
7 minute read
West Midlands - How do Allied Health Professionals Contribute to Public Health

How do Allied Health Professionals contribute to public health?
Author : Enza Leone, Dr Nicky Eddison, Dr Aoife Healy, and Professor Nachiappan Chockalingam Trust: RWT
Over the last decade, the ageing populations, the rising numbers of people living in suboptimal health and the resulting increase in health and social care costs have highlighted the need to focus on a preventative model of care. This model needs to be aimed at improving population health and well-being while keeping costs under control. With over 4 million patient contacts per week, the 170,000+ UK Allied Health Professionals (AHPs) from 14 different occupations – who represent the third largest professional group in the NHS making up 6% of the total NHS workforce – have a large-scale routine contribution to the public’s health and wellbeing. Through their interventions, AHPs can affect the physical, mental, and social well-being of individuals, communities, and populations.

October 2022



AHPs’ significant impact on public health was officially recognised in 2015, following the publication of Rethinking the Public Health Workforce report, which acknowledged that AHPs are an integral part of the wider public health workforce. UK AHP professional bodies have responded to the call to action on public health contribution with enthusiasm and an appetite to understand how AHPs can make every contact count for improving the public’s health. This resulted in the production, in the same year, of the first AHP public health strategy (2015-2018), which saw the representatives of 12 AHP professional bodies, who constitute the AHP federation, and Public Health England (PHE), now known as The Office for Health Improvements and Disparities, (OHID) coming together to define the public health role of AHPs and the future AHP public health strategy.
The 14 AHP professions in England include art therapists, drama therapists, music therapists, chiropodists/podiatrists, dietitians, occupational therapists, operating department practitioners, orthoptists, osteopaths, paramedics, physiotherapists, prosthetists and orthotists, radiographers, speech and language therapists. Available from: https://www.england.nhs.uk/ahp/role/

October 2022



Four years later, a UK-wide AHP public health strategic framework4, which built on the previously published 2015-2018 strategic document valid for England and Wales3, was developed representing the collective intentions of the UK nations to adopt a united approach to public health for the allied health professions. The four UK countries agreed on a shared vision for how AHPs may contribute to public health across four domains (Figure 1):
·Wider determinants, also known as social determinants, are social, economic, and environmental factors that influence health and wellbeing. By addressing the wider determinants of health through specific targeted interventions, AHPs have the potential to contribute to reducing health inequalities.
·Health improvement describes the work that promotes healthy choices and addresses factors influencing healthy lifestyles (e.g., poverty and lack of educational opportunities), thereby improving the health and well-being of individuals and communities.
·Population healthcare aims to enhance health outcomes by focusing care on the population’s needs and providing person-centred services across the whole health care system.
·Health protection aims to prevent, assess, and mitigate risks and threats to people and populations’ health caused by infectious diseases and other preventable hazards.

October 2022


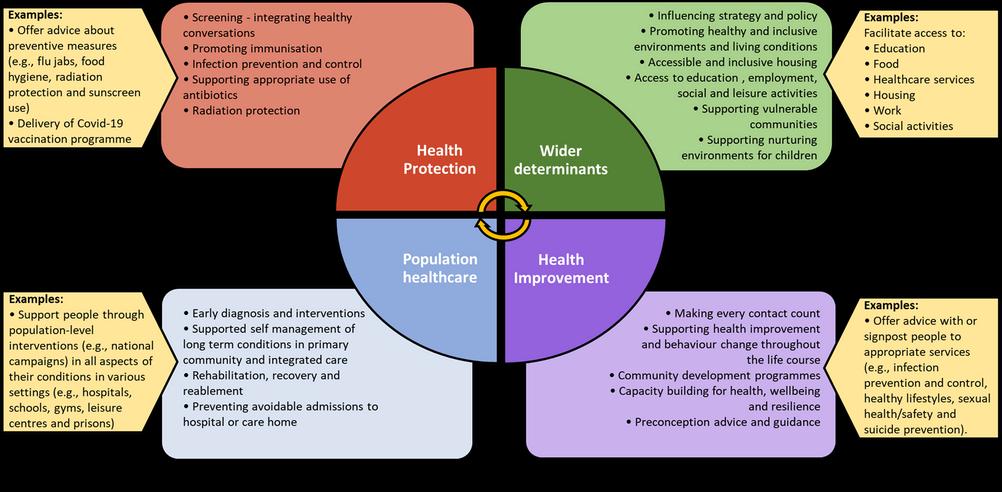
Figure 1. Public health model for Allied Health Professionals (AHPs). Adapted from UK Allied Health Professions Public Health Strategic Framework5.

The AHP federation represent 12 AHP professional bodies, including art therapists, dietitians, drama therapists, music therapists, occupational therapists, orthoptists, paramedics, podiatrists, prosthetists and orthotists, physiotherapists, radiographers and speech and language therapists.

October 2022



This four-domain public health model was considered relevant to the roles of the different AHP groups. Researchers at Staffordshire University discovered that although AHPs from the different professions were engaging in public health interventions across the four main public health domains, many were not recognising their interventions as public health despite them being linked to prevention and health improvement. This highlights that AHP interventions cover a broad and diverse range of public health practices. When interviewed about the public health areas they were engaging within their role, AHPs provided examples of their interventions in relation to each of the four public health domains (Figure 1). The way AHPs contribute to public health varies by profession and the following examples are not intended to be exhaustive.
·Wider determinants: AHPs carry out work to support people with access to a full range of health, welfare, educational and leisure time services (e.g., education, food, healthcare services, housing, work, education, and social activities). As part of this, they can support people overcome the barriers to access and the challenges they face (e.g., poor digital literacy and access to technology), thereby reducing health inequalities.

October 2022



Health improvement: AHPs integrate Making Every Contact Count into their practice and have conversations with service users about areas of health they can offer advice with, or signpost them to appropriate services (e.g., infection prevention and control, physical activity and healthy lifestyle, smoking cessation, stress ·management, sleep hygiene, sexual health and safety, suicide prevention, and weight management). ·Population healthcare: AHPs can offer population-level interventions (e.g., national campaigns) aimed at supporting people with certain illnesses, disabilities, or special needs (e.g., mental health conditions, eating disorders, learning disabilities, attachment disorders, neurological conditions, and cardiac diseases) in the physical, communication, emotional, social, intellectual, and mental aspects of their condition and with the impact of their short- and long-term rehabilitation. AHP services are provided in a range of diverse settings, including inpatient and outpatient hospital services, mental health care, social care, gyms, leisure centres, schools, prisons, and the voluntary sector. ·Health protection: AHPs can offer advice about measures (e.g., flu jabs, food hygiene, radiation protection and sunscreen use) to adopt to prevent, avoid, and mitigate adverse health effects from communicable diseases or other preventable hazards. In response to the Covid-19 pandemic, AHPs have been involved in various schemes to address vaccine reluctance as well as encourage Covid-19 vaccine uptake and have actively participated in the immunisation campaign as vaccinators.

October 2022






October 2022



[1] MECC encourages conversations based on behaviour change methodologies (e.g., brief advice, behavioural change techniques) empowering individuals to make healthier lifestyle choices and exploring the wider determinants influencing their health.
Since the publication of the first UK AHP public health strategic document, AHPs have made a significant impact on the health of individuals, communities, and populations through a series of local and nationwide public health initiatives5. The Covid-19 pandemic has emphasised the importance of public health measures, prevention, and reduction of health inequalities and has highlighted the remarkable contribution that AHPs make to public health. Despite the significant progress already achieved to date, public health and disease prevention still need to be firmly embedded into AHP education programmes and the roles of all AHP professions, and pathways to public health careers for AHPs still need to be enhanced. These achievements represent key milestones along the path to embedding public health into every AHP role by 2024, which will hopefully result in increasing the profile of AHPs as valuable public health experts.

October 2022











