Biophillia in the Workplace











With long-term sickness at a record high, the Department of Work and Pensions (DWP) has pledged to tackle economic inactivity as a priority. As OH professionals you can help shape the UK government's consultation
“Occupational Health: Working Better” a proposal aimed at increasing employer use of Occupational Health (OH) Services. In addition “Tax Incentives for Occupational Health”, a joint HMTHMRC consultation on the role of tax incentives in boosting occupational health provision by employers is under consultation. Watch out on the iOH Facebook and iOH Blog area for details of iOH sessions to gather your views for submission, led by Libby Morley. Alternatively, you can provide your input directly by completing the response form by 12 Oct 2023.
The last few months have continued to be busy for the iOH Board. We are delighted to welcome our 1000th member last month. A huge thank you to all our members who completed the iOH Feedback Survey. It was interesting to see the breadth of organisations where our members work. 10% work for the NHS, 24% work for OH providers, 30% in-house, 18% are contracting or self-employed and 6% are business owners. A hefty 70% have been working in OH for over 10 years which could demonstrate how much we love OH, but also the necessity to encourage new blood to keep the pipeline of OH
professionals coming into our professions. The value of our membership was rated 4.5/5 which is very pleasing. Your Board will be meeting shortly to discuss our longerterm strategy and consider the survey results which will help to shape our future.
Once again, iOH are proud to partner with Health and Wellbeing at Work for the annual conference on 12th & 13th March 2024 at the NEC, Birmingham. An iOH discount code is coming soon. Meanwhile you can register interest. We are also planning the annual iOH Ruth Alston Memorial Lecture and Dinner on the evening of 12th March at the Hilton Metropole which will be open to all iOH members as a priority.
iOH grants designed to support iOH members, including trainees, with CPD and career progression have been relaunched. To find out more and apply view the link in the members area of the website. The closing date is 31 Oct 2023.
Finally, a warm welcome to Mandy Kelly, who has joined the iOH Board as Director of Occupational Therapy (OT). Mandy comes with a wealth of experience having worked as an OT in OH for over 25 years. Mandy’s role will bring additional diversity to our multidisciplinary team.
 Lynn Pratt President iOH
Lynn Pratt President iOH

 By Tracie McKelvie, TJM Occupational Health and Wellbeing
By Tracie McKelvie, TJM Occupational Health and Wellbeing
AMental Health Foundation report highlighted our relationship with nature, and noticing, thinking about, and appreciating our natural surroundings is critical in supporting good mental health, and preventing distress. If allowed, nature permits us to momentarily lose ourselves in an innocent but reflective “fantasy” of speculative fiction involving magical elements that occasionally interrupts our thoughts.
Nature (or elements thereof) is an appealing environment to enhance and improve our mental wellbeing. When we are exposed to, or when we think about nature, our five senses are stimulated and tentatively teased in such a way that when “activated”, helps us to perceive and interact with our environment. This encourages creative thinking and allows us an objective perception of reality. –which in turn allows us to absorb, understand, and process information from our surroundings.
In the right surroundings, this can exude positive reactions and emotions that are difficult to ignore - regardless of how we are feeling at that moment in time. Our five senses are intricately connected to our emotions and memories 4. They can considerably influence how we feel and respond to certain situations.
The process of converting stimuli can be experienced from the body’s senses, such as touch, sight, sound, and/or from chemical senses, such as taste and smell. Beyond the five senses, we can also sense a lot more within our environments. For example, we can (intuitively) tell how hot or cold it is, we can feel pain, and we can sense how our
body is positioned. Even though we may not always be as aware of these other senses as we are of the five main senses, they can still have a significant impact on us 4 .

Our “ sense” reactions can be from the anticipation of what we may expect, as well as from our reactive responses to the natural elements that are around us. Our senses can influence our health and wellbeing and can have a positive knock effect on how we function and respond. In today’s fast-paced climate, when it comes to our work this can be crucial especially if others are reliant upon us for our expert input, or if we need to make important business decisions.
The Mental Health Foundation share a consensus view that nature can generate positive emotions, such as calmness, joy, and creativity. Exposure to calming and natural environments can help to facilitate concentration and nature connectedness and is also associated with lower levels of poor mental health, particularly lower depression and anxiety 1 .

This became more apparent in very recent years when accessibility, and the ability to freely engage with nature was interrupted during the COVID-19 pandemic. This lack of exposure to nature and the outdoors led to increased stress levels amongst those who were forced to stay indoors during several lockdowns. For some, the lockdowns meant that they had little, or no access to environmental greenery, water, and open spaces.
Despite moving on, today’s reality in achieving a positive and balanced exposure to the natural elements during our typical working day/s, or nights can be difficult. Our relationship with other
The Mental Health Foundation share a consensus view that nature can generate positive emotions, such as calmness, joy, and creativity.
less appealing and less natural surroundings such as a windowless office, darkened/small/noisy/enclosed working spaces, or shift work can have the opposite effect when it comes to supporting good mental health. Whilst nature can mostly be found anywhere, accessibility to high-quality nature spaces are not equally available to everyone in the UK.


While the Oxford Languages Dictionary defines biophilia as “an innate and genetically determined affinity of human beings with the natural world” the word biophilia originates from the Greek with “philia” meaning “love of.” As humans, we have a deeply ingrained and inherent love of nature which is an intuitive and natural drive imprinted into our DNA.
Biophilic design is a concept used within the building industry to increase occupant connectivity to the natural environment using direct nature, indirect nature, and space and place conditions. Used at both the building and city scale, it is argued that in addition to health benefits, there are also environmental, and economic benefits. Although its name was coined in recent history, indicators of biophilic design have been seen in architecture from as far back as the Hanging Gardens of Babylon 2 .
In terms of health and wellbeing, biophilic design has been found to support cognitive function, physical health, and psychological well-being 3 , and the idea of incorporating “biophilic design” into indoor workspace is hoped to encourage the connection between humans and nature, as well as promote staff wellness and productivity.
Common biophilic design elements include skylights, green walls, or living walls covered with living greenery; and the presence and sound of water, such as fountains or ponds.
This is especially important since the increase in home or hybrid working has rocketed over the past few years. But whether we are working from home, from the office, or hot-desking, making small changes to enhance our surroundings can have a significantly positive impact on our mood, and on our general health and wellbeing.
Simply opening blinds or curtains and having access to an open window will complement our “downtime” by allowing us to immerse ourselves in natural light, and the gentle fresh breeze that circulates around us. This open access will also allow us to absorb the natural aromas and sounds of birds chirping, or agricultural processing (such as bailing and ploughing), or even the sound and smell of falling rainwater – although for some, feeling able to take some time out may be more of a challenge.
Other ideas to promote biophilia into our home and/or office working environments could include:
✓ Mimicking, and bringing indoors some of the visuals and aromas that natural elements from the outdoors offer - such as plants, plant and wood smells, earth smells, the smell of freshly cut grass, wild garlic, and freshly growing herbs. It may be that a balcony or deck area could be transformed into a mini “indoor garden.” Or a simpler
it is argued that in addition to health benefits, there are also environmental, and economic benefits
transformation could involve growing herbs on your kitchen windowsill. Along with the vision of, and smell of freshly growing indoor herbs, there is nothing as lovely as cooking with fresh, fragrant herbs right from your very own indoor “garden patch.” Herbs such as mint, coriander, thyme, basil, and oregano are very easy to grow in little pots on your kitchen windowsill. All you need is a little fresh air, a bit of sunlight, and some water. Oh, and if you are anything like me, put a label on each to remind you which is which!
✓ Creating a green wall – by simply entwining greenery of choice through a trellis on one wall, or even on a wooden static structure near your workspace, this can create a tranquil and mesmerising statement.
✓ Creating a living wall – with similar effects, this will require a little more planning, and some great tips can be found at Gardeners World or Age UK
✓ You can incorporate botanical prints – regardless of whether your space is big or small, a statement wall with leafy prints or wallpaper with delicate floral prints can help mimic nature within your indoor environment. Wallcoverings that have textures and colours from outdoors go a long way towards lightening and refreshing a room, but if you are unable to, or you don’t want to go bold with an entire “botanical wall”, photographs or posters will also do the trick!

✓ You can also fill your home, (or where appropriate, your office space) with potted plants know that besides adding much needed oxygen, many plants are also
known to regulate temperatures and remove pollutants from indoor air. So why not see whether you can slot one or two into a sneaky nook or cranny? Alongside smaller potted plants, leafy tropical palms in large pots are also statement pieces that will invigorate and add movement to tired indoor spaces. You could even add in a lovely fragrant Jasmine hanging plant!
For ideas on suitable indoor plants, you can visit:
12 DIY Indoor Plant Pot Ideas
The Best Indoor Plants For Every Home And Skill Level
Gardeners World Best House Plants
✓ Decorating or adding to your home/office environment with sustainable, organic materials. Some examples could include items like jute rugs (made with a soft natural fibre derived from tropical plants), rubberwood furniture, bamboo blinds, driftwood artifacts, natural material throws, wickerwork lamps, a decorative bowl of organic dried locus pods, or a display of seashell beach décor.
✓ The sound of water. Welcoming the water element into our space and listening to the sound of gently flowing water soothes and refreshes the senses, reduces stress levels, and infuses space with positivity. Just by adding a small tabletop water feature closer to where your working space is
can make a world of difference to the energy around you, and it can act as a great enchanting visual too.
✓ Lighting is also an important factor - in addition to promoting well -being, biophilic lighting has been shown to have positive impacts on mood, productivity, and cognitive function 5, 6. As such, the aim would be to achieve varying intensities of light and shadow that change over time in order to mimic the lighting conditions and imagery that we might experience out in nature i.e., following the circadian lighting cycle (the natural sleep/wake cycles of the human body). This is referred to as “dynamic” and “diffuse” lighting.
Sunlight that filters through clouds or trees
Skylights that allow for natural light Lamps that adjust their brightness and colour temperature throughout the day Light fixtures that create patterns or shadows on the walls or ceiling
Ways in which to achieve biophilic lighting in line with the circadian lighting cycle include:

Dynamic control of light intensity, colour temperature, and distribution to imitate natural daylight
White LED lights can adjust colour temperature throughout the day
Designing lighting schemes that highlight patterns, textures, and shapes found in nature
In summary, creating a workplace that facilitates optimal performance and better productivity makes good business sense. This notion is a heavily researched, and talked about topic, and as an employer, getting the best out of people is key for performance and productivity; as an employee, feeling good when at work is also key for health and wellbeing, job satisfaction, and personal performance and productivity.
While the notion of biophilia and how this may be introduced may vary from individual to individual, (depending on personal choice and preferences), the advantages that biophilia can bring to an indoor space appear to be very beneficial in promoting positivity, and in enhancing physical and psychological wellbeing. This in turn impacts favourably on our cognitive functioning.
As individuals, we do have an element of control in terms of considering our working environments, and in making changes – i.e., bringing a little bit of nature indoors. Remember, the smallest of changes can make a significant difference.
1.Ref: Mental Health Foundation (MHF) 2021, Nature; how connecting with nature benefits our mental health, https://www.mentalhealth.org.uk/our-work/research/nature-how-connecting-nature-benefits-our-mental-health
2.https://en.wikipedia.org/wiki/Biophilic_design
3.https://www.nrdc.org/bio/maria-mccain/bringing-outdoors-benefits-biophilia
4.https://www.harleystreetent.com/blog/the-five-senses-and-why-they-are-important/
5.https://workinmind.org/2020/02/17/the-benefits-of-biophilia
6.https://www.ies.org/research/fires/double-dynamic-lighting-bringing-qualities-of-natural-light-into-the-office/
Tracie McKelvie is an Independent Specialist Nurse Practitioner in Occupational Health, Queens Nurse and Founder of TJM Occupational Health and Wellbeing.

