ALSO IN THIS ISSUE
GENERAL SURGERY AT CHI SAINT JOSEPH LONDON
PULMONOLOGY & CRITICAL CARE AT NORTON HEALTHCARE
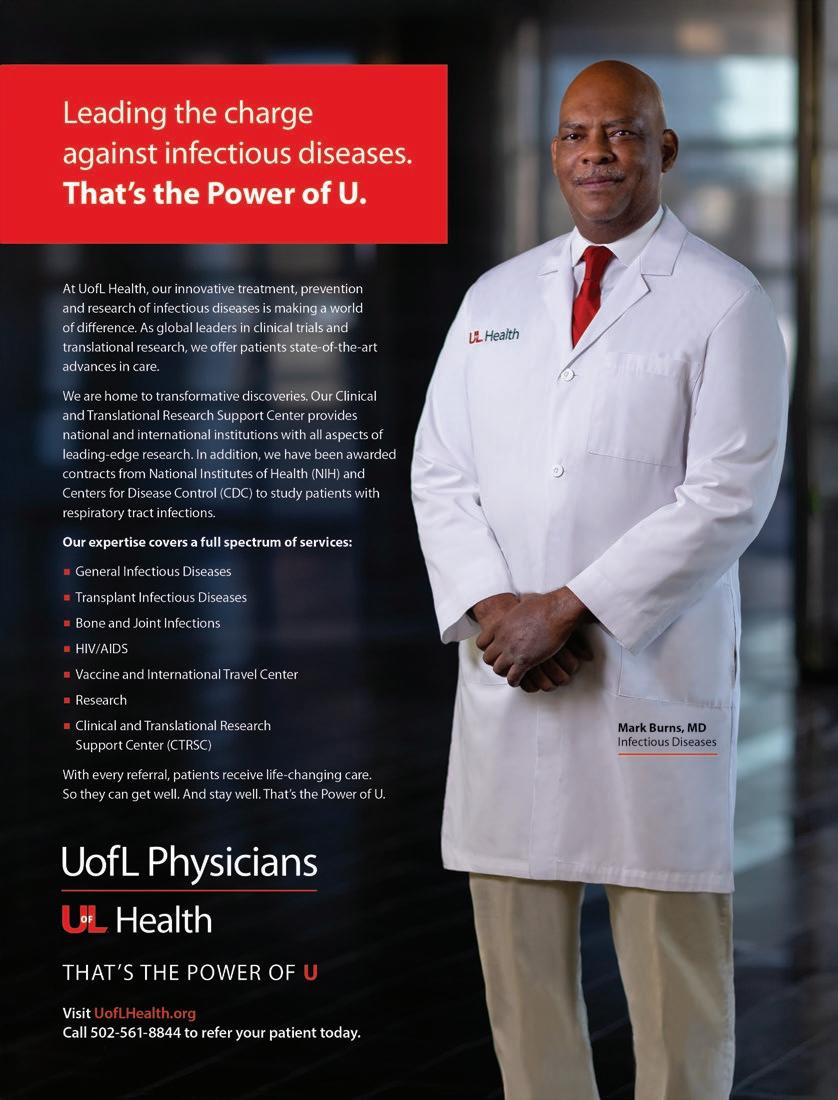
ENDOCRINE SURGERY & RESEARCH AT UOFL HEALTH
LUNG CANCER SCREENINGS & INFECTIOUS DISEASE AT KY DEPARTMENT FOR PUBLIC HEALTH




ALSO IN THIS ISSUE
GENERAL SURGERY AT CHI SAINT JOSEPH LONDON
PULMONOLOGY & CRITICAL CARE AT NORTON HEALTHCARE
ENDOCRINE SURGERY & RESEARCH AT UOFL HEALTH
LUNG CANCER SCREENINGS & INFECTIOUS DISEASE AT KY DEPARTMENT FOR PUBLIC HEALTH
At Medical Transformation Center, Carl Paige, MD, has found his model of healthcare


2025
ISSUE #158 (June)
WOMEN & CHILDREN’S HEALTH
OB-GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology
ISSUE #159 (September)
MUSCULOSKELETAL HEALTH
Orthopedics, Physical Medicine & Rehabilitation, Sports Medicine, PT/OT
ISSUE #160 (October)
CANCER CARE
Hematology, Oncology, Plastic Surgery, Radiology, Radiation
ISSUE #161 (December)
IT’S ALL IN YOUR HEAD
ENT, Mental Health, Neurology, Neuroscience, Ophthalmology, Pain Medicine, Psychiatry
2026
ISSUE #162 (February)
HEART & LUNG HEALTH
Cardiology, Cardiothoracic Medicine, Cardiovascular Medicine, Pulmonology, Sleep Medicine, Vascular Medicine, Bariatric Surgery
ISSUE #163 (April)
INTERNAL & EXTERNAL SYSTEMS
Dermatology, Endocrinology, Gastroenterology, Geriatric Medicine, Internal Medicine, Integrative Medicine, Infectious Disease Medicine, Lifestyle Medicine, Nephrology, Urology
Editorial topics and dates are subject to change
To participate, please contact Gil Dunn, Publisher GDUNN@MD-UPDATE.COM
859.309.0720 (direct) • 859.608.8454 (cell) Send press releases to gdunn@md-update.com
Finding your place and embracing your space is an underlying theme for the doctors we profile in this issue of MD-Update. In reading their stories, I think you’ll see that each of them talks about their medical practice as “a calling,” something they were drawn to, or led to, and are comfortable with, while serving others.
In our cover story, Dr. Carl Paige puts it simply that large healthcare wasn’t performing optimally for his patients or intellectually for him, so he set out to create his own space in cellular medicine at the Medical Transformation Center. Dr. Mahsa Javid says that she chose surgery because it was a specialty that was under-represented by women and that her mentor was an endocrine surgeon. Other mentors showed her the value of teaching and research and sharing that information with future generations.
Dr. Samantha Baah says that “finding a solution to extend patients’ quality of life is a calling,” which she experienced in multiple waves as a critical care pulmonologist during the COVID-19 pandemic. Dr. Nickolas Capal says “fixing people who are sick, dealing with whatever comes through the door, is what I signed up for, it’s what I love to do.”
MD-Update Mental Wellness columnist Dr. Jan Anderson recounts her interesting journey from the corporate world to a professional career in counseling high achievers and parents estranged from adult children. One step at a time she found her way to a fulfilling practice helping others.
I invite you to get to know your Kentuckiana colleagues by reading their stories inside.
Artificial intelligence is a hot topic. I’m grateful that one of Kentuckiana’s thought-leaders on the subject, Dr. Danesh Mazloomdoost, founder and medical director of Wellward Medical, has contributed his award-winning essay on AI to MD-Update on page 8. Contact me if you have a response or thoughts on a different subject.
It’s allergy and outdoor season, so Kentucky’s Department for Public Health reminds us of the importance of early lung cancer screening and the danger of tickborne disease. The American Heart Association’s annual Heart Balls in Lexington and Louisville were great events to attend. We have some photos for you in case you missed them.
The 2025 MD-Update editorial calendar is on the preceeding page. When you see your specialty, contact me. If your specialty isn’t included, and you have a story to tell, that’s another reason to reach out to me. I’m looking forward to hearing from you.

