Health Technologies





SAN ANTONIO

TABLE OF CONTENTS


PUBLISHED By: traveling Blender, llC. 10036 Saxet Boerne, tX 78006
PUBLISHER louis doucette louis@travelingblender.com
BUSInESS MAnAgER: vicki Schroder vicki@travelingblender.com
ADVERTISIng SALES:
AUSTIn: Sandy Weatherford sandy@travelingblender.com
SAn AnTOnIO: Gerry lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE:
Bexar County Medical Society
4334 n loop 1604 W, Ste. 200
San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES:
Call (210) 301-4391 or
Email: membership@bcms.org
SuBSCription rAtES:
$30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE:
louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006
www.travelingblender.com
For advertising rates and information
Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MeDICINe is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MeDICINe the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2024 Smithprint, inc.
prin tE d in tHE u SA

SAN ANTONIO 4 SAN ANTONIO MEDICINE • April 2024
THE OFFICIAL PUBLICATION OF THE BEXAR COUNTY MEDICAL SOCIETY • WWW.BCMS.ORG • $4.00 • APRIL 2024 • VOLUME 77 NO.4 HEALTH TECHNOLOGIES Demystifying AI Diagnostic Tools: Musings of a Tech-handicapped Physician By Soma Jyothula, MD, FCCP 12 Big Data and AI By John J. Seidenfeld, MD 14 UT Health San Antonio Develops Tool That Counts Brain Lesions in Seconds Courtesy of Will Sansom, UTHSCSA 16 Leveraging Technology to Improve Primary Care Quality and Access By Prisiliano Salas Jr., MD 20 Patient Hacking: Wearable Medical Devices Vulnerable to Malice By David Alex Schulz 22 University Health’s Pharmacy Services Embrace Technology and Artificial Intelligence for Efficiency and Accuracy By Jennifer Hillman, PharmD, MBA 24 Orthopaedic Robotic Surgery By San Antonio Orthopaedic & Spine Treatment Center 26 BCMS President’s Message 8 BCMS Alliance Message 10 Physicians Health and Rehabilitation Program (PH&R): Remembering a Role Model and a Leader By Monica Jones, BCMS COO 28 Alcoholics Anonymous: Only You Can Decide By Teresa C., PICPC Chair 31 Our Founding Father: Dr. Robert Francis Gossett By Amanda Lozano 32 We Are All Public Health – Celebrating National Public Health Week – April 1-7, 2024 By the City of San Antonio Metropolitan Health District 34 In Memoriam 35 An HR Professional’s Guide to Data Privacy, Compliance and Security By John Rhoades, Managing Director, Data Privacy & Technology Compliance, Insperity 36 Securing Mobile Devices in Healthcare Courtesy of MedPro Group 38 LASO Streaming Healthcare By M. Hamed Reza Mizani, MD 39 BCMS Vendor Directory 40 Auto Review: 2024 Volkswagen Tiguan By Stephen Schutz, MD 44 Recommended Auto Dealers 46

BCMS BOARD OF DIRECTORS

ELECTED OFFICERS
Ezequiel “Zeke” Silva, iii, Md, President
lyssa ochoa, Md, Vice President
John Shepherd, Md, President-elect
Jennifer r. rushton, Md, Treasurer
lubna naeem, Md, Secretary
John Joseph nava, Md, Immediate Past President
DIRECTORS
Woodson “Scott” Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
M. “Hamed” reza Mizani, Md, Member
priti Mody-Bailey, Md, Member
dan powell, Md, Member
Ana rodriguez, Md, Member
raul Santoscoy, do, Member
lauren tarbox, Md, Member
nancy vacca, Md, Member
Col. Elisa d o’Hern, Md, MC, FS, Military Representative
Jayesh Shah, Md, tMA Board of Trustees Representative
John pham, do, UIW Medical School Representative
robert leverence, Md, UT Health Medical School Representative
Cynthia Cantu, do, Medical School Representative
lori Kels, Md, Medical School Representative
ronald rodriguez, Md, Medical School Representative
victoria Kohler-Webb, BCMS Alliance Representative
Carolina Arias, Md, Board of Ethics Representative
Melody newsom, BCMS CEO/Executive Director
George F. “rick” Evans, Jr., General Counsel
BCMS SEnIOR STAFF
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Al ortiz, Chief Information Officer
Brissa vela, Director of Membership & Corporate Partnerships
phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
PUBLICATIOnS COMMITTEE
Monica Jacqueline Salas, Md, Co-chair
Jennifer C. Seger, Md, Co-chair
lokesh Bathla, Md, Member
Elizabeth Clanton, Md, Member
Erika Gabriela Gonzalez-reyes, Md, Member
timothy C. Hlavinka, Md, Member
John robert Holcomb, Md, Member
Soma S. S. K. Jyothula, Md, Member
Kristy Yvonne Kosub, Md, Member
Jaime pankowsky, Md, Member
George-thomas Martin pugh, Md, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
John Joseph Seidenfeld, Md, Member
Boulos toursarkissian, Md, Member
Francis vu tran, Md, Member
Faraz Yousefian, do, Member
louis doucette, Consultant
Brissa vela, Consultant
Monica Jones, Staff Liaison
trisha doucette, Editor
deepthi S. Akella, Student
Moses Alfaro, Student
victoria Ayodele, Student
tue Felix nguyen, Student
Andrew ta, Student
Alixandria Fiore pfeiffer, do, Resident
Elizabeth Allen, Volunteer
Adelita G. Cantu, phd, Volunteer
rita Espinoza, drpH, Volunteer
natalie reyna nyren, pA-C, Volunteer
david Schulz, Volunteer
6 SAN ANTONIO MEDICINE • April 2024

Maximizing Physician Advocacy Through the Texas Medical Association: A Call to Action
By Ezequiel "Zeke" Silva III, President, Bexar County Medical Society (BCMS)
As the newly elected President, one of my primary goals is to bolster our engagement with the Texas Medical Association (TMA). The Bexar County Medical Society (BCMS) serves as a vital link in this association, representing a collective voice from our region within the larger medical community in Texas. This connection offers both an opportunity and an obligation to actively contribute to shaping the future of healthcare in our state.
Why Active Participation Matters:
Effective advocacy within the medical field is inherently bidirectional. The experiences and challenges faced at the local level can significantly inform statewide policies and strategies, creating a feedback loop that enriches the entire medical community. This dynamic relationship underscores the importance of active participation from physician volunteers. At BCMS, we are committed to ensuring that physicians who choose to engage with the TMA find their experience rewarding and feel that their time is used efficiently and effectively.
Exploring TMA Opportunities – The TMA offers numerous avenues for physicians to get involved, each providing unique opportunities to influence healthcare policy and practice:
• BCMS Delegation to the TMA: Serving as the voice of Bexar County's physicians, our delegation plays a critical role in presenting local concerns and insights to the broader TMA community. The legislative and policy-making arm of the TMA, the HOD comprises approximately 500 voting members, with BCMS contributing 42 delegates. This assembly is pivotal in crafting and evaluating resolutions that influence state healthcare policy.
• TMA Councils and Committees: These bodies are instrumental in developing and implementing policies that shape the future of healthcare in Texas. Participation in a council or committee allows physicians to apply their expertise to specific areas of interest, from public health to medical education. These groups focus on specific areas of healthcare, providing detailed studies and policy recommendations to the HOD.
• TMA Board of Councilors: This board addresses ethical issues and interprets the TMA's constitution and bylaws, ensuring that the association's standards are upheld. Acting as the ethical compass of the TMA, this board plays a crucial role in maintaining the integrity and professionalism of the medical community in Texas.
• General TMA Meetings:

Attendance at these meetings offers a broader perspective on the challenges and opportunities facing the medical community in Texas.
Local Engagement:
Recognizing the busy lives of our members, BCMS encourages local involvement as a practical way to contribute. Our meetings offer vital updates and discussions on policy changes at both the state and national levels, allowing members to stay informed and engaged without the need for extensive travel. Furthermore, local participation enables physicians to address specific challenges and opportunities within their practices, making a direct impact on the quality of healthcare in our community.
The Historical Context and Impact of BCMS:
Founded in 1853, just 17 years after the fall of the Alamo, BCMS holds the distinction of being the first constituent county medical society of the TMA. With over 5,500 members, we stand as the thirdlargest CMS in Texas and the eighth largest in the United States. Our members, who represent all medical specialties recognized by the American Medical Association, are united in their commitment to promoting high standards of medical care.
The significance of advocacy in advancing high-quality clinical care cannot be overstated. TMA President Dr. Richard Snyder recently emphasized this point at a BCMS General Membership Meeting, highlighting advocacy as the most critical activity for promoting excellence in healthcare.
As BCMS continues its long-standing tradition of participation and leadership within the TMA, we encourage our members to consider the immense value and fulfillment that comes from representing BCMS at the TMA. Your involvement not only contributes to your professional growth but also plays a vital role in shaping the future of healthcare in Texas and beyond.
Ezequiel “Zeke” Silva III, MD, is the 2024 President of the Bexar County Medical Society. Dr. Silva is a radiologist with the South Texas Radiology Group, Adjunct Professor of Radiology at the UT Health, Long School of Medicine, and Vice-Chief of Staff at Methodist Hospital Texsan. He serves on the TMA Council on Legislation and is a TMA Delegate to the AMA. He chairs the AMA RVS Update Committee (RUC).
8 SAN ANTONIO MEDICINE • April 2024 PRESIDENT’S
MESSAGE

Why Train in San Antonio?!
By Heather Davila, RDH
Every year around the second Friday of March, the nation’s medical students will come to meet their fate on the infamous “Match Day.” Match Day will dictate the projection of an individual’s medical career forever with its binding contract. When surveying applicants, the top four reasons an applicant will rate a program are quality of training, cost of living, geographical location and work/life balance.
San Antonio is home to two medical schools: University of Texas Health Science Center (UTHSCSA) and University of the Incarnate Word School of Osteopathic Medicine (UIWSOM). The San Antonio Military Medical Center (SAMMC) is a modern, top-notch healthcare facility that provides Level 1 trauma and graduate medical education. Between the two highly accredited schools and the Military, San Antonio has almost every residency or fellowship opportunity available making it a very popular pick for medical school graduates nationwide in a highly desirable geographic location.
San Antonio, known as Military City USA, has been home to a military presence for approximately 300 years, and has the largest active and retired military population. SAMMC encompasses the busiest DoD graduate health education training platform in the country. It contains 34 GME programs and 22 Allied Health Programs with a 95 percent first-time board pass rate. For an applicant that desires a surgical residency, the trauma center is one of the best in the country and recognized nationally for its burn unit. UT Health is one of the nation’s leading universities and largest academic research institution in South Texas. It offers advanced cancer care research and advanced specialized surgical training.
Recent analysis of primary care shortages in Texas shows that as of July 2021, 249 of Texas’ 254 counties have areas with shortages of primary care physicians. In 228 of them, the entire county has a shortage, nearly double what it was as of 2019. Institutions such as UIWSOM have seen the need to combat this growing issue by developing robust training committed to strengthening the academic and clinical abilities for applicants wishing to pursue primary care.
Aside from its medical training, San Antonio has the third fastest growing economy in the country with much of that growth coming from healthcare and biomedical science. For new doctors making approximately $60,000 in residency and graduating with a six-figure student loan debt, the low cost of living is very attractive. Medical applicants pursuing a Public Service Loan Forgiveness (PSLF) or
Military Health Profession Scholarship Program (HPSP) that helps with loan repayment are happy to match in San Antonio as it is very family-friendly with the ability to find qualifying jobs. There are many rural underserved areas surrounding the metropolitan area making it desirable for training or fulfilling loan repayment obligations while having a great quality of life.
As the rigorous nature of medical school and residency cannot be avoided, San Antonio has a plethora of activities for all people. For the history lover, the Alamo and the other four historic Spanish Missions, the only UNESCO World Heritage Site in Texas, are a great way to experience the roots of Texas and how Texas came to be. Home of the Culinary Institute of America and Conde Nast top-rated Hotel Emma, the Historic Pearl District is a compilation of unique restaurants, trinket shops and farmers markets. If a trainee’s schedule does not allow the time to grab a Broadway show at the Majestic Theatre or a performance at the Tobin Center for the Performing Arts, art enthusiasts can attend First Friday every month in Southtown’s Blue Star Arts District for an art walk. People come out to see local area artists put on art shows and sell crafts.
So, whether it is a quick trip to the wine country in Fredericksburg or a two-hour drive to the coast, there is a San Antonio for everyone and every budget that makes San Antonio a top pick for training.

