The Utility and Limitations of Video-Based Review and Wearable Technology for the Assessment of Robotic Surgery Skills Nicholas 1Donald
1 Favazza ,
Yossef
3 Rubinov ,
Gary Deutsch,
1,2 M.D.
and Barbara Zucker School of Medicine at Hofstra/Northwell, 2Long Island Jewish Medical Center, North Shore University Hospital, 3Yeshiva University
Hypothesis
Conclusions
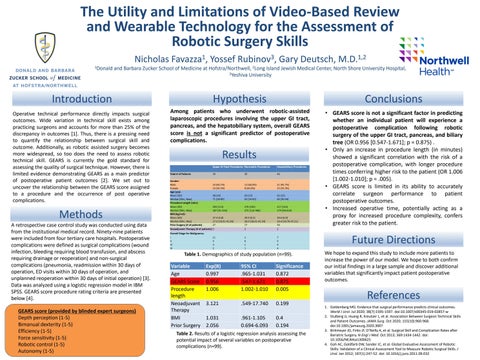
Among patients who underwent robotic-assisted laparoscopic procedures involving the upper GI tract, pancreas, and the hepatobiliary system, overall GEARS score is not a significant predictor of postoperative complications.
• GEARS score is not a significant factor in predicting whether an individual patient will experience a postoperative complication following robotic surgery of the upper GI tract, pancreas, and biliary tree (OR 0.956 [0.547-1.671]; p = 0.875) . • Only an increase in procedure length (in minutes) showed a significant correlation with the risk of a postoperative complication, with longer procedure times conferring higher risk to the patient (OR 1.006 [1.002-1.010]; p = .005). • GEARS score is limited in its ability to accurately correlate surgeon performance to patient postoperative outcomes. • Increased operative time, potentially acting as a proxy for increased procedure complexity, confers greater risk to the patient.
Introduction Operative technical performance directly impacts surgical outcomes. Wide variation in technical skill exists among practicing surgeons and accounts for more than 25% of the discrepancy in outcomes [1]. Thus, there is a pressing need to quantify the relationship between surgical skill and outcome. Additionally, as robotic assisted surgery becomes more widespread, so too does the need to assess robotic technical skill. GEARS is currently the gold standard for assessing the quality of surgical technique. However, there is limited evidence demonstrating GEARS as a main predictor of postoperative patient outcomes [2]. We set out to uncover the relationship between the GEARS score assigned to a procedure and the occurrence of post operative complications.
Results
Methods A retrospective case control study was conducted using data from the institutional medical record. Ninety-nine patients were included from four tertiary care hospitals. Postoperative complications were defined as surgical complications (wound infection, bleeding requiring blood transfusion, and abscess requiring drainage or reoperation) and non-surgical complications (pneumonia, readmission within 30 days of operation, ED visits within 30 days of operation, and unplanned reoperation within 30 days of initial operation) [3]. Data was analyzed using a logistic regression model in IBM SPSS. GEARS score procedure rating criteria are presented below [4]. GEARS score (provided by blinded expert surgeons) Depth perception (1-5) Bimanual dexterity (1-5) Efficiency (1-5) Force sensitivity (1-5) Robotic control (1-5) Autonomy (1-5)
Future Directions Table 1. Demographics of study population (n=99).
Variable Age GEARS Score Procedure length Neoadjuvant Therapy BMI Prior Surgery
Exp(B) 0.997 0.956 1.006
95% CI .965-1.031 .547-1.671 1.002-1.010
Significance 0.872 0.875 0.005
3.121
.549-17.740
0.199
1.031 2.056
.961-1.105 0.694-6.093
0.4 0.194
Table 2. Results of a logistic regression analysis assessing the potential impact of several variables on postoperative complications (n=99).
We hope to expand this study to include more patients to increase the power of our model. We hope to both confirm our initial findings in a large sample and discover additional variables that significantly impact patient postoperative outcomes.
References 1. Goldenberg MG. Evidence that surgical performance predicts clinical outcomes. World J Urol. Jul 2020; 38(7):1595-1597. doi:10.1007/s00345-019-02857-w 2. Stulberg JJ, Huang R, Kreutzer L, et al. Association Between Surgeon Technical Skills and Patient Outcomes. JAMA Surg. Oct 2020; 155(10):960-968. doi:10.1001/jamasurg.2020.3007 3. Birkmeyer JD, Finks JF, O’Reilly A, et al. Surgical Skill and Complication Rates after Bariatric Surgery. N Engl J Med. Oct 2013; 369:1434-1442. doi: 10.1056/NEJMsa1300625 4. Goh AC, Goldfarb DW, Sander JC, et al. Global Evaluative Assessment of Robotic Skills: Validation of a Clinical Assessment Tool to Measure Robotic Surgical Skills. J Urol. Jan 2012; 187(1):247-52. doi: 10.1016/j.juro.2011.09.032