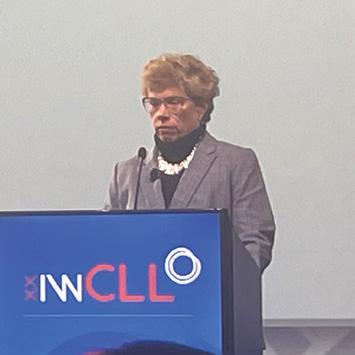
Researcher Spotlight: Jennifer Brown, MD, PhD
Dr. Jennifer Brown has dedicated her more than 20-year career to understanding and treating lymphoma, particularly chronic lymphocytic leukemia (CLL).
10




Dr. Jennifer Brown has dedicated her more than 20-year career to understanding and treating lymphoma, particularly chronic lymphocytic leukemia (CLL).
10



Pulse is a publication of the Lymphoma Research Foundation, providing the latest updates on the Foundation and its focus on lymphoma research, awareness, and education.
The Lymphoma Research Foundation is devoted to funding innovative lymphoma research and serving the lymphoma community through a comprehensive series of education programs, outreach initiatives, and patient services.
Foundation Leadership
Steven Eichberg Chair, Board of Directors
Ann S. LaCasce, MD, MMSc Chair, Scientific Advisory Board
Meghan Gutierrez Chief Executive Officer
Editor Nichole Musumeci
Associate Editor
Paige Butler





Contact Us
National Headquarters
Wall Street Plaza
88 Pine Street, Suite 2400
New York, NY 10005
212 349 2910 lymphoma.org
Helpline
800 500 9976
helpline@lymphoma.org
Editorial Board
Micah Banner
Victor Gonzalez
Kyle Haines
Fatima Hameed
David Meehan-Romero
Eva Migliore
Sarah Quinlan
Laura Wallenstein

The Lymphoma Research Foundation’s YouTube channel offers a wide variety of educational videos to help the lymphoma community learn about lymphoma. These videos provide disease-specific information as well as education regarding diagnosis, treatment options, clinical trials, and other resources for people dealing with a lymphoma diagnosis. Visit YouTube.com/c/LymphomaResearch to watch and subscribe.
For over 20 years, Dr. Brown has led teams at DanaFarber Cancer Institute to new understandings of chronic lymphocytic leukemia (CLL) and run clinical trials that have improved outcomes for countless patients.
Meet the 2024 Lymphoma Scientific Research Mentoring Program Scholars
The new class of Foundation Scholars are pursuing projects covering a diverse range of lymphoma subtypes, with a goal to improve the lives of all those touched by lymphoma.
In June 2022, Carly Stafford Dixon was looking forward to marrying her fiancé, Wil, and beginning their lives together. However, when Carly was unexpectedly diagnosed with lymphoma shortly after they said “I do,” their lives took a turn neither one of them was prepared for.




The Lymphoma Research Foundation’s brand evolution modernizes and differentiates the Foundation’s look and defines our place at the center of the lymphoma community.
Though our colors and our appearance may have changed, our lifesaving mission remains the same: to realize the promise of science, to eradicate lymphoma, and serve the community touched by this disease.
Grounded in Research. Committed to Community.

The Lymphoma Research Foundation is focused on bringing the promises of the future into the present. We have been at the forefront of crucial biomedical breakthroughs that have brought about new therapies and deepened understandings of lymphoma and chronic lymphocytic leukemia (CLL) – and nowhere is this better exemplified than in our commitment to supporting the next generation of blood cancer researchers.
I’m privileged to introduce you to the 2024 class of the Lymphoma Research Foundation’s Lymphoma Scientific Research Mentoring Program (LSRMP) in this issue of Pulse. The scholars that you will meet represent the best and brightest scientific minds who have committed their careers to studying and treating lymphoma. This crucial program provides the expert training, support, mentorship, and funding that early career researchers need to build successful careers in lymphoma and CLL research.
This issue also profiles Foundation Scientific Advisory Board member and senior advisor to the Foundation’s CLL Working Group, Dr. Jennifer Brown, who has dedicated her career to understanding and treating the disease. For over 20 years, her work as Director of the CLL Center at Dana-Farber Cancer Institute has deepened our knowledge of why people develop CLL and how to best treat it.
Finally, this issue spotlights Carly Stafford, who was diagnosed with primary mediastinal B-cell lymphoma after finding herself uncharacteristically winded while hiking. Thrown into an unexpected cancer journey as a 28-year-old newlywed and looking for support, she turned to the Foundation as a resource before starting CAR T-cell therapy. Now cancer-free for just over a year, she’s focused on using her experience to help patients and survivors like herself, completing the Great Smoky Mountain Half Marathon in support of the Foundation’s lifesaving work.
As we mark Blood Cancer Awareness Month in September, we are more dedicated than ever to our work of investing in the future of research, empowering the best and brightest minds in our field, and supporting, uplifting, and amplifying lymphoma patients, survivors, and care partners. Though our community is made up of many different voices, we are all united in our common goal: a world without lymphoma. Thank you for your continued support and your belief in our shared mission.
Sincerely yours,

Meghan Gutierrez Chief Executive Officer



The Lymphoma Research Foundation hosted Partners in Purpose, A Scientific Social at The Casino Club in Chicago, Illinois, on Thursday, May 30. Over 170 guests, including survivors, caregivers, members of the Foundation’s esteemed Scientific Advisory Board (SAB), Foundation research grantees, industry and medical institution partners, and Foundation supporters, joined together to recognize and celebrate former Foundation SAB chair Sonali M. Smith, MD, FASCO, with the Hope Award. This year’s event, chaired by Susan and Keith Hoogland, Kim Metcalf, and Laura and Michael Werner, raised $137,000 to support the Foundation’s critical work supporting the lymphoma community.
Over 150 participants and volunteers walked to honor and support the lymphoma community at the 2024 Minnesota Lymphoma Walk on Saturday, June 8. This year’s walk, which raised over $55,000 to power the Lymphoma Research Foundation’s lifesaving mission, was chaired by former Foundation Scientific Advisory Board chair Thomas Habermann, MD, and honored Theresa Deutsch of Team Knockouts and Jerilyn Lubahn with the Lee Grubman Caregiver of the Year Award as well as The Lymp-homies team, led by Hayley Hanson, with the Team of the Year Award.
Paolo Strati, MD, credits support from the Lymphoma Research Foundation with helping him build his career in blood cancer research as a recipient of the Foundation’s Career Development Award as well as his participation in the Lymphoma Scientific Research Mentoring Program. Now, he’s inspired his loved ones to give back, with his fourth grade daughter, along with her younger brother and three friends, starting the Money Jar Club at their elementary school to raise funds to support the Foundation’s mission. Through bake sales, art sales, and donations from friends, family, and neighbors, these young supporters of the Foundation raised over $200 and were honored in a special ceremony at their school with Board of Directors member emeritus Donna Reinbolt present representing the Foundation.