Heather Davila, RDH, is the 2024 Vice President of Communications for the Bexar County Medical Society Alliance.
For more information on the Bexar County Medical Society Alliance, scan the code below:

10 SAN ANTONIO MEDICINE • April 2024 BCMS ALLIANCE


Visit us at www.bcms.org 11
Demystifying AI Diagnostic Tools: Musings of a Tech-handicapped Physician
By Soma Jyothula, MD, FCCP
The tip of the spear for Artificial intelligence (AI) in my social consciousness is Chat GPT. Chat GPT has entered physician parlance like CBC, CMP for a first-year medical student rounding in the ICU. My 14-year-old son has an opinion on Chat GPT about how it can be a contribution for his academic excellence. And again, his school district had to temper his expectations by making him sign a pledge to avoid using Chat GPT to generate his school reports — “What a bummer,” were his final words. PLOS Digital Health published an article showing Chat GPT can pass USMLE exams with a 60 percent accuracy.1 In this era of the viral spread of news on social media, lo and behold, the doomsday predictions started showing up. Is AI going to replace physicians if a natural language program like Chat GPT can pass USMLE? Time to go down the rabbit hole during my pre-sleep internet browsing routine, leaving my Tik Tok app alone (I can already see my sleep physician buddy rolling his eyes after the chat he gave me on “Sleep Hygiene,” San Antonio Medicine magazine, March 2024). And again, I had to convince myself that the act was driven by the core human drive of self-preservation.
Scientific inquiry underpins our profession as a practitioner of medical science. So, the first question will be, “What is AI?” AI is a technology that enables machines (computers) to simulate human intelligence and problem-solving capabilities. 2 Three broad categories exist. Artificial Narrow Intelligence (ANI) is AI trained and focused on specific tasks. This technology is widely available outside the confines of the medical field. Siri, on your iPhone, utilizes this to provide you with the answer for how many meters in so and so feet. Facebook uses it to suggest tagging all your colleagues in the last office party picture you posted. The medical equivalent will be uploading an Xray into a program and asking whether there is a pneumothorax. Yes, we will be flavored by pulmonary medicine (country cousin
to Cardiology in the thorax). The other categories are Artificial General Intelligence (AGI) and Artificial Superintelligence (ASI). AGI is a machine with an intelligence equal to humans. The machine will be self-aware with a consciousness and has the ability to solve problems, learn and plan for the future. This is like having a robot that will handle the patient after you are done with your bronchoscopy — place appropriate orders, monitor recovery, provide discharge instructions and follow up in the post-discharge clinic with an empathetic disposition (the ideal pulmonologist). ASI will be a machine that will supersede humans in intelligence and ability. The same robot can predict the needs of the patient, chart the course of procedure, and provide the outcomes and prognosis — like a psychic predicting your future and health (not happening). AGI and ASI exist only in science fiction and occasionally appear on your TV/iPad/smartphone as a streaming movie or show (aka Cyborg in Terminator movies). Pun aside, they are theoretical constructs and will be our replacements when they manifest (‘when’ is highlighted deliberately).
AMA uses the term “Augmented intelligence” as a surrogate for AI, emphasizing the conceptualization of AI’s assistive role, designed to enhance human intelligence and not to replace it.3 So, the fear of AI replacing a homeothermic, living and breathing physician is farfetched

HEALTH TECHNOLOGIES
12 SAN ANTONIO MEDICINE • April 2024 Figure 1
for now. The next question is when AI intruded the medical field. As any researcher worth his salt, PubMed was queried with the search term “Artificial Intelligence.” Lo and behold, the first paper was published in 1951 and titled “Matter over mind: a neurological research robot.” 1980 was the first year when more than 10 papers related to AI were published and, at last count, 37,808 scientific papers were published in 2023 (Figure 1). AI entered my professional domain when I became part of a research group evaluating an AI tool to diagnose patterns and predict outcomes of Pulmonary fibrosis based on CT Chest images.4
For the sake of brevity, I will confine further discussion specifically to diagnostic AI tools and how to evaluate them as a clinician. The FDA has a digital center of excellence and all software incorporating AI in medical devices requires approval by the FDA. The PAPNET™ testing system, an automated computer-assisted pathology tool to evaluate pap smears, was the first FDA-approved AI tool in 1995. Since then, 692 medical devices with AI tools have been approved to date and are predominantly in the field of radiology and cardiovascular medicine.5 The struggle I faced was, if I see a paper talking about AI tools in medicine, how does a non-tech professional like me review it. In the end, AI tools are clinical prediction tools like the Well’s score for pulmonary embolism prediction. The difference is that instead of humans curating the data points and performing statistical analysis, software programs replicate human intelligence in providing the output (risk of Acute PE based on prespecified patient characteristics).
As any clinical tool we use, for widespread use it must be evaluated in a robust and scientific manner for validity of the result and replicated in various cohorts of patients. As an example, we are going to evaluate a new tool that will report the presence of pneumothorax on an X-ray. And yes, it happens to an experienced pulmonologist like me after performing a bronchoscopy (much to my chagrin). First, the query, which here will be the presence of pneumothorax. The input will be all chest X-rays done after a bronchoscopy along with expert diagnosed pneumothorax (say 2 percent). We will input the chest X-Rays (1,000 images) acquired in a specific format into the software. The software will use some of the images as part of the training set, use its machine-learning algorithm, and will be labeled pneumothorax (yes or no). Then we will use the rest of the images and evaluate the robustness of the AI program as part of the tuning set. Once we have the algorithm tuned, we will use another cohort of patients’ chest X-rays (500 images) and validate the algorithm. We will evaluate the performance metrics (usual statistical tools like positive and negative predictive value). Any tool that will provide a 100 percent PPV and NPV will be incredible and essentially mimics a trained radiologist in accuracy. In the real world, no tool has come close. This is where you must look under the hood and trust your judgment as a physician. Is 95 percent good for you? Will it mean I can blindly trust the algorithm? Probably not. Remember, it is an artificial
augmented tool — we still need to apply our clinical nous. As my mentor would remind me again and again in my research days, trash in means trash out for any research study. Good data and robust analysis lead to good results. JAMA published an excellent article to evaluate articles using machine learning, and I highly recommend reading it.6
A recent survey published by AMA on physician sentiments towards AI shows 65 percent of physicians see an advantage with AI. Forty-one percent of physicians reported they were equally excited and concerned. Seventy-two percent see promise in supporting diagnosis, and 69 percent on workflow. Patient physician relationship and privacy remain major concerns.7 AI tools are here to stay, and we will notice them more in our field in administrative, diagnostic and delivery domains. As members of the scientific field, it is our responsibility to critically evaluate every tool for accuracy, bias, privacy and ethics. The impact of Siri giving wrong recommendations due to my Indian accent will be a temporary irritation compared to missing a pneumothorax based on AI recommendation, which can have profound deleterious effects on a patient.
References:
1. Kung, TH et al. Performance of ChatGPT on USMLE: Potential for AI-assisted medical education using large language models. PLOS Digit Health. 2023 Feb 9;2(2):e0000198. doi: 10.1371/journal.pdig.0000198. PMID: 36812645; PMCID: PMC9931230
2. https://www.ibm.com/topics/artificial-intelligence
3. https://www.ama-assn.org/practice-management/digital/augmented-intelligence-medicine
4. Walsh, SLF et al. Learning-based Outcome Prediction in Progressive Fibrotic Lung Disease Using High-Resolution Computed Tomography. Am J Respir Crit Care Med. 2022 Oct 1;206(7):883-891. doi: 10.1164/rccm.202112-2684OC. PMID: 35696341
5. https://www.fda.gov/medical-devices/software-medical-devicesamd/artificial-intelligence-and-machine-learning-aiml-enabledmedical-devices
6. Liu, Y et al. How to Read Articles That Use Machine Learning: Users' Guides to Medical Literature. JAMA. 2019 Nov 12;322(18):1806-1816. doi: 10.1001/jama.2019.16489. PMID: 31714992
7. https://www.ama-assn.org/system/files/physician-ai-sentiment-report.pdf

Soma Jyothula, MD, FCCP, is a practicing pulmonary and critical care physician, and is the Chief of Pulmonary Medicine and Lung Transplantation at Methodist Hospital. Dr. Jyothula is a member of Bexar County Medical Society and serves on the Publications Committee.
Visit us at www.bcms.org 13
HEALTH TECHNOLOGIES
Big Data and AI
By John J. Seidenfeld, MD
If Data is like the size of the Earth, then Big Data is the Sun. A byte of data is eight bits or 0 or 1 in sequence. The new unit of measurement is an exabyte, which is one billion gigabytes. The National Institutes of Health (NIH) is planning on-line databases, which will contain 40 exabytes of data. “We have the opportunity to be able to deliver so much more in terms of real high-quality, well understood results that can help guide care for people,” said new NIH chief, Monica Bertagnolli, a renowned cancer surgeon and in her last position was the first woman to lead the National Cancer Institute (NCI). These breakthroughs are possible using the combination of Big Data and Artificial Intelligence (AI).1
Big data sources include data sets from medicine such as clinical and research-automated health records, wearable devices and home monitor data, pharmacologic data, health insurance claims data, pathologic studies, radiographic studies and laboratory data, DNA sequencing and other genomic data, and protein structural analyses including folding patterns. Other sources of big data are audio recording masters, film studio archives, virtual reality media assets, geophysical maps, all user interfaces from computers and phones, and more. It is estimated that in 2025 (next year), 463 exabytes of data will be generated daily. These are big data sets often stored in the “cloud,” in external storage, and targets of hackers and other illegal miners.
How does big data analytics (BDA) concern medical practitioners and other healthcare professionals?
What are aspirational goals as well as current realities?
• In a primary care setting, a physician may see 10 people or less with a relatively unusual condition over a lifetime. That physician could gain from the experience with up to millions of such patients through big data analytics. New tools will aid us by presenting the clinician with inexpensive, always available, and complete and exhaustive knowledge of all medical literature based on billions of hours of clinical experience. The practitioner may gain from these tools for understanding, diagnosis and treatment in real time, and this may lead to earlier diagnosis and treatment before the threat of severe complications.2
• The New England Journal of Medicine has begun a new journal on AI with the first edition in January of 2024.3 It is one of many new journals devoted to BDA studies. Newspapers like the Washington Post have introduced stories and columnists like Leana Wen to report on AI tools.
• Pandemic recognition might occur within days of new virus recognition by claims data, sewage data analytics and international data sharing techniques.