MD-UPDATE
MD-Update.com
Volume 15, Number 2 ISSUE #157
EDITOR/PUBLISHER
Gil Dunn gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda DeBord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC
Hope Cottrill, MD
Evelyn Jones, MD
Danesh Mazloomdoost, MD
Scott Neal, CPA, CFP
Nirvana Nawar, MHA
Morgan Smith, MPH, CPH
ADVERTISING AND INTEGRATED PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com
Mentelle Media, LLC 38 Mentelle Park Lexington KY 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2025 Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you.
Individual copies of MD-Update are available for $9.95.

Until next time, all the best, Gil Dunn Editor/Publisher MD-Update
SEND YOUR LETTERS






BY KMA PRESIDENT EVELYN MONTGOMERY JONES, MD, AND LEXINGTON MEDICAL SOCIETY PRESIDENT HOPE COTTRILL, MD
Kentuckians suffer from a host of troubling health conditions. Through the Kentucky Medical Association (KMA) and Kentucky Foundation for Medical Care (KFMC)’s “Small STEPS, Big Impact,” campaign, Kentucky physicians have been highlighting ways we can make small changes that can add up to a big impact on overall health. From issues with food insecurity, tobacco use, and exercise, there is plenty of room for improvement in our state. However, while more difficult to calculate, stress remains an underlying factor in nearly every health condition.


eight free sessions each calendar year with licensed psychologists through The Woodland Wellness Group for active and retired physicians and residents and fellows, and twelve free sessions for UK medical students each calendar year.
Through these initiatives, KMA and LMS have made physician wellness a priority, but continued advocacy and engagement from members is crucial. The well-being of our physicians is directly tied to the health of our communities, making this issue one of Kentucky’s most critical. By acknowledging the issue, supporting solutions, and fostering a culture of wellness, we can ensure that those who dedicate their lives to healing others receive the care they deserve in return.
Evelyn Montgomery Jones, MD, is president of the Kentucky Medical Association and a dermatologist from Paducah. Hope Cottrill, MD, is president of the Lexington Medical Society and a Lexington oncologist. Both physicians are graduates of the 2021 class of the KMA’s Kentucky Physicians Leadership Institute (KPLI).
Long hours, seemingly endless administrative tasks, and the emotional weight of patient care all contribute to our rising levels of stress and burnout. A 2022 KMA survey found that more than 54% of Kentucky physicians indicated they are feeling more stress now than before the pandemic, with most citing administrative burdens and work/life balance issues as the main sources.
The impact of physician burnout is profound, and it is one that we must tackle head on. Recognizing the gravity of this issue, the KMA and the Lexington Medical Society (LMS) have each created support programs that can be a first step for member physicians struggling with burnout and other stressors.
“It’s really important to try to emphasize prevention and ongoing maintenance of selfcare because it is so easy to just gradually start to overwork yourself,” said Shawn C. Jones, MD, president of the Kentucky Foundation for Medical Care and author of “Finding Heart in Art: A Surgeon’s Renaissance Approach To Healing Modern Medical Burnout.”
In 2020, LMS launched its Physician Wellness Program (PWP). The program connects physicians with counselors and provides
KMA launched a similar program in 2021. The Association’s “Be Well, Stay Well Physician Health Program” provides up to six free visits with a licensed therapist, also through The Woodland Wellness Group, for KMA physician members in rural areas of the state. Both KMA and LMS ensure complete confidentiality, encouraging physicians to seek help without fear of professional repercussions. Additionally, KMA supports policies that reduce administrative burdens and have helped secure protections for physicians seeking mental health assistance. This includes the passage of 2023’s Senate Bill 12, which encourages physicians to seek care through a wellness program and ensures that a record of a physician’s participation in such a program is confidential.
While outside support is crucial, individual physicians can take steps to mitigate stress and burnout in their own lives. Strategies include
• Setting Boundaries
• Seeking Peer Support
• Practicing Mindfulness
• Prioritizing Physical Health
• Utilizing Available Resources


“What can we do to deal with this topsy-turvy world we find ourselves living in today?” Some version of that question is the one most frequently asked of us so far in 2025. Undoubtedly, it’s prompted by the volatility in today’s markets, or the uncertainty created by on-again, off-again economic policies. Usually, the question hangs on one or two data points that have been broadcast throughout the day in nearly every media outlet. Make no mistake, I am all-in for everyone having access to their personal financial data at their fingertips. What we advisors work against are the pressures to make quick, sometimes reactive, decisions based on insufficient or incorrect data. Understanding these challenges and developing strategies to navigate them is essential for anyone seeking to manage their personal finances effectively in this data-rich world.
Another challenge is the emphasis on quantity over quality when it comes to financial data. Many financial tools and platforms encourage users to input as much information as possible, tracking every expense, analyzing every market trend, or monitoring progress for each goal from the bottom-up. While advisors intend to provide a comprehensive picture of a family’s financial health, too many metrics can often lead to a focus on excessive data collection rather than the quality and relevance of the data itself.
For example, when we ask about spending, nearly everyone begins with itemizing their monthly expenditures in fine detail. A much better approach, in my opinion, is to approach the question from the top down and collect six data points: 1) total all the inflow, 2) subtract the amount of taxes owed on the income, 3) subtract the amount needed to pay on existing debts, and then 4) save some, 5)
BY D. SCOTT NEAL, CPA, CFP®, CEPA
give some, and 6) spend the rest. Cash flow is a zero-sum exercise. Make big decisions before drilling down to the finer data points.
While data can offer valuable guidance, personal finance is also deeply tied to human emotions and behavioral tendencies that data alone cannot capture. Financial decisions influenced by fear, overconfidence, or emotional attachment to certain investments are rarely optimal. In a data-driven world, these emotions can sometimes cloud an individual’s judgment, especially when the data presents a clear but counterintuitive conclusion.
The rapid pace at which financial data is generated today can create a sense of urgency, compelling individuals to make quick financial decisions. While this can be helpful for capitalizing on time-sensitive opportunities, it also carries the risk of making hasty decisions that could harm long-term financial goals. Does “first, do no harm,” sound familiar?
To effectively manage personal finances, individuals need to adopt strategies that help filter out unnecessary noise, focus on high-quality data, and incorporate both data and human judgment into their decision-making. Here are several approaches designed to improve personal financial decision-making:
1. Set Clear Financial Goals and Prioritize Data To Be Collected.
The first step in managing personal finances is to establish long-range financial goals and then work from the “top down” toward accomplishing those goals. Defining the necessary conditions to meet the objectives and subsequently drilling down to more specific data requirements is a much better way to do planning.
2. Focus on Data Quality, Not Quantity.
Rather than collecting vast amounts of financial data, one should focus on high-quality, actionable information that directly impacts financial goals. Instead of obsessively checking the balance in an account or following every single stock ticker in your portfolio daily, greater benefit might be derived from tracking a few key metrics: net worth, savings rate, and the long-term performance of investments. Finding core constraints to goal achievement requires clear, logical thinking, not more data.
3. Incorporate Human Judgment and Behavioral Awareness
While data is a critical part of financial decision-making, individuals should also recognize the importance of behavioral and emotional factors. Given the fast-paced nature of data delivery today, it’s easy to feel pressure to make financial decisions quickly. However, effective financial management requires patience and a long-term mindset. Rather than reacting impulsively to short-term market fluctuations or personal financial stress, prioritize long-term strategies that align with your own values and financial objectives. Emotional intelligence plays a vital role in financial success, and being aware of one’s tendencies to panic, become overconfident, or procrastinate can aid decision making. Mindfulness is key.
Navigating personal finances in a data-driven world can be overwhelming. Better outcomes can be achieved by adopting strategic approaches that focus on clear financial goals, human judgment, and patience. Data should serve these ends, not the other way around.
Scott Neal is president of D. Scott Neal, Inc., a fee-only fiduciary financial planning and investment advisory firm with offices in Lexington and Louisville. Write to him at scott@dsneal.com or call 1-800-344-9098.