Follow on Linkedin.
Contact Tracie - tracie@tjm-ohw.co.uk


Working is important for an individual’s health and well-being, as well as providing the employee with income, social interaction, purpose, and identity. Workplaces are required to be safe and free from risks to health and there is a legal duty for employers to maintain this. However, there are some instances where workers may develop a
disease called occupational asthma (OA) in the workplace where they may become allergic to certain substances and chemicals which cause airflow obstruction, i.e. some healthcare workers may develop a latex allergy by breathing in the powder from the inner lining of the gloves or some workers may be exposed to substances like ammonia and develop asthma as the result of an irritant effect, not an allergic reaction.
Before delving deeper into occupational asthma (OA) it is important to discuss what is asthma, according to GINA (2022), “Asthma is characterized by chronic airway inflammation, there are two key defining features of asthma, which include variable respiratory symptoms such as wheezing, shortness of breath, chest tightness, and cough. Also, variable expiratory flow and airflow limitation”. Approximately 360 million people have asthma around the world, for those workers with asthma, their asthma control may be affected by factors in
the workplace, especially if the asthma is related to the workplace. This leads to the development of the term ‘work-related asthma’ (WRA). It is suggested that 25% of adult-onset asthma is WRA. WRA can be subdivided into phenotypes which include work-aggravated asthma (WAA), which affects people with pre-existing asthma or report symptoms worsened by non-specific factors in the workplace. Causes include workplace temperature
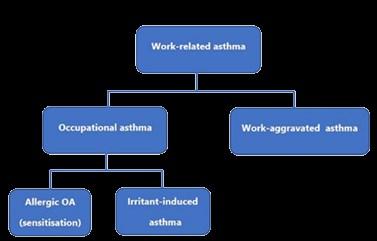
or humidity extremes, exertion from manual work tasks, workplace stress, or anxiety. In contrast, occupational asthma (OA) is caused by airborne exposures in the working environment and accounts for 1 in 6 cases of adult asthma. OA can be subdivided into two categories Allergic OA due to sensitization and Irritant induced asthma as shown in Figure 1.
There are over 400 known causes of OA, and most cases in the UK are mainly related to exposure to a small number of allergens, commonly flour dust, and isocyanates. Allergic OA sensitization requires a period of repeated allergen exposure and the duration of time between first exposure and symptom onset is referred to as the ‘latent period’. The asthmagens that cause Allergic OA can be divided into two categories: high molecular weight (HMW) agents, and low molecular weight (LMW) asthmagens.
HMW includes animal proteins, cereal grains, and natural rubber latex. Some examples of workers at risk of this are bakers, laboratory workers, and
detergent manufacturers, to name a few.
LMW includes di-isocyanates, metals, and acrylic monomers. Workers who may be at risk of this are adhesive workers, welders, spray painters, and many others.
OA caused by exposure to HMW asthmagens is an IgE-associated response involving T-helper cells and this is a common allergic response to asthma. The immune response is also relevant to a small number of LMW, such as anhydrides and platinum salts. It is suggested the highest risk of OA is within the first year of exposure, and reported latency is variable ranging from a week to many years.
A main risk factor for the development of OA is the level of exposure to the cause. Individual susceptibility is also important, as only a proportion of similarly exposed workers become sensitized, and only some of these will ever develop OA.
The diagnosis of OA involves first confirming the presence of asthma and evidence that asthma is caused by workplace conditions with various investigations involved. The best diagnostic approach for OA is having a good combination of clinical history and objective diagnostic tests. The diagnostic process aims to confirm or exclude OA; no single diagnostic test exists for OA, and the exact approach used will vary based on the individual patient's circumstances, the level of practice and expertise of healthcare professionals, and the testing facilities available. Clinical and occupational history plays a key role in making diagnosis in OA, this includes an overview of full occupational history, a fully detailed discussion of respiratory symptoms and their relationship to work. NICE recommends checking for possible OA by asking organisations to regularly monitor their employees with new adult-onset symptoms. It is important to note a diagnosis of OA cannot be made based on history alone, as some of the symptoms may improve away from work. Sensitized workers are also at risk of other related forms of occupational allergies such as rhinitis. Therefore, cautious precautions should be taken in the investigation.
A UK study has shown the duration of symptoms prior to diagnosis is 4 years,
and reasons for a late diagnosis varied. These include lack of awareness or patient engagement and in some cases, diagnostic delays resulting from missed opportunities to ask simple screening questions during health surveillance.
Investigations into OA should be carried out as early as possible, prior to the commencement of any medical interventions and while patients are still working in the job considered to be the cause of their OA. Health surveillance programs are a way of preventing occupational health diseases and can help to identify those with OA early on, reducing the severity and impact of the disease. However, few workers are identified via health surveillance programs as only 30% of workers have access to health surveillance.
There are a variety of objective tests available for investigating OA. Serial PEF offers a cheap and simple first-line approach to assessing the physiological responses to inhaled agents in the workplace. However, it is important to note serial PEFs are only helpful if the patient is still exposed to the potential agents. Serial work-related PEF measurements do not usually confirm a specific cause for OA and may be seen in other conditions such as WAA and occupational hypersensitivity pneumonitis. Depending on the local protocol, occupational health professionals can initiate serial PEF recording or upon referral to secondary care. In serial PEF recording, this involves the patient
“According to the BTS, annual health surveillance is generally carried out by an occupational health provider and usually consists of a respiratory symptom questionnaire and spirometry. In some special circumstances, such as the detergent and precious metal refining industries, immunological surveillance is also used”
learning how to use the PEF monitor and understanding the charts outputted from the data collected. There is software available for healthcare professionals that analyzes the data such as the Oasys software, which looks for pattern recognition and produces an Oasys score to show positive or negative work effects. The serial PEF data should be collected over a long period of time, and the worker should make recordings before and during work, as well as on periods of annual leave.
A positive SPT or high level of IgE antibodies related to the workplace allergen confirm sensitization but not the presence of OA. The diagnostic usefulness of immunological testing for OA is greater for HMW allergens with a clear immunological mechanism (enzymes, laboratory animals, latex and wheat flour). Specific IgE tests are also available for a limited number of LMW agents and when present, have high specificity for diagnosis.
All workers suspected of having OA should have their PEF, FEV1 and FVC measured and interpreted according to international spirometry guidelines. Some measured values are commonly within normal limits, but in some cases, a bronchodilator responsiveness test may need to be performed to confirm reversible airflow obstruction. In addition to its diagnostic value, spirometry is important in providing a baseline measurement for monitoring throughout employment.
Monitoring FEV1 has proven beneficial in OA however, if available, the pattern of previous spirometry results (often from health surveillance) can be informative. For example, if a drop in FEV1 is followed by a marked improvement, that can clearly be linked to a reduction in exposure.


“Workers found to have new symptoms of asthma, airflow obstruction, accelerated forced expiratory volume (FEV1) decline (≥15% from baseline, in addition to expected age-related loss) or sensitization to a workplace allergen, may be referred to an occupational physician, their General Practitioner (GP) or directly to a specialist centre”.
A common way of measuring airway inflammation is by fractional exhaled nitric oxide (FeNO), or by induced sputum eosinophil counts. This has an established role in the assessment of patients with suspected asthma, but normal levels may be found in a proportion of patients with OA. Although limited data is available in their assessment of inflammatory response, these types of tests are more useful with OA due to HMW chemicals, as LMW chemicals are less likely to cause eosinophilic disease. Elevated FeNO levels were found in OA induced by HMW agents where an IgE-mediated mechanism was involved (e.g. baker’s asthma), as well as in OA induced by some LMW agents such as diisocyanates. It is suggested that FeNO levels were more consistently increased in patients with OA to HMW agents than in those with LMW agents.
An option for measuring airway reactivity is by using mannitol or histamine as a specific test, although this has low sensitivity for OA diagnosis, and in some early cases of the disease the airway reactivity resolves with a few days away from work. The test is very useful in those who are symptomatic with recent exposure, where the absence of non-specific bronchial hyper-responsiveness makes OA unlikely. Nevertheless, this type of testing is performed within a secondary care setting.

A common consensus across this article is that correct diagnosis is essential for a favorable outcome in the management of occupational asthma. NICE lists occupational exposures as a risk factor for poor asthma outcomes. The diagnostic process should involve a combination of diagnostic tests and questionnaires. Having an objective test involved in the diagnostic process increases the confidence of the healthcare professional in their diagnosis, and the confidence of the worker who may be diagnosed with OA. Management of occupational asthma involves asthma education, control of exposure to environmental triggers, and initiation of appropriate pharmacotherapy. If OA is not diagnosed correctly, and the worker is not protected or able to avoid exposure to the triggers, permanent changes can present themselves in the lung.
Barber, C.M. et al. (2022) ‘British Thoracic Society Clinical Statement on occupational asthma’, Thorax, 77(5), pp. 433–442. doi:10.1136/thoraxjnl-2021-218597.
Global strategy for asthma management and prevention (2016 update) - gina. Available at: https://ginasthma.org/wp -content/uploads/2016/04/GINA-2016-main-report_tracked.pdf
Asthma: Diagnosis, monitoring and Chronic Asthma Management. Available at: https://www.nice.org.uk/guidance/ ng80/resources/asthma-diagnosis-monitoring-and-chronic-asthma-management-pdf-1837687975621
Tiotiu, A.I. et al. (2020) ‘Progress in occupational asthma’, International Journal of Environmental Research and Public Health, 17(12), p. 4553. doi:10.3390/ijerph17124553.
Occupational asthma (2022) Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/ occupational-asthma/symptoms-causes/syc-20375772

 By Mesothelioma UK
By Mesothelioma UK
While the import, supply and use of asbestos was banned from 1999, it is still present in most buildings built before the year 2000. According to the Health and Safety Executive (HSE), asbestos is still in around 300,000 non-domestic buildings including hospitals, schools, prisons, council offices and more.
Before its ban, asbestos was used in a wide range of industries because of its resistance to chemicals, heat, water and electricity. In particular it was used as an insulator in the shipbuilding industry and as a cheap construction material for post-war buildings.
The first documented death from asbestos was as far back as 1906, however it wasn’t until the 1950s that the first report linking asbestos and lung cancer was produced.
From the 1950s onwards there was an understanding in the medical community of the link between asbestos and cancer, although the first report linking asbestos to mesothelioma specifically wasn’t until 1960.
In 1985 the first mandatory ban on asbestos was introduced, but this only covered blue and brown asbestos. White asbestos is far more common in the UK, and was not banned until 1999. Whilst there has been some debate previously about whether white asbestos was harmful, it is now widely accepted that all types of asbestos are carcinogenic.
HSE statistics on asbestosis, mesothelioma and lung cancer in Britain, show that asbestosrelated deaths have now climbed to over 5,000 each year. In 2020, there were 2,544 mesothelioma deaths in total (Health and Safety Executive ‘Mesothelioma statistics for Great Britain, 2022’), with a similar number of lung
cancer deaths linked to past exposures to asbestos.
Mesothelioma is a cancer caused by exposure to asbestos in up to 90 per cent of all cases. It affects the mesothelium which is a thin membrane that lines the inner surface of:
• The chest wall, where it is known as the pleura
• The abdomen where it is known as the peritoneum
• The heart where it is known as the pericardium
• The testes
Mesothelioma is more common in men than in women and nearly half of the people diagnosed with the disease are over 75 years old (Royal College of Physicians 2020 ‘National Mesothelioma Audit report 2020’) and there is usually a long delay (between 15 and 45 years) from exposure to the onset of the disease.
Mesothelioma used to be thought of as ‘an old man’s disease’ but there is increasing evidence demonstrating how the demographic and occupation of those dying is changing. Teachers, healthcare workers, and younger people who have never worked with asbestos are all at risk of contracting an asbestos-related disease. This is something that has also been identified by Mesothelioma UK nurses, who are seeing patients from occupational backgrounds previously not considered at high risk of exposure to asbestos.
Research by Howie concluded that teachers and nurses experienced about four and two times higher mesothelioma deaths. (Howie R. 2017 ‘Mesothelioma Deaths in Teachers and Nurses in Great Britain’ . Environmental Health Scotland 2017;29(4):35-37)

Mesothelioma can sometimes be treated with immunotherapy, chemotherapy or, less commonly, surgery. However, whilst some progress is being made to find new treatments there is no cure and sadly, it can progress quite quickly after diagnosis with only 10 per cent of people living three years beyond diagnosis (Royal College of Physicians 2020 ‘National Mesothelioma Audit report 2020’). Mesothelioma has a high burden of symptoms
Asbestos was commonly used in building materials that were used in workplace and industrial buildings in the 1950s – 1990s. Therefore, it is possible that asbestos containing materials may be found in any workplace premises built or refurbished before the year 2000, including many schools and hospitals. It is thought that up to 81 per cent



which includes breathlessness, pain, weight loss and fatigue. It is a devastating diagnosis for patients and families and the fact that this disease is preventable can make it even harder to come to terms with.
of schools (Department of Education 2019
‘Asbestos Management Assurance Process report’) and 94 per cent of hospitals in London contain asbestos (BBC News, London 2017).
A detailed list of typical locations where asbestos materials can be found in industrial and workplace properties can be found on the HSE website
It can be difficult to identify asbestos, as it is
often mixed with other materials. The HSE asbestos image gallery shows a number of common materials that contain asbestos. These include ceiling tiles, floor tiles, roof panelling, pipe lagging and many more.

Mesothelioma UK is dedicated to providing specialist mesothelioma information, support and education, and to improving care and treatment for all UK mesothelioma patients and their carers. It aims to prevent mesothelioma happening to future generations.
In addition to supporting patients and families through a network of clinical nurse specialists, Mesothelioma UK funds research, produces a National Mesothelioma Audit, promotes clinical trials and collaborates with organisations and campaigns seeking to promote better management or removal of asbestos.
In July 2023, the Sunday Times launched a campaign, Act Now on Asbestos, highlighting the dangers of asbestos in public buildings and calling for a national plan for the removal of all asbestos over the next four decades.
“Former pupils and teachers are dying after exposure to asbestos in classrooms, decades ago, while children continue to be taught in schools full of the material The Sunday Times believes there should be a national register of buildings with asbestos.” Sunday Times front page, 2 July 2023.
Mesothelioma UK fully supports the Sunday Times’ efforts to raise awareness of the dangers of asbestos and as part of it’s Don’t Let The Dust Settle campaign, encourages people to sign a parliamentary petition calling for a register and a phased removal plan. https://petition.parliament.uk/ petitions/635817
In 2021, Mesothelioma UK Chief Executive, Liz Darlison, gave evidence at a Work & Pensions Select Committee inquiry into the Health and Safety Executive’s asbestos policy. The resulting report referred to asbestos-related illness as ‘one of the great workplace tragedies of modern times’, with the HSE estimating that the total annual cost of death from mesothelioma is £3.4 billion. The report recommended a cross-government strategy for the removal of asbestos from public buildings within 40 years and a central register to record the location and condition of asbestos in public buildings.
These recommendations were robustly supported by Mesothelioma UK. Unfortunately, the Government/HSE response to the W&P Select Committee report showed little movement on any of the recommendations. On the phased, prioritised removal of asbestos from at-risk buildings –something Mesothelioma UK strongly advocates – the Government says: ‘The Government could only advocate a proactive course of action in this area if there is compelling evidence that the, undoubted, increase in exposure to asbestos workers that will result from active removal, possibly prematurely, is justified in terms of reducing risk of exposure to building users. At present this evidence is not there.’
With the continued danger of asbestos exposure, particularly to public sector workers, Mesothelioma UK will press the Government to empower the Health and Safety Executive to deliver better research, measurement and monitoring of asbestos risk, to ensure enforcement of and compliance with Control of Asbestos Regulations.
Until progress is made in terms of asbestos removal on a national scale, it’s vital that employers take the issue of asbestos seriously.
The UK has strict regulations to prevent people’s exposure to asbestos fibres. These regulations are the Control of Asbestos Regulations 2012. The regulations detail what actions need to be taken to identify and manage asbestos in the workplace, who can carry out work on asbestos, what training they need, what controls they need to use and what records they need to keep.
Regulation 4
Regulations 2012 requires the risk from asbestos in all workplace premises to be managed. This means that the location and condition of all asbestos within the premises needs to be identified, and the risk presented by any asbestos present has to be managed to prevent harm to anyone who works on the building, or to the building occupants. More details on the duty to manage asbestos – who, where, what, how etc is here on the HSE website and this useful guide will tell duty holders what steps to take to meet their responsibilities and keep their workplace safe for employees.
Until asbestos is removed from all buildings, people are still at risk of contracting asbestosrelated diseases. Mesothelioma UK will continue to campaign for change and encourages all employers to do all they can to raise awareness of the dangers of asbestos and take all possible steps to keep employees safe.
ATAC - the Asbestos Testing and Consultancy Association represents specialists in asbestos surveying and testing

NORAC – the National Organisation of Asbestos Consultants represents asbestos consultants
ARCA - the Asbestos Removal Contractors Association represents specialist licensed asbestos removal contractors
UKATA - the UK Asbestos Training Association represents asbestos training providers
For more information on mesothelioma, or if you would like to know more about our work and how to get involved please contact Mesothelioma UK at info@mesothelioma.uk.com or visit www.mesothelioma.uk.com




One of the primary goals of public health is to establish conditions that allow people to live healthy lives for as long as feasible. People are believed to spend around one-third of their lives at work. As a result, protecting the health of the working population through occupational health services has been recognised as an important component of public health strategy (WHO, 2001).
Occupational Health Nurses (OHN’s) deploy a variety of evidence-based clinical and risk management interventions to ensure that an employee's work tasks do not have a negative impact on their health (WHO, 2001).
This case study will outline the health and safety recommendations provided to a local authority in accordance with evidence-based clinical and risk management guidance.

The author was contracted by a maintenance team manager regarding occupational health advice. Management provided information about the employees’ occupational health history which included stress (work-related) and epilepsy.
The Health and Safety Executive (2009) advises employers on how to keep their employees physically and psychologically safe at work. According to the HSE, all workers have the right to work in environments where risks to their health and safety are effectively managed (Health and Safety and Executive, 2009).
The Health and Safety Executive (HSE) has identified six fundamental features that can contribute to work-related stress in the workplace (Health and Safety Executive, 2019). These features will be addressed in the section below and linked to the employee-reported workplace issues. According to HSE (2022), the estimated number of workers in the United Kingdom suffering from a work-related illness is 1.8 million, with stress, depression, and anxiety accounting for over half of all instances.
It is estimated that 50 million worldwide suffer from epilepsy, Epilepsy is defined as recurrent, unpredictable, and usually unprovoked seizure activity. Individuals with epilepsy are among the most vulnerable members of society because epilepsy is a hidden disability that remains a highly stigmatized condition to this day (Mula and Kaufman, 2020).
Evidence suggests that individuals with epilepsy face several challenges when it comes to finding and obtaining employment (De Boer, 2005). There are a variety of external factors that contribute to the disadvantages that individuals with epilepsy encounter when it comes to finding and retaining work. Researchers observed that employers were often unfamiliar with the different types of epilepsy, the varying ways in which epilepsy can affect different people, and the fact that anti-epileptic drugs can control the condition in some people (Francis, Byford and Wilson, 2019). The aforementioned factors were considered when developing a robust OH intervention plan for the employee in question.
The management team informed the author that the employee had recently had frequent sickness absences, all of which were attributed to work stress. The maintenance worker was initially hired as a Slater. However, in the last 18 months, the individual has been redeployed to another positionworking in a canteen. The employee is currently absent from his workplace due to reported work-related stress.
An initial fitness for work assessment was conducted as soon as operationally feasible as evidence suggests that intervention-based case management in OH can result in people returning to work sooner, which is cost-effective for the organization (Parsons et al., 2021).
Following a recent absence, the author assessed the employee's fitness for work and discovered that the source of the

all workers have the right to work in environments where risks to their health and safety are effectively managed
perceived work stress was twofold. The author discovered that the employee had a known epilepsy diagnosis and had a single seizure 18 months ago. This appeared to be the first seizure in a decade. The employee stated that he experienced multiple absences due to work-related stress during the 18-month period of redeployment. The employee felt unsupported by the management team and desired to return to his substantive work as a slater. The author wished to gain clarity on the employees’ health history. To do so, further medical evidence was sought from the employees’ GP and neurologist. The employee’s treating specialists provided evidence about the employee’s medical diagnosis, how his condition presents, and what treatment pathways have been recommended.
The first level of risk management in the workplace is risk assessment. It is the process of considering all of the aspects in a given circumstance, including recognising the dangers, the potential degree and nature of any risk, and those who may be affected (Williams, Dotson and Maier, 2012).
Risk assessment's findings serve as the foundation for ongoing planned management. Risk management is a plan, strategy, or programme that tries to manage an incident, event, or danger by removing or lowering factors that may cause harm and allowing any chance for beneficial outcomes to be taken as safely as possible (Aven, 2016)
1. Demands – The employee reported working in a deployed role where tasks allocated did not match his skill
set and where he felt that his specialist skills were not being utilized.
2. Control - The employee stated that he felt that he had little control over his current work environment and whether he would be able to return to his substantive post.
3. Support - The employee stated that he had not had much interaction with management since changes in management structure, and his health/work situation had not been reviewed as previously recommended.
4. Relationships at work - The employee reported that he was having difficulty blending in with the catering staff because they had been working together for many years and had a fixed ‘culture’. He added that he missed his colleagues in his substantive role, with whom he had worked for many years.
5. Role - The employee was unclear as to why, after several months in his redeployed function and with his condition having stabilized, he had not yet been reviewed or spoken with management about the possibility of returning to his previous role.
6. Change - The employee felt that the combination of changes in management structure, his job role, and the changes to his typically good attendance record were all too much and that he was unable to envision staying in the workplace if things remained the same.
The author was able to provide management with advice on health, safety, and risk management for this individual employee after reviewing and observing the employee's medical history and specialist reports. According to the employee's specialist, the individual had focal (partial) seizures without loss of consciousness. It was established that the diagnosis was given to him as a child, and he had been seizure free for ten years. It was noted that the disease was adequately managed with prescription antiepileptic drugs, and that the seizure 18 months prior was caused by unforeseeable circumstances. It was noted that the employee had gone on holiday without taking his prescribed medication for ten days.
Regarding risk management and the employee’s role, the author’s OH opinion was that the employee was fit for his substantive role which includes working from heights with a few recommendations. The employee should always be harnessed and wear protective headgear when working at heights, he should never be the first ascender and these recommendations should be kept in place for a minimum of 2 years. The author carried out an individual risk assessment with guidance from the specialist report and Epilepsy Action. The risk assessment was to be reviewed and updated every 6 months.
Risk management in the workplace is determined by four pillars. These include the employees' current capacity to perform their work tasks and whether
they have any physical or psychological issues that may interfere with their performance. The other three pillars entail the employees’ work tasks, work means / equipment, and the working environment. Collaboration between management and employees is required for occupational health to provide effective health and safety advice. Employers must follow good safety practices established by legal frameworks from apt governing authorities and legislation. (Jardine et al., 2003). Occupational Health Services (OHS) play an essential role in protecting all workers' health and wellbeing. Our primary engagement with employers as OH practitioners is through management referrals.
Ensuring that all Bio-Psycho-social components and workplace contributors are addressed in a consultation allows OHN's to provide fitness-for-work (Nicholson, 2017) advice as well as education and support for those managing the employees.
Phina is a Specialised Occupational Health Nurse (SCHPN) currently working for PAM Group. She is particularly passionate about community health and is a trustee of a charity focusing on tackling mental ill-health within the African / Caribbean communitiesBaba Yangu foundation.

 By Jo Vallom-Smith
By Jo Vallom-Smith
Introduction

The occupational therapy (OT) and occupational health (OH) professions emerged in the same periods for similar, work-focussed reasons. Over the centuries, we went in different directions and have remained relatively separate for far too long. Happily, however, we are now coming together to benefit employees and employers alike.
The following quotes are taken from Occupational Health: The Value Proposition (2022, Dr Paul J Nicholson OBE):
"Occupational health disability case management interventions that include early contact with workers on sick leave and specific agreements around work modifications result in faster returns to work and are cost saving"
"It is suggested that active occupational health care aimed at prevention and rehabilitation is more profitable than a focus on treatment"
A large meta-analysis of what works in occupational health found that interventions that were proactive and followed a rehabilitation model were effective and provide a good return on investment.
In Mark Howard's wonderful 2023 article, he explains the potential downsides of traditional OH services, which, in my experience, make up the majority of OH provision in the UK. He quotes Peckham, et al., (2017) who says "researchers and practitioners entering the field are largely being trained to assess and control exposures using approaches developed under old models of work and risks." and goes on to argue that "we need to better align with the current realities of work and health and to prepare practitioners for the changing array of workplace health challenges."
The Vocational Rehabilitation Association defines vocational rehabilitation as "a multidisciplinary intervention offered to those with physical, psychological and/or social difficulties enabling a return to work or preventing loss of work". Vocational rehabilitation interventions use a rehabilitation approach, which usually means working with the same person over a period of time to support them to work towards certain work-focussed goals. This kind of intervention has a strong evidence base for return on investment, especially for chronic and fluctuating conditions such as ME/CFS and fibromyalgia.
Following a referral, VR practitioners undertake an initial assessment, which is usually much more in-depth than a standard management referral. The VR practitioner may then make some initial recommendations, and the service may be complete at this stage.
More often, however, the practitioner will book a follow-up appointment to review the interventions and make further recommendations accordingly. In this model,
the interventions continue as long as there is a need and cease when this has been resolved. This creates the possibility for a more personcentred and targeted approach.
Whenever appropriate, VR practitioners will liaise with other stakeholders, such as HR representatives or the line manager, to gain a fuller perspective on the workplace situation to plan interventions appropriately.
Another element that often forms a part of VR interventions by OTs is "functional restoration" or "work hardening" programmes (the former being the preferred term). These can be delivered as an outpatient or in-house service. Functional restoration programmes (FRPs) may include time in the gym or the workplace, specifically working on factors that are preventing a return to work. These are widely used in the US, Canada and Australia and have a good evidence base for efficacy.
In this article, I often refer to the "OT" as this is my field of experience (and bias!). However, in many cases, these services are expertly delivered by a "VR practitioner" who may come from a vast range of backgrounds, including but not limited to nurses, psychologists, social workers and "non-qualified" workers.
VR provision within OH is not standard, and there is a wide diversity in how VR is delivered. In some OH companies, OTs are providing a hybrid VR-OH approach which has been received incredibly well with employers, who come back time and again for this service. Using this hybrid approach, all management referrals are undertaken by OTs, who will make a clinical judgement for each case as to whether they will follow up with this person to deliver VR interventions or if the one-off management referral was sufficient.
In other OH companies, OHAs or OHNs screen employees, who will then signpost, as needed, to an OT for VR interventions. In my
experience, many employers want VR for their employees but cannot access vocational rehabilitation through their existing OH provider. Therefore, a growing number of employers, particularly SMEs, are seeking these interventions through external specialist VR companies, most often from the insurance and medicolegal sector, where VR interventions are more commonplace.
I want to caveat this section by acknowledging my obvious bias towards OTs! However, I will try to back up my bias with evidence. OTs were created in response to a huge societal need for VR in the moral treatment movement and post -WW1. Our degree focuses on understanding
One of the cases that, I feel, best demonstrates the unique contribution of OTs delivering a VR approach to OH, is that of Mr X, who had worked as an operations manager for a public service organisation for many years. He sustained a road traffic injury which resulted in an amputation of his non-dominant upper limb below the elbow. Before returning to work, HR referred him to an occupational therapist. It was felt that their in-house OH team might not have the skills required for this complex and high-profile case. In the referral, practical concerns were raised regarding Mr X's ability to use DSE and operate a vehicle, but HR also identified some significant anxiety and low mood symptoms, which they felt may present an additional barrier to returning to work.
The occupational therapist met with the employee, completed an initial assessment and wrote an initial report. The occupational therapist then met with Mr X on several occasions over the following months and supported the implementation of various recommendations:
Voice recognition software to reduce the typing demand of his job
Arrangement of vehicle control adaptation

Engagement with the employer's EAP (employee assistance programme) for cognitive behavioural therapy
Signposting to peer support groups for amputees
A phased return to work. Not only the hours of work but gradually increasing the particular demands of Mr X's job that he found most challenging.
The occupational therapist liaised with the employee, HR, H&S and line manager throughout this process to ensure a smooth and sustained return to work.
In other settings, this gentleman may have been seen by an OHA or OHN, a physiotherapist and perhaps a physician. Mr X may have needed to repeatedly share his traumatic story and disclose the needs that made him feel incredibly vulnerable to people he may only see once. In this case, however, Mr X was seen by one health professional throughout, who was able to build a therapeutic relationship and coordinate all relevant services to meet all of his occupational needs. As well as seeing one professional, the VR approach was key in reviewing recommendations to ensure they met the identified needs.
I honestly believe that, without a VR approach, this case may have ended very differently. With a VR approach, everyone is a winner. The employee feels valued and listened to, the business retains important talent, and the occupational therapist has the satisfaction of going on a journey with a person and following a case to its conclusion.
the person, the task they’re required to do, and the environment in which they do it. We are rehabilitation experts and work in many rehabilitation fields. Our training covers not only mental health and physical health but also cognitive, neurodivergent, neurological, ME/CFS, chronic pain conditions and most other types of conditions that humans experience.
OTs consistently focus on function over pathology. Whilst we understand and consider diagnoses, medication and treatment, these are rarely our focus. We are hyper-focused on how any condition (or conditions) impact the functional ability of any individual worker. From day one of our degree, we learn to break down any task into the minutiae of its physical, social, cognitive and myriad other components using "activity analysis". Throughout our degree, we are taught about the biopsychosocial model and how to incorporate this into all areas of our practice.
OTs can and do work as occupational health advisors (OHAs), delivering traditional one-off management referral services and achieving the
same quantity and quality of work as their nurse colleagues. However, they also work as "specialist OTs", delivering a vast range of assessments and interventions. This may include cognitive assessments, functional capacity evaluations (FCEs), ergonomics and specialist mental health assessments.
A recent work-related development in the OT world is that we now work widely in GP surgeries, offering VR interventions and writing fit notes. OTs are well placed to offer this service due to their understanding of VR, breadth of training and focus on function.




In this article, I hope to have convinced you that occupational therapists have a key role in occupational health provision. Whether through specialist assessments, working as OHAs or delivering vocational rehabilitation interventions. There is a river of untapped potential here, and employees and employers will be the beneficiaries if we can make this shift together.
I'd like to leave you musing with a question.
What would a working population look like if all employers used a VR approach to OH instead of the traditional OH provision?
Jo Vallom-Smith is an occupational therapist who has specialised in the field of occupational health. Jo is the director of OTforOH, a specialist recruitment agency placing OTs in OH roles. Jo runs an informal networking group for OTs who work in occupational health. Jo is also on the national executive committee for the Royal College of Occupational Therapists, Specialist Section Work and is the Occupational Health co-lead. Follow Jo www.OTforOH.com. w.linkedin.com/in/jo-otforoh/
(2) Facebook

OHNAPS Conference to be held on 12 – 13 October 2023 at the College of Policing
The Occupational Health Nurse Advisers to the Police Services is a professional association of occupational health clinicians. Our members work in the OH departments of the police forces throughout the UK and support the National Police Chief Council and College of Policing governance and project boards. The patron is Chief Constable and College of Policing CEO Andy Marsh, QPM. There is an active membership, steered by an executive committee who work closely with the Oscar Kilo – National Police Wellbeing Service.
OHNAPS provides subject matter expertise and peer support to professionals working in OH departments and for strategic leaders of these departments. It promotes best professional practice by sharing policies and procedures. In conjunction with Oscar Kilo a course for those in this speciality is currently being developed.

The 2023 conference: “Sharing Best Practice” will be on 12-13 October. There are two free places per force, if your OH Service looks after two forces then there are four free places. If you have more delegates attending, then the cost is £120 per-delegate. Places include delegate attendance on both days, overnight accommodation, and formal dinner at the College of Policing. This is possible due to the generosity of the Oscar Kilo NPWS and our exhibitors. Certificates of attendance for CPD will be issued. The conference is open to all clinicians: OH Nurse Advisors, Technicians, OHP’s, RMN’s and other health professionals and managers & Heads of OH Services. The main speaker on Day 1 is Dr John Harrison the National Police Chief Medical Officer - Oscar Kilo - NPWS. He will be speaking on: “The police covenant and OH: potential and pitfalls”. One of our guest speakers on Day 2 is Janet O’Neill – Deputy Head of the National School of OH. She will be taking us through the remit of the NSOH, projects they are working on and blue sky thinking for future workforce development. Other topics on the programme include “CBRN - What is the OH role?”: “Overview of psychological health surveillance.”: “Should you ask for OH records when an officer is transferred between Police Services?” and more.
To register as a delegate please email: College Events events@college.police.uk College of Policing, Leamington Road. Coventry. CV8 3EN
Iwas a high achieving professional, working as Group Health and Safety Manager for a large PLC. Also, an academic achiever, having recently completed an Executive MBA and was on course to commence a PhD. However, in 2017 I sustained a concussion in a mountain bike accident and within a split second my life turned upside down. Initially, I thought it was just a bump on the head, but it became so much more than that. For many people, me included, it is a life-changing experience, and not always a positive one.
There is an ongoing debate about whether concussion should be renamed as a mild traumatic brain injury (mTBI). Literature uses the terms interchangeably (Clark and Guskiewicz, 2015, Graff, 2020)

Concussion is frequently described as a traumatic brain injury or functional injury, caused by a direct or indirect blow to the head, neck, or body (McCrory et al., 2017, Boshra et Al, 2020 and Patricious et al, 2023). An impulsive force is transmitted to the brain. It does not involve damage or change to the structure of the brain and is not visible on most readily available imaging in the emergency care setting (Lunkova et al., 2021, Pinky et al, 2022). Imaging is, however, important to rule out more
serious traumatic brain injury (Pinky et al., 2022, Patricious et al, 2023).
Typically, people with concussion will make a full recovery within 3 months; however, there are people (19%) whose symptoms still affected their work after this time; the most common symptoms in this group were workplace fatigue and an inability to maintain previous workload/standards (Cooksley, 2018).
There are 160,000 people who experience traumatic brain injuries each year in the UK (Radford, 2018). Concussion recovery is different for everyone, no two recoveries will be the same. (Karmali, 2022).

Much is still unknown about the wholebody impact of a concussion, and research is primarily undertaken with male elite athletes. Translating this to the general population, taking account of hormonal changes and physiological differences between genders is not easy. However, Patricious et al 2023, reports longer recovery times for females, due to the cyclical nature of female hormones and metabolic effects.
Ongoing symptoms of concussion (or post-concussion syndrome (PCS)) may be non-specific and may be due to other exacerbating factors such as mental health issues, sleep disturbance, learning and attention difficulties, vestibular problems and even menopause (Patricious et al, 2023).
For many people, me included, it is a life-changing experience, and not always a positive one.
Figure 1 below, demonstrates the number of functions of the brain and therefore the challenges in recovering from concussion. Understanding the points of impact that led to the concussion can be helpful to understand where there are likely to be challenges with areas of executive function (Dooley, 2022). Previously, it was thought that the only recovery from concussion was protection and rest, sitting in a dark room and avoiding any kind of activity that would stimulate the brain, however, given the interconnectedness of the human body, rehabilitation should have a whole-person approach, especially with the metabolic effects reported by Patricious et al, 2023.

A holistic and targeted rehabilitation programme can be helpful. I personally found immense success working with a practitioner who used a combination of Neuro Kinetic Therapy, Proprioceptive Deep Tendon Reflexes, and CranioSacral Therapy.
There are still questions about how to optimise a return to work given the variation in mechanisms of injury, personal experience, and symptoms (Patricious et al 2023).
Concussion has a complex pathophysiology that disrupts the normal neuro metabolic activities within the brain, causing an inflammation response. It may take up to 30 days to rebuild energy stores (Sun et al., 2008, Concussion Alliance)
The Consensus Statement in Concussion in Sport advocates a brief period of rest, which includes a reduction in activities of daily living during the initial 24–48 hours following a concussion, then proposes a framework for returning to work/learn then progressing in more vigorous activities/sport (Schneider, 2023).
(Adapted from Return to Learn, Consensus statement in Concussion in Sport, 2022)
Daily activities that do not result in more than a mild exacerbation of symptoms related to the current concussion
Typical activities during the day (e.g., reading) while minimising screen time.
Start with 5–15 min at a time and increase gradually.
Gradual return to typical life management activities
Dedicated cognitive activities
Setting aside time to perform cognitive activities such as reading or completing puzzles, logic games, crosswords, or similar outside of the workplace place
Increase tolerance to cognitive in readiness for work
Return to work part-time
A gradual introduction of work.
May need to start with a reduced day or with greater access to rest breaks during the day.
Increase cognitive load activities & reintroduction to workplace
Return to work full time
Gradually progress into full work activities until a full day can be tolerated without more than mild symptom exacerbation.
To return to full workload capacity
Individuals can then return to light-intensity physical activity, which does not more than mildly exacerbate symptoms, such as walking. Gentle exercise (without any risk of falls) is also great for regulating the nervous system and mobilising the lymphatic system to reduce inflammation. When I think about my own journey, it took some time to start normal daily living activities. Swimming was my saviour during most of my recovery, primarily as I did not have to worry about balance and coordinating my body.
Where there are cognitive difficulties, sleep disturbances, dizziness, headaches, and neck pain that persist for more than ten days, then further support should be gained from an appropriately trained and experienced physical therapist
Persistent PCS can have long-term consequences for return to work (Cancelliere et al., 2014) and influence selfesteem and quality of life (Mani et al.,2017). This is something that was very much part of my own journey. The one thing from my own journey that has really stood out, was that my recovery was anything but linear. This made it both frustrating and difficult to plan incremental milestones for both me and my employer. This is something that is repeated frequently by my clients and recalled anecdotally by my colleagues. A typical example would be completing routine work tasks successfully for several consecutive days, but then producing lower quality work whilst not displaying an overt return of symptoms. Working through this requires patience from both sides. Table 2 details the challenges involved for both employers and employees in successfully navigating returning to work.
Employee Employer
• Understanding of concussion
• Understanding their own capability
• Dealing with non-linear recovery
• Sensitivity to light and noise
• Visual and vestibular processing issues
• Reading comprehension
• Trouble finding words/word amnesia.
• Taking part in conversations with multiple people
• Insomnia
• Fatigue
• Tinnitus
• Headaches
• Attention span
• Anxiety & loss of confidence
• Emotional regulation
• Nausea
• Digestive issues and food sensitivities
• Balance and co-ordination issues
• Cognitive capacity and processing
• Personal Organisation
• Memory and recall
• Support from family and friends
• Support from an appropriately qualified and experienced rehabilitation team.
• Travelling for work – particularly at dawn/ dusk or in rush hour
• Understanding of concussion
• Referral pathways and signposting
• Understanding the employee capabilities
• Dealing with non-linear recovery
• Adjusted working hours.
• Changes to shift pattern (such as not working nights)
• Flexible working
• Increased breaks
• Physical changes to the working environment (quiet room, reduced lighting, blinds, moving closer to entrance/ exits, working on the ground floor, different lenses in safety specs)
• Temporary secondment
• Working from home
• Decreased workload
• Re-allocation of tasks
• Less complex work allocated.
• Non-computer-based work
• Using additional technology (dictation & transcript)
• Buddy system
• Support of employer & colleagues
I know that from my own experiences, my ability to self-organise and be in the right place at the right time was deeply affected – as someone who was always unflustered no matter what and never late, this was hard to comprehend and accept. Other areas that I struggled with were memory recall, being able to keep up with the flow of conversation in meetings and being able to multi-task (e.g., listening and note-taking). I still struggle with memory recall now and being able to call things the right name spontaneously. Through a mindset shift and reframing, I no longer see this as a weakness, stressful or embarrassing. It is about creativity and finding new ways to use language.
Coming from a background in exercise rehabilitation, learning more about effective rehabilitation for concussion was key for me and my journey to where I am today. Even more so as the support and onward referral for specialist support from my GP was lacking. It consisted of you just need to rest, and that is as good as it’s going to get for you, so you need to accept it. I feel lucky to have learnt about concussion with some of the world’s leading educators.
• Dr Kathy Dooley - Immaculate Dissection
• Dr Ryan Foley and Dr Kyle PaxtonIntegrated Kinetic Neurology
• Dr Cameron Marshall – Complete Concussion
• Dr Molly Parker – Concussion Compass
• Carrick Institute
• University of Calgary
Claire is a Health Coach, Rehabilitation Therapist, Sports Scientist and Chartered Health & Safety Practitioner. Before moving to independent practice and consultancy she worked in senior leadership positions in highprofile safety-critical organisations leading their health, safety, and wellbeing programmes.

In her independent practice, she practices a whole-person approach, working with all aspects of women’s health, particularly perimenopause & post-operative recovery, and concussion rehabilitation, alongside supporting organisations with their workplace health and wellbeing programmes.
www.restoring-balance.co.uk
PS I didn’t get to start my PhD, but I have accepted that my brain just does not work that way anymore and that I have gone a different but more fulfilling path.





 By Rachel Rowe SiSU
By Rachel Rowe SiSU
In late July, the Department for Work and Pensions (DWP) and Department of Health and Social Care (DHSC) announced they are looking at plans to widen access to health support in the workplace. Employers will be encouraged to take up Occupational Health offers to help employees access vital mental and physical health support at work. But how do we scale quickly and provide occupational health services that are affordable, particularly for the smaller and medium organisations? Traditional occupational health services often face challenges in reaching a large number of employees due to logistical constraints and costs.
It was announced in June that Digital NHS Health Checks (free for those eligible over 40 years old), will be rolled out from next Spring to alleviate the pressure on GP surgeries. The initiative will deliver one million checks in the first four years, according to the DHSC. Tens of thousands of cases of hypertension are expected to be identified and hundreds of strokes and heart attacks prevented with patients accessing the health check via digital means. A great example of how innovative
technologies can be rolled out at scale and can transform the healthcare system in the UK.
When will this technology be available to utilise in the workforce? Technology that gives you detailed real-time data and insights on the health of your workforce, facilitating early intervention of those who might become unfit for work is already available today.
Leading companies such as Aldi and Currys have been early adopters of selfservice health check technology in their

SiSU Health Stations have empowered the Health and Wellbeing Teams
workplaces. SiSU Health Stations have empowered the Health and Wellbeing Teams with detailed insight into their workforce health, well-being and the productivity impacts over time.
This technology offers cost effectiveness and increased efficiency when compared to traditional people-embedded service. By digitising various aspects of health monitoring and data collection, Occupational Health Teams can optimise resource allocation, and offer more personalised services to a larger employee base. The data collected can be used to target and tailor wellness programs enhancing the effectiveness of these initiatives with ongoing, accurate measurement of impact.
The increased accessibility, real-time monitoring, data driven insights and personalised user experiences, can empower occupational health practitioners to transform employee health and wellbeing propositions at scale. Embracing such digital solutions not only benefits the individual employees but enables employers to monitor health at scale whilst reducing costs and enhancing productivity and wider society benefits in the long run.
The data produced by these digital solutions is both accurate (measured by a medical device and not self-reported) and incredibly powerful. For example, did you know that employees in Transportation have the highest number of health risks (and the highest levels of smoking). Transportation also has the highest proportion of employees living in deprived areas. However, we also see the greatest improvement in BMI risk in Transportation when platforms such as SiSU health are implemented. (Source).
With NHS services stretched to their
limits, employers are needing to re-consider their role in supporting the health of their employees. But to truly scale and be fully inclusive, these solutions also need to flex to the different needs of individuals and to the new hybrid ways of working and therefore cannot only be available in the physical workplace or just via apps. Solutions need to exist in places where people live their daily lives – supermarkets, pharmacies, leisure centres, libraries.
Local authorities such as Luton Borough Council and Buckinghamshire Council are already being proactive in adopting digital health check technology for their communities. Working together with workplaces, the promotion of self-service health checks in the community, can not only positively impact the health of workforces but also the wider community in improving longer term health and addressing health inequalities
Christina Gleeson, Public Health Manager at Luton Borough Council and says “Working with SiSU Health has enabled localised, tailored opportunistic health screening aiming to tackle modifiable health risk among some of our poorest and marginalised communities in the town. The high proportion of the calls to action identified has enabled greater support to be provided by our local integrated wellbeing service already tackling health inequalities faced by such communities.”
Health inequalities arising from poor access and poor engagement with healthcare services result in low health literacy and preventable health risks. This results in a cost to business and to the NHS. It costs the NHS c.£4.8 billion each year for the greater use of hospitals by people in deprived areas (source). This is because those living in more socio-economically disadvantaged neighbourhoods and minority ethnic groups have higher rates of hypertension, diabetes, asthma, COPD heart disease, liver disease, renal disease, cancer, cardiovascular disease, obesity and smoking.
SiSU analysed millions of data points from their UK health checks to better understand the issues around health inequalities.

The results highlighted that 74% of people who completed a health check, had not had their blood pressure measured in the last 12 months, but in males who recognised as being of mixed ethnicity, it was over 80%. Put another way and more concerning, 62% of people who measured a blood pressure risk, had not recently measured it and so were likely unaware. Users identifying as Black, reported the highest levels of BMI and blood pressure risk with the prevalence of people with BMI obesity (BMI 30+) strongly aligned to their deprivation.
Regarding the potential impact on health literacy and motivation to improve health, 35% of people reported not being aware of the health risks identified by the health check and that rose to over 50% for Asian people. Over 70% of people who completed a health check reported they were motivated to make positive changes to improve their health because of the check and that rose to over 90% in those identifying as black. Demonstrating the real power and impact of these highly accessible,
scalable solutions for everyone.
Testimonials from that cohort are formidable:
“Now l am more aware that if I do not keep my weight and BP in check, I might suffer stroke and heart diseases.”
However, these platforms not only come with the ability to identify and support health risks, but also to integrate and signpost people to the most appropriate health service for them, according to their level of risk and the services available. For example, by directing people with high blood pressure, high perceived stress, high BMI, smoking, alcohol risk etc. to an onward service, whether that be an occupational health service, pharmacy, partner or an NHS service.
In the rapidly evolving landscape of healthcare, the integration of technology has proven a powerful force for change. The realm of occupational health services is no exception as digital health checks emerge as transformative tools to drive costeffective scaling, promoting employee wellbeing and addressing health inequalities
SiSU Health provides highly accessible, self-service health checks, utilising a medical device (class 11a) health check machine, the SiSU Health Station. A typical health check takes about 5 minutes and includes Height, Weight, BMI, Blood Pressure (BP), BP medication and recency of check, Heart Rate, Body Fat, Smoking, CVD risk, Alcohol, Physical Activity and Perceived Stress. No supervision is needed. SiSU Health’s Mission is simple: “to help people live a healthy life”. Read the UK Health Equalities Report in full: https:// www.sisuhealth.co.uk/uk-health-report


 By Lucy Kenyon
By Lucy Kenyon
Technology that might move our industry forward is subject to the mathematical modelling behind policies. In this article, I am exploring the factors that influence Insurance Risk Assessment. Selfinsuring organisations such as the NHS, primary care, prevention and treatment services are already using the latest wearable technology, the use of which is subject to consent to share data with AI. OH services are required to hold insurance policies and their records are ‘Special data’ with additional safeguards over and above patient records.
Clinical decision-making pathways have been featured in NICE guidelines since 2002 when the first clinical guideline was published on schizophrenia. They are designed to improve consistency of treatment across the UK and this makes the model ideal to address the public concerns around variability in OH advice. Pre-placement recommendations are probably the most automated OH process at present. Applicants and new starters answer yes or no to a series of questions, often
resulting in the need for a follow-up call from a health professional to clarify whether there is an impact on work and/ or adjustments required.
A McKinsey study reported the lowest automation potential for professionals managing people (9%) of work time and those applying expertise (18%). Other factors were costs to automate, availability and cost of skilled workers, quality gains), and regulatory and social -acceptance considerations. Professions applying medical expertise were rated low-risk overall.
We cannot discuss the digitisation of OH and the use of AI without considering policy underwriters for OH businesses. My own experience is that most underwriters still have little understanding of the scope and purpose of OH beyond listed chargeable activity titles with no requirement to clarify the decision-making processes involved. Actuaries and underwriters working with experienced OH brokers such as BHIB report being wary of services using
AI has the potential prevent incidents becoming tragedies tragedies themselves being repeated.
triage and automated decision-making. OH needs technology that facilitates efficiencies, learning and growth at a similar rate to other areas of healthcare. Would training help the financial and insurance sectors to safely remove or reduce the barriers to technological advancement whilst maintaining data protection?
The recent conviction of a health professional is a powerful example of the consequences of not understanding or learning from incidents. It also generated earnest discussions amongst fellow OH professionals regarding the consequences of and liability for ‘fitness for work’ recommendations, as we contemplate the outcome and impact of a new Clothier style enquiry into how fitness to practice might best be assessed. AI has the potential to prevent incidents from becoming tragedies and tragedies themselves being repeated.
Custom and practice continue to see the term ‘Fitness Certificate’ issued by OH services. Most of us have experienced the frustrations of our service users when a relatively new starter experiences difficulties before the end of their probationary period despite having been issued with a Fit certificate at the time of the job offer. It is clear from the number of employers expressing at best disappointment or referring individuals within the first 6 months of employment that their expectations and interpretation of these certificates are a guarantee of fitness.
One positive legacy of COVID is how it changed managers’ perceptions of OH advice. Our reports were suddenly welcomed enthusiastically as sources of evidence for protective arrangements or reassurance that the available evidence
suggested that they were unlikely to experience severe illness. Although R Kelly v Royal Mail (UKEAT/0262/18/RN) is not a landmark judgement, Justice Choudhury was eloquently clear in his recommendations about OH advice; “That assistance and guidance may be to the effect that the employee is a disabled person: and, unless the employer has good reason to disagree with the basis of such advice, he will ordinarily respect it in his dealings with the employee. In other cases, the guidance may be that the opinion of the adviser is that the employee is not a disabled person. In such cases the employer must not forget that it is still he, the employer, who has to make the factual judgement as to whether the employee is or is not disabled: he cannot simply rubber-stamp the (OH) adviser’s opinion that he is not.”
This raises fundamental questions about the nature, reach and outcomes of OH advice in a digital age. As soon as AI apps and systems appeared, my business partner asked me whether it was safe to use one of the familiar AI systems to generate an OH report.

In 1948 the first radiology images were sent 24 miles over a telephone line. Since then technological developments have paved the way for the transmission of psychiatric consultations via closedcircuit TV and in-flight monitoring and self-reporting of heart rate, temperature and respiration via microphone in the ‘60s. 1982 saw the first digital health assessment using a wearable biometric sports watch.
In 1983 the American Industrial Hygiene
potential to incidents from tragedies and themselves repeated.
Association reported that “The use of the microcomputer offers a simple, inexpensive solution to the numerous problems associated with data management in an OH program”. I first used an OH records management system when helping Peter Mattison set up health surveillance for Body Shop manufacturing in 1995. In the last 30 years, implementation on a large scale has remained challenging on technical, logistical, and financial levels. Comparative studies of digital diagnostics have published reassuring data on safety and feasibility, but the implementation challenges referred to above highlight the need for training and the knowledge of pitfalls.
The DHSC code of conduct lists the following behaviours expected from those developing, deploying and using datadriven technologies:
Many clinicians remain reluctant to sign off reports on selfassessment questionnaires alone and are concerned about reporting without the clinical consultation that has historically represented their profession.
Cost-efficiency analyses and OH issues need to be addressed comprehensively. Health risk assessment is being blended into the traditional OH workflow, and the approval of AI for routine assessments is beginning to challenge human evaluation as the gold standard.
The addition of artificial intelligence coupled with technical challenges to increase availability and efficiency in OH is already driving changes to the profession, and we must retain ownership if we are to maintain the protection of the ‘special data’.
Historically, completed questionnaires were digitized for detailed evaluation and record keeping, audit and teaching. The introduction of “tele-assessment”, pioneered in OH in the early 2000s, saw consultations carried out by telephone rather than in person, challenging the idea that visual assessment of the individual would provide greater diagnostic accuracy than competent clinical assessment. The intention was to reduce
time away from the workplace for the individual and time lost by clinicians and service users in case of late arrival and unplanned or complex documentation.
Faxed or scanned images of forms and letters within OH workflows have propelled us into digital medicine (DM). Digital images and video streams can now be shared in real-time (telemedicine), bridging the physical distance between clinicians and service users. For me, this has led to real-time case conferences at the end of consultations to ensure that the manager has immediate recommendations to consider pending the final report.
Digital health surveillance images can now be evaluated by OH physicians for early signs of occupational disease with digital record keeping developing the capability for new trend recognition and analysis that outstrips the traditional assessment of symptoms and links images to clinical data. For me, the most exciting aspect is the opportunity to record and monitor decision-making using AI and make occupational disease truly preventable and ultimately a thing of the past.
Digital OH provides enables in-house validation of representative cases and techniques. Should OH work to the Digital Imaging and Communications in Medicine (DICOM), standard to ensure that diagnostically used data storage is adequate?
In conclusion, the digitisation of routine diagnostics is complex and requires expertise, human resources, and a continuous focus on technical advances.
Clinicians may also need external professionals to define specifications for major hardware procurements and compare vendors’ offers in-depth meaningfully.
A quick search for AI clinical workflow produced several applications providing analysis of reports before actual signout, configured to analyse the assessment report as well as images of screening to automatically alert the clinician to potential diagnostic discrepancies before final sign-out. I understand that AI that collects and analyses human input has been proposed to triage cancer pre-screening cases for reporting and to balance workload distribution. This has huge potential for mesothelioma and other occupational cancers.
AI applications have been shown to benefit from human input for increased classification performance and reduced training. This concept is called “Humanin-the-loop”.
With the majority of OH professionals operating independently, costeffectiveness can only realistically be achieved with a digital assessment workflow that does not cost more than the human processing time and also enables human audit on request.
We cannot talk about the use of technology within OH without considering the foreseeable risks associated with continuous DSE use. Time-efficient hardware and software must consider digital eye and upper limb strain. Between 64% and 90% of computer users experience visual symptoms such as dry eyes, headaches,
eyestrain, burning eyes, diplopia, and blurred vision when using (computer) screens (M Rosenfield, 2011). Musculoskeletal injury from computer use has been estimated to account for at least half of work-related injuries (PC Bohr, 2000).
Keywords:
digital occupational health; machine learning; artificial intelligence; occupational health; computer vision syndrome; automation; clinical guidelines, clinical protocols, underwriting, medical malpractice, medical negligence, public liability
Lucy Kenyon is a Specialist Independent OH Nurse Consultant who has been teaching and mentoring Occupational Health since 1996 for the RCN, Universities of Birmingham, Coventry, Derby and West of Scotland. She delivers professional development courses for the National Performance Advisory Group, Cordell Health and employers. Lucy was President of iOH from 2017 until 2020. She has been a NonExecutive Director since 2021. She has a Master of Medical Science and International Certificate in Occupational Hygiene from Birmingham, where she has taught and worked on research projects. Follow Lucy on LinkedIn.

In this article, Dr Nikki Cordell, CEO of Cordell Health, and a keen proponent of technology in the occupational health sector shares how we can use data to improve the quality and evidence base of occupational health practice. She will also explore how the profession can harness the power of technology to support their clinical practice and improve outcomes.

How should clinicians use data in decision-making? Whilst clinical experience is a key factor, as clinicians we need to be careful that unconscious bias doesn’t influence the specialist advice we provide to both employee and employer. Within the sector, we promote occupational health as being independent and evidence based, but how much of our decision-making meets these criteria. Therefore, it is essential we consider what data we use to help inform our decisions and opinion, its quality and how it’s both accessed and interpreted.
“You can’t manage what you can’t measure” is a well-known quote by management guru Peter Drucker
This does have relevance to occupational health practice. The more sophisticated we are in how we measure, what we measure and how we manage data, the more robust and evidencebased our specialist advice becomes. Data collection and analysis of health metrics, combined with harnessing targeted information published in evidence based publications relevant to the case in hand, can provide a tailored approach to the advice and recommendations we provide as clinicians.
Primarily because the better the quality of the data available to practitioners, the more confident we can be in the advice we provide to inform decision making within our day to day work. Good quality
data helps us move beyond mere assumptions and subjective judgments avoiding our unconscious biases. Stepping back to objectively assess the facts, and where useful, undertake trend analysis of data for target populations, provides us with a powerful tool to advise employers in order that their decision-making can become more evidence based and grounded in the facts.
A practical example of this would be in providing advice for shift workers. We understand that rotating shift patterns can have adverse impacts on employees. We can use this information with data provided on a night worker questionnaire to advise at employee level and organisational level on interventions which might improve health. How much more tailored would the advice be if we add data on cognitive performance over the working shift pattern, heart rate monitoring and sleep patterns? This would allow us to provide bespoke advice to the employee on measures to optimise their health whilst working shifts.
As occupational health practitioners, we want to be able to identify potential hazards and advise organisations on potential mitigation of occupational risks before they escalate into significant health issues. In the example above, an analysis of trends on cognitive performance and sleep would help identify for the employer if there are elements of the shift pattern which may present potential health and safety risk in order that they can manage this more effectively or, provide reassurance that no change to shift design is required from a health perspective.
Data can only bring benefits if both occupational health practitioners and employers are able to access what they need

Much of the data used by occupational health practitioners has been a measurement of a particular point in time. Assessments and medicals were done periodically which, while helpful, also carried the risk that any subsequent changes wouldn’t be detected until the next assessment. With real-time data and analytics currently being developed in the health and safety field to support employers meeting their health and safety responsibilities to reduce risk, we now have an incredible opportunity to apply this also to workplace health. The use of wearable devices, sensors and monitoring equipment can all contribute to providing data to optimise health as well as manage risk better.
By integrating health data with data on workplace injuries, illnesses, and nearmiss incidents, organisations can identify high-risk areas or job roles that present potential risk to health and implement targeted interventions to where they are most needed.
As with all new advances in the technological world, real-time monitoring does present potential risk in how data is used. There is nervousness as a result which needs to be addressed. In particular addressing ethical and governance issues transparently and putting in place measures to ensure that data is used appropriately in accordance with data protection law will be key to successful
transformation in the health, safety and wellbeing world.
In most occupational health practice, we often have data in multiple places, in different formats (electronic and paper) and with key data points in scanned or pdf files which make any aggregated analysis challenging. The development of technology, particularly in Artificial Intelligence holds great potential in data-driven delivery of healthcare, but the current software platforms available to the occupational health sector do not have this capability.
Our new Information System for Health and Work, ISHAW, and its occupational health application, MediWork will be a game changer. The unique combination of human clinical expertise and leadingedge technology will radically transform occupational health delivery with the aim of doing so much more with less investment. The first phased of development is complete for launch on 01 September 2023 including modules for post-offer screening including healthcare worker/student screening, health surveillance, and case management. An exciting road map of development of tools is planned over the next decade with the aim of optimising health and wellbeing at work.
Transformational change of occupational health, safety and wellbeing services are at a place is incredibly exciting, with the potential for significant benefit to both employees and organisations. By having robust, ethical and reliable systems to support data driven decisions, organisations can be supported in identifying and mitigating risks. However, data can only bring benefits if both occupational health practitioners and employers are able to access what they need. Data systems designed to empower rather than hinder are an absolute requirement to support this transformation and play its part in creating healthier employees and more productive organisations as a result.
MediWork is a secure, cloud-based comprehensive occupational healthcare management application for delivery of occupational health services. It is part of the ISHAW suite of tools that aim to transform work health for the future. It is designed for efficiency whilst capturing key data. The aim is to build a robust database of information to provide trend analysis and data analytics with a key focus on outcome data which will help inform occupational health practice. The system will empower clinicians with data to support their service delivery whilst minimising the administrative burden of day to day clinical practice.
Find out more about ISHAW and MediWork
If you would like further information, please contact us at MWenquiry@cordellhealth.co.uk
Dr Nikki Cordell is co-founder and CEO of Cordell Health. An experienced specialist occupational physician, she passionately believes in improving the health of workers, pursuing excellence and bringing innovation to the way that health and wellbeing is delivered in the workplace.

 Michael Whitlow, Case Manager,
Michael Whitlow, Case Manager,
Demonstrating the case for the skill of work coaching in supporting those back to work and in work. A personal reflection.
Dr Shriti Pattani, past SOM president, promoted employment support for the over 50s who may have chronic health conditions. She and SOM advocate primary care services to capture this group and piloted a scheme of Work Coaches within GP practices (SOM Jan 23). The Government, recently published a consultation – Occupational Health Working Better (Chapter 3:66 August 23), where they say they will consider the “emergence of innovative new approaches to low-intensity work and health” including the “SOM-led initiative which also involves a pilot ‘join up’ between OH, primary care, and DWP Work Coaches to reduce worklessness due to ill-health”
According to the DWP, “Work Coaches
are customer-focused, dedicated individuals, able to deliver exceptional service with empathy and compassion to people who need their support”. Work Coaches use sound judgement and tailored coaching to help people’s ability to find, stay in, and progress in a job.
This is an insight from a Work Coach perspective:
Having worked as a Work Coach and experienced many situations, I discovered a lot of what I did was to help those in need with their confidence in work and their ability within it. It always seemed to come down to a few things:what they have to offer, their skills and recognizing competency.
Competency questions are always the biggest obstacle, no one enjoys answering competency questions:
“

Give me an example of when….”
This is difficult for most as it asks them
PAM Wellbeing.
a lot of what I did was to help those in need with their confidence towards work and their ability within
to think of a time when they have succeeded or made a mistake. Two things rise from this:
Difficult to think of success, as at the end of the day it is their job! People can’t perceive something as successful if it’s just a part of their day-to-day tasks. Getting them to understand this can be enlightening for them.
No one wants to acknowledge that they have made a mistake as they feel it will go against them. However, I discovered that encouraging them to rephrase it in their own mind and instead of “mistake”, look at it as a lesson, rephrase the question from “when have you made a mistake” to “tell me a time when you have learned from a negative experience”. I found that people can engage far more when rephrasing a mistake.
Key skills are also a huge part of someone’s confidence. I found that most people don’t know what skills they have. They know what their job role was and what their day-to-day was, but they’re unsure how to bullet points this. Asking them to describe an average day would usually give me an idea as to what key skills they have.
Transferable skills: Like key skills, it’s useful to know what these are, but people find it difficult to put into words what skills they have to offer.
Confidence: As I stated at the beginning, confidence is such a huge part of why people find it difficult to get back into work or into a different career because they’re unsure as to what they can bring to the table. Going over my previous two points can help them to realise their potential, thus increasing their confidence.
I discovered very quickly that mental and physical health impacts an individual significantly harder than we think. As someone who experienced mental health problems that impacted work, I am not only passionate but knowledgeable about this.
Moving from Work Coach to Case Manager within Occupational Health Psychological Services
A Case Manager role within EAP (Employee Assistance Program) provides short-term interventions for employees (DeGenarro 2008).
Transferable skills, moving from a Work Coach to a Case Manager within EAP (Employee Assistance Program) were a lot more obvious than I had anticipated. Working with the public, helping them to realise their potential and supporting them back into work, gave me the skills and understanding to support those already in work but struggling. I have found that people need someone to speak to when they’re feeling low or unmotivated. An ear can be enough in some circumstances.
I quickly discovered that the positions are very similar in the respect that anyone I speak to is going to need me to be patient and able to listen. Most people are unsure what to do, they’re confused, upset, and can sometimes be annoyed. So, it’s very important to recognise the intentions of the individual, i.e., what exactly is motivating them to get in touch. Having gone through it myself in the past, I find that I’m able to empathise and put myself in their position. Although listening tends to be one of the best things you can do for someone, being able to effectively understand what it is they’re going through can help just as
much if not more so. It is my job to accommodate everything being said, let them know they’re being listened to and give tailored advice specific to that individual.
The first thing I tend to do is note that they have acknowledged that there is something wrong. That this is courageous. Some people can’t see past their pride so keep struggling each day. It is important to respect that it’s difficult to even ask for help.
The second thing is to make notes and be able to repeat back any important thing they have shared. There is nothing worse than trying to explain something and having to repeat it, especially when you’re not in the best mental state.
The third thing is patience, some people may talk slowly or take a little bit of time to say what they mean, so just allowing them to get to that point organically can help them to open up.
I have always tried not to act like I know what they’re going through, it can be frustrating for some people if someone keeps saying they understand or they get it because usually, you feel like you’re the only person going through it so no one can understand, which is why it’s best to listen. This aside, sometimes solidarity can be a very useful tool in certain cases but again, it comes down to the individual and it’s up to the skill of the Case Manager to determine this and then tailor the experience to them.
Wanting to help people is a huge part of either role. Knowing that you’re making even the slightest difference makes either role easier. Admittedly, it can be emotionally demanding but wanting to help can make any day better with the knowledge that someone will benefit. Applying a different perspective can make all the difference, especially when it comes to mental health. Not only can it help the caller, but it can also help you to apply a more positive phrase to things that may appear tedious and unhelpful.
To conclude, most of the skills I learnt while working as a Work Coach, I have easily applied to the case manager role. The day-to-day within both positions is very similar in the respect that every call and every email is from someone looking for support at work. We all understand the importance of needing to work so anyone willing to reach out to overcome their battles is already making huge steps. Although each call is different they all share the same goal. Thanks to my experience as a work coach, I have started to understand what it takes to actually support somebody who, without us there to help, would otherwise get worse in the long term. There are many uncertainties so being consistent for those reaching out is very positive.
Michael is a Case Manager for PAM Wellbeing part of PAM Group. Originally studying to be an English teacher, then working in customer services, he went on to become a Work Coach and Training Facilitator before moving into case management. PAM Wellbeing case managers ensure that all counselling cases are matched to the most appropriate counsellor for the individual's needs and monitor the ongoing activity of the case.
He is a keen musician and has been a guitar teacher as well as a mental health advocate. He has always been fairly goaldriven & ambitious and always looking for his next challenge.

Imanaged this case between September and December 2021, during the Covid 19 Pandemic. I spoke with Debbie on three occasions, supporting her and guiding her employer. What started as upset and tears ended up with laughter and tears for both of us! Below is an extract from my book “Mental Health in the Workplace: A Practical Guide for Occupational health Practitioners on Consultations and Report Writing.”
Debbie is a 55-year-old female, working fulltime as a community nurse. She has been working throughout the Covid pandemic and has been off work for four weeks but feeling mentally unwell for nine months. Her GP has diagnosed PTSD. She was also diagnosed with ADHD at the age of 40.
Self-care: Showering less often and wearing pyjamas all day. Having encouragement to self-care from her husband and friend gives her a nudge to do so, but if she lived alone, she feels she would stay in pyjamas all day and
 By Libby Morley-Hassanali
By Libby Morley-Hassanali
rarely shower.
Concentration/focus: Watching TV for long is not possible. When scrolling Facebook, she is not taking anything in. Nods off to sleep watching YouTube videos.
Motivation for hobbies/interests: Usually likes to read about quite distressing things but now she is unable as it is upsetting her. Photography, but feels less interested lately. Says she has the thought to do things but then feels no motivation.
Sleep: Wears a tracker and it shows sleep is poor. Bad dreams about work. Says she feels tired and is going to bed early but wakes a lot during the night. Is not sleeping during the day.
Suicide risk: Says no thoughts of selfharm or suicide currently but did attempt when younger. Says, “occasionally I think oh god I could have another 20 years of this sh*t”. No current risk apparent.
As well as providing her lived experience of PTSD or burnout symptoms, her words also provide valuable insight into her experience of living with ADHD.
She is now back at work. Her contribution to my book is further evidence that people can and do recover from an episode of mental illness. You might need a tissue!
In Debbie’s’ words:
When I first spoke with Libby, I was dreading the call. As someone who has come up against many well-meaning health care professionals in the past, I was dreading another list of things I was supposed to do.
I have ADHD and it means I am a super over achiever that cannot keep simple things together. I can take care of the seriously ill and manage their care but seem unable to focus on my own needs or those of my family. I often tie my self -esteem to my job and so when I started to struggle with my work, I became fearful and nervous.
The pandemic started slowly changing how I felt about people. I have always thought that I was an endless supplier of tea and sympathy, always trying to fix people. I went further than others because I thought it was my responsibility to care for them when they had lost their way physically. I rarely held people responsible for their behaviours or actions and often felt that, given the right kind of care, I could make a difference. I arrive early and stay late out of my desire to always give 100%
I caught covid, and later I was diagnosed with long covid. During the time of investigations, I was working full time and studying for my master’s degree. My husband also contracted covid and suffered ill health for the next 18 months.
By the time I had to admit that I was not
OK I was tired, emotionally distant, and constantly angry. I am sure anyone close to me was worried about my constant obsession with the covid stats and my inability to focus on anything positive. I wanted to shout at patients who continued to come with their seemingly ridiculous issues. I had constantly tried to understand that they were going through this too, but eventually I just wanted to tell them that they had no idea what we were going through.
Just before I went off work there were some incidents that left me traumatised. Patients were becoming aggressive, there were patients self-harming in the department and staff were all feeling the same burnout. I had reacted out of character to a patient, and this had left me feeling ashamed to the point where I have put my head in my hands just thinking about it.
I went to my GP and sobbed to her about how I was feeling. I was not sleeping, was scared of everything, I jumped at loud voices or noises, and most upsettingly I had lost my empathy for others and spent my time either at work or at home thinking about work. Mostly instead of the accepting and helpful person I sought to be I was angry...really angry. I was scared by the depth of my feelings and totally overwhelmed.
So, as I sat in my car, parked near my church so that my husband didn’t hear the depths to which I had sunk, I got my first call with you. I remember little of what was said, I know I sobbed through most of it...I felt beyond sad, I felt broken.
I remember you said, “Debbie, you are very sick.” I felt like a weight was lifted at that moment. Finally, someone who wasn’t trying to negate my feelings or

I remember you said, “Debbie, you are very sick.” I felt like a weight was lifted at that moment.
give me some well-meaning advice. We did talk about some things that would hopefully help such as podcasts and mindfulness, and these were things I felt I could achieve. We finished with you telling me to rest and take care of myself and not to worry about letting coworkers down as I needed to be well to be able to help others. I remember thinking that for once I had not been blamed for feeling the way I did, I felt that someone had given me permission to feel it without having to justify my feelings. I felt legitimised.
My discussions with Libby were always about how I was feeling rather than what I was doing. In reality, of course there were always discussions about what I was doing but they never felt like that was the only point of the talk. Libby encouraged me to think about what I could do for me, rather than what I had to do for me. That might not seem like much of a difference, but it really was. Obviously, the older we get, the more emotional baggage we have. As a woman with ADHD, I had challenges that impacted my life. I was diagnosed late in life, and it made a huge difference in my ability to understand some of my issues. I never leaned on my diagnosis. I hadn’t really given myself permission to be different and not feel like others would find me odd. Wearing a mask of normalcy can be exhausting day after day. I had suffered abuse as a child and had an eating disorder for many years. This had all been dealt with by me having a better understanding of why I had been vulnerable to such things. Low self-esteem and feeling like an imposter are two of the many challenges that have been there throughout my life.
Libby believed me when I told her that
my past was part of my journey but not part of this journey. I have always felt that GPs looked at me as my issues and not as a person. I found myself worrying that they would judge me by my past diagnoses. I now also understand that not advocating for myself gives them little else to base their judgement on.
Libby helped me to allow myself to be kind to myself, and to stop blaming myself for not being more resilient. Instead, I looked for ways to build resilience again. To allow me the time to think without worrying. I truly believe that without Libby to support and guide me that I would have floundered further into a life disability. Having someone who knew how to push me and when to push me while being there if I failed was amazing. I have rebuilt my structure and reconnected with myself. I am sleeping well, eating better, I do Pilates, which is fantastic, I listen more and worry less. I have stopped stressing about the small stuff, and I find myself stopping to question my assumptions or actions and changing course appropriately. Self-education and opening to new things are powerful when we are encouraged and supported.
If you asked me how Libby did this, I would say by being supportive, constructive, and honest. Of course, I know she used all her professionalism and training to do what she does very well, but the best bit is that I never felt managed. I felt treated.
I have learnt to say no, I have learnt that I do not have to be extra just because I’m not neurotypical...that has been fantastic for me. I am embracing my differences and learning to use my newfound strengths.
Libby has become part of my journey, one which I will always remember with a grateful heart. I am not religious, but I do believe as I sat there next to the church, baring my soul, I found the best person to help me, and I cannot thank her enough.
Libby is an Independent Occupational Health Nurse Practitioner and trainer in Stress & Mental Health. She is the Author of the book “Mental Health in the Workplace: A Practical Guide for Occupational Health Practitioners on Consultation and Report Writing”, published in March 2022.