• Individualized therapy based on genetic analysis could lead to improved and targeted therapy in cancer and other conditions. The cost of a gene sequencing study has dropped in part due to BDA from one million dollars in 2007 to one hundred dollars in 2023.
• Drug development might be streamlined by better understanding of protein folding patterns and use of targeted protein attached ligands. These ligands will be used to approach specific targeted cells and receptors.
• BDA might improve the business of medicine by a) creating complete views of consumers, patients and physicians in a community, b) iden-
14 SAN ANTONIO MEDICINE • April 2024
HEALTH TECHNOLOGIES
tifying geographic markets with a high potential for growth, c) boosting healthcare marketing with information about consumer, patient and physician needs and preferences, and d) optimizing hospital growth by improving care efficiency, effectiveness and personalization.4
• BDA will help us to work toward the goals of understanding an increasing volume of healthcare data, reducing healthcare costs to a GDP figure closer to that of other industrialized countries from currently 18 percent to 12 percent, and improving the care experience.
• BDA helps communicate with patients in the language they understand or at their level of health literacy. The platforms for patient communication can “learn to speak” as the patient might find comparable to their own.5
• Supercomputers are being used to simulate brain neural networks and may eventually help with thought simulation, brain disorder simulation, hormonal release sequencing and presurgical mapping to name a few uses. Many countries employing BDA are involved in so called “Blue Brain” projects.6, 7, 8
What concerns should we have about BDA?
Eric Perakslis9 cautions us to be concerned about the quality of data entered which needs upgrading from the present “cut and paste” approach, which may lead to easy but false data entry.
Many researchers and other clinicians are using games to improve attention to treatment, questionnaires, instructions and consent forms. Merriam-Webster defines “gamification” as the process of adding games or game-like elements to something to encourage participation. Perakslis cautions about serious “gamification” or games used to treat depression, anorexia or insomnia, for example, that need to have excellent databases and extensive testing before use to assure safety and efficacy. This also applies to the use of “gamification” to continue participant interest in entering data for clinical trials and allowing patients to ask questions to achieve a more complete informed consent.
Also of great concern in these processes are the development of algorithms, which reflect the biases of the developers. Bias control through testing and revision is essential in creating algorithms for widespread multicultural use and if not controlled could lead to serious errors in data interpretation.
Of course, privacy and safety of data use will continue to threaten any work in this field. Data leaks, hacking, dark web replication and mal actors of many types including bots may be magnified with access to BDA.
Perakslis warns us, “People need to be really focused. Tech companies that are promoting AI and rolling out these new tools quickly are going to be in the cross hairs of the aftermath when those tools are inevitably misused. It’s important to be thoughtful in picking partners to work with and making sure you ask the right questions before proceeding.
The bleeding edge of these technologies is human talent, so if you’re struggling to keep up in this space, hire smart people. It’s also important to focus on the basics (cleaning up your data, etc.) before jumping into these new technologies to ensure the technologies work in your favor.”
Summary
We are embarking on a new era with BDA and nothing short of a revolution will occur in medicine.10 We must be forever both aspirational and skeptical as we navigate the complex changes that are occurring. The information we use should improve patient care and be trustworthy. We must continue to be lifelong learners. Our patients are counting on us to get the best and most up-to-date information for improved diagnosis and treatment and to do no harm. Let us use BDA and all the other tools available to accomplish the goal of care while being careful about processes used and data quality.
References:
1. https://www.science.org/content/article/once-reluctant-new-nihchief-monica-bertagnolli-has-embraced-her-leading-role?utm _source=sfmc&utm_medium=email&utm_content=alert&utm_c ampaign=DailyLatestNews&et_rid=38463735&et_cid=5038241
2. Geoffrey Hinton: Large Language Models in Medicine. They Understand and Have Empathy (substack.com), interview with Gregory Hinton and quote from Ilya Sutskever, chief scientist at OpenAI
3. https://ai.nejm.org/toc/ai/current
4. https://webmdignite.com/faq/what-is-healthcare-big-data
5. https://www.ucsf.edu/news/2021/12/422006/ai-points-way-better-doctor-patient-communication
6. https://www.irjmets.com/uploadedfiles/paper/issue_5_may_ 2023/38790/final/fin_irjmets1684264272.pdf
7. https://www.newscientist.com/article/2408015-supercomputerthat-simulates-entire-human-brain-will-switch-on-in-2024/
8. https://www.nature.com/articles/d41586-023-03954-y
9. https://rethinkingclinicaltrials.org/news/grand-rounds-august-42023-ai-ml-want-to-play-a-game-eric-perakslis-phd/
10. Peter Lee, Isaac Keohane, et al The AI Revolution in Medicine: GPT-4 and Beyond. 2023. ISBN-13 978-0138200138 1st Edition

John Seidenfeld, MD, MSHA, FACP, is an Associate Professor, CASE, at the University of the Incarnate Word School of Osteopathic Medicine. He is a member of the Bexar County Medical Society and serves on the Publications Committee.
Visit us at www.bcms.org 15
TECHNOLOGIES
HEALTH

UT Health Science Center San Antonio Develops Tool That Counts Brain Lesions in Seconds: Novel AI algorithm precisely quantifies perivascular spaces that signal risk of stroke
Courtesy of Will Sansom, The University of Texas Health Science Center at San Antonio
16 SAN ANTONIO MEDICINE • April 2024 HEALTH TECHNOLOGIES

An artificial intelligence (AI) tool developed at The University of Texas Health Science Center at San Antonio accurately counts brain lesions on MRI scans within seconds. Once it is adapted to the clinic, the AI tool should help neuroradiologists to evaluate patients’ brain diseases at earlier stages.
“Certain kinds of brain lesions are tremendously difficult to quantify without AI,” said researcher Mohamad Habes, PhD, of the health science center’s Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases. Habes is Assistant Professor of Radiology and Director of the Biggs Institute neuroimaging core.
In a study published April 2024 in JAMA Network Open, Habes and colleagues from eight institutions demonstrated the AI tool’s utility in identifying and counting enlarged perivascular spaces (ePVS’s). These spaces, filled with cerebrospinal fluid, surround arteries and veins and are a marker of cerebral small-vessel disease that can lead to stroke and dementia. The study was a follow-up analysis of 1,026 individuals who participated in the Multi-Ethnic Study of Atherosclerosis (MESA). “We have developed an innovative deep-learning tool to precisely quantify every single enlarged perivascular space in the brain and provide us with a map of the patient’s small-vessel disease,” Habes said.
Taking a painstaking task and making it possible
Before this tool, ePVS’s were ignored because of the difficulty of counting them on MRI scans. “On average a middle-aged person might have maybe 500 or 600 of these small spaces on an MRI,” Habes said. “Think about a neuroradiologist who is going to sit down and count all of them. That’s not really going to happen. He or she would spend one or two hours per scan, or even more, and that amount of laborious effort is not feasible in the workflow of a busy clinic.”
The team described the automated deep-learning method for ePVS detection in the journal Neuroimage: Reports on March 7, 2023. “We have trained an algorithm with expert knowledge to be able to quantify these lesions on its own,” Habes said. “This tool recognizes them, tells us their exact locations, counts them and tells us their volumes. It tells us a ton of information about them, far more than what a human can do.”
In the JAMA Network Open report, Habes and coauthors studied enlarged perivascular spaces throughout the brain. “Before, people were not able to do whole-brain ePVS quantification,” Habes said. “We can now do it with our advanced deep learning tools. In our study, we realized that enlarged perivascular spaces in two regions, the basal ganglia and the thalamus, are the most significant lesions because they showed association with stroke and small-vessel disease markers.”
Left: Dr. Mohamad Habes, UT Health Science Center San Antonio
continued on page 18
Visit us at www.bcms.org 17
TECHNOLOGIES
HEALTH
HEALTH TECHNOLOGIES
continued from page 17


San Antonio Team
San Antonio Brain Scans
Opposite page: Patient receiving MRI at UT Health Science Center.
18 SAN ANTONIO MEDICINE • April 2024
Above: UT Health Science Center
Left: UT Health Science Center

The basal ganglia is a deep-brain region important for neurodegenerative disorders and is related to movement and decision-making, Habes said. The thalamus, a region near the basal ganglia, is related to sensory functions such as taste and touch.
The researchers’ hope is that the AI tool for enumerating brain lesions will be further studied at the Alzheimer’s Disease Research Centers (ADRCs), which are U.S. National Institute on Aging-Designated Centers of Excellence. The South Texas ADRC, the only such center in Texas, is a collaboration of UT Health Science Center San Antonio’s Biggs Institute with The University of Texas Rio Grande Valley. “This is a great breakthrough for our ADRC, which is focusing a lot on cerebrovascular disease and its contribution to dementia,” Habes said. “This is one of the unique themes of our ADRC, and we think our novel AI methodology can benefit largescale studies conducted across the nation’s ADRCs.” The AI tool leverages the power of UT Health Science Center San Antonio’s Genie supercomputer, Habes said.
Assessment of Risk Factors and Clinical Importance of Enlarged Perivascular Spaces by Whole-Brain Investigation in the Multi-Ethnic Study of Atherosclerosis
Sokratis Charisis, MD; Tanweer Rashid, PhD; Hangfan Liu, PhD; Jeffrey B. Ware, MD; Paul N. Jensen, PhD; Thomas R. Austin, PhD; Karl Li, MD, PhD; Elyas Fadaee, MD; Saima Hilal, MD, PhD; Christopher Chen, MD; Timothy M. Hughes, PhD; Jose Rafael Romero, MD; Jon B. Toledo, MD, PhD; Will T. Longstreth Jr, MD; Timothy J. Hohman, PhD; Ilya Nasrallah, MD, PhD; R. Nick Bryan,
MD, PhD; Lenore J. Launer, PhD; Christos Davatzikos, PhD; Sudha Seshadri, MD; Susan R. Heckbert, MD, PhD; Mohamad Habes, PhD
First published: JAMA Network Open, April 24, 2023
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2 803993
The University of Texas Health Science Center at San Antonio (UT Health San Antonio), a primary driver for San Antonio’s $44.1 billion healthcare and biosciences sector, is the largest academic research institution in South Texas with an annual research portfolio of more than $360 million. Driving substantial economic impact with its six professional schools, a diverse workforce of 7,900, an annual operating budget of $1.23 billion and clinical practices that provide 2.6 million patient visits each year, UT Health San Antonio plans to add more than 1,500 higher-wage jobs over the next five years to serve San Antonio, Bexar County and South Texas. To learn about the many ways “We make lives better®,” visit www.uthealthsa.org.
The Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases is dedicated to providing comprehensive dementia care while advancing treatment through clinical trials and research. The Biggs Institute is a National Institute on Aging (NIA)-designated Alzheimer’s Disease Research Center (ADRC). In addition to patient care and research, the Biggs Institute partners with the School of Nursing at UT Health San Antonio to offer the Caring for the Caregiver program.
Visit us at www.bcms.org 19
TECHNOLOGIES
HEALTH

Leveraging Technology to Improve Primary Care Quality and Access
By Prisiliano Salas Jr., MD
As 21st century physicians, we have seen how quickly the medical care delivery model has evolved, largely in part to technological advancements. Although a tried-and-true physical exam is still a key component to a medical assessment, the 21st century offers a plethora of technological tools for medical diagnosis that have significantly impacted the healthcare field. How have we leveraged technology in the setting where most medical care starts?
Primary care is where health technology has the greatest potential to increase access and improve healthcare delivery, for both individuals and the community at large. The invention of the telephone addressed one of the biggest barriers to healthcare access by eliminating geographical distance. This “primal” invention dating back to the mid-19th century spearheaded a more prompt healthcare delivery and follow up. With a simple telephone call, you could quickly obtain a medical history, subjective information, objective data like vital signs, and make
an educated assessment and plan for many medical ailments without the patient leaving their home; especially for those with reduced access to care in rural or underserved locations.
Since then, healthcare technology has evolved even faster into the late 19th century and the 20th century with the inventions of computers and the internet. Modern computers and high-speed internet have led to the development of health applications, health wearables and remote monitoring devices. They can provide access to virtual primary and specialty consultations, as well as general healthcare information, symptom checkers and even medication reminders. These platforms are often used simultaneously and can be consumer-focused or medical-grade, are available in mobile or web-based forms, and allow patients to be more proactive in managing their health and receiving timely support for their primary care needs.
All this data can now be accessed and documented in electronic
HEALTH TECHNOLOGIES
20 SAN ANTONIO MEDICINE • April 2024
health records, health information exchanges, patient portals and other communication tools to add an extra layer of health access — offering a more direct way for providing updates on health metrics to a patient’s primary care clinician. These tools are proving to be most useful in the management of chronic medical conditions by tracking vital signs and/or monitoring medication adherence, allowing PCPs to intervene proactively and adjust treatment plans when necessary in an effort to enhance continuity of care, reduce clinic visits and decrease hospitalization rates.

