




When you’re over age 45, there’s a moment you realize you’re not immortal like you thought, and that your health isn’t on autopilot. That’s when you should talk to CHI Saint Joseph Health about the health of your heart. If you have an ongoing heart condition or suspect that there might be an issue on the horizon, we can help you keep doing the things in life that really matter.

Learn more about your heart health and your risk for developing heart disease by answering a few questions with our free online Heart Health Risk Assessment and visit CHISaintJosephHealth.org/HeartHealth.
Scan for your Heart Health Risk Assessment

ISSUE #145 (April)
INTERNAL SYSTEMS
Endocrinology, Gastroenterology, Geriatrics, Internal Medicine, Integrative & Regenerative Medicine, Infectious Diseases, Lifestyle Medicine, Nephrology, Urology, Wound Care
ISSUE #146 (June)





WOMEN’S & CHILDREN’S HEALTH
OB/GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology,















ISSUE #147 (September)
MUSCULOSKELETAL HEALTH
Orthopedics, Sports Medicine, Physical Medicine & Rehabilitation, PT/OT





ISSUE #148 (October)
CANCER CARE
Oncology, Plastic Surgery, Hematology, Radiation, Radiology




















ISSUE #149 (December)
IT’S ALL IN YOUR HEAD
Neurology, Neuroscience, Ophthalmology, Pain Medicine, ENT, Psychiatry, Mental Health
Editorial topics and dates are subject to change
It is a tumultuous time in Kentucky healthcare for our doctors.
The AMA and 118 other medical societies agree with the results of a survey conducted by the Kentucky Medical Association that prior authorization is an obstacle to delivering quality healthcare. The KMA’s survey tallied 81% of the respondents who said “prior authorization sometimes, often, or always delayed access to care.”

I am interested in hearing from the 19% of respondents who don’t find prior authorization a problem. I would like to do a story on how they deal with the issue to share with our readers. Maybe they all practice elective medical specialties.
On page 5 in this issue, Eric Riley of Dean Dorton Healthcare Solutions gives us a synopsis of the new CMS rule outlining prior authorization pathways on services rendered by physicians. I invite you to read Eric’s column.
On February 16, 2023, the Kentucky Supreme Court ruled that the state’s near total bans on abortion will remain in place while lawsuits continue. A bill, HB 300, was introduced into the Kentucky Legislature by Rep. Emily Callaway (R-37) who represents parts of Louisville and Bullitt County. Callaway’s bill, if passed, could result in a pregnant woman, who had an abortion, being charged with homicide.
I invite any Kentuckiana physician who wants to state their opinion, on either side of the abortion issue, to contact me for possible publication of their view.
Sometime in the next four to six months, the KY Supreme Court will rule on two lawsuits that involve the Certificate of Merit statue and the effects it has on medical malpractice lawsuits. Our legal columnist, Andrew DeSimone, of Sturgill, Turner, Barker & Moloney, shares his insights that the court’s rulings will have on page 8.
I hope you enjoy reading the Lifewise by Dr. Jan columns as much as I do. She constantly surprises me with her topics, insights into human behaviors, helpful strategies, and humor. This issue’s column is one to put on the refrigerator, if anyone still does that sort of thing. She tells us how to live with someone who’s politics are the opposite of yours. Check it out on page 24.
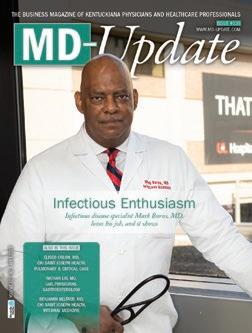
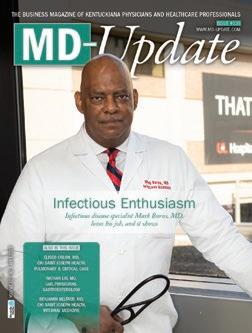
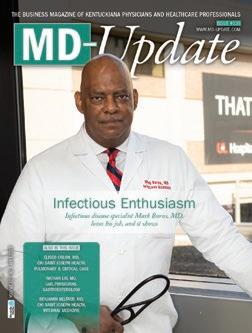
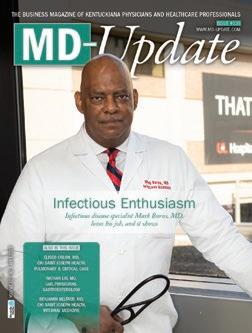
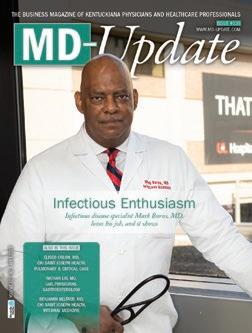
It’s a target rich environment if you practice cardiology in Kentuckiana. I feel honored to be able to share in this issue of MD-Update, some stories of the women and men who care for the hearts of their patients, starting with our cover story on page 10.
Look for your specialty among the topics on the MD-Update editorial calendar on the preceeding page. When you see it, give me a call. I am sure that you have a good story to tell.
MD-UPDATE
MD-Update.com
Volume 13, Number 1
ISSUE #144
EDITOR/PUBLISHER
Gil Dunn gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda Debord
CONTRIBUTORS:
Jan Anderson, PSyD, LPCC
Ellen Cartmell, MPA
Scott Neal, CPA, CFP
Eric riley
Heather Shaw, NCTIP Andrew D. DeSimone, Esq.
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com

Mentelle Media, LLC

38 Mentelle Park Lexington Ky 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky.
Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington Ky 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2023 Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you.
Individual copies of MD-Update are available for $9.95.







During February — American Heart Month — the American Heart Association, the leading voluntary health organization devoted to a world of longer, healthier lives for all, is urging at least one person in every household to “Be the Beat” by committing to learning hands-only CPR.
Cardiovascular disease remains the leading cause of the death in both Kentucky and the United States. According to the American Heart Association, more than 350,000 out-of-hospital cardiac arrests occur in the United States each year.

“About 90 percent of people who suffer out-of-hospital cardiac arrests die,” Ashley Sokoler, executive director of the American Heart Association in Kentuckiana says. “The results of CPR, especially if performed immediately, are staggering. In fact, it can double, or even triple, a cardiac arrest victim’s chance of survival.”
Hesitancy to perform CPR is often due to a perceived lack of training or knowledge. Approximately three in ten people are unfamiliar with the Good Samaritan Laws that exist to protect those acting in good faith, are concerned about hurting someone, or are afraid of legal consequences. However, because about 70% of cardiac arrests happen at home, it’s most likely that the person who needs CPR will be someone you know.
“If you are called on to give CPR in an emergency, you will most likely be trying to save the life of a loved one, whether it be
a spouse, a parent, grandparent, child, or friend,” says Andrea Ooten, executive director of the American Heart Association in Central and Eastern Kentucky. “You don’t have to be CPR-certified to save a life, which is why we are calling on all Kentuckians to be prepared for a cardiac emergency by learning the two easy steps to perform hands-only CPR.”
Hands-only CPR involves two simple steps, and anyone can learn it from a 60-second video available at heart.org/handsonlycpr.
Step 1: If a teen or adult in your home suddenly collapses, call 911 immediately.
Step 2: Place one hand on top of the other as shown in the video and push hard and fast on the victim’s chest.
According to the American Heart Association, people also feel more confident performing hands-only CPR and are more likely to remember the correct rate when trained to the beat of a familiar song. The beat of songs like “Stayin’ Alive,” by the Bee Gees, “Crazy in Love,” by Beyoncé, and “Walk the Line,” by Johnny Cash are all 100 – 120 beats per minute, the same rate at which rescuers should perform compressions when administering CPR, which means they can “Be the Beat” to save a life.
 BY ERIC RILEY
BY ERIC RILEY
On December 6th, CMS released the proposed rule outlining systematized prior authorization pathways for healthcare services rendered by providers and hospitals. The proposed rule outlines the goals to improve the prior authorization process and drive more transparency and efficiency to all stakeholders involved including payers, providers, vendors, and patients. Current prior authorization processes have created burden on payers and providers and is a major source of burnout for providers, thereby possibly impacting the health inefficiencies of patients in the potential delay of care
The burden of prior authorization has been well documented in the American Medical Association (AMA) Study released in December 2021. The study indicated not only had there not been an increase in prior authorization efficiency, it had actually become worse.1 The study outlined the operational time, human capital, and lack of technology impacts that negatively affect the efficient delivery of care.1 Furthermore, physicians reported that most prior authorizations are completed via phone calls and faxes, with only 26 percent reporting
that they have access to an EHR system that supports electronic prior authorization for prescription medication.2
The proposal currently outlines requirements that would be applied to payers:
• Build and maintain a Prior Authorization Requirements, Documentation, and Decision (PARDD) API to automate the process for providers to determine whether a prior authorization is required, identify prior authorization information and documentation requirements, and facilitate the exchange of prior authorization requests and decisions from providers’ electronic health records (EHRs) or practice management systems
• Include a specific reason when they deny a prior authorization request


• Send prior authorization decisions within 72 hours for expedited (urgent) requests and seven calendar days for standard (non-urgent) requests
• Publicly report certain prior authorization metrics annually by posting them on their website or through publicly accessible hyperlinks3
CMS is seeking comment related to the proposal, including alternative time frames for prior authorization decisions. Comments on the rules are to be received March 13, 2023.

