Today’s nurses fulfill many roles and serve in diverse settings that fit their interests while specializing in caring for unique patient populations. Every day brings different challenges in nursing, offering the opportunity to provide patient care, promote health and education in the community, coordinate care and conduct research to improve practice and patient outcomes. Nurses play an integral role in the healthcare system and improve patients’ lives daily.

Publisher of Branded Content and Special Publications
EMMA WOLFF (emma.wolff@gmgvegas.com)
+ ART
Special Publications Editor SIERRA SMART
Managing Editor/News DAVE MONDT
Staff Writers GRACE DA ROCHA, HILLARY DAVIS, KATIE ANN MCCARVER, EMMA BROCATO


Roseman University’s College of Nursing announces its newest program!
DOCTOR OF NURSING PRACTICE IN NURSE ANESTHESIA (DNPNA)


Aspiring nurses wishing to embark on a transformative educational experience may earn their Doctor of Nursing Practice in Nurse Anesthesia (DNPNA) to become a Certified Registered Nurse Anesthetist (CRNA). This innovative 36-month, full-time hybrid-online program has a July start. Approximately 90% of clinical sites are local to Las Vegas and Henderson, NV.
Copy Editor ABRAHAM KOBYLANSKI
Photo Coordinator BRIAN RAMOS
Staff Photographers CHRISTOPHER DEVARGAS, STEVE MARCUS, WADE VANDERVORT
Publisher of Digital Media KATIE HORTON
Senior Advertising Manager MIKE MALL, ADAIR NOWACKI, SUE SRAN
Account Executives MARY CHARISSE DIMAIN, LAUREN JOHNSON, ANNA ZYMANEK
Sales Executive Assistants APRIL MARTINEZ
Web Content Specialist CLAYT KEEFER
Vice President of Manufacturing MARIA BLONDEAUX
Production Director PAUL HUNTSBERRY
Production Manager BLUE UYEDA

Learn more at roseman.edu


Roseman’s Six-Point Mastery Learning Model® leverages unique teaching methods to facilitate deep and lasting active learning, reduce competition, increase collaboration and teamwork, and expose students to the healthcare setting early, allowing for greater competency, mastery, and confidence.





Associate Marketing Art Director BROOKE EVERSON
Marketing Graphic Designer CARYL LOU PAAYAS
Publication Coordinator DENISE ARANCIBIA
Traffic Coordinator ALEX HAASE
Production Artist MARISSA MAHERAS
Route Administrator KATHY STREALU
Fulfillment Operations Coordinator CASANDRA PIERCE
Distribution Relations Liaison JIDAN SHADOWEN




Events Director SAMANTHA PETSCH
Events Manager HANNAH ANTER
Events Coordinator ALEXANDRA SUNGA
CEO , Publisher & Editor BRIAN GREENSPUN




Chief Operating Officer ROBERT CAUTHORN
Managing Editor RAY BREWER
VEGAS INC
2275 CORPORATE CIRCLE, SUITE 300 HENDERSON, NEVADA 89074 | 702.990.2550


This publication marks the 18th year of Health Care Headliners. For almost two decades, members of the public have thoughtfully nominated doctors, nurses, administrators and others for this honor, and we have had the privilege to celebrate some of Southern Nevada’s most esteemed health care professionals.
I’m grateful for medical innovation and researchers who work hard to treat the needs of our community every day. I’m grateful for the contributors who willingly share their expertise and experience. And finally, I’m grateful that so many individuals are striving to make health care more accessible to those in need.
One of these individuals is 2024 Health Care Headliner Matthew Thacker, who provides free dental care to veterans through the Adopt a Vet dental program. He also works with local youth and education institutions to prepare the next generation of health care providers, modeling dedicated service to the community.
protect public health by spreading awareness and eradicating misinformation.
Desert Hope Treatment Center addresses the increasing danger of fentanyl overdoses as the opioid crisis in the United States continues to escalate. It also offers solutions and resources that could save many Nevadans from overdose-related deaths.
You’ll also learn about clinical trials that are taking place right here in the Las Vegas Valley to advance precise personalized treatment.

The Lifetime Achievement Health Care Headliner, Charles Bernick, has served Nevadans since 1994. His exceptional, cutting-edge work with brain health has influenced thousands, from local research on Alzheimer’s disease and dementia, to the ongoing Professional Athletes Brain Health Study.
This year’s Research and Science Award goes to Aimee Foord, director of research at Cure 4 The Kids Foundation. A champion of comprehensive health care, she looks for barriers and gaps in the system and works to build bridges that allow children access to care, especially for those with chronic diseases.
In other sections of this publication, we hear from organizations in Southern Nevada that
Dignity Health–St. Rose Dominican is responding to the findings of its most recent Community Health Needs Assessment by implementing programs that promote wellness and treat chronic diseases, including Alzheimer’s disease, dementia and prediabetes. These programs give hope to suffering patients and their families.
Mark Stradling, of Nevada Eye Physicians, discusses risks associated with prolonged exposure to UV rays and heat, which is especially relevant to construction workers, lifeguards and others who work outdoors.
It is my immense pleasure to present this magazine, written by and for Nevadans, with hope that it will educate and inspire anyone interested in local health care.
I also want to congratulate this year’s Health Care Headliners and personally thank them for the care and attention they provide the community.
Wishing you health and happiness,
Sierra Smart Special Publications EditorThe Kirk Kerkorian School of Medicine at UNLV announced a collaboration with Volunteers in Medicine of Southern Nevada to provide improved patient access and free health care for uninsured individuals in Las Vegas. The UNLV Community Clinic, inside the Ruffin Family Clinic, is located at 1240 N. Martin Luther King Blvd. The clinic features primary medical care, pediatrics, OB/GYN, dental care, social and behavioral health services, and various specialties along with an on-site pharmacy. All services and medications are provided at no cost to uninsured and low-income members of the community.

The Nevada State Board of Medical Examiners incorporated a new digital fingerprinting option into its licensing process for physicians, physician assistants, respiratory care practitioners, perfusionists and anesthesiologist assistants. Individuals applying to the Board for licensure must submit to a criminal background investigation and can now do so electronically rather than via traditional mail.
12 Vegas Inc honors the Valley’s 2024 Health Care Headliners
32 UMC doctor gives patients another opportunity to breathe
36 Screening key to combating rising colon cancer rates in young adults
42 State of residence plays a large role in health outcomes and costs
46 What you need to know about health care for senior Nevadans
48 News and updates from the Las Vegas medical community
Dr. Andrew Priest
2024 Health Care Headliner





Touro Nevada is fortunate to have DR. ANDREW PRIEST leading the students, faculty and staff of the first medical school started in southern Nevada.
For more than a decade, Dr. Andrew Priest has brought invaluable leadership to Touro University Nevada, the state’s only college of osteopathic medicine, graduating more physicians annually than any other Nevada medical school.
In addition to Touro graduating future physicians, physician assistants, occupational therapists, physical therapists, nurses, and well-trained educators, Dr. Priest has made it his mission to have Touro students provide free healthcare services within our southern Nevada community.
As Dr. Priest continues to cultivate his role as Touro’s Campus President and Provost, his institutional vision remains driven by a deep desire to improve the quality of life for residents in the Silver State and beyond.







Touro University Nevada’s goal is to place an additional 1000 highly qualified physicians and medical professionals in our community by 2030. Learn more about us at WWW.TUN.TOURO.EDU .






 Nicole Mackie DDS, MS, FACP, is a Prosthodontist at Nevada Dental Implant Specialists
Nicole Mackie DDS, MS, FACP, is a Prosthodontist at Nevada Dental Implant Specialists
Asurgical prosthodontist’s job is to craft the perfect functional, healthy smile for patients. Yet an overlooked aspect of oral health is the intricate connection between the gut and the mouth and what one can tell you about the other.
The mouth and digestive system have microbes or groups of bacteria that work to keep the body healthy. This complex network of bacteria, viruses and fungi—collectively known as the microbiome—connects these two areas together. The gut microbe and the mouth biome are like close cousins; they get along well together and support each other. However, an imbalance in either can lead to health issues in the other.
For example, tooth decay is a warning sign that a patient’s gut microbiome isn’t functioning the way it should.
includes the teeth, which begin to decay without proper nutrition.
An imbalanced gut microbiome can also increase inflammation throughout the body, affecting the gums and elevating the risk of periodontal diseases.
The gut microbe and the mouth biome are like close cousins; they get along well together and support each other. However, an imbalance in either can lead to health issues in the other.
The gut has the very important responsibility of absorbing food, processing it and converting it into nutrients that will be sent throughout the body. A balanced gut microbiome works to eliminate toxins, digest food, protect the body against infections and regulate mood.
An imbalance means not all the nutrients consumed make it out of the gut and into the rest of the circulatory and organ systems. This
Cavities and gum disease are common issues that stem from or contribute to imbalances in the oral biome. When harmful bacteria overrule the mouth, periodontal disease can fester, characterized by inflammation, bleeding and tooth loss.
Swallowing that harmful bacteria will inevitably introduce them to the gut, where they’ll disrupt the delicate balance of the gut biome. This disruption leads to increased risk of gastrointestinal disorders, such as inflammatory bowel disease and irritable bowel syndrome. It also contributes to the development of systemic conditions, such as diabetes and cardiovascular conditions.
So how can you keep your gut microbiome and mouth healthy?
Eat a diet rich in fruits, vegetables and whole grains to feed the good bacteria in your gut, which help keep everything balanced. Take probiotics or eat foods that contain good bacteria, such as greek yogurt, and fermented foods, such as sauerkraut and kombucha, to introduce beneficial bacteria to your gut. And, of course, take care of your oral hygiene. Find a routine that works for you and your lifestyle and stick to it.
Every person has stress in their life that can be overwhelming—a demanding job, responsibilities at home, the unexpected hurdles life inevitably brings.
While stress is a physical and emotional reaction of the body, if stress or anxiety becomes chronic or overwhelming, it can affect your health by contributing to or worsening existing health conditions, said the National Institutes of Health National Center for Complementary and Integrative Health.
According to a study performed by researchers at New York University School of Global Public Health, individuals suffering from anxiety and depression are more likely to report an increase in drinking than those without mental health issues. This study also notes that older adults with anxiety and depression are more likely to develop alcohol dependence.
Instead of combating stress and anxiety by turning to alcohol, adults must learn healthy coping skills to manage their stress.
trol and Prevention, regular physical activity is one of the most important steps you can take to manage your health.
In addition to strengthening bones and muscles, helping with weight management and reducing risk of chronic diseases, physical activity may also reduce your risk of depression and anxiety.
While stress is a physical and emotional reaction of the body, if stress or anxiety becomes chronic or overwhelming, it can affect your health by contributing to or worsening existing health conditions, said the National Institutes of Health National Center for Complementary and Integrative Health.
Strategies center around relaxation techniques to counteract the ill effects of stress. Other coping skills can include:
According to the Centers for Disease Con -
According to the CDC, conversation can be a powerful coping tool. Talking to those you trust about your feelings may help manage stress and promote resilience.
According to the National Institute of Mental Health, exploring a relaxing activity that incorporates meditation, muscle relaxation and breathing exercises can improve your mental health.
Be aware of how stress and subsequently turning to alcohol to relieve that stress can be harmful to your health. The next time you’re feeling stressed, it may be a good time to try one of these healthy coping skills.
Talk with your doctor before significantly increasing your activity level. This is especially important for those with underlying medical conditions. Ask about the amounts and types of activities that may be best for you.

 K. Saad Jahangir, MD, is Director of Research and Clinical Trials–Nevada at Optum Cancer Care
K. Saad Jahangir, MD, is Director of Research and Clinical Trials–Nevada at Optum Cancer Care
While there is still much room to grow, with the establishment of the Kirk Kerkorian School of Medicine and the expansion of other medical schools like Touro University Nevada, Roseman University of Health Sciences College of Medicine, Nevada State College School of Nursing and the University of Nevada School of Medicine, significant advances are being made to ensure that quality, groundbreaking care is being delivered right here in Southern Nevada.
In fact, medical research is taking place throughout our community and throughout Southern Nevada in the form of clinical trials—more than 2,000 of them, according to ClinicalTrialsGPS.com.
Nevada Optum Cancer Care opened a clinical study for stage 4 prostate cancer, part of competitive multinational study. It is the fourth site in the world to open the study.
Some unique trials available at Nevada Optum Cancer Center are not offered nationwide. These clinical trials have attracted clients from out of state to relocate and receive treatment in Southern Nevada.
Advances in medical research improve our future. Without patients willing to participate, research for cures can’t move forward. Finding new, safer and more tolerable treatments is important to everyone.
The ability to conduct clinical trials further shows a commitment to provide cutting-edge molecular biology and technology-based treatment options for patients.
There are still many conditions without cures or treatments, and these research studies offer
hope to patients who may have exhausted all other treatment options.
Using a patient’s health information, such as their genetic profile, can help their care. This is called personalized medicine. It guides health care providers’ decisions about finding, treating and stopping illnesses. Precision medicine gives patients choices for:
n measuring an individual’s cancer risk.
n finding new cancer before it shows up on scans.
n finding the best care plan when the origin of the cancer is unknown.
n physical, spiritual and social support during cancer care.
n cost-effectiveness.
Professionals at Optum Cancer Care focus on the right treatment at the right time for the right patient via the precision medicine program, which has the ability to open clinical trials within three weeks, compared to the health care industry average of three to six months.
By combining clinical trials and personalized medicine with other care services, Optum’s goal is to improve all parts of a patient’s health during their cancer journey.
The clinical trials program is in the very early stages of development, and much more work is needed. As it progresses, Optum’s goal is for patients and the community to become part of this journey. Optum’s philosophy is a holistic approach where mind, body and soul must be in synergy to get the best therapeutic outcomes.
For information, visit optum-cancer.com/ clinical-trials.
At Dignity Health, we believe humanity holds the power to heal. That’s why we’re honored that two of our own have been recognized by Health Care Quarterly as 2024 Health Care Headliner honorees. Thank you for your dedication and unending pursuit of excellence.
 Carla Laos, MD Medical Director, Siena Pediatric ED
Carla Laos, MD Medical Director, Siena Pediatric ED
 Ryan Grabow, MD Orthopedic Surgeon
Ryan Grabow, MD Orthopedic Surgeon

Vegas Inc’s Health Care Headliners honors some of Southern Nevada’s most creative and industrious health care leaders. These 10 headliners are dedicated to their craft and to the health and well-being of the community. They are scientists, doctors, educators, and they represent the resilient spirit of the Las Vegas Valley through their work each day.

Keyona Cole, regional chief nursing o cer at Intermountain Health, began her career in health care as a senior at an inner-city high school in Milwaukee, Wisconsin. The school provided two health care tracks for students, and Cole began her training to become a certified nursing assistant, graduating with her license.
Cole went on to receive her bachelor of science in nursing from Alverno College in 2001. She is a board-certified nurse practitioner and a member of the American Academy of Nurse Practitioners and the American Nurses Association.
Cole’s proudest accomplishment to date is the inception of Intermountain Health’s medical assistant program, which she helped establish with NV Careers.


The program provides applicants with the necessary training to pursue a career in health care, regardless of their financial situation. It creates opportunities for individuals in underserved communities, while also helping address sta ng shortages. It’s on its way to becoming a state-recognized apprenticeship program.
Cole also serves as a diversity, equity and inclusion leader and board member of Goodwill of Southern Nevada, dedicating herself to reducing poverty and its e ect on Southern Nevadans’ health.



When asked what health advice she’d share with everyone, Cole said, “Prevention, prevention, prevention. Living healthier lifestyles that focus on healthy eating, physical activity, and spiritual and mental well-being are key to preventing health care problems. Getting preventative exams and completing lab work and testing can help to identify and stop or prevent advancement of health issues.” + + + +

Regional Chief Nursing O cer, Intermountain Health
27 years in health care

“The more providers we can get to live and practice here, the less patients will have to ‘wait or wander’ to get the health care they need.”

Touro University is Nevada’s largest school of medicine and only school of osteopathic medicine. It trains doctors, nurses, physical and occupational therapists, physician assistants and medical educators, many of whom choose to stay in Nevada after graduation.
As the campus president and provost, Andrew Priest’s vision for the school is driven by a deep desire to improve the quality of life for Nevadans.
“Many of our graduates choose to practice in Nevada and are selected by residency programs here,” Priest said. “The more providers we can get to live and practice here, the less patients will have to ‘wait or wander’ to get the health care they need.”
As part of his mission, he’s made it possible for Touro’s students to provide free health care in the community by playing an instrumental role at Project Homeless Connect, which o ers services to more than 2,500 individuals experiencing homelessness each year.
He also led Touro in partnerships with the Engelstad Foundation and the Las Vegas Metropolitan Police Department that provided medical training and equipment to first responders.
Overseeing one of the fastest-growing medical schools in the western U.S., Priest wants all students to achieve their dreams.
Priest serves on the board of the Foundation for an Independent Tomorrow, Las Vegas HEALS and Las Vegas Global Economic Alliance. He and his wife also work with their church’s 12-step addiction recovery program.
Campus President and Provost, Touro University Nevada 35 years in health care

“Your health is your most valuable asset, but people often take it for granted until issues arise. During my time in health care, I’ve learned that you have to make your health a priority.”
For the past 26 years, Shana Tello has devoted herself to service, setting an example of compassion and resilience for fellow health care professionals and administrators.
Tello oversees UMC’s partnerships and government a airs, including its innovative collaboration with the U.S. Air Force. Through this program, approximately 100 Air Force physicians, nurses and medical technicians work with UMC sta to provide high-level care to Southern Nevadans while preparing for future deployments. It’s the largest military-civilian partnership of its kind in the U.S. Because of her trusted leadership and support, the Air Force designated Tello as an honorary commander.
One of Tello’s priorities for advancing health care in Southern Nevada is improving access. She’s played a key role in opening seven new clinic locations, including quick care, primary care and specialty clinics.
She’s also excited about the expansion of telemedicine, especially the UMC Online Care app. Community members can use the app to contact health care providers at UMC at any time of the day or night with an average wait time of six minutes for online urgent care visits.


Tello also provides valuable service in the community, working with local organizations such as Courtney Children’s Foundation, which provides mentorship and support for teenage mothers.
“As a former teen mom, I served as a mentor for two young mothers, sharing my experience and o ering valuable guidance at a critical point in their lives,” Tello said.
She also supports Vegas Stronger, a nonprofit dedicated to helping community members struggling with substance abuse, mental illness and homelessness.


Academic and External A airs Administrator, UMC 32 years in health care


At Roseman University, Matthew Thacker leads the Advanced Education in General Dentistry Residency and manages Roseman’s dental clinic in Summerlin, partnered with Cure 4 The Kids Foundation.

Thacker expanded the AEGD program from one clinic with two residents to two clinics with four fulltime faculty and four residents. He’s also increased the number of patients. In 2022, the Summerlin clinic saw four patients a month. By August 2023, the clinic was registering 73 a month.
Thacker served four years in the U.S. Navy after graduating from dental school, and his current leadership continues to embody the Navy’s four attributes of initiative, accountability, integrity and toughness.

“My previous service as a dental o cer in the U.S. Navy instilled in me a profound dedication to serving those who serve,” Thacker said. “This dedication didn’t end with my military service; it evolved into a heartfelt mission to make a lasting di erence in the lives of service members and veterans.”
Working with the Adopt a Vet Dental Program, Thacker provides local veterans with prioritized, comprehensive dental care at no cost.
Thacker has worked tirelessly to develop and establish a comprehensive care model with the Roseman College of Medicine. This model is built on communal referrals, shared patient records and open lines of communication between providers.

He’s also working with the college of pharmacy to coordinate rotations for pharmacy students to review medications for complex polypharmacy patients. To encourage future medical providers of Southern Nevada, Thacker also supports Roseman’s Aspire program to expose local high school students to the dental profession.

Clinic Director and Program Director of the Advanced Education in General Dentistry Residency, Roseman University of Health Sciences 10 years in health care












Carla Laos began leading the Pediatric Emergency Department at Siena Hospital in 2022.
Before relocating to Nevada, Laos practiced medicine in Florida, Alaska, Texas, California and Peru. New to the hospital and to Nevada, Laos’ goal was to provide the highest quality of care to gain the trust of the community.
To accomplish this, Laos staffed the pediatric emergency department with physicians double-boarded in pediatrics and pediatric emergency medicine. She introduced coaching and team building, cultivating medical professionals who were focused on delivering quality compassionate care to every patient.
Leading a pedi-
atric emergency department is no small feat.
“This involves interfacing with a myriad of different services external and internal to the hospital,” Laos said. “The art of orchestrating multiple teams to work together towards a common goal is incredibly fulfilling.”
Laos is excited by the upcoming generation of physicians and their potential. She’s also encouraged by the technological advancements in the medical field and the evolution of medical education and care augmented by AI.
She remains involved in the education of future medical professionals by hosting medical students from Touro and UNLV in Siena’s pediatric emergency department.
Outside of work, Laos enjoys hiking, biking and spending time with her family. She coaches her daughter’s soccer teams and encourages them in their academic endeavors.
Medical Director, St. Rose Siena Pediatric Emergency Department, Pediatrix
19 years in health care

Giving me my chance to be mom again
Comprehensive Cancer Centers has participated in the development of 100 new FDA approved cancer treatments. With 150 ongoing clinical research studies, right here in Southern Nevada, we are entering a new age in cancer treatment — where people are no longer entrenched in their battle against cancer, but instead living with cancer These new cancer therapies are increasing the quality of life for our patients and their families, and most importantly, giving them the opportunity to live their lives to the fullest.

“I take great satisfaction in decreasing the stigma of mental health that prevents many from seeking care.”

As a licensed clinical social worker, LaTeisha Morgan chose a career path that aligned with her core values of compassion, empathy and service to others. After graduating with a bachelor’s degree in criminal justice from the University of Mississippi, Morgan moved to Las Vegas to pursue her master’s degree in social work. She now serves as a clinical manager and licensed social worker with Intermountain Health.
“What I find most rewarding about my job is witnessing the transformative impact on individuals’ lives as they develop healthy coping habits and regain their ability to make empowering choices,” Morgan said.
Morgan strives to provide inclusive and culturally sensitive care as she integrates mental health services into primary care.
In her opinion, suicide prevention is one of the most critical issues in Southern Nevada and should be a health care priority. Morgan’s work allows her to connect with patients and teach them coping skills.
Her advice for living a healthful life includes being present in the moment. “By embracing the present moment, we can fully engage in activities that bring us joy and cultivate a sense of gratitude,” Morgan said.
Morgan also participates with local community organizations, firmly believing in contributing to positive change for everyone. In addition to the service she provides in her profession, Morgan has been a member of the Las Vegas Urban League Young Professionals, Junior League of Las Vegas, Top Ladies of Distinction and the National Association of Black Social Workers.
Clinical Manager/Licensed Clinical Social Worker, Intermountain Health 16 years in health care
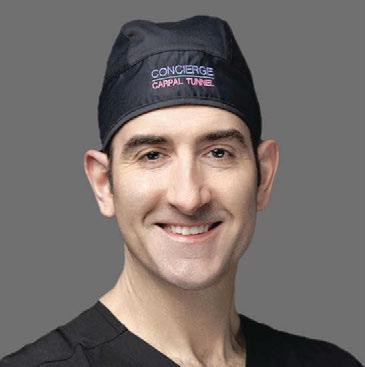
Ryan Grabow is the owner and medical director of Concierge Carpal Tunnel and Hand Surgery, the only National Carpal Tunnel Center of Excellence in Las Vegas and the entire West Coast.
In his practice, Grabow implements modern technology to perform surgery as minimally invasive as possible. With the help of ultrasound guidance, he can treat carpal tunnel and trigger finger quickly using only local anesthesia and an incision the size of a breath mint.
Many patients return to work in a matter of days and only need overthe-counter pain medications for postoperative discomfort.
“I believe I was inspired to pursue a career relieving my patients’ pain and restoring function to their hands, wrists, elbows, and shoulders because my own hand use defines who I am as a person,” Grabow said. “My hands have always been the tools of my creative mind. I understood early on in my medical training that a patient with carpal tunnel syndrome or a broken wrist doesn’t just have a problem with what they can do, they are also su ering a crisis of who they are due to their loss of hand function. While it may be a calling or career for some of us, we all use our hands as musicians, artists, mechanics, chefs, and healers. It is good for our soul to create with our hands. Having the privilege to use my hands to restore my patients’ ability to use theirs, is not just what I do, it is what I was called to do, it’s who I am.”
Instilled with the belief that a doctor’s job is not just to treat illness and injury but also to prevent it, Grabow educates his patients on safety measures. He also creates informational videos, shared via social media, to spread awareness of common hand injuries, including cutting avocados incorrectly and su ering unnecessary burns in the kitchen.
Owner and Medical Director, Concierge Carpal Tunnel and Hand Surgery
18 years in health care


Aimee Foord wears many hats as the director of research at Cure 4 the Kids Foundation. She meets with patients, conducts research studies, coordinates care, champions comprehensive health care, and acts as an adjunct assistant professor at Touro University to prepare and train the next generation of hematologists.
Foord specializes in pediatric hematology, including benign disease such as bleeding disorders, thrombophilia, abnormal blood counts and sickle cell disease.
She is a key member of Cure 4 the Kids Foundation—the only pediatric hematology and oncology practice in Southern Nevada.
“Studies show that with chronic disease like sickle cell disease, patients do clinically better when taken care of in a comprehensive approach,” Foord said.
At her clinic, this means the patient will meet with the physician and undergo routine labs; see the nurse coordinator who will educate the patient and parents and provide referrals and plans for the next year; go over medications and storage with a pharmacist; discuss emotional, financial and educational needs with social workers, an education team and neuropsychologist; receive screenings by pediatric dentists and physical therapists; and meet with a representative from a community organization that supports families of patients.
In 2022 only 27 of 200 Cure 4 the Kids patients were cared for in comprehensive clinic. After identifying barriers and addressing concerns, 57 patients were seen in comprehensive clinic in 2023—more than double the number of patients who received that level of care the previous year.
Director of the Bleeding and Clotting Disorders Clinic, Cure 4 The Kids Foundation 11 years in health care








Make The Valley Health System YOUR CHOICE




All Valley Health System hospitals are accredited by The Joint Commission for meeting performance standards for delivering safe, high-quality care.
Our acute care hospitals hold national certifications in stroke and heart attack care. Our hospitals consistently earn recognition from the American Heart Association® and American Stroke Association® for meeting or exceeding national standards for heart and stroke care.
The Valley Health System hospitals also consistently earn national quality awards for services such as wound care, orthopedics, maternity care, weight-loss surgery and more.

“Helping a child achieve their best possible vision also sets them up for a lifetime of success.”Wade Vandervort/Sta
Naomie Warner, ophthalmologist subspecializing in pediatric ophthalmology and pediatric neuro-ophthalmology, is the only physician with her specific set of subspecializations and fellowships. Warner has treated patients of all ages but takes special pride in caring for children, even removing pediatric cataracts from two newborn patients.
Warner uses burgeoning technology and techniques, such as Luminopia, an alternative lazy eye treatment that has shown significant results in correcting children’s vision. Luminopia utilizes a VR headset to strengthen the eyes as a substitute for traditional lazy eye treatments such as wearing a patch that children find uncomfortable.
“I love helping people,” Warner said. “I love when I can improve vision, eliminate double vision or improve someone’s self-confidence.”
She also champions the needs of children with visual impairments through her service on the board of the Nevada Blind Children’s Foundation. The nonprofit organization provides a preschool for young visually impaired children and after school services for older visually impaired children.


“This is important to me because it’s the only program of its kind in Las Vegas, and Nevada is one of the only states in the country without a dedicated school for the blind,” Warner said. “We need to create more services like this for our children.”
Warner suggests that anyone concerned about their vision see a specialist as early as possible so an e ective treatment plan can be made, noting that most eye problems are easier to solve with an early diagnosis.
She is grateful for the ongoing support she receives from her husband, two children, and parents.



Charles Bernick has dedicated nearly four decades to researching and improving brain health in Nevada and beyond.
In 1994 Bernick moved to Las Vegas and became the only neurologist specializing in dementia in Southern Nevada. Since then, he has conducted more than 30,000 patient visits.

Bernick was also the first physician hired at the Lou Ruvo Center for Brain Health where he has been the lead primary investigator of every major Alzheimer’s or dementia trial in the center’s portfolio for the past 15 years.
“I came to Las Vegas, like a lot of people, with the intent to build or create something needed and hopefully lasting,” Bernick said. “In my case, it was to develop a statewide system of Alzheimer’s care in Nevada that would equal or exceed anywhere in the nation. I believe we accomplished that.”
As early as 1996, Bernick pioneered telemedicine via video conferencing, enabling rural Nevadans to receive care.
In addition to his work with Alzheimer’s and dementia, Bernick has led research on Chronic Traumatic Encephalopathy since his launch of the Professional Athletes Brain Health Study in 2011. The study examined the e ects of repetitive head impacts in professional and retired boxers and MMA fighters. It continues to study early detection of accumulating brain injury and early risk factors of Chronic Traumatic Encephalopathy in an expanded range of athletes including more than 900 particiapants ranging from professional bull riders to motorsport competitors.


Senior Director, Cognitive Disorders, Cleveland Clinic Lou Ruvo Center for Brain Health
40 years in health care
















UMC pulmonologist rst to bring revolutionary lung procedure to Nevada patients
Imagine not being able to wash dishes, take a shower or get up from the couch to answer the door without gasping for air. These everyday tasks can feel like climbing Mount Everest for individuals living with severe chronic obstructive pulmonary disease.
“Upstairs was only for sleeping, and once I got downstairs, I couldn’t go back up again for the rest of the day,” said John Ricker, a 63-year-old Las Vegan with severe emphysema.
Ricker was diagnosed more than 12 years ago. “As my emphysema progressed, it became more di cult to do normal activities, like taking the trash out or even walking short distances,” Ricker said. “I had to give up the sport that I love—disc golf.”
According to the Centers for Disease Control and Prevention, chronic obstructive pulmonary disease a ects almost 16 million Americans and is the sixth-leading cause of death in the United States. In the Silver State alone, the CDC estimates the disease a ects more than 6% of the adult population.
COPD happens when damage to the airways or di erent areas of the lungs causes restricted air ow and makes it di cult to breathe. Emphysema is a form of COPD that occurs when there is damage to the walls between the air sacs of the lungs, making it harder to exhale. While most cases are linked to smoking, excessive air pollution and a rare genetic condition called alpha-1 antitrypsin de ciency can also cause the disease.

Ricker hit his breaking point during the Thanksgiving holiday when he couldn’t play catch with his young grandson. “That’s when I realized how much this disease has taken from me,” Ricker said. “I wanted to be able to throw a football around with my grandson. I wanted to get back to disc gol ng with my friends.”
Ricker approached his pulmonologist for help and learned about a procedure o ered at UMC that would change his life.
There is no cure for COPD, but innovative treatments and procedures are giving patients a chance for a better quality of life.
Arthur Oliver Romero, MD, UMC practitioner, started as a pulmonologist in Nevada in 2010 and is an associate professor at the Kirk Kerkorian School of Medicine at UNLV.
In 2019, he underwent an advanced fellowship in interventional pulmonary medicine at University of California, San Francisco, and brought his skills back to Southern Nevada to establish the only interventional pulmonology program in the state.
“Oftentimes, these patients had to go out
Continued on page 35

Continued from page 33
of state to get the procedures they needed, so my goal was to narrow this gap and bring a higher level of pulmonary care to Nevada,” Romero said.
During his time at UCSF, Romero learned many new procedures, including bronchoscopic lung volume reduction, a minimally invasive procedure that improves lung function and quality of life for patients suffering from emphysema. In 2022, Romero became the first physician to bring this groundbreaking treatment to patients in Nevada at UMC.
“Imagine your lung as a sponge. When you have emphysema, the sponge has large holes.” Romero said. “As those holes grow, they trap in air that occupies extra space in the chest; and if your lungs are already filled with air and you try to take another deep breath, there’s no more room. That’s why these patients are so out of breath.”
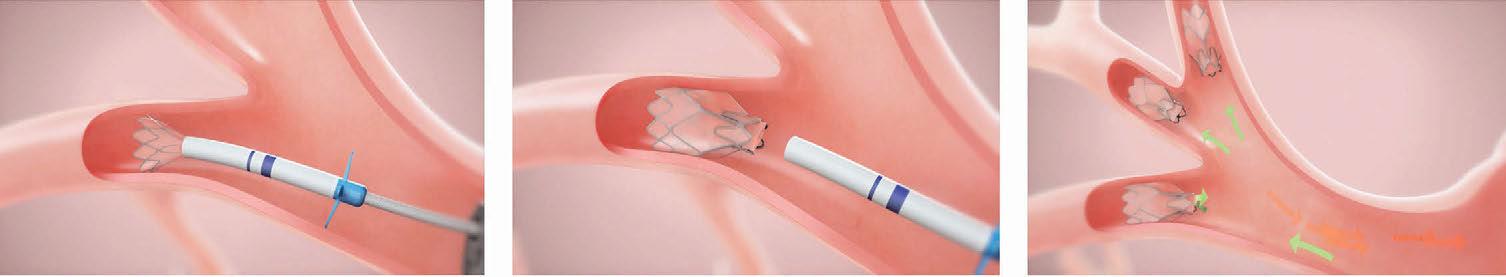
During bronchoscopic lung volume reduction, a pulmonologist uses a bronchoscope—a thin and flexible camera inserted through the mouth—to place tiny valves directly into the airways. The one-way Zephyr Endobronchial Valves allow the damaged areas of the lungs to deflate and release the trapped air, while helping the healthier areas of the lung expand and let more air inside. On average, three to five valves are used in each procedure. With no incisions required, Romero said some patients experience near-instant relief.
Considering the severity of the disease and the effectiveness of this procedure, Romero said he receives inquiries from patients living in all parts of Nevada and surrounding regions,
including southern Utah and western Arizona.
While the demand is growing, Romero cautioned bronchoscopic lung volume reduction is not for everyone.
“This procedure doesn’t come without risks, and there is a very stringent screening process,” Romero said. “The patients who are candidates for bronchoscopic lung volume reduction have disease severity that has to fit into this small window. Their lungs are damaged enough that we must intervene, but not so damaged that they wouldn’t be able to handle the procedure and possible complications.”
After patients receive a referral from their primary pulmonologist, they must meet several other criteria and go through extensive testing, including a pulmonary function test, a CT scan, a six-minute walking test and cardiac function evaluations.
“It’s just amazing how we can now offer this kind of advanced treatment for our patients,” Romero said. “Previously, many patients had no option but to undergo a lung transplant, which is even more difficult to qualify for and is only available out of state,” Romero said.
“From the moment I heard of this procedure, I was all in. It gave me hope,” Ricker said. He underwent bronchoscopic lung volume reduction in September, and he’s now playing catch with his grandson and back on the disc golf course. “I’m back to doing the things I love and the things I haven’t been able to do in years,” Ricker said. He credits his second chance at life to Romero, whom he refers to as a rock star.
“Something as simple as the ability to take a deep breath is something we all take for granted until it’s gone,” Romero said. “It’s so rewarding to help these patients achieve more fulfilling and functional lives.”

“Oftentimes, these patients had to go out of state to get the procedures they needed, so my goal was to narrow this gap and bring a higher level of pulmonary care to Nevada.”
— Arthur Oliver Romero, MD

Fadi Braiteh , MD, is a medical oncologist and Director of the GI Malignancies Program at Comprehensive Cancer Centers and an associate clinical professor at UNLV School of Medicine
BY FADI BRAITEH, MDIn industrialized countries, the majority of new patients with colon cancer (four out of five) are diagnosed in an early stage, as opposed to half a century ago when it was one in five cases. This change in statistics may be attributed to colon cancer screening programs implemented over time and efforts to recognize alarming early symptoms and signs.
In the U.S., this has resulted in a first-time reduction in colon cancer mortality. While this is accurate for patients older than 52, the same does not apply to younger patients. The early symptoms of colorectal cancer are often ignored by younger individuals, and even overlooked by some health care providers because of the similarity of symptoms with other conditions. As a result, colorectal cancer might go undetected until it reaches an advanced stage.
This lack of awareness is partly due to misconceptions about risk factors such as family history, diet and age, which has led to a limited understanding of the warning signs.Consequently, and because of other unknown factors, there has been a noticeable increase in the number of younger adults being diagnosed with colorectal cancer.
To address this issue, it’s crucial for individuals in their 20s, 30s, and 40s to have open discussions with their doctors about any suspicious symptoms they may experience.
The American Cancer Society released a report in early 2023, revealing a concerning trend in colorectal cancer diagnoses among younger individuals. According to the report, 20% of diagnoses in 2019 were found in patients younger than 55, which is a significant increase compared to the rate in 1995
Additionally, the report highlighted that rates of advanced disease have been steadily rising by
approximately 3% annually in individuals under the age of 50. The ACS further projected that in 2023, an estimated 19,550 new cancer diagnoses and 3,750 deaths would occur in people younger than 50, emphasizing the urgent need for early detection and intervention strategies.
What is leading to this statistical increase in cases in young adults? Based on current scientific knowledge, there is no definitive identifiable cause. Experts find themselves in a bit of scramble to discover why rates are increasing. Several factors have been linked to this trend, including a sedentary lifestyle and rising rates of obesity, heavy smoking, excessive alcohol consumption, consuming low-fiber and high-fat diets or diets rich in processed foods. Environmental factors may contribute as well.
The answer likely lies in a combination of all these factors. It’s common to assume that having a family history of colorectal cancer or polyps can increase the risk of developing colorectal cancer, but it’s a little-known fact that conditions like inflammatory bowel disease can also increase risk.
Two decades ago, colorectal cancer was the fourth leading cause of cancer death in men and women under the age of 50. According to the Journal of the American Medicine Association for the same age group, it’s now the leading cause of death in men and the second leading cause in women, with breast cancer remaining the primary cause of death in women under 50
According to the American Cancer Society, almost 10,540 Nevadans will be diagnosed with colorectal cancer, and 2,190 will lose their battle in 2024 alone.
To reduce your risk of colorectal cancer, it’s important to make certain lifestyle changes. Smoking and excess alcohol consumption have been linked to an increased risk of colorectal cancer—try to quit smoking altogether. Drink in moderation. Regular exercise is also beneficial










in reducing the risk of colorectal cancer. Walking, jogging, swimming and cycling can all be e ective in maintaining a healthy colon.

Adequate ber intake is essential for a healthy colon, and it’s recommended to consume 25 grams of ber per day to maintain optimal colon health. This can be achieved by incorporating more fresh fruits, vegetables, whole grains, beans and legumes into your diet. Reducing red meat consumption is also crucial.
Don’t lose sight of the increasing importance of screening measures. The colonoscopy is widely regarded as the most e ective method for detecting colorectal cancers and has proven to be life-saving because it allows removal of precancer lesions.
It’s important to connect with medical professionals who make you feel comfortable throughout the testing process. Other modalities such as cancer DNA detection in stool, a virtual colonoscopy and even occult blood screening in the stool can be attempted.
Self-advocacy is key. If you, as a patient, feel like something is amiss, speak up because sometimes you must be your biggest advocate.
 Andrea Roa is Communications and Marketing Manager for St. Rose Dominican Health Foundation.
BY ANDREA ROA
Andrea Roa is Communications and Marketing Manager for St. Rose Dominican Health Foundation.
BY ANDREA ROA
According to the Centers for Disease Control, six out of ten adults in the U.S. are dealing with a chronic disease, and four out of ten are dealing with more than one.
Dignity Health–St. Rose Dominican is the only not-for-profit, faith-based hospital system in the Las Vegas Valley. Guided by the values of the founding Adrian Dominican Sisters, St. Rose is helping residents fight chronic diseases through the latest proven treatments and prevention education.
Chronic diseases are illnesses that persist over a long period of time and require ongoing medical attention. Heart disease, cancer, stroke, chronic lung disease, diabetes, Alzheimer’s disease—these are some of the chronic diseases many Americans cope with. These chronic diseases take lives and drain trillions of dollars in healthcare resources, $4.1 trillion annually, according to the CDC.
“What we do at our health centers changes lives,” Kelly said. “Chronic diseases need constant attention, and we empower individuals, families and caregivers through education. We’re truly the best-kept secret in town that you don’t need a prescription or referral for.”
Thanks to the generosity of private donations and grants, the CST program launched in 2022 and immediately began making a difference for individuals and their families.
CST is an evidence-based treatment for people with mild to moderate dementia. It involves group activities twice a week, each focusing on a different cognitive function.
“WE HELP PEOPLE TAKE CONTROL OF THEIR HEALTH AND SHOW THEM THAT BEING HEALTHIER IS POSSIBLE WITH THE RIGHT SKILLS, KNOWLEDGE, AND SUPPORT.”
—Shelley Williams, nurse and lead diabetes educator
The community health needs that St. Rose is helping to address were identified in the hospital’s most recent Community Health Needs Assessment. These include access to care, transportation funding and a topic at the top of many residents’ minds: chronic disease.
Mary Ann Kelly oversees the cognitive stimulation therapy program for St. Rose Dominican’s Community Health and Wellness Centers. She knows how important knowledge is in fighting chronic diseases.
“I know it might seem like she’s not understanding,” said the caregiver of a cognitive stimulation therapy client, “but she gets up Tuesday and Thursday, gets dressed by herself, and is ready to come here. Before this program, she didn’t know when Tuesday and Thursday were.”
Even though the program was initially designed to last for seven weeks, research shows that people who continue with regular maintenance can experience positive results. Kelly said that 70% of individuals who finish the program have better cognitive scores, and 83% report feeling less depressed and have a better quality of life.
About 6.7 million Americans 65 and older have Alzheimer’s or dementia. Programs like CST at St. Rose give patients, families and caregivers hope and tools to battle chronic disease.

Another equally important chronic disease focus for St. Rose is prediabetes, where blood sugar levels are higher than normal but not high enough for a diagnosis of diabetes. About 98 million American adults have prediabetes, but 80% of them don’t know they have it.
“We help people take control of their health and show them that being healthier is possible with the right skills, knowledge, and support,” said Shelley Williams, a nurse and lead diabetes educator.
Simple changes like losing weight, being more active, and eating healthier can prevent many medical problems, including type 2 diabetes.
The National Diabetes Prevention Program research study showed that people who participated in the program saw a 58% reduction in their risk of developing type 2 diabetes, and individuals 60 and older saw a 71% reduction.
St. Rose is a CDC-recognized provider of the Diabetes Prevention Lifestyle Change program. This past year, 80% of the participants reached the goal of 5% or greater weight loss, reducing their risk of developing
type 2 diabetes.
For people who already live with diabetes, diabetes self-management education and support services are available. This past year, 87 % of individuals who participated in the diabetes self management program reached their self care behavior change goal, which are steps to improve their overall health and reduce their A1 c (average blood glucose) levels. A reduction in A 1c helps to reduce the risk of complications of diabetes, such as kidney disease and eye disease.
Fighting a chronic disease isn’t something you can do alone, it takes a community working together. St. Rose Dominican has served southern Nevada for 77 years and continues its mission and ministry to serve our community.
By providing more than 119 free or low-cost resources, St. Rose Community Health and Wellness Centers are taking a proactive approach to the fight against chronic diseases and more. If you or someone you know needs resources, contact a St. Rose Community Health and Wellness Center near you.

Mark
Stradling , DO, is an ophthalmologist and cataract surgeon at Nevada Eye Physicians
BY MARK STRADLING, DOConstruction will be in full effect in Las Vegas this summer, along with 110-degree heat and intense UV exposure. The combination can lead to an increased risk of eye damage for all indviduals who spend time outside, particularly those who work outdoors.
Any amount of exposure can be a risk for everyone. However, for those working outside, the sun reflecting off surfaces can cause a painful sunburn called photokeratitis on the front part of the eye. It causes redness, blurry vision, sensitivity to bright light, and in rare cases, temporary vision loss.
Prolonged exposure to UV rays and heat can result in abnormal eye growth known as Pterygium, which is a growth on the clear tissue that surrounds the white part of the eye. It can spread to the cornea (the clear part of the eye where light passes through). The effect is decreased vision and irritated eyes. The growth results from years of ultraviolet light exposure, heat, wind and dust. Everyone who spends a lot of time outdoors without proper UV protection is at risk of developing pterygia. Wearing wrap-around style sunglasses with proper UV protection and keeping the eyes well lubricated is the best way to minimize your risk.
common eye conditions and can be identified as growths on the eye with blood vessels. They can begin as Pinguecula which are white or yellow fleshy growths consisting of anything from calcium to protein or fats that appear on the eye. They are not dangerous unless they go untreated and grow to cover the cornea. At that point, the individual can be at risk of vision issues, and in severe cases, can contract scarring over the cornea. Some symptoms to be on the lookout for include:
ANY AMOUNT OF EXPOSURE CAN BE A RISK FOR EVERYONE. HOWEVER, FOR THOSE WORKING OUTSIDE, THE SUN REFLECTING OFF SURFACES CAN CAUSE A PAINFUL SUNBURN CALLED PHOTOKERATITIS ON THE FRONT PART OF THE EYE.
n Dry, itchy or burning eyes
n Blurred vision
n Yellowish or white bump on the whites of the eye
n Conjunctiva swelling or redness
Pterygiae can be uncomfortable, but the good news is that they can be easily treated with medication such as steroid eye drops or removal with either an autograft or amniograft.
It’s important to keep in mind they are easily preventable. Some of the most common and helpful preventative measures include:
n Always wearing proper UV eye protection, such as wraparound sunglasses, when going outdoors for prolonged periods.
n Ensuring the sunglasses are equipped with UVA and UVB full-spectrum protection.
n Keeping eyes lubricated with eye drops when they become dry or irritated.
According to the American Academy of Ophthalmology, Pterygiae is also known as “surfer’s eye” because it more commonly appears in surfers who spend prolonged periods of time in unprotected sun exposure. Pterygiae, are fairly
n Avoiding climates with extreme wind and dirt that can cause severe irritation to your eyes. The best way to prevent Pterygiae is early detection with regular check-ups with your ophthalmologist.










 Patty Starr , top, is President and CEO of Health Action Council, and Craig Kurtzweil is Chief Data and Analytics Officer
BY PATTY STARR AND CRAIG KURTZWEIL
Patty Starr , top, is President and CEO of Health Action Council, and Craig Kurtzweil is Chief Data and Analytics Officer
BY PATTY STARR AND CRAIG KURTZWEIL
Afirst-of-its-kind study reveals that community health and nonclinical social barriers have a much more profound effect on workforce health than previously recognized.
The report, which focused on Health Action Council members’ claims across more than 217,000 covered lives, marks the first study to examine social factors within any claims data. It unveils some of the most comprehensive findings on social determinants of health—the conditions in which people live, learn, work, play and worship—ever released at the member level.
Titled “Community insights: Key factors that influence employee health,” the seventh annual white paper by HAC and UnitedHealth Group, highlights crucial insights for HR and benefits managers to utilize when customizing their plans, ultimately helping to improve the health and productivity of their workforce.
One of the white paper’s most striking takeaways is the connection between where employees live, its effect on their life expectancy and costs for employers and their employees.
There is an extreme disparity in mortality rates among employees who work for the same company across various states.
When analyzing claims data across the 10 states with the most HAC members, South Carolinian employees are 55% more likely to die before age 75 than their Californian coworkers.
Approximately 66% of HAC members live within the 20 least healthy states, according to America’s Health Rankings data. If those mem-
bers lived in the 20 healthiest states, the total covered per member per month amount would be reduced by $61 million — 7% of spend.
Four in 10 children have a parent battling at least one high-risk social determinants of health hardship, such as social isolation or financial, food or housing insecurities.
Those children faced higher rates of suicidal ideation, depression and ER visits.
Thirty percent of adults are at risk for social isolation, which increases the risk of dementia by 50%, stroke by 32% and heart disease by 29%.
Adults diagnosed with a condition such as diabetes or depression face even higher rates of food insecurity and social isolation, respectively.
Millennials have the highest rates of social determinants of health risk across generations, as 13% of them are facing three or more risks.
This study marks a turning point in benefits strategy, transitioning from the traditional focus on retrospective claims data, company culture and budgets, to a more comprehensive approach. It emphasizes a need for employers to consider the geographic locations of their employees and the associated community health and SDoH data to help advance employee health, boost productivity and optimize costs.
The evidence presented is a clear testament of the profound effect that strategic decisions can make in workforce health, operational efficiency, and business performance. For more than 13 years, HAC employers have experienced better health outcomes and beat industry trends, regardless of where their employees are based.
1. Conduct comprehensive analysis:
Broaden your data analysis by integrating geographic, community health and SDoH risk factors. This expanded view should also consider identifying key subpopulations within your workforce to go beyond generic disease categories. Use this in-depth analysis to assess the impact of location on health outcomes and costs, factoring in state health rankings and regional health expenditures. A holistic approach allows for a nuanced understanding of your workforce’s health needs, setting the stage for more targeted interventions.
2. Tailor health solutions: A one-size-fits-all approach is ineffective in addressing the diverse needs of your workforce. Recognizing the unique health challenges among your employee groups allows you to move beyond standard solutions to design health plans and initiatives that are truly reflective of your employees’ varied lifestyles. Engaging directly with employees to understand their specific concerns enables the development of custom tools and resources to help address individual health needs and foster a more inclusive and supportive workplace environment.
3. Educate your workforce: Empower your employees with knowledge about the importance of timely health care access, the benefits of establishing strong relationships with primary care providers, and the value of engaging in preventive health care practices. Educating your workforce is crucial in fostering a culture of health awareness and proactive health management, which may ultimately lead to improved health outcomes and enhanced organizational health.
By embracing these strategies,

benefits managers can spearhead transformative health management initiatives within their organizations. This approach helps ensure that interventions are grounded in comprehensive data analysis, tailored to meet individual needs, and enhanced by educational efforts to foster a proac-
tive and informed culture of health.
Health Action Council is a not-forprofit organization representing large employers to enhance human and economic health through thought leadership, innovative services, and collaboration.
 Jon Sprecher , RN, is the Director of Nursing at Desert Hope Treatment Center
BY JON SPRECHER, RN
Jon Sprecher , RN, is the Director of Nursing at Desert Hope Treatment Center
BY JON SPRECHER, RN
As the country continues to grapple with the ongoing opioid crisis, and intentional fentanyl use becomes increasingly common, it is imperative to take actionable steps to save lives.
According to the National Institute on Drugs Abuse, 193 people die from opioid-related overdoses every day. Many of these deaths are preventable. Naloxone distribution is effective in preventing overdose deaths.
When addiction specialists and policymakers discuss the opioid crisis, it’s usually in the context of waves. While heroin has been on the black market for decades, the significant increase in opioid prescribing in the 1990s led to the first wave of the opioid overdose crisis.
The second wave began in 2010, with a rapid increase in heroin-related overdose deaths.
to manufacture, and its increased potency (up to 50 times more potent than heroin and 100 times more potent than morphine) makes it highly addictive and dangerous.
THERE’S A MISCONCEPTION THAT
HAVING
NARCAN AVAILABLE ENCOURAGES DRUG USE, HOWEVER, THIS ISN’T TRUE. LIKE A FIRE EXTINGUISHER DOESN’T ENCOURAGE ARSON, NARCAN DOESN’T CAUSE DRUG USE. HAVING NARCAN ON HAND IS A NECESSARY SAFETY PRECAUTION.
The third wave started in 2013, with an alarming rise in deaths involving illicitly manufactured fentanyl and other synthetic opioids.
We are still in the third wave, though a fourth wave—increased deaths involving stimulants such as methamphetamine mixed with fentanyl— is threatening lives across the country.
Fentanyl is ubiquitous; it’s relatively cheap
Just a few years ago, most people weren’t aware of how frequently drugs were adulterated with fentanyl, a significant driver of overdose deaths. Now, there are patients who come to in-patient rehab in Las Vegas, and their primary drug is fentanyl. While people may have started out using prescription opioids or heroin, they seem to be migrating to fentanyl because it’s cheaper, overwhelmingly powerful and it’s everywhere.
The danger of fentanyl primarily lies in two intertwined factors: its potency and its lethality. Any opioid has the potential to be deadly, but because fentanyl is so potent, the line between a “safe” dose and a deadly overdose is dangerously thin. In fact, it can take as little as 2 mg of fentanyl to cause an overdose death; that’s roughly equivalent to 10 grains of table salt.
Because illicitly manufactured fentanyl has made its way into so many street drugs, anyone using illicit drugs or counterfeit pills—not only opioids—is at risk of a fentanyl overdose. Fentanyl has been found in nonopioid illegal drugs such as counterfeit Xanax pills, cocaine and meth.
An overdose can happen anytime, anywhere

and to anyone. One of the best tools to prevent overdose deaths is taking simple steps to be prepared. Every second counts in an overdose situation. Having Narcan at the ready can mean saving a life.
Narcan is a well-known brand of the nasal spray form of naloxone, the opioid overdose reversal drug. Because of growing national efforts to mitigate deaths resulting from opioid overdose, Narcan is more accessible than ever.
In Clark County, the Department of Health started an initiative to get Narcan to as many people as possible. As part of this initiative, department staff can come into local workplaces and give a course on steps to respond to an overdose, which will include instructions of administering Narcan.
This medication is an easy-to-use nasal spray and can be safely administered to anyone you may suspect is overdosing. Someone not overdosing on opioids will feel no effects, so it is safe to use even if you’re not 100% sure the person is experiencing an opioid overdose.
There’s a misconception that having Narcan available encourages drug use, however, this isn’t true. Like a fire extinguisher doesn’t encourage arson, Narcan doesn’t cause drug use. Having Narcan on hand is a necessary safety precaution.
Having Narcan in a workplace’s first aid kit helps employees to be prepared to help someone in their most critical moment.
The opioid crisis continues to affect Clark County and every corner of the nation, with fentanyl’s alarming rise adding a new layer of urgency. While the path to lasting solutions requires addressing the root causes of addiction and getting people the help they need, there are lifesaving measures we can take right now. Equipping Southern Nevada’s workplaces and communities with Narcan is a crucial step in this fight. Using Narcan offers a critical window of opportunity when mere seconds can mean life or death.

 Allison Tierney , above, is External Communications Program Manager at ArchWell Health
Judith Ford , MD, top, is Chief Clinical Officer at ArchWell Health
BY ALLISON TIERNEY
Allison Tierney , above, is External Communications Program Manager at ArchWell Health
Judith Ford , MD, top, is Chief Clinical Officer at ArchWell Health
BY ALLISON TIERNEY
Nevada’s population of indvidiuals 55 and older grew by 32% between 2011 and 2019, according to Elders Count Nevada 2023. In 2021, 14% of Clark County residents were 65 or older. As the population ages, it’s important for older adults and their caretakers to understand the health concerns that come with aging and the resources available to them.
Why is primary care for older adults so important?
Aging can introduce many new health concerns. From insomnia to high blood pressure and incontinence to breast cancer, older adults find their overall health and lifestyle constantly changing.
Research shows nearly 80% of adults over 65 in the United States are living with two or more chronic conditions. These conditions are best managed when a care team of doctors, nurses and medical assistants sees their senior patients regularly, orders tests, conducts screenings and builds a relationship of trust.
Primary care is also the best way to take care of problems early so older adults can try to avoid the ER and major surgeries. Major surgeries and health scares can really hurt older adults’ ability to stay independent and active.
What questions should everyone ask at their primary care visits?
I love it when patients come to their appointments with a list of questions. Some of the best questions for older adults are: Am I taking my medications properly? What should my exercise routine look like? What screenings am I due for? Should I be concerned about memory loss?
Patients should also bring medication and supplements to their appointment to review with their provider. This ensures prescriptions are working well together and allows the doctor to provide timely refills.
What role should specialists play as you age?
Specialists, such as cardiologists, neurologists and oncologists, play a vital role for seniors with serious health problems. This is especially true when an older adult has been diagnosed with one or multiple conditions like diabetes, cancer or heart disease. A specialist should be seen as a part of a larger health care team, and a primary care provider is a senior’s partner in choosing when and which specialist to involve in their care.
One of the most significant issues that arises from visiting specialists is what we call fragmented care. That is why it is crucial that patients have a primary care doctor who monitors results from various specialists and makes sure follow-up is occurring and care is being delivered.
How do you know when it’s time for a caregiver, child or friend to come to a doctor’s appointment?
At any time, patients should invite anyone they wish to their appointments, assuming the doctor’s room can hold them. Patients should feel confident and empowered when they leave their health care provider’s office.
If older adults are forgetting what the doctor said, are unable to ask important follow-up questions, or are feeling extra nervous about an appointment, it may be time to have someone else in the room.
This looks different for everyone, and older

patients should make sure they choose a family member or friend who helps them feel safe and heard. Almost all providers welcome this individual’s presence during an appointment.
How is the value-based care model helping seniors?
We are seeing really positive and productive outcomes for seniors receiving value-based primary care. In addition to having higher patient satisfaction ratings than traditional fee-for-service medicine, experts are finding that seniors experience fewer hip and knee replacements, back surgeries and emergency room visits when receiving primary care through a health maintenance organization.
At ArchWell Health, our patients love our high-touch model with frequent appointments, social workers and same-day access.
How do you find a primary care doctor that specializes in care for older adults?
Generally, patients should be on the lookout for terms such a geriatricians and geriatric doctors. They can also find senior-focused primary care centers in their city.
Primary care centers like ArchWell Health, which only sees individuals on Medicare plans, not only have a team of doctors focused on aging adults but can provide a better patient experience for those who are 60 and older. Amenities such as calm waiting rooms without kids running around, easy parking, and inhouse screenings and tests can make a big difference in the health care experience later in life.
What are some additional services doctors’ offices can provide that seniors may not know about?
We know health care is not just about doctors’ appointments. That’s why so many providers and practices offer additional services that can help older adults stay healthy and active. At ArchWell Health, we have on-site social workers to make sure our members have access to safe housing, reliable food, behavioral health services and much more. Many health care offices are offering to coordinate transportation for patients who may not have reliable access to a car. Others host social activities and workout classes. Our chair yoga and Zumba classes are a hit. The point is, if you aren’t talking to your doctor’s office about other events and offerings that can contribute to your overall health, you should be.
Pacific Dental Services moved its headquarters from Irvine, California to Nevada and changed its name to PDS Health as part of its evolution as a dental and medical support organization. PDS is one of the largest and most successful dental support organizations in the U.S., achieving more than $2 billion in revenue in 2023 .
The U.S. Department of State ’s Bureau of Educational and Cultural A airs recognized Roseman University of Health Sciences for being a top producer of Fulbright U.S. Scholars among special focus institutions. Roseman was one of only 11 special focus institutions recognized.
Rose Dominican Hospitals named Katherine Vergos, RN, MHA, FACHE, as the new Dignity Health Las Vegas market president and president and CEO of the Siena Hospital campus. Vergos is also a fellow of the American College of Healthcare Executives and has received recognition and numerous awards for her contributions to health care. Vergos will be responsible for all Southern Nevada operations and joint ventures, including four Dignity Health neighborhood hospitals, 15 physical therapy clinics, six community wellness centers and other services.
The Pavilion, a behavioral health unit at Southern Hills Hospital and Medical Center celebrated five years of providing psychiatric care to the community. During that time, the Pavilion grew from a 14-bed unit to an 80-bed facility catering to individuals 12 and older.
Southern Hills Hospital opened its level III neonatal intensive care unit. With 15 beds, including six private rooms, spanning over 7,062 square feet, the unit provides space and privacy for families during their stay. The new NICU incorporates Angel Eye cameras, allowing families to securely access live video feeds of their infants from any location.
Sunrise Health Graduate Medical Education Consortium announced its 2024 class of medical residents during the annual national Match Day. Seventy-eight residents and fellows matched at MountainView Hospital, and 34 new residents and fellows matched at Southern Hills Hospital and Medical Center Touro University Nevada College of Osteopathic Medicine achieved a 99.4%
residency match/placement for 157 medical school graduates. More than one-third of the Class of 2024—54 graduates—will remain in Nevada for their residencies, helping to address Nevada’s physician shortage.
The College of Nursing at Roseman University of Health Sciences announced its new doctor of nursing practice in nurse anesthesia program to address the national demand for certified registered nurse anesthetists. The program was approved by the Council on Accreditation of Nurse Anesthesia Educational Programs and will be based at its Henderson campus. The 36-month hybrid format includes a didactic curriculum online, and clinical experiential learning on campus and at partner clinical sites throughout Southern Nevada. Upon successful completion of the program, students will earn a doctor of nursing practice degree, be fully skilled in administrating anesthesia and be prepared to apply for CRNA licensing.
Optum Primary Care has added a new health care provider to help meet the growing need for health services in the Las Vegas community. Yeo Young “Amy” Yoon, APRN, joins Optum Primary Care at 8526 Del Webb Blvd. and specializes in neighborhood care.
Southern Hills Hospital and Medical Center received certification from DNV as a Comprehensive Stroke Center, reflecting the highest level of competence for treating severe stroke events. The DNV Comprehensive Stroke Center Certification is based on standards set forth by the Brain Attack Coalition and the American Stroke Association and measures the full spectrum of stroke care—diagnosis, treatment, rehabilitation and education—and establishes clear metrics to evaluate outcomes.
Galen College of Nursing, an a liate of HCA Healthcare, announced plans to open a new campus in Las Vegas.

MountainView Hospital Paramedic Institute , Sunrise Health Graduate Medical Education Consortium and MountainView Hospital organized and led a simulation of a mass causality incident at a church.
The goal was to train paramedic students and emergency medicine GME residents, while testing the capabilities of all agencies and the hospital in a large-scale event. Agencies involved included: Amplus Academy Charter School EMT program, AMR , Clark County Fire Department , Clark County School District Police Department , Community Ambulance , Guardian Elite Medical Services , Henderson Fire , Las Vegas Fire and Rescue , Medic West , MountainView Hospital, MountainView Hospital Paramedic Institute, North Las Vegas Fire and Sunrise Health Graduate Medical Education Consortium
Located in Southern Hills Hospital, the campus will o er a two-year associate degree in nursing program and a three-year bachelor of science in nursing program. Spanning 38,909 sq. ft., the campus will include a simulation center to prepare students for real-world health care scenarios.
Nathan Adelson Hospice announced that Celena DiLullo has joined its board of trustees. President of PalmMortuaries and Cemeteries, with more than 25 years of experience in the funeral industry, DiLullo’s knowledge and profes-
sionalism in end-of-life grief makes her an asset to the board.
The Henderson Fire Department was a recipient of the American Heart Association’s Mission: Lifeline EMS Gold achievement award. The department earned this award for providing residents with the most severe heart attacks and strokes with prompt, evidence-based care, saving lives and enhancing patient outcomes. The department also received recognition for the Heart Attack Honor
Continued on page 50


MountainView Hospital dedicated its new patient tower, the fi nal phase of a multiphase, multiyear project that expanded MountainView’s ER and building and added a new parking garage. The new tower adds 64 beds and 71,714 square feet to MountainView Hospital.
Continued from page 49
Roll and is the only pre-hospital provider in Southern Nevada to receive this recognition.
Roseman University of Health Sciences introduced a dual accelerated doctor of pharmacy and master of sciences in pharmaceutical sciences 3+1 program. It’s the first program of its kind o ered in Nevada. The program is a partnership between Roseman’s Colleges of Pharmacy and Graduate Studies to o er students the opportunity to earn both the PharmD and MSPS degrees in four years by shortening the MSPS program by one year.

Tonn
Cure 4 The Kids Foundation , Southern Nevada’s only pediatric cancer and rare disease treatment center, announced the appointment of Christine Tonn as its new chief executive o cer. This promotion is part of a board of directors-supported management succession plan. Tonn has been a part of Cure 4 The Kids Foundation for more than 15 years,
initially serving as the chief financial o cer and later as president in 2021. Annette Logan-Parker , the founder and former CEO of Cure 4 The Kids Foundation, will assume the role of chief advocacy and innovation o cer. Logan-Parker will advocate for the medical needs and services of pediatric cancer and rare disease patients with lawmakers at the local, state and national levels. She will also focus on developing external strategies to enhance C4K’s ability to serve an increasing number of patients and expand research opportunities, including donor engagement and physician recruitment. Logan-Parker will also remain president of the Cure 4 The Kids Foundation Board of Directors.

Comprehensive Cancer Centers hired Paul Dieter as executive director. He brings 30-plus years of executive experience and will provide support to physicians within the practice, while maintaining administrative oversight. He also manages, develops and directs organizational framework to ensure positive results for Comprehensive Cancer Centers and its patients. Prior to joining Comprehensive, Dieter was vice president of radiation oncology and diagnostic imaging for the US Oncology Network in Houston. He led the radiation oncology and diagnostic imaging team across the network’s 35 independent practices and 150 radiation sites of service.
The City of Henderson received 200 automated external defibrillators from the Nevada Department of Health and Human Services through grant funding by the Helmsley Charitable Trust The AEDs will be placed in Henderson Police Department patrol vehicles. The use of the AED will help increase the cardiac survivability rate in Henderson.



Roseman University is training the next generation of compassionate and highly competent healthcare providers in pharmacy, nursing, dental medicine and graduate studies to thrive in the ever-changing world of healthcare.
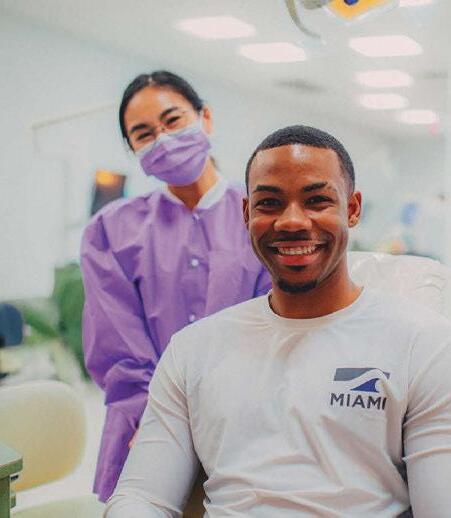



With more than two decades of building from a firm foundation to a broad universe of healthcare education, Roseman continues to develop innovative programs that train a diverse student body to be exceptional leaders in their chosen fields. We look ahead to the limitless promise of the future, in providing our communities unparalleled patient care, scientific discovery, and commitment to improving healthcare outcomes in our region and beyond.

Developed Roseman’s Six-Point Mastery Learning Model®, changing the way healthcare students learn





Developed the first and only College of Pharmacy in Nevada, with an innovative, accelerated three-year program
Developed hybrid-online and on-campus Accelerated BSN programs
Developed an innovative, three-year, team-based DMD program
Developed the first Master of Pharmaceutical Sciences program in the Intermountain West



Learn more at roseman.edu
Transforming Education. Reimagining Healthcare. Embracing Discovery. Committed to Community.
roseman.edu | @rosemanuhs