On a community level, technology can facilitate large-scale primary care health initiatives through mass outreach, education and engagement. This wider health information dissemination can be done through digital media, social platforms and many online resources to promote healthy behaviors, provide validated health information and encourage proactive engagement with primary care services at all sectors of the population.
To further enhance primary care access and delivery today, artificial intelligence (AI) is the latest technological advancement available now to both consumers and healthcare professionals. AI is quickly evolving and becoming embedded in many healthcare systems and platforms. AI can provide diagnostic decision support tools, AI-powered algorithms in imaging interpretation, and even note taking or predicting health outcomes, all in an effort to improve healthcare access and clinical decision-making, as well as reduce diagnostic errors.
All this is great, but there are some downsides to technology use in healthcare. Some downsides include accuracy and technical challenges, privacy and security risks as well as dependency, anxiety and data overload concerns. However, technology offers a significant opportunity to revolutionize medical care — providing improved access, patient empowerment, personalized medical care and optimization of treatment plans, medication management and lifestyle recommendations for each patient’s needs that extends beyond the single in-person medical visit of yesteryear.
References:
- Dorsey ER, Topol EJ. State of Telehealth. New England Journal of Medicine. 2016;375(2):154-61. DOI: 10.1056/NEJMra1601705
- Mehrotra A, Jena AB, Busch AB, Souza J, Uscher-Pines L, Landon BE. Utilization of telemedicine among rural Medicare beneficiaries. JAMA. 2016;315(18):2015-6. DOI: 10.1001/jama.2016.2186
- Huckvale K, Prieto JT, Tilney M, Benghozi PJ, Car J. Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment. BMC Medicine. 2015;13(1):214. DOI: 10.1186/s12916-015-0444-y
- Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. Journal of the American Medical Informatics Association. 2007;14(3):269-77. DOI: 10.1197/jamia.M2270
- Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. Journal of the American Medical Informatics Association. 2010;17(3):288-94. DOI: 10.1136/jamia. 2010.004820
- Rajkomar A, Dean J, Kohane I. Machine learning in medicine. New England Journal of Medicine. 2019;380(14):1347-58. DOI: 10.1056/NEJMra1814259
- Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313(5):459-460. DOI:10.1001/jama.2014.14781
- Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. British Journal of Sports Medicine. 2014;48(13):1019-1023. DOI:10.1136/bjsports-2014-093546
- Bonato P. Wearable sensors and systems. IEEE Engineering in Medicine and Biology Magazine. 2010;29(3):25-36. DOI:10.1109 /MEMB.2010.936298

Prisiliano Salas, Jr., MD, is board certified in Family Medicine and Lifestyle Medicine with more than a decade of experience. Dr. Salas is co-owner and CEO of Salveo Direct Care, and a member of the Bexar County Medical Society.
Visit us at www.bcms.org 21
TECHNOLOGIES
HEALTH

Patient Hacking: Wearable Medical Devices Vulnerable to Malice
By David Alex Schulz
When Vice President Cheney’s cardiologist disabled his pacemaker’s wireless in 2007, the logic was unassailable. "It seemed a bad idea for the vice president to have a device that somebody on a rope line or in the next hotel room or downstairs might be able to hack into," said Dr. Jonathan Reiner last year. He was prescient in 2007 with today’s common wisdom. As the popularity of personal “wearable” connected devices has grown, so has anxiety over cybersecurity.
To be clear, this article concerns only devices in a patient’s personal care. Hospital- and clinic-resident devices are covered by HIPAA security guidelines, and require regular personnel training and strict technical practices.
Patients and consumers, on the other hand, are offered little guidance on protection from cyber-incursion. The threat is just as significant. To help simplify and define these threats, we must distinguish wearables into categories of passive and active devices.
Passive devices collect and aggregate health information without directly altering bodily functions. They monitor various health parameters and provide valuable data insights to users and their healthcare providers. Common examples include fitness trackers, glucose monitors, wearable ECGs and blood pressure monitors. Such instruments are even incorporated into “smart clothing,” offering continuous vital sign monitoring while being comfortable and discreet. Their risk is that they each become warehouses of electronic personal health information
22 SAN ANTONIO MEDICINE • April 2024 HEALTH TECHNOLOGIES
(ePHI). Cyber-pirates lust medical data. It’s rich in personal information from the mundane like personal identifiers to the more obscure relating to diagnosis and disease. This information is enormously useful to fraudsters to create fake IDs, submit false insurance claims and defraud Medicare and Medicaid. ePHI records go for anywhere from $100 to $1,000 dollars on the black market. To a sophisticated crook, a Fitbit is potentially more valuable than a Rolex.
Active Devices are those that directly affect physiology, as well as collecting data. They intervene in the body’s processes to manage medical conditions. These devices have the potential to affect users' health in real-time and require precise control to ensure safety and effectiveness. They include wearable insulin pumps and other drug delivery systems, electronic neurostimulation devices, and assistive devices for patients with disabilities or chronic conditions. Examples include wearable exoskeletons for mobility assistance or devices that help monitor and manage symptoms of neurological disorders.
Although diverse in purpose and approach, all active devices share common weaknesses in the communication between the host’s metabolism, the device, its home monitoring system, the relay to a central data archive, the provider’s office, and finally to the care team (Figure 1).
tions over less than a decade. Innovative crime waves always descend the victim food-chain from whales down to minnows: from institutions down to individuals. Since COVID, ransomware has become as widespread for home users as office workers. Now, extend that to extortion, not of a victim’s data but instead … of their health. Holding a person’s heartbeat for ransom by remote control seems like a ludicrous plot for a movie-of-the-week, until it happens in real life.
The Journal of the American College of Cardiology points out that, “for patients with implantable cardioverter-defibrillators (ICDs), it is possible for hackers to interrupt wireless communications, inhibiting the value of telemonitoring and allowing any clinically relevant events to go undetected by the system. Oversensing may inhibit pacing or result in inappropriate or life-threatening shocks. Battery depletion can lead to a device being unable to deliver therapies during life-threatening arrhythmias.”
The prevailing industry belief, until recently, was that medical devices constituted a low risk to security. Budgets for security features were minimal and most devices did not have built-in security features. A study of nearly 5,000 medical devices that included a software component found that only 2.13 percent of their manuals included any cybersecurity content.

A breach anywhere in the chain of information custody, from device to phone (RF or blue tooth), to the cloud (home wi-fi router or G4 cellular), to the data-center (TCP/IP), to the healthcare portal, back to the healthcare provider, creates access points to the larger world of web servers, targets for serious hacking and ransomware injection. These types of attacks are, ultimately, the greater threat. Responding to the growth of Internet of Medical Things (IoMT), Congress established the “Ensuring Cybersecurity of Medical Devices” act, amending the Federa l Food, Dr ug, and Cosmetic Act, creating a new paradigm and set of resources for practitioners and public alike. Taking effect less than a year ago, the FDA features a new website replete with tools for mitigating cybersecurity risks, instructional videos, ongoing advisories and white papers, workshops and webinars, and advice on counseling patients who utilize such devices. It can be found at www.fda.gov/medical-devices/digital-health-center-excellence/cybersecurity and deserves consideration.
If security isn’t assured, the road to major health crises is short. Right now, the major primary risk is “only” the loss of an individual’s PHI and resulting fraud. But reflect for a moment on the stunning growth of ransomware attacks on hospitals, city services and financial institu-

David Alex Schulz is certified in HIPAA privacy and security compliance, serves on the BCMS Publications Committee and is a contributing writer to San Antonio Medicine magazine.
Figure 1
(Courtesy of the National Institute of Standards and Technology)
Visit us at www.bcms.org 23 HEALTH TECHNOLOGIES
University Health’s Pharmacy Services
Embrace Technology and Artificial Intelligence for Efficiency and Accuracy
By Jeniifer Hillman, PharmD, MBA
Technology and artificial intelligence are transforming the healthcare industry at an ever-increasing speed. The pharmacy department at University Health prides itself on utilizing state-of-the-art technology, automation and intelligence to prepare all medication doses. We are an industry leader serving as a beta site for many pieces of technology and a think tank for expanding pharmacy automation.
University Health’s Pharmacy Department uses more than 15 different automated or intelligence systems. The COVID-19 pandemic escalated our development of automated programs when supply chain and workforce disruptions forced us to find new ways to perform a variety of functions.
The pandemic is in part the reason University Hospital became the first hospital in Texas where the pharmacy team installed and operated a fully functional sterile medication compounding intravenous robot. Sterile medication compounds are prepared at all hospitals to administer life-saving medications for the most critically ill patients. These sterile preparations vary in complexity but all require 100 percent accuracy and integrity. The majority of intravenous medications were prepared manually. The labor shortage incurred during the pandemic, coupled with the increase in need for sterile medication preparations, directed our focus to compounding automation and intelligence. The robot we selected performs multiple tasks simultaneously for improved efficiency. It allows the pharmacy technician to focus on other tasks that cannot be automated while the robot is operating. The robot can only be operated by highly trained and skilled pharmacy staff with certification in automation and sterile compounding. University Health’s pharmacy team has trained the robot to recognize and compound with over 100 unique medication vials and diluents. In addition, the robot has smart technology to recognize partially exhausted medication vials as opportunities for future use during a compounding run. That limits waste.
Planning for the new Women’s and Children’s Hospital has also been a key driver for the selection and use of technology within the department. We needed technology that could prepare doses for our smallest patients in the NICU and a technology that was versatile enough to adjust for our adult women health patients. With this new population came an increased demand for non-sterile oral liquid medication doses. A large percentage of oral medication bulk bottles come in dry powder forms that must be further diluted for patients’ use. Previously, we per-
formed this task manually with graduated cylinders and large volume diluent bottles. To keep up with demand while still ensuring accuracy, we decided to automate and install automated diluent dispensers for oral dry powder medications. Now, the medication library is programmed by pharmacy staff to recognize NDC specific medications and the corresponding volume of diluent. The technology calibrates the volume of diluent required and dispenses only what is needed.
The additional patient capacity created with the opening of University Health’s Women’s and Children’s Hospital in December 2023 also increased the number of outpatient pharmacy prescriptions written for discharging patients. Previously, prescriptions ready for pick up were placed manually in totes that used a number system. When patients arrived at the window to pick up their medication, it took some time for staff to locate completed orders. The pharmacy has decreased the time needed to locate and deliver the medication to patients by installing intelligent pick-to-light technology. Pharmacy staff scan a barcode on the completed prescription. That lights up the patient prescription in a translucence bag identified with radio frequency, making it easy to locate quickly. Staff only need seconds to retrieve the prescription as opposed to minutes under the manual system. In addition, we installed high-speed prescription automation to fill vials, which is five times faster for preparing outpatient prescriptions. Instead of the staff waiting on the robot, the robot is now waiting on the staff to retrieve completed prescriptions. That makes a huge difference in efficiency for a pharmacy that dispenses thousands of prescriptions each day.
The pharmacy department at University Health is continuously seeking ways to incorporate state-of-the-art technology to improve safety and efficiency for our patients. We are a designated center of excellence for technology and automation, and are always willing to share our expertise with others to improve healthcare for all.

Jennifer Hillman, PharmD, MBA, is the Executive Director of Pharmacy for University Health Inpatient Pharmacy, and works extensively with pharmacy automation and technology, incorporating nearly 15 unique pieces of technology into the department. She recently completed a large-scale multi-site automated medication dispensing cabinet conversion project. Under her leadership, the Health System implemented the first IV compounding robot in Texas, and she partnered with a robotics company to create the first oral syringe filling fully autonomous robot.
HEALTH TECHNOLOGIES
24 SAN ANTONIO MEDICINE • April 2024

Orthopaedic Robotic Surgery
By San Antonio Orthopaedic & Spine Treatment Center
In recent years, the field of orthopaedic surgery has witnessed a revolutionary transformation with the addition of robotic technology.

