








Get back to the little things you love with stronger joints. Dignity Health –St. Rose Dominican has a highly specialized physician and patient care staff who work with each patient to establish a personalized treatment and rehabilitation program. Because the only way back to the life you love is your way. Learn more at St.RoseHospitals.org/Ortho.
Publisher of Branded Content and Special Publications
EMMA WOLFF (emma.wolff@gmgvegas.com)
Special Publications Editor SIERRA SMART
Managing Editor/News DAVE MONDT
Staff Writers GRACE DA ROCHA, HILLARY DAVIS, CASEY HARRISON, KATIE ANN MCCARVER, DANNY WEBSTER
Copy Editor ABRAHAM KOBYLANSKI
Photo Coordinator BRIAN RAMOS
Staff Photographers CHRISTOPHER DEVARGAS, STEVE MARCUS, WADE VANDERVORT
Publisher of Digital Media KATIE HORTON
Senior Advertising Manager MIKE MALL, ADAIR NOWACKI, SUE SRAN
The wait is over. We’ve united leaders in the field of cardiology to provide you world-class, patient-centered care, close by.
Account Executives DEREK EIGE, LAUREN JOHNSON, ALEX TEEL, ANNA ZYMANEK
Sales Assistant APRIL MARTINEZ, NANCY RAMOS
Web Content Specialist CLAYT KEEFER
Vice President of Manufacturing MARIA BLONDEAUX
Production Director PAUL HUNTSBERRY
Production Manager BLUE UYEDA
Associate Marketing Art Director BROOKE EVERSON
Publication Coordinator DENISE ARANCIBIA
Production Artist MARISSA MAHERAS
Shadi Daoud, MD, FACC
Alfred Danielian, MD, FACC, FASE
Jeffrey Levisman, MD, FACC, FSCAI
Niuton Koide, MD, FACC
Ronny Jiji, MD, FACC
Anthony P. Dota III, MD
Melissa Plies, APRN
Find out if you’re at risk for heart disease in less than 5 minutes.
Route Administrator KATHY STREALU
Fulfillment Operations Coordinator CASANDRA PIERCE
Distribution Relations Liaison JIDAN SHADOWEN
Marketing Research Manager CHAD HARWOOD

Events Director SAMANTHA PETSCH
Events Manager HANNAH ANTER
Events Coordinator ALEXANDRA SUNGA
GREENSPUN
CEO , Publisher & Editor BRIAN GREENSPUN
Chief Operating Officer ROBERT CAUTHORN
Managing Editor RAY BREWER
VEGAS INC
2275 CORPORATE CIRCLE, SUITE 300 HENDERSON, NEVADA 89074 | 702.990.2550
I’ve been thinking about the importance of support systems. I recently experienced big life changes, and adjusting was physically, emotionally, and mentally tiring. Through this transition period, I was grateful to be surrounded by loved ones and encouraged by friends. The experience made me think about community and how a network of support can encourage success.
The same holds true for our health. In 1938, scientists began the Harvard Study of Adult Development, intending to better understand health and aging. More than 80 years later, the results show that individuals who have strong relationships of trust or support are happier; and happy people live longer.
Health issues are often beyond our control, regardless of how well we care for our bodies, minds and relationships, but when unexpected circumstances occur, many find solace in communities of care.
As I worked on this issue, I was awed by the health care support systems in place for residents of Southern Nevada.
Nigro Construction explains the unique considerations when building medical facilities, including making sure buildings and equipment are tailored to the needs of providers and patients alike.
HopeLink of Southern Nevada, a nonprofit organization that provides support for Nevadans experiencing poverty and homelessness, gives insight into the medical needs and challenges for underserved populations.
These stories demonstrate that the health care industry does not exist in isolation. There are countless fields that overlap health care, all
working together to improve the health and safety of Nevadans.
Medical research is critical to the development of safe and effective medical procedures. Our cover story highlights research happening right now that is focused on preventing and curing cancer.
Touro University and the Kirk Kerkorian School of Medicine at UNLV are dedicated not only to educating tomorrow’s physicians, but to researching the human body and practice of medicine. The organizations and individuals working within these entities are committed to making cancer care better and more accessible.
Cancer will not be eradicated through the effort of any single individual, but by doctors, nurses, and researchers all over the world together making strides to find solutions against this horrific disease.
Desert Radiology has been successful in researching and implementing innovative technologies to target cancer and protect patients. Comprehensive Cancer Centers is developing vaccinations against cancer, and Genesis Care provided actionable steps for cancer prevention.
I hope that as you read these stories, you will feel inspired by the progress being made, not only in the medical field at large, but also in the lives of Southern Nevadans.
Sierra Smart Special Publications Editor sierra.smart@gmgvegas.com
Dr. Nicholas J. Vogelzang, a world-renowned researcher and caring physician, died in September at 72. Through his groundbreaking research and dedicated patient care, he positively affected the lives of many in Southern Nevada and around the world.

As Comprehensive Cancer Centers’ chairman of medical oncology and a pioneer in the field of GU oncology, he led groundbreaking clinical trials aimed at identifying new therapies and treatments for patients with a variety of cancers, including prostate cancer, bladder cancer, kidney cancer, and mesothelioma. He led countless clinical trials for genitourinary malignancies, and in one of his most renowned accomplishments, helped lead several studies to FDA-approval for therapies such as Tecentriq, Provenge, and Xofigo.
In Nevada, he served as clinical professor of medicine at University of Nevada, Reno School of Medicine and UNLV School of Medicine. For his impact on the profession and his community, he was named a “Giant of Cancer Care” by OncLive in 2018.
— Andrew M. Cohen, MD, practice president of Comprehensive Cancer Centers
MountainView Hospital was named one America’s 250 Best Hospitals for 2023, according to new research released by Healthgrades. This puts MountainView Hospital in the top 5% of hospitals nationwide for overall clinical performance across the most common conditions and procedures.
“For MountainView Hospital to be named among America’s 250 Best Hospitals now three years in a row is a major recognition and a demonstration of the focus by all colleagues to deliver safe and quality care to all of our patients,” said Hiral Patel, MountainView Hospital chief executive officer. “This is an astounding achievement and a testament to the focus by all colleagues to accurate, safe care to every patient, every time.”
Virtual Surgical Planning (VSP) is technology that uses patient imaging to create virtual 3D models to plan surgical procedures. It is commonly used in reconstructive surgery of the jawbone, or mandible, where bone from the fibula is used to recreate the jaw.
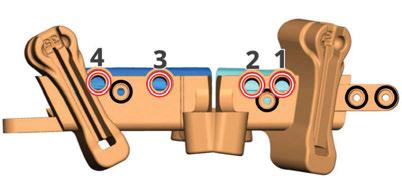
The software helps plan cuts through the mandible bone and fibula, and a custom plate is designed to fixate the fibula bone piece to the native mandible.
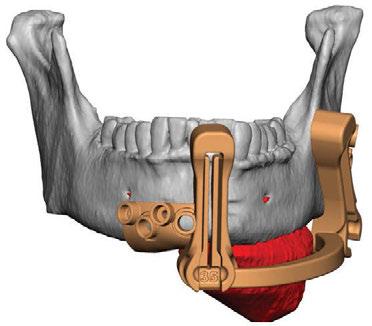
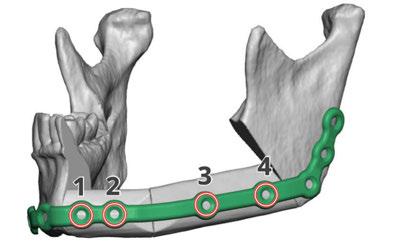
Companies providing this service then print cutting guides and mill custom plates used during surgery, providing a patient-specific product that increases precision, decreases operative time, and potentially avoids some of the pitfalls of improvising surgery.
The result is optimizing restoration of form and function.

The path to becoming a physician is long and arduous. However, all of the challenges are worth it when a physician reflects on the patients helped on the road to recovery.
While patients are the top priority, supporting the next generation of health care professionals should also be considered. Fellow physicians know the challenges young professionals face, and having a good mentor can be the difference between career success and failure.
The No. 1 reason to become a mentor is to support up-and-coming health care professionals reach their goals. The guidance provided will give them the confidence needed to stay on course, regardless of the stage of their journey. Other reasons to become a mentor include:
n Shaping tomorrow’s talent: Ensuring that the next generation of health care professionals exceeds expectations often begins with a mentor who is willing to show them the way. The individual a physician mentors today may be the person treating them in the future.
n Learning about yourself: There is great joy and satisfaction in mentoring a trainee and watching them grow. Along the way, mentors also learn about themselves. They learn their teaching style and pinpoint areas of personal and professional improvement. They may even find ways to change their approach to practicing medicine.
n Improving your skills: Through the mentoring process, mentors will hone interpersonal skills and emotional intelligence. Conversations with mentees will improve the way mentors communicate with patients.
Physicians don’t have to look far to find an opportunity to become a mentor. In Las Vegas, there are multiple medical schools in need of local doctors to assist with clerkships and clinical rotations.
If that’s not the right opportunity, others include:
n Teaching a medical student or a resident how to write a research paper
n Guiding a student with medical school or residency applications
n Assisting prospective medical school students with interview preparation
Doctors should keep an open mind and stay active within the medical community to find these opportunities
Maintain relationships with local medical schools. Share the desire to mentor with colleagues. Attend medical conferences. There are plenty of eager trainees in need of a helping hand.
Physicians choose the path of lifelong learning. By becoming a mentor, they share their knowledge while simultaneously working toward personal and professional development. With this approach, mentors are doing their part in supporting the next generation of physicians. A positive impact on one life today could translate to saving countless lives tomorrow.
ENSURING THAT THE NEXT GENERATION OF HEALTH CARE PROFESSIONALS EXCEEDS EXPECTATIONS OFTEN BEGINS WITH A MENTOR WHO IS WILLING TO SHOW THEM THE WAY.
As private institution costs rise, obtaining a degree to find a well-paying job becomes increasingly difficult. Many entry-level positions offer no room for advancement and no applicable training for different careers down the line.
For this reason, Nevada Eye Physicians implemented a six-week ophthalmic trainee course, free of cost and with potential for growth. It provides information necessary to work independently at any of its facilities as an ophthalmic technician, including all of the procedures needed to work on the technician floor. Trainees receive a certification of achievement and a position within the company.
Six months after completing the course, employees are eligible to take the Certified Ophthalmic Medical Assisting exam, which provides the necessary qualification to work as an ophthalmic medical assistant at any practice nationwide.
There are few opportunities to be trained on the job with no prior experience, particularly on the West Coast. The only requirements to apply at Nevada Eye Physicians are a high school-level education and customer service experience, such as hospitality or food and beverage. Previous work experience in
the medical field is not required.
The professional environment is fast-paced and people-oriented. The ability to observe major surgical procedures and learn about patient care, vision checks, glasses prescriptions, diagnostic imaging, professional testing, and equipment operation without a college education, and at no personal cost, is an opportunity that is difficult to find elsewhere.
This has proven to be a life-changing opportunity for some. “I feel like I came into this job and I’m motivated, I’m proud of what I’m doing,” said Alex Cendejas, a student of the program. “It’s a good opportunity; I feel like the medical field will always need people. This is for my family. I want to do something that I can make them proud of.”

This career is also flexible and accommodating to all lifestyles. For example, it’s possible to simultaneously attend school and maintain an ophthalmic technician position.
Nevada Eye Physicians prioritizes five key values: teamwork, growth, integrity, professionalism, and accountability. This can be seen in any employee, from entry-level positions to management, and it is instilled in the technician training program just as much as technical skills.
The workplace is a welcoming and productive environment, which is why it’s able to recruit and develop some of the strongest employees and trainees in the eye health industry.
The only requirements to apply at Nevada Eye Physicians are a high school-level education and customer service experience, such as hospitality or food and beverage. Previous work experience in the medical field is not required.

UMC Orthopedic & Spine Institute combines top surgeons and collaboration to transform care in Southern Nevada
Recognizing a need for improved access to highly specialized orthopedic surgery in Southern Nevada, UMC recruited a team of industry-leading surgeons to establish the UMC Orthopedic & Spine Institute. Located in the heart of the Las Vegas Medical District, the practice offers a comprehensive selection of subspecialties, including orthopedic trauma, joint replacements, adult and pediatric spine, orthopedic oncology, sports medicine and pediatric orthopedics.
“We have assembled this world-class team of 14 orthopedic surgeons to provide our community with convenient access to life-changing surgeries and follow-up care,” said UMC Chief Operating Officer Tony Marinello. “With a strong focus on research, innovation, and training future generations of orthopedic surgeons, the UMC Orthopedic & Spine Institute will play a valuable role in the future of our local health care industry.”
Continued on page 14

Continued from page 12
With leadership from two of the community’s most well-known surgeons, Drs. Michael Daubs and Erik Kubiak, the UMC Orthopedic & Spine Institute expects to serve 30,000 to 40,000 patients each year. A robust team of specialized surgeons takes on many of the most complex cases that previously would have required referrals to out-of-state surgeons.
“Our goal is to become one of the top orthopedic surgery programs in the country,” said Dr. Daubs, a UMC spine surgeon who also serves as the chairman of the Department of Orthopedics at the Kirk Kerkorian School of Medicine at UNLV.

Dr. Kubiak, UMC’s Chief of Orthopedic Surgery, provides all phases of fracture care and joint reconstruction for many of the community’s most critically injured trauma patients. Dr. Kubiak said patients of the institute benefit from the group’s unparalleled level of collaboration and commitment to continued progress.
“We come together as a team and
critically evaluate every single case to determine the best method of treatment,” Dr. Kubiak said. “With a team of industry thought leaders participating in this peer review process, we are constantly evaluating and refining our processes to support the best possible outcomes for our patients.”
The group performs surgeries at UMC and offers outpatient visits within a new clinic directly across the street from the hospital campus at 2231 W. Charleston Blvd. As part of UMC’s health care system, the practice has access to the state’s most advanced surgical technology, including a groundbreaking artificial intelligence system that provides enhanced precision during hip replacement surgeries. UMC also offers a specialized robotic surgery platform for knee replacements.
Supporting an expansive medical residency program and a nationally recognized orthopedic trauma fellowship through the Kirk Kerkorian School of Medicine at UNLV, the UMC Orthopedic & Spine Institute remains committed to training orthopedic surgeons and encouraging them to stay in Southern Nevada.
“We’ve recruited the best and brightest in each of our fields to help build the next generation of orthopedic surgeons to serve our community,” Dr. Daubs said.
Dr. Brandon Romero serves as a prime example of this approach. After graduating in the first class of orthopedic surgery residents training at UMC through UNLV in 2021 and completing a prestigious fellowship at the University of Pennsylvania, he returned to UMC and now specializes in shoulder and elbow surgeries and is a member of the institute
“We’re having a positive impact on the quality of orthopedic care in the valley,” Dr. Romero said. “This program will put Las Vegas on the map for orthopedics.”

Following its introduction in late 2022, the institute began to have an immediate and lasting effect on the lives of Southern Nevadans.
In November, Ronan Towns was rushed to the UMC Trauma Center after sustaining injuries in a sledding accident on Mt. Charleston. He fractured his tibia in two places and his ankle.
To treat Ronan’s injuries, Dr. Abby Howenstein performed surgery to place a rod inside his tibia and inserted a screw in his ankle. Within three weeks, the 15-yearold was back on his feet.

“I felt like he had the best care in the city” said Ashley Towns, Ronan’s mother.
The UMC Orthopedic & Spine Institute is
also home to Nevada’s only full-time orthopedic oncologist, Dr. John deVries. Orthopedic oncology is a rare subspecialty focused on treating tumors, cysts and growths affecting bones and connective tissue.
“There are probably fewer than 300 of us [orthopedic oncologists] in the country,” said Dr. deVries. “Our practice offers a wide range of subspecialists, and we work together in and outside of the operating room to address many of Nevada’s most difficult orthopedic cases. This culture of collaboration elevates the quality of care available in Southern Nevada.”
Learn more about the UMC Orthopedic& Spine Institute by visiting www.umcsn.com/ bone or calling 702-383 -BONE (2663).

ancer is the second leading cause of death in Nevada, with the American Cancer Society estimating there will be more than 17,000 new cases and 5,850 deaths this year. These numbers are only increasing.

The Nevada Cancer Plan, created by the Nevada Cancer Coalition, is released every ve years to evaluate important cancer trends and to outline overarching goals in improving the quality of cancer care within the state. This report is created in collaboration with multiple local, state and federal agencies to address the speci c needs of Nevadans.

The four main components of the plan are prevention, early detection, equitable access, and quality of life. Within those silos, there are several encouraging indicators. For instance, the number of HPV vaccination completions for boys and girls is up; the number of late-stage breast, colorectal, and lung cancer diagnoses are down; the number of school districts with UV policies is up.
There are also some key indicators that have worsened or shown no improvement during recent years, including the percentage of adults who are overweight and the
percentage of young people who use tobacco. When looking at cancer, the de nition of progress is subjective, and success is not always linear. Where some prevention indicators may su er, research promises may soar. Where some survivorship trends may dip, policy obstacles may clear. In the continuum of cancer care, any encouraging shift can mean individual lives saved and quality of life for patients and families improved. In Southern Nevada, the improvements being made across all verticals — prevention, early detection, equitable access, and quality of life — are meaningful. Comprehensive Cancer Centers is making signi cant strides in clinical research trials and implementing lesser-known, and lesser-available therapies to patients in need. Touro University is ushering in a new era of groundbreaking research on metastasis prevention. Desert Radiology is using cutting-edge technology to treat lung cancer — an especially prevalent cancer in Nevada. Genesis Care is promoting prevention e orts within the community. This is only a glimpse of the many ways Southern Nevada is shaping and reshaping the landscape of cancer care within the state.
Comprehensive Cancer Centers of Nevada prides itself on o ering the latest cancer care to thousands of patients each year. The practice participates in more than 100 clinical research studies annually and has played a role in developing more than 100 Food and Drug Administration-approved cancer therapies including Opdivo, Keytruda, Tecentriq, Provenge, Xofigo, Hercepin and others.
In 2022 alone, six drugs that Comprehensive participated in trials for were approved by the FDA for cancer treatment. Additionally, Comprehensive contributed to several trials of drugs approved for other health conditions.
Comprehensive’s physicians continue to collaborate with global partners and push the boundaries of clinical cancer research.
Continued on page 18
Oscar B. Goodman, Jr., M.D., Ph.D., is a medical oncologist and clinical researcher at Comprehensive Cancer Centers

Monitoring and mitigating risk factors is important when it comes to being proactive against cancer. Two of the largest cancer risk factors in Nevada are smoking and obesity, among other risk factors that can span hereditary to environmental factors.
According to the CDC, 15.7% of adults in Nevada use cigarettes, compared with the national average of 12.5%. While other states may have a higher percentage of cigarette users, Nevada also faces the issue of workers and patrons in casinos or bars being exposed to indoor smoking and toxic levels of secondhand smoke. The CDC also reports that Nevada’s prevalence of self-reported obesity is 31.3%.
Smoking and obesity are two of the biggest preventable causes of cancer that individuals should take into consideration for their daily health.
For decades, many thought of a patient’s diagnosis of cancer as a death sentence. That’s no longer the case. Many forms of cancer are now viewed as chronic diseases with treatments becoming much more personalized, leading to fewer patients facing a terminal diagnosis.
Doctors can take a personalized research approach, based on the genetic makeup of the patient’s tumor. For example, if a patient’s tumor possesses a requisite genetic marker for a specific trial, it may lead a physician to create a personalized treatment plan on their behalf.
Recently it was announced that U.S. Oncology Research and Sarah Cannon Research Institute will partner to create increasing availability and access to clinical trials for community oncology providers, like Comprehensive. We expect this will facilitate participating practices to better match patients with lifesaving treatments.
According to the U.S. Census Bureau, Nevada is one of the fastest-growing states. Another report from the Tax Foundation looked at states people were moving to since the COVID-19 pandemic, and Nevada ranked eighth, with a population increase of 1.3%.
While continued growth is beneficial for the state, Nevadans need to be aware of how the population increase can a ect resources, including the health care industry.
According to U.S. News, Nevada ranks 50th in the country in Health Care Access. A lack of access to health care can overburden primary care providers and make it di cult for patients to be seen. This results in a lack of regular screenings, which can lead to undiagnosed cancers.
Since 2020, Comprehensive physicians have cared for patients presenting with advanced forms of cancers that could have been diagnosed at an earlier stage. It’s crucial for people to talk to their doctors about screenings and for everyone to stay proactive with regular check-ups to avoid this occurrence.





During vaccine trials, a patient’s blood is used to create a vaccine just for them that’s based on their genetic markers. The notion of cancer vaccines started with prostate cancer, but we’re now seeing an influx of vaccines for all major types of cancer across the board. Comprehensive has multiple trials open for cancer vaccines and is optimistic about the possibilities.
Provenge was the first therapeutic cancer vaccine to receive approval from the FDA, and it has become a mainstream treatment.
Comprehensive saw the potential in this type of cancer treatment from the beginning and worked on the trial for Provenge more than a decade ago.
Another related aspect of this research deals with ‘cold’ tumors that don’t respond to immunotherapy. Cancer cells start as normal cells and the immune system often does not recognize them as foreign. Because of this, Comprehensive investigators have researched how the immune system can distinguish cancer as a foreign entity. Major progress has been made in the past decade trying to apply this concept to other cancer types previously thought to be immune-resistant cancers. For select trials at Comprehensive, we’ve added a second drug onto immunotherapies with this goal in mind.
treatment for O’Hanlan’s type of cancer, but she agreed to try the procedure. To date, O’Hanlan has had three CyberKnife procedures that have eliminated her existing tumors, and she’s had no new tumors since.
This is where O’Hanlan’s story began. She is now a member of the GCT Survivor Sisters group on Facebook, where she is passionate about sharing her CyberKnife journey with patients needing a miracle themselves.
O’Hanlan’s advocacy within the group and beyond has led to lifelong friendships and helped patients nationwide. These patients include Lavonne Schroeder in Brayton, Iowa; Tammy Bowen in Conway, Arkansas; and Michelle Houston in Quincy, Illinois. These GCT patients were told there were no further treatment options, but they were inspired by O’Hanlan’s story, and asked doctors to perform a targeted therapy like CyberKnife. Today, they are alive and well.
In reflection of O’Hanlan’s journey, Parikh and Curtis discussed what could be learned from her experience.
protocol, and it has paid off for Helen and many other patients with her condition.
What advice would you give to patients that may be encountering a journey like Helen’s?
Curtis: We learned from Helen that this can work for those with her genetic makeup. Every patient is different. If you’ve had more than a couple of surgeries related to a specific type of cancer and the tumors seem to be coming back, you should discuss the possibilities with your oncologist and/or radiation oncologist.
Parikh: I consider Helen a lifelong friend now. It’s bonds like these that drive us each day, and these patients become our family and inspire us. Perhaps less advice for patients, but more for the medical realm as a whole in Nevada, is that we need to think outside the box and continue to advocate for measures and laws that allow us to do so. We all have a voice and can generate many more success stories just like Helen’s.
Regular screenings can identify the most common types of cancer. When caught early, many cancers can be treated through surgery or radiation therapy.
Lung cancer may be prevented by abstaining from smoking, and maintaining a balanced and healthy lifestyle. For current or previous smokers, a lowdose chest CT scan can help detect tumors early.
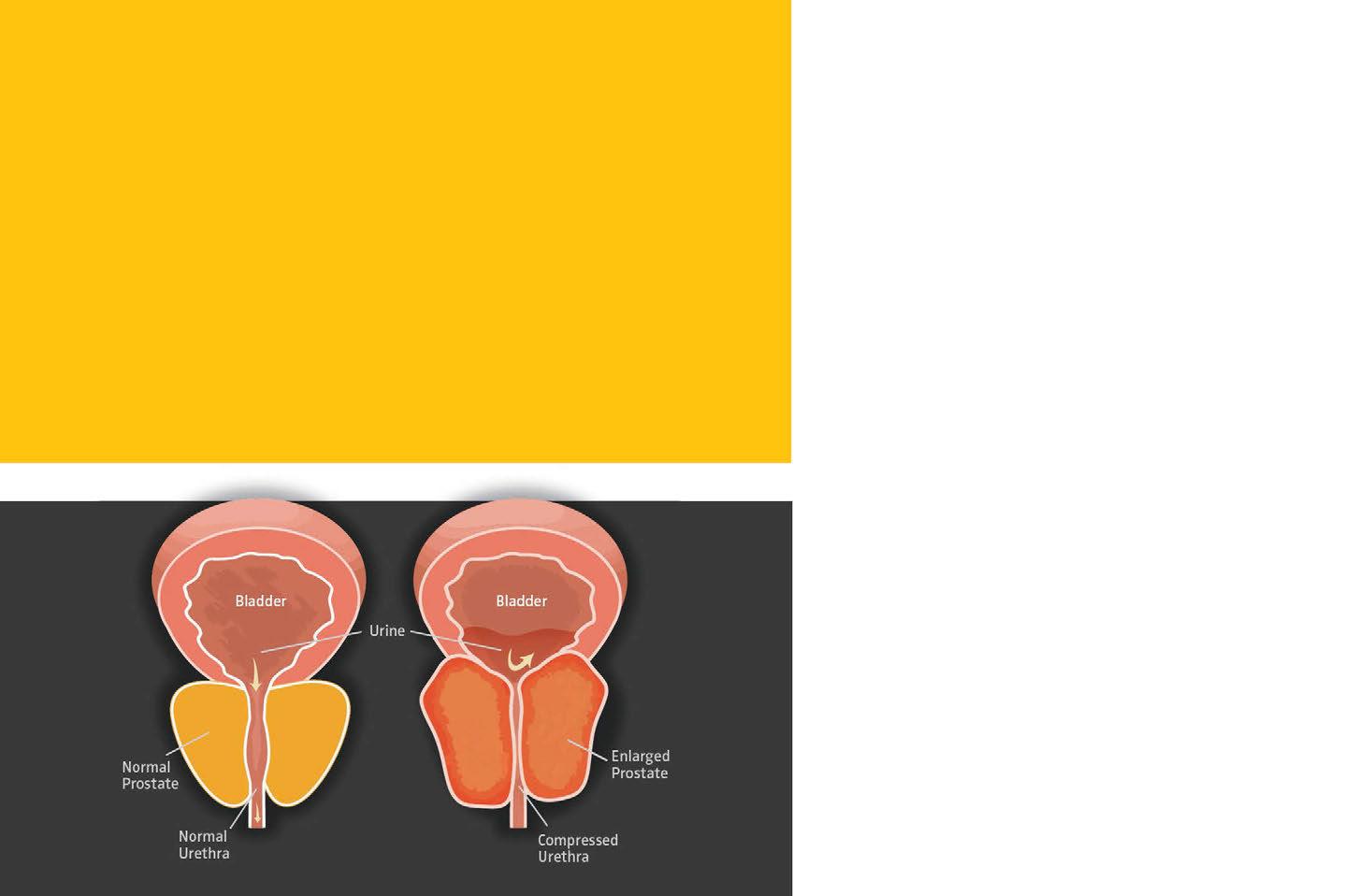
It is imperative that patients start screening for colorectal and prostate cancers at the recommended ages, 45 and 55 respectively. Patients should consider screening earlier if there is a known genetic predisposition or previous family history of one of those cancers.
In the case of skin and breast cancer in particular, it is important to keep a close watch on your body. Take note of changes to the shape or feel of your breasts, or new and concerning spots on the skin. These concerns can be valid reasons to schedule an appointment with your primary physician to get a clinical opinion.
The American Cancer Society estimates there will be more than 17,000 new cancer cases in 2023 in Nevada alone. How can you avoid becoming one of these cases? Prevention begins with following a healthy lifestyle, including a nutritious diet rich in fruits and vegetables, regular exercise, avoiding smoking, and limiting alcohol intake. Some people are more at risk than others, so it is important to get regular screenings to detect cancer as early as possible to treat it successfully.
The Centers for Disease Control and Prevention’s Division of Cancer Prevention and Control promotes early screenings for many types of cancers, noting that many are not life threatening if caught early, especially for the most common types.

During the height of the pandemic, many Americans delayed regular screenings that can detect cancer in the early stages. Now that people are getting back to their routines, it is essential that individuals maintain a healthy lifestyle, stay mindful of their personal health, and keep up with regular screenings. These actions give the best chance of preventing or, if detected early, beating cancer.
The most common cancers in Nevada are often the most treatable if caught early.

In 2021, Touro University Nevada, the state’s largest school of medicine and its only school of osteopathic medicine, received a grant from the National Institutes of Health to pursue ongoing research on a more effective cancer treatment associated with a new potential anti-cancer drug. The scientific work involves collaborators throughout the world, including Germany, Italy and Japan, along with faculty and medical students from the national Touro University System.
Given that more than 90 percent of cancer deaths are attributed to some form of metastasis — the spread of cancer from the original site (a primary tumor) to other parts of the body — our research is
focused on how to prevent or impair the formation of metastases. This is an especially important area of study given that there are many proven ways to stop or delay cancer growth, but little is known about the mechanism of metastasis formation. We do know that there is mutual communication between cancer cells and normal cells, and the key to changing long-term behavior in a cell is gaining entry into the nucleus, or “control center,” of a cell.
We suspected that the communication that allows metastasis to happen is associated with exosomes, which are extremely small bags of proteins and nucleic acids that are produced by cells in the body, including cancer cells. Exosomes, otherwise known as small extracellular vesicles, are so tiny, we have billions of them in just a single drop of blood. They are so minute, even advanced microscopes can’t see them. To allow us to study them, Touro spent nearly half a million dollars on three machines — a hi-resolution fluorescent microscope, a flow cytometer, and a laser particle analyzer.
With these tools, we’ve discovered highways that travel deep into the nucleus of a cell. We found that these highways are large enough for exosomes to flow
evidence that the drugs we’ve created work to miti gate metastases originating from breast cancer, colon cancer, and melanoma. No one has ever targeted the discovered molecules with a drug, so this is an exciting new insight into how cancer might be treated. Our next step is to continue testing to ensure these drugs are nontoxic before moving them into a clinic setting.
The process of identifying a new pathway associated with metastatic cancer and designing potential drugs to block it hasn’t been easy, and there is still much to do. We are acutely aware of the long road ahead before patients can benefit from these drugs. Research is always a serendipitous search for the unknown, with a high probability of dead ends. With this work, we have reached a point where we are receiving more recognition from the medical research community and funders of research. While the time frame is uncertain, given the large
Lung cancer is one of the most common cancers, and it’s the leading cause of mortality among cancer patients.
Although lung cancer most commonly occurs in patients with a history of smoking and those who have experienced prolonged exposure to secondhand smoke, it can also occur in people who have never smoked. For example, patients with a family history of lung cancer are at an increased risk of developing the disease.

While traditional cancer treatments like chemotherapy and surgical tumor removal are options to help eradicate cancer cells from the lungs, innovations in the industry and advanced CT scans have allowed doctors to use heat energies such as radiofrequency or microwave, and cold energy such as cryoablation.
Thermal ablation is a minimally invasive procedure that destroys tumors and cancer cells by applying intense heat or cold to the tumor. During the procedure, radiologists use a CT scan of the lungs to guide them as they place thin needles around the tumor. The needles then produce extreme heat or cold to destroy the cancerous cells with minimal risk to the patient.
Sameer Rehman, M.D., a diagnostic radiologist at Desert Radiology, is passionate about the percutaneous thermal ablation procedure and is one of a small number of doctors who perform the procedure in Southern Nevada.
It is recommended for people with a history of smoking (20 packs a year), a family history of lung cancer, and those age 50 and up to have a treatment plan in place should lung cancer begin presenting. As with most diseases, lung cancer treatment is most effective in the early stages, and an early diagnosis and treatment plan lead to the highest chance of survival and lower the risk of long-term complications.
Minimal side effects and complications
Better preservation of lung function compared to traditional surgical tumor removal

Patients can resume chemotherapy almost immediately after the procedure
The procedure can be used on patients who are not candidates for surgery or have multiple tumors
Often a one-time treatment procedure that may require CT scans every three months and a PET scan every six months to ensure no complications occur or diseases remain after the procedure
There are a few factors that come into play when Rehman is deciding on which type of thermal energy procedure to use.
“I prefer using cryoablation based on its safety profile and if I’m treating a lung cancer closer to the chest wall where nerve endings are,” said Rehman. “In addition to tumor ablation, cold energy also provides local anesthetic effect secondary to the freezing nature. Hot energy, which is microwave ablation or radiofrequency ablation, has shown the same effectiveness in treatment as cold energy, but I use microwave technology when treating a larger size tumor such as 3-centimeters in size.”
Following the procedure, patients may have an imaging scan performed to review the outcome of the ablation. Most patients are discharged the same day with a prescription for antibiotics and/or pain medications.
Although thermal ablation is a great option for treating cancerous tumors within the lungs, there are a few prerequisites patients will have to meet before being considered for the procedure.
Thermal lung ablation is best suited for patients who are in stage 1 of lung cancer, where tumors three centimeters in size or less are present, and before the cancer has spread to lymph nodes throughout the body. Additionally, patients will need to get cardiac clearance to ensure the heart is in good shape for the procedure. Patients with pacemakers are okay to undergo a thermal ablation procedure if they also meet the other prerequisites.
Centennial Hills Hospital is the only hospital in Las Vegas that offers the thermal ablation procedure but there have been promising results from bigger medical centers in California and New York, meaning more medical centers are likely to begin performing the procedure.
“Thermal ablation is definitely growing as we speak,” said Rehman. “With more research coming out, the field is bound to grow to provide competitive care for cancer patients that is safe, less invasive, and has equally effective and sometimes even better outcomes than traditional methods of cancer treatment. I foresee the procedure becoming more common for cancer treatment based on the growing body of evidence-based research and literature. Improving outcomes of the procedure is also attributed to advancement in technology and needle designs.”
Mucosal cancers of the oropharynx — those affecting the tonsils, back of the tongue, and the throat — were classically considered diseases of smokers and alcoholics.
Historically, oropharyngeal cancers were preferentially treated with radiation and chemotherapy because of the morbidity of surgery in this part of the body. Radiotherapy of oropharyngeal cancer was either wildly successful, or the cancer recurred.
Two decades ago, it was discovered that oropharyngeal cancers responsive to treatment were more likely to carry a unique signature: They were a byproduct of human papillomavirus infection. Burkitt lymphoma and Merkel cell carcinoma are examples of virus-driven cancers. The same strains of human papillomavirus linked to oropharyngeal cancer can cause cervical, anal and penile cancers.
Smoking has been on the decline since the 1980s, as have cancers associated with smoking and alcoholism. However, an epidemic of HPV-related head and neck cancers has been on the rise. In the 1980s, HPV-related oropharyngeal cancer accounted for 20% of all oropharyngeal cancer. By the 2010s, HPV-related cancer was responsible for more than 70% of oropharyngeal cancer.
Human papillomavirus is the most common sexually transmitted infection. Rates as high as 80-90% of the world population are said to have been infected at some point in life. However, the overall risk of oropharyngeal cancer in the general population is less than 1%. The odds of developing cancer from an HPV infection are quite low, and the factors that guide HPV from a common sexually transmitted infection to a life-threatening cancer are poorly understood at this time.
We know that 14 strains of HPV are high-risk
for cancer. HPV-16 and HPV-18 account for most HPV-related cancers. In fact, HPV-16 accounts for 90% of all HPV-related oropharyngeal cancers. HPV-16 and -18 strains are protected against in HPV vaccine products. Time will tell if these vaccines lead to a drop in HPV-related oropharyngeal cancer.
Acute HPV infections do not cause cancer in the immediate future. Research has shown that the development of cancer from an HPV infection can take decades.
HPV-related oropharyngeal cancers tend to affect men more than women, usually in their forties or fifties. It often presents as a painless, growing mass in the neck. Such masses are usually a lymph node, or a conglomerate of lymph nodes, that the cancer has metastasized to. The originating, or primary, site is usually in the tonsil or tongue base. Patients will often observe an unabating neck mass for months, but disbelief and denial can lead to delays in diagnosis and treatment.
Treatment paradigms for HPV-related oropharyngeal cancer include radiation and/or surgery. Chemotherapy alone is not curative but can be administered along with radiation in advanced cases. Because traditional open approaches to the oropharynx are so morbid, radiation with or without chemotherapy has long been the standard-of-care for treating oropharyngeal cancers, regardless of HPV status. The recommended dose of radiation has been called into question because of the robust response of HPV-related tumors to radiation.
Alternatively for low-stage tumors, advancements in robotic surgery have made minimally invasive oropharyngeal approaches possible with success rates comparable to radiation. In some cases, cure with surgery alone may be feasible. Paradigms combining robotic surgery followed by lower dose radiation postoperatively are currently being investigated but are promising so far.


Dr. Alice P. Chen received her bachelor’s degree in Psychology from UCLA with an emphasis on developmental psychology. She graduated cum laude from Boston University and pursued her specialty degree in pediatric dentistry at Temple University Hospital.
Dr. Chen is board certified by the American Board of Pediatric Dentistry and combines warmth and care with excellent clinical expertise in her interactions with patients. Her sunny personality puts children of all ages at ease. While treating every child with kindness and patience, she does an exceptional job in catering specifically to individual personalities.
Dr. Chen is highly trained in treating children with special needs and brings her extensive practice experience to Roseman Dental & Orthodontics in Henderson, and Roseman Dental in Summerlin.

Roseman’s Clinics provide a wide range of pediatric, dental and orthodontic services to all patients at a reduced cost, cutting-edge technology, and exceptional, compassionate patient care.
4 Sunset Way, Bldg. B Henderson, NV 89014 702-968-5222
Dr. Glen Roberson graduated from the University of Medicine and Dentistry of New Jersey, New Jersey Dental School as valedictorian in 2004.
Following graduation from dental school, he completed a general practice residency program at Overlook Hospital in Summit, N.J., followed by a full-time associateship in Hillsborough, N.J.

Dr. Roberson enrolled in the orthodontics and dentofacial orthopedics residency program at the UNLV School of Dental Medicine. In 2010, Dr. Roberson joined Roseman as a full-time faculty member in the Advanced Education in Orthodontics and Dentofacial Orthopedics Residency Program.
Dr. Roberson is an active member of the American Association of Orthodontists, Pacific Coast Society of Orthodontists, and American Dental Education Association.
Dr. Roberson volunteers his time treating babies and children with cleft lip and palate anomalies, helping patients that are just a few days old feed and thrive.
& ORTHODONTICS
4 Sunset Way, Bldg. C Henderson, NV 89014 702-968-5222
Dr. Matthew Thacker is the program director for the Advanced Education in General Dentistry Residency and Clinic in Henderson.

After earning his bachelor’s degree in Biology with a concentration in integrative physiology from UNLV, he attended UNLV’s School of Dental Medicine and received his DMD degree in 2018.
After graduating from dental school, Dr. Thacker served in the U.S. Navy as a Fleet Marine Force dental officer for four years aboard the Marine Corps Air Ground Combat Center in Twentynine Palms, California.
He serves the community as a volunteer dentist for the Special Olympics, Give Kids a Smile®, UNLV’s Sgt Ferrin Memorial Veteran’s Clinic, Adopt-a-Vet, Project Homeless, and Roseman University’s EMPOWERED Program.
Dr. Thacker is a member of ADEA, Nevada Dental Association, Southern Nevada Dental Society, is a Fellow of the Academy of General Dentistry, and oversees the dental side of Roseman Dental & Orthodontics in Henderson, offering pediatric and adult patients dental services at reduced costs.
4 Sunset Way, Bldg. B Henderson, NV 89014
702-968-5222
At GenesisCare, you gain access to a global network in cancer care. That means thousands of the world’s most brilliant cancer minds collaborating with you, giving you local access to the most advanced radiation oncology technology and treatments for the best possible life outcomes. This is a better world of care. This is GenesisCare.

 BY RUSSELL GOLLARD, M.D.
BY RUSSELL GOLLARD, M.D.
n October 2022, a voluntary product recall from a manufacturer of popular hair products, including several dry shampoo brands, may have slipped under the radar for some of us, but it should be cause for conversation about the potential dangers in everyday goods. The affected products contained trace amounts of benzene, a chemical that can be dangerous with potentially cancer-causing properties. Many reports indicate that prolonged exposure to benzene can lead to an increased risk of leukemia.
A chemical common in beauty product aerosols , antiperspirants , and cleaning supplies is the cause of major health concerns
Benzene is a chemical that occurs naturally and in manmade products. In our natural environment, benzene is present in volcanic eruptions and wildfire smoke In our manmade environment crude oil, gasoline, and cigarette smoke all expel benzene. It’s naturally colorless and, at room temperature, takes on a light-yellow hue. It also tends to have a sweet odor, similar to gasoline, and is extremely flammable.
Benzene is an organic solvent, which means it can dissolve or disperse other substances and, as a wide body of research suggests, organic solvents can be carcinogenic and potentially hazardous to our health. Its main industrial uses are as a constituent in motor fuels and as a solvent for various products such waxes, oils, paints, and plastic. Aside from these sources, benzene emission also comes from tobacco smoke that accounts for nearly half of all national exposure.
The risk of benzene exposure is heightened because of its prevalence in the natural world and in our modern environment. Outdoors, the air itself contains some level of benzene, though typically small amounts. Debris from volcanic eruptions and wildfire smoke contain benzene. It’s also found in highly concentrated amounts in less avoidable situations, such as car exhaust and industrial emissions. Fortunately, benzene levels from outdoor sources are typically low enough that, unless you’re repeatedly exposed over a long period of time, they’re likely not detrimental to your health.
When present, indoor air concentrations of benzene are typically higher because of the chemical’s use in so many common products. Cleaning and paint supplies, office equipment such as printers and photocopiers, tobacco smoke, stored fuels, and automobile emissions in attached garages are all sources of indoor benzene. Some of these are unavoidable, but for exposures that can be controlled, start by disposing of unused paint supplies and fuels as instructed, provide maximum ventilation in your home (especially when painting), and eliminate indoor tobacco smoke.
In the case of the October recall, benzene was found to be present in the shampoos’ aerosol propellent. Every time a consumer used one of the products, they were possibly exposing themselves to a carcinogen.
There is no “safe” level of benzene exposure, but it also doesn’t mean your need to throw away all cleaning supplies. What’s important is to recognize the potentially dangerous nature of this chemical, heed warnings and notices such as product recalls, and limit unnecessary exposure. It is impractical to assume all benzene contamination can be eliminated from the environment, but safety precautions limiting exposure can decrease potential health problems.
This exposure caused acute, short-term risks, which necessitated the urgency of the recall. Breathing in the fumes from the aerosol propellent had the potential to lead to drowsiness, confusion, and rapid or irregular heart rate. At high enough concentrations, exposure can lead to loss of consciousness. These same symptoms, along with stomach irritation and vomiting, can also present if someone inadvertently ingested benzene (think: contaminated food sources). At extremely high levels, even short-term exposure has the potential to be fatal.
The inherent dangers of prolonged benzene exposure are wide-ranging and not entirely predictable, which is part of the reason for caution. In the simplest terms, one of its effects is causing cells to work incorrectly. At high levels and/or for prolonged periods of time, this can lead to a host of potentially serious issues.
Benzene exposure has been known to affect the normal functioning of bone marrow, specifically by inhibiting the production of red blood cells, which carry oxygen throughout the body. Decreased production of red blood cells can lead to anemia, a condition wherein the body doesn’t get enough oxygen, and can cause myriad symptoms, from shortness of breath and dizziness to severe headaches and heart problems.
Ongoing studies are also investigating possible links between long-term exposure and complication leading to cancers. In a 2012 study, the International Agency for Research on Cancer found a cause-and-effect link between benzene exposure and leukemia. The same study found more limited evidence of benzene exposure potentially leading to other cancers, including lymphoma.
 BY TRACY WAKEFIELD, M.D. AND ERIC JORDAN
BY TRACY WAKEFIELD, M.D. AND ERIC JORDAN
From the COVID-19 pandemic to the highest inflation rates in decades, Las Vegas residents have weathered difficult years — especially seniors whose physical and mental health has been disproportionately affected.
According to the U.S. Census Bureau’s 2021 survey, the Las Vegas population includes more than 105,000 residents who are 65 and older. The number of seniors has increased almost 45% since 2011, and the population continues to grow. More than 80% of seniors live with one or more chronic conditions, driving a major need for quality, senior-focused care in the community. However, because seniors often visit multiple specialists to manage their conditions, their health care can become fragmented. It is crucial that our health care providers work synergistically to provide comprehensive, personalized care that meets seniors’ unique health needs.
We recommend that providers tailor their care model to meet the needs of senior patients. CenterWell Senior Primary Care operates 11 locations in the Las Vegas area with facilities that include wider hallways for wheelchairs, nonslip floors to prevent falls, and custom exam chairs that help patients sit and stand safely. These facilities follow a value-based care team approach that includes doctors, pharmacists, social workers, and behavioral health special-
ists who can help address the lifestyle factors affecting health, including transportation, access to nutritious food, and mental health issues.
CenterWell physicians often spend up to 40 minutes with each patient compared with the average 10 to 15-minute visit at a traditional doctor’s office. This extra time allows us to build relationships with patients and provide recommendations for their unique needs. For example, if a patient is one of the 5.2 million seniors facing food insecurity, we refer them to a social worker who can help locate community resources. If a patient reports social isolation and loneliness — which has been a major issue among seniors and was exacerbated by the pandemic — we may send them to the in-house behavioral health specialist for support.
Depending on a patient’s needs, we may recommend home health care services. In-home health care providers can perform a variety of services, including managing chronic conditions or helping a patient recover from injury, illness, surgery, or hospitalization.
CenterWell Home Health’s team works closely with health care providers to ensure that their care plans are personalized for each patient’s needs. Further, home health care clinicians can also assess the lifestyle factors affecting health. A home health nurse may evaluate a patient’s home for food insecurity or review prescriptions to ensure a patient’s medications are up to date.
In these ways, cooperative providers like CenterWell Senior Primary Care and CenterWell Home Health work together to coordinate care, utilizing a holistic approach. This working relationship improves patients’ continuity of care, which research shows improves health outcomes, including a reduction in hospitalization rates, emergency room visits, mortality rates, disease-related complications and health care expenses.
The Las Vegas health care system needs to come together around the common goal of improving health outcomes, especially for seniors. That means tailoring our offices and care models to their unique needs, addressing the lifestyle factors affecting health, coordinating personalized care plans with other doctors, and increasing access to holistic health care.
OUR MISSION:
To provide excellent patient care and advance the field of vascular neurology. WWW.VNLVEGAS.ORG


CONDITIONS TREATED:
Headache and migraine • Stroke • Brain Aneurysm • Blockages in brain and neck vessels • Compression fracture of vertebral body • Middle meningeal embolization • Chronic subdural hematoma • Intracranial stent and angioplasty • Head and neck tumor embolization •
Brain and spine arterial malformation (AVM) • Spine tumor embolization
We have 24/7 coverage at Sunrise Hospital, Southern Hills Hospital and Mountain View Hospital as well as outpatient care in our clinic. Contact us to schedule your appointment today!

While February is a time to celebrate love, there is another matter of the heart that is just as important — American Heart Month. Even though heart disease is generally thought to be a health issue that predominantly affects men, it is the No. 1 cause of death for women in the United States.
Smoking damages the heart and blood vessels, leading to heart disease. Even if you are a long-time smoker, quitting yields rapid and dramatic health benefits while reducing your risk of a heart attack.
R.D.N.,Men and women share many similar symptoms of heart attack, including pressure in the chest, but women are more likely to experience a variety of other symptoms. These symptoms can often be attributed to blockages in the smaller arteries of the heart, as well as the main arteries. This condition is known as small vessel heart disease or coronary microvascular disease.
Symptoms may include nausea and vomiting, sweating, lightheadedness, and pain in the neck, jaw, shoulder, or upper back.
Risk factors, such as family history of heart disease, are out of many individuals’ control, but 73% of heart attacks in women aged 35-44 can be attributed to unhealthy lifestyles. Making healthier choices is one of the most effective ways to affect that which we can control. Studies show that healthy lifestyle changes have resulted in 330 fewer women dying from heart disease per day.
According to the American Heart Association, cardiovascular disease affects about 92.1 million Americans and is responsible for one in every three deaths. Fortunately, the condition is often preventable and reversible. At right are tips that can help people ensure a healthier heart at any age.
Consider these lifestyle changes to help lower your risk of heart disease. They are a great way to keep your heart healthy and to take preventable action before symptoms appear. By understanding the risks and symptoms of heart disease, you can make simple lifestyle changes that may help you avoid cardiovascular disease and live a healthier life.
The American Heart Association recommends consuming a maximum of one alcoholic drink a day for women. Excessive drinking may lead to increased heart health risks including high blood pressure, cardiomyopathy, cardiac arrhythmia, and even death from alcohol poisoning.
The American Heart Association recommends that adults get at least 150 minutes each week of moderate-intensity aerobic activity or 75 minutes each week of vigorous aerobic activity. Living a more active lifestyle not only reduces your risk of heart disease, but it also reduces risk of type 2 diabetes, colon and lung cancers, and early death.
2 6
Not everyone experiences severe chest pains during a heart attack, and symptoms may vary by gender, age, and other factors. Early detection and fast treatment save lives. Regular checkups with a primary care physician are important to help monitor and prevent issues.
82% of people aged 20-49 have a “poor” rating on the American Heart Association’s healthy diet score. Eating a hearthealthy diet with fiberrich foods consisting of fruits, vegetables, whole grains, nuts/seeds, and lean protein may help control your weight, cholesterol, and blood pressure. Limit saturated fats, sodium, sweets, and sugary beverages.
3 7
Low-quality sleep can be linked to an increased risk for high blood pressure. According to the American Heart Association, most people need seven to nine hours of sleep each day. Getting too little or too much sleep may also influence your heart health.
Workplace stress, financial stress, and other common types of stress can impact your heart. Activities like meditating, exercise like yoga, and even sleep can all help to ease stress.
4 8
About 69% of women aged 65-75 have high blood pressure. Checking blood pressure at a doctor’s visit and at-home monitoring is beneficial in detecting any changes in patterns.
Though Alzheimer’s disease has been recognized and studied for more than a century, researchers have not been able to determine its exact cause. The number of cases of this devastating neurological disease, which affects memory, thinking, learning, and organizational skills, continues to skyrocket worldwide, propelling a global research effort to identify its underpinning so that therapies can be developed to slow or prevent progression of the disease.
At the forefront of the effort to develop therapeutics has been the amyloid hypothesis — the idea that amyloid protein, responsible for the characteristic plaques seen in the Alzheimer brain, is the driver of the disease process. Amyloid deposits are one of the earliest features of the disease, and in addition to being toxic to brain cells, are involved in all the genetic forms of the disease. Thus, it is thought that amyloid buildup in the brain triggers a cascade of events leading to cell damage and death. The sooner that trigger is removed (if it can be removed), the more likely we’ll be able to intervene in the disease process.
With so many in the field lending enthusiasm to this hypothesis, anti-amyloid drugs comprise the majority of the experimental approaches in the Alzheimer’s drug pipeline. However, the amyloid hypothesis is just that, a hypothesis, and science requires us to validate it through
clinical research. This is where our current efforts lie, with several recent developments reinforcing that we are on the right path.
In November, the New England Journal of Medicine published Phase 3 results of the Clarity Alzheimer’s Disease trial revealing that the anti-amyloid drug, Lecanemab, was effective in removing amyloid plaque and slowing cognitive decline in individuals with the earliest symptoms of Alzheimer’s
In addition, biomarkers, including another toxic protein termed “tau,” and measures of amyloid in the blood, are going in the right direction with Lecanemab, providing further indication that this drug is able to intervene in the disease process.
The results of the Clarity AD study support the amyloid hypothesis and we anticipate further validation to be forthcoming. Donanemab, another anti-amyloid drug, had encouraging Phase 2 results for the treatment of early Alzheimer’s and is now undergoing a Phase 3 trial and an open label extension, with results expected later this year.
In January, the U.S. Food and Drug Administration granted accelerated approval of Lecanemab for the treatment of Alzheimer’s at the mildest symptomatic stage. This accelerated approval is an exciting step forward in treatment.
Researchers are testing Lecanemab to see if it can be effective even earlier in the disease state.
The AHEAD trial is testing Lecanemab in patients with normal cognitive function, but at risk for Alzheimer’s because of amyloid plaque buildup in the brain, with the ultimate goal of determining if the drug can prevent or delay symptoms. If successful, the effect on the Alzheimer’s landscape would be huge, with many more benefiting from this approach.
Cleveland Clinic Lou Ruvo Center for Brain Health, the only trial site for the AHEAD study in Nevada, is seeking individuals who are:
n Age 55-80
n Healthy, non-smoking
n Have not been diagnosed with Alzheimer’s disease, but may have a higher risk of it because of having a close family member with the disease or noticing some memory symptoms in themselves
Those interested in learning more about the AHEAD study can visit healthybrains.org/ AHEAD or call 702-701-7944.







From a medical office space to a state-ofthe-art Class A medical building, there are many reasons that a custom-built medical facility would be important for physicians, patients, and the community.
 Cory Frank is Vice President of Business Development and Project Management at Nigro Construction
Cory Frank is Vice President of Business Development and Project Management at Nigro Construction

It is vital to know the needs of the facility before beginning the design process. For example, surgery centers have more diverse code requirements than an exam clinic or a standard medical office. These varied needs can include designing the layout to optimize workflow, incorporating specialized equipment and technology, and creating a comfortable and welcoming environment for patients. Even the size of hallways needs to be considered — wide hallways can accommodate stretchers and wheeled beds.
Cleaning and disinfecting requirements are also important to consider because walls and surfaces must be able to withstand frequent sanitization for infection control.
There are four key steps to the design-build process, and each has unique elements, depending on the function of the facility. This helps clients prepare by providing cost estimates, budgets and schedules, civil and site development, drawings, land development, utility coordination, value engineering/cost saving, and zoning packages prior to signing a construction contract.
The design-build process in four steps
This is the beginning stage where you will start to get a clear vision on the overall process.
Nigro Construction broke ground on a Class A medical build, Queensridge Medical Center, in 2021. The state-of-the-art facility is under construction with anchor tenant Dr. Crovetti of Crovetti Orthopaedics and is expected to be completed this year. (Ronda Churchill/Courtesy)

This step is crucial to the forecasting process and ensures that everyone is aligned with the project priorities. In medical construction, value engineering and cost analysis are beneficial in ensuring that the project meets the necessary functional requirements, while also being financially viable. This step can help identify cost saving opportunities, optimize the use of resources, and ensure that the finished project is high quality.

Nigro Construction’s improvement for Couture
Dermatology included the creation of a reception area, multiple offices, exam rooms, Category II procedure rooms, support rooms, and circulation areas.



The team creates the floor plan and you begin to see the project come to life. This gives the most insight into the new build.
Time is one of the most important components when constructing a medical building. Having the latest information about materials, logistics and local municipal agencies is crucial. Transparent updates throughout the process allow the client to be in the loop until the project is complete.
According to the 2021 Southern Nevada Homeless Census and Survey, there are 5,083 individuals experiencing homelessness in Southern Nevada on any given night and 13,076 Southern Nevadans — including families with children, couples, and individuals of all ages — who will experience homelessness at some point this year.
other ailments.
The percentage of the homeless population affected by some health conditions can be double or triple that of the general population.
On average, people who are homeless have higher rates of illness and have a 12-year shorter life expectancy than the general U.S. population.
HopeLink of Southern Nevada’s mission is to prevent homelessness and keep families together. It provides residents of Southern Nevada with housing, food, medical care, employment, utility, and low-income homeless assistance programs.
Homelessness and other hardships can happen in the blink of an eye, and the residual hopelessness of these situations can leave individuals with mental and physical health concerns.
Former HopeLink of Southern Nevada client Lorinda worked with debilitating pain to support her young daughter. She had received a raise just before a life-threatening cyst on her spine required immediate surgery and a 12-week recovery.
 Stacey Lockhart is chief executive officer of HopeLink of Southern Nevada
Stacey Lockhart is chief executive officer of HopeLink of Southern Nevada
Daily experiences of homelessness are traumatizing and challenging because of competing needs for survival. The best, most coordinated medical services are not very effective if the patient’s health is continually compromised by street and shelter conditions.
According to the National Health Care for the Homeless Council, even inpatient hospitalization, residential drug treatment and mental health care do not have lasting effects if a client returns to the streets or shelters upon discharge.
Many of us don’t often think about how stable housing affects our overall health, but it provides privacy, safety, and a place to rest and recuperate from illness and
Lorinda kept her employer up to date regarding the situation and filed the appropriate FMLA paperwork. Her employer fired her and denied her unemployment. Lorinda could not afford a lawyer to represent her, and her surgical recovery and unemployment left her on the cusp of homelessness.
For about six months, Lorinda and her daughter lived in their car as she frantically searched for help. She was later diagnosed with PTSD from her experience.
HopeLink helped Lorinda find housing and provided assistance with rent and utilities. It helped her find a work-from-home job with a major communication technology company. Lorinda was also able to replace a car that was repossessed. At age 50, she’s going back to school, pivoting her career from customer service to data analysis.
Lorinda’s story demonstrates the tie
Many of us don’t often think about how stable housing affects our overall health, but it provides privacy and safety and a place to rest and recuperate from illness and other ailments.
UNHOUSEDHOUSED





































Risk of heart attack

















35 %

17 %
Risk of depression
49 % 58 %
8 %














Risk of substance abuse
































































16 %
between housing security and overall health. Reliable housing is necessary to realize a healthier society, and communities that invest in affordable housing incur lower public costs and achieve better health outcomes.


Stacey Lockhart joined HopeLink in 2019, and has steered the organization through incredible growth, resulting in an increase of 1000% as the end of 2022. This includes expanding from 14 to 50 employees, strategically expanding the number of board members and influence, annual budget growth from $1.2 to $13.5 million and opening a second office in midtown Las Vegas and additional outreach centers.






4 The Kids Foundation , Nevada’s premier pediatric cancer and rare disease treatment center, was selected as chairperson of the Nevada Rare Disease Advisory Council. The council’s mission as an advising body is to provide a platform for those affected by rare diseases, including pediatric cancer.
Cure 4 The Kids Foundation announced the Englestad Foundation ’s support, which provides $556,000 to fund the behavioral health needs of childhood cancer and rare disease patients.
The Englestad Foundation funding covers a year’s worth of Behavioral Health Team services to assist patients and their families with the effects of a childhood cancer diagnosis and other childhood diseases with highly challenging medical journeys.
Southwest Medical , part of Optum Care , added thirteen providers to help meet the need for health services in Las Vegas. Paige Cejka , P.A. joined Optum Care Primary Care and specializes in adult medicine. Eric Lee , M.D. joined Southwest Medical and specializes as a hospitalist. Donald Todd Swain , D.O. joined Southwest Medical and specializes in adult medicine. Tuong Bui , D.O. joined Southwest Medical and specializes in adult medicine. Southwest Medical’s Oakey Healthcare Center location welcomed Sara Fitzgerald , P.A., who specializes in rheumatology, and Chelsea Musci , P.A., who specializes in adult medicine. Southwest Medical’s Siena Heights Healthcare Center welcomed Landero Maria , M.D., Dustin Ran-
dy , P.A., and Domonique Katona , P.A., who all specialize in adult medicine. Rancho Urgent Care welcomed Savannah Pearson , APRN, and Chiamaka Faith Ibeabuchi , APRN, who both specialize in urgent care. Eastern Healthcare Center welcomed Shanna McManus , APRN, who specializes in adult medicine. Tenaya Healthcare Center welcomed Tammy Collander , APRN, who specializes in adult medicine.
Robert Smith , M.D. joined Optum Care Anesthesia

Southwest Medical Surgery Center – West Charleston was recognized by Newsweek as one of America’s Best Ambulatory Surgery Centers for 2023, and No. 1 in Nevada. It’s one of about 500 facilities across the U.S. with this honor.
Nathan Adelson Hospice ’s Chief Operating Officer and Chief Nursing Officer, Angela Collins , was elected to the Nevada Nurses Association state board of directors as director-at-large and was appointed to serve on its legislative committee. During the three-year term, Collins will serve as a committee liaison for membership, by-laws, and legislative works, aid in promoting the Nevada Nurses Association to the general public, assist in membership recruitment and retention, communicate association updates and happenings to members and industry colleagues, as well as other duties assigned by the executive committee, board of directors, or by-laws.
Nathan Adelson Hospice announced the Food Assistance Program to help homebound vet-
erans in Pahrump. Volunteers will package and deliver nonperishable food items to veterans’ homes. “We saw a need and wanted to make a difference,” said Karen Rubel , Nathan Adelson Hospice President and CEO. “Thanks to the kindness of our donors, this program will allow us to meet the needs of folks right at their doorstep.”
Four Valley Health System hospitals received an “A” Hospital Safety Grade from the Leapfrog Group Summerlin Hospital Medical Center and Valley Hospital Medical Center each earned their first “A” grades; Desert Springs Hospital Medical Center earned its second consecutive “A” grade; and Henderson Hospital earned its 9th consecutive “A” grade for Fall 2022.
Nevada Donor Network Foundation announced that Foundation President Steven Peralta will join University of Nevada, Reno Foundation board of trustees. Peralta brings more than 20 years of leadership experience in philanthropy, donor relations and fundraising to his role on the board. The board of trustees was created in 1981 to provide a way for private individuals, corporations, and foundations to make charitable gifts to University of Nevada, Reno. Peralta will assist the board as the foundation receives, invests, and administers funds to benefit the university, while honoring the philanthropic intent of its generous donors.
Viticus Group, a leading provider of continuing education for veterinary and medical healthcare professionals
Continued on page 48







Located at at the corner of Edmond Street and O’Bannon Street, The Home For Now Hope For Tomorrow House will eliminate a long waiting list for families with critically ill children in Las Vegas who have nowhere to stay. With increasing numbers of families staying longer than a month, the second house will offer families stability and independent space during their extended stay.

worldwide, announced its 2023 Veterinary Academy lineup, consisting of year-round veterinary health education programs and hands-on laboratory training held at its two campuses in Las Vegas. New courses added in 2023 include: dermatology, gastrointestinal endoscopy, advanced veterinary technician education, and more. With more than 50 courses offered between January and December 2023, professionals have a one-stop shop to earn continuing education credits and enhance their skills that can be utilized at their own practices. “Practical, hands-on training is the core of what we do at Viticus Group,” said Andrea Davis, chief executive officer, Viticus Group. “We work alongside world-renowned veterinary health experts to deliver the highest caliber, innovative education to those who save
Three new Intermountain Healthcare clinics specializing in senior care opened Dec. 5. All three are Intermountain myGeneration clinics that specialize in primary care for those 65 years and older. “Our caregivers at these three new clinics will provide care, including overall preventative medicine for one of the most highneed populations in our communities: our seniors,” said Dr. Paul Krakovitz , region president of Intermountain Healthcare. “ The three new clinics, all serving the Henderson area, are among more than 60 Intermountain
Continued on page 50
WE KNOW





STAY IN THE KNOW WITH EVERYTHING VEGAS SIGN UP TO RECEIVE OUR NEWSLETTERS AND EVENT INVITATIONS!
STAY IN THE KNOW WITH EVERYTHING VEGAS SIGN UP TO RECEIVE OUR NEWSLETTERS AND EVENT INVITATIONS!

















[SUBSCRIBE AT GMGVEGAS.COM]
[SUBSCRIBE AT GMGVEGAS.COM]






SCAN TO SUBSCRIBE
SCAN TO SUBSCRIBE



Healthcare clinics throughout Southern Nevada, including specialty care and InstaCare locations.
Make-A-Wish Southern Nevada partnered with Resorts World Las Vegas to give Harli , 10, the “Time of Her Life” experience, including a visit to Enchant , pizza-making at Mulberry Street , a makeover at Miss Behave , family dinner at Kusa Nori , an evening at the David Blaine Show, and a visit to Horses4Heroes Harli has a rare respiratory rheumatology disorder. Her wish marks 2,500 wishes that Make-A-Wish Southern Nevada has granted for children in the Valley.
Nevada’s statewide LGBTQ+ civil rights organization, Silver State Equality , launched its



new evidence-based campaign, “Vaccinated and Proud.” The campaign, which is funded through a grant from the Southern Nevada Health District , aims to increase awareness of and access to COVID-19 and flu vaccines for Black and Latinx LGBTQ+ communities in Southern Nevada, and to encourage LGBTQ+ community members to get vaccinated.
Nevada Donor Network Foundation announced its newest board members: Gordon Prouty , Karla Perez , Damon Schilling and Michael Young Together, they bring decades worth of leadership experience to the NDNF board and will help the foundation’s efforts to expand transplantation capabilities to the State of Nevada.




Only UMC provides truly breakthrough treatments for southern Nevadans.




UMC is where you’ll find Nevada’s only organ transplant center, only verified burn care center, only dedicated heart failure clinic, and the state’s only designated pediatric trauma center. And we’re home to Nevada’s most advanced robotic surgery program, too.




We’re keeping our eyes on the horizon—so we can provide the most advanced care to you now.






Clinical Research at Comprehensive has led to







Comprehensive Cancer Centers has participated in the development of 100 new FDA approved cancer treatments. With 100 ongoing clinical research studies, right here in Southern Nevada, we are entering a new age in cancer treatment — where people are no longer entrenched in their battle against cancer, but instead living with cancer . These new cancer therapies are increasing the quality of life for our patients and their families, and most importantly, giving them the opportunity to live their lives to the fullest.

More precious moments with my princess