














The iOH board have been working tirelessly getting ready for the Health and Wellbeing at Work conference at the NEC, Birmingham on 12th and 13th March 2024. If you haven’t booked yet, register at https://healthwellbeingwork2024.reg.buzz/ioh using code IOHSAVE10 to save 10% on the two-day ticket as a member. Don't forget to call in see us at Stand 47 to receive a gift, meet other members and hear about what's coming up.
We are excited to meet members and friends at the iOH annual Ruth Alston Memorial Lecture & Gala Dinner at the NEC Hilton Metropole Hotel on Tue 12th March. This is guaranteed to be a relaxing evening of networking and fantastic food and drinks. The lecture will be given by Professor Neil Greenberg, consultant, academic, occupational and forensic psychiatrist on “Creating a psychologically resilient workplace – lessons from the military”. iOH members tickets are discounted at £45 which includes pre-drinks, a 3course meal, and drinks. Tickets are still available and can be purchased for any non-member colleagues or friends.
We are delighted to offer Educational Grants for members to help with short courses. Details are available in the members area of the website. We are also supporting OH Educational Providers to promote their courses and the benefits of an Occupational Heath career. Our Director of Student Affairs
Debbie Easby and Professional Development Director Janet Garner are available to discuss educational or OH placement queries. They have done a sterling job over the last year to support our student population choose courses and look at funding options available.
Our next webinar delivered by Dr Jain Holmes and Mandy Kelly on Occupational Therapy, Vocational Rehabilitation and Occupational Health – What’s It All About? is open for booking on Eventbrite.
As always, the iOH board value the support of members and partners. We offer partnerships and advertising to those who meet our ethical and charitable purposes and may benefit from our growing membership. This helps to keep our membership admin fee at just £10 annually so it is affordable for all. More information at Corporate Partnership and Advertising
My sincere thanks go to the entire iOH board and supporters who volunteer to keep our charity running. Finally, you can contact the iOH Support Service if you require any confidential advice on OH matters or your OH career.
Lynn Pratt, President iOH


The Ruth Alston Memorial Lecture will be delivered by : Professor Neil Greenberg


The title of the Lecture will be:
Creating a psychologically resilient workplace – lessons from the military
Professor Neil Greenberg is a consultant academic, occupational and forensic psychiatrist based at King’s College London. Neil served in the United Kingdom Armed Forces for more than 23 years and has deployed, as a psychiatrist and researcher, to a number of hostile environments including Afghanistan and Iraq.
Event open to Members/Non-members Join the iOH
Event details can be found on the iOH Website
Tickets are limited and available at Eventbrite discount for members

Record numbers of workers are signed off work, as sick. GPs issued 10.4m Fit Notes in 2022 and sickness absence levels are the highest for 15 years. (People Management, March 2023)
The most significant factors include stress, depression, and anxiety; MSK, Long COVID, burnout, poor sleep, and fatigue.
In 2022/23, 35.2 million working days were lost due to work-related ill health. Stress, depression, and anxiety accounted for 24m lost working days with 79% of CIPD survey respondents declaring a work-related stress absence during the year. (CIPD)
In the UK, 2m people are estimated to have Long COVID, with fatigue being the most common symptom. (Source: ONS).
Alongside this, whilst we are thankful for and highly value our NHS, it is facing unprecedented pressures on multiple fronts including lengthy waiting lists and reduced access to GP care.
Add to this bleak picture, increasing financial pressures, the cost-of-living crisis, barriers to accessing resources and support; care responsibilities falling to families, friends and neighbours, long working hours, and the constant demands being placed upon people, it’s no wonder that we’re seeing the fallout of this impacting on the physical and


We are fighting a battle gaining momentum and raging like a forest fire across the health of our nation’s workforce.
mental health of the UK’s workforce.
• The annual cost of poor mental health to UK employers is between £53-56bn. Burnout, exhaustion, mental distance from the job, insecurities, and uncertainty have intensified absenteeism, presenteeism, and labour turnover. (Deloitte)
• 48% of employees are feeling fatigued, driven by workload, a lack of control and support levels (CH 2024)
• 47% of employees experience MSK pain with 1 in 2 of those saying it impacts their work productivity (CH 2024)
• 11.6m women in the UK live with an MSK condition and are twice as likely to experience pain as men (CH 2024)
• 37% of employees report experiencing headaches or migraines while at work with 47% impacting productivity (CH 2024)
• 61% of employees cite tiredness as impacting their productivity at work (CH 2024)
• Over 1 in 3 employees rate their sleep as poor (CH 2024)
It’s no wonder that workplace stress has increased by 50% since 2023 (CH 2024) and that stress severity levels (Moderate -High levels) are rising with a 14% increase from 2022 to 2023. We know that within the workplace, line managers themselves are squeezed, with 50% reporting feeling burned out at work. High workload and limited resources are cited as the main causes,


Occupational Therapists may not have a magic wand in their toolboxes, but what they do have is dual training in both physical and mental health.
with managers having to care for their struggling teams as well as manage their health, family lives and workload.
So, what can we do? Workplace adjustments are necessary and helpful, but are they enough given the back story and the unprecedented pressures people are under and facing every day?
Occupational Therapists may not have a magic wand in their toolboxes, but what they do have is dual training in both physical and mental health. A unique profession where work is integral to the ethos of the profession and who can provide biopsychosocial assessment and intervention programmes with recommendations for both physical and mental health conditions.
A referral will often be made to an Occupational Therapist by the employer, Occupational Health, or HR department with the reason for referral often including but not being limited to:
Physical symptoms such as:
• Fatigue
• Exhaustion
• Headaches
• IBS type symptoms
• Pain
• Changes to sleep quality and patterns.
Cognitive symptoms such as
• Poor concentration
• Brain fog
• Difficulty making decisions.
• Poor short-term memory.
Emotional changes such as
• Irritability
• Low mood
• Anxiety
• Negative outlook
• Emotional lability.
Behavioural changes such as
• Withdrawal or increased mental distance.
• Reduced work performance
• Procrastination
• Absenteeism.
The PEO model is an occupational therapy model - Person, Environment and Occupation. It helps determine the relationship between a person’s health and the work activities they conduct in their environment but crucially too, how they manage this in conjunction with their daily lives. Having a holistic or whole life approach for identifying and managing sickness absence including health and optimising energy can make the difference with engagement and sustainability, specifically when we are helping organisations maintain a healthy and thriving workforce. Crucially, the support provided to employees when returning to the workplace or trying to remain well at work, must be about more than work. We need to consider the whole life which is why occupational therapists partner so well with existing occupational health professionals in providing that additional bespoke clinical intervention.
The employee may be struggling at work, but an Occupational Therapist will also spend time assessing what is taking place outside of the workplace and how the employee is using their energy during the remaining hours in the day
and across a 24-hour period. For example:
• Do they have another job?
• Are they a carer for an elderly relative or young child?
• Are they studying and having to write essays/prepare for exams?
• Are they struggling financially and worried about mounting debts and losing their home?
• How is this impacting sleep/ nutrition/exercise and usual ways of managing stress and taking care of themselves?
The sooner a referral is made, the better. A diagnosis is not required-it can simply say ‘struggling with low energy and fatigue.’ An occupational therapist can then assess the whole person including their work role and responsibilities, what this entails, ergonomics, and any current or adjustments.
As part of that assessment, the Occupational Therapist will also look at pain, mood, anxiety, energy, sleep, routines, activities of daily living, personal care, diet and nutrition, movement and exercise, social activities and whether they are accessing the financial support available.
From this comprehensive assessment of an employee’s 24-hour energy spend, a report will outline and highlight areas for change and support, both inside and outside of work. It’s as important, if not more important to consider what needs to change at home with usual daily chores and activities including sleep, diet and movement to give the person the best chance of being able to do their job and fulfil their employment responsibilities without it having a
detrimental impact on their physical and mental health such as pain, fatigue, migraine, mood or anxiety.
As an example, if an employee is working all day, then going straight to their caring role, with no time to eat, pause or rest and arriving home to take care of their chores and responsibilities before falling into bed tired but wired and with a banging headache, it’s unlikely they will have a good quality sleep; nutrition may be compromised; the body will be stressed and under pressure and not well rested which doesn’t put them in an ideal position to carry out their role at work.
However, a carefully devised Occupational Therapy programme will include actions for home, focussing on the presenting difficulties, sleep routines and daily activities. Rest, and how to achieve an effective resting routine will be incorporated into a simple programme to ensure the employee has an opportunity to recharge their batteries regularly over the day. Adjustments within the workplace will also be considered and discussed with all major stakeholders and the Occupational Therapist can support with regular reviews to ensure the programme is achievable and on track. Where a return to work is being planned, an Occupational Therapist who is trained in vocational rehabilitation will understand how to consult with all parties to make sure the return to work is realistic and sustainable and all other rehab goals are planned as part of the overall picture.
It is much better to keep an employee well at work and if possible, avoid them going off sick.
Although an employee may not have a
medical diagnosis, by taking a proactive approach, the line manager, HR or occupational health teams can access occupational therapy support early before things become more difficult, mistakes are made, or a situation becomes more challenging. This will result in light touch remote support, with simple and often cost-free solutions that will have influence across the whole life of the employee.
More supportive options are commonly required when an employee has been off work for some time. However, it is still possible to provide a bespoke programme which supports a whole life approach to return to work but may take a little longer.
Other benefits can include enhanced productivity and performance at work; reduced absenteeism and staff turnover; improved morale and job satisfaction; improved energy levels and sleep and reduced fatigue; greater resilience and an understanding of what to look out for in colleagues and an opportunity for organisational and team culture to change.
Occupational Therapy makes all the difference to an employer whose employees are coping with fatigue, poor sleep, MSK problems, migraines, poor mental health, or cognitive difficulties such as brain fog or poor concentration. One professional for physical and mental health whose role is deeply rooted in occupation does sound like magic!
1. Mayne, M. (2003) People Management
2. Chartered Institute of Personnel and Development (CIPD)
3. ONS
4. The Health Foundation
5. Deloitte: Mental Health and Employers: The case for investmentpandemic and beyond; March 2022
6. The Workplace Health Report: 2024, Champion Health






2023 was an incredibly busy training calendar delivering weekly courses extending well beyond the usual Quarter 4 of the budget year into Quarter 3 of the following. My hypothesis is that employers are actively trying to address the evolving health & well-being needs of the post-COVID workforce.
The greatest challenge for me was balancing my desire to be accommodating & adaptable with the demands of a cross-generational cohort of school leavers and professionals who had to adapt to home-working at short notice and who have no desire to adapt back to a commute, let alone travel to the Midlands to attend training. Feedback was sparse, and the few with strong opinions about their learning experience were our only opportunity to reflect on and develop our offering.
A key difference was the expectation to attend my whole-day in-person participatory training remotely. I considered the request using a dynamic risk assessment, and decided upon 2
half-day sessions for each course to reduce the risks to trainers of vocal stress from ‘speaking into a void’ (Garcia-Real, 2024) and “technostress” (Wang, 2024) associated with co-ordinating breakout groups with variable internet speeds and monitor settings remotely. (Bonfim, 2024)
These reflections led me to some fundamental questions:
• Why did I feel exhausted rather than exhilarated at the end of each session?
• Why did I not feel inspired to research the ideas and insights contributed by delegates?
• Was I “burning the candle at both ends?
• Was I experiencing Garcia’s burnout?
• What was the purpose of teaching?
• Had I fallen out of love with teaching?
• Did I really want to teach this any more?
It was this final question that drove me to distraction; “I show people different ways to think. I don’t tell them how to recognise & follow a process”. My ensuing journey to understand and evaluate my values and philosophy led me straight to Freire. I could not believe that I had never heard of this brilliant Brazilian whose “pedagogy of the oppressed” (Freire, 1968) expressed exactly how I was feeling. He describes traditional pedagogy as a "banking model of education" treating learners as empty vessels to be filled with knowledge, like putting coins a piggy bank. His argument that learners should develop a “critical consciousness” (Freire, 1973) and be considered co-creators of knowledge, resonated with me – those of you who have been on my courses know that my introduction is usually something along the lines of “I always leave these courses feeling that I’ve learned more than I’ve taught”.
I realised that, although there appeared to be some healthy interaction and debate happening on screens behind mute buttons, the inability to move together in the same room reduced the delegates’ connections, questioning and the opportunity for peer- sharing and mentorship.
I did, however, discover a wealth of systematic reviews extolling the virtues of a shared learning approach to teaching for healthcare professionals. This was rather cleverly renamed “emancipatory pedagogy” by Cabey (2024) with the goal to “develop a workforce that is equipped to address patients’ social and structural determinants of health and to contribute to health equity”.