Orthopaedic robotic surgery has emerged as a cutting-edge approach that combines precision, efficiency and personalized care. This innovative technology is reshaping the way orthopaedic procedures are performed, providing surgeons with advanced tools to enhance surgical outcomes and improve patient recovery. In this article, we will delve into the world of orthopaedic robotic surgery, exploring its applications and the positive impact it has had on surgical and patient outcomes.
The Evolution of Orthopaedic Robotic Surgery
Orthopaedic robotic surgery has evolved from traditional surgical methods, incorporating robotic systems to assist and collaborate with surgeons during surgical procedures. The first generation of robotic systems primarily focused on computer-assisted navigation, aiding surgeons in planning and executing precise incisions. Over time, technological advancements led to the development of more sophisticated robotic platforms capable of real-time adjustments and greater autonomy. These tools are now regularly used in many orthopaedic practices across the world.
Applications in Orthopaedics
Orthopaedic robotic surgery has found applications across a range of orthopaedic procedures, including joint replacement surgeries, spine surgery and arthroscopic interventions. The precision offered by robotic systems is particularly beneficial in joint replacement surgeries, where accurate implant placement is critical for long-term success. Robotic-assisted joint replacement allows for a high level of customization, accommodating variations in anatomy and optimizing implant positioning.
In spine surgery, robots assist surgeons in navigating complex spinal structures with enhanced precision. This is especially crucial in minimally invasive procedures, where the surgeon's visibility and dexterity are limited. Robotic systems provide three-dimensional imaging and navigation, aiding in the placement of screws and ensuring optimal alignment of spinal implants.
Arthroscopic interventions, such as meniscus repairs and ligament reconstructions, benefit from robotic assistance as well. The precise control offered by robotic instruments enhances the surgeon's ability to perform delicate maneuvers in confined spaces, leading to improved outcomes and reduced recovery times.
Benefits of Orthopaedic Robotic Surgery
Utilizing advanced robotic-assisted technology offers several benefits for both surgeons and patients. Here are some of the key advantages of orthopaedic robotic surgery.
Precision and Accuracy: Robotic systems excel in executing precise movements with minimal deviations. This accuracy is particularly crucial in orthopaedic surgeries where precise incisions, implant placement and alignment significantly impact the success of the procedure.
Personalized Treatment: Orthopaedic robotic surgery allows for a high degree of customization based on each patient's unique anatomy. This personalized approach ensures that the surgical plan is tailored to individual characteristics, optimizing outcomes and reducing the risk of complications.
Minimally Invasive Procedures: Robotic assistance facilitates minimally invasive approaches, reducing the need for large incisions. This results in less tissue damage, decreased blood loss and faster recovery times for patients.
Enhanced Visualization: Three-dimensional imaging and real-time navigation provided by robotic systems enhance the surgeon's visualization during procedures. This heightened awareness contributes to better decision making and improves overall surgical precision.
Improved Patient Outcomes: The combination of precision, personalization and minimally invasive techniques often leads to improved patient outcomes. Patients undergoing orthopaedic robotic surgery may experience reduced pain, shorter hospital stays and faster rehabilitation compared to traditional surgical methods. While orthopaedic robotic surgery offers numerous advantages, it's important to note that the appropriateness of this approach depends on the specific case and the surgeon's expertise.
Schedule your consultation today
If you’re interested in learning more about these procedures, contact us and schedule your consultation today at 210-804-5400 or visit San Antonio Orthopaedic & Spine Treatment Center | TSAOG at www.tsaog.com for more information.
HEALTH TECHNOLOGIES
26 SAN ANTONIO MEDICINE • April 2024

Visit us at www.bcms.org 27

Physicians Health and Rehabilitation Program (PH&R): Remembering a role model and leader
By Monica Jones
2024 Alcohol Awareness Month
Alcohol Awareness Month is a valuable opportunity to reflect on our relationship with alcohol and its impact on our lives. It's a chance to educate ourselves and others about the potential risks associated with excessive alcohol consumption and to promote healthier habits.
Texas Alcohol Abuse Statistics1
• 17.6 percent of Texas adults over the age of 18 binge drink at least once per month.
• The median number of drinks per binge is 5.6; the 25 percent most active drinkers consume a median 9.0 drinks per binge.
• An average of 10,647 annual deaths in Texas are attributable to excessive alcohol use.
• The 5-year average annual rate of excessive alcohol deaths per capita in Texas increased by as much as 44.2 percent from 2015 to 2019.
• Texas averages one (1) death from excessive alcohol use for every 2,737 people aged 18 and older, or 4.90 deaths for every 10,000 adults.
• 71.1 percent of people who die from excessive alcohol use in Texas are male.
• 56.9 percent of excessive alcohol use deaths are from chronic causes, such as Alcohol Use Disorder.
• 81.9 percent of deaths in Texas from excessive alcohol use are adults aged 35 years and older.
• The CDC estimates 274,633 years of potential life is lost to excessive alcohol use each year.
• Texas taxpayers spent $18.821 billion as a result of excessive alcohol use in 2010; adjusted for inflation, this is equivalent to $25.408 billion or $2.69 per drink in 2022 U.S. dollars.
An estimated 10-15 percent of doctors will develop a problem with substance abuse at some point in their careers. Due to different stressors and access to drugs, the discipline of a physician will often have an impact on the substances that they use.2 To learn the risk factors for physicians in different specialties, visit https://americanaddictioncenters. org/healthcare-professionals/substance-abuse-in-doctors-accordingto-physician-specialty.
BCMS Physicians Health and Rehabilitation Program
The BCMS Physicians Health and Rehabilitation Program (PH&R) would like to use this month as an opportunity to raise awareness about alcohol-related issues in our community as well as promote our resources we offer to our members.
The BCMS PH&R program is confidential and led by a committee of physician colleagues that identify and facilitate the recovery success for other physicians whose abilities are impaired by alcohol or drugs. The goal is to help the impaired doctor return to practice and their home life free of alcohol and drugs. The program helps doctors learn how to cope with the stresses of modern medical practice and learn to live in a safe and peaceful environment without the need for their former coping mechanisms.
The BCMS PH&R program has set the standards for other programs across the state, receiving the Profiles of Excellence award in the Advocacy category from the American Association of Medical Society Executives (AAMSE) in July of 2022. In the almost 40 years of its existence, the committee has helped hundreds of physicians successfully recover while keeping patients safe. Those being helped are able to safely practice medicine and return to their families and practices whole again and renewed.
28 SAN ANTONIO MEDICINE • April 2024 ALCOHOL AWARENESS MONTH
Quote by the late PH&R Chair, Dr. Oliver Johnson:
“Caduceus meetings are critical; Caduceus is a protected forum where physicians with addiction problems can share their challenges openly and offer suggestions and encouragement to their fellow physicians. This exclusive forum where issues of practice difficulties and stresses can be aired and help offered is vital. These special considerations simply cannot be discussed in regular AA meetings.”
Caduceus meets at BCMS every Thursday night at 7 pm.
For more information about the Physician Health and Rehabilitation program, visit our website at www.bcms.org/phr.php or call Monica Jones, COO and staff liaison for PH&R at 210-301-4373.
Resources:
1. National Center for Drug Abuse Statistics (NCDAS)
2. American Addiction Centers

Monica Jones is the Chief Operating Officer and PH&R Staff Liaison at BCMS.


Visit us at www.bcms.org 29 ALCOHOL AWARENESS MONTH
Dr. Oliver Johnson with the PH&R Profiles of Excellence award, Advocacy category, from the American Association of Medical Society Executives.
Dr. Oliver Johnson
By Monica Jones

Sadly, we lost PH&R Chair Dr. Oliver Johnson last year to cancer. The PH&R Committee, together with his family, would like to share the eulogy from Dr. Alejandro Gonzalez (current PH&R Chair) to demonstrate the bond formed among individuals in our program.
“Hello, my name is Alejandro Gonzalez, and Oliver Johnson was my friend. What can I tell you about my friend, Ollie? Can I tell you he was very smart and very funny? That his dad was literally a rocket scientist? Ollie attended very good schools and got a wonderful education. He was a medic for four years in the USAF and he became a pharmacist before he became a Doctor of Medicine. He subsequently specialized in anesthesiology. He later developed a deep interest in photography and exhibited genuine talent. These indeed are interesting facts and say a lot about his work ethic and intelligence, but do they say anything about the “inside” man, Oliver Johnson?
Ollie and I met in November 1991. It was at Starlight Village Hospital, just outside of Center Point, Texas. I had “sobered up” at Starlight three years earlier, in August 1988. I was speaking that night at the Saturday AA meeting and Oliver was in the audience. He came up afterwards and introduced himself to me, and we experienced an instant bonding that lasts for a lifetime. A few weeks later, he left Starlight and got back to his home and professional life. He became very focused on “recovery.” When he spoke at meetings, there was an obvious sincere sense of gratitude, dignity and humility in his shares.
Fast forward to the summer of 1995. I was serving as the chairman of the Bexar County Medical Society PH&R committee. It was time to step down and ask someone else to serve as chair and, of course, I believed Ollie to be the ideal person. Ollie was genuine and was committed to recovery. He started to serve as chairman in June 1995 and continued for 28 years until his passing! The committee and Ollie won several awards for the work of the committee, with at least one of these awards being a very prestigious national recognition for our BCMS.
Ollie and I had many long conversations about recovery, and he would emphasize the fact he had a chronic, progressive, fatal malady. He needed to take his daily medicine for this malady. We reminded each other about the prescription given to us folks in recovery. The remedy for our malady was in the form of a three-legged stool. The legs of the stool were: Trust God, Clean House and Help Others! Ollie kept it simple. Ollie practiced what he preached. Being chairman of the BCMS PH&R committee was a lot of work. Many times, Ollie would go talk to doctors (who found themselves in trouble) late at night, holidays and weekends. Many of us on the PH&R committee were called by Ollie to go help with an intervention or two.
What I’m trying to give you is a picture of this human being who practiced the three-legged stool of recovery on a daily basis — trusting

God, cleaning house and being of service to his fellow man! Again, it was a simple concept, but it was not easy — it involved a lot of work. And Oliver Johnson did a lot of work. Ollie was all about service! All for free! This, Ollie believed, was love in action.
I will close with some thoughts about Ollie’s last nine months on this physical earth. Ollie contracted another fatal malady, which he succumbed to. He dealt with this one as he did with the other one for 32 years (one day at a time). Daily, Ollie and his family acted out an attitude of gratitude. Daily, Ollie and his family acted out an attitude of dignity. Daily, Ollie and his family acted out an attitude of humility unparalleled! He showed me not only how to live life on life’s terms but also how to die. The last time I laid eyes on Oliver Johnson was the night prior to his passing. Ollie was known for two sayings that he would repeat often in AA meetings: “I’m just another Bozo on the Bus,” and, “We don’t get a diploma/we don’t graduate from this program.” He was awake and I said to him, “I heard you’re getting a diploma, that you’re graduating from the program.” He gave me the most beautiful smile ever. I kissed him, held his hand and told him I loved him, and we said good-bye.
There is a Yiddish word meaning a person with integrity, dignity, with a sense of what is right and responsible. A stand-up guy. The word is Mensch. I asked who is the “inside” man, Oliver Johnson? The word is MENSCH. May his memory be a blessing to us all.”

Alejandro B González, MD, FAAP, is the Chair of the BCMS PH&R Committee, and Simulation consultant to UT Health Neonatology Fellows Simulation Program and University Health Services Perinatal Outreach Program.
30 SAN ANTONIO MEDICINE • April 2024 ALCOHOL AWARENESS MONTH
Photo by Dr. Oliver Johnson, taken in Scotland.