Remember 2019? Congress passed a huge piece of legislation called the Setting Every Community Up for Retirement Enhancement Act of 2019. It became known as the SECURE Act. It included a provision that raised the requirement for mandatory distributions from retirement accounts and increased access to retirement accounts.
Now, just three years later, another massive ($1.7 trillion) spending bill contains many changes to our retirement laws. It has been called SECURE ACT 2.0 and is designed to encourage Americans to save for retirement. It is long overdue in my opinion, and gives recognition that Americans are living and working longer than ever before. The impact on savings will be biggest on our younger readers, but there are plenty of changes that will impact even those who are already retired, or about to be.
This new law has plenty of provisions that impact you as an employer if you are in private practice and have employees.
1. Changing the age of the required minimum distributions (RMD). Three years ago, SECURE 1.0 increased the age for taking the required minimum distribution (RMD) to 72 years from 70½. If you turn 72 in 2023, the age required for taking your RMD rises to 73. If you turned 72 in 2022, you’ll remain on the old schedule.
For those who turn 72 in 2023, you may delay your RMD until 2024, when you turn 73. Or you may choose to take your first RMD to as late as April 1, 2025. Just be aware that you will be required to take two RMDs in 2025, one no later than April 1 and the second no later than December 31. Tax projections covering several years are made more beneficial because
of these changes. Your advisor can help you with these. Starting in 2033, the age for the RMD will rise to 75.
Employees enrolled in a Roth 401(k) will not be required to take RMDs from their Roth 401(k). That begins in 2024.
2. RMD penalty relief. Beginning this year, the penalty for missing an RMD is reduced to 25% from 50%. And SECURE 2.0 goes one step further. If the RMD that was missed is taken in a timely manner and the IRA account holder files an amended tax return, the penalty is reduced to 10%. But just to be clear, while the penalty has been reduced, you’ll still pay a penalty for missing your RMD. Pay attention.
3. A shot in the arm for employer-sponsored plans. Congress felt that too many Americans do not have access to employer plans or simply don’t participate. So, starting in 2025, companies that set up new 401(k) or 403(b) plans will be required to automatically enroll employees at a contribution rate between 3% and 10% of their salary. Employees may opt out of the employer-sponsored plan. To encourage employees to sign up, employers will be allowed to offer gift cards or small cash payments.
The new legislation also allows for automatic portability, which will encourage folks in low-balance plans to transfer their retirement account to a new employer-

sponsored account rather than cash out.
4. Increased catchup provisions. In 2025, SECURE 2.0 increases the catch-up provision for those between 60 and 63 from $6,500 in 2022 ($7,500 in 2023 if 50 or older) to $10,000, (the greater of $10,000 or 50% more than the regular catch-up amount). Furthermore, the amount is indexed to inflation. One caveat — catch-up dollars are required to be made into a Roth IRA unless your wages are under $145,000.
5. Charitable contributions. Starting in 2023, SECURE 2.0 allows a one-time, $50,000 distribution to charities through charitable gift annuities, charitable remainder unitrusts, and charitable remainder annuity trusts. One must be 70½ or older to take advantage of this provision. The $50,000 limit counts toward the year’s RMD. It also indexes an annual IRA charitable distribution limit of $100,000, known as a qualified charitable distribution, or QCD, beginning in 2023.

6. Back-door student loan relief. Starting next year, employers are allowed to match student loan payments made by their employees. The employer’s match must be directed into a retirement account, but it is an added incentive to sock away funds for retirement.
7. Disaster relief. You may withdraw up to $22,000 penalty-free from an IRA or an employer-sponsored plan for federally declared disasters. Withdrawals can be repaid to the retirement account.
8. Help for survivors. Victims of abuse may need funds for various reasons, including cash to extricate themselves from a difficult situation. SECURE 2.0 allows a victim of domestic violence to withdraw the lesser of
Many Americans lack adequate savings, and SECURE 2.0 helps address some of the challenges for many in planning for retirement.
50% of an account or $10,000, penalty-free.
9. Rollover of 529 plans. Starting in 2024 and subject to annual Roth contribution limits, assets in a 529 plan can be rolled into a Roth IRA, with a maximum lifetime limit of $35,000. The rollover must be in the name of the plan’s beneficiary. The 529 plan must be at least 15 years old. This can be huge for any 529 and should be considered before the 529 is used. In the past, families may have hesitated in
fully funding 529s amid fears the plan could wind up being overfunded and withdrawals would be subject to a penalty. Though there is a $35,000 cap, the provision helps alleviate some of these concerns.
Once again, at our firm, we welcome these changes. Many Americans lack adequate savings, and SECURE 2.0 helps address some of the challenges for many in planning for retirement.

What we have provided here is a high-level overview of the SECURE Act 2.0. Keep in mind that it is not all-inclusive. We are always here to assist you, answer your questions, and tailor any advice to your needs. Additionally, you should reach out to your tax advisor for her or his input.
Scott Neal is president of D. Scott Neal, Inc., a fee-only financial planning and investment advisory firm with offices in Lexington and Louisville. He can be reached at 1.800.344.9098 or scott@dsneal.com.

In 2017, in an effort to prevent “frivolous” lawsuits, the Commonwealth of Kentucky’s General Assembly passed the Medical Review Panel Act (MRP). The Act created a panel of healthcare providers to review prospective malpractice lawsuits, ensuring that qualified experts agreed that malpractice likely occurred before allowing a lawsuit to proceed. In 2018, the Kentucky Supreme Court held that this legislation was unconstitutional as it violated the guarantee of open courts provision of the Kentucky Constitution.1

In 2019, the General Assembly passed the Certificate of Merit Statute (KRS 411.167), which requires the plaintiff at the outset of the litigation to certify that that the matter has been reviewed by a qualified expert, and that after examining that review, the claimant has decided that there is some reasonable basis to allow the lawsuit to proceed. Like the MRP, the Certificate of Merit was an attempt to ensure that a potential claimant obtain an expert review prior to filing a lawsuit. Most medical malpractice claims require an expert to testify that the medical provider erred, and that the error led to a patient’s injury. These necessary elements are defined as (1) breach of the standard of care (what a reasonably competent provider would do under the same or similar circumstance) and (2) causation. Both elements are necessary to succeed under a malpractice claim.
The lack of substantive requirements for the expert review makes it difficult under the statute to effectively gauge whether lawsuits should or should not proceed.

First, the Certificate of Merit statute does not actually require an expert to opine that a defendant medical provider breached the standard of care and caused injury, nor does it provide the opinion be used as expert testimony in court. Instead, it requires at best a cursory analysis by an expert witness, which is not subject to review or validation by anyone other than the claimant.
Second, even if multiple specialties are involved, the claimant must only consult with one expert in any field; for example, a neurosurgeon could opine about the care provided by a radiologist.
Third, the consulting expert does not even have to believe that the providers breached the standard of care; instead, the claimant must only believe the lawsuit has a reasonable basis to proceed. “The claimant has reviewed the facts of the case and has consulted with at least one (1) expert . . . and has concluded on the basis of review and consultation that there is a reasonable basis to commence the action.” Therefore, under this plain language, it is sufficient if only the claimant believes that the lawsuit should proceed, not whether there is sufficient expert proof to support the lawsuit.
The Certificate of Merit statute itself also has numerous exceptions, including filing a claim that does not require expert proof, i.e., a retained sponge, or the inability to obtain the necessary medical records for a review in a timely fashion. However, the courts have generally determined that the Certificate of Merit is required to be filed with the complaint. If it is not attached at the outset, then the complaint should be dismissed.
Enough time has passed since the statute was enacted for the appellate courts in the
There are currently two opinions pending before the Kentucky Supreme Court that may alter the effectiveness of the Certificate of Merit Statute in weaning out frivolous lawsuits.
Commonwealth of Kentucky to provide guidance on it. In a federal case styled Dumphord v. Gabriel, Federal Judge Danny Reeves dismissed the medical negligence claim against the defendant hospital because the plaintiff failed to attach the required Certificate of Merit. In Judge Reeves’ opinion, the Certificate of Merit Statute required either the certificate of merit be attached to the complaint or expert information be provided at the time of filing of the complaint. Without this necessary information, the lawsuit cannot proceed. A similar result was reached in a Kentucky Court of Appeals’ opinion, Evans v. Baptist Health Madisonville, where the Court of Appeals found that the failure to attach the Certificate of Merit required dismissal of the lawsuit.
However, there are currently two opinions pending before the Kentucky Supreme Court (the highest court in the Commonwealth of Kentucky) that may alter the effectiveness of the Certificate of Merit Statute in weaning out frivolous lawsuits. Moreover, with the departure of Senator Ralph Alvarado, MD, from the General Assembly, it is unknown if further legislative attempts to shield medical providers from a lawsuit will be forthcoming.
The two opinions being actively litigated before the Kentucky Supreme Court are Sanchez v. McMillin and McWhorter v. Baptist Healthcare System, Inc. The issue in both cases is whether a motion can be filed shortly after the complaint, asking the trial court to allow additional time to file the Certificate of Merit. In McWhorter, the Court of Appeals affirmed the lower court’s decision dismissing the medical negligence claim because the plaintiff failed to attach the required Certificate of Merit. In Sanchez, the Court of Appeals determined that a litigant could file a motion, and the trial
court would have the discretion to allow the late filing, as long as the litigant could show “excusable neglect.” That could include being unable to find a relevant expert, or their expert not completing a timely review. Quite possibly, the Certificate of Merit decisions will only have an effect upon pro se litigants (plaintiffs without an attorney), as they will likely find it difficult to navigate these claims and provide the certificate required without being allowed the late filing option.
We expect the Supreme Court will rule on this issue in the next four to six months, offer-
ing the definitive opinion on whether further exceptions are allowed for litigants to meet the requirements of the statute. This should not make a major difference in the number of malpractice lawsuits, but it could have an effect on the number of cases dismissed early in the proceedings.
Andrew D. DeSimone is a medical malpractice defense attorney with Sturgill, Turner, Barker & Moloney, PLLC, and chair of the firm’s healthcare law practice group. He can be reached at adesimone@ sturgillturner.com or 859.255.8581. This article is intended to be a summary of state or federal law and does not constitute legal advice.