EDITOR’S NOTE: The Lexington Medical Society had an essay contest for practicing physicians, residents, and medical students. Dr. Mazloomdoost’s essay received first place in the practicing physician category. Dr. Mazloomdoost is the founder and medical director of Wellward Medical, a regenerative medicine practice in Lexington. He is a board-certified anesthesiologist from Johns Hopkins and fellowshiptrained in interventional pain from MD Anderson.
LEXINGTON No one wants to feel obsolete. That fear fuels much of our anxiety about AI in medicine: Will it replace us, make mistakes, or serve corporate interests? Underneath, we fear the unknown—and with good reason. The implementation of electronic health records (EHRs) has scarred many of us. Intended to streamline documentation, it ironically devolved our profession one step closer to mindless data-entry. Still, I believe AI will be different. It will bridge gaps in medicine we did not even realize existed, much like other historic deficits that, in hindsight, seem painfully obvious.
In the early 1800s, diseases associated with foul odors, or “putrid scents,” were attributed to miasma—bad air thought to carry illness. A Hungarian physician, Ignaz Semmelweis, observed that a maternity ward run by midwives had significantly lower illness rates than another staffed by medical students who moved directly from autopsies to delivering babies. By implementing rigorous handwashing, mortality rates plummeted, confirming his theory that providers—not smells—were the cause. His peers largely dismissed him, offended by the implication that doctors spread disease. It took Louis Pasteur’s insights several decades later—and the microscope, which had been around for nearly two centuries—to confirm that invisible microorganisms caused disease.
BY DANESH MAZLOOMDOOST, MD
Just as 19th-century medicine was once blind to germs, our current system risks blindness to the gradual threats of chronic illness, now the world’s leading cause of death. Nevertheless, healthcare still focuses on acute cure rather than sustained prevention. In chronic illness, prevention is the cure.
Chronic illnesses often whisper warning signs well before the defined thresholds we use to quantify disease, yet these soft signals go unchecked. Patients may only see a doctor annually or when symptoms worsen. Our surveillance tools—physical exams, vital signs, lab work, imaging—occur at isolated moments, offering snapshots that demand extensive extrapolation. It is like watching a movie in 15-minute segments, separated by days or weeks, -- critical changes often remain hidden.
Meanwhile, modern life teems with metrics—step counts, blood pressure readings at home, or even subtle changes in gait. However, these data points vanish into an ethereal waste basket. We need a modern “microscope” that not only records data but synthesizes it—the next evolution beyond today’s EMRs—so we can shift medicine upstream into prevention rather than cure.
The challenge is not just gathering data but interpreting it at scale. Historically, healthcare tackled complexity by subdivision—orthopedics branched off from surgery, cardiology branched off from internal medicine, and so on. While this specialization fosters deeper expertise, it can undermine the holistic view that chronic diseases demand.
Concurrent with the exponential growth of medical knowledge is the petabytes of
data that each and every individual creates daily—from genetic profiles to continuous heart rhythm monitoring. Creating deeper and more branched niches of medicine cannot keep up with this. No human mind can sift through such complexities unaided; here, AI is an asset. Just as microscopes expanded our vision beyond the naked eye, AI broadens our capacity to detect and comprehend patterns hidden in millions of data points. Such insights may not arise from a single patient-physician visit, but from broadly applicable patterns delivered efficiently to large patient populations.
Tools already exist where subtle, weeklong changes in heart or respiratory rate can signal impending cardiac or respiratory decompensation; where the tone and inflection of voice can quantify depression; where gait analysis can predict risk for falls. Chronic illnesses transform from ominous, unstoppable forces into manageable, closely watched conditions which, more importantly, offer vast opportunities for intervention. This is the power we stand on the threshold of wielding. A rudimentary example is the GPS, a limited AI we use every day—it prevents mistakes before they happen and helps course-correct when we make one. Prevention is powerful; wrong turns cost time and fuel, just as late interventions cost health. AI could detect atherosclerosis early by analyzing subtle shifts in our arterial pressure waves, prompting lifestyle changes long before medication is necessary. These “digital therapeutics” shift diagnosis and treatment from reactive to preemptive.
Personal health AI's can act as part of physician-led teams, offering coaching and guidance to patients daily. Chatbots are already

From the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care and medical negligence defense attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth.
Put our experience to work for you.
Sturgill, Turner, Barker & Moloney, PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ STURGILLTURNER.COM
offering emotional support and companionship for some. While it may be unsettling to trust genuine comfort to a machine we might view as “soulless,” medicine has a long history of championing calm objectivity. Sir William Osler—often called the father of modern medicine—encouraged physicians to cultivate “Aequanimitas,” or steady composure, arguing that such poise best serves patients’ emotional and clinical needs. AI could further this vision, not by replacing human empathy, but by offering consistent, round-the-clock support that complements and extends what clinicians provide.
Despite the frustration many physicians feel about current EMR systems, a physician’s greatest asset remains the analog mind— adapting nuanced knowledge to each unique case rather than pigeonholing ideas. Where EMRs and the codification of medicine often reduce us to data-entry technicians, AI can augment our skill by letting us scale our insights and assume more creative roles as conceptual architects.
Indeed, AI can be used to create art or music, but it “creates” by building on past masterpieces—without original human creativity, it has no foundation. As we develop AI for medicine, a democratization of protocols and solutions will emerge, letting innovators shine with scalable solutions to challenges we often resign to failures as a result of compliance. AI offers an additional resource physicians can wield in guiding patients toward health-based care rather than care based on illness.
Without the microscope, we might still be mystified by infections. Now, as we grapple with streams of patient data, AI offers the chance to detect metaphorical “infections” in the form of chronic diseases before they flare out of control. This empowers earlier interventions, guided in real time by scaling our collective knowledge and insights. Human creativity remains central to innovation. By integrating our individual ideas with the scalable power of AI, we can shape a future in which care is more
proactive, personal, and profoundly effective— an era worthy of Semmelweis, Pasteur, and every trailblazer who challenged medicine’s dominant paradigms.
To respond or offer a different opinion, contact Gil Dunn at (859) 309-0720 or gdunn@md-update.com

