eye at bedtime, and only lower the concentration if children complained of light sensitivity or blurriness when reading, he explained. The 0.05% atropine has been shown in the LAMP trial to offer the best balance between efficacy and minimal side effects.1
Dr. Ashley Tucker, director of The Contact Lens Institute of Houston, agreed: “Clinically, I can say low-dose atropine is very effective. I tend to reserve it for my younger patients and then transition them into a myopia control contact lens.” 1
The future? Sydnexis’ SX-601 (California, USA), a once-daily, pediatric-specific atropine drop, is currently under FDA review and, if approved, would become the first pharmaceutical treatment specifically authorized in the U.S. to slow childhood myopia.2
“Clinically, I can say low-dose atropine is very effective. I tend to reserve it for my younger patients and then transition them into a myopia control contact lens.”
- Dr. Ashley Tucker
2
Here’s a twist: What if we didn’t wait for kids to become myopic? “We can predict myopia onset with good accuracy,” Dr. Walline shared. “We can screen children and apply the drug to those likely to become nearsighted.”
A study by the Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) showed that this approach can delay the onset and reduce the severity.3 “We submitted a grant to determine whether it works
in children in the United States,” Dr. Walline added.
The big challenge? Getting access to children before they land in your chair. Dr. Walline suggests outreach to schools or siblings of myopic children may be key. If this catches on, we may be entering an era of preemptive pharmacology.
3
What else is out there? So far, alternatives to atropine are more “promise than practice.”
7-Methylxanthine: A caffeine derivative with the potential to slow axial elongation. A Danish trial showed it was associated with reduced myopia progression and reduced axial elongation.4 However, randomized, controlled trials are needed.
Pirenzepine: Pirenzepine ophthalmic gel 2% was effective compared with placebo in slowing the progression of myopia over a two-year treatment period and demonstrated a clinically acceptable safety profile in early 2000s trials.5 However, development fizzled, possibly due to its reduced efficacy as an antimyopia treatment compared with topical atropine, and the requirement of twice-daily rather than once-daily dosing.6

Dr. Tucker noted, “I have read about them, but I am not aware of anyone using them or any clinical trials.”
4
You could have the best molecule on earth, but it’s only as good as the delivery system.
Daily eye drops? Annoying for kids. Easy to forget. Easy to fumble. That’s where drug delivery innovation enters the chat.
Sustained-release ocular inserts: Imagine atropine-releasing tiny ocular inserts. Compliance? Solved.
Microneedle patches: Still largely experimental, these ocular patches could deliver drugs directly into the eye.
“There is a lot of promise… but achieving the sustained release has proven to be very difficult,” Dr. Walline admitted. “As new technologies become available, I hope these therapies will prove to be more effective than daily dosing.”
5
Gene therapy is all the rage in ophthalmology, but is it realistic for myopia? Dr. Walline was skeptical.
“Myopia genetics are very complicated. Over 200 genes have been linked to myopia, and we can only explain a small amount of excessive eye growth with them. I don’t think gene therapy for myopia is realistic within the next decade, but I hope to be proven wrong,” he said.
However, Dr. Tucker was more optimistic. “I think anything is possible, honestly. It would be most beneficial for patients who have one or two parents with high or pathological myopia.”
Gene therapy is a cool idea, but don’t throw away your atropine just yet.
6
Red-light therapy—specifically, repeated low-level red light (RLRL)—
is gaining traction, especially in China. In myopic children, RLRL therapy with 100% power significantly reduced myopia progression over six months compared with those treated with a sham device of 10% original power.7
But not everyone is convinced.
“I am skeptical,” said Dr. Walline. “Red-light therapy tends to reduce nearsightedness and shorten the eye, which doesn’t happen naturally. When the treatment is ceased, the gain is likely to be lost.”
A study has also shown that when the treatment was discontinued, there was a rebound effect, which means that the benefits of treatment were lost in a relatively short period.8
1. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology. 2019;126(1):113-124.
2. Sydnexis. Sydnexis Announces FDA Acceptance of New Drug Application and PDUFA date for SYD-101, for the Treatment of Progression of Pediatric Myopia. Available at https://www.sydnexis. com/post/sydnexis-announces-fdaacceptance-of-new-drug-application-andpdufa-date-for-syd-101-for-the-treatment-ofprogression-of-pediatric-myopia. Accessed on July 10, 2025.

