

FOR unmatched insight, VIS ion matters

FORward VISion thrives
We applaud that your goals and aspirations begin with a vision of achieving peace of mind. Our vision is helping make yours a reality. At FORVIS Private Client™ our forward-thinking advisors help high-net-worth individuals and multigenerational families, trusts, estates, investment partnerships, and private foundations thrive through complexity and change so you can prepare for what’s next.



Bringing physicians together to improve the health of our community.



Editor’s Note: All materials for the Journal must be submitted by the first of the month prior to publication.
Co-Editors:
Jim Blaine, MD
Minh-Thu Le, MD
Junior Co-Editor:
Andrew K. Le
Managing Editor:
Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
Frank Cornella, DDS, MD
Dalton Boyer
Andrew Le
Jean Harmison
Barbara Hover
Nancy Yoon, MD
Jana Wolfe
SOCIETY OFFICERS
James Rogers, MD President
Vu Le, MD Secretary
Jim Blaine, MD Treasurer
Sanjay Havaldar, MD
Immediate Past President
Council Members:
David Haustein, MD
Melissa Gaines, MD
Steven Gradney, MD
Keith LeFerriere, MD
Kyle John, MD
Jaya LaFontaine, MD
Nancy Yoon, MD
Managing Director:
Jean Harmison
Executive Office:
4730 S. National Ave. Suite A1
Springfield, MO 65810
email: director@gcms.us
www.gcms.us
All
for
will be
EDITOR'S PAGE
by Jim Blaine, MDFormer GCMS President John P. Ferguson OB/Gyn, for many years before and after he retired, selflessly performed hundreds of SAFE (Sexual Assault Forensic Examination) exams on children who had been victims of sexual abuse. Dr. Ferguson finally fully retired and moved out of state in 1995. Greene County Prosecutor Tom Mountjoy then asked the GCMS to step up, and six physicians did volunteer to take SAFE training; however, it was obvious that we needed to do more to fully fill the void left by our patron saint (John P.). The Springfield area community came together in 1995 to support the founding of the Child Advocacy Center (CAC) and the Greene County Medical Society has been involved in the e ff ort from the start. Please check out the 1995 and 1996 GCMS Journal articles reprinted in this issue to learn more.
The current CAC Medical Director is former GCMS President Dr. Matt Stinson; he and current CAC Executive Director Kat Dull are eager to have increased participation from GCMS members. Kat has written a “Call to Action” for this Journal, and we have no doubt that she will receive her desired response as the GCMS Foundation Board is meeting at the CAC on April 8 to further discuss our involvement going forward. Please call the GCMS office at 417-887-1017 if you would like to set up a tour or obtain additional information; we will have regular updates for you in the Journal.
According to the DEA, fentanyl overdose is the leading cause of death in Americans ages 18 through 45 and the addictive drug is responsible for 70% of the U.S. 107,000 drug overdose deaths in the past year. Nancy Yoon, MD is the Springfield/Greene County Health Department Medical Director and writes in this issue about the “New Initiative to Combat Overdose Fatalities in Greene County”.
As we know, most drug overdoses are caused by drug addictions. Drew Shoemaker, MD is the Medical Director of Addiction Medicine at Burrell/ Brightli Medical Group and has written about the rewards of treating patients with addictions.
Attention-Deficit/Hyperactivity Disorder (ADHD) is an interesting condition. Over the years, I have received many requests from teachers to treat their students (who are my patients) for ADHD. My response is always the same: I refer them to a mental health professional for diagnosis, and then work with them on the treatment plan. Interestingly, many of the students ended up with an anxiety diagnosis rather than ADHD. Amit Jagtiani,