has found his model of
BY GIL DUNN
LOUISVILLE Diagnosis isn’t always simple. Sometimes it takes time, experience, analysis, and trial and error. For Carl Paige, MD, his decision to become a doctor was spot on, but once immersed in the conflicting and confounding interests of the U.S. healthcare system, he became increasingly frustrated and realized he wasn’t doing the work he wanted to do. That was his diagnosis. The cure was creating a new way of providing healthcare.
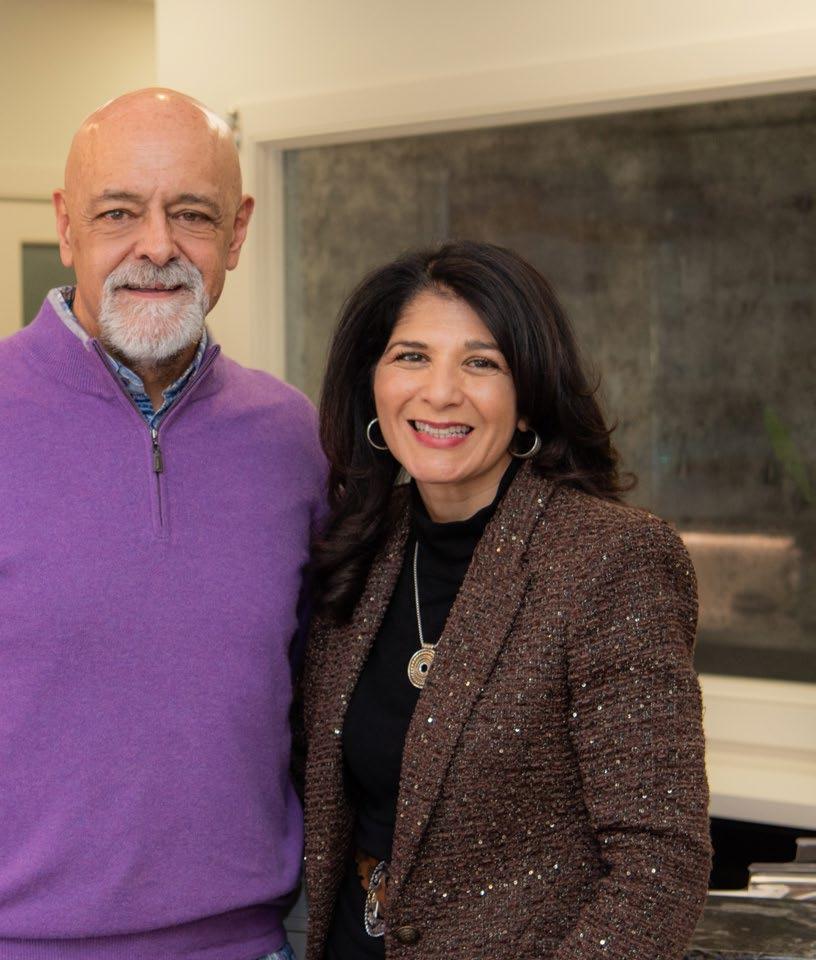
“I feel the way we have now is a better way to take care of patients,” says Paige, who co-owns Medical Transformation Center in Louisville with his wife, Terri. “We don’t bill or collect anything from any insurance company. I tell my patients, I work for me to feed my family, and I work for you to make you healthy. Those are my commitments.”
Paige was born in Homestead, Florida, but his family moved to Kentucky when he was young. He grew up in Muhlenberg County, where he and Terri would become high school sweethearts.
Planning to be a doctor all along, Paige attended the University of Kentucky for his undergraduate work, as well as medical school at the UK College of Medicine, before completing his residency in internal medicine and pediatrics at the University of Louisville in 1992.
Soon thereafter, he set up practice in Oldham County, where there was no full-time pediatrician at that time. The rural setting proved to be welcoming, and Paige’s patient base quickly expanded from pediatrics to the whole family.
“Within a year we were ridiculously busy,” Paige says. “Back then I could see 50-60 patients a day. It was the rural area between La Grange and Cincinnati, where there was essentially no healthcare. I was their primary
care doctor and had to be their front-line specialist. The patients didn’t want to go another hour into the city to see somebody.”
Initially, the practice consisted of Paige, a nurse, and Terri, who did the billing and administration, such as it was back then. The practice was thriving and grew to include other physicians, but it wasn’t fulfilling for Paige. He found insurance companies’ billing tedious, and needing prior-approval for tests or treatments was obstructive. He believed there had to be a way he could practice medicine the way he felt was right. So, he sold the practice and started Medical Transformation Center (MTC) in 2013.

Nutrition and patient education are vital parts of health and wellness at Medical Transformation Center
“I went into the cellular medicine space,” Paige says. “How could we make the cell run efficiently and be more flexible from an energy standpoint? If you can achieve that, the organism will function better. A lot of the information that we use in cellular medicine comes from the human performance and athletic world. They translate well to aging and chronic health problems. Given the right tools, in most cases, the body can heal itself, especially if you’re more active.”
With Terri as his co-partner and CEO, Paige has found success and, more importantly, satisfaction at MTC. He has patients in 38 states. They come to see him in person once a year, and any other appointments are conducted remotely.

“I didn’t know I would end up here, but I knew where I was, and where the healthcare system was and I didn’t like it,” Paige says. “I didn’t think it was performing optimally for my patients or intellectually for me.”
“It was an organic evolution in how we changed the business model,” Terri says. “We don’t bill, code, or collect insurance payments at MTC. We have a membership fee, but we are not a primary care practice. We refer for labs and tests where people can use their insurance, but we got out of that system so Carl can have the latitude to use every tool that he has.”
Paige treats a variety of conditions by focusing on different ways that the body heals itself and how patients can tap into those natural remedies. For many of his patients, it’s not a matter of being healed, but more a matter of optimizing the body’s healing powers and potential.
“We tell patients up front that they should maintain their primary care physician relationship,” Paige says. “We don’t do cough, cold, fever anymore. I think other physicians thought we would steal their patients, but we want patients to keep their primary care. We
are just here to offer access to types of care that you cannot offer in that setting.”
Approximately 64 percent of MTC’s patients are women. The primary reasons patients come to MTC are not gender based, however. Instead, it tends to be a desire to maximize the body’s potential in terms of performance, healing, and aging.
“It’s not anti-aging, it’s optimized aging,” Paige says. “People want to be at their top form.”
Terri and Carl Paige with their oldest son, Jason, and Carl’s mother Jane, who died in 2015, at Carl’s graduation from the UK College of Medicine in 1988. Terri and Carl have 8 children and 3 grandchildren.
To help them get there, Paige educates his patients on the human anatomy, particularly at the cellular level.
“The science is there to support this,” Paige says. “We approach it from what’s wrong at the cellular level, the immune level, and the gut level and address those issues to get patients optimized.”
Patients are initially educated on gut health and the environmental factors that affect the body.
“Lifestyle, nutrition, and exercise are always the base of everything,” Paige says. “Then

it’s gut health and stabilizing and optimizing immune function and energy production at the cellular level. Once you clean all that up, then you get into what is specifically broken and didn’t get better. It may be nutritional supplementation, a specific diet, or limitations in food you are exposed to. We use traditional prescription medicines and a lot of repurposed pharmaceuticals that have many benefits when you understand the mechanism of how they actually impact the cell.”
Paige further educates his patients on how their bodies function. He helps them identify their paths to managing and maximizing their health.
“You’re basically modifying how your genome interacts with the environment,” Paige says. “That’s going to be food, lifestyle, and exercise. Then you get into the bio-regulators and small molecules and peptides that literally enhance the signal.”
MTC’s happy patients have spread the word, leading to MTC’s growth and probable expansion. With help from Terri, who is a certified life coach, Paige is helping teach other practitioners the things he has learned. He hopes others will experience the same success he has seen in his own practice.
“I get personal satisfaction from being able to offer these things and to have patients come back in and say they have never felt so good or that their symptoms are so much better.”
There is always a better way. And Carl Paige is glad he found it.
Patient receives a stem cell facial performed by Dr. Carl Paige.