Over 350 participants rocked out for a good cause at the second annual Harmony4Hope music festival, organized by Lymphoma Research Foundation Board of Directors member Bob McAuley. This year’s event, held on June 9 at Mango’s Bar & Grill in Moneta, Virginia, raised $250,000 – more than double the amount it raised in its first year – and featured a dual performance by lymphoma survivor Kimberley Dahme, of the rock band Boston, with vocals and banjo from former Foundation Scientific Advisory Board member Dr. Bruce Cheson.
Wanting to honor the memory and legacy of his wife, Corlette, a lymphoma patient, Los Angeles chef Bernard James, owner of popular LA restaurant Taste of the Caribbean, organized the inaugural Miss Caribbean Los Angeles pageant on June 1, 2024. This year’s event, which amplified and celebrated leaders making a difference in the Caribbean community in Los Angeles and was attended by hundreds of supporters, raised $5,000 in support of the Foundation’s mission and crowned Jahmea Bent Miss Caribbean Los Angeles 2024.
On Sunday, July 28, more than 500 supporters gathered to get us one step closer to a world without lymphoma at the 2024 Chicago Lymphoma Walk. Participants celebrated together while raising $227,000 in support of the lymphoma community, enjoying a beautiful day at Chicago’s Montrose Harbor and a special performance from The Jesse White Tumblers. This year’s event also honored Aimee Lanphere with the Champion of the Year Award; Team Frank! with the Team of the Year Award; and Sarah Lopez with the Lee Grubman Caregiver of the Year Award.

Steven “Steve” J. Prince, former Chair of the Lymphoma Research Foundation’s Board of Directors and current Director Emeritus, grew up in a New York family that prioritized giving back – a tradition he has continued.
“Giving back came naturally to me, as it’s always been a priority for my family,” said Prince. “My grandfather did not have much money, but every year, he would receive annual appeals from several organizations, and he would donate to every one of them. My parents were very philanthropic as well, and it was just something that we were brought up with – that you give back when you can.”
A lifelong New Yorker, now living in Purchase, New York, with his wife of 47 years (Debbie), Steve led a successful New York commodities firm from which he retired as CEO in 2008. With three children and seven grandchildren, he has spent his retired life serving in several roles at various philanthropic organizations, including Let’s Get Ready, Gift of Life, and the Lymphoma Research Foundation.
When it comes to lymphoma, however, Steve’s involvement is personal. In 2003, Steve was diagnosed with chronic lymphocytic leukemia (CLL) and began treatment with Dr. Morton Coleman, a longtime member of the Lymphoma Research Foundation’s Scientific Advisory Board.
“I had a pretty aggressive case of CLL,” he explained. “It did not respond to the then best practices, so Dr. Coleman suggested an innovative treatment that he had successfully used with his multiple myeloma patients. That protocol was effective for about 10 years, which helped me bridge the gap until science could catch up with my treatment needs.”
Dr. Coleman introduced Steve to the Foundation, and by 2006, Steve was a member of the Foundation’s Board of Directors. Over the last 20 years, Steve has served the Foundation in several roles, including Chair of the Audit Committee, Treasurer, Chair of the Board, and currently as a Director Member Emeritus.
Having undergone lymphoma treatment himself, Steve knows firsthand the importance of funding research to advance new treatment protocols and has worked tirelessly to help raise these critical funds over the years.
“Thanks to continued research, we have several new immunotherapies that Foundation research dollars have contributed to developing. I’m living proof of the Foundation’s impact, having benefited from treatments that the organization helped get developed and approved.”
When he first joined the Board, Steve got right to work setting up a direct funding program for CLL research, one that is still in place today. He also started and co-ran the Foundation’s Golf Invitational event for 11 years, which raised over two and a half million dollars to support the Foundation’s mission. Additionally, Steve has been integral in helping to initiate multiple named grants, including the
Kanti R. Rai Clinical Scholar Award, the Errol M. Cook Memorial Scholar Award, and most recently, the Morton Coleman, MD, Innovation Fund. The money raised through this fund will support planned areas of scientific focus and allow future researchers to build upon the important work and achievements of experts like Dr. Coleman.
Thanks to continued research, we have several new immunotherapies that Foundation research dollars have contributed to developing. I’m living proof of the Foundation’s impact, having benefited from treatments that the organization helped get developed and approved.
In recognition of his 20 years of contributions to the Foundation, the Foundation is awarding him the 2024 Distinguished Leadership Award at this year’s Annual Gala on September 25 at the Ziegfield Ballroom in New York City.
“It’s an incredible honor to be recognized with the Lymphoma Research Foundation’s Distinguished Leadership Award,” said Prince. “To me, the most impactful leaders within the lymphoma community are the doctors and researchers who are searching for cures, so to be singled out amongst these world leaders is truly humbling.”
Steve remains proud to work with an organization that does so much to impact the lymphoma community. From advancing research to supporting patients, survivors, care partners, and their loved ones, Steve feels the Foundation has a unique way of bridging the gap between research and people.
“The Lymphoma Research Foundation is a reliable resource that helped me better understand my disease’s progression and the various treatment regimens available,” says Prince. “I am proud of the fact that we genuinely help patients, their families, and their care partners better understand their disease and the treatment options available.”
While Steve originally got involved with the Foundation to learn more about CLL, he is happy that he can now make an impact on others who are facing their own lymphoma journey.
“As my knowledge about CLL and other lymphomas developed, I’ve been able to educate other newly diagnosed patients and help them find the right path to treatment, which has been very rewarding,” said Prince.
“The Foundation’s continued investments in research have yielded life-saving results – advancements that are likely to extend my life and the lives of others. Overall, I think my association with the Foundation has enabled me to live my life without being under an umbrella of fear and instead to adopt an outlook of optimism.”
The Foundation’s continued investments in research have yielded life-saving results –advancements that are likely to extend my life and the lives of others.

Lymphoma Rounds provides a series of accredited CME activities that provide a forum for healthcare professionals to meet regularly and address issues specific to the diagnosis and treatment of lymphoma patients. Participants share best practices and learn the latest information on the treatment and management of lymphoma through interactive case studies.

9/26 – Philadelphia Lymphoma Rounds
10/10 – Washington DC Lymphoma Rounds
10/17 – New York Lymphoma Rounds
10/22 – Los Angeles Lymphoma Rounds
11/7 – Seattle Lymphoma Rounds
11/14 – New England Lymphoma Rounds
11/21 – San Francisco Lymphoma Rounds
1/23 – National Lymphoma Rounds
1/30 – Chicago Lymphoma Rounds
2/6 - New York Lymphoma Rounds
2/12 - Puerto Rico Lymphoma Rounds
2/20 – Washington DC Lymphoma Rounds
3/6 – San Francisco Lymphoma Rounds
4/9 – New England Lymphoma Rounds
4/24 – Philadelphia Lymphoma Rounds
5/8 – Seattle Lymphoma Rounds
5/14 – Los Angeles Lymphoma Rounds
5/28 – National Lymphoma Rounds
Visit lymphoma.org/hcpeducation to register and learn more.
Lymphoma Rounds programming is supported by educational grants from: Acrotech; ADC Therapeutics; AstraZeneca; Lilly USA, LLC; Secura Bio
Dr. Jennifer Brown, the Worthington and Margaret Collette Professor of Medicine in the field of hematologic oncology at Harvard Medical School and Director of the CLL Center and Institute Physician at Dana-Farber Cancer Institute (DFCI), has dedicated her career to understanding and treating lymphoma, particularly chronic lymphocytic leukemia (CLL). For over 20 years, Dr. Brown has led teams at Dana-Farber to new understandings of CLL and run clinical trials that have improved outcomes for countless patients.


I got very interested in genetics in high school and have been strongly oriented toward science from then on
When she’s not exploring the jungles of Uganda, climbing Machu Picchu with her husband, or swimming in the Atlantic Ocean near her beach house in the summer, Dr. Brown is solely focused on her patients and her research. Science has always been a particular passion for Dr. Brown. Growing up on Long Island, she was the first in her family to pursue a career in medicine.
“I got very interested in genetics in high school and have been strongly oriented toward science from then on,” she says. “Specifically, I was interested in the control of cell growth, and that lends itself to oncology and cancer in general.”
While attending medical school, she developed a fascination with hematology and majored in molecular biophysics and biochemistry (MB&B). Her early research focused on knocking out genes involved in growth control within cell lines. Her research helped her understand the genetic abnormalities of unregulated cellular growth compared to normal cells, which have practical applications in the study of lymphoma.
After enrolling in the Harvard Medical School dual-path MD/PhD program, Dr. Brown discovered the draw of hematology. During her fellowship, she found her affinity for studying malignant hematology and lymphoma. The heterogeneity of lymphoma and the clinical and biological variety appealed to her. She came to respect the varied patient experiences, too, and developed a sensitivity to the challenges that people go through when faced with a lymphoma diagnosis.
“At the time, medicine felt broader, while scientific research was feeling more and more narrow,” said Dr. Brown. “I wanted to have an impact on people, and due to the many subtypes of lymphoma, there are a lot of different patient experiences, which, in turn, offer a wide variety of experiences to a healthcare provider. I liked that, so that’s how I got into lymphoma.”
Working on the PhD part of her dual degree showed her how important the research side of the care equation was to her and how she could have a greater impact on medicine through research, especially her chosen specialty of improving the lives of lymphoma patients.

During her medical residency at Massachusetts General Hospital, she joined the hematology and medical oncology division at the Dana-Farber Cancer Institute. While there, she worked with a mentor in a small lab, participating in a program known as the Clinical Investigator Track, which was created for people who take care of patients and run clinical trials.
From her fellowship, she joined the faculties of DFCI and Harvard Medical School, and in 2021, she was awarded an endowed professorship at the medical school.
Dr. Brown’s research is centered around improving treatment options for chronic lymphocytic leukemia (CLL), a type of cancer that starts in the bone marrow and affects the blood. She is working on understanding why and how certain CLL cells become resistant to treatments over time as well as why people get CLL and the inheritance of it at the genetic level.
“My day-to-day schedule is a mix of seeing patients and managing research,” said Dr. Brown. “I have one full day of clinic each week, and the other days are a mixture of running the lab, advising my people in the lab, dealing with issues with clinical trials, and getting the clinical trials through the institutional review process. Currently, I’m working on getting two clinical trials going that have arisen from research we’ve done in the lab. So that’s exciting.”
A key element of her current research involves studying BTK inhibitors, a class of drugs that target a protein called Bruton’s tyrosine kinase (BTK). BTK plays a crucial role in the development of B cells (white blood cells). Drugs that inhibit BTK can effectively shrink cancerous lymph nodes to manage the disease. However, not all patients respond to these treatments in the same way, and some eventually develop resistance to the drugs.
“What’s interesting is that patients’ white blood cell counts sometimes went up, which was very counterintuitive, and no one understood why,” explained Dr. Brown. “But we came to understand that it appeared to be a redistribution phenomenon rather than disease progression. This evolved into a novel response criterion where the white count going up was no longer a sign of progression.”
As Dr. Brown was working on identifying why drug resistance happens, her team discovered that in many cases, when BTK inhibitors stop being effective, it’s because the cancer cells have found ways to activate proteins that bypass the drug’s effects.
A pivotal component of Dr. Brown’s lymphoma research is DFCI’s extensive CLL tissue bank that has over 3,500 patients enrolled and more than 20,000 individual stored samples. Started over 25 years ago, the tissue bank is foundational for the groundbreaking work done at DFCI. Dr. Brown took the leadership role for the CLL bank when she joined DFCI faculty in 2004. Ever since she started working with it, she has spearheaded the collection of serial samples from patients – samples from them before, during, and after their treatment – even patients not in trials with targeted inhibitors.
“What is really novel about our tissue bank is the extensive clinical annotation that we have,” said Dr. Brown. “We have all the clinical data for all the patients, all the prognostic markers. There is a lot of interest in the evolution of cancer under the influence of different drugs, and with serial samples, we have the opportunity to study that because we have the whole natural history of the disease.”
The tissue bank supports the development of precision medicine. By analyzing the stored samples, Dr. Brown’s team can identify specific genetic profiles and biomarkers that predict how a patient’s disease will respond to different treatments. This insight allows for personalized treatment plans tailored to each patient’s cancer.
There is a lot of interest in the evolution of cancer under the influence of different drugs, and with serial samples, we have the opportunity to study that because we have the whole natural history of the disease.
In addition to developing therapies for CLL, Dr. Brown also wants to understand why people get CLL in the first place. While there is a strong hereditary component to developing CLL, it’s a highly variable disease. Some genetic mutations are common to many CLL patients, while others are rare or individualized, suggesting multiple genetic contributions to CLL. This complicates the search for universal genetic markers for CLL and points to the development of personalized, targeted approaches to prevention and treatment.
Dr. Brown knows that when markers for CLL are discovered in a patient, it’s likely a highly traumatic event for them. But she reminds us that living with CLL, even when it is manifesting in the patient, is different than it was years ago. Today’s treatment for the disease is far more effective than what was available previously, even though there is no outright cure for CLL today.
She notes that today, people can get diagnosed early with the disease, and they usually don’t have any symptoms and may not develop any for years. Multiple treatment options are available to patients based on several factors, not the least of which is what the patient wants. The most critical issue for patients is monitoring and caring for their immune systems, as CLL puts them at greater risk for infections and secondary cancers.
“The important thing is to have a conversation with the patient to understand what their priorities and goals are and how different treatments will work,” she says.
Dr. Brown notes that the Lymphoma Research Foundation has been at her side for over 15 years. The Foundation has provided her with several research grants that have been instrumental in allowing her to explore innovative treatment strategies for CLL. The Foundation has also been an active partner in patient communication and education critical to maintaining the two-way dialog central to long-term research challenges.
Today, Dr. Brown is a member of the Foundation’s Scientific Advisory Board (SAB) and is a senior advisor for the Foundation’s CLL Working Group. The group is currently finishing a paper that will help guide physicians regarding managing CLL.
“The Foundation does great work for patients as well as for researchers,” she notes. “I encourage all in the lymphoma field to seek out their counsel and potential grants whenever possible. I’m proud to be on the Scientific Advisory Board and work with a great group of people moving us closer to cures for the diseases that don’t yet have cures.”
Dr. Brown is optimistic about the future of CLL research and feels grateful to play a part in ensuring a brighter future for all those affected by this disease.
“There’s still so much we need to understand,” said Dr. Brown. “We have the potential to cure people, and we have many new kinds of treatments for CLL that are just in their infancy of being studied. It’s an exciting time to be in lymphoma research.”
When did you become interested in the study of medicine? In lymphoma specifically?
After realizing in high school that only 1% of astronauts went to space, I shifted my love for science to medicine. I became further interested in medicine after my grandfather was diagnosed with lung cancer. I watched the way his oncologist treated him as a person, not just a patient, and the way he involved our incredibly large family. While challenging, I loved the deep bond between a family and their physician that occurred from the moment they met. This passion for oncology continued, and when I was in medical school, I was able to work with Dr. Jennifer Pearce. Dr. Pearce is an extraordinary pediatric oncologist who inspires me every day. She is one of several physicians who I will always strive to be like.
I went to St. Jude Children’s Research Hospital for fellowship to pursue a career in international oncology. During my time there, I learned the global applicability of lymphoma research, given how curable the disease is, and established a research career with a focus on Hodgkin lymphoma.
Why were you particularly interested in pediatric oncology?
I have always loved working with children. From the time I was young, my mother worked as a certified occupational therapy assistant and treated children with disabilities. I learned the resilience of children and the way they can overcome impossible situations and come out stronger. They have always had a place in my heart.

