Black Women

EPR and


Make to





Make to

As numerous commentators are fond of saying, however, ‘we are where we are’. I do wonder whether the Prime Minister and Chancellor of the Exchequer ruminate the same phrase whilst reading the cereal packet first thing of a morning. Simply saying ‘we are where we are’ has become a sort of shorthand for venturing the idea that we should forget what has caused a situation and simply get on with planning a move forward. I doubt that the electorate will be quite so minded in 2024.
Right now, for any of us working in health and social care, the financial anxieties gripping our workforce are many and very serious. Whatever the size of your organisation, from small domiciliary care specialist to large general hospital, you can be certain of the following:-
Some of your staff will be very worried about being able to afford to pay a mortgage or rent.
Some of your staff will be very worried about being able to afford heating bills. Some of your staff will be very worried about being able to afford to travel to work.
I can’t recall a recent time when the mood of the country and its people was
We are clearly living through tumultuous times. Nobody reading this is immune from the economic fallout caused by a combination of factors, many external to our nation, but too many self-imposed.

so riddled with financial anxiety across the lower and middle pay bracket. Perhaps my most recent experience was the late 1980s and early 1990s as Britain suffered high interest rates and inflation and the end of participation in the European Exchange Rate Mechanism. Whatever the recollection, however, it doesn’t alter the effect that those times had.
How to address this with your people therefore?
First, I’d suggest making it easy for them to come forward and discuss anxieties or difficulties with you. Assuming that you have at least a weekly meeting, use that opportunity to say something like “it is clear that the economic and financial situation at present is difficult. If any of you are experiencing problems linked with the current situation, please let me know and I’d be very happy to talk to you about how I/we might help.”
Second, gather every resource that you can together and create a support hub within your organisation or department. This might include, for example, information about how to access citizens advice, housing association, debt counsellors, legal aid, mental

health charities, energy companies and more. Bring it all together in one place and make someone (even yourself) responsible for keeping information up to date and comprehensive. Help your people to understand that they are understood and supported. If you can, set the support hub up in a room where people can meet to discuss or access the resources. As part of this, provide a PC with internet access so that people can access online support too.
Third, where you have members of staff in clear difficulty, do the right thing. Find a way, however small, to help. Be on the right side of history when, at a future date, we can all reflect on what happened and who turned to support rather than turned away. By a good and empathetic listener in the knowledge that simply doing that is an effective first step for many.
This is a horrible time but if my life has taught me anything it is that dark clouds do eventually clear away and brighter times are on everybody’s horizon if they can be helped to get there. Be that help.
Stay safe, stay strong and thank you for the brilliant work you are all doing.
As we know, Covid-19 inspired the speedy take-up of a range of efficiency-focused delivery approaches.
Judith Shaw, Managing Director, Liaison Workforce


As we know, Covid-19 inspired the speedy take-up of a range of efficiencyfocused delivery approaches. Whilst patient initiated follow-up (PIFU) was not a new approach to outpatient care, its take-up was a positive change for increasing choice and flexibility for patients accessing outpatient services.
PIFU empowers patients to take control of their own care. It ensures they can see a specialist sooner than planned if they need to, as well as avoid an unnecessary trip to hospital if they have no need to be seen. It also helps clinicians manage their waiting lists in a safe and effective way, meaning fewer appointments of low clinical value, freeing up time to support the patients most in need.
Allowing patients to choose when they are followed up with is doing the right thing for patients and, at the same time, is helping trusts to reduce their waiting lists and get more patients seen. Clinical task management also enables trusts to better manage their workforce as they can see the skills and experience needed to undertake tasks. It enables workforce redesign, promotes multidisciplinary team working, and boosts morale, leading to better rostering.
Sir Jim Mackey also recently recommended the “industrial rollout” of PIFU in the HSJ, stating: “There still is a lot to work through [on virtual outpatients], we’re going to be testing the concept… We need to work through how all the wiring and plumbing needs to work. For example, what happens if the patient needs a diagnostic locally, having seen a clinician virtually in another part of the country?
“It would be great also to try and stimulate more of a consumer drive on this – encouraging patients to ask about virtual outpatients when the waits locally may be too long, so they don’t just think they have to go to their local hospital. I think this could really help shift the model if we can get it right.”
He also refreshed his calls for patient initiated follow ups (PIFU) to be rolled out on an industrial scale.
Sir Jim said: “I do believe strongly that we really need to have a go at inverting the outpatient model, and for trusts to have a go at doing their version of what Norfolk and Norwich are doing.”
Norfolk and Norwich University Hospitals Foundation Trust is currently overseeing the NHS’s most ambitious PIFU programme, with Liaison Group partners, Infinity Health, providing the task management platform to the project. In this programme, which we’ll be discussing in an upcoming webinar, the Trust has categorised around half of its outpatient follow-up list as “possible or probable opportunities” for patient-initiated pathways.
The implementation of PIFU should be encouraged – it ticks all the boxes; what is right for patients in today’s age, for staff, and for the long-term sustainability of outpatient services.
If you’d like to discuss how Liaison Workforce can support your PIFU solution, please get in touch at info@liaisongroup.com

BWIC is a Community Interest organization founded in 2020, born out of the founder’s 15-year experience in the Health and Social Care sector. BWIC Founder Olayinka Thomas started her Career as a Care Assistant. She rose to become a Registered Manager after many years of experience, now a Social Care Consultant and a renowned Trainer.
Having seen and experienced first-hand cases of discrimination and workplace equality but rising through them with a skill set, Olayinka founded the BWIC Community Platform to support Black women and other minority ethnic groups that work in Health & Social Care sector. Alongside other seasoned care industry experts, Olayinka believes that the well-
being of the BWIC community group has utmost priority on Personal and Professional development. Similarly, it was profoundly prompted by the George Floyd protests for the Black Lives Matter movement that started in the US in March 2020.
At BWIC, we support women working within the health and social care sector-Nurses, Care Assistants, Social care Managers, to mention a few, we support and encourage our members to rise into senior and managerial roles and promote inclusivity, and well-being within the workplace through various needbased, well-tailored projects.