MD, is a Child and Adolescent Psychiatrist who has written on “Decoding ADHD” for this issue of the Journal. His article included many pearls for me.
Many years ago while scuba diving in Grand Cayman with friends, we met a retired ENT physician whose retirement plan was to dive everywhere in the world, and then do it again. Of course, we had to ask his favorite, and he did not hesitate to say, "Truk Lagoon!" Missouri State Medical Association Executive Vice President Je ff Howell and his son Rex recently did that trip and brought back some great pictures along with an even better story. The aerial picture can be found on the cover of this issue.
Last week GCMS immediate past president Dr. Sanjay Havaldar invited Dr. Jim Rogers, Dr. Norman Myers (founding President of OTC), me, and our wives to a Colo-Rectal Awareness party (CRAP) at the Bass Pro White River Convention Center. We had great fun and were impressed by our hostess Cox’s Lisa Alexander, and speaker Dr. John Trombold. It is impressive that our colorectal surgeons and gastroenterologists have put together such a passionate fundraiser in an obvious e ff ort to make life saving colonoscopies accessible for patients who otherwise might not be able to a ff ord them. We asked Dr. Trombold to write us an article on “CRAP” and he did not hesitate. His article is in this issue. Please consider attending next year; it is a lot of entertainment for such a serious topic.
Finally, we are taking reservations for GCMS Rocky Mountain Medicine 2024 in Breckenridge Colorado July 14-20 at the Residence Inn by Marriott. We had a great time last year! Attendees provide a total of 12 hours CME facilitated by Triesa Massey at Cox. Barb and I have attended all of the GCMS CME trips over the past 28 years and always have fun; so great to spend extended time with colleagues and their families! Please call me at 417-861-9286 if you have any questions.

Join Up & Join In
Several recent reports and now multiple articles indicate the health benefits of human interaction on well-being, mental and physical health and even longevity. I find the evidence compelling enough that my “life style” speech for my patients includes avoiding dangerous substances, excess, moderate diet, daily exercise, dental hygiene, proper screenings and vaccines and now “active philanthropy.“
While the evidence bestows the gains to the individual for personal improvements, these studies fail to note the tremendous collective and community benefits when the support group has a philanthropic purpose. Just some local examples are Child Advocacy Center, Care to Learn,


and Crosslines. All of these organizations need volunteers.
Take the typical physician profile of a busy work life, long hours, frustrations over poor or broken processes that impede or complicate care and magnify them by a pandemic that forced isolation. Predictably, outcomes of frustration, burnout, and ghosting manifest.
It is time to reclaim our own empowerment to become a Physician Community. So join up to do good, live better and longer lives, and to create a caring and supportive group of physicians." Our advocacy for health has to include individuals we care for, the community we live in, and ourselves.

Mortgage Loans for Medical Professionals
Whether you’re starting a residency, specializing to meet unique needs, or growing your own practice, you’ve worked for every opportunity. We have the right loan to finance the perfect home for you. Let us help your opportunity take shape with a mortgage or refinance. Ask
• Financing available up to 103%
• Loan amounts available up to $2,000,000 based on LTV
• No mortgage insurance required
• Warrantable and non-warrantable condos
• Fixed and ARM products
• Available for the purchase, refinance or cash-out refinance of primary residence or secondary homes
• Can close 120 days prior to the start of employment with an executed employment agreement

Tim Prater
Mortgage Loan Officer
NMLS#554842
417.827.4755
tim.prater@cadencebank.com
CadenceBank.com/TimPrater

Scott Davis
Mortgage Loan Officer
NMLS#948397
417.988.4089
scott.davis@cadencebank.com
CadenceBank.com/ScottDavis

Brandon Fisher
Area Production Manager, MLO
NMLS#484932
417.840.2577
brandon.fisher@cadencebank.com
CadenceBank.com/BrandonFisher
TRUK LAGOON, MICRONESIA DIVE
by Jeffrey S. Howell, Executive Vice President, Missouri State Medical AssociastionMy son, Rex, is a senior in high school. He has enlisted in the United States Marine Corps, and he’ll ship out not long after he graduates this spring. I wanted to take him on a father-son trip before he left. Scuba diving is a hobby we share, so we decided on a trip to a distant, little-known island in Pacific Ocean. Over the holidays, we traveled to Truk Lagoon, located in Micronesia, for some diving.