BY LIZ CAREY
UofL Health endocrine surgeon Mahsa Javid,
MB, has multiple roles and enjoys all of them
LOUISVILLE For Mahsa Javid, MB, BChr, MA, DPhil, FRCS, FRCSC, delving into the causes of endocrine pathologies is a way to help her patients avoid surgery.
Javid, an academic endocrine surgeon at UofL Health, not only researches endocrine issues, but also teaches about them and performs the surgeries to treat them. Helping patients address issues earlier, and helping her students understand the disparities in healthcare can help save lives, she says.
Born in Iran, Javid’s family moved to England in the 1970s as the country fell into turmoil before the Iranian revolution in 1979.
Javid’s father was a district attorney and economist and he and his wife decided to take the family where their children could get a good education, she says. Javid earned her undergraduate, medical, and master’s degrees from the University of Cambridge. In 2001, she moved to the University of Oxford to complete basic surgical training, higher specialist training, and general and emergency surgery fellowship training and to earn her doctorate in biomedical and clinical sciences.
In 2014, she moved to the United States to do a specialty fellowship in endocrine surgery at Yale University under the supervision of Robert Udelsman, MD.
Javid’s brother, Babak Javid, MD, also became a doctor and is a world leading infectious disease physician scientist at the University of California, in San Francisco.
“During the year of my fellowship, basically all I did was endocrine surgery,” she says. “I’m highly specialized. All we did week in, week out — 400 cases over the year — was just endocrine surgeries.”
Javid’s specialties include the management of benign and malignant endocrine disease,

Mahsa Javid, MB, endocrine surgeon, UofL associate professor, endowed chair in surgical endocrinology.
complex cases including re-operative surgeries, conventional open and minimally invasive procedures for neck procedures, and posterior retroperitoneoscopic approach for adrenal disease.
Choosing endocrine surgery came from her desire to represent women in the field of surgery and her experiences with one of her mentors, Greg Sadler, MD, with whom she worked at the University of Oxford.
“I went into surgery itself because I felt that there was an under-representation of women in the field,” she says. “Then as I was doing all that training, I worked under Dr. Sadler who is probably one of the best surgeons I’ve ever had the privilege of being affiliated with, and he was an endocrine surgeon. As I was working with him, I began to understand the complexity of what he does and the intricacy of the surgeries, as well as all the medicine and physiology that go along with endocrine surgery. That’s why I chose endocrine surgery.”
It was her work with Sadler and her doctoral supervisor, Rajesh Thakker, MD, that also made her want to teach.
PHOTO BY GIL DUNN
“They really taught me how to diagnose, how to think, how to do proper research, how to present properly at the top level, and that’s something that really motivates me to pass on as well,” she says. “Amongst all this surgery, I’m also an educator, and I take that job very seriously. There are students, undergrad and post grad; there are trainees, residents, fellows, all of whom come through our department, and I feel it’s an honor to take on all that responsibility of training the future generations.”
As a researcher, Javid is currently looking at thyroid cancer and how metabolites accumulate in the body and potentially contribute to tumorigenesis, and what is the mechanism in them that contributes to thyroid cancer formation.
When it came time to practice medicine, she felt Louisville was the right place to focus on her endocrine specialty.
“There are only a few jobs a year that are advertised if you want to stay academic in endocrine surgery and want to pursue meaningful research,” she says. “There was an opening at UofL Health, and I felt it was a field that the institution was interested in focusing on, and it gave me the opportunity to really grow a program.”
Naturally, her weeks are busy ones. Javid says she typically has one or two days of surgeries and a full clinic day to see referred patients. On days when she is not with patients, she’s doing translational and clinical research and meeting with students and trainees to help them with their research.
The types of diseases she deals with center around multiple areas: the thyroid, parathyroid and adrenal, and other neuroendocrine tumors in the abdomen. That means the patient group also varies widely, she says.
“The age group is all encompassing. I see all ages, including pediatrics and patients into their late 80s and 90s who are fit and well enough,

but their condition requires my help. My patients are predominantly women. I tend to get a lot of patients from the Black population. And I’m also seeing a lot of immigrants. So, I really do see a wide variety of race, socio-economic status, job status, insurance status — I tend to see more of the underserved population than most other specialties.”
Research into the causes or contributing factors for endocrine pathologies in underserved communities and whether factors like the environment, social, economic status, access to healthcare, and race, contribute to endocrine

pathologies ending up requiring surgery, is one of her ongoing interests, she says.
“It’s irrefutable that there are disparities in healthcare, and the short-sighted manner in which those disparities are dealt with actually leads to inefficiencies for everybody,” Javid says. “In the end it negatively impacts the entire healthcare system.”
One thing Javid sees frequently is patient delays dealing with their presentations,



which leads to a later diagnosis and more complications. Typically, by the time patients see her, their delays mean they are more likely to need surgery.
“There’s a lot of fear and apprehension, especially around needing surgery. So, what I’m trying to do is increase the visibility of my presence and willingness to see people,” Javid says.
To do that, she’s focused on opening a clinic in the West End of Louisville to have a presence where there is a high patient population. That presence, she believes, may help with other non-endocrine diseases as well.
“I think one way to improve the entire system is to be more available and to be where there are higher incidences of all types of related diseases that people may not think of, for example, hypertension or diabetes and obesity. All these things are connected to endocrine-related problems as well.”
Focusing on preventative measures, and helping underserved communities feel comfortable reaching out early with their concerns benefits more than just the patient, she says. “It really would make such a huge difference, and I think it would bring healthcare systems cost savings as well,” she says.
Delving into the links between what is going on with patients and how that creates endocrine-related pathologies is what she loves most though.
“The whole point about research is that we don’t know something, and we’re trying to know it, and that is the discovery aspect,” Javid says. “It’s innovative, and we’re trying to bring about positive changes. So, it’s something that can change the field. My priority will always be the patients who are under my care, but I think ultimately getting the research out is most exciting.”




BY LIZ CAREY
Pulmonologist at Norton Healthcare sees long-term COVID and environmental factors in her practice.
LOUISVILLE The profound impact COVID-19 had on patients not only colored the view Samantha Baah, MD, had on her specialty as a pulmonary and critical care physician, but continues to impact her practice, she says.
Baah, a pulmonary and critical care specialist with Norton Pulmonary Specialists, was completing her pulmonary and critical care fellowship at the University of Rochester Medical Center in upstate New York, when the COVID-19 pandemic hit. As she began her career at Norton Healthcare in mid-2021, she found herself working through the second wave of the pandemic.
“It was devastating what we were seeing, and it taught me a lot,” Baah says. “The amount of collaboration and camaraderie and teamwork in the ICU… it was quite remarkable. It would be me, a respiratory therapist, and one of the bedside nurses. The amount of resuscitation these patients needed every day… it's something that I often think about and reflect upon. It was an unfortunate time, but it really taught me a lot about healthcare and teamwork and how this is what we were put on this earth to do.”