The health and social care sector, in general, depends heavily on migrant workers, and with the current changes to immigration policy, a further rise is imminent.
Recent findings show that 12% of the UK population are of Black/African/ Caribbean/Black British backgrounds and account for over 50% of the Black and other Minority Ethnicity (BAME) adult social care workforce.
Another report discloses that women perform over 85 percent of the direct care jobs in adult social care. It is evident that BAME, particularly black women make up a large part of the workforce in this sector.
Our monthly empowerment series project, BWIC Careers’ Forum has reached over 2000 BAME women. You can register for a free account at https://blackwomenincare.com/ membership/ to become a BWIC member
Similarly, our annual Awards recognize passionate health and social care workers, and in 2021, the premier Black Women in Care (BWIC) Awards and Summit had an enormous impact as veteran carers from African/Caribbean backgrounds who have never received such recognition in their care careers were awarded duly, here are some awardees' feedback
Adebimpe, Business Development Associate, Black Women in Care (BWIC)The BWIC Skip for Carers event will hold between the 1st and 10th of October 2022, kindly find attached the event flyer, it seeks to encourage people to skip/or walk-in carers’ shoes by taking 2000 steps or doing 100 - 200 skips daily for 10 days while supporting carers to raise funds for offsetting their bills amidst the ongoing costing of living crisis. More information on the event and donation is at: https://www. justgiving.com/crowdfunding/black-women-in-care?utm_ term=96dAK3qjG
We would equally be pleased if this is shared within your network for participation.
The 2022 Awards and Summit will take place on 26th of November 2022 and we are currently receiving nominees at https://docs.google.com/forms/d/e/1FAIpQLScOWL uRHw67O8FuJs1cHDuw889W0TSRgHVZKF6BcIUGl0Fz uA/viewform?usp=sf_link or https://blackwomenincare. com/events/nominate-here/ we would be delighted if this is shared with health and social care managers in your network, Private and Public, to nominate their outstanding colleagues.

Please note that the nominations will close on Friday, 30th of September 2022.
We hope to share insights into specific ways and best practices for Nurses, Care Workers, & Care managers to support and manage their BAME staff as well as sensitize the UK community in general on workplace equality and diversity.
We will continue to share insights into black women as they relate to the health and care sector.
Thanks for reading and do let us know if you have any questions at info@blackwomenincare.com or call us on 03301749695
operational needs and
Support your with Cerner
Use data to inform your care, predict outcomes and improve the health of your population.
Managers, clinicians and health authorities around the world benefit from our value-driven, community-wide approach. Discover how we could help you by visiting our population health management page.
How much time do you spend at work? It has been estimated on average that, depending on their job role, a person may potentially spend over 84000 hours at work during their lifetime, based on a 35 hours a week work pattern.
This is why it is essential to promote well-being in the work place. As I have worked over 25 years for NHS will discuss the improvements.
What is the beating heart of any organisation? - The staff. Do you agree?
As a result of Covid, a lot more staff are tired.
How can we stop them? How can we transform them into happy, engaged and fulfilled staff?

Dr Ivy Glavee, Innovative Dentist, NHS

Happy engaged staff are prepared to go the extra mile which increases morale and productivity at work.

If you remember, organisations that did well during the lockdown were led by compassionate leaders. (EI)
One may ask. What is EI- emotional intelligence? It is managing your own emotions and that of others.
Metaphorically it is equivalent in walking in your staff shoes.
As I look at improvements I would make to society if I were in position of power, I prefer to focus on improvements in the working environment.
What I will do is as follows:
1. Create a garden which serves 2 purposes. A garden where staff can relax, reset and recover with scented roses, lilies, sunflowers and a water fountain.
The other purpose is a vegetable garden that staff can tend to which grows vegetables such as carrots, lettuce and others. When the vegetables are harvested it will be used to prepare meals reflecting the heritage of the staff.
As an alumni of my university we were encouraged to make a difference in society.
We went to a famous hospital in London to grow vegetables and flowers. This act of service inspired me to write an acrostic
poem which I dedicate to all health care professionals who work so hard.
Who is healing the healers?
B stands for Brave;
U stands for Unique;
R stands for Resilience;
N stands for Nice;
O stands for Outstanding, and; T stands for Transformation.
2. I will create a day of gratitude, celebration, issue citations, M & S vouchers to all who have gone an extra mile for the organisation.
3. I will encourage reverse mentoring.
4. I will create a job swap board listing skills and values whereby employees can transfer to other departments without leaving the organisation.
5. Use dead spaces around hospitals to build hostels for retired staff to come in and work on pay as you go who take over a department for the day to give current staff some time off work for the day to relax, reset and recover
Thank you for reading. Let us be the change we wish to see in the world which becomes a ripple effect to inspire the next generation.
In this report a critical examination of the classification, diagnosis, treatment of mental health disorder of (GAD) General Anxiety Disorder from the ICD-10 will be provided.
General Anxiety Disorder, according to the NHS (2021). IS defined as a constant feeling of stress, extreme panic and fear which can have a serious detrimental impact on an individual’s everyday life, affecting physical and mental health and wellbeing.
GAD is classified within F40F48 Neurotic, stress-related and somatoforms disorder. GAD is under F41.l. Causes of anxiety, (Aetiology), signs and symptoms. When anxiety can be diagnosed.
The symptoms of (GAD), General Anxiety Disorder, can cause both psychological (mental and physical symptoms). These vary from person to person, but can include;
1: Feeling restless or worried.
2: Having trouble concentrating or sleeping.
3: Dizziness or heart palpation.
4: Being easily fatigued.
5: Having headaches, muscle aches, stomach-aches, or unexpected pains.
6: Being irritable.
These are some of the symptoms. You are most likely to be diagnosed with GAD if you had symptoms for 6 months or more. Funding it difficult to manage your feelings of anxiety, is also an indication that you may have the condition.
To help with the diagnosed, the GP may carry out a physical examination or blood test to rule out other conditions that may be causing the symptoms such as: anaemia (a deficiency in iron or vitamin B12 and folate), or an overactive thyroid gland hyperthyroidism). Questionnaire can be completed by the patient.
Current treatment (give an evaluation = positive and negative). Divide the treatments according to the severity. Measurements of rehabilitation. These are all the tools to chart progress/treatments and to check the effectiveness of treatments provided.
In order to assess the effectiveness of the treatment, it is important to know the Measurements of rehabilitation. This is because if the treatment is not effective, it should be changed....
Jainaba Jum, CEO, Queen Holistic Initiative
One of the rehabilitations in GAD is the General Anxiety Disorder QUESTIONNAIRE. (GAD-7). This questionnaire is a tool to measure the level of anxiety over a period of two weeks.
Recommendations for improvement of anxiety (Complementary Therapies). Use of complementary therapies. For example, students such as Shohani et al. (2018), demonstrated the effectiveness of yoga in reducing anxiety in women.
This will have a positive impact as it will reduce the use of drugs and their side effects. (NICE).

Although at times the anxiety that all people experience can be somewhat severe, a characteristic of GAD is that this anxiety is usually more intense and long-lasting.
If you have more severe anxiety than most people you know, then it may be more than “normal “ anxiety.
It is imperative for the system to change from being reactive to proactive, with an increased focus on prevention, and earlier detection and diagnosis. In parallel, we need to recognise that a holistic approach to care is essential where two-thirds of adults aged over 65 are expected to be living with multiple health conditions by 2035. 1 Managing people with multiple chronic conditions and complex care needs is a challenge for health and care systems and anecdotally there is frequent feedback from people about their suboptimal experience of coordinated care.
The people best placed to act on their multiple conditions are the individuals themselves and/or their carers. They are the only ones that have a holistic perspective of their care, especially across multiple services. For them to effectively manage their conditions, they need access to their healthcare records and the ability to drive their care via a shared care plan that is based on their goals and what matters to them. This self-management is done in partnership with – and supported by – their primary care team, multi-disciplinary and
specialist teams, community providers such as pharmacists, and voluntary, community and social enterprise (VCSE) services if and when they are required.
Patient or resident portals are one way of engaging and supporting people to be empowered in their care and selfmanagement, which are associated with improved health outcomes. 2 As Claire Morgan, patient partner for St George’s University Hospitals NHS Foundation Trust says, "I have long wanted to access my medical records in the same way I access my bank statements…”
Through an app or web-based access, portals provide the capability for individuals and/or their carers to securely access and view their electronic health and care information. This allows them to input information that directly integrates into their record (after professional review) – such as completing online assessments, PROMs3 and PREMs 4 - request prescriptions and engage in bidirectional messaging
with care teams. They are also able to receive notifications, view and manage appointments, access test results, and read clinical documentation – such as clinic and discharge letters, educational resources, condition and appointment information – and more.
Portals are also a key enabler in the modernisation of outpatient services through supporting virtual consultations and online assessments, enabling effective and safe triage of patients for various care pathways, PIFU5 and streamlining pathways. These digitally enabled pathways can reduce the need for follow-ups and free up time for care professionals to offer enhanced inperson interactions for those patients who would benefit most from this appointment type.
There are many cited benefits to these new appointment types, such as patient convenience, parking and transport (cost or finding a driver), not having to take time off work or find childcare, and reducing carbon footprint. Portals support personalisation of care and work as an enabler for joined-
 Justine Patterson, Senior Health Network Strategy Executive, Cerner Corporation
Justine Patterson, Senior Health Network Strategy Executive, Cerner Corporation