Even though there are places to dive in Missouri, it’s more rewarding – and warmer – to find a tropical place to scuba. It’s more fun, too.
During World War II, the Japanese chose Truk Lagoon as the location to build their main naval base in the South Pacific. Known as Naval Base Truk, the Japanese navy was able to conveniently operate against allied forces at New Guinea and the Solomon Islands. It

was the forward anchorage for the Japanese Imperial Navy and its heavy fortifications earned it the moniker “The Gibraltar of the Pacific,” among the allies.

In February 1944, the allies launched Operation Hailstone against Truk. Even though the big Japanese warships had already left for Palau, American airmen were able to sink 12 smaller warships and 32 merchant ships. This made Truk Lagoon one of the largest ship graveyards in the world, and it is colloquially known as “Japan’s Pearl Harbor.”


After spending a few days in Japan, we landed in Chuuk State via Guam. Chuuk is one of the Federated States of Micronesia. After meeting up with the rest of the divers from our mid-Missouri dive shop, we boarded the Odyssey, a full-service dive charter, where we would live for the next seven nights.

In a normal day, the Odyssey would stop at a wreck in the morning where we would do two dives. During lunch, the captain would move us to a different wreck, where we would dive two more times. Most of the ships were large enough that it took two dives to explore the entire thing.

Most of the shipwrecks sat in more than 150 feet of water, which meant we had to perform a number of safety protocols before surfacing. Some of them laid on their sides, but most that we visited were sitting

upright. Many war artifacts are still visible in cargo holds and other areas of the wrecks – some have tanks and trucks still sitting on their decks. The sea life on the wrecks was also excellent. We saw moray eels, rays, sea turtles, a wide variety of reef fish, corals, and even a couple of curious dolphins.

After seven days in Micronesia, we started our long trip home – Chuuk to Guam to Honolulu to Los Angeles to Dallas to Columbia – 40 hours altogether. The best part of the trip wasn’t the diving or the wrecks or the history. It was being able to make some unforgettable memories with my son.

www.goscubaadventure.com
A CALL TO ACTION TO PREVENT CHILD SEXUAL ABUSE
by Katiina Dull, Springfield Child Advocacy Center Executive DirectorFor 28 years the Child Advocacy Center has worked in our community providing services to child victims of abuse and neglect. Among the services primarily provided are forensic interviews and forensic medical exams. A forensic interview is a structured conversation designed to obtain statements from child victims in a developmentally and culturally sensitive, unbiased, legally defensible, and information-gathering manner. The forensic interview is also utilized to assist in the identification of needs and services for the child victim and their supportive, nonoffending caregivers.
The forensic medical examination is a non-invasive comprehensive medical exam conducted at the CAC by SAFE/CARE providers who have specialized training in the medical evaluation of child abuse and neglect. The exam is not much different than a typical well-child check-up, but it does play an important role in gathering information and potential evidence for a child abuse investigation. Moving away from the original concept of assessing the guilt or innocence of perpetrators, forensic medical exams and the SAFE/CARE providers who conduct the examinations play an important role in assessing a child’s well-being, connecting them to healing services as needed, and educating investigative teams and testifying in court proceedings as to the physical condition of a child victim and explaining what those specific conditions (or lack of physical findings) may indicate.
Over the years we have seen some truly horrific acts and laid witness to the physical, emotional, and mental damage inflicted on children in our community. In 2023 alone, the CAC provided 1,238 forensic medical exams. 47% of these medical exams involved allegations of child sexual abuse. 90% of the time the child knew their perpetrator. 20% of the time it was a parent and 38% of the time it was another family member. Only 10% of the time was the perpetrator a stranger. These are our children. They live here among us. In our community. We need to do more. We can’t do it alone.
Child sexual abuse, the most insidious form of abuse, is rarely a one-time event. Rather it is a process that starts with manipulation and grooming, builds to desensitization and boundary violations, and ultimately violates both children and their non-offending caretakers. Perpetrators of child sexual abuse infiltrate communities, organizations, and families. They build a reputation of being a caring and trusted adult. It is the