More concerning are anecdotal reports of vision loss. Dr Tucker was blunt: “At this point, the potential risks outweigh the potential benefits,” she noted.
While RLRL is technically not a drug therapy, it shares space in the wild frontier of myopia control and shows how enthusiasm can sometimes outpace evidence.
Across the board, experts agree that long-term safety and patient adherence remain top concerns.
“Atropine has been studied for a meaningful amount of time,” said Dr. Walline. “While there weren’t any significant side effects detected, the long-term efficacy was questioned.”
From drops and inserts to red lights and gene codes, the future of myopia control is teeming with ideas. Some may flame out. Some will fizzle. But others could redefine what it means to manage pediatric myopia. So keep your eyes peeled. The next blockbuster in myopia control might just be a drop or a patch away.
Dr. Ashley Tucker graduated Summa Cum Laude from the University of Houston College of Optometry, where she also completed a Cornea and Contact Lens Residency. She received extensive training and experience in the diagnosis and treatment of corneal diseases and in complex contact lens fits including patients with keratoconus, corneal transplants, and refractive surgery. Dr. Tucker is the director of The Contact Lens Institute of Houston which focuses on finding the perfect contact lens option for all patients. She is passionate about fitting scleral contact lenses and myopia management. She has earned her Fellowship from the Scleral Lens Education Society which distinguishes her as an expert scleral lens fitter. She serves as the Public Education Chair for the Scleral Lens Education Society. She is certified in fitting orthokeratology lenses in both children and adults and has extensive experience and knowledge in myopia management. In 2024, she was named a Global Ambassador for Myopia Management by the World Council of Optometry. Dr. Tucker is also a visiting assistant professor at the University of Houston College of Optometry. She is a member of the Speaker’s Bureau for the specialty division of Bausch & Lomb, a member of the Professional Advancement consultant team for CooperVision, and a consultant for Topcon and a lecturer for the STAPLE (Soft Toric and Presbyopic Lens Experience) program. In her spare time, she enjoys traveling and spending quality time with her husband, daughter and son.
ashley.w.tucker@gmail.com

3. CU Medicine. CUHK world’s first study proves myopia in children can be prevented by low-concentration atropine eyedrops. Available at https://www.med.cuhk.edu. hk/press-releases/cuhk-world-s-first-studyproves-myopia-in-children-can-be-preventedby-low-concentration-atropine-eyedrops. Accessed on July 10, 2025.
4. Trier K, Cui D, Ribel-Madsen S, Guggenheim J. Oral administration of caffeine metabolite 7-methylxanthine is associated with slowed myopia progression in Danish children. Br J Ophthalmol. 2023;107(10):1538-1544.
5. Siatkowski RM, Cotter SA, Crockett RS, Miller JM, Novack GD, Zadnik K; U.S. Pirenzepine Study Group. Two-year multicenter, randomized, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. J AAPOS. 2008;12(4):332-339.
6. Ganesan P, Wildsoet CF. Pharmaceutical intervention for myopia control. Expert Rev Ophthalmol. 2010;5(6):759-787.
7. Dong J, Zhu Z, Xu H, He M. Myopia Control Effect of Repeated Low-Level Red-Light Therapy in Chinese Children: A Randomized, Double-Blind, Controlled Clinical Trial. Ophthalmology. 2023;130(2):198-204.
8. Xiong R, Zhu Z, Jiang Y, et al. Sustained and rebound effect of repeated low-level red-light therapy on myopia control: A 2-year posttrial follow-up study. Clin Exp Ophthalmol. 2022;50(9):1013-1024.

Dr. Jeffrey J. Walline, OD, PhD, is the associate dean of Academic Affairs at The Ohio State University College of Optometry. He received his Doctor of Optometry degree from the University of California, Berkeley School of Optometry and his Master’s and PhD degrees from The Ohio State University College of Optometry. Dr. Walline has led several pediatric contact lens studies and is the study chair of the Bifocal Lenses In Nearsighted Kids (BLINK and BLINK2) Studies, a National Eye Institute (NEI)sponsored study of soft multifocal contact lens myopia control, and co-chair of the Delaying the Onset of Nearsightedness Until Treatment (DONUT) Study, an NEI-sponsored planning grant to prepare an application for a study to determine whether low concentration atropine can delay myopia onset. Dr. Walline specializes in treating several conditions, including myopia, keratoconus, and corneal trauma, and is highly regarded for his expert knowledge of contact lenses and their associated risk factors.
walline.1@osu.edu


by Tan Sher Lynn
With soaring prevalence rates of a global myopia epidemic, practitioners must now understand the complete picture of disease onset and progression—including both environmental factors and genetic predispositions. This holistic approach, from tracking family history to leveraging new polygenic risk scores, is becoming essential for personalized myopia management.
Optometrists are often the frontliners of vision care, and understanding the underlying causes of myopia has become more critical than ever. With prevalence rates soaring—particularly in urban Asia, where adult myopia now affects up to 83% of the population1 practitioners must grasp not only environmental drivers but also the genetic predispositions that shape disease onset and progression. Why family history matters in practice
Prof. Seang-Mei Saw, Distinguished Wallace Foulds Professor at the Eye
Academic Clinical Program, DukeNUS Medical School, and head of the Myopia Unit at the Singapore Eye Research Institute, described myopia as resulting from a combination of hereditary and lifestyle-related causes.
“Myopia is both environmental and genetic in origin. Several hundred small genes have been identified for myopia and thus optometrists should evaluate parental history to determine any genetic origins of myopia,” she said.
Tracking family history isn’t just a routine question; it’s a key diagnostic
tool. A comprehensive family history helps predict risk and inform early intervention. Twin and population studies estimate the heritability of refractive error between 60% and 90%,2,3 yet identified genetic variants only explain a fraction of that risk. Still, Dr. Saw emphasized that parental history remains a potent indicator.
“Optometrists should let parents know that if there is a family history of myopia, the risks of myopia will be higher. The family history of myopia may denote genetic heritability or a common lifestyle in the family,” she noted.
It’s not genes or environment—it’s both. Evidence now supports geneenvironment interactions: Genetic susceptibility amplifies the impact of lifestyle factors like near-work and outdoor exposure.
“There is interaction between near-work and greater genetic susceptibility as well as outdoor and greater genetic susceptibility,” Prof. Saw explained. “Thus, children who have a genetic predisposition and spend more time on near-work or less time outdoors may have risks of myopia greater than expected.”
This insight reshapes how optometrists counsel families. Those with genetic predispositions should be especially mindful of lifestyle management.
While rare Mendelian forms of extreme myopia exist, typical myopia arises from the additive effects of multiple small genes across pathways in the retina and sclera.
“There is no major gene for myopia, but multiple small genes are involved in different pathways, including in the layers at the back of the eye, such as the retina and sclera,” Prof. Saw explained.

Genome-wide association studies (GWAS) have identified hundreds of single-nucleotide polymorphisms (SNPs), including variants near ZC3H11B and other axial-lengthrelated genes. Although each SNP confers only a modest risk, its cumulative effect can significantly influence susceptibility. Recognizing this polygenic contribution offers a more refined approach to risk prediction and personalized myopia management.
The concept of a polygenic risk score (PRS) is evolving from research into clinical application, offering a promising tool for personalized risk prediction. Prof. Saw and her colleagues have developed an Asianspecific PRS to predict high myopia in Chinese children, based on data from the Singapore Cohort of Risk Factors for Myopia (SCORM) cohort.4
“We have developed a genetic risk score for myopia, and the top genes for myopia could be tested in children. The child’s DNA may be obtained from the cheeks or saliva, and the genetic risk scores calculated to determine the risk of myopia and best management,” she explained.
The researchers found that adding the PRS to other clinical information, such as a child’s age, time outdoors and parental myopia, improves the prediction of high myopia risk (AUC= 0.77) in teenagers. The PRS alone performed well in the prediction of high myopia, with children in the highest PRS risk percentile having increased odds of developing high myopia.
These findings highlight the potential clinical value of integrating the PRS with parental myopia to improve the predictive performance to detect children at risk of high myopia, enabling more targeted preventive strategies.
“Genetic testing will help to identify high-risk children who can benefit from treatment to slow myopia progression and prevent high
myopia with the associated visual complications. High-risk children may be treated with stronger interventions or a combination of interventions,” Prof. Saw further said. “Stronger interventions include higher doses of atropine eyedrops (for example, 0.1%), or a combination of eye drops with optical devices such as special defocus contact lenses or spectacles,” she explained.
Nevertheless, while genotyping costs have dropped dramatically, routine deployment of PRS-based genetic testing still faces financial barriers.
“The biggest challenge is the cost of the test,” she acknowledged. “Large-scale implementation in government or private clinics will depend on whether patients are interested in genetic prediction to guide treatment, and whether they are willing to pay for it.”
Looking ahead, Dr. Saw envisioned models combining genetic, environmental and ocular data. “A comprehensive management plan for the child can be developed based not only on the genetic profile but also on important ocular factors such as the age of onset and progression of myopia,” she noted.
1. Ministry of Health Singapore. August 16, 2019. Speech by Dr. Lam Pin Min, Senior Minister of State for Health, at the opening of the Singapore National Eye Centre’s Myopia Centre. Available at https://www.moh.gov. sg/newsroom/speech-by-dr-lam-pin-minsenior-minister-of-state-for-health-at-theopening-of-the-singapore-national-eye-centres-myopia-centre-16-august-2019. Accessed on July 15, 2025.
2. Lopes M, Andrew T, Carbonaro F, et al. Estimating Heritability and Shared Environmental Effects for Refractive Error in Twin and Family Studies. Invest Ophthalmol Vis Sci 2009;50(1):126-131.
3. Dirani M, Chamberlain M, Shekar SN, et al. Heritability of refractive error and ocular biometrics: the Genes in Myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2006;47(11):4756-4761.
4. Lanca C, Kassam I, Patasova K, et al. New Polygenic Risk Score to Predict High Myopia in Singapore Chinese Children. Transl Vis Sci Technol. 2021;10(8):26.

This approach reflects the essence of precision optometry, tailoring the intensity and type of intervention not solely on refractive error but on a child’s broader risk profile as well.
Understanding genetic susceptibility to myopia is no longer optional for today’s optometrists—it’s essential. From the foundational SCORM study to emerging polygenic risk scores, genetics is becoming a key component of personalized care.
Staying informed about actionable genetic insights isn’t just good clinical practice; it’s a gateway to delivering more precise and effective myopia management for the next generation.
Prof. Seang-Mei Saw is the Distinguished Wallace Foulds Professor at the Duke-NUS Medical School, Singapore; cohead of the Myopia Department, at the Singapore Eye Research Institute (SERI); and a professor at Saw Swee Hock School of Public Health, National University of Singapore (NUS). She received her medical degree from NUS, and her MPH and Ph.D. from the Johns Hopkins Bloomberg School of Public Health, USA. Prof. Saw’s work has been instrumental in building our current understanding of environmental and genetic influences, treatments and the burden of myopia. She has pioneered large-scale longitudinal myopia studies, including SCORM, STARS and GUSTO Myopia, and developed the fitness tracker FitSight for myopia prevention. Prof. Saw has an H-index of 145, with over 600 publications in international journals including the Lancet, Nature Genetics and JAMA . Her accolades include the prestigious national President’s Science Award Singapore (Team) in 2019, the Chew Sek Jin Memorial Lecture Award, International Myopia Conference (IMC 2013), and a place on the Top 100 Ophthalmologist Power List in The Ophthalmologist (2014, 2023). ephssm@nus.edu.sg


by Diana Truong
Atropine, red light, spectacle lenses… Myopia management is no longer a one-track script. As evidence stacks up and options multiply, eye care professionals are finding themselves in the director’s chair, balancing science, strategy and patient realities to keep progression in check.
Myopia management is a bit like binge-watching a Netflix drama with endless pot twists. Just when you think you’ve figured out the main character (Atropine? Red light therapy? Fancy lenses?), a new development drops. Optometrists, much like dedicated fans, have to stay sharp, keeping up with shifting data, heated debates and incomplete story arcs.
One of the hottest subplots in the myopia control series centers around atropine eye drops. What concentration actually works and keeps side effects at bay?
“While 0.01% was once considered the default choice due to its excellent safety profile, accumulating evidence suggests that it may be suboptimal in efficacy, particularly in younger or fast-progressing children,” said Dr. Li Lian Foo, a consultant at Singapore National Eye Centre. “The 'sweet spot' many clinicians and researchers are coalescing around is 0.025% to 0.05%."
When it comes to race, iris color and atropine performance, the waters get murky. "Melanin binding plays a role in drug absorption and pharmacodynamics; in individuals with darker irides,” explained Dr. Foo.
“The slower systemic release may partly explain the relatively lower incidence of side effects."
Then there’s the dreaded rebound effect—when myopia speeds up again after stopping atropine. Dr. Glenda Aleman-Moheeputh, president and CEO of OK Love Myopia Control Experts (Florida, USA), approaches it cautiously. “I won’t even think about tapering until I’ve had two years of no change in refractive error or axial elongation,” she said.
What about once tapering stops? It’s a slow and steady fade-out. “We drop one day per week each month—so from seven days to six days for a month, then five days the next month, and so on,” she explained.
Low-level red light (LLRL) therapy is one of the buzziest new treatments in myopia control. Promising results? Yes. But there’s a twist.
"Recent case reports and regulatory reviews have highlighted the need for caution, particularly regarding prolonged exposure, improper use or unregulated devices," warned Dr. Foo, adding that "the long-term effects of repeated retinal exposure to red light in developing eyes are not fully understood, and this
uncertainty warrants a conservative approach."
In response, China has tightened regulations, effectively removing sketchy devices from the market.* A solid step forward, but this storyline is far from resolved.
Forget plain glasses. Today’s spectacle lenses are designed to do more than correct vision. They’re now engineered to slow myopia progression too. These new designs “offer a solution that sidesteps the pharmacological side effects of atropine and the compliance or infection-related risks of contact lenses,” explained Dr. Foo.
Dr. Aleman-Moheeputh believes that, though not yet available in the United States, these lenses will open the door for more eye care professionals (ECPs) to enter the myopia management space.
"Having spectacles for myopia management really brings down all those barriers because we all know as optometrists how to prescribe glasses,” she predicted. “So, I think that this is going to allow a larger percentage of ECPs to feel comfortable having those conversations and start prescribing these spectacles for myopia management."
For high-risk patients, combination therapies are gaining ground…and showing promise. "Combination therapies represent a promising frontier in myopia management, particularly for children with rapid progression or high myopia risk,” said Dr. Foo. “Current evidence suggests that combining low-dose atropine (typically 0.01% to 0.05%) with optical interventions can yield synergistic effects, achieving greater axial length control than either modality alone."
That’s exactly the approach Dr. Aleman-Moheeputh takes in practice. "If I have a three year old
that is already myopic, I’m going to automatically start them with a combination therapy because they’re high risk,” Dr. Aleman-Moheeputh said.
Her go-to pairings? Orthokeratology (ortho-K) and low-dose atropine, or soft multifocal lenses with atropine.
For many families, the biggest challenge isn’t choosing the right treatment, it’s affording it and getting the child on board.
"In my office, I don’t let any child go untreated because of finances," stated Dr. Aleman-Moheeputh firmly. Her solution? Start with low-cost atropine, space out follow-ups when appropriate and offer flexible payment plans.
But even the most affordable or cutting-edge option won’t work without patient buy-in.
“The patient is the star of the show,” she added. “Even if the parent loves the idea of ortho-K, if the child isn’t comfortable or willing to wear the lens, it’s not going to succeed.”
"Hopefully every eye care practitioner will be talking about myopia management,” envisioned Dr. Aleman Moheeputh. “It's going to become the standard of care, not something only specialists discuss.” She predicted that spectacle lenses will serve as an entry point for many U.S. practitioners, while complex cases may be referred to specialized clinics.
Dr. Foo shared a similar forwardlooking perspective, foreseeing “more widespread integration of artificial intelligence and big data analytics to enable precise risk stratification and tailor interventions to individual patients based on genetic, environmental and biometric profiles.

Dr. Foo emphasized the importance of aligning care to both medical and personal realities. “By tailoring recommendations to the socioeconomic realities of each family, practitioners can help ensure that effective myopia management remains equitable and sustainable," she said.
That includes selecting treatments that balance between efficacy, safety and cost, as well as delivering age-appropriate education to help patients and parents understand the importance of adherence, what to expect and how to stay on track.
What’s coming next?
The future of myopia management might look both more mainstream and more personalized, thanks in part to artificial intelligence.

Like your favorite streaming saga, myopia control is a story that’s still unfolding. From atropine and LLRLto futuristic lenses and combination therapies, optometrists will want to keep watching, learning and adapting.
The best practitioners? They’re the ones who follow every subplot closely, always keeping the main character— the patient—in focus. And with new innovations and data on the horizon, one thing’s for sure: this is one show worth staying tuned into.
Reference
* Wang YX, Wang N, Wong TY. Red Light Therapy for Myopia-Current Regulatory Changes in China. JAMA Ophthalmol. 2025;143(3):197-198.

Dr. Li Lian Foo is a consultant at the Cataract and Comprehensive Ophthalmology Department, Singapore National Eye Centre (SNEC). She graduated with First Class Honors in Chemical Engineering from NUS in 2008 and earned her MD from Duke-NUS in 2012. She became a Fellow of the Royal College of Ophthalmologists in 2016 and attained a Master of Medicine in Ophthalmology and a Graduate Diploma in Family Medicine in 2017. An accomplished researcher and author, Dr. Foo has published nine peer-reviewed papers, presented at international conferences and co-authored two ophthalmology guidebooks. She received the Young Investigator Award at SGH’s Annual Scientific Meeting in 2011. Dr. Foo’s passion for innovation led her to the MIT-Harvard Medical School Healthcare Innovation Bootcamp in 2019, where her team was runner-up in the elevator pitch competition. She also completed the Eureka-Singapore Monsoon School on Translational Medicine. As SNEC’s first Myopia Fellow, Dr. Foo is dedicated to addressing the myopia epidemic through innovative solutions. With a vision to enhance clinical care, she strives to develop novel tools and treatments, bridging gaps in ophthalmology and improving patient outcomes.
drfoolilian@gmail.com
With over 20 years of experience in the optometry field, Dr. Glenda AlemanMoheeputh is a vision expert. She graduated from Nova Southeastern University in Florida, USA, with a Bachelor of Science degree in Vision Science. She went on to receive her Doctor of Optometry degree from NSU’s College of Optometry in which she led the class of 2017 as vice president. Dr. Aleman-Moheeputh is certified to practice optometry in Florida with a certification in orthokeratology and scleral lens fitting specializing in Paragon CRT, Contex OK lens, GOV Ortho-K lens, Euclid Emerald lens, Europa lens, and Zen lens. She currently serves as the president of the American Academy of Myopia Control and Orthokeratology (AAOMC) South Florida Chapter. She also holds the position of lead ambassador for the Optometry Divas Miami Chapter and acts on the Chair Advisory Committee of the Broward College Opticianry program. Presently, Dr. Aleman-Moheeputh is an acting optometrist and business owner, managing her own private practice, iSmart Vision Care. She performs comprehensive eye exams, specializes in treating corneal disease and myopia control, and has a specialty contact lens clinic. In her mission to stop the myopia epidemic, Dr. Aleman-Moheeputh has recently launched her new venture, OK Love Myopia Control Experts (www.orthoklove.com), designed to educate and consult fellow optometrists about myopia control treatments.
gmoheep@gmail.com

by Hazlin Hassan
For decades, Malaysian optometry has sought formal recognition aligned with global standards, a pivotal step now closer to reality with the upcoming Optometry Bill. This longawaited legislation promises to redefine the profession's scope, introduce subspecialties and tackle the pressing shortage of qualified eye care professionals nationwide.

Malaysia’s Health Ministry will table the long-awaited Optometry Bill in Parliament in October this year, a move aimed at strengthening professional standards, which experts hope will expand access to qualified eye care across the country.*
Photo: Kolomiyets Viktoriya/Shutterstock.com
The proposed law aims to elevate optometry into a fullyregulated healthcare profession, enhance public safety and improve early detection of eyerelated complications from noncommunicable diseases (NCDs).
Health Minister Datuk Seri Dr. Dzulkefly Ahmad described the Bill as a ‘stand-alone Act’ that will govern training, registration, practice and scope of duties for optometrists— distinct from opticians. It also seeks to regulate the online sale of optical products, a long-standing concern among eye care professionals.
“This legislation is crucial in elevating optometry as a recognized, qualified, safe and effective professional field,” Dr. Dzulkefly said after launching the Primary Eye Care Service Guidelines for the Optometry Profession on June 17.
Malaysia, with a population of about 35 million, has only one optometrist for every 16,000 residents. This is well below the World Health Organization’s recommended ratio of 1:10,000. Dr. Dzulkefly noted that the country only produces about 200 optometrists annually, a number far short of what is needed to meet growing demand, especially in underserved areas.
For Prof. Dr. Bariah Mohd Ali, a professor in Optometry and Vision Science at the National University of Malaysia, the Optometry Bill marks a long-overdue update to an outdated legislation. The current Optical Act of 1991 took effect in 1994 when only some 200 optometrists practiced nationwide. As such, it no longer reflects the realities of a profession that now numbers over 3,000 registered practitioners.
“Only by updating the Act can Malaysia guarantee high-quality, standardized and accessible eye care,” said Dr. Bariah, who also serves as president of the Malaysian Academy of Optometry. The new law is expected to formally recognize optometrists as primary eye care providers, a role that has long been under-acknowledged.
The Bill will also introduce regulations around subspecialties in optometry, such as low vision and binocular vision, as well as the optometrist’s role in screening ocular diseases.

This shift will require a revamp of optometry education, with undergraduate training incorporating more advanced instruments and technologies, and postgraduate pathways offering enhanced curricula and clinical training to meet evolving demands.
“Only by updating the Act can Malaysia guarantee high-quality, standardized and accessible eye care.”
- Prof. Dr. Bariah Mohd Ali
Dr. Bariah is optimistic that by enhancing professional recognition and expanding subspecialty opportunities, the Bill will also attract more students to the field.
“This will help Malaysia move closer to the WHO-recommended ratio in the near future,” she said.
Despite progress in urban areas, eye care remains patchy in rural Malaysia. Nearly half of optical outlets in rural areas operate without qualified optometrists, according to Dr. Bariah. This opens the door to incorrect prescriptions and missed diagnoses of serious ocular diseases.
Mr. Muhammad Syimir Shahrul Izam, a practicing optometrist and founder of Quest Eyecare, Malaysia, described the pending legislation as “a significant and long-overdue step forward” for the profession and for public health. However, he warned that the law would be ineffective without strong enforcement mechanisms.
“One of my concerns is that despite the legislation, many optical shops will continue to operate without qualified optometrists, allowing unlicensed individuals to perform eye examinations,” he said. “People may assume all ‘eye tests’ are the same, regardless of who performs them.”
He also raised an alarm over the unregulated sale of spectacles and
contact lenses, both online and over the counter, without professional advice. “Contact lenses are medical devices,” he pointed out, adding that improper fittings and lack of followup care can lead to infections and serious complications.
Mr. Muhammad Syimir, who previously practiced in the UK, noted the stark difference in regulatory oversight there. “Only qualified and registered professionals are allowed to perform eye examinations or prescribe corrective devices,” he added.
“One of my concerns is that despite the legislation, many optical shops will continue to operate without qualified optometrists, allowing unlicensed individuals to perform eye examinations,”
- Mr. Muhammad Syimir Shahrul Izam
Beyond regulation, the Health Minister flagged the issue of affordability. The cost of eye care, including cataract surgeries, prescription lenses and screenings, can sometimes be a burden for patients, disproportionately affecting low-income and rural communities.
Dr. Dzulkefly called for a sustainable and progressive financing mechanism to ensure equitable access to care.
Malaysia is not alone in grappling with optometry’s regulatory lag. In the Philippines, there are only about 4,000 optometrists for a population of around 115 million. Increasing student intake in optometry schools is one way this challenge is being addressed.
Dr. Carmen Abesamis-Dichoso, a leader in Philippine Optometry and the chair of PODs Learning and Development Team, who also served in the World Council of Optometry, Legislation, Regulation and Standards Committee, reported that the Philippines is establishing its first state-run optometry program at the University of the Philippines. Expected to open in 2026, it will utilize global competency frameworks from the World Health Organization and World Council of Optometry.
According to Dr. Abesamis-Dichoso, the move was a step in the right direction. “This will ensure that eye care is accessible, affordable and of high quality,” she said.
However, she stressed that training more optometrists must go hand in hand with policies to ensure they are equitably distributed.
“There must be incentives for wider dispersion of optometrists,” she said, suggesting that governmentsponsored optometry graduates serve in underserved areas for a number of years after obtaining their licence.
She added that changes to professional regulation must be institutionalized through legislation.

She also expressed hope that regulatory agencies would take the lead in enforcing laws, including those prohibiting the online sale of ophthalmic products without proper optometrist guidance.

Prof. Dr. Bariah Mohd Ali is a professor in Optometry and Vision Science at the National University of Malaysia and president of the Malaysian Academy of Optometry. She received her Bachelor’s degree in Optometry from the National University of Malaysia and her Ph.D. from The University of New South Wales, Australia. She was fundamental in the development of a specialty contact lens clinic, which now acts as a referral and training clinic for postgraduate and undergraduate students. She is actively involved in research, with interests in specialty contact lenses and myopia control and has published and presented her research findings locally and internationally. In recognition of her expertise in the area of contact lenses, she was admitted as a Fellow by the Association of Malaysian Optometrist (FAMO) in 2008, British Contact Lens Association (FBCLA) in 2012, Malaysia Academy of Optometry (FAOM) in 2019, and is the recipient of the prestigious IACLE Contact Lens Educator Award for the Asia Pacific region in 2020. Prof. Dr. Bariah is a strong advocate for continuous professional development in the optometry profession. She was elected as a council member in the Malaysian Optical Council (MOC) from 2020-2022 and was instrumental in the development of Malaysian Academy of Optometry (PAOM) in 2018. She is currently the president of PAOM and is actively involved in planning, organizing and delivering seminars for local and international optometrists. In recognition of her leadership contributions to the optometry profession, she was elected as a Fellow by the American Academy of Optometry (FAAO) in 2019. bariah@ukm.edu.my
Experts feel that passing the Bill is only the beginning. Mr. Muhammad Syimir stressed that public education campaigns must be followed to help Malaysians understand the difference between optometrists, opticians and unlicensed practitioners.
“Without clear public education and proper enforcement, many might question the purpose of the Bill or, worse, diminish the value of the optometry profession altogether. It could reinforce the harmful idea that ‘anyone can do it’ or that our role is easily replaceable,” he warned.
Robust enforcement will also be key. This includes licensing checks and audits for optical outlets, penalties for

Dr. Carmen AbesamisDichoso earned her Doctor of Optometry in 1989 and her Master of Arts in Teaching in 2001 from the Central Colleges of the Philippines. She specializes in special contact lens design for keratoconus, children and high astigmatism, and visual assessment for individuals with mental challenges, autism, ADHD, cerebral palsy and learning disabilities. Practicing orthokeratology since 2005, she has had a private practice at Medical Plaza Makati since 1998. She was named Outstanding Optometrist of the Year in 2017 by the Optometric Association of the Philippines. Currently, she chairs the International Affairs Committee of the Optometric Association of the Philippines and holds roles such as director of Special Olympics Opening Eyes in the Philippines and program manager of the Vision Screening Program. Dr. AbesamisDichoso is a fellow of the American Academy of Optometry, a founding fellow of the Philippine College of Optometrists, a fellow of the International Association of Contact Lens Educators and holds positions with the Asia-Pacific Council of Optometry. carmen.dichoso@gmail.com
violations and easy channels for the public to report malpractice.
With Malaysia’s aging population and rising rates of diabetes and other chronic illnesses, the role of optometrists in early disease detection is becoming increasingly urgent. By enacting the Optometry Bill, the government hopes to empower a new generation of frontline eye care professionals: those who can spot complications before they become irreversible.
“The Bill should represent more than regulation,” said Mr. Muhammad Syimir. “It stands for professional integrity, patient safety and the elevation of eye care standards in Malaysia.”
Reference
* Bernama. Optometry Bill to be Tabled in October - Dzulkefly. Available at https://www. bernama.com/en/news.php?id=2435024. Accessed on July 10, 2025.

Mr. Muhammad Syimir Shahrul Izam is a graduate of the University of Bradford, UK, with a BSc (Hons) in optometry and has been practicing for almost 10 years. After training at Specsavers, UK, for two years, he returned to Malaysia. He has worked as a full-time clinician and chief optometrist at Thomson Hospital, attending to pediatric patients. He is trained in assessing children with cerebral visual impairment. In 2024, he underwent a clinical attachment with a vitreoretinal surgeon and was awarded the Professional Certificate in Macular Disease Counselling by the National University of Malaysia. A member of the Association of Malaysian Optometrists, Mr. Muhammad Syimir recently established Quest Eyecare, his own primary eyecare practice. He is passionate about eye care in children, providing and promoting myopia management.
syimir_shahrul@yahoo.com
TRYPTYR (acoltremon ophthalmic solution 0.003%) stimulates tear production via TRPM8 activation and is now available in the U.S.
An intriguing novel mechanism of action is coming to the American dry eye landscape.
On Tuesday, Alcon (Texas, United States) announced the U.S. commercial launch of TRYPTYR (acoltremon ophthalmic solution 0.003%). The news release comes just a few months after the drug’s FDA approval in May for the treatment of dry eye disease (DED).
The launch expands available treatment options for the estimated 38 million U.S. adults affected by dry eye disease.
“TRYPTYR is highly anticipated in the DED treatment space as the first neuromodulator eye drop to rapidly increase natural tear production,” said Lisa Praeger, vice president and general manager of U.S. Ocular Health Pharmaceuticals at Alcon.
“We’re committed to making this option available to eye care professionals and patients seeking new approaches to DED management.”
How does TRYPTYR work?
TRYPTYR’s new approach has intriguing potential.
As a first-in-class transient receptor potential melastatin 8 (TRPM8) receptor agonist, TRYPTYR stimulates corneal sensory nerves to enhance basal tear production. Alcon claims that this addresses potential underlying tear deficiencies, rather than solely managing symptoms.
The targeted TRPM8 receptors are cold-sensing thermoreceptors on the ocular surface which activate trigeminal nerve signaling to boost natural tear production. This neuromodulatory approach contrasts with existing treatments that aim to reduce ocular inflammation.
The evidence behind the approval
FDA approval was supported by two Phase III trials, COMET-2 and COMET-3, which enrolled more than 930 patients with DED.
Participants were randomized 1:1 to receive TRYPTYR or vehicle control, one drop per eye two times daily for 90 days. The primary endpoint, a ≥10 mm increase in unanesthetized Schirmer’s score by Day 14, was achieved by 42.6% of TRYPTYR patients in COMET-2 (vs. 8.2% for vehicle) and 53.2% in COMET-3 (vs. 14.4%), with p < 0.0001 in both studies.
While current therapies often require weeks to achieve clinical benefit, TRYPTYR demonstrated increases in tear production as early as Day 1 in the COMET-2 and COMET-3 clinical trials.
These tear production improvements were sustained through Day 90, with no serious ocular adverse events reported. The most common side effect was mild, transient instillation site pain, affecting approximately 50% of patients.
TRYPTYR is available in preservative-free, single-dose vials, with a recommended dosing of one drop per eye, two times daily. Alcon is offering initial patient support through a First Fill Free trial and copay assistance via BlinkRx, with home delivery for eligible patients.
Thought leaders in the space have since spoken on what this could mean for clinical practice in approved areas.
“TRYPTYR represents an important milestone in the treatment of dry eye disease,” said Dr. Preeya Gupta (United States). “Alcon is also supporting clinicians with educational resources to help integrate new treatments like TRYPTYR into practice.”
With only 13% of surveyed DED patients reporting adequate symptom control and the market projected to reach $9.85 billion by 2028, this rapid-onset, first-in-class therapy could help fill a major treatment gap.
For now, TRYPTYR offers a refreshing option. One that promises to leave both patients and prescribers with a little more sparkle in their eyes.
Editor’s Note:
