
















ASRT
The RAD Dash 5K Run/ Walk in Albuquerque, New Mexico, promotes a sense of community and family among colleagues.
COVER STORY
Imaging professionals see a future driven by a focus on automated processes, be they in image acquisition and refinement or software-assisted decision-making.


RISING STAR
AdventHealth Medical Group Practice
Administrator Ayeska Rosario hopes to serve on a larger scale.
FEBRUARY 2026


Catch up on the latest news from around the diagnostic imaging world.


New technology and a rising demand power the X-ray market. X-ray continues to incoprorate new technology asseen in these devices.
Leaders define the tone for their teams. The energy they bring and the consistency they model impact everything from employee engagement to patient experience to operational success.
MD
1155 Senoia
Phone:
President
John M. Krieg
john@mdpublishing.com
Vice President
Kristin Leavoy kristin@mdpublishing.com
Vice President of Business Development
Jayme McKelvey jayme@mdpublishing.com
Senior Account Manager
Megan Cabot megan@mdpublishing.com
Editorial John
Editorial
Beth
David
Kimberly
Megan
Dean
Art
Karlee
Taylor
Kristin
Webinars
Digital
Accounting

Let's meet at booth 203 at the Imaging Conference and Expo Feb. 20 - 22



AdventHealth Medical Group Practice Administrator Ayeska Rosario hopes to expand her leadership and influence over the next five years.
AdventHealth Medical Group Practice Administrator Ayeska Rosario is thriving in her career. Jason Theadore, vice president radiology operations with AdventHealth Florida Specialty Network and chief operating officer of ambulatory services for the AdventHealth Central Florida Division, nominated Ayeska as a Rising Star in the imaging realm. She recently shared more information about herself and her goals for the future in a Q&A with ICE Magazine.
Q: WHERE DID YOU GROW UP?
A: I grew up in New York.
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION? WHAT DEGREES/CERTIFICATIONS DO YOU HAVE?
A: I do not hold any imaging certifications; however, I bring a strong academic foundation and leadership experience to the field. I earned a Bachelor of Science in Health Services Administration from the University of Central Florida and a Master of Science in Health Services Administration from Grand Canyon University. My expertise lies in operational leadership, team development, and process improvement, which have
been instrumental in supporting imaging services and driving organizational success.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I was recommended for an opportunity back in 2021. At the time, I didn’t know much about imaging, but it quickly became a passion of mine. I don’t believe in coincidences – I truly believe God had a plan for me, and this role has allowed me to grow and make a meaningful impact.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: What motivates me most is knowing I’m making a difference – seeing my team grow and work toward becoming the best version of themselves. I love witnessing the results of the work we do together and knowing that everything we accomplish ultimately serves our patients, even if indirectly.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: I truly value working with such a dynamic group. I love that, despite our differences, we always find common ground in our shared commitment to the community and population we serve.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: Imaging is like no other field. I’ve worked in several specialties, and nothing compares to the complexity of radiology. From our rapid growth to the fast-paced environment, I truly enjoy collaborating with such talented radiologists, team members, and administrative leaders. Seeing everyone’s passion and compassion come together to innovate and elevate the care we provide is inspiring.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishment so far has been leading a complete team transformation – restructuring roles and workflows while cleaning up and streamlining our onboarding and credentialing process. This not only improved efficiency but also enhanced the experience for both our team and the physicians we support.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: Over the next five years, my goal is to continue working on becoming the best version of myself. I want to keep serving those God has entrusted to my care – from my children to my team members – while growing my skills and using them to make a greater impact on the community. Ultimately, I hope to expand my influence and leadership to reach and serve on a larger scale. •
FAVORITE HOBBY:
Spending time with my family, traveling, dancing, running, reading and volunteering
FAVORITE SHOW: “Grey’s Anatomy”
FAVORITE FOOD: Asian cuisine
FAVORITE VACATION SPOT: North Carolina
1 THING ON YOUR BUCKET LIST: I would love to create a traveling Christmas tradition.
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU:
I serve as vice president of my daughter’s middle school PTSA and also partner with my middle child’s elementary school PTA to support in any way I can. One of my interests has been creating partnerships with local businesses to support schools and vice versa – one example is a partnership between AdventHealth and the schools.

Baylor Scott and White Health All Saints Fort Worth Radiology Director Sarah M. Franks, BSRS, RT (R) (CT) (ARRT), CRA, was led to a career in healthcare when her father was diagnosed with cancer.
“He spent a significant amount of time in the hospital undergoing tests and treatments, and he always spoke highly of the compassionate care he received,” Sarah recalls. “That experience left a lasting impression on me. I knew I wanted to pursue a career in healthcare, but I also recognized that I become emotionally invested in patients. Radiology became the perfect fit – it allows me to contribute meaningfully to patient care while maintaining the professional boundaries I need to thrive.”
It is a career and environment in which Sarah thrives. She leaned into her role within healthcare during the COVID-19 pandemic and counts her service during that time as a highlight.
“During the COVID-19 pandemic, I led a high-impact collaboration with a major university in Fort Worth to provide cardiac MRI exams for student-athletes who had previously tested positive for COVID-19,”
Sarah shares. “These exams were critical for detecting myocarditis – a potentially life-threatening condition – and ensuring athletes were medically cleared to safely return to play.”
“I personally coordinated with university physicians to design and implement a streamlined initiative,” she explains. “Despite operating with only one MRI scanner, our team completed 130 cardiac MRI exams in just 32 days. We operated around the clock, delivering finalized radiology reports within 24 hours to support timely clinical decisions. This initiative not only safeguarded the health of student-athletes but also generated nearly $1 million in additional revenue in just over a month – demonstrating both clinical excellence and operational efficiency under extraordinary circumstances.”
The COVID-19 pandemic was a stressful time, but it also provided a reminder to Sarah regarding one of the reasons she enjoys her role as a professional in an imaging department.
“I love the collaboration, the opportunity to impact patient care, and the constant evolution of the field,” Sarah says. “Radiology is an exciting space where AI and emerging technologies are continuously improving outcomes and reducing human error.”
As a leader, Sarah sees herself as a member of the team. Everyone works together for a common goal.
“I consider myself a servant leader. My goal is to support and empower others, fostering growth and autonomy. I provide clear guiderails, offer consistent support, and focus on developing my team so they can thrive independently and confidently,” she says.
“My first unofficial mentor was a theologist and leader at a company I worked for in my early twenties. He took the time to talk with me about my goals and interests, then guided me on how to achieve them,” Sarah shares. “He played a pivotal role in helping me climb the career ladder and introduced me to other leaders who helped build my confidence.”
“Today, I firmly believe that mentorship is valuable at every stage of life,” she adds. “I do mentor others in the imaging field and find it incredibly rewarding to help others grow both professionally and personally.”
Sarah has her eyes on the horizon when it comes to what’s next in imaging.
“The future of imaging lies in AI-assisted tools that enhance diagnostic accuracy and efficiency. These innovations will help reduce variability and improve consistency in results, ultimately elevating patient care,” Sarah says.
Away from work, Sarah enjoys spending time with her large extended family, especially her grandchild.
“Family is everything to me. I’ve been happily married to my husband, Kenny, for 23 years. We have three grown children and one grandchild. I come from a large family – I’m the youngest of 12 siblings. Being the caboose, I like to say I learned from the mistakes of the other 11! If you ask them, though, they’d probably say I was the spoiled one,” she shares. •
BSRS, RT (R) (CT) (ARRT), CRA, Radiology Director at Baylor Scott and White Health All Saints Fort Worth
1. Last book you read? “The 5AM Club”
2. Favorite movie? “Jurassic Park” I’m especially excited about the newly released Jurassic Park movie!
3. Something most coworkers don’t know about you? I enjoy watching MMA and bare-knuckle fights.
4. Current mentor? An entrepreneur with a healthcare background who offers strategic guidance and support.
5. Morning routine? Five-minute journaling followed by a workout.
Sarah Franks and colleagues celebrate the Fab 25 Speak Up for Patient Safety initiative. It is an annual celebration that highlights the top 25 most notable “good catches” for patient safety within the previous fiscal year.


6. Best advice received? “You are the average of the five people you spend the most time with. Choose those people wisely.”
7. Biggest influence? My mother. She raised 12 children while working full-time, managing the household, and always making time for her family. She was witty, humble, kind and faithful. Though we had little, she made sure we never felt that way.
8. Superpower of choice? Time travel – to eliminate my onehour commute and gain two hours back in my day, and to strategically plan by glimpsing into the future.
9. Hobbies? RVing, rifle deer hunting, shooting a compound bow, gardening and raising Highland cattle.
10. Perfect meal? Crab-stuffed salmon, rice, and broccolini, paired with a glass of white wine.
BY MATT SKOUFALOS
Shakespeare famously wrote, “What’s in a name?”
“That which we call a rose/By any other name would smell as sweet,” Juliet’s soliloquy continues – a timeless meditation on the difference between the written word and the symbolic meaning we charge it with conveying.
For Mario Pistilli, executive director of imaging services at Children’s Hospital Los Angeles (CHLA) and recent ICE Dia mond Award winner, his first name came with more attention than he’d have preferred as a youngster.
The Bahamian-born Mario moved to the Chicago, Illinois area in the 1970s, just prior to entering the first grade, and experienced a fair amount of culture shock in the transition.
“I’d never seen a snowflake, nor a paved road; everything was new to me,” Mario said. “We didn’t have TV, so I was not familiar with anything on TV.”
Growing up around
cousins with names like Michael, Ronald, Bradley and Hank, he was the only Mario in the family. His Italian father liked its connection to Mars, the Roman god of war, and said it sounded masculine and strong. But as a kid, being the only Mario made a lot of extra work for his social interactions.
“I always hated my name, from the get-go,” Mario said. “I have a bunch of male cousins who all had regular names; then I come to Chicago, and nobody is named Mario. I always wanted to be Joe, Mike, Jim, Bob – anything but Mario.” However, by the time Mario had entered college at the University of St. Francis in Joliet, Illinois, his name had undergone a significant cultural shift, due in no small part to the 1981 release of the Nintendo game Donkey Kong.

According to a 2022 feature on IGN.com, game designer Shigeru Miyamoto had pursued the licensing rights to characters from Popeye. After failing to acquire them, Miyamoto created Mario, initially called “Jumpman,” a ladder-climbing, mallet-wielding, princess-pursuing plumber; the playable protagonist of the story.
Donkey Kong was followed by several video games featuring Mario including the wildly popular Super Mario Bros. and Mario Kart.
There’s no telling how much the popularity of that name was driven by popular fascination


with the gaming platform. A review of American baby naming trends shows that “Mario” peaked in commonality in 1980, the year prior, at the 102nd position. In Italy, it’s declined in usage since the late 1990s.
But for Pistilli, the moniker that had been his albatross as a youth transitioned to a pleasant icebreaker in his young adulthood.
“That’s when I was like, ‘Oh, this isn’t so bad,’” he said.
“People instantly made the connection when they heard my name, so I just rolled with it, and it became a thing.”
Beyond chatting him up with catchphrases, people occasionally gifted him Mario-related items – artwork, figurines and such. After accepting a position at Children’s Hospital of Los Angeles, however, his former team at St. Joseph’s Hospital in Joliet sent along the package that burst the dam of Mario-related giving.
“They got together and surprised me with this big tube of Mario graphic wall clings,” Mario said, “so I decorated my office with the Mario stuff. As people saw that, they started adding to it and adding to it.”
In Pistilli’s office at CHLA, there’s a shelf with Mario figurines, toys, mints, stickers, a lapel pin, Christmas ornaments and more. When he earned his doctorate, Mario suddenly found himself in


possession of a Doctor Mario statuette. As he is central to institutional construction projects at CHLA, Mario is the proud owner of a hard hat with the signature “M” over the brim. And every year on March 10 – MAR10, when “Mario Day” is observed unofficially – he’s found his office decorated with Nintendo graphics.
“One year they passed around a Mario hat and took selfies,” Pistill said. “It’s just become a thing.”
The article in his collection that brings Mario the greatest pride is an illustration of Mario that a pediatric patient drew for him. The child unfortunately succumbed to the illness that had brought her to the hospital, but her artwork is a fixture in his workplace and his heart.
“I have it in my office, and it’s my reminder of why I’m here and why I do what I do,” Mario said. “It’s a real source of strength for me.”
For the kid who grew up rejecting the attention his uncommon name drew, Mario ultimately has embraced it; taken ownership of it, if you will. In the pediatric space, it’s become an even more powerful touchstone; a way to connect with children who are going through some of the most challenging health circumstances anyone may face.
“I’ve totally embraced it for years now,” Mario said. “It’s a great way to connect. I love it when people give me Mario stuff. It’s a sign they’re thinking of

me in a good way.”
Through working in pediatrics, Mario said, the resilience of children has bolstered his own outlook on life’s challenges, and given him the benefit of perspective on his own struggles.

“Even the worst stuff I deal with in a day is nothing compared to what our patients deal with every day,” Mario said. “They do it with a smile, and laughter, and hope.”
“There’s so much to love about pediatrics,” he said. “We have insanely smart people; caring and passionate people. It’s exciting to be in that incubator of talent and knowledge with people who are so willing to share it.”
“The culture here, because we’re all in this for kids – everyone here is welcome to contribute,” Mario said. “It’s a great atmosphere for people who are willing to work. You can walk out of here satisfied and fulfilled.”
If stepping into the mythical space held by an iconic hero like Super Mario can help him to perform under those circumstances, Pistilli is happy to do it.
His childhood peers who didn’t understand what being a Mario could mean have given way to new generations who are delighted by that same name — and all, as Shakespeare once wrote, that’s in it. •
OA K BROOK, Ill. | The Radiological Society of North America’s 111th Scientific Assembly and Annual Meeting (RSNA 2025), held at Chicago’s McCormick Place Nov. 30-Dec. 4, offered nearly 38,000 registrants a wealth of opportunities to engage with the latest research, education and advanced imaging technologies. The meeting’s theme was “Imaging the Individual.”
“As the largest medical imaging gathering in the world, the RSNA annual meeting draws radiology professionals and influencers from across the globe to share knowledge and learn about the latest technological advances,” said RSNA Executive Director Mark G. Watson. “With a multitude of lively sessions, hundreds of education exhibits and courses, a robust technical exhibition, and unique opportunities to network or recharge, RSNA 2025 attendees enjoyed a multifaceted meeting experience. It truly is radiology’s biggest week.”
The meeting offered inspirational plenary sessions from renowned thought leaders on timely topics, such as precision imaging, clinician well-being, AI challenges and imaging breakthroughs in treating neurodegeneration.
In his President’s Address, Umar Mahmood, M.D., Ph.D., highlighted radiology’s transformative role in precision medicine, where imaging is evolving from a diagnostic tool into the cornerstone of personalized care.
“We have an increasing ability to understand how changes –in genes, in cells, in organs – can interact and lead to disease,” Mahmood said. “We can now target specific abnormalities in each individual patient – with higher fidelity.”
Beyond the plenary lectures, popular meeting features like the Image Interpretation Session, Case of the Day, and “The PACS and the Furious: An RSNA Family Feud” game show offered interactive opportunities for attendees. “Fast 5” sessions delivered brisk, novel presentations related to the “Imaging the Individual” theme.
Research and education presentations covered all radiologic subspecialties and modalities. The Learning Center Theaters offered dynamic scientific presentations in rapidly developing


areas of interest. Learning Center Theater topics included “Opportunistic Screening: Enhancing Diagnostic Impact from Routine Imaging,” “Next-Generation Imaging: Advances in Low- and Non-Contrast Techniques,” “Translating Innovation: Radiologist-Industry Collaboration in Clinical Integration of New Technologies” and “Imaging-Guided Oncologic Therapies: From Histotripsy to Theranostics and Beyond.”
RSNA 2025 also offered a rich mix of industry programming, product launches and demonstrations, immersive workshops and live symposiums.
RSNA 2025’s technical exhibits covered 419,500 square
feet and featured 720 exhibitors – including 142 first-time RSNA exhibitors – demonstrating the latest medical imaging advances and solutions in CT, MRI, AI, theranostics and more.
The technical exhibits featured the expansive AI Showcase and Theater, the “Radiology Reimagined” demonstration, the Innovation Theater, 3D Printing and Mixed Reality Showcase, First-time Exhibitor Pavilion, Educators Row and Recruiters Row. The newly introduced “RSNA Road Trip” feature provided attendees with an interactive way to navigate the show floors.
The AI Theater hosted several engaging presentations, as well as a recognition event for the teams with the top performing models in the RSNA Intracranial Aneurysm Detection AI Challenge.
Attendees with Virtual Access can view an abundance of RSNA 2025 content until Feb. 27, 2026, at 12 p.m. CT.
RSNA 2026: At the Center of Care, the Society’s 112th Scientific Assembly and Annual Meeting, will take place Nov. 29-Dec. 3, 2026, in Chicago. •

