IHSCM Regional HUB









4. West Midlands Intro
5. West Midlands Going Green with the patient moving and handling team
8. West Midlands Integrated Front Door Service
11. West Midlands Outreach Support Team
16 West Midlands From the Back to the Future: Overcoming the Challenges
of Being an Outlier. A Multidisciplinary Team Approach to Quality Improvement for Hip Fracture Patients.
20. West Midlands CPEP and Beyond!
32. West Midlands A Journey into Clinical Practice : A Focus on the AHP Support Worker
42. West Midlands Clinical Exercise Physiologists : Important (but not new) Members of the Multidisciplinary Team
50. West Midlands How are AHP's Embracing the Green Agenda and Sustainability
59 West Midlands How do Allied Health Professionals Contribute to Public Health
67 London HUB Intro
68. London HUB Changing the Narrative for Testicular Cancer Patients Through Innovation and Collaboration
74 South East Care HUB Intro Oxfordshire CA
75. South East Care HUB Intro Berkshire CA
76. Primary Care HUB Intro Williams Medical Supplies
77. East Midlands HUB Intro
78. North West HUB Intro
79 South West HUB Intro
80. Wales Country HUB HEIW Intro
81. South East Care HUB Intro
82. West Midlands Care HUB Intro
83. West Midlands Education HUB Arden University Intro GMTS Intro
84. London Education HUB University Wales Trinity Saint David
85. Northwest Care HUB Lancashire and South Cumbria ICB

86. Northeast HUB GMTS Intro
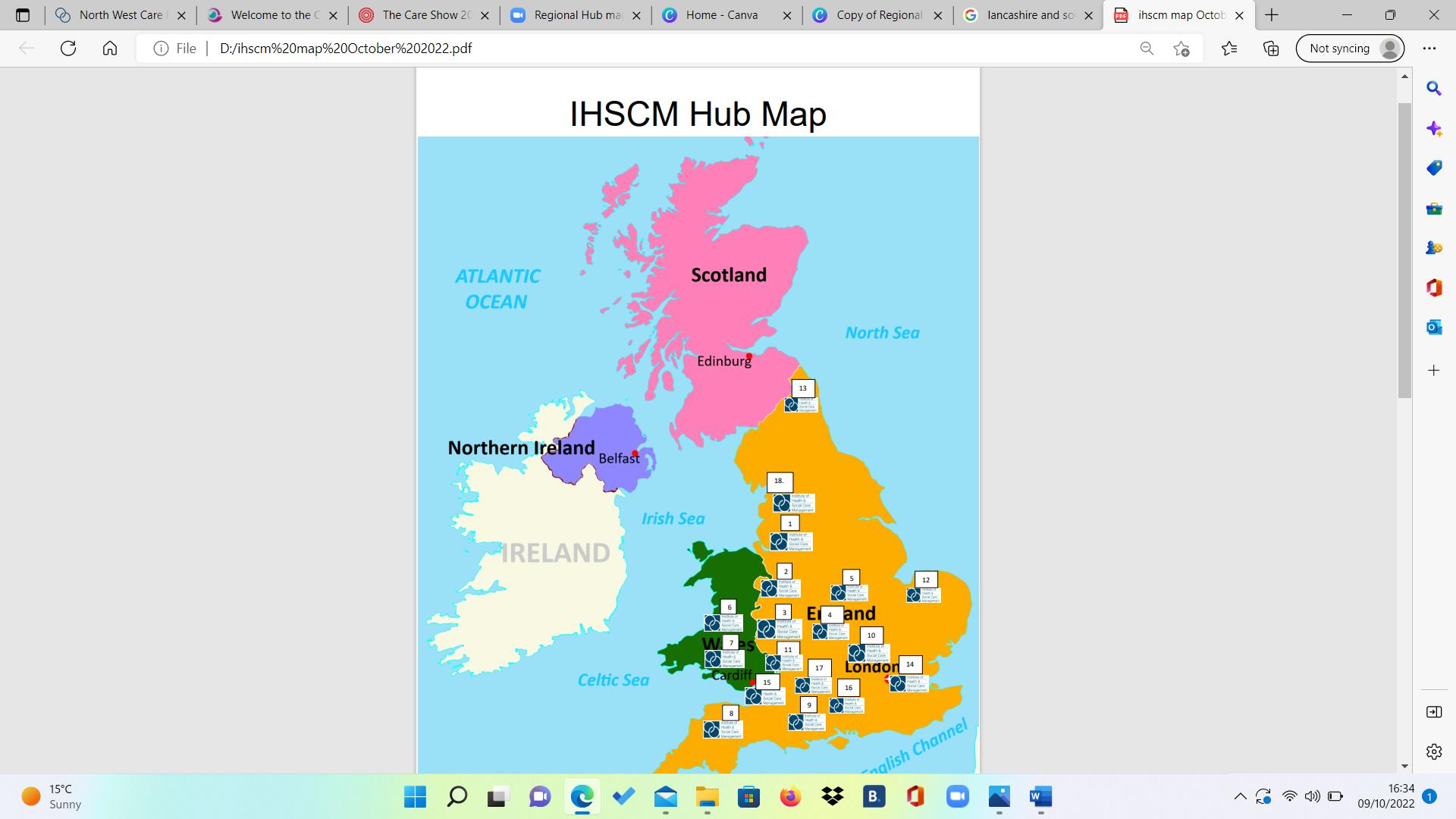
87. IHSCM HUB Map



IHSCM West Midlands HUB is the Royal Wolverhampton NHS Trust and Walsall Healthcare NHS Trust. In this edition we have lots of input from this HUB and we thank you for sharing all of your great work. We currently have over 500 members and growing across our West Midlands HUB








In September 2018 following an NHS clinical review of slide sheets, the Royal Wolverhampton NHS Trust Patient Moving and Handling team began a piece of work to look at the use of this equipment within the Trust. The usage at that time identified that we were using over 19 different types of slide sheets. The Patient Moving and Handling Team commenced a review of the equipment and evaluating the findings by undertaking a Quality Improvement project for the organisation.
The aim was to introduce a new slide sheet into clinical areas which could be used throughout the whole patient stay within the Trust and on discharge, with the use of CQI methodologies to improve patient and staff safety.


Initially the pilot focused on providing continuity of practice and equipment across the Trust as a whole. However, the potential to reduce the carbon footprint and support the sustainability ethos of the Trust became a key driver whilst retaining the objectives of the project.

In partnership with GBUK Banana, a company who is committed to reducing the carbon footprint of their products and operations, the project was piloted in various areas of the Trust, including Cannock Chase, West Park and New Cross Hospitals with feedback collected from both staff and patients.

Having stalled on several occasions due to staff changes and the pandemic, what started three years ago has now become a reality.

Working closely with the new clinical procurement lead, Sian Fumarola, a passionate sustainable procurement champion, we are pleased to announce the new slide sheets have been introduced as standard across the Trust from the 1st of April 2022. This move will realise a £1,500 recurrent financial savings and contribute a reduction of approximately 1.8 tonnes of CO2e to the Trust carbon footprint.