up, personalised care. For example, portals can reduce anxiety for people on cancer surveillance programmes through having timely access to their test results. 6
However one size doesn't fit all. Although it may improve equity for many people, virtual appointments may also risk introduction of access issues, e.g. for people who lack digital skills or access. When implementing patient portals, there are several considerations that health and care organisations or systems should factor into the care redesign process and how portals can augment the therapeutic relationship. Examples of factors to consider include: reason for requiring assessment and treatment (e.g. acute problem or longterm condition), a first consultation or follow-up, type of specialism or service, availability of a digital alternative that is as/more effective (i.e. what does the evidence show), and most importantly, individual preferences and choice.
Involving patients and public representatives/partners as the end users from the start in the design decisions and localisation when implementing patient portal solutions is essential to keeping the patient at the centre. Organisations that have used a coproduction approach in their deployments have valued the perspective and healthy challenge these key team members bring to ensure that the portal is considered within the wider context of health and care service provision.
As with most technology solution deployments, it’s important to invest in the change process to optimise benefit for care professionals and individuals and/or their carers. It’s not ‘just a piece
of tech’ being deployed; it provides the next generation engagement methodology. Clinical networks and services are excited about the potential of portals to transform care pathways and are working together to reimagine workflows across the various services patients interact with.
NHSE’s plans to use the NHS App as the ‘front door’ for patient portals are progressing at pace. A substantial proportion of the population downloaded the NHS App during the pandemic to access COVID vaccination certificates, and people now request prescriptions and appointments from care providers, such as GP practices, that are already integrated. The recent government announcement7 outlines ambitions for the NHS App and timelines for additional functionality to be delivered by 2024 with development support for the established portal suppliers to integrate.
Although portals are increasingly being used to support engagement with health and care services, their full potential in supporting selfmanagement is yet to be realised. As Claire Morgan says, “a patient portal is an important tool, but it shouldn't be the centre – the patient should be the centre”.
1 https://evidence.nihr.ac.uk/alert/multi-morbidity-predicted-to-increasein-the-uk-over-the-next-20-years/
2 https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.0452
3 Patient Reported Outcome Measures (PROMs) measure a patient’s health status or health-related quality of life from the patient perspective at a single point in time. They are collected through short, self-completed questionnaires.
4 Patient Reported Experience Measures (PREMs) are questionnaires that focus on the patients’ experiences of the care they receive.
5 Patient Initiated Follow-Up (PIFU) is when a patient initiates an appointment when they need one, based on their symptoms and individual circumstances. https://www.england.nhs.uk/outpatient-transformationprogramme/patient-initiated-follow-up-giving-patients-greater-controlover-their-hospital-follow-up-care/
6 https://youtu.be/P68TY4IhSaghttps://www.nhsx.nhs.uk/key-tools-andinfo/digital-playbooks/cancer-digital-playbook/patient-portal-in-wirraluniversity-teaching-hospital/
7 https://www.gov.uk/government/speeches/health-and-social-caresecretary-speech-to-policy-exchange

NHSE guidance states “our ambition is to improve core digital and data services in hospitals to ensure we have the basics right.” As the leading EPR provider in the UK and globally, Cerner supports systems to reach the minimum digital foundation and strive for HIMSS Stage 7 and beyond.
We work across provider collaboratives to enable shared instances of the EPR. ICS-level collaboration reduces total cost of ownership and enables sharing of resources, such as PMO, training, back office and support. For example, a shared instance of
Ensuring that patient pathways are digitally enabled and person centred is critical to tackling the elective backlog.
Cerner accelerated provider collaboration across North West London ICS. Imperial and ChelWest began sharing a domain in 2019 and now London North West and Hillingdon are set to join. According to Kevin Jarrold, ICS data and digital lead, “We have a growing agenda around collaboration across care pathways and the shared domain is absolutely fundamental.”
A shared domain has enabled NWL to gain efficiencies and generate muchneeded capacity. Leaders can see across the system and transfer patients more effectively from one site to another. Virtual ward capacity is also managed centrally and embedded into the core EPR. Remote patient monitoring is leveraged from a variety of vendors, with all data feeding centrally into virtual wards created within
the core EPR, enabling more efficient workflows and the sharing of virtual care staff.

The national guidance outlines care must be prioritised based on clinical urgency, the impact of waiting on individuals and potential inequalities. To achieve this, North Central London (NCL) ICS uses Cerner HealtheIntent®, a data and analytics platform that provides a single longitudinal record for every citizen, comprising data from all health and care organisations across the ICS. According to Amy Bowen, director of system improvement, “[We built] an elective waiting list dashboard in HealtheIntent.
Patricia Wynn, Director and sales leader, international public sector health, Cerner CorporationNow we can show GPs for the first time ever what their waiting list looks like.
We can cut that data by all the demographic factors, e.g. how many people have long-term conditions and how many?
We can look and see by ethnicity, by deprivation – we can combine several factors. And we can actually understand that population at a practice level, at primary care network (PCN) level; by specialty, by borough.”
NHS guidance outlines transformation should focus on flexibility, ease of access and citizen control. Reenvisioning patient pathways – and ensuring they are digitally enabled and person-centred – will be critical.
Royal Free London (RFL) has standardised and digitised 40 pathways. Cerner experts are involved from the beginning of pathway design. Dr John Connolly, CEO of the Royal Free Hospital and group director of clinical pathways shares, “The goal of this ambitious programme is to ensure every patient can get the same highquality treatment in any of the Trust’s three hospitals… and to create value for the entire healthcare system in the
locality – not just our hospitals, but also primary care and public health services in an area that has high levels of deprivation.”
Ultimately, a person-centred, digitalfirst approach must include the person at the centre. Cerner Patient Portal UK, delivered in collaboration with Induction Healthcare, enables interaction and engagement between caregivers and their populations.

A prostate cancer survivor in the Wirral explained, “I cannot emphasise how much the patient portal has improved the quality of my life. Those two weeks of waiting – the stress of revisiting the room where I was given my diagnosis – all that is gone now.”
NHSE’s operating priorities will not be achieved by overworking caregivers and staff, but by enabling them to work smarter and more collaboratively.
Contact us if you share our belief in the power of technology-enabled transformation and want to discuss how we can support your system as you look to tackle the unprecedented backlog of demand.
mii Rota and mii Roster are integrated solutions designed by the NHS for the NHS ensuring workforce optimisation, compliance with current rules, and flexibility for policy changes in the future.
Available for all staff groups, these market changing solutions deliver an exceptional mobile app-enabled user experience, true interoperability, and intelligent reporting.
mii Rota enables the creation of rotas based on demand, while mii Roster replaces existing manually intensive medical rostering processes with an NHS designed cloud-based solution, helping you to optimise your medical workforce.

Part of the mii platform, facilitating a shared vision for procurement, data, intelligence and best practice to drive improvements across the NHS.
To find out more, visit liaisongroup.com/liaison-workforce or get in touch at info@liaisongroup.com or telephone 0845 603 9000
Northfield Care Centre was moved into special measure,, by the care inspectorate just nine month., ago, but after a new management team was introduced, the facility has now jumped up not just one, but two ratings to 'Good'.
The facility was inspected by the CQC who said residents had already benefited from the "improvements to the quality and safety of the service".
The inspector said; "Relatives felt listened to and told us complaints were appropriately dealt with and resolved. People told us their views were obtained to continually drive improvements”.
A
in
which was previously rated as
the
(CQC) has achieved a

"Feedback from staff was extremely positive about the improvements to the service, they worked better as a team and were well supported”. The inspection report praised the facility's staff saying they were "well-trained" and "knowledgeable about people’s needs".
The report said; "Staff ensured peoples safety and people told us they felt safe. Staff understood safeguarding and whistleblowing procedures and there were sufficient staff employed to meet people's needs and respond in a timely way”.
"The provider operated a robust recruitment process and monitored accidents and incidents, which ensured staff learned lessons when things went wrong”.
"Staff followed safe medicine, management systems and people received their medicines as prescribed.
People were supported to have maximum choice and control or their lives and staff supported them in the least restrictive way possible and in their best interests".
During the inspection, residents and relatives also shared positive feedback about the team.
The report revealed; "People told us staff were extremely kind and caring. Relatives were also positive about the care and support provided. They told us they had noticed improvements over the last few months since the new registered manager had been in post. Staff understood people's needs and respected their dignity”.
Following the inspection the facilities registered manager, Thomas Ogden, has become the youngest manager to lead a care team to achieve a 'Good' rating after previously being rated ‘Inadequate'.
He said: "I would like to thank all our staff, residents, relatives and professionals who have all worked together to make this achievable. Our home was rated 'Inadequate' and is now 'Good' I couldn't be any prouder. It’s a remarkable achievement for all involved. Well done and thank you”.
Paula Newbert, the group's Clinical and Operations Director, praised Thomas for his efforts and revealed he has now been appointed to the Board of Directors. She said; "We are the proud employers of the youngest manager to lead a home from
'Inadequate' to 'Good' in just nine months.
"We would like to express our thanks to Thomas who we have invited to the Board of Directors, and will be registered as the Nominated Individual with the Care Quality Commission.

"We would like to congratulate the full team at Northfield for their extremely hard work on achieving an exceptional CQC Report."
Inspectors said some small improvements are still needed in areas such as meal time experience and medicine management, but the report said the provider had already identified these issues and was already working to implement solutions.
To read the full inspection report visit: https://www.cqc.org.uk/ location/1-3562136917/reports
Thomas Ogden, registered manager at Northfield Care Centre in Thorne has become the youngest manager to lead a care team to move from an 'inadequate' CQC rating straight to 'good'.

MA LLB(Hons)
Our Living Memories reminiscence resources are available on https://www.livingmemoriesonline.com and https://livingmemories.imagencloud.com
Enquiries to: brian.norris@livingmemories.io Phone: 07922 233363/01297 552358

Our Living Memories reminiscence resources are available on https://www. livingmemoriesonline.com and https://livingmemories.imagencloud.com
Enquiries to: brian.norris@livingmemories.io Phone: 07922 233363/01297 552358
Living Memories CIC is a non-profit community enterprise that we created in 2017 to use archive films from the 20th century to help to reduce the isolation of older people, including those living with dementia.

During Covid, with support from major UK film archive collections we created a unique interactive online streaming platform, Living Memories Online, offering over 3,600 archive films and newsreels. We were very fortunate to be able to trial the use of Living Memories Online during and after the Covid lockdown in one national care home group and below is the practical feedback that we received.
Both the Living Memories DVDs and Living Memories Online (LMO) resources have great benefits for the residents in our homes, whether for those living with dementia or those who need to connect through conversation with others to enhance their wellbeing and to stimulate the mind with memories of their lives.
Bringing folk together and generally watching short archive film clips sparks much conversation and this type of archive of adverts, film and other historical content just triggers the memory of things they may not have thought about for many years.
When we hold sessions, there is much fun and laughter and you never quite know what will be triggered. Recently one older lady shared how she was a milk(wo)man!
So often when people are sharing, their fellow residents and staff never knew
that about that person’s life, which then stimulates further discussion after the sessions and keeps a conversation going.
With the pandemic and isolation and lockdowns, the Tea and Memories sessions run were vital for enhancing wellbeing and now we can begin to open the doors again to the public, staff are inviting in visitors to join in with these sessions. Very often family members learn things they didn’t know about their loved ones!
The Living Memories Online archive films and newsreels really do help activities coordinators, staff and volunteers to plan topical sessions with the residents on subjects they would like to be reminded of. Very often those leading the sessions may be young and the printable reminiscence guides with the LMO service and DVD’s make it much easier for them to run a session.
Staff can pre-plan sessions by looking through the archive online and store the film clips in their collection on LMO.
As mentioned above, staff often discover things about people that they care for day in day out, that they never knew about them. That is great for personalised care because you can build on that and then find other stimulating things from their past experiences, work, family etc.”
Dr Chloe Sellwood. Deputy Head, EPRR, NHS London, co-chair of the London NHS EPRR EDI Group


Surriya Subramanian, Emergency Planning and Business Continuity Manager, Central and North West London NHS Trust
Francesca Davies, EPRR Manager, South East London Integrated Care Board

These questions, and more, have stimulated the NHS emergency preparedness, resilience and response (EPRR) community in London to establish a growing group of members to understand more about equality, diversity and inclusion (EDI).
We are looking with curiosity to understand the diversity of our own community of ~140 practitioners in NHS organisations across London, considering protected characteristics as well as aspects of part-time/flexible working and career development.
We were pleasantly surprised to learn we are representative for gender, but saddened that our ethnic diversity was heavily skewed towards white groups. We are now considering how we can encourage more diversity of people joining our profession, and support people within the profession to grow and progress.
We have started this with a small step of sharing some powerful stories of leaders in NHS EPRR to encourage and empower our more junior colleagues –stories of overcoming racism or gender discrimination.
Through a better understanding of ourselves, we’ll also be better able to support patients and staff by being more inclusive in our planning for major incidents and emergencies.
We are identifying existing good practice that may be unseen or underchampioned in our network to share our experiences of what has worked and what hasn’t.
We are championing links with patient experience and engagement groups – to better understand our local and London populations, as well as to be able to invite patient and population groups to potentially engage in developing and testing response arrangements.

An early example of this has been inviting members of the gay and queer community in London to share their reflections of the monkey pox response in the capital.
Their candid views are supporting our ongoing planning for response, but also about wider engagement. And finally, its early days, but we are also actively exploring the connection between EDI and reducing health inequalities.
The effects of disproportionality were bought in to stark relief during the pandemic, we want to do everything we can in our profession to address this in planning for and responding to future emergencies.
We’ve taken a few small steps this year, but we are growing in momentum and can absolutely see the potential for our work.
By recognising our diversity (or lack of) we will better support the diversity of Londoners (staff and patients) that we work for in preparing for and responding to emergencies.
Contact chloe.sellwood@nhs.net
Gemma Price, HR Trainee, NHS Graduate Management Training Scheme

Working within healthcare, communication and collaboration are frequently considered virtues that all colleagues should uphold.
Indeed, in any organisation, an inability to share, develop and learn from each other only hinders our progress.
THE LOOP
Embracing shared knowledge and lived experience is the main reflection that I have from my first year on the NHS Graduate Management Training Scheme.
Working as a lone trainee in an NHS Trust can be isolating, and yet our scheme comes with over two hundred colleagues in the same position in NHS organisations across the country.
Having worked in the NHS prior to joining the scheme, my knowledge was limited on the ramifications of collaboration; for me, that word meant working with colleagues in my office or with a related department. However, over the past year I have come to understand that there is no limit to who can support you within the NHS.
As a HR Professional I frequently update policies and guidance to incorporate new legislation and to embed just culture. Early in my career, this was something that I developed in a silo, combing over recent publications to ensure our policies were the most up to date and factual they could be.

After joining the GMTS, I realised that every NHS organisation has similar sets of policies, and yet this wealth of resource is not routinely embraced. Unfortunately, it is all too easy to default to working in an vacuum when faced with the daily pressures in each NHS organisation.
Over the past year, I have consulted with both my local network and my national GMTS colleagues when enacting change, resulting in service development based on our shared learning. Through this, I’ve discovered a wealth of wellbeing
resources accessible to staff across the country, despite only being advertised locally in some areas.
Working with this national network also enables elimination of unconscious bias. Policies, procedures, organisational change, and service development all can negatively affect those involved if not implemented correctly. By learning from colleagues that have already affected change, we can mitigate potential issues that may not have been identified otherwise.
Even within the GMTS itself, there is potential to learn from other services under Health Education England, and yet this is still limited at present. One such improvement would be the complex nature of sharing information between employers and hosts, which I am aiming to develop from building on learning from another HEE shared service.
Whilst of course there is a concern around intellectual property, I truly believe only benefits can come from colleagues sharing best practice or mistakes to avoid and will ultimately change health and social care for the better.
As I move into my new role in an ambulance service, I look forward to incorporating this learning in such a different NHS organisation to the Acute Trusts I am used to. Ultimately, I would encourage everyone to expand their networks nationwide, and get to know colleagues outside of your region for your own development and that of your service.



Managers account for around 2% of the NHS workforce, considerably less than the 9.5% of the workforce in the wider UK economy made up of managers, directors and senior officials1 .
This means it is vital for the NHS to have good strong leaders in any position and at any level to ensure the continuity of a successful NHS. A good leader can positively propel a team/organisation to excel, they encourage and motivate, they inspire and set good examples. Leaders communicate and support the team and are always striving for the best resolution.

All the while, blazing a trail for future leaders to follow. In practice, leadership and management are closely interconnected and healthcare employees at all levels often have to deploy both leadership and management skills to carry out their job effectively1 . There are many different leadership styles, many heavily documented and effective. I found compassion in a healthcare setting to be one of the most powerful influences on my career and job satisfaction.
Compassionate leadership enhances the intrinsic motivation of staff and reinforces their fundamental altruism. It helps to promote a culture of learning, where risk-taking (within safe boundaries) is encouraged and where there is an acceptance that not all innovation will be successful – an orientation diametrically opposite to a culture characterised by blame, fear, and bullying.
Compassion also creates psychological safety, such that staff feel confident in speaking out about errors, problems, and uncertainties and feel empowered and supported to develop and implement ideas for new and improved ways of delivering services 2 .
My experience of compassionate leadership is explained entirely in the above reference. I had always enjoyed my job, and always found to enjoy working as part of a team, but I rarely deviated from the job role I had held for over a decade. I have worked with a range of different managers and seemingly as long as I did my job everyone seemed to be happy. No more, no less.
The COVID pandemic illustrated, more than ever, the need for compassionate leadership. My manager, Nicky, stayed
supportive as we were all redeployed.
At a monthly Teams meeting the clerical group were offered a small service improvement project to get involved in, Nicky was encouraging and supportive, it was a team-building exercise and I felt my eyes light up and my brain start whirring about what we could do to improve our service.
The challenge we were given was to come up with one service improvement idea and implement or trial it, this proved to be a catalyst for other improvements. My manager has always been passionate about learning, and I was inspired by this passion. Nicky encouraged me to overcome the fear of failing, and instead learn from it.
From this positive outlook, encouragement, support, and superb communication from my leader, my confidence grew. I have since presented my work, and chaired meetings, completed a range of courses, written articles, and taken on a different job role. I also led a service improvement project that has won an award and has recently been shortlisted for another. I have incorporated compassion into my own leadership and hopefully,
I can inspire someone too. Without a compassionate leader who was invested, caring, encouraging, positive, and supportive the door to opportunity may still have been firmly closed for me and I could still be in the same seat in the same office for years to come.
1. Jones, Jones, Horton, Home. Strengthening NHS management and leadership : priorities for reform. 2022;(February):1-22. http://usir.salford.ac.uk/id/eprint/63275/.
2. Rosenman. Caring to Change. Volunt Sect Rev. 2011;1(2):239-44.

Available from October 2021
Developed to meet the increasing demand for managing and leading preventive health services in communicable and non-communicable diseases.
Arden University offers you the opportunity to study online around your current job
MASTER OF PUBLIC HEALTH Aligned to APHEA European Public Health competencies, this programme will prepare you for a career in the public health sector with particular focus on the latest digital and analytical skills sought by employers.


Designed in collaboration with leading employers , this course focuses on issues that impact health but transcend national boundaries.
More full and short qualifications coming in early 2022, including leader and senior leader apprenticeship routes
For more information or to apply please visit arden.ac.uk
We seem to spend most of our time dealing with immediate and urgent problems – and then digging ourselves out of one hole, followed by the next.
Paul Mercer, Chair, Strategic Estates Management Technical Platform
We seem to spend most of our time dealing with immediate and urgent problems – and then digging ourselves out of one hole, followed by the next.
Yes, there are ‘plans’ for aspects of the business which need to be prepared and agreed but these often require amendment as events unfold.
But there is – in many but not all cases –one strategy which seems evasive and, if produced at all, is lightly discarded due to the inevitability of “events”. An Estates Strategy.
There is much to be unpicked about what one of these is – and there will be many views and versions across the healthcare sector.
One thing we can say for sure is that the current approaches – in many but not all cases – produce some less than sustainable outcomes; sustainable in all meanings of the word.
Things start to go wrong often at the very beginning of new proposals – the lightbulb moment followed by the likely expectation that the project will be fast tracked and finished faster than any before.
Now, the sketch above is more prevalent where organisations have authority and means to get things moving. There is a whole different picture where large and very large schemes are proposed. For these, the speed of progress is at the snail’s pace end of the spectrum but there are some common factors which can be wrung from any of these.
These common factors are tools that might be available to inform the immediate aftermath of the lightbulb moment. There is, for example, a tendency to assume what the capital cost will be and to likewise assume how quickly things
can happen. Hurried figures will come back to haunt.
And there are other factors which could be of use around such things as: is there a written and adopted brief, revenue, staffing, appropriate selection and appointment of advisors and designers, design quality, achieving net zero carbon, use of BIM, procurement options and so forth.
One key skill which will provide a backbone to the scheme will the engagement of healthcare planning. But how do you find such a skill and know that their input will be a match for your scheme? There are many flavours of healthcare planners and there is currently no accepted benchmark against which to check: anyone can cell themselves a healthcare planner.
May I then introduce you to the Strategic Estates Management Technical Platform of IHEEM, recently formed and still finding its feet but looking to explore and collect the tools which might help avoid projects going off in the wrong direction and also hoping to better categorise and eventually professionalise the role of healthcare planner.

The new TP will be making its first appearance at the Healthcare Estates conference in Manchester on 4th and 5th October and we look forward to opening the debate to as wide an audience across the service as we reasonably can.
Contact paulmerceruk@googlemail.com 07905 582 094 https://www.iheem.org.uk/
It is important to note that there are many ways to manage workplace stress and no one model fits all. The goal here is to make everyone aware of the importance of managing workplace stress and the ways to go about it. So here are some of my top 10 ideas of how a manager can reduce workplace stress.
The healthcare arena is always understaffed. It is key to get this fixed. The less staff you have the quicker your current workforce will be burnt out and leading to long-term sickness.
Start working with the recruiting teams as well as staff to fast-track the process
Rayhan Abdullah Zakaria, Chartered MCIPD MSc, Lecturer and Doctoral Researcher, Chester Business School, University of Chester.

of good quality staff hiring and make sure you can hold on to your current staff too. You can do this by listening, communicating and understanding their needs and concerns. Make them feel valued, help them with their daily challenges, empower them, and build trust and a culture of care and honesty. This is a slow and difficult process but if get it right the benefits are unimaginable.
You would never get it 100% correct but as a manager, you got to work with your team and get everyone together with regards to designing work rota making sure all services are met.
This blog is mainly aimed at the managers who are having to think of innovative ways to reduce stress for healthcare workers. It is impossible to eradicate workplace stress however there are ways to reduce it significantly or better manage it.
This is a team effort so don’t be afraid of trying new ways out, keep it fresh, but most importantly hear all staff's opinions, feelings and commitments. Let them have a key role in designing, shaping and monitoring the work rota. Empower them so that they take responsibility and ownership of implementing a good worklife balance.
These are simple actionable tools which take minimal time to implement example let your staff have time to name their challenging emotions such as am I feeling anger, exhaustion, or concern. Naming allows us to self-manage. Also, allow staff to take a moment or micro break in between tasks and reflect and aligning themselves.
Strictly enforce your staff take adequate break, if they do not take a break it will affect their output. Get the staff together to design their breakout space and breakout activity, and allow them to switch off completely
Look for ways to improve management of noise, healthcare environment is highly pressurised with various types of sounds and lights. Look at ways to get natural lights, natural sounds, fresh air in. Use calming colours, and pictures.
Cut out noise by implementing reduce noise procedures will help a lot. Having indoor plants, living wall, and water features all helps towards combating stressful stimuli.
Make sure staff get wholesome good quality natural food in the canteen, better even let the staff design good quality wholesome meal plan for the canteen. Sell these at heavily reduced prices. Your staff works so hard for you so offering them good quality free food (if possible) is the least you can do. Having a well-fed, hydrated workforce will enhance your service delivery.
Look at corridors, pathways alcoves and think of the best ways to use these to reduce stress. For example, a nurse's or doctor's daily routes could have small calming alcoves for a moment of rest by adding soft cushions, natural or soft lights, or a quiet place to call family etc.
Use real plants and greenery in small to large spaces. Having floorto-ceiling windows, letting in natural lights, and fresh air, make outdoor spaces a haven for flowers, insects
and birds, flowing water features, and living walls, so that staff get a lot of natural stimuli, all of this help to cut out stress.
Clutter breeds more stress. Having a clean tidy work area, walkway, path, lift, and stairs will help staff relax more. This should be throughout the hospital site indoors and outdoors from the parking space to every area around the hospital trust.
This is one of my favourites as to help your staff to reduce stress you should know them better. This is where you should talk to them daily, build one team mentality, hear their concerns, give them a voice, and let them feel they are genuinely valued and listened to. Get them together to build a positive working culture. When your staff feels valued, listened to, respected and can be who they are this will help in reducing work stress issues.
So there you have my 10 tips on how to manage staff stress within a healthcare environment, I hope you have found it informative and maybe try some of the tips for your selves within your teams.

https://hronetoone.com/services/

Visiba Care is an innovative, scalable platform for online and video consultations that enables healthcare providers to provide accesible, effective, and secure care through their branded virtual clinic.
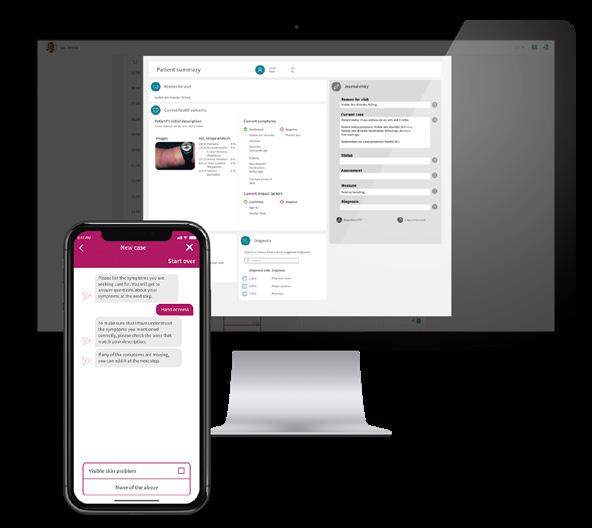

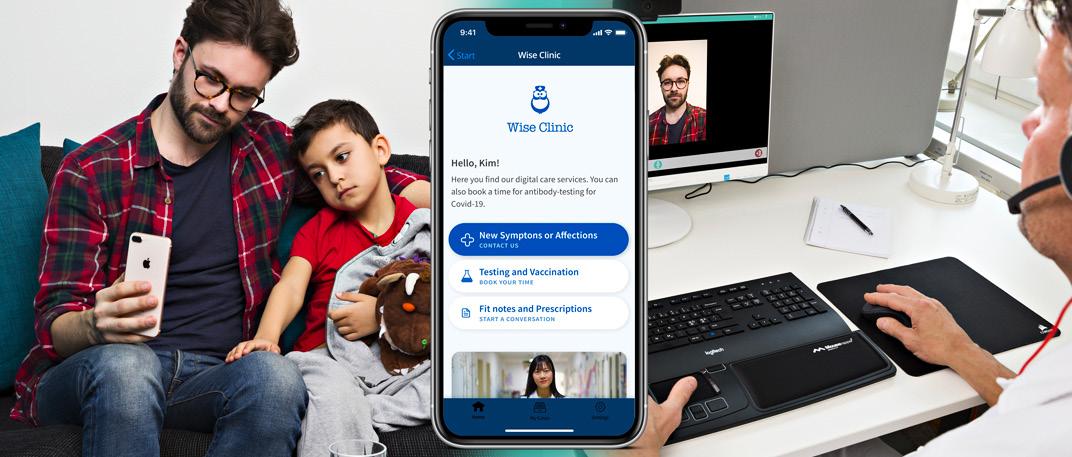
Transform patient pathways and give back time to your clinicians. Visiba Care can help

you increase the throughput of patients while optimising patient outcomes. Red Robin, the AI tool for medical history and triage, guides the patient to the right place in the digi-physical pathway and supports healthcare professionals in medical assessments in the front line of care.