I show people different ways to think. I don’t tell them how to recognise & follow a process
In the ever-evolving landscape of education, educators seek approaches that not only disseminate knowledge but also foster critical thinking and empowerment among health professionals. Paulo Freire's pedagogy, rooted in the principles of critical pedagogy and dialogical learning, has proven to be a transformative force in various fields. When applied to health sciences education, Freire's approach goes beyond traditional methods, creating an environment that encourages active participation and holistic understanding.
Why am I committed to waiting till people are ready to go back to the classroom?
Freire emphases dialogue as a means of co-constructing knowledge. By engaging delegates in meaningful conversations, I feel that I can bridge the gap between theory and practice, allowing delegates to apply theoretical concepts to realworld health scenarios. This dynamic interaction fosters a deeper understanding of health issues and promotes a sense of ownership over one's learning.
In health sciences, where interdisciplinary collaboration is crucial, Freire's pedagogy facilitates the development of teamwork and communication skills. The dialogical nature of his approach encourages delegates to appreciate diverse perspectives, fostering a collaborative spirit that mirrors the interdisciplinary nature of the healthcare field.
Furthermore, Freire's focus on critical consciousness aligns with the evolving demands of healthcare professionals.
Health sciences delegates are not just memorizing facts; they are encouraged to question, analyse, and critically evaluate information. This critical mindset prepares future healthcare practitioners to adapt to emerging challenges, navigate ethical dilemmas, and contribute to continuous improvement in healthcare practices.
Freire's pedagogy also addresses the social determinants of health, urging delegates to explore the broader societal factors influencing health outcomes. By connecting health sciences education to social issues, delegates gain a more comprehensive understanding of the complexities surrounding healthcare, preparing them to advocate for health equity and contribute meaningfully to community well-being.
In summary, critical pedagogy is a powerful philosophy of education that:
Emphasises democracy and equality, insisting that teaching and learning are inherently political acts. Educators use this approach to create learning environments that prioritize democracy, equality, and social justice.
Authentic materials, generative themes, and teachable moments become the building blocks of transformative learning experiences.
Cultivates hope and symbolic resistance in the face of challenges, encouraging symbolic resistance empowering learners to question oppressive systems and envision alternative futures.
Addresses ideology and power by delving into ideology, hegemony, resistance, and power dynamics. By analysing these concepts, educators empower delegates to critically engage with knowledge construction and
societal norms.
Promotes social justice and aligns with social justice efforts. It equips learners with tools to combat racism, sexism, and oppression. Through dialogue and critical consciousness, delegates become advocates for change.
Connects education to real-world issues rather than treating education as neutral or objective, critical pedagogy links classroom learning to broader social issues. It encourages delegates to explore the intersections of knowledge and action.
Fosters Inter- and, more importantly for us, Multi-disciplinary Collaboration to prepare learners for interdisciplinary work. By appreciating diverse perspectives, delegates develop teamwork and communication skills essential in fields like healthcare.
In essence, critical pedagogy transcends traditional boundaries, inviting educators and learners to engage in transformative dialogue, challenge norms, and work toward a more just and equitable world.
In conclusion, Freire's pedagogy offers a transformative approach to teaching health sciences. By embracing dialogue, critical consciousness, and a holistic understanding of health, educators can empower delegates to become not just knowledgeable practitioners but also compassionate advocates for positive change in the healthcare landscape.
Through the lens of Freire's pedagogy, health sciences education becomes a dynamic and empowering journey towards a more equitable and enlightened healthcare future.
Bonfim, M.M.F., Ferreira, L.P., de Medeiros, A.M., Constantini, A.C. and Masson, M.L.V., 2024. Voice Disorder, Job Stress, and COVID-19 in Teachers: Impacts in Times of Pandemic. Revista de Investigación e Innovación en Ciencias de la Salud, 6(1), pp.8-23.
Freire, Paulo (1968). Pedagogy of the Oppressed. Translated by Ramos, Myra Bergman [1970]. New York: Herder and Herder.
Freire, Paulo (1992). Pedagogy of Hope: reliving pedagogy of the oppressed. (translated by Robert Barr, 1992 original version), London & New York, Bloomsbury Publishing
Freire, Paulo, ed. (1997). Mentoring the Mentor: A Critical Dialogue with Paulo Freire. Counterpoints: Studies in the Postmodern Theory of Education. Vol. 60. New York: Peter Lang.
García-Real, T.J., Díaz-Román, T.M. and Mendiri, P., 2024. Vocal Problems and Burnout Syndrome in Nonuniversity Teachers in Galicia, Spain. Folia Phoniatrica et Logopaedica, 76(1), pp.68-76.
Kilag, O.K.T., Malbas, M.H., Miñoza, J.R., Ledesma, M.M.R., Vestal, A.B.E. and Sasan, J.M.V., 2024. The Views of the Faculty on the Effectiveness of Teacher Education Programs in Developing Lifelong Learning Competence. European Journal of Higher Education and Academic Advancement, 1(2), pp.92-102.
Wang, Q., Zhao, G. and Yao, N., 2024. Understanding the Impact of Technostress on University Teachers’ Online Teaching During the COVID-19 Pandemic with the Transactional Theory of Stress (TTS). The Asia-Pacific Education Researcher, 33(1), pp.187-198


Lucy Kenyon is a Specialist OH Nurse Consultant and digital health entrepreneur. She is an Honorary Senior Lecturer at the University of Chester and has been teaching and mentoring in Occupational Health since 1996 for the RCN, Universities of Birmingham, Chester, Coventry, Derby and West of Scotland. She delivers professional development courses for the National Performance Advisory Group, Cordell Health and employers, for whom she researches and develops evidence-based practice. She has been a member of the iOH board since 2014, President from 2017 - 2020 and a NonExecutive Director since 2021. She has a Master of Medical Science and the International Certificate in Occupational Hygiene from Birmingham, where she has taught and worked on research projects.



Many organisations are now more aware of the contributors to better workplace health, business performance this brings? The answer lies in not only having wellbeing initiatives, engaging with them. This is an area that I believe offers Occupational Health (OH) a real
This article discusses some of the areas OH practitioners can help organisations to focus case.

health, but how can they achieve lasting employee wellbeing along with the improved initiatives, but in embedding them into the culture so that employees feel comfortable real opportunity to exert influence and create a healthier workplace.
focus on, improve and embed workplace wellbeing, starting with a compelling business
While there should never need to be a financial case for investing in better employee health and wellbeing, the question does get asked. Fortunately, there is a body of evidence to suggest that it brings tangible returns. OH can refer organisations to research from Deloitte in 2022 which found that employers see a return of £5.30 on average for every £1 invested in employee wellbeing. And the CIPD’s Health and Wellbeing at Work survey states that when organisations focus on their workplace wellbeing strategy, they experience better employee engagement, lower rates of sickness absence and an overall healthier and more inclusive culture.
Burnout, stress, anxiety, worries about job security and the continuing impact of the current cost of living crisis all have the potential to affect employee mental health. But while employers want to support better mental health, research by mental health charity MIND has found that 30% of employees don’t feel that they can talk openly with their line manager if they were feeling stressed. If employees don’t feel comfortable discussing their mental health, any help that OH may have in place risks low levels of take up. So how can OH support line managers to help their employees feel more comfortable in opening up?
To embed better mental health, organisations need to focus on making these sensitive conversations easier. Line managers have a big role to play
here with understanding and empathy, but a more supportive culture starts at the top. Leaders exert powerful influence when it comes to mental health issues. They can set the tone of the whole organisation by their actions so, the more OH can influence the normalisation of talking about mental health, the more likely others will feel comfortable doing the same.
If you’d like to read more about how to open up conversations around mental health, this article on the Cordell Health blog will help: Mental health in the workplace - how to get the conversation started.
As well as being a contributor to poor mental health, stress is another challenge for organisations as it’s often brushed off as ‘coming with the territory’ in a demanding role. But here’s why organisations need to take stress seriously. It’s a significant factor in mental health problems and can lead to anxiety and depression. It is also linked to physical health problems like heart disease, problems with our immune system, insomnia and digestive problems. Line managers may not be aware of this, but OH are.
Given that a certain amount of stress is inevitable, if OH can help organisations to develop the skills to cope with stress, build resilience and protect the health of remote workers, this in turn will help to reduce stress related illness.
Maintaining physical activity, assessing adequate home workstation setup for remote workers and being mindful of the need for good sleep and nutrition are all things that OH can influence.
Despite the challenging cost of living for many, financial wellbeing is still often the least common area in an employee wellbeing strategy. OH practitioners often see financial challenges as a contributor to poor mental health, stress and anxiety. What’s more, the CIPD estimate that one in eight workers are now facing financial hardship. It stands to reason that the financial challenges affecting employees outside of work will impact on them, and their performance, inside the workplace.
Employees are far more likely to feel that their employer is having a positive impact on their wellbeing when they have a financial wellbeing strategy in place. Such a strategy also plays a part in creating an attractive culture which has a positive impact on retention rates. But a financial wellbeing strategy won’t succeed without a culture of understanding and the ability for line managers to manage sensitive conversations.
If you’d like to read more about employee financial wellbeing including guidance on developing a strategy, this article on the Cordell Health blog will help: Employee Financial Wellbeingunderstanding the need for good financial health.
At Cordell Health we believe the promotion of good workplace health has a positive impact on the prevention of illness whether that be physical or mental. I am sure we are not alone in this proactive approach in our profession, but how can OH take the lead in promotion and prevention? One
way is to help organisations capture the data they need to be able to develop and deliver employee wellbeing programmes. For example, we’ve managed surveys and focus groups that have not only revealed valuable data, they’ve also left a positive impression with employees that their employer wants to invest in their wellbeing. This data can point towards the areas that need support. This could be in areas such as levels of emotional resilience and how employees feel about the organisation’s culture. For example, are they working with good psychological safety with the freedom to speak up without fear of punishment or humiliation? For anyone feeling stressed about an issue they feel they can’t raise, if the problem risks remaining hidden it can be highly stressful. Data can also point to more traditional interventions where OH can support organisations with awareness of better nutrition, smoking cessation and healthier lifestyles.
Workplace wellbeing also becomes more embedded in an organisation’s culture if awareness of the issues and how you communicate them are planned across the year. One of the things we’ve done at Cordell Health is to create an annual wellbeing calendar of all the main health awareness initiatives. Each month we help clients focus on two health and wellbeing issues that have an awareness day or week that month. We create resources to help clients understand the issues ranging from guides and podcasts for line managers and employees to workplace posters you can place around your building. This is
another example of how OH can be proactive with workplace health promotion which in turn creates a more health aware workplace.
I believe that OH can play a key role in how health and wellbeing are embedded in an organisations culture. Research and performance show that it’s well worth the effort with far-reaching benefits for the organisation, its employees, and even a healthier society as a whole. By helping to embed a culture of employee wellbeing, OH in turn helps to create a more resilient, engaged, and successful workforce capable of meeting the challenges of today's dynamic business landscape.


Dr Nikki Cordell is co-founder and CEO of Cordell Health. An experienced specialist occupational physician, she passionately believes in improving the health of workers, pursuing excellence and bringing innovation to the way that health and wellbeing is delivered in the workplace.


Managers have become more important than ever for work doesn’t make people sick. However, according Health and Wellbeing report from the CIPD, some managers, unfortunately, have a negative impact on employee wellbeing. the single most important thing employers can do to boost the their workforce in 2024 is to equip managers with the skills, support competency to manage wellbeing.
This article reviews the impact that managers have on employee and the role of managers when it comes to creating a culture of This is followed by a discussion of a framework that has been developed upskill managers, including tools for the wellbeing toolbox which implemented inclusively within the workforce.

work, what
ensuring to the 2023 managers, This means the health of support and employee wellbeing of wellbeing.
developed to which can be

The impact that managers have on employees’ wellbeing (PAM Group Health at Work report 2021)
Employees want help to stay healthy and believe their employer, and their line manager, is responsible for their health and wellbeing (PAM Group, 2021 Figure 1). A lot of this is driven by the fact that over half of all employees have been affected by delays in accessing support with the NHS. This puts the
onus on employers to take a more proactive approach to health and wellbeing, helping employees avoid becoming sick in the first place. This is a huge task, but, with the right tools, skills and framework, managers can support wellbeing.

One of the key barriers for managers supporting their employee's health and wellbeing, is how comfortable employees feel in discussing these issues (Figure 2). The report by PAM Group in 2021, portrayed that two-thirds (68%) of employees don’t feel comfortable discussing workload and deadline challenges with their line manager; three out of five (61%) people feel able to discuss equality and inclusion with their manager, but just one in two employees (53%) are comfortable discussing mental health or childcare challenges. A similar number of employees feel uncomfortable discussing social health challenges, relationship challenges and neurodiversity challenges, such as dyslexia or autism (PAM Group, 2021). Lastly, it’s no surprise that financial worries emerged as the topic that most people feel uncomfortable discussing.
To address this, we need to create a psychologically safe culture. This means creating a psychologically safe workplace, where people feel like they won’t be rejected, punished or embarrassed for speaking up. An essential ingredient to creating a culture of health. This can be achieved by giving managers the appropriate communication skills to have the confidence to open conversations about loneliness and relationships. Truly knowing their team so that managers are aware and mindful of the challenges that different sex and age groups will experience. For example, research shows that women are less likely to feel comfortable discussing relationships, whilst workers over the age of 55 are less likely to feel comfortable discussing personal wellbeing issues across the board (PAM Group, 2021).

Managers play a role in knowing what wellbeing tools are already available and making employees aware of these benefits. There are valuable opportunities in using healthcare tools and benefits in a more proactive approach, rather than being portrayed as something managers should use as a last resort.

The PAM Group (2021) report survey, (Figure 3) shows the uptake of benefits, from flexible working to private GP access, DSE assessments and wellbeing webinars. Flexible working, paid-for optical or dental care and mental health counselling services are the top three wellbeing benefits for around half the workforce. This is closely followed by access to a private GP, health screening and blood tests, private health insurance and occupational health services. Organised sport/walking/ cycling groups and wellbeing webinars emerged as the least popular benefits, although over a third of employees still valued this form of support. This shows the importance of offering a wide range of benefits to meet everyone’s needs and to be inclusive.
Critical to turning this around is proactively promoting health and wellbeing benefits as tools for wellness, rather than sickness. For example, by encouraging people to get physiotherapy advice when they change their working environment, or at the first sign of a twinge, rather than waiting until their back hurts them too much to work.
• Make sure employees know the support is to help them stay healthy, not just if they get sick.
• Work with benefits providers who are willing and able to proactively promote services to employees.
• Reassure people that sensitive services, such as debt or emotional counselling, are fully confidential.

Burnout is a key outcome when workplaces aren’t proactive in wellbeing support. Individuals become emotionally exhausted, cynical, and disengaged from the job and feel a sense of ineffectiveness and loss of purpose. Retaining and recruiting people is difficult as
has been the experience of the NHS where there are significant levels of burnout. But there isn’t a one-size-fits-all approach; for example, in healthcare compassion fatigue is a known phenomenon that you may not get in other industries.
Primary intervention is essential, i.e. looking at the root cause for that organisation. Compounding elements (Figure 4) could be:
• Workload, shift patterns, autonomy, and leadership: Are there high demands and intensity; long hours with few breaks; short staffing; lack of control; poor management and poorly managed change?
• Support and working relationships: i.e. low support from managers; bullying and victimisation; lack of appreciation and respect; stigmatization of those who seek help.
• Training and development: i.e. lack of opportunities for development and inadequate training.
• Work-home interface: work-life conflict; long shifts; little time for recovery.
• The individual: existing mental health problems; poor self-care; overcommitment; low resilience, caring responsibilities.
• Inequalities: Although many organisations are ethnically diverse, ethnic minority staff are at greater risk of bullying and abuse which has implications for mental wellbeing.
Case Study: Paul was sent to work from home during COVID. After a few months, he started to perform below his usual standard and complaints arose. (He was in a customer service role). During the OH consultation, it emerged, that he was isolated at home with no one to speak to, he had had several managers, and poor communication meant he wasn’t sure what the latest process was and became confused. This gentleman had been a high achiever and performer previously and was found to have lost confidence, lost interest and was extremely fatigued.
A wellbeing framework (Figure :
Organizational health is a continuous cycle, everything interacts. But if we had to have a starting place it would be with business awareness and building the business case, which requires stakeholder engagement. Often businesses put effort into ESG (Environment, Social and Governance), focusing efforts externally. However, the S i.e. social in ESG applies as much to employee wellbeing as it does to community wellbeing (Personnel Today, 2023). Supporting the internal community will influence the external community which is the moral perspective for business awareness. Then there is the business perspective which includes maximising
productivity, cost savings, and efficiency. If an organisation focuses on the moral and the business perspective, the business case almost writes itself.
Engaging stakeholders is crucial for a culture of wellbeing. But this needs to be top-down and bottom-up. Although the top can influence wellbeing with decent work practices and encouraging a culture of awareness, the top cannot dictate wellbeing, there must be buy-in.
The strategy comes from the bottom-up approach. Having a voice and being involved helps to contextualize solutions, making them appropriate for the organisation. This includes
the tasks, people, risks, and concerns relating to that business, not that of the competition and therefore running the risk of being tokenistic. Involving the people of the business in planning and problem-solving.
Aligning and integrating with existing systems and ways of working helps to make initiatives easier to accommodate, improve or elevate as opposed to complete change. An example in PAM is our triage process; - we brought together a working group top, bottom, and middle within a certain team to look at making this more effective. This made a significant difference not only to the process but to the engagement of the team and retention.
Utilising expertise in health, especially workplace health, provides credibility, and ensures there is a multifocal view and delivers objective advice. Programs that look at an
organisation's particular risks from a physical perspective and psychosocial perspective, health trends in the socioeconomic environment plus the community employees come from, can provide insights that may be difficult for organisations to do on their own. Occupational Health (OH) is a strategic health partner.
However, no wellbeing interventions will be effective, OH input or not, without collecting data as evidence. Data can be both quantitative i.e. surveys and statistics that come out of e.g. OH, wellbeing and EAP (Employee Assistance Program) services and data from conversations i.e. qualitative discussions with employees. This then feeds into business awareness and stakeholder engagement.

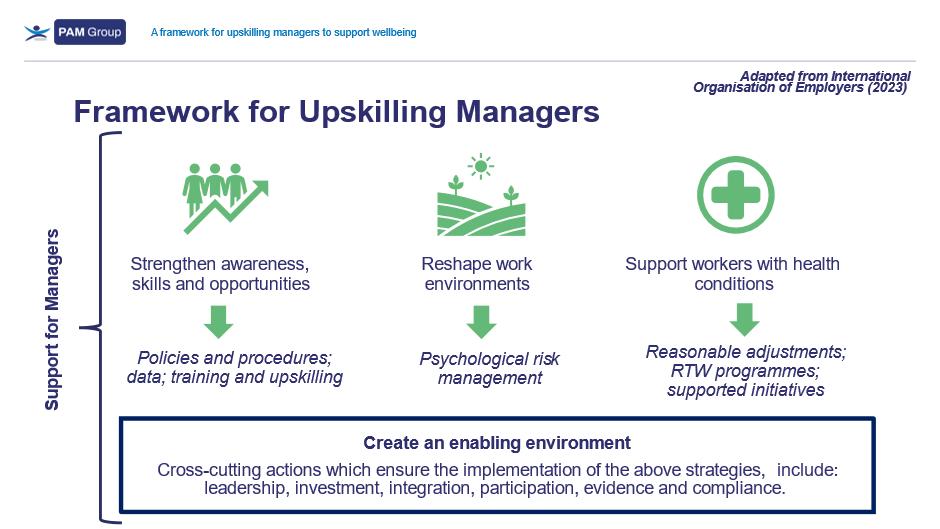
Line managers are fundamental to making a wellbeing strategy work (Forbes 2020). They are the most important person in an individual’s working life and keep the organisation on track with performance. A lynchpin as described by Forbes. Figure 5 is a useful starting point when building a line manager competencies framework, a strategic tool in supporting line managers to optimise mental health and wellness. Managers are commonly striving to get the task done and if competencies aren’t developed, they, as fallible human beings, may judge or label those with an invisible disability. Nonetheless, they can’t do this on their own. They need the support of the organisation, i.e. a top-down approach.
There are tools to support reshaping the environment with a risk approach such ISO 45003 and HSE management standards. A
whole organisation approach ensures a wellbeing approach to organisational culture looks at the type of work and how it is carried out, the make-up of the workforce, the social environment they live in and the tasks they are required to do e.g. a patient-facing environment will be different to a rail or firefighting or logistic or manufacturing or service industry. Reducing physical and mental health risks is an essential part of line manager competencies. It isn’t much use if a manager can have a good conversation but doesn’t protect their team member from ill health or places pressure on them to take risks. No manager will enact good wellbeing strategies if they
• Don’t look after their own wellbeing and set an example.
• Don’t understand the rationale.
Case Study: During COVID, M&S supported 1200 managers to complete “Mental health conversations” training and found colleagues and managers were more confident to talk about how they were feeling, creating a culture where employees could ask for help.
Therefore, organisations need to provide managers with reputable training based on evidence. This needs to include a foundation knowledge of health and safety including mental health awareness, stress management, and the impact of work on overall health. WHO (2022) researchers found evidence that suggests training managers on spotting the signs of reduced mental health, along with support routes, helps to increase their confidence and improve attitudes around mental health within the workplace. PAM Group have a free recorded webinar: Courageous Conversations for Managers
For example
• Workplace needs assessment.
• Line manager competencies
• Engagement/pulse surveys.
• Communication skills.
Managers need upskilling to support equality and inclusivity. Making sure an individual has everything they need to reach the same level of success as someone who may not need accommodations takes time and far more thought than a one-size-fits-all approach. The results are more effective and enable psychological safety, reducing the risk of work exacerbating health. (TED talk Hidden Disabilities, 2024).

• Signposting resources e.g. EAP, physiotherapy, mental health support, CAB, etc.
• WRAP plans.
• Stress risk assessments
• Policies and procedures with HR support (CIPD).
• Return to work interviews.
• Educational sessions.
• Encourage reward, recognition and a growth mindset.
Internal Data:
• Wellbeing dashboards such as Workday or Darwin
• Engagement survey data
• Employee representation groups
• Exit interviews.
External Data:
• Local socio-economic health data.
• Wellbeing data including EAP (Employee Assistance Program); OH; MSK services; health education and promotion.
• Consider the need to utilise people with the skills to collect and interpret data or technology to automate data collection and analysis.

• Create a top-down and bottom-up culture of psychological safety
• Enable and empower managers and colleagues to thrive
• Consider the individual but also the collective within the environment particular to that organisation
• Evaluate policies and procedures to support line management and colleagues.
• Review what is in the toolkit and upskill line managers for effective conversations
• Review data continually to inform and develop
• Create inclusive initiatives that are accessible to all





Laura Jordan is Commercial Director of PAM Wellness and a physiologist with many years of experience in the world of Occupational Health and Wellbeing.

GP surgeries are under pressure, so why can't the occupational health profession alleviate some of the workload and refer patients to NHS specialist services? Rosalyn Jones explains why this would be helpful to all involved.
Aquestion has been bugging me: why can’t occupational health practitioners refer to specialist departments in the NHS?
I have asked this question many times, particularly since the Covid-19 pandemic and in light of the problems many employees have obtaining a GP appointment or report.
The answer seems to be because most occupational health services are not associated with the NHS. It is not bias – it's just how things have always been.
I recently spoke to a secretary at the local NHS hospital, and she concurred what I am always told: the individual can only be referred by their own GP. So why is there so much difficulty, or reticence, to approach their GP?
I am often told that it takes a huge amount of time just to make that initial contact with a GP surgery. Many patients must call at 8:00am just to get through to the receptionist, and then they will have to wait for a call back to be offered an appointment in-person or over the phone. Sometimes the process can take hours, which is difficult for most working adults to fit into their busy schedules.
I have been told by employees in manufacturing, construction, teaching and nursing that they simply cannot telephone their GP in the morning because of their work commitments. Many employees in these roles are unable to use their mobile phones in the workplace, and permission is often required before they can have their phone with them.
These barriers to obtaining an appointment and being able to attend one when it is offered, can put individuals off approaching their GP. I worry about the consequences of this.
The NMC code of practice states that nurses must put the interests of people using or needing nursing or midwifery services first; must make
their care and safety their main concern; must make sure that their dignity is preserved; and must ensure their needs are recognised, assessed and responded to.
The areas of the code that I feel apply to the issue of NHS referrals are: “work co-operatively”, “recognise and work within the limits of your competence” and “act without delay if you believe that there is a risk to patient safety or public protection”. Surely by not allowing OH nurses to refer employees directly to the NHS, we're not upholding these parts of the code?
Yes, we can write to the individual's GP, and I suppose this has covered our duty to prioritise the needs of the person before us, but the frustrating part is whether this is followed up and the length of time it takes to have any diagnosis or treatment.
Many individuals are reporting that their appointments, surgeries have been cancelled, and not just the once. This then has an impact at work – time off, financial implications, anxiety and stress.
Another worrying area is the length of time it is taking a medical report to be sent back to OH from the individual's GP. I have experienced a couple of medical practices who are prioritising NHS work first. Again, because our OH service is not NHSdriven, some are delaying the issuing of these reports. This could be detrimental to the individual if there are any health or underlying issues to be navigated in the workplace.
The General Medical Council's ethical guidance on disclosing information for employment, insurance, and similar purposes details how a doctor should respond to such requests; it does not say concentrate on NHS work first.
Another issue is extensive waiting lists for NHS treatment. Some individuals have advised me that they will have to wait as long as 12 months for a hip replacement, or 35 weeks for a non-urgent neurological appointment. This length of time
beggars' belief and leaves me questioning why this area of medicine is treated as non-urgent.
If the individual is being referred to a specialist and the referral form needs to be triaged, I would like to know why only an NHS GP is allowed to do this? Why is a competent, qualified medical person like an OH nurse not allowed to complete a referral form?
Allowing OH professionals to refer individuals to the NHS would provide a quicker and more efficient solution than the current situation, where the employee must leave their OH consultation, get an appointment with their GP – which may take weeks – and then wait to be referred – may take months. This would require a robust referral process, taking into account that occupational health is not and does not have the same responsibilities as a GP/ medical practice.
It appears the situation has worsened since the Covid-19 pandemic, and a recent news article on the BBC put the issue into the spotlight: a patient saw eight GPs before his cancer was spotted. This article mentions a patient safety watchdog, the Health Services Safety Investigations Body, which was recently launched and will be investigating NHS care in GP practices and the independent health care sector.


Of course, workloads and staffing shortages in GP surgeries could be driving the delays. A recent Royal College of General Practitioners report set out recommendations for the government to tackle the crisis and support GPs and their teams to meet the healthcare challenges of the 21st century. The recommendations included the development of a properly funded plan to enable general practice to respond to surges in demand; greater investment in IT systems; rolling out new, properly funded GP retention schemes; and slashing unnecessary box-ticking requirements and workload so that GPs can focus on patient care.
OH professionals have huge expertise, and could be utilised as a pathway for signposting or referring patients for NHS care. Like doctors and nurses employed by the NHS, we are all qualified medical professionals following the NMC and GMC codes of conduct.
This is not a criticism of the dedicated staff in the NHS who work very hard to help patients; this is just an offer of potential help and a reflection of the issues faced by a hard-working OH professional.

Rosalyn Jones has worked as an independent OH Nurse since 1996 in the NHS, private and public sectors. She is a keen menopause and breast cancer advocate.

Spirometry is the most widely performed lung function test worldwide and can help to identify and monitor those who have a respiratory condition. As the role of the spirometer is examining an individual’s health, it is essential to ensure it is working accurately over a long period of time. Regular care and maintenance for your Vitalograph VCore spirometer will help to ensure the device can be used reliably for many years. As such, it is a worthwhile investment to regularly spend time maintaining your spirometer.

Spirometer care can be broken down into 4 simple steps:
• Understanding your spirometer
• Quality Assurance
• Cleaning and Hygiene
• Planned Preventative Maintenance
When a new spirometer is purchased, it is useful to have a thorough read of the device Instructions for Use (IFU). This document contains the necessary information to ensure it is used optimally. The IFU also contains information about registering the spirometer for an extended five year warranty. The IFU for your V-Core spirometer can be found on the corresponding device page on the Vitalograph website
As well as learning about the spirometer through reading the IFU, there are free online training modules available for the following Vitalograph V-Core spirometers:
• Alpha
• Pneumotrac
• Pneumotrac RMS
• Micro
To enroll in the relevant spirometry training, you should visit the Device Training page on the Vitalograph website. If a face to face training session for how to use your spirometer is preferred, a Vitalograph clinical trainer can attend your site to deliver a 2 hour training session specific to your spirometer. For further information about face to face spirometer training, please complete the form on the Live Training page on the Vitalograph website.
Prior to using your spirometer, it is good practice for the first step to be a quick visual inspection of the device. This includes ensuring all the parts are fitted together correctly, and ensuring there is
no damage to the spirometer. Once this initial visual check is complete, you can perform the daily calibration verification.
According to the ATS/ERS 2019 Spirometry standards1, calibration verifications must be undertaken daily for all spirometers. This includes precalibrated spirometers. Calibration verification is a procedure to ensure that the measurements the spirometer makes are accurate and reliable. Once the calibration verification option is selected on the device, a 3 litre syringe is attached, and air is pumped through at low, medium and high flow rates (between 0.5 – 12 L/s). Performing the verification at different flow rates helps to ensure your spirometer is measuring accurately over the entire physiological range. The measured volume at each flow rate must meet the accuracy requirement of ±3% for both inspiratory and expiratory flows.
The range of Vitalograph V-Core spirometers features quick and easy calibration verification routines, as recommended by 2019 ATS/ERS spirometry guidelines.
If the calibration verification fails, please follow the troubleshooting guide which can be found on the device IFU on the corresponding device page on the Vitalograph website
One common mistake when performing the calibration verification is not using the full range of the syringe handle, therefore not delivering 3 litres of air to the device. It is vital to push the syringe handle the full way in and pull it the full way out, this will ensure you are delivering the full 3 litres of air to the spirometer.

Spirometer accuracy can also be checked with a biological control. In this case, the healthcare professional or operator (who can perform highly reproducible spirometry) should know their own FEV1 and FVC. This individual can quickly perform a test on their spirometer if they suspect there is a problem with the device to assess whether it is working properly. It is important to note that this should not replace syringe verification, but it can be a useful addition to departmental quality assurance protocols.
The use of a new Bacterial Viral Filter (BVF) for every patient provides significant protection for the patient, the device, and the healthcare professional against the risk of cross contamination. Using BVFs also prevents the need to decontaminate the inside of the VCore flowhead as the mesh will stop exhaled droplets from reaching the Fleisch element. The BVF prevents any damage that a build-up of droplets or residue may cause, therefore ensuring your spirometer can be used reliably for longer.

Following each patient test, it is recommended that the outer surface of the spirometer and tubing is cleaned with a 70% isopropyl alcohol wipe. If contamination of the flowhead is suspected, instructions for a higher level of decontamination of your spirometer can be found here.
ATS/ERS 2019 Spirometry Standards1 state that spirometers should undergo routine maintenance at intervals specified by the manufacturer. All Vcore spirometers should undergo a planned preventative maintenance (a “service”) annually by a Vitalograph service technician. During the annual service, certain parts of the spirometer are replaced, and it receives a detailed check to ensure it is in full working order. This includes having its flowhead
and tubing replaced, an updated calibration, accuracy, and function check and thorough clean and disinfection. The annual service helps to ensure the spirometer is in optimal working order and helps to prolong the lifespan of the device.
For more information on training, or maintaining Vitalograph V-Core devices, please contact us on 01280 827110 or sales@vitalograph.co.uk Reference list
1. Graham, B.L. et al. (2019)
'Standardization of Spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement,' American Journal of Respiratory and Critical Care Medicine, 200(8), pp. e70–e88. https:// doi.org/10.1164/rccm.201908-1590st.




Vacancy
Occupational Health Manager
Salary: £48,474 – 51,575 plus £3K market supplement and relocation allowance
Location: Bradford / Hybrid Working
Contract: Full-time / Permanent
Employer: City of Bradford Metropolitan District Council
Closing date: Midnight Sunday 10 March 2024
Find out more and apply: https://nyresourcing.co.uk/bradford-counciloccupational-health-consultants/


Vacancy
Occupational Health Advisor
Salary: £35,745 - £43,421 plus relocation allowance
Location: Bradford / Hybrid Working
Contract: Full-time / Permanent
Employer: City of Bradford Metropolitan District Council
Closing date: Midnight Sunday 10 March 2024
Find out more and apply: https://nyresourcing.co.uk/bradford-counciloccupational-health-consultants/

The professional and educational body for occupational medicine in the UK, the Faculty of Occupational Medicine, has announced that Dr Robin Cordell will be their next President. Dr Cordell will take over from current President, Professor Steve Nimmo, in September.
The President is the Faculty’s chief ambassador and public spokesperson, working closely with other medical and allied health professional leaders, organisations and stakeholders.
Commenting on his appointment as President Elect, Dr Cordell said:
"I feel privileged to be asked to represent the Faculty later this year in what continues to be a time of some challenge and significant opportunity for our specialty, and the real potential for enhancing health and work nationally. I will seek to continue the momentum built by Steve Nimmo and his work with the other colleagues who have been engaged at a senior level in Government and the NHS, as well as work to build the occupational health workforce. In my view the Faculty is central not only to increasing capacity, but also to making a critical contribution to assurance of the quality of services required to meet this need. I see an inclusive and collegiate approach as essential, including building on the DipOccMed workforce, and the new DipOHPrac, and working with the full breadth of those engaged in health and work.”
Dr Cordell brings a wealth of experience to the role. He is in daily practice as an occupational physician and Chair of a social enterprise delivering occupational health services and providing specialty training, with five GMCapproved posts, and supporting doctors progressing towards CESR. He has held senior medical leadership roles in Defence, been a past President of SOM, and is a director of the Council for Work and Health. He is an examiner for the faculty diploma and membership exams and led on the recent SEQOHS Standards Review for the Faculty.
As President Elect, Dr Cordell will work with the current President to ensure a smooth handover of presidential responsibilities when Professor Steve Nimmo leaves office in September 2024.
In the 2023 Spring Budget, the Chancellor announced a £2billion package to support disabled people and people with health conditions to start, stay and succeed in work. This included two OH consultations: Tax Incentives for Occupational Health, and the other by Occupational Health: Working Better, which sought views on ways of increasing employer uptake of occupational health.
Professor Dame Carol Black, an experienced health policy advisor, will lead a new taskforce to improve employer awareness of the benefits of occupational health in the workplace. The taskforce will be part of the government’s initiatives to tackle in-work sicknesses and help the economy.
It is proposed that a voluntary occupational health framework for businesses will be developed which will include specifying minimum levels of occupational health and help businesses support workers returning to work after ill-health.
Only 28% of employers in Britain provide occupational health in some form, with large employers (89%) three times more likely than SMEs (28%) to do so.
This framework which is expected this Summer will form part of the Government’s drive to reduce inactivity levels and waiting list times.
The Taskforce comes as the Government pilot of a new WorkWell service commences, which is aimed at helping 60,000 people with health conditions remain and succeed in work through health support and integrated employment.
Several OH professionals have provided information to the health and care section within the Policy Exchange think tank. They are preparing a paper on the role employers can play in supporting employee health and the future of occupational health. The report will be broad and will include national strategy, delivery models of OH and incentives for employers with recommendations. This report is one to watch out for.
The National School of Occupational Health (NSOH) has completed the 2023 to 2024 round of funding for nurse and Doctor OH qualifications. There has been a good uptake of funding and, anecdotally, the school is informed that 2023 intake was the first with no self-funded students within SCPHN (Specialist Community Public Health Nursing) courses. Funding for exams of those who were successful will continue through the 2024 to 2025 financial year. Further funding is being looked at for 2024 and 2025 and further information will be available on the website in due course
The Universities delivering SCPHN-OH courses are going through the new NMC standards of accreditation that will require them to deliver at MSc level. Those currently delivering these courses are considering providing them as an apprenticeship. New courses will be coming on board, e.g. Bolton and Manchester Universities are working on delivering, and the University of Western Scotland (UWE) are revising their qualification.
Glasgow University have joined the group of providers delivering the DipOccMed for Doctors. Newcastle and Healthwork Ltd deliver their course to doctors, nurses and AHPs jointly. TOPHS delivers their DipOccPrac course to nurses and AHPs. More information can be found on the FOM website.
Do not forget to view our OH Today special education edition (members only). For OH educators, we have an unrestricted access page on our website for you to provide information on your course Educational ProvidersiOH - The Association of Occupational Health and Wellbeing Professionals. Please contact us at admin@ioh.org.uk if you wish to showcase your course.
The Equality and Human Rights Commission have published this guidance. Menopause in the workplace: Guidance for employers | EHRC (equalityhumanrights.com). The guidance provides statistics on how menopause affects women at work and focuses on the legal requirements for employers i.e., the Equality Act. Focusing on age, gender and disability, they outline the risks of failing to make adjustments and discrimination within the workplace.
More, in the guidance, could have been made of what reasonable means to an employer when it comes to adjustments. Highlighting clinical treatment and lifestyle management support for individuals with symptoms and an improved quality of life would have been helpful. It does come across as if work is the deciding factor and the onus on managing menopause is solely on the employer. However, their video guide on conversations around menopause is helpful. It is interesting to note that there is no mention of Occupational Health in the guidance.
It is 50 years since the HSAW Act came into play. Last year Angela Whitehead, non-executive director, and trustee of iOH, produced a blog, A window into OH of the past, describing OH nursing at the time the Act was published. A fascinating read.
HSM in their article on this topic, feel that the legislation is unlikely to change in 2024, however, the focus of the HSE, will be on mental health, musculoskeletal health, and occupational lung diseases. NFP predict the focus will also be on mental health, manual handling and musculoskeletal disorders, as well as hybrid working.
National Living Wage increase for those employing people on minimum wage will be effective from 1st April 2024 and will increase to at least £11 an hour for workers aged 23 years old and over.
Pension (Extension of Automatic Enrolment) Act 2023 Amendments – The minimum age for automatic enrolment will be lowered from 22 years old to 18 years old and there will be no minimum earnings threshold.
Employment Relations (Flexible Working) Act Changes – In the summer of 2024 employees will be able to submit two flexible working requests in any 12-month period and employers must respond within 2 months.
Eligibility will be from day one of employment.
Carer’s Leave Act – This will guarantee eligible employees, the statutory right to take one week’s unpaid leave per year to care for a dependent from the start of their employment. This could be enacted as early as April 2024.
Neonatal Care (Leave and Pay) Act – Under this legislation, employees who are parents of babies requiring neonatal care will be entitled to 12 weeks of paid leave, if employed for a minimum of 26 weeks prior to the leave being requested, and an average earning of at least £123 a week.
Protection from Redundancy (Pregnancy and Family Leave) Act – Due in April 2024, this will extend the protection for pregnant women and new parents from redundancy. It will now provide protection from the end of their maternity or adoption leave to six months after their return to work.