At what point in your career did you receive funding from the Lymphoma Research Foundation? What kind of grant(s) did you receive?
I have been incredibly fortunate to have exceptional mentors in my life. I will never forget when Dr. Kara Kelly, an extraordinary physician, mentor, and human, suggested I apply for the Lymphoma Research Foundation Scientific Research Mentoring Program (LSRMP). At the time, I was looking to study a rare subtype of lymphoma called nodular lymphocyte-predominant Hodgkin lymphoma. The project was in its infancy and the LSRMP program changed my life and career.
What scientific project did you pursue as part of your research grant(s)?
I planned to open a global clinical trial for pediatric nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL), and I left the program with a global consortium for both pediatric and adult NLPHL. The consortium’s goal was to study it retrospectively and then to utilize that information to inform a global frontline clinical trial with a career-long trajectory.
How has the treatment landscape for lymphoma/CLL changed since you first started conducting your research?
New drugs continue to emerge that are efficacious in the treatment of lymphoma. The goal is to continue to find the right combination of these medications to cure patients with less late effects.
Was the support and grant funding you received from the Foundation vital to advancing/ dedicating your career to studying lymphoma?
My LSRMP grant was everything for me. It was a chance to discuss my ideas with world experts and completely change the scope of my project from just that, a project, into a lifelong career-defining project. The faculty leading the mentoring program invested not just their time but also their energy and expertise into each one of us, and it was hands down the most pivotal week of my career. I returned from maternity leave early and attended the program with my 8-week-old baby – and it was amazing
Why is there such a great need for adolescent and young adult (AYA)/pediatric research? Why is a greater investment needed?
There are many reasons there is such a need for AYA/ pediatric research, given that this is the most common cancer in this age group. Beyond that, this is a very challenging time in life to make major decisions while trying to attend school, start a career, etc. Insurance and access to medical care is shifting around this time, and this group needs extra attention and focus.
More than all of this, pediatric and AYA patients are young with a long life ahead of them. For a very curable diagnosis, it is essential to treat them with therapy that will be both efficacious and minimize late effects of therapy to ensure they live both a long and healthy life. As new drugs arrive on the market, they need to be applied to this population if we are certain they will not have increased toxicity compared to our known standards of care, as we have been able to cure this disease for years and there are many great treatment regimens.
Can you tell us about the GLOW consortium?
How has the Foundation helped support that?
GLOW is the Global Nodular Lymphocyte Predominant One Working Group. (Glowconsortium.org). We are a group that I cofounded with Michael Binkley, a radiation oncologist from Stanford University. We have grown into a formal consortium with over 140 researchers from 26 countries and counting. I am so thankful for this group of dedicated researchers who have come together to research this rare disease.
How has your involvement with the Foundation evolved since being a Scholar?
From Day 1 I was so thankful to become part of the Lymphoma Research Foundation family. Since that time I have also received a Career Development Award from the Foundation to continue to support my work on this effort.
Why is the Foundation’s mission and focus on lymphoma-specific research and programming important? Put another way: How would the lymphoma community be impacted if there was no Lymphoma Research Foundation?
The Lymphoma Research Foundation is incredibly important to the field of lymphoma to help advance research and science while educating and connecting patients and families to factual information and resources.
As we learn about lymphoma we must also provide education to help treat each patient today the best we can, and the helpline is an exceptional resource for patients and families. In addition, the mentoring program is investing in and supporting young investigators to ensure robust research continues each and every day.
What research or projects are you currently pursuing that you would like to share with our readers?
Currently, I am working on finding ways to cure lymphoma “better” by achieving the same cure rates with less late effects of therapy. Additionally, I am looking at ways to increase diagnostic capabilities for lymphoma in places around the world with limited resources.
What is the most exciting thing happening in AYA/pediatric lymphoma research right now? What are you most excited about in the field of lymphoma research in general? Why?
New technologies continue to emerge that allow us to better understand the microenvironment of Hodgkin lymphoma, which is incredibly exciting. Given that only 1%-2% of the cells in a Hodgkin lymphoma tumor are the “cancer” cells, there is a large inflammatory component to the disease. The more we can learn about the tumors with novel techniques, the more we can learn how else to treat it!
The Lymphoma Research Foundation’s Lymphoma Scientific Research Mentoring Program (LSRMP) is a first-of-its-kind education and mentoring program for junior scientists who wish to focus on lymphoma and CLL research, whether in the lab or in the clinic.
The primary goal of the LSRMP is to retain its talented participants – called LRF Scholars – in the field of lymphoma by providing mentoring and education programming and fostering research collaboration among expert faculty and grantees.
Led by the 2024 LSRMP Clinical Research co-chairs, Jeremy Abramson, MD (Massachusetts General Hospital), and Nancy Bartlett, MD (Washington University in St Louis), and Laboratory/Translational Research co-chairs, David Scott, MBChB, PhD (BC Cancer), and Michael Green, PhD, MD (University of Texas MD Anderson Cancer Center), the new class is boasting translational and clinical researchers pursuing a diverse range of research projects with a goal to improve patient outcomes.

Adam DuVall, MD
University of Chicago
Chike Springer Foundation Scholar
Adolescents and young adults with cancers such as lymphoma have unique emotional and psychosocial needs as a result of their disease and treatment. While survival outcomes rates are high, these burdens can lead to longterm negative consequences and high rates of depression, anxiety, and post-traumatic stress disorder (PTSD). Dr. DuVall’s research is focused on optimizing the use of appbased cognitive behavioral therapy (CBT) to meet the specific experiences of young people with lymphoma to help improve social-emotional outcomes in this population.
Dr. Duvall earned his medical degree from Case Western Reserve University in Cleveland, Ohio, where he also earned a Master of Public Health. He is currently an assistant professor at the University of Chicago, where his work focuses on improving both survival and quality-of-life outcomes for young people with cancer. “All of my patients inspire my research and help direct the area that I study,” he says. “Whether it be mental health outcomes, sexual health, or other psychosocial outcomes, the incredible young people I am privileged to care for in clinic tell me what is most important to them and drive my desire to improve these domains of their life and care through

Looking ahead to the future, Dr. Duvall is excited to continue his work on efforts to amplify the patient voice in lymphoma research, particularly for adolescents and young adults. “The focus on quality of life in addition to quantity while integrating new agents into the therapy for lymphoma by amplifying the patient voice through patient-reported outcomes gives me great hope,” he says. “It will allow us to focus our interventions that we are currently developing to improve our patients’ outcomes when they are most vulnerable during and after therapy to maximize

Diffuse large B-cell lymphoma (DLBCL) is an aggressive form of non-Hodgkin lymphoma, with many patients experiencing relapse after first-line therapy. Many patients now receive treatment with a chimeric antigen receptor (CAR) T-cell therapy such as axicabtagene ciloleucel (axicel) in the second-line setting, which is effective for many patients. The efficacy of CAR T-cell therapy is highest in patients with low tumor burden, though, and Dr. Goldstein’s research aims to identify ways to treat patients when their tumor burden is the lowest. Using circulating tumor DNA (ctDNA) as a marker of residual disease, Dr. Goldstein is evaluating the efficacy and safety of axi-cel after first-line chemoimmunotherapy in patients with persistent disease who are more likely to relapse. By treating patients right after first-line therapy, when their tumor burden should be the lowest, he hopes to improve outcomes and reduce the likelihood of relapse for patients with DLBCL.
Dr. Goldstein’s interest in lymphoma research began during his time in medical school at Emory University in Atlanta, Georgia. “I’ve been fortunate to benefit from outstanding mentorship from lymphoma experts at each level throughout my medical education, all of whom are involved with the Lymphoma Research Foundation,” he says. As an independent physician researcher, he hopes not only to use novel technologies to improve the lives of lymphoma patients but also to give back to the next generation of lymphoma researchers. “I hope to have mentees of my own, contributing to future generations of lymphoma researchers and ‘paying it forward’ for the amazing mentorship I have received,” he says.

Mwanasha Merrill, MD Dana-Farber Cancer Institute
Diagnosis of lymphoma is currently based on the use of biopsies and imaging scans to detect cancer cells and tumors. Challenges exist with the use of these techniques, though – biopsies can be invasive and cause discomfort, imaging tests are expensive, and both carry a risk of procedural complications. Additionally, the reliability of these tests may be questionable in certain circumstances, as many patients determined to be in complete remission by imaging later relapse. “Safer and more sensitive diagnostic approaches for detecting lymphoma are, therefore, urgently needed,” says Dr. Merrill. “We propose to fill this diagnostic void with an innovative new ‘liquid biopsy’ test optimized for T-cell lymphomas.” As Dr. Merrill explains, this test is used to detect circulating tumor DNA in the blood, which she hopes will help detect T-cell lymphomas more accurately than conventional imaging scans.
Dr. Merrill earned her medical degree from Tufts University School of Medicine in Boston, Massachusetts. She is currently a hematology/oncology fellow at Dana-Farber Cancer Institute, where she is excited about building a career in lymphoma research at the intersection of cutting-edge molecular diagnostics and experimental therapeutics. “I am fortunate to work in an environment that fosters clinical research in lymphoma,” she says. “I know the importance of advancing our knowledge in this field, improving detection and treatment options. I hope that this will ultimately improve the quality of life for people affected by lymphoma.”
Dr. Merrill hopes to leverage her experiences as a Lymphoma Scientific Research Mentoring Program (LSRMP) fellow to establish herself as a clinical research expert in the treatment of lymphoma, with a focus on developing new diagnostic assays that can help serve resource-poor environments. She is continually motivated by the patients she sees in the clinic, who inspire her to keep working to develop better ways to diagnose and treat lymphoma. “Witnessing the challenges these individuals face and their courage in fighting the disease is a powerful motivator to improve treatments,” she says.
Christina Poh, MD University of Washington/Fred Hutchinson Cancer Center
Stephanie A. Gregory, MD, Distinguished Scholar
Survival outcomes with peripheral T-cell lymphoma (PTCL) are poor, with many patients relapsing after their first line of treatment and only about 1 in 5 patients surviving for at least five years after diagnosis. To help reduce the likelihood of recurrence and extend survival in these patients, Dr. Poh is working to develop a novel therapeutic approach using low-dose non-chemotherapeutics that can be employed after initial treatment. By tracking the number of patients whose disease remains under control with this additional therapy and by correlating treatment responses with tumor genetics, Dr. Poh hopes to establish a new maintenance strategy to improve outcomes in patients with PTCL.
Dr. Poh earned her medical degree from Loma Linda University School of Medicine in California. She completed a hematology/oncology fellowship at the University of California, Davis, and is currently an assistant professor of medicine at the University of Washington and Fred Hutchinson Cancer Center. She was inspired to a career in cancer research following the loss of her grandmother. “Her memory serves as a constant reminder of the countless individuals worldwide who are battling this relentless disease,” she says. “Through my dedication to cancer research, I strive to honor her legacy by contributing to the collective effort to improve outcomes and provide hope to those affected by cancer.”
Dr. Poh is optimistic about the future of lymphoma research and treatment in light of recent advances that allow for a more individualized approach to treatment. “These advancements not only improve survival rates but also enhance the quality of life for patients, with fewer side effects and more effective long-term outcomes,” she says. “As a result, I am filled with hope and optimism for a future where lymphoma may one day be a manageable or even curable condition for all those affected.”
Lauren Shea, MD
University
of Alabama
Kanti R. Rai, MD, Clinical Scholar
Better therapies are needed for patients with relapsed or refractory peripheral T-cell lymphoma (PTCL), and Dr. Shea’s research aims to identify a novel, improved treatment approach in this setting. The EZH1/2 inhibitor tazemetostat has been found to be effective in other types of lymphoma, and preclinical data in T-cell lymphomas have been promising. Dr. Shea is conducting a phase 2 clinical study to evaluate the safety and efficacy of tazemetostat in patients with relapsed/refractory PTCL, which she hopes will provide a meaningful and urgently needed advancement for the treatment of T-cell lymphomas.
Dr. Shea first became interested in lymphoma research from a scientific angle. “I found the molecular biology and immunology of lymphoma fascinating,” she explains. “Later, however, it was my experience with patients and mentors in lymphoma that left me committed to a career in lymphoma research and patient care.” She earned her medical degree from Washington University School of Medicine in St. Louis, Missouri, where she also completed her hematology/oncology fellowship. She is currently an assistant professor of medicine in the division of hematology and oncology at the University of Alabama at Birmingham, where her research focuses on transplant and targeted therapies for T-cell lymphoma.
With the support of the Lymphoma Scientific Research Mentoring Program (LSRMP), Dr. Shea hopes to refine her skills as a clinical trialist studying T-cell lymphomas. She also looks forward to giving back to the next generation of researchers. “Mentorship is fundamental. I have been blessed with many amazing mentors throughout my career,” she says. “I would love to be able to serve as a mentor to early career clinical investigators interested in lymphoma research as well.”

Danielle Wallace, MD
University of Rochester
Mindy Camp Fedida Memorial Scholar
Older patients with diffuse large B-cell lymphoma (DLBCL) are often treated with lower doses of chemotherapy, which may contribute to an incomplete cure of the disease. Residual tumor cells in the body release pieces of DNA into the blood, and detection of this circulating tumor DNA (ctDNA) may serve to help identify patients who are at increased risk for disease relapse. “My proposal suggests that if they still have ctDNA in their blood, we should start additional treatment, even if a PET scan shows no obvious lymphoma,” says Dr. Wallace. In this project, patients will receive additional therapy with the bispecific antibody mosunetuzumab, which should help facilitate immune clearance of remaining tumor cells. “The concept is that the mosunetuzumab might be able to address the low levels of lymphoma still present and improve the chances of curing patients,” she explains.
Dr. Wallace is hopeful that the results of her project will help to improve cure rates for older patients with DLBCL. “Nearly a third of patients with DLBCL are over the age of 75, and these patients do not have the same cure rates as younger patients,” she explains. “In addition, if they experience relapse, they are not eligible for intensive therapies. Therefore, trying to improve the initial cure rates is important for older patients.”
Dr. Wallace was drawn to a career in lymphoma research during her medical training at SUNY Upstate Medical University in New York. “I have always been interested in the care of older patients, though,” she says. “My father is a geriatrician, so early on I knew the importance of specialized care for older adults.” She is continually inspired by her patients, and her goal as a researcher is to develop more effective, more personalized, and less toxic therapies for these individuals. Through the support of the Lymphoma Scientific Research Mentoring Program (LSRMP) fellowship, Dr. Wallace is eager to optimize the details of her clinical trial and develop her skills as a lymphoma researcher and clinician.

Caitlin Gribbin, MD
New York-Presbyterian/Weill Cornell
The Kellie and Jeff Fellinge Scholar
The follicular lymphoma (FL) tumor microenvironment is made up of a wide variety of non-lymphoma cells that contribute to the growth and progression of tumor cells. “We are particularly interested in the role of follicular dendritic cells (FDCs), which are abundant cells both in FL and in healthy lymphoid tissue that we hypothesize provide supportive factors to lymphoma cells and represent a potential therapeutic target in the early stages of FL formation,” Dr. Gribbin explains. Dr. Gribbin hopes that by characterizing and understanding how interactions between these cell types contribute to FL growth, novel targets will be identified that can be leveraged to interrupt signaling between these cells and effectively eradicate FL.
“The opportunity to translate scientific findings and principles to effective lymphoma-directed treatments is exciting, as this field is evolving quickly and remains integrally connected to its underlying scientific principles,” says Dr. Gribbin. Building on the translational nature of her research, she hopes to develop early-phase clinical trials in lymphoma to leverage the knowledge gained to provide the best treatments possible for her patients. “Patients provide the greatest inspiration in terms of recognizing all of the work that we have yet to accomplish in effectively understanding and treating lymphoma,” she says. “It is so gratifying to be able to connect scientific advances with people who are affected by lymphoma and who can truly benefit from the emerging knowledge in the field.”
Dr. Gribbin is a hematology/oncology fellow at NewYorkPresbyterian/Weill Cornell in New York, NY. She credits her mentors at Weill Cornell for helping guide her career development and growth as a lymphoma researcher and specialist and is excited for the continued support of the Lymphoma Scientific Research Mentoring Program (LSRMP).

David Russler-Germain, MD, PhD Washington University
in St. Louis
Follicular lymphoma (FL) is typically a slow-growing disease with high response rates to initial therapy, but disease outcomes vary considerably from patient to patient. Dr. Russler-Germain, therefore, is researching how circulating tumor DNA (ctDNA) can be used as a marker to help guide treatment decision-making before therapy even begins. “We hope that our pre-treatment ctDNA profiling can accelerate personalized treatment choices for individual patients, ideally pairing their FL pathobiology with the optimal therapy regimen,” he explains.
Dr. Russler-Germain completed his MD/PhD training at Washington University School of Medicine. He was a hematology/oncology fellow at Barnes-Jewish Hospital in St. Louis, Missouri, before returning to Washington University as an instructor in the division of oncology. He was drawn to lymphoma research, given his family’s personal experiences with lymphoma, and has been excited by the intellectual opportunities of the field and the many unanswered questions that remain. “My overall aspiration as a lymphoma scientist and physician is to confront the diverse areas of uncertainty in this field,” he says. “I hope to design and conduct laboratory experiments, translational studies (such as this project specifically), and clinical trials to answer these questions, reduce the uncertainty that patients face, and improve their outcomes.”
Building on his translational research, Dr. Russler-Germain is looking forward to continuing his career studying FL and other lymphomas, as well as continuing to care for patients within the clinic. He is grateful to the mentors who have helped guide him in his career and also hopes to continue his involvement with the Lymphoma Research Foundation as a mentor himself in the future.

Christoph Weigel, PhD
Ohio State University
Epstein-Barr Virus (EBV) is a ubiquitous virus that infects many people across the globe without any serious or immediate symptoms. In certain circumstances, however, such as older age or after organ transplant, EBV can transform blood cells into cancer cells, leading to lymphoma. Identification of EBV-driven lymphoma can have important implications for treatment, but current methods do not reliably detect the virus in lymphoma. “In my project, I will deploy a new technology that specifically reads out molecular features on EBV DNA to classify and distinguish EBV versus non-EBV lymphoma,” explains Dr. Weigel. “This technology will allow physicians to better diagnose and treat EBV-associated blood cancer.”
Dr. Weigel’s interest in EBV-associated lymphoma was sparked during his time as a graduate student at the German Cancer Research Center in Heidelberg, Germany. During this time, he met Dr. Harald zur Hausen, the scientist who uncovered the role of human papillomavirus (HPV) in cervical cancer development. “To me, the story of HPV is a blueprint for the combination of basic, translational, and clinical science,” says Dr. Weigel. “I have made it my mission to apply similar concepts to tumor-causing viruses like EBV. My Lymphoma Scientific Research Mentoring Program (LSRMP) project will hopefully be my starting point, paving the way to better detection, treatment, or even prevention of EBV-associated lymphomas.”
Alongside his research goals, Dr. Weigel looks forward to giving back to the lymphoma research community. “I will hopefully also possess the same outstanding mentorship qualities that impressed me so much at the LSRMP workshop,” he says. “For me, being an outstanding mentor myself has become another important career goal.”

Xia, PhD Weill Cornell Medicine
Among the different subtypes of diffuse large B-cell lymphoma (DLBCL), ABC-DLBCL represents one of the most aggressive forms, with low response rates to standard chemotherapeutic approaches. Improved treatment approaches in this space are urgently needed, and an improved understanding of ABC-DLBCL biology may help to identify novel therapeutic targets. To this end, Dr. Xia’s research is focused on characterizing alterations in the BCL10 gene, which are common in ABC-DLBCL, to understand how they contribute to the development of lymphoma and how interruption of these processes may help to improve treatment outcomes. “We believe understanding the fashion of lymphoma initiation and progression will unravel novel perspectives to treat lymphoma patients with BCL10 mutations,” she says.
Dr. Xia completed her doctoral research at the Shanghai Institutes for Biological Sciences at the Chinese Academy of Sciences. She is currently an instructor of cancer biology at Weill Cornell Medicine in New York, where she is working to establish herself as an independent researcher focused on the pathogenesis of lymphoma and the development of novel therapeutic regimens. “Lymphoma is a complex, hard-to-treat, and highly heterogeneous disease with different subtypes, hence, it requires tailored treatment for better overall outcome,” she says. She is driven to better understand the mechanisms of lymphoma formation and progression, with the hope that these advances will lead to the development of more effective treatment options and improved prognosis for lymphoma patients.

Haopeng Yang, PhD
University of Texas MD Anderson Cancer Center
Super-enhancers are regions of the genome responsible for regulating expression of an unusually high number of genes. For his Lymphoma Research Foundation-funded project, Dr. Yang is characterizing the activity of superenhancers in different subtypes of diffuse large B-cell lymphoma (DLBCL), with the goal of understanding how these regions contribute to DLBCL growth and progression and how these processes may be interrupted to help treat the disease.
Dr. Yang completed his doctoral research at the University of Houston and is currently an instructor in the department of lymphoma/myeloma at MD Anderson Cancer Center in Houston, Texas. “My research interest is focused on understanding the complex epigenomics of B-cell lymphoma by using cutting-edge techniques and developing novel therapeutic approaches to benefit lymphoma patients within a mechanism-driven strategy,” he says. “By integrating basic and translational research, I aim to lead [the development of] innovative therapeutic interventions by a profound understanding of epigenetics and immune cell biology in B-cell lymphoma.”
As part of his research, Dr. Yang utilizes patient-derived xenograft (PDX) models of DLBCL to understand the disease-causing processes and potential therapeutic responses in real tumor cells. “I hold deep respect for all patients who provide their consent to use their biopsies for the development of PDX models and, therefore, aim to generate impactful data that contribute to the lymphoma community,” he says.
By integrating basic and translational research, I aim to lead [the development of] innovative therapeutic interventions by a profound understanding of epigenetics and immune cell biology in B-cell lymphoma.
Whether you are newly diagnosed, want detailed information about your lymphoma subtype, are looking for ongoing support, or are seeking help with long-term survivorship, we are here to help.

9/18 - Ask the Doctor: Treatment Options and Clinical Trials
9/24 - Ask the Doctor: Newly Diagnosed Patients
10/15 - Update on Chronic Lymphocytic Leukemia/ Small Lymphocytic Lymphoma Webinar
10/23 - Update on CAR T-Cell Therapy Webinar
10/26 - 10/27 - Educational Forum on Lymphoma
In June of 2022, Carly Stafford Dixon, a 30-year-old high school college counselor from Nashville, TN, was thrilled to be getting married to her fiancé (now husband), Wil, and beginning their lives together as a married couple. However, when Carly was unexpectedly diagnosed with lymphoma shortly after they said “I do,” their lives took a turn neither one of them was prepared for.


Carly and Wil were excited to finally be getting married after a long engagement due to COVID-19. After celebrating their nuptials with family and friends, the couple began searching for their first home and planning their future. Everything seemed to be falling into place.
In August, just two months after their wedding, Carly went on a fall outdoor retreat with her students and started feeling out of breath while taking them on a hike. Having grown up in Colorado and hiking her whole life, this was certainly unusual for her.
“The school I work for conducts an annual student retreat every fall for a few days of hiking, bonding, and outdoorsy stuff,” said Carly. “I was leading the hiking portion of the retreat and found myself feeling so winded on those trails, which is not like me – I had no idea what was going on.”
Carly’s first thought was that she might have COVID, but the tests all came back negative. She returned home from the retreat and flew to Colorado that weekend for a friend’s wedding. Again, she found herself short of breath and having difficulty breathing.
“I wondered if I might just be out of shape, but when I returned home, I was still feeling crummy and had to take the week off work to recover,” said Carly. I had planned to return to Colorado again over Labor Day weekend, but we canceled at the last minute because I was still feeling so ill.”
Thankfully, my family kept me occupied, and since I was running from test to test, I barely had time to worry.
Not wanting to take any chances, she decided to see a doctor, but the only place open Labor Day weekend was an urgent care facility at a local drugstore. The doctor on staff there examined Carly and sent her to get an X-ray.
The X-ray showed a large shadow in Carly’s chest, and she was immediately referred to get a CT scan. The CT scan confirmed that Carly had a large mass, at least six inches in diameter, lodged in her thorax (her upper chest) that was pressing on her lungs and making it difficult for her to breathe.
The urgent care facility instructed her to wait for a referral to a pulmonologist, but a family friend in medicine urged her to go to the emergency room immediately. Carly went to the emergency room with her husband on September 9, where she underwent a battery of tests.
“I was a bit scared in the beginning, but we felt we needed to be realistic about what they might find because we knew that a tumor that big could never be a good thing,” said Carly. “Thankfully, my family kept me occupied, and since I was running from test to test, I barely had time to worry.”
On September 13, after being cooped up in the hospital for four days awaiting test results, Carly just wanted to be outside and see her dog, Maggie. After receiving special permission to venture into the hospital courtyard, her mom wheeled her outside, IV pole in tow, where she was met by her husband and her dog Maggie at his side.
Coincidentally, the doctor handling Carly’s case called with biopsy results while they were in the courtyard and said that he would meet them there to talk. There, in the hospital courtyard, he gave Carly, her mom, and her husband the diagnosis: primary mediastinal B-cell lymphoma (PMBCL), an extremely rare form of nonHodgkin lymphoma, primarily affecting women aged 25 to 40 for no known reason.
“Despite the news, it just felt good to have an answer – to know what was going on, that they had seen this before, and that there was something to be done about it,” said Carly. “For some reason, I wanted to get a picture before we went back into the hospital, so we have this picture that my mom took of me, my husband, and my dog. We’re all smiling in the picture despite having received some very bad news, but I remember thinking, ‘So that’s the last picture we’ll have together before my treatment starts.’”
Naturally curious and solution-oriented, Carly immediately went into discovery mode. She started asking her doctor as many questions as she could regarding treatment options, side effects, what to expect, and the road ahead. Along with her healthcare team, Carly decided that the chemo regimen called R-EPOCH would be the best for her. Carly moved into a new hospital room that night and started treatment the next day on September 14.

As a young adult diagnosed with lymphoma, Carly had some unique concerns that impact many other adolescents and young adults who are facing a cancer diagnosis. Being a 28-year-old newlywed, her first concern was surrounding her fertility.
“I was interested in pursuing fertility preservation, and one of the most difficult pieces of news I received was that we didn’t have enough time to freeze my eggs prior to starting treatment due to the fast-growing nature of the mass in my chest,” explained Carly. “Sometimes I find myself thinking that if I had not been diagnosed with cancer, we might be a few steps ahead in the family planning process compared to now, but I try not to dwell on it.”
Another concern for her centered around her professional life. How should she share this news with her boss? Would she be able to keep her job? How would her lymphoma diagnosis affect her career?
“Even though I’m fortunate to work in a supportive environment, I was still nervous about sharing my diagnosis with my boss,” said Carly. “I was worried about job security and about my own professional growth, but I knew I wouldn’t be able to work while receiving treatment.”
Luckily, her co-workers were incredibly supportive, making it clear that her recovery was the most important thing and that her job would be waiting for her when she finished her treatment.
Carly’s first line of treatment consisted of six rounds of inpatient chemotherapy lasting five days and five nights each (120 hours of chemo per round), followed by two weeks off, over the course of four months. While her first-line treatment made a significant impact, it didn’t fully eradicate the tumor, and Carly required additional treatment. Her doctors suggested she undergo an immunotherapy approach called chimeric antigen receptor (CAR) T-cell therapy. CAR T uses patients’ own immune cells to treat their cancer.
She underwent two shorter stints of chemo before receiving CAR T in the summer of 2023. The treatment worked exactly as intended, and she was able to return to work cancer-free in the late summer of 2023.
“I’m so fortunate to have an amazing family, friends, and colleagues who supported me throughout this process,” said Carly. “My parents and two sisters came out to visit
often, and they coordinated a calendar of friends and family to take care of me between rounds of chemo so that I was never alone. My husband, in-laws, colleagues, friends, and community here in Nashville were all fantastic and helped keep my spirits up.”
Now cancer-free for just over a year, Carly is focused on her life as a survivor and how she can use her own experience to help others navigate a similar diagnosis.
I’m so grateful for the treatment and support I received, and it makes me want to give back to the greater lymphoma community.
In her effort to learn more about lymphoma and her subtype, Carly found the Lymphoma Research Foundation website and dove into the Foundation’s rich resources.
“I first came across the Lymphoma Research Foundation when I was about to start CAR T,” explained Carly. “I found a lot of really helpful resources on the Foundation’s website, and after finishing treatment, I wanted to support the great research that the Foundation was helping to fund.”
In early September of 2023, shortly after finishing CAR T, Carly pursued a longtime personal goal and ran the Great Smoky Mountain Half Marathon in support of the Lymphoma Research Foundation. Carly was so successful in her fundraising that she was a finalist for the Rookie of the Year Award at the Foundation’s annual Fundraise Your Way awards in March 2024, and she was the top fundraiser of the entire half marathon.
“The Foundation impacted my life by providing resources that I would not have been aware of on my own – not just for me, but for my husband and family as my care partners as well,” said Carly. “CAR T saved my life, and the Foundation helps fund research that leads to the discovery of novel therapies like CAR T. That’s a huge reason I wanted to give back.”
“I think it’s tempting to say that survivorship is moving on with your life, but that’s not it exactly. Whether you are ‘cancer-free’ or still going through it, it’s now part of your life forever, part of your lived experience,” said Carly. “To me, survivorship is about owning your experience and learning how to assimilate this experience you’ve just had with cancer into your life and into your life story. It’s also about taking time to reflect on what you’ve learned from having cancer and taking time to be thankful for those who helped you, to be thankful for your body’s healing, and to be thankful for the wonders of modern medical science. That’s what I’m continually wowed by.”
Carly has even taken to TikTok to document her lymphoma experience, sharing equal parts information, inspiration, and humor. While she never thought she would be sharing something as personal as her lymphoma journey on such a public platform, her channel has reached patients, survivors, and caregivers who have benefited from the content.
“I’m so grateful for the treatment and support I received, and it makes me want to give back to the greater lymphoma community.”

The Lymphoma Research Foundation’s volunteer Scientific Advisory Board, comprised of 45 world-renowned lymphoma experts, guides the Foundation’s research activities, seeking out the most innovative and promising lymphoma research projects for support.
Ann S. Lacasce, MD, MMSC Chair
Harvard Medical School Dana-Farber Cancer Institute
Andrew M. Evens, DO, MSc, FACP Chair-Elect
Rutgers Cancer Institute of New Jersey
Ranjana Advani, MD Stanford University School of Medicine
Ash A. Alizadeh, MD, PhD Stanford University School of Medicine
Stephen Ansell, MD, PhD Mayo Clinic, Rochester
Kristie A. Blum, MD
Winship Cancer Institute of Emory University
Jennifer Brown, MD Dana-Farber Cancer Institute
James Cerhan, MD, PhD Mayo Clinic, Rochester
Ethel Cesarman, MD, PhD NewYork-Presbyterian Hospital Weill Cornell Medicine
Sandeep Dave, MD, MS Duke University
Kieron M. Dunleavy, MD Lombardi Cancer Center of Georgetown University
Kojo S.J. Elenitoba-Johnson, MD Memorial Sloan Kettering Cancer Center
Todd Fehinger, MD, PhD Washington University School of Medicine
Christopher R. Flowers, MD, MS The University of Texas MD Anderson Cancer Center
Jonathan W. Friedberg, MD, MMSc University of Rochester
James P. Wilmot Cancer Institute
Leo I. Gordon, MD, FACP Past Chair, 2015-2017
Robert H. Lurie Comprehensive Cancer Center of Northwestern University
Michael Green, PhD MD
The University of Texas MD Anderson Cancer Center
Thomas M. Habermann, MD Past Chair, 2017-2019 Mayo Clinic, Rochester
Alex Herrera, MD
City of Hope Medical Center
Steven M. Horwitz, MD Memorial Sloan Kettering Cancer Center
Eric D. Hsi, MD
Wake Forest
Kara Kelly, MD
Roswell Park Comprehensive Cancer Center University at Buffalo Jacobs School of Medicine
John P. Leonard, MD Past Chair, 2012-2015
NewYork-Presbyterian Hospital
Weill Cornell Medicine
Kami Maddocks, MD
Ohio State University Comprehensive Cancer Center
Peter Martin, MD
Weill Cornell Medicine
Ari Melnick, MD
NewYork-Presbyterian Hospital
Weill Cornell Medicine
Lindsay Morton, PhD National Cancer Institute
Markus Müschen, MD, PhD
Yale School of Medicine
Loretta Nastoupil, MD
The University of Texas MD Anderson Cancer Center
Teresa Palomero, PhD
Institute for Cancer Genetics, Columbia University
Laura Pasqualucci, MD
Institute for Cancer Genetics, Columbia University
Barbara Pro, MD Columbia University

Lisa Rimsza, MD
Mayo Clinic, Arizona
Lisa Roth, MD
Weill Cornell Medicine
Gilles Sales, MD, PhD Memorial Sloan Kettering Cancer Center
Kerry J. Savage, MD
British Columbia Cancer
David Scott, MBChB, MD
BC Cancer, Vancouver
Laurie Sehn, MD, MPH
BC Cancer, Vancouver
Margaret Shipp, MD
Harvard Medical School
Dana-Farber Cancer Institute
Sonali M. Smith, MD
Immediate Past Chair, 2021-2023
The University of Chicago
Eduardo M. Sotomayor, MD
Tampa General Hospital
Christian Steidl, MD
BC Cancer, Vancouver
John M. Timmerman, MD
UCLA Jonsson Comprehensive Cancer Center
Hans-Guido Wendel, MD
Memorial Sloan Kettering Cancer Center
Andrew D. Zelenetz, MD, PhD Past Chair, 2019-2021
Memorial Sloan Kettering Cancer Center
SAB Emeritus
Morton Coleman, MD
NewYork-Presbyterian Hospital
Weill Cornell Medicine
Brian Link, MD University of Iowa
Kanti R. Rai, MD
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
Michael E. Williams, MD, ScM University of Virginia Cancer Center
9.14
West Coast Lymphoma Workshop
9.18
Ask the Doctor: Treatment
Options and Clinical Trials
9.24
Ask the Doctor: Newly Diagnosed Patients
10.15
Update on Chronic Lymphocytic Leukemia/ Small Lymphocytic Lymphoma Webinar
10.23
Update on CAR T-Cell Therapy Webinar
10.26-10.27
Educational Forum on Lymphoma
10.31-11.3
Disney Wine & Dine Half Marathon Weekend
11.3
TCS New York City Marathon
Want to receive information about Lymphoma Research Foundation events happening in your area? Visit lymphoma.org/emailsignup to select your email preferences and stay up to date with the latest from the Foundation.