Alcoholics Anonymous: Only You Can Decide
By Teresa C., PICPC Chair
Since April is Alcohol Awareness Month, I would like to share some information about what Alcoholics Anonymous is — what it isn’t:
First and foremost, YOU are the only one who can decide if you are an alcoholic. If you think you may have a drinking problem, there are some questions that may help you decide:
1. Do you drink because you have problems?
2. Do you drink when you get mad at other people, your friends or parents?
3. Do you often prefer to drink alone, rather than with others?
4. Are you starting to get low marks, skipping work or responsibilities?
5. Do you ever try to stop, or drink less — and fail?
6. Have you begun to drink in the morning, before school or work?
7. Do you gulp your drinks, as if to satisfy a great thirst?
8. Do you ever have loss of memory due to your drinking?
9. Do you avoid being honest with others about your drinking?
10. Do you ever get into trouble when you are drinking?
11. Do you often get drunk when you drink, even when you don’t mean to?
The answers to these questions are nobody’s business but your own. If you can answer yes to any one of these questions, maybe it’s time you took a serious look at what your drinking might be doing to you.
Alcoholics Anonymous, otherwise known as “AA,” is a worldwide
fellowship of men and women who help each other maintain sobriety by sharing their own experiences, strength and hope with each other that they may solve their common problem and to help others to recover from alcoholism. AA is not allied with any sect, denomination, politics, organization or institution. It is a peer-based program derived of 12 steps, spiritual in nature, designed for personal recovery from alcoholism. AA is concerned solely with the personal recovery and continued sobriety of individual alcoholics who turned to the fellowship for help. They do not engage in any controversy, hold any position on outside issues nor engage in any research in alcoholism or medical or psychiatric treatment, and does not endorse any causes — although members may participate as individuals. Its members offer support freely, as it was given to them.
There are hundreds of AA meetings: “open” meetings are those that are open to the public, or “closed” meetings, for only those that identify as alcoholic. There are also women’s meetings, men’s meetings, gay, lesbian, LGBTQ, etc. You can find any of them by calling the Alcoholics Anonymous central office at 210-828-6235, or there is an app you can download called “Meeting Guide” (blue background with a white chair in the middle), which is available for your smartphone and filter those meetings that interest you.
Alcoholics Anonymous is grateful to the many non-alcoholics, professionals and others who have supported and recommended the AA program of recovery. Thousands of us owe our lives to them and our debt of gratitude knows no bounds.
Visit us at www.bcms.org 31 ALCOHOL AWARENESS MONTH

On September 7, 1977, the South Texas Regional Blood Bank honored the father of South Texas blood banking.
Dignitaries, including Mayor Lila Cockrell, gathered at 7078 San Pedro Ave. for the grand opening of the blood bank’s newest location, one dedicated to Dr. Robert Francis Gossett. A plaque was included on the building — a lasting reminder of his contribution.
He was the driving force for and first president of the locally based blood bank, making him the founding father of BioBridge Global. But very few know his story.
Creating a local blood source
In July 1972, South Texas was experiencing chronic blood shortages, mainly caused by a recent national move away from paid donors. Blood Services, the local blood bank, had become a large national organization. Any blood collected in San Antonio wasn’t guaranteed to stay.
In 1973, the Bexar County Medical Society’s Ad Hoc Blood Services committee — with Dr. Gossett at the forefront — proposed a local blood bank to provide for Bexar and 25 surrounding counties. After much negotiation with Blood Services, the South Texas Regional Blood Bank was chartered in November 1973, agreed to buy out Blood Services in January 1974, and completed the transfer in August.
His leadership brought hospitals and medical circles, and community together to create
Our Founding Father: Dr. Robert Francis Gossett
By Amanda Lozano (This story originally appeared in the January edition of Heart to Heart, the employee magazine at BioBridge Global.)
San Antonio’s first and only locally sourced blood bank. From a small building on 112 Auditorium Circle, Dr. Gossett led 12 employees to something greater.
An impressive resume
Born on February 22, 1910, in Dallas, he received his MD from the University of Texas Medical Branch in Galveston in May 1935. He began his practice in San Antonio in 1936, and except for four years in the United States Army Air Corps during WWII, continued well into the 70s. A renowned professional, Dr. Gossett served on countless medical boards and committees. He was active at Baptist Memorial Hospital, serving as Chief of Staff of Surgery. A longtime member of the BCMS, Gossett served as President in 1955.
BCMS Presidency
In 1955, polio was disabling thousands of Americans annually, but field trials of a vaccine were taking place in multiple locations, including San Antonio. Dr. Gossett worked with supply houses to bring 45,000 vaccines for local children. He ensured a fair distribution system was set up. By 1956, polio had plummeted, with only 96 cases and four deaths reported. The following year, cases fell to a 10-year low. Dr. Gossett helped make it possible. He also publicly campaigned for more hospital beds in San Antonio, stating the city had only 42 percent of its needs. According to sta-
tistics conducted by BCMS doctors, the city had 1,426 beds and needed 1,600 more to meet national standards. That effort helped lead to what is now Methodist Hospital, built in September 1963.
In April 1955, Dr. Gossett traveled to Fort Worth and advocated for integration within statewide medical organizations. He said doctors of color should undergo the same review process as any other BCMS members did, ensuring anyone approved was “ethical and professional,” regardless of race.
He also spearheaded one of the first locally aired television shows: Bexar, M.D., a weekly 15-minute segment aired on WOAI Channel 4. It shed light on the modern practice of medicine and featured doctors from the Bexar County Medical Society.
Kindness as a kid
Dr. Gossett’s contributions to San Antonio’s medical advancement were vast, but his altruism began as a child. A story shared by Frank Dodson, one of Dr. Gossett’s former patients, paints a picture: “Dr. Robert, while operating on my big toe, relayed to me, I think to distract me, how he got into the cattle business. He said when he was around my age, about 10, that he used to go to the rail line in Devine when they were loading cattle. Many of the young calves were too weak to make the load so they were just discarded next to the tracks. He would put a rope on them, take them
32 SAN ANTONIO MEDICINE • April 2024 SAN ANTONIO MEDICINE
home and nurse them. He stated it was those cows which enabled him to go to college and that he still had a fine herd of cattle as a result.”
Dr. Gossett’s father, William Calvin Gossett died when he was 1 year old. The loss of a father so young may have accounted for the empathy exhibited throughout Dr. Gossett’s life. He had a heart for people, particularly youth and underrepresented communities.
His mother, Lula Teel, lived with Dr. Gossett and his wife, Anne, for many years after her retirement from teaching. She was 80 when she died in 1962.
Contributing to the community
Gossett joined the board of directors of the Mexican Christan Institute in 1954. Its kindergarten, clinic and recreational programs were a lifeline for many poorer West Siders. During the Biafra War in 1967, he worked to save starving children.
In 1955, he became the volunteer onsite doctor at Boysville, “the farm home with a heart for homeless boys.” He was named honorary director in 1962 and served as the onsite physician for 20 years. Upon his retirement, Boysville lauded his service as a “true dedication beyond the call of duty.”
But he had one major project left.
His final act
Despite retiring, Dr. Gossett was determined to create a local blood bank. He brought together local physicians, hospitals and community leaders to create an organization that would serve the region to this day.
That organization quickly outgrew its original location and obtained a building on San Pedro Avenue in 1977.
Photos from September 7 portray Dr. Gossett with an air of dignity. Smartly dressed, his eyes exude kindness behind the spectacles, albeit a little tired, even as he accepted a copy of the plaque from colleague Dr. Charles Robinson. The unveiling of the plaque at the new location was the final act of a long and remarkable career.



cumbed to cancer. He was buried in Devine, where his dreams began as a young boy. Forever memorialized on his grave is a reference to The House on the Side of the Road, by Sam Walter Voss: “Build me a house by the side of the road and let me be a friend to man.”
Little did he know how much his foresight would affect the Alamo City. By 1984, more than 50,000 people had donated blood. Another larger location was needed. When the South Texas Regional Blood Bank expanded
to an even larger facility on McCullough Av enue in 1984, Dr. Gossett’s widow, Anne, was present for the ribbon-cutting ceremony.
It was a tribute to the man who made it all happen: Dr. Robert Francis Gossett.

Amanda Lorraine Lozano is a multimedia specialist at BioBridge Global. She creates content used internally for the company. A former newspaper woman, she loves to research, interview and photograph people of interest.
Visit us at www.bcms.org 33 SAN ANTONIO MEDICINE
Top left: Anne Gossett did the honors at ribbon-cutting ceremonies at the downtown location in 1984.
Top right: The Father of South Texas Blood Banking, Dr. Robert Gossett addresses the public during the grand opening of the South Texas Regional Blood Bank’s second location on 7078 San Pedro.
Bottom: Dr. Robert Francis Gossett (left) accepts a copy of the plaque from colleague Dr. Charles Robinson (right). The plaque was a dedication to Gossett, who spearheaded the South Texas Regional Blood Bank’s grand opening on September 7, 1977.
We Are All Public Health: Celebrating National Public Health Week – April 1-7, 2024
By The City of San Antonio Metropolitan Health District
Every year during the first week of April, communities across the nation celebrate the role and impact of public health. The American Public Health Association (APHA) brings communities together across the United States to observe National Public Health Week (NPHW). From April 1-7, the City of San Antonio Metropolitan Health District (Metro Health) will celebrate NPHW by recognizing the contributions of public health and highlighting issues that are important to improving the health of communities.
This year’s theme is “Protecting, Connecting and Thriving: We Are All Public Health," emphasizing the relationships we foster in our communities and the importance of coming together to support public health. We are all interconnected. When we all come together to support public health, all of us — individuals, families, communities — can achieve the goals of public health.
During NPHW, each day represents a specific public health topic and encourages individuals to find ways to contribute to it. These topics are essential for building the healthiest nation in one generation, and everyone is encouraged to play a role in improving public health. Through promoting civic engagement, fostering healthy neighborhoods, addressing climate change, leveraging new and innovative tools, prioritizing reproductive and sexual health, preparing for emergencies, and envisioning the future of public health, everyone can play a role and thrive in healthy communities.
Metro Health is also celebrating the secondyear achievements of its SA Forward Plan, the department’s community blueprint. SA Forward takes a community-informed approach by addressing pressing issues learned from the COVID-19 pandemic, including health disparities, social justice, public health capacity
and the state of its workforce. All key achievements are included in Metro Health’s latest annual report, which is now available by visiting www.sa.gov/health.
To celebrate key achievements and the role of public health, Metro Health will be hosting its annual Public Health Fest, which will take place on April 4th from 3 p.m. to 6 p.m. at Mission County Park (6030 Padre Dr). Guests can enjoy the festivities by learning about Metro Health programs, access to medical care, nocost food tastings and Fiesta medals.
Public health is more than just healthcare. It is about working together to create safe, interconnected, healthy communities for everyone. While a doctor treats individuals, public health looks at the health of a community.
We are ALL public health! For more information, visit www.sa.gov/nphw.

SAN ANTONIO MEDICINE 34 SAN ANTONIO MEDICINE • April 2024
In Memoriam
William Lloyd Henrich, MD, MACP
August 7, 1946 – March 14, 2024
William L. Henrich, MD, MACP, a specialist in kidney diseases, served as the president of The University of Texas Health Science Center at San Antonio (now called UT Health San Antonio) since 2009.
Dr. Henrich received his undergraduate degree from Columbia University and his medical degree from Baylor College of Medicine, and later completed a residency in Internal Medicine at The University of Oregon Medical School and a fellowship in Nephrology at The University of Colorado School of Medicine.
During his career, Henrich served as Professor of Medicine at The University of Texas Southwestern School of Medicine, as Professor and Chair of Medicine at the Medical College of Ohio, and as the Theodore Woodward Professor and Chairman of the Department of Medicine at The University of Maryland School of Medicine in Baltimore. He became the Dean of the School of Medicine and Vice President for Medical Affairs at UT Health San Antonio in 2006 prior to being selected as its President in 2009. He is the inaugural holder of the John P. Howe, III, MD, Distinguished Chair in Health Policy.
Dr. Henrich authored over 300 original articles and chapters, and was the founding editor of the popular dialysis textbook, “Henrich’s Principles and Practice of Dialysis.” An elected member of several prominent research societies, he also served as President of the American Society of Nephrology.
Dr. Henrich was passionate about mentoring students, residents and young physicians, and received teaching accolades in every institution in which he has served.


“Dr. Henrich was a longtime member and advocate of the Bexar County Medical Society (BCMS). Under his leadership, every UT Health San Antonio resident, medical student and physician leader became a BCMS member. His legacy is forever marked by their contributions to BCMS and subsequent achievements in their careers.”
– Zeke Silva, MD, President, Bexar County Medical Society
“Dr. Henrich was a born leader and a visionary. He had a passion for medical research and it was remarkable to see the results of his leadership in expanding access to cutting-edge medicine for the residents of San Antonio and South Texas over the past 14 years. Dr. Henrich was a strong supporter of organized medicine. He will be greatly missed.”
– Michael J. Darrouzet, Executive Vice President, CEO, Texas Medical Association
“We mourn the sudden passing of Bill Henrich, MD, our President for the last 15 years, from complications of a second stem cell transplantation. He previously had a successful stem cell transplantation 12 years ago with stem cells from his son. He was able to return to preside over the unprecedented growth of UT Health San Antonio in medical care, discovery and training of the next generation of health care providers. More than a visionary leader, he was a wonderful person, and we will carry his values and character in our hearts forever.”
– Robert Hromas, M.D., F.A.C.P., Dean, Joe R.
and Teresa Lozano Long School of Medicine,
Vice
President for Medical Affairs, UT Health San Antonio
Visit us at www.bcms.org 35 IN MEMORIAM
William L Henrich, MD, MACP, receiving the BCMS Distinguished Service Award from Sheldon Gross, MD, BCMS Past President, in 2020.

