

Cancer Care in Central Kentucky
Saint Joseph Health - Cancer Care Center provides people-centered care in a newly renovated space
ALSO IN THIS ISSUE
RADIATION THERAPY AT ARH
Q&A WITH DR. MARK EVERS, UK MARKEY CANCER CENTER
4D CLINICAL TRIAL AT BAPTIST HEALTH HARDIN
THORACIC SURGEON AT BAPTIST HEALTH LOUISVILLE


BREAST SURGERY & RECONSTRUCTION AT NORTON HEALTHCARE
THYROID CANCER CARE AT UK HEALTHCARE
GI CANCER SURGERY AT UofL HEALTH



Editorial topics and dates are subject to change
ISSUE #162 (February)
HEART & LUNG HEALTH
Cardiology, Cardiothoracic Medicine, Cardiovascular Medicine, Pulmonology, Sleep Medicine, Vascular Medicine, Bariatric Surgery
ISSUE #163 (April)
INTERNAL & EXTERNAL SYSTEMS
Dermatology, Endocrinology, Gastroenterology, Geriatric Medicine, Internal Medicine, Integrative Medicine, Infectious Disease Medicine, Lifestyle Medicine, Nephrology, Urology
ISSUE #164 (June)
WOMEN & CHILDREN’S HEALTH
OB-GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology
ISSUE #165 (September)
MUSCULOSKELETAL HEALTH
Orthopedics, Physical Medicine & Rehabilitation, Sports Medicine, PT/OT
ISSUE #166 (October) CANCER CARE
Hematology, Oncology, Plastic Surgery, Radiology, Radiation
ISSUE #167 (December)
IT’S ALL IN YOUR HEAD
ENT, Mental Health, Neurology, Neuroscience, Ophthalmology, Pain Medicine, Psychiatry
Welcome to the Cancer Care issue of MD-Update.
I GREW UP in the 1960s when the life expectancy for American men was 66 and 73 for women. Heart disease and cancer were the main causes of death. Now those averages are 76 for men and 81 for women.
As a child, I recall that when hearing that someone “had cancer,” it was understood that they would be dying soon. The type or site of the cancer was rarely discussed. Cancer, the “Big C” was enough said.
The “War on Cancer” was announced by President Richard Nixon in 1971 by virtue of the National Cancer Act, which created the National Cancer Program and gave the National Cancer Institute new and expanded powers and funding to conduct research and clinical trials and establish cancer centers, such as we have at the UK Healthcare Markey Cancer Center, directed by Dr. Mark Evers, who is featured in this issue.
In speaking with the Kentucky oncologists for this issue, three things stood out to me. One, we now speak of organ-specific cancer, i.e., breast cancer, lung cancer, colon cancer, etc. Two, we talk in stages: 1, 2, 3, or 4 of the disease. And third, the biggest change is that we talk of treatment options, disease management, a chronic illness, and in the best cases, survival and recovery.
In this issue of MD-Update, we are very proud to bring you the stories of the physicians who are treating cancer patients in Kentuckiana. I hope you enjoy reading them.
Golf Anyone?
I don’t play golf. It wasn’t something we did very much of on the Eastern Shore of Maryland in the 1960s. We played baseball or spent summers in the salty waters of the Chesapeake Bay, fishing, crabbing, sailing, boating, swimming. The past few months, I’ve been in attendance at two different golf scrambles, one sponsored by the Greater Louisville Medical Society and another one, sponsored by Lexington Clinic. The players seemed to be having a good time and a lot of money was raised for different charities. I took a lot of pictures of the golfers. The GLMS pictures are on page 46, and the Lexington Clinic scramble will be in the December issue. l tried to get the names correct for the captions. If there are mistakes, I’m sorry about that.
The 2026 MD-Update editorial calendar is on the preceding page. When you see your specialty and you have a story to tell, contact me. If your specialty isn’t included, that’s another reason to reach out to me. I’m looking forward to hearing from you.

MD-UPDATE
MD-Update.com
Volume 15, Number 5 ISSUE #160
EDITOR/PUBLISHER
Gil Dunn
gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda Debord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC
Nirvana Nawar, MHA
Scott Neal, CPA, CFP
Christine L. Stanley, Esq.
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING: Gil Dunn
gdunn@md-update.com
Mentelle Media, LLC 38 Mentelle Park Lexington KY 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2025 Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you.
Individual copies of MD-Update are available for $9.95.

Until next time, all the best, Gil Dunn Editor/Publisher MD-Update
SEND YOUR LETTERS TO THE EDITOR TO:
Gil Dunn, Publisher gdunn@md-update.com, or 859.309.0720 phone and fax







A Conversation with Dr. B. Mark Evers, Director Markey Cancer Center, UK HealthCare
Increased patient volumes, clinical trials, cancer vaccines, and federal funding
“The shift from one-size-fits-all treatment to precision medicine has been transformative.”
— Mark Evers, MD, Director Markey Cancer Center, UK HealthCare
LEXINGTON (Editor’s Note) We asked B. Mark Evers, MD, to update us on the Markey Cancer Center 12 years after achieving NCI designation.
What is the mission of the Markey Cancer Center (MCC)?
MARK EVERS, MD: The mission of the UK Markey Cancer Center is to reduce cancer burden with a focus on Kentucky and its most vulnerable populations through research, prevention, treatment, education, and community engagement.
The MCC was designated a National Cancer Institute Center in 2013. Every five years there is a review process. In 2023, the MCC achieved the title of NCI Comprehensive Cancer Center. What does the added “Comprehensive Cancer Center” mean to MCC’s work?
Achieving Comprehensive status in 2023 was ten years in the making — the fastest pace possible. Markey is now one of only 57 Comprehensive Cancer Centers in the U.S. and the first and only in Kentucky.
This designation means we meet the highest standards across three pillars: laboratory
research, clinical research and treatment, and population science and prevention. What that means for Kentuckians is that no patient needs to leave the state for outstanding clinical care and cutting-edge research.
The designation also secured a five-year, $13.5 million NCI Cancer Center Support Grant renewal to support Markey’s research programs and shared resources.
Describe the staff of the MCC, recent growth in patient volumes, and an overview of Markey’s patient population.
As a matrix cancer center, we have 250 faculty researchers spanning 49 departments across 12 colleges at UK. Our research enterprise includes more than 370 research projects representing $58.6 million in research funding, plus $4 million in education and training funding.
We’ve experienced tremendous growth in patient volumes over the past several years. In 2023, we saw 5,060 new cancer cases, a number that has nearly doubled in the past decade.
We expect this growth to continue, anticipating more than a 50% increase in visits over the next decade. Our new 550,000-squarefoot Cancer and Advanced Ambulatory Building, opening in 2028, will help accommodate this demand along with plans to add more than 300 new employees and nearly 50 new physicians.
Ninety-seven percent of Markey patients are from Kentucky, with half from Eastern Kentucky. Our most common presentations reflect Kentucky’s cancer burden: lung cancer, breast cancer, gynecologic cancers, and hematologic malignancies.
What is the most exciting development you've seen in cancer treatment in your 30+ years as a surgical oncologist?
The past five to ten years is the most exciting time I’ve ever seen in cancer treatment. When I started 30 years ago, treatment options
were very limited. Today, we have remarkable options including immunotherapy that uses a patient’s own immune system to fight cancer, as well as personalized medicine that is based on each tumor’s genetic fingerprint.
The shift from one-size-fits-all treatment to precision medicine has been transformative. We now recognize that everyone’s cancer is different, just like we are all different as individuals. Instead of giving the same treatment to all patients, we can tailor therapy based on specific molecular mutations in each patient’s tumor. Today, we’re talking about cures for certain cancers — something I never thought I’d see in my lifetime.
Which of Markey's 90 clinical trials has you most excited and why?
We have a clinical trial testing a personalized vaccine designed to prevent pancreatic cancer recurrence after surgery. I’m particularly excited about this trial because, as a GI surgical oncologist, I’ve dealt extensively with pancreatic cancer throughout my career, and unfortunately patients often present when it’s too late and the disease has already metastasized. This trial tests a personalized vaccine designed to prevent recurrence after surgery, made specifically for each patient’s tumor. Given how challenging pancreatic cancer has been to treat, it represents a real breakthrough in how we might approach this devastating disease.
What cancer breakthrough do you predict we'll see in the next five years?
Building on trials like our pancreatic cancer vaccine, I believe personalized cancer vaccines will be one of the next major breakthroughs. We’re seeing promising developments for melanoma and kidney cancer as well, and I expect these targeted approaches will significantly extend survival for patients with our most challenging cancers.
Additionally, I expect continued advances in cellular therapies like CAR T-cell therapy expanding beyond blood cancers to treat solid tumors, and radiopharmaceutical therapies that can deliver targeted radiation directly to cancer cells. The combination of AI with precision medicine will also accelerate our ability to match patients with the most effective treatments.
How has Kentucky's cancer landscape changed since you started your role as director? What makes treating cancer patients in Kentucky unique?
The transformation has been remarkable. When I arrived in 2009, Kentucky unfortunately ranked number one in both cancer incidence and mortality. While we still lead in incidence, our mortality rates have improved to number two nationally — that's progress, though we still have significant work to do.
Our lung cancer screening program exemplifies this progress. Despite Kentucky’s 200-year
history with tobacco, we’re now second in the nation for lung cancer screening, behind only Massachusetts. Late-stage lung cancer diagnoses are declining at double the national rate.
What makes Kentucky unique is our focus on health disparities, particularly in Eastern Kentucky, where socioeconomic factors, high smoking rates, and geographic isolation create complex challenges. Our 19-hospital affiliate network ensures rural Kentuckians can access cutting-edge care close to home, something that sets us apart from other cancer centers.
Has funding from the NIH to MCC been cut? How will this affect MCC, its staff and the work of MCC?
Markey currently holds more than $35.7 million in NIH funding supporting cancer research, clinical trials, and cancer prevention. While there have been various proposals and policy discussions around federal research funding, there is tremendous bipartisan support in Congress for cancer research.
This federal investment is essential to our mission of reducing Kentucky’s cancer burden. We continue to work closely with our congressional delegation and remain optimistic about sustained support for the critical cancer research we’re conducting at Markey.
What's the biggest challenge facing cancer care today?
The biggest challenge is workforce, specifically ensuring we have adequate staffing to meet growing patient demand. Our patient numbers have doubled over the last ten years, and cancer centers across the country are all competing for the same talented oncologists and specialized staff.
It’s a nationwide challenge because there’s a limited pool of trained cancer specialists, and we’re seeing increased demand everywhere. Sometimes providers choose private practice or industry positions, which creates ongoing recruitment needs.

Markey Cancer Center currently holds more than $35.7 million in nIH funding supporting cancer research, clinical trials, and cancer prevention.
Opening Doors, Saving Lives Rallying for lung cancer screening in November
BY nIRVAnA nAWAR, MHA, PROGRAM ADMInISTRATOR, KEnTUCKY LUnG CAnCER SCREEnInG PROGRAM
FRANKFORT Lung Cancer Awareness Month reminds us not only of the disease’s devastating impact but also our shared responsibility to act. Lung cancer takes more lives than any other cancer in Kentucky and the United States, but it remains misunderstood and for some, filled with stigma and shame. This November, we invite survivors, families, friends, advocates, and healthcare providers to recognize and remember the impact of lung cancer, as well as to promote a tangible step communities can take to reduce lung cancer deaths. Lung cancer is often a silent threat that develops without symptoms until at an advanced stage. With early detection, survival rates can significantly improve. Low-dose computed tomography (LDCT) is the recommended method for lung cancer screening and can catch the disease in its early, treatable stages. Unfortunately, only 18% of eligible Kentuckians get screened each year. This is partially due to difficulties in accessing screening, such as people living in rural areas, working adults who can’t get time off and people with transportation barriers.
Lung Cancer Screening Day is an opportunity to address some of these barriers by opening screening facilities during non-standard hours, such as weekend or evening hours. This is also a reminder to healthcare facilities to engage in conversations with patients about the benefits of lung cancer screening and that early detection works.
How Can You Help
Healthcare Providers and Facilities:
• Host a Weekend Screening Event: Open your facility during Lung Cancer Awareness Month for LDCT screenings for expanded hours, especially on Saturdays or evening-hours where working Kentuckians

may be more likely to attend.
• Reach Out to Eligible Patients: Use reminders and checks with electronic health record systems to proactively contact high-risk individuals and encourage screening appointments.
• Embed Smoking Cessation Referrals: Link every screening opportunity to support for quitting tobacco.
• Reduce Stigma: No one starts smoking because they want to get sick. Talk with patients in a non- judgmental way, recognizing the barriers they have to quitting.
Advocates and Community Organizations:
• Amplify Real Stories: Survivors and caregivers have powerful voices. Sharing their stories can help normalize screening and reduce stigma.
• Join the Movement: Help distribute flyers, promote events, or co-host a community awareness activity.
Policymakers and Public Health Leaders:
• Support Local Screening Campaigns: Ensure communities have what they need to organize outreach, education, and transportation for those at risk.
• Champion Prevention: Consider long-term
strategies that reinvest in early detection as a proven, cost-effective intervention.
The Kentucky Lung Cancer Screening Program (KY LCSP) remains committed to protecting lives through access, education, and evidence-based action. We will continue to work with partners across the Commonwealth to reach high-risk individuals and ensure no one is left behind.
This month we’re collaborating with hospitals, health departments, and nonprofits to plan community- centered screening events, especially in regions with the highest burden. We’re also working alongside our colleagues in the Tobacco Prevention and Cessation program to share data and integrate screening and cessation services whenever possible.
Behind every data point is a life. Behind every screening is a chance.
In a time of tightened budgets and shifting priorities, we can’t afford to retreat from prevention. Instead we must show what’s possible when we step forward together. Whether you’re a clinician, policymaker, advocate, or community member, your voice—and your action—matters.
Let’s turn Lung Cancer Awareness Month into a month of momentum. Open your doors. Start the conversation. Save a life!

nirvana nawar, MHA
Talk to patientsyour about lung cancer screenings!
Lung cancer can be treated if caught early.