LOUISVILLE As a specialty, it can be argued cardiology dates all the way back to the 1620s when William Harvey observed and demonstrated blood circulation. The field, however, continues to evolve in fascinating and life-saving ways, as with the emerging subspecialty of cardio-oncology.
Baptist Health Louisville offers one of the few cardio-oncology programs in the nation where cardiologists, oncologists, and radiation oncologists all come together to provide this integrative care to cancer patients. Three key members of the Baptist Health team are cardiologists Mini K. Das, MD; Rebecca McFarland, MD; and Jamie Kemp, MD.
The role of cardio-oncology is to identify, assess, monitor, and treat any conditions of the heart that may occur as a result of chemotherapy, immunotherapy, or radiation therapy. These conditions include pericarditis, arrhythmias, coronary artery disease, valvular damage, hyper- and hypotension, and overall heart failure.
According to Das, “We are trying to attack this from a multidisciplinary process, both from cardiology and oncology, because you don’t want to just treat the heart and not treat the tumor and vice versa.”
Das comes from a family of physicians. Her father is an internist, her mother a psychiatrist; one sister is a pediatrician, and the other a cardiologist. She attended medical school at University of Alabama School of Medicine in Birmingham, then completed both her residency and fellowship at Mayo Clinic College of Medicine and Science in Rochester, Minnesota. Following, she served on staff at Mayo Clinic prior to entering private practice in Tennessee before joining Baptist Health where she has been for almost 20 years.
Over the past decade, the medical community has realized and addressed the need of
hand-in-hand cardiac care and cancer treatment. Thus, the subspecialty of cardio-oncology emerged.
McFarland explains, “There are certain chemotherapeutic agents and types of radiation protocols which increase cardiovascular risk. The patients receiving those therapies are referred into cardio-oncology. We also evaluate patients who have cardiac risks or known cardiovascular disease and are entering into chemotherapeutic regimens that require additional monitoring of their cardiac pathology.”

McFarland received her medical degree from the University of Toledo in Ohio and remained at the University of Toledo Health Science Campus for her residency and fellowship.
One might assume it is only the treatments for cancer of the chest area, such lung as breast, that carry risk, but this is a misconception. Despite the type of cancer, there is usually some risk of cardiac side effects from treatment. As Kemp points out: “Over time, some — but not all — breast cancer treatments can increase the risk of congestive heart failure, weakness of the heart muscle, coronary artery disease, strokes, and high blood pressure. Rapidly developing treatments for other types of cancer, including some lung
cancers, some blood cancers, and kidney cancer, have also been identified as potentially leading to increased risk as well. Additionally, some radiation treatments may incur cardiac risk over time.”
After graduating from the Washington University School of Medicine, Kemp did her residency and internship at Warren Alpert Medical School of Brown University in Rhode Island. She followed up with a fellowship at the University of Louisville School of Medicine and Department of Cardiology.
McFarland adds, “Oncology has made so many advances offering effective targeted therapy for cancer, but some chemotherapeutic regimens affect other organ systems. Patients are referred to us based on the planned oncologic therapy and their history of cardiac disease and risk factors. Referrals are usually not based on the type of cancer.”
For patients entering or undergoing cancer treatments, the physicians perform a comprehensive cardio-vascular disease assessment beginning with a thorough medical history to gauge risk factors along with a physical exam. The next step is often an echocardiogram with strain imaging to evaluate heart function. Blood work to detect biomarkers is also common. In addition, the doctors may utilize a traditional stress test, chest x-ray, or MRI. Many of the risk factors for the development of cardiac side effects are predictable, as they are common comorbidities. These include high blood pressure, diabetes, elevated cholesterol, obesity, prior heart abnormalities/disease, and a family history of coronary disease. Das reiterates: “We know that people who have diabetes, have high cholesterol, have high blood pressure, are sedentary, who smoke, who are overweight, and who already have underlying heart disease are going to be at much higher risk for having a complication. So, those are the people that we really focus on. You want to make sure they are followed closely.”
Specific oncology drugs also have higher instances of being linked to heart disease. Among these are anthracycline drugs, such as doxorubicin (Adriamycin), trastuzumab (Herceptin®), cyclophosphamide (Cytoxan®), fluorouracil (5-FU), and mitoxantrone (Novantrone®), along with others.
A two-pronged treatment regimen also garners greater risk. “If you have a patient that’s had chemo and radiation, they are the highest risk, because they have already had one potential insult and now require another. They are considered the higher risk population,” says Das.
However, it can still be difficult to predict exactly who develops cardiac complications. Das explains, “To what degree cardiac complications occur is interesting because not everybody has the same risk. In addition, not every drug has the same risk profile. Some are very dose dependent. However, many are not and are more dependent on the receptors they target which are present on the tumor but can also be present in the heat and vascular system, which then leads to some bleed over negative effects to the heart and vascular system thus leading to toxicity.”
To offset the unpredictability, the European Society of Cardiology recently released new guidelines for assessing risk based on a combination of factors and organizing them by specific drugs, which had not been done previously. Based on which drugs patients have been administered in conjunction with age, gender, and the risk factors previously mentioned, patients are given a ranking of low, intermediate, high, or very high risk. This risk determines baseline testing, frequency of evaluation, and subsequent cardiac treatment.
As is often the case, Das expects the American College of Cardiology will follow the Europeans’ lead and adopt the latest guidelines or a version of this in the future.
Once risk has been established, a treatment protocol is put in place. “If we see changes from their baseline, we start to understand that that person is starting to have some negative effect, and we try to incorporate heart failure medicines. Hopefully with subsequent improvement
in cardiac function we do not have to stop the drugs that fight the tumor so they can complete their treatment for the cancer,” Das explains. “At the end of it, the goal is the heart will stay strong, so that down the road, we can potentially deregulate the meds. At the end of the day, we have cured the tumor without sacrificing the heart.”
Flexibility, balance, and cooperation are key when it comes to treating cardio-oncology patients. McFarland states, “It is challenging as chemotherapeutic treatment plans can be fluid with frequent changes. Patients’ therapies, the dosage of the therapy, the timing of the therapy, all change depending upon patient tolerance of the cancer treatment and response of the cancer to the treatment.”
She continues, “It’s a balance of what is important for their cardiac issues as well as their oncologic issues. For cardiologists treating oncology patients, it is important that we maintain flexibility and timeliness with visits and testing, to ensure that we are not delaying what is an important therapy for that cancer.” Ensuring the patient comes through “as healthy as possible requires constant communication between radiation oncology, medical oncology, surgery, and the cardio-oncology teams,” says McFarland.
For their work in the field, Baptist Health’s cardio-oncology department has been named a Global Center of Excellence by the International Cardio-Oncology Society. There are only 29 facilities in the country and 40 worldwide who have garnered this distinction. Of the achievement, Das says, “We’re very systematic and organized. We have very caring, dedicated, knowledgeable staff and we have had a lot of support from administration. We’re the first one in the state to get accreditation from the International Cardio-Oncology Society. We are humbled to be charged with this task.”
The department’s greatest achievement is positive patient outcomes. McFarland states, “We want them to beat the cancer, but we don’t want them to have survived the cancer only to then suffer significant morbidity or mortality due to cardiac disease. So, the best of all worlds is to closely follow these patients, to initiate early effective therapy from a cardiac perspective that allows them to survive the cancer and also survive any cardiac pathology that could arise as well.”
Das notices that patients, who have been consumed with their cancer diagnosis and treatment, find hope in the fact that the team is focused on their overall health and quality life after cancer. She gleans satisfaction in making certain that her patients know they are not just identified as a tumor and helping them look forward to a future beyond.

Kemp echoes this sentiment: “I love providing cardiac care for our oncology patients and working with that team. Knowing that we can help our patients live longer, healthier lives is very fulfilling.”

“Knowingthat we can help our patients live longer, healthier lives is very fulfilling.” – Jamie Kemp, MD
“It’s a balance of what is important for their cardiac issues as well as their oncologic issues.” – Rebecca McFarland, MDPHOTOGRAPHY BY ALEXANDRA ROGERS

LEXINGTON The collegial culture and institutional values at CHI Saint Joseph Health in Lexington bring out the best in many healthcare providers. For cardiothoracic surgeon George Dimeling, MD, it lets him ensure that his patients feel known and cared for. He leverages the communication and collaboration of his environment to bring what he calls “boutique treatment” to them. Whether Dimeling is providing lifesaving heart surgery or a more elective, preventative procedure, his approach is the same. “I really customize their medical treatment before and after surgery to their unique situation.”
A Pittsburgh native, Dimeling was inspired early. His interest in cardiac surgery arose when, as a teenager, he witnessed a heart transplant. A serendipitous favor from a neighbor allowed him to shadow the entire process from meeting the patient prior to surgery until the final stitch. The impact was lifelong and inspiring. Dimeling has remained in touch with that surgeon, and he has even kept in contact with the patient.

