














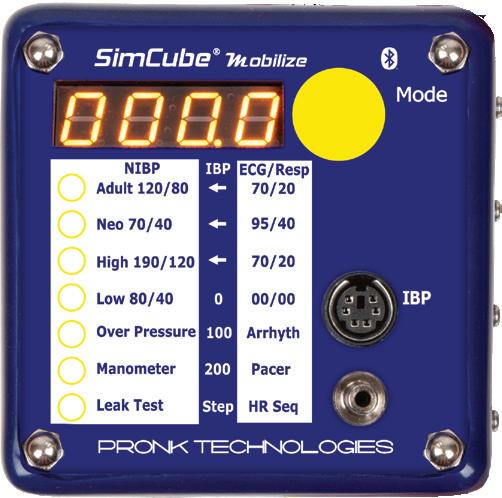












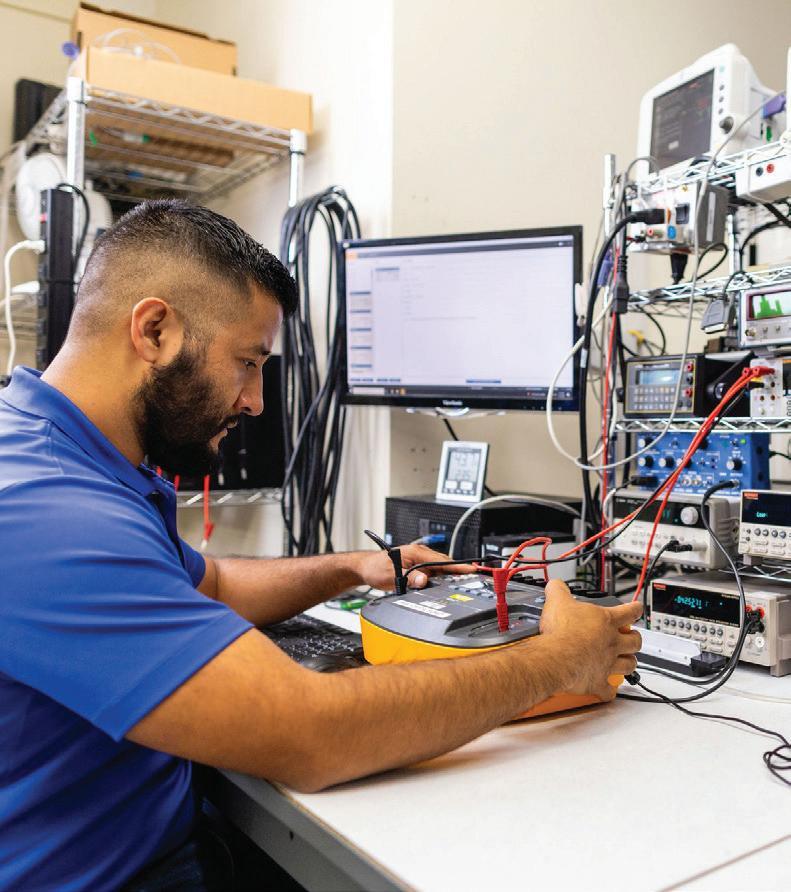


































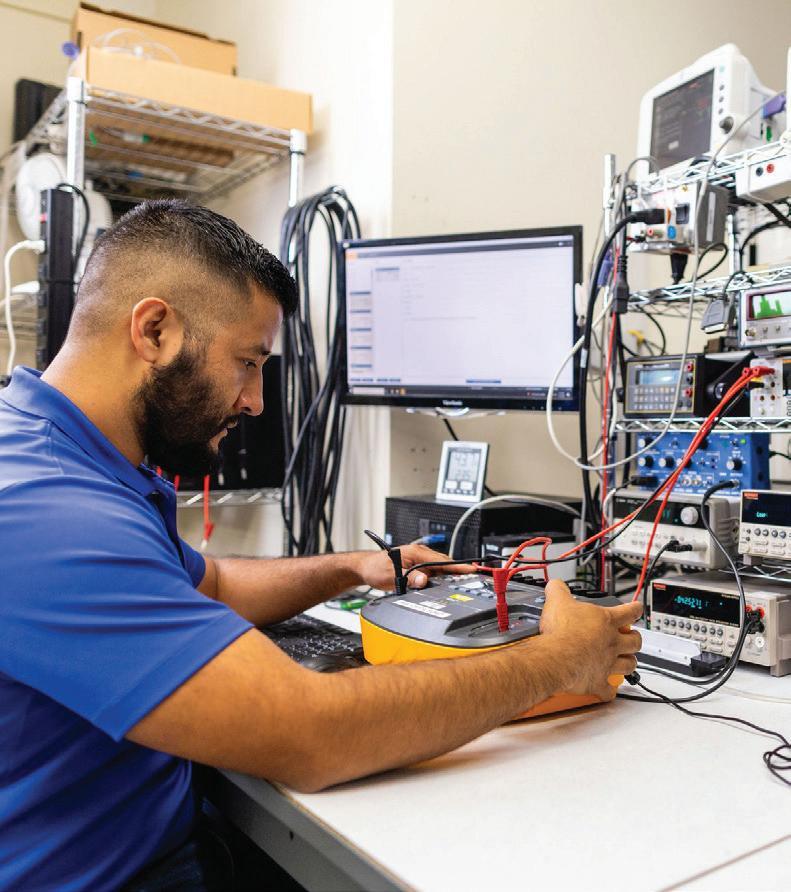


Our test equipment calibration service will:
• Eliminate shipping costs and damage
• Reduce downtime from weeks to hours
• Increase productivity
Our calibration management software will:
• Allow us to identify and notify you when your equipment is due for calibration
• Provide an online history of calibration and repair services performed on your test equipment









Let's meet at booth 203 at the Imaging Conference and Expo Feb. 20 - 22


P.12 SPOTLIGHT
p.12 Professional of the Month: Chris Shores
p.14 Department of the Month: The Emplify Health Biomedical and HTM Department
p.16 Next Gen: Kierra Morrow
p.18 Association of the Month: Michigan Society For Clinical Engineering (MSCE)
INDUSTRY UPDATES
p.20 News & Notes
p.25 TechNation Pulse
p.27 Ribbon Cutting: FDM Enterprises
p.30 AAMI Update
p.32 ECRI Update

p.34 Dental Update Revolutionizing the Way We Manage Devices
P.36 THE BENCH
p.36 Biomed 101
p.38 Webinar Wednesday
p.39 Tools of the Trade
P.42 FEATURE ARTICLES
p.42 Roundtable: RTLS
p.50 CORPORATE PROFILE: USOC
p.54 Cover Story: AI & HTM Revolutionizing the Way We Manage Devices

P.60 EXPERT ADVICE
p.60 The Future
p.62 MedWrench Guru
p.64 The Massey Method
p.66 Networking Notes
p.68 Cybersecurity
p.70 Right to Repair
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
VICE PRESIDENT Jayme McKelvey BUSINESS DEVELOPMENT
EDITORIAL John Wallace
CONTRIBUTORS
K. Richard Douglas
Joie Marhefka
Steven J. Yelton
Garrett Seeley
Nathan Proctor
Carol Davis-Smith
Eric Massey
Gay Gordon-Byrne
Dave Francoeur
Andrew Whyte
James Linton
Christopher Walters
ACCOUNT Megan Cabot
EXECUTIVE
ART DEPARTMENT Karlee Gower
Taylor Hayes
Alicia Brown
DIGITAL SERVICES Cindy Galindo
Kennedy Krieg
Haley Harris
EVENTS Kristin Leavoy
Sydney Krieg
WEBINARS Linda Hasluem
HTMJOBS.COM Sydney Krieg
ACCOUNTING Diane Costea
CIRCULATION Joanna Manjarrez
Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC
Nadia ElKaissi, CHTM, Biomedical Engineer, HTM, VA Central Office (19HTM)
Bryant Hawkins Sr., Site Manager, Children’s Hospital of New Orleans
Earl Morris Jr., BMET, Director of Clinical Engineering, Harrison County Hospital
Leticia Reynolds, Clinical Engineering Operations Manager at UCHealth Parkview Medical Center

p.72 Word Search
p.72 [Contest] What’s on Your Bench?
p.73 Biomed Brainbuster
p.74 FBS Scrapbook
p.76 HTMA-NTX Scrapbook
p.79 The Social
p.80 Service Index
p.83 Alphabetical Index
p.84 Preferred Vendors



College of Biomedical Equipment Technology, we are setting standard for excellence in HTM.
Our nationally recognized programs include Biomedical Equipment Technology (BMET), Biomedical Equipment Support Specialist (BESS), and the Dental Repair Technician (DRT) Certificate. Each is designed to equip you with the advanced skills needed to thrive in today’s evolving healthcare and dental technology landscape.
nationally recognized programs include Equipment Technology (BMET), Equipment Support Specialist (BESS), Dental Repair Technician (DRT) Each is designed to equip you with the skills needed to thrive in today’s healthcare and dental technology Courses



Networking
Infection Control*


BY K. RICHARD DOUGLAS
More than 20 years ago, mission trips to two developing countries sparked an interest in HTM for one biomed.
“When I was in my 20s, I used to go on mission trips all over the world, remembers Chris Shores, a clinical engineering tech II in the Department of Clinical Engineering at Fairview Hospital in Cleveland, Ohio. Fairview Hospital is a part of the Cleveland Clinic system. Back in 2004, we went to a small village not far from Guatemala City. They [had]

year and that sparked my curiosity. As time moves on, electronics or power when In 2006, I went to Ghana.
countries, but who repairs them? He told me they don’t have too many people, if any, to work on them. He shared that they need help in those regards.”
Shores went on to get his formal training to enter HTM and transition from his former occupation.
“In 2013, I received my degree in electrical engineering technology. Before that, I was a state tested nursing assistant for 15 years at a nursing home and a patient care nursing assistant for three years at Cleveland Clinic Hospital,” he says.
Since entering HTM, Shores has been advancing with a goal to continue to reach new heights.
“I started as a tech I and now I’m a tech II. I’m currently trying to be the next work leader for the West Region of Cleveland Clinic,” he says.
Shores says that he has a focus on dialysis as an area of specialty.
“I’m the only one in the West Region Cleveland Clinic who works on dialysis. I take care of echo, EKG, lab, pharmacy, multi-specialty, neurology, cardiac rehab and cancer departments (radiation oncology, hematology oncology, breast health, breast surgical, chemo infusion suite),” he says.
malfunctions?’ I know donated medical equipment from other
Many biomeds had their mettle tested during the COVID-19 pandemic when circumstances required resourceful thinking, out-of-the box ideas and stamina. Shores was involved in preparation and overflow management during this period.
“During the pandemic, I played a key role in ensuring our hospital was ready for patient surges. This included overflow planning: coordinated setup of additional patient care spaces to handle increased volume, monitor preparation: I configured and deployed extra patient monitors on mobile stands for rapid deployment in overflow areas,” he says.
He was also involved with IV pole procurement in which he ordered and distributed additional IV poles to support expanded treatment zones and equipment readiness where he ensured all devices were tested, calibrated and ready for immediate use in critical care environments.
Beyond pandemic-related projects, Shores has kept busy with other projects.
“I was involved in the shadow box project, Philips telemetry upgrades, new dialysis department relocation and expansion. I was involved in relocation of the clinical engineering supply room as well as Environmental Services’ storge relocation. Philips monitoring upgrades in OR, dialysis, and ICU. In charge of leading the West Region monthly Leader Guided Discussion (Avon Hospital, Lutheran Hospital and Fairview Hospital). I oversaw the phone upgrades for our department,” he says.
The shadow box project involved walk-throughs across the hospital and placement of shadow boxes which shows patient room and vital signs without breaking HIPPA.
“[I was] involved with Philips with what’s needed for the monitors. Making sure they all function properly and educating the rest of the clinical engineering team on purpose and repair. Worked with other third-party vendors on installation,” Shores says.
Away from work, Shores is most comfortable with a pair of drumsticks in his hands.
“I’m a percussionist! I teach two drum lines, I give private drum lessons and I drum at church. The first drum line I co-coach with my older brother, Ivan. The organization is called ‘The Deputies Club.’ It’s a baton and drum corps. This organization has been around for 44 years. We’ve performed in multiple countries, Cavs NBA games, parades, churches, Walt Disney, etcetera,” he says.
Shore met his wife, Rachel, in high school.
“She was in the KACP drum line with me back in the ’90s. We were reacquainted back in 2019. She’s a nursing supervisor for a rival hospital. She has two daughters and I have two sons. Her girls are 19 and 16 and my sons are 18 and 16. We raised our kids to be drummers; go figure. We have a three-year-old dog named Pearl,” Shores says.
He says that he loves working as a biomed. His mother was a nurse in a hospital, and Shores spent a lot of time around the hospital environment growing up. He actively tries to introduce the profession to young people.
“Hard work pays off and I’m still pushing forward to be an example for my children and anybody else who wants to pursue a career in saving lives through technology. I currently bring in high school students to see what I do and encourage the youth at the different drum lines I teach,” Shores says.
He has been a biomed for nine years, in healthcare for decades and has been drumming since he was seven. Shores has been an example of why practice and experience pay dividends with perseverance and focus.
FAVORITE BOOK: Holy Bible
FAVORITE MOVIE:
“War of the Worlds” with Tom Cruise
FAVORITE FOOD:
Seafood boil
HIDDEN TALENT: Empathy
FAVORITE PART OF BEING A BIOMED?
Saving lives through technology and bringing smiles to clinicians’ faces.
WHY DO YOU READ TECHNATION?
Informative and encouraging


BY K. RICHARD DOUGLAS
As the nation’s top producer of cheese and milk, Wisconsin rightly owns the moniker “The Dairy State” and has capitalized upon that fact for years. While the term “cheesehead” is commonly known, the historical fact that the ice cream sundae was born in the state is less well known.
A major healthcare provider, with headquarters that span Wisconsin from east to west, is Emplify Health.
With 729 licensed beds, Emplify Health is a major provider of healthcare services. The medical device inventory of such a large provider requires an equally robust HTM department.
Headed by Enterprise Director Melissa Wilke, CBET, BSHA, ITDS, the Emplify Health Biomedical and HTM Department has a total of 43 team members. There are three supervisors. Supervisors Josh Bachim and Darren Budde are positioned in La Crosse. Supervisor Jessica Paul is positioned in Green Bay. Jason Young is the enterprise manager.
“Emplify Health is a not-for-profit, patient-centered, community-focused healthcare network with headquarters in Green Bay and La Crosse, Wisconsin. Formed by a merger between Bellin Health and Gundersen Health System, Emplify Health has nearly 16,000 employees, including more than 1,400 clinicians, in 11 hospitals and more than 100 clinic locations in Wisconsin, Minnesota, Upper Michigan and Iowa,” Wilke says.
She says that with community partners, Emplify Health strives to lead – with love – a local, regional and national healthcare transformation to inspire people’s best lives at every stage.
“Biomed team members are assigned to specific departments, equipment or applications. OEM training is provided for team members to adequately and efficiently support both equipment and departments. Some areas of specialty support include linear accelerators, dialysis, nuclear medicine, anesthesia, NICU, respiratory therapy and mammography. Additionally, Emplify Health Biomed has several technicians that support rural critical access hospitals. This makes each of them especially unique as their strength is adaptability and flexibility to support a multitude of departments and equipment,” Wilke says.
She says that the biomed department has been working for the past several years to align service contracts under the
biomed accounting unit. This ownership of service contracts brings responsibility and opportunity. The advantage of centralizing contract ownership is the ability to create a standard workflow.
“It is crucial to involve team members as it leverages their expertise in service and support of equipment to identify the actual needs without any fluff,” Wilke says.
The convergence of HTM and IT integration operations happen under the CIO.
“As new equipment is evaluated and inventoried, collaboration with IT ensures that all devices meet rigorous security standards and are seamlessly integrated into the existing network infrastructure,” Wilke says.
New construction and facility update projects can often mean additional challenges for biomed departments. Extra care is demanded to provide quality healthcare to the tiniest of patients.
“One of the most transformative projects the team has supported is the development of the Emplify Health Family Integrated Neonatal Intensive Care Unit (NICU) in Green Bay, Wisconsin, which opened in 2022. This unit introduced ‘couplet care,’ which is a model that allows mothers and their newborns, who require intensive care, to stay together in the same room. Emplify Health is the first hospital in Wisconsin to offer this approach,” Paul says.
She says that from the beginning, the biomed team was deeply involved in the planning and implementation of this innovative care model. The team ensured that each room could safely support maternal and neonatal intensive care needs, integrating advanced monitoring systems, neonatal ventilators, maternal care equipment and secure data connectivity – all within a single, family-centered space.
“Currently, the team is proud to be supporting the next phase of this journey: transitioning from a Level II to a Level III NICU designation. This upgrade involves expanding clinical capabilities, increasing equipment complexity, and ensuring readiness for higher-acuity neonatal cases. Biomed is actively working on equipment evaluations and compliance with regulatory standards to meet the rigorous requirements of Level III care,” Paul adds.
She says that this transition has also created exciting opportunities for professional growth. The biomed team has been training in a range of new technologies, including the


Giraffe Shuttle, which allows seamless transitions between rooms without interrupting patient care. The team is also preparing for neonatal transport with integrated systems –including an incubator, gas blender, ventilator, suction and vitals monitor – and scheduling training on new oscillators to support advanced respiratory care.
“ It’s been a rewarding experience for biomed, knowing that their work directly contributes to seamless, high-quality care during a vulnerable time for families. This project exemplifies how biomed professionals not only support clinical excellence but also help create environments where healing and connection can thrive,” Paul says.
The HTM team has also demonstrated its problem-solving skills in conjunction with its IT colleagues and a vendor.
“ When one of the hemodynamic monitoring systems began crashing, it became an ‘all-hands-on-deck’ situation between biomed, IT and the vendor. Biomed provided in-room support, initially assisting the cath lab team in navigating the errors and completing the current case. We then began troubleshooting the problem and calling in other IT teams,” Bachim says.
H e says that it became apparent that a network security issue was corrupting the system and ultimately required the hard drive to be replaced.

“ Biomed worked with the vendor to get a replacement hard drive shipped overnight. After installation, biomed partnered with the IT network security team to ensure the system was correctly assigned to the appropriate organizational unit (OU) and configured with the correct security permissions,” Bachim adds.
H e says that after sitting through several days of patient cases actively monitoring the system, the team was confident the issue was resolved.
Away from the work setting, team members remain active in the HTM community.
“ The Emplify Health Biomed and HTM Department is an active participant in the Wisconsin Biomedical Association (WBA). There are several team members who currently serve on the WBA Board of Directors. This includes Darren Budde and Ladd Dafoe. I serve as the treasurer. Outside of attending annual WBA conferences held across the state of Wisconsin, attending HTM Mixers in Milwaukee have been highlighted events. The team always enjoys these incredible events in their own backyard,” Wilke says.
In The Dairy State, the HTM professionals at Emplify Health are making a difference in the lives of patients and supporting clinical colleagues.

Lead Biomedical Equipment Technician
Kierra Morrow grew up in Buffalo, New York, full of wonder regarding the world around her with an early interest in science and how things work. Her curious nature continues to thrive as an adult working at Buffalo General Hospital where a colleague nominated her as a member of the Next Gen of HTM.
TechNation discovered more about this rising star in a recent Q&A
Q: WHERE DID YOU GROW UP?
A: Born and raised in Buffalo, N.Y., I grew up with a strong interest in the world around me, fascinated by how things functioned and how science might help others. That early desire for exploration affected the direction I take today.
Q: WHERE DID YOU RECEIVE YOUR HTM TRAINING/ EDUCATION?
A: I began my journey with a degree in biotechnology, graduating in 2022. That foundation opened the door to the world of healthcare technology management, where I further developed my skills and earned my CABT certification through AAMI.
Q: How did you first discover HTM?
A: I originally learned about healthcare technology management while looking for a job that would combine my passion for science with a practical, significant influence. Clinical engineering quickly captivated my heart. It provided an ideal blend of technology, innovation and patientcentered treatment.
Q: WHY DID YOU CHOOSE TO GET INTO THIS FIELD?
A: I chose HTM because I wanted a career where my work would truly matter. Where I could help bridge the gap between life-saving technology and the patients who depend on it. Every device I touch, every system I support,

is part of a greater mission to improve and save lives. That’s what drives me every day.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: What I love most about my role is the opportunity to lead, teach and grow – not just within myself, but within my team. Mentoring new technicians and seeing their confidence bloom reminds me why leadership in this field is so powerful. We aren’t just fixing equipment; we’re building the future of healthcare technology.
Q: WHAT INTERESTS YOU THE MOST ABOUT HTM?
A: What draws me most to HTM is the way it constantly evolves. Technology never stands still and neither do we.

I love the challenge of staying ahead, learning new systems and finding innovative solutions that directly enhance patient care.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: One of my proudest moments was earning my CABT certification and being promoted to lead technician. Stepping into a leadership role, where I guide and support BMET technicians, felt like a true turning point. It is proof that hard work, passion and perseverance can create real change.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: In the next five years, I see myself advancing further into leadership, taking on greater challenges and continuing to mentor the next wave of HTM professionals. I also plan to pursue additional certifications, broaden my technical expertise, and help shape the future of healthcare technology through innovation and education.
FAVORITE HOBBY:
When I’m not working with cutting-edge medical technology, I’m deeply immersed in the world of herbalism. I’m currently working towards creating my own apothecary, blending my love for science and natural healing to make a positive impact in new and meaningful ways.
FAVORITE SHOW OR MOVIE:
“The Office”
FAVORITE MEAL: Green curry
WHAT WOULD YOUR SUPERPOWER BE?
Reality warping – the ability to transform ideas and dreams into reality
1 THING ON YOUR BUCKET LIST?
To study in a monastery for six months
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU:
I initially pursued my education with the goal of becoming a dentist.


BY K. RICHARD DOUGLAS
The state of Michigan covers a lot of ground from its southern border with Ohio and Indiana to Traverse City in the northwestern portion of the lower peninsula and to Copper Harbor in the far northern portion of the upper peninsula. Surrounded by the Great Lakes, the state is a mecca for boaters, fishermen, hunters and more.
The state is also home to the Michigan Society for Clinical Engineering (MSCE), the statewide biomed organization that unites the state’s HTM professionals.
The group’s mission is to promote professional development, advance the development of excellence in patient care in hospitals and related healthcare facilities and to provide a forum for the exchange of information among the members and organizations.
Officers in MSCE include President Eric Ebejer, Vice President Jahan Azizi, Secretary Jason Walewski and Treasurer John Crissman. Members of MSCE Board of Directors include Jay W. Hall, M.S., P.E.; Kyle Farrell; Thomas
Brown and Bill Fox. Lindsey Peterson serves as the MSCE webmaster.
The society has a long history going back to 1977. The same year that “Star Wars” hit theaters an initial focus group meeting was held in Lansing, Michigan, at the Michigan Hospital Association. It was at that meeting that a steering committee was established to consider how best to interact.
The steering committee had its first meeting two months later. By January of 1978, the core group had developed the new organization’s bylaws and structure. Those bylaws were approved in September of 1978. It was decided at that meeting that members of the newly formed organization should hold a degree in engineering or the life or physical sciences and work in healthcare. The bylaws were later amended to allow anyone actively employed in the field to become a member.
In 1982, incorporation papers were submitted to the state of Michigan and the society was officially recognized as a nonprofit society.
The new group’s first officers included President Tom Bauld, Vice President Chuck Jones and Secretary Dale Petty. One of the original board members – Jay Hall – remains an active board member today. While he is retired from the industry, he still has an active and welcome voice in the MSCE.
The society continued to develop and gain membership
throughout the coming decades. In July of 1999, MSCE launched a new website designed by George Award.
While education is one element of the organization’s focus, Ebejer says that its goals are multifaceted.
“While our meetings are educational in format, the purpose of the MSCE is to promote the professional development of the membership, advance the development of excellence in patient care in hospitals and related healthcare facilities and provide a forum for the exchange of information amongst the members and with other organizations. With many boomers soon to retire in the HTM community, there are strong undertones of the MSCE trying to place graduates in these positions,” he says.
Ebejer adds that at every meeting MSCE takes time to announce any new job openings and provides information from the employers as to where someone can apply.
Those meetings include eight to 10 monthly meetings annually, February through November. MSCE also hosts an annual golf outing in July.
As Ebejer mentioned, MSCE is active in helping to replenish the ranks of HTM in the state and has partnered with some local biomed college programs, both in Michigan and in nearby Canada.
“The MSCE has been working closely with Schoolcraft College in Livonia, Michigan for years and even one of our current board members –Secretary Jason Waleski – is an instructor/teacher at the school,” he says.
Ebejer also says that MSCE has built a strong relationship with James Linton and the BME program at St. Clair College in Windsor, Canada, over the past year.
“Many of their students attend our meetings since they’re right across the border from Detroit, Michigan in hopes that they could also find employment here in Michigan and the U.S.,” Ebejer adds.
Many biomed organizations were impacted by the pandemic. Those restrictions caused MSCE to shift gears to continue operations.
“The pandemic halted any/all MSCE meetings but has allowed us to more easily hold meetings remotely or have presenters present from a remote location,” Ebejer says.


While MSCE does not hold an annual conference, it does host a fun event each summer that has become a tradition.
“The closest thing the MSCE has to an annual conference/symposium is our annual golf outing which invites any/all HTM professionals, vendors, suppliers and MSCE board members that want to get together in a casual setting on the golf course which has been taking place for at least 20 years. I’m looking into organizing an annual conference/symposium (ETA 2027) as I know the HTM community in Michigan could and would support it,” Ebejer says.
He says that the group’s attendance declined in recent years because of the COVID pandemic, but it is growing again.
“I’m currently in the process of lining up manufacturers, suppliers, service providers, etcetera, for next year’s MSCE monthly meetings. The annual golf outing will be held, as usual, in July,” Ebejer says.
In the Great Lakes state, the state’s biomeds have plenty of recreational activities, but they also can stay plugged into the profession through MSCE.

Repair.org recently announced that Binseng Wang, recently retired from Sodexo, has agreed to join its board of directors.
“Binseng will not be bored as we push state legislation in support of the right to repair for medical equipment,” The Repair Association Executive Director Gay GordonByrne wrote in an email announcing the appointment. “His first task will be to help us answer questions in Vermont where H.160 is underway. More state legislators are seeing the need for better access for repair materials which are necessary to keep medical equipment up and running.”
“Please join us in welcoming Binseng to the Right to Repair team,” she added.
The IAM Union (International Association of Machinists and Aerospace Workers) is calling on Philips Healthcare to reach a fair first contract with 17 field service engineers (FSEs) in San Diego who voted to join the IAM, according to a news release. These highly trained engineers are responsible for maintaining and repairing hospital imaging and diagnostic systems across San Diego and the Inland Empire, the release adds. This equipment is critical to patient care and lifesaving diagnoses.
“The bargaining committee has been in negotiations since January 2025. Philips continues to resist negotiating in good faith to help IAM members establish industry-standard wage structures, safety protections, and training commitments for maintaining the operation of CT, MRI, X-ray, ultrasound and other diagnostic systems at hospitals and clinics throughout the region,” the release posted on the IAM Union website states.
Workers are seeking “fair pay” that reflects the advanced skills required to service various types of imaging equipment, as well as improved compensation for overnight and emergency calls. They also want paid training, stronger safety protections, predictable schedules and fair reimbursement for the travel their jobs require.
“These improvements will help prevent burnout and support the essential work field service engineers do to keep hospital imaging systems running safely for patients,” the release reads. “IAM leaders warn that delays at the negotiating table are creating unnecessary tension and instability in a workforce


essential to the region’s medical infrastructure.”
“These engineers are the invisible backbone of our healthcare system,” said IAM Union Western Territory General Vice President Robert “Bobby” Martinez. “Without them, hospitals cannot diagnose strokes, detect cancers or deliver timely emergency care. Philips must recognize their skill, respect their critical role and negotiate a contract that protects both workers and patients.”
The IAM will continue to amplify this issue and organize actions to raise awareness about the delay in receiving a first contract after nearly a year of negotiations.
“Philips has the opportunity right now to be a leader in patient safety, worker retention and healthcare quality,” said IAM Union District 725 Assistant Directing Business Representative Justin Mauldin. “We are urging the company to come to the table with real solutions so these workers can continue performing their life-saving roles without being stretched thin.”
The IAM Union is one of North America’s largest and most diverse industrial trade unions, representing approximately 600,000 active and retired members in the aerospace, defense, airlines, shipbuilding, railroad, transit, healthcare, automotive and other industries across the United States and Canada, according to the news release.

LANDSTUHL, Germany | A team from Landstuhl Regional Medical Center (LRMC) once again demonstrated its exceptional skill and readiness, securing a top position in the demanding Europe Best Medic Competition. The brutal, multi-day event, held Dec. 9-12 in the Rhineland-Palatinate training areas, is a stark simulation of battlefield conditions designed to identify the most resilient, technically proficient, and mentally tough medics in Europe.
For many, the event is also a tribute.
Sgt. Alredo Martinez, a biomedical equipment technician at LRMC, noted the competition is dedicated to Cpl. Wilson, a combat medic who saved soldiers’ lives even while injured.
“This competition assesses your physical and medical knowledge, along with your ability to collaborate with a partner,” said Martinez. “I am not a medic; I am an equipment operator. By participating in this competition, I have learned basic medicine and how to save lives.”
The annual competition pushes military medical personnel to their absolute limits.
The LRMC competitors faced a grueling sequence of events from the start. The first day began with a combat water survival event, immediately followed by the Expert Physical Fitness Assessment. With little time to recover, participants then zeroed their M4 weapons before their medical knowledge was challenged with a comprehensive written exam. The day concluded with a demanding land navigation course and the task of establishing a battalion aid station, requiring quick thinking and flawless execution under fatigue.
Day two tested the medics’ composure with a stress shoot, followed by a resupply mission and tactical lanes. The
challenges continued with late-night land navigation that stretched into the early hours of the third day. Afterward, the weary participants donned 35- to 45-pound rucksacks for an unknown-distance foot march. The final day’s trials concluded with a critical test of their skills in chemical, biological, radiological, and nuclear (CBRN) operations, a vital component of modern military readiness.
The event, which began in Grafenwoehr in December 2023, is a key measure of medical readiness across Europe.
“Competitions like this are beneficial for the Army because they are a way to assess soldiers’ capabilities, and they are not part of our daily routine,” said 1st Lt. Donovan Hinton, a medical officer with the 2nd Cavalry Regiment and the 2025 EBMC winner.
The impressive performance by the LRMC team is a direct reflection of the high standards of training and dedication at the medical center. These competitions are more than just a contest; they are a critical tool for building courage, fostering professionalism and ensuring that every medic is prepared for the unpredictable nature of combat. As one leader remarked, “You need people that will stand up and say, ‘Let me challenge myself.’ ”
The LRMC medics have once again answered that call, serving as an inspiration to their formation. Their success not only highlights their readiness but also prepares them for future representation at the U.S. Army Command Sgt. Maj. Jack L. Clark Jr. Best Medic Competition in the United States. LRMC personnel contributed to the event as both competitors and cadre, advancing mission-critical medical proficiency across the force.

TRIMEDX has launched TRIMEDX-AIQ, a breakthrough AI intelligence offering that sets a new standard for clinical asset optimization, according to a press release.
“Purpose-built for health systems, TRIMEDX-AIQ combines the largest and most comprehensive data set in the healthcare technology management (HTM) industry with next-generation AI capabilities to deliver real-time visibility, predictive maintenance intelligence and supply chain automation – all within a single unified offering,” the release states.
“With more than 6.1 million device records, 25-plus years of longitudinal insight, and visibility into 90-95% of all active U.S. medical equipment, TRIMEDX has built the industry’s most powerful dataset – refined and AI-ready in ways that cannot be replicated. This scale, combined with over $200 million in recent technology advancements and a national workforce of 3,400 clinical engineering experts, positions TRIMEDX as the only organization capable of delivering an AI offering of this magnitude and insight. This foundation fuels TRIMEDX-AIQ, the only enterprise AI offering that unifies visibility, prediction, security and automation to reduce operational waste, improve medical device uptime and unlock significant cost savings for health systems,” it adds.
Across the country, health systems face a critical opportunity to unlock significant operational, financial and performance gains by tackling longstanding barriers: device inventory records that can be inaccurate by up to 40%, equipment failures that disrupt patient care, rising rental and replacement costs and supply chain inefficiencies that delay critical repairs. Fragmented data, manual workflows and operational blind spots limit visibility and keep teams reacting to problems after they occur. Existing tools – ranging from CMMS platforms to episodic inventory audits and spreadsheet-driven planning – do not provide the predictive intelligence or unified visibility required to solve these issues at scale.
“When these barriers are eliminated, the opportunity is transformative: 10-20% reductions in clinical engineering costs, 25-35% capital expense avoidance and deferral, and equipment uptime reaching 99%. Without that shift, the result is millions of dollars in unnecessary spending and thousands
of hours lost to avoidable downtime every year,” the release states.
TRIMEDX-AIQ combines clinical asset visibility, predictive intelligence and supply chain automation into a single AI-native offering built specifically for the needs of health systems, according to the release. “Rather than relying on disconnected tools and manual updates, TRIMEDX-AIQ provides continuous, automated visibility into the health system’s entire device ecosystem – delivering accurate, real-time asset inventories and resolving the inaccuracies that can reach up to 40% in many health systems today. This enhanced visibility reduces rental overspend, strengthens cybersecurity by identifying unknown devices, and improves capital planning and budgeting by giving leaders a true picture of what they own and how it’s being used.”
“Health systems are facing unprecedented operational pressure, from rising costs to staffing shortages,” says TRIMEDX CEO Neil de Crescenzo. “TRIMEDX-AIQ gives leaders the visibility, predictability and automation they need to run a more resilient, cost-effective operation at scale. It represents the future of clinical asset management, powered by AI and built for the realities of modern health care.”
The release continues:
“TRIMEDX-AIQ applies predictive intelligence to maintenance and repair workflows, equipping clinical engineers with the insights they need to prevent failures before they happen, accelerate turnaround time and work more efficiently. Using TRIMEDX’s multi-vendor dataset in combination with health system data, TRIMEDX-AIQ anticipates likely failures, automates preparation steps such as preventative maintenance kits & parts ordering and synthesizes task lists using generative AI. The result is improved uptime, faster repairs and a more resilient workforce. The offering further strengthens operational resilience by automating supply chain steps that frequently create bottlenecks. By integrating predictive maintenance insights, asset condition data, and repair workflows, TRIMEDX-AIQ ensures that parts and resources are aligned precisely when needed. This reduces delays, speeds up repair cycle and unlocks measurable savings.”
The “Medical Equipment Repair Services Market-Global Forecast 2025-2032” from Research and Markets reports that the market is valued at $44.04 billion in 2024 and projected to grow to $90.49 billion by 2032.
As healthcare organizations depend heavily on the seamless functioning of equipment from MRI scanners to infusion pumps, these services mitigate risks associated with system failures that can lead to postponements and elevated patient safety risks. The industry must navigate challenges such as aging equipment and tight budgets while aligning with regulatory standards, highlighting the importance of strategic planning and risk mitigation in operational decisions.
Navigating the post-pandemic landscape, the medical equipment repair sector is leveraging digital transformations and service delivery innovations to enhance repair dynamics. Remote monitoring and AI-driven predictive maintenance are becoming standard, enabling proactive service interventions that result in improved equipment uptime and reduced service cost. Hybrid service models, combining on-site expertise with centralized support, empower technicians with mobile tools,
thereby improving repair efficiency and competitive advantage Service segmentation shows a growing emphasis on preventive maintenance as foundational to equipment reliability, supported by critical calibration services. The demand for innovative service models highlights a shift toward subscription frameworks, offering predictable costs and driving provider revenue. Equipment segmentation underscores the necessity for specialized services across different equipment types, with hospitals and clinics forming core service customers interested in comprehensive, round-the-clock service commitments.
Global service demand varies significantly across geographies. North America’s mature infrastructure supports advanced predictive services, while Latin America seeks cost-effective repairs. In Europe, the focus is on sophisticated service networks with early adoption of innovative service agreements. In Asia-Pacific, the rapid modernization of healthcare infrastructure, particularly in China and India, presents substantial opportunities for market entry strategies tailored to diverse service maturity levels.

The recent webinar “Laser Safe: The Biomed’s Path to LSO Certification” highlighted the importance of training and certifying biomedical engineers to serve as Medical Laser Safety Officers (MLSO) in a healthcare facility.
Presenters Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, FAAN, and Patti Owens, MHA, BSN, RN, CMLSO, CNOR, pointed out that biomeds make ideal candidates for laser safety officer roles in healthcare facilities.
Biomedical engineers should be Medical Laser Safety Officers (MLSOs) because their technical expertise with medical devices, understanding of safety protocols, and familiarity with equipment maintenance and calibration make them ideal for managing complex laser systems and ensuring patient, staff and public safety in healthcare environments. Their technical background directly aligns with the need for precise risk assessment, implementation of control measures, and adherence to strict ANSI standards.
Over 50% of laser-based hospitals and outpatient surgical centers are considered deficient because they lack an MLSO, which puts patients and staff at risk. Without proper credentialing, classified laser systems, updated standard operating procedures, or appropriate protective eyewear, serious injuries can happen. Incidents can quickly lead to costly penalties, regulatory actions and litigation. Ensuring compliance with national regulations, state laws, laser standards and practice guidelines is essential for fostering a culture of safety.
An MLSO is a specially trained professional responsible for
The Healthcare Technology Management Association of Ohio (HTMA-Ohio) will host its 2026 HTMA-OH Conference and Expo on Feb. 5-6, 2026, at the Renaissance Hotel and Conference Center in Westerville.
The two-day event will bring together healthcare technology management (HTM) professionals, industry leaders and solution providers for education, leadership development and networking. The conference will feature a keynote presentation, leadership development workshop, multiple educational sessions, roundtable discussions and an expansive exhibit hall.
The keynote speaker for the conference will be Bryant Hawkins, HTM leader, CEO of Elevate HTM, author and influencer.
Programming begins Feb. 5 with a three-hour leadership development course led by industry expert Carol Davis-Smith, focused on developing effective HTM strategies. Attendees will also have the opportunity to connect with peers during a free Smash Park social outing that evening.
On Feb. 6, the conference will offer 14 educational sessions,

ensuring the safe use of lasers in medical settings such as hospitals, surgical centers, vision clinics or dermatology offices. The webinar reviewed the MLSO role as defined and guided by ANSI Z136.3, the American National Standards Institute (ANSI) standard for the Safe Use of Lasers in Healthcare.
Education to prepare for the role of a MLSO are offered via Medical Laser Safety Officer (MLSO) Excellence live virtual training sessions in 2026. The sessions are designed to prepare healthcare professionals to become a certified laser safety officer. MLSOs can come from a variety of backgrounds. This training is designed for healthcare professionals looking to enhance their laser safety knowledge and improve the quality and safety of patient care at their facility. Professionals who should consider obtaining MLSO certification include laser safety officers, biomedical/clinical engineers, radiation safety officers and surgical technologists.
Find out more and register today at medicallasersafety.com/
a keynote presentation, a roundtable discussion with industry experts, and access to 40 vendor tables showcasing products, services and solutions for HTM professionals.
Additional highlights include free food, a complimentary happy hour, prize giveaways and extensive networking opportunities.

“Whether you are new to HTM or an experienced professional, this conference offers something for everyone,” HTMA-Ohio organizers said. “The goal is to create an engaging environment where attendees can learn, exchange knowledge and build meaningful connections across the industry.”
The Renaissance Hotel and Conference Center is located at 409 Altair Parkway, Westerville, OH 43082.
For more information about the 2026 HTMA-OH Conference and Expo, including registration details and updates, visit HTMA-OH.org

Coming off the largest MD Expo ever, TechNation parent company MD Publishing has announced the addition of a reverse expo to the spring conference.
HTM professionals are invited to register for the MD Expo Baltimore (April 7-9) that is supported by the Baltimore Medical Engineers and Technicians Society (BMETS).
Attendees will connect with industry peers, gain insights into the latest advancements in HTM and expand their professional network.
MD Expo Baltimore will also feature newly popular and older favorites at this can’t-miss event. A few of the offerings include:
• Welcome Reception
• Tech Choice Awards Presentation
• Networking Lunch (open to everyone)
• Lunch & Learn (ticketed event for attendees only)
• Exhibit Hall Grand Opening
• Young Professionals Event
• Hands-On-Training (H.O.T.) Workshops
MD Expo strives to provide healthcare technology management professionals with a unique, intimate and rewarding conference second to none. Clinical engineers, biomedical technicians, directors and managers, procurement/asset managers and others responsible for medical technology will gather in a one-of-a-kind warm and welcoming environment to network with peers, learn the latest technologies and advances in HTM.
As always, MD Expo offers free registration for hospital employees, students and members of the U.S. Armed Forces.
Register today at MDExpoShow.com.
MD Expo has worked with the host hotel to provide a discounted rate for attendees. The deadline to reserve rooms is March 7, 2026 (room block may sell out prior to deadline).
Check out the details at mdexposhow.com/location/
Webinar Wednesday benefitted from amazing presenters, generous sponsors, Tools of the Trade demonstrations and more in 2025.
New in 2026 is a webinar version of the popular monthly TechNation Roundtable article. HTM insiders will come together for a panel discussion where they will add to their responses shared in the article. This is an exciting opportunity to learn more about the latest technology, features and devices in HTM from experts with powerful insights.
The Roundtable webinars are designed to enhance the continuing education TechNation offers the HTM community. Attendees benefit greatly from the free webinars and CE credits from the ACI.
“Webinar Wednesday allows the advancement of knowledge and brings people together in the HTM profession,” said Melissa Jumbo, administrative assistant, Fort Defiance Indian Hospital Board Inc.
“These webinars provide unique insights into our industry and many different ways to advance our experience as well as our careers,” said Larry Hamilton, biomedical services manager, Venture Medical.
“Webinar Wednesday provides valuable information on the biomedical industry. It brings subject matter experts to BMETs all across the nation. With this information, we are all able to learn more and make decisions for our career and industry,” said Isaiah Ledesma, faculty, biomedical engineering technology, St. Philip’s College.
View on-demand recordings of the 2025 webinars and register for upcoming webinars at WebinarWednesday.live.
The Tech Choice Awards shine a spotlight on the vital and outstanding work HTM professionals provide to the nation’s health care industry. These men and women play a role in delivering life-saving care to millions each year.
HTM professionals generated over 1,500 nominations for the 2026 Tech Choice Awards with the top 5 nominees for each of the 14 categories named as finalists. Voting began on October 1 and closed on January 9, 2026. Votes are being tallied as this report is being written.
The Tech Choice Awards (also known as the Wrenchies) are the people’s choice award for the HTM community. The winners are based 100 percent on the number of votes each finalist received during the voting period. A special thank you goes out to the sponsors who help make the Tech Choice Awards possible. The sponsors do not have any input when it comes to selecting winners.
Wrenchie winners will be announced in the March issue of TechNation with an award ceremony planned for the MD Expo Baltimore in April 2026.

The Tech Choice Award categories are:
1. Professional of the Year, sponsored by Innovative Radiology
2. Large Department of the Year (500+ beds) sponsored by USOC Medical
3. Mid/Small Department of the Year (up to 500 beds) sponsored by USOC Medical
4. ISO Professional of the Year sponsored by Healthmark
5. Young Professional of the Year sponsored by Prescott’s Med
6. Director/Manager of the Year sponsored by MW Imaging
7. Educator of the Year sponsored by MAULL BIOMEDICAL TRAINING LLC
8. Women in Leadership sponsored by Avante Health Solutions
9. ICON sponsored by Renovo Solutions
10. Industry Influencer sponsored by Soma Tech Intl
11. Outstanding Vendor
12. Military BMET of the Year sponsored by College of Biomedical Equipment Technology
13. Association of the Year sponsored by MultiMedical Systems, LLC
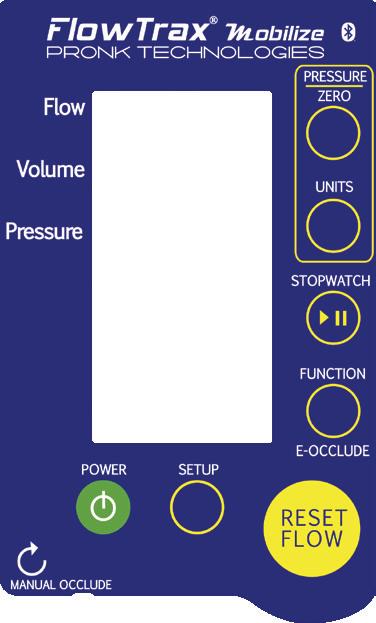
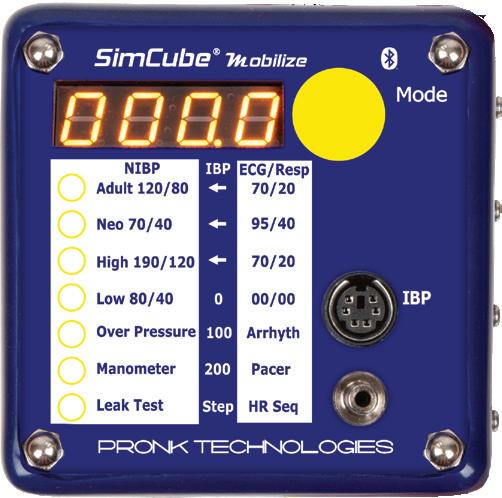
14. Humanitarian of the Year sponsored by Pronk Technologies
TechNation is thrilled to announce that nominations are now open for the 2026 40 Under 40, powered by YP at MD. Now in its third year, this prestigious program shines a spotlight on the next generation of leaders in the healthcare technology management (HTM) industry.
Each year, TechNation honors a diverse group of accomplished young professionals who are driving innovation, excellence and progress in HTM. Last year’s honorees exemplified the intelligence, creativity and dedication that make this field so impactful — and now it’s time to recognize the next wave of outstanding talent!
If you know an exceptional HTM professional under 40, we encourage you to nominate them for this honor. Applications are open now at https://1technation.com/2026-40-under-40/ with a submission deadline of April 24. Help TechNation highlight the best young biomeds shaping the future of HTM!
The YP at MD program, supporting the 40 Under 40, is a dynamic community of young professionals in the HTM field. Members benefit from exclusive networking opportunities at MD Expos, HTM Mixers, and through online platforms, fostering connections and sharing ideas for a bright future in HTM.
For more details about YP at MD, visit 1technation.com/yp. Together, let’s celebrate the talent, hard work and innovation that keep the HTM industry moving forward.




After 25 years in the medical imaging trenches and a career that started in the U.S. Army, Omar W. Jarrah knew there was room to improve how service and support were delivered in the imaging space. It was that idea that inspired him to create FDM Enterprises.
“I’ve spent decades watching big companies forget the little things,” he says. “And in this industry, those ‘little things’ are usually what keep patients waiting, hospitals frustrated and engineers running around in circles.”
His mission to address that frustration fueled the launch of FDM Enterprises – a company dedicated to offering preventive maintenance, troubleshooting, and repair support with the kind of persistence, preparation and precision you would expect from someone with a military background. TechNation recently found out more about FDM Enterprises including what to expect in the future.
Q: CAN YOU TELL US A LITTLE ABOUT YOUR COMPANY?
JARRAH: As a veteran with 25 years’ experience, I started FDM Enterprises to support others in the industry with their MRI, CT and injector service needs. We offer PMs and service support to peers and clients with highly competitive rates. We have been expanding into titanium tools and are looking to offer other services.
Q: HOW DOES YOUR COMPANY STAND OUT?
JARRAH: It comes down to one principle: support
– done better, faster and without the inflated price tag. While many service providers focus on locking in giant contracts and dazzling sales metrics, FDM Enterprises puts its energy into what matters most: customer satisfaction and reduced downtime. Hospitals and imaging centers are often surprised to learn that with FDM, they can get their MRI, CT and injectors serviced in a single service event – a rarity that minimizes disruptions to patient care. We’ve all seen the chaos when three different vendors are needed for three different systems. Why not fix it all at once and let the clinicians get back to doing what they do best?
Q: WHAT IS ON THE HORIZON FOR FDM ENTERPRISES?
JARRAH: In the next five to 10 years, I see FDM Enterprises not just as a service provider, but as a driver of competition and quality improvement in the imaging service industry. My long-term goal is to raise the bar by proving that proactive, customer-focused service doesn’t have to come at premium rates. And at the heart of it all is a very simple philosophy: solve problems, fix things and make life easier for both peers in the industry and the patients relying on those machines. Honestly, the best part of this job is knowing that when I fix something, I’ve played even the smallest part in helping a patient get the care they need. That’s the kind of satisfaction you can’t put a price on.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE TO SHARE WITH THE TECHNATION COMMUNITY?
JARRAH: Please reach out and connect. Who knows how we may be able to help each other to improve patient care.
For more information, visit fdmenterprises.com .






The Clinical Engineering Association of Illinois (CEAI) celebrated a landmark moment during its 14th annual conference, where record-breaking attendance underscored the growing importance of grassroots associations for professionals in the healthcare technology management (HTM) field. In a series of on-site interviews, Founders Alan Moretti and Joe Bandra, alongside current CEAI President Kelley Harris and Vice President Greg Czajka, reflected on CEAI’s origins, growth and enduring contributions to the profession.
According to CEAI, the run of their annual conference reached its highest attendance figure yet, with more than 215 participants. AAMI’s Danielle McGeary, vice president of HTM at AAMI expressed her gratitude for the chance to take part in the event, noting its vibrant atmosphere and the professional value it provided. “It’s truly remarkable to see
such a dedicated group of professionals come together to share knowledge and build connections.”
The event was marked by an impressive array of presentations, workshops and networking opportunities. Moretti was quick to commend the new generation of CEAI leadership for the event’s success.
“This has been our most attended conference yet,” he exclaimed. “The leadership team, led by Kelley and Greg, truly blew it through the roof. It’s humbling to see how far this organization has come.”
“CEAI has always been about bringing people together, and this event exemplifies that spirit. The turnout is proof of the community’s commitment,” Harris said.
CEAI was founded in 2005 when Moretti and Bandra identified a need to unify Illinois’ HTM professionals. Inspired by an ad hoc meeting at Triton Community College, they organized the first gathering at Loyola University Chicago. While uncertain about the initial turnout, they were thrilled when over 35 attendees arrived.
“That first meeting showed us the energy and need for something like CEAI,” Moretti explained.

This enthusiasm catalyzed 12 additional grassroots meetings in 2005 and 2006, culminating in the formal establishment of CEAI and the election of its first officers in 2007. Today, CEAI has grown into a thriving organization that continues to shape the HTM landscape in Illinois.
One of CEAI’s cornerstones is its investment in education and the development of future leaders. The association has awarded more than $40,000 in scholarships to date, a point of pride for founders and members alike. Several scholarship recipients, who are now working in the HTM field, attended this year’s conference.
Bandra, who personally donated $10,000 to the scholarship fund, shared his excitement. “It’s incredible to see students we’ve supported now excelling in their careers. That’s what CEAI is all about – creating opportunities and building the future of HTM,” he said.
Harris echoed this sentiment, highlighting the importance of mentorship and education. “The scholarship program isn’t just about financial support. It’s about fostering a pipeline of talent and inspiring young professionals to carry the torch forward,” he said.
The success of CEAI has inspired HTM professionals in other regions to consider forming their own associations.
McGeary commended CEAI for its legacy of leadership and community-building. “You’ve created something that not only serves Illinois, but also sets an example for HTM organizations nationwide. The dedication and vision here are inspiring,” she said.
Moretti and Bandra offered practical advice, emphasizing the importance of energy, planning and financial sustainability. “No money, no mission. You need sponsors, exhibitors and committed members to make something like this thrive.”
Bandra noted that building strong digital infrastructure is also key. From the start, “having a well-designed website helped CEAI connect with members and communicate effectively.” In today’s world, that’s not optional – it’s essential, he said.
Reflecting on 14 years of progress, Moretti and Bandra also acknowledged the contributions of collaborators like the late Pat Lynch and Robert Shu, who were instrumental in drafting CEAI’s bylaws and operational framework. “It truly took a village to get CEAI to where it is today.”
As CEAI continues to grow, its focus remains on education, collaboration and leadership succession. This year’s record-breaking conference is a testament to its success and the unwavering commitment of its members. With its strong foundation, CEAI is poised to drive innovation and excellence in HTM for years to come.


Healthcare has yet to realize the benefits of applying human factors engineering (HFE), in part because HFE solutions developed for other high-risk industries have been applied without appreciating the important ways that healthcare differs from those industries.
Like aviation, ground transportation, and nuclear power, healthcare is:
• High-risk – Errors have profound consequences for patients, staff and organizations.
• Complex and interdependent – Outcomes depend on seamless interaction between people, processes and technologies.
• Decision-intensive – High-stakes choices must be made under time pressure and uncertainty. However, healthcare also has unique challenges, which must be taken into account when designing safety strategies:
• Every patient is different – No two “inputs” are alike. Standardization is limited by biology and individuality.
• Care plans evolve constantly – Decisions are revisited and adapted several times a day.
• Communication is fragmented – Providers often work asynchronously, connected only through electronic health records.
• Outcomes are subjective – “Health” looks different depending on the patient’s goals and values.
• Motivation drives performance – Healthcare relies on
judgment, collaboration and intrinsic commitment so it cannot require or deliver strict controls. These differences mean healthcare organizations cannot simply copy-paste HFE solutions developed for other high-risk industries. Instead, healthcare systems must apply proven HFE principles to develop solutions tailored for their specific system.
The most effective way to improve healthcare safety is to redesign health system environments, tools and workflows to support people to do their best work, even under stress. This is the only way to manage healthcare complexity and prevent inevitable human slips from causing significant harm.
Realizing profound safety improvements requires not only designing systems that make safe care the path of least resistance but also fostering and sustaining environments where staff are empowered to speak up without fear of blame. In other words, great system design and great safety culture are both required to enable healthcare systems to continuously learn from failures and near-misses.
By embracing HFE and applying systems thinking, healthcare systems can become not only safer, but also more compassionate, adaptive and sustainable, leading to better patient outcomes, healthier providers, lower costs, greater efficiency and stronger public trust.
Visit ecri.org to learn more.


BYRANT HAWKINS
HTM Leader, CEO, Author & Influencer


CAROL DAVIS-SMITH
Business Owner, Clinical Engineer, & Expert Strategist
Explore
FEBRUARY
February 5th
3 Hour Leadership Development course
Develop your HTM strategy
Social Outing - hosted at Smash Park
February 6 th
14 Educational sessions
Keynote session
Round table discussion with industry experts
40 vendor tables
Free Food
Free happy hour
Free prizes
Great Networking

BY JOHN WALLACE
Several times in the 2009 American comedy film “The Hangover” Stu states that he is a doctor only to have it pointed out that he is a “dentist.” The gag plays on the belief many hold that a doctor is “not a real doctor.”
Yet, go to any dentist’s office and you will find medical devices and equipment that require regular maintenance and repair exactly like the medical devices found in urgent care clinics, hospitals and surgery centers.
The devices and equipment in dental settings continue to catch the eye and attention of more and more healthcare technology management (HTM) professionals – also known as biomeds.
One example of this growing attention to the dental sector was the 2024 UptimeHealth Dental Fix Summit in Nashville, Tennessee. It was supported by a popular provider of HTM education – the College of Equipment Technology.
The four-day event was designed “to equip independent dental equipment repair technicians and biomedical technicians with the latest technical training, business strategies, and networking opportunities in the dental industry.”
More recently, AAMI decided to spotlight the dental device and equipment sector of technology as this excerpt from a
2025 news release states: “UptimeHealth, a software and services company for outpatient healthcare, has built a strong presence in dental equipment management through its annual Dental Fix Summit. In a bid to bring that resource to the wider HTM community, AAMI has acquired the annual summit, with plans to make it a key feature of the association’s next annual HTM conference in Denver, Colorado, May 29 to June 1, 2026.”
College of Biomedical Equipment Technology President Dr. Richard L. “Monty” Gonzales, an early proponent of the dental equipment management movement, noted that a biomedical equipment technician (or BMET) background provides a strong foundation for transitioning to dental equipment repair.
He pointed out that core competencies, including electronics, troubleshooting, mechanical and pneumatic systems, preventive maintenance, calibration, safety and infection control protocols, as well as imaging, sterilization and IT transfer directly to dental devices and systems.
However, much like a patient would not ask a primary care doctor to perform a root canal, hospital biomeds need additional education and training to service dental devices.
“These types of technical skills align with the proficiencies employers value and enable entry into many unique roles in the dental industry. Success in dental equipment service, however, necessitates targeted additional training,” Gonzales said. “Specialized components require focused expertise, including high- and low-speed handpieces, dental unit waterlines, advanced plumbing, amalgam separators,
clinic-specific utilities, procedural workflows, and digital integrations distinctive to the dental environment. This specialized knowledge is typically acquired through original equipment manufacturer (OEM)specific certifications or dedicated programs, such as those offered by the College of Biomedical Equipment Technology.”
However, there are many similarities especially when it comes to new technology.
“Mirroring the transformation and escalating technological complexity observed in traditional HTM roles – where networked devices, advanced imaging, and integrated software systems increasingly drive service demands – the dental sector similarly experiences robust demand fueled by the rapid adoption of digital dentistry technologies and ongoing needs for dental operatories,” Gonzales said. “Traditional equipment, such as highand low-speed handpieces, dental chairs/ treatment centers, air compressors, vacuum systems, and autoclaves, continue to generate high repair volume due to frequent mechanical wear and daily clinical use.
Like the HTM industry, the dental industry demands timely maintenance and repair services.”
He added that biomeds have an advantage when it comes to expanding their services to include dental equipment saying it is “generally less complex than hospitalbased medical devices, which feature advanced electronics, integrated software, networked connectivity with cybersecurity risks, and life-critical functions requiring rigorous calibration, electrical safety testing, and strict regulatory compliance.”
“In contrast, dental systems – such as chairs, delivery units, and autoclaves – focus on mechanical, pneumatic, and hydraulic components in compact, standalone setups with less emphasis on digital integration,” Gonzales said.
“However, dental equipment introduces unique challenges necessitating specialized training beyond standard BMET/HTM curricula,” he added.
Read what else Gonzales shared about HTM and dental equipment online at 1technation.com/htm-dental.


BY RAVIN JANI
he speed at which AI has enveloped our collective consciousness today is astounding, further compounded by the hype that it is the panacea for all that ails healthcare community. This has left patientfocused and financially strapped executives in a quandary.
Investments in enhancing and/or maintaining patient care continue to be the priority of the healthcare community. Allocating limited budgets for nascent back-office technology solutions that haven’t quite demonstrated ROI isn’t on their radar. To remain competitive and to attract and retain talents, these executives are challenged with evaluating the way forward.
Fortunately, the proposition isn’t “Nothing or All-in.” There are incremental steps requiring a fraction of total investment that can get the healthcare community
started on building up their analytical information domains.
Data is the foundation on which information and intelligence is built, which in turn drive our decisions and actions. The healthcare community has access to a wide variety of data including:
• First-party data refers to internal data that is created through daily interactions and transactions, such as patient intake information.
• Second-party data refers to the data that is created in collaboration with trusted partners such as external service providers.
• Third-party data refers to the data that is acquired from external sources and agencies such as compliance and privacy standards.
Every provider in the healthcare community is on various stages of maturity with respect to how and how much they leverage the data they have access to, to complement their decision-making process.
Purpose Descriptive Indicative Predictive Prescriptive Proactive
To understand what happened
To explain why it happened
Output Tools / Processes
Example
Historical insights
Dashboards, reports, spreadsheets
Patient demographics, monthly invoices report
Causation insights
Correlation analysis, data engineering, spreadsheet formulas
Patient re-admission rate increase analysis
Usage of data to inform our decisions and actions has evolved from simply describing the past (descriptive) to anticipating future outcomes (predictive) to recommending a course of action (prescriptive) to executing the best course of action (proactive).
As we move from less mature to more mature evolution stages, each stage progressively enriches the information to enhance our decision making as well as providing better intelligence to drive our actions.
Regardless of the stage, the reliability of the information output and therefore the intelligence gained is predicated on three critical elements for the underlying data:
• Comprehensive – access to only the first-party data is an information silo. It will provide an incomplete understanding of the situation or the challenge. To gain holistic intelligence, access to second-party and third-party data is also needed.
• Quality – the adage, “garbage-in/garbage-out” holds especially true in this situation. It is compounded by the fact that the healthcare community so far hasn’t had the imperative to refresh technology and data infrastructures.
• Security – given the sensitive and private nature of data healthcare community has access to, it is of paramount
To forecast what is likely to happen
Future forecast
Machine learning, gen AI, regression models, time series analysis
Identifying patients with readmission risks
To recommend what potential actions to take to remedy a situation
Data-driven decisions and recommended actions
To execute a recommended course of action
Executing recommended action based on a specific diagnosis
Advanced ML, learning, gen AI, complex data engineering AI/ML, Agentic AI
Recommending timely interventions for at-risk patients
Scheduling an appointment with pulmonary specialist upon machine identification of irregularity on a patient’s lungs x-ray image
importance that any modernization journey undertaken has well-defined guardrails to safeguard all data.
Before making any significant investment to address the perceived or real gaps in your ability to gain intelligence from the data you have access to, I would recommend going back to the fundamentals and performing an assessment of what requirements you are trying to meet, what are the objectives and ROI of the investment you are making. It may turn out that descriptive and indicative stages are sufficient for what you need now and that the comprehensiveness, quality and security of the data is adequate.
An objective assessment of your requirements and infrastructures is a logical first step. This assessment can be performed internally by the appropriate teams within the healthcare system, their bandwidth and resources permitting. Alternatively, you can engage external independent consultants who have access to appropriate methodologies and toolsets to do so. Regardless of who does it, it is important to understand the baseline before embarking on the next step of the journey.

Ravin Jani is the chief digital officer with Fortuneline Business Consulting LLC.
Watch these webinars on-demand

The TechNation Tools of the Trade LIVE Demo webinar “Laser Safe: The Biomed’s Path to LSO Certification” was presented by Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, FAAN, Perioperative Consultants LLC; and Patti Owens, MHA, BSN, RN, CMLSO, CNOR, FAORN, AestheticMed Consulting International LLC. The webinar is eligible for 1 CE from the ACI.
Owens has extensive experience in medical safety programs and laser safety and provides valuable consultation services. She has held significant roles, including president of the AORN eChapter, secretary of the ANSI Z136.3 committee for 12 years, and the safety officer of the American Society for Laser Medicine and Surgery. She has been recognized for her achievements with the Nurse Excellence Award in 1999 and 2014. In 2024, she received the R. James Rockwell Jr. Education Achievement Award. In addition, she was recently designated as a Fellow with AORN for 2026.
Dennis is a consultant for Perioperative Consultants LLC. She is an active member in several professional organizations including the Association of periOperative Registered Nurses (AORN), American Academy of Nursing, and Laser Institute of America. She is a fellow for AORN and the AAN as well as the recipient of the 2026 Award for Excellence in Nursing. The webinar highlighted the importance of training and certifying HTM professionals to serve as Medical Laser Safety Officers (MLSO) in a healthcare facility. Biomedical engineers can be Laser Safety Officers (LSOs) because their technical expertise with medical devices, understanding of safety protocols, and familiarity with equipment maintenance and calibration. These important attributes make them ideal for managing complex laser systems and ensuring patient, staff and public safety in healthcare environments. Their technical background directly aligns with the need for precise risk assessment, implementation of control
measures and adherence to strict ANSI standards.
The presenters also invited attendees to register for a MLSO Excellence training session designed to prepare healthcare professionals to become a certified laser safety officer. Three two-day sessions are planned for the remainder of 2026 with one in April, July and November. More information about the two-day live virtual training sessions is available at medicallasersafety.com/
More than 100 healthcare professionals registered for the webinar with 58 logged in for the live session. A recording of the webinar is available for on-demand viewing at WebinarWednesday.live.
Webinar attendee Scott Williams, a BMET III with Trimedx, correctly answered a trivia question to win a Swiss Force Meister Multi-Tool.
Attendees rated the presentation high and provided very positive feedback via a post-webinar survey that included the question, “What was your single biggest takeaway from today’s webinar?”
“A clearer understanding of the LSO responsibilities and what biomed technicians often overlook in laser safety,” said Navya Sharma, a student at St. Clair College.
“Just an overall introduction on what biomed needs to do to complete an LSO certification,” said Jeff Grubb, a director of biomed with Piedmont Medical Center.
“MLSO certification needs to come from a reputable source. And that it is a valuable certificate for any biomed,” said Laurence Robert, CHTM, CBET, an associate director at the University of Vermont.
“Biomeds make good LSOs because they already have a lot of the technical knowledge that is needed,” said Christina Bottomley, a tech manager and BMET II at Rolling Plains Memorial Hospital.
Check out a recording of this webinar or register for the next webinar at WebinarWednesday.live.
Registration on WebinarWednesday.live
Eligible for 1 CE credit from the ACI.

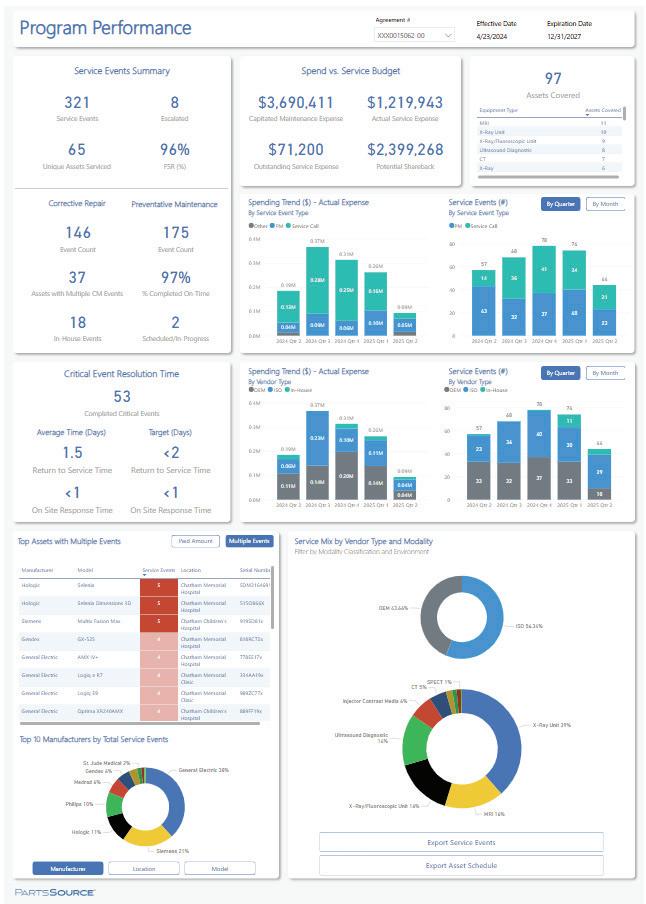
Healthcare organizations face growing pressure to keep critical equipment running while controlling service costs, managing complex contracts, and coordinating dozens of service vendors—all with limited visibility and stretched internal teams. PartsSource PRO Service is designed to solve these challenges by helping hospitals and health systems simplify service management, reduce unnecessary spend, and operate with confidence.
PRO Service gives organizations a clear, enterprise-wide view of their equipment service landscape—what assets are covered, where dollars are being spent, how vendors are performing, and where opportunities exist to improve. By bringing service data, contracts, vendors, and workflows into one centralized experience, PRO Service replaces fragmented processes with consistency, accountability, and actionable insight. The result is fewer surprises, faster resolution, and service decisions that are
guided by data rather than guesswork.
In this Tools of the Trade Live Demo, attendees will see how PRO Service uses a structured, technology-enabled Service Assessment to uncover savings opportunities, right-size coverage strategies, and improve service outcomes. You’ll learn how customers achieve meaningful upfront cost reductions, free up thousands of hours for their HTM teams, and gain the confidence that every service dollar is aligned to organizational priorities.
Trusted by healthcare organizations to manage more than 172,000 service events across 23,000 assets, PRO Service helps teams move from reactive service management to a more predictable, efficient, and cost-effective operating model. Join us to see how PRO Service enables healthcare organizations to spend smarter, work more efficiently, and deliver more reliable equipment performance across the enterprise.

Medical equipment everywhere, yet nowhere?
Safe, timely and effective care is jeopardized because the equipment that makes it possible is everywhere … and yet nowhere at the same time. Midmark CareFlow ™ RTLS leverages Bluetooth ® Low Energy (BLE) technology to rapidly and cost-effectively deliver facility-wide visibility—helping biomed and clinical teams locate equipment faster, improve utilization and optimize medical asset inventory.
Learn more at: midmark.com/RTLStracking













Healthcare technology management departments often reply on a real-time location system (RTLS) to help them complete their many tasks and responsibilities. RTLS has evolved over the years matching the rapid advances in technology in the consumer and healthcare markets. TechNation recently spent some time finding out more about RTLS and how HTM professionals rely on it as well as some of the latest trends and newest features.
Participants in this roundtable article on RTLS are:
• Duke Health Senior Director of Clinical Engineering Benjamin Scoggin, MBA, MMCi;
• ECRI Associate Consultant, Device Safety Consulting Dustin K. Telford, AAMIF, CHTM, CBET, CRES, CLES;
• HID Healthcare RTLS Vice President of Sales Kerry Brock; and
• Midmark RTLS Senior Director HT Snowday.
Q: HOW IS RTLS CHANGING THE WAY HTM DEPARTMENTS FORECAST EQUIPMENT DEMAND OR PLAN CAPITAL REPLACEMENT?
SCOGGIN: RTLS has shifted forecasting from anecdotal, and utilization-survey driven to data-validated, defensible planning. Instead of relying on staff perceptions such as “we’re always short on pumps,” we can now evaluate actual utilization rates, dwell times, idle percentages and cross-campus movement patterns. From an HTM standpoint, this directly influences capital replacement decisions by identifying true over- or under-capacity, highlighting assets that appear old but are lightly used, and surfacing newer devices that are over-utilized and approaching functional end of life faster than expected. It also supports fleet right-sizing and redistribution across hospitals and clinics, often delaying capital spend while improving availability and clinician satisfaction.
TELFORD: RTLS doesn’t replace capital equipment replacement planning – it finally gives us the missing data to do it properly. Location states like “in-use,” “standby,” “in-transit,” and “stored” reveal the truth about utilization
that questionnaires and anecdotal reports never could, but the real power comes from weaving this data together with complementary sources like bed management systems, device-generated utilization logs, and CMMS maintenance patterns. When you discover that 40% of your infusion pumps spend most of their time in “storage” mode while nursing units are calling for rentals, you’ve found money sitting in closets rather than a justification for capital purchases. The magic happens when HTM teams stop viewing RTLS as a standalone solution and start treating it as one instrument in an orchestra – where location data harmonizes with clinical workflows, preventive maintenance schedules, and actual patient census to create a symphony of evidence-based asset management that finally separates real equipment shortages from poor distribution strategies.
BROCK: RTLS provides real-time utilization data, enabling HTM teams to identify underused or overused assets and make data-driven decisions. This visibility helps optimize fleet size, reduce unnecessary purchases, and prioritize replacements based on actual usage rather than estimates. Ultimately, it shifts planning from a reactive to a proactive approach, improving both efficiency and cost control
SNOWDAY: RTLS is enabling HTM departments to shift from assumption-based capital planning to decisions driven by real utilization data. By showing how often equipment is used, where it spends time idle and how demand varies over time, RTLS helps distinguish true shortages from redistribution opportunities. This allows HTM teams to better forecast future needs, right-size equipment fleets and prioritize capital replacement based on actual wear, risk and clinical impact. The result is more defensible capital requests and smarter, data-backed investment decisions.
Q: HOW DO YOU EVALUATE WHETHER A PIECE OF EQUIPMENT TRULY NEEDS AN RTLS TAG, AND HOW DO YOU AVOID “OVER-TAGGING?”
SCOGGIN: We start by asking what decision the data will enable. If RTLS data will not meaningfully influence clinical workflow, capital planning, patient throughput, or HTM operations, then the asset likely does not need a tag. From an HTM perspective, the strongest candidates are mobile, shared assets with high search time, high loss risk, high rental substitution cost or frequent preventive maintenance dependencies. We avoid over-tagging by piloting on a limited asset class, validating the value of the data and then scaling intentionally. Tagging everything increases cost, noise and maintenance burden without increasing insight.
TELFORD: Start with two fundamental questions: “Can this equipment move?” followed immediately by “Does this equipment actually move in our facility?” – because tagging wall-mounted devices or equipment that’s been sitting in the same storage room since 2023 is just burning budget on battery replacements. Before investing in any tagging infrastructure, ask the penetrating questions: Does
this device already report its location through the vendor’s proprietary software or our existing hospital wireless network? If this equipment travels to areas with coverage gaps like outpatient pavilions, arboretums, or parking structures, will our RTLS infrastructure even work there? The emerging sweet spot is leveraging RTLS solutions that tap into devices’ own internal wireless capabilities plus your existing IT infrastructure – avoiding vendor-specific tags entirely – and intelligently mixing passive RFID tags (which are remarkably affordable, let you print your own biomed asset numbers, and have no batteries to maintain) with active tags reserved only for high-value assets where clinical practitioners need “find it right now” capabilities. Remember: if you’re tagging IV poles while your $80,000 ultrasound systems wander freely through the enterprise, you’ve missed the point entirely and probably need to revisit what “strategic asset management” actually means.
BROCK: We start by assessing the asset’s mobility, criticality and impact on clinical workflows. High-value, frequently moved or patient-facing equipment typically qualifies for tagging, while stationary or low-impact items do not. This criteria-based approach prevents overtagging and ensures ROI by focusing on assets that deliver measurable operational benefits
SNOWDAY: HTM departments should evaluate the need for RTLS tagging by considering device value, utilization frequency, mobility and the clinical impact if the equipment is not immediately available. High-value, frequently moved assets or devices that directly affect patient care and throughput when unavailable are strong candidates for tagging. RTLS data helps avoid over-tagging by identifying equipment with low utilization, limited movement or minimal operational impact. This targeted approach ensures tagging investments are focused where visibility delivers the greatest clinical and financial return.
Q: HOW DO EMERGING TECHNOLOGIES SUCH AS AI-POWERED ANALYTICS, UWB, BLE, OR WI-FI 6 IMPACT EXPECTATIONS FOR NEXT-GENERATION RTLS SOLUTIONS?
SCOGGIN: Expectations are evolving beyond simple location awareness to predictive and prescriptive intelligence. AI-driven analytics should help anticipate shortages, predict failure risk based on movement and usage patterns and automate alerts tied directly into CMMS and clinical workflows. Technologies such as UWB improve room-level precision, while BLE and Wi-Fi 6 expand scalability and reduce infrastructure barriers. From an HTM standpoint, the most important expectation is interoperability. RTLS must integrate cleanly with CMMS, asset life cycle systems and cybersecurity frameworks without becoming another siloed platform that requires manual reconciliation.
TELFORD: AI-powered analytics are shifting RTLS from a “where is it now” tracking system to a “what should we do about it” predictive intelligence platform that can forecast equipment shortages before they impact patient care,

“The biggest failure point isn’t technology – it’s treating RTLS as a magic solution rather than recognizing it’s merely a tool, and the actual solution requires a skilled team that continuously refines workflows, educates users and integrates new capabilities as they become available.”
identify abnormal movement patterns suggesting theft or misuse, and automatically optimize asset distribution across an enterprise. Ultra-wideband technology delivers the room-level accuracy that healthcare finally demands – knowing a ventilator is “somewhere on 4-West” isn’t acceptable when minutes matter in patient deterioration scenarios. The convergence of these technologies with existing IT infrastructure like WiFi 6 and BLE reduces deployment costs and creates opportunities for HTM departments to integrate RTLS data with CMMS platforms, EHR systems, and supply chain management tools, but organizations must resist vendor promises of “AI magic” and demand transparent algorithms with validated accuracy metrics before making million-dollar infrastructure investments.
BROCK: Emerging technologies enhance accuracy, scalability and actionable insights. AI-driven analytics transform raw location data into predictive models for workflow optimization, while UWB and BLE improve precision and flexibility. Wi-Fi 6 supports higher device density and faster connectivity, setting the stage for RTLS systems that are smarter, faster and more integrated.
SNOWDAY: Emerging technologies are raising expectations for RTLS to move beyond basic location visibility into predictive and prescriptive intelligence. AI-powered analytics are now enabling health systems to anticipate a variety of operational needs – such as forecasting PAR levels for high-demand assets like IV pumps, helping ensure the right equipment is available at the right time while reducing excess inventory. Advances in UWB have the potential to deliver roomlevel precision that supports clinical workflows requiring high accuracy, while BLE offers a cost-effective way to achieve facility-wide coverage. When BLE is paired with infrared (IR) technology that delivers proven, room-level precision, RTLS platforms can meet both operational and nursing needs, driving broader adoption and measurable ROI.
Q: WHAT LESSONS LEARNED FROM PREVIOUS RTLS DEPLOYMENTS WOULD YOU SHARE TO HELP OTHERS AVOID COMMON PITFALLS?
SCOGGIN: The most important lesson is that RTLS is not an IT project or a technology install. It is an operational transformation initiative. Deployments struggle when governance, ownership and workflows are not clearly defined upfront. Additional lessons include involving HTM, nursing, supply chain, IT and security early; validating infrastructure assumptions before largescale tagging; piloting and measuring outcomes before expanding; and budgeting for ongoing tag maintenance, battery replacement and data stewardship. RTLS success depends far more on process design and adoption than on hardware.
TELFORD: Before you buy a single tag, answer two critical questions: “Who owns this system?” and “Who’s actually supporting it three years from now when the implementation team has moved on?” – because I’ve watched organizations mothball expensive RTLS deployments within a few years when nobody’s looking at the whole picture or evolving the system to solve real problems for end users. The biggest failure point isn’t technology – it’s treating RTLS as a magic solution rather than recognizing it’s merely a tool, and the actual solution requires a skilled team that continuously refines workflows, educates users and integrates new capabilities as they become available. Start with brutally honest success metrics beyond “we can find equipment faster” – quantify reduction in rental costs, decreased time clinical staff spend searching for devices, or improved equipment availability during rapid response events – then pilot with a small scope where you can demonstrate quick wins and learn from failures cheaply. Here’s the uncomfortable truth: if your RTLS implementation doesn’t include a dedicated champion who treats innovation, education, and integration as ongoing responsibilities rather than one-time checkboxes, you’re not deploying a solution –you’re installing a very expensive equipment museum that documents dysfunction rather than fixing it.
BROCK: Start with clear objectives and stakeholder alignment – unclear goals often lead to scope creep and poor adoption. Validate infrastructure readiness early, as network limitations can derail timelines. Finally, invest in staff training and change management to ensure the technology delivers its intended value
SNOWDAY: One important lesson learned is that siloed RTLS deployments – where different departments implement separate systems – often increase costs, complexity and long-term maintenance challenges. Taking an enterprise approach allows health systems to share infrastructure, data and insights across asset management,


clinical workflows and safety use cases. It’s also critical to plan for operational realities such as ongoing battery replacement for sensors and tags, whether managed internally or through a third-party service. Partnering with a vendor that offers strong local support helps ensure the system remains reliable, adopted and sustainable over time.
Q: HOW DO YOU MEASURE AND VALIDATE THE ACCURACY OF YOUR RTLS SYSTEM, AND WHAT STEPS DO YOU TAKE
SCOGGIN: Accuracy is validated through real-world testing rather than vendor specifications. We perform physical audits, timed movement studies and room-level verification against known locations. We also monitor exception reports, such as assets showing impossible movement patterns or extended lost states. When accuracy issues arise, we follow a structured approach that includes validating infrastructure coverage, reviewing tag placement and orientation, assessing environmental interference and confirming system calibration. We also reassess whether the use case truly requires room-level precision or whether zone-level accuracy is sufficient for the operational goal.
TELFORD: Establish baseline accuracy expectations in your RFP and vendor contract with specific metrics – like “95% room-level accuracy within 30 seconds of asset movement” – then conduct quarterly validation audits by physically locating a random sample of tagged equipment and comparing actual locations to system reports. When accuracy issues emerge, the root cause is usually environmental interference (new construction creating RF dead zones), infrastructure changes (relocated access points or receivers), or tag failures (depleted batteries or physical damage), so systematic troubleshooting should follow a documented protocol rather than ad-hoc responses. The most sophisticated organizations integrate RTLS accuracy monitoring into their daily workflows by having clinical engineering techs verify and document equipment locations during preventive maintenance


“RTLS is enabling HTM departments to shift from assumption-based capital planning to decisions driven by real utilization data.”

visits, creating a continuous validation loop that identifies degradation before it impacts clinical operations. Remember that accuracy isn’t just about technology – it’s also about user behaviors like improper tag placement, removal of tags, or failure to update home locations when equipment is permanently redeployed between units.
BROCK: Accuracy is validated through controlled testing against known locations and ongoing performance audits. We monitor key metrics, such as location error rates and response times, and promptly investigate any anomalies. When issues arise, we recalibrate hardware, optimize software algorithms and adjust environmental factors to restore performance.
SNOWDAY: RTLS accuracy is measured by validating system performance against defined location requirements for each use case, such as room-level or zone-level visibility. IR technology delivers the power of inherent room certainty. A one-to-one relationship between the sensor and the location allows accuracy to be focused down to approximately 2 feet in open areas. For broader, facility-wide coverage, BLE typically delivers 3- to 5-meter accuracy, which can be improved through calibration or by adding additional BLE sensors or gateways. When accuracy issues arise, teams reassess use-case requirements, finetune calibration and adjust sensor placement to ensure reliable, clinically relevant performance.
Q: WHAT ELSE SHOULD TECHNATION READERS KNOW ABOUT RTLS SYSTEMS?
SCOGGIN: RTLS delivers the most value when treated as a strategic operational platform rather than a tracking tool. The strongest returns come from improved clinician efficiency, reduced rentals, smarter capital planning, stronger regulatory readiness and tighter asset life cycle management. For HTM leaders, RTLS has become a data credibility tool. It allows us to engage capital, finance and executive stakeholders with objective evidence rather than estimates. When deployed thoughtfully and governed well, RTLS becomes a force multiplier for both clinical operations and HTM performance.
TELFORD: Here’s what vendors won’t tell you in their glossy presentations: RTLS success depends on organizational change management as much as technical
implementation – without clear policies on equipment ownership, accountability for missing assets, and consequences for hoarding behaviors, you’ve just installed an expensive system that documents which nursing units are best at hiding equipment. The future of RTLS lies in creative integrations that most organizations haven’t imagined yet – predictive maintenance alerts triggered by abnormal movement patterns, automatic charge capture when devices enter patient rooms, or AI-driven redistribution recommendations based on predictive patient census and acuity forecasting. Don’t let perfect be the enemy of good; start with achievable goals that demonstrate value quickly, then expand strategically rather than pursuing the mythical “comprehensive enterprise solution” that becomes a multi-year implementation nightmare. And here’s my favorite reality check: if your RTLS deployment doesn’t make nurses’ lives easier – if it adds clicks, creates workflow friction, or feels like Big Brother surveillance rather than helpful technology – they’ll find creative ways to sabotage it, and you’ll discover that even the most sophisticated tracking system is useless when staff members “accidentally” leave tags in drawers or mysteriously forget to attach them to newly purchased equipment.
BROCK: RTLS systems have matured significantly in the past 5 years, but the industry is still not that close to plug-and-play solutions. A successful RTLS solution is a collaborative effort and is an ongoing, evolving relationship. To do this, it’s important to have knowledgeable, available and a geographically proximate partner.
SNOWDAY: TechNation readers should know that the most successful RTLS strategies move beyond siloed point solutions to an enterprise, hybrid approach. By combining BLE for cost-effective, facility-wide visibility with IR for room-certain precision, health systems can support multiple use cases – assets, staff, patients and safety – on a single scalable platform. That same system can integrate with Epic EMR to deliver real-time location data directly into clinical workflows, automating tasks, improving patient flow and reducing manual documentation. The result is a scalable RTLS foundation that maximizes existing investments while driving meaningful clinical and operational impact.




• A niche job board for the HTM and imaging communities powered by TechNation.
• 3,800+ activelylooking biomedical and imaging professionals
» Completely free and confidential registration and application process.

Featured Employers: Agiliti, Block Imaging, Intelas Health, Renovo Solutions, TRIMEDX, and more!
htmjobs@mdpublishing.com for posting inquiries htmjobs.com to register today
• The fastest growing HTM talent network in the country.
• 350+ open opportunities throughout the United States.
» A variety of posting options ranging from single-job postings to 12-month unlimited memberships.

or more than a decade, USOC Medical has evolved from a trusted biomedical repair provider into a nationally recognized partner supporting hospitals, ambulatory surgery centers, biomedical departments, and healthcare networks across the United States.
What began as a focused, service-oriented organization has grown into a full scale, ISO certified business supporting every major patient monitoring ecosystem, including Philips, GE, Mindray, Spacelabs, Masimo, and others. Along the way, USOC has built a reputation for technical excellence, responsiveness, and quality. These attributes have driven strong organic growth and long-standing customer relationships.
Today, USOC Medical stands at a pivotal inflection point.
Increasing demand for high-quality repair, refurbishment, and lifecycle support, combined with rising cost pressures within healthcare delivery, has accelerated the need for partners that can deliver both reliability and value. USOC’s next chapter of growth is focused on scaling these strengths while expanding capabilities, solutions, and customer impact sustainably.
That next phase is further strengthened by USOC’s alignment with CSAT, a leading provider of complex aftermarket services with deep expertise in repair, refurbishment, reverse logistics, and lifecycle management.
CSAT’s proven operating model, quality systems, and supply chain capabilities provide a powerful foundation to enhance USOC’s offerings. This alignment allows the organization to deliver broader solutions, improved turnaround times, and increased value to healthcare providers nationwide.

This evolution is guided by new commercial leadership with the addition of Michael Smith as Chief Commercial Officer of both CSAT and USOC Medical. Smith brings more than three decades of experience building, scaling, and leading global aftermarket services organizations across highly technical and regulated industries. His background includes driving growth through customer-centric solutions, operational alignment, and disciplined commercial execution, often in environments where

quality, uptime, and trust are mission-critical.
Smith’s appointment reflects a deliberate shift toward a more integrated, customer aligned commercial strategy, one that tightly connects sales, marketing, operations, and product development into a single, cohesive growth engine. Drawing on CSAT’s proven aftermarket capabilities and operating discipline, this approach is focused on expanding the depth and breadth of USOC’s solutions while maintaining the quality and responsiveness customers rely on.
At the core of this strategy is a commitment to partnership. Rather than a transactional service model, USOC is deepening collaboration with health systems, IDNs, and biomedical teams to better understand clinical workflows, asset utilization, and cost pressures. This insight enables the development of differentiated repair, refurbishment, and lifecycle solutions that extend equipment life, improve availability, and reduce total cost of ownership, creating measurable value for healthcare providers.
As USOC Medical moves forward, its focus remains unchanged: delivering dependable, high-quality service. What is evolving is the scale, sophistication, and integration of how that value is delivered. With the combined strengths of USOC and CSAT, and a renewed emphasis on customer collaboration and lifecycle value creation, the organization is well-positioned to support the healthcare community with smarter solutions today and a more resilient service model for the future.
USOC Medical has expanded significantly beyond its original service footprint. What once centered around device repair now includes a diverse set of offerings that support every stage of the equipment life cycle.
USOC Medical operates one of the nation’s largest, most skilled technical repair teams – delivering speed, precision, and
reliability at every step. Our ISO-certified facility handles:
• Patient Monitors
• Modules & Transmitters
• Telemetry Systems
• Ventilator Components
• Infusion Pump Accessories & Modules
• Cables, Sensors & Accessories
• Surgical & Critical Care Monitoring Devices
Every repair follows rigorous ISO-certified processes for repeatability, traceability, and safety. With consistent turnaround times, detailed documentation, and proven quality metrics, USOC Medical has earned the trust of biomedical teams nationwide.
USOC Medical offers one of the most comprehensive inventories of refurbished equipment in the industry, delivering cost-effective solutions without compromising quality. Our portfolio includes:
• Refurbished Monitors & Monitoring Systems
• Modules, Telemetry Transmitters & Parameter Devices
• Reliable Replacement Parts – All Backed by Warranty
• Complete Patient Monitoring Configurations for Expanding Care Areas
As hospitals prioritize cost savings and predictable capital planning, this segment continues to accelerate.
Our modernized e-commerce platform puts thousands of products at your fingertips, fast, easy, and reliable. The catalog features:
• Cables & Sensors
• Compatible and OEM Components
• Refurbished Testing Equipment
• Batteries, Power Supplies & Accessories
• Full Patient Monitoring Bundles

Enhanced with intuitive navigation, SEO optimization, faster quoting tools, and rich product content, USOC Medical’s online experience is designed for speed and simplicity, so you can keep care moving.
USOC Medical’s commitment to quality has always been at the core of the business. The company follows strict procedures aligned with ISO 13485 certification standards, with an emphasis on:
• Consistent repair quality
• Full documentation and traceability
• Clean, controlled repair environments
• Component testing and validation
• Repeatable and audited processes
These standards provide confidence to clinical engineering teams who rely on stable, predictable, and safe outcomes from every repair.
With new leadership and expanded capabilities, USOC Medical is positioning itself as a scalable, modern, and nationally recognized biomedical solutions partner. The strategic priorities for the future include:
1. Enhanced National Footprint
The company aims to serve more health systems, large biomedical organizations, IDNs, and government facilities. Building deeper, long-term partnerships remains a top priority for the commercial team.

2. Modernized Digital Infrastructure
USOC Medical is expanding digital operations through:
• Streamlined online quoting
• Expanded e-commerce product coverage
• Improved product photography and detailed product data
• Stronger SEO and content strategy
• Expanded customer support touchpoints
These updates make it easier for customers to find products, request quotes, and get the information they need quickly.
3. Scalable Operations & Inventory Management
The leadership team is investing in processes and tools that support efficient scaling, including improved inventory controls, smarter forecasting, and stronger supplier relationships.
4. Greater Product Breadth & New Clinical Categories
Future expansion includes more:
• Critical care devices
• Accessories and cables
• Replacement modules
• Specialized components for new equipment generations
The goal is to provide clinicians and technicians with a full ecosystem of compatible and reliable equipment.
The strength of USOC Medical lies in its team. Technicians, quality specialists, customer service professionals, and commercial leaders all contribute to an environment built around trust and performance. Continuous training ensures that each technician remains up to date on changing device platforms and new generations of technology.
The company is also investing in internal development programs, employee growth paths, and cross functional collaboration to make sure the team remains highly skilled, responsive, and customer focused.
As the healthcare landscape evolves, hospitals and clinical engineering teams are under increasing pressure to deliver reliable equipment performance, fast turnaround times, and cost-efficient solutions. USOC Medical is building its future with these realities in mind.
Through expanded product offerings, improved digital tools, stronger internal systems, and new commercial leadership, the company is preparing for a new era of growth built on reliability, service excellence, and trust.
USOC Medical’s mission remains unchanged: to deliver dependable biomedical solutions that enhance patient care, support clinicians, and help healthcare organizations operate with confidence.
The future is bright, and USOC Medical is ready to scale.
Find out more at USOCMedical.com/







BY K. RICHARD DOUGLAS
rtificial intelligence (AI) has rapidly transitioned from a futuristic concept to a transformative force reshaping industries worldwide, with its impact being particularly profound and personal within healthcare.
This technology refers to the ability of machines to perform tasks that typically demand human intelligence, such as learning, reasoning and problemsolving. AI utilizes computers and machine processes to simulate human thought and execute complex automated tasks.
Crucially, AI-enabled systems are capable of exceeding human capacity in specific ways, primarily by efficiently sifting through immense volumes of big data to identify patterns, anomalies and trends.
AI is an umbrella term covering several specialized technologies frequently used in medicine, including machine
learning (ML), deep learning (DL) and natural language processing (NLP). ML involves training algorithms on datasets, such as health records, to create models that predict outcomes.
DL, a subset of ML, uses extensive data and multiple layers of algorithms to form neural networks capable of more complex tasks. Furthermore, NLP enables machines to interpret human language, helping to analyze and understand clinical notes, reports and published research.
The integration of AI is changing how healthcare professionals provide care and how patients receive it, offering a wealth of opportunities to enhance common medical processes. Researchers view AI not as a replacement for healthcare professionals but as a supportive force designed to improve their work.
One of the most mature areas for AI innovation is medical imaging and diagnostics. AI algorithms analyze complex medical scans like X-rays, CTs and MRIs to identify anomalies, acting as a
“AI is no longer optional for HTM – it’s becoming essential.”
second set of eyes for radiologists.
These systems enable faster, more accurate diagnoses; for instance, some AI systems have achieved 94 percent accuracy in detecting lung nodules and 90 percent sensitivity in breast cancer detection, often matching or exceeding human performance when used as a complementary tool.
AI is also central to precision medicine, helping to produce personalized treatment plans that account for factors such as a patient’s genetic makeup, medical history, lifestyle and environmental factors. Predictive analytics powered by AI models can assess patient data to forecast health risks, such as the likelihood of cardiac arrest, allowing medical teams to intervene earlier and improve survival rates.
In the operating room, AI enhances robotic surgery by providing enhanced precision and control. Robotic surgical equipment outfitted with AI can help surgeons perform better by decreasing physical fluctuations and offering updated information during the operation. Beyond clinical applications, robotic process automation (RPA) uses AI in computer programs
to automate administrative and clinical workflows, improving daily facility functions and managing massive volumes of data efficiently.
To ease the burden on doctors, AI-based ambient listening can reduce the time it takes for physicians to dictate notes of patient interactions.
With all AI can do to aid clinicians in the diagnosis and treatment of patients, it also has a place for those who support the clinicians.
For some HTM professionals, AI is viewed as a critical part of proactive service strategies. AI acts as a force multiplier for biomed, supercharging a technician’s abilities to make repairs faster and diagnostics more accurate.
“I’ll start by saying I think AI is the new buzzword. There’s this thought process that AI will fix all that ails us in HTM, but the reality is it will always be a reflection of the core data. Just like with any CMMS, if you put garbage data in, you’ll get garbage
data out. I truly believe AI needs to be leveraged as a tool, with a watchful eye, and not as cure,” says Josh Virnoche, MBA, AAMIF, CHTM, CBET, director, Clinical Engineering at UT Southwestern Medical Center.
The perspective that AI is a tool that is only as good as the data it depends on is a good reminder of the cautious approach required as the technology becomes more prevalent.
“Artificial intelligence is everywhere in healthcare conversations. For healthcare technology management professionals, it’s not about robots replacing engineers or technicians, it’s about using smarter tools to enhance patient safety and operational efficiency. Think of AI as a second set of eyes: from predicting when a ventilator or CT scanner might fail, to streamlining workflows across departments,” says Salim Kai, MS, CHTM, CBET, visiting faculty, Miami University-Teaching in Clinical Engineering and Hospital Instrumentation.
He says with AI innovation comes a catch.
“If the data is biased or incomplete, AI can mislead. That’s why HTM professionals play a critical role: validating algorithms, ensuring service data accuracy and advocating for transparency. In short, we are the ones who make sure AI is safe for patient care before it ever reaches the bedside,” Kai says.
These AI applications are not futuristic. They’re already beginning to shape HTM practice. Kai says that HTM’s responsibility is to be certain that AI applications in medical equipment and clinical technology are safe, ethical and effective.
AI’s ability to analyze vast
streams of operational data offers HTM teams leverage in several key areas:
• Optimizing Operations: AI contributes to the efficient management of equipment within healthcare facilities. Platforms can optimize operating room schedules by accurately predicting case duration and improving resource allocation, which may lead to five to 15 percent reductions in operational costs.
• Boosting Productivity & Addressing Staffing Gaps: The U.S. faces a critical shortage of skilled biomedical equipment technicians. AI helps bridge this gap by enabling diagnostics and streamlining workflows, allowing technicians to service more devices in less time, thereby reducing the need for a larger workforce and cutting repair backlogs. Furthermore, embedding AI into workflows shifts technician time away from administrative tasks and toward more strategic and complex work.
• Proactive Planning: AI-driven predictive services ingest live telemetry, error logs and service histories to forecast component failures days in advance. This shift from scheduled or reactive maintenance to predictive maintenance reduces unexpected device downtime, prevents costly emergency repairs and can extend equipment lifespan. For instance, certain AI tools can predict a CT tube failure at least 72 hours before it occurs.
Virnoche has been actively working on training an AI model to review work orders for quality documentation.
“Big picture would be that on a periodic basis, an automated workflow pulls the team’s work orders from a defined timeline, runs them through the trained AI model and provides letter grade feedback on the quality of the documentation on work orders. Right now, this would be a reactive process, only catching issues after the fact, but would provide actionable insights on how to improve documentation in the future,” he says.
Virnoche adds that on a longer timeline, he would love to see this integrated into the CMMS to give real-time feedback as the documentation is being completed.
“Like I said earlier, the key here is getting the core data right. I need to focus heavily on training the AI to specific, well-defined quality measures like ISO9001/ISO13485 and good documentation practices to ensure it’s not being biased to my own preferences,” Virnoche says.
He says that this is a pet project, but points out that it is a great use case of how AI can provide unbiased feedback to improve quality rather than completely replacing the process itself.
At least one engineer, who has given presentations on AI and HTM, finds the emerging technology indispensable.
“AI is no longer optional for HTM – it’s becoming
essential. When Norton Healthcare transitioned to an ISO 13485-based Quality Management System (QMS) in 2021, we anticipated the FDA’s upcoming Quality Management System Regulation (QMSR) requirement for manufacturers and third-party servicers in 2026. That shift created a need for smarter tools to manage compliance, documentation and risk. AI has filled that gap,” says Mark Cooksey, CLSSMBB, MBA, DME quality engineer and ISO 13485 quality management system leader in the clinical engineering department at Norton Healthcare.
He says that he first presented on the topic to a full-capacity audience at MD Expo New England in 2024 and more recently to a packed audience at AAMI eXchange in June 2025. Since then, he has seen AI adoption grow exponentially.
“For Norton Healthcare’s Clinical Engineering, AI streamlines ISO 13485 and FDA-compliant documentation, accelerates risk assessments and enhances audit readiness. It also delivers measurable financial impact. This year alone, I’ve used AI to evaluate third-party service contracts and draft negotiation responses, saving hundreds of thousands of dollars through AI-guided communications and strategy. When integrated securely, AI improves efficiency, compliance, and cost control, making it one of the most practical tools HTM leaders can deploy,” Cooksey says.
He offers these applications of AI within HTM:
• Streamline Compliance & Documentation: Documentation of your QMS can be overwhelming. AI simplifies ISO 13485 and FDA-compliant documentation – generating policies, procedures and checklists while reducing complexity by over 80 percent.
• Accelerate Risk Assessment & Decision-Making: AI performs statistical trend analysis and can evaluate risk when changing from an OEM PM schedule to an AEM or even a repair as needed (RAN) PM for low-risk medical equipment. Using AI to calculate risk via risk priority numbers (RPN) has guided us in evaluating preventive maintenance changes, enabling data-driven decisions.
• Enhance Audit Readiness: AI drafts corrective action plans (CAPAs) that meet ISO 13485 requirements, helping close gaps faster and maintain accreditation.
• Boost Productivity &Deliver Real Cost Savings: AI automates tasks like creating presentations, analyzing large datasets and generating control charts – cutting hours of manual work down to minutes.
• Improves Communication & Training: AI helps create more effective training materials, job aids and interactive content for CBET education, supporting workforce development without adding administrative burden.
Combining AI with virtual reality provides a whole new set of tools. Natural language tools help techs digest OEM manuals, service bulletins and regulatory changes in real-time during on-site repairs. Additionally, advanced AI tools in the field include augmented reality (AR) headsets that provide hands-free repair guides overlaid in real-time. With real-time AI guidance and AR overlays, even new hires can perform sophisticated tasks earlier in their careers, reducing the burden on senior staff and enabling faster training across teams. AI can also remotely identify issues, allowing centralized teams to provide assistance without deploying a technician for every call.
Kai says that there are some potential challenges with adoption.
“AI is not a replacement for HTM expertise, it’s a partner. By combining human judgment with machine intelligence, HTM professionals can ensure that healthcare technology remains safe, reliable and ready to serve patients. The future of healthcare technology will be shaped not just by innovation alone, but by the vigilance and expertise of those who manage it – HTM professionals,” Kai says


“Of course, every opportunity comes with responsibility. For AI in HTM, the challenges are as important as the benefits,” he says.
Kai notes the following examples:
• Algorithm Bias: If training data lacks diversity, AI may misinterpret results for certain patient populations. For example, adult patient equipment data versus pediatric patient equipment data, or differences between hospital and home care environments.
• Transparency: Some AI models operate as “black boxes,” making it difficult to understand how decisions are reached.
• Validation: AI must be tested in each hospital’s environment, not just in a lab setting, to ensure reliability.
• Data Quality: “Garbage in, garbage out.” Poor service log documentation or inaccurate equipment validation trends can lead to misleading predictions.
Virnoche says that as his team starts to expand internally, they will work to leverage AI in their inventory management systems, allowing them to forecast parts needs based on historical parts usage for PMs.
“Longer term, I’d like to start using AI to grade supplier performance in terms of delivery, quality return rate, cost effectiveness, to create a mechanism to remove technician bias from parts orders. Best part at best value, regardless of vendor relationship. We’ll also explore using AI to streamline our PMs and ensure we have the right technician in the right place at the right time and maybe explore some technician escalation paths based on skill sets defined in our CMMS,” he says.
Virnoche says that finally, a big one for him is going to be contract management.
“Using AI to analyze contract performance metrics and help determine what the best coverage levels are based on historical need, current need, equipment age and any other detailed data we may find, all while determining whether it’s a better value to the organization to maintain the service contract or in-house items,” he says.
Ultimately, AI is a tool designed to augment human knowledge and abilities, ensuring that medical equipment remains functional, safe and ready when patients need it most, even as devices become more complex.
“AI is not a replacement for HTM expertise, it’s a partner. By combining human judgment with machine intelligence, HTM professionals can ensure that healthcare technology remains safe, reliable and ready to serve patients. The future of healthcare technology will be shaped not just by innovation alone, but by the vigilance and expertise of those who manage it – HTM professionals,” Kai says.
Cooksey says that the key to effective AI use is through improved prompting: to provide context, set clear expectations and validate outputs.
“AI is a powerful assistant, not a replacement for human expertise. When integrated securely (e.g., Microsoft Copilot for HIPAA compliance), it enhances quality, safety and operational performance across HTM,” he says.
If the Internet could be described as a “trend” in 1983, then AI could be described as a trend today. What wasn’t fully understood in 1983 is better understood today.
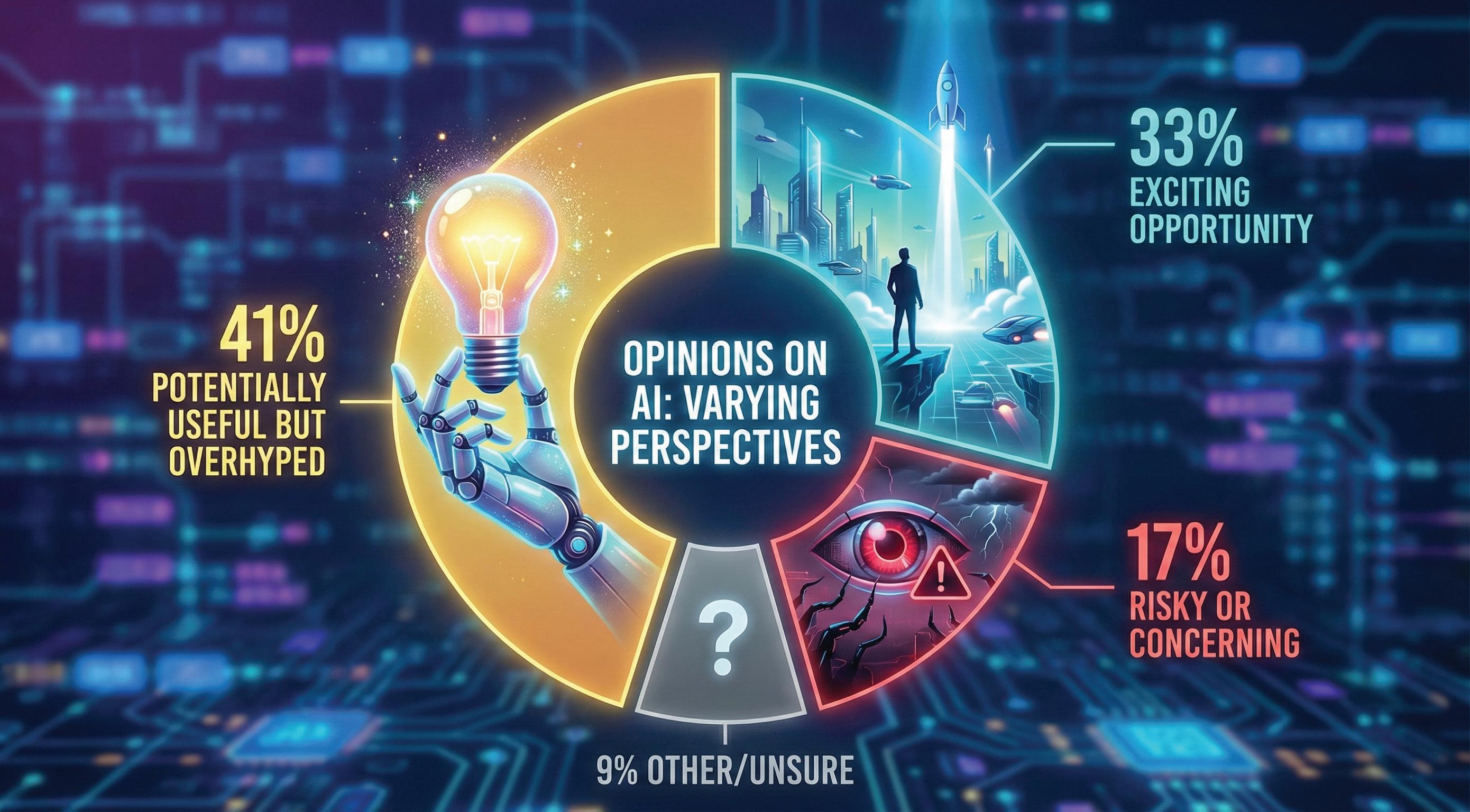
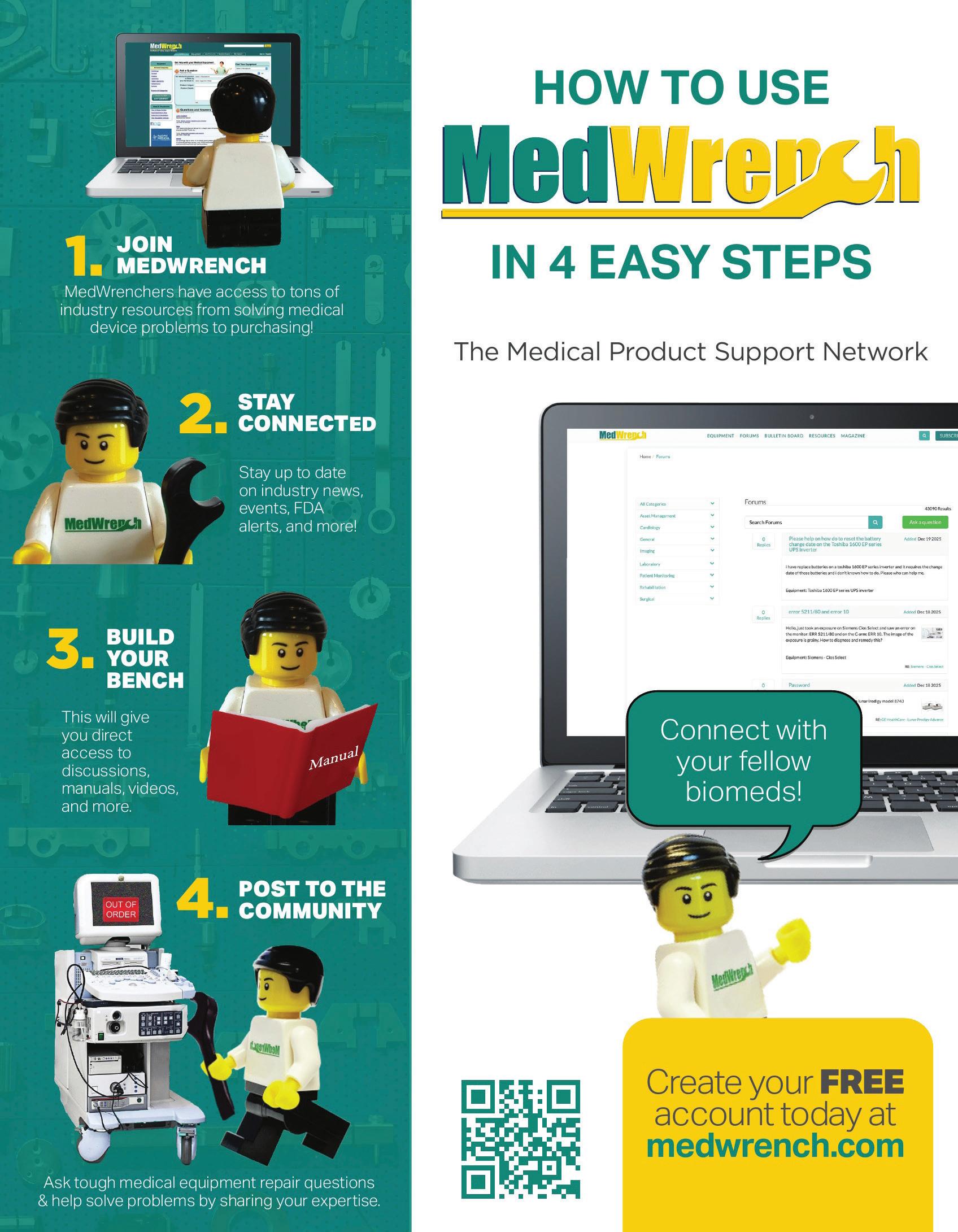

BY STEVEN J. YELTON, P.E., AAMIF
Iattribute much of the success of the HTM program at Cincinnati State Technical and Community College to the educational partnerships that have been developed over many years. These partnerships include employers, advisors, graduates and faculty from other educational institutions. In this installment of The Future, I want to share a somewhat different partnership that we have not traditionally had at the college. I hope that this provides you with some ideas for your institution whether you are at a hospital, company or college. We have found this to be quite valuable to our students and the college.
Over the years, our main employers in the cooperative education and internship area – as well as full time employment – have been hospitals. This could be working directly with the hospital or through a third-party partnership. Most of our students enter the program at Cincinnati State with the expectation of working for a hospital group. However, there are consistently more
students who are looking for employment in other areas for various reasons. Students may now be looking for employment that would enable them to relocate easily and, more recently, have been looking at other opportunities in the HTM area.
We have had a partnership with Elite Biomedical Solutions in Cincinnati, Ohio for several years now. This relationship offers our students opportunities that traditionally haven’t existed in the past.
Glenn Schneider of Elite Biomedical Solutions and I have worked together for many years in many different roles and most recently when he joined Elite. Glenn was a student of mine after he left the military. He went to work in the hospital world and quickly became a great resource for me at Cincinnati State. Glenn became an advisor, employer and eventually an adjunct professor.
Glenn and I have been team teaching the HTM courses at Cincinnati State for many years. We have a collaboration with area hospitals as well as Elite to provide training for our students on site. We offer classes within hospitals that provide access to equipment and medical systems that we
do not have on campus. The hospitals where we meet include Cincinnati Children’s Hospital and The Christ Hospital Health Network. This has been an extremely valuable resource to the college. This started many years ago when Glenn was a director at Cincinnati Children’s and Greg Herr was an advisor and adjunct professor at Cincinnati State and a director at The Christ Hospital. In addition to other individuals, hospitals and employers, Glenn and Greg have been valuable resources for the HTM program at Cincinnati State and its students.
Most recently, Elite has offered their resources to provide our students with exposure to an area of HTM that many of them had never thought about. Elite Biomedical Solutions not only is a manufacturing facility but also provides on-site service and repairs. They offer customers HTM services such as cleaning, adjustments, calibration, device service and repair, preventative maintenance and documentation of service. We feel that this provides our students with an opportunity to see the HTM field from another view as well as additional employment opportunities. Another offering Elite provides that would be worth mentioning is their educational training called “The Elite Edge.” It currently consists of three hands-on training sessions, Basics (four days), Philips Patient Monitoring (two days), and GE Patient Monitoring (two days). They are looking to expand into other manufacturer models. Each session consists of a classroom overview and hands-on disassembly, reassembly and testing on at least four devices. The basics include IV pumps and an introduction into telemetry. We have found this to be a great option for our students as well as graduates because we are not able to offer it at the college.
We have strived to provide a diverse educational experience, and our partnerships with a children’s hospital, adult hospitals, independent service organizations and biomedical companies is a huge benefit to our students. As part of our accreditation requirements, as well as a way of improving our program, we rely heavily on these relationships.
Cincinnati State’s HTM program requires students to complete two semesters of paid cooperative education assignments. As you can see, the partnerships that we have developed help everyone involved. The hospitals and companies that employ our cooperative education students are provided with productive employees and have access to available, carefully vetted full-time employees if needed. We could not have an HTM program of the current quality without the advisors and employers as well as the donations that our partners provide.
Steven J. Yelton, P.E., AAMIF, is a senior HTM consultant for Elite Biomedical Solutions in Cincinnati, Ohio and is a professor emeritus at Cincinnati State Technical and Community College where he teaches biomedical instrumentation (HTM) courses.


BY ANDREW WHYTE, CBET
If nothing else, I’m an expert in older medical equipment but maybe not an expert regarding equipment built before I was born. If you give me a broken first-generation M11 sterilizer, I’ll have that thing running like a champ in no time. Those units went out of support well over a decade ago, but we still have the manuals. We still have third-party part suppliers and, by gosh, we have customers who’ll never let them go. Today, I’d like to write about out-of-date equipment and the roll MedWrench fills with access to knowledge, documentation and the handy third-party service provider directory.
Medical facilities today face a problem. Equipment fleets are aging faster than organizations replace them. Budget constraints, long procurement processes and supplychain inconsistencies mean that biomedical technicians and independent service providers are often responsible for keeping devices operational well beyond their stated life cycle. End of life (EOL) letters mean little when you can’t buy the latest and greatest every few years. In this environment, practical tools and shared resources play an important role in supporting legacy devices.
MedWrench.com has become one of the few platforms that service professionals can use to locate technical documentation, and to draw on knowledge of other professionals around the world. It serves as a supplemental resource that can help prolong the use of dated medical equipment, especially when OEM information becomes difficult to access.
A primary challenge when working with older equipment is the gradual or abrupt loss of service information and knowledge. Manuals may be become unavailable, handwritten notes get photocopied too many times and OEM support often fades as products age. Some manufacturers cut support the moment an EOL letter is published. Many devices still have years of usable life, but technicians need accurate information to maintain them.
MedWrench’s library of manuals, service guides, and its archive of users’ questions in the forums provide a mountain of resources. Technicians, providers and, in some case even patients, regularly pop into the forums looking for the documentation that may be impossible to find elsewhere. By the way, obtaining and uploading documentation to the site is important – especially so for out date/end of life equipment. Also, if you have a manual that you don’t see on the site, share it! Having a
centralized place to look for manuals, passwords and advice is crucial for aging equipment.
For smaller clinical engineering teams or ISOs with limited internal documentation repositories, this type of shared archive can be a lifesaver, literally and figuratively.

Financial pressures continue to influence equipment management across healthcare. Smaller hospitals, rural facilities and outpatient centers often rely heavily on legacy systems because replacing them simply isn’t feasible in the short term.
Resources like MedWrench support these environments by helping service professionals identify parts, locate alternative suppliers and get documentation that is otherwise hidden behind paywalls on other sites. Accessing the forums is a great (and free) way to see if anybody else has had the same or similar issues as you. Sometimes having a knowledgeable person declare that repair is likely a lost cause can be the catalyst that drives an organization to finally replace a device. Don’t think of that as a failure, it’s being efficient.
None of these tools eliminate the challenges of outdated equipment or the need for careful risk assessment, but they give technicians additional data points to work with when budgets are tight.
Electronic waste remains a growing environmental concern, and medical equipment contributes significantly to the volume of materials exiting healthcare facilities and entering the e-waste stream each year. We’ve all probably seen the dumpster behind the hospital out by the loading bays. There’s also that big box on a pallet where the interns dump the electronic components they just took from a gutted device. That’s all e-waste. The “Reduce” in “Reduce, Reuse, Recycle” isn’t just first because it would sound weird otherwise. It’s because reduce saves the most money in the long run. Many devices are retired not because they are beyond repair, but because documentation or parts are no longer readily available. I’m looking at the OEMs that change the shape of consumables so we have to buy a new widget.
By helping technicians locate information and vendors that might otherwise be hard to find, MedWrench plays a role alongside refurbishers, parts suppliers and HTM professionals in extending the functional life of devices.
When older equipment can be repaired or safely maintained for additional years (or decades in some cases), facilities may delay disposal and reduce the environmental impact associated with premature retirement.
This aligns with broader sustainability goals many health systems have adopted. Though extending equipment life must always be balanced with clinical, regulatory and safety requirements.
Another practical function of MedWrench is the opportunity for technicians to share knowledge from years and years of experience. The forums where I regularly haunt allow users to ask questions, share troubleshooting insights or compare notes on equipment compatibility.
This type of peer-to-peer communication supports new and experienced technicians by providing access to a large pool of knowledge. I’ve enjoyed many back-andforth discussions with users and the other Gurus while working on issues only to learn something new. The collaborative environment helps technicians find common solutions to issues across many makes and models. Once this knowledge is shared it’s available forever and that benefits everyone.
As healthcare facilities continue to rely on aging equipment, access to shared knowledge and resources becomes increasingly important for clinical engineering and service teams. MedWrench.com functions as a practical supplemental tool that supports technicians with legacy devices, budget-restricted environments and long-term sustainability goals.
Its value lies not in replacing OEM guidance or model specific training, but in helping technicians locate information, understand equipment issues and collaborate with peers as they navigate maintaining older medical technology.

MedWrench Guru Andrew Whyte, CBET, is the owner and operator at Maple Tree Biomedical. He began his biomed career in the U.S. military and has more than a decade of HTM experience.

BY ERIC MASSEY
In HTM, we’re trained to diagnose equipment, not emotions. We solve problems with logic, data and technical precision. The moment you step into leadership, the work changes. You’re no longer repairing devices, you’re influencing people. And in that world, emotional intelligence (EQ) becomes the single most important predictor of leadership effectiveness.
Technical mastery may get someone promoted. Emotional mastery determines whether they succeed.
Most operational failures I’ve seen over the years weren’t because of technical incompetence. They came from breakdowns in communication, mismanaged emotions during pressure moments or leaders who couldn’t read the signals their teams were sending until it was too late.
EQ isn’t a “soft skill.” It’s a performance skill. And in HTM, where every decision touches patient care, it is a strategic advantage.
The most dangerous moment in leadership is not when something goes wrong, it’s when you don’t realize you are contributing to it.
Self-awareness means knowing:
• How you show up under pressure
• What triggers you
• How your tone shifts when stressed
• What your team sees but doesn’t say
One director I worked with had outstanding technical instincts but struggled with reactive communication. When something went wrong, he jumped straight to an intense tight voice, clipped instructions, escalated urgency. He thought he was “driving accountability.” His team perceived it as anger.
When he became aware of that pattern, everything changed. His communication softened. His team stepped up. His compliance numbers improved. His turnover dropped. Self-awareness doesn’t make you less decisive. It makes you more trusted.
If you want lasting influence in HTM, build your emotional intelligence with the same rigor you once built your technical skills.
HTM leadership is filled with pressure moments, OR calls, administrator escalations, equipment outages, regulatory reviews and end-of-month performance expectations.
EQ shows up in how you respond before you speak. A leader with low EQ reacts emotionally and immediately. A leader with high EQ regulates, pauses and chooses the right response.
Here is a simple discipline used by top performers:
1. Stop for two seconds.
2. Breathe once, slowly.
3. Shift tone intentionally before speaking.
4. Communicate with clarity, not force.
This isn’t theory. It is operational advantage. Teams follow steady leaders more than intense ones. When you control your emotional temperature, you instantly elevate the performance of the people around you.
Empathy is not softness, it’s situational awareness.
Technicians, nurses and administrators operate in completely different pressure environments. When a clinician sounds frustrated, it’s rarely about the device; it’s about the patient behind the device. When a tech seems disengaged, it’s rarely lack of care, it’s often lack of clarity, overwhelm or burnout.
True empathy sounds like:
• “Tell me what you’re experiencing on your end.”
• “Walk me through what’s creating the pressure for you right now.”
• “Help me understand what success looks like from your perspective.”
Empathy builds bridges faster than authority ever will. When people feel understood, they become more collaborative, more respectful and more solution oriented.
Influence doesn’t come from your title; it comes from your presence.
High-EQ leaders build trust through:
• Predictable communication
• Consistent follow-through
• Coaching over correcting
• Clear expectations
• Recognizing small wins
• Protecting morning block time and honoring it
One leader I coached implemented a simple practice: every Thursday afternoon, he sent five short notes of
recognition to his team. Not for big achievements but for effort, growth and consistency.
The impact was immediate:
• Engagement went up
• Rework went down
• His team became more proactive
• Difficult conversations became easier
When relationships are strong, performance accelerates. When relationships are weak, even basic tasks become friction filled.
Great leaders see issues before they surface.
They recognize:
• When a technician is nearing burnout
• When a hospital partner is quietly frustrated
• When a system change is causing confusion
• When competing priorities are overwhelming the team
In HTM, problems rarely appear suddenly. They build in the background. High-EQ leaders detect them early because they pay attention to emotional patterns, shifts in behavior and subtle cues others dismiss. This skill prevents escalations, reduces turnover and strengthens partnerships. It is one of the most overlooked forms of intelligence in our industry.
Emotional intelligence (EQ) separates leaders who manage from leaders who inspire.
It turns conflict into collaboration, burnout into alignment and pressure into clarity.
In a field defined by technology, it is still people who determine performance.
The leaders who will define the future of HTM aren’t the ones with the deepest technical credentials; they’re the ones who understand themselves, understand their teams and lead with disciplined emotional awareness.
If you want lasting influence in HTM, build your emotional intelligence with the same rigor you once built your technical skills.
That is the leadership advantage of the next decade.

Eric Massey is the regional director of operations with Intelas and founder of The Massey Method.
BY GARRETT SEELEY
Serial Digital Interface, or SDI, is a high-definition (HD) video connection that originated in the professional television video camera industry. It is widely used for video devices, including gastrointestinal (GI) and surgical video systems, because of its superior image quality and extended transmission distance. Since it comes from the television broadcast industry, this standard is made for high resolution and multiple devices into a standard mixing or control board. It is one directional in nature but can use two conductors for bidirectional control.
SDI operates on a dedicated unidirectional digital line using 75-ohm coaxial cabling, like the cabling used in a 10Base5 network. The video transmitted through SDI is digital, uncompressed and unencrypted. In a classic SDI video system, the camera output is sent directly to a mixing board, which acts as a receiver for processing the video output stream. Data rates can exceed 12 Gbps in full HD video range. Typically, several cameras are connected to a professional grade mixing board, which selects the appropriate camera feed for main output.
There is no control required because a camera operator is on the other end, with a headset for communication. This is how a TV setup works at a large, live event, such as a football game.
Modern SDI systems can incorporate computergenerated effects, such as multi-screen or picture-inpicture options. USB connections facilitate timing for capture, processing and storage, enabling full digital storage and editing of the output. This setup is often used by modern online video streamers to integrate multiple cameras into one output. A popular manufacturer of this equipment is Blackmagic, and the mixing boards are known as ATEM Control Panels, although they are also referred to as mix boards or switchers.
CABLING
SDI cabling can be converted to various formats, including HDMI, DVI, Coaxial BNC connectors or Fiber links. The unidirectional nature of the SDI signal means that two coaxial cables or two fiber optic cables are necessary for longer-range controlled connections. BNC connectors are the most used in medical applications, with one input line and another separate output line needed for bidirectional communication, often referred to as Dual Link HD-SDI.
In gastrointestinal video applications, such as endoscopy
towers, the endoscopy camera is controlled directly by a Camera Controller, which serves as the image source. The Camera Controller typically has a separate control line, often marked as Y/C, that is distinct from the video signal. This line refers to the two data streams in the Dual Link HD-SDI protocol, enabling bidirectional connections between system components. The SDI video signal can be an SDI BNC connection or an RGB connection that runs through an SDI converter. From the image source, the output BNC connects to the input BNC at the destination. It’s important to note that this video signal is typically one output to one input without using a splitter, converter or duplicator.
In radiology applications, such as room camera systems, most cameras are unidirectional and do not require a control SDI cable. These cameras’ BNC output lines connect to the control panel’s BNC input. For long distances, a fiber converter can be used. If controllable devices are involved, input and output cables run between the control panel and the device. A fiber optic patch cable can be adapted for long, bidirectional digital runs. For systems with multiple devices, the control panel often connects to a converter that functions as a hub, managing communication with each device, which is typically assigned to a control ID using setup software.
SDI communication standards offer a fast, fully digital HD video solution for medical applications. It provides longevity to the older BNC ThickNet cabling, which was always designed to maximize range. SDI communication surpasses HDMI or DVI in capability for these specialized applications, exceeding the typical 50-foot range of home use HD cabling. This is the primary takeaway, that of range and a native dataflow of one direction. Since the HD SDI standard is unidirectional, requiring two connections for bidirectional communication. Be careful to hook it up with an input receiving from an output. The ports are ideally labeled, and the OEM documentation should be consulted as the ultimate guide. Also remember that although BNC connectors are the preferred choice in medical systems, manufacturers may use other connections for proprietary applications. Let’s just say that the documentation is of key importance in SDI setups.

Garrett Seeley is a Biomedical Equipment Support SpecialistImaging with VISN 17: VA North Texas Health Care System, U.S. Department of Veterans Affairs.

BY NADIA ELKAISSI, CHTM
Picture this: During a procurement review, a vendor states that their product is “FIPS compliant.” When asked for details, they are unable to immediately provide a certificate number or clarify whether the cryptographic module is validated under FIPS 140-2 or FIPS 140-3. This is often the moment when teams realize why understanding FIPS matters before moving forward.
If you are new to cybersecurity, have no fear! You do not need to understand cryptography in order to understand FIPS. FIPS exists so organizations do not have to rely on guesswork or deep technical expertise to trust that encryption is being implemented safely.
FIPS stands for Federal Information Processing Standards. These standards are developed by the National Institute of Standards and Technology (NIST), a U.S. government standard organization. FIPS provides
guidance on how sensitive information, especially data used by the federal government, must be protected. While there are multiple FIPS standards, one of the most referenced in cybersecurity, is FIPS 140, which focuses specifically on encryption.
Encryption is a foundational security control. If it is implemented incorrectly, other security measures may not matter. FIPS validation helps ensure that only approved and well-tested cryptographic methods are used and that encryption keys are generated, stored and handled securely. For U.S. federal agencies, FIPS compliance is mandatory. For healthcare organizations, financial services, cloud providers, and government contractors, FIPS is often required by contracts, audits, or regulatory expectations. In practice, FIPS serves as a trusted baseline for cryptographic security.
FIPS 140 focuses on cryptographic modules, which are the parts of software or hardware responsible for
performing encryption-related functions. Encryption is the process of turning readable data into unreadable data unless the correct key is used. These cryptographic modules handle tasks such as: encrypting and decrypting data; creating and protecting encryption keys; authenticating data; detecting and responding to cryptographic failures. It is important to note that FIPS 140 does not evaluate the entire product. Instead, it ensures that the encryption component itself meets well-defined security requirements.
There are two versions of FIPS 140 that are commonly referenced today, FIPS 140-2 and FIPS 140-3. FIPS 140-2 was published in 2001 and became widely deployed and established. It is still present in many existing environments, but it is no longer approved for new validations. FIPS 140-3, published in 2019, is based on modern international security standards and is better suited for today’s technologies, including cloud and virtualized environments. New FIPS 140-2 validation ended in 2021. While existing FIPS 140-2 validated modules may remain in use until their certificates expire, FIPS 140-3 is the standard moving forward.
As a general rule, FIPS 140-3 should be required for new investments to include: new hardware or software procurements; cloud-based or virtualized systems; systems expected to remain in service for many years; and environments that may support government or regulated data in the future. Requiring the current standard helps avoid compliance and life cycle challenges later. FIPS 140-2 may still be acceptable in limited situations such as if it supports legacy environments or it is maintaining existing or previously approved systems. In these cases, organizations should treat FIPS 140-2 as a transitional solution and ensure there is a document plan to move toward FIPS 140-3.
TIPS WHEN EVALUATING FIPS CLAIMS
If you are new to FIPS, vendor FIPS claims can be confusing. The tips below can help cut through marketing language and focus on verifiable facts.
1. Always ask for proof
Request the NIST CMVP certificate and verify that the
certificate is in the NIST CMVP database. While brochures or marketing materials may reference FIPS, they should never replace independent verification.
2. “Compliant” is not the same as “Validated”
The term “FIPS compliant” is not the same as “FIPS validated.” FIPS validation means the cryptographic module has been tested and approved by NIST. Only validated modules meet FIPS requirements.
3. Confirm What is Actually Validated
Vendors may claim their product is FIPS validated, but it’s important to identify which cryptographic module is validated. Ensure the specific module in use – not just the product name – has validation. Request an SBOM or vendor attestation confirming the validated module is in use.
4. Check Certificate Status
Even if a certificate exists, verify its current status. Some FIPS 140-2 certificates are now listed as “historical.”
Historical certificates are typically acceptable only for existing deployments and are not appropriate for new procurements.
5. Require a Transition plan
If you are purchasing a product that currently relies on FIPS 140-2, consider future requirements. Request a roadmap for FIPS 140-3 validation, including expected timelines, and discuss plans for upgrades or recertification.
Now let’s recap. FIPS validation ensures encryption is implemented correctly and independently tested. FIPS 140-3 is the current and future standard, while FIPS 140-2 remains acceptable only in limited transition scenarios. Procurement decisions should be based on validation status, not marketing language. In short, FIPS enables organizations to trust encryption without needing to be cryptography experts – as long as the validation is real and current.

Nadia ElKaissi, CHTM, is a biomedical engineer in healthcare technology management with the VA Central Office (19HTM).



BY NATHAN PROCTOR
The U.S. military is the most powerful defense force in the world, but just like average Americans, service members can’t fix the equipment they rely on every day.
Right to repair is the simple idea that if you own it, you should be able to fix it. And right now, even the military doesn’t have the right to repair its own equipment and systems. All too often defense contractors block military personnel from accessing the tools, parts and information they need to repair equipment, resulting in escalating costs for the taxpayer, reduced readiness for the forces, and lives at risk for the men and women in uniform.
Over the past year, military Right to Repair has gained significant momentum. After the Army announced it would prioritize getting repair access as part of its ongoing procurement, bipartisan legislation was filed in the House and Senate to require Right to Repair access. This proposal ended up incorporated into the National Defense Authorization Act (NDAA), the legislation which funds the U.S. military. Both the U.S. House and Senate passed versions of the NDAA with Right to Repair included. These provisions had strong support outside of Congress. The Trump administration, in addition to the Secretaries of the Army, Navy, and Air Force, have all expressed support for military Right to Repair.
But major defense contractors are waging an intense lobbying push to strip these provisions from the bill and prevent the military from having the right to repair. We found out in December that Congressional leadership has removed bipartisan military Right to Repair provisions from the FY26 NDAA.
The change happened at the very end of the process, in the least accountable and open part of the negotiations, when just a handful of Congressional leaders hammered out the final text.
Just as Right to Repair for the military earned bipartisan support, removing it caused bipartisan outrage. Sens. Elizabeth Warren (D-Mass.) and Tim Sheehy (R-Mont.) issued this joint statement:
“For decades, the Pentagon has relied on a broken acquisition system that is routinely defended by career bureaucrats and corporate interests … We support the Pentagon using the full extent of its existing authorities to insist on right to repair protections when it purchases equipment from contractors, and we will keep fighting for a common-sense, bipartisan law to address this unnecessary problem.”
As the statement indicates, while the NDAA language has been settled, Congress can still pass separate legislation to enshrine military Right to Repair, and it appears Sens. Warren and Sheehy will pursue this. The battle isn’t over.

Nathan Proctor is senior director of the U.S. PIRG Campaign for the Right to Repair.

Empowering BioMed Teams with Real-Time Location Intelligence
• InVIEW Asset Management: Locate critical assets instantly
• Environmental Monitoring: Temperature monitoring in real-time
• Hand Hygiene: Automated compliance 24/7

The words can appear horizontally, vertically, diagonally, and may be spelled forwards or backwards.
Jonathan Hatley
CBET, Technical Manager, Biomedical Services, McLeod Health
• Laptop - without it I would be up the creek without a paddle for my job
• Fidget spinner - because I fidget when on meetings
• 1,000 sticky notes (some with random numbers on them)
• Phone for music - when I am working in the database running reports or making spreadsheets
• Small ECG simulator, spo2 simulator, multi meter
• Drink - because I get thirsty
Submit your bench to be featured in TechNation at 1technation.com/my-bench/. You could win a $25 Amazon gift card via the “What’s On Your Bench” Contest!
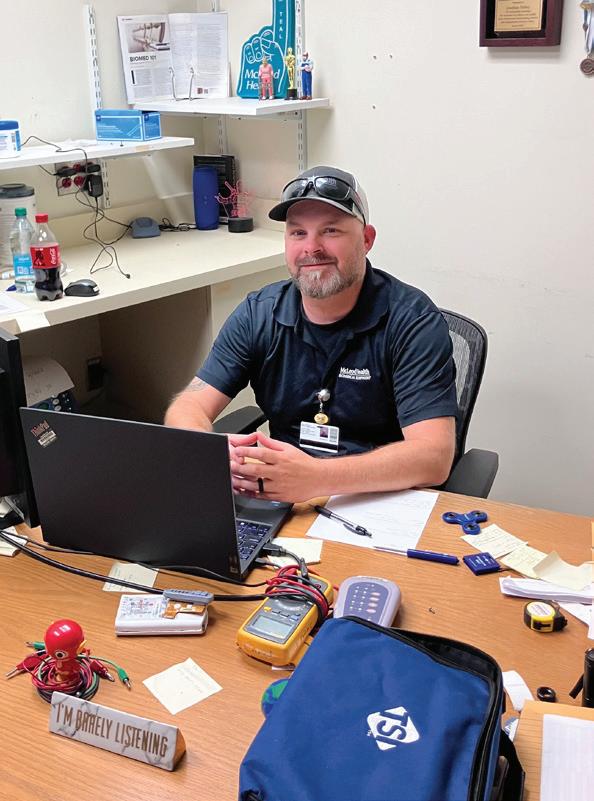
The 2025 Florida Biomedical Society Symposium concluded Dec. 7 at Disney’s Beach Club Resort in Lake Buena Vista with high marks from attendees, exhibitors and industry partners. The annual FBS Symposium, held Dec. 4–7, drew biomedical professionals from across the country for four days of education, networking and product demonstrations focused on the management and care of medical technology. The event featured a robust schedule of technical sessions, hands-on workshops and peer-to-peer learning designed to support quality patient care and efficient clinical engineering practices. Vendors showcased the latest technologies. In addition to core programming, social events like the FBS golf outing offered further opportunities for connection among professionals dedicated to advancing biomedical technology management. Organizers reported strong participation and expressed optimism about continued growth in 2026.
MD Expo returns to Florida this year with support from FBS. The MD Expo Orlando is set for October 13-15. Find out more at MDExpoShow.com.


1 3 4 2
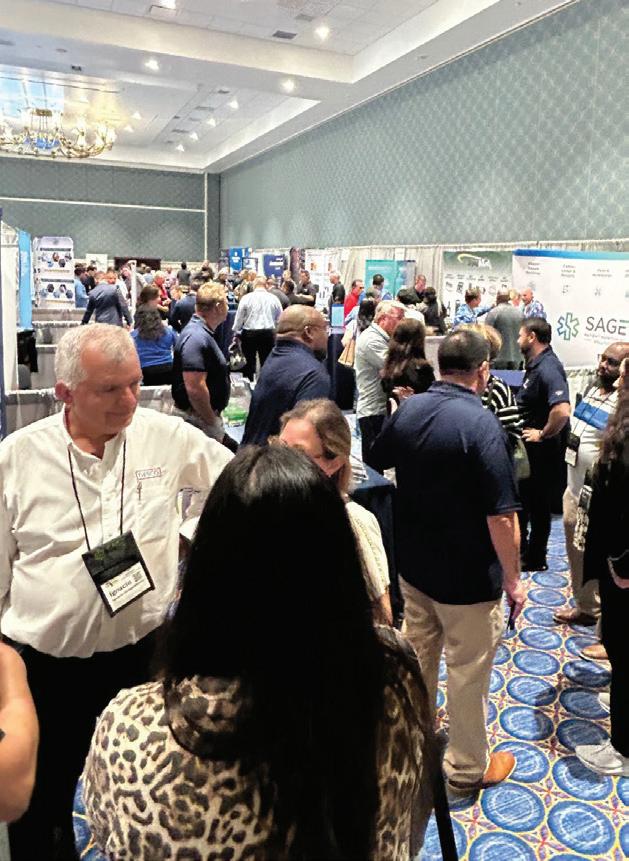

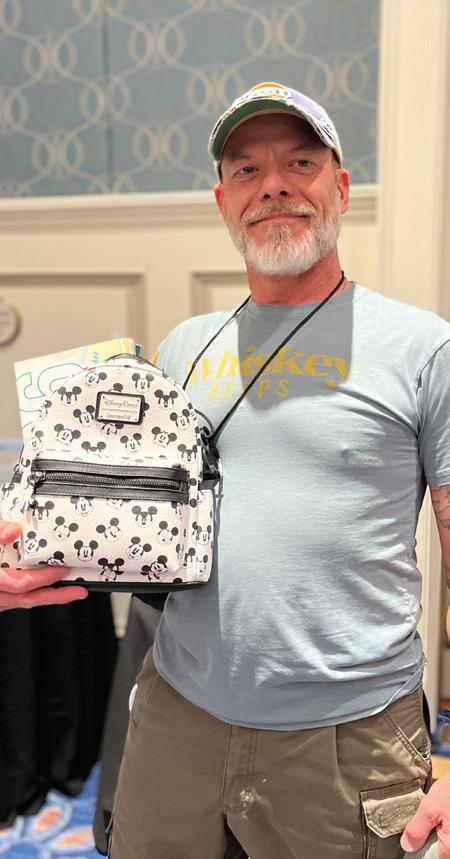
5
1. Integrity Biomedical owner Michele Shahbandeh accepting the FBS Presidential Award, honoring Integrity’s continued support, leadership, and dedication to advancing the HTM industry.
2. Vendors were welcomed at a special harborside reception, offering an alfresco setting to connect, network, and enjoy the evening.
3. The exhibit hall was buzzing with energy as attendees explored more than 40 vendor booths.
4. Sunny skies and 70-degree temperatures in Orlando this December made for an exceptional golf event.
5. MedWrench was excited to award a Mickey Mouse Loungefly bag and matching water bottle to one lucky attendee during the door prize drawing.


6. Set against the charm of Disney’s Beach Club Resort, this year’s symposium was truly magical.
7. Exhibit hall smiles from Kristin Leavoy and Jayme McKelvey of the TechNation team.
8. Education took center stage, delivering continuing education credits and important updates across the HTM industry.
9. John WallaceJohn I do not know what this photo is depicting. Please reach out to Amy Hobbs to ask.
10. A powerhouse lineup. Pictured are industry leaders Bryant Hawkins, Sr., Rana Helou, and Kim Rowland. 6 8 9 7 10




HTMA-NTX hosted its second annual Sparky Awards on December 4 at the Hilton Arlington, bringing together HTM professionals, vendors and partners from across North Texas for an evening of red-carpet celebration. Sponsored for the second consecutive year by PartsSource, the event honored the standout contributors who helped propel the association through another milestone year. The night blended recognition with purpose, as attendees donated toys for Children’s Health and Cook Children’s, continuing a cherished holiday tradition. A memorable moment came when iServe Biomedical announced a donation to the Ohm’s Law Foundation, supporting scholarships and professional development for future biomeds.
• Collaborator of the Year: Jake Powell, iMed Biomedical
• Innovator of the Year: Chace Torres, CBET, CHTM
• Rising Star: Matthew Abad, Collin College
1. The HTMA-NTX 2026 Sparky Award Winners pictured (from left to right) are Collaborator of the Year Jake Powell from iMed Biomedical, Lifetime Achievement winner David Braeutigam, Innovator of the Year Chace Torres, Rising Star Matthew Abad, Department of the Year representative Guillermo Diaz from Children’s Plano, MVP Andrea Brainard from Children’s Health, and Sponsor of the Year representative Elizabeth Kudla from PartsSource.
2. PartsSource is the HTMA-NTX Sponsor of the Year. Pictured (from left to right) are HTMA-NTX Vice President Josh Virnoche and PartsSource representatives Elizabeth Kudla, Sydney Humes, Webb Clark and Greg Goree.
3. iServe presents a donation to Ohm’s Law. Pictured (from left to right) are Ohm’s Law Foundation Founder Chace Torres, Jake Powell from iMed Biomedical, Javier Valdez from iServe
• MVP: Andrea Brainard, CBET, CHTM
• Sponsor of the Year: PartsSource Inc.
• Department of the Year: Children’s Health Plano
• Lifetime Achievement: David Braeutigam
Biomedical, Savannah Valdez from iServe Biomedical and Sydney Humes from PartsSource.
4. Rising Star Award winner Matthew Abad (center) is pictured with UT Southwestern’s Jamal Guio (left) and Collin College’s Daniel Irving.
5. MVP Award winner Andrea Brainard, from Children’s Health, is pictured with HTMA-NTX President Webb Clark.
6. iMed’s Jake Powell was presented with the Collaborator of the Year Award. iMed team members include (from left to right) Wendy Solis, Jake Powell, and Morgan Acquafredda.
7. HTMA-NTX members Andrew Mckelroy, Jamal Guio, Ryan Hobley, Damion Mackenzie, Caleb Rogers, Tim Wicker and Jai Patel enjoy of evening of celebration.







FEBRUARY 4
SPONSORED BY

TOOLS OF THE TRADE
Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.
FEBRUARY 11

ROUNDTABLE WEBINAR RTLS

All webinars, podcast, and product demos are eligible for 1 CE credit from the ACI.
SPONSORED BY

TOOLS OF THE TRADE Ultrasound Probes In-Depth: Use, Care, and Repair

ROUNDTABLE ON PATIENT MONITORS
SPONSORED BY

PATCH ME IF YOU CAN Shared Responsibility in Medical Device Cybersecurity

From social media to the pages of TechNation. Tag us to be featured in The Social. #technation


“But if you ask a Biomedical Engineer (BME) working in a hospital to check the helium level in an MRI, he might respond,
‘I’ve just finished replacing the ABG machine’s reference electrode and completing its calibration. On my way, I’ll take a quick look at the chemistry analyzer, then head to the ICU to replace the ventilator’s oxygen sensor—after that, I’ll check the MRI helium level.’
Yes, Biomedical Engineers working in hospitals are truly versatile. They know everything needed to keep the entire system running smoothly.”
“Fun Friday Fix on a Penlon dinosaur! These things just keep going! Stay safe out there, LinkedIn!”

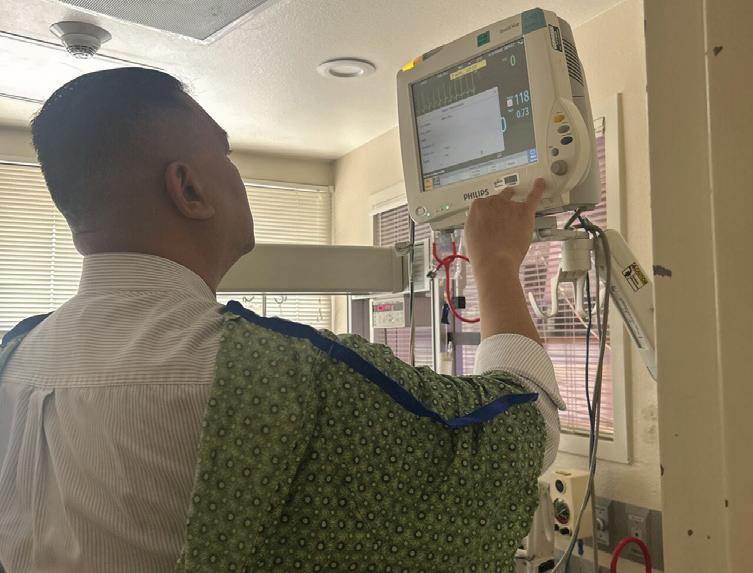
“Just some “In-Action!” shots of some of the work and learning my team and I have been able to tackle! Again can’t thank HERO Business Inc enough along with Mr. John for spreading your knowledge and allowing me to develop!”


“Not every issue is what it seems on the surface. Sometimes it could have been easy — but in our field, it’s all about taking things one step at a time, following the evidence, and getting the equipment back to the clinical team safely and reliably.
@ Belinda Rosas

This is the part of HTM where persistence, curiosity, and process really shine.”
Admar
J2S
J2S
Pronk Technologies, Inc. pronktech.com
Innovatus Imaging innovatusimaging.com
International X-Ray Brokers internationalxraybrokers.com
Metropolis International, LLC Metropolismedical.com • 718-371-6026
Admar Neuro admarneuro.com • 728-900-3969
Diagnostic Solutions diagnostic-solutions.com • 330-296-9729
International X-Ray Brokers internationalxraybrokers.com
508-559-9441
Inc.
Oxygen Blender
Patient Monitors
• 888-587-6759
Group International, Inc BCGroupStore.com • 314-638-3800
Befour, Inc. befour.com • 800-367-7109
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Southeastern Biomedical, Inc sebiomedical.com/ • 828-396-6010
Tenacore LLC tenacore.com • 800-297-2241
USOC Medical usocmedical.com • 855-888-8762
Refurbish
Admar Neuro admarneuro.com • 728-900-3969
AMX Solutions
www.amxsolutionsinc.com • 866-630-2697 85
General Anesthetic Services generalanestheticservices.com • 800-717-5955 7
Innovatus Imaging innovatusimaging.com • 844-687-5100 8
Rental/Leasing
General Anesthetic Services generalanestheticservices.com • 800-717-5955 7
J2S Medical
www.j2smedical.com • 844-342-5527 86
Admar Neuro admarneuro.com • 728-900-3969 85 P P AIV
P P
aiv-inc.com • 888-587-6759
AMX Solutions
www.amxsolutionsinc.com • 866-630-2697 85
BC Group International, Inc BCGroupStore.com • 314-638-3800 85,88
CM Parts Plus cmpartsplus.com • 877-267-2784
General Anesthetic Services generalanestheticservices.com • 800-717-5955 7
Innovatus Imaging innovatusimaging.com • 844-687-5100 8
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441 23
PM Biomedical pmbiomedical.com • 800-777-6474 61,86 P P
Rytex Industries rytexindustries.com • 727-557-7450 84
Tenacore LLC tenacore.com • 800-297-2241
aiv-inc.com • 888-587-6759
Diagnostic Solutions diagnostic-solutions.com • 330-296-9729
General Anesthetic Services generalanestheticservices.com • 800-717-5955 7
J2S Medical
www.j2smedical.com • 844-342-5527 86
PartsSource, Inc. partssource.com • 877-497-6412




Solutions is a customer service based parts provider that specializes in all imaging modalities and manufacturers. Created to offer hospitals and ISO’s a cost effective and time saving solution for ordering imaging replacement parts, equipment moves, ultrasound probe repair and on-site service.
Admar Neuro admarneuro.com • 728-900-3969
AMX Solutions amxsolutionsinc.com • 866-630-2697
BC Group bcgroupstore.com.com • 314-638-3800
Befour befour.com • 800-367-7109
Interlight interlightus.com • 800-743-0005
J2S Medical j2smedical.com • 844.DIAL.J2S
Metropolis International metropolismedical.com • 718-371-6026
OHMS Law Foundation ohmslawfoundation.org
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Rytex Industries rytexindustries.com • 727-557-7450




chacetorres@ohmslawfoundation.org
ohmslawfoundation.org/foundationpartners















P
P Complete control + data capture
P Run user-defined / manufacturers’ checklists
P Generates a complete electronic test report
P Faster testing of Defibs/AEDs/Ventilator & Anesthesia Systems










Ready for a borescope that offers partnership in every pixel?
Scan to get started.
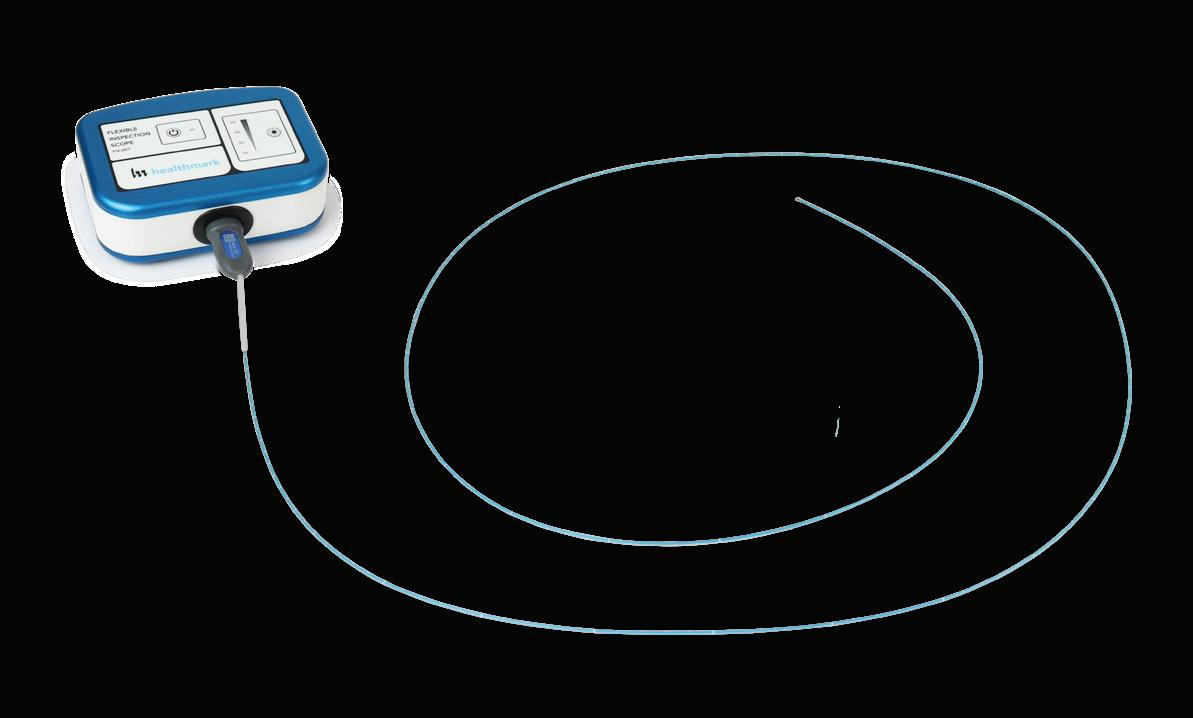
From capturing detailed lumen images to building complete inspection workflows, Healthmark stands with you every step of the way. The Flexible Inspection Scope pairs precision optics with a full network of support—including a team that customizes implementation and training to ensure your success. Because when it comes to borescopes, it’s more than pixels that matter—it’s partnership.