Metropolis International has been in business for over 20 years now, approaching 21 years next month. All the while it’s president, Leon Gugel, has been around for 27 years. Over the years, Metropolis has definitively established itself with an excellent reputation as a great and reliable partner
Located in the heart of the NYC, Metropolis International is the only stocking dealer based out of the New York City center itself.
“Being here has many positives, least of which is that NYC is the capital of the world! We get a lot of customers from all over the world visit us, as well as local East Coast dealers, and decision makers from various hospital institutions from the NY Metro area. We’ve established a consistent history of helping our partners with the best equipment with reasonable price,” Gugel says..
As well as on-demand service for end-users in the area.
Metropolis has an office and warehouse geographically located in the center of New York City so that it can cover the entire metro area within 20 minutes of travel. It is located just two blocks from the Ed Koch, 59th St. Bridge, overlooking Manhattan.
“Our knowledge and expertise in the market for various systems as well as having the technical knowledge to assist customers, is second to none!” Gugel says. “
Because of our longevity, creativity and responsiveness, we are the first to know about systems coming out, what hospital is selling its older systems, and pricing on these systems.”
Metropolis International is also FDA registered and was one of the first dealers to be so for 15 years now.
“This helps us navigate large institutions as well as be able to help various OEM partners,” Gugel says. “And, I truly mean partners. It is not just about buying a system and flipping it to another dealer, but actually enhancing the customer/enduser experience.”
This is a reason many OEMs have been using Metropolis to help customers during all these years.
“What truly makes us different – and better – is that we truly have that personalized approach to doing business. It is built on real, long-term and meaningful relationships,” Gugel says. “We also pride ourselves on learning the technical aspects of the systems we sell. This helps our customers and other end-users down the line.”
Regardless of whether our customers are brokers, dealers, or the actual end-users, Metropolis strives to help everyone and thus build relationships to enable repeat business to occur.
The world has truly become a smaller place for doing business, both domestically and internationally. More facilities require third-party companies to be FDA registered here in the U.S.
“As such, because we are also FDA registered, it gives us a leg up on the competition and a few others still that do not operate with honesty,” Gugel explains.The years of success did not come without challenges. It is how a business adapts and overcomes obstacles that leads to continued success, simply translating into solutions for customers and partners.
As everyone knows, there has been a lack of consistency in the market over the last decade. The elections last year and COVID a few years before that, which sadly still controls how some smaller facilities operate.
More recently, it is international wars, tariffs and AI integration into more aspects of the industry, not just the system it is built into by some companies.
All of these factors contribute to wild fluctuations in demand, pricing curves, inflation, ACA subsidies, venture capitalists continuing to go after companies in the healthcare arena, and overall performances of some major companies that have not gone to plan.
“As I stated before, the disappearance of some smaller players over the years from the industry has changed the face of smaller markets too,” Gugel says.Metropolis operates on old-fashioned basics of customer-centric approach to working together, not just for themselves, and that has allowed the company to thrive!
“In the end, the relationships we’ve built have been growing still!” Gugel says. “
It is our core competencies and our ability to locate and purchase 95% of our systems directly from medical facilities that gives our customers the peace of mind of getting great prices from us.”
“As I noted in years past, this result, along with our prices, are more in tune with modern spending trends for both wholesale as well as retail customers,” he says. “We sell all imaging modalities, and have demonstrated a continued ability to work with OEMs and hospitals alike in acquiring systems direct and be able to get them removed and deinstalled in a professional and quick manner.”
After all these years, Gugel says he still gets excited about the fact that Metropolis still sells more C-arm systems of all types than anyone else in the industry – worldwide!
Metropolis International has also continued to expand its servicing capabilities and refurbishment of various systems.


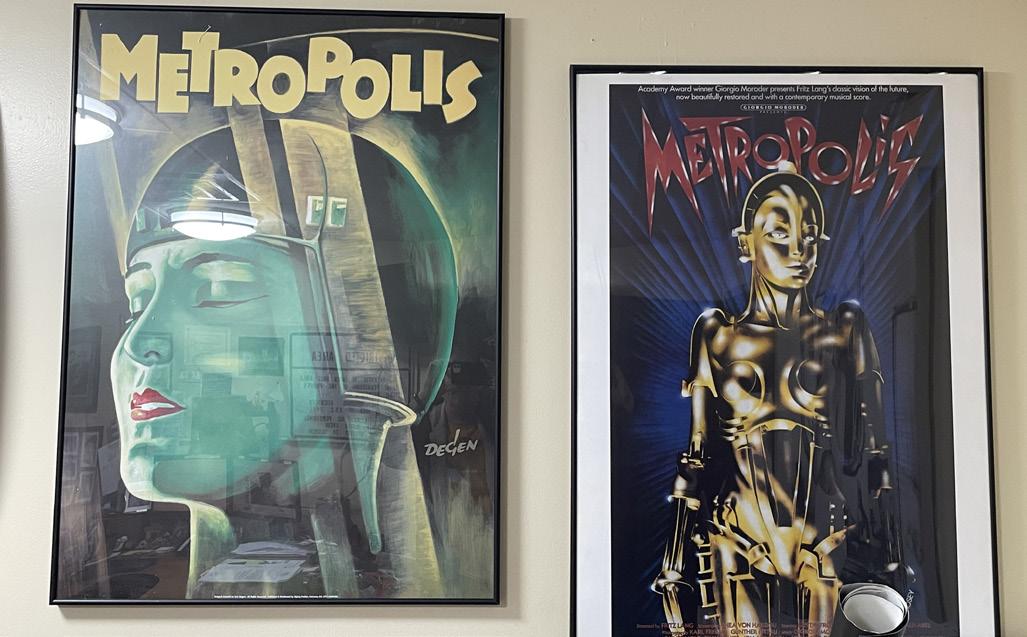
Metropolis has partnered with a few other strategic dealers around the country to create and expand more offerings and capture a higher market share with large hospital chains.
Another positive change has also been a larger footprint in the digital marketspace.
“From a revamped website, to LinkedIn, to advertising here, to Instagram and Facebook, we’ve been able to connect with more customers, especially from overseas,” Gugel says. “Both Asia and Europe.”
“Traditionally both markets have been greatly fragmented, but they have been growing too. These all factor into our long-term plans,” he adds. All of these behind-the-scenes moves, assure both present and future success for Metropolis. Gugel says he is humbled and grateful to be part of a greater process!
“To be able to help small clinics and private practices in extending patient care,” Gugel says. “As well as our dealers from all over the world.”
In the end, Metropolis is continually striving to build a legacy for the next 100 years!
For Metropolis to rival GE or Philips or anyone else out there so that doctors and dealers in the future can recognize the value of working with a company that has a personal touch.
Metropolis is evolving and it will only get better! •
more information, visit



Agfa Radiology Solutions, the Association for Medical Imaging Management (AHRA), and Cleveland Clinic are joining forces to help the next generation of radiology administrators showcase their potential and drive meaningful change in radiology. Together, the organizations are launching the RadX National Case Competition, the first U.S. case competition focused exclusively on radiology administration.
The winning team will be announced in April 2026.
Highlights:
• The competition is designed to foster innovation, leadership and operational excellence in medical imaging.
• Student teams will apply classroom knowledge to a real-world radiology administration challenge developed by Cleveland Clinic.
• Eligibility is open to students currently enrolled in AS to BS Radiology Administration programs across the United States.
“RadX is an additional and important new initiative that supports Agfa Radiology Solutions’ commitment to empowering X-ray experts to deliver the best patient care possible. We are proud to bring this opportunity for learning and recognition to the next generation of radiology administrators, and to do it with the support of healthcare industry leaders Cleveland Clinic and AHRA,” says Jordan Hermiller, MHA, RT(R) (QM) CPHQ and Advanced Imaging Consultant at Agfa Radiology Solutions.
Case competitions are widely recognized for strengthening academic programs through real-world, experiential learning.
For RadX, student teams will receive a detailed case study developed by Cleveland Clinic that focuses on a current challenge in radiology administration – such as AI adoption, productivity benchmarking, capital budgeting, dose management, staffing and workforce planning, or imaging workflow and operations. Teams will have two weeks to analyze the case, develop a solution, and create their presentation.
Submissions will be evaluated by industry experts from AHRA, Agfa Radiology Solutions, and Cleveland Clinic. The winning team will receive a cash prize, professional recognition, free AHRA student memberships, and additional opportunities for visibility and networking.
“AHRA is proud to join Agfa and the Cleveland Clinic in supporting the RadX National Case Competition. This initiative reflects our commitment to cultivating the next generation of leaders in medical imaging. By engaging students in real-world challenges, RadX not only strengthens academic learning but also inspires innovation and excellence in radiology administration,” says AHRA President Wesley Harden, CRA, FAHRA.
For lots of families, putting together jigsaw puzzles is a fun and stress-releasing group activity: If all the pieces are present, that is.
A specific feeling of disappointment arises when the hours of puzzle assembly result in an incomplete picture of a seascape or collection of movie posters, the bonnet of a lighthouse unfinished or letters missing from the title card of a Hollywood classic.
For decades, patients with lung diseases and their doctors would start down the path of diagnosis and treatment in a similar way, working around the edges of the problem to get to its center, and hopefully a complete picture. But the available tests would often leave patients suffering from cystic fibrosis, chronic obstructive pulmonary disease (COPD), asthma, farmer’s lung and other lung diseases without answers.
Researchers at the University of Missouri and MU Health Care have helped find an answer using magnetic resonance imaging (MRI).
Radiologist and hyperpolarized xenon expert Talissa Altes, MD; asthma, MRI physics and hyperpolarized gas expert Robby Thomen, Ph.D.; and pulmonologist Zach Holliday, MD, wanted a better way to treat lung diseases for their patients.
“This test has been helpful in research, and it’s shown to be helpful in clinical care,” said Holliday. “In one patient’s case, this may be a single puzzle piece, or in another patient’s case this may be half the puzzle. And it may really shed light on a puzzle that we lost pieces to and now, finally, we can complete that puzzle.”
It’s an innovation that’s decades in the making, and MU Health Care is one of only two hospitals in the United States who offer the test clinically for patients.
MRI machines use magnets to align the hydrogen atoms in your body, which is why they have traditionally been used to scan every type of body tissue except the lungs. Because our lungs are full of air, not water, MRI struggles to get a clear picture. But MRI scanners can be programmed to image hyperpolarized xenon gas.
“The traditional treatment for asthma has been
a stepped approach, trying different drugs to see what works, clearly not precision medicine,” Thomen said. “This new technology is completely different and allows patients to see their own breath in their own lungs. It doesn’t compare the patient to a pool of similar people, but shows us what makes you unique, medically.”
The FDA-approved scan is identical to a traditional MRI but asks patients to inhale the non-reactive xenon gas and hold their breath during a 10to-15-second scan. The resulting images show how a breath of air is drawn into the lungs. This gives patients and their doctors a better understanding of lung function, leading to faster and better treatments.
“The images do all the talking,” Thomen said. “You see it side-by-side and the xenon MRI images are so much clearer.”
In the past, some patients with lung diseases received two CT scans per year to check their lungs. These tests showed lung structure clearly but didn’t tell doctors how well the lungs were working. In addition, each CT scan uses a small amount of radiation that adds up over years of treatment.
“MRI gives us a fantastic picture with no radiation, and if we can replace the radiation from a CT scan with something like xenon gas MRI, now we have taken a lot of radiation, relatively speaking, and turned it into no radiation,” Holliday said.
The innovative technology will help doctors and patients make better decisions more quickly about which treatments to try, and whether those treatments are having the intended effect, leading to better results for patients and saving time and money.
“From stubborn asthma to rare lung diseases, it’s unique to have this technology and the specialists who can treat these diseases in mid-Missouri,” Holliday said. “If you live nearby, it means you don’t have to travel long distances, and because we’re one of the only ones with this technology, I have patients who drive six hours to come here. It’s a great addition to what we can provide to Missourians and people across the country here at MU Health Care.”

Royal Philips has entered into an agreement to acquire SpectraWAVE Inc., an innovator in enhanced vascular imaging (EVI) of coronary arteries, angiographybased physiology assessments, and the use of AI in medical imaging. SpectraWAVE’s intravascular imaging and physiological assessment technologies provide advanced solutions for the treatment of patients with coronary artery disease, the most frequent type of heart disease, affecting more than 300 million people worldwide. SpectraWAVE, based in Bedford, Massachusetts, was founded in 2017 and currently employs more than 70 people.
“Our global leadership in image guided therapy is driven by deep clinical collaboration combined with our latest technology insights across hardware, software and AI, to innovate interventional procedures for better and more patient impact. Our world-class portfolio integrates interventional systems and devices into one platform, Azurion, serving patients worldwide.
“We are doubling down on image-guided therapy and expanding our portfolio in the coronary intervention segment with the addition of SpectraWAVE’s AIpowered innovations in high-definition intravascular imaging and angio-based physiological assessment, enabling us to deliver better care for more people,” said Roy Jakobs, CEO of Royal Philips.
Percutaneous coronary interventions are minimally invasive procedures that leverage intravascular imaging and physiological assessment to treat coronary artery disease. A significant and growing body of evidence shows that the use of intravascular imaging and physiological assessment technologies significantly improves patient outcomes for percutaneous coronary
interventions. With its industry-leading Azurion imageguided therapy platform, integrated with its expanding portfolio of advanced diagnostic and treatment devices, Philips is driving the adoption of advanced healthcare technology to treat a growing and increasingly complex patient population.
SpectraWAVE’s HyperVue Imaging System is an intravascular imaging platform that combines DeepOCT (next generation comprehensive optical coherence tomography) and NIRS (near-infrared spectroscopy) into the Enhanced Vascular Imaging (EVI) novel imaging segment to provide detailed structural and compositional images of the coronary arteries during percutaneous coronary interventions, with rapid setup, acquisition, and automated AI image analysis. Combined with Philips’ Eagle Eye Platinum digital IVUS and IntraSight technologies, HyperVue will expand clinicians’ intravascular imaging toolbox – IVUS, DeepOCT, NIRS, and wire and angio-derived physiology – all orchestrated through integrated systems to tailor guidance to each patient and lesion.
SpectraWAVE’s X1-FFR is an angiography-derived, AI-enabled physiology solution that calculates Fractional Flow Reserve (FFR) from a single coronary angiogram, providing a non-invasive ischemia assessment and turning routine X-ray images into coronary physiology data for simplified percutaneous coronary intervention workflows. X1-FFR complements Philips OmniWire iFR technology by extending physiologic guidance to wire-free scenarios and equipping clinicians with a versatile toolkit to broaden the adoption of coronary physiology in daily practice.
Laser technology has transformed modern medicine and healthcare disciplines, utilizing lasers to perform precise procedures. These advances can pose risks to patients and professionals. A new virtual course designed and taught by perioperative consultants Patti Owens, MHA, BSN, RN, CMLSO, CNOR, FAORN, and Vangie Dennis, MSN, RN, CNOR, CMLSO, FAORN, FAAN, prepares individuals to become certified laser safety officers.
Regulations require each facility to have a medical laser safety officer. Individuals who obtain medical laser safety officer certification are valuable members of the staff who can gain additional compensation for their role as a safety officer.
The in-depth virtual course is offered three times on April 18-19, July 18-19 and November 7-8.
The use of lasers in healthcare is associated with a variety of hazards, such as eye exposure, misaligned laser beams, use of unfamiliar equipment, and improper handling, which can affect the safety of personnel and patients and are non-compliant with regulations and guidelines. The American National Standards Institute (ANSI) and the Association of PeriOperative Nurses (AORN) Lasers Guidelines has developed a series of standards for the safe use of lasers in the healthcare environment.
The ANSI Z136.3 standards and the AORN Guidelines require the designation of a laser safety officer (LSO), implementation of safety and engineering control measures, and training
of authorized personnel. LSOs are responsible for enforcing a hospital’s laser safety procedures. Healthcare facilities manage these risks by assigning safety duties to an LSO. These standards and guidelines are enforceable by the Occupational Safety and Health Administration (OSHA), Center for Medicare and Medicaid Services (CMS), national accreditation organizations and numerous state regulatory statutes.
This new Medical Laser Safety Officer course is designed to provide healthcare personnel with a foundation of laser biophysics, tissue interaction, safety and administrative responsibilities. Technical aspects, as well as established best practices, will be reviewed on multi-wavelength lasers. Laser safety protocols and documentation will be addressed according to the ANSI 136.3–2024 “Safe Use of Lasers in the Healthcare Facilities Standards,” and the AORN Laser Safety Guidelines 2020. Applicable national accreditation standards will be shared for laser safety program compliance. Instruction is accomplished through didactics and group discussion.
MLSOs can come from a variety of backgrounds. This training is designed for healthcare professionals looking to enhance their laser safety knowledge and improve the quality and safety of patient care at their facility. Professionals who should consider obtaining MLSO certification include imaging professionals, radiation safety officers, perioperative nurses, perioperative educators, laser safety officers, biomedical/clinical engineers and surgical technologists.




Siemens Healthineers has received Food and Drug Administration clearance for the 70cm bore Magnetom Flow. platform, a 1.5 tesla (T) platform for magnetic resonance (MR) imaging with a closed helium circuit and no quench pipe, which reduces helium dependency and annual energy consumption. The upgradable platform covers the entire range of MR applications. It offers image reconstruction based on artificial intelligence (AI) for shorter scan times with improved image quality. The second virtually helium-free 1.5T MR platform from Siemens Healthineers, it follows the 60cm bore Magnetom Flow.Ace. Siemens Healthineers also manufactures the low-helium 0.55T Magnetom Free platform.
“The 70cm Magnetom Flow. platform is an intelligent magnetic resonance scanner that exceeds clinical expectations and simplifies workflows while doubling down on our commitment to sustainability in healthcare,” said Katie Grant, head of magnetic resonance at Siemens Healthineers North America. “This platform can help healthcare institutions meet the demands of higher patient throughput in less time than previous generations of MR scanners while also lowering the total cost of ownership.”


The Magnetom Flow. platform requires only 0.7 liters of liquid helium for cooling, compared with conventional MRI scanners that typically require over 1,000 liters. This minimal helium requirement, made possible by the magnet’s DryCool technology, can lower costs and conserve resources by removing the need for helium refills. The system design also eliminates the need for a quench pipe to vent gaseous helium directly into the atmosphere during an emergency shutdown. This lack of a quench pipe, along with the scanner’s compact size, can reduce installation requirements and costs compared to other 1.5T MR scanners.
AI supports automated workflows, including new cardiac workflows that simplify and standardize the setup of scan parameters. Deep Resolve 2D and 3D image reconstruction technology enables accelerated image acquisition, removes noise and improves image sharpness. The myExam Assist and myExam Autopilot features provide adaptive, automated strategies for simplifying complex scans, and the tools in the myExam Implant Suite provide straightforward setup to safely scan patients with implants, including pacemakers. • - New Windows 10 Platform with Dynamic Digital DR Panel - Eliminates the OEM Saturn Windows 95 Platform - Dose Reduction
- HIPAA Compliant, 510k approved.
- Fluoroscopy digital recording loops for MBS studies
- Upgrade Provided to your Proven R/F System in 4 days.
- Complete Refurbished Systems Available


SPONSORED BY: X-RAY AMERICA

ICE Magazine invited imaging leaders to participate in this month’s Director’s Circle feature on X-ray technologies in diagnostic imaging. Topics touched on in this discussion include the latest technology, how to evaluate systems, dose reduction and more. Participants in the article are:
• SSM Health, St Louis Regional Service Line Director of Imaging Jessica Chambers;
• University Hospitals Radiology Director, West Market Michelle Dossa;
• Hartford Hospital Imaging Director Sandra Smith Phillips;
• Oklahoma City Indian Clinic Director of Radiology Lisa Walling; and
• AdventHealth Director of Ambulatory Imaging and Imaging Safety Program Cory Whitehouse.
Q: HOW HAVE X-RAY TECHNOLOGIES EVOLVED IN RECENT YEARS, AND WHAT ADVANCEMENTS ARE HAVING THE GREATEST IMPACT ON CLINICAL WORKFLOWS?
CHAMBERS: The shift to the digital platform continues to advance, while I would assume most everyone has converted from CR to DR the AI and dose optimization tools that are coming with the digital technology is impressive. From enhancements to line placements to pneumothorax algorithms, these new technologies will both improve efficiencies within our departments and, most importantly, outcomes for our patients. I also appreciate the attention to detail the OEMs have with workflows and body mechanics; detectors 10 years ago were heavy and difficult to move. I feel each year the imagine quality improves as well as the ergonomics to move them and weight.
DOSSA: AI has truly improved the images/care we can give our patients with self-calibrating systems and units that flag maintenance issues as well as predictive analytics for early disease detection and smart triage AI to prioritize imaging cases for our radiologists. The automation that X-ray equipment has in setting up for image views is something I never had as a technologist that can be used to make our techs as efficient as possible.
PHILLIPS: X-ray technology has shifted toward digital radiography (DR) as the standard, offering faster image acquisition and improved image quality. Recent advancements include wireless detectors, mobile systems and integrated workflow automation that reduce manual steps. AI-driven tools for image enhancement and positioning guidance are also streamlining processes, minimizing retakes and improving throughput.
WALLING: The use of automation – such as auto-positioning, auto-exposure and protocol-driven workflows – has improved exam turnaround time and improved consistency.
WHITEHOUSE: One of the most significant advancements in recent years has been the widespread adoption of digital radiography (DR). DR technology has dramatically improved efficiency by reducing radiation exposure and minimizing the need for repeat exams, which enhances patient safety and throughput. Additionally, DR systems provide faster image acquisition and immediate availability for interpretation, streamlining workflows and improving diagnostic turnaround times. However, an unintended consequence is that technologists may rely heavily on system automation, potentially reducing their proficiency
in manual technique selection. This underscores the importance of ongoing education and competency training to maintain high standards of image quality and patient care
Q: WHAT FACTORS SHOULD IMAGING LEADERS CONSIDER WHEN EVALUATING NEW X-RAY SYSTEMS FOR THEIR FACILITY?
CHAMBERS: I oversee seven hospitals and multiple outpatient centers, and it’s easy to get caught up in the desire for the latest and greatest technology. However, with declining reimbursements and rising levels of bad debt and charity care, we must be good stewards of our resources. The priority should always be leveraging your organization’s identity to ensure you have the best technology for your specific patient population. You may not always need the newest AI feature if it significantly increases costs without clear benefit. As imaging utilization continues to grow, dose reduction strategies remain top of mind. Beyond that, decisions will vary based on each hospital’s unique needs and operational priorities.
DOSSA: As an organization that has a 10-year equipment non-obsolescence plan with OEMs, we work closely with our vendor of choice for X-ray. A team of key stakeholders (radiologists, technologists, physicists, rad IT, HTM, leaders, strategy, supported service lines, i.e., oncology, cardiology, ortho, etc.) worked together with the OEM to review available fleet, software options, AI capabilities, dose optimization capabilities, and what may be on the horizon when developing our equipment configuration plan. We have a general equipment configuration for stationary X-ray, fluoroscopy, portables and C-arms based on location (academic hospital, community hospital, ambulatory site).
We strive for consistency for patient access and staffing flexibility, the ability to properly provide clinical support for existing and future caregivers/service lines over the course of multiple years.
PHILLIPS: Imaging leaders should consider:
• Staff engagement: Involve technologists early – they are the primary users. Conduct demos with subject matter experts.
• Volume and case mix: Choose equipment that aligns with your patient load and exam types.
• Mobility: For portable systems, prioritize ease of use and consistent image quality.
• Advanced features: Look for positioning assistance, workflow integration and AI tools that enhance efficiency and image quality.
• Dose optimization: Select systems with advanced dose monitoring and reduction technologies.
• Interoperability: Ensure seamless integration with PACS/ RIS and EMR systems.
• Service and maintenance: Review service contracts and preventive maintenance options.
WALLING: Leaders need to analyze their facility’s demands and staffing realities when evaluating new systems. Things to consider are the types of cases (trauma, orthopedic or bedside), how the system can enhance workflow efficiency, dose management, flexibility of the system and cost.
WHITEHOUSE: Cost is always a consideration, but decision-makers should prioritize value and long-term ROI over initial price. Key factors include compatibility with existing RIS/PACS infrastructure, scalability for
future upgrades, and flexibility to support multiple clinical applications. Mobile DR units can be particularly advantageous, enabling bedside imaging and improving access for patients with limited mobility. Leaders should also assess automation features, dose optimization capabilities, and integration with AI-driven tools to enhance positioning accuracy and workflow efficiency. Ultimately, the goal is to select systems that align with organizational strategy and deliver both clinical and operational benefits.
HOW ARE FACILITIES BALANCING RADIATION DOSE REDUCTION WITH THE NEED FOR HIGH IMAGE QUALITY, FASTER THROUGHPUT AND DIAGNOSTIC ACCURACY?
CHAMBERS: This really is the million-dollar question. In my opinion, the best solution is to move toward a truly quality-focused reimbursement structure rather than a per-click model. We continue to see imaging utilization rise. Our emergency department imaging volumes are growing even though overall emergency department patient volumes have not. This highlights that it’s imaging utilization, not patient visits, that’s increasing. A few years ago, CMS explored appropriateness criteria for imaging, but unfortunately, that initiative has fallen by the wayside. I believe organizations need to dive deeper into utilization as the first line of defense for improving throughput and reducing dose. From an operational standpoint, I feel our organization is already as lean as possible; expecting staff to simply work faster is not a sustainable solution. We need to shift the focus from quantity to quality.
DOSSA: Our in-house medical physicists participate in our equipment non-obsolescence planning and guide us with dose reduction needs. It needs to be a balance to ensure quality imaging, efficient patient throughput and appropriate radiation dose for our patients. Taking a quality image the first time versus repeating is another great way to reduce dose, so ensure your technologists are part of the equipment process. They need to have an easy-to-use piece of equipment that allows them to be as efficient as possible given the heavy demands on their time and talents.
PHILLIPS: At Hartford HealthCare, we brought our imaging and radiation safety team in-house. This enables real-time support and stronger collaboration with technologists, radiologists, oncologists, physicists and patients across our system. The team oversees dosimetry and dose-reduction tracking software, monitoring performance consistently to improve communication and achieve meaningful dose reductions without compromising image quality or efficiency.
WALLING: Facilities are leveraging smarter technology to help with dose reduction. Advances in detector sensitivity and better image processing are allowing lower doses. Ongoing technologist education and dose monitoring programs are critical – allowing departments to identify outliers and continuously refine protocols without compromising image quality or speed.
WHITEHOUSE: Modern DR systems have been instrumental in achieving this balance. They allow for significant dose reduction while maintaining diagnostic image quality through advanced detector technology and image processing algorithms. Facilities are leveraging protocol optimization and software-driven exposure controls to ensure consistency across exams. Additionally, continuous monitoring of dose metrics and adherence to ALARA (As Low As Reasonably Achievable) principles remain critical. These strategies collectively support patient safety without compromising throughput or diagnostic confidence.
Q: WITH THE RISE OF AI-ASSISTED POSITIONING, WORKFLOW AUTOMATION,
CHAMBERS: I believe AI tools are significantly improving image quality while helping to standardize workflows. They provide an added level of confidence for newer technologists by having protocols programmed directly into the equipment. Reducing cognitive burden not only enhances efficiency but also helps manage workload across teams. Even small improvements, like reducing the number of clicks per exam can add up to meaningful time savings in the long run.
DOSSA: AI is a tool that we use to support our diagnostic imaging. We want our technologists to be working at the top of their licenses, so if there are tasks that AI can support so they can, that is the very best. AI tools showing lines, pneumothorax, etc. are helpful for techs and radiologists as well.
PHILLIPS: AI is transforming X-ray imaging by reducing variability and improving efficiency. Positioning guidance minimizes retakes, while automated workflow orchestration accelerates exam completion. AI-driven image enhancement improves clarity for faster interpretation, and predictive analytics help optimize equipment utilization. In some cases, AI even supports staffing shortages by enabling remote technologist assistance.
WALLING: AI-assisted positioning and collimation reduce repeats and variability, while automated image quality checks flag issues before the patient leaves the room. AI-based image enhancement improves visualization in challenging patients and reduces retakes. Over time, these tools will help address staffing shortages, support less-experienced technologists, and create more standardized, reliable imaging across sites.
WHITEHOUSE: AI is poised to transform X-ray imaging by reducing variability and improving efficiency. While adoption of AI-assisted positioning is still emerging, these tools can significantly benefit less experienced technologists by guiding patient alignment and minimizing repeat exposures. AI-driven workflow automation – such as intelligent exam routing and predictive scheduling – can streamline operations, while image enhancement algorithms improve clarity and diagnostic accuracy. As these technologies mature, they will play a pivotal role in standardizing quality and optimizing resource utilization across imaging departments.
Q: WHAT COMMON MAINTENANCE OR QUALITY ASSURANCE ISSUES SHOULD IMAGING LEADERS MONITOR TO KEEP THEIR X-RAY FLEET PERFORMING OPTIMALLY?
CHAMBERS: I would say my number one pet peeve is dropped detectors. While the advancements in detector technology over the years have been incredible, the downside is that the more advanced they are, the more expensive they become. Nothing is worse than starting the day and hearing from the morning tech that a detector won’t associate because it registered a drop. With any high-cost piece of equipment, preventive maintenance is critical, along with implementing safeguards to ensure staff handle the equipment properly and avoid unnecessary damage.
DOSSA: Our radiology leaders work closely with our HTM leadership and teams on the ground that support our imaging equipment. We all participate in quarterly business reviews with each vendor in an effort to ensure our equipment is working as intended and its producing quality images throughout its expected life cycle. Our HTM team performs some preventative maintenance and/or first looks for specific modalities while we choose to have other modalities serviced by OEMs. It is not an all or nothing strategy and has helped build the relationships between our HTM teams, our OEMs and our medical physicists. Ensuring PMs and QAs are performed per manufacturers’ recommendations is critical. Setting up PMs in the beginning of the year versus on the fly is incredibly helpful to the technologists and patients. We never want to be the reason a patient is rescheduled. Ensure a solid workflow for notification and escalation of equipment issues. Ensure everyone is aware of the process and review throughout the year. We have found that it works well versus waiting for an issue to come up and the technologist is unsure of the process.

JESSICA CHAMBERS




PHILLIPS: Regular calibration, detector checks, software updates and preventive maintenance are critical. Leaders should track image quality trends, dose reports and system uptime to identify issues early. Compliance with regulatory standards and maintaining technologist competency in QA protocols are essential. Having in-house physicists greatly enhances preventive maintenance and testing capabilities.
WALLING: Some key areas to consider are detector performance, tube output consistency, alignment and collimation accuracy, and software updates. Wireless detector handling and battery health are frequent pain points. Leaders should also monitor repeat/reject rates, exposure index trends and downtime patterns. A proactive QA program – combining routine physicist testing, technologist feedback and vendor service data – helps prevent small issues from becoming costly disruptions.
WHITEHOUSE: Here at AdventHealth, we have a robust quality assurance (QA) program. Facilities should implement systems to track retake rates, monitor equipment performance and identify technologists who may require additional training. Routine preventive maintenance, calibration checks and software updates are critical to sustaining image quality and minimizing downtime. Data-driven QA programs not only ensure compliance with regulatory standards but also provide actionable insights for continuous improvement.
Q: WHAT ADVICE WOULD YOU GIVE FACILITIES PLANNING TO EXPAND, REPLACE OR MODERNIZE THEIR X-RAY CAPABILITIES IN 2026 AND BEYOND?
CHAMBERS: I would start by ensuring you have a clear understanding of your organization’s strategic goals. Capital is often limited, so it’s important to invest in solutions that will meet your needs not just today, but for the next 5 to 10 years. Understanding your organization’s identity helps avoid unnecessary features while ensuring you have the essentials to succeed. AI can feel overwhelming right now. With it being so new, it’s easy to get caught up in the excitement of the latest technology, but it may not be necessary for your specific location. Instead, focus on partnering with an OEM that offers flexibility, one that can customize and scale with you over time without requiring major hardware purchases. Building a relationship with an OEM that acts as a true partner, rather than just a transactional vendor, can be a key factor in your long-term success.
DOSSA: It seems as if we are always in the process of expanding throughout our system. Having vendors of choice via a non-obsolescence replacement plan and established equipment configurations are significant improvements for us. Our vendors know what we need which makes quoting/
selection process much easier and less time consuming. While it will take a few years to replace a lot of equipment, the standardization we have seen in 3 years is already paying off in patient care/access, staffing confidence/flexibility, HTM and physics efficiencies. AHRA offers a white paper on equipment non-obsolescence planning that is incredibly helpful if your organization is interested in pursuing.
PHILLIPS: Engage stakeholders early – radiologists, technologists and IT – to ensure smooth adoption. Meet with vendors and conduct thorough research to identify solutions that fit your organization’s volume, throughput and financial goals. Visit other facilities to gather feedback from leaders and frontline staff. Finally, develop a strong business plan with a clear ROI, as budgets remain tight across healthcare organizations.
WALLING: Start with workflow and patient needs, not just equipment specs. Engage technologists early, standardize protocols across rooms and sites, and prioritize systems that support automation, AI-readiness and interoperability. Plan for flexibility – volumes, staffing models and clinical demands will continue to shift. Finally, think long-term: invest in platforms with clear upgrade paths and strong vendor support to ensure your X-ray fleet remains efficient, safe and future-ready.
WHITEHOUSE: Futureproofing your investment is key. Select systems that offer modularity and scalability, enabling upgrades without full replacement. Prioritize interoperability with RIS/PACS and consider mobile DR solutions to enhance flexibility and patient access. Evaluate vendors based on service support, training programs and technology roadmaps to ensure alignment with long-term goals. Finally, remember that lowest cost does not always equate to best value – focus on solutions that deliver durability, adaptability and clinical excellence. •
This month’s article was sponsored by X-ray America. For more information on this company, visit x-rayamerica.com.

AMarketsandMarkets.com report on the diagnostic imaging market states that the market is projected to reach $32.90 billion by 2030 from $26.51 billion in 2025, at a CAGR of 4.4% from 2025 to 2030.
The primary factors propelling the expansion of this market are the introduction of innovative, technologically advanced products by leading industry players and the rising incidence of chronic diseases among the global population. These advanced products, which often incorporate cutting-edge technologies such as artificial intelligence, telemedicine, and personalized treatment solutions, are designed to enhance patient outcomes and streamline healthcare delivery. Additionally, the increasing prevalence of chronic conditions such as diabetes, cardiovascular diseases, and respiratory disorders is intensifying the demand for effective and efficient medical interventions, further driving market growth.
The global medical X-ray generator market is projected to grow from approximately $2.8 billion in 2026 to $4.9 billion by 2036, representing a CAGR of 5.8%, according to a press release from FactMR.
This growth is fueled by rising demand for diagnostic imaging, healthcare infrastructure expansion, and rapid adoption of digital radiography. The market is transitioning from conventional analog systems to high-frequency, AI-enabled X-ray generators, enhancing image quality, workflow efficiency, and patient safety.
The press release adds that market drivers include:
• Healthcare Infrastructure Expansion: The number of hospitals and diagnostic centers is increasing globally, especially in Asia-Pacific, which now accounts for 35% of global X-ray installations. Replacement and upgrade cycles in mature markets contribute 25-30% of annual unit sales, reflecting continuous demand for high-performance generators.
• Aging Population and Chronic Diseases: Global chronic disease prevalence is increasing at an annual rate of 3-4%, while the population aged 65+ is projected to reach 1.6 billion by 2050. This demographic requires frequent imaging; X-ray procedures are expected to rise by 6-7% annually, driving generator demand.
• Technological Advancements: High-frequency X-ray generators now account for 60% of total sales, replacing legacy low-frequency units. AI-assisted imaging adoption is projected to grow from 10% of installed systems in 2025 to 45% by 2036, improving diagnostic accuracy and reducing repeat scans by 20-25%.
• Digital Radiography Transition: Digital radiography adoption has reached 70% in North America and Europe, with emerging markets like India and Brazil expected to exceed 50% by 2030. Digital systems reduce radiation exposure by 30-40% and accelerate image processing by 50-60%, driving widespread replacement of analog generators.
In conclusion, the press release states that the medical X-ray generator market is poised for sustained, data-driven growth through 2036. Adoption of AI, digital radiography, and portable systems will reshape the industry via increasing global accessibility while improving diagnostic efficiency and patient safety. With projected revenue nearing $4.9 billion, stakeholders have clear opportunities to leverage technological innovation and regional expansion.
Future Market Insights reports that the global X-ray system market is estimated to be valued at $12.2 billion in 2025 and is projected to reach $16.7 billion by 2035, registering a compound annual growth rate (CAGR) of 3.2% over the forecast period.
The X-ray system market is undergoing steady transformation driven by increased healthcare digitization, rising imaging volumes and sustained investments in radiology infrastructure. The market is witnessing a consistent shift toward digital radiography and flat-panel detector technologies to improve workflow efficiency and image quality.
Healthcare providers are prioritizing equipment upgrades to reduce radiation exposure and enable advanced imaging protocols supporting early disease detection. Regulatory initiatives incentivizing the replacement of legacy analog systems with digital solutions have contributed to modernization across public and private health systems.
Additionally, integration of artificial intelligence for image enhancement and workflow automation has been recognized as a critical factor supporting future growth. As demographic trends accelerate chronic disease incidence, the X-ray system market is expected to benefit from sustained capital spending and broader access to diagnostic services. •

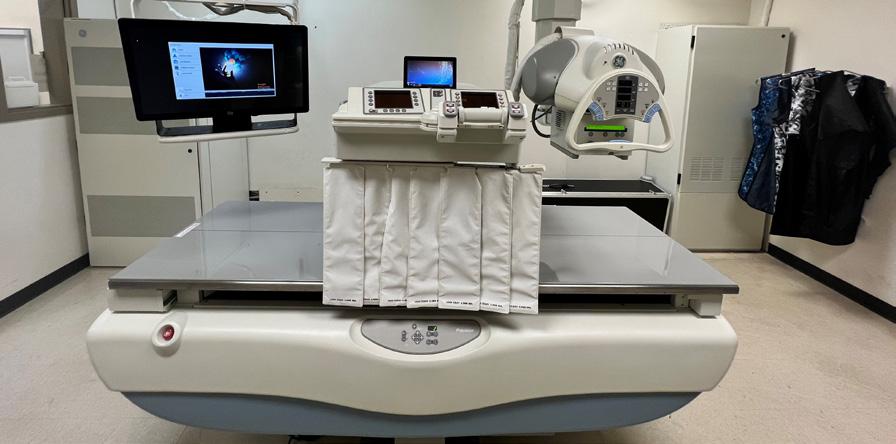
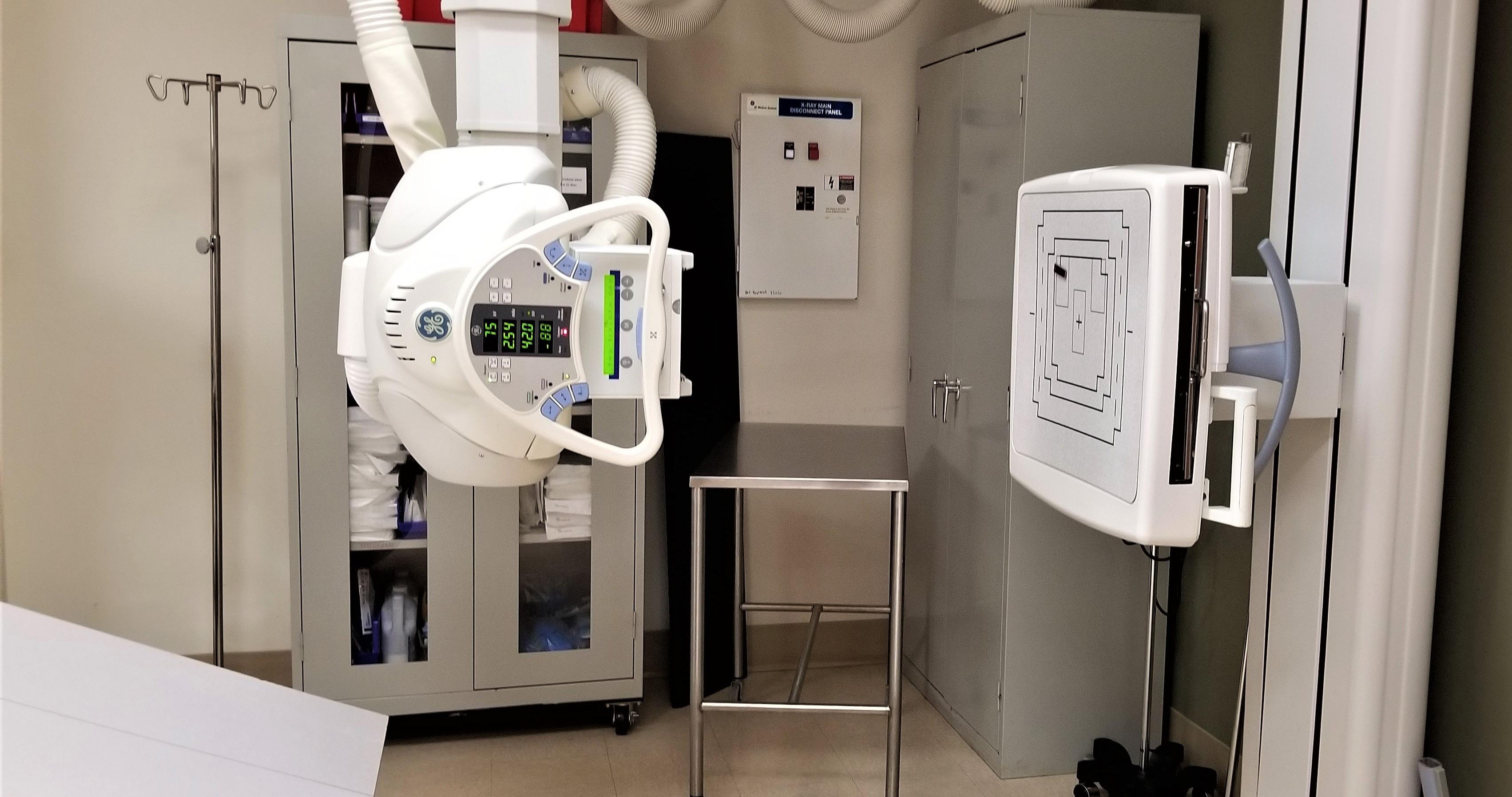
GE HealthCare’s Definium Pace Select ST is a tool X-ray departments can use to conquer today’s challenges. This versatile, digital, floor-mounted system can produce consistent, high-quality images typically generated on premium systems at a value price point. This image quality can be easily achieved – even with novice technologists operating the systemthanks to a combination of hardware, software, and assistive technology. A high-powered X-ray generator and large, high-resolution FlashPad Select detectors are the key components that enable imaging of a complete range of anatomies and patient sizes. In addition, the system acts as a personal assistant for technologists to help with protocol and exposure factor selection, positioning of the system and with making quality checks before images are sent to radiology. AI-driven Helix advanced image processing software provides consistent image quality despite variations in exam condition with customized image looks that radiologists demand. With a simple, easy-to-learn and operate design, the system can help prevent user errors and also help technologists efficiently deliver imaging exams that impart clinical confidence, helping to lower staffing burdens and reduce rejects and repeats.

Konica Minolta Healthcare Americas Inc.’s new KDR FMT and KDR FMT+ digital radiography (DR) systems represent the next evolution in floor-mounted DR systems from Konica Minolta, designed to deliver high image quality, reliability and workflow efficiency. Building on the trusted performance of the KDR product line, the KDR FMT and KDR FMT+ feature Konica Minolta’s signature tube-mounted control interface for a streamlined patient workflow. The KDR FMT is a fully manual system, ideal for low- to mid-volume imaging needs, offering precision and ease of use. The KDR FMT+ adds motorized
Micro-X Limited has updated its Rover mobile X-ray system with the international launch of the next-generation platform, engineered to deliver improved workflow, imaging performance, and ease of use. The new Rover evolves Micro-X’s proven lightweight, motor-free design, with enhancements including the latest Lumen glass-free high-resolution detector, in-bin charging for improved readiness, a larger high-definition touchscreen interface, improved serviceability, and a more compact stowage footprint for use in constrained clinical environments. Together, these upgrades strengthen the Rover’s role in fast, accurate, point-of-care digital radiography. Using Micro-X’s proprietary Nano Electronic X-ray Technology, the Rover delivers high-quality digital radiography with exceptional maneuverability, gentle navigation across hospital floors and lifts, and minimal maintenance requirements. The new in-bin charging solution removes the need for external cabling and reduces downtime, ensuring the Rover remains ready when clinicians need it most.
*Disclaimer: Products are listed in no particular order.
movement and automatic detector tracking, making it the perfect solution for mid- to high-volume practices seeking to boost throughput and enhance patient care. The systems deliver imaging flexibility with a table that supports up to 700 pounds and a wall stand for all imaging views required in general radiography, accommodating patients who are standing, sitting or lying on the table. Both systems are available with Konica Minolta’s ULTRA imaging software featuring REALISM image processing for exceptional contrast sensitivity and sharpness.


Philips’ Radiography 7300 C, a ceiling-mounted digital radiography solution, addresses fast throughput and diagnostic confidence to address challenges. Its AI-enabled Smart Collimation Thorax (SCT) algorithm adjusts detector height and proposes collimation for each chest-upright patient based on data from a 3D Camera. Smart Collimation Thorax reduces exam time by
up to 35 seconds, resulting in up to 20 minutes of daily time savings for the medical team. To further reduce costs, Philips is backing this system with a 20-year expected service life (15 years of full support, 5 years of limited support), which helps avoid unnecessary additional investment in X-ray equipment and room construction.
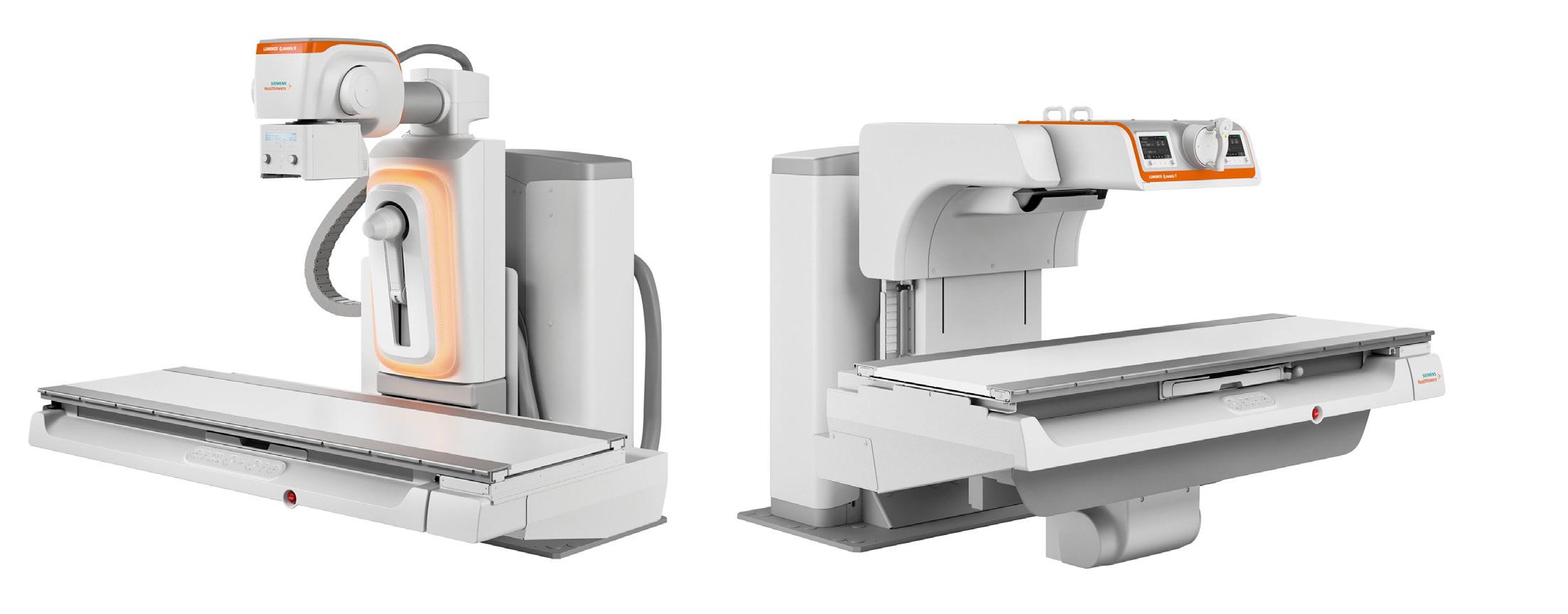
Luminos Q.namix R and Luminos Q.namix T
The Luminos Q.namix R and Luminos Q.namix T multifunctional imaging platforms from Siemens Healthineers are designed for specialized and complex radiography and fluoroscopy examinations. The platforms can simplify workflows at low patient radiation doses through intuitive ergonomic controls, integrated components and built-in workflow guidance supported by artificial intelligence. The remote-controlled Luminos Q.namix R can be operated either in the control room or from inside the exam room at the bedside. It is designed
for fluoroscopy procedures that include lower and upper gastrointestinal exams, as well as swallow and joint injection studies that require contrast media. It also can be used for radiography exams, including general exams of the chest, bones, and joints; and orthopedic imaging, including automated long leg and long spine imaging. The Luminos Q.namix T with tableside control is ideal for non-ambulatory patients and examinations that require intensive patient interaction, including pediatrics, bariatrics and gastroenterology. •






• A niche job board for the HTM and imaging communities powered by TechNation.
• 3,800+ actively looking biomedical and imaging professionals.
» Completely free and confidential registration and application process.

Featured Employers: Agiliti, Block Imaging, Intelas Health, Renovo Solutions, TRIMEDX, and more!
htmjobs@mdpublishing.com for posting inquiries htmjobs.com to register today
• The fastest growing HTM talent network in the country.
• 350+ open opportunities throughout the United States.
» A variety of posting options ranging from single-job postings to 12-month unlimited memberships.
BY MATT SKOUFALOS

As diagnostic imaging study volumes spiral and patient wait times for service increase, technology vendors and market-watchers alike all seem to be solving for the same, underlying issue: efficiency. With shortfalls in access to skilled, experienced professionals in the technologist
space, and telehealth options increasing in speed and quality, equipment manufacturers believe the answer lies where most of the rest of the economy believes it is to be found as well: artificial intelligence (AI) powered solutions.
At the outset of 2026, they foresee a landscape that for the foreseeable future will be driven by a focus on au-
tomated processes, be they in image acquisition and refinement or software-assisted decision-making. The fundamental questions underpinning this push that remain to be answered nonetheless linger. Just how good is AI at doing all the things it’s being tapped to do, and, perhaps as important, who’s going to be paying for it?
These questions were hot topics at the Radiological Society of North Amer-
ica’s (RSNA) 111th Scientific Assembly and Annual Meeting (RSNA 2025).
Pooja Pathak, vice president and general manager of mammography at GE HealthCare, said that her customers are looking for cost-effective technological (and non-technological) solutions that will help drive clinical impact and streamline workflow.
Breast imaging is a “very high-volume” line of service, Pathak said, with 40 million mammograms performed every year. Ninety percent of images come back normal, and so radiologists who are looking for changes to breast tissue over time, need high-quality images that are clear, consistent, and support high-confidence decision-making, screening out negative results to sharpen their focus on tougher cases.
“In mammography, what we offer is transforming the exam workflow,” Pathak said. “On the gantry itself and in the room, we provide zero-click acquisition, so that when the exam starts, the technologist can be focused on the patient and not the screen or the equipment.”
“We’ve eliminated and simplified steps, and brought in prior information to compare different laterality of images at the console itself,” she said. “This ensures that the exam quality is maximized in efficient workflow.
The primary GE HealthCare mammography platform is Senographe Pristina, which competes on a reputation for being patient-centric and clinically reliable. The Pristina Via, which debuted at the end of 2024, is designed to emphasize workflow efficiency, with a fast image-to-image cycle time that relies upon vendor-neutral prior image comparison to eliminate slowdowns. Pathak described it as “thinking systematically to simplify in-room workflow.”
Pristina Recon DL, its latest offering, leverages advanced AI-powered software to detect cancers as early as possible with enhanced 3D image reconstruction.
“It uses two deep learning models to provide clear, sharp, consistent
image quality,” Pathak said. “It seamlessly integrates with the customer’s existing technology. In addition, it allows customers to have simplified workflows, and deploys in multivendor fleets.”
AI-driven technologies are embedded throughout the mammography workflow, from image reconstruction to reading and interpretation, thanks to a partnership between GE HealthCare and imaging informatics partner DeepHealth, which produces a cloud-based, AI-enabled viewing system for exam room workflow and interpretation.
“Radiologists can prioritize their work lists to look by severity of cases, and have an AI aid in the diagnosis itself to assess risk and have faster,
“Saving time and the mindshare of radiologists to work on critical cases, that’s where we see future direction and impact of AI.”
- POOJA PATHAK
more confident diagnoses,” Pathak said. “Any findings there are automatically uploaded to the report. You have clinical insights into where the radiologist is reading.”
Pathak said that GE HealthCare is working to seek out other opportunities to embed AI-powered solutions into mammography functionality that helps with risk assessment in a way that helps eliminate “one-size-fits-all” delivery of care.
“What’s the optimal, more personalized imaging experience for women?” she said. “There’s lots of exams that need to be retaken, and AI
technology is available, almost like a copilot, to have a second pair of eyes before they rule out whether the study needs to be recalled. Saving time and the mind-share of radiologists to work on critical cases, that’s where we see future direction and impact of AI.”
The inclusion and expansion of AI-powered technologies in the medical imaging space underscores how many formerly hardware-driven solutions are now being approached with software-based approaches; Pathak said GE Healthcare is working on both.
“We’re innovating in both areas, and you will see more from us,” she said. “Evidence does show that AI in mammo can be an effective aid to diagnosis. All of these things are not just about speed and delegating [diagnostic responsibility]; they’re also about improved patient access.”
“I do think that there’s some guardrails that will keep a good tension between having the right level of evidence about how much you can automate and how much you can scale while still providing the best clinical outcomes in the safest possible way,” Pathak said. “We are continuing to get more involved in creating that change so that industry can be a partner with clinicians and key government officials to drive at the same speed as access and reimbursement.”
Michael Cannavo, president of Image Management Consultants of Winter Springs, Florida, said that radiology administrators’ goals may differ only slightly depending upon their work environments. In a hospital setting, Cannavo said, the majority of those motives are profit-driven, including employee retention. In private practice, however, decisions turn around what is best for the radiologists who own and operate the business. Like technology vendors, decision-makers are relying upon AI-powered technologies to deliver on both.
“You’ve got to serve God and Caesar both,” Cannavo said. “They’ve got to keep the radiologist happy and keep the hospital happy, and they have two entirely different agendas.”

“In a hospital setting, administrators want to keep their technologists happy because it’s hard to find a good tech,” he said. “Here, the use of AI is very important moreso from the reporting than the diagnostic standpoint; workflow versus clinical. AI can look more closely at clinical indications for the report, and how the report is being generated is a lot faster.”
“There are significant benefits of the advancements made in the image processing AI space, and radiologists still use it. they wish things could be a little faster in terms of automating their workflows.”
- PARAG PARANJPE
“Anything that is going to streamline the process is of value,” Cannavo said. “It all comes down to what’s going to make us money, save us money, keep employees happy, and make their jobs easier. We all want to improve patient care, but they’re not going to take the money out of their pockets to improve patient care. If AI is one of the ways that it’s going to do it, people are going to use it.”
Cannavo cited vendors like Aidoc and RadAI, producers of software solutions that generate findings from imaging studies that help inform radiologists’ diagnoses. As these technologies continue to advance, he said there are rumblings among larger practice groups that AI-powered solutions could be leveraged to produce preliminary imaging reports. The question remains whether the products are themselves airtight enough to be used in such a fashion.
“Is there a potential for a lawsuit from a misdiagnosis?” Cannavo asked. “Absolutely. Ninety-eight to ninety-nine-percent accuracy sounds good, but two percent of 200,000 procedures is a lot of missed diagnoses. That’s why it’s an adjunct to radiology, it’s not a replacement for it.”
“The reality is that a radiologist is the only one who’s recognized to sign the report, and CMS is not going to pay for AI to do it,” he said. “If AI


misses something, can you sue the AI company?”
Cannavo also spoke about the landscape for AI vendors as being distributed among several hundred small, specialized vendors, each of whom may produce only a few, purpose-built algorithms with very specific utilities. He wondered at the future commodification of the product in a landscape where only a few buyers are shopping for mostly the same things.
“There’s almost 1,200 algorithms for diagnostic imaging interpretation from 600 or 700 different vendors,” Cannavo said. “The market is nowhere big enough to support that. Outside of the vendors, a lot of facilities are using their own databases to train an AI model so they don’t have to pay a third-party company.
“A lot of these algorithms are going to come down into the sub-$20 and sub-$10 level,” he said. “Are they doing better for the patient if there’s a better algorithm out there?”
Cannavo also pointed to how AI-powered algorithms are being utilized in the practice space at present as an indication of future trends. Two of the largest diagnostic imaging practice groups in the marketplace – teleradiology provider vRad and the 400-center network Radnet – are offering patients additional fees-forservices to have AI over-read their diagnostic imaging studies in addition



to getting radiologists’ takes.
“It’s great in one sense, but in another sense, it sets up a dividing line between the haves and have-nots,” he said. “If I’m a Medicare patient, I’d love to have it, but I might not be able to spend the money to have AI to provide that second opinion.”
“The goal is to get the cost down and the quality up,” Cannavo said. “If you’re using AI, somebody has to pay for it, whether it’s CMS or the hospital.”
Parag Paranjpe is CEO of HealthLevel, based in Mountain View, California. The company is behind Foundations, a software solution that provides analytics and workflow tools to improve operational efficiency. Paranjpe said that efficiency remains top-of-mind for any decision-maker in the field. Although many technological developments are advertised as being AI-enabled, or AI-capable products, frontline radiologists remain focused on features that can improve the speed and quality of their diagnostic reads, he said.
“There’s always advancement and improvement of the ‘pixel’ AI tools,” Paranjpe said – those designed to improve diagnostic quality – “but I haven’t heard about the universal ‘I love this’ capability just yet.”
“There are significant benefits of the advancements made in the image processing AI space, and radiologists still use it,” he said; “they wish things could be a little faster in terms of
automating their workflows.”
Paranjpe said that discussions among radiology leaders is consistently focused on how to abate their ever-expanding volumes of unread images while delivering the quality and speed required by industry performance metrics, which prominently includes reimbursements. HealthLevel is focused on addressing operational inefficiencies through greater data transparency to reveal which strategies and technologies are working and which are not.
“We work with customers who had a feeling that the solutions that already exist go beyond image management and integrity,” Paranjpe said. “They have found more accuracy putting all that information together to drive the benefits.”
“Once you start observing it, you start doing a better job.”
In addition to the question of “who’s paying for AI,” Paranjpe said key differentiators in the sector have more to do with their ability to integrate the technology into their existing operations. For a company like HealthLevel, which provides an integrated data platform, the task that remains is collecting information about how the technology is being used, and how to drive interoperability among those discrete offerings.
“At HealthLevel, we use AI tools extensively, and everyone in the company is expected to know, learn and
practice how to use AI tools,” Paranjpe said. “But in a healthcare setting with controlled workflows, it’s not so simple. How these tools actually become useful at the fingertips of practitioners is really important. This is the whole zeitgeist. It’s here to stay, and it’s a good thing, but just like any new technology, we have to learn how to use it.”
Whereas many laypeople are familiar with public-facing software tools like OpenAI’s ChatGPT, enterprise-class AI technologies must improve operational workflow for businesses in order to be valuable, he argued. Software-based solutions that strive to deliver a “zero-worklist” status in the imaging suite is the aspirational aim of all workflow-driven solutions.
“There is so much data, so many drivers, that the computer knows better than anyone else which is the highest-priority study,” Paranjpe said. “That will change the background incentives.”
Katie Grant, Ph.D., head of the magnetic resonance (MR) business at Siemens Healthineers North America, described its recently cleared Magnetom Flow platform and 510(k)-pending Biograph One PET/MR scanner as two of the most recent developments the company is offering to address the overarching customer demands for anything that will help improve workflow and efficiency.
“Folks are so bogged down by the
number of patients coming through, and, as we all hear about daily, the number of people to do the work is dropping,” Grant said. “The staff needed to run it — the nurses, the technologists, the assistants, even the radiologists — are now in shortage. How do we make it easier for our customers and the patients?”
The 70-cm-bore, low-helium Magnetom Flow is a 1.5-Tesla system built around DryCool low-helium technology that helps contribute to its smaller footprint and more versatile deployments. The lighter-weight scanner is as easily installed in an interventional radiology suite or an emergency room as other places such devices previously couldn’t be added. Grant said its energy efficient design also “hits on a lot of sustainability targets,” with the
our automation off at any point if you have a really strong technologist who can manipulate the machine. We’ve tried to build in as much intelligence into these systems as we can.”
Another expression of the AI-powered software approach to diagnostic imaging at Siemens Healthineers is the Deep Resolve Boost software, which Grant said can help to cut exam times in half, greatly reduce motion-driven image artifacts, and enhance patient comfort.
“A lot of our customers have fourto eight-week backlogs,” she said. “If you’re hurting, that’s a long time to wait to get an exam. We were able to shorten exam slot times to sometimes double the amount of exams our customers can order in a day, and that really helped chip away at that backlog.”
“In a hospital setting, administrators want to keep their technologists happy because it’s hard to find a good tech”
- MICHAEL CANNAVO
potential to cut energy consumption by as much as 30 to 50 percent per system for one of the most intensive electricity-using devices in the hospital. And, of course, like the other technological improvements most customers are seeking, it’s compatible with AI-powered technologies that automate decision-making, limit software interactions, and generally enable lower-skilled or less-experienced staffers to support the high-volume needs of most diagnostic imaging workspaces.
“We’ve tried to simplify MR as much as possible as we move towards automated MRI,” Grant said. “Push-button exams means you no longer have to have a very knowledgeable or experienced tech, improving speed. You can also turn
The Biograph One combination PET and MR scanner capitalizes on Siemens Healthineers pioneering PET-MR on a single platform, making it useful for theranostics applications as well as shortened patient prep times. The device leverages a new type of simplified, extra-large body coil that enables rapid image collection as well as full-body imaging, which is increasingly in customer demand, Grant said.
“In my mind, it allows you to bring imaging to the patients rather than making them come to you, which will also help from an access perspective,” she said.
“We are really helping to drive access to care as much as we can through our technologies.” •
RSNA 2025 also featured the introduction of new technologies via the latest medical imaging advances and solutions in CT, MRI, AI, theranostics and more. A few highlights were:
• Fujifilm Synapse One: Cloud-based enterprise imaging solution for outpatient imaging centers: integrates RIS, PACS, scheduling, 3D imaging, physician portals – scalable end-toend workflow.
• Bayer MEDRAD Centargo CT Contrast Injection System: 510(k) clearance from the FDA to expand the use of compatible contrast agent presentations to include single-dose vials in addition to the previously cleared Imaging Bulk Package (IBP) presentations for Ultravist (iopromide), Isovue (iopamidol), Optiray (ioversol) and Omnipaque (iohexol).
• GE HealthCare Signa Bolt 3T MRI Scanner: High-field, clinical wide bore 3.0T MRI system seeks to combine ultra-high gradient performance, intelligent digital RF architecture, and sustainable design to deliver precision imaging, fast workflows, and seamless clinical-to-research flexibility, all with exceptionally low energy consumption and operational costs.
• Carestream 360° Analytics Dashboard: Enterprise-level analytics platform for radiology departments; provides real-time data and actionable insights to optimize operations, resource use, image quality and team productivity – helpful for high-demand environments.






As diagnostic imaging systems continue advancing in sophistication, connectivity, and performance expectations, the technical demands placed on imaging service professionals grow accordingly. Today’s service responsibilities require an understanding of system design, operating behavior, diagnostics, performance verification, and safety – not simply procedural familiarity. Training quality directly influences the ability to sustain up-time, manage life cycle performance, and support patient care.
Since 1985, RSTI has maintained a training philosophy centered on relevance, technical integrity, and real-world readiness. Imaging systems evolve; effective training evolves with them.
To prepare service professionals for current healthcare environments, RSTI continually invests in acquiring and maintaining the systems that technicians actively support in the field. These platforms are fully operational and used to teach servicing, diagnostics, maintenance, repairs, and
verification in conditions that reflect real experience. Recent additions include: Philips Azurion, Siemens Artis Q, Philips Ingenuity CT, GE Pristina 3D Tomosynthesis Mammography, GE 450W MRI Platform (covering GE Signa, Optima, and Discovery MRI Family including 450W/750W, Voyager, Architect, Artist, Creator, Explorer, Star, Aviator), Siemens Force CT
Supporting these systems also requires investment in infrastructure such as power delivery, cooling, RF considerations, networking environments, safety systems, and specialized diagnostic tools. The intent is simple: match the technical reality of the field so training aligns with what professionals encounter every day.
Imaging platforms continually change through design evolution, software revision, and updated performance expectations. Training must therefore remain current, disciplined, and technically accurate. RSTI conducts ongoing curriculum review to ensure material reflects present technology conditions and real service requirements.
Core curriculum priorities include:
• maintaining accuracy in system architecture content
• integrating relevant failure scenarios and service lessons
• aligning maintenance and verification practices with current standards
• refining troubleshooting methodologies to support efficient diagnostics
• upholding safety, compliance, and performance expectations
Training structure is deliberately progressive: understanding how systems function, examining subsystem interaction, applying diagnostics, executing maintenance and repair, and validating performance. The outcome is readiness supported by comprehension —rather than reliance on procedural repetition.
RSTI treats hands-on activity as essential. Imaging service responsibilities involve tactile procedures, analytical decision-making, adjustment, alignment, testing, and QA verification – skills that develop through direct engagement.
To support learning effectiveness, RSTI reinforces training through the VARK learning approach: Visual – system schematics, diagrams, and performance visualization, Auditory – guided explanation and collaborative discussion, Reading/Writing – technical documentation and structured reference learning, and Kinesthetic – applied, hands-on system interaction. This combination improves retention, strengthens comprehension, and builds confidence when transitioning from training to live service environments.

High-quality training strengthens industry workforce stability as much as individual capability. As healthcare organizations continue to face staffing challenges and technology demands, structured and technically credible training is essential to sustaining service readiness.
RSTI also supports the military community as part of this broader capability effort. The organization is DoD SkillBridge™ approved and GI Bill® approved, helping transitioning service members apply their technical backgrounds toward imaging service careers.
Todd Boyland, CEO of RSTI Training, describes the responsibility clearly:
“Our industry relies on imaging systems performing exactly as designed. To support that responsibility, service professionals deserve training built on real equipment, real experience, and curriculum that reflects the systems in the field today. That commitment guides every decision we make.”
CT platforms continue advancing in speed, efficiency, and image computation. MRI systems evolve in RF behavior, gradient capability, and software environments. Interventional, fluoroscopy, and mammography systems integrate increasingly sophisticated control and quality systems. Across modalities, technical complexity and integration continue to expand.
Meeting these realities requires training environments grounded in: continual system investment, disciplined curriculum maintenance, structured learning design, meaningful hands-on participation, sustained commitment to workforce capability. This remains RSTI’s standard. •
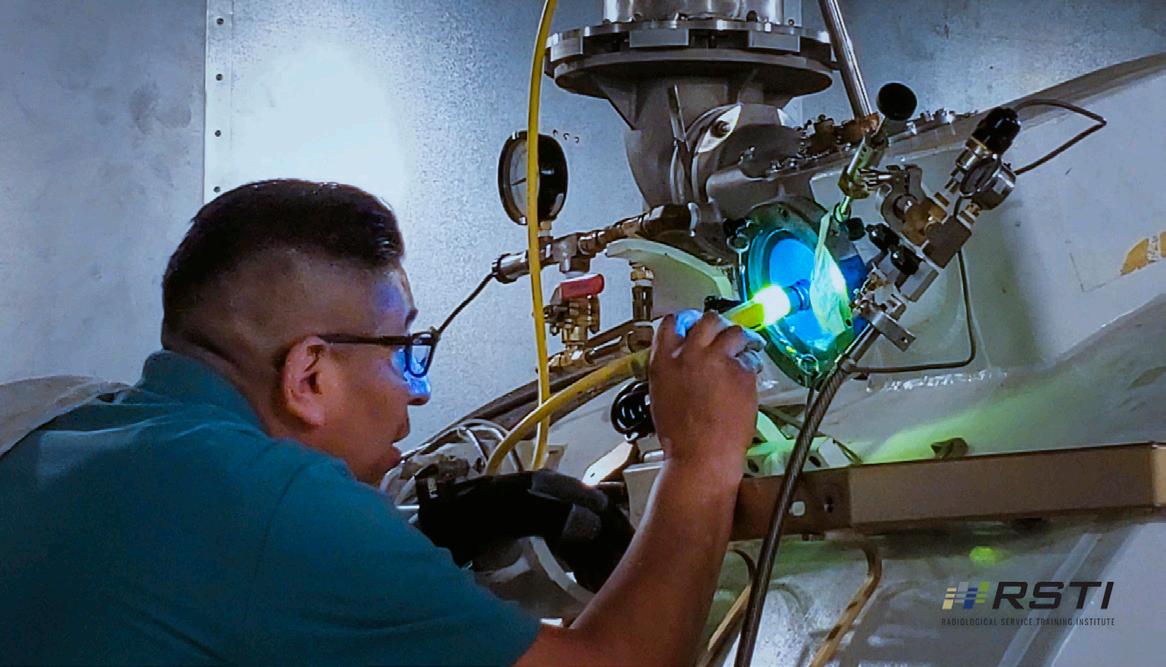

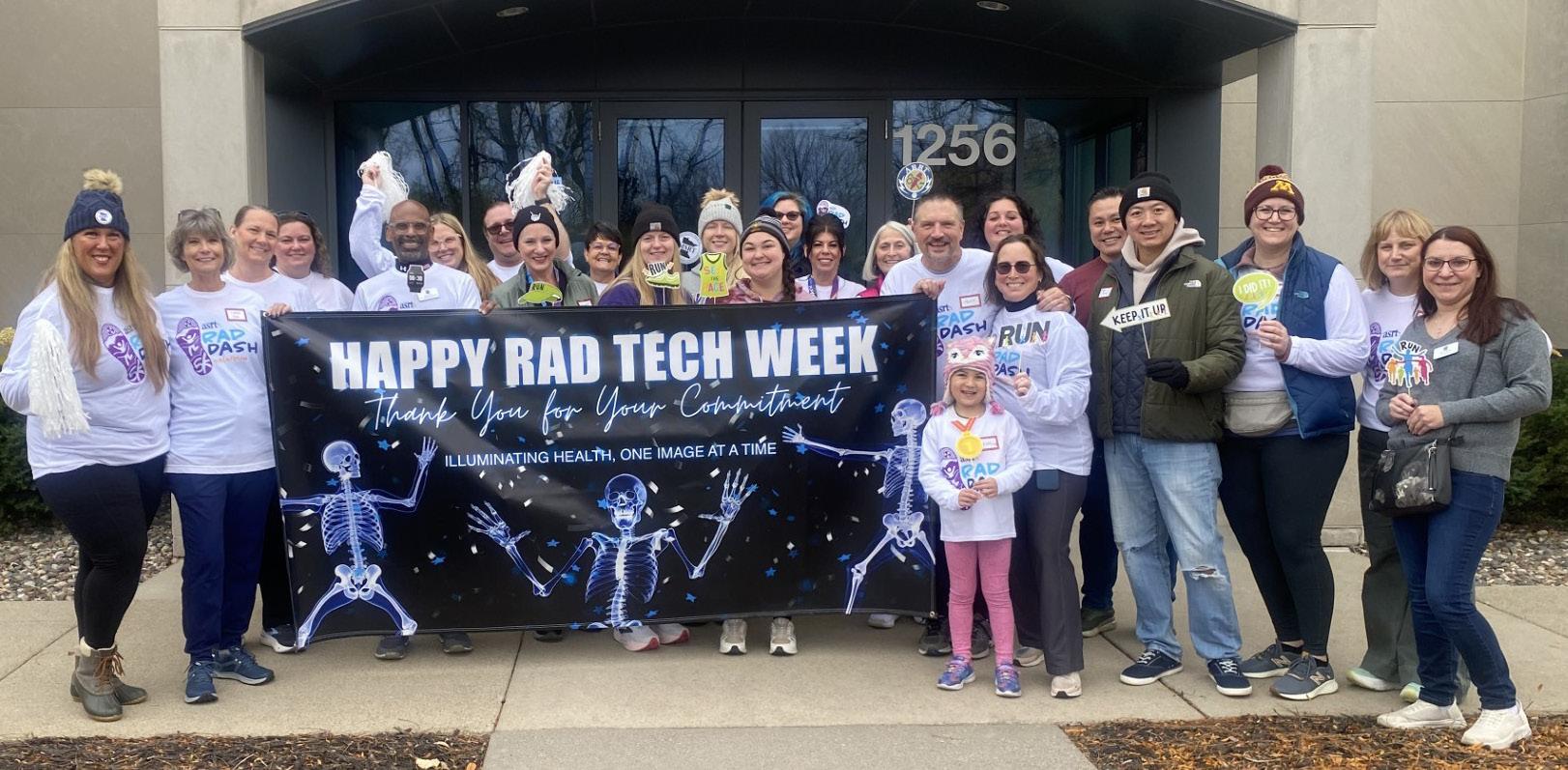

BY LEE ROSS
On Nov. 8, 2025, the American Society of Radiologic Technologists held the RAD Dash 5K Run/Walk in Albuquerque, New Mexico. Medical imaging and radiation therapy professionals from around Albuquerque and beyond enjoyed the sunny, late-fall day. The event was held to celebrate medical imaging and radiation therapy professionals, and the meandering, sandy trails and cottonwood trees lining the Rio Grande offered a great location to do just that.
In addition to the local event, ASRT affiliate societies, businesses and other groups participated virtually, holding events across the country. These events are not only an excuse to exercise and enjoy the outdoors but also build connections with other members of the profession, according to Josh Lucero, A.S., R.T.(R), a technologist at Presbyterian Rust Medical Center in Rio Rancho, New Mexico, a city near Albuquerque.
“It was all around a great time,” he said. “I love being able to run with patients and other technologists from across modalities and facilities, and to meet their significant others.”
Lucero brought his 6-year-old son, Landon, with him. On the day before the race, Lucero
took Landon and Landon’s cousin to the prerace packet pickup at the ASRT office, which is nestled at the foot of the Sandia Mountains.
Picking up the packet was like a takeyour-child-to-work day, Lucero said, because they toured the ASRT Museum and Archives’ interactive displays and educational exhibits. Landon and his cousin’s favorite display was a digital touchscreen, which allows visitors to assemble a complete skeleton using individual medical images.
“He was amazed by the technology we use, and he loved putting the skeleton together. It was great because he learned a lot about what his dad does, and on the next day, at the race, he saw the type of community we have in our profession,” Lucero said.
Visitors often remark on ASRT’s museum, which showcases the progress of the profession, starting from Wilhelm Conrad Roentgen’s discovery of the X-ray on Nov. 8, 1895 – not coincidentally the same day as the RAD Dash. In addition, the museum tracks ASRT’s history, including how it was founded by just over a dozen individuals in 1920 and grew to about 2,500 members by 1946, when the Society established its first office in Fond du Lac, Wisconsin. (The Society has nearly 156,000 members today.)

That history is the reason the Wisconsin Society of Radiologic Technologists held its RAD Dash in Fond du Lac, according to Christina Smith, Ed.D., R.T.(R)(M). Smith, who is president of the WSRT, added that the event’s venue, Lakeside Park on the shore of Lake Winnebago, includes a 40-foot-tall lighthouse and covered bridges.
“We chose Fond du Lac due to its history, its great park and because it’s centrally located,” Smith said. “Our members were excited about the tie-in to ASRT.”
Another way Wisconsin helped build excitement was by framing it as a rivalry against its neighbor, the Minnesota Society of Radiologic Technologists. MSRT President Afton Jena, B.S., R.T.(R)(M)(BD), said she developed the idea with WSRT Chair of the Board Miranda Hurley, M.Ed., R.T.(R), to drum up a “friendly border battle,” similar to the Green Bay Packers-Minnesota Vikings rivalry.
Minnesota won the numbers game with 49 participants to 30, but “in the end, both societies won because we collaborated and it got people talking about the event,” Jena said. “I’ve spoken to affiliate leaders in Missouri, Iowa and North Dakota, and they love the idea of a friendly competition. Who knows? We could call it a Cornfield Clash for the RAD Dash.”
For the Minnesota event, the MSRT also collaborated with the American Registry of Radiologic Technologists, whose headquarters are in St. Paul. They partnered under the name “The North Star Scanners.”
Collaborative events like these align with one of Jena’s goals as MSRT president: to foster a family atmosphere among society members. To that end, MSRT participated in the Making Strides Against Breast Cancer event hosted by the American Cancer Society in October 2024 and held a Relay for Life event on Aug. 9, 2025. The society has plans to work with local Marines on a Toys for Tots event, and host or participate in events that benefit Susan G. Komen for the Cure for Breast Cancer, the Special Olympics and Ronald McDonald House Charities.
“We want to let patients and their loved ones know that they aren’t alone in their journey. Their fight is our fight,” Jena said. “These events make memories that become the glue holding our professional family together. They transform ordinary days into extraordinary ones and strengthen the bonds that make us resilient, visible and united.” •
Lee Ross is the managing editor of Scanner, the American Society of Radiologic Technologists member magazine.






BY NICOLE DHANRAJ
There are specific radiology questions we ask so often that they become automatic.
“Can you take that off?” is one of them. Most days, it truly is simple. Jewelry comes off, the exam proceeds, and no one gives it a second thought. But now and then, that question lands with a weight we don’t immediately anticipate.
I once had a Native American patient wearing a lot of beaded jewelry around his wrists and ankles. He told me the beads honored deceased ancestors, and I paused to acknowledge their sanctity and asked if he could take them off. He told me he had them on for 7 years, and he would have to explain this to his elders.
I paused again, not because I didn’t believe him, but because I wasn’t immediately sure how to proceed. I explained that I understood the importance of what he was wearing, but that they needed to be removed for the exam. I also explained that because I couldn’t identify the materials or paint used on the beads, I couldn’t safely determine whether scanning him as-is
would be appropriate, especially given the possibility of burns. I told him, as clearly and calmly as I could, that he should let me know what he needed to do.
There was no clasp or stretchiness to the bracelets, and then, with a heavy sigh, he said he would cut them off.
That wasn’t what I wanted. Cutting something that meaningful felt wrong, and I didn’t like that decision resting solely on his shoulders without further consideration.
I called the radiologist to see if there was any way we could safely proceed with the beads in place. After reviewing the situation, the radiologist agreed that it was a risk we couldn’t responsibly take.
So, we explained the imaging limitation again and offered options, proceed (but with the beads off) or reschedule. There was no pressure. No urgency imposed.
But “reschedule” isn’t always a simple alternative.
For many patients, delaying an exam means time off work they can’t afford, transportation challenges, childcare issues or prolonged anxiety while waiting for answers. In some systems, it means weeks or months
before another appointment is available. Access to imaging is not evenly distributed, and patients know this. The choice to proceed is often shaped as much by practicality as by preference.
And still, it was awkward. He continued to talk about his elders and how they wouldn’t be happy as he cut the beads. I kept reiterating that he had a choice not to proceed. The exam moved forward. But the moment didn’t feel resolved.
That same weight shows up in other, quieter ways.
We see it when we ask some of our patients to remove clothing or change into a hospital gown. For many, modesty isn’t simply about comfort; it is tied to religious practice and personal dignity. Being asked to disrobe, even partially, or wear an open-back gown can feel deeply exposing or distressing, especially if privacy, coverage or the gender of staff isn’t carefully considered. What feels like a routine preparation step to us may feel like a loss of dignity to them.
Again, the issue isn’t that imaging requirements are unreasonable. Positioning, access, safety and image quality still matter. But it’s easy to forget how vulnerable these moments can be when we’re focused on getting the exam done.
What stayed with me wasn’t uncertainty about whether we followed protocol as we did. It was the weight of witnessing patients give up something meaningful to access care, even when the choice was informed and voluntary.
Across many cultures, items worn on the body and the way bodies are covered carry meaning far beyond what we can see. Sikh kara bracelets, Hindu sacred threads, Christian crosses, hamsa pendants worn in Jewish and Muslim communities as symbols of protection, Native American beads or medicine items, and religious clothing tied to modesty; these are not simply accessories or preferences. They can represent faith, ancestry, protection, grief and identity.
This isn’t about lowering imaging standards. Safety, diagnostic accuracy and image quality remain essential. It’s about recognizing that what feels routine to us can carry profound significance for someone else.
I still think about that patient. About the pause before I spoke, and the feeling of standing there knowing there was no perfect option. I had done what was clinically necessary, and I had done my best to be respectful, but that didn’t make the moment light. It made it heavy in a different way.
“Can you take that off?” is a question we ask without thinking.
But every once in a while, we feel the full weight of that question because we understand what it costs the patient, even when there is no other way forward. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.



DIRECTOR’S CUT
BY MICHELLE NOCERA
The start of a new year is an opportunity to reset. In radiology, where the pace is fast and the expectations are high. A new year becomes more than a calendar milestone. It is an opportunity to re-establish priorities, strengthen culture and refocus on what matters most – our people, our patients and ourselves.
As leaders, we define the tone for our teams. The energy we bring, the clarity we set and the consistency we model impact everything from employee engagement to patient experience to operational success. When we take time to intentionally set goals and embrace a positive, forward-thinking mindset, we don’t just elevate our own performance, we create a ripple effect across multiple departments.
Below are strategies for radiology leaders and setting the foundation for growth.
One of the most powerful motivators for any team is clarity. People want to know where we are going, why it matters and what role they will play in getting there.
Now is the perfect time to revisit your department’s vision.
Think about:
• What are your top three priorities?
• What clinical, operational or improvements are needed?
• What do you want your team to feel at the end of the year – supported, empowered, accountable, appreciated?
Once your vision is clear, communicate it early and often. Incorporate it into huddles, staff meetings and recognition efforts. When staff see consistency between your words and actions, engagement and trust grow with it.
The most effective goals are those that are realistic, measurable and connected to outcomes people care about.
Consider goals in three key areas:
• Employee Engagement
• Engaged teams outperform disengaged teams in quality, safety, productivity, retention and even patient satisfaction. Consider goals such as:
» Improving communication transparency with structured feedback
» Strengthening professional development opportunities
» Implementing new recognition strategies
» Increasing leader rounding frequency
• Patient Experience
• Radiology plays a unique role in the patient journey. Patient experience goals may include:
» Reducing wait times through better scheduling
» Enhancing staff-to-patient communication and scripting
» Improving wayfinding and physical spaces
» Ensuring technologists have the tools and support needed to succeed
• Personal and Professional Growth
• Too often, leaders put their own goals at the bottom of the list. Leadership requires commitment to your own development.
» Building organizational relationships
» Completing a certification or training
» Improving work-life balance
Positivity in leadership is not about ignoring challenges, it is about choosing how we respond to them. We experience equipment downtime, staffing constraints and clinical demands as part of our daily operations. We must be steady anchors in the storm.
Practice intentional positivity:
• Celebrate small wins weekly
• Highlight stories of compassion or teamwork
• Encourage gratitude practices within the team
• Redirect negative conversations into solution-focused ones
• Model grace under pressure
The tone you set influences the emotional environment of the entire department.
The most effective radiology departments are those where collaboration thrives across technologists, nurses, schedulers, radiologists, transport, IT and leadership teams. Prioritize:
• Rounding regularly with purpose
• Creating consistent communication pathways (emails, huddles, newsletters)
• Creating open-door spaces for staff to voice concerns and ideas
• Strengthening relationships between modalities
• Partnering closely with radiologists to align workflows, protocols and patient safety
When people feel informed and included, they take ownership of the work and contribute at a higher level.
Radiology professionals are skilled, compassionate and dedicated but we are also human. Burnout remains one of the top risks in imaging departments across the country. Leaders must drive conversations about wellness and model behaviors that prevent burnout.
• Encourage staff to take their breaks
• Rotate difficult assignments fairly
• Offer flexibility where possible
• Recognize when workloads are becoming unsustainable
• Support cross-training to reduce pressure on understaffed areas
• Advocate for resources when needed
A team with a healthy work-life balance is more productive, more accurate and more engaged.
Recognition is a cornerstone of engagement and retention. When people feel valued, they’re happier at work and more committed to providing great patient care.
Use a structured recognition plan:
• Incorporate peer-to-peer recognition
• Celebrate milestone achievements (certifications or years of service)
• Spotlight “wins of the week” in meetings
• Share patient kudos
• Honor technologist, nurse, scheduler and support staff contributions
• Celebrate monthly themes (Compassion Month, Teamwork Month)
When recognition is built into the culture, positivity becomes the norm not the exception.
Leadership in radiology is challenging and rewarding. By setting clear goals, choosing positivity, fostering relationships, recognizing our teams and caring for ourselves, we build the culture that drives outstanding patient care. Let this be the year you lead with purpose, create a lasting impact and inspire your teams to thrive professionally, personally and together. •
Michelle Nocera, MBA, CRA, CIIP, RT (R)(CT)(M), is the director of radiology academic market & ambulatory locations with University Hospitals.

BY MARK WATTS
Artificial intelligence (AI) is in healthcare systems and there has been a recent change to the post-deployment requirement from the FDA. My goal is to raise awareness of the requirements and help define roles for responsibility.
The FDA’s evolving regulatory framework for Software as a Medical Device (SaMD), particularly AI/ML-enabled medical devices, represents a fundamental shift from traditional medical device regulation. Unlike static hardware devices, AIbased SaMD continuously learns, adapts and updates – creating unique challenges for safety, effectiveness and cybersecurity assurance.
The FDA’s approach, outlined in multiple guidance documents including the 2023 “Marketing Submission Recommendations for a Predetermined Change Control Plan for Artificial Intelligence/ Machine Learning (AI/ML)-Enabled Device Software Functions,” emphasizes a total product life cycle (TPLC) regulatory approach requiring ongoing post-market surveillance, performance monitoring and cybersecurity maintenance.
Healthcare organizations deploying AI-based SaMD must understand that FDA compliance is not a one-time premarket approval event but an ongoing obligation extending throughout the device’s operational lifetime.
The convergence of FDA medical device regulations, HIPAA security requirements, and emerging AI-specific guidance creates a complex compliance landscape
that demands systematic planning, documentation and continuous monitoring.
Traditional medical devices were regulated primarily at the premarket stage –manufacturers demonstrated safety and efficacy before commercialization, and post-market requirements focused on adverse event reporting and recalls when problems emerged. This model assumed the device would function identically throughout its life cycle unless explicitly modified through new regulatory submissions.
AI/ML medical devices fundamentally break this model. Machine learning algorithms are designed to learn from new data, adapt to changing patient populations and continuously improve performance. An AI diagnostic algorithm deployed in January may function quite differently by December after processing millions of additional patient cases. This “locked algorithm” versus “adaptive algorithm” distinction drives the FDA’s TPLC approach.
The FDA recognizes three types of modifications to AI/ML-enabled devices:
• Performance modifications: Changes to the algorithm’s clinical performance characteristics, such as sensitivity, specificity or predictive accuracy
• Input modifications: Changes to the types or sources of data the algorithm accepts
• Intended use modifications: Expansions or changes to the clinical conditions, patient populations or use contexts
The TPLC approach requires manufacturers to establish predetermined change control plans (PCCPs) describing the types of modifications they anticipate making, the methodology for implementing changes safely and the monitoring mechanisms ensuring modifications don’t compromise safety or effectiveness. Crucially, healthcare organizations deploying these devices share responsibility for monitoring performance and reporting issues.
The FDA’s 2023 guidance “Cybersecurity in Medical Devices: Quality System Considerations and Content of Premarket Submissions” (draft) establishes cybersecurity as an ongoing quality system requirement, not merely a premarket checkbox. This guidance, combined with the 2014 “Content of Premarket Submissions for Management of Cybersecurity in Medical Devices” and 2016 postmarket guidance, creates a comprehensive framework emphasizing:
• Security by Design: Cybersecurity must be integrated throughout the device life cycle from initial design
third-party libraries, open-source components and dependencies – enabling rapid vulnerability identification and patching.
• Coordinated Vulnerability Disclosure: Manufacturers must establish processes for receiving, assessing and responding to vulnerability reports from security researchers, healthcare organizations and other stakeholders.
• Continuous Monitoring and Updates: Post-market cybersecurity requires ongoing threat intelligence monitoring, vulnerability scanning, penetration testing and timely security updates – all while maintaining device functionality and clinical performance.
For AI/ML devices, cybersecurity complexity increases exponentially. Training data poisoning, adversarial attacks designed to fool algorithms, model inversion attacks extracting sensitive training data and model theft represent novel threat vectors beyond traditional software vulnerabilities. The FDA expects manufacturers and healthcare organizations to address these AI-specific risks systematically.

In Part 2, we will explain the process steps to meet
is an experienced imaging professional who founded an AI company called Zenlike.ai.

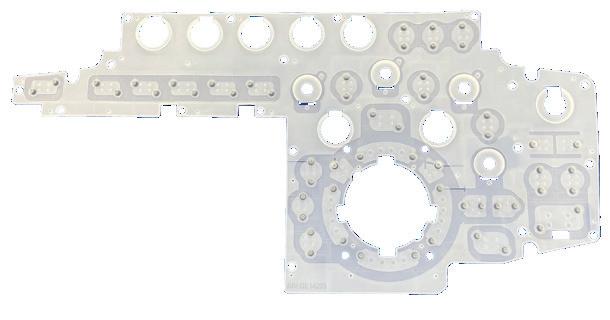
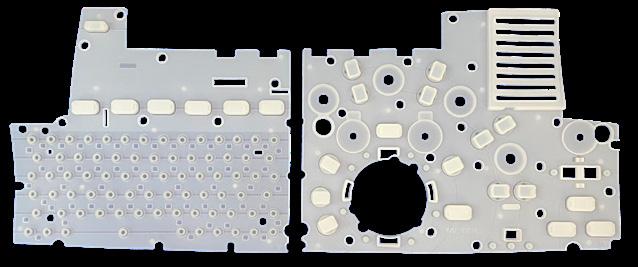


BY DANIEL BOBINSKI
tatistically, by the time February rolls around, about 80% of all New Year’s resolutions have already fallen by the wayside.
If that’s happened to you, I have some good news: It’s not too late. If you set goals for yourself or for your team and they’ve already started to slip, I’d like to share three techniques that are valuable for achieving goals.
1. Clarify your goals in writing every day.
2. Stay focused on the path you must take.
3. Find someone you trust and stay accountable.
Let’s start by talking about clarifying your goals in writing every day. One famous success story here is Scott Adams, creator of the Dilbert cartoon strip. Before his cartoon became famous, Adams wrote out by hand the following sentence 15 times a day: “I will become a syndicated cartoonist.” Yes, in his books and in interviews, Adams says he did this 15 times a day!
Writing down goals is an important part of any goal-setting process, but writing them out every day by hand is ultra-powerful, and neuroscience backs that up. When you write out your goals, you activate what’s called the Reticular Activating System (RAS) in your brain. This RAS acts as a filter for the thousands of bits of information your brain receives every day, allowing it to prioritize and focus on what’s most relevant to your objectives.
Think of your RAS as your brain’s personal assistant. It’s the same system that enables you to hear your name whispered across a crowded room. When you consistently write your goals, your RAS begins collecting pertinent information and routes it to the conscious part of your mind. You become aware of opportunities you would never have noticed otherwise. Then, when you recognize those opportunities, it’s much easier to step into them.
Recent research confirms this power. Dr. Gail Matthews at Dominican University found that people who wrote down their goals and shared weekly updates with a friend had a 76% success rate, compared to just 43% for those who didn’t write them down.
So step one is to establish specific, measurable goals and write them by hand every day.
The second step is mentally picturing yourself doing the activities needed to achieve your goals. Whereas the first step uses words, this second step capitalizes on visual imagery. Think about it. Driving instructors and motorcycle safety instructors tell their students to focus on where they want their vehicle to be, not where it currently is.
Allow me to give an example of when I put this trick to work. Decades ago I would ride my bicycle to work, and on the way home I had to ride up a long hill. My goal was always to reach the top without stopping, and because I was giving it all I had, my focus was on the ground a few feet in front of me. Sometimes I would see a small rock in my path and I would think to myself, “I’m going to miss that rock.” Except I didn’t. If I was looking at the rock, I ran over the rock, no matter what words I spoke in my head.
After a few times of that happening, I remembered my motorcycle safety training, and that we go where we’re focused. After that, whenever I saw a rock in the path of my bike tire, I would simply focus my eyes a few inches to one side of the rock, and behold, my bike tire would go where I was looking, thus avoiding the rock.
This same practice is powerful for achieving goals. Myriad distractions exist in our lives, so one glance in the right direction doesn’t do it. To achieve our goals, we need to regularly “see” ourselves on the path to what we’re trying to achieve.
Finally, let me talk about having an accountability partner. A word to the wise: Choose this person carefully! It should not be your spouse (too close to you) nor someone who is not concerned about your success.
A good accountability partner should be someone you trust, and someone who has experience in pressing through obstacles to reach their goals. It’s best if this person is outside of your chain of command, but still has an appreciation of what you’re trying to achieve. It should also be someone whom you don’t want to let down.
The research on accountability partners is striking. According to the Association for Talent Development, individuals have a 65% chance of completing a goal if they commit to someone. That number jumps to 95% when they schedule specific accountability appointments.
Finding the right person can take some time, but it’s important to find someone who wants you to succeed, plus someone who has time to connect with you regularly. Meetings don’t have to be long, just consistent. You can even meet over the phone or online.
Once you’ve identified an accountability partner, connect with that person a minimum of twice a month. Weekly is even better. Talk about your progress, but also talk about the obstacles you’re facing. It’s also best if your accountability partner does not lecture you. Ideally, he or she should patiently ask you pertinent questions to help you think through your own solutions and actions, offering advice and pointing out cautions only as needed.
“You
Also, don’t feel like you need to limit yourself to one accountability partner. There is a proverb that says, “Plans fail for a lack of counsel, but with many advisors they succeed.” Still, if all you have is one, that’s way better than none.
Bottom line: There’s no reason to be shrugging your shoulders three months from now wondering why you didn’t make progress on your goals. You will go where you’re focused, so if you want the best chances of success, write out your goals every day and get focused on the path for what needs to be done. Then get an accountability system in place, and soon you’ll be achieving your goals and enjoying success. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@protonmail.com or 208-649-6400.
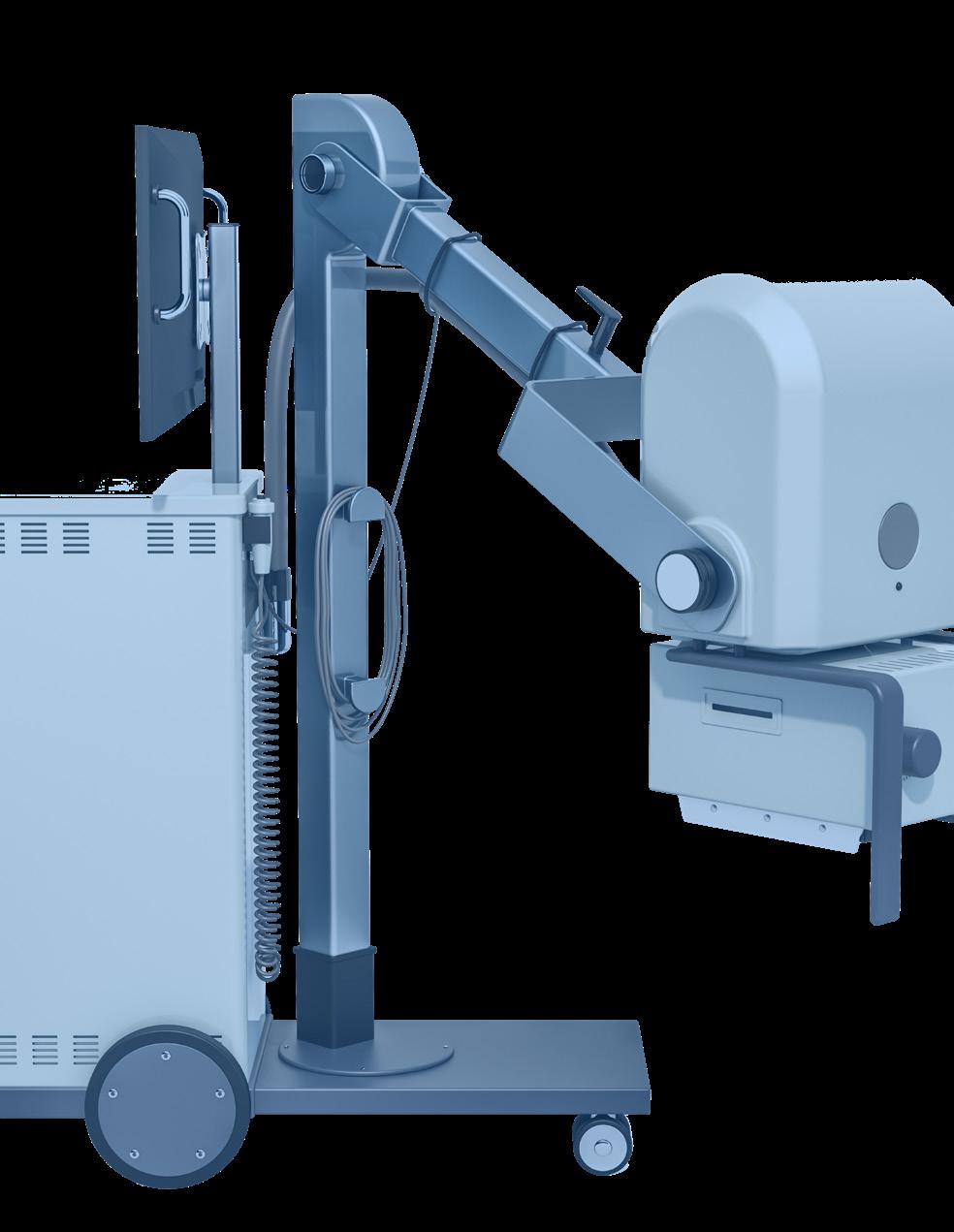
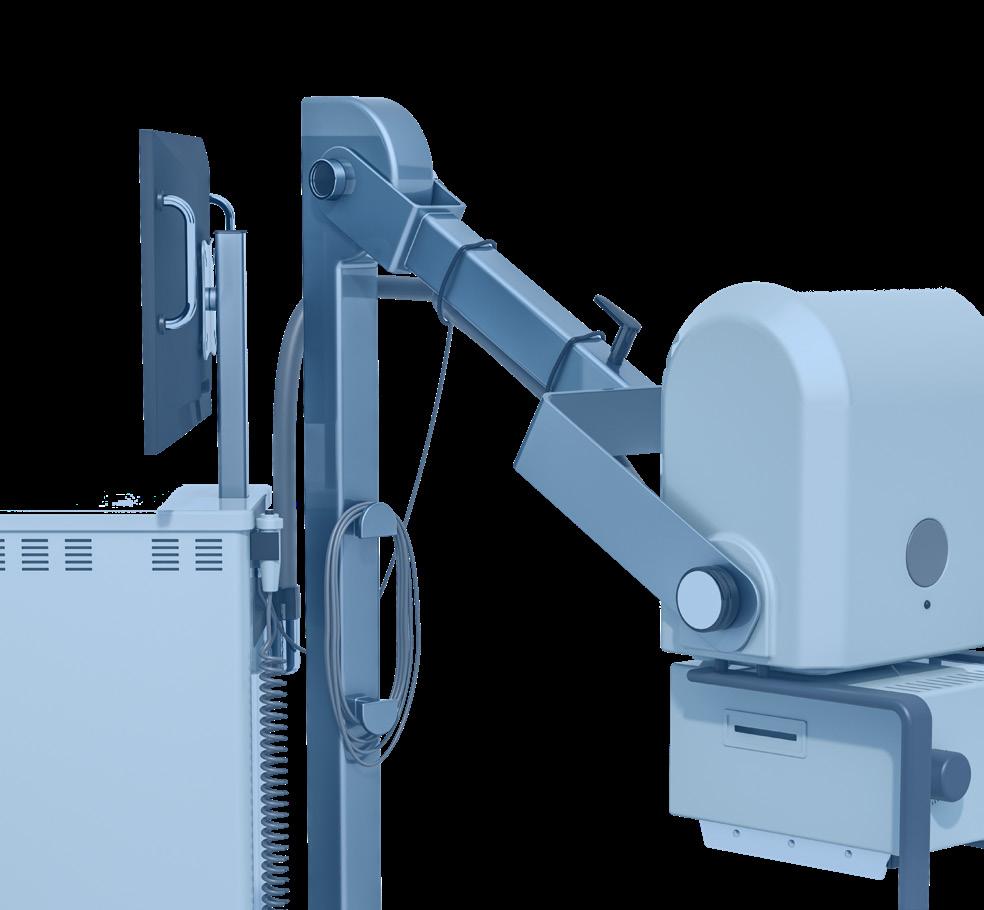



Physical fitness, physical activity and screen time are associated with brain mechanisms underlying mental health and learning, according to two recent studies from the University of Eastern Finland and Kuopio University Hospital. Research into the effects of lifestyle and physical fitness on adolescent brain function remains limited to date.
“Our new findings highlight the importance of an active lifestyle, good physical fitness and moderate screen time for brain development in adolescence,” says Doctoral Researcher Hannamari Skog from the Institute of Biomedicine at the University of Eastern Finland.
In the first study, participants’ physical fitness and lifestyle habits were monitored from childhood. The researchers found that better physical fitness was associated with increased excitability and stronger inhibition of the motor cortex in adolescence – with excitability and inhibition regulating brain development and learning processes. The second study examined the associations of screen time and physical activity with brain function. According to the results, the amount of screen time is not the sole critical factor for brain development, but the way people engage with various digital devices also plays a significant role.
“Passive engagement with digital devices, such as scrolling on the phone or watching TV and videos, weakened adolescents’ cortical inhibition, that is, the so-called ‘braking system’ of the brain,” Skog says.
Conversely, active engagement with digital devices was associated with increased cortical excitability, as was participation in organized sports in sports clubs.
According to Skog, it is beneficial for adolescents to have access to organized sports:
“Besides supporting social well-being, participation in organized sports also seems to promote adolescents’ brain health.
Screen time should be kept within reasonable limits, and it should preferably involve digital media that stimulates activity and movement.”
The studies, conducted as part of the Physical Activity and Nutrition in Children study (PANIC) and the FitBrain study, involved 45 healthy Finnish adolescents aged 16-19, including 25 girls and 20 boys. Cardiorespiratory fitness was assessed via a direct maximal cycle ergometer test, muscular strength via a standing long jump test, speed and agility via a 10 x 50 meter shuttle run test, and upper limb coordination via a box and block test. Questionnaires were used to evaluate screen time and participation in organized sports, supervised exercise other than sports, and unsupervised physical activity.
Transcranial magnetic stimulation, TMS, was used to measure, e.g., the brain’s response to stimuli induced by a magnetic pulse, and the brain’s ability to inhibit or suppress activity as needed. These measurements reflect excitatory and inhibitory brain function regulated by neurotransmitters such as glutamate and GABA. These same neurotransmitters influence brain plasticity, and their dysregulation is associated with problems with attention, and with mental health disorders.
The findings were published in Neuroscience and in Frontiers in Neuroscience. •
RESEARCH ARTICLES:
Skog HM, Määttä S, Säisänen L, Lakka TA, Haapala EA. Associations of physical fitness with cortical inhibition and excitation in adolescents and young adults. Front Neurosci. 2024 Apr 29;18:1297009.https://doi.org/10.3389/fnins.2024.1297009
Skog HM, Määttä S, Säisänen L, Lakka TA, Haapala EA. Associations of Screen Time and Physical Activity with TMS-based Measures of Motor Cortical Excitability in Adolescents. NeuroScience: 587, 2025; 98–107. https://doi.org/10.1016/j.neuroscience.2025.09.054.






Register to view the webinars each month
Watch recorded webinars on-demand
3.EARN
ARRT Category A CE credits pending approval


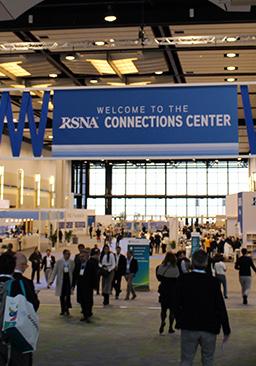

The RSNA 111th Scientific Assembly and Annual Meeting (RSNA 2025) in Chicago offered close to 38,000 attendees a wide variety of opportunities to interact with the latest research, education and advanced imaging technologies. The meeting’s theme was “Imaging the Individual.”


1. The AI Showcase was a popular destination at this year’s meeting.
2. Imaging professionals from around the world flooded Chicago’s McCormick Place.
3. The Innovation Theater was just one of many venues to receive continuing education.
4. The Bark Park provided a great spot to rest and relax inside the exhibit hall.
5. The theme for 2025 was “Imaging the Individual.” • 1 2 3 5 4











Anesthesia
USOC Medical
usocmedical.com • 855-888-8762
Breast Imaging
Radon Medical radonmedicalimaging.com • 866-723-6698
800-229-7784
AMX
866-630-2697
Espin Medical www.espinmedical.com • (206) 755-1768 5
Metropolis International, LLC Metropolismedical.com • 718-371-6026
X-ray America, LLC x-rayamerica.com • 854-999-6888 17
Cables Engineering Services eng-services.com • 330-425-9279 2
Computed Tomography
CM Parts Plus cmpartsplus.com • 877-267-2784
Espin Medical www.espinmedical.com • (206) 755-1768 5
FDM Enterprises fdmenterprises.com • 615-479-5572 25
ImageOne Medical image1group.com • 877-304-9000 4
Innovative Radiology innovative-radiology.com • (888) 909-9894 37
KEI Medical Imaging Services keimedicalimaging.com • 512-477-1500 51
LASO Imaging Solutions lasoimaging.com • 800-674-5276 45
Metropolis International, LLC Metropolismedical.com • 718-371-6026 18, 66
Radon Medical radonmedicalimaging.com • 866-723-6698
Ray-Pac ray-pac.com • 843-767-8090
RSTI rsti-training.com • 800-229-7784
W7 Global w7global.com • (855) 974-5622 63
X-ray America, LLC x-rayamerica.com • 854-999-6888 17
Contrast Imaging
Maull Biomedical Training maullbiomedical.com • 440-724-7511
FDM Enterprises fdmenterprises.com • 615-479-5572
Think of us as forensic experts… …in the field of Nuclear Imaging
Think of us as forensic experts… …in the field of Nuclear Imaging
Complete Solutions for your Imaging Department!
Multi-Vendor Service
& Upgrades
as forensic experts… …in the field of Nuclear Imaging
Think of us as forensic experts… …in the field of Nuclear Imaging
•
•
•
Multi-Vendor Service
-General
-General Electric
-General
-Siemens
-Philips
Think of us as forensic experts… …in the field of Nuclear Imaging
•
Multi-Vendor
-General
•
•
-Siemens
Think of us as forensic experts… …in the field of Nuclear Imaging Multi-Vendor
Think of us as forensic experts… …in the field of Nuclear Imaging Multi-Vendor
Think of us as forensic experts… …in the field of Nuclear Imaging Multi-Vendor
Contact Us Today (630) 780-6363 NCSI@NuclearCameraServices.com NuclearCameraServices.com
-General Electric
-Siemens -Philips
Electric | Siemens |

-Siemens -Philips Contact Us Today (630) 780-6363 NCSI@NuclearCameraServices.com NuclearCameraServices.com






NCSI@NuclearCameraServices.com