An HR Professional’s Guide to Data Privacy Compliance and Security
By John Rhoades, Managing Director, Data Privacy & Technology Compliance, Insperity
Reprinted from www.Insperity.com
As an HR professional, you work daily with sensitive, highly confidential employee and business data. But how knowledgeable are you about HR data privacy compliance and security?
Think about every data point you regularly touch regarding employees (Social Security numbers, salaries, health care and retirement plans, background checks, etc.) and proprietary business information (customer data, mergers and acquisitions, planned layoffs, etc.).
You may be familiar with high-profile, large-scale breaches and their impact. Information on more than 140 million Americans was stolen from Equifax, one of the nation’s largest credit reporting companies, in 2017. Target, one of the largest U.S. retailers, had up to 70 million customers’ data hacked in 2013. Anthem, an American health insurance company, had nearly 78 million American’s medical data stolen in 2015.
But what about the inadvertent disclosure of personally sensitive data? What about the time when a manager sent a performance evaluation to another employee? Or when a sales representative sent a different company’s information to another client? In all of these cases, if that information gets into the wrong hands, that’s bad news for everyone involved. This can lead to enormous liability — both legally and for the business’ reputation.
To mitigate the most important consequences of a sensitive data breach, you should undertake two parallel efforts: Ensure compliance with state and federal laws, and advocate for data protection best practices.
Here is what you need to know about ensuring compliance with data privacy laws and maintaining HR data protection practices.
36 SAN ANTONIO MEDICINE • April 2024 SAN ANTONIO MEDICINE
What state and federal laws govern HR data privacy compliance?
HR professionals have many responsibilities, but none as important as their duty to protect employees and the company. That means they must take on a much different role than in years past and understand what federal and state laws apply to your company when it comes to data privacy compliance.
The U.S. lacks a comprehensive federal law regulating how personal information is collected and used. Instead, it regulates how specific sectors must handle sensitive information. State laws vary in how they address data breaches, generally, and sensitive data, specifically. Look to state laws as they apply to your company. Newly added state laws may also overlap with other laws.
State laws may have additional requirements and restrictions on how employers use, store and transmit employee information. An employer’s liability for data breaches vary state by state. California and Massachusetts, for example, have been more active than other states in passing data privacy legislation so they have more compliance requirements.
How do you stay compliant with federal and state laws?
A robust HR data protection strategy starts with checking state laws to ensure that the company is in compliance with the relevant data privacy laws.
1. Understand what state, federal and international laws apply to your business. Because the U.S. “patchwork” system of federal and state laws and regulations is constantly changing, you should be aware of relevant pending bills on data privacy and security. Consider setting automated alerts to stay up to date on news of new cybersecurity and data protection laws.
2. Assess your company’s compliance requirements by industry, location, clientele and

types of data processed. Not only do the governing bodies and regulations vary by state, but it also varies by industry. For example, a financial services company licensed in New York must comply with specific state laws about cyber preparedness and protecting personal privacy data. Or, a business operating only in the U.S. will face different compliance requirements than a global consumer-facing organization with physical stores and online commerce.
3. Build and share your knowledge base. Become well versed about these matters to help inform employees and clients about their data privacy rights. The more you understand data privacy, the more effective you will be in advising leadership on how these regulations impact a company’s business.
4. Help set expectations with staff. Stress the importance of protecting sensitive information and what it means to adequately balance individual privacy concerns against the requirements of running a business. Create a culture of compliance with expected data privacy best practices.
5. Maintain transparency in the process. Work to build trust with all the constituents of a
business — employees, clients, third parties and vendors. Taking this approach requires HR professionals to go beyond knowing employment laws or understanding the cybersecurity focus of most IT professionals. Viewing data privacy and compliance through the lens of relevant laws and regulations will help inform HR professionals on where HR data should be kept and how best to store and protect it.
Data protection is essential for all HR professionals. Data protection goes beyond a corporation’s social responsibility in a digital age. It has become an essential compliance function for any organization that collects, uses or shares personal information or other potentially sensitive data.
Clients and employees alike place their trust in us to be good stewards of their data and how we handle its confidentiality. Managing this responsibility well is a fundamental piece of best business practices.
If you’re looking to modernize your HR department, download and read our complimentary e-magazine at www.insperity.com/ resources/magazine/derailed-by-data-the-insperity-guide-to-hr-technology-issue-6. www.insperity.com
Visit us at www.bcms.org 37 SAN ANTONIO MEDICINE
Securing Mobile Devices in Healthcare
Courtesy of MedPro Group
Mobile devices are convenient, but using them also carries risks. Mobile data security and HIPAA compliance are ongoing concerns that healthcare organizations must address. To address these issues, healthcare leaders should establish mobile device policies and procedures to safeguard protected health information (PHI). Additionally, they should ensure that all mobile device users are educated about these protocols and aware of ongoing privacy and security concerns. Healthcare organizations also should implement data breach incident response protocols.
The following tips provide guidance for healthcare organizations and mobile device users on best practices for device security and ways to avoid risk.1
1. Enable password/PIN protection or biometric authentication on mobile devices to restrict access to authorized users and safeguard PHI.
2. Require appropriate levels of password complexity and periodic password changes as well as multifactor authentication. Ensure passwords are masked when users enter them.
3. Install and enable encryption, firewall protection and security software (including applications that help identify and prevent viruses, malware, spyware, phishing, etc.).
4. Install and activate remote wiping and/or remote disabling. Require users to immediately report lost/stolen mobile devices so data wiping can occur before exposure.
5. Research mobile applications before downloading. Download only HIPAAcompliant applications, and use secure messaging applications.
6. Ensure that operating systems, applications and security software are configured for full functionality and maximum security.
7. Use a secure virtual private network when connecting mobile devices to residential wireless networks, and ensure that security features are properly configured and have
up-to-date firmware/operating system software.
8. Update mobile devices and applications as soon as updates are available. Automatic update deployment and installation should be used when it does not interfere with device operations.
9. Establish mobile device policies and procedures, and train staff members on them as well as on HIPAA privacy and security awareness.
10. Reinforce that staff members should maintain physical control of their mobile devices at the healthcare organization, at their residences and in transit. Establish requirements to secure passwords, health information and other sensitive data.
11. Implement a policy that all mobile devices used to access PHI must be registered with the healthcare organization and authorized to add, modify, remove and access PHI.
12. Strongly encourage staff members to report any security incidents resulting from using their mobile device.
13. Do not a) install or use file-sharing applications, b) share passwords or user authentication, c) knowingly allow unauthorized access to mobile devices, d) store or send unencrypted PHI, e) download applications without verifying that they are from a trusted source, f) leave mobile devices unattended, or g) use unsecured Wi-Fi networks.
14. Delete all stored PHI and other proprietary information before discarding or reusing mobile devices. Be sure to use proper disposal techniques as delineated in organizational policy.
Reference:
1. The tips in this publication are based on information from the following sources: U.S. Department of Health and Human Services Office of the National Coordinator for Health Information Technology. (n.d.).
Your mobile device and health information privacy and security. HealthIT.gov. Retrieved from www.healthit.gov/topic/privacy-security-and-hipaa/your-mobile-devic e-and-health-information-privacy-and-security; U.S. Department of Health and Human Services Health Sector Cybersecurity Coordination Center (HC3). (2023, March 23). HC3: HPH mobile device security checklist (Report: 202303231700). Retrieved from www.hhs.gov/sites/default/ files/hph-mobile-device-securitychecklist-tlpclear.pdf; U.S. Department of Health and Human Services. (n.d.). Mobile devices: Know the risks. Take the steps. Protect and secure health information. Retrieved from www.healthit.gov/ sites/default/files/mobile_devices_and_health_inf ormation_privacy _and_security.pdf; Clements, J. (2023, April 10). 10 tips for HIPAA compliance when using mobile devices. MOS Medical Transcription Services. Retrieved from www.medicaltranscrip tionservicecompany.com/blog/10-tips-forhipaa-compliance-when-using-mobile-devices/
This document does not constitute legal or medical advice and should not be construed as rules or establishing a standard of care. Because the facts applicable to your situation may vary, or the laws applicable in your jurisdiction may differ, please contact your attorney or other professional advisors if you have any questions related to your legal or medical obligations or rights, state or federal laws, contract interpretation, or other legal questions.
MedPro Group is the marketing name used to refer to the insurance operations of The Medical Protective Company, Princeton Insurance Company, PLICO, Inc. and MedPro RRG Risk Retention Group. All insurance products are underwritten and administered by these and other Berkshire Hathaway affiliates, including National Fire & Marine Insurance Company. Product availability is based upon business and/or regulatory approval and may differ among companies. © 2024 MedPro Group Inc. All rights reserved.
38 SAN ANTONIO MEDICINE • April 2024 SAN ANTONIO MEDICINE


Dear BCMS Members,
I hope this letter finds you well. I wanted to take a moment to introduce a new initiative from my San Antonio-based startup LASO Health, aimed at supporting individuals in our community — and across the country — with affordable access to prescription medications. We appreciate your support in sharing our new program with your business partners and those who might benefit from it.
We're thrilled to announce the launch of LASO Rx Zero, our new, low-cost monthly prescription medication membership program. We have meticulously designed this program to ease the financial burden associated with prescriptions, and to provide our members with unlimited access to our formulary of more than 600 generic medications for only $24.99 per month. Through strategic partnerships and a commitment to accessibility, LASO Rx Zero aims to ensure that individuals in Bexar County and beyond have affordable access to prescription medications and the important refills they need for their well-being and peace of mind.
Our LASO Rx Zero program offers a range of benefits including:
• Substantial discounts on a wide variety of more than 600 generic medications
• Free shipping and delivery direct to our Rx Zero members’ doorsteps
• A low-monthly fee of $24.99 for individual members
It’s our goal to ensure that quality healthcare remains within reach for everyone. And we believe that our LASO Rx Zero initiative aligns perfectly with the mission and values of the Bexar County Medical Society in promoting accessible healthcare for all.
Beyond LASO Rx Zero, the LASO Health platform offers members low-cost access to quality telemedicine for primary, urgent and behavioral health needs as well. If you’re unfamiliar, I encourage you to take a look at our new site at LasoHealth.com or LASO Health mobile app available for Apple and Google devices in the app stores. Our team would love the opportunity to discuss our LASO Rx Zero program further and explore potential collaboration avenues to extend its benefits to those in need within your practices and our community. Please feel free to contact me and the LASO Health team for a meeting or call us at 866-527-675.
Thank you for your time and consideration. We look forward to potentially partnering with fellow members of the Bexar County Medical Society to make a meaningful difference in the lives of our friends and neighbors.
 M. “Hamed” Reza Mizani, MD
M. “Hamed” Reza Mizani, MD
Visit us at www.bcms.org 39
Shop Businesses Who Support BCMS
BCMS Business Directory
We encourage you to use our friends of medicine businesses whenever you or your practice need supplies or services.
ACCOUNTING FIRMS

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 jprice@ssacpa.com
www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
ASSET WEALTH MANAGEMENT

Aspect Wealth Management (★★★ Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”
BANKING

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com
“We’re here for good.”

The Bank of San Antonio (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the
state who specialize in medical malpractice and all lines of insurance for the medical community. Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com
www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking
210-343-4494
Scott.Gonzales@amegybank.com
www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333
info@synergyfcu.org
www.synergyfcu.org
“Once a member, always a member. Join today!”
CLINICAL DIAGNOSTICS

Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison
210-503-0003
yulia@genicslabs.com
Kevin Setanyan
Managing Partner
210-503-0003
kevin@genicslabs.com
Artyom Vardapetyan
Managing Partner
210-503-0003
www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease, & Genetics. Robert Castaneda, CEO
210-316-1792
Robert@livingstonmedlab.com
www.livingstonmedlab.com/home
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
CREDENTIALS VERIFICATION ORGANIZATION

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor) Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com
www.BexarCV.com
“Proudly serving the medical community since 1998”
FINANCIAL ADVISORS

Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM

www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com
www.edwardjones.com/elizabeth-olney "Making Sense of Investing"
FINANCIAL SERVICES

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Your wealth. . .All aspects”

Hancock Whitney (HHH Gold Sponsor)
www.hancockwhitney.com
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork, and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana, and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
40 SAN ANTONIO MEDICINE • April 2024
Larry Anthis
Corporate Banking, Relationship Manager
210-507-9646
Larry.Anthis@hancockwhitney.com
Serina Perez
San Antonio Business Banking
210-507-9636
Serina.Perez@hancockwhitney.com
Erik Carrington
Texas Regional Wealth Management Manager 713-543-4517
Erik.Carrington@hancockwhitney.com
GERIATRICS/PRIMARY CARE

Conviva Care Center (HHH Gold Sponsor)
Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter 812-272-9838
KGary4@humana.com
www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
HOSPITALS/ HEALTHCARE FACILITIES

UT Health San Antonio MD
Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager
210-450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD
Anderson Mays Cancer Center
Laura Kouba
Business Development Manager
210-265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio
7979 Wurzbach Road
San Antonio, TX 78229
HOSPITALS/ HEALTHCARE
SERVICES

Equality Health (HHH Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager
210-608-4205
cleos@equalityhealth.com
www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
HR HUMAN RESOURCES
INSURANCE/MEDICAL MALPRACTICE

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting, and defending physicians.
Patty Spann
Director of Sales and Business Development
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, one-stop-shop, comprehensive health solution.
Ruby Garza, MBA
210-212-2622
rgarza@texaskidneycare.com
www.lasohealth.com
MEDICAL SUPPLIES AND EQUIPMENT

Henry Schein Medical (HH Silver Sponsor)
Insperity (
★★Silver Sponsor)
Insperity’s HR solutions offer premium service and technology to facilitate growth by streamlining processes related to payroll, benefits, talent management and HR compliance. We provide the tools to help you lighten your administrative load, maximize productivity and manage risks – so you can focus on growth.
Cynthia Marshall
Business Performance Advisor 210-558-2520
cynthia.marshall@insperity.com
Dayton Parker Business Performance Advisor
210-558-2517
dayton.parker@insperity.com
www.insperity.com
“Insperity’s mission is to help businesses succeed so communities prosper”
INSURANCE

TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England
Director of Member Benefits
512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”
The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group
(HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com
www.medpro.com
IT – TELEMEDICINE SERVICES
LASO Health Telemedicine and Rx App (★★★ Silver Sponsor)
LASO Health is the industry’s only solution that makes health care services accessible, cost-transparent and convenient. Its mission is to reinvent “health care” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care. LASO combines an intuitive,
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”

PHYSICIAL SUPPORT SERVICES
Provider's Choice Scribe Services (★★★ Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar
COO
915-691-9178
yaguilar@pcscribes.com
Luis Chapa
MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
continued on page 42
Visit us at www.bcms.org 41
BCMS Business Directory
PRACTICE MANAGEMENT
Equality Health (★★★ Gold Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination, and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
cleos@equalityhealth.com
www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care.”
PROFESSIONAL ORGANIZATIONS
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President
210-797-8412
healthcareleaderssa@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
gmeyn@vestedbb.com
https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber
President
210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler Program Coordinator
210-904-5404
Valerie@thehealthcell.org
www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org
www.samgma.org
RETIREMENT PLANNING

Oakwell Private Wealth Management (★★★ Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
STAFFING SERVICES

Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Mike DeQuattro
Director of Operations - Texas & New Mexico
210-918-8737
Mike.DeQuattro@ favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing
continued from page 41
your wellbeing and patient care. Pedro Caretto, VP of Business Development
786-437-4009
pcaretto@eleosvhs.com www.eleosvhs.com
TRANSCRIPTION SERVICES

Provider's Choice Scribe Services (★★★ Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
yaguilar@pcscribes.com
915-691-9178
Luis Chapa MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
42 SAN ANTONIO MEDICINE • April 2024



Visit us at www.bcms.org 43

2024 Volkswagen Tiguan
By Stephen Schutz, MD




AUTO REVIEW 44 SAN ANTONIO MEDICINE • April 2024
In 2006, the late great Volkswagen CEO and Board Chair Ferdinand Piech, unhappy with the company’s fortunes in the U.S., famously criticized management with the words, “Some understand this business better than others.”
He may have been referring to the Gen 1 Tiguan, a vehicle that 15 years ago didn’t hit the U.S. market the way it was meant to. Aimed at compact crossover SUV segment leaders Honda CRV, Toyota RAV4 and Ford Escape, the Tiguan cost almost as much as mid-size SUVs like the Honda Pilot, Toyota Highlander and Ford Explorer. Not a good situation, and Tiguan sales disappointed.
In 2016, Volkswagen debuted a second-generation Tiguan, which was significantly larger than its predecessor and better styled. It’s now priced competitively, thanks mostly to it being imported from Mexico rather than Germany, as well as currency fluctuations, which always play a role.
The 2024 model has been updated but keeps Gen 2’s angular lines, which look good. A short but wide grille and thin headlights give the Tiguan a pensive look, but from the rear it looks very “generic midsize SUV.” The sides of the Tiguan tie the ends together with two character lines that run from just behind the front fenders to the rear end and just above the rear fenders, respectively.
The larger Atlas SUV and smaller Golf hatchback echo the Tiguan’s exterior design, which is what you’d expect with different vehicles from the same manufacturer. I don’t think any reader would be surprised by that, but I’ll bet very few of you know that all three of those aforementioned vehicles are built from the same flexible platform, known internally at Volkswagen as MQB. That’s where we are in 2024 — modular platforms and powertrains underpin many quite different vehicles with a myriad of brand names.
So, it’s logical to conclude that the Tiguan would drive like either a stretched Golf or a shrunken Atlas, and it does. The same 2.0L TSI in-line four-cylinder engine is there, as is the familiar 8-speed automatic transmission. And the Germanic engine sounds and quick shifts tell you this is a Volkswagen. Still, everything’s slower than the last GTI you drove, like the friend you haven’t seen in five years who now weighs 50lbs. more and, seriously dude, needs to go to the gym.
Fuel economy is 24 MPG City and 31 MPG Highway for front wheel drive models, and slightly less for Tiguans with AWD.
The Tiguan’s interior is also bigger Golf/smaller Atlas. Volkswagen’s obsession with eliminating buttons and knobs thankfully hasn’t had too much effect in the current model, but of course there’s a central touchscreen and lots of tech. Interior space is about what you’ll get in a RAV4, which is to say good but not great (if you need more, your salesperson will happily walk you over to an Atlas, I’m sure).
One nice thing unavailable in competing crossovers is a 40-20-40 rear seat, which enables you to keep the outward rear seatbacks up so they can be occupied while folding the center seatback down to ac-

commodate longer cargo like skis.
OK, major switch now. While the Tiguan I tested was brand new, I would be remiss if I didn’t point out that Volkswagen Tiguan Mk3 is about to be launched, and it is all new. Like “don’t buy the current Tiguan unless you get a big discount” new.
The 2025 Tiguan will be significantly larger than the current model, with most of the extra size focused on the passenger compartment. While the current generation Tiguan has decent interior space with an optional third row of seats available, you don’t want to put average size or larger adults in the third row. And the second row isn’t all that great either. That promises to be different with the next Tiguan.
Note to skiers: according to Car and Driver, the 2025 Tiguan will switch to the more popular 60-40 second row seatback. Sigh.
While the same 2.0L engine and 8 speed transmission described above carry over, a plug-in hybrid that VW hints will be able to go 62 miles on all-electric power will be an available option.
The 2024 Volkswagen Tiguan is a sportier alternative to the more popular Toyota RAV4 and Honda CRV, and it’s worth a look if you’re in the market for a compact crossover SUV. Just remember that it’s due to be replaced soon, so insist on a discount if you choose the 2024 model (BCMS’ Phil Hornbeak will help you get the best deal on a Tiguan or any other new car or truck you want).
As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367) for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.

Stephen Schutz, MD, is Board-Certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.
AUTO REVIEW Visit us at www.bcms.org 45

Kahlig Auto Group

11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
As of November 1, 2023, our loan rate will be 5.5% for 60 months with approved credit.
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Call Phil Hornbeak 210-301-4367 or email phil@bcms.org








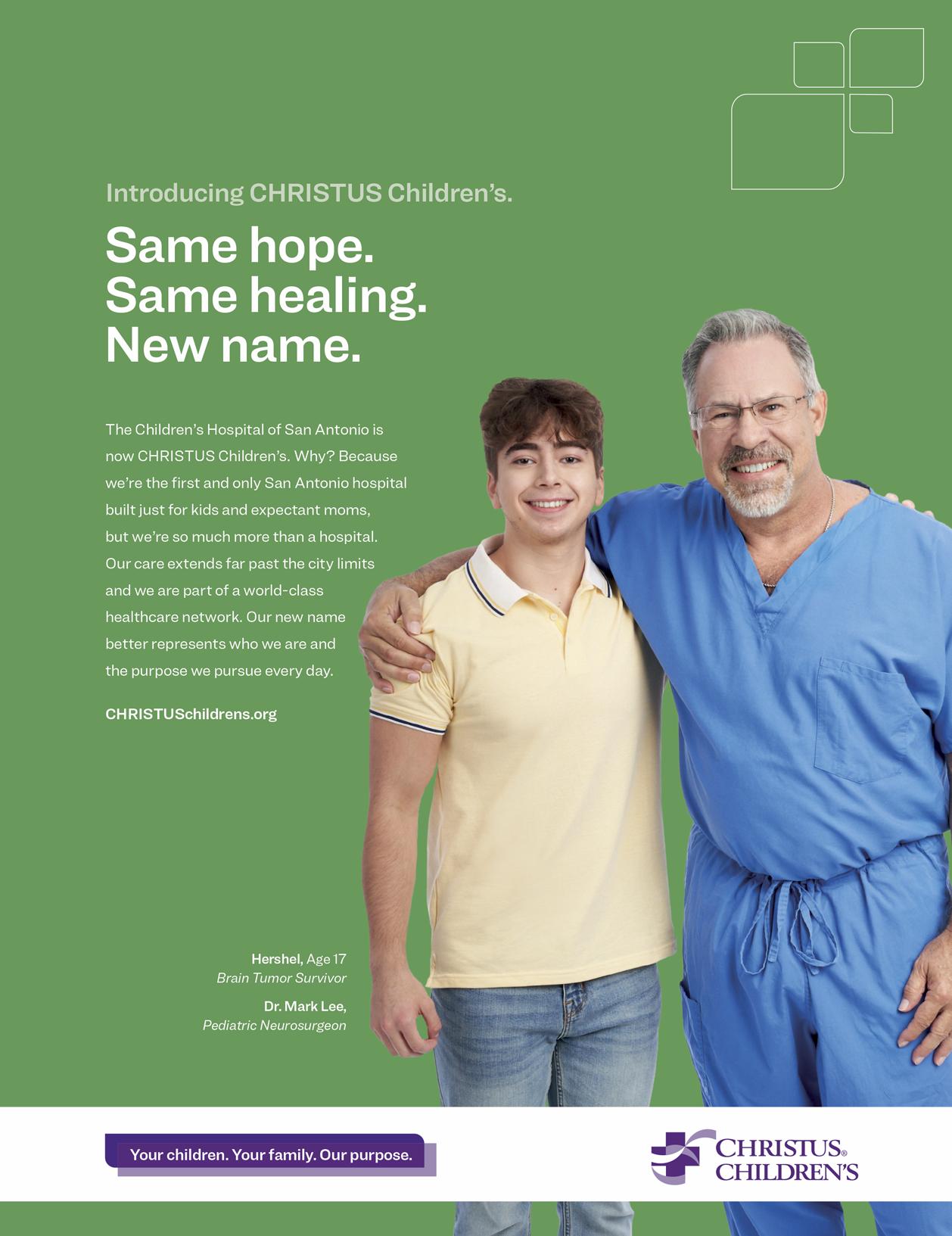




















































 M. “Hamed” Reza Mizani, MD
M. “Hamed” Reza Mizani, MD




























