LIVER TRANSPLANTATION
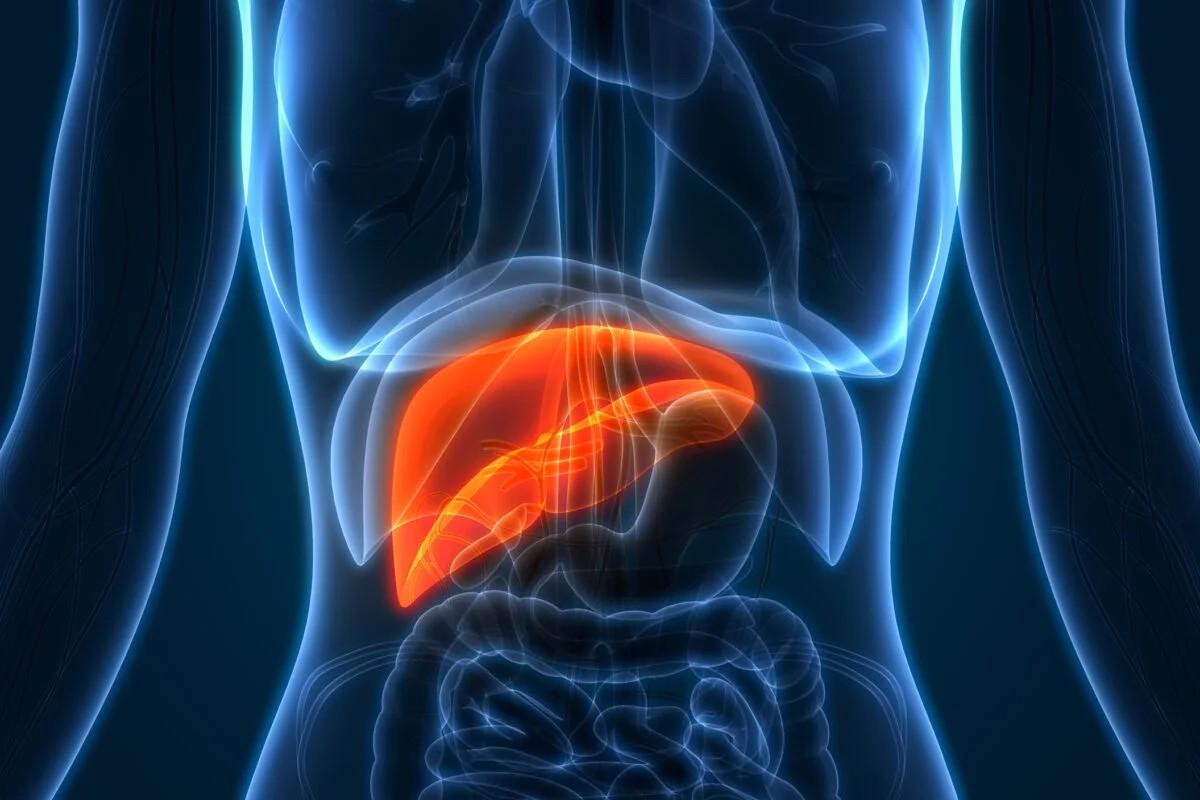
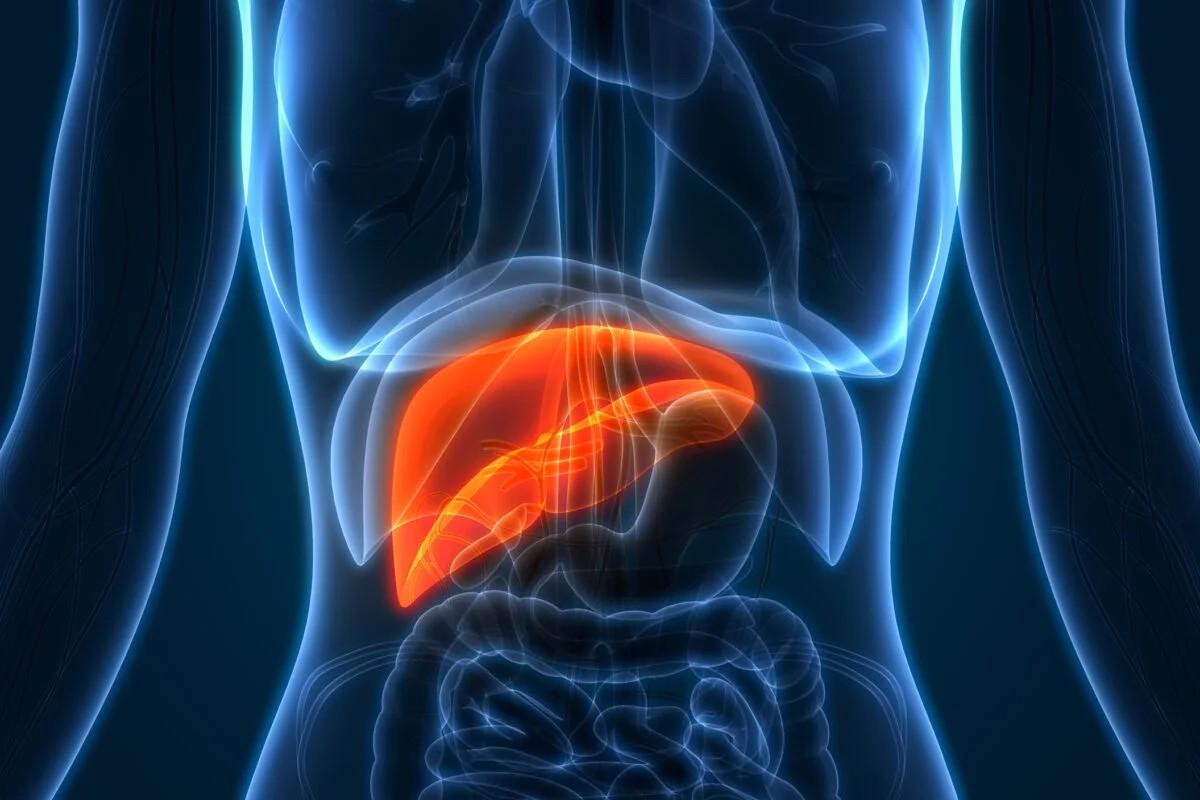
Liver transplantation is a life-saving procedure for patients with end-stage liver disease. This presentation explores the journey from diagnosis to transplantation, the surgical procedure, post-transplant care, and the impact on patients' lives. We will discuss the challenges faced by patients with liver disease, the organ allocation process, advancements in surgical techniques, the importance of immunosuppression, and the critical role of organ donation in saving lives.

Liver disease encompasses a range of conditions that affect the liver, such as cirrhosis, hepatitis, alcoholic liver disease, and genetic liver disorders. As liver disease progresses, it can lead to end-stage liver disease, characterized by severe liver damage and loss of liver function. In such cases, liver transplantation becomes necessary as the only viable treatment option.

1. Pre-operative Preparation: including blood tests, imaging studies, and consultations with a transplant team
2. Anesthesia and Incision: The surgery is performed under general anesthesia. Once the patient is sedated, the surgeon makes an incision in the upper abdomen to access the liver.
3. Removal of the Diseased Liver (Recipient):The surgeon carefully disconnects the blood vessels and bile ducts connected to the recipient's diseased liver
4. Preparation of the Donor Liver: If the donor liver is from a deceased donor, it is retrieved and preserved to maintain its viability.
5. Implantation of the Donor Liver:The surgeon carefully implants the donor liver into the recipient's body.
6. Reconstruction and Closure: Once the liver is successfully implanted, the surgeon ensures that all connections are secure and functioning correctly.
7. Post-operative Care: Medications, including immunosuppressants, are administered to prevent organ rejection.
8. Recovery and Follow-up: The patient's recovery period varies, but typically they remain in the hospital for several weeks.
Whole Liver Transplantation: In this technique, the entire liver from a deceased donor or living donor is transplanted into the recipient. This is the most common approach and is suitable for patients who require a full liver.
Split Liver Transplantation: In split liver transplantation, a single donor liver is divided into two parts. One part is transplanted into an adult recipient, while the other part is transplanted into a pediatric recipient. This technique helps maximize the use of available donor organs.

1. Intensive Care Unit (ICU) Monitoring:This allows healthcare professionals to closely observe vital signs, organ function, and address any immediate postoperative complications.
2. Immunosuppression Medications:To prevent organ rejection, patients must take immunosuppressive medications for the rest of their lives.
3. Follow-up Appointments:These appointments typically involve blood tests, imaging studies, and evaluations to monitor liver function, medication levels, and overall health.
4. Lifestyle Modifications:These may include maintaining a healthy diet, avoiding alcohol and tobacco, engaging in regular exercise, and adhering to any specific recommendations from the transplant team.
5. Infection Prevention:Patients are educated about infection prevention strategies, such as proper hand hygiene, avoiding exposure to sick individuals, and receiving vaccinations as recommended by the healthcare team.
6. Emotional and Psychosocial Support:Support from family, friends, and healthcare professionals is important to address these issues.
7. Long-term Monitoring and Maintenance: Patients will continue to have periodic check-ups to assess liver function, monitor for potential complications, and adjust medication dosages as needed.
1. Improved Physical Health:

2. Increased Longevity:
3. Enhanced Psychological Well-being:
4. Freedom from Restrictions:
5. Improved Cognitive Function:
6. Reduced Healthcare Utilization:
7. Impact on Relationships and Social Life:
The cost of a liver transplant can vary significantly depending on various factors such as the country, the hospital, the complexity of the case, the patient's overall health, and any complications that may arise during the procedure. It is important to note that the following figures are approximate estimates and can vary widely:
1. Pre-transplant Evaluation and Workup:$5,000 to $10,000.
2. Transplant Surgery:$250,000 to $800,000
3. Hospitalization and Post-transplant Care:$30,000 to $60,000
5. Follow-up Care and Monitoring:$5,000 to $10,000.
In India, liver transplant surgeries are conducted in several reputed hospitals known for their expertise in transplantation. Some of the well-known hospitals for liver transplantation in India include:
1. Apollo Hospitals, Chennai
2. Fortis Hospital, Delhi
3. Max Super Specialty Hospital, Delhi
4. Manipal Hospitals, Bangalore
5. Kokilaben Dhirubhai Ambani Hospital, Mumbai
6. Medanta - The Medicity, Gurgaon
7. All India Institute of Medical Sciences (AIIMS), New Delhi
The cost of a liver transplant in India can range from approximately INR 20 lakhs to INR 40 lakhs or more (USD 28,000 to USD 55,000 or more). This cost generally includes pre-operative evaluations, surgery, hospital stay, surgeon fees, anesthesia charges, and post-operative care for a specific period.
1.Life-saving treatment: Liver transplantation is often the only effective treatment for end-stage liver disease or acute liver failure. Without a transplant, these conditions can be fatal. A successful liver transplant can significantly extend the recipient's life and improve their quality of life.
2. Resolves liver failure: Liver failure can lead to numerous complications, such as jaundice, fatigue, fluid accumulation, mental confusion, and bleeding disorders. Liver transplantation replaces the diseased liver with a healthy one, resolving liver failure and restoring normal liver function.
3. Improved quality of life: Liver transplantation can greatly enhance the recipient's quality of life. Once the transplanted liver starts functioning properly, many symptoms associated with liver disease, such as fatigue, itching, and pain, are alleviated. The recipient can resume normal daily activities and enjoy a more active and fulfilling life.
1.Organ rejection: One of the main risks after liver transplantation is the recipient's immune system recognizing the transplanted liver as foreign and launching an immune response to attack it. To prevent this, recipients must take immunosuppressive medications for the rest of their lives, which can have side effects and increase the risk of infections.
2.Infection: Immunosuppressive medications that are necessary to prevent organ rejection can weaken the immune system, making the recipient more susceptible to infections. Common infections after liver transplantation include bacterial, viral, and fungal infections. Careful monitoring and appropriate preventive measures are taken to minimize the risk of infections.
3.Surgical complications: Like any major surgery, liver transplantation carries risks related to the surgical procedure itself. These can include bleeding, blood clots, infections at the surgical site, bile leakage, and damage to surrounding structures.
HMSDESK assists patients to find the best medical services in India. Get Cost Estimates for Best Surgeons from leading Hospitals in India within 24 Hrs.