“I am always inspired by the patient.”- Samantha Baah, MD
she took her position at Norton Healthcare in pulmonary and critical care and he took a position in interventional radiology at UofL Health.
Finding solutions to extend patients’ quality of life is a calling, she says.
One of eight children, Baah was the first in her family to graduate high school and college. After earning her medical degree from the American University of Antigua College of Medicine, she completed her internal medicine residency at Cooper University Hospital in South Jersey, followed by her pulmonary disease and critical care fellowship at the University of Rochester in upstate New York.
In 2021, Baah and her husband, Nana Ohene Baah, MD, moved to Louisville where
“When I first started, I had a sweet little lady in her late 60s who was on two liters of oxygen around the clock. She came to me for a second opinion,” Baah says. “She had pulmonary fibrosis and COPD and was told to ‘put her affairs in order’ because she was told she was dying. I was able to optimize the treatment for her COPD and sent her for some additional testing. By the time I saw her the second time in clinic, we had removed her from the oxygen, and with treatment for her COPD, she was able to get her life back.”
Living in Kentucky where pulmonary issues are more profound, she sees an inter-relationship between pulmonary diseases and the environment.
“We are here in the Ohio River Valley where there's a lot of granulomatous disease with acute and chronic changes in the lungs. This patient population is very unique and can be challenging,” Baah says. “When I was in New York I would see what I thought were rare manifestations of granulomatous disease and would want to write the case up and get it published because we didn’t see it as often. When I came here, I often see various clinical manifestations of granulomatous disease, some life threatening. I'm constantly learning how complex this patient population is.”
Baah didn’t start out in pulmonology, however. Pulmonology as a specialty chose her as much as she chose it, she says.
“When I was in medical school, it was unclear to me what my calling in medicine was. At one point I wanted to do OB-GYN, at another point I wanted to do surgery, then GI,” she says. “But there was just something about seeing a patient who had a chronic pulmonary condition that really sparked my interest. Patients with shortness of breath from chronic lung disease often feel they are prisoners to their own bodies. We take breathing for granted every single day, but these patients are crippled by it. I wanted to find ways to help these patients breathe better, live longer, and truly be free from the crippling effects of their chronic pulmonary condition.”
The need for pulmonologists is increasing, she says. “I think with COVID and other
respiratory viruses, there can be both short- and long-term consequences in the lung. Some of these patients can develop bronchitis, inflammation in the airways and lung tissue and even some scarring of the lungs. “I’ve had patients in clinic several months from their viral infection who still have significant symptom burden. Viruses may alter the airway and cause patients to suffer from respiratory symptoms like shortness of breath and cough that they never had before.”
And those issues are affecting younger patients, something she attributes to a changing environment. “It's a common misconception that only smokers have lung disease. We see a wide array of lung disease, in the very young, the very old, and everyone in between. By the time most patients see a pulmonologist, they have been struggling for years.”
Pulmonology is adapting to new technologies using robots and artificial intelligence to assist in the early detection and diagnosis of lung cancer, Baah says. “Previously, there were spots in the lung that were too small to biopsy or in a location we simply couldn’t get to safely. With robotic assisted bronchoscopy, we can reach areas in the lung we couldn’t reach before.”
“With robotic assisted bronchoscopy, if there's a lesion that looks suspicious, we now have the technology to get a tissue diagnosis. The patient is sedated while a 3.5 mm catheter is inserted through an endotracheal tube. We control this catheter to move through the tiny airways of the lung to reach the lesion or nodule of interest,” she says. “Most times we are able to provide patients with preliminary information the day of the procedure.”
Baah works with GSK with inhalers for COPD and teaches robotic bronchoscopy with Intuitive Surgical for robotic bronchoscopy.
In Baah’s opinion, AI will be an asset to building an incidental pulmonary nodule program to capture lung cancer patients earlier. “Often times patients with lung cancer don’t present with any symptoms of lung cancer until their disease has progressed to a more advanced stage. With AI, we are able to capture patients with incidental pulmonary nodules found on imaging studies done for unrelated reasons in hopes of capturing and diagnosing patents with lung cancer sooner.”
Baah says that her passion is providing those patients with pulmonary disease the hope of a brighter future. Too often, she says, patients come to pulmonologists when they are late in their diagnosis.
“When patients have end-stage lung disease, we still have something to offer; having end-stage lung disease is not a death sentence,” she says. “If we can catch patients earlier, we can get them on treatment plans to decrease risk of progressive disease and discuss ways to improve morbidity and mortality. Even when patients have lost hope, I feel there is always something that we can offer to optimize their treatment.”
“I am always inspired by the patient. There's always hope. My goal is to connect with my patients, provide them with an understanding of their lung disease, and ensure they received quality, evidence-based pulmonary care,” says Baah.

our patients. Patients in southeastern Kentucky need only to travel to London for access to surgeries with this advanced technology, which provides a quicker recovery time than traditional surgical procedures,” says Yanes.
Like other internal medicine specialties, general surgeons see the effects of poor health habits, lifestyle, and lack of access to healthcare in their patients. Obesity can complicate abdominal surgery, says Capal, but the da Vinci robot is an asset with the 360° articulation in the robot’s hands. “The robot can get to places to make cuts in a way that a straight laparoscopic tool cannot,” he says.
Capal says that unfortunately he is seeing cancer in younger patients, in their 20s, 30s and 40s, a trend that is reflected in national statistics. “I did cancer tumor resection surgeries on a 20-year-old and a 30-year-old last year,” he says.

A particular life-saving surgery occurred when a female car crash victim was brought into his OR. “She was literally dying in front of me on the operating table from massive abdominal injuries,” he recalls. “We were able to surgically stabilize her and then helicoptered her to UK trauma, where she survived and recovered. I found out recently that she is related to one of our staff members. That made her story personally very rewarding for me,” says Capal.
When discussing elective, or even emergent, surgeries with his patients, Capal says straightforward, easy to understand, and open communication is key.
"I tend to take extra time talking to my patients. And it is my duty as their surgeon to be able to break down complex medical and surgical problems and simplify them into terms they can understand. I try to explain what is going on, why it's going on, and what we can do to fix it. We need to have a common understanding of the decision to proceed with
surgery. After our conversation, I frequently ask my patients to explain, in their own words, what surgery we will be doing and why. Because I believe if a patient cannot do that, and does not understand what the basic problem is and the steps we can take to fix it, then I have failed them as their doctor."
“How grateful my patients are to have top quality care close to home is my motivation. It’s why I’m here, doing what I love to do,” says Capal.
Nicholas Capal, DO General Surgery 1025 Saint Joseph Lane
606.330.2370
A comprehensive approach

BY NIRVANA NAWAR, MHA, KENTUCKY LUNG CANCER SCREENING PROGRAM ADMINISTRATOR
FRANKFORT Team Kentucky knows that building healthy communities is one of the most important things we can do for future generations. The Kentucky Department for Public Health and the Kentucky Lung Cancer Screening Program are committed to strategies that promote lung health for Kentuckians. With the increasing prevalence of lung-related conditions such as chronic obstructive pulmonary disease (COPD), asthma and lung cancer, it is imperative for the medical community to prioritize lung health through prevention, early detection, and effective case management.
The key factors that influence respiratory well-being and presenting evidence-based strategies to mitigate the impact of lung diseases, enhance our collective capacity to deliver superior care and improve patient outcomes.
Lung cancer is the leading cause of cancer death globally, accounting for approximately 1.8 million deaths annually. In the United States, lung cancer is responsible for more deaths than breast, prostate and colorectal cancers combined. According to the American Cancer Society, an estimated 238,340 new cases of lung cancer were diagnosed in 2023, with around 127,070 deaths attributed to the disease.

Nirvana Nawar, MHA
Kentucky continues to face significant challenges regarding lung cancer incidence and mortality. The state has the highest rate of new lung cancer cases in the nation, with 84.9 per 100,000 individuals, compared to the national average of 53.6 per 100,000.
According to the American Lung Association's 2024 "State of Tobacco Control" report, Kentucky has an adult smoking rate of 21.4% and a high school tobacco use rate of 29.7%. These rates are among the highest in the nation, indicating a significant public health concern.
While Kentucky is a leader in the nation in lung cancer screening rates, this success is just a small step forward, and significant efforts are still needed to combat the state's high smoking rates and to improve overall lung health. Efforts to address lung cancer in Kentucky
have centered on raising awareness, expanding screening programs and encouraging smoking cessation initiatives.
Although challenges persist, early detection and advancements in treatment have led to improved lung cancer survival rates in Kentucky.
The most significant risk factor for lung cancer is smoking, which accounts for about 85% of all cases. However, non-smokers can also develop lung cancer due to exposure to secondhand smoke, radon gas, asbestos and other carcinogens. Genetic predispositions and a family history of lung cancer also contribute to increased risk.
The decline in smoking rates over recent decades has led to a reduction in lung cancer incidence. Yet the disease remains a major public health challenge, particularly among populations with high smoking rates or limited access to healthcare. The Centers for Disease Control and Prevention (CDC) emphasizes the need for continued public health efforts to reduce smoking and promote healthy behaviors to lower the burden of lung cancer.
Promoting lung health requires a multifaceted approach that includes public health initiatives, policy changes and individual actions.
• Reducing Air Pollution: Implementing policies to reduce emissions from vehicles, industries and other sources can significantly improve air quality. Encouraging the use of public transportation, renewable energy
sources and green spaces can also contribute to healthier environments.
• Tobacco Control: Comprehensive tobacco control measures, including smoke-free policies, cigarette and e-cigarette taxation and public education campaigns, have proven effective in reducing smoking rates. Providing support for smoking cessation programs can help individuals quit smoking and improve their lung health.
• Addressing High Radon Levels: In promoting lung health, addressing radon exposure is vital, especially in Kentucky, where many areas exceed the EPA's action level. As a leading cause of lung cancer among non-smokers, increasing awareness and encouraging radon testing and mitigation in homes, schools and workplaces can significantly reduce risks and improve lung health statewide.
• Vaccination and Infection Control: Vaccinating against respiratory infections like influenza and COVID-19
can prevent serious lung complications. Promoting good hygiene practices and timely medical treatment for infections can also safeguard lung health.
• Regular Health Check-ups: Routine health check-ups and lung function tests can help in the early detection and management of lung diseases. Individuals with risk factors or symptoms should seek medical advice promptly.
Early detection of lung cancer through screening is crucial for improving survival rates. Low-dose computed tomography (LDCT) screening is the most effective method for detecting lung cancer at an early stage, when it is more likely to be treatable. The National Lung Screening Trial demonstrated that LDCT screening reduced lung cancer mortality by 20% compared to chest X-rays among high-risk individuals.
The U.S. Preventive Services Task Force recommends annual LDCT screening for adults aged 50 to 80 years who have a 20-packyear smoking history and currently smoke or have quit within the past fifteen years. This recommendation underscores the importance of identifying high-risk individuals and encouraging them to undergo regular screening.
In 2023, the Kentucky Lung Cancer Screening Program Committee developed a strategic plan to increase lung cancer awareness, reduce mortality and morbidity and lower the costs of treatment. By expanding screening efforts and raising public awareness, the program aims to detect lung cancer early, improve survival rates and reduce the financial burden of care, especially for underserved populations. Healthcare professionals, policymakers and individuals working to improve their own health are all taking important steps toward protecting lung health and addressing lung cancer. Thank you for being part of this important journey.
ing for ticks in their natural environment. Surveillance is typically conducted in early spring through summer months by students with the UK-Ent program and members of the Public Health Protection and Safety (PHPS) branch with KDPH. As of 2024, 19 Kentucky counties have been identified with established populations of blacklegged ticks.
In October, 2024, KDPH collaborated with the Centers for Disease Control (CDC), UK-Ent, and the state and national parks systems, to complete a week of tick surveillance in select Kentucky parks near the northern and southern borders. The primary goal was to see how many blacklegged ticks we could find and if they carried any pathogens. We surveyed 29 sites in 15 counties and collected 162 blacklegged ticks. 160 ticks were tested by the CDC for pathogens, including Borrelia burgdorferi (Lyme), Borrelia miyamotoi (hard tick relapsing fever), other Borrelia species, ehrlichiosis, and anaplasmosis.
Forty ticks tested positive for Borrelia burgdorferi (Lyme) and 2 ticks tested positive for Borrelia miyamotoi (Hard Tick Relapsing Fever[5]), the first identification of this pathogen in Kentucky. These results indicate that blacklegged ticks and tickborne disease pathogens, including Lyme disease, are present in Kentucky. Continued efforts such as this will enhance surveillance capacity and improve data to inform Lyme Disease education to the

public of and enhance communications with healthcare providers about the increasing risk of Lyme and other tickborne diseases.
Collaboration with healthcare providers is crucial to improving surveillance of human cases of Lyme disease; reporting of this disease can be complicated. Reportable disease cases are classified based on case definition criteria that has been standardized nationally by the CDC’s National Notifiable Diseases Surveillance System (NNDSS). For Lyme disease, the case definition is very specific for both clinical and laboratory criteria. Clinical criteria must include one of the following as reported by a healthcare provider: erythema migrans rash (aka bullseye rash), or involvement of the musculoskeletal, nervous, or cardiovascular system (see the NNDSS Lyme case definition page[6] for more details). These clinical manifestations must be clearly described in the medical records, otherwise the case will not meet the appropriate criteria to be classified as a confirmed or probable case. This is crucial to accurately assess the impact of Lyme disease on Kentuckians and communicate data trends to our healthcare providers. Increased awareness and understanding of Kentucky-specific Lyme disease data will help ensure patients receive timely
treatment to avoid the long-term and more severe symptoms that can occur with Lyme disease.
Ultimately, the shared goal of public health surveillance and healthcare is to protect and improve the health of our communities. For Lyme, or any tickborne disease, the most important messages are to prevent tick bites and to seek early treatment. KDPH will continue to make gathering enhanced and timely data a primary goal to increase awareness and inform public health activities.
Morgan Smith, MPH, CPH, vector-borne disease epidemiologist, Kentucky Department for Public Health, morgans@ky.gov, 502.545.9286
RESOURCES
1. L. Eisen, R.J. Eisen. “Changes in the Geographic Distribution of the Blacklegged Tick, Iozdes scapularis, in the United States” Ticks and Tickborne Diseases, 14 (2023)
2. Ohio Department of Health. “Estimated Distribution of Blacklegged Ticks in Ohio Map.” Available at: https://odh.ohio.gov/know-ourprograms/zoonotic-disease-program/media/blacklegged-tick-distribution-map
3. West Virginia Department of Health. Tickborne Diseases, “Blacklegged Tick Species Distribution.” Available at: https://oeps.wv.gov/ arboviral/documents/tick/data/ixodes_scapularis_2019.pdf
4. Kentucky Department for Public Health. “Kentucky Environmental Health Tracking, Tickborne Disease in Kentucky.” Available at: https://storymaps.arcgis.com/stories/ d6d2533ab2cf4e30b037eb4e9e3838c4
5. Centers for Disease Control and Prevention. “About Hard Tick Relapsing Fever (HTRF).” Available at: https://www.cdc.gov/ relapsing-fever/about/about-htrf.html
6. Centers for Disease Control and Prevention. “Lyme Disease (Borrelia burgdorferi) 2022 Case Definition.” Available at: https://ndc. services.cdc.gov/case-definitions/lyme-disease-2022/


BY JAN ANDERSON, PSYD, LPCC

I didn’t take the traditional path to becoming a therapist.
I didn’t start in social services. I didn’t work in a nonprofit. I landed in the corporate world out of necessity.
I graduated into a recession with a psychology degree and zero job prospects. So, I pivoted. I joined the business world — an entry-level position in a big company.
And honestly? It was the best thing that could have happened to me.
Real-world business experience grounded me. It gave me practical skills. It taught me how to drive results. And, ironically, it taught me more about human nature than my psychology degree ever did.
The business world shaped the way I approach therapy today—especially when it comes to resilience.
I saw firsthand how high achievers navigate career challenges, relationship hurdles, and personal roadblocks.
The pressure to perform was relentless. The stakes were high. And many people were barely holding it together—burnout, imposter syndrome, perfectionism, you name it.
That’s when I started looking for ways to manage stress.
I took a yoga class (before yoga was trendy). For the first time, I remember feeling truly relaxed. So, I kept going back. I didn’t talk about it much—no one at work wanted to hear about something as “weird” as yoga.
My colleagues were busy pursuing MBAs and climbing the corporate ladder. I wanted to excel, too. But I trusted my instincts and started a graduate program in counseling psychology.

When it came time for internships, I didn’t fit into the usual social service placements. So, I landed in an executive outplacement firm, coaching professionals who had just lost their jobs.
I helped them dust themselves off, rebuild their confidence, and prepare for their next opportunity. Learning how to network, build a resume, and interview effectively was resilience in action—before I even knew resilience would become my specialty.
Then the stock market crashed. My job was eliminated. And suddenly, I had to apply my own career counseling advice—to myself.
That challenge led to a better-paying job, more opportunities, and a promotion—right after having a baby. I even developed a product that earned me a special bonus from the board of directors.
But the pressure never stopped. The expectations were sky-high. So, I deepened my mindfulness practice, adding meditation to my routine. Then—another economic downturn. This time, I was told my job would now require 70% travel nationwide.
Ever tried explaining that to a five-year-old? So, I jumped off a cliff.
Instead of taking the assignment, I took a severance package, got my counseling license, and started building what would become LifeWise by Dr. Jan.
No corporate safety net. No guarantees.
Fortunately, I had no idea what I was getting into—starting a counseling practice that didn’t accept insurance, with no name recognition or contacts. On top of that, I was incorporating mindfulness-based practices before “mindfulness” was a buzzword.
In my spare time (I had a lot at first), I did volunteer grief counseling at a progressive local hospice. They asked me to incorporate mindfulness into their grief support groups—and that program won a national award.
I started the seven-year journey of my doctoral thesis, focusing on resilience. I discovered that building resilience is not a one-size-fits-all approach. I began studying five evidence-based ways people learn to get a grip, get back up, and keep going when life knocks them down.
Then, I made a huge business mistake.
I moved into an office before my landlords fulfilled their promises. I moved out. My landlords sued me (unsuccessfully, whew!) I had to run my practice from home temporarily.

Then, another challenge: A major corporation in town told me, “We never refer to a therapist whose practice is in their home.” That stung.
Until I realized I had the perfect setup:
9 A comfortable, confidential space in a nice neighborhood.
9 A central location—accessible from anywhere in town.
9 No waiting room. No sign out front. Total privacy.
So, I flipped the script. I reframed my shame attack into a snappy new marketing strategy. Soon, I started booking more clients—including some from the company that dumped me.
Through my own personal and professional challenges, I’ve learned that resilience isn’t about being unbreakable—it’s about being adaptable. It’s about learning to recover, recalibrate, and move forward, even when life doesn’t go as planned.
9 Resilience isn’t about pushing through at all costs. It’s about knowing when to persevere and when to pivot.
9 Building resilience doesn’t require digging through your past. You can start exactly where you are, right now.
9 Resilience is personal. Some people need neuroscience-backed strategies to rewire thought patterns. Others thrive with

mindfulness-based practices or solutionfocused problem-solving. The key is finding the right fit for you.
As I applied these principles to my work, I saw how they resonated with high-achievers, executives, and professionals — many of them couples — looking for practical, results-driven strategies.
My boutique practice grew as my column in MD-Update attracted more healthcare professionals, sending me referrals or seeking for themselves more resilience and less stress at work or home.
My practice has since expanded into another unexpected and challenging area: the growing number of parents estranged from an adult child.
My resilience-oriented approach has attracted a national audience of parents searching for a way forward and is the basis of my upcoming book, Embracing Space: A Parent's Guide to Navigating Low or No Contact Estrangement.
Resilience isn’t just for the rare few who are naturally tough. It’s a skill anyone can develop with the right tools, mindset, and support.
I’ve seen firsthand why my Counseling with a Coaching Edge approach resonates with high achievers, couples, and estranged families alike: It’s not about endlessly analyzing problems—it’s about solving them.
If you’re ready to move forward, build resilience, and take action, let’s talk:
9 Solution-Focused.
9 Evidence-Based.
9 Results-Oriented.
Your next step starts here. Schedule a consultation at www.DrJanAnderson.com or call 502.426.1616.

Andrew Cocieru, MD
LEXINGTON Andrei
Cocieru, MD, has joined CHI Saint Joseph Medical Group – Surgery in Lexington bringing extensive general surgery and surgical oncology expertise.
Cocieru specializes in hepato-pancreato-bili-
ary (HPB) surgery, addressing complex conditions affecting the liver, pancreas, and bile duct. Originally from Moldova, Cocieru discovered his passion for healthcare early in life.
“My mom was a family physician and served as an example to me,” says Cocieru.
Cocieru specializes in the surgical management of liver, pancreas, and bile duct diseases, offering both open and minimally invasive, laparoscopic procedures.
LONDON Saint Joseph London has earned The Joint Commission’s Gold Seal of Approval® for Certification in Spine Surgery, the fourth hospital in Kentucky to earn the certification. The hospital received this certification by demonstrating continuous compliance with its performance standards. The Gold Seal is a symbol of quality that reflects a healthcare organization’s commitment to providing safe and quality patient care.
“Providing safe, high-quality care is at the center of everything we do, and this certification reflects our unwavering commitment
to excellence and enhancing access to advanced clinical care close to home,” said John Yanes, president, Saint Joseph London.
“Earning this certification is a big milestone for Saint Joseph London and, more importantly, for our patients,” said Vincent DePalma, MD, spine surgeon, Saint Joseph London. “It shows that we’re delivering the highest level of spine care, using the most advanced surgical techniques and main taining a strong focus on patient safety.”
Cocieru earned his medical degree in Chisinau, Moldova. After moving to the United States, he completed his surgical residency at Danbury Hospital in Connecticut and pursued a research fellowship at the Cleveland Clinic in Ohio. He then completed advanced training at Duke University Medical Center to further hone his hepato-pancreato-biliary surgery skills. Cocieru is board-certified in both HPB surgery and general surgery.













LOUISVILLE According to the organizers of the 2025 Kentuckiana Heart Ball, “It was a huge success, bringing together 500 attendees for an evening dedicated to heart health and community impact.” With live and silent auctions and pledges, the event raised $200,000 to support the American Heart Association’s mission.
A spokesperson said “Our auction exceeded last year’s totals, thanks to the generosity of our supporters. It was an inspiring night filled with meaningful stories, celebration, and a shared commitment to fighting heart disease and stroke.”
The Kentuckiana Heart Ball was March 8 at the Downtown Marriott in Louisville.

WEDNESDAY, MAY 21
University Club of Kentucky
4850 Leestown Road, Lexington, KY
12:00p Registration/Lunch
1:00p Start
SCRAMBLE format
Lunch & Awards Dinner
$200/player or $800/foursome
ALL PROCEEDS TO BENEFIT MEDICAL NON-PROFITS IN THE LEXINGTON AREA LEXINGTON MEDICAL SOCIETY

Presented by

LUNCH SPONSOR

CONTRIBUTING SPONSORS