Searching for a higher level of healthcare in Las Vegas? At ArchWell Health, you’ll enjoy a community of caring that’s totally focused on you and your needs as an older adult. Plus, we’re:
• Right in your neighborhood
• Ready to see you today
• On a first-name basis with our members



Special Publications Editor SIERRA SMART
Managing Editor/News DAVE MONDT
Staff Writers KYLE CHOUINARD
GRACE DA ROCHA, HILLARY DAVIS, KATIE ANN MCCARVER, AYDEN RUNNELS
Copy Editor ABRAHAM KOBYLANSKI
Photo Coordinator BRIAN RAMOS
Staff Photographers CHRISTOPHER DEVARGAS, STEVE MARCUS, WADE VANDERVORT
Publisher of Digital Media KATIE HORTON
or call (725) 269-3368.
Primary Care for Las Vegans Age 60+ Start your journey at


Senior Advertising Manager MIKE MALL, ADAIR MILNE, SUE SRAN
Account Executives LAUREN JOHNSON, GIANNA PUCCI, ANNA ZYMANEK
Sales Executive Assistants APRIL MARTINEZ
Web Content Specialist CLAYT KEEFER
Vice President of Manufacturing MARIA BLONDEAUX
Production Director PAUL HUNTSBERRY
Production Manager BLUE UYEDA
Associate Marketing Art Director BROOKE EVERSON
Marketing Graphic Designer CARYL LOU PAAYAS
Senior Traffic Coordinator DENISE ARANCIBIA
Traffic Coordinator KIMBERLY CHANG
Production Artist MARISSA MAHERAS
Route Administrator KATHY STRELAU
Fulfillment Operations Coordinator CASANDRA PIERCE
Distribution Relations Liaison JIDAN SHADOWEN
Events Director SAMANTHA PETSCH
Events Manager HANNAH ANTER
Event Sales Coordinator MELINA TAYLOR
CEO , Publisher & Editor BRIAN GREENSPUN
Chief Operating Officer ROBERT CAUTHORN
Managing Editor RAY BREWER
Associate Publisher ALEX HAASE
VEGAS INC
2275 CORPORATE CIRCLE, SUITE 300 HENDERSON, NEVADA 89074 | 702.990.2550
Creating the Top Doctors issue of Health Care Quarterly takes many months. Doctors across the Valley received letters in the spring of 2024 soliciting nominations for their peers. They then submitted an online form recommending local doctors. Once nominations were received by Vegas Inc, they were checked against the Nevada State Board of Medical Examiners or the Nevada State Board of Osteopathic Medicine.
The resulting list is comprised of doctors recommended by doctors. It includes specialists and general practitioners from a range of medical disciplines. We know how important it is to have a health team you can trust, and it’s an honor to share this resource in the hopes that it will help Southern Nevadans find the best doctor to meet their health care needs.
We also benefit from the many individuals who donate their time to educating the public by writing for this publication. Dylan Wint, Medical Director at Cleveland Clinic Lou Ruvo Center for Brain Health shared a recap of the progress made by the clinic during the past 15 years and how that progress lays the groundwork for future research in the treatment of neurological diseases.
programs and UMC of Southern Nevada. They are committed to fostering an environment that will offer the highest levels of care to Southern Nevada and meet the needs of the growing community.
A growing community also needs resources for specialized care. HealtHIE Nevada works diligently to coordinate information between Veterans Affairs and local health care providers to improve patient care for active-duty military and veterans. With hundreds of thousands of veterans and active-duty military in Nevada, organization and collaboration for health care is essential to take the best possible care of these service members.

UNLV is also laying a foundation with the development of its academic health center. An academic health center, by definition, consists of a medical school, at least one other health profession school or program and at least one affiliated or owned teaching hospital.
The UNLV academic health center consists of a partnership between the Kirk Kerkorian School of Medicine, UNLV Health, the UNLV schools of Nursing, Public Health, Dental Medicine, Integrative Health Sciences, other behavioral health
Specialized care can also mean spreading awareness of health factors present because of the climate we live in and the environmental systems in place around us. Rick Vinuya, chief of Optum Allergy Care weighs in on what local flora cause seasonal allergies and how to avoid and respond to allergy flare ups.
The health care providers that live and work in Southern Nevada are dedicated to the residents here, demonstrated time and time again by the exceptional care they provide for their patients and for the time and talent they invest in research and education.
I want to thank the doctors who nominated their peers for this publication and the Top Doctors themselves for their tireless commitment to their community. You provide health and healing to many and we honor you for it.
Sierra Smart
Special Publications Editor sierra.smart@gmgvegas.com
Comprehensive Cancer Centers would like to congratulate the 2024 Vegas Inc Top Doctors.
Our local health care professionals work selflessly to provide compassionate treatment to patients across Southern Nevada, certainly inclusive of so many honored here. We are proud to support and recognize the heroes in our health care community, including some of our own physicians, by sponsoring this program each year.
For more than 40 years, the physicians at Comprehensive have provided the highest quality care in medical oncology, hematology, radiation oncology, breast surgery, pulmonary services, cancer genetic counseling and clinical research.

The dedicated professionals at Comprehensive are committed to continuing to enhance the patient experience by recruiting the best physicians and advanced practice providers, investing in technology, spearheading proactive community initiatives and advocating for the vitality of our community wherever possible.
It is a priority to recruit and retain top talent in our community to increase access to patient care. Comprehensive has embarked on a recruitment effort to hire new oncologists, breast sur-
geons and advanced practice providers, with plans to start a benign hematology clinic where patients with blood disorders can see a provider faster than waiting for an oncologist. This will allow our doctors to prioritize cancer patients.Long term plans also include adding another location in a growing area of the Las Vegas valley.
Comprehensive remains committed to the Las Vegas valley so that residents can receive the best possible care closest to home without having to leave the city. We are proud to support the health care community and recognize outstanding medical professionals by sponsoring this program for twelve years strong. Congratulations to all the 2024 Top Doctors on your noteworthy contributions. May we together continue to push the local medical community forward while making our patients proud.
Sincerely,
Paul Dieter Executive Director Comprehensive Cancer Centers




































































All of the Dignity Health acute care hospitals in Southern Nevada—Siena Hospital, San Martin Hospital and Rose de Lima Hospital—have been recognized as LGBTQ+ health care equality high performers in the Human Rights Campaign Foundation’s 2024 Healthcare Equality Index. Each hospital updated dozens of policies to support LGBTQ+ health care outcomes, expanded training for staff and clinicians, updated patient forms and IT processes to better capture preferred pronouns and solicit feedback from LGBTQ+ patients, and clarified wording in employee benefits to be explicitly inclusive of LGBTQ+ employees.

The neonatal intensive care unit at Sunrise Children’s Hospital in Las Vegas, celebrated 50 years of care in the community. The NICU, which cares for more than a thousand babies every year, opened in 1974. Sunrise Children’s Hospital offers a full array of comprehensive care for the state’s smallest and sickest babies and has an extensive neonatal surgical program.
14 Examining how medical devices are classified, approved and brought to market
16 UNLV’s academic health center laying foundation for our health care future
20 Vegas Inc unveils its list of 2024 Top Docs
34 Transform your space into a place that promotes health and harmony
40 UMC’s transplant capabilities extend to pancreas
48 News and updates from the Las Vegas medical community
At Dignity Health, we believe humanity holds the power to heal. That’s why we’re honored that three of our own have been recognized by Health Care Quarterly as 2024 Top Doctors. Thank you for your dedication and unending pursuit of excellence.

Alexandra Aguilar, MD Pediatric Endocrinology

Nelson Huang, MD Emergency Medicine

Michael Wood, MD Cardiovascular Surgery





BY ALI KHALAF, MS, CGC
Approximately 10% of all cancers have a hereditary component. During a cancer genetic counseling session, these components and risk factors are assessed and tested for. Not everyone with a change in a cancer gene will develop cancer, but their risk is increased.
Genetic risk assessments and counseling are vital for early detection efforts and customizing management and treatment plans.
Some of the common hereditary cancer conditions that may contribute to a cancer diagnosis include hereditary breast and ovarian cancer syndrome and Lynch syndrome.
According to the American Cancer Society, changes in specific genes are attributed to more than 50 hereditary cancer syndromes. Many people with changes in these cancer genes have increased risk of developing cancer at younger ages. Genetic testing for high-risk patients is recommended and a standard of care in oncology today.
It is important to know if you or your family members have a hereditary predisposition to cancer because there are options that may reduce the risk of developing cancer. Treatment options are tailored to an individual’s risks and lifestyle, but management care plans can include specific cancer screening exams, medications and/or preventive surgery. If possible, the best person in the family to test is the person who has cancer.
Initial cancer genetic counseling sessions typically take less than an hour. A medical provider will gather your personal medical history, family history, provide education and collect your DNA via a simple saliva or blood test.
Your medical history and family history are the foundation for the risk assessment and the basis
for identifying if you are at an increased risk for developing certain cancers. This includes information about your mother, father, aunts, uncles, grandparents, siblings and your children—who had cancer, what type, and how old they were when diagnosed. These histories determine whether further discussion or genetic testing is needed.
If it is determined that testing is recommended, educational materials on cancer genetics and hereditary syndromes will be provided.
Meeting with a cancer genetic counselor is a necessary step in the process and critical in helping make informed decisions about testing. During the meeting, you will be provided with information on the specific test being performed, what the results mean, psychological implications of test results, confidentiality issues and the options for risk estimation without genetic testing. Additionally, you will learn about the risk of passing a gene change to a child, fees involved in testing, options and limitations of medical surveillance, strategies for prevention after testing and the importance of sharing your genetic test results with at-risk relatives. Results are typically available two to three weeks after testing. Results are disclosed in a way that helps patients understand the implications of a positive, negative or inconclusive result. Providers will offer guidance on how to share the results with family members and how the test results may affect them. There are many medical management options available to those who test positive and you will be referred to the appropriate medical provider for follow up.
Comprehensive Cancer Centers’ genetic screening program helps ensure that patients receive the most current and recommended services in oncology care. This program was the first of its kind at an oncology practice in Southern Nevada and has been fortified in recent years with a strong genetic counselor/nurse practitioner team that carries out the testing.
BY MARSHALL HILL, DO
Asteroid hyalosis is a degenerative eye condition that gives the appearance of glittering yellow or white particles inside the eye, creating an effect that resembles a galaxy.
This occurs when small white calcium deposits float in the vitreous humor in the back of the eye. The deposits are attached to the collagen fibers of the vitreous, which means they will remain suspended there rather than sink to the bottom of the eye.
The calcium deposits look white in direct light but appear gold when viewed from the side with an ophthalmoscope. Fortunately for the patient, it doesn’t usually cause vision problems. Patients often don’t realize they have asteroid hyalosis because it does not affect their eyesight, and treatment is rarely needed.
Asteroid hyalosis is considered common, occurring in about one in 200 people, usually in adults 60 or older. According to the Cleveland Clinic, 80% of people with this condition only have it in one eye, and men account for about 60% of cases.
Asteroid hyalosis rarely causes visual symptoms, and treatment is not necessary, but once the condition has developed, it is permanent. If visual symptoms do occur and are significant enough to decrease vision, a surgical procedure called a vitrectomy can be performed.
The crystals that form the asteroid bodies have some similarities to gallstones and kidney stones. Because of these similarities, some researchers believe there is a link between these conditions, but more research is necessary to solidify the connection.
While doctors aren’t exactly sure of a cause, studies have found that people with diabetes
Type 2, high cholesterol and high blood pressure could be more likely to develop asteroid hyalosis. It may also be a rare side effect of certain eye procedures, like cataract surgery. Asteroid hyalosis can be diagnosed by an eye exam using lenses and lights to look into the back of the eyes. Your doctor may also recommend additional tests to rule out other conditions that can have similar effects.
Tests could include fluorescein angiography, which detects issues like new blood vessel growth due to diabetes-related retinopathy, or optical coherence tomography that is used to detect diabetes-related retinopathy, tumors in the eye, macular conditions or glaucoma.
Asteroid hyalosis rarely causes visual symptoms and treatment is not necessary, but once the condition has developed, it is permanent.
If visual symptoms do occur and are significant enough to decrease vision, a surgical procedure called a vitrectomy can be performed to remove the deposits and replace the vitreous in your eye.
During a vitrectomy, the vitreous of the eye is removed and replaced with either saline fluid, silicone oil or a gas bubble to maintain the natural shape of the eye. If you experience any of the following vision symptoms you should seek immediate attention: sudden vision loss, sudden flashes of light (known as photopsia), black spots or floaters (especially if they appear suddenly) and/or darkening vision.


Dylan Wint, MD, is Medical Director at Cleveland Clinic Lou Ruvo Center for Brain Health
BY DYLAN WINT, MD
This year is the Cleveland Clinic Lou Ruvo Center for Brain Health’s 15th anniversary. The progress that has been made in the treatment of cognitive disorders, movement disorders and multiple sclerosis since the clinic opened in Las Vegas in 2009 is worthy of reflection.
Perhaps the most significant milestone impacting care for Nevadans was administering the clinic’s first infusion of the anti-amyloid drug, lecanemab, for the treatment of mild Alzheimer’s disease in 2023. After more than 20 years without any new treatments for the disease, this was a breakthrough. It was the first fully FDA approved drug to slow the progression of Alzheimer’s disease.
In addition to drug development, there is a growing recognition of the importance of lifestyle modifications in reducing the risk for cognitive decline from Alzheimer’s disease. The 2020 opening of the Women’s Alzheimer’s Movement Prevention and Research Center at Cleveland Clinic is a prime example of this.
By focusing on sustainable healthy lifestyle modifications, this center aims to reduce the risk of Alzheimer’s disease and is the first and only such program in the country exclusively for women.
The momentum today in the treatment of Alzheimer’s disease is similar to the success seen in the field of multiple sclerosis nearly 30 years ago when the FDA approved the first drug shown to reduce disability and slow down disease progression. Many other effective medications have emerged since, including five MS treatments that were tested at the Lou Ruvo Center for Brain Health and are now available nationwide as standard-of-care.
The Lou Ruvo Center for Brain Health will
continue to be at the forefront of clinical milestones in the treatment of neurological diseases. By identifying indicators of Parkinson’s disease progression, physician-scientists will be able to better predict disability and, ultimately, slow or prevent it. As the only site in Nevada to participate in the Michael J. Fox Foundation’s Parkinson’s Progression Markers Initiative study, the Cleveland Clinic is taking a step in that direction.
In the next 15 years, professionals expect to see more profound breakthroughs in Alzheimer’s disease care, especially the development of new therapies targeting different aspects of the disease beyond amyloid. The Cleveland Clinic anticipates a greater emphasis on prevention, early intervention and caregiver support programs in the years to come.
In MS care, researchers are working to develop new therapies that can not only slow down disease progression but can repair or reverse nerve damage.
Although there is no cure for these neurological conditions, the Lou Ruvo Center for Brain Health continues to improve the lives of Nevadans affected by these devastating diseases. As the number of treatments in the pipeline grows, so does the number of people needed to test these medications, underscoring the necessity of “citizen scientists”— research volunteers.
Individuals from various age groups, ethnic and racial backgrounds, sexual orientations, gender identities, and even people with normal cognitive function are needed to participate.
Participation in Cleveland Clinic Lou Ruvo Center for Brain Health’s clinical trials program is free and open to the public.
To learn more about how you can get involved, visit HealthyBrains.org/AHEAD or call 702-701-7944.
BY RICK VINUYA, MD
Does your nose get stuffy and do your eyes start to itch each spring or fall?
If you’re sneezing, sniffling, dripping and frequently clearing your throat, you could be suffering from allergies.
According to the Centers for Disease Control and Prevention, more than 25% of adults and 18% of children suffer from seasonal allergies. Allergic rhinitis, when your nose gets irritated by something you’re allergic to, accounts for 4.1 million doctor’s office visits per year. Moreover, allergies can predispose a person to shortness of breath, fatigue and headaches.
An allergy occurs when your immune system encounters an allergen—which can be an otherwise harmless foreign substance like dust mites, pet dander or pollen—and responds as if it were a germ or virus. This response causes unpleasant symptoms such as itching, sneezing and more.
So, what are the most common allergens in Southern Nevada?
Fall can be a difficult allergy season because ragweed pollen is present from late August to November. Sagebrush and other weeds can also cause fall allergies.
Spring allergies often occur because mulberry and olive trees are pollinating. Though they are banned from being planted and sold in the Valley, they are still found in many areas, and pollen from these trees is the primary cause for many local allergy symptoms. Other spring allergens include grass pollen, especially Bermuda grass, and pollen from trees such as mesquite and oak.
Following basic preventative measures and re-
ducing exposure to things that trigger allergy symptoms are the best ways to respond to allergy flare-ups. Here are some tips for surviving allergy season:
n The highest pollen counts typically occur earlier in the morning, so try to move your outdoor recreation to early evening and shower afterwards.
n Change and wash the clothes you wear after outdoor activities.
n Wash your bedding frequently.
n Keep your windows and doors shut.
n When grooming your pet, do so outside the home to reduce the amount of pet dander inside.
n Wash your pet once a week and wash your pet’s bedding on a regular basis.
n Use certified asthma and allergy friendly filters and change them as recommended.
n Check the local news or online sources for pollen forecasts and avoid time outdoors when pollen levels are high.
n Don’t forget to take your medicine.
Many allergy treatment options can be found over the counter, making it easier to get ahead of your symptoms. Common treatments include antihistamines, nasal sprays and decongestants. Nasal steroids (i.e., corticosteroids) are one of the most effective medicines used to treat nasal allergies.
If your quality of life is significantly affected by a high symptom burden or if you have other conditions affected by allergies, see your doctor. Patients are encouraged to schedule a visit with an allergist-immunologist to discuss allergies and more definitive treatment options including medications and allergy shots.
Being proactive can go a long way to combating, or at least controlling, those pesky allergies.

F rom bandages to breast implants, dental oss to hearing aids, wheelchairs to condoms, we all use medical devices with varying degrees of oversight from the Food and Drug Administration. Here’s a look at how these devices are classi ed, approved and brought to market.

47% of medical devices fall in this category and 95% of those are exempt from the regulatory process.
Class I devices are subject to the least amount of oversight because they present the least amount of risk.
These devices undergo general controls after manufacturing to ensure they are safe, e ective and ready for market. General controls consider good manufacturing practices, standards and reporting adverse events to the FDA, registration and recordkeeping requirements.
Examples include bandages, handheld surgical instruments, bedpans, tongue depressors and electric toothbrushes.
According to the Food, Drug and Cosmetic Act Medical Device Amendments of 1976, medical devices fall into one of three classes.

As health care professionals and researchers identify needs for medical devices, they begin the product concepting process. Product developers will create a “proof of concept” document that outlines the product’s feasibility. Part of this process includes classifying the product.
Once a product idea has been developed, researchers will build a prototype. Prototypes are tested in laboratory conditions.
PATHWAY TO APPROVAL: Most Class I devices are exempt from premarket submission.

The application process depends on the device’s risk classification.
There are two lesser used approval pathways that may be relevant for a small number of medical devices. De Novo is sometimes used for Class I or Class II devices that have not been marketed in U.S. previously but are reasonably understood and considered safe. Humanitarian Device Exemption (HDE) may be used for some rare diseases for which there is not enough clinical evidence to meet the FDA standard of reasonable assurance of safety and e ectiveness.







43% of medical devices fall in this category.


Class II devices may pose a moderate risk and a higher risk than Class I. These devices may have labeling requirements and may be subject to performance standards and testing requirements specific to the type of device, as well as general controls like Class I devices.
Examples include wheelchairs, tampons and some pregnancy test kits.
PATHWAY TO APPROVAL: Class II devices require a premarket notification called a 501(k). These devices continue to be monitored while on the market and can be found in FDA’s patient registries.

10% of medical devices fall in this category.
Class III devices are the most highly regulated and are used to sustain or support life, are implanted and/ or present potential risk of illness or injury. Manufacturers of Class III devices must prove that the device is safe and e ective. Once the device receives premarket approval and passes general controls, it may be labelled as FDA approved.
Examples include implantable pacemakers, breast implants, HIV diagnostic tests and closed-loop artificial pancreas systems.
PATHWAY TO APPROVAL: Class III devices require premarket approval (PMA). To receive premarket approval, there must be scientific evidence that the benefits of using the device outweigh the potential risks, and that the device will help a large part of the target population.
Southern Nevadans who are interested in learning more about medical device safety can search medical device databases at fda.gov. They may also seek out clinical trials to support local research for emerging needs in the community.
Once data has been gathered and the relevant application or notification has been filed, the qualifying medical device will be reviewed by the FDA. The FDA may consult an advisory committee of experts who have relevant experience and can provide independent advice. Once all factors have been considered, a decision is reached determining whether or not the medical device is approved. This decision, along with pertinent evidence, is published in the Federal Register.

Approved devices continue to be monitored for unintended risks. Manufacturing facilities are subject to routine inspections by FDA o cials. The FDA has power to shut down facilities that are not meeting standards and following good manufacturing practices. FDA programs such as MedWatch and Medical Product Safety Network allow organizations and individuals to report problems with approved medical devices. Consumers can subscribe to MedWatch safety alerts or the MedSun newsletter to receive regular information about medical device safety.
The FDA also uses the Sentinel Initiative for active surveillance. Sentinel collaborates with higher education institutions and health care organizations to follow trends in electronic health databases and monitor the safety of approved medical products as they are used.



Source: U.S. Food & Drug Administration


BY MARC J. KAHN, MD, MBA, MACP, FRCP
The population of Nevada increased by an average of 1.4% every year between 2010 and 2022. Unfortunately, Nevada’s health care infrastructure is woefully inadequate to support the population. According to The Physiciains Workforce in Nevada Report 2022 from the Nevada Health Workforce Research Center, the state ranks 45 in the number of physicians per 100,000 and 49 for the number of primary care and surgeons per capita.
Ne vada also lags in health services for vulnerable populations. For example, every state has a cleft palate and craniofacial health care services program except Alaska and Nevada.
In an effort to improve the state of health care in Nevada and specifically, Southern Nevada, UNLV has made the development of an academic health center a strategic priority.
Continued on page 18

Continued from page 17
An AHC, as defined by various national organizations, consists of an allopathic or osteopathic medical school, at least one other health profession school or program, and at least one affiliated or owned teaching hospital. AHCs are traditionally focused on providing the highest standards of clinical care and treating the most complex illnesses, conducting clinical, laboratory and health sciences research, educating future health professionals and engaging with the community. The terms academic health center and academic medical center are often interchangeable, but because an AHC represents a medical school and other health professions, we prefer the term AHC at UNLV.
AHCs typically represent the concerted efforts of multiple universities, programs, and/or hospitals to improve the care of a community through research, education, patient care and community engagement. According to the National Academy of Sciences, the university is at the core of an AHC, striving for excellence in education, community engagement and research. AHC participation does not preclude member institutions from pursuing other outside partnerships.
Although AHCs account for only about 5% of all hospitals, they deliver a disproportionate amount of care for:

Number of students who graduate annually from UNLV AHC programs
n Medicare and Medicaid patients
n Uninsured individuals
n Transfer of patients with complex needs
n Trauma and burn patients
n Cancer patients
With the breadth and depth of health care services that an AHC brings to a community, the Kirk Kerkorian School of Medicine at UNLV and its associated clinical practice, UNLV Health, are proud to partner with the UNLV schools of Nursing, Public Health, Dental Medicine, Integrative Health Sciences, the other UNLV behavioral health programs and the University Medical Center of Southern Nevada to provide Southern Nevada the AHC it deserves.
Together, these organizations are focused on developing coordinated plans for education, community engagement and research, while providing opportunities for collaboration, information sharing on best practices and ongoing discussions of research directed at community needs. Interprofessional education programs continue to be expanded as we focus on improving care coordination.
Already, the UNLV AHC has obtained more than $1 million of state appropriations to support its mission and racked up more than $11 million in research expenditures and $38 million in research awards. Together, the components of the AHC have produced more than 320 publications per year and, in 2023, saw more than 230,000 clinical visits. Approximately 630 students
An AHC, as defined by various national organizations, consists of an allopathic or osteopathic medical school, at least one other health profession school or program, and at least one affiliated or owned teaching hospital. AHCs are traditionally focused on providing the highest standards of clinical care and treating the most complex illnesses, conducting clinical, laboratory, and health sciences research, educating future health professionals and engaging with the community.

graduate annually from UNLV AHC programs. These programs also host an annual interprofessional education and practice day, with more than 400 AHC student participants, and support 30+ team-based and interdisciplinary educational events annually.
As an AHC, UNLV is championing innovative approaches to mental and behavioral health and physical well-being. This is demonstrated through our two community/schoolbased health care clinics established through a UNLV Health and Clark County School District partnership, our three UNLV community mental health training clinics, including the school of medicine’s center for individual, couple and family counseling, and the newly launched UNLV Community Clinic, established as a partnership between the school of medicine and the Volunteers in Medicine of
Southern Nevada.
The UNLV AHC continues to establish itself in the community and is currently reestablishing a cleft palate and craniofacial team, expanding health care programs and graduate medical education opportunities, offering more collaboration opportunities and increasing interdisciplinary research.
To have an AHC at UNLV is not only good for the university, it is good for the community and all of Nevada. That is why it has already received more than $9 million in philanthropy annually.
If you would like to support academic health or the school of medicine’s role in academic health, please reach out to the development and alumni relations department at 702-823-3705 or development@medicine.unlv.edu.
It can be difficult to find the right doctor for your family’s needs. Each body is different, and it’s important to have the right team taking care of your health. That’s why Vegas Inc releases the annual Top Doctors list.
a






The physicians on this list have been recommended by other doctors through a con dential survey. Nominated doctors are then checked against the proper boards. The nal result is a list of more than 100 top physicians working in Southern Nevada, recommended by their peers, and published with the hope that when you need a doctor, you know where to look.







Andrew Sean McKnight, MD Allergy Partners of Nevada 702-212-5889 allergypartners.com
David H Tottori, MD Tottori Allergy & Asthma Associates 702-432-8250 tottoriallergy.com
Steven Brown, MD Desert Hills Plastic Surgery Center 702-899-1157 deserthillsplasticsurgery.com
Stephanie Davidson, DO U.S. Anesthesia Partners–Nevada 702-878-0070 usap.com
Rainer Vogel, MD Comprehensive and Interventional Pain Management 702-990-4530 cipmnv.com
Darren Soong, MD Surgical Weight Control Center of Nevada 702-313-8446 surgicalweightcontrolcenter.com
Ruben Acherman, MD Children’s Heart Center Nevada 702-732-1290 childrensheartcenter.com
Sean Ameli, MD Ameli Dadourian Heart Center 702-906-1100 ameliheartcenter.com
Keshav Chander, MD Smart Heart Care & Smart Medical Care 702-473-5333 4smartcare.com
Alfred Danielian, MD Las Vegas Heart Associates 702-962-2200 lasvegasheartassociates.com
William Evans, MD Children’s Heart Center 702-732-1290 childrensheartcenter.com
Samuel Green, MD Nevada Cardiology Associates 702-233-1000 nevadacardiology.com
Zia Khan, MD Desert Cardiovascular Consultants 725-726-3162 desertcardiovascular.com
Je rey Levisman, MD Las Vegas Heart Associates 702-962-2200 lasvegasheartassociates.com

Gary Mayman, MD
Children’s Heart Center Nevada 702-732-1290 childrensheartcenter.com
Robert Rollins, MD
Children’s Heart Center Nevada 702-732-1290 childrensheartcenter.com
Deepak Malhotra, MD
MountainView Cardiovascular & Thoracic Surgery Associates 702-962-5920 heartandlungnv.com
Paul Mazur, MD MountainView Cardiovascular & Thoracic Surgery Associates 702-962-5920 heartandlungnv.com
Michael Wood, MD
Dignity Health Cardiovascular Thoracic Surgery Clinic 844-996-0717 dignityhealth.org

Francis Teng, MD Dr. Francis Teng 702-838-5888 fwtengbariatrics.com
Sanjay Malhotra, MD Nevada Heart & Vascular Center 702-227-3422 nevadaheart.com


























David Cotter, MD Las Vegas Dermatology 702-456-3120 lasvegasdermatology.com
Victoria Farley, MD Vivida Dermatology 702-255-6647 vivida.com
H.L. Greenberg, MD Las Vegas Dermatology 702-456-3120 lasvegasdermatology.com








Candace Spann, MD Couture Dermatology and Plastic Surgery 702-998-9001 couturemedical.com
Douglas Thomas, MD Thomas Dermatology 702-430-5333 thomasderm.com
Linda Woodson, MD Linda Woodson Dermatology 702-202-2700 lindawoodsondermatology. com
Frederick Goll, MD Ear Nose & Throat Consultants of Nevada 702-792-6700 entc.com
Sina Nasri, MD Nasri & Physicians 702-804-4729 drnasri.com
Matthew Ng, MD UNLV Health 702-671-6480 unlvhealth.org
Jonathan Salinas, MD Ear Nose & Throat Consultants of Nevada 702-792-6700 entc.com
Walter W. Schroeder, MD Ear Nose & Throat Consultants of Nevada 702-792-6700 entc.com
Ashley Sikand, MD Ear, Nose and Throat Consultants of Nevada 702-792-6700 entc.com
Randall Weingarten, MD Randall T Weingarten MD 702-617-9599





Leslie Denton, DO Ask Dr. Denton 702-726-6963 askdrdenton.com
Clarence Dunagan, MD MountainView Hospital 702-962-5000 mountainview-hospital.com
Nelson Huang, MD Dignity Health 702-259-1228 dignityhealth.com
Alexandra Aguilar, MD Dream Fund Pediatric Endocrinology Clinic 702-707-7399 dignityhealth.org
W. Reid Litchfield, MD
Desert Endocrinology 702-434-8400 desertendo.com
Omer Tarar, MD
Platinum Continuity & Specialty Clinic (725) 205-1249 platinum-pcsc.com
Claudia K. Vogel, MD


Claudia Vogel M.T. LTD 844-414-1386
Travis Hailstone, DO Southern Nevada Internal Medicine and Pediatrics 702-253-5410



























Thomas Shang, MD Valley Hospital Medical Center 702-388-4000 valleyhealthsystemlv.com
Joseph Adashek, MD Desert Perinatal Associates 702-341-6610 desertperinatalassociates. com









Carrie Bedient, MD The Fertility Center of Las Vegas 702-254-1777 fertilitycenterlv.com
Je Fisch, MD Green Valley Fertility Partners 702-722-2229 greenvalleyfertility.com
Bruce Shapiro, MD The Fertility Center of Las Vegas 702-254-1777 fertilitycenterlv.com
Howard Baron, MD Pediatric Gastroenterology & Nutrition Associates 702-791-0477 pgnalv.com
David Shih, MD Comprehensive Digestive Institute of Nevada 702-483-4483 nevadagastro.com
Martin Shill, MD Martin Shill, MD 702-901-0673 martinshillmd.com
Sean Dort, MD Southern Nevada Surgery Specialists 702-914-2420 southernnvsurgery.com
Nick Fiore, MD Sunrise Hospital & Medical Center 702-233-8101 sunrisehospital.com
Kelly Kogut, MD Pediatric Surgery Associates 702-233-8101 nvpediatricsurgery.com



Charles Walton, MD Southern Nevada Surgery Specialists 702-914-2420 southernnvsurgery.com
Alvin Lin, MD Alvin Lin, MD 888-505-7769
Julie Zacharias-Simpson, DO Touro University 702-777-3982 tun.touro.edu
Fadi El-Salibi, MD Centennial Hills Hospital 702-835-9700 centennialhillshospital.com
Brian Lipman, MD Henderson Hospital 702-776-8300 hendersonhospital.com
Asher Shahzad, MD First Person Care Clinic 702-380-8118 dignityhealth.org


Kevin Rayls, MD Mountain West Surgical 702-796-0022 mwsvegas.com
Constantine George, MD EPITOMEDICAL 702-419-3482 epitomedical.com
Robert Gong, MD Siena Hills Primary Care 702-614-0850 sienahillsprimarycare.com






Renu Mahajan, MD Smart Heart Care & Smart Medical Care 702-473-5333 4smartcare.com














Make The Valley Health System YOUR CHOICE




All Valley Health System hospitals are accredited by The Joint Commission for meeting performance standards for delivering safe, high-quality care.
Our acute care hospitals hold national certifications in stroke and heart attack care. Our hospitals consistently earn recognition from the American Heart Association® and American Stroke Association® for meeting or exceeding national standards for heart and stroke care.
The Valley Health System hospitals also consistently earn national quality awards for services such as wound care, orthopedics, maternity care, weight-loss surgery and more.




Daniel Malone Jr., MD Southwest Medical, Part of Optum Care 702-877-5199 smalv.com
Angela Miller, MD Concierge Medicine Las Vegas 702-850-2422 conciergemedicinelasvegas. com
Cli ord Molin, MD Priority Health 702-382-1599







Lawrence Lehrner, MD Kidney Specialists of Southern Nevada 702-877-1887 ksosn.com
Chidi Okafor, MD Kidney Specialists of Southern Nevada 702-877-1887 ksosn.com
Vincent Yang, MD Kidney Specialists of Southern Nevada 702-877-1887 ksosn.com



Azin Azma, MD Las Vegas Neurology Center 702-432-2233 lvneuro.com
Robert Balsiger, MD Las Vegas Neurology Center 702-432-2233 lvneuro.com
Omar Cabahug, MD Omar Cabahug MD 702-914-6994
Bess Chang, DO Medical Neurology 702-851-1065 medicalneurologylv.com
Paul Janda, DO Las Vegas Neurology Center 702-432-2233 lvneuro.com
Jay Mahajan, DO Las Vegas Neurology Center 702-432-2233 lvneuro.com
Efrem Cox, MD
The Spine & Brain Institute 702-896-0940 thespinebrain.com
Derek Duke, MD
Joseph Adashek, MD Desert Perinatal Associates 702-341-6610 desertperinatalassociates.com
Donna Miller, MD For Women 725-777-0414 nvforwomenobgyn.com
Waseem Alhushki, MD Cure 4 The Kids Foundation 702-732-1493 cure4thekids.org
Edwin Kingsley, MD
Comprehensive Cancer Centers 702-952-3400 cccnevada.com
Rupesh Parikh, MD Comprehensive Cancer Centers 702-856-1400 cccnevada.com
Ann Wierman, MD
Ann M. Wierman, MD 702-749-3700 annwiermanmd.com



The Spine & Brain Institute 702-896-0940 thespinebrain.com
Gary Flangas, MD
Las Vegas Neurosurgery & Spine Care 702-737-7753 dignityhealth.org
Mark Doubrava, MD Eye Care for Nevada 702-794-2020 eyecarefornevada.com






Weldon Havins, MD Nevada Eye Physicians 702-710-5209 nevadaeyephysicians.com








With surgeons like Dr. Erik Kubiak, we’ll help you regain your strength.
Building upon our rich history of groundbreaking care, UMC has assembled a world-class team of orthopedic and spine surgeons. The new UMC Orthopedic & Spine Institute offers industry-leading care in a wide range of sub-specialties, including:
• General orthopedics
• Hip and knee
• Shoulder and elbow
702.383.BONE (2663) umcsn.com/bone
• Spine
• Sports medicine
• Orthopedic oncology
• Orthopedic trauma
• Pediatric orthopedics
• Reconstruction




Grace Shin, MD Ideal Eye Care 702-896-2020 idealeyecarelv.com
Irene Voo, MD Irene Voo MD 702-583-3300 irenevoo.com
Andrew Bronstein, MD Bronstein Hand Center 702-458-4263 bronsteinhandcenter.com
Rainer Vogel, MD Comprehensive and Interventional Pain Management 702-990-4530 cipmnv.com
Ryan West, DO Innovative Pain Care Center 702-684-7246 painfreenevada.com
Willis Wu, MD Innovative Pain Care Center 702-684-7246 painfreenevada.com
Constantine George, MD EPITOMEDICAL 702-419-3482 epitomedical.com
Atousa Ghaneian, MD Healthy Kids Care at Sunrise 702-357-5727 healthykidscarelv.org
Kim LaMotte-Malone, MD Anthem Hills Pediatrics 702-566-2400 anthemhillspediatrics.com




Jenifer Powers, MD Crovetti Orthopedics 702-990-2290 crovettiortho.com
Christine Estrada, DO Reliant Palliative Care 702-202-0534 reliantphysicians.com
Ineada Okafor, MD Anthem Hills Pediatrics 702-566-2400 anthemhillspediatrics.com
Laura Weidenfeld, MD Sunshine Valley Pediatrics 702-363-3000 lasvegaspediatricdoctors.com








Daniel Burkhead, MD Innovative Pain Care Center 702-684-7246 painfreenevada.com
Paige Kozlowski, DO Platinum Hospitalists 702-407-7700 platinumhospitalists.com
George Alexander, MD Dr. Alexander & Co. 702-625-4233 alexandermd.com



Ho Dzung, MD Innovative Pain Care Center 702-684-7246 painfreenevada.com



Alvin Lin, MD Alvin Lin, MD 888-505-7769
Clevis Parker, MD ProCare Hospice of Nevada 702-380-8300 procarehospice.com
Hayley Brown, MD
Desert Hills Plastic Surgery Center 702-899-1157 deserthillsplasticsurgery.com
Arthur Cambeiro, MD



Bennett Vitug, DO Platinum Hospitalists 702-407-7700 platinumhospitalists.com
SurgiSpa 702-734-4100 surgispa.net
Stephen Miller, MD



Sarah Chamanara, DO Anthem Hills Pediatrics 702-566-2400 anthemhillspediatrics.com
Stephen M Miller MD 702-710-5869 drstephenmiller.com
Je rey Roth, MD Je rey J. Roth, MD 702-872-3039 jjrothmd.com


















We proudly acknowledge our 2024 Top Docs honorees. Trusted by patients and admired by colleagues, they’ve earned a reputation for going the extra mile, and more. They’re a valued part of our Optum family, committed to positively impacting the lives of every patient.
optum.com/nevada


Daniel Malone, MD
Internal Medicine
Southwest Medical, part of Optum
Dr. Malone’s professionalism, compassion and thorough communication has led many of his patients to confidently put their health in his hands for decades.

Jason Zommick, MD
Urology
Urology Specialists of Nevada
In his quest to provide new and effective treatment options for his patients, Dr. Zommick has helped to initiate lifechanging clinical research.
©2024 Optum, Inc. All rights reserved. The company does not discriminate on the basis of race, color, national origin, sex, age, or disability in health programs and activities. We provide free services to help you communicate with us. Such as, letters in other languages or large print. Or, you can ask for an interpreter. To ask for help, please call 1-702-877-5088.
ATENCIÓN: Si habla español (Spanish), hay servicios de asistencia de idiomas, sin cargo, a su disposición. Llame al 1-702-877-5088. (Chinese), 1-702-877-5088




Lesley Dickson, MD BHG Recovery 702-796-0660 bhgrecovery.com
Shaily Jain, MD Cairn Center 702-508-9461 cairncenter.com
Faisal Suba, MD Alliance Mental Health Specialists 702-485-2100 alliancemhs.com
Michael Anderson, MD Comprehensive Cancer Centers 702-952-3444 cccnevada.com
Joseph Candela, MD Las Vegas Urology 702-385-4342 lasvegasurology.com
Jessica Casey, MD Children’s Urology 702-369-4999 cualv.com
Chadwick Plaire, MD Children’s Urology 702-369-4999 cualv.com




David Steinberg, MD Steinberg Diagnostic Medical Imaging 702-732-6000 sdmi-lv.com
Peter Weidenfeld, MD Red Rock Radiology Associates 702-527-8945 redrockradiology.org
Jason Zommick, MD Urology Specialists of Nevada 702-877-0814 usonv.com








Michelle Danielian, MD Nevada Critical Care Consultants 702-483-6200
Hrishikesh Kulkarni, MD Platinum Hospitalists 702-407-7700 platinumhospitalists.com
William Rosenberg, MD Silver State Sports Medicine 702-591-1874 silverstatesportsmedicine. com
Nasim Daoud, MD Sagebrush Health 702-385-6468 sagebrushhealth.com



Craig Nakamura, MD Children’s Lung Specialists 702-598-4411 childrenslungspecialists.com




Mitchell Forman, DO UNLV Health 702-671-5060 unlv.edu



Philip Huang, MD VA Rheumatology va.gov
Saju Joseph, MD Summit Specialty Physicians 702-478-6393 summitmed.com


























Roseman Medical Group’s dedicated team of primary care providers offers a wide range of care for adults to maintain health, treat illness, and manage chronic diseases.
RMG SERVICES
Adult and Geriatric Medicine

WE OFFER


Wellness and Preventative Visits


Chronic Disease Management



Immunizations





Same-day appointments


Most insurances accepted



Convenient location FOR APPOINTMENTS

CLINIC HOURS
Monday – Friday 8am – 5pm
MEET OUR RMG MEDICAL DIRECTOR
Dr. Gregory Schneider, Physician
Professor and Associate Dean for Clinical Education at Roseman University College of Medicine Board Certified, Family Medicine























































Leslie Denton, DO is an accomplished board-certified physician licensed in Nevada and California with experience spanning over seventeen years.
Denton graduated from Western University of Health Sciences, College of Osteopathic Medicine of the Pacific, completing her board certification in Emergency Medicine while working the front lines in busy emergency rooms. She has provided care for the critically ill, as well as comprehensive/preventative care. Her competence, empathy, compassion and ability to explain medical concepts in clear and understandable terms has made her invaluable as a medical consultant. She assists patients in understanding diagnosis and develops strategies for optimizing their health care options in Nevada as well as out of state.
Denton also serves as a physician collaborator for nurse practitioners and performs attorney medical chart review. Her personalized approach is tailored to patients’ individual needs, preferences and values. Her focus is on what’s important—patient care.
410 South Rampart Blvd. Suite 390 Las Vegas, NV 89145
702-726-6963 askdrdenton.com

In 2024, Ali Khalaf joined Comprehensive Cancer Centers as a board-certified genetic counselor, where he provides comprehensive genetics education and patient care.
As a genetic counselor, he prioritizes empathy, collaboration and empowerment. He believes in tailoring the counseling process to each person’s unique needs and values, ensuring they feel supported and empowered throughout.
Khalaf started his career as a behavioral therapist in Montclair, California, while also working as a research assistant at the University of California Riverside’s life events lab. His pursuit of a master’s degree at the University of Utah marked the beginning of an intensive didactic training, where he dove into the intricacies of medical genetics. Khalaf transitioned into clinical and laboratory rotations within various clinical specialties, including in-person and telehealth genetic counseling.
Khalaf discovered his passion for oncology during his tenure providing cancer genetic counseling services for pediatric and adult patients across outpatient and inpatient settings.
CENTER–CENTRAL VALLEY/TWAIN
3730 S Eastern Avenue
Las Vegas, NV 89169
702-952-3400

Dr. Vishisht Mehta is the Director of Interventional Pulmonology at the Lung Center of Nevada, a division of Comprehensive Cancer Centers, and the Department Chair of Pulmonology at MountainView Hospital. He believes the two most important aspects of the patient-physician relationship are the patient’s goals of care and shared decision-making.
Mehta is a recipient of the prestigious Fellow of the College of Chest Physicians designation from CHEST (American College of Chest Physicians), serves on the Nevada Leadership Board of the American Lung Association and is the Founder of the Nevada Lung Foundation, which is his personal philanthropic effort to improve lung health and lung cancer screening in the state. For his work, he was recognized by Vegas Inc. with its prestigious “40 Under 40” award in 2023. His growing interest and expertise lie in the application of artificial intelligence in pulmonology. He is also the founder of Pulmonary.ai.
LUNG CENTER OF NEVADA–TENAYA
3150 North Tenaya Way Suite 125 Las Vegas, NV 89128 702-869-0855

Gregory Schneider, MD, is the medical director for Roseman Medical Group. Prior to coming to Las Vegas, he was a clinical educator at the Florida International University Herbert Wertheim College of Medicine in Miami. There, while also practicing family medicine, his teaching focused on clinical skills, ethics, and the social factors involved in health.
In over 20 years as an educator, he has taught undergraduate literature, philosophy, math, and science; directed medical school courses; and trained family medicine residents in both inpatient and outpatient care. At FIU, he saw patients at underserved clinics in South Florida and oversaw a medical student home visit program.
His career has come full circle, as he joins the Roseman medical school clinic committed to serving our community.
RMG’s team of primary care providers offers a range of care for adult and geriatric patients to maintain health, treat illness and manage chronic diseases.
5380 S. Rainbow Blvd. Suite 120 Las Vegas, NV 89118 702-463-4040 rosemanmedicalgroup.com

Dr. Thein is a medical oncologist with a passion for genetic-driven combinatorial strategies to improve the outcomes of cancer patients through personalized and precision medicine approaches.
He believes the evolution of biomarker-driven trials and testing is leading-edge as it is helping guide targeted therapy. His main clinical interests include thrombosis, head and neck, thyroid, genitourinary and rare cancers. Thein is also interested in investigational cancer therapeutics, including early phase clinical trials and phase 1 drug development to advance the treatment of cancer.
Thein was an Assistant Professor in the Division of Hematology and Medical Oncology at OHSU/Knight Cancer Institute. Thein also specialized in developing novel therapeutics as he coled the early phase clinical trials program at OHSU. Thein has authored over 50 peer-reviewed articles and book chapters in prestigious publications such as CA: A Cancer Journal for Clinicians, Cancer Discovery and Nature Communications
3730 S. Eastern Avenue Las Vegas, NV 89169
702-952-3400
BY HEDY WOODROW
In today’s fast-paced world, our homes are often our sanctuaries as they provide a retreat from the constant barrage of information and daily stressors. By transforming our living spaces into places of harmony, we can foster a sense of peace, health and well-being.

The layout of your rooms should be open and inviting. Arrange your furniture to create clear, open pathways and avoid blocking views, both inside and outside. This helps create a flow that promotes calmness and discovery. Incorporating greenery, such as indoor plants, can invigorate the space and add a touch of nature, which has been shown to improve mental well-being. The indoor-outdoor biophilic philosophy we incorporate with Blue Heron homes is an example of this, showing how open space, coupled with water features and nature, can create a sense of calm.
2
1
When decorating for wellness, opt for natural color palettes. Creams and neutrals can warm up a room, while ocean blue hues evoke the calming essence of water. Incorporating natural elements such as plants, water fountains, and even rocks can stimulate your senses and create a peaceful environment. The sound of water from a fountain, for instance, can be particularly soothing and enhance the space’s overall ambiance. 1 2
Finally, personalizing your space with thoughtful touches can make a notable difference. Whether it’s cozy, stylish loungewear that makes you feel good after a long day, or strategically placed decorative pillows that change with the seasons, these small details can enhance your overall sense of well-being.

By implementing any of these ideas and strategies, you can transform your home into a place of harmony, promoting wellness and providing a sanctuary from the outside world. In an era of information overload and constant stress, creating a harmonious and inviting home environment is more important than ever.
4 3 5
Continued on page 36
3 4
Scents and textures play a significant role in creating a calming environment. High-quality candles with soothing scents can bring feelings of tranquility to your home. Luxurious aromatic soaps in the bathroom can elevate everyday routines into moments of relaxation. In the bedroom, down-filled comforters and high-threadcount bedding can enhance your sleep quality, adding to overall mental wellness as well.
One of the simplest yet most effective ways to promote wellness at home is to maximize natural light and minimize clutter. A well-lit space can significantly improve your mood and energy levels. Keep windows and glass doors unobstructed to allow sunlight to flood your rooms. Decluttering your space not only makes it more aesthetically pleasing but also reduces stress and anxiety. Every item should have its place and unnecessary items should be removed to create an open, inviting environment.

6 6
Modern wellness tools are becoming increasingly popular in homes. Light therapy devices, saunas, and cold plunge pools are a few examples. These tools, such as the LightStim therapy equipment used by athletes and wellness enthusiasts, can help with relaxation and physical recovery. Incorporating items like Pilates reformer chairs or light therapy beds can transform your home into a personal wellness retreat.
The exterior of your home should not be overlooked. A welldesigned garden or landscape with a pleasing color pattern and flowers can offer a sense of calm as you approach your home. If you have a pool, placing rolled towels on lounge chairs can create a relaxing, resort-like feel.

Establishing a central focal point in your home can be soothing and offer a sense of stability. A beautiful round table adorned with a standout floral arrangement provides a welcoming sight as you enter your home. Colors play a crucial role in setting the mood: blue is known for its calming effects while white signifies cleanliness and tranquility. These colors can be incorporated into your focal point to enhance feelings of wellness.
Designating specific areas for wellness activities can significantly enhance your home’s tranquility. For example, a yoga mat basket in a room can be a reminder to take time for relaxation and stretching. Position these wellness spaces where they receive the best natural light. Additionally, transforming your bathroom into a spa-like retreat with rolled towels, candles, and eucalyptus spray can provide a serene escape within your home.
7 8 8 9 9 10 10
Keeping your home clean and organized may also improve emotional well-being. For instance, regularly cleaning dishes, the kitchen sink and counters ensures you start each day fresh. Beautifully arranged flowers and bowls of colorful fruit, like lemons and limes, can add visual appeal and enhance your mood. Fresh flowers, especially, should be maintained by changing the water every two days and removing pollen to keep the scents vibrant.
Hedy Woodrow is President of Atelier Blue Heron Interiors, a division of Blue Heron. Founded in 2004, Blue Heron is a design-led development firm specializing in custom homes and boutique communities in Southern Nevada.





David Nichols is a Licensed Master Social Worker at ArchWell Health
BY DAVID NICHOLS
Social workers play a vital and expanding role in improving health outcomes. Acting as advocates and allies for individuals navigating complex medical systems, social workers engage in resource coordination and community outreach to address social barriers impacting health equity and access to care.
Research from organizations like the Kaiser Family Foundation has shown how a patient’s physical environment (i.e., safe housing and reliable access to utilities), social support networks, literacy and more circumstances affect overall health. These barriers to care are extremely diverse across the country, and social workers are on the front lines learning about their patients’ unique lifestyle factors and communities.
Social workers not only connect individuals to vital community resources, but they also collaborate closely with doctors and the rest of the care team to ensure patients are getting their mental, physical and social needs met. By closing this gap, social work teams often improve health outcomes and enhance the overall quality of patient care. In fact, a 2020 report published in Healthcare Policy found that in primary health care, social workers’ delivery of mental health care and other support services “contribute to the individual’s health and wellbeing.”
Despite this evidence, many patients have fears and misconceptions about working with social workers. Some people are initially uneasy about speaking with a social worker out of fear that it may compromise their independence or determine whether they can live alone. The reality is that social workers are person-centered and work to connect members with resources that the member personally feels would best support their lifestyle goals. Social Workers can be
a great resource for older adults living alone by connecting them with local nonprofits that can help with transportation, home repair, medical supplies and many other topics.
An individual who lived alone and coped with mobility issues and memory loss had a history of falls that resulted in several hospital admissions. She struggled to secure food on a regular basis or maintain her home due to her medical conditions. Despite conversations with her medical team, the member was not open to transitioning into a group or assisted living setting.
After building rapport, a social worker was able to connect her to long-term, in-home support that helps with housekeeping, laundry, and errands like shopping or medication pick-up. The social worker got her on a microwavable food delivery service and connected her to a local nonprofit for seniors that provided in-home safety modifications. She now has access to scheduled transportation to and from events and activities in the community. She now feels confident about engaging the care network for any other need she may have.
As the U.S. population ages, stories like this will become more common, and the role of social workers in senior care will need to expand. The number of individuals over 65 in the United States is expected to increase by nearly 50% in the next 15 years. It is the community’s responsibility to consider how the well-documented lack of caregivers, the increasing number of adults living alone and the growing poverty rate among individuals over 65 will affect the already strained health care system.
Social workers are in a unique position to support older adults by acting as a central part of their health care team and connecting them with community resources while collaborating with stakeholders and policymakers on innovations needed to better support our senior members.

Emily Antuna is a Public Relations Coordinator at UMC
‘All the world’s a stage,” as William Shakespeare famously wrote, “And all the men and women merely players.” Ron Herz, 62, has played an important role for more than 30 years as an elementary school teacher with a passion for bringing the magic of drama and music to his students.
Behind the curtain, however, Herz faced a conflict that prevented him from taking center stage throughout most of his life. “I was diagnosed with Type 1 diabetes when I was 20 years old,” Herz said. Living in New York City at the time, he shared his new diagnosis became more frightening than he would have ever imagined,
“I would have hypoglycemic reactions in the middle of a busy sidewalk and fall unconscious, only to wake up in a hospital bed.”
In more than 40 years with this debilitating disease, Herz made more than 40 trips to the hospital.
“I wanted a normal life without fear of losing control,” Herz said. “I never got married or had children because I was afraid of being a burden on someone else.”
Everything changed four years ago when Ron met Roberta, the grandmother of one of his students.
“I was a volunteer in his class,” Roberta said, smiling while holding her husband’s hand. “He made me feel like a teenager again. I would drop things around him in class because I was so nervous.”
Roberta, a certified nursing assistant at UMC, quickly realized the challenges diabetes brought to Herz’s life and took it upon herself to change his story forever. The moment Roberta learned UMC was starting to perform pancreas transplants, she shared the news with Herz.
“Not only was I surprised to learn this was a possibility for me, but also that I would be the first one,” Herz said.
Since performing Nevada’s first kidney transplant in 1989, the UMC Center for Transplantation has provided thousands of patients with life-saving kidney transplants and highly skilled care. In 2023, the Scientific Registry of Transplant Recipients recognized the UMC Center for Transplantation as the top kidney transplant program in the United States. Compared with 257 programs across the country, UMC had the shortest wait times for a kidney transplant and the highest one-year kidney survival rate.
“As Nevada’s only transplant center, UMC is constantly looking for ways to expand access to meet the community’s growing transplant needs,” said David Tyrell, Clinical Director of the UMC Center for Transplantation. “Pancreas was just a natural progression from the kidneys.”
The hospital launched a new pancreas transplant program in 2022, offering community members in need a new lifeline without having to leave the Silver State. According to the National Institutes of Health, diabetes is a leading cause of kidney failure in the United States.
“Many of our transplant patients have diabetes and depend on insulin to regulate their blood sugar levels,” said Dr. Oleh Pankewycz, Transplant Nephrologist and Medical Director of UMC’s Pancreas Transplant Program.
Patients suffering from kidney failure and diabetes can see dramatic results from a kidney and pancreas transplant, and many patients receive both at the same time, Dr. Pankewycz said. Since 2023, UMC has performed six pancreas transplants, five of which happened in conjunction with a kidney transplant. Only one patient received a standalone pancreas transplant—Ron Herz.
According to the United Network for Organ Sharing, the nonprofit organization that manages


the country’s organ transplant system, 914 pancreas transplants were performed nationwide in 2023. Of those, only 102 were standalone pancreas transplants.
“Not many people do a pancreas transplant alone because of the risks associated,” said Dr. Sunil Patel, Program Director and Primary Surgeon for UMC’s Kidney and Pancreas Transplant Programs. According to Dr. Patel, the surgery is more complex and there is a greater risk of the patient’s body rejecting the pancreas.
“The volumes are much lower in general because it’s tough to find a viable pancreas. The pancreas is a more delicate organ, and the transplantation requires a bit more in terms of expertise and experience,” Dr. Patel added.
Despite the risks, Herz was ready to flip the script on a disease that has taken so much from him.
“I was a little scared because of the total change I knew my body would have to go through, but I wanted to live a normal life. I wanted to be a better husband and a better person for the world,” Herz said.
Above: Dr. Sunil Patel, Program Director and Primary Surgeon for UMC’s Kidney and Pancreas Transplant Programs, consults with pancreas transplant recipient Ron Herz and his wife, Roberta, at the UMC Center for Transplantation.
Left: Dr. Patel prepares for a transplant surgery at UMC.
In Feburary, Herz answered the phone call every transplant patient hopes to receive.
“Roberta and I were eating dinner when we got the call. We were in the car almost immediately. We already had our bags packed. I was ready,” Herz said.
The days after surgery came with a shocking adjustment for Ron. “I woke up thinking, ‘Where’s my insulin pump?’ After 42 years, it was a part of my existence, but now I am no longer diabetic,” Herz beamed.
The future is bright for transplant patients in the Silver State. “We’re looking to do big things,” Tyrell said. “Kidneys continue to be the greatest need for Nevada patients. The next would be liver, and then heart.”
Dr. Patel believes it is only a matter of time before his team will be able to provide community members with a vital new lifeline. “We have everything that supports liver transplantation,” Dr. Patel said,” We are poised to be successful. It’s a matter of developing the right infrastructure, hiring the right people and essentially starting a chronic liver disease clinic.” Tyrell agrees. “We need to do this for our community, and UMC is highly committed to doing that,” Tyrell said.

Michael Gagnon is Executive Director of HealtHIE Nevada
BY MICHAEL GAGNON
When the VA Mission Act was passed in 2018, it allowed Military Veterans to seek care from community providers.
HealtHIE Nevada, the statewide health information exchange, became crucial in providing care coordination between VA facilities and the community providers treating our veterans. Then in September of 2018, the VA and DOD signed a joint commitment to coordinate on the creation of interoperable electronic health record systems.
HealtHIE Nevada is a private, nonprofit, statewide health information exchange dedicated to connecting health care organizations by managing real-time, secure and accurate exchange of clinical information.
Certified by the Nevada Department of Health and Human Services, HealtHIE Nevada operates throughout the entire state, and is the only health information exchange serving the Nevada health care community for the last 12 years. Ensuring data security and privacy, HealtHIE Nevada is accredited by HITRUST, the most extensive program of its type in the nation.
To put this in perspective, according to the latest U.S. Census Bureau statistics, there are more than 226,000 veterans and more than 13,000 active-duty military personnel in Nevada. Many veterans receive care both in the VA system and from non-VA community providers and coordinating care is critical for improving quality and patient safety.
With this new connection, providers at the VA will have access to clinical patient information from health care organizations who participate in the HIE including Renown Health, Dignity Health, Saint Mary’s Medical Center, University Medical Center, Valley Health System, Southwest Medical Associates, Desert Radiology, Reno
Diagnostic Center and several more.
HealtHIE Nevada went through a major technology transition in 2020 and deployed new services to more than 140 participants. It took almost two years to stabilize the new technology platform and two more years to get the connection to the VA and DOD, but this connection was recently completed, allowing a secure network to connect all Nevada providers’ electronic health records to the U.S. Department of Veterans Affairs and Department of Defense electronic health records. This provides a valuable service to active-duty military, veterans and their family members.
With this new connection, the VA and DOD make clinical patient information available to the HealtHIE Nevada network when necessary for community patient care. Information includes laboratory results, medications, imaging reports, discharge summaries and care summaries. HealtHIE Nevada, in turn, makes patients’ medical records available to VA and DOD providers.
Whether on active duty, reacclimating to civilian life or years into their retirement journey, HealtHIE Nevada is honored to help active-duty military and veterans by allowing doctors and other health care providers access to their medical records in a seamless and secure manner. This new service is designed to enhance care coordination between VA, DOD and local health care facilities to improve patient experience wherever they receive care in Nevada.
Without the connection to the HIE, patients are required to collect and transport paper records to all providers, exacerbating an already arduous health experience for veterans. To enable this type of data exchange, HealtHIE Nevada ensures strict compliance with all state and federal medical privacy regulations.





BY HANNAH WEST
In the world of health care, there is a focus on child milestones and critical interventions. While these benchmarks are important, it is also crucial to remember the profound impact of everyday moments on child development. Vroom, a web-based resource, and early relational health highlight the importance of these ordinary interactions and emphasize how these moments contribute to a child’s cognitive and emotional growth. Nevada’s health programs are at the forefront of promoting relational health within families.
Vroom is an initiative of the Bezos Family Foundation and is designed to empower parents and caregivers with simple, effective tools to nurture early brain development through daily interactions. Vroom translates the latest neuroscience into practical tips that transform everyday moments into brain-building opportunities. By integrating Vroom’s principles into their routines, caregivers can support their children’s cognitive and emotional growth in meaningful ways.
Vroom’s approach centers around five Brain Building Basics, that provide framework for engaging with children in ways that promote their development:
1. Look: Making eye contact and observing a child’s cues is foundational. This engagement helps children feel seen and valued, fostering a sense of security and connection. When caregivers respond to a child’s expressions and actions, they validate the child’s feelings and
encourage communication.
2. Follow: By following a child’s lead, caregivers show that they value the child’s interests and curiosity. This practice encourages children to explore and discover their environment, reinforcing their confidence and sense of agency.
3. Chat: Engaging in conversation with children, even before they can speak, builds their language skills and cognitive development. Narrating activities and responding to their sounds and expressions help form the building blocks of communication.
4. Take Turns: Interactive play and conversation teach children the dynamics of social interaction, including patience, cooperation and empathy. This back-and-forth exchange is crucial for developing relational skills.
5. Stretch: Introducing children to new experiences and ideas extends their learning and problem-solving abilities. This encourages resilience and adaptability, preparing them for future challenges.
Early relational health focuses on the quality of relationships between children and their caregivers. Positive, responsive interactions in the early years lay the foundation for healthy emotional regulation, social competence and cognitive skills. Vroom’s brain building basics align seamlessly with ERH principles, emphasizing nurturing, responsive and engaged caregiving.
Nevada’s health programs are crucial for nurturing the relational health of families with young children and supporting their well-being through initiatives like the Nevada Maternal,

Infant and Early Childhood Home Visiting Program. These programs enhance parenting skills, promote child development, strengthen familial bonds and empower parents with essential resources. First 5 Nevada, a website and eligibility portal, makes it easy for families to find and access the programs to help their children thrive. By focusing on early intervention and preventive care, these initiatives improve immediate child health and lay a foundation for long-term emotional and cognitive development.
The Nevada Association for Infant and Early Childhood Mental Health is another initiative that recognizes the impact of early experiences on children. It supports practitioners endorsed by Infant and Early Childhood Mental Health and provides valuable resources and free professional development opportunities to equip practitioners with the latest research and best practices in promoting healthy social and emotional development in young children. Moreover, these initiatives foster community resilience by addressing socio-economic disparities and ensuring equitable access to health care services through programs like Nevada Check Up. By supporting comprehensive health care coverage, including essential medical services and preventive care, these efforts contribute to family well-being by addressing broader social determinants such as housing stability and educational access. Collaborative efforts with health care providers, educators, and community organizations create a supportive environment where every child can thrive and reach their full potential in a nurturing and healthy family context.
Everyone, including parents, educators, health care professionals, policymakers and others, can play a vital role in a young child’s life. Research consistently shows that supporting children’s development in early childhood lays the foundation for their lifelong success. To explore the range of resources available to Nevada families, please visit First5Nevada.org for more information.

Arsalan Salamat , MD is the director of the Breast Care Program at Optum
BY ARSALAN SALAMAT, MD
Physicians and health care providers emphasize the importance of ensuring that patients are aware of the symptoms and risk factors for breast cancer. There are steps patients can take to improve their health, lower their risk of getting breast cancer and possibly detecting it early.
Who is at risk for breast cancer?
According to the Centers for Disease Control and Prevention, breast cancer is the second most common cancer among women in the United States. Each year in the U.S., about 264,000 cases of breast cancer are diagnosed in women and about 2,400 in men.
Although deaths from breast cancer have declined, breast cancer is still the second leading cause of cancer death among women overall. In addition, breast cancer is the leading cause of cancer death among Hispanic and Black women.
What is the best way to detect breast cancer?
Encouraging mammograms, as appropriate, is important because it may detect breast cancer at an early stage when there are no apparent symptoms. It is also important to make sure that patients are aware of the possible symptoms of breast cancer, including:
n New lump in breast or underarm
n Changes in size or shape of breast
n Thickening or swelling in parts of the breast
n Pulling in of the nipple or pain in the nipple area
n Pain in any area of the breast
n Nipple discharge other than breastmilk, including blood
n Irritation or dimpling of breast skin
n Redness or flakiness in nipple area or breast
What are the breast cancer screening recommendations?
Screening recommendations vary between experts but for women at average risk for breast cancer, the American Cancer Society recommends an annual mammogram for women between 40 and 75 years old. Women with certain risk factors for breast cancer may need to start screening at an earlier age and may need more frequent screening based on their family history.
Screenings can find cancer before symptoms begin. Therefore, getting screened is important even for those who have no symptoms or complaints. It’s a good idea to talk with your patients about potential risk factors and various types of screenings, including mammograms.
How do you prepare for a mammogram?
The American Cancer Society provides several steps to prepare for a mammogram that would be ideal to share with patients, such as avoiding deodorants, anti-perspirants, powders, lotions, creams and perfumes under the arm or breasts on exam day. Some of these products can show up as white spots on X-rays.
Medical professionals are encouraged to guide patients toward breast health and overall well-being by reminding them throughout the year of the tips and guidelines for preventing breast cancer.

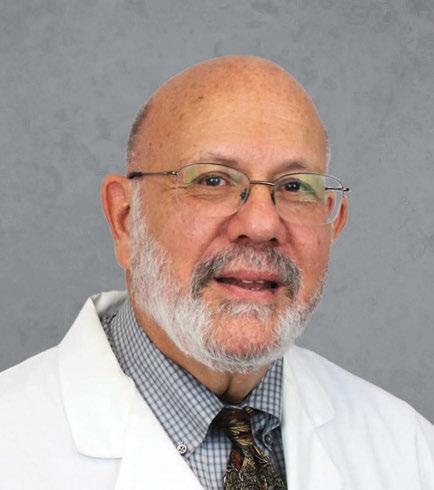



























Comprehensive Cancer Centers announced the hiring of two board-certified physician assistants. Valerie Chang, MMS, PA-C, OMD, sees patients at Comprehensive’s Southwest–Southern Hills treatment center, 9280 W. Sunset Rd. Nicholas Tieu, PA-C, works out of Comprehensive’s Central Valley–Twain treatment center, 3730 S. Eastern Ave.
Two Dignity Health-St. Rose
Dominican hospitals were named as high performing in multiple categories in U.S. News & World Report ’s 2024-25 Best Hospitals. High performing is the highest distinction a hospital can earn. Siena Hospital earned high performing ratings in ten categories, including: chronic obstructive pulmonary disease, diabetes, heart attack, heart failure, hip replacement, kidney failure, knee replacement, leukemia, lymphoma, and myeloma, pneumonia and stroke. San Martin Hospital earned high performing ratings in two categories — heart failure and kidney failure.
Touro University Nevada College of Osteopathic Medicine received $500,000 from the Engelstad Foundation to advance cancer research and develop a drug that prevents cancer metastasis. The gift will be applied during the next two years and supports research conducted within the Engelstad Research Complex.
Select Health opened its Nevada headquarters and the Intermountain Health Maule Clinic at 6795 Agilysys Way. The headquarters serves as a hub for all members to access care, explore health insurance products and services, ask questions face-to-face, and receive immediate assistance. The clinic provides specialized primary care services exclusively for Select Health Medicare members. The clinic also o ers traditional primary care services for commercial Select Health members, expanding health care options for the community.
The Nevada Transplant Institute announced the inauguration of its board of directors. Board members include, Joe Ferreira, founding chair; Brian Erling, MD, MBA, president and CEO, Renown Health; Jim DeVolld, managing director, Commercial Banking, First Independent Bank; Dr. Thiago Beduschi, chief of the University of Florida Division of Transplantation and Hepatobiliary Surgery and Director of the UF Health Abdominal Transplant Center; Ernesto P. Molmenti, MD, PhD, MBA, director and executive vice president and leader in the field of organ transplantation. Consulting NTI faculty members include Dr. David Mulligan and Dr. Harrison Pollinger
Nevada Donor Network acquired a building located at 1050 E. Sahara Avenue. The


35,000 square-foot building will serve as the cornerstone for Nevada Donor Network’s innovative donor care unit, an initiative designed to enhance e ciencies and improve outcomes across all facets of the donation process.
Cedric Ojeda, APRN joined Southwest Medical’s Tenaya Health Care Center at 2716 N. Tenaya Way and specializes in adult medicine.
The Kirk Kerkorian School of Medicine at UNLV honored two faculty members as endowed chairs. David N. Jackson, MD, professor and chair, department of gynecologic surgery and obstetrics, was conferred as the Intermountain Healthcare of Nevada endowed chair in gynecologic surgery and obstetrics. Erik N. Kubiak, MD, professor in the department of orthopaedics, was conferred as the Optum and Dr. Tony and Renee Marlon endowed chair in the department of orthopaedics.
Desert Hope Treatment Center promoted Kristin Berg to executive director. Berg has more than 15 years of experience in the Las Vegas behavioral health industry, and dual certification as a licensed alcohol and drug counselor and supervisor. She most recently served as chief operating o cer. Berg will oversee operations at Desert Hope’s inpatient and outpatient locations.
Roseman University of Health Sciences appointed Geena Mattox as vice president for philanthropy and alumni relations. Mattox has an extensive

background in securing major gifts, corporate sponsorships, and successful capital campaigns.

Nevada Donor Network promoted Elizabeth Shipman to vice president of organ operations. Shipman is responsible for overseeing, directing, and managing hospital relationships, organ operations, family support, and the clinical laboratory for the nonprofit organization. She has been leading Nevada Donor Network’s organ services team since 2021 as senior director of organ services.
The Collaboration Center announced the appointment of co-founder Cindy Goussak to executive director. Goussak is focused on emphasizing the organization’s mission to provide a comprehensive,
centralized support system that enhances independence and quality of life for those living with intellectual, developmental, physical and learning disabilities. With a variety of on-site disability service partners like the Children’s Heart Foundation, Let’s Talk Therapy, Boy’s Town Nevada, the Nevada Medicaid O ce, and more, the Collaboration Center serves as a centralized hub that brings together crucial resources for individuals and families.
Dee for Dentist is now the exclusive Nevada a liate partner for Renew. Renew provides dental implant anchored dentures, a fixed-removable full-arch denture that is snapped onto dental implants. The implants help keep the denture in place and provide better function, stability, and comfort compared to conventional dentures.
Boys & Girls Clubs of Southern Nevada received a $140,000 grant from UnitedHealthcare Plan of Nevada Medicaid The contribution will support before, after-school and school-break programs.
Birth Collaborative LV , a local organization focused on cultivating a strong professional birth care workforce and community, received $100,000 from Molina Healthcare of Nevada . The investment will fund 40 scholarships to train the next generation of community perinatal doulas in Southern Nevada.