way they gain access to children. It is this masquerade that makes it hard for children and even their nonoffending caregivers to see what is happening. While we continue to raise awareness and implement prevention programming we must remember that the solution cannot be to expect children to protect themselves. There is no other health crisis we ask children to solve. This must be an adult-led initiative and the medical community must take a leading role.
A 2023 study performed by Parental & Caregiver Perspectives on Child Sexual Abuse Prevention found that 92% of parents want their pediatrician to give them information about protecting their child from sexual abuse. Just as you provide information on safe sleep, seat belt safety, and bike helmets, we need to be intentional in providing information about body safety and protecting children from sexual abuse. That information should include both discussions and resource materials. It needs to be ongoing and embedded into each well-child checkup. The medical community needs to be mythbusters and truth-tellers. There are simple ways to tackle this topic.
The Mama Bear Effect (https://themamabeareffect.org/) has a range of resources and best practice guidance for weaving sexual abuse prevention into pediatric practices. This guidance includes using anatomically correct names for body parts and explaining to parents the importance of doing so – it empowers children to communicate clearly and without embarrassment which can help if an investigation becomes necessary. Talk with children during their exams about private parts of the body. Explain the importance of privacy even within the family unit and encourage independent self-care for children. Model consent throughout the exam by asking children for permission to touch them, take time to explain why you need to touch or look at their genitalia before doing so, and, explain that their caregiver or another adult is also there for safety (there should always be a second adult in the room). This helps children distinguish safe and unsafe situations and models for parents the ongoing conversation about safety they need to have with their children.
Effective child sexual abuse prevention goes beyond the exam room. Pediatric specialists at Children’s Wisconsin developed Awareness to Action – a framework for all
Continued on page 11
ADDICTION TREATMENT & RESOURCES IN SOUTHWEST MISSOURI
by Drew Shoemaker, MD, DABFM, FASAM Medical Director of Addiction Medicine Burrell/Brightli Medical GroupThe first time that I saw Donnie, he was in our Rapid Access Unit and he was in acute opiate withdrawal. He was 33 years old, and had been using opiates and methamphetamine for most of his adult life, starting in his teens. He had made several attempts at obtaining sobriety in the past, but was only able to abstain from use for a few weeks at a time. His parole officer had assisted him in making the decision to get sober by threat of revocation of his parole. He had experienced several overdoses, and one had been nearly fatal, necessitating hospital admission and a long hospital stay. I began to see him in my weekly addiction clinic soon after our initial interaction at the Rapid Access Unit. His path to sobriety was like many. He would have brief relapses, but he continued to follow up. Within six months his urine drug screens showed no substances other than the buprenorphine that was prescribed for his opiate use disorder. Within another six months, he was allowed to leave sober living and live on his own. After two years of sobriety, Donnie completed his Peer Specialist training and passed the Peer Specialist Exam. He is now working in the recovery field helping others find their path to sobriety.
All of us have patients like Donnie in our offices every day. In 2022 48.7 million Americans (17.3%) met criteria for a substance use disorder. Sadly, the most optimistic statistics suggest that only about 6% of Americans who meet criteria for a substance use disorder receive any form of treatment. It is a rare American who does not know a family member, coworker or acquaintance who has struggled with a substance use disorder. Unfortunately since the entry of fentanyl into the illicit drug supply, it is even becoming uncommon for persons not to have known someone who has suffered a fatal overdose.
The American Society of Addiction Medicine defines addiction as “a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment and an individual’s life experiences”. Another way of thinking about addiction is the compulsion to use a substance or engage in a behavior despite adverse outcomes as a consequence of use of a substance or engagement in a behavior. Persons experiencing addiction often make decisions which are contrary to their best interests and difficult to understand from the point of view of an observer. It is difficult to