You are eligible for screening if:

50 20 You are 50 to 80 years old
You smoked a pack of cigarettes a day for 20 years
You currently smoke or quit within the past 15 years 15

SCAN THE QR CODE TO LEARN MORE
LUNG CANCER SCREENING IS EASY
Covered by most insurance (Medicare 50 - 77)
Quick and painless No needles, IVs or dyes Get screened every year to catch cancer early
Lexington Medical Society Leader Was a Trailblazer
Carolyn Heppler Kurz, retired EVP/CEO of the Lexington Medical Society, passed away August 9, 2025, after a nine-year battle with cancer
LEXINGTON During her 43 years as EVP/CEO of the Society, membership increased dramatically as the Society developed new, innovative programs including the LMS Exchange which still answers patient, nurse & physician calls 24/7/365, a CVO which verified a doctor’s education, training & experience for local hospitals & medical facilities, and a mini internship shadowing program that allowed community leaders an opportunity to follow physicians & gain a deeper understanding of healthcare operations.
Carolyn received numerous awards throughout her career including being named one of the Top Women in Business by The Lane Report in 1994. In 1995 she was awarded the FCMS Layperson Award, while in 1996 she received the KMA Layperson Award. In 2007 she received the Lexington Rotary Club President’s Cup, and in 2011 she was recognized with the AMA’s Medical Executive Lifetime Achievement Award. Upon her retirement in 2014, LMS honored her by creating an award presented to a
Tributes

non-physician dedicated to improving community health.
Beyond her organizational achievements, Carolyn was a devoted mentor who actively guided & supported her physician members & staff, fostering their growth & development. She was deeply engaged in her
community serving as the first female president of the Rotary Club and held leadership roles with the BBB, United Way, and Toyota Bluegrass Miracle League. Carolyn also used her expertise in various educational & advisory roles including serving on the Board of the Sanders-Brown Center on Aging Foundation & advocating health & wellness through the Cystic Fibrosis Foundation of Kentucky.
Carolyn was an avid University of Kentucky basketball and football fan. She was also a world traveler, traveling to South Korea for 11 months before becoming the leader of the Society in 1971. She and her husband of 38 years, Jim Kurz, have traveled to 13 other countries and visited most of the 50 states.
A memorial to celebrate Carolyn’s life was held Wednesday, September 10 in Lexington. Contributions in her honor can be made to Surgery on Sunday, 1594 Harrodsburg Road Lexington, KY 40504; the Lexington Rotary Club, 401 W. Main Street #305, Lexington, KY 40507; or the McDowell House, 125 S. 2nd St, Danville, KY 40422.
FROM LEXINGTON MEDICAL SOCIETY PAST PRESIDENTS:
When I was elected president of the Lexington Medical Society, it was comforting to know that Carolyn Kurz would be an invaluable help to me and the whole society as she had done for my predecessors and the society for many years. Her wise counsel was invaluable to the any successes that the society accomplished. The call center, the golf tournament, and professional relationships were all things that she helped all of us who were members of LMS. She became a very beloved friend. We often joked about the seasons/colors of our personalities. She was
‘Spring’ while was I was ‘Winter.’ ‘Hello Spring,’ or ‘Hello Winter,’ was an affectionate greeting needing no name. She will be missed by so many for so many reasons.”
— Lisle Dalton, MD LMS President 1998
It is with the heaviest of hearts we share the passing of Carolyn Kurz, former EVP/CEO of Lexington Medical Society. Carolyn was with LMS for 43 years, was a member of several professional societies, and won many awards including the AMA 2011 Medical Executive
Lifetime Achievement Award. If you had the privilege to know this remarkable woman, you’d recall her sly smile and knowing glances, her tenacity, and her ability to get things done! She was driven, but somehow kind and nurturing at the same time. Although Carolyn had retired when I met her, I had the honor of being her physician for these past 9 years. In that time, I grew to appreciate her many strengths, but I was most inspired by her determination to live life on her own terms. We will miss her dearly.”
— Hope Cottrill, MD LMS President 2025
Carolyn Kurz was the face of the Lexington Medical Society. Her determination, persistence, and smile helped to make the Society what it is today.”
— Emery Wilson, MD LMS President 2010
I met Carolyn Kurz in September 1982, while a first-year medical student. She immediately told me that to have an impact I needed to be active in organized medicine. She never let me go, mentoring and assisting me as I rose through leadership roles. I hate that I have to let her go now.”
— David Bensema, MD
LMS President 2002
Carolyn worked hard to help the doctors understand all the changes occurring both in medicine and in Lexington.”
— Alan Grimes, MD LMS President 1978
Carolyn will always be remembered as the driving force of the Lexington Medical Society and a wonderful, caring person. Her excellent direction and guidance made our leadership jobs easier and purposeful. Her loving and enduring friendship meant so much to Lynn and me. We will never forget her sweet smile and enrichment. We will miss her greatly.”
— Daniel Kenady, MD
LMS President 1996
When I came back to Lexington and had the opportunity to join the Fayette County Medical Society, I did so and met Carolyn, a powerful leader, concise in her planning and super knowledgeable about all things related to organized medicine. For many of us, I suspect we were some of her ‘projects!’ Little did I know that my path forward under her guidance would take me to a place I could never have imagined. Carolyn became a dear friend and mentor. Early in my career, she gave me a book entitled Even Eagles Need a Push, and to this day , I am so grateful to her for her leadership and guidance, not only for me, but for so many physicians and medical leaders in our community.”
— Ardis Hoven, MD
AMA President 2013-14
LEXINGTON MEDICAL SOCIETY


I first met Carolyn in 1980 when she was the EVP of the Fayette County Medical Society and I was a new member. She was always a very dedicated employee and is largely responsible for the Lexington Medical Society that we have today. I was president of the society and had the privilege of working closely with her that year and for several years before when I served on the executive committee. She is largely responsible for the current location of the Society offices, the Medical Society Exchange and the change of name. She has received numerous rewards from the KMA and AMA as the executive vice president. She continued to support me as I became the KMA President in 2007. I think that everyone who knew her had the greatest respect for her dedication to the Society and to the members of the society.”
— Thomas K Slabaugh Sr, MD LMS President 1990
The principal voice & resource for Central Kentucky physicians
LMS DINNER SOCIAL International Medical Missions Symposium
Past Presidents Dinner Reunion
November 19, 2025
The Signature Club 6pm
Sponsored by ProAssurance & WesBanco
LMS DINNER SOCIAL Presidential Transition & Legislative Review
January 13, 2026
The Signature Club 6pm
In 1637 the French philosopher, mathematician and father of modern philosophy Rene Descartes said the phrase, ‘I think, therefore I am.’ However, ‘I do, therefore I am,’ is a more befitting phrase for Carolyn Kurz. Through her forty-three years with the LMS, her involvement with and presidency of Rotary Club, BBB, Commerce Lexington and more, she put words and thoughts into action and produced results. She was and always will be a giant of the Lexington Medical Society.”
— Tom Waid LMS President 2014
Carolyn was a straight-shooting mentor to many medical society executives and rarely lacked an informed answer to most any question posed to her about the industry. Her immense experience and connections at every level helped to make her a model for any successful association executive."
— Pat Padgett EVP of the Kentucky Medical Association

Texting in Healthcare Legal, ethical, and practical risks
BY CHRISTINE L. STANLEY
IN TODAY’S VERY fast-paced healthcare environment, convenience often drives communication choices. Text messaging, with its immediacy and simplicity, may seem like an efficient way to connect with patients and colleagues. However, medical providers must be aware that texting patients, other providers, and business associates, especially when it involves protected health information (PHI), can expose them to significant legal, ethical, and professional risks. This article outlines why standard text messaging is problematic and why secure messaging through platforms like Epic or other electronic medical records (EMRs) is the safer, smarter alternative.
Text Messages Are Discoverable in Legal Proceedings
One of the most overlooked risks of texting patients, colleagues, or even family and friends, is that these messages are discoverable in court. In both civil and criminal cases, courts routinely admit text messages as evidence. Whether the communication occurred on a personal or work device, if it pertains to patient care or medical decision-making, it can be subpoenaed and scrutinized.
Text messages can be used to establish intent, demonstrate negligence, or support malpractice claims. Even deleted messages may be recoverable through forensic analysis or service provider records. Healthcare providers should assume that any message could one day be read aloud in a courtroom.
HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) sets strict standards for the protection of PHI. Standard SMS texting platforms—such as iMessage, WhatsApp, or regular phone messaging—do not meet HIPAA’s technical safeguards. These platforms lack encryption, audit trails, and access controls, making them vulnerable to
interception, unauthorized access, and data breaches.
HIPAA does not explicitly prohibit texting, but it requires that any electronic transmission of PHI be secure. This includes:
• Encryption during transmission and at rest
• Access controls to ensure only authorized users can view messages
• Audit trails to track who accessed or modified PHI
• Authentication protocols to verify user identity
Most consumer-grade messaging apps fail to meet these requirements. Even if a patient consents to receive texts, the provider remains responsible for ensuring compliance. A breach resulting from unsecured texting can lead to fines, lawsuits, and reputational damage.
Unsecured Communication: A Gateway to Data Breaches
Healthcare is one of the most targeted industries for cyberattacks. Insecure communication methods, like texting, can be exploited by malicious actors to gain access to sensitive patient data. According to recent studies, over 93% of healthcare organizations have experienced data breaches in the past five years.
Risks include:
• Interception of messages during transmission
• Loss or theft of devices containing unencrypted messages
• Forwarding of messages to unauthorized recipients
• Lack of control over message retention on third-party servers
These vulnerabilities not only violate HIPAA but also may compromise care quality.
The Illusion of Convenience
While texting may seem convenient, it often leads to fragmented communication. Messages
sent via personal devices are not automatically documented in the patient’s medical record, creating gaps in clinical documentation. This can result in missed follow-ups, inconsistent care plans, and increased liability.
Moreover, texting lacks the structure and accountability of EMR-integrated communication. There’s no guarantee that the message was received, read, or acted upon. In contrast, secure messaging platforms offer read receipts, timestamps, and patient linkage, ensuring continuity and traceability.
Secure Messaging Through EMRs
EMR platforms like Epic’s Secure Chat or OnPage offer a HIPAA-compliant solution for clinical communication. Integrated directly into the EMR, these tools allow providers to:
• Communicate in real time with other clinicians and patients
• Attach messages to specific patient records
• Ensure encryption and access control
• Maintain audit trails for compliance
Epic Secure Chat, for example, is accessible via desktop and mobile apps (Haiku, Canto, Rover), and supports group messaging, patient-specific threads, and asynchronous communication.
Legal and Ethical Best Practices
To protect themselves and their patients, providers should adopt the following best practices:
• Avoid using personal devices for patient communication unless they are managed by Mobile Device Management (MDM) software.
• Do not send PHI via standard text messaging apps.
• Use secure messaging platforms integrated with your EMR.
• Document all patient communications in the medical record.

Bond Vigilantes and the Risk of Recession What physicians should know
YOU RIGHTLY FOCUS on patient care, not the bond market. Yet the bond market—at roughly $50 trillion, about twice the size of the U.S. stock market—quietly shapes the financial environment in which hospitals, research labs, and even federal health programs operate.
Over the next 12 months, if investors in long-term U.S. government bonds (some are referred to as “bond vigilantes”) begin to fear that a recession is coming, they could sell heavily. That kind of reaction would drive interest rates higher, raise the government’s borrowing costs, and put pressure on healthcare budgets and hospital financing. For medicine, the implications are significant: capital projects may stall, research grants could face cuts, and state Medicaid programs could be squeezed.
What Are Bond Vigilantes?
Think of the bond market as the circulatory system of the global economy. Just as vessels deliver oxygen and nutrients, the bond market delivers financing to governments, businesses, and hospitals. When “bond vigilantes” lose confidence in fiscal or monetary policy, they sell long-term bonds.
Here’s why that matters:
• Bond prices and interest rates move in opposite directions. When investors sell, bond prices drop and yields (interest rates) rise.
• When yields rise, all borrowing—whether for a hospital building, a research lab, or government healthcare programs— becomes more expensive.
• If you follow the bond market, you may hear the term basis points. Bear in mind that 100 basis points = 1%. So, a 200-basis-point rise means a 2% jump in borrowing costs.
The key idea is that investor actions in the bond market can instantly ripple into the real economy, including medicine.
BY D. SCOTT NEAL, CPA, CFP®, CEPA
Historical Case Studies
1994: A Costly Surprise
In 1994, the Federal Reserve unexpectedly raised interest rates to fight inflation. Investors worried the move would choke growth and began selling government bonds. Yields on 30-year bonds surged nearly 200 basis points (2%) in just months. That sudden jump raised mortgage rates, business loan rates, and municipal bond costs. Hospitals and universities planning expansions suddenly faced millions in extra annual interest costs—forcing some projects to be delayed or canceled.
2001:
Skepticism After the Dot-Com Bust
When the dot-com bubble burst and recession followed in 2001, the Fed slashed shortterm rates. But long-term investors were not convinced. Yields fell only modestly, reflecting doubts about recovery. Credit became harder to obtain, especially for smaller businesses, biotech startups, and research-driven organizations. This episode showed how investor caution can blunt the impact of supportive policy.
2008:
Crisis and
the “Safe Haven”
In the 2008 financial crisis, the reaction was different. Investors fled into Treasuries, not away from them. Long-term yields plunged, making government borrowing cheap. Washington used that opportunity to fund stimulus programs and bailouts. But healthcare was not immune: collapsing tax revenues forced states to cut Medicaid, and private capital for hospitals dried up. Even when bond yields fell, the wider economic damage still hit healthcare hard.
Today’s Situation
The current environment shares features of all three cases. Like 1994, there’s uncertainty about the Fed’s rate decisions. Like 2001, many investors are unsure whether recent softness is just a slowdown or the start of a deeper recession. And like 2008, government debt is extremely high.
The difference today is scale: U.S. federal debt is now over 120% of GDP, far higher than in those earlier episodes. That makes the government more vulnerable to the bond market’s judgment. If vigilantes push yields higher, Washington’s interest bill could balloon, leaving less money for programs like Medicare, Medicaid, and NIH funding.
Why Physicians Should Care
The bond market may feel remote, but its effects on medicine are real:
1. Hospital Expansion and Infrastructure: Hospitals often borrow through municipal bonds to finance new wings, imaging centers, or research labs. If long-term Treasury yields rise, hospital borrowing costs rise too. A 200-basis-point increase (as in 1994) could mean tens of millions of dollars in extra interest over the life of a large project.
2. Government Healthcare Spending: Rising borrowing costs force Washington to spend more just servicing debt. That leaves less room for discretionary spending, including healthcare programs and research. In practice, this could slow growth in Medicare reimbursements, Medicaid funding, or NIH grant awards.
3. Private-Sector Innovation: Many biotech firms and medical device companies depend on private financing. If bond yields rise and credit spreads widen, venture and corporate financing dries up. Fewer startups get funded, slowing the pace of new therapies and technologies.
4. Funding Volatility: Even when bond yields fall, as in 2008, recessions still shrink tax revenues. States may respond by cutting Medicaid, just as they did then. For physicians in community hospitals or safety-net systems, this can mean immediate strain on budgets and staffing.
Looking Ahead: Scenarios
• Mild Vigilante Response: Investors sell modestly, pushing yields up by 50–75 basis points. Borrowing costs rise but remain manageable. Hospital projects face pressure, but most proceed with adjustments.
• Severe Vigilante Panic: If recession fears intensify, yields could spike 150–200 basis points. The Treasury’s financing costs soar, and policymakers respond with budget cuts. Hospitals could see bond financing costs double, while states trim Medicaid programs sharply.
• Policy Countermoves: The Federal Reserve could step in by buying bonds (as it did during the 2020 pandemic).
But if inflation is still above target, such moves could trigger new problems, leaving policymakers with tough trade-offs.
In Conclusion
For physicians, the message is simple: what happens in the bond market matters, not only for your portfolio if you are invested in bonds, but also for healthcare. It affects whether a new hospital wing gets built, whether NIH grants are funded, and whether Medicaid reimbursements hold steady or get cut. In other words, you really should be paying attention to the bond market as well as the stock market.
Just as unexpected changes in a patient’s vital signs demand attention, sudden moves in
the bond market can destabilize the financial environment that supports medicine. Staying aware of these dynamics helps physicians understand the broader forces shaping the resources available for patient care and medical innovation.
Scott Neal of Lexington, KY is a Senior Wealth Advisor of Mercer Advisors, a Denver-based financial advisory firm. He can be reached by calling 1-800-344-9098. Any opinions expressed by the author are his own and not necessarily those of Mercer Advisors. The information is believed to be accurate but is not guaranteed or warranted by Mercer Advisors. The content provided should not be construed as personalized financial advice. Readers are cautioned not to place undue reliance on forward-looking statements as actual results will vary. Mercer Global Advisors Inc. is registered with the Securities and Exchange Commission.

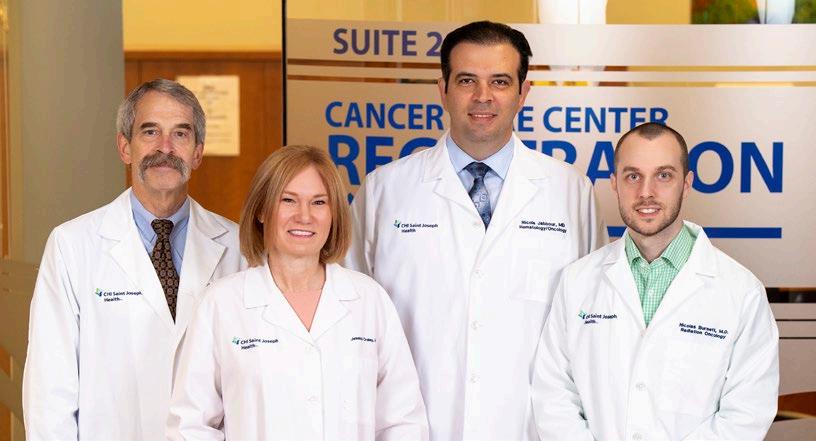
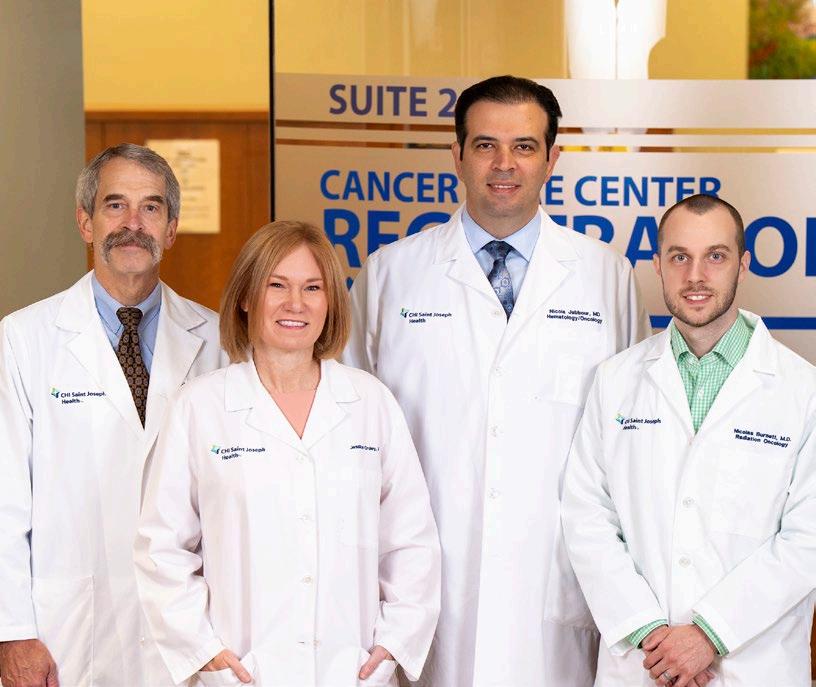
Cancer Care in Central Kentucky
Saint Joseph Health - Cancer Care Center provides people-centered care in a newly renovated space
BY LIZ CAREY
LEXINGTON The Saint Joseph Health – Cancer Care Center in Lexington is just one aspect of what CommonSpirit Health sees as its vision of cancer care in the Central Kentucky region. Saint Joseph Health is a member of CommonSpirit.
At a ribbon-cutting event earlier this year, the center showcased the unified medical oncology services that the hospital feels will provide the region with more accessibility and convenience for its patients. Jessica Croley, MD, Saint Joseph Medical Group – Cancer Care, says the new medical oncology suite is a healing environment for patients and caregivers and recognizes the importance of “people-centered care.”
“People-centered care adds a focus on the health and well-being of entire populations or communities, aiming to improve healthcare systems and access for all. Ensuring that all demographics and geographies have access to the most effective, least toxic therapy for their cancer and the support they need to complete it,” she says. “The team here at Saint
Joseph Health excels in bringing not only new technology, but also social workers, nurse navigation, financial assistance, and nutrition services to all.”
In addition to the Cancer Care Center at 3470 Blazer Parkway, Suite 300 in Lexington, the Center also provides radiation oncology at 701 Bob-O-Link Drive, Suite 120, in Lexington. The Center provides access to the latest cancer screenings, advanced treatments, comprehensive support services, and oncology specialists, Croley says.
DJ Bodziony, market director, oncology services for Saint Joseph Health, says the facility is just one of several cancer care centers in the state. In partnership with Croley, the two maintain a strategy of what the Centers will provide and how they want them to grow.
“We’re looking at opening additional cancer care sites where we see the greatest needs are to reach patients, and what new treatments and therapies we can bring to them,” says Bodziony. “We have a team of directors and managers that work to make the doctor’s job easier, so they can spend their time seeing patients. It’s a great opportunity in Kentucky to continue to
improve not only the patient experience, but the treatment offerings.”
Bodziony became market director of the oncology service line at Saint Joseph Health in April 2025. He previously served as regional director for the oncology service line at CommonSpirit Health in Denver, Colorado. For him, working in oncology is all about the patient.
“Working in cancer is very rewarding, because almost everyone has been impacted by cancer in some way,” he says. “You have the opportunity to care for the entire family and not just the patient. That is what drew me to cancer care. We want to take care of the patient medically, but we also want to be sensitive to the fact that this is a really rough patch in their lives and do what we can do to make that experience a little better for them.”
A Family Connection to Cancer Care
Croley, a medical oncologist and hematologist for Saint Joseph Health, has been in practice for 12 years. She grew up in Muhlenberg County in Western Kentucky and attended the University of Kentucky earning her bachelor’s
degree.She stayed to earn her medical degree and did her residency at UK. Since completing her training in 2013, she has been with Saint Joseph Health.
Her cancer-treating journey began when her father was diagnosed with sarcoma.
“I was a sophomore in undergrad when he was diagnosed. At the time, I was looking at potentially a career in genetics or biomedical engineering,” she says. “I pivoted from the scientific side of healthcare to the clinical side. Just seeing his interactions with his surgical oncologist and staff as he went through his cancer journey, it became very obvious to me that this is what I was meant to do.”
During her time at Saint Joseph Health, she felt she could be of more use as the Cancer Center’s medical director.
“I had served as the chair of the cancer committee for several years in Lexington, but as we started looking more as a system across our cancer centers, I saw that there was a need to standardize the care that patients were being offered wherever they were,” she says. “As much as I love clinical medicine, there’s only so many patients I can see in a day. I felt like those same approaches that I took with my new cancer patients were needed for every patient and that they should be offered those same opportunities.”
Those standards and opportunities were then applied across the system. On top of treating patients according to national guidelines, the Saint Joseph Health cancer centers started a market-wide tumor board process where all the doctors participate in several disease specific tumor boards where new cases are presented. There the group develops the most complete and effective treatment plan for each new patient.
New Member of the Team
Nicola Jabbour, MD, medical oncologist, and hematologist at Saint Joseph Health –Cancer Center, says the initial meeting with patients is an important part of determining how to treat a patient.
“Oncology is a tricky specialty because the first meeting is about building trust,” he says. “During the first meeting, I spend a lot of time listening to the patient, their personal story, what their expectations and goals are, what


their medical history is before I get into the cancer diagnosis. After that, we talk about the staging and the prognosis in a language that they can understand. That’s very important, because no matter how smart the oncologist is, if the patient doesn’t feel the trust and doesn’t feel the connection, they will not be as invested in their treatment.”
Jabbour was born in France, and his family moved to Syria when he was a child. After high school and college in Latakia, Syria, he came to the United States to do his medical training. His internal medicine residency was at the University of Illinois at Chicago, and his oncology and hematology training were at the University of Connecticut.
In 2010, Jabbour came to Hazard, Kentucky, establishing a cancer center for Appalachian Regional Health, ARH. In 2014, he moved to Danville to work at the Commonwealth Cancer Center, and in 2024, he joined Saint Joseph Health.
Part of the challenges facing oncologists in Kentucky, Jabbour says, are the comorbidities they see in patients. Heart disease, diabetes, high blood pressure, obesity, along with poor diet, smoking, and lack of physical activity, all contribute to cancer rates and cancer diagnosis.
“These conditions can impact both the cancer risk and also the treatment outcomes,” he says. “In my practice, I usually address them on two levels. First, I try to integrate treating those comorbidities into treatment planning… to ensure that the patients can tolerate and benefit from the cancer treatment safely. The second
BY MARK MAHAN
level is to focus on education and prevention, realistic steps that they and their family can do. We are not only treating their cancers, but also trying to support their overall health and quality of life. The goal is to empower these patients in their journey to fight the cancer with tools that can hopefully make them live longer, with better lifestyles beyond their cancer journey.” Jabbour says treatment options start with conservative medically appropriate approaches, like nonsurgical treatments, and then in some cases move to more aggressive treatments when necessary.
“For example, in some breast cancer cases, systemic therapy could be hormonal therapy, or chemotherapy, or targeted radiation therapy to shrink the tumor,” he says. “That will hopefully help the patient avoid more extensive surgery. In other cases, we might need to do the surgery up front as an initial step, followed by other treatments. The decision is always individualized based on the cancer biology, the patient’s health, and the patient’s preferences. I involve the patient in every step of the decision-making process. The best treatment plan is the one that is not only scientifically sound, but it is also aligned with what matters most to the patient.”
New treatment options and therapies continue to evolve in oncology. “This is all important, and it is an exciting time now for medical oncologists, surgeons, and radiation oncologists because the pace of progress is directly improving outcomes for the patients that we see every day,” Jabbour says.
PHOTOS
Nicola Jabbour, MD, medical oncologist and hematologist at Saint Joseph Cancer Center.
Jessica Croley, MD, medical director, Saint Joseph Medical Group – Cancer Care.
Radiation Is a Treatment Option
From highly targeted drug therapies that are matched to a tumor-specific molecular or genetic profile, to directed therapies like CDK inhibitors and PARP inhibitors, new treatments allow oncologists to more effectively treat the specific cancer, while minimizing side effects. Additionally, oncologists use less invasive techniques that remove targeted areas, like lymph nodes in breast cancer cases, which reduces complications. Highly targeted radiation treatments mean fewer treatments with lower doses of radiation, improving the procedure’s safety. Focusing on personalized care can not only treat the cancer, but also preserve the quality of life, bodily function, and body image.
Nicolas Burnett, MD, is the radiation oncologist at the Saint Joseph Health – Cancer Care Center. The Murray, Kentucky, native received his undergraduate degree from the University of Louisville and his medical degree from the UofL School of Medicine before heading to UK for his residency. His practice primarily consists of breast, lung, prostate, and rectal/anal cancers.
Burnett highlights some major advancements is his specialty area. “In rectal cancer, we have moved toward using combination chemotherapy and radiation to offer eligible patients a chance to avoid surgery which previously was not widely available. For advanced breast cancer patients, we can often deliver treatment in three to four weeks now, rather than five to six weeks. And for eligible prostate patients, we can give higher doses of radiation directly to the tumor without increasing the side effects of
treatment leading to better rates of control and cure,” he says.
Burnett states that there’s conflicting information published about the role of radiation in oligometastatic and oligoprogressive disease. Some studies show benefit; others show no difference. “The short answer is, we still don’t know exactly which patients will benefit from it and which won’t. For now, we still offer a fair amount of stereotactic body radiation therapy, SBRT, for this population. Some patients will see a true benefit to their cancer outcomes, but in others there are ancillary benefits such as improved pain control and reduced treatment toxicity.”
Meet Scott Pierce, MD
Scott T. Pierce, MD, is a hematologist and oncologist with Saint Joseph Health at the Cancer Care Center. Pierce graduated from the University of Wisconsin-La Crosse, then received his medical degree from the University of Illinois College of Medicine at Chicago. He did his residency and fellowship training at the University of Kentucky and joined Saint Joseph Health in 1993.
His wide-ranging patient population includes lung cancer, chronic leukemia, breast, gastrointestinal, and prostate cancer. Pierce credits advances in molecular profiling with developing more targeted therapies for his patients. Immune checkpoint inhibitors “release the brakes on immune cells, empowering T-cells to recognize and attach to tumors,” he states.
CAR T-cell therapy, which extracts a patient’s own T-cells, then modifies the cells genetically
before they are reinfused to the patient, has produced high remission rates for specific leukemias and lymphomas, notes Pierce.
Many doctors can identify with Pierce’s view that “as an oncologist in Central Kentucky, one of the primary challenges is confronting some of the nation’s highest cancer incidence and mortality rates, especially in rural Appalachian counties.”
“This situation is made worse by patient access issues, health disparities, and specific risk factors associated with the regional population. Patients in rural communities often face significant travel times to reach oncology centers and specialty clinics in urban hubs like Lexington. Many cannot afford the gas or do not have a reliable vehicle for long-distance travel,” say Pierce.
The Future of Cancer Care at Saint Joseph Health
Bodziony says that focus on patient-centered care will continue as the Cancer Center looks to the future.
“Future growth is driving the strategic vision,” he says. “From cancer screening through cancer survivorship and everything in between, bringing specialties and subspecialists into one oncology program where we create a comprehensive program for patients, with physicians talking to each other, creating multi-disciplinary care, and where we have one common vision for all those different providers and specialties.”
That level of care seems to be growing. In 2024, the Cancer Care Center saw 936 patients. In 2025, they’ve already seen 1,021. In addition to locations in Bardstown and London, the center has additional outreach sites in Mount Sterling and Corbin and is looking at additional care sites in Berea and Jessamine County.
The mission, Bodziony says, will remain the same.
“We exist to meet the needs of all patients that need our care,” he says. “We strive to work with patients on any insurance needs that they have and to make sure that we can find a way for them to be seen here. We want to make it easy for the patient by bringing all the providers together. That way, the patient can focus on healing and getting better.”
Scott T. Pierce, MD, hematologist and oncologist at Saint Joseph Cancer Center.
Nicolas Burnett, MD, radiation oncologist at Saint Joseph Health Cancer Center.
Two Surgeons, One Mission
At Norton Healthcare, Tiffany Berry, MD, and Brian Thornton, MD, are leading breast cancer surgery through multidisciplinary integration
BY DONNA ISON
LOUISVILLE Breast cancer care has advanced rapidly over the past two decades, with modern treatment increasingly defined by multidisciplinary coordination, individualized planning, and cutting-edge surgical techniques. At Norton Cancer Institute, two physicians exemplify this integrated model: Tiffany
Berry, MD, a breast surgeon who directs the Prospective Breast Health Program, and Brian Thornton, MD, a reconstructive surgeon specializing exclusively in breast restoration.
As the medical director of the Prospective Breast Health Program at Norton Healthcare’s downtown campus, Berry oversees an integrated approach that guides patients from diagnosis to survivorship. “We have a highly
integrated team all the way from the diagnosis with radiology through survivorship,” she says. “I think that's something that patients really pick up on.”
Called to Cancer Care
After attending the University of Alabama on a swimming scholarship, Berry returned to her hometown of New Orleans for medical

PHOTOS BY JAMIE RHODES
Tiffany Berry, MD, a breast surgeon, directs the Prospective Breast Health Program, and Brian Thornton, MD, a reconstructive surgeon, specializes exclusively in breast restoration.
school at Louisiana State University School of Medicine, where her interest in oncology took root. During her general surgery residency at the University of Kentucky, Berry undertook a “mini breast fellowship” in her second year. “I found that to be very rewarding, taking care of a population, mostly made of women and helping them in a very tumultuous, emotionally rocky time.” She went on to complete a breast surgery fellowship at the Cleveland Clinic, training exclusively in breast surgical oncology.
Berry joined Norton Healthcare in October 2010, initially directing the entire breast program across multiple hospital sites. She led the system to NAPBC accreditation, later focusing her leadership on the downtown campus.
Berry sees a wide spectrum of patients— most women, but about 1% men—with ages ranging from their 30s to their 80s. She has observed a rising rate of breast cancer in younger women. “We have seen, per the data, that there is a rising population in the younger women. We're not exactly sure why that's happening. I assume it's something environmental, something we're eating, something that's outside of what we understand at this time.”
Risk factor counseling is a key component of her practice. She regularly addresses smoking cessation and obesity, noting that “In breast cancer specifically, up to 20% of breast cancers are related to obesity.” These factors influence not only cancer risk but also surgical outcomes and recovery. She is also a huge proponent of screening accessibility: “Women need to be screened. Early detection is the name of the game.”
Technology Is Shifting the Treatment Paradigm
In her role, Berry often serves as the first physician to outline a treatment plan. “We know from studies that the level of anxiety is extremely high for patients until they get to the point where they have a plan,” she explains. Whether the path begins with surgery or systemic therapy, she values the multidisciplinary clinic where surgical, medical, and radiation oncologists align on a strategy the same day.
Technological and procedural advances have shaped her 15 years in practice. She has witnessed the “de-escalation of surgery” with fewer complete lymph node removals, increased use of genomic testing to guide chemotherapy, and new localization techniques that eliminate the need for wire placement before surgery. Looking forward, she envisions preventative vaccines and even genetic interventions as potential game-changers in breast cancer care.
According to Berry, “As far as advances go, I think there’s data that shows we can do less surgery with the same outcomes for cancer. There are studies that even talk about avoiding surgery altogether. I’ve always predicted that, by the end of my career, we wouldn’t be doing breast surgery on the majority of patients anymore.”
But, for now, Berry’s operative schedule is steady—two days in the operating room and two in clinic—allowing her to maintain family balance. Far from feeling depleted by oncology work, she says, “It actually feels like this is where I'm supposed to be. And when you are in the place where you're supposed to be, you don't get drained by your work, but rather energized by your work.”
For Berry, the mission is clear: “Our job as surgeons and providers is to try to not only treat the cancer, but to restore the most normalcy that we can for a woman and get her back to the life that she expected to lead.”
The Role of Reconstruction
In Norton Healthcare’s model, surgical oncology and reconstructive surgery operate in tandem, giving patients the opportunity to make informed choices about their reconstruction timeline and options from the very start. This seamless hand-off between cancer treatment and restoration is where the expertise of Brian Thornton, MD, Director of Breast Restoration, plays a vital role.
Thornton built his career around a singular mission—providing specialized, long-term reconstructive care for breast cancer patients. His path to becoming one of the most sought-after reconstructive surgeons in the region began far from the operating theater. “I developed an interest in medicine very
early on,” Thornton recalls. “I grew up on a working family farm in Paris, Kentucky, and that was not what I wanted to do for a living. I always geared towards medicine or being a chef, for some reason.” The culinary industry's loss is the medical field's gain.
After earning his undergraduate degree at the University of Louisville, Thornton pursued a PhD and later a medical degree at the same institution. He completed his integrated residency program at the University of Kentucky, returning to Louisville to begin practice in 2005. A few years later, he furthered his leadership and administrative knowledge by earning an MBA from the University of Louisville in 2008.
Committed to Complex Cases
Though initially drawn to cosmetic surgery, Thornton quickly realized that his passion lay in helping patients through the physically and emotionally complex process of breast reconstruction. “I’ve always had an interest in taking care of patients. I enjoyed cosmetic surgery but—with all due respect—never felt like I was really helping patients in a way that I wanted to help. I really fell in love with helping breast cancer patients and their special needs.”
Unlike plastic surgeons who shift towards lucrative cosmetic procedures, Thornton chose to remain focused on breast reconstruction. “I stuck with it and I got better at it. I was committed in my practice to the breast cancer patients and their needs. I just kept getting more and more referrals. I'm not that special, it was just you won't find too many people that just have spent their life doing a limited number of surgeries in the breast, and dealing with breast cancer patients, and that turned out to be me.”
Thornton treats a wide age range of patients, from as young as 21 to those in their 80s. Some have newly diagnosed breast cancer, while others require revisions or maintenance decades after their original surgeries. “Cancer is a forever event, but so is reconstruction to some degree,” he notes.
In 2024, after nearly two decades in private practice, Thornton officially joined Norton Healthcare. In reality he had been closely

integrated with their breast care model for years—attending breast conferences, collaborating with surgeons, and operating on their patients.
Reducing Risks and Optimizing Outcomes
Patient selection is at the heart of Thornton’s reconstructive approach, particularly when working with higher-risk populations. According to Thornton, “From the reconstructive side, the challenge of unhealthiness, especially smoking and obesity, really leads to a high risk of complications associated with breast reconstruction. Mitigating those risks, making sure every woman is afforded the opportunity for breast reconstruction, is very important to me. It is my job to decide how we mitigate their risk and achieve those goals.” One way Thornton mitigates risk is by insisting that all patients stop smoking for at least four weeks before and four weeks after surgery.
He also spends considerable time educating patients. “I’ve developed what I call the ‘song and dance’ to patients about breast recon-
struction. I really try to come in and offload all the cancer stuff from the patient. Then the first thing we talk about is when to do the reconstruction. Some patients opt to undergo reconstruction immediately, while for others it is ideal to wait four to six months,” Thornton says.
Current and Coming Techniques
Implant-based reconstruction remains his primary method, representing roughly 80% of all breast reconstructions in the United States. “The remaining 20% is where a tissue can be taken from anywhere on the patient’s body and used to refill the breast, which is an amazing surgery, but very complex,” he says. Louisville currently lacks surgeons to perform these microsurgical procedures, though Norton Healthcare is recruiting to meet this need. Nipple-sparing mastectomy is another priority for Thornton, when clinically appropriate. “It is much more like a breast when a woman can maintain her nipple.”
In addition, patients now have access to new silicone implant options that expand what is possible in reconstruction. Traditional
silicone implants are preferred over saline for their natural feel, appearance, softness, and durability, but until recently, women requiring very large volumes were limited to saline devices. With FDA approval, a new generation of large-volume silicone implants, the Mentor™ Memory Gel Enhance Breast Implant—ranging from 930 to over 1,400 ccs—has become available, meeting the needs of heavier patients undergoing mastectomy who previously had no ideal option.
As the field of breast reconstruction evolves, Thornton remains steadfast in his focus to give women comfort and confidence. His dedication has built a reputation for both technical expertise and unwavering commitment to a vulnerable patient population.
The integration of Berry’s precision in oncological surgery with Thornton’s dedication to specialized reconstruction underscores a shared vision: comprehensive breast cancer care that restores health, confidence, and normalcy. Their combined approach reflects the evolving standard in oncology—where survival is just the starting point, and the ultimate goal is a life fully reclaimed.
Tiffany S. Berry, MD, and Brian P. Thornton, MD, have perfected a team approach to helping patients navigate a mastectomy and reconstruction.
Breast cancer care that goes beyond the standard.
When you refer your patients to Norton Cancer Institute, you’re connecting them to one of the region’s most advanced and comprehensive breast cancer programs.
Our team of more than 100 cancer specialists includes fellowship-trained, subspecialized breast oncologists who are nationally recognized leaders and active researchers, giving patients access to the latest therapies and clinical trials close to home.
With a fully integrated, multidisciplinary approach, we deliver seamless care:
• Multiple outpatient, infusion and radiation centers
• High-risk breast services and genetic counseling
• Coordinated nonsurgical and surgical treatment options, including reconstructive plastic surgery
• Dedicated patient navigators and emotional support services
• Specialized programs, including our Sexual Health Program and Cancer Survivorship Program

From diagnosis through survivorship, your patients receive coordinated, evidence-based care that raises the standard at every step.
Referring is simple: Call (888) 4-U-NORTON / (888) 486-6786 or (502) 629-4673. Providers using Epic or NortonEpicCareLink.com can place an order for Adult Oncology and Hematology and then select Breast Subspecialty



BY JIM KELSEY
As He Builds It, They Will Come
Omar M. El Kawkgi, MD, leads the building of UK Healthcare’s Markey Cancer Center’s thyroid cancer program
LEXINGTON Endocrinologist Omar M. El Kawkgi, MD, joined the University of Kentucky Markey Cancer Center in July of this year, 2025. His reason for coming is reminiscent of the famous line from the movie, Field of Dreams: “If you build it, they will come.” The difference is, El Kawkgi came not because it was built, but to do the building himself.
“I was at a point in my career where I wanted to start thinking about how I could leverage my perspective on thyroid cancer on a greater level,” El Kawkgi says. “I was looking for a place where I could create and develop a thyroid cancer program, and UK was looking for that person.”
El Kawkgi came to Kentucky from the Mayo Clinic in Rochester, Minnesota, where he completed a fellowship in endocrinology. After his fellowship, he remained at the Mayo Clinic for a few years as an assistant professor of medicine.
While he never expected to come to Kentucky, El Kawkgi is no stranger to a change of scenery.
“I was fortunate to grow up in a diverse and multicultural environment,” he says. “I was born in Egypt, raised in Toronto, Canada, and spent my summers in Egypt where I learned Arabic and developed a deep appreciation for Middle Eastern culture. My family moved frequently in my adolescent years, and I had the opportunity to spend parts of my childhood in Atlanta and Abu Dhabi as well.”
El Kawkgi completed his undergraduate degree in biomedical science at the University of Ottawa, then attended medical school at the Royal College of Surgeons in Dublin, Ireland. He completed his residency in internal medicine at the University of MassachusettsBaystate Medical Center before joining the Mayo Clinic.

He comes from a medical family. His uncle is an internist and his great aunts and uncles all practiced in medicine. Additionally, El Kawkgi’s aunt is a pediatric medical oncologist in Egypt.
“My aunt has been my inspiration since childhood,” he says. “I recall her unwavering dedication to her patients, no matter the time of day. I will never forget when a young man approached her in public to thank her for her care years after she was involved in the diagnosis and treatment of his childhood cancer. That moment left a lasting impression on me because it showed the profound and lifelong impact a physician can have on a patient’s life, far beyond the walls of the hospital. This continues to inspire me to strive for that same level of compassion and commitment in my own career, reminding me that every interaction has the potential to make a meaningful difference.”
The Lure of Endocrinology
Drawn to endocrinology early in his training, El Kawkgi receives satisfaction in diagnosing and treating thyroid cancers. It is a
challenging specialty with a wide range of presentations and outcomes.
“I am a big picture thinker, and endocrinology often involves multiple organ systems and requires connecting seemingly unrelated symptoms into a cohesive diagnosis,” he says. “I was intrigued by thyroid cancer because it is a disease with such a wide spectrum of presentations. It can vary in the age of the people who come to see me, in their background, and in terms of their disease. It varies from indolent micro-papillary cancers that may sometimes need only surveillance to aggressive anaplastic cancers requiring intensive, multidisciplinary care. Each case is unique, and it challenges me to partner with my patients to tailor a treatment plan that fits their disease and their lives.”
Detection and Treatment
El Kawkgi says most thyroid cancers are detected incidentally by primary care providers, ENTs, general surgeons, and even dentists. He adds that the cancer is more likely to present in women than men and is most commonly found in asymptomatic patients ages 20 to 40. He estimates that he sees between five and ten new cases of thyroid cancer per week. This aligns with national numbers that demonstrate an increase in the incidence of thyroid cancer over the last few decades.
“We did some studies when I was with Mayo Clinic, and we found that, although the incidence has increased, the mortality from thyroid cancer has not,” El Kawkgi says. “In fact, it’s been quite steady, suggesting to us that there may be an increase in detection as opposed to an increase of the actual pathology.”
Fortunately, mortality rates for thyroid cancer are low compared to many other cancers. El Kawkgi points out that the vast majority of thyroid cancer patients have very positive outcomes, with an approximate survival rate
Endocrinologist Dr. Omar M. El Kawkgi joined the University of Kentucky Markey Cancer Center in July of 2025.
of 98 percent at five years after diagnosis. Additionally, the recurrence risk is generally low and varies between 1% and 10% in most cases but can be as high as 30%.
El Kawkgi sees patients who have already been diagnosed and those who are referred to him for diagnosis. In both cases, his first meeting with the patient is important and focuses on educating the patient and understanding their needs and concerns with an emphasis on shared decision-making.
“Very frequently in this field, there is no one right answer. We operate in the gray,” he says. “Not every treatment for one patient is going to look the same as for another patient. We are at a stage where we are starting to
understand how to stratify patients based on their particular disease, their particular situation, and design a treatment that works for them. When we do it that way, we see improvement in outcomes because we avoid burdening patients with treatments they may not need.”
El Kawkgi is in the early stages of building his medical practice at UK HealthCare and sees 15 to 25 patients per week, with additional time divided between clinic, teaching fellows, and other administrative duties. He also serves as an associate editor for the Journal of Clinical Thyroidology.
“I am fortunate to work with a highly collaborative team at UK,” he says. “I collaborate

closely with surgeons, oncologists, radiologists, pathologists, and nuclear medicine teams among others. It takes a village to take care of thyroid cancer patients.”
Treatment Options
Despite the relatively low mortality and recurrence rates, the detection and treatment of thyroid cancers can be quite complicated and vary from patient to patient. For patients who have undergone successful treatment, the focus is on monitoring it for recurrence. Sometimes that means surveillance only, while other patients might be at higher risk and in need of preventative measures or treatment such as radioactive iodine.
“The important part of my job is to help identify patients who do not have that favorable prognosis so that we can utilize various treatment strategies in that subgroup,” El Kawkgi says.
He points to advancements that help prevent over-diagnosis. For instance, high-resolution ultrasound can aid in the creation of risk stratification scores based on the sonographic characteristics of thyroid nodules. This helps identify which nodules do, and do not, need to be biopsied.
“Molecular profiling and genetic testing are now routinely used in this space,” he adds. “It’s particularly useful when the biopsy results are indeterminate to help us decide where to go from here.”
Patient input can be a deciding factor as well. El Kawkgi shares the story of a patient who was an opera singer. After the initial procedure, she expressed concern about additional surgeries and potential damage to her vocal cords.
“With multi-disciplinary input we were able to design a treatment plan that accounted for her circumstances, while still monitoring her risk of cancer recurrence appropriately. By doing that we were able to save her from having surgery, and I think that had a very large impact on her life,” he says.
“What drives me is to remember that the patient in front of me is more than a diagnosis. When I approach care that way it gives me immense satisfaction to be able to see how I can have a positive impact on people’s lives.”
High-resolution ultrasound can aid in the creation of risk stratification scores based on the sonographic characteristics of thyroid nodules.
BY GIL DUNN
Returning to His Roots
Don Stacy, MD, radiation oncologist at ARH, learns that you can go home again
HAZARD The famous line from the twentieth-century American novelist Thomas Wolfe that says “you can’t go home again” is often misunderstood. The “home” that Wolfe refers to is not the physical place, but the psychological and emotional place of your childhood. That “home” doesn’t exist anymore because you are different and most likely, so is the place. When you return to your childhood home, you are both different; you can’t turn back time.
Don Stacy II, MD, radiation oncologist at Appalachian Regional Healthcare (ARH) grew up in Hazard, Kentucky, and lived there through high school when he left to attend the University of Kentucky in 1991. “When I left Hazard for Lexington, I thought there was a 99.9% chance that I would never live there again,” he says.
Stacy graduated from UK with his BS in physics. Both of Stacy’s parents were educators. His mother, Vera, was a high school social studies and history teacher who eventually became a guidance counselor. His father Don was a teacher at A.B. Combs Grade School and principle at M.C. Napier High School. A professional career was always expected for the younger Stacy. “In college I was deciding between engineering, law, or medicine,” he says. “I finally decided that medicine was where I belonged.”
Stacy received his medical degree from the University of Louisville School of Medicine, followed by his residency and a fellowship at Vanderbilt in 2004. He returned to Louisville and worked for a radiation clinic until 2018 when he was recruited by ARH because the radiation oncologist there, P. I. Narayan, MD, was transitioning into semi-retirement.
Stacy recalls that some of Narayan’s staff knew he was from Hazard. “I had not really considered returning to home, but I thought it was worthwhile to come for the interview

and discuss the options, and their vision for the radiation oncology department,” he says.
“I was ready to take on a different challenge, to really build a practice. The practice in Louisville was set up, and there wasn’t much more to build, we had maxed out. Here at ARH Hazard, the goal was to transform the radiation oncology department into the modern era, using the most modern equipment and sophisticated forms of radiation,” says Stacy.
Stacy recalls the Hazard of the 1970s and 80s as being very isolated, “Of course, there was no internet, or cell phones, and only a couple of early model Commodore computers,” he says. The major employers were coal companies and the school system. Healthcare was a distant third.
A different, less isolated Hazard greeted Stacy in 2018. Better roads, with the internet and cell phones and much less coal mining. Healthcare had become a dominant industry with ARH leading the way. “I felt that I had come home to a different place,” he says.
Also, having worked in Louisville for over ten years, he had an immediate appreciation
for the role of the practitioner in the rural setting, where he felt more comfortable.
“When you’re in an urban area, you’re just one of multiple options for patients. That’s not really a bad thing, but in a rural area, like Hazard, where you’re the only game in town, your patients really rely on you because you’re their only option. That brought me a lot of fulfilment, and I was finally happy in my work,” he says.
Radiation Oncology at ARH in 2025
As the sole radiation oncologist at the ARH Regional Medical Center in Hazard, Stacy’s adult patient population is predictably large and wide-ranging. It includes the most common cancers found in the lungs, throat and neck, colon, breast, rectum, and prostate, as well as skin melanomas. Common comorbidities include obesity, diabetes, smoking, and hypertension. Pediatric patients are referred to Saint Jude or Cincinnati Children’s Hospital.
In a typical work week for the ARH Hazard radiation department, Tuesdays are reserved for current patients who are receiving radiation. With the skilled assistance of nurse practitioner Jessca Ivy, NP, and nurse navigator Shannon Morton, RN, patients are seen nonstop for vitals examination, discussing how their treatment is going, and making appropriate adjustments. Morton helps patients with travel issues, social issues, and gas cards, and with arranging patient transportation from home to the cancer center to get their treatment.
The remainder of the work week is devoted to new patients who have never received treatment, or to patients who have received treatment in the past and have either developed a new cancer or have recurrence. Referrals come from medical oncologists, general surgeons, some primary care physicians, and dermatologists.
For any doctor, the first patient meeting is always critically important for gathering
Don Stacy II, MD, radiation oncologist at Appalachian Regional Healthcare, grew up in Hazard, Kentucky.
Our goal really is to be the best cancer center in southeast and Eastern Kentucky.” — Don Stacy, MD

information, insight into the patient’s condition and goals, and establishing trust between patient and physician.
Stacy describes it this way: “Usually it’s an hour-long discussion because whenever we do a course of radiation, we want the patients to understand what the treatment side effects would be, the long-term risk, the benefits of treatment, and the number of treatments, if they choose radiation as part of treatment.”
Many of Stacy’s radiation patients come with a preconceived negative impression of what radiation therapy does to the patient, because they saw it in their parents or grandparents who received it twenty-plus years ago. In his first meeting with his patients, Stacy explores those notions and seeks to calm their fears.
“It’s very common for patients to say, ‘Well, my grandmother or a family member got radiation treatment twenty years ago, and it was horrible,’” says Stacy.
He continues, “We explain that back then, we didn’t have the computers and appropriate imaging that could really target the radiation. Now it’s all computerized. I explain to patients that when we do a CT scan, we fuse together their other MRIs and PET scans with very sophisticated imaging. That lets us draw out exactly where the tumor is, and where all the normal tissue is that we want to avoid. We then use very sophisticated computer mapping to plot the best way to deliver the radiation to where it’s much more targeted, much more effective, and much less toxic than it was before. It’s all computer and robot driven,” says Stacy.
The newer radiation modalities of IMRT, intensity modulated radiation therapy, and stereotactic radiation have dramatically improved radiation oncology for patients at ARH, says Stacy.
“In the past, we would use three or four larger beams of radiation, but with IMRT we’re asking the computer to evaluate about a million different ways of giving the radiation. Then we’re giving tumors two to three hundred very tiny beams of radiation. When you do it that way, you can really focus the radiation to just the tumor, and limit the radiation to other surrounding normal tissue,” he says.
“Stereotactic is the even fancier version. Instead of doing little tiny doses over several weeks, you’re doing one to five very large doses of radiation. That, by definition, requires the IMRT type treatments. When we do super focused radiation, we can safely give very large doses of very few treatments. We’ve always known that that’s the best way to get radiation, It’s just that in the distant past, we didn’t have the technology to even consider it,” Stacy says.
The Team Approach
When Don Stacy joined ARH, it was his goal to expand the radiation department with additional providers, services, and eventually more patient access points. Some of that has come into fruition with the addition of Ivy, nurse practitioner, and nurse navigator Morgan. The practice has also added registered dietician Cassidy Marshall, RD, LD.
“She’s a crucial part, part of the team,” says Stacy, “because a key issue with patients not completing treatment, is their nutrition status. When patients lose a lot of weight during treatment, they tend to end up in the hospital, and then they can’t complete the treatment. Having Cassidy in the Cancer Center has allowed us to prevent that. Since she’s come on board, our patient missing treatment rates have dropped and completion rates have risen.”
Stacy continues, “We also now have a licensed clinical social worker. Kaitlyn Warfield, MSW, LCSW. A lot, nearly all cancer patients, have depression, anxiety, a variety of mental health issues. That’s just never addressed unless you have someone to take care of that. We now have a person to see every possible patient and have those discussions.”
In Conclusion
Stacy is currently the 14th-District trustee member for the Kentucky Medical Association. He’s been on the board of trustees for the last three years and was re-elected this year for another three-year term. Initially, he got involved with the KMA because of the medical cannabis issue, of which he was an early proponent of legalizing.
It’s been a long road, but Stacy feels he has found his place and his work. “Our goal really is to be the best cancer center in Southeast and Eastern Kentucky. If we aren’t now, our goal is to continue to build to that.”




ARH has a team of providers who specialize in medical oncology, radiation oncology, and surgical oncology that work alongside a staff of highly qualified oncology nurses, social workers, pathologists, and radiologists. Collaboration is a vital part of our approach to excellent care. Our staff’s expertise, combined with advanced technology, and state of the art Oncology centers provide our patients with the highest quality care.
To learn more about Oncology services at ARH visit arh.org/cancer-care.










Join our team
• Great Base Pay with Signing Bonus
• Starting Bonus
• Student Loan and Relocation Assistance
• Collegial Work Environment
• Integrated Physician Lead Network
• Work Life Balance
To learn more about open Oncologist positions at ARH go to arhphysiciancareers.com

Detect Early, Treat Precisely: Optimizing Outcomes for Lung Cancer
At
Baptist Health Louisville, Angela Mahan, MD, is improving lung cancer outcomes through advanced technologies, early detection, and minimally invasive surgery.
BY DONNA ISON
LOUISVILLE For Angela Mahan, MD, a thoracic surgeon at Baptist Health Louisville, technology is not just a tool—it’s a lifeline. New diagnostic systems are providing detection at the earliest level, which for lung cancer means a 90% chance of five-year survival: “If we can just shift that stage of diagnosis, we save lives, and that’s why I’m excited about all of our new technology here,” says Mahan. Artificial intelligence, navigational bronchoscopy, and robotic surgery are revolutionizing how lung cancer is detected, diagnosed, and treated, and Mahan is at the forefront of this evolution.
When Cancer Hits Close to Home
Mahan's passion for cancer care was shaped in large part by her family’s deep history with breast cancer. According to Mahan, “My mom is one of 11, and my family has the BRCA gene. When I was growing up, a lot of my family members had cancer and subsequent treatment. I decided when I was in medical school that I wanted to be involved in cancer care. I fell in love with surgery, so I wanted to do something surgical oncology related.”
However, because of the personal proximity of breast cancer, she chose to take a slightly different path: “Thoracic surgery offered an avenue to not have to deal with something that was too close to home, but still be able to be a surgical oncologist.” Now at Baptist Louisville, Mahan leads a high-volume thoracic surgery practice focused primarily on lung and esophageal cancers.
After earning her undergraduate degrees in chemistry and biology at the University of Kentucky, Mahan completed medical school at the University of Louisville in 2006. She

went on to the University of Colorado for general surgery residency, where she decided to specialize in thoracic surgery. She returned to Kentucky to complete a thoracic surgery fellowship and stayed on as faculty at the University of Kentucky until transitioning to Baptist Health Louisville in 2018.
Prioritizing Prevention
As Kentucky remains one of the most affected states for new cancer diagnoses, Mahan finds herself seeing upward of 50 patients per week. “There is an awful lot of lung cancer everywhere. In Kentucky, we are 48th in the nation for the number of new cancers diagnosed,” she stated.
Her patient base has historically been older men with significant smoking histories. However, she notes a trend that is gaining national attention: “Nowadays, though, I'm seeing—and the whole country is seeing—a rise in women being diagnosed with lung cancer and
non-smokers being diagnosed with lung cancer for reasons we don't understand yet.”
With this rise, Mahan realizes preventing cancers in the first place is even more paramount. She is passionate about smoking cessation, dedicating substantial time and resources to helping her patients quit. “Out of all the things that you can do to decrease your chances of getting lung cancer, stopping exposure is the most important.” Mahan also has strong opinions on vaping and the misconception that it is somehow safer than cigarette smoking. She states, “It's not so much the tobacco that's injuring the lungs, right? It's the additives, it's the smoke itself. Vaping has those same things, and so no matter what you're doing to inhale into your lungs, you're causing injury to the lungs, which causes the problem.”
Innovations Are Increasing Lifespans
Mahan says that what excites her most are the technologies that are making earlier detection and optimal outcomes possible—among them: AI software that scours every imaging report across the Baptist system to flag lung nodules for immediate follow-up. “Over the past five years, there have been AI software programs that scrub the medical records of every single imaging scan done at Baptist Health, which allows us to recognize problems and get patients in sooner.”
Baptist Health is at the forefront of utilizing minimally invasive surgical—including robotic surgery—options to further enhance recovery and longevity. She states, “Robotic surgery is a minimally invasive technique that allows us to go into the chest without making big incisions. We've done about 1,400 robotic lung surgeries at Baptist. I can't remember the last time I did an open surgery.”
Angela Mahan, MD, thoracic surgeon at Baptist Health Louisville, is trained on the da Vinci Surgical System.
PHOTO BY BRUCE MORRIS, MORRIS IMAGES

YOU CARE FOR EVERYONE♦ WE TAKE CARE OF YOU♦
From the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care and medical negligence defense attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth.
Put our experience to work for you.
Sturgill, Turner, Barker & Moloney, PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ www.SturgillTurner.com
Mahan is trained on the da Vinci Surgical System. She also utilizes the Ion system to perform robotic navigational bronchoscopy, which allows surgeons to navigate to lesions in the lung using GPS technology. The technique boasts a high safety profile with less than 2% chance of complications happening with the procedure.
These innovations have led to measurable changes. In the words of Mahan, “Before all the new technology came out, we were diagnosing about 35% of people with Stage 1 lung cancer and about 35% or higher with Stage 4. Since we have implemented these programs, we're at about 55% Stage 1 and climbing. We have decreased our stage four diagnoses to 20% or less.”
The Proof Is in the Prognosis
Mahan is deeply involved in collaborative care. She participates in multiple tumor boards each month across the Baptist Health system. “We have a tumor board that meets weekly at Baptist Louisville, another that meets weekly at Baptist Health Hardin, and one that gathers every other week at Baptist
Health Floyd.” While Stage 1 lung cancer patients are typically surgical candidates, treatment decisions—especially for more advanced stages—are made by a multidisciplinary team that includes medical and radiation oncologists. This team approach, coupled with the aforementioned technologies, allows for more tailored treatments leading to previously unachievable results.
One of Mahan’s most memorable cases exemplifies this: “About a year ago, I had a 67-year-old patient with a nine-millimeter lung nodule. He got his screening scan on a Wednesday. I saw him the following Thursday. He had his biopsy the following Tuesday, and he had his lung out a week after that… From his diagnosis of lung nodule to his cure from his lung cancer was two weeks.” That kind of timeline, though not always feasible for every patient, is her goal. “That's the case that I would like to do for every patient. I would like every patient to get through their cancer treatment within a month.”
And though the initial diagnosis and treatment may only last a month, follow-up care is critical and continuous. She explains, “If you
have Stage 1 lung cancer, you know you're going to see me at least twice a year for five years, and then every year for ten years.”
Reflecting on the Past, Looking to the Future
Mahan’s dedication and passion are deeply tied to her past. “Growing up and seeing my family with cancer, and seeing the care that they got from their specialists… If we can give someone a cure from their lung cancer or a cure from their esophagus cancer, then that gives that person back their life. That gives that family their mom or their dad or their grandpa back… that’s so powerful to me and so motivating to me.”
As for the future, Mahan hopes that lung cancer, like breast cancer, will become a survivable diagnosis through early detection. “I think it’s important to stress that… we are seeing a significant stage shift to early-stage lung cancer. And I would hope that the earlier we are able to find those lung nodules and lung cancers, that that changes their survival curve for lung cancer, just like breast cancer.”
New Technology at Baptist Health Hardin
Serving ten rural Kentucky counties, Baptist Health Hardin adds 3D Ion® bronchoscopy for lung cancer screening, and is the first to begin in-human trials of new 4D mammography technology
BY GIL DUNN AND DIANE STATON
ELIZABETHTOWN Advancements in radiology and imaging are happening in a big way at Baptist Health Hardin in Elizabethtown, Kentucky.
Baptist Health Hardin is the first hospital to begin in-human clinical trials of a revolutionary breast imaging technology that could transform the way breast cancer is detected and diagnosed.
This first clinical trial is expected to enroll approximately 60 patients over the next several months. The study is being led by principal investigator Craig Kamen, MD, chair of the imaging service line for Baptist Health System. Kamen is also president of Radiology Associates, Inc., a 50-person-plus radiology practice.
“As primary investigator, I ensure regulatory compliance and appropriate candidates for the study with the help of the most amazing research team at Baptist Health. This is one of the first radiology research studies we're doing within the system,” says Kamen.
Kamen received his medical degree at the Medical College of Ohio, in Toledo. He did his diagnostic radiology residency at Mount Sinai Medical Center, in Cleveland and then a two-year neuro-radiology fellowship at University Hospitals/Case Western Reserve.
The Need for Advanced 4D Imaging
Calidar, Inc., a pioneer in precision diagnostic imaging, developed the world’s first clinical system for X-ray diffraction imaging of breast cancer. The investigational 4D mammography device reads molecular level “fingerprints” in tissue, offering information that is not available using currently approved imaging technology.

“There
are times we see findings on mammograms that we’re not sure if it’s potentially malignant or benign.” — Craig Kamen, MD
PHOTOS PROVIDED BY BAPTIST HEALTH, CALIDAR, INC, AND GISELLE SMITH

Breast cancer remains difficult to diagnose without invasive procedures, leading to millions of unnecessary biopsies and delayed care each year. Using 4D mammography, researchers will test the technology’s potential ability to identify cancers earlier and more accurately with the goal of giving doctors and patients better answers, faster.
The trial launched in August 2025 with the imaging of the first research volunteer, using the 4D mammography system designed by Stefan Stryker, Josh Carpenter, and Mitchell Greene of Calidar, Inc. The device uses X-ray diffraction to measure how X-rays scatter at the molecular level, producing a unique “signature” that reflects the internal composition of breast tissue. Unlike traditional X-ray images which rely on shape and density, this technology reveals what the tissue is made of — not just what it looks like — offering a new dimension of diagnostic data.
Kamen states, “There are times we see findings on mammograms that we're not sure if it's potentially malignant or benign. That's when we decide to do a breast biopsy. The hope would be that by using X-ray diffraction, we may be able to discriminate between benign and malignant tissue and do fewer biopsies or limit follow-up diagnostic imaging exams.”
“This is more than a study milestone — this is the start of a new era of medical imaging,” says Stryker, CEO of Calidar. “X-ray diffraction has unlocked some of the most iconic achievements in science — from discovering
the structure of DNA to revealing the composition of another world on the Mars rover — and now we are bringing its power into the clinic to look inside the human body in a completely new way. Our 4D mammography system brings this capability to the challenge of breast cancer diagnostics where high-precision noninvasive imaging tools are urgently needed.”
Stryker is from Wilmore, Kentucky. When his North Carolina-based company developed the novel X-ray diffraction technology for breast cancer detection, he reached out to local connections that he had with some of the administration at Baptist Health Hardin and brought both parties together. The hospital has a large presence in women's imaging in Central Kentucky, and they had the space and the personnel to carry out the study.
“We are honored to be participating in this first-in-human clinical trial focusing on advancing care for mammography patients,” said Bert Jones, the hospital’s director of medical imaging. “This groundbreaking research has the potential to change the course of treatment for countless people. Being part of this pivotal moment in medical innovation represents more than just scientific process — it’s a step forward in improving the lives of women everywhere.”
“Baptist Health Hardin is committed to ensuring our patients have access to next generation technology,” says hospital president Robert Ramey. “Being chosen as the first hospital to conduct in-human trials of 4D mammography reflects the dedication of our physicians and staff to setting a new standard in patient care.”

Study Criteria Parameters and Benefits
Study volunteers will meet specific criteria following 3D screening and diagnostic imaging that would typically lead to a biopsy. Volunteers must be at least 22 years of age, between 4'10" and 6'2" inches in height; be able to stand for five minutes; and have had a digital breast tomosynthesis diagnostic exam in the last 90 days with an abnormality of at least three millimeters or larger in size and eight millimeters from the chest wall.
Data from the trial will help determine the system’s effectiveness and guide future studies including potential use in routine breast cancer screening. Data gathered will not impact or influence the routine diagnosis and treatment of the study volunteers.
Kamen points out multiple benefits that could come from 4D mammography research. “We will save time, money, and patients’ anxiety. That's where the promise lies within this technology; that we may be able to mitigate those patients that fall in the middle of ‘not sure it's malignant, and not sure it's benign,’” he says.
Baptist Health Foundation Hardin supported the project by funding a portion of the necessary renovations to house the new 4D mammography equipment and services.
The 4D mammography system is investigational and has not been cleared or approved by the U.S. Food and Drug Administration. It is not available for commercial sale and is limited to investigational use in the United States under FDA’s abbreviated IDE requirements.


Craig Kamen, MD, chair of the imaging service line for Baptist Health System
Robert Ramey, president, Baptist Health Hardin.
Stefan Stryker, PhD, CEO of Calidar, Inc.
Aaron Mulhall, MD, pulmonary and critical care.
Baptist Health Hardin
Now Offering 3D
Robotic-Assisted Bronchoscopy
Baptist Health Hardin has launched a powerful new upgrade to its Ion® bronchoscopy program: 3D imaging technology. The upgrade, considered the gold standard in lung cancer diagnosis, makes the Elizabethtown hospital one of just a few programs in the state to offer this level of diagnostic precision in lung cancer care.

The 4D data can be visualized in color
With Kentucky leading the nation in lung cancer incidence and smoking rates, this investment offers transformative potential. The upgraded 3D Ion system enables physicians to identify and biopsy small lung nodules—often located in hardto-reach outer areas of the lung with greater speed, precision, and safety.
“Lung cancer remains the deadliest cancer in America, and the reality is that too many patients are diagnosed at later stages,” says Ramey, hospital president. “This technology helps us change that story—right here, close to home.”
Finding lesions early, when they are smaller, allows for the most treatment options and improved patient outcomes.
“This technology transforms how we find and treat lung nodules," says Aaron Mulhall, MD, a physician with Baptist Health Medical Group Pulmonary & Critical Care. “It’s like finding a needle in a haystack—but the haystack is always moving. The enhanced 3D capability allows us to lock in on the nodule quickly and accurately, giving patients the best chance at a full, thriving life after cancer.”
The hospital has already performed more than 700 lung screening procedures since Ion was introduced in 2022 and anticipates continued growth in the number of patients served through this upgraded technology.
These advancements reflect Baptist Health Hardin’s mission to deliver excellence in care. In smaller, rural regions where early detection
can be the difference between a full, healthier life and serious health complications, these investments are deeply personal.
“Our goal is to give every person in our community the greatest possible chance—not just to survive cancer, but to truly thrive
beyond it,” says Ramey. “When we invest in advanced care, we’re not only supporting individuals on their cancer journey—we’re strengthening families, uplifting neighborhoods, and improving the health of our entire region.”
Stronger Financial Planning for the Medical Community Starts Here
Achieving your financial goals requires effective planning. That’s why we’re excited to announce that D. Scott Neal, Inc. — a name long trusted by Kentucky’s medical community — is now part of Mercer Advisors. Together, we provide an extensive array of services for your success, spanning from tax and estate planning to exit strategies for practicing physicians.
Ready to amplify and simplify your financial life? Contact Scott today. Scan the QR code to schedule an appointment. Scott Neal, CFP®, CPA 3292 Eagle View Lane, Suite 290 Lexington, KY 40509 Call 800.344.9098 | 859.254.3036


3D versus 4D mammogram. A 3D mammogram slice where density and benign/cancerous masses can show in the same grey color and be hard to differentiate vs a 4D mammogram where X-ray scatter data is collected for a region of concern.

Call It a Gut Feeling
Choosing to treat cancer patients was
a
clear choice for UofL Health’s surgical oncologist Michael Egger, MD
LOUISVILLE Some people know at a very early age what they want to be when they grow up. Others stumble into a profession that suits them or maybe try several before they find the right one. By the time he was a senior in high school, Michael Egger, MD, surgical oncologist specializing in cancers of the gastrointestinal tract and melanoma at UofL Health – Brown Cancer Center, knew what he wanted to do.
Egger was born in Rock Island, Illinois, but his family moved to Louisville when he was two, and then to Nashville when he was in middle school. His father worked for Humana and his mother was a nurse, so a medical career was already on his mind. What happened next solidified his plans.
“My mom was diagnosed with breast cancer the summer before I started my senior year in high school,” says Egger, who is also associate professor of surgery at the University of Louisville School of Medicine. “That was a significant change in our lives for a year as she underwent all the treatments.”
His mother beat the cancer and went back to school to become a nurse practitioner before recently retiring. Egger graduated from the University of the South, then went to Emory University in Atlanta for medical school, with an eye on becoming a surgical oncologist. He and his wife Rachael both graduated from Emory in 2008 – he from medical school and she from physical therapy school.
Egger spent the next seven years at UofL, completing five years of surgical training and two years of surgical oncology research. From 2015-2017, he did a surgical oncology fellowship at the University of Texas MD Anderson Cancer Center in Houston. Upon completing his fellowship in Houston, Egger and Rachael returned to Louisville and to UofL Health in 2017.
“We wanted to raise our family here and I wanted to be part of UofL, at the cancer center
BY JIM KELSEY

“We still need to be the face of patient care… you’re going to be looking the patient in the eye, offering an operation and promising to take care of them.” –Michael Egger, MD.
that had a lot to do with my maturation as a surgeon when I trained here,” Egger says. “The opportunity to conduct research and to teach were big reasons why I wanted to come back.”

Egger was also drawn to the opportunity to work with the UofL’s School of Public Health and Information Sciences, where he could explore his interest in research. He now works with the School of Public Health’s biostatisticians, data scientists, and population health experts analyzing how healthcare is delivered.
“We work with health economists looking at how do we deliver cost-effective care; what are the gaps in care delivery; how do patients access high-quality, comprehensive multidisciplinary cancer care,” Egger says, noting that
they are currently working on a nationwide research project funded by the American Cancer Society.
A Full and Satisfying Work Week
Egger devotes two or three days a week to surgery and one day in clinic. The remaining time is split between research, working with the quality department at UofL, or teaching. Egger points to the multidisciplinary setting as one of the main reasons he wanted to come back to UofL.
“The things I most heavily rely on at the Brown Cancer Center are the additional support systems that we have — social work support and our dieticians helping our patients with nutrition support that has been particularly important for GI cancers,” Egger says. “There are challenges to making sure they are getting the appropriate nutrition that they need to get through the cancer treatments. We have a great team that can help with that.”
Egger also works closely with Brown Cancer Center’s cancer rehab specialists, who also practice the concept of “pre-habilitation.”
“Sometimes our patients are getting either chemotherapy or radiation therapy prior to undergoing surgery,” Egger says. “Rather than sitting on our hands and not doing anything, we get them working with our cancer rehab specialists and physical therapists to get them strong or maintain their fitness so that they are ready to undergo the operation they need.”
Gastrointestinal Cancer in Kentuckiana
Cancer of gastrointestinal organs is a major public health concern in Kentucky. Egger notes that Kentucky ranks among the top 10 to 15 in the nation in colorectal, pancreas, liver, bile duct, and stomach cancers.

Egger is often the first cancer specialist the patient sees. It is not easy to deliver the news to patients about any of these cancers and the challenges of beating them.
“As a surgeon, I’m trying to figure out if surgery is appropriate for them,” Egger says. “We’re trying to determine what stage they have and if we have a firm diagnosis or if we need more biopsies. We have to decide if surgery is appropriate for the kind of disease they have and if they can handle the operation from a medical comorbidity standpoint.”
While the next steps are vital, Egger’s primary focus in those initial patient meetings is to try to understand the impact of the diagnosis on the patient.
“Cancer is one of the things that people really fear in life. We are around this every day. It becomes our day in, day out. If we’re not aware of it, we can be sort of numb or desensitized to just how powerful and profound that word can be to patients,” Egger says. “I challenge myself and our trainees to understand how challenging, how upsetting this experience can be for our patients. I think our job is also to instill confidence — for them to know that this is not the first time that we have done this.”
AI and Advancements in Gastrointestinal Cancer Care
Egger can also provide hope thanks to the continual advancements in gastrointestinal cancer care. He points to minimally invasive surgery and resulting reduction of surgical complications and improved recovery. Additional advancements of systemic therapies including immunotherapy can even eliminate the need for some surgeries.
“Less surgery and less invasive surgeries are the major advances we have made,” Egger says of the changes in cancer treatment. “I think AI will help us get a handle on the vast amount of information we have that simply cannot be consumed and interpreted by any normal human being. The medical literature is now so vast that there is now a study for almost every clinical situation you may encounter, but the challenge is finding it and applying the lessons from that study to your patient. AI is going to help us get to this personalized medicine

approach where we can understand the data that is out there and apply it to the patient.”
AI promises to be an increasingly powerful tool in the treatment of cancers and other diseases. It will not, however, replace the human element of care.
“We still need to be the face of patient care,” Egger says. “In the end, you’re going to be looking the patient in the eye and offering an operation and promising to take care of them. That’s a responsibility that I don’t think AI can replace.”
Caring for the Individual
Not all patients can be cured. Not every story has a happy ending. But Egger understands that every moment matters and tries to help terminal patients meet whatever final goals they might have.
“Some of the cases that have stuck with me most are taking care of patients at the end of
Michael Egger, MD, surgical oncologist, specializes in cancers of the gastrointestinal tract and melanoma at uofL Health – Brown Cancer Center.
their life and understanding their goals and helping patients be well enough to attend a wedding or somebody’s graduation,” he says.
“I had a young patient who really wanted to get to prom, so we did everything we could to get them out of the hospital so they could get to prom. Sometimes that is all you can do. Understanding what the patient’s goals are and how you can get them to that goal can be just as rewarding as curing a cancer.
“The patients are the reason I do this. You see them on some of the worst days of their life. I take the responsibility very seriously to help them through that. One of the great things about being a surgical oncologist is that I can see patients throughout their journey. To develop those relationships with them, to see them move through different phases of their life, to help them on some of the worst days of their life, that’s why I do this.”

Estrangement and the Gift Dilemma
Choosing dignity over desperation
BY JAN ANDERSON, PSYD, LPCC
What Do You Do When Every Thoughtful Gift Disappears Into Silence?
Most estranged parents push harder—bigger gifts, longer letters, one more “just checking in” text. But here’s the hidden cost: your peace, your dignity, and the energy you need to heal.
That’s exactly where one couple found themselves. When they walked into my office, they carried more than stories about their estranged son and his family. They carried confusion, heartbreak, and a sense of helplessness that was slowly eroding the quality of their lives.
The husband admitted, “I don’t know what to do that will make a difference.” His wife added, “It feels like we’re always in a holding pattern—waiting to be let back in.”
Estrangement can leave even strong people feeling powerless. That’s where we began—by exploring a counterintuitive move that helped them move forward and reclaim dignity without giving up.
The Hidden Rules of Estrangement
At first, the couple wanted answers.
The wife said, “I don’t even know what I did wrong. All I know is that I must have broken one of our daughter-in-law’s unspoken rules.”
The husband reflected, “I’ve been living like I’m waiting for parole.”
As we unpacked their story, a picture emerged: Estrangement rarely comes down to one dramatic event. It’s usually the product of unspoken expectations and shifting power dynamics.
The first step wasn’t “fixing” the estrangement. It was learning to respond to it differently.
A Response to Silence: The Gift Dilemma Worksheet
Silence in estrangement isn’t neutral. It lands like rejection, corrodes self-worth, and fuels self-blame.
So how do you make decisions in that painful space?
The couple was facing one of the hardest questions estranged parents ask: After two and a half years of no contact, do we continue to acknowledge birthdays?
The wife wrestled with it: “Sending a birthday card is more about acknowledging my role as a mother and a grandmother.”
So I introduced a tool: “When I do X, I get Y, and it costs me Z.”
It’s deceptively simple. But it changed everything for her.


THE GIFT DILEMMA WORKSHEET
Step 1: What’s the Dilemma?
Should I send a birthday gift to my granddaughter?
Wife: “When I send gifts, I get nothing back, and it costs me my dignity.”
Step 2: Identify the Behavior Options
• Option 1: Send a gift
• Option 2: Don’t send a gift
Step 3: Use the Three-Step Formula + Triangle of Experience
When I do X, I get Y. It costs me Z.
• If I send a gift, I get…
» Thoughts: “She’ll know I remembered.”
» Emotions: Hope, love, but sadness if ignored.
» Body: Tight chest, heaviness if silence follows.
• It costs me: Feeling dismissed when there’s no reply.
• If I don’t send a gift, I get…
» Thoughts: “She might think I don’t care.”
» Emotions: Guilt, fear of rejection.
» Body: Knots in the stomach, restless energy.
• It costs me: Feeling dismissed when there’s no reply.
Step 4: Is There a Bigger, Better Offer?
The wife sighed, “This feels like a Catch-22. Both options feel wrong.”
I nodded. When both choices feel lose-lose, no wonder it’s hard to decide. What if there was a third option? A way to protect your vulnerability while continuing to reach out? A way to respect their boundaries without giving up?
She reflected: “I want to stop sending overthe-top gifts because it costs me my dignity when they’re ignored. I can still love my grand-
daughter without over-giving. I could send a small gift with a simple card.”
• Option 3: If I send a small gift with a simple card, I get…
» Thoughts: “She’ll know I still care, but I’m not desperate.”
» Emotions: Love, less anxiety, less guilt, more dignity.
» Body: Calmer, steadier.
• It costs me: Feeling unfamiliar and a little uncomfortable. But also more balanced. I’m not giving up, and I’m not begging for closeness
Step 5: The Dignity Test
Ask: If this doesn’t get the response I want, will I still feel good about doing it?
I reminded her: You’re not just doing this for them and hoping for a reaction. Just as importantly, you’re doing this for yourself.
Using the Gift Dilemma Worksheet, she discovered a powerful middle path: not begging, not quitting, but stepping back with intention and self-respect.
A single respectful card says: We care, we’re here, and we’re not desperate.
Her realization was powerful: “I want to stop needing their permission to feel okay.”
Silence hurts. But it doesn’t have to define you.
You can’t control your children’s response. But you can control how you show up. You can choose dignity-based gestures, reclaim your narrative, and stop waiting for permission to feel okay.
Final Thought
You don’t have to stay stuck in silence or keep guessing what to do. Recovery begins when you choose dignity over desperation— and that choice is always available to you.
If you’re struggling with your own “gift dilemma,” use the Gift Dilemma Worksheet to get clarity.
If you’re looking for guidance and practical strategies for navigating estrangement, let’s talk. Visit drjananderson.com to schedule a fifteen-minute no-cost, no pressure consultation.
1. What’s the Dilemma?
GIFT DILEMMA WORKSHEET
Example: Should I send a birthday gift to my granddaughter?
2. Identify Your Behavior Options
Option 1: Send the gift
Option 2: Don’t send the gift
(Optional) Option 3: Find a middle path
3. Use the Three-Step Formula + Triangle of Experience
When I do X, I get Y. It costs me Z.
Option 1: If I send the gift, I get thoughts:
Emotions:
Body sensations: It costs me:
Option 2: If I don’t send the gift, I get: thoughts:
Emotions:
Body sensations: It costs me:
4. Ask: Is There a Bigger, Better Offer?
Instead of two extremes, is there a way to balance both?
Option 3: If I do , I get: thoughts: Emotions:
Body sensations: It costs me:
5. The Dignity Test
If I don’t get the response I want, will I still feel good about doing this?
REMINDER: You’re not just doing this for them. You’re also doing it for yourself.
Baptist Health Welcomes New Doctors
Joshua Bentley, MD, Joins Baptist Health

LOUISVILLE Joshua Bentley, MD, a family medicine specialist, has joined Baptist Health Medical Group. Bentley is certified by the American Board of Family Medicine. He trained at the University of Louisville School of Medicine and was a family medicine resident there.
Bentley’s services include everything from well visits and disease prevention to health maintenance and care for urgent conditions. He is accepting new patients at BHMG Primary Care, 1603 Stevens Ave., Louisville, KY 40205.
Baptist Health Medical Group Welcomes Sean Beattie, DO

DO
LOUISVILLE A board-certified neurologist and fellowship trained in epilepsy, Beattie provides skilled and compassionate care. He treats patients with seizures and transient neurological spells, such as epilepsy and potential mimics that require advanced testing, i.e., continuous EEG monitoring.
Beattie specializes in drug resistant epilepsy and is trained in managing neuro-modulatory devices, such as vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation for epilepsy.
Beattie completed professional training at the University of Pikeville – Kentucky College of Osteopathic Medicine, served a neurology residency and epilepsy fellowship at the University of Kansas Medical Center, and received a Master of Science in neuroscience from Tulane University.
His associations include the American Academy of Neurology, American Epilepsy Society and American Osteopathic Association.
Beattie will practice at the Baptist Health Medical Group Neurology, 4003 Kresge Way, Suite 400, Louisville, KY.
Baptist Health Medical Group
Welcomes Collin Henry, MD

Collin Henry, MD
LOUISVILLE Baptist Health Medical Group welcomes Collin Henry, MD, to its team of specialists, expanding access to high-quality digestive health care in Louisville.
Henry is board certified in both gastroenterology and internal medicine by the American Board of Internal Medicine. He provides comprehensive diagnosis and treatment for conditions affecting the esophagus, stomach, intestines, colon, and more, offering patients compassionate, patient-centered care.
Henry earned his medical degree with distinction in research from the University of Louisville School of Medicine. He went on to complete his residency in internal medicine and a fellowship in gastroenterology at the University of Tennessee Health Sciences Center.
Henry is now accepting new patients at Baptist Health Medical Group Gastroenterology, located at 2400 Eastpoint Parkway, Suite 350, Louisville, KY 40223.
Baptist Health Medical Group
Welcomes Anthony Grzeda, MD

LOUISVILLE Baptist Health Medical Group welcomes Anthony Grzeda, MD, to its vascular surgery team in Louisville. Grzeda brings advanced training and expertise
in treating a wide range of vascular disorders, including peripheral vascular diseases, aortic and thoracic aneurysms, vascular malformations, and cerebrovascular disease.
Grzeda is board-certified in general surgery and dedicated to delivering patient-centered care. He is now accepting new patients and looks forward to helping individuals and families manage their vascular health.
Grzeda received his medical degree at Saint Louis University School of Medicine, St. Louis. He did a general surgery residency at the University of Louisville School of Medicine followed by a vascular surgery fellowship at the University of North Carolina School of Medicine.
He is certified by the American Board of Surgery, Advanced Trauma Life Support, and Advanced Cardiovascular Life Support and is a member of the Society for Vascular Surgery, American College of Surgeons, and American Medical Association.
Grzeda will practice with the Baptist Health Medical Group-Vascular Surgery at 4003 Kresge Way, Suite 300, Louisville, KY 40207
Zachary Hagemeyer, DO, Joins Baptist Health Medical Group

Zachary Hagemeyer, DO
LOUISVILLE Internal medicine specialist
Zachary Hagemeyer, DO, has joined the Baptist Health team to offer services including everything from well visits and disease prevention to health maintenance and care for urgent conditions.
Hagemeyer completed his professional training at Marian University College of Osteopathic Medicine in Indianapolis and was an internal medicine resident at the University of Louisville.
He is a member of the American College of Physicians, the Kentucky Medical Association, and the Indiana Osteopathic Association.
Hagemeyer is accepting new patients at
Joshua Bentley, MD
Sean Beattie,
Anthony Grzeda, MD
Baptist Health Medical Group Primary Care, 2400 Eastpoint Parkway, Suite 550, Louisville, KY 40223.
Owen Brown, MD, Has Joined Baptist Health Plastic & Reconstructive Surgery

Owen Brown, MD
LOUISVILLE Owen Brown, MD, has joined the Baptist Health Plastic & Reconstructive Surgery team to offer compassionate, patient-centered care.
He specializes in a variety of surgical procedures, including breast, wound and nerve reconstruction; body contouring and liposuction after weight loss; facial aesthetic procedures and more. Brown completed his professional training at the University of Michigan Medical School and was administrative chief resident at Emory University School of Medicine in Atlanta, where he received the highest in-training examination score.
He is board-eligible for the American Board of Plastic Surgery and is associated with the Southeastern Society of Plastic and Reconstructive Surgeons and the Kentucky Society of Plastic Surgeons.
Brown is accepting new patients at Baptist Health Medical Group Plastic & Reconstructive Surgery, 3950 Kresge Way, Suite 302, Louisville, KY 40207.


CommonSpirit Welcomes New Doctors to Saint Joseph Medical Group
Saint Joseph Health Welcomes New Member to Surgery Team
Rebecca Douglass, DO, returns to Kentucky ready to assist patients

Rebecca Douglass, DO
LEXINGTON Saint Joseph Health Medical Group –Surgery welcomes Rebecca Douglass, DO, to its Lexington team. A native of Frankfort, Kentucky, Douglass was inspired at a young age to pursue a career in medicine after hearing stories from her grandmother, a nurse. After gaining valuable experience practicing in Michigan and Kansas, she returns to her home state with a deep commitment to serve local patients and improve the health of her community.
“Making someone feel heard is half the battle in medicine, so that a patient feels like we’re listening to them and we’re trying to make them feel better,” Douglass says. “Patient autonomy and making patients feel heard are at the heart of my patient care philosophy. I’m there to support them and help them, making sure they understand and are comfortable.”
Douglass says she knew at an early age that she wanted to be a surgeon, and that working with her hands and building things, paired with her passion for medicine, made a perfect match.
“I like that I can make a patient’s day better in a day,” says Douglass. “I have the ability to resolve that problem right away, for instance, if they have pain in the gallbladder. I can help fix that for them without having to wait months, and provide immediate relief to patients.”
Douglass holds a Doctor of Osteopathic Medicine from the Kentucky College of Osteopathic Medicine and a Bachelor of Science from the University of Kentucky. She completed her general surgery residency at Metro Health University of Michigan Health in Wyoming, Michigan.
Douglass currently lives in Lexington with her husband and their three children. The family recently completed a home renovation together and enjoys home improvement projects. Outside of work, Douglass enjoys traveling to different national parks and hiking. A proud Kentucky native, she is also a true University of Kentucky fan at heart.
Douglass will serve patients at CHI Saint Joseph Medical Group – Surgery, located at 1401 Harrodsburg Road, Suite B355, in Lexington.
Saint Joseph Health Welcomes New Member to Cardiology Team
Dr. Shengnan Zheng brings global experience to local cardiology

Shengnan Zheng, MD
LEXINGTON Saint Joseph Medical Group welcomes Shengnan Zheng, MD, to the cardiology team. As an interventional cardiologist, Zheng brings not only clinical expertise but also a lifelong passion for health care. With both parents working in the medical field and a powerful experience when her uncle faced a serious medical issue, Zheng felt a strong calling early on to make a difference in patients’ lives.
“My uncle had an acute heart attack and was nearly gone, but they brought him back,”
says Zheng. “They opened the blocked vessel, and within an hour, he was already improving. It was a really touching and life-changing event. I was really close to him, and in that moment, I knew: If I’m going to be a doctor, that’s what I want to do. I knew I wanted to be an interventional cardiologist. There was no other alternative.”
Zheng will serve the Lexington community and believes in providing patient-centered, evidence-based care. “My role as a physician goes beyond simply presenting the most up-to-date medical options – it's about truly partnering with my patients. I focus on clear communication, shared decision-making, and helping individuals understand what each option means for their lives. I want to support them in achieving their personal health goals. I’m especially passionate about patient safety, patient education, and shared decision making.”
Zheng holds a Doctor of Medicine from the Ross University School of Medicine in Dominica, a country in the West Indies. She holds a BS in biology and chemistry from Slippery Rock University in Pennsylvania, where she graduated with honors. She completed her internal medicine residency at Mercy Catholic Medical Center in Pennsylvania, during which she also obtained a Postgraduate Certificate in Medical Education from the University of Dundee in the UK. She then served as chief resident and clinical instructor at Albany Medical Center and Stratton VA in New York. Most recently, Zheng completed her fellowship in cardiovascular disease at the University of Louisville, where she also held the role of chief fellow of cardiology, and a year-long interventional cardiology fellowship at the Albert Einstein College of Medicine/ Montefiore Medical Center in New York.
Zheng has lived across the world. Born in China, she immigrated to the Caribbean at a young age before completing her undergraduate studies in the United States. Her passion for medicine is matched by a love of learning and teaching, which she has shared with patients, students, and physician assistants. Outside of her professional life, Zheng enjoys a wide range of creative pursuits, including jewelry making, knitting, and crocheting. She’s also an avid lover of music and enjoys horseback riding, skiing, and reading in her free time.
Zheng is part of the Saint Joseph Medical Group – Cardiology team located at 1401 Harrodsburg Road, Suite C-100.
Saint Joseph Health Welcomes
Armaghan Soomro, MD, to Cardiology Team

Dr. Armaghan
Soomro was inspired by his Pakistani parents to pursue a career in medicine
LEXINGTON Saint Joseph Health announced that Armaghan Soomro, MD, FACC, FSCAI, RPVI, has joined Saint Joseph Medical Group – Cardiology in Lexington. Soomro grew up in Pakistan and says he was inspired to pursue a career in medicine at an early age.
“I’ve always been fond of medicine. My parents were both doctors, and I saw them as role models,” Soomro says. “Later in life, when I was in high school, I realized I was drawn to science and that challenge and the betterment of society motivated me. Fortunately, the journey worked out.”
Cardiology, he said, became a focus for him both personally and professionally.
“My father had a heart attack and bypass, and I was inspired to serve my role to make sure families do not have to go through similar circumstances,” he says. “Once I got into medicine, cardiology was extremely interesting to me – how it works, the science of it. That interest grew, and I knew I wanted to pursue cardiology.”
Soomro said Kentucky was a natural place to continue his career. “There is a large underserved population in Kentucky, and it is close to my heart to treat patients who need care the most,” he says.
His patient care philosophy emphasizes compassion and respect. “I treat my patients with respect, dignity and compassion, as I would want my family or myself to be treated,” Soomro says. “It’s a relationship, and I respect the sanctity of that. I feel I am an ambassador to advocate for new treatments while also respecting what the patient prefers.”
Soomro earned his medical degree from
Dow Medical College in Pakistan and completed a clinical research training program from Drexel University in Pennsylvania. He finished an internal medicine residency and a general cardiology fellowship at Hofstra Northwell School of Medicine – Northwell Health in Staten Island, followed by an interventional cardiology fellowship at the University of Arkansas for Medical Sciences and a structural heart disease fellowship at Oregon Health Sciences University.
He is board-certified in internal medicine, cardiovascular disease, interventional cardiology, nuclear cardiology, and echocardiography, and is a registered physician in vascular interpretation. Soomro is a Fellow of the American College of Cardiology, the American College of Physicians, and the Society for Cardiovascular Angiography and Interventions.
Outside of medicine, Soomro enjoys traveling, playing tennis, swimming, and spending time with his family, including his seven-yearold daughter.
Soomro will see patients at Saint Joseph Medical Group – Cardiology, located at 1401 Harrodsburg Road, Suite 300, in Lexington.
Saint Joseph Health Welcomes
Thomas Troy to Family Medicine Team

Thomas Troy, MD
Dr. Troy has a passion for primary care and being the first point of contact for patients
LEXINGTON Saint Joseph Health announced that Thomas Troy, MD, has joined Saint Joseph Medical Group – Family Medicine at Fountain Court in Lexington. Troy, originally a native of Ohio, says his interest in medicine grew out of a love of science and the desire to apply it in meaningful ways.
“I grew up with an interest in science, and when it came time for college, I realized I had an interest in the practical application of science,” Troy says. “I shadowed a couple of providers, and a career in medicine seemed like a path where I could do the most good in the world and have a lifelong, fulfilling career.”
During medical school, Troy says he discov-
Armaghan Soomro, MD,
ered a passion for primary care. “I love the idea of being the first point of contact for people,” he says. “There’s so much information out there, and it can be hard to navigate. I like being that trustworthy person who can help people transfer science and evidence into their daily lives.”
Troy is passionate about holistic care and lifestyle medicine. His patient care philosophy emphasizes prevention and empowerment.
“I’m a big believer that an ounce of prevention is worth a pound of cure,” Troy says. “We have really good evidence that intervening on things early can prevent long-term, dangerous consequences. Patients are individuals and make their own decisions, and my role is to provide the information they need to make choices that line up with their values.”
Troy earned his medical degree from the University of Cincinnati College of Medicine and completed his residency in family medicine at the University of Utah. He also holds a BS in biology from Ohio Northern University, where he played varsity soccer.
Troy said the decision to practice in Kentucky was influenced by family and lifestyle. “We felt the draw to come back close to home, and Lexington made a lot of sense to us,” he says. “It’s close to family and to outdoor adventures in the Red River Gorge. We’re really excited about becoming part of the community and becoming Kentuckians.”
Outside of medicine, Troy enjoys rock climbing, hiking, backpacking, soccer, and attending FC Cincinnati matches.
Troy will see patients at Saint Joseph Medical Group – Family Medicine, at 211 Fountain Court, Suite 120, in Lexington.
Saint Joseph Medical Group – Cardiology Welcomes New Member to its London Team

City and brings a deep passion for cardiology that began with a life-changing experience in his youth.
“When I was younger, my dad suffered a heart attack, and the hospital staff treated him immediately,” says Rashid. “That moment, I decided to go into health care, and cardiology specifically, for that reason: to help patients when they are most in need. It’s very rewarding, because results are often immediate. In many cases, it’s instant gratification.”
Rashid emphasizes the importance of heart health and patient education. “Cardiovascular disease is the number one cause of death in the United States, so patients must understand their conditions and how we can customize their care.”
At the core of Rashid’s patient care philosophy is trust and collaboration. “The most important thing is building a relationship where the patient trusts you. It’s important for patients and doctors to work together rather than telling the patient what to do.”
Rashid earned his Bachelor of Science in life science from the University of Toronto in Mississauga, Canada, before completing his medical degree at Poznan University of Medical Sciences in Poznan, Poland. He went on to complete post-graduate training and research at several medical centers in New York.
Outside of work, Rashid enjoys spending time with his wife and living an active lifestyle, from hiking to playing tennis and pickleball.
Rashid is now accepting patients at Saint Joseph Medical Group – Cardiology, located at 1025 Saint Joseph Lane, London, KY.
Saint Joseph Health Welcomes
Sarah Bissmeyer to Primary Care Team in Lexington
Dr. Syed Rashid brings passion for patient-centered care
LONDON Saint Joseph Medical Group – Cardiology in London has welcomed Syed Rashid, MD, to its team.

Sarah Bissmeyer, MD,
Lexington. Bissmeyer, a native of Louisville, says her interest in medicine was inspired by family members and her father’s illness when she was younger.
“I always wanted to do something where I could help people, and I also had an interest in science,” Bissmeyer says. “My great-grandmother was a nurse during World War II and I heard her stories about what it was like. When I was in middle school, my dad had a stroke and I saw the influence doctors had on his recovery.”
During medical school, Bissmeyer says she discovered a passion for primary care. “I love preventive medicine,” she says. “I’ve seen people get past the point where we have to treat the disease versus preventing it. That always makes me sad.”
Bissmeyer enjoys getting to know her patients and working with them as individuals, addressing their needs with compassion and understanding where they are in their journey.
“Compassion is very healing in itself,” she says. “There are multiple layers of health –spiritual, mental and physical – and I think you have to combine them. Getting to know what needs people have is really important in their care. Some people want to be told something in a very blunt way; other people maybe they need more education. You’ve got to get to know a person to find out what’s going to be best for them.”
Bissmeyer earned her medical degree from the University of Kentucky and completed her residency in family medicine at St. Elizabeth Family Medicine in Edgewood. She also holds a BS in biology from the University of Louisville.
Outside of medicine, Bissmeyer enjoys playing pickleball, ping pong, and pool, as well as being involved in arts and crafts.
Dr. Bissmeyer brings compassion and a love for helping others to practice
LEXINGTON Saint Joseph Health welcomed Sarah Bissmeyer, MD, to Saint Joseph Medical Group – Primary Care at the Saint Joseph Office Park in
Sarah Bissmeyer will see patients at Saint Joseph Medical Group – Primary Care, located at 1401 Harrodsburg Road, Suite B-160, in Lexington.

Syed Rashid, MD
Rashid joins the London team from New York
Lexington Clinic Welcomes New Urologist, Ophthalmologist,
and Internal Medicine
Physicians

Andrew M. Todd, MD
LEXINGTON Lexington Clinic announced that Andrew M. Todd, MD, has joined Commonwealth Urology/Urologic Associates, a part of Lexington Clinic. Board-certified by the American Board of Urology, Todd brings a wealth of experience and a patient-centered approach.
Todd graduated from Miami University (Ohio) and received his medical degree from the University of Louisville School of Medicine. He then completed a general surgery internship followed by a urologic surgery residency at Ohio State University. Todd is fluent in Spanish, ensuring high-quality care for Lexington Clinic Spanish-speaking patients.
Todd offers treatment of kidney stones, benign prostate disease, prostate cancer, kidney cancer, bladder, cancer, testicular, cancer, infertility, low testosterone, erectile dysfunction, voiding dysfunction and incontinence.
Todd has a professional interest in advanced kidney stone management, men's sexual and urinary health, and treatment of enlarged prostate/BPH. He specializes in minimal-
ly invasive procedures for the prostate and kidney such as holmium laser nucleation of the prostate (HoLEP), aquablation, Urolift, penile implant, percutaneous nephrolithotomy (PCNL), and ureteroscopy.
Todd joins a team of ten board-certified urological providers. Lexington Clinic Urology and Commonwealth Urology/ Urologic Associates offer a wide range of comprehensive urological services.
Lexington Clinic also announced the addition of two new physicians in its Ophthalmology and Internal Medicine departments: Andrew Fink, MD, and Chase Thornton, MD.

Fink is a board-eligible ophthalmologist who will see patients at Lexington Clinic East. Fink received his medical degree at the University at Buffalo Jacobs School of Medicine and Biomedical Sciences in Buffalo, New York. He completed his internal medicine internship and ophthalmology residency at the University of Cincinnati. He offers a wide range of services relating to adult

eye care, including small-incision cataract surgery, medical and surgical glaucoma treatment, macular degeneration, and diabetic retinopathy screenings. He also performs laser eye surgery and non-invasive OCT imaging for early detection of eye disease.

Thornton is board-eligible in internal medicine and practices at Lexington Clinic's Central Kentucky Medical Group in Versailles. Thornton received his medical degree at the University of Kentucky College of Medicine in Lexington before completing his internal medicine residency at Wright State University's Boonshoft School of Medicine in Dayton, Ohio. Thornton offers services in primary and preventative care in addition to treatment of minor injuries and illness. Thornton is bilingual and speaks Spanish.
Founded in 1920, Lexington Clinic is central Kentucky’s oldest and largest physician-owned group practice. With 350+ providers in 35+ specialties, Lexington Clinic has more than 25 locations and serves about one million patients yearly.

Andrew Fink, MD
Chase Thornton, MD
Norton Healthcare Welcomes New Doctors
LOUISVILLE/SOUTHERN INDIANA Norton
Healthcare and Norton Children’s serve adult and pediatric patients throughout Greater Louisville, Southern Indiana, and beyond. The not-for-profit hospital and health care system has six Louisville-based hospitals and three hospitals in Southern Indiana.
Norton Healthcare is Louisville’s second largest employer with more than 23,000 employees, over 2,100 employed medical providers and more than 4,000 total providers on its medical staff, It provides care at more than 400 locations throughout Kentucky and Southern Indiana.
New doctors who recently joined Norton Healthcare include:






The Norton Healthcare hospitals provide inpatient and outpatient general care as well as specialty care, including heart, neuroscience, cancer, orthopedic, women’s and pediatric services. A strong research program provides access to clinical trials in a multitude of areas.





Kelli R. Albrecht, DO family medicine
Peter L. Albrecht Jr., DO vascular surgery
Hussayn Alrayes, DO interventional structural cardiology, Norton Heart & Vascular Institute
Megan C. Bath, DO pediatrics, Norton Children’s Medical Group
Amy Beard, DO emergency medicine, Norton Women’s & Children’s Hospital
Chloe Braun, MD pediatric critical care, Norton Children’s Critical Care
Robert Brooks, MD hospital medicine
Angela Cao, MD otolaryngology
Phillip Chuong, MD pediatrics, Norton Children’s Emergency Medicine
Vincent D. Clark, MD family medicine
Riley Coots, MD emergency medicine
Eric DeGeare, MD emergency medicine
Megan A. Edlin, DO obstetrics/gynecology
Trevor Fain, MD general surgery
Josephine A. Gilkeson, DO pediatrics, Norton Children’s Medical Group















Scarlett B. Hao, MD colon and rectal surgery
Tyler B. Harp, MD pediatrics, Norton Children’s Medical Group
Meredith Linley Harvie, MD pediatric gastroenterology, Norton Children’s Gastroenterology
Nicole Henry, MD pediatrics
Alexandra Howard, MD pediatrics
Elvis Joseph, MD emergency medicine, Norton Healthcare Emergency Medicine
Danielle Kamenec, DO emergency medicine
Sarah A. Landes, MD gastroenterology
Rebecca Leavitt, MD emergency medicine
Tyler David Leiva, MD pediatric surgery, Norton Children’s Surgery
Lucia Rivera Matos, MD gastroenterology
Shelby T. Meshinski, MD pediatrics, Norton Children’s Medical Group
Azmina Mohammed, MD emergency medicine, Norton Healthcare Emergency Medicine
Caroline “Callie” Ray, MD pediatric neurology, Norton Children’s Neuroscience Institute
Nicholas E. Rebhan, MD pediatric and congenital electrophysiology, Norton Children’s Heart Institute
Ana L. Risse, MD family medicine
Morgan Robinson, MD pediatric hospital medicine
Amy C. Shah, MD behavioral medicine
Ping Shi, MD, PhD neurology, Norton Neuroscience Institute
Natalie Shipley, MD pediatrics








Mark Siefring, MD family medicine
S. Kyle Skaggs, DO pediatrics
Michele Snow, DO pediatric emergency medicine
Shawn P. Stallings, MD maternal-fetal medicine at Norton Children’s Maternal-Fetal Medicine
Matthew B. Thomas, DO cardiology
Nathaniel R. Toop, MD neurosurgery
Michael A. Basso-Williams, DO, MPH orthopedic surgery, Norton Orthopedic Institute
Christopher S. Watkins, MD obstetric hospital medicine
Saint Joseph Hospital Foundation Holds 10th
Annual Yes, Mamm! Yes, Cerv! 5K
NICHOLASVILLE The CHI Saint Joseph Hospital Foundation’s (SJHF) annual Yes, Mamm! Yes, Cerv! 5K celebrated its 10th year, bringing together families, friends, supporters, volunteers, physicians, and cancer survivors. The event was held on Saturday, October 11, 2025, at the RJ Corman Railroad Group Headquarters in Nicholasville, KY.
According to Marie Murray, SJHF EventsCommunity Program Manager, over $57,000 was raised from 360 runners and sponsors.
“We are grateful to our host sponsor RJ Corman Railroad Group and presenting sponsor, LBX, for their continued commitment to the Yes, Mamm! program,” said Delaine Theil, VP of philanthropy, SJH Foundations.

“The Yes, Mamm! program has grown because of the generous sponsorship support from our community. Many race participants have been part of the race since the beginning, which makes for a very special event. We had the perfect fall morning for celebrating our cancer survivors, and look forward to doing it again next year, for the 11th annual race,” said Theil.
The Yes, Mamm! Yes, Cerv! 5K was open to runners of all ages. Proceeds support Yes, Mamm! Yes, Cerv! programs statewide, providing free mammography and cervical cancer screenings, diagnostic testing, and program support to thousands of underinsured and uninsured patients across Kentucky.
During the event CHI SJHF hosted a family-friendly health expo with vendors, a kid’s zone, food truck, and DJ.

The MD-Update team included: (Front) Allison Buckley, Leonard Bussell, Heather Thompson, Gideon Maddie Dunn, Spencer Johnson; (Back) Fanta Kabah, Piper Phillips, Jean Robens Normil, Dada Karulenzi, Marcus Pernell, Mary Catherine Dorsett, Collier Porter, Megan Mannering, Brittany Thompson, Ray Debolt, Jill Debolt, and Kim Nawjokas.
PHOTOS BY GIL DUNN
1 Priscilla Johnson, CHI Saint Joseph Health Foundation volunteer.
2 Gil Dunn, MD-Update, with daughter Gideon Maddie Dunn.










3 Heather Thompson with her mother Regina and nephew Colton.
4 Delaine Theil, vP of philanthropy, SJH Foundations, and Kim Stigers, MD.
5 Dada Karulenzi with niece and nephews who took part in the kid-friendly face-painting.
6 Dada Karulenzi, Spencer Johnson, and Fanta Kabah.
7 Jill Debolt and Kim Nawjokas.
8 Gideon Maddie Dunn and Megan Mannering.
9 Jean Robens Normil and Leonard Bussell.
10 Piper Phillips, Allison Buckley, and Brittany Thompson.
11 Marcus Pernell and Mary Catherine Dorsett at the finish line!
12 Collier Porter.

Post-race, some of the MD-Update team got together for one more photo including: (Front) Fanta Kabah, Mary Catherine Dorsett, Marcus Pernell, Collier Porter, Heather Thompson, Leonard Bussell, Jean Robens Normil, Gideon Maddie Dunn, Jill Debolt, Spencer Johnson, Kim Nawjokas. (Back) Megan Mannering and Gil Dunn. (Not pictured: Allison Buckley, Piper Phillips, Dada Karulenzi, and Brittany Thompson)

15th Annual Greater Louisville Medical Society Golf Tournament
LOUISVILLE The 15th Annual Doctor’s Cup Golf Scramble, held on September 29, 2025, at Hurstbourne Country Club, brought together 108 players and 44 sponsors, raising $101,476 in donations and sponsorships. These funds provided ten UofL medical students with $12,500 scholarships each.
The team from Republic Bank and Trust was the first-place winner. UofL Health was the presenting sponsor, and Stock Yards Bank & Trust was the all-tourney sponsor. “We’re grateful to everyone who made this event a success and look forward to continuing this tradition of supporting future healthcare leaders,” said Jeremy Clark, MD, Doctor’s Cup committee chair.







David Bottom, Eric Gleis, Steve Fackler, and Tim Woock played for Dr. Linda Gleis’ team.
Dan Watkins and brother David Watkins, MD, cofounder of the Doctor’s Cup, teamed up with Tom Gregory and Ron Stambaugh.
Oliver Montoya, PhD, Jason Brown, CCP, Jimmy Byrnes, PhD, and Bhagwan Bhimani, MD, played for the UofL cardiothoracic surgery team.
Nelco, Inc., Louisville-based cabinet makers, sponsored the team of Steve Parman, Ken Karl, Josh Phelps, and Charlie Schlich.
The UofL ENT team was Travis Shutt, MD, Kevin Potts, MD, Skylar Trott, MD, and Bradley Ledford.
Linda Gleis, MD, cofounder of the Doctor’s Cup Golf Scramble, was at the 2025 UofL scholarship awards presentation.
Heather Hensley represented hole sponsor Aurelius Golf.
Jeremy Clark, MD, chair of this year’s Doctor’s Cup committee, urged the medical students to “Mentor and be mentored. Get involved with your community of doctors.”















Silas Boyle, John DeWeese, Miller DeWeese, and Cy Radford played for the Professionals Insurance Agency, Inc. team.
Timothy Beacham, MD, Clarence Benboe, Houston Mills, and Maurice Sweeney played for the Restorative Pain Institute team.
The Doctor’s Cup winning team from Republic Bank with a scramble score of 50 was Sean Francis, MD, David Buchanon, Alex Campbell, and Tim Wesley.
UofL Orthopedics team #1 was Andrew Duffee, MD, Brent Bohlig, MD, Ellis Thompson, PA-C, and Daniel Glenn, PA-C.
UofL Orthopedics team #2 was Alaina Schmitt, Alex Carrasquer, MD, Keven Harreld, MD, and Jarod Richards, MD.
Jeremy Clark, Doctor’s Cup committee chair, with the UofL Ophthalmology team of Mark Ihnen, MD, Aaron Young, and Chris Compton, MD.
Norton Healthcare was represented by Brandon Freiberger, MD, Thomas Cunningham, MD, Matthew Iles, DO, and Chris Moser, DO.
All-tourney sponsor Stock Yards Bank & Trust fielded multiple teams including Jennifer Knific, Seth Blann, Jimmy Johnson, and Robert Hecht.
Stock Yards Bank & Trust sponsored a team of UofL medical students: Thomas Hislope, 4y, Braden Fairbanks, 4y, John Davis, 4y, and Caden Seraphine, 2y.
The Louisville Orthopedics team was Scott Kuiper, MD, Bryce Fitzgerald, David Hance, and Ben Van Nevel.
Another Stock Yards Bank & Trust sponsored team was Bob Frank, David Krebs, Bill Cheatham, and Rick Tobe.
Enjoying a day away from the office was the team of CPAs from Dean Dorton: Jim Tencza, Curtis Applebaum, Nick Reynolds, and Cole Bruner.
Merrick Printing fielded the team of Justin Merrick, Matt Newman, Bryant Merrick, and Omar Elayan.
MDF Instruments teamed up with Falls City Medical Society for the foursome of Casey Bond, Luke Youngblom, Andre Duff, MD, and Griff Steiner, MD.
Playing for the UofL School of Medicine were Glenn Gittings, PhD Dwayne Compton, EdD, Doug Craddock, PhD, and Jim Broschart.

Medical students who received GLMS scholarships from the Doctor’s Cup Golf Scramble are shown above. Starting top left: Kylie Stava, Logan Davis, Cathy Spencer, Caroline Hourigan, Olivia Bosch, Grae McCarty, (front row) Thomas Hislope, John Davis, Braden Fairbanks
Not pictured: Lily Wilding Photo by Amanda Hall, GLMS
Myka G. Metastatic Breast Cancer, 2017

Living Life.
The Power of Academic Research
At UofL Health–Brown Cancer Center, you’ll find inspiring stories like Myka’s, thanks to our collaborative approach, early detection and pioneering treatments. Here, hope comes to life with our expert second opinions, advanced technology and personalized holistic care. We harness the power of academic research and groundbreaking clinical trials, only found here, to help survivors make more memories and keep living their stories.
Now your patients can experience the power of world-class care, close to home at our three locations. Call 502-562-HOPE (4673) to refer your patient today.

To find Myka’s story and other survivor stories, visit UofLHealth.org/BCCStories.