After receiving his medical degree from Drexel University’s College of Medicine in Philadelphia, Dimeling did an integrated residency program at Stanford University with six years of cardiothoracic surgery training. His first position was in Norfolk, Virginia, where he developed the aortic surgery and mitral valve surgery programs at Sentara Heart Hospital, bringing many innovations from his Stanford program. His use there of TEVARs and the David procedure, the valve-sparing aortic root replacement for an enlarged aortic root wall, and his work in charge of their blood transfusion protocols garnered attention, and Cleveland Clinic recruited his whole team. With the onset of the pandemic, he relocated to Lexington to be closer to his wife’s family.
Dimeling’s weekly routine is similar to most cardiothoracic surgeons, though his approaches can differ. He does an ample amount of bypass surgery, but he prefers to use multiple arterial graphs. He says, “Though 85% of surgeons don’t use these, I believe they are better
for the patient because they last longer and the native blood vessels improve circulation following the surgery.” Dimeling says he is among only a handful of surgeons who choose to never stop the heart when employing a heart bypass machine during surgery. Instead, he employs an aortic pump assist. He says this technique reduces the risk of stroke, blood transfusions, and kidney injury.
Dimeling also treats patients with valvular disease and is trained to perform open or percutaneous valve replacement. Dimeling is also trained in aortic surgery to repair aneurysms and tears in the aorta. He says few facilities offer this, yet patients with connective tissue diseases such as Marfan’s Syndrome often need it. Another of his specialties is mitral valve repair, often an elective surgery that relieves shortness of breath from a lifelong heart murmur, which typically worsens with age. Dimeling considers this a valuable quality of life procedure “because it allows people to have a lifelong issue resolved.” He also welcomes complicated surgical problems such as surgery corrections and aged valve replacement repairs.
“I really customize their medical treatment before and after surgery to their unique situation.”
— George Dimeling, MD, Cardiothoracic Surgeon
Dimeling’s patient population is not what it might have been 40 years ago, he says. “As we learn more about cardiac surgery and coronary disease, we are finding that the traditional populations are changing,” he explains. He sees more women whose impaired heart conditions are being detected earlier, and young people whose drug abuse has strained their hearts. There are now more people in their 70s and 80s who are getting bypass surgery. He explains that “Our ability to support older patients with physical therapy and other types of post-op care allows many older patients to go home in 3–4 days.” He currently has a load of about 175 cases per year, a relatively low number which plays to his strength — and his patients’ benefit.
Dimeling’s schedule, commitments, and work environment have allowed him to develop a patient-centered approach that he calls “boutique treatment.” While this may connote special care for an elite patient population, that is not what it means to Dimeling. He simply treats each patient with 360-degree attention. “I treat the patient as a whole. This starts with building trust. If you take the time to connect with a patient, to really listen to them, the barriers come down. Getting them to trust me, and me to trust them, is very important because of the complicated procedures I am doing,” says Dimeling.
Boutique treatment extends to other needs. He pays careful attention to new medications so he can fine tune patient regimens, and he is an advocate for patient physical fitness.
“Oftentimes I will take them by the arm and walk them around the ward with the nurse or the physical therapist,” he says fondly.
Dimeling sees each patient on his rounds each day, stating, “That is when you get to deliver more doctoring than just cardiac surgery fixes. I deal with a lot of other patient issues.” He gets involved in their post-discharge care and lets patients know their relationship can continue. Each patient hears from him, “Once I have had my hands in your chest, I am always available to you.”
Dimeling has long had his vision for boutique treatment, and CHI Saint Joseph Health has proven to be the fertile ground to make it manifest. There are multiple factors that have enabled this. Foremost is the palpable culture of collegiality, collaboration, and attentiveness among the professionals there. He states that “It is really something I have not experienced in any of the other hospitals I have been in. Physicians talk to each other like they are human beings, and they listen.” Regular meetings across disciplines facilitate this, as do casual lunches together in the hospital dining hall. This plays into his ability to deliver the boutique experience because everyone can weigh in. Dimeling can do what is best for each patient.
Dimeling considers this culture of CHI Saint Joseph Health something of a throwback. The un-anxious pace, attitude, and respect bespeak a commitment to service that Dimeling thinks comes from the nuns who founded and ran Saint Joseph. “I have heard lots of stories about
the nuns, and I love every one of them.” More than anything, he concludes, “It comes from the current culture, a lot of people here feel that this work is a mission.”
Dimeling also discerns a congruity in the values of the patient population. He is encouraged and spurred on by the Central Kentucky family values of support and togetherness. He says, “I have never seen more family and friends in the waiting room and by the patients’ bedsides. It is really special!”
Dimeling’s personal philosophy of care allows him to develop a crucial and highly valued program at CHI Saint Joseph Health. Two components have been with him for a long time. He believes you must stay current and be compassionate, putting yourself in the patient’s shoes. The third is taking form here in Lexington. He summarizes, “Boutique care is key. You must surround each patient with care on either side of surgery; you must think of each patient and their personal and financial capabilities.”
Dimeling knows that CHI Saint Joseph Health is the right place to make that possible. He concludes, “I do feel that there is a sense of mission here.”

For patient referrals contact:
859.278.2334

LOUISVILLE We all have that one thing that really gets our heart pumping, that piques our interest, that gains our undivided attention. For Dinesh Kalra, MD, ironically, that one thing has always been the heart. That is why he is chief of cardiovascular medicine at University of Louisville School of Medicine Division of Cardiology, a part of UofL Health.
Born in India, Kalra attended the All India Institute of Medical Science, the top medical school in India. He was one of 35 medical students selected from approximately 250,000 who took the entrance exam. Even before he enrolled, he knew where he wanted to specialize.
“I knew right from the get go I wanted to be a cardiologist,” says Kalra, who is also the governor elect of the American College of Cardiology, Kentucky Chapter. “I was fascinated by cardiology and especially cardiac imaging. Once I graduated, I looked around to see which programs were doing fantastic work in cardiology. I was very enthusiastic about Baylor College of Medicine in Houston where they were doing fascinating work in echocardiography.”
Kalra was accepted into the residency program at Baylor’s College of Medicine and went on to do a cardiology fellowship there as well, including a year in echocardiography. He continued with an electrophysiology fellowship at the University of Michigan and an advanced cardiac imaging fellowship at WeillCornell New York Presbyterian Hospital. He then worked in Boston and Chicago, where he started the cardiac imaging program at RUSH and built it into a Regional Center of Excellence. The University of Louisville School of Medicine was interested in building a similar program and recruited Kalra, who accepted and moved to Louisville in 2021.
“There was not a cardiac imaging program here,” says Kalra, who also is an endowed
professor of cardiovascular innovations at UofL. “There was not a lipid clinic, despite Kentucky having a lot of problems with lipid and heart disease. They needed those holes to be plugged.”
Kalra began the process of plugging those holes immediately, embracing the goal of raising the quality and depth of care at UofL Health and research at UofL School of Medicine. That has meant taking on a demanding schedule that includes both clinical and academic duties. He sees patients in clinic one day a week and does in-patient rounding and cardiac imaging. He reads the majority of the cardiac CT scans, MRIs, and echocardiograms.
“I do teaching and administration, plus leadership and research,” says Kalra, who is vice chair of quality in the Department of Medicine. “This is a profession where you dedicate yourself to doing whatever it takes to better the lives of people and to help people around you. We have to get the institution to be a Regional Center of Excellence. This is a fantastic opportunity, and it would be sad to waste it.”
Kalra says that being a university health system provides many opportunities to be at the forefront in medical care, research, and technology.

“You can be a fantastic community hospital that is giving state-of-the-art medical care, but you might be lacking on newest scientific innovations,” Kalra says, noting that the Division of Cardiology is participating in about 50 clinical trials. “You have the research component, the teaching component, and the clinical care component. We’re leading the forefront in terms of research and innovation, and that’s possible only because we have all of these three components.”
One of the areas being examined is the causes behind health inequities. Kalra and his team are publishing a paper in a cardiology journal that looks at the rates of cardiovascular screening of Caucasians versus ethnic minorities in UofL Health – UofL Physicians clinics. The results show that, for the same risk factors of cardiovascular disease, the minority patients are being screened at a lower rate by the same physicians.
“Not intentionally, but there are differences in the way different races are being screened and treated,” Kalra says. “One of my goals is to eliminate those disparities – not just eliminate them, but actually correct them. I don’t quite understand why there should be differences in an academic care environment, but research is looking at factors that lead to that and how we can appropriately educate our physicians as to correct that.”
Increasing the diversity among the medical personnel is also a priority, and Kalra proudly points out that UofL School of Medicine’s current medical class has more women than men and that the University of Louisville is “at the forefront across the country of supporting LBGTQ rights and encompassing diversity and inclusion in its ranks.”
“This is a profession where you dedicate yourself to doing whatever it takes to better the lives of people and to help people around you.”
— Dinesh Kalra, MD
UofL Health is also at the forefront of the latest medical studies and advances. In addition to the many duties and titles held by Kalra, he is also the Director of Advanced Cardiac Imaging, Lipid Clinic & Infiltrative Heart Disease Program. Within the lipid clinic, Kalra says there are significant advances that more of his colleagues need to be aware of.
“In the past we only had statins to deal with high cholesterol,” he says. “Now we have about 14 or 15 different kinds of drugs to reduce cardiovascular risk. Unfortunately, most cardiologists – just because they haven’t specialized in lipidology – are not aware of many of these drugs. As the only lipid clinic in the region, we can take care of people with these complex lipid problems.”
Kalra and his team are also well equipped to deal with the complexities of infiltrative heart diseases, such as amyloidosis, which was not recognized as an important heart disease until the last few years. Now, Kalra says, it is understood that 1 in 10 older people may be impacted by amyloidosis, which can result in heart failure.

“We are one of the specialized centers of excellence for these kinds of infiltrative heart
disorders,” Kalra says. “These diseases are uncommon and not on the radar of many cardiologists. They are difficult to diagnose and treat. So, we have all the elements that are needed to diagnose and treat these patients.”
Kalra acknowledges that the innovations and discoveries in cardiology are coming at an increasingly rapid pace and that it can be difficult to keep up. “It’s really a time of explosive change in the world of cardiology, and I’m just amazed at the amount of discovery and innovation that is happening,” he says.
Among the discoveries that he would like more cardiologists to be aware of are procedures that are more effective treatments for blockages than some of the traditional methods, such as stents. It is a common misconception that cardiologists are essentially plumbers – finding the blockage and fixing it.
“The sad reality is multiple clinical trials have shown that fixing a blockage with a stent often does not extend a patient’s life or make them live any longer or feel better if they don’t have angina,” Kalra says. “Atherosclerosis is a systemic disease – you can’t play Whac-AMole. If you fix an 80 percent blockage, the patient can still have a heart attack because another 20 percent blockage that you ignored
will rupture and cause a heart attack. We take a more holistic, scientific approach to a heart disease. Instead of focusing only on the problem once the damage has occurred, we try to prevent the problem in the first place. Quit mopping the floor again and again. Turn off the faucet. I’m not saying stenting is always wrong, but it’s become widely applied, indiscriminately to asymptomatic people.”
The many advancements, trials, and new drug options often result in multiple different courses of treatment in cardiology or any other medical specialty. That, says Kalra, is why it is so important to treat each patient as a unique individual case, which means getting to know them.
“Technology has definitely improved the world, but there’s a certain element in medicine that requires the human touch and presence and compassion, which will never be replaced,” Kalra says. “Unless I know more about this individual and understand them on a personal level, I am not able to fix them appropriately. The clinical space when I’m sitting next to a patient is sacrosanct – it’s our opportunity to bond and for them to see me as somebody who cares about them. Medicine to me is a holy calling and an art. It is a blessing and a charge and I take it very seriously.”
Kalra, you might say, takes his profession to heart.
LOUISVILLE According to the Centers for Disease Control and Prevention, heart disease is the No. 1 killer of women, taking the lives of about one in every five women. In addition, conditions associated with heart disease, including hypertension, diabetes, obesity, and being overweight, along with lifestyle habits like smoking, put more women at risk.
“While these risk factors are not unique to women, the treatment and approach to care of women is different,” says Li Zhou, MD, cardiologist, and medical director of Norton Heart & Vascular Institute Women’s Heart Program. “As a specialist in women’s cardiology, it is my job to advocate for women’s health, spe-
cifically women’s heart disease, which often goes under-recognized and undertreated. I believe focusing on women’s heart disease will ultimately make their families and communities healthier, especially in Kentucky, where women’s risk for heart disease is higher than in neighboring states.”
There are many stages in life when a woman’s heart sustains additional risk, for example, during and after pregnancy, an area of special interest to Zhou.
“Heart conditions that arise during or after pregnancy come with an added layer of complexity,” says Zhou. “Every medication the mother takes will interfere with her baby, and many times, the mother’s heart condition also dictates how and when the baby will be
delivered.”
Zhou and Lauren R. Albers, MD, cardiologist with the Women’s Heart Program, work closely with primary care providers, OB/ GYNs, maternal-fetal medicine specialists, and other referring providers to establish a care plan tailored to each patient.
Physicians can refer patients to the Women’s Heart Program, which offers care to meet the unique needs of a woman’s heart during all stages of life, including pregnancy and menopause. The team specializes in comprehensive cardiac care of female-patterned heart conditions, including ischemic heart disease and spontaneous coronary artery dissection (SCAD), peripartum cardiomyopathy, and stress cardiomyopathy.

• Pregnant women with cardiovascular symptoms such as chest pain, palpitations, tachycardia, postural tachycardia syndrome, syncope, and others
• Postpartum women who have experienced a cardiac issue during pregnancy, including hypertension, preeclampsia, or eclampsia
• Women planning to become pregnant who have an existing cardiovascular condition or history of cardiac-related complications during pregnancy
• A history of congenital heart disease
• A history of coronary artery disease, including s/p percutaneous coronary intervention, and coronary artery bypass graft or spontaneous coronary artery dissection
• Refractory hypertension or familial hyperlipidemia
• Women with cancer who are undergoing potentially cardiotoxic chemotherapy
In addition to the Women’s Heart Program, the Norton Heart & Vascular Institute team has added four female cardiologists and several advanced practice providers to its staff over the past two years. Many of these providers subspecialize in electrophysiology, heart failure, structural cardiology, and other areas.

The Women’s Heart Program offers two fellowship-trained providers who take great interest in and study women’s heart care.
Zhou practices a patient-centered philosophy of care that is born from a desire to become a care partner at every stage of a woman’s life. She believes a physician needs to provide not only accurate information for their patient to make a reasonable decision, but also all treatment options.
“The best treatment plan is the one that is tailored to the patient’s needs and values,” she says.
Before joining Norton Heart & Vascular Institute, Zhou led the Women’s Heart Clinic

“It is my job to advocate for women’s health, specifically women’s heart disease, which often goes under-recognized and undertreated” – Li Zhou, MD Wherever
at Wake Forest University, Winston-Salem, North Carolina, for more than six years and served as medical director of cardiac rehabilitation. She graduated from Zhejiang Medical University in Hangzhou, China, and earned her PhD from the prestigious Peking Union Medical College in Beijing, China. Zhou completed an internal medical residency at Jacobi Medical Center/Albert Einstein College of Medicine, Bronx, New York, and completed general cardiology training at University of Illinois, Chicago. Zhou studied pathogenesis of atherosclerosis (how coronary artery disease develops) at UT Southwestern Medical Center, Dallas, Texas, using genetically modified murine models. She won the Postdoctoral Fellowship Award from the American Heart Association in 2008. In addition, Zhou led the ADAPTABLE trial at Wake Forest University that assessed the benefits and long-term effects of aspirin dosing in patients with heart disease. She has over 30 publications published in peer-reviewed journals, including the New England Journal of Medicine and JAMA Cardiology. Albers completed her residency and fellowship in cardiovascular medicine at the University of Louisville School of Medicine. She earned her doctor of medicine from St. George’s University College of Medicine in Grenada, West Indies.
More information on the Norton Heart & Vascular Institute Women’s Heart Program, is at NortonEpicLink. com or (888) 4-U-NORTON/486-6786.
 PHOTOS BY JAMIE RHODES
PHOTOS BY JAMIE RHODES
LOUISVILLE Norton Heart & Vascular Institute has been recognized as the second-most experienced program in the country for an innovative treatment of long-standing persistent atrial fibrillation (A-fib). Known as hybrid ablation, the procedure combines minimally invasive treatment of the inside and outside of the heart to interrupt the cause of A-fib and restore a normal rhythm.
“This type of A-fib impacts about 45% of patients living with A-fib,” says Kent E. Morris, MD, associate medical director of Norton Heart & Vascular Institute and electrophysiologist with the Norton Heart & Vascular Institute Heart Rhythm Center. “Typically, these patients have tried multiple medications and lifestyle modifications to no avail.”
Heart Rhythm Center electrophysiologists review the patient’s case to determine if hybrid ablation is an option. Through collaboration

with Norton Heart & Vascular Institute cardiothoracic surgeons, the dual treatment uses precise tools to deliver heat (radiofrequency) to the inside and outside of the heart muscle. The treatment creates scar tissue that interrupts abnormal electrical signals that cause A-fib and may minimize the symptoms the patient feels.
“The specialists at Norton Heart & Vascular Institute have been performing hybrid ablation since 2017, longer than any other providers in the area,” says Steven M. Peterson, MD, cardiothoracic surgeon with Norton Heart & Vascular Institute. “It has been exciting to offer a groundbreaking procedure to patients whose lives have truly been challenged by their A-fib, with this advanced technology.”

Approved in 2021 by the Food and Drug Administration, the hybrid ablation procedure is more commonly available specifically for patients who have been in persistent A-fib lasting more than one year.
“The longer a patient lives in persistent A-fib, the more potential damage can be done to their heart,” says Morris. “The heart muscle weakens, their risk for stroke increases and their overall quality of life is reduced, potentially due to shortness of breath, low blood pressure, and pain or pressure in the chest. This procedure is changing these patients’ lives for the better and offering a treatment option that they never had before.”

Hybrid ablation can be an effective procedure for patients with consistent atrial fibrillation.Steven M. Peterson, MD, cardiothoracic surgeon with Norton Heart & Vascular Institute. Physicians from across the country are traveling to Louisville to learn the procedure with the Heart Rhythm Center team. Kent E. Morris, MD, associate medical director of Norton Heart & Vascular Institute and electrophysiologist with the Norton Heart & Vascular Institute Heart Rhythm Center.
In addition to Norton Heart & Vascular Institute performing the second-highest volume of cases to date, physicians from across the country are traveling to Louisville to learn the procedure with the Heart Rhythm Center team. Program coordinator Tara U. Mudd, APRN, nurse practitioner with Norton Heart & Vascular Institute, is working to help establish best-practice guides to improve treatment protocols at hospitals nationwide.
“This type of procedure is a true collaboration between subspecialists who want the best outcome for the patient. Having been part of this procedure for more than six years now has been remarkable,” says Peterson.

The two-part procedure requires close collaboration between an electrophysiologist and a cardiothoracic surgeon. The procedure starts with a pericardioscopic epicardial ablation that applies radiofrequency energy to the posterior left atrial wall. The aim is to create durable and contiguous lesions while reducing risk of injury to the adjacent heart structures. The device is cooled on the back side with saline solution to prevent injury to healthy tissue. On the underside, vacuum pressure pulls heart tissue into the radiofrequency coil,
while perfusion conducts energy downward into tissue — all while circulating blood absorbs excess heat.
The second stage is an endocardial ablation that uses mapping and ablation to target the heart regions that need additional treatment and any areas impeded by pericardial reflection during the epicardial part of the treatment. This part of the procedure is a conventional cardiac ablation achieved with a catheter.
“A study of 153 patients at 27 different centers performing the hybrid ablation procedure found that patients were twice as likely to no longer need A-fib medication; and after one year, patients spend 90% less time in A-fib,” Morris says.
More information on the Norton Heart & Vascular Institute Heart Rhythm Center for hybrid ablation and other A-fib treatment options, is at NortonEpicLink.com and 888. 4-U-NORTON/486-6786.
“The specialists at Norton Heart & Vascular Institute have been performing hybrid ablation since 2017, longer than any other providers in the area.” — Steven M. Peterson, MD

FRANKFORT New data has revealed that nearly nine in ten Kentucky adults who smoke want to quit!1 Quit Now Kentucky has launched new tools that can help providers get their patients the help they need to quit and stay quit. According to the U.S. Surgeon General, quitting smoking is the best thing patients can do for their health, no matter their age2, and brief advice from a clinician about quitting smoking yielded a 66% increase in successful quit rates3
For years, Quit Now Kentucky has worked with providers to help people who want to stop using tobacco products. Quit Now Kentucky provides no-cost, one-on-one guidance 24/7 through coaches who are trained to help people overcome nicotine addiction. The quitline can connect patients to nicotine replacement therapy, which can be provided to many Kentuckians at no cost to them. There are specialized programs for those who are pregnant or postpartum, are under 24 years old, or have been diagnosed with a behavioral health condition. These interventions work: people who use a tobacco quitline like Quit Now Kentucky are twice as likely to quit successfully as people who try to quit alone or “go cold turkey.”
Providers play a vital role in helping patients quit, which is why Quit Now Kentucky has launched an improved referral program providers can use to help their patients quit smoking, vaping, or using smokeless tobacco products. Now providers who refer to the quitline receive a description of their patient’s

engagement with the program and a list of the services the patient selected upon enrollment. Providers also receive a copy of the patient’s treatment plan, including coaching and any recommended nicotine replacement therapy. These improvements allow providers to work collaboratively with Quit Now Kentucky to help their patients quit.
Providers now have the option to share patient consent to receive texts from Quit Now Kentucky. Those patients receive text messages that explain what they can expect as a quitline participant and how they can enroll online. This is important because 2020 research revealed fewer than half of Kentucky adults who smoke are aware of the quitline. Provider-referred patients who agree to receive a text message have a nine percent higher reach rate compared to referred patients who do not consent to receive a text message. Quit Now Kentucky has improved technology, allowing the program’s name to be displayed on a patient’s phone when they receive a coaching call. This increases the chances the
patient will answer or return a call rather than dismissing it as spam.
Historically, when a provider has made a referral to Quit Now Kentucky, multiple attempts have been made to reach the referred patient over the first ten days. This year Quit Now Kentucky will improve this process by repeating that ten-day outreach process again three months after the initial referral. Piloting this referral-repeat process resulted in 15% of previously unreachable patients connecting with the quitline and 60% of those reached choosing to enroll.
Quit Now Kentucky is a service of the Tobacco Prevention & Cessation Program at the Kentucky Department for Public Health. More information about the quitline is available at QuitNowKentucky.org. The Tobacco Prevention & Cessation Program has additional resources on talking to patients about tobacco use, prescribing nicotine replacement therapy, and more at CHFS.ky.gov.
Nearly nine in ten Kentucky adults who smoke say they want to quit according to the 2020 Kentucky Behavioral Risk Factor Surveillance System.


Are you one of those rare people who hasn’t had an argument with someone about politics? How about someone close to you? Like maybe your spouse or partner?
When it comes to politics, there’s not much that my husband and I agree on. And we’re by no means the only ones. According to a recent Pew report, political affiliation has become the primary marker people use to decide who they want to associate with. The study found that your politics is far more important than your age, race, ethnicity, gender, educational attainment, and religious affiliation in determining whether you like someone and want to hang out with them.
On top of that, people today feel freer to treat those with differing political views with ridicule, contempt, and even aggression, according to a Stanford study.
Wow. I guess that puts it in perspective. No wonder my husband and I have found our conversations “contentious” at times. Here’s the good news: Our political views haven’t changed. How I handle the differences in our views has changed.
It hasn’t been easy. And I’m a marriage therapist.
When a conversation begins on a negative note, there’s a 96% chance that it will end on a negative note. Marriage researcher John Gottman calls it the “harsh startup.”
And it doesn’t take long to make that very accurate prediction. Gottman says you can tell within the first three minutes of the conversation.

What if you don’t realize how negative you’re feeling? What if you think you’re calmer and more rational than you actually are? The three-minute negativity timer is ticking,
but you don’t hear it until it’s way too late to walk things back.
If you can relate to this, take heart. The way this triggering thing works is quite subtle. That’s what makes it so lethal.
The first time I avoided getting triggered by a political discussion, I was hooked. I did something different and it changed everything. The triggering event was very innocent and totally random. I happened to walk into the room as my husband was watching the news. Not a political show, just the news.
As I walked in front of our big-screen TV, I found myself within three inches of one of my most polarizing political figures.
I startled slightly, quickly recovered, and walked through the room without saying a word. No big deal, right?
But this time was different. As soon as I got around the corner, I uncharacteristically paused.
That brief pause may sound like a nothing-burger, but it wasn’t. It was a split-second game-changer. Here’s why:
The pause created a chance for me to slow down enough to actually pay attention.
The pause prevented me from going my usual route of ignoring what was happening. (Hint: Ignoring can be a lame attempt at emotional regulation. It often doesn’t work very well.)
The biggest problem with ignoring is that it’s something that happens in your mind. Meanwhile, your body and emotions are doing something very different.
Psychologists call it the “triangle of experience.” Like it or not, we humans constantly go around in a “triangle of experience” of physical sensations, emotions, and thoughts, all playing off each other.
I had entered my own personal Bermuda triangle of experience.
Only this time, I was paying attention to what it felt like. I was surprised to notice that my heart rate was up and my hands were trembling a little. Then I noticed that my nostrils were … flared, like an animal. OMG, I’ve gone totally instinctual, I thought as I felt my eyes widen.
Rather than ignoring big chunks of your experience, it can be smarter and saner to pay attention — in a curious, non-judgmental way — to all levels of what’s happening at the moment:
a. The sensations in your body.
b. The emotions you’re feeling.
c. The thoughts you’re thinking— what you’re telling yourself about the experience.
It’s called embodied awareness. It’s a felt sense of what’s happening. It gives your brain more complete data to work with, so you can



Here’s the best part. Not only did I feel better right away, but I was in a less reactive frame of mind when I walked back into the room later.
Here’s the big takeaway from my experience: If I hadn’t stumbled into this simple process, I would have walked back into the room, dangerously unaware that I was activated. I would have been in a bad mood at best, maybe downright testy or — even worse — looking for a fight.
And I wouldn’t even have realized it.
My favorite part of the experience? I found the flush of success to be a confidence-builder and highly motivating. I want to keep getting more skillful.
This is important, so listen up:
Doing what I’m describing is a skill that you can learn, just like you learned to ride your bicycle. Yes, it takes some practice and you’ll probably need some help. No biggie. It means you just joined the human race. Come on in. The water’s fine.
make better decisions.
The felt-sense thing with my nostrils piqued my curiosity. That made it easy to keep paying attention to the interweaving of thoughts, emotions, and sensations.
Here’s how the back and forth of “old response” and “new response” played out:
Thought: Good grief, this really affected you, didn’t it?
Emotion: Concern
Thought: You’re being ridiculous. Stop it.
Emotion: Embarrassed.
Sensation: Upper body muscle tension.
Field of vision narrowed.
It was clear I could use some help. But how?
It’s counterintuitive. You’d think acknowledging your feelings would make you more upset, but it does the opposite: It helps you get a grip and emotionally regulate. Here’s what I mean:
Thought: This feels awful.
Thought: Jan, do you know how many people are feeling the same way you’re feel-
ing right now? You’re not the only one going through stuff like this. There are people in houses all over the country experiencing this. Even therapists like you.
Emotion: Calmer.
Once I was calmer, the more rational, problem-solving part of my brain could come back online.
4. Do It Now.
The promise of a future feel-good won’t cut it. Later is too late. Do something now. That doesn’t mean immediately solving the problem. It’s about doing something right now to help yourself calm down and focus, so you can slide into a problem-solving mindset.
Often all that’s needed is a simple gesture of acknowledgment: maybe a big sigh or lightly pressing your palms onto the tops of your thighs. Other times, a self-protective gesture is needed: breaking eye contact, changing the subject, or leaving the table.
Interestingly, steps one and two provided all the help I needed in my triggering experience.
If you want to get more skillful at dealing with your differences — with your partner or anyone else — here’s how to get started right away: Check out three questions that quickly help you figure out if I’m the right helping professional for you. See them on my website at www.DrJanAnderson.com or text me at 502.426.1616.

LOUISVILLE Baptist Health is welcoming a new primary care practice and two new doctors. Family Care Physicians, located at 2701 Chamberlain Lane in eastern Jefferson County, is joining the Baptist Health Medical Group and is now called Baptist Health Medical Group Primary Care. The change was effective February 1, 2023.
Patients will continue to see the practice’s two doctors, Veronica Kavorkian, MD, and Karen Langness, MD. Kavorkian and Langness are both graduates of the UofL School of Medicine and board certified in family medicine. They have been recognized
gical experience and has received national board certification from the American Board of Plastic Surgery. He is certified by the American Heart Association in Basic Life Support and Advanced Cardiovascular Life Support.
He is a member of the American Society of Plastic Surgeons, American Medical Association, American Burn Association and Louisiana State Medical Society.
Maguire will be practicing at Baptist Health Medical Group Plastic & Reconstructive Surgery, located at 511 Robinbrooke Rd., Ste. 100, in Elizabethtown.

LEXINGTON In July 2022, Gery Tomassoni, MD, an electrophysiologist at Baptist Health Lexington, performed an ablation on a patient’s heart using the OCTARAY Mapping Catheter in the treatment of atrial fibrillation.
Karen Langness,MD
by Louisville Magazine as “Top Docs under 40” and are members of the American Academy of Family Physicians, Kentucky Medical Association and Greater Louisville Medical Society.

ELIZABETHTOWN Stephen Maguire, MD, has joined Baptist Health Medical Group Plastic & Reconstructive Surgery to offer compassionate, patient-centered care.
ELIZABETHTOWN Scott Rotterman, DPM, has joined Baptist Health Medical Group Podiatry to offer compassionate, patient-centered for foot care.
Rotterman specializes in procedures involving foot and ankle arthritis, trauma, reconstruction, flatfoot repair, elective foot surgery, and more. Rotterman graduated with his DPM degree from Kent State University College of Podiatric Medicine. He also completed a podiatric surgery residency at Norton Audubon Hospital, where his training focused on trauma, sports medicine, diabetic wound care, and limb salvage. During his residency, Rotterman served as chief resident and earned reconstructive rearfoot and ankle certification.
Traditionally, a mapping catheter (PENTARAY) is used to reconstruct the heart anatomy and locate the cardiac sites for ablation. Now with the new OCTARAY technology, the time required to create the atrial anatomy is shorter and identification of the ablation sites is more accurate.
Stephen Maguire, MD
Maguire specializes in cosmetic surgery, breast reduction surgery, and breast reconstruction surgery following cancer treatment. He graduated from the UofL School of Medicine. He completed his general surgery residency at Louisiana State University Health Sciences Center. He then completed a fellowship at UofL School of Medicine.
Maguire has more than 25 years of sur-
He has received national board certification in foot surgery and rearfoot/ankle surgery from the American Board of Foot and Ankle Surgery. He is a member of the American College of Foot and Ankle Surgeons and the American Podiatric Medical Association.

Rotterman will be practicing at Baptist Health Medical Group Podiatry, located at 551 Westport Rd, Ste. A in Elizabethtown.
“OCTARAY technology provides additional catheter splines resulting in a higher number of electrodes that also have a shorter distance between them. In addition, the electrodes have a higher recording fidelity. As a result, the electrical signal quality is significantly improved,” explains Tomassoni. “The better quality of electrical signals hopefully will allow us to guide ablation more successfully to eliminate the abnormal heart rhythm.”
“Electrical mapping of the chambers using OCTARAY technology is more efficient resulting in a faster acquisition of both the electrical signals and reconstruction of the overall heart anatomy,” says Tomassoni. “Reduction in procedural time and enhancement of workflow efficiency can improve patient care. Less time in the procedure is better for the patient because you’re reducing the potential risks associated with longer procedures.”
Hamlin, APRN,
CHI Saint Joseph Medical Group – Cardiology
NICHOLASVILLE CHI Saint Joseph Medical Group –Cardiology welcomed Fred Hamlin, MSN, APRN, FNP-BC, to its practice at Saint Joseph Jessamine and in Lebanon. Hamlin, originally from McCreary County, brings more than two decades of professional experience to the health care group and even more years of passion, as his love for the medical field, especially the heart, started at age 5.
“The heart and its inner workings have always been an interest of mine since I was very young,” says Hamlin. “I’ve always been fascinated by its plumbing, electricity, and structure. There’s so much that goes into caring for the heart.”
Hamlin’s love for the medical field heightened in high school when his father became seriously ill. As he watched his mother care for his father at home, much like a nurse would do, Hamlin saw how significantly this care impacted his father’s life and how working in the health care field could help others.
“I felt like that was a calling from God to pursue a career in nursing,” says Hamlin.
Hamlin graduated from Morehead State University in 2000 with a BS in nursing. He cared for patients from the bedside and in the sky. Hamlin was a flight nurse with the Air Evac Lifeteam for four years. Hamlin pursued his MS in nursing at Indiana State University to enhance his education and training. Hamlin has continued his work in his home state of Kentucky and has kept his childhood dream alive, focusing on caring for his patients’ cardiovascular health.
Hamlin is a board-certified nurse practitioner by the American Nurse Credentialing Center (ANCC). He is also board certified in basic life support, advanced cardiac life support, and pediatric advanced life support.
In his spare time, Hamlin enjoys spending time with his wife, an ER/ICU nurse, and their three sons. He also enjoys playing the piano, hiking, attending church, and constantly learning more about his field.
Hamlin is practicing at CHI Saint Joseph Medical Group – Cardiology at Saint Joseph Jessamine, located at 1250 Keene Road, Suite 102, and CHI Saint Joseph Medical Group – Cardiology in Lebanon, located at 325 Walnut Street, Suite 300.
MOUNT STERLING John Yanes, FACHE, CPPS, has been named the new president for Saint Joseph Mount Sterling. Yanes replaces Jennifer Nolan, who is taking on a ministry role with CHI Saint Joseph Health, in addition to her role as president at Flaget Memorial Hospital.
Yanes joined CHI Saint Joseph Health in 2019 as president of Saint Joseph London and Saint Joseph Berea and will continue to lead those hospitals as well.

With this realignment within the ministry, the new leadership team at the three hospitals will consist of Yanes, Shelley Stanko, MD, chief medical officer, Andrea Holecek, EdD, MSN, MBA, RN, NE-BC, CENP, FACHE, vice president of nursing, and Brady Dale, RT(R) (ARRT), vice president of operations.
“We are excited to serve the Mount Sterling community and to work with the caregivers at Saint Joseph Mount Sterling,” says Yanes. “Our caregivers across our ministry work hard to deliver on the Saint Joseph promise each and every day. Our leadership team considers it a privilege to be able to fulfill our mission across three Saint Joseph hospitals.”
Yanes previously served as chief executive officer at Andalusia Health in Andalusia, Ala., and also served as a president and CEO in Ohio, Tennessee, Pennsylvania and Florida for 17 years. He began his career in Florida as an administrator and executive director for clinics and health networks in Jacksonville, Daytona
Beach and Pompano Beach. Yanes received a bachelor of science in business administration, an MBA and a master of health science from the University of Florida. He completed the Executive Program in Managed Care at the University of Missouri-Kansas City, is board certified in health care management from the American College of Healthcare Executives in Chicago and received the designation as Certified Professional in Patient Safety from the Institute of Healthcare Improvement in Boston.
Stanko is a native of London and has served as the chief medical officer for Saint Joseph London for nine years and Saint Joseph Berea for four years. Stanko is a member of the CHI Saint Joseph Board of Directors and the Executive Committee. She sits on the Saint Joseph Medical Group Board and chairs the Quality Committee. A graduate of Georgetown College, the UK College of Medicine, and the Cabarrus Family Medicine Residency, she has practiced family medicine for the past 18 years.
Shelley Stanko, MD

Andrea Holecek, EdD, MSN, MBA, RN, NE-BC, CENP, FACHE, joined the ministry in June, 2019, as the vice president of Patient Care Services and chief nursing officer for Saint Joseph London. She previously served as the senior director of Patient Care Services and Magnet Program Director at Bayhealth Medical Center in Delaware. Holecek holds several academic degrees including a master’s in nursing, a master’s in business administration, and a doctorate of education in innovation and organizational leadership. She is a board-certified nurse executive and a Fellow of the American College of Healthcare Executives.
Andrea Holecek, EdD, MSN, MBA, RN, NE-BC, CENP, FACHE

Dale is a native of Mount Sterling, and has been with CHI Saint Joseph Health since 2001, when he joined Saint Joseph Hospital in Lexington as a staff technologist in the cardiac catheterization department. He came to Saint Joseph London in 2008 as director of

cardiac catheterization and cardiopulmonary rehabilitation. He was named director of cardiopulmonary services in 2014 and then director of cardio-ancillary services in 2018. Dale started his career at Mercy Hospital Anderson in Cincinnati as a staff technologist, radiologic special procedures, and cardiac catheterization.


later in life stemmed from watching her father, an engineer, suffer at the end of his life due to cancer.
“Watching him suffer at the end of cancer was hard,” says Kaur. “Many of his symptoms could have been managed, and I wish he would have had a geriatrician. This is what drew me into the medical field. There is a huge need for geriatricians and palliative care doctors here, and I hope to make a difference in the community.”
patients and palliative care, she treats adults of all ages. She prides herself on putting her patients first and being realistic with them, even when she says reality can be hard to hear.
Kaur brings years of medical experience to CHI Saint Joseph Health – Primary Care in London. She attended medical school at Grigore T. Popa University of Medicine and Pharmacy in Romania, was a resident with the Icahn School of Medicine at Mt. Sinai’s Inter nal Medicine Program in Queens, New York, and was a fellow with the NYU Grossman School of Medicine in New York City.
Regina Kaur, MD
LONDON Regina Kaur, MD, has joined CHI Saint Joseph Health – Primary Care in London. Kaur was born and raised in Malaysia, and as a child, she often volunteered in her community with her father, including assisting at vaccination camps, which sparked her interest in serving others. She said her passion for helping others
Kaur personifies CHI’s values as she cares and leads with compassion and inclusivity. She says she is happiest when helping others, and she is excited to be a part of a team that feels the same way and is changing lives. Her favorite part of being a physician is creating genuine relationships with her patients, learning how to work with them and understand their medical history.
“The best part about my job is the patient connection,” says Kaur. “I love talking to people. Everyone has their own story, and the amazing stories I hear help me to grow as a person and a physician. While this job can be stressful, the lives you touch and those who touch you are worth it. There is a lot of love in this field.”
While Kaur enjoys a focus on geriatric
Kaur has been part of multiple published articles and medical conference presentations and is certified by the American Board of Internal Medicine (ABIM). Along with her medical knowledge, she is also fluent in English, Punjabi, Hindi, and Malaysian languages.
In her time away from work, Kaur enjoys spending time with her husband, who also practices medicine, exploring Kentucky, renovating their home, and trying all the downhome Southern cooking.
Kaur is practicing at CHI Saint Joseph Health – Primary Care in London, located at 1025 Saint Joseph Lane.
LONDON The Nurturing Children Program at Saint Joseph London has launched a pilot project at Lynn Camp Elementary School aimed at keeping kids safe when they come in contact with a firearm. The Eddie Eagle GunSafe® program kicked off January 5th at the school.
“Through this program, we are eager to provide an effort that builds awareness to help children remain safe around guns,” says John Yanes, president, Saint Joseph London. “We are pleased to be able to partner with schools in southeastern Kentucky to prevent tragedies.”
According to the Gun Violence Archive, in 2022, two children under age 11 were killed and 19 injured in gun incidents in Kentucky. Six teens were killed and 53 were injured in the same year in the commonwealth. Across the U.S. between 2015 and 2020, there
were at least 2,070 unintentional shootings by children that resulted in 765 deaths and 1,366 nonfatal gun injuries, according to the Gun Violence Archive.
The Eddie Eagle program focuses on one mission: to teach children four simple steps so they know what to do if they ever come across a gun. Those easy-to-remember steps are: Stop; Don’t Touch; Run Away; and Tell a grown-up. The program was developed in 1988 by a task force comprised of educators, school administrators, curriculum specialists, urban housing safety officials, clinical psychologists, law enforcement officials and National Rifle Association firearm safety experts.
“Through our violence prevention work, we are always looking for ways to make sure kids understand different situations that could
put them in danger,” says Mollie Harris, manager, Violence Prevention Program. “This project could not be possible without the support and work of the Knox County Sheriff’s Department and the Knox County School System.”
Representatives with the Knox County Sheriff’s Department and Knox County Schools lauded the opportunity to work with CHI Saint Joseph Health in efforts to protect children.
“The safety and well-being of our children is the greatest priority,” says Steve Owens, school resource officer from the Knox County Sheriff’s Department. “Anytime an opportunity comes along to develop or use a new approach to protect these children, it is our responsibility to try, and then to nurture that. I am beyond excited to have the oppor-
LOUISVILLE The College of Education and Human Development and the School of Medicine at U of L have launched a new, fully online master of science degree in Health Professions Education (MSHPE).
“The goal of the MSHPE program is to magnify the impact of the health professions educator. Not only do health professions educators improve the outcomes of their patients, but they significantly improve the educational outcomes of their practitioner learners and impact the patients that those learners ultimately care for in the future,” Staci Saner, program director and assistant professor of medicine, said.
Employment in the health care industry is booming, with expected growth of 2.6 million jobs from 2020 to 2030 according to the U.S. Bureau of Labor Statistics. The curriculum within UofL’s MSHPE program will meet this need by equipping educators with the skills and expertise to be a highly effective health professions educators.
Additionally, many accrediting bodies are moving towards requesting background knowledge in teaching and learning for health professions educators. This degree will provide this necessary credential.
The new degree plan focuses on the needs for health care professionals who currently teach or plan to teach in their respective discipline — medicine, nursing, dentistry, pharmacy or other health fields — and who want to become effective educators in a clinical or classroom setting.
Graduate programs in HPE — including certificate and degree programs — are viewed by many as a key strategy to contribute to a health professional’s conversion from competent clinician to academic leader, says Susan Hildebrand of the College of Education and Human Development’s Department of Organizational Leadership and Learning.
“The professionalization of the HPE workforce has been driven by a number of institutional and regulatory dynamics,” says
BY CHRISTOPHER DYEHildebrand. “Many clinicians have made education the focus of their professional roles, and institutions have responded by creating career tracks, such as clinician educator and scholar.
“Also, accreditation bodies increasingly require that residency leaders have the requisite specialty expertise and documented educational and administrative experience. With this explicit requirement, and with the need to maintain an educational environment conducive to educating the residents in graduate health care education competencies, institutions recognize the value of employing leaders who possess advanced training in education to maintain and improve their residency programs.”
Assistant Professor of Comprehensive Dentistry Wil Abshier has completed the program. “I recommend this program to anyone who just simply wants to be a better educator for their students,” says Abshier. “So many people in HPE are clinicians at heart but have no formal education in teaching. This bridges that gap.”
tunity to be a part of this effort to reach our children in a new way.”
Principal Emily Haneline said Lynn Camp Elementary is honored to be selected as the pilot location for the program.
“The safety of our students is always our number one priority and this collaboration with CHI Saint Joseph Health and the Knox County Sheriff Department allows us to extend beyond just our school and provide our students and families with critical knowledge to keep our students safe across all settings,” says Haneline. “We are grateful to Mollie Harris for her vision; without it none of this would have been possible. I am excited to see the impact that this program will have for not only our students, but for students throughout Knox County.”
The Nurturing Children Program at Saint Joseph London is made possible through a grant from the CommonSpirit Health
Mission and Ministry Fund. The goal of the program is to reduce child abuse and neglect as well as child fatality. Schools interested in participating in the Eddie Eagle GunSafe® program can contact Mollie Harris at mollie. harris@chisaintjosephhealth.org.
LEXINGTON On January 24, 2023, Lee Dossett, MD, hospitalist and CMO at Baptist Health Lexington, became the new president of the Lexington Medical Society, which was founded in 1799 and is the second oldest medical society in America. Dossett graduated from UK both as an undergraduate and from the UK College of Medicine. He assumed the president’s role from outgoing president Khalil Rahman, MD.
In his acceptance remarks, Dossett named physician advocacy and improving value in healthcare as his two priorities. He stated that “It is our duty to advocate for our patients and ensure that they receive the best care possible. That requires us to be proactive in speaking out about issues that affect the quality and accessibility of healthcare.”
“One way we can do this is through organized medicine,” stated Dossett. He said that in his time as a hospitalist he could see the waste that can be present in the medical system. “I hope to provide information,




Lee
MD,
context, and resources for all of us to do our part to reign in wasteful healthcare spending,” he stated.

Pat Padgett, executive vice-president of the Kentucky Medical Association, relayed results from a survey of its members. Padgett’s survey results showed that administrative burdens were the main cause of stress and it was affecting the personal and professional satisfaction that doctors felt about their work. He specifically noted that 81% of the respondents said that “prior authorization sometimes, often, or always delayed access to care for patients.”
Cory Meadows, deputy executive VP and director of advocacy for the KMA, gave an update to the audience on potential legislative activity in the 2023 Kentucky legislature. Senator Donald Douglas, MD, R-Ky., and Rep. Killian Timoney, R-Ky., spoke about healthcare and their legislative interests.
The next general membership meeting of the Lexington Medical Society is Tuesday, May 9 at the Signature Club in Lexington.
Find more information about the Lexington Medical Society at 859.278.0569 and www.lexingtondoctors.org.