understand why they would leave important relationships, endure legal consequences and make choices that are injurious to their health in favor of substance use. Essentially, their reward system, the system put in place to promote activities that ensure health and connection have been “hijacked” by the drug of choice. Substances of abuse can stimulate the reward system in a way that normal activities like eating a good meal or engaging in meaningful relationships simply can’t. Using basal dopamine levels as a proxy for reward strength, we see a good meal increasing dopamine levels to about 150% of baseline. Sexual activity will increase it to about 250% of baseline. By contrast, methamphetamine can increase dopamine levels to 1100% of baseline and opiates up to 300% or more. Although this is a somewhat reductionist view of the pathophysiology of addiction, this is what, in part, explains those behaviors commonly seen in persons suffering from addiction.
Currently, the USPSTF recommends screening all adults 18 and over for addiction once a year. There are a great number of tools that are easy to utilize and can be administered by our staff as a part of a routine visit or annual physical. These include the very easy to use CAGE (have you ever felt the need to Cut down/have you ever been Annoyed when people criticize your drug use/ do you ever feel Guilty about your drug use/do you ever have to have an Eye opener). There is also the DAST-10 for adults, and the CRAFFT screening tool for adolescents as well as several other well validated screening tools.
In response to the opioid crisis, the current presidential administration has removed the requirement to obtain a waiver (DATA-2000) to prescribe medications for opiate use disorder. These medications include full opiate antagonists, full opiate agonists and partial opiate agonists. Included in these medications are various formulations of buprenorphine, methadone, naltrexone and naloxone. Prescription of methadone for opiate use disorder is currently restricted to opioid treatment programs, however the remaining medications are highly effective at preventing overdose and relapse in persons struggling with opiate use disorder, and can be used for treatment in an office based setting. Even though the waiver is no longer in effect, there is still an 8 hour training that must be attested to before prescribing these medications for opiate use disorder. It is very
high quality, free training and available at (pcssnow. org) and click on the 8 Hour MOUD Course. If you have any questions or are interested in providing medication assisted treatment (MAT) for you patients with opiate use disorder, please feel free to reach out to me. My contact information is at the end of this article.
One of the barriers to treatment is identifying the resources in the community to which patients can be referred for treatment. Springfield and Greene County are rich with recovery resources, including multiple providers who offer sober living, detox, residential setting substance use treatment and intensive outpatient therapy (IOP). We have a very active number of alcoholics anonymous (AA) meetings as well as a large number of narcotics anonymous (NA) meetings. There are multiple providers who can provide office based treatment of substance use disorder also, and those can be accessed at mcrsp.org or at www.samhsa.gov/find-help and entering the city of Springfield or your city.
When I was in medical school and residency, we had no lectures on identifying and developing a treatment plan for our patients with addiction issues. I am very happy to say that we now have medical students and advanced practice provider students doing rotations with us at the Rapid Access Unit and addiction clinics regularly. Substance use is a significant medical issue and those of us providing care for Southwest Missourians stand in the position to address this important concern. One of the most rewarding parts of treating persons with substance use disorders is celebrating their successes with them. The difference in the quality of life of a person celebrating a year of sobriety contrasted to the life they would be living if they had continued in their addiction is remarkable. To be even a small part in helping them attain sobriety is one of the most rewarding things that I have been fortunate to experience in my medical practice.
Continued from pg. 9 "A Call to Action to Prevent Child Sexual Abuse"
in protecting children from sexual abuse. Awareness to Action is based on the Center for Disease Control and Prevention’s guide Preventing Child Sexual Abuse Within Youth-serving Organizations and guides operational policies from employee screening and hiring, to creating safe environments, and how to respond when policy violations occur. Organizational cultures that make a paradigm shift from risk management (policies intended to protect against accusations) to prevention (policies that protect children from predatory practices) are better protected from perpetrators infiltrating their workplaces.
The medical community is a uniquely trusted part of our society, and the Greene County Medical Society has deep roots in the founding and support of the Child Advocacy Center in Springfield. Please see the 1995 and 1996 GCMS Journal reprints in this issue. The CAC is now calling on you again to be a part of the solution. Too many of our children are sexually abused. One is too many, and we cannot do it alone. To learn more visit //childadvocacycenter.org/community-education/ pediatric-resources/, join us at our monthly open house Coffee for a Cause events, and follow the CAC on social media for opportunities to join the CAC in our efforts to truly protect the children in our community from sexual, physical and emotional abuse. You can also call the Greene County Medical Society at 417-887-1017 if
you would like for them to contact you with additional information on how to participate.
CHILD ABUSE FACTS
• