Invisible Capes

The doctors aren’t the only superheroes at Norton Children’s Heart Institute









The doctors aren’t the only superheroes at Norton Children’s Heart Institute







In the last 16 months, while so much attention has been focused on prevention and treatment of COVID-19, women in Kentuckiana have continued to give birth. We don’t know yet if there was a 2020-21 work-at-home baby boom. We do know that doctors, nurses, and midwives attended to their patients, both mothers and infants, during the pandemic.
In the midst of anything but business as usual, the doctors and staff at Norton Children’s Heart Institute prepared expectant parents for the procedures that would take place when their infant with cardiac abnormalities was born.
We were able to meet Brian J. Holland, MD, pediatric cardiologist, and Bahaaldin Alsoufi, MD, pediatric cardiothoracic surgeon for this issue’s cover story. As the doctors described the process for neonatal pediatric cardiac care, we were reminded again of life’s miracles and the care given to the most vulnerable in need.
I invite you to read their story beginning on page 12.
Two of our Special Section physician profiles illuminate new treatments and approaches in women’s care. Vaginal birth after a caesarean delivery is a trend that reverses the previously held belief, “Once a c-section, always a c-section.” Ann Grider, MD, partner at Women First of Louisville, talks about the VBAC.
Pelvic pain in women, often as a result of childbirth, can be treated by pain-mapping, a process that isolates specific elements and follows multi-dimensional treatment. Danesh Mazloomdoost, MD, of Wellward Regenerative, explains the HEALS system on page 22.
We have two opinion columns in this issue of MD-Update that address current issues in American culture and healthcare: the need for diversity in the healthcare workforce and the need for more physician-driven data on intersex and transgender treatment in pediatrics and adolescents. I expect some readers to have counter opinions to our contributing columnists and I invite those readers to share those opinions with us.
The opinions of the columns are those of the columnists and do not necessarily reflect the views of MD-Update
Looking ahead to the fall, we’ll be talking to orthopedics, sports medicine, oncologists, radiologists and neurologists. If you see your specialty in the editorial calendar and have a story to tell, let us hear from you.
MD-UPDATE MD-Update.com
Volume 11, number 3
ISSUE #134
PUBLISHER
Gil Dunn gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda DeBord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC Chip Dalton
Scott neal, CPA, CFP
Cameron S. Schaeffer, MD, FACS, FAAP

Geraldine Q. Young, DPn, APRn, FnP-BC, CDE, FAAnP
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com
Mentelle Media, LLC

38 Mentelle Park Lexington KY 40502
(859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky.
Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2021 Mentelle Media, LLC. All rights reserved. no part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter.
Thank you.
Individual copies of MD-Update are available for $9.95.
All
SEND YOUR LETTERS TO THE EDITOR TO: Gil Dunn, Publisher gdunn@md-update.com, or 859.309.0720 phone and fax






LEXINGTON On April 28, 2021, CHI Saint Joseph Health officially welcomed new CEO Anthony A. Houston, FACHE, during an investiture service at Saint Joseph Hospital. The service came as Houston concluded his first few weeks as CHI Saint Joseph Health CEO and president of Saint Joseph Hospital and Saint Joseph East.
“As I have made my rounds across the ministry these first few weeks, I have asked these two simple questions – ‘How long have you worked at CHI Saint Joseph Health, and what do you love most about working here?’ said Houston. “Family, home, community, trust, and a love for one’s vocation are the themes that came from my rounding.”
“I would suggest there is a DNA thread that makes CHI Saint Joseph Health a distinctive and special ministry. I am truly blessed to serve with you, and I can tell you that I love what I do, and I love doing it here,” said Houston to the assembled audience.
Houston has more than 20 years of healthcare leadership experience and joined CHI Saint Joseph Health from CHI Memorial in Chattanooga, where he was the president and market COO. He previously served as president of CHI St. Vincent in Hot Spring, Arkansas. Like CHI Saint Joseph Health, CHI Memorial and CHI St. Vincent are part of the southeast division of CommonSpirit Health.
Houston had been passionate about CHI Saint Joseph Health long before taking on this new role of CEO. Houston was raised in Cincinnati, graduating from the University of Cincinnati and receiving a master’s in health
services administration from Xavier University. His father was born in Stanford, Kentucky and was raised in Rockcastle County. At age 12, the senior Anthony Houston was hit by a vehicle while riding his bike. He was taken to Saint Joseph Hospital and over the course of three weeks had multiple surgeries on his legs. He attributed his survival to the care he received at Saint Joseph Hospital, and Tony Houston said he would not be here today if not for the care his father received.
Houston’s grandfather was a dairy farmer in Rockcastle County and was committed to his community and loved serving Kentuckians. Houston says he looks forward to leading CHI Saint Joseph Health and the patients it serves across Kentucky with this same commitment his grandfather once exemplified.
“My grandfather loved what he did and loved doing it for his community,” said Houston. “That same commitment to high quality, service, and accountability and a passion for doing good for others fires my drive to do this work here at CHI Saint Joseph Health.”
In an interview with MD-Update, Houston said that the pandemic accelerated a trend in healthcare, both the challenge and the opportunity to “meet people where they are.” Healthcare is not a hospital-only based industry, he says, “and our goal is to provide care as close to the patient’s home as possible. There are now so many points of access, telemedicine being the most dynamic. The hospital is vital, and the pandemic taught us the importance of keeping the supply chain intact and ensuring we have the right people with the right skill set and materials.”

One of Houston’s skill sets is listening, he says. Listening to patients, and listening to physicians and staff to hear what they need. “The power of relationships between primary care doctors, patients and specialists; we need to make sure those relationships are initiated and sustained. Turning healthcare into a lifelong relationship, not just in emergency or during critical care,” he says.
On May 26 CHI Saint Joseph Health announced an expansion of its affiliation with Cleveland Clinic Cancer Center to the CHISaint Joseph Health hospitals in London/ Corbin, Mount Sterling, and Flaget Memorial Hospital in Bardstown. The affiliation gives Kentucky cancer patients access to second opinions and input into treatment plans without having to travel.
“Since we launched the affiliation in October 2019, more than 220 patients have benefited through consultations, tumor board review, and input into treatment plans, all without having to leave their home communities,” says Houston.

Other initiatives for CHI Saint Joseph Health will be a new electronic health system, the EPIC System, next year beginning in the summer of 2022, says Houston. “This will be the first time that the entire ministry of CHI Saint Joseph Health will be on the same electronic medical records system. This platform will allow us to extend services beyond the brick and mortars, to remote locations,” says Houston.
It doesn’t take long to get from CHI Saint Joseph Health hospitals in Mount Sterling, London or Bardstown to rural areas. Houston notes that increased broadband in rural areas of Kentucky needs to be a priority of leaders in Frankfort and Washington D.C.
Workforce development is a passion for Houston, encouraging young people to enter healthcare, not only as doctors and nurses, but also technicians and other employees. “We all have the capacity to lead,” says Houston. “Physicians are leaders and I encourage all doctors, regardless of title, to continue to lead. We have an open door at CHI Saint Joseph Health. We ask doctors to lean in and tell us what is working well and where we can improve and innovate.”
The CHI Saint Joseph Health Foundation was part of Houston’s interview process, meeting with Foundation members. Houston gave mention of the Foundation’s “Evening of Hope” and the exceptional staff and volunteer organization. “This organization of Saint Joseph Health was founded in 1877
by women at a time when they couldn’t vote. The spirit of commitment, fellowship, entrepreneurship, and dedication to ‘a greater good’ continues today, says Houston.

 CHIP DALTON, HEALTHCARE SERVICES SENIOR CONSULTANT
CHIP DALTON, HEALTHCARE SERVICES SENIOR CONSULTANT

An effective and patient-friendly customer service team is critical to ensuring a positive patient financial experience. With increased focus on pricing transparency and more knowledgeable consumers, it is the customer service unit within your organization that can greatly determine a patient’s overall financial experience.

These four key principles can help improve your customer service function.
• Handling all patient complaints and billing concerns. Patients need someone knowledgeable who can help them navigate their statements, be empathetic, and address any concerns they may have about the experience they have had at the organization.
• Delegating all correspondence and insurance remits. Customer service representatives can provide essential assistance by assigning specific correspondence and remits from insurance companies to the appropriate party.
• Coordinate and monitor early out vendor. The customer service representatives are vital in monitoring patient statements being sent to the patient in a timely manner and in sequence.
• Monitor and complete self-pay refunds. If a patient pays more than their responsibility, the customer service department can confirm these overpayments and complete a refund for the patient.
As you assess the efficacy of your patient financial experience, consider these key questions:

1. Does your organization have a dedicated customer service unit and place a specific emphasis around the patient from end to end of the revenue cycle (scheduling through payment)?
2. Does your organization have personnel whose main job function is answering phone calls from the patient and addressing their concerns?
3. Do you consistently field complaints from patients on not receiving their statements in a timely maner, not understanding their bill, or feeling as their issue is not addressed?
4. Does your organization offer tools to the patient that keep them engaged in their care through an online patient portal or secure messaging system, so the patients can efficiently and effectively reach customer service staff members?
As organizations develop a holistic approach to treating patients, the customer service unit will be critical to addressing a patient’s concerns. This unit can potentially lead to recurring patient volumes, increased patient collections, higher HCAHPS scores, fewer patient complaints, increased efficiency in revenue cycle processes, and risk mitigation. Our experienced healthcare team can aid in implementing a new customer service team and assessing other areas around improving a patient’s experience.
I don’t suppose that I need to spend a lot of time reminding you that 2020 and Q1 2021 have been tumultuous in the financial markets. But the markets are arguably at a critical juncture as we emerge from the pandemic. Now would be an excellent time to look forward.
It is time to stop and take stock of what happened to YOU specifically over the past 18 months. If you are like most people, you began 2020 thinking that it was going to be a pretty good year. Pundits agreed. If you recall, I speak often of the five things (and only five things) one can do with all the money received each year: 1) pay taxes, 2) pay on debt, 3) give some, 4) save some, and 5) spend the rest. It’s pretty easy to know the first 4 with a reasonable degree of certainty. That means if you know how much came in (hint: check your tax return) you can solve for how much you must have spent by simply subtracting the first four. (If you have seen cash build up in checking accounts be sure to claim that increase as savings.) This little exercise will likely reveal that you didn’t spend as much as you do in more “normal” years. That makes sense. Millions of Americans are in the same boat, spelling pentup demand. More on that in a minute.
One Harvard economist estimates that there is $1.8 trillion of accumulated disposable income since the start of the pandemic. This should make for a very robust increase in GDP in the second quarter. Like most, our data collection tool measures economic details in year-over-year comparisons as well as month-over-month growth or decline. The year-over-year numbers for the next couple of quarters compared to last year are going to look outstanding. Take a long view.
Now, add in 1) an administration that is ready and willing to provide stimulus, and 2) an accommodative Federal Reserve (keeping interest rates low and buying bonds), and the stage is set for some hearty growth. But this
situation is not without its risks. By almost any measure, stocks are overvalued. And just consider what has happened to home prices. Over the past three months, we have spoken to many about either buying or selling a house. Nearly everyone has been shocked that actual selling prices are routinely above the asking price. This provides what economists call wealth effect.
Back to risks. The greatest threat is likely to be rising interest rates. Even if the Fed is successful in maintaining low short-term rates, ultimately, the Fed and President Biden will learn that it is the bond market that is in charge of long-term rates. Big deficits don’t necessarily mean higher rates. The bond market will stand behind (i.e., keep rates low on the long end despite huge deficits) as long as it can see a positive rate of return (properly determined) on projects being funded by the debt. Inflation remains a key variable.
Suppose for a moment that inflation kicks up to 3%, or 4%, or higher. Will the bond market continue to buy bonds that pay 2% and suffer negative real return (net of inflation)? Not likely. Bonds are bought at auction. Interest rates will be bid up in the face of inflation. The question of whether inflation will be temporary or permanent is on a lot of minds. One noted British economist has deduced from demographics that the next major round of inflation will occur in the U.S. between 2025 and 2050.
Some have pointed to the flow of money into the economy and have said that it must be inflationary. That is not correct. We just need
to look at the period since 2008 for proof. Very large deficits were combined with unparalleled stimulus and extremely low unemployment, yet no inflation. The one cause of inflation/ deflation is the movement of supply and demand. If the demand curve moves out faster than the supply curve, inflation will ensue. Without a doubt, the pandemic has negatively affected supply of many goods, notably computer chips, causing the supply curve to move backward just as huge pent-up demand is being unleashed. Expect inflation, but do not expect it to be permanent. At least not for now.
One risk to a full recovery is the likelihood, perhaps small, that the vaccines are not as effective as we thought they would be in the long run, and that variants to the virus will derail herd immunity. I trust that this readership knows a lot more about that than I do, and I welcome your input.

Another risk that we see a lot of today is the desire of investors to take on more risk at just what could become the wrong time. Speculation has replaced investing in many circles, especially young investors who follow Reddit or some other social medium. Buying on margin and participation rates of IPOs for companies that aren’t even profitable carry substantial risk.
So what do you do? In the short run, keeping an eye on the ball is crucial. Know where you stand. We continue to monitor stock prices. As they hit new highs, we move up our alerts. When prices pull back a bit, the alert fires and we must decide whether to take profits or continue to hold. Whatever you do, do not fall into a complacency trap.
“Speculation has replaced investing in many circles.”
— Scott Neal
 BY CAMERON S. SCHAEFFER, MD, FACS, FAAP
BY CAMERON S. SCHAEFFER, MD, FACS, FAAP
LEXINGTON When I met “Tom,” he was a teenage boy lying in the fetal position on my exam table, sucking his thumb. He had been referred to me for comprehensive female to male genital reconstruction, having been born XY with dysfunctional androgen receptors (androgen insensitivity syndrome), which caused his genitalia to virilize inadequately during development. Because his phallus resembled a clitoris, and because his cleft scrotum resembled labia majorae, a team of doctors made the decision to remove his abdominal testes, to further reduce his diminutive phallus, and to split further his scrotum. The procedure was successful, but the results were disastrous.
Years later, I met “Kathy,” another XY patient with a severe defect in “his” testosterone receptors. Like Tom, she had also been reconstructed as a female as an infant. A tomboy all her life, she liked to hunt and fish and was enrolled in high school ROTC. She had a boyfriend, and she wanted a vagina. The “team” got lucky with her.
Over the years, I have cared for a few XY patients with cloacal exstrophy. These patients are born with an unusable, split phallus, so they were historically reconstructed as females. Every XY cloacal exstrophy patient I have met identifies as a male or is a lesbian.
More frequently, I have cared for XX patients with congenital adrenal hyperplasia. Due to elevated levels of fetal androgens, these patients can be born with utterly ambiguous genitalia. But female CAH patients are potentially fertile,
and, while often tomboys, most of them go on to become well-adjusted women.
From these anecdotal experiences, I learned that the most important sex organ is the brain which, when partially androgenized, is unpredictable, and that protecting the emotional health and potential fertility of a patient is sacrosanct. We know from the Nuremburg Trials that group psychology is more powerful than personal morality. Sometimes the judgment of a team of specialists, which can be subject to groupthink and bullying, is no better than the judgment of a single surgeon, and sometimes worse.
Intersex patients, like those just described, are not transgender, and gender is not sex. Transgender individuals have normal chromosomes, normal enzymes, and normal anatomy. If a transgender woman commits a crime and leaves her blood at the scene, the cops will be looking for a man.
A few years ago, I examined a small boy who, much to my surprise, was wearing girls’ panties. I made a light-hearted remark about it being laundry day at my house too, and, as if I had uncorked a bottle, I was met with a torrent of angst from his mother. The boy apparently only wanted to wear his sister’s clothes and to play with her dolls and to play dress up and what should she do? I reassured her it was likely a phase and counseled love, patience, and observation. But I wasn’t sure if that was good advice.
These days, that mother can easily find a clinician at one of the pediatric gender clinics popping up all over the country, including clinics in Lexington, Louisville, and Cincinnati. That clinician might affirm her child’s inchoate transgenderism and lead her and her child down a path of body-changing steroids and counselors ready to assist everybody with the transition. But are these clinics built on solid foundations of data, or just well-intentioned compassion? And to what extent are these clinics phenomena of physicians and hospital administrators responding to an emerging marketplace? The Transgender Health Clinic at Cincinnati Children’s Hospital invites to its clinic children as young as five years old! Is this approach superior to love, patience, and observation? Who knows?
Until recently, transsexuals had to pay out of pocket for care, which certainly tested their commitment, especially if surgery was pursued. Under the pressure of activists, medical care for transgender individuals is increasingly being covered by insurance of various sorts, so expect more clinicians to jump into the business.
When chaos reigns, laws get written. Sometimes those laws can be rash. If lawmakers perceive that the pediatric community is not
adequately protecting children, they will step in. The Arkansas legislature recently passed a bill banning transgender medical therapy for children. Governor Asa Hutchinson vetoed the bill, citing government overreach into medical and parental matters. The legislature overrode the veto, enacting the law. The AMA stepped into the debate, decrying any encroachment of government on patient privacy and the doctor-patient relationship. That is rich coming from an organization that is now essentially a government-sponsored medical coding business, colluding with payers to label patients with codes that reveal their most personal secrets, accessible by complete strangers.
Both the legislative and executive branches of the Arkansas government likely did the right thing, yet nothing has been solved, as those institutions, and the people they represent, are still groping in the darkness we physicians have failed to illuminate with data. In the meantime, confused and sometimes suffering children have been turned into political pinballs.
For centuries, humans have recognized that adolescence is a time of confusion, experimentation, and risk-taking. This is probably evolutionarily adaptive. It is the duty of adults to offer love and guidance during this period, but also to set boundaries. A person’s judgment may not fully mature until the age of 25.
These days, a collision of economic dislocation, community breakdown, family breakdown, individualism and “personal truth,” the political assertiveness of activists obsessed with genitalia and what they and others do with their genitalia, and the internet has fueled an epidemic of transgenderism. A confused adolescent now has hand-held, ready access to pornography depicting every conceivable combination of human beings having sex, and to anonymous online activists ready to give affirmation, advice, and encouragement. This is child abuse hiding behind the First Amendment.
We know that transgenderism can be a passing phase for some adolescents, occurring acutely and in clusters of children just try-
The Pain Treatment Center of the Bluegrass announces our partnership with CHI Saint Joseph Health system. As one of the oldest and largest private multidisciplinary pain centers in the region, delivering comprehensive pain care, The Pain Treatment Center of the Bluegrass will be the preferred pain management provider to all hospitals in the CHI Saint Joseph Health system. The Pain Treatment Center of the Bluegrass will now be performing its procedures at CHI Saint Joseph Health Outpatient Surgery Center.
NEUROLOGY/NEUROIMAGING
Peter D. Wright, M.D. Medical Director Director of Neuroimaging ANESTHESIOLOGY
Ballard D. Wright, M.D. Founder and Medical Director
Dennis Northrip, M.D.
Karim Rasheed, M.D.
ADDICTION MEDICINE
Traci Westerfield, M.D.
FAMILY PRACTICE
Laura Hummel, M.D.
PHYSICAL MEDICINE AND REHABILITATION
Lauren Larson, M.D.
INTERNAL MEDICINE
Anand Modadugu, M.D.
PALLIATIVE CARE
Christopher Lyon, M.D.
BEHAVIORAL MEDICINE
Narda Shipp, APRN
Kellie Dryden, LCSW
Marie Simpson, LCSW
PHYSICAL THERAPY
Jason Goumas, PT, CSAS
PHYSICIAN ASSISTANTS
Lois Wright, MBA, PA-C
Celeste Christensen, PA-C
Shari Pierce, PA-C
Jing Ye, PA-C
NURSE PRACTITIONERS
Becky Moore, APRN
Teri Partin, APRN
Lynne Shockey, APRN
Dijana Duval, APRN
April Luttrell, APRN
Tabitha Knight, APRN
LEXINGTON: 2416 Regency Rd. SOMERSET: 110 Hardin Ln., Ste. 4 (859) 278-1316 ext 258 (859) 276-3847 pain-ptc.com
ing to fit in. We also know that transgender youths have high rates of depression and suicidal ideation. It is not at all clear that gender affirming hormonal therapy and surgery are helpful. Surgery is usually irreversible, and hormonal therapy can permanently alter bone growth and impair fertility. The studies needed to determine the proper care of these children will require many years and many patients to yield meaningful data. Such studies will be difficult to perform because of the emotionally and politically charged nature of transgenderism, but they need to be done. In the meantime, any therapy that permanently affects these children mentally or physically obviously calls for prudence.
Unfortunately, this is all occurring in the milieu of “wokeness,” which seeks to redefine individuals, the family, the community, and the nation’s institutions, often with a whiff of intimidation. The pendulum will likely swing. There is plenty to debate in the era of wokeness, but we physicians should submit to data, not political agendas, to determine the proper mental and physical care of children.
FAX (Both locations) 859 275 5434

Changes have occurred since the Civil Rights Movement of the 1960s to improve the treatment of Black people; however, the underpinnings of systemic and structural racism are alive and well in the United States. Through the inequitable outcomes of the COVID-19 pandemic, 2020
bestowed upon us an undeniable reality check on the national impact of systemic and structural racism in our healthcare delivery system. As of March 17, 2021, the Centers for Disease Control (CDC) reported 533,057 COVID deaths in the U.S. Of the 289,119 deaths in which the race was known, 14% of the victims were identified as Black, non-Hispanic. Although underrepresented in the U.S., Black people disproportionately led the death toll rates as they suffer from existing socioeconomic hardships in addition to the adversities brought on by the pandemic.
The COVID-19 pandemic has shone a light on the health disparities and inequalities that people of color suffer from daily. The lack of trust for the COVID-19 vaccine embodied within the Black community due to historical and current medical negligence and bias provided by a vastly white population of healthcare professionals compounds this problem. In November 2020, a survey conducted by the National Association for the Advancement of Colored People (NAACP) revealed that only 14 percent of Black respondents trusted the vaccine and only 18 percent indicated that they would definitely get vaccinated.
Healthcare disparities extend beyond the pandemic, however. For example, according to 2017 data from the CDC, Black women are three to four times more likely to die of pregnancy complications than white women. Contributing factors to these disparities are financial, bureaucratic, transportation, language barriers, and care that is not consistently culturally appropriate or respectful.

To abate these tragic, disproportionate outcomes and build trust within the U.S. healthcare delivery system, the healthcare workforce must become more diverse. Our nation’s population is continuously changing and becoming more diverse. The healthcare workforce must change to match. The United States Census Bureau predicts that by 2045, over half of the U.S. population will consist of minority populations. The American Association of Colleges of Nursing (AACN) states, “With projections pointing to minority populations becoming the majority, professional nurses must demonstrate a sensitivity to and understanding of a variety of cultures to provide high-quality care across settings.”
Culturally congruent health care providers representing racial, ethnic minority populations improve trust in the health care delivery system, quality of care, and outcomes of minority populations. A 2017 report by the National Institutes of Health determined that cultural respect was an essential factor in
reducing healthcare disparities and improving access to quality health care for diverse patients. According to data from the National League of Nursing and the U.S. Census Bureau, approximately 80% of registered nurses, nurse practitioners, and nurse-midwives are white. Schools of nursing must also develop strategies for increasing diversity within the nursing workforce.
An example of this shift can be found at Frontier Nursing University, which, over the past decade, has placed an emphasis on diversity, equity, and inclusion (DEI), with a particular focus on increasing the enrollment and graduation rates of students of color.

FNU included DEI in its strategic plan to address issues surrounding access to healthcare, health outcomes, health disparities, and health inequities, and to increase diversity in nursing. These efforts will play a significant role in ameliorating health disparities and inequities. FNU’s SOC enrollment has grown from 9% in 2010 to over 25% in 2020. FNU is continuing on the trajectory of integrating
DEI and antiracism throughout the university to support racial, ethnic underrepresented students. Resilience during the COVID-19 pandemic permitted FNU to graduate 841 students, including 208 students of color, yielding an increased workforce diversity to care for diverse, rural, underserved populations. Additionally, FNU’s current retention rate for SOC is 84%, exceeding the university’s goal of 80%, and the number of faculty of color is on the rise, currently standing at 14%.
FNU is an example of the intentional focus required to begin building a more diverse, culturally competent health care system. We have known and understood for a while now that the lack of diversity among primary health care providers is a contributing factor to the glaring disparities in health care outcomes among diverse populations. The past year only acted to exacerbate the problem and heighten our awareness of the need for immediate change and action. If we have learned anything from the pandemic, it is that diversity, equity, and inclusion are the keys to the future success of our nation’s health care delivery system.
 BY JIM KELSEY
BY JIM KELSEY
LOUISVILLE In the movies, the Avengers are a group of superheroes of varying superpowers and talents. They come from countries – even planets – far and wide, joining together in a fight against a singular foe.
At Norton Children’s Heart Institute (NCHI) in Louisville, the superheroes don no special costumes. Their masks are worn to protect those they serve, not conceal their identities. Rather than superpowers, they are armed with advanced technology, essential tools, and extensive education and experience. These, it turns out, are often all they need to save a child’s life.
Perhaps their greatest power is their ability to teach many of the same powers to “mere mortals,” creating a whole new team of superheroes prepared to take care of these children during their treatment and recovery. In this case, those
empowered mere mortals are usually the child’s parents or other family members.
“I sometimes joke that they become super parents,” says Brian J. Holland, MD, pediatric cardiologist at NCHI. “They have invisible capes behind them. They become experts ready for whatever their babies need.”
While there is no way for expecting parents to prepare for the news that their baby has a heart defect, there is a way to help them prepare to care for such a baby. Thanks to early detection often made by the obstetrician, parents can learn about the baby’s congenital heart abnormality, what they can expect, and how they can be ready when the baby is born. To make it as comforting as possible for the families, prior to the birth, parents have a meeting with the medical team that will be taking care of their child.
“They have multiple appointments scheduled in the same setting, where they
see the surgeon who explains to them based on the echocardiogram what is the anticipated treatment that is required,” says Bahaaldin Alsoufi, MD, chief of the Division of Pediatric Cardiac Surgery, University of Louisville School of Medicine, and director of pediatric cardiac surgery, Norton Children’s Heart Institute. “We prepare them. We talk to them about expectations, risks, any potential complications. They leave with a large packet that explains not only what they need to know about the specific heart defect that their child has, but also explains the post-operative care and long-term care. At the same time, they see the neonatal intensive care unit physicians, who explain to them about the delivery and what they’re going to do to stabilize the baby until we do the surgery. They meet the nurse practitioners who are going to continue to follow the patients at home. They meet others who are going to be taking care of them, for
example interventional cardiology. It gives them a lot of time to digest the information, to learn more, and to coordinate the care.”
Originally from Syria, Alsoufi obtained his medical degree from the University of Damascus in Syria. He then moved to the United States and did his residency in general surgery at the University of Massachusetts. He then did a fellowship in cardiothoracic surgery at Oregon Health & Science University and another fellowship in pediatric cardiac surgery at the University of Toronto’s Hospital for Sick Children.
He served as associate professor of surgery at Emory University and as a congenital cardiac surgeon at Children’s Healthcare of Atlanta before coming to Louisville in 2018. Alsoufi, who is married with four daughters, specializes in all aspects of pediatric and adult congenital cardiac surgery with special interest in complex neonatal cardiac surgery, single ventricle palliation, pediatric valvular heart disease, and heart transplantation.
Alsoufi’s patient population includes any children under 18 and adults with congenital heart disease requiring heart surgery.
“I initially became interested in cardiothoracic surgery itself because of exposure during childhood with multiple members of my family needing cardiac surgery,” Alsoufi says. “I became especially interested in the pediatric cardiac surgery subspecialty because I found it much more fascinating because of the complexity of the congenital anomalies that the babies are born with and the critical situation that they’re in. It is a very rewarding profession.”

Though he was born in Pittsburgh, Pennsylvania, Holland’s path to Louisville— like Alsoufi’s—included a bit of world travel. He attended high school in Augusta, Georgia, and went to college at the University of Pennsylvania, majoring in bioengineering. He went to medical school at the Medical College of Georgia. He then served in the Army, completing a three-year residency in pediatrics at Tripler Army Medical Center in Hawaii.
“I owed four years of service to pay back my college scholarship and got assigned as a pediatrician in Germany,” Holland says. There he delivered babies and took care of the American families who were stationed in Germany. “In the eyes of the Army, they thought that a lot of soldiers were just glorified teenagers in that they were healthy and didn’t

have a lot of other medical problems. They had pediatricians deploy as physicians for units that were going into either Iraq or Afghanistan. I was deployed for a year in Afghanistan with an infantry unit to take care of the soldiers who were there.”
Perhaps influenced by his military experience, he liked the idea of taking care of children who needed specialty care. When he returned to the United States, Holland completed a fellowship in pediatric cardiology at New York-Presbyterian Hospital. A year later, he came to Louisville, joining NCHI and the University of Louisville Division of Pediatric Cardiology in 2010.
At the University of Louisville and NCHI, Holland treats patients with congenital heart disease. He also sees patients in clinic and in some outreach clinics, including a three-day trip to Paducah every month with two physicians, sonographers, medical assistants, and front desk staff.
Together Alsoufi and Holland are part of a comprehensive team dedicated to the care of the sickest of children. Alsoufi estimates that more than 90 percent of pediatric heart disease cases are congenital. The presentations in these babies vary, with some requiring neonatal surgery while others can wait until a later age. Because of advanced detection, the majority of the neonatal cases are diagnosed before birth. This allows the time for the family to be informed and educated, and to prepare to care for their child.
“It makes the whole experience completely different than if the baby wasn’t known to have a heart problem and got transferred in the middle of the night because they turned blue,” says Holland.
That doesn’t mean the process is easy on the parents. The first “Meet the Team Day” when the parents learn more about the condition of their unborn child is impactful, informative, and emotional.
“At that first visit oftentimes there are tears,” Holland says. “We need to have Kleenex in the room and it is a long conversation. I usually start by drawing them a picture of a normal heart and drawing a picture of what we can see on the ultrasound, and then trying to explain what the heart condition is, just from the map, from the anatomy, from the chambers and the walls and the blood vessels, et cetera. We have experience with these types of heart conditions and that I think is a great source of comfort to them.”
The key to being able to prepare both the family and medical team is early detection. Holland performs fetal echocardiography, which utilizes an ultrasound to find heart problems during pregnancy.
“Sometimes when we’re looking during pregnancy, we get the chance to be the first ones to map out that baby’s heart,” Holland says. “It’s a very complicated thing, because it’s a map that’s rotating in three dimensions, even in front of your eyes, to try to figure out what the connections are and are they normal or abnormal, and then help to guide the treat-
ment if we do find that the baby has a heart condition.”
Some of those heart conditions include babies with a single ventricle. In some cases with babies who have major problems with the heart muscle or valves, a heart transplant is required and ventricular assist devices might need to be implanted to support the patients until they are able to receive the transplant.
“The heart is small and the defects are complex,” Alsoufi says. “There are technical and physiological challenges in these surgeries. However, that’s where adequate training and adequate experience becomes important. We are fortunate to live in an era where congenital heart surgery has developed substantially. We have the experience and the technology to be able to take care of these patients as compared to 50 or 60 years ago when many of those patients did not make it.”
Alsoufi and Holland want to spread the word about the advances in detection, treatment, and care and the increasingly positive outcomes. “We have a very comprehensive and experienced team that can take care of the most complex heart defects in children without any exception,” Alsoufi says.

It’s a team of superheroes that includes, but is not limited to, 20 pediatric cardiologists, sixteen nurse practitioners, three pediatric heart surgeons, six neonatal intensive care doctors, and five cardiac anesthesiologists.
“I don’t think that one really well-trained physician is in any way the current best way to provide the best care,” Holland says. “You have to have teams of people. You have to have the different parts of the care connected and coordinated in order to really provide the best possible care.”
These superheroes’ capes may be invisible, but they wear their hearts on their sleeves.
“We are fortunate to live in an era where congenital heart surgery has developed substantially. We have the experience and the technology to be able to take care of these patients as compared to 50 or 60 years ago when many of those patients did not make it.”
— Dr. Bahaaldin Alsoufi, MD, chief of the Division of Pediatric Cardiac Surgery, University of Louisville School of Medicine and director of pediatric cardiac surgery, Norton Children’s Heart Institute.Brian J. Holland, MD, pediatric cardiologist at NCHI and the University of Louisville Division of Pediatric Cardiology.
With three campuses, expanded outreach locations and over 500 pediatric providers, getting your patients into a Norton Children’s specialist has never been quicker or easier. As our footprint grows, so does our commitment to you and your smallest patients.
To make a referral to a Norton Children’s provider, call (844) 629-KIDS (5437) or use the new and improved NortonEpicLink.com. For assistance, email epiclink@nortonhealthcare.org

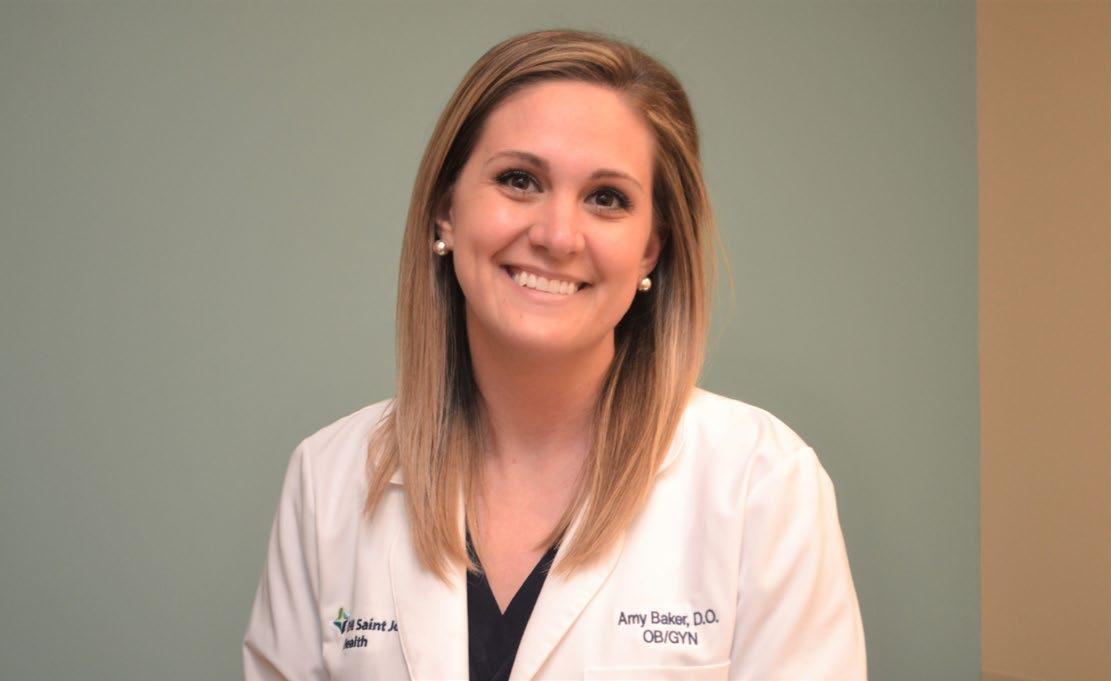
LEXINGTON During her third year at Pikeville College of Osteopathic Medicine, Amy Baker, DO, underwent a life-changing experience— she helped deliver a baby. “The day that I got to assist with my first delivery is the day I knew I wanted to be an OB-GYN. I knew that getting to deliver babies was something I was never going to get tired of,” Baker says. “After the end of that day, I called my mom and my face just hurt from smiling so much. It really just brought me that much joy to help deliver that baby.”
Upon her graduation from Pikeville College, Baker completed her residency at Grandview Medical Center in Dayton, Ohio. She then immediately returned to her beloved home state of Kentucky to join CHI Saint Joseph Medical Group – Obstetrics & Gynecology.
Baker credits her background in osteopathic medicine with allowing her to better serve her patients. By taking a more “whole-person” approach to medicine, Baker is able to address many of the pain issues that normally accompany pregnancy. She stated, “I think the biggest thing that being a DO has added to my training is the extra knowledge of the musculoskeletal system. I think that I use it most with my obstetric patients who are having the common aches and pains of pregnancy. I can give them ways to help with that during the pregnancy and even postpartum.”
Baker elaborates, “There’s muscle energy techniques we can use here in the office for management. Oftentimes I give people stretches they can do at home for low back pain and sciatic leg pain to get them through the pregnancy while we wait for those symptoms to resolve over time and after delivery.”
As an OB-GYN, obstetrics is only a portion of Baker’s practice. She treats women in all phases of their life with a focus on achieving gynecological health in all ages and at all stages. According to Baker, “I really do a pretty even mixture of both obstetrics and gynecology. We see women of all ages, from our adolescents to women that are past menopause.”
CHI Saint Joseph Medical Group –Obstetrics & Gynecology offers a full range of services. For those in their reproductive years, they provide family planning, pregnancy testing, prenatal and postpartum care, and labor and delivery. Females reaching middle age can benefit from their menopausal symptom and osteoporosis care and treatment. Women of all ages have access to preventive and gynecological cancer screenings and breast health assessments and advice. CHI Saint Joseph Health is also at the forefront of utilizing minimally invasive gynecological procedures and state-of-the-art, robotic surgery.
With women of all ages, two of the most important treatment components are education and emotional support. Often, this starts
with a conversation about gynecologic health and family planning.
During an initial visit, she may also discuss the HPV vaccine, GARDASIL 9, which has been proven to prevent the vast majority of cervical cancers as well as other gynecologic cancers and genital warts. Baker states, “It’s just a wonderful vaccine we now have available for our patients. And it’s not just for young patients. That is the ideal time for them to get it, but it can be given to people all the way up to age 45.”
For her patients who have become pregnant, supplying a comprehensive understanding of breastfeeding is a main priority. Early in the third trimester, Baker establishes whether or not the patient desires to breastfeed. Baker states, “It’s not ever something that I want to force on moms. The general knowledge is that it is what is best for babies, but fed is really best. So, we just base it on mom’s desire, and how she wants to feed her baby.”
If the woman indicates that breastfeeding is her method of choice, she is encouraged to attend the free classes offered at CHI Saint Joseph Health, and Baker opens the topic for further discussion and questions. “We really like to talk about breastfeeding during the pregnancy so the patient knows what to expect and what services are available if she were to have problems with breastfeeding. And we like to follow up in two weeks to make sure moms aren’t having signs of pain, which could be indicative of poor latch, or that they’re not having redness or fevers that could be symptoms of mastitis.”
During this follow-up, Baker also brings up the important topic of postpartum depression. According to Baker, “We normally see people back at least twice after a normal, uncomplicated delivery. Something I am very passionate about is screening for postpartum depression during that time. We do a screening with a
Utilizing her background in osteopathic medicine, Amy Baker, DO, is dedicated to providing the most holistic gynecologic care for women in all stages of life.
“The day that I got to assist with my first delivery is the day I knew I wanted to be an OB-GYN. I knew that getting to deliver babies was something I was never going to get tired of.”
— Amy Baker, DOPHOTO BY GIL DUNN
standard Edinburgh postpartum form.”
Some of the symptoms for which the form screens are sadness, crying, inability to cope with everyday activities, feelings of anxiousness, irritability, and sleep disturbances. If it is determined the patient is suffering from postpartum depression, Baker may make a referral to a psychiatrist or a psychologist as well as prescribe an SSRI medication that is deemed safe for use during breastfeeding.
For many women, a yearly visit to a gynecologist is the only time they see a physician, so being in-tune with the emotional, as well as the physical, well-being of her patients is a primary goal. “It’s kind of a joke that we practice ’gynechiatry.’ Mood issues are related
to our relationships and our sex life, and so a lot of time the psychology problems come up in our histories and exams with our patients. I definitely think it’s important as an OB and a GYN to have a pretty strong understanding of psychology,” Baker says.
In closing, Baker reiterates her role in the overall health of all women: “I think it’s important for patients and other people in healthcare to know that gynecologic care doesn’t just stop when you’re done having babies or when you’re done having periods. We care for women of all ages, not just women during those reproductive years. We really do have a lot to offer women in those early teenage years and well past menopause.”

“We care for women of all ages, not just women during those reproductive years. We really do have a lot to offer women in those early teenage years and well past menopause.”
— Amy Baker, DO
LOUISVILLE When Ann Grider, MD, joined Women First of Louisville in 1998, the pendulum had gone from the long-time assumption in medicine of “Once a C-section, always a C-section to the 1990’s, when women practically had to beg for a repeat C-section once they’d had a C-section,” Grider says. “Today women have more choices for vaginal birth after cesarean. It’s good to give them a full picture of their options and risks so they can make informed decisions.”

According to the American College of Obstetricians and Gynecologists (ACOG), in 1970 about 5% of babies in the United States were delivered by cesarean section. By 1988, that number had climbed to nearly 25%. Today about one third of births happen by C-section, making it one of our nation’s most common operating room procedures. Various technical, professional, and legal factors likely contributed to this increase. Yet, despite increased risk for childbirth-related complications when a woman has multiple C-sections, rates for vaginal birth after cesarean section (VBAC) are low—just 13.3% in 2018. One contributing factor for the low rate might be that smaller or rural hospitals may lack specialized facilities or staff to perform an emergency C-section should it become necessary during an attempted VBAC. In circumstances like this, a repeat C-section is generally a safer choice.
Grider explains that a successful VBAC and planned repeat C-section delivery generally have comparable risks. However, in a situation when an attempted VBAC fails and a repeat C-section becomes necessary, the risks
for both mom and baby go up.
“The safety of our moms and babies must always come first,” Grider says.
Women First focuses on maximizing safety and minimizing potential VBAC risks. The practice has an 85-90% VBAC success rate in patients who have a trial of labor after a C-section. The national success rate, as recently reported by the National Institutes of Health, is 75%.
Grider credits their success to three factors:
• The practice delivers exclusively at Baptist Health Louisville. Working with one hospital offers certain advantages, such as 24/7 access to anesthesiologists, laborists, and a Level II neonatal intensive care nursery with neonatal staffing.
• The team is highly selective in approving VBAC candidates. They thoroughly assess each candidate’s delivery history, including scar-related risk factors and whether her previous cesarean was done for reasons that could tend to recur.
• They work closely with approved VBAC candidates to help them develop personalized birth plans.
Women First considers a personalized birthing plan a critical element of a successful VBAC delivery. Each patient’s plan reflects the birthing process and experience she expects for herself and her baby. It also includes key information about mom’s overall health, risk factors, and cesarean history.
Some of the plan’s components can be confusing or sensitive. Weight, for instance, is a significant VBAC risk factor and can also be a
personal worry for many moms. Grider suggests patients use an online risk calculator to help gather data-driven answers to their questions.
“This useful tool provides specific numbers that can help women see potential risks in an objective way,” says Grider.
Plans typically help prepare patients for what to expect during trial of labor after cesarean (TOLAC). This acronym is a general term that describes a patient’s journey through pregnancy to VBAC.
One part of that journey may include the steps to take once labor begins. Although labor induction is not prohibited in VBACs, it may increase the risks of complications. One of the biggest predictors of VBAC success is spontaneous labor. For this reason, Women First takes a “cautionary stance” and does not aggressively induce labor in patients attempting a VBAC.
“We work with VBAC patients to select a day near their projected due date. If labor does not spontaneously begin by that point, we often recommend moving forward with a C-section,” says Grider.
By the time a patient arrives at labor and delivery, Women First makes sure she has:
• Discussed her birth plan in detail with her physicians, her partner or husband, and others who may be part of her delivery.
• Understood that changes in her birth plan—up to and including the need for a repeat C-section—may become necessary.
Plan changes are driven by the safety and well-being of mom and baby. Grider and her colleagues strive to make every woman’s birth
At
Compared
See our Maternity Care services at womenfirstlouisville.com. Or call 502.891.8700 for more information.
502.891.8700
womenfirstlouisville.com
experience reflect her plan, yet that is not always possible.
“Sometimes our expectations and the pictures we create in our minds can become a source of disappointment,” she says. “The reality is babies don’t always cooperate with anyone’s expectations.”
While Grider rarely has to act outside a patient’s wishes, she says being prepared for such a situation speaks to the importance of building trust. “It is my job to help a mom understand why her birth plan may not be the
safest for her or her baby.”
“I’ve never had a mom go against my medical advice in an emergency situation when I’ve had to make the call to change a VBAC birth plan,” says Grider.

In 2010, the NIH described VBAC as a “reasonable option” for many women. Updated practice guidelines released by ACOG echoed a similar conclusion.
One significant benefit of VBAC is a faster
recovery time compared to what is typical following a C-section.
Vaginal deliveries have lower rates of infection than C-section procedures. They typically carry less risk for bleeding and blood clots, and are also less likely to require blood transfusion or admission to an intensive care unit.
VBAC complications can happen, yet they are generally not life-threatening. The Centers for Disease Control and Prevention reported in 2018 that women who deliver vaginally after a previous cesarean are less likely to experience birth-related morbidity than women who have repeat cesareans.
These findings underscore the importance of lowering our nation’s high incidence of cesarean sections.
• A two-part goal from the Office of Disease Prevention and Health Promotion seeks to reduce cesarean births among low-risk women with no prior births and among low-risk women with a prior cesarean birth.

• A Healthy People 2020 goal strives to increase VBAC to 18.3% among women with a previous cesarean delivery.
Procedures like VBAC reflect Women First’s ongoing commitment to meet each woman’s health needs with highly personalized, innovative care. Innovation is nothing new for the practice, which was the Louisville area’s first allwoman-run obstetrics and gynecology office.
The practice currently includes 11 physicians board-certified in OB- GYN, eleven nurse practitioners and physician assistants, plus additional clinical and support members. Their services range from annual health exams and screenings to advanced contraception and pregnancy care, plus numerous specialized diagnostic and surgical procedures.
Grider and her partners believe there are always valid reasons to reassess past customs or practices and question whether there are better ways to work toward positive outcomes.
“There is no single right answer for every patient. Whether or not a patient decides on VBAC is dependent on her history, risk factors, and personal desires,” she says. “Our ultimate aims are, and should always be, to reduce risks and make deliveries as safe as possible for babies and moms.”
Women First, we help women champion their own birth experience with a Birthing Plan guide and personal options that include vaginal birth after cesarean section (VBAC).
 BY PAT HENDERSON
BY PAT HENDERSON
LOUISVILLE While it may be debated as to whether the “dream job” actually exists or is just a fantasy, Traci Edwards, MD, knows her job is pretty dreamy.
“I love what I do, and I never dread coming to work,” says Edwards, who is a family medicine physician at the UofL Health-Medical Center Southwest, just off the Dixie Highway. “I see new things every day, I dry tears every day, I see a lot of smiles every day, and it is such a rewarding career.”
Edwards grew up on Louisville’s West End before moving to the east side of town and attending Wagner High School. Following her undergraduate days at Western Kentucky University, she attended medical school at the University of Kentucky College of Medicine and then did her residency at St. Elizabeth’s Medical Center in Dayton, Ohio. She returned to her hometown in 1996, and set up shop as a family practitioner.
“I always wanted to go into medicine, from the time I was very small,” she says. “Once I was in medical school and did rotations in a variety of specialties, I liked family medicine because you get to see something different every day.”
Another sign that she was fated for family practice is the fact she and her husband’s first child was born during her final year of residency when she was serving as chief resident at St. Elizabeth’s.
“Having our first child wasn’t part of my family practice planning,” she notes with a
laugh, “but a family medicine doctor I worked with did deliver our son! Since being around family was important, we ended up coming back to Kentucky.”
Clearly being in family medicine requires doctors to have a vast body of knowledge. One moment they may be treating a broken wrist or swollen feet and the next kidney failure or heart palpitations.

“I think the belief that your primary care doctor treats low-complexity cases is a big myth,” Edwards says. “We actually see a variety of problems—I will see heart failure, cancer—and we often make those major diagnoses. That initial work is often done by a primary care provider.”
In a time when specializing is common, she offers a reminder about one very important aspect of being a family practitioner.
“Specialty practices seem to be more attrac-
PHOTOS BY CHRIS WITZKEtive to grads coming out,” she says. “If you are going into medicine for the income, primary care isn’t at the top of the scale, but I think it is at the top of the rewards scale.”
Family practice doctors must have a broadbased medical knowledge and be very flexible because of the nature of not knowing what is coming through the door each day, says Edwards.
The population around UofL Health-Medical Center Southwest is predominantly seniors and, as a result, Edwards’ patients have a range of conditions: diabetes, heart and lung disease, high blood pressure, obesity, and COPD.
In addition to working with those issues, Edwards recognizes other factors, such as finances, transportation, and culture, that can impact her clients’ treatment and care.
“I think, based on my background and coming from Louisville, I have more insight into the potential factors, often financial or cultural, that keep some people from getting healthcare,” she says. “I really try to get to understand them better as a person, which helps overcome some barriers.”
She cites rising medication costs and high deductibles as reasons why some patients won’t have certain procedures done. Another, more practical, problem is transportation, as many depend on a family member or friend to get them around.
“Some patients have trouble just getting in for an office visit,” says Edwards. “And, there
are a lot of specialists who aren’t in the south end of Louisville, and when we make a referral to a provider on the other end of town, patients might say, ‘I can’t get there, you just need to figure it out,’ and we try to. But that impacts care.”

Speaking of obstacles that impact care, COVID-19 was a big one. As the whole world came to a halt and there were restrictions, especially for the first few months, about in-person gatherings, doctors had to rethink the traditional office visit.
Enter telehealth.
“Telehealth wasn’t something that was really on my radar or that I thought I’d be interested in,” Edwards says. “All of a sudden, we had to become very knowledgeable on it, and I have found that I like it a lot.”
Since some of her patients have difficulties getting in the office, telehealth provides a way for them to stay connected. Positive outcomes include flexibility to schedule a consult on short notice, staying connected to their healthcare provider more regularly, and the visual
Dr. Edwards emphasizes the importance of lifestyle as a way to better health. Here are three of her thoughts on that topic:
1. “One lifestyle change I advocate to patients is rest. Rest is also important to your mental health, which has an impact on your physical health. You have to rest both your body and your mind.”
2. “With exercise, people may say they don’t have time. So, we have a conversation about how much time they spend on their cell phone or watching TV instead of going for a walk. Patients understand it in those terms.”
3. “When advocating for dietary changes, I need to be cognizant of what is available in their community. If they don’t have access to fresh fruits and vegetables, frozen fruits and vegetables are just fine, and that may fit what’s in the budget. I do stress fresh or frozen over canned for both.”
aspect—they are still “seeing” their doctor.
“They also seem to be more relaxed and comfortable at home; one even wanted to show me their garden!” quips Edwards.
While COVID isn’t over yet, physicians are seeing more patients in the office again. That is a good thing, but Edwards is quick to note that isn’t the only option for her moving forward.
“I do a mixture of telehealth and in-office visits, since there are still patients who don’t feel comfortable coming in and others who just can’t,” she says. “Through telehealth, we are more able to meet their needs, which is crucial. You may have to get a little crafty with telehealth, but it is obviously here to stay.”
Behind every good doctor is, well, a good patient. Edwards has worked with thousands of patients over the years, and the deep, long-standing relationships she’s developed have a positive impact regarding care.
“I believe that healthcare is a group project,” says Edwards. “I can’t be the only one worried about your diabetes; we both have to work on it, and you have to take some ownership of your care.”
One of her goals is to help fill what she calls “care gaps.” Good communication is key, from finding out if medications are working to making sure patients come in for follow-up visits and are doing what they need to in terms of preventative care.
“And now have a different platform to reach patients, telehealth, so we aren’t limited to just the office visit anymore,” she says. “We also have electronic health records, and we can get information so quickly and easily from other medical providers, which helps us make more informed decisions.”
Edwards has been a doctor long enough that she has seen multiple generations of families, a fact that she loves.
“I will have the grandparents, then the mother and father and their children, and then the grandchildren as patients,” she says. “It is very rewarding and very humbling, and I don’t take for granted that they choose to come to me. I like forming a bond with the people that I treat; they get to know me and I get to know them.”
And that simple fact makes Edwards’ job as a family practitioner pretty much her dream job.
LEXINGTON Pelvic pain and dysfunction are one of the most elusive conditions a woman can experience. In a culture preoccupied with pain management, Lexington’s Wellward Regenerative Medicine is giving hope that resolution can supplant management for those women. And this is a hope many women and their healthcare providers have been waiting for. Danesh Mazloomdoost, MD, “Doctor Danesh,” as he is known, is the founder of Wellward, an institution that integrates several fields to create that sense of hope. He says,
“The central element of the practice is the confluence of three overlapping realms: cellular and biological; kinesiology; and behavior, lifestyle, and psychology.” Together, in the hands of Mazloomdoost and his team, lasting solutions to pelvic pain are being produced.
As many as 1 in 6 women reportedly suffer from pelvic pain at some point in their lives. This is classified as persistent pain that adversely affects function including symptoms such as dyspareunia, paresthesia, stress incontinence, loss of libido, and anorgasmia, among others. While studies report prevalence as high as 30%, Mazloomdoost knows that this may still be an underrepresentation of functional impairment particularly among postpartum women since, “…it is an intimate concern that people often minimize as a normal part of aging.”
While its presence may be underacknowledged, the impact of pelvic pain and dysfunction are hard to dismiss: it changes lives. Pain drives behavior, and behavior determines who we are and how we act towards others. For Mazloomdoost, “Resolving pelvic dysfunction gives women back their old selves and allows them to live their lives fully again.”
He knows many PCPs and GYNs whose desire to help their patients
has been precluded by the complexity of pelvic pain, and he is excited to offer them hope.
While some pelvic afflictions have straightforward causes, pelvic pain often involves a combination of multiple organ systems, the autonomic nervous system, and the musculoskeletal system, not to mention psycho-emotional elements. As such, it can be daunting to confront, for both doctor and patient. Mazloomdoost says “Everybody shies away from pelvic pain — they just are not sure how to deal with it. There are very few resources for these patients — not to mention their physicians.”
Vague diagnoses often result, with interstitial cystitis, pelvic pain, vaginismus, and endometriosis among the most common, Mazloomdoost reports. These lack specific and reliable treatment pathways, leaving patients and their physicians who desire more that pain medication frustrated. In fact, he says “The didactics around it are really in their infancy.” Mazloomdoost sees a way forward and is developing his integrated practice to provide that.
Wellward has existed since 2014. It grew out of Mazloomdoost observation of his parents’ practices: his mother, Camellia Shirazi, MD, has a background in both anesthesiology and psychiatry, and his father, Manoocher Mazloomdoost, MD, (known as “Dr. Maz”), is a board-certified anesthesiologist and pain specialist. Influenced by both their training in Iran and their many years practicing in the U.S., his parents developed an integrative approach to pain treatment that Mazloomdoost considers progressive and dynamic. It has fueled his vision for Wellward, and he says, “The most potent innovation comes when you are bridging two environments.”
Wellward’s method of providing enduring relief for pelvic pain sufferers has emerged in

this context, with Mazloomdoost’s sister, a urogynecologist in Maryland, providing valuable input. Mazloomdoost says “I built the practice as a living laboratory of translational science. We want to pull it all together so that it is integrated in one location. Our treatment plans vary, as no two of our patients are alike.” There is, however, a consistent treatment philosophy across cases.

Mazloomdoost combines psychological, physiological, kinesiological, and pharmacological elements in a longitudinal approach. It begins with Pain Mapping™ a proprietary process to isolate specific elements (he calls this Hearing the pain message), includes psychological overviews (Envisioning the life being led), moves on to Alleviating symptoms (both medically and through therapy) and then Leverages repair mechanisms, which includes physical and regenerative therapies and addressing socio-behavioral issues. He


takes his patients through the HEAL process in depth over the course of several months, as each part has multiple elements and each patient has a unique pain profile.






He recently used the HEAL process to meet the needs of a menopausal homemaker who was experiencing a case of dyspareunia that was fraying her relationship with her husband. At a loss for a functional diagnosis, she blamed herself and questioned her commitment to her marriage, resulting in a downward spiral. First, pain mapping showed Mazloomdoost and his staff a small clitoral branch nerve that was entrapped. Then the psychological overview revealed detachment from her husband fueled by her own loss of purpose in her life, as her grown children had moved on. Ketamine treatment helped give her some perspective on herself to see and comprehend that a significant part of her inability to enjoy intimacy was due to this identity crisis.



Alleviation of symptoms in this patient came two ways. The nerve entrapment was


addressed non-surgically, and her newfound awareness facilitated more intimate conversations with her husband, which garnered his acceptance and support. She continues to come to Wellward for additional follow up consultation on nerve well-being and how to do the hard work of relationship management as she ages, but the trajectory of her libido and marriage are upward.
She is experiencing increased fullness in her life, and she tells Mazloomdoost that she feels empowered to further this.






For Mazloomdoost, the HEAL process can deliver women suffering from pelvic pain to an embrace of his belief that “It is easier to deal with a painful known than an unknown annoyance.” It’s rarely quick to resolve pelvic pain, but giving women an awareness that there are treatment options and that someone else validates their concern goes a long way. He concludes, “At Wellward, demystifying the body is one of the most therapeutic things that we do.”


VERSAILLES Meeting your clients and patients where they are has never been more applicable than at Frontier Nursing University (FNU), where over 80 years ago nurse-midwives rode horses to see expectant mothers and their families in the hills and hollows of Eastern Kentucky.
Today Frontier Nursing University has over 2,500 nurse-midwife, family nurse practitioner, women’s healthcare nurse practitioner, and psychiatric-mental health nurse practitioner master’s and doctoral nursing students enrolled from all 50 states and several foreign countries.
Underlying the concept that students who are educated in their communities are likely
to stay and serve those communities, FNU’s online and distance education allows its students to complete their graduate degrees using their home communities as the classroom. FNU students are already practicing registered nurses seeking to advance their careers into nurse-midwifery or nurse practitioner specialties. By staying at home, the new FNU graduates serve their communities in a rich mixture of cultural, economic, and geographic settings.
“We are relationship-based practitioners,” says FNU president Susan E. Stone, CNM, DNSc, FACNM, FAAN, who is also a certified nurse-midwife and graduate of Frontier School of Midwifery and Family Nursing, as it was once called, and spent 10 years practicing midwifery in upstate New
York before joining FNU. “We can address the needs of our clients because we have created a ‘culture of caring.’ Through our

conversations and multiple meetings with our clients we learn their challenges. Not just healthcare, but all aspects of health such as, ‘Is there enough food in the house? Will you be going back to work? What about child care and transportation?’”
Educating nurse-midwives and nurse practitioners about the importance of teaching their clients self-care is part of FNU’s core mission. “We train our students to teach clients how to stay healthy and what signs they need to watch out for,” says Stone.
For years FNU has emphasized training midwives and nurse practitioners who look like and understand their patients and clients. In 2006, 9% of the FNU student body identified as persons of color. In 2020, that diversity percentage is 28% and continues to increase every year, says Stone.
“Growth in nurse-midwifery throughout the U.S. may lead to a decrease in infant and maternal mortality in Black communities,” says Stone. “The rate of infant and maternal mortality in Black communities is three times higher than in white populations.1 Having more Black, Hispanic and Native American midwives in rural and underserved communities where access to healthcare is limited, has a positive impact,” she states.
1 https://www.kff.org/report-section/racial-disparities-inmaternal-and-infant-health-an-overview-issue-brief/
Stone is a leader in strategic development seeking to increase the quality and capacity of the nurse-midwifery and advanced practice nursing workforce, with the specific goal
of improving health care for families. During her last two decades as president of FNU, the university has grown from a community-based school of nurse-midwifery offering a basic certificate program with 200 students enrolled, to an accredited university offering master’s and doctoral degrees to nurses seeking graduate education as nurse-midwives and nurse practitioners.

Stone also served as the president of the American College of Nurse-Midwives (ACNM) from 2018-2020 where her agenda included increasing the midwifery workforce through educational quality and capacity strategies, midwifery advocacy focusing on the maternal mortality and morbidity crisis, and growing diversity in the healthcare workforce.
She was inducted into the National Academy of Medicine (NAM) Class of 2018 as one of only two nurses in her class. She believes collaboration with other healthcare professionals is essential to improve the health of women and families and fosters this approach in her various roles.


“Why do you keep going back if it’s making you feel worse?” my boyfriend asked.
We were talking about one of the most unsettling experiences of my young adult life — don’t laugh — psychotherapy.
No snowflake, I was surprised that my hands were often trembling as I drove home after sessions. Sometimes my chest was pounding, or I found myself crying.
I didn’t have an answer for my boyfriend (other than to yell, “I’m not a masochist!”). But it didn’t keep me from faithfully showing up for my appointment every other week.
Here’s what I know now:
1. It’s amazing how quickly our brain can change when it recognizes a bigger, better offer.
We’re wired for what feels good. Neuroscientists have located a specific area of the brain (nucleus accumbens) designed
to constantly compare rewards and instantly recalibrate us toward the most rewarding option. That nimbleness is necessary to adapt to changing conditions so we can survive and thrive.
The therapy sessions were obviously shaking me up. So why was I so drawn to an experience that was often disorienting and uncomfortable?
Well, a part of me liked being shaken to the core — was irresistibly drawn to it, even. But not like some inner adrenaline junkie. I didn’t enjoy the disorienting sense of discomfort and uncertainty. But on some level, I could sense the shakeup was serving a purpose — a chance to reshuffle the cards and give myself a shot at a better hand.
I didn’t have to force myself or will myself with a «no pain, no gain” mentality to show up for my counseling sessions. And I wasn’t delaying gratification in the quest for some future reward. The present-moment rewards of therapy were the driving force: Every week, l was listened to by someone fully present, emotionally engaged, and non-judgmental. That need for authentic human connection is another survival-inspired part of our human programming. And it was hugely rewarding.
The emotional risk-taking we do in therapy sets us up to “do” our relationships with others better. It gets easier to break out of old, less-functional behavior patterns and replace them with better ones. Like breaking up with my narcissistic boyfriend and trading up for a better type of guy.
But it did take me a while to dump the bad boyfriend. What I know now is that my brain was just doing what it’s supposed to do.
If humans are wired for what feels good, homeostasis might be at the top of the list. And what’s more stable than sameness or
more comforting than the familiar? Like recognizing a friend in a crowd of strangers or spotting a KFC in a foreign country, the known is a comforting balm compared to the unknown, particularly when we’re feeling a bit vulnerable.
The familiar is most seductive when we’re stressed. Right when we most need to pay attention closely and critically, the comfort of the familiar fakes us out. It lulls us into an autopilot mode that keeps us stuck in a toogood-to-rock-the-boat but too-bad-to-keep-it afloat holding pattern.
No wonder change is usually forced upon us and catches us off guard.
So how do we deal with the brain’s need for certainty while making the changes we need and want to make? How do you engineer a breakthrough instead of a breakdown? How do you manage to a dump bad boyfriend when you’re afraid to be alone, along with all the other unknowns that go with it?
3. Let it RAIN.
RAIN is an acronym for a mindfulness practice developed to help us tread into unfamiliar territory and not get overwhelmed. Neuroscientists call this thinking skill “opening the window of tolerance,” which expands your field of awareness to hold conflicting aspects of complex situations.

I think of RAIN as a way of exploring our feelings without freaking out and making change feel safe and doable.
Here’s a brief description of RAIN:
RECOGNIZE that an uncomfortable feeling is coming on.
ACCEPT and ALLOW the feeling to be there. Don’t try to avoid it or make it go away. Instead, catch the wave of sensation and ride the experience all the way to shore.
INVESTIGATE the feelings and sensations happening moment-to-moment, studying them carefully with a friendly curiosity.
NOTE and NURTURE: 1) NOTE: Use short words and simple phrases to note the body sensations coming and going moment by moment. 2) NURTURE: Based on the information you gather, explore ways to help yourself feel better right now.
4. How to adapt RAIN to a counseling session:
I think of friendly curiosity, a primary component of RAIN, as an antidote to criticism and judgment. Curiosity can neutralize an Inner Critic attack and make room for the second component, compassion, to move in and jumpstart some productive problem-solving.
In the abbreviated example below, notice how the combination of curiosity and compassion in RAIN can help us get unstuck and moving forward:
CLIENT I overate last night and I’m so upset with myself. Just when I think I’m doing well and on my way to getting this COVID weight off, I do something like this. I hate it.
THERAPIST What did it feel like in your body when you overate the last night?
CLIENT I felt bloated and overfull. I was miserable.
THERAPIST What’s it like to feel bloated and miserable like that?
CLIENT I get really upset with myself. I beat myself up and say, “You’ve got to do better!”
THERAPIST How do you feel right now, as you reflect on what happened?
CLIENT Appropriately sad.
THERAPIST Appropriately sad. What’s it like to feel “appropriately sad”?
CLIENT I noticed as I said that, there was a little bit of a softening around it.
THERAPIST So you’ve gathered some data. You’re aware of this appropriately sad feeling and how noting it also softened it a little bit. So based on what you’ve noted so far, how could you help yourself feel better right now?
CLIENT Well, I could be compassionate instead of critical. I already feel terrible about it. It won’t help me feel better to keep castigating myself. But I’m afraid if I give myself a pass, I’ll slack off and really get off track!
THERAPIST Yeah. What’s it like when you don’t give yourself a pass and keep the pressure on?
CLIENT I feel really down and worried the rest of the day. I’m starting to wonder if criticizing myself makes me feel terrible and may just set me up to overeat again.
THERAPIST How do you feel about experimenting? See what happens when you criticize yourself and when you comfort yourself and compare the results?
CLIENT Then I’ll know which way works better.

THERAPIST What can you do to comfort yourself when you feel upset like this? Something that would help you feel better right now, in this moment?
CLIENT I could get curious instead of critical. One thing that makes me feel better when I’m having an Inner Critic attack is to do some very gentle, relaxing yoga poses. I’ve found them to be very comforting.
Some important points about RAIN:
RAIN is not a technique to make yourself not do something. It’s a tool to make you more aware.
Whether you get yourself to not do something (procrastinate, smoke, drink, yell, overeat, etc.) isn’t as important as gathering data about what does happen, particularly on a feeling level.
The awareness component of RAIN, coupled with the compassion component, makes it possible to freely choose better behaviors without so much forcing and pushing. The effort of RAIN doesn’t exhaust us or wear us down.
RAIN is a deceptively powerful tool. I hope you look forward to hearing more about it from me and exploring it for yourself!

LOUISVILLE Mehyar Mehrizi, MD, received a bachelor’s degree in biology from the University of California, Berkeley, graduating with honors in neuroscience. He earned a medical degree from the University of Kentucky College of Medicine, where he was class president, and completed a residency in neurology at Indiana University School of Medicine.

Remaining at Indiana University, he completed a fellowship in clinical neurophysiology with an emphasis on epilepsy. His research has been published in peer-reviewed journals, including Neurology and Muscle and Nerve. “Medicine, for me, is the convergence of my love of science and people,” he says. “I
enjoy teaching my patients about their disease process and helping to improve their quality of life and health.”

His philosophy of care relies on mutual respect and developing a good relationship between the patient and physician, which is key to successful treatment of a neurological disorder.
Mehrizi grew up in Lexington, Kentucky, and attended Breckinridge Elementary School, Morton Middle School, and Henry Clay High School. He and his wife, Jane, have one daughter, Marcella. In his free time, he enjoys traveling, playing soccer, and spending time with family and friends.



LEXINGTON Lexington Clinic welcomes Hamza Tantoush, MD, to Lexington Clinic Rheumatology. Tantoush received his medical degree from the University of Tripoli in Libya. He completed his residency in internal medicine at Creighton University in Omaha, Nebraska, and a fellowship in rheumatology at the University of Kentucky.
Tantoush is board-certified in internal medicine and rheumatology He provides services in inflammatory rheumatic diseases such as rheumatoid arthritis, psoriatic arthritis, systemic lupus erythematosus, inflammatory
muscle diseases, Sjogren’s syndrome, scleroderma, vasculitis, mixed connective tissue disease, gout, pseudogout, enteropathic arthritis, systemic autoinflammatory disease, Sarcoid arthritis, osteoarthritis, and osteoporosis. Lexington Clinic was founded in 1920 and is Central Kentucky’s oldest and largest group practice. Lexington Clinic has more than 180 providers and serves more than 600,000 patients every year. Lexington Clinic has providers in 30 different specialties and has more than 25 locations throughout Central Kentucky.
the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth. Put our experience to work for
LONDON Bruce Lyman Allen, MD, has joined Saint Joseph London as a general surgeon. Born and raised in the Bay Area of California, Allen has spent the last 40 years practicing as a surgeon on the West Coast.

Although the move to Kentucky is happening late in his career, Allen says he’s looking forward to the transition and new opportunities.
“At this stage in my career, patients and col-
leagues frequently ask when I intend to retire,” says Allen. “Retire? I have the greatest job in the world. Why should I retire as long as I enjoy the work, and, more importantly, as long as the results of my surgery remain excellent?”
Allen earned his undergraduate degree from Harvard College and received his medical degree from Stanford University School of Medicine. After completing a general sur-
gery residency at the University of California San Francisco, he joined his father in the practice of general surgery in San Mateo, California.
Allen has been the surgeon champion for the National Surgical Quality Improvement Project at his community hospital. “The best way to improve the quality of our work is to measure the outcomes.”
Following that line of interest, he obtained a master’s degree in medical informatics from Northwestern University in Chicago. Allen is board certified by the American Board of Surgery and the National Board of Medical Examiners.
As a general surgeon, Allen enjoys sharing with his patients his knowledge about surgery, what results to expect and what recovery should be like. “The nice thing about my specialty is that we take care of common problems such as hernias and gallstones, as well as the more serious illnesses like diverticulitis or colorectal cancer,” says Allen. “Now because of imaging and equipment advances, coupled with the use of cameras and small incisions, we can do so much more with less disability after surgery. Our patients get better faster, so they don’t have to live with chronic conditions, and they return to their usual activities more quickly.”
Allen began looking for general surgery positions in Kentucky when his son was accepted to Stewart Home & School, a residential school in Frankfort that serves individuals with intellectual or developmental disabilities. Since making the cross-country move, Allen says he’s already enjoying working at Saint Joseph London.
“Today, more than ever, surgery is a team sport. The best results come from each of us doing his or her own job well. The team at Saint Joseph is excellent. It is a pleasure to work with them.”
When Allen is outside of the hospital, he enjoys spending time with his wife, Christina, their four children, and their rescue dogs. He also enjoys restoring old cars and working on his golf game.


LEXINGTON On May 26, 2021 CHI Saint Joseph Health announced an expansion of its affiliation with Cleveland Clinic Cancer Center to serve its patients across Kentucky. This affiliation will now extend to Flaget Memorial Hospital in Bardstown, Saint Joseph Mount Sterling and Saint Joseph London.
The affiliation will enhance the hospitals’ capabilities and provide patients in each of the service communities with a higher level of cancer care closer to home. The announcement follows the CHI Saint Joseph Health and Cleveland Clinic Cancer Center affiliation in Lexington that was launched in 2019.

“Our physicians will have easy access to second opinions and can easily connect with world-renowned experts and subspecialists on cases,” said John Yanes, president, Saint Joseph London. “Our patients won’t have to leave their home community to access this level of care.”
“This affiliation means that our patients in Montgomery County and in Bardstown and the surrounding counties will have access to second opinions and input to treatment plans from one of the nation’s most respected cancer programs,” said Jennifer Nolan, president, Saint Joseph Mount Sterling and Flaget Memorial.

Beyond direct patient care, Lexington’s cancer care centers have leveraged this relationship to make programmatic and clinical improvements, like adding a HOPE line call center for new patients and streamlining second opinion requests. Starting next week, the HOPE line –844.940.4673 (HOPE) – will also be used for scheduling cancer screening appointments in an effort to provide easier access to preventative measures.
“Cleveland Clinic Cancer Center is thrilled to be working with CHI Saint Joseph Health because of our shared values and priority for clinical excellence,” said Hetty Carraway, MD, Department of Hematology & Medical Oncology, Cleveland Clinic Cancer Center. “CHI Saint Joseph Health has been incredibly engaged and dedicated to a multidisciplinary team-based approach to patient care.
Our DSN TEAM is even stronger, thanks to the addition of Michael Reich, Financial Planning Specialist

LEXINGTON Lexington Clinic marked a milestone on May 15 with a ribbon-cutting ceremony to celebrate the completion of its newest facility on South Broadway, which opened its doors to patients about a month ago. Attendees included Lexington Clinic leadership, representatives from the board of directors, Mayor Linda Gorton, representatives from Brett Construction and Commerce Lexington, and current and retired physicians of Lexington Clinic.
The new Lexington Clinic facility is an investment of over $30 million, and the final square footage is just over 116,000 sq. feet. All areas of the new facility are designed for a patient-friendly care experience, with large waiting areas and exam rooms, comfortable furnishings, and ample natural light.
“This new state-of-the-art facility is much more than a building. It is a testament to our vision of perfecting the patient experience, not just today, but decades into the future,” said Andrew Henderson, MD, Lexington
Clinic CEO. “I’m grateful to everyone who believed in the vision for this facility and worked so hard to make it a reality.”
Located at 1221 South Broadway, the new facility provides the region’s residents access to multiple healthcare specialties and services in a centralized location.
The new facility houses the following specialties: audiology/ENT; cardiology; center

for breast care; dermatology; endocrinology; general surgery; gynecology; internal medicine; neurology; pain medicine; phlebotomy; radiology; rheumatology and urology.
“We now have a state-of-the-art facility to match our world class providers and staff,” said Michael Cecil, MD, president of the board of directors. He added, “Our board would like to thank everyone involved for their hard work and persistence through many challenges, including the pandemic.”
Lexington Clinic was founded in 1920 and is Central Kentucky’s oldest and largest group practice with more than 180 providers. It serves more than 600,000 patients every year. Lexington Clinic has providers in 30 different specialties and has more than 25 locations throughout Central Kentucky.

LEXINGTON Kraig Humbaugh, MD, MPH, Lexington-Fayette County commissioner of health, was presented the Jack Trevey Award for Community Service by James Borders, MD, Lexington Medical Society president, on May 11, 2021. This award is the society’s highest honor and is not presented every year but only when a worthy recipient is selected. Borders continued, “Dr. Kraig Humbaugh calmly guided our community through the COVID-19 pandemic from the first indication of the virus to the vaccination efforts. His leadership represents the best in the practice of medicine and an inspiration to us all.”

The Lexington Medical Society (LMS) is a nonprofit professional association of physicians in Fayette County, Kentucky. LMS is a voluntary organization founded in 1799. It is one of the oldest medical
societies in the country. It is a component of the Kentucky Medical Association which, together with other state medical societies, forms the American Medical Association.
Through its elected officers, committees, and full-time staff, LMS seeks to serve as the principal voice and resource for Central Kentucky physicians to enhance their professional lives and improve the health of the community. LMS provides a forum for the interchange of ideas and information. Each year LMS members contribute many hours to help guide the development of medical practice and to nurture awareness of medicine’s importance to the community.
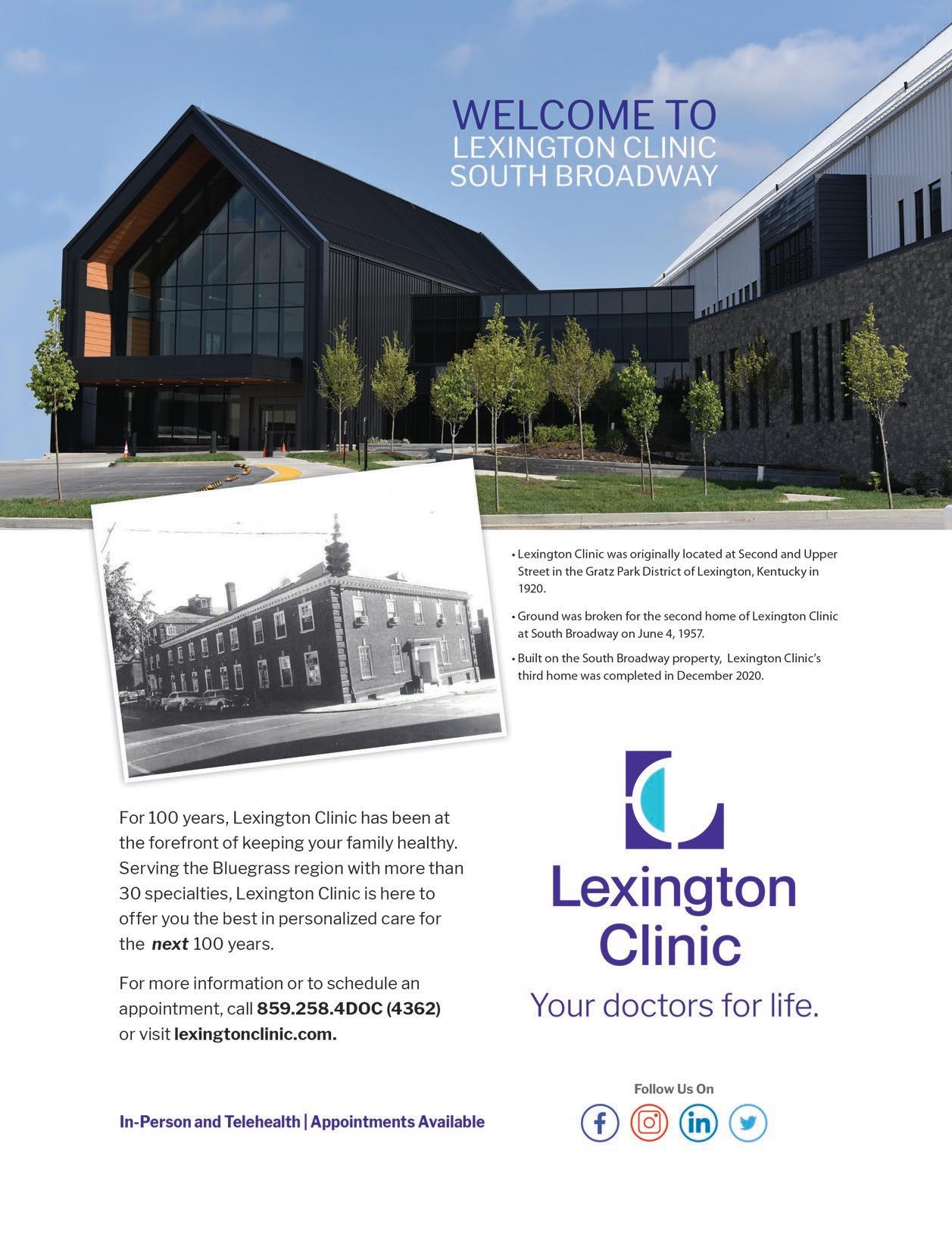
Shriners Hospitals for Children Medical Center
Corporate Council Members present:
August 21, 2021

Keeneland Entertainment Center
6:00pm - Midnight Cocktail Attire
Emcee Bill Meck
Elegant Sit-down Dinner
Live & Silent Auctions

Music & Dancing to The Sensations
Tickets & Info: (859) 268-5770
Proceeds benefit Shriners Hospitals for Children Medical Center - Lexington