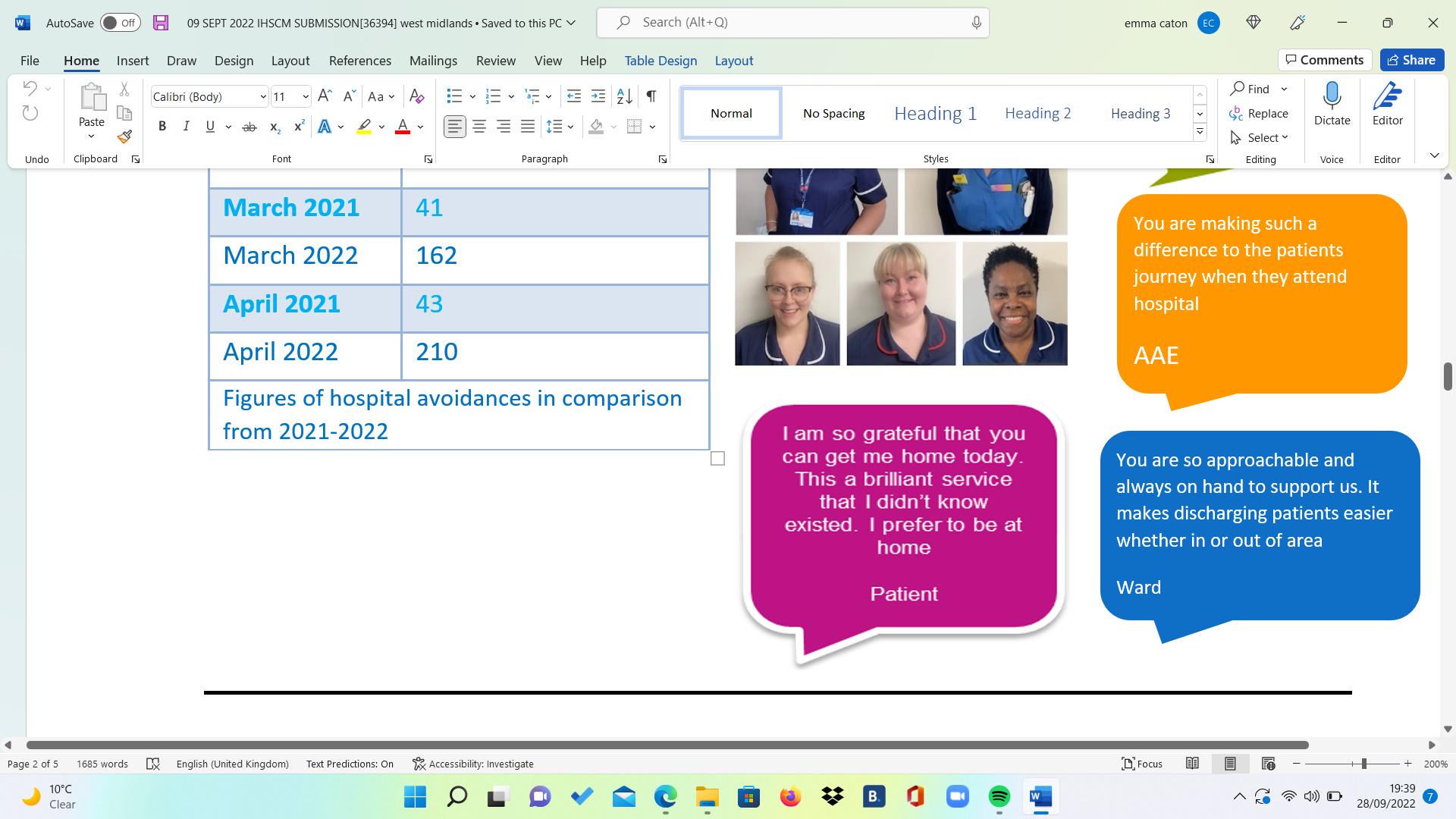
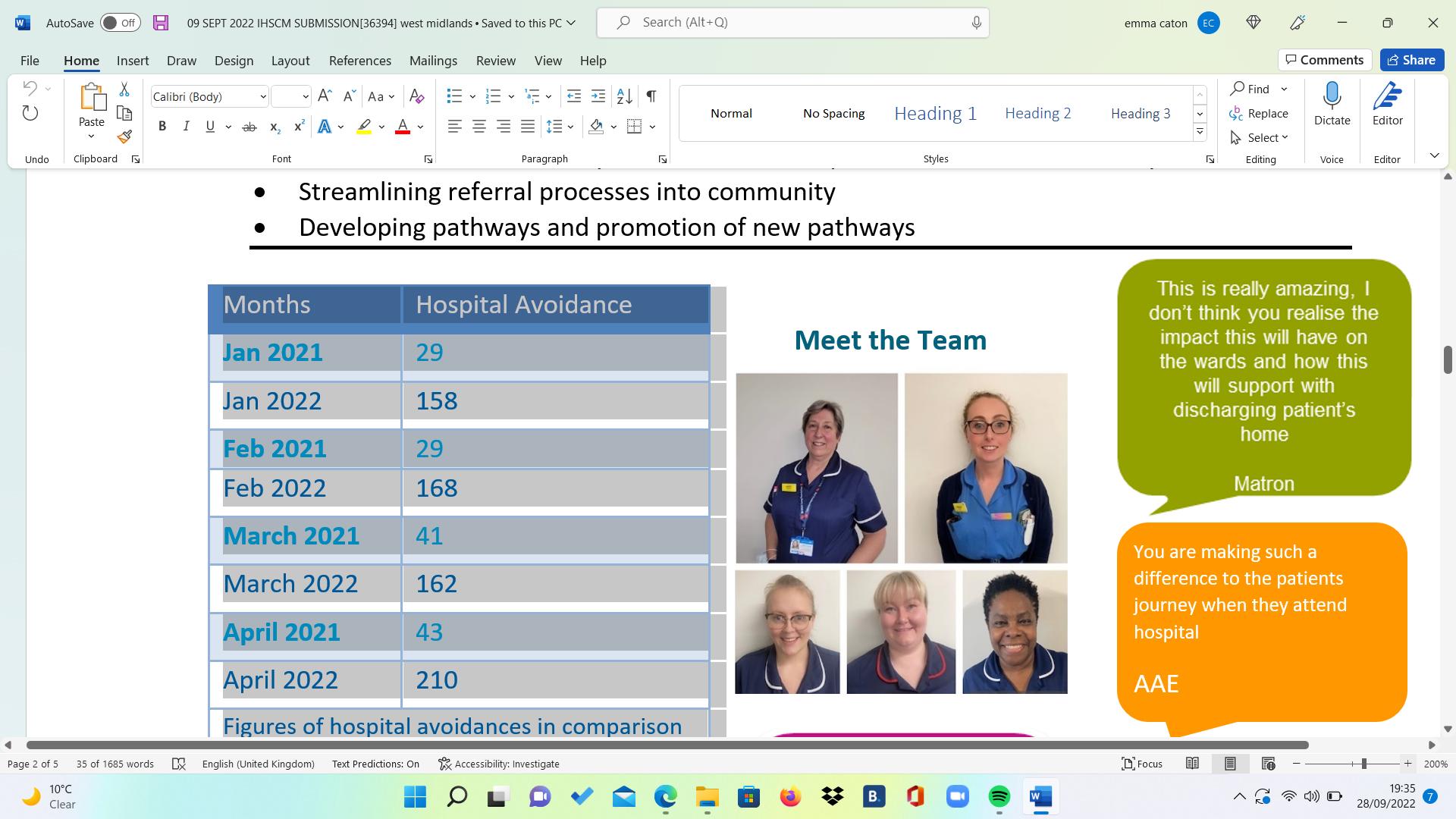
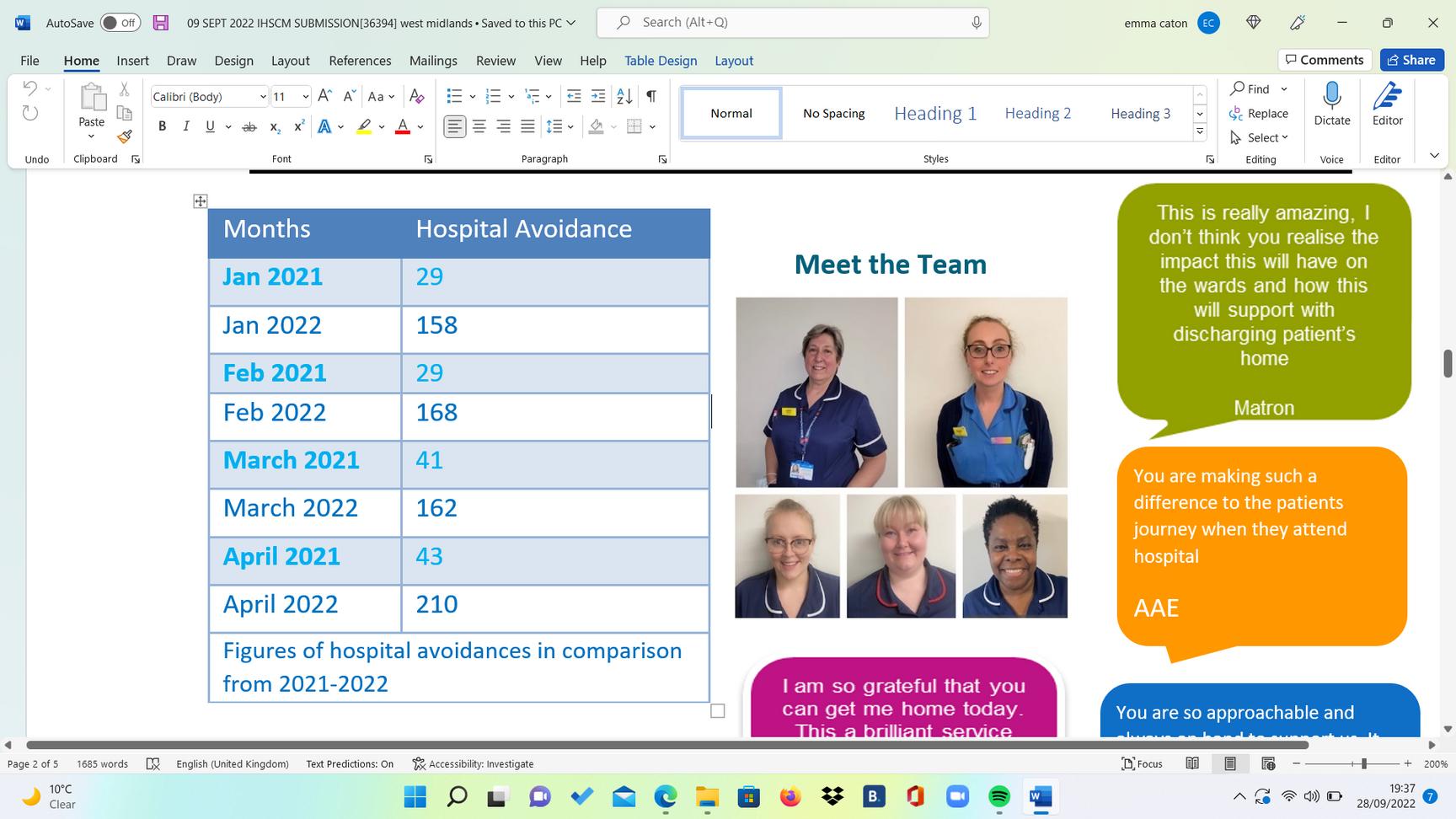
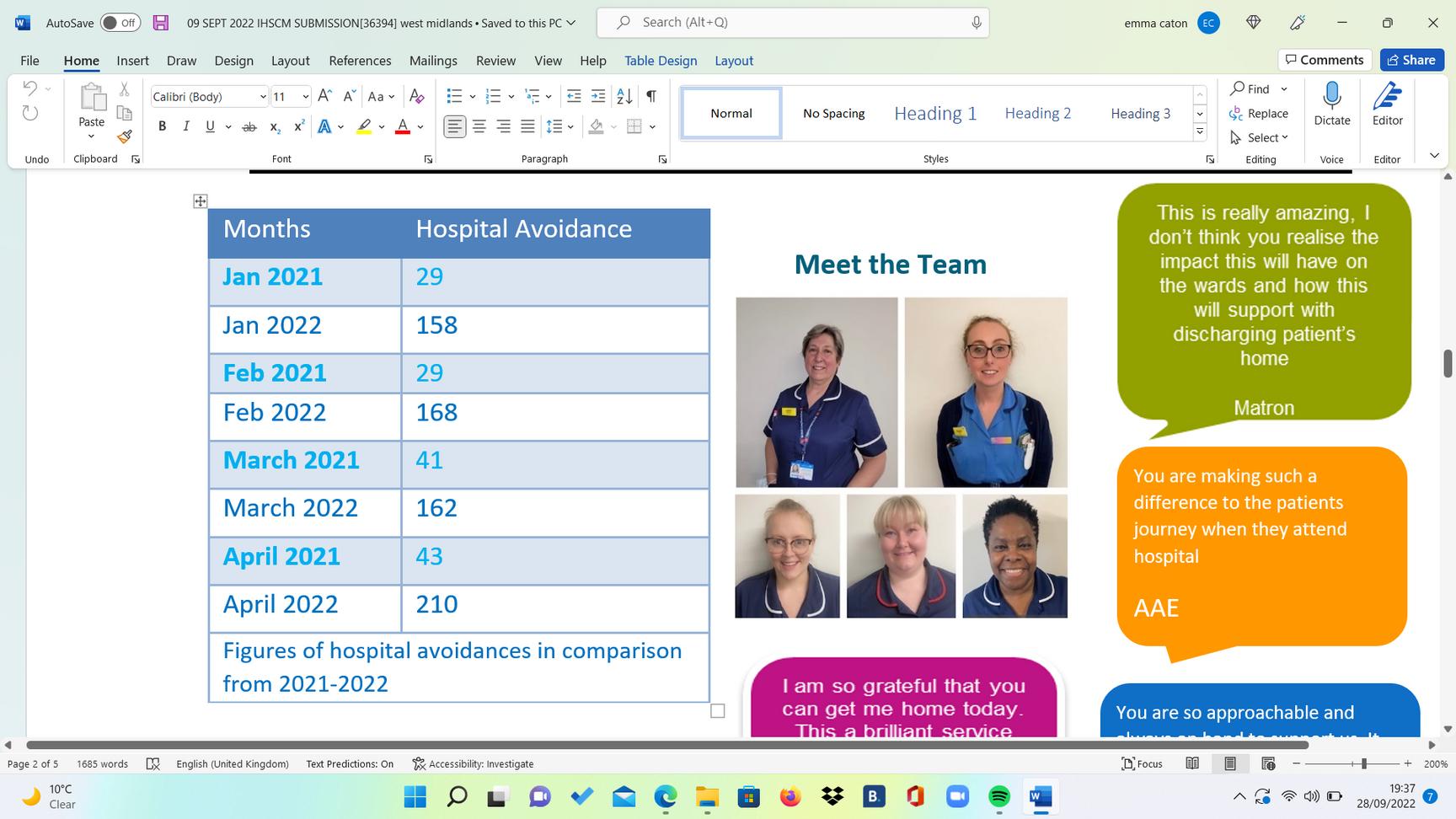
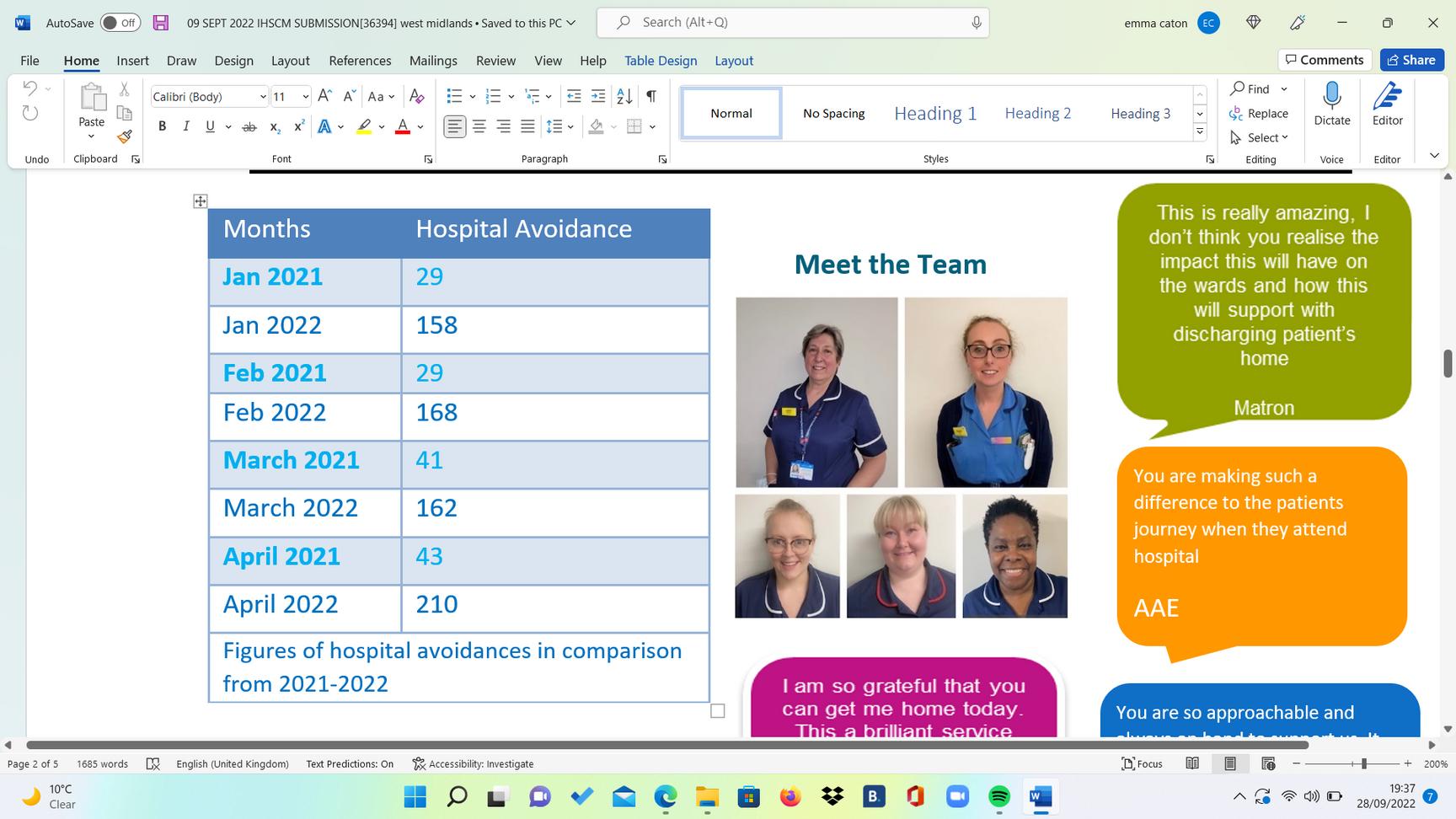
The Integrated Front Door Service (IFDS) has brought community nurses into the acute to identify anyone over the age of 18 who could be discharged home from the front door emergency areas, as well as deeper wards, onto alternative community pathways. Creating community service awareness, education and implementing new pathways along the way. The team are permanently based at the hospital.


Background:
The Service was launched December 2020 in response to the pandemic and is one of the first of its kind in the country. The team currently work 8am-6pm with the aim of avoiding hospital from the front door of the hospital whilst supporting wider department areas to identify patients that can otherwise be cared for at home to support earlier discharges and prevention of re-admissions.

Since its launch, the service has a focus on the front door of the hospital and directly stream patients into a community assessment unit (POD 2) outside of AAE. This allows for patients to be seen, diagnosed, treated, and referred onto community services to prevent







A cancer or palliative diagnosis can leave you facing many challenges, from coping with your illness and treatment. Our Outreach Support Team based at the Walsall Palliative Care Centre are on hand to provide responsive and effective emotional support, using a holistic approach. They can help you understand every stage of the journey and answer any questions you might have. They will also help guide you to the services you need the most.
Within our team we facilitate Walsall’s only BAME Ladies Breast Cancer Support Group. This group provides support for women from disadvantaged communities who struggle with their cancer diagnosis due to various cultural and language barriers.

Our Outreach Support Team promotes equal access and aims to reduce social, cultural and language barriers, to ensure all individuals receive accurate information and access to all cancer and palliative care services within the local community.

During the Coronavirus pandemic, the support group had ceased to meet face to face. The health and wellbeing of our members was paramount as many were feeling isolated, experiencing a loss of independence, struggled with anxieties and health issues.Many did not understand the English literature on the pandemic or who to ask for help with testing kits. This encouraged the Outreach Team to look at innovative ways to contact and keep in touch with the support group.



We swiftly overcame this challenge by setting up our very first virtual BAME Ladies Breast Cancer Support Group. However, we stumbled across many difficulties. Firstly, not all group members had an email account.The instructions on creating an email account and installing MS Teams were predominantly in English. Hence, we resourced and provided this written information in different languages and videos. Soon we discovered and asked the more IT proficient group members to help the ladies that were struggling. Furthermore, our Trust IT department assisted with setting up and resolving software complications. With all involved we soon launched the first virtual support group meeting.

Members of the BAME Breast Cancer Support Group said they have become more confident with technology. They thoroughly enjoyed the visual interaction and felt fully supported.

Positive feedback from members:



“It has been a lifeline to speak and see someone”
“I am glad the Outreach Officer can explain this information in my own language”
Following on two years, due to technology advances and growing IT confidence the BAME Breast Cancer Support Group continue to meet virtually once a week opposed to monthly face to face. Overall, the support group look forward to the virtual support group meetings but would like face to face meetings to recommence in additional, when safe to do so.
Further to this the Outreach Team also set up a BAME Breast Cancer What's App Support Group for members to join.

(image below ) This was the last face to face BAME Ladies Breast Cancer Support Meeting before the coronavirus pandemic, this session was a Macmillan Art Workshop.




(image below) Our Information & Outreach Support Service also won an award for the work we do with the BAME and Hard to Reach communities.




In 2018, Walsall Healthcare NHS Trust was identified as a negative outlier in the National Hip Fracture Database, with an adjusted case mortality rate of 11.3% compared to 6.1%. In effect the pathway for fractured neck of Femur was…. broken.

During 2019 an MDT which consisted of Senior House Officer, Advanced Clinical Practitioner, Physiotherapist and T&O Consultant embarked on a Quality Improvement (QI) project to improve hip fracture care.Initially their aim was to reduce the mortality rate to below national average, but they needed to identify what was causing the problems. Analysis revealed concern in 3 areas: time to theatre, early patient mobilisation, and prompt delirium assessment.



The MDT members completed a series of PDSA cycles, making small improvements in all three areas. They completed fishbone and driver diagrams which helped identify specific factors leading to poor clinical outcomes. This systematic approach avoided overlap in improvement cycles and ensured that they did not try to change too many things at once and could see the benefits from their changes. And things were looking up, improvements in the three areas were being seen and the Trust’s position on the national fractured neck of femur database was moving forwards.
In 2020, a challenging pandemic year, 9% more patients underwent prompt surgery with a reduced average time from admission to theatre, aligning with the national average. Physiotherapist assessment the day after surgery improved by 7% and 99.7% of patients underwent 4AT delirium assessment. By April 2020,





The QI methodology combined with an MDT committed to small, consistent changes has reduced mortality and improved KPI’s. The team achieved its aim and have been work towards sustaining and making more improvements for a better, brighter future. In July 2021, the team submitted posters to the QI Awards event at the Trust, an overarching poster, and separate posters for the three areas previously identified.The independent judges scored the overarching poster the overall winner of the QI Awards.
And they did not stop there! The team have continued to look at other elements they can improve, applying consistent QI methodology, engaging their stakeholders, and measuring their data over time to see the improvement. Clinical Audits were used as a tool to study the overall outcome as well.

The team has been nominated in the Healthcare Quality Improvement Partnership (HQIP) Influencing Change Hero awards the results of which were announced on 15th June 2022 and… Yes! They were successful and have won the award, the amount of improvement, the level of involvement and the better experience for patients is fully deserving of this national recognition and there is no sign of them stopping there, they continue to see what other improvements they can make and ensure they are sustained.






Congratulations to the Team, a well-deserved award to recognise all the work that they have undertaken. Bravo!
 Trust: RWT
Trust: RWT
In August 2020, Health Education England (HEE) announced that £15m would be made available through its Clinical Placement Expansion Programme (CPEP) to increase clinical placements in the NHS and support growth in nursing, midwifery and AHPs. Aligning with the NHS Long term plan1, we are the NHS people plan2, and the new white paper Integration and innovation: working together to improve health and social care for all3, to have a future workforce fit for the NHS.




The Royal Wolverhampton NHS Trust (RWT) was successful in its bid and used the allocated funding to increase its annual physiotherapy student placements. The funding facilitated collaboration with RWT, Keele and Wolverhampton Universities to pilot innovative placement models and share case studies and best practice. Increasing placement capacity in community rehabilitation teams and primary care, improving the student experience, and giving them vital skills for the delivery of future health care. Improving educator experience, enabling physiotherapy students to experience the patient rehabilitation pathway post-pandemic, and improving the patient experience.

To enable the successful implementation of the programme the funding was used to recruit a link tutor. This position was vital in enabling the growth of placement capacity over the year.



The programme resulted in 72 additional placement offers (58% increase), 38 were apportioned to the University of Wolverhampton and 34 to Keele University. In total, RWT offered 196 placements during the 2020-2021 academic year.
Despite the challenges posed by the COVID-19 pandemic we successfully piloted innovative placement models, increased placement capacity, and enabled physiotherapy students to experience the patient rehabilitation pathway during a pandemic by utilising innovative service models incorporating telehealth consultations, which allowed an increase from a 1:1 model to a 4:1 model in some specialities. All of which ensured that students developed the skills required for the delivery of future health care.




To explore how students experienced the placements an anonymous online survey was distributed to students who were allocated new or alternative placement models to increase capacity. Out of the ten students who responded to the survey 100% reported they would recommend the placement to other students. Reporting they found peer learning particularly useful. Those who had self-directed study days found this beneficial, reporting it allowed them the time to consolidate their learning and research areas that they found more challenging.

Educators who trialled new or alternative placement models to increase capacity were also surveyed. Out of the five educators who responded, 100% reported they would recommend the alternative placement model to other educators. Those who offered a selfdirected study day a week found this day useful for both themselves and the students. They found it allowed them to catch up with administrative tasks whilst also allowing the students to catch up with reflections and consolidate their learning.





To enable the maintenance of the innovative placement model and expansion post-pilot the additional income from the placement tariff was used to embed the link tutor post within the physiotherapy workforce establishment. For our larger teams who can manage an overlap between placement dates or are providing a 2:1 model or greater, we plan to offer placements to both Keele University and the University of Wolverhampton. Work is also continuing to expand the community practice placements. To provide an additional four community teams able to facilitate regular placement opportunities as well as an additional three outpatient teams onto our placement rota. We have also embedded a successful Leadership Placement into our placement program by using a 2:1 model allowing students from both Universities to work collaboratively with one another whilst on placement. During the 2021-2022 academic year we have been able to offer 203 placements so far, with this number expected to rise further by offering ad hoc placements over the summer to students living locally but attending other universities not local to RWT.


We are also exploring the possibility of long-arm placements within care homes and hospice environments within Wolverhampton to allow students to gain experience in non-traditional settings.

Long-arm practice supervision is a process of supporting students in placements where their supervisor is located at a distance from the clinical practice learning area but is available for support. This means that the long-arm practice supervisor will not be with the student on a day-to-day basis so another named member of staff would support the student whilst they are on shift4.







The successful clinical placement expansion bid from RWT was an extremely well thought out and planned project, facilitating physiotherapy students to undergo placements during an extremely difficult time during a pandemic, enabling all Keele students to progress or graduate into the workforce. The project encouraged wider collaboration and sharing of innovation and best practice across the Trust and Keele University but also encouraged higher education institutes (HEI) to work together to ensure physiotherapy students at both Keele and Wolverhampton benefited from exposure to placements at RWT. The project was managed through a steering group, ensuring all stakeholders' outcomes focused not only on increasing the number of placements but also on the quality of placements, as described earlier in collating survey data to measure this.


The HEIs ran an engagement event for staff at RWT to educate and encourage the different placement models which had been accelerated due to COVID-19 and encouraged by the Chartered Society of Physiotherapy who state ‘There is no one-size-fits-all placement structure anymore as we need to change and adapt to meet the demand of increasing student numbers and the changes in the healthcare landscape’5. For example, 3:1/4:1 and hybrid approaches, where students rely less on a 1:1 Practice Educator approach and have self-directed study time to reflect, consolidate their learning and carry out service improvement projects. Keele students who took part in placements at RWT utilising these placement models, fed back that it encourages them to be more autonomous, an independent learner and use their initiative and the self-directed learning time, helping to develop their reflective skills and explore case studies in more depth. Educator support is crucial and HEIs have offered increased opportunities for collaboration, problem-solving and open discussion throughout the project, with the need to continue as the outcomes of the project are maintained.




The role of the link tutor, funded by the clinical placement expansion project, was key to success, being a consistent link between Practice Educators at RWT and the HEIs, increasing effective communication and problem-solving skills. RWT’s project plan ensured this was not a short-term goal and there is sustainability of all the work achieved in 2021-22. The Physiotherapy placement expansion project at RWT creates innovative opportunities for our students which will enhance their skills and exposure and will increase further, as the project is maintained and continues to evolve.





One of the key ambitions of the NHS Long Term Plan has also been to develop sustainable growth in the NHS workforce. A reduction in the number of NHS hospital beds in the last 30 years and movement of services out of hospitals has led to an increased need to examine placement learning opportunities needed for graduates to gain the clinical exposures to meet their programme outcomes. The total number of NHS hospital beds in England, including general and acute, mental illness, learning disability, maternity and day only beds, has more than halved over the past 30 years, from around 299,000 in 1987/88 to 141,000 in 2018/9, while the number of patients treated has increased significantly6. Enabling growth in placements in this historical context but also under the pressures of a pandemic have been challenging, however, this project has shown that adaptable thinking and target resource of a clinical educator and training can make all the difference.




The collaborative work undertaken with RWT and the Universities including the University of Wolverhampton has not only led to an increase in placement offers but also allowed creative thinking about the types of placements including the development of leadership placements and utilisation of different models such as team-based and hybrid approaches. This builds a rich legacy of supervision and assessment models for allied health professionals, including role emerging placements and long-arm supervision. From our learner perspective, 100% of students received a placement allocation and 100% would recommend the placement to a peer. The project has demonstrated an appetite for exploring diversification in the models used to support educators and students in the clinical setting. It also demonstrates where targeted funding can have a significant impact on placement offer growth.




1. The NHS Long Term Plan. Published Online First.; 2019. https://www.longtermplan.nhs.uk/
2. NHS England. We Are the NHS: People Plan 2020/21.; 2020. https://www.england.nhs.uk/wp-content/uploads/2020/07/We-AreThe-NHS-Action-For-All-Of-Us-FINAL-March-21.pdf
3. Smith, Helen. Integration and Innovation: Working Together to Improve Health and Social Care for All.; 2021. Accessed April 19, 2022. www.gov.uk/official-documents.



4. NHS Employers. Clinical placement supervision models. Accessed June 22, 2022. https://www.nhsemployers.org/articles/clinical-placement-supervisionmodels
5. The Chartered Society of Physiotherapy. Student placement innovations showcased in new CSP films. Accessed June 22, 2022. https://www.csp.org.uk/news/2021-05-17-student-placementinnovations-showcased-new-csp-films
6. The King’s Fund. The number of hospital beds. Kings Fund. Published 2019. Accessed June 22, 2022. https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/hospital-beds


 Author : Dr Nicky Eddison, Charlotte Tarbuck, and Dr Ros Leslie Trust : RWT
Author : Dr Nicky Eddison, Charlotte Tarbuck, and Dr Ros Leslie Trust : RWT
Our clinical workforce has a diversity of skills and experience. The journeys staff have taken into a clinical role are also diverse. This article explores the path taken by Charlotte Tarbuck, one of the Trust’s Assistant Practitioners, and discusses the role of the Allied Health Profession (AHP) support worker.
I started working in the NHS doing bank work on reception at a mental health hospital Trust. I progressed to a fixed-term contract post as a data input clerk at the Royal Wolverhampton NHS Trust, working as a band two in the therapy services department. My progression continued as I moved into a clerical officer role. In these roles, I learned many skills including organisation, communication, and IT skills. It was whilst I was in this role, I realised I would like to be more involved in patient care. I wanted a role which had a clinical element to it.
I have a history of competitive kickboxing, with a keen interest in running and swimming so physiotherapy was naturally of interest to me. I spoke to my manager who suggested spending some time shadowing the clinical teams on the wards to see what the roles involved. Shadowing the team cemented my ambition to become a support worker. I knew it wasn't going to be a glamorous role, but I could see how much the physiotherapists and occupational therapists were helping people and the impact of their work. I decided to apply for a band three AHP support worker role, and I was delighted to be appointed, becoming a member of the rehabilitation team.




I have a history of competitive kickboxing, with a keen interest in running and swimming so physiotherapy was naturally of interest to me. I spoke to my manager who suggested spending some time shadowing the clinical teams on the wards to see what the roles involved. Shadowing the team cemented my ambition to become a support worker. I knew it wasn't going to be a glamorous role, but I could see how much the physiotherapists and occupational therapists were helping people and the impact of their work. I decided to apply for a band three AHP support worker role, and I was delighted to be appointed, becoming a member of the rehabilitation team. Initially, it was frightening, and I felt overwhelmed by the amount of knowledge required. I felt out of my comfort zone and away from my previous skill set. I found the medical knowledge and abbreviations very difficult for the first few months and I felt the pressure of the increased expectations. Communicating with a large multi-disciplinary team (MDT), including consultants, was also daunting. I learned as I went along and eventually, I knew what I was doing and LOVED the job. I was able to make a difference in people’s lives and send them safely home from the hospital. I learned how to speak comfortably with the MDT to facilitate safe and effective care. Moving from an administration role, where I felt comfortable and knew what I was doing, to a scary acute medical ward where I felt out of my depth took courage, but it was the best thing I have ever done!




Even the smallest of things I do or say can make such a huge impact on a patient’s well being or quality of life. Listening to patients makes a huge difference. The skills I learned in my administration roles were all transferrable and helped me enormously.
My progression to an AHP Assistant Practitioner has given me increased responsibility, to be able to work unsupervised in an outpatient setting. I now carry out home visits and have my own caseload of patients, all whilst being able to seek input from registered AHPs when needed. My confidence has grown, and I have developed clinical and life skills beyond what I had envisaged. I am now hoping to start an access to healthcare course at college as a route into university to become a registered AHP in the future.








Charlotte’s experience, whilst outlining her journey into clinical practice, also explores the role of the AHP support worker. The importance of their work, the skills they have and the level of autonomy they practice. The role of the AHP support worker in providing high quality care across a range of services is varied. Take, for example, their vital role in public health. Being ideally placed to contribute to ‘make every contact count’ (MECC) conversations. Our AHP support workers are encouraged to talk to service users about healthy lifestyles, offering information about smoking, healthy eating, alcohol consumption, and physical activity. Signposting to appropriate services when required. Dietetic support workers provide lots of support for people with or at risk of diabetes, offering services for diabetes prevention, early intervention, and early detection of type 2 diabetes. Physiotherapy and occupational therapy support workers often signpost service users to community services as part of a holistic approach to their health and wellbeing.

Other examples of the role include occupational therapy support workers supporting employment, and vocational rehabilitation, of our service users. They play a key role in supporting individuals with health and disability issues to gain and stay in work. Physiotherapy support workers encourage independence for older children with learning difficulties or disabilities. They run training courses to encourage them to do as much as they are able for themselves, teaching them how to self-manage their condition and providing more information and training about the transition into adulthood. Referring children and families to charities for extra equipment e.g., medical devices needed for the home, a tricycle etc., to promote wider physical and social activities. They also help families to understand what support they are entitled to e.g., disabled living allowance for children, Motability, and advice on how charities can support them with funding for additional equipment.
Support workers often work with vulnerable patient groups. For example, occupational therapy support workers can support service users with dementia by establishing links with local community services. Support workers who work with vulnerable populations play a key role in monitoring their wider health and well-being. This includes screening the home during visits to ensure that they are looking after themselves.




Theatres in hospitals use the skills of our support workforce to reduce the anxiety associated with hospital visits and surgery, particularly for our vulnerable populations. During their visit, operating department practitioner support workers can work to maintain a calm, safe working environment for these groups so that they are comfortable during their procedure.




Orthoptic support workers can carry out the visual tests required by the Driver and Vehicle Licensing Agency (DVLA) to assess whether service users are fit to drive.

Safeguarding (supporting vulnerable communities) is a significant part of a podiatry support worker's role. This often involves partnerships with other professionals to ensure service users are safe and aware of the procedures which they are about to undergo. They also monitor signs of poor self-management or neglect when carrying out domiciliary visits or following up on missed appointments to see if the service user is at risk.




Support workers play an integral role in delivering safe and effective care and are a vital support to our registered allied health workforce. The Allied Health Professions Support Worker Competency, Education, and Career Development Framework1 was launched in October 2021. This new framework has been designed to enable employers to effectively plan, progress, and utilise their AHP support workforce. The framework guides training, education, and competencies. Providing a platform to harness the potential of the AHP support workers, ensuring they can achieve standardised levels of competency and access relevant training and development.



If Charlotte’s story resonates with you and you have an interest in becoming a support worker, reach out, ask questions, and take some time to shadow a colleague to learn more about the role. Step out of your comfort zone and challenge yourself! Similarly, if you have a story about your career journey please get in touch, we would love to share your story.


1. NHS Health Education England. Allied Health Professions Support Worker Competency, Education, and Career Development


Framework.; 2021. Accessed July 11, 2022. https://www.hee.nhs.uk/our-work/allied-health-professions/enableworkforce/developing-role-ahp-support-workers/ahp-support-workercompetency-education-career-development
 Dr Nicky Eddison
Dr Nicky Eddison



 Author : Dr R Leslie, C Scordis, and Dr N Eddison Trust: RWT
Author : Dr R Leslie, C Scordis, and Dr N Eddison Trust: RWT

Long term chronic conditions are the largest financial burden on public healthcare, furthermore, longer lives will affect the total amount of ill health and disability in the population, resulting in a major shift in the allocation of NHS resources. A vast body of evidence demonstrates the efficacy of targeted exercise interventions for the prevention and management of ageing long term conditions.By embedding exercise into clinical services, we can ensure that ageing and long term conditions are appropriately managed, reducing long term healthcare utilisation.


hysiotherapists working in NHS services have long delivered exercise interventions, with some physiotherapists choosing to undertake postgraduate study in exercise prescription and physiology to complement their physiotherapy practice. As with many NHS services, the demand for exercise rehabilitation services is growing rapidly and the current workforce cannot meet this demand. In some NHS Trusts, such as The Royal Wolverhampton NHS Trust (RWT), physiotherapists work alongside exercise physiologists, particularly in services such as pulmonary and cardiac rehabilitation. Having appropriate educational, professional, and regulatory standards for healthcare professionals is crucial for the delivery of safe, high-quality care.

The British Association of Sport and Exercise Sciences (BASES) has recently been working in partnership with Clinical Exercise Physiology UK (CEP-UK) to establish and promote the role of clinical exercise physiologists (CEPs) in the treatment and management of chronic and complex health conditions within the UK healthcare system. In December 2021, BASES, the professional body for sport and exercise sciences in the United Kingdom, and CEP-UK announced that CEPs had become eligible for professional registration.



TTheir collaborative work resulted in exercise physiologists being eligible for professional registration with the Registration Council for Clinical Physiologists (RCCP) which holds a voluntary register regulated by the professional standards authority for Health and Social Care. Enforcing high standards of practice and maintaining a public database9. This means that appropriately qualified individuals can apply to become registered and will be awarded the title of clinical exercise physiologist upon successful acceptance on the register.



These newly registered CEPs, working as part of a multi-disciplinary team of healthcare and rehabilitation providers, will be qualified health professionals. Proficient in exercise testing, exercise prescription and delivery of evidence-based interventions for the prevention, treatment, and long-term management of acute, subacute, chronic, and complex conditions.


CEPs require a minimum of 4 years of equivalent study up to Level 7 with a relevant undergraduate degree and Master’s degree in the area of clinical exercise physiology, such as cardiovascular health and rehabilitation. This training results in an excellent understanding of acute and chronic responses and adaptations to exercise in healthy and unhealthy individuals, as well as special considerations such as the influence of comorbid conditions and medications.
CEPs working in NHS settings will often be responsible for conducting exercise tolerance tests, designing exercise programmes, and formulating individualised exercise prescriptions for patients with chronic diseases. Additional competencies include patient counselling and education regarding risk factor management, including addressing barriers to maintaining exercise compliance.



The Scope of Practice for a UK clinical exercise physiologist clearly outlines the role of a CEP, provides examples of the conditions a CEP can work with, and suggests areas of employment. To ensure patient safety the outline of the scope of practice for CEPs, based upon knowledge and skills from an RCCP-accredited Master’s degree includes the criteria outlined in figure.





The document also describes core rules, regulations and boundaries and reminds CEPs that they must practice in accordance with the RCCP standards of Professional Conduct & Ethical Practice.




There are currently several exercise physiologists employed by the physiotherapy department at RWT, some working in cardiac and pulmonary rehabilitation whilst others are employed as physiotherapy support workers. Chris Scordis, who has recently applied for CEP accreditation, is a specialist exercise physiologist and lead for cardiac rehabilitation. Chris completed an undergraduate degree in sports science with physical education and chemistry and worked for two years in the fitness industry, while he completed a spin qualification and advanced personal trainer (with GP referral) qualification. This led him to start an applied sport and exercise science post-graduate diploma, with the link between Wolverhampton University and RWT’s cardiac rehabilitation service affording him an invaluable work experience opportunity within the department. Invaluable in that it resulted in RWT deciding to explore the benefits of recruiting exercise physiologists.

Throughout his two decades working at RWT, Chris has worked alongside physiotherapists and feels that the two professions complement each other well. Being a clinical educator for physiotherapy students, Chris is aware that there are aspects of exercise physiology and behavioural change that are not covered in detail in traditional physiotherapy degree courses. Thus, as an experienced exercise physiologist, Chris can share his knowledge with students whilst on placement in cardiac rehabilitation.




Figure 2: Chris Scordis in his role as a clinical exercise physiologist

Chris feels that professional registration is an important step towards creating workforce capacity and professional standards that will help integrate the fitness sector into healthcare pathways whilst recognising the knowledge and skills of CEPs. If you are an exercise physiologist with an interest in healthcare, Chris advises you to approach NHS Trusts for work experience/shadowing opportunities and keep up to date with vacancies.
CEP accreditation and registration have received mixed reactions from the physiotherapy profession, with some physiotherapists championing the role of exercise physiologists whilst others have expressed concern that the Chartered Society of Physiotherapy (CSP) council is in support of the development of CEPs13. As physiotherapists and CEPs, we must understand each other’s roles and value the knowledge and skills that each profession contributes to the delivery of safe and high quality patient care. Ensuring that rehabilitation is accessible to all who need it.


Chris Scordis is a Clinical Exercise Physiologist


Dr Nicky Eddison is an Associate Professor and AHP Research Lead.


Dr Ros Leslie is the Non Medical Research Lead and Chief AHP



 Author:Dr Nicky Eddison and Dr Ros Leslie Trust: RWT
Author:Dr Nicky Eddison and Dr Ros Leslie Trust: RWT

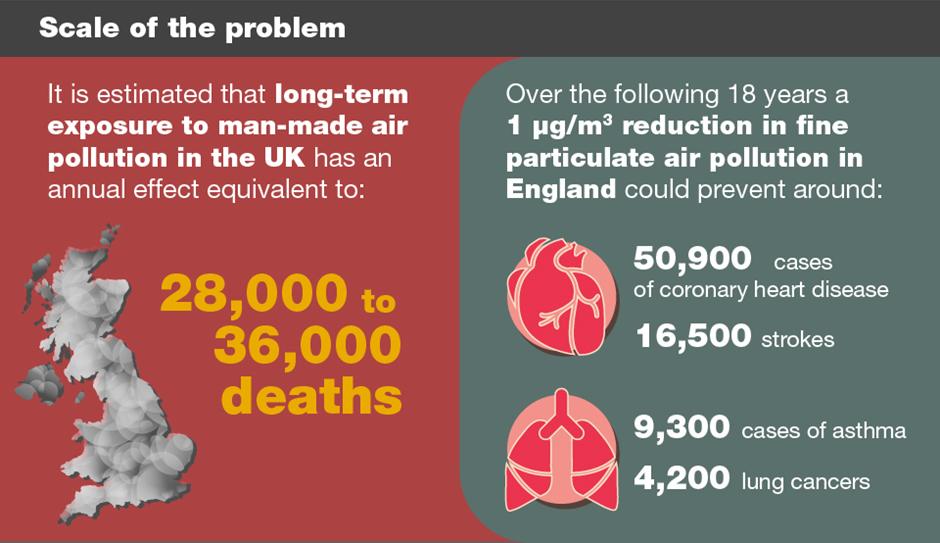
Poor air quality poses a significant environmental risk to public health in the UK. Long term exposure to air pollution is linked to chronic conditions such as cardiovascular and respiratory diseases as well as lung cancer, leading to reduced life expectancy. Similarly, the World Health Organization (WHO) provides evidence of links between exposure to air pollution and type 2 diabetes, obesity, systemic inflammation, Alzheimer’s disease and dementia. Thus, air pollution adds increased pressure on the NHS and health services across the globe.
Recently released air quality guidelines indicate that most people live in areas with poor air quality. Significant changes are required to ensure the UK meets these standards and in doing so reduces the 40,000 premature deaths each year in the UK due to air pollution4. Achieving NET Zero targets and becoming a more sustainable environment is a key NHS target5, including the reduction of face to face outpatient appointments by one third within the next five years.



The orthotics service at the Royal Wolverhampton NHS Trust (RWT) set out to adapt to the restrictions imposed by the COVID 19 pandemic whilst ensuring any changes met the goal of becoming a more sustainable, environmentally friendly service.
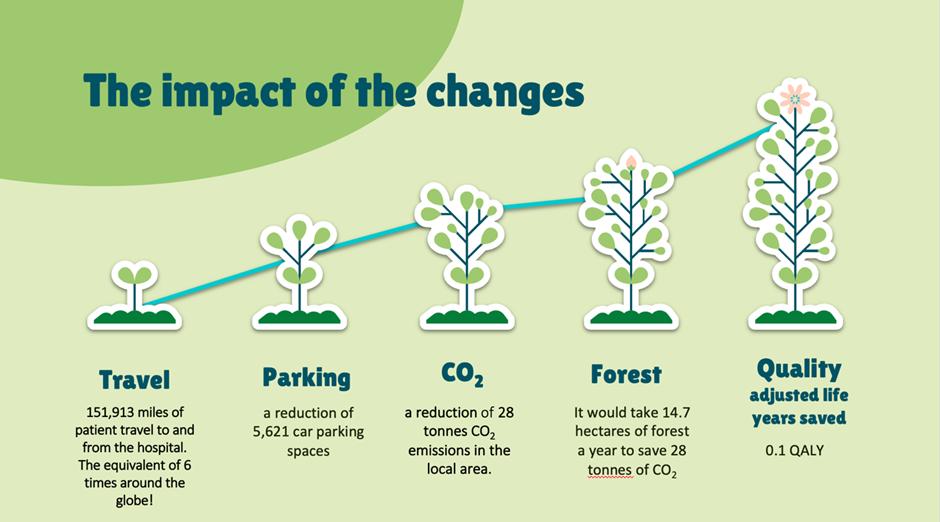
During March 2020 and September 2021, the introduction of telehealth consultations, that is a consultation carried out via a video call, saw a reduction of 53% of patients attending the department in person. This change in how select consultations were carried out resulted in a saving of 151,913 miles of patient travel to and from the hospital, which equates to a reduction of 28 tonnes CO2 emissions in the local area. To put it into perspective this is the equivalent miles it takes to travel around the world just over 6 times and would take 14.7 hectares of forest a year to capture that amount of CO2 (see figure 2).


The impact of this change is considerable when you consider the relatively small size of the orthotics service compared to other out patient services in the NHS and highlights the impact smaller services can have on the carbon footprint of the NHS.






A Freedom of Information request revealed that almost 80 per cent of mobility aids, such as walking sticks and crutches, are never returned to the NHS by patients. Statistics from 66 NHS Trusts in England revealed that over £14 million was spent on almost 560,000 walking aids over a 5 year period and 241,779 were never returned.The RWT are contributing to NHS England’s ‘Return and Reuse’ scheme for walking aids during 19 25 September 2022, in partnership with WRAP’s national Recycle Week. The RWT continues to encourage the return of metal walking sticks, crutches and frames and is refurbishing anything that is deemed safe to be reused within the NHS or elsewhere through donations to charities.



Medical Aid International is a company that works to improve healthcare across the developing world by supplying medical equipment and accessories. They are working with the physiotherapy department at the RWT to recycle and repair returned walking aids and will arrange for them to be delivered to low to middle income countries safely, quickly and with the correct paperwork.





Our diagnostic radiology department has recently installed a new MRI scanner which has “BlueSeal technology”, it contains virtually no helium. A traditional scanner uses liquid helium to chill the magnet to 269oC. This is what makes it superconducting and allows it to be super strong (It’s also what makes MRI scanners dangerous as you cannot turn a superconducting magnet off).
Helium reserves are running low and MRI scanners account for 20% of the helium consumption, it is therefore important to ensure we conserve stocks. Also, it takes a lot of energy to keep that helium compressed and in a cool liquid state. It wants to be a gas at room temperature and if that was allowed to happen, it would generate a huge plume of white helium smoke which would be emitted into the environment The Trust’s new BlueSeal scanner has new micro cooling tec This means it consume mperature as there is





All the initiatives discussed contribute to the Trust’s Green Plan (2020 25) which focuses on how the workforce can continue to provide high quality care for patients, while at the same time protecting our local environment and communities. The plan looks to review services and our use of resources to reduce carbon emissions and slow global warming. The RWT aims to become a sustainable Trust by using resources efficiently and responsibly within energy, water, waste, travel, procurement, and buildings. Whilst planning future service developments and new technologies there will be due consideration of the environmental impact of products, buildings, and services.

Action from the entire AHP community will ensure we collectively achieve the ambitions of improving health, saving money, and preserving the planet. The recently published AHP strategy for England9 has environmental sustainability: and greener AHPs as one of its areas of focus. With the ambition to embed new ways of working by building net zero into everything AHPs do including encouraging AHP services to Include net zero as a fundamental design principle in models of care. To achieve this, all AHPs will need a good understanding of the net zero agenda, and it will form a crucial part of their competencies.



The orthotics service was the 2021 winner of the Fab Change Sustainability Award and has been shortlisted for the Chief Allied Health Professions Officer’s Going Green award 2022.




“The orthotics team receiving their sustainability award: (Left to right: Ndana Mupawaenda, Lyn Wesley, Janet Smith, Sudi Nayyar, Miriam Williams, Nicky Eddison, Rachel Irwin, Kate Pugh, and Jo Billin Team members absent from the photo: Amie Dawson, Lisa Jones, Sharon Scott, Andy Parkes and Chris Bowdler).”



 Author : Enza Leone, Dr Nicky Eddison, Dr Aoife Healy, and Professor Nachiappan Chockalingam Trust: RWT
Author : Enza Leone, Dr Nicky Eddison, Dr Aoife Healy, and Professor Nachiappan Chockalingam Trust: RWT
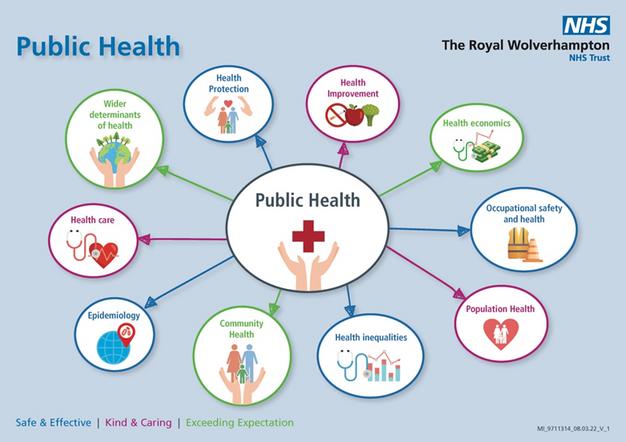
Over the last decade, the ageing populations, the rising numbers of people living in suboptimal health and the resulting increase in health and social care costs have highlighted the need to focus on a preventative model of care. This model needs to be aimed at improving population health and well being while keeping costs under control. With over 4 million patient contacts per week, the 170,000+ UK Allied Health Professionals (AHPs) from 14 different occupations who represent the third largest professional group in the NHS making up 6% of the total NHS workforce have a large scale routine contribution to the public’s health and wellbeing. Through their interventions, AHPs can affect the physical, mental, and social well being of individuals, communities, and populations.

AHPs’ significant impact on public health was officially recognised in 2015, following the publication of Rethinking the Public Health Workforce report, which acknowledged that AHPs are an integral part of the wider public health workforce. UK AHP professional bodies have responded to the call to action on public health contribution with enthusiasm and an appetite to understand how AHPs can make every contact count for improving the public’s health. This resulted in the production, in the same year, of the first AHP public health strategy (2015 2018), which saw the representatives of 12 AHP professional bodies, who constitute the AHP federation, and Public Health England (PHE), now known as The Office for Health Improvements and Disparities, (OHID) coming together to define the public health role of AHPs and the future AHP public health strategy.
The 14 AHP professions in England include art therapists, drama therapists, music therapists, chiropodists/podiatrists, dietitians, occupational therapists, operating department practitioners, orthoptists, osteopaths, paramedics, physiotherapists, prosthetists and orthotists, radiographers, speech and language therapists.

Available from: https://www.england.nhs.uk/ahp/role/



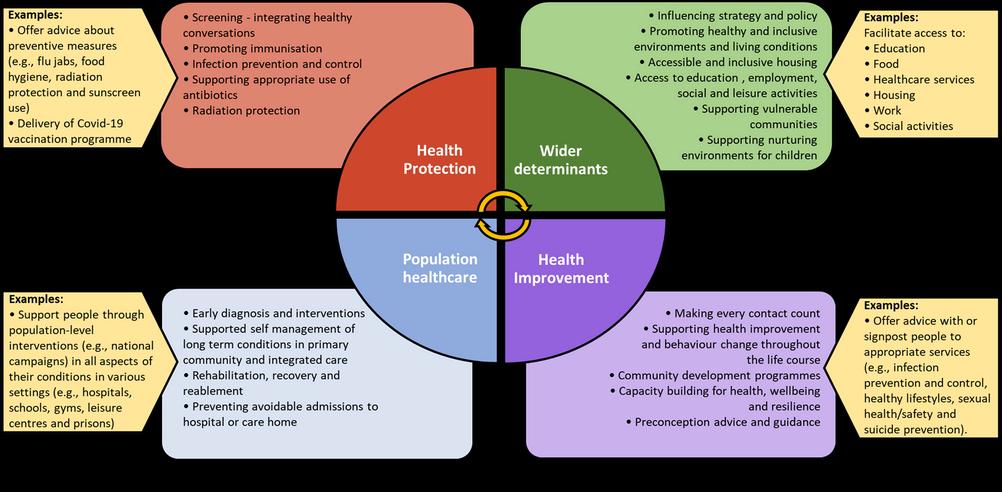
Four years later, a UK-wide AHP public health strategic framework4, which built on the previously published 2015-2018 strategic document valid for England and Wales3, was developed representing the collective intentions of the UK nations to adopt a united approach to public health for the allied health professions. The four UK countries agreed on a shared vision for how AHPs may contribute to public health across four domains (Figure 1):
·Wider determinants, also known as social determinants, are social, economic, and environmental factors that influence health and wellbeing. By addressing the wider determinants of health through specific targeted interventions, AHPs have the potential to contribute to reducing health inequalities.



·Health improvement describes the work that promotes healthy choices and addresses factors influencing healthy lifestyles (e.g., poverty and lack of educational opportunities), thereby improving the health and well-being of individuals and communities.

·Population healthcare aims to enhance health outcomes by focusing care on the population’s needs and providing person-centred services across the whole health care system.
·Health protection aims to prevent, assess, and mitigate risks and threats to people and populations’ health caused by infectious diseases and other preventable hazards.
Figure 1. Public health model for Allied Health Professionals (AHPs). Adapted from UK Allied Health Professions Public Health Strategic Framework5.


The AHP federation represent 12 AHP professional bodies, including art therapists, dietitians, drama therapists, music therapists, occupational therapists, orthoptists, paramedics, podiatrists, prosthetists and orthotists, physiotherapists, radiographers and speech and language therapists.


This four-domain public health model was considered relevant to the roles of the different AHP groups. Researchers at Staffordshire University discovered that although AHPs from the different professions were engaging in public health interventions across the four main public health domains, many were not recognising their interventions as public health despite them being linked to prevention and health improvement. This highlights that AHP interventions cover a broad and diverse range of public health practices. When interviewed about the public health areas they were engaging within their role, AHPs provided examples of their interventions in relation to each of the four public health domains (Figure 1). The way AHPs contribute to public health varies by profession and the following examples are not intended to be exhaustive.

·Wider determinants: AHPs carry out work to support people with access to a full range of health, welfare, educational and leisure time services (e.g., education, food, healthcare services, housing, work, education, and social activities). As part of this, they can support people overcome the barriers to access and the challenges they face (e.g., poor digital literacy and access to technology), thereby reducing health inequalities.



Health improvement: AHPs integrate Making Every Contact Count into their practice and have conversations with service users about areas of health they can offer advice with, or signpost them to appropriate services (e.g., infection prevention and control, physical activity and healthy lifestyle, smoking cessation, stress ·management, sleep hygiene, sexual health and safety, suicide prevention, and weight management).
·Population healthcare: AHPs can offer population-level interventions (e.g., national campaigns) aimed at supporting people with certain illnesses, disabilities, or special needs (e.g., mental health conditions, eating disorders, learning disabilities, attachment disorders, neurological conditions, and cardiac diseases) in the physical, communication, emotional, social, intellectual, and mental aspects of their condition and with the impact of their short- and long-term rehabilitation. AHP services are provided in a range of diverse settings, including inpatient and outpatient hospital services, mental health care, social care, gyms, leisure centres, schools, prisons, and the voluntary sector.



·Health protection: AHPs can offer advice about measures (e.g., flu jabs, food hygiene, radiation protection and sunscreen use) to adopt to prevent, avoid, and mitigate adverse health effects from communicable diseases or other preventable hazards. In response to the Covid-19 pandemic, AHPs have been involved in various schemes to address vaccine reluctance as well as encourage Covid-19 vaccine uptake and have actively participated in the immunisation campaign as vaccinators.







[1] MECC encourages conversations based on behaviour change methodologies (e.g., brief advice, behavioural change techniques) empowering individuals to make healthier lifestyle choices and exploring the wider determinants influencing their health.
Since the publication of the first UK AHP public health strategic document, AHPs have made a significant impact on the health of individuals, communities, and populations through a series of local and nationwide public health initiatives5. The Covid-19 pandemic has emphasised the importance of public health measures, prevention, and reduction of health inequalities and has highlighted the remarkable contribution that AHPs make to public health. Despite the significant progress already achieved to date, public health and disease prevention still need to be firmly embedded into AHP education programmes and the roles of all AHP professions, and pathways to public health careers for AHPs still need to be enhanced. These achievements represent key milestones along the path to embedding public health into every AHP role by 2024, which will hopefully result in increasing the profile of AHPs as valuable public health experts.






Royal Brompton and Harefield hospitals became part of Guy's and St Thomas' in February 2021, bringing together world-leading expertise and research in heart and lung disease.

We have over 500 IHSCM members from our London HUB.




Author: Elsie Mensah, Consultant Urologist, GSTT

Daghni Rajasingham, Deputy medical director, GSTT

Maj Shabbir, Consultant Urological Surgeon, Lead for Andrology, male infertility and genitourinary reconstruction, GSTT
Trust: GSTT
Guys Urology has a Friday educational meeting and one of the unique aspects is that consultants who have reached their 10 year anniversary are invited to reflect on their career and future aspirations. Maj Shabbir’s ten-year talk reflected on building the andrology unit including, male infertility, a sickle cell priapism service and the testicular Onco-tese service, which has radically changed practices for testicular cancer patients.
Maj Shabbir had an encounter with a testicular tumour patient and due to his background in fertility, decided to evaluate this patient’s semen parameters, though this was not standard practice at the time. He found that this patient was azoospermic (absent sperm in ejaculate) and this led to a series of events that highlighted to Maj the depth of this problem and the need for the uro-oncology community to serve these patients better.
He had already successfully established a micro-tese service at guys. This is a procedure for infertile men with low or absent ejaculated semen where areas of active sperm production are identified by examining the testicle under a microscope in theatre. He had high success rates in identifying sperm which could subsequently be used by these families in assisted reproduction techniques such as IVF. He led research work to retrospectively review tumour bearing testicles that had been removed in the past and showed >60% of these also contained areas of sperm production which could have been utilised to preserve fertility options for these men at the time of their surgery for testicular cancer. This procedure in tumour bearing testicles is called onco-tese.




Collaboration was essential to the success of the onco-tese service as colleagues from andrology, embryology and gynaecology needed to work at relatively short notice to meet the oncological timeframes for these patients.
Beyond GSTT however, real leadership has been required to ensure that testicular cancer patients across the country also have these fertility assessments and options. Education has been key. This work has been presented widely in local, European and international meetings and formed part of the basis for which the European Association of Urology amended guidelines to include a recommendation for semen parameters to be assessed in patients diagnosed with testicular cancer. There are further recommendations for appropriate patients to be offered Onco-tese, something Maj and indeed GSTT can be proud of.

The plan for the future is to develop nominated Onco-tese centres nationally to ensure that every patient has access to a local service thus ending the postcode lottery.



He remarks that GSTT is a place where innovative ideas which improve patient care are encouraged and nurtured. 'People line up to help’. Tips for clinicians keen to innovate and develop services is to have a clear plan, identify which individuals or teams are required and keep it personable - a face to face conversation often achieves more than several emails.



Finally, sharing positive outcomes helps to keep the team enthused. The team have a growing wealth of feedback, compliments and baby pictures from patients who have been helped through the range of fertility preservation options that this team is able to provide.










Our core existence is to support adult social care providers across Oxfordshire.

Currently we have Members covering more than 160 locations and we continue to develop links with many more with regular communications. We have annual contact with around 85% of registered providers in Oxfordshire and many non-registered services.
We work with Oxfordshire County Council and alongside our sister care associations as part of the Berkshire Oxfordshire and Buckinghamshire Integrated Care System.

We provide regular briefings for Members and the wider sector across the Thames Valley and we are part of the national Care Association Alliance.
Our strength is your engagement.


We are the local and national voice for adult social care providers across the six unitary local authority areas in Berkshire


All Care Quality commission registered providers are members of Berkshire Care Association providers and we provide an enhanced service for Executive Members.
We work with six small unitary councils; three are part of the Berkshire Oxfordshire and Buckinghamshire Integrated Care System and three
Williams Medical Supplies in Wales is our Primary Care HUB. We have worked with Williams for the past year and have helped to facilitate some of their great events. Williams Medical Supplies Ltd is a Wales based manufacturer and retailer of medical products to the primary care and secondary care markets. It is the largest supplier to general practice in the United Kingdom with a portfolio of products ranging from surgical instruments to pharmaceuticals.



Northamptonshire Healthcare NHS Foundation Trust and the University Hospital of Leicester are the home of our East Midlands HUB. IHSCM Membership is growing for our newest Regional HUB. and we are looking forward to an eventful 2022!






St Helens and Knowsley Teaching Hospitals make up the IHSCM North West Regional HUB. We currently have hundreds of members across this trust and have started planning some exciting in person events at this HUB for 2022! We look forward to hearing more about this trust in the next magazine edition.







The Integrated Care System for Devon (ICSD) is a partnership of health and social care organisations working together with local communities across Devon, Plymouth and Torbay to improve people’s health, wellbeing and care.
We have many exciting events planned for 2022 and we look forward to hearing more from our newest hub in the next edition.

Health, Education and Improvement Wales makes up the IHSCM Wales Country HUB.



HEIW have a leading role in the education, training, development and shaping of the healthcare workforce in Wales. Ensuring we have the right staff, with the right skills, to deliver world class healthcare to the people of Wales both now and in the future.
Established in 2018 as a Special Health Authority HEIW sit alongside health boards and trusts as part of NHS Wales.
At Hampshire Care Association, the goal is to ensure that care provision in Hampshire is of the highest standard and quality and that those requiring care receive it with dignity and compassion.

HCA membership consists of care providers of Residential, Domiciliary, Nursing, Learning Difficulty and Mental Health homes.



HCA work with:
Hampshire County Council (HCC)
Portsmouth City Council (PCC)
Southampton City Council (SCC)
HCA also continue to negotiate passionately with all of the above for a Fair Price for Care.
The West Midlands Care Association has been the voice of the care industry within the region for over twenty years. The Association offers the crucial support care providers require to deliver sustainable excellence within community, nursing, special needs and residential home settings.

The Association offers the crucial support Care providers require to deliver sustainable excellence within community, nursing, special needs and residential home settings.

Most services are delivered by the dedicated team at the Association office with support from our board members (Executive Team and Board Members)
A raft of far-ranging services enables members to spend more hours doing what they do best - care - while we carry out essential, timeconsuming tasks necessary for CQC compliance and business
Arden has a proud heritage in flexible learning. We’ve grown and evolved from our beginnings in 1990 as the chosen online learning partner for universities across Britain, to offer a new kind of learning experience, providing both online and blended learning that meets the changing needs of modern life.
Today, we offer more than 70 degree courses, many of which are accredited by leading professional bodies such as the British Psychological Society, the Chartered Management Institute, the Chartered Institute of Marketing, the Agency for Public Health Education Accreditation, and more.


We strive to do things differently, and believe in doing things better. With study centres across the UK in Manchester, Birmingham, London, and Leeds, as well as in Berlin, Germany, we offer our students the chance to gain life-changing degree qualifications no matter their background or personal circumstances.

Operational since March 2012, the London campus has become a key part of the UWTSD Group. Ideally located within the centre of one of the world’s most famous capitals, students are able to widely benefit from all that the city has to offer.

Studying at UWTSD London creates a unique experience combining the University’s nearly 200 years of academic learning with inspiring and innovative teaching and learning environment.

The London campus boasts a wide range of computing, business management, accounting, and health and social care courses. Featuring undergraduate courses such as BA (Hons) Business Management, BSc (Hons) Applied Computing as well as the Certificate of Higher Education: Skills for the Workplace and Skills for the Workplace (Health and Social Care) programmes.


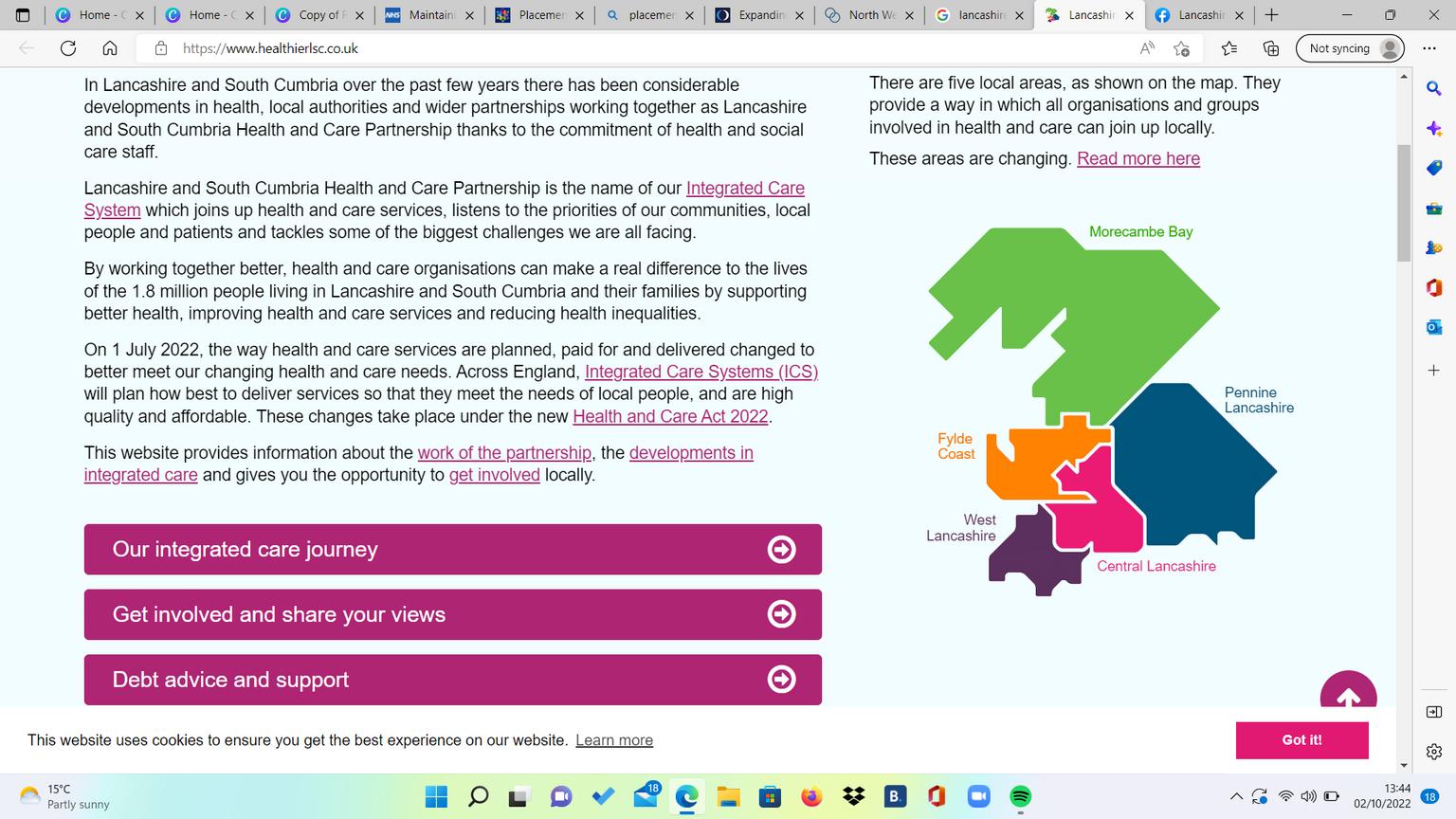
Lancashire and South Cumbria Integrated Care Board are home to our North West Care Hub.

Lancashire and South Cumbria Integrated Care Board (ICB) are part of the Lancashire and South Cumbria Health and Care Partnership, covering four local authorities: people’s health and wellbeing, and make sure everyone has the same
Lancashire CC Blackpool CC

The NHS Leadership Academy Graduate Management Training Scheme (GMTS) is home to our North East Education Hub.


The NHS Graduate Management Scheme (GMTS) is part of the NHS Leadership Academy since 2012, recruiting and developing NHS leaders with their multi award winning graduate training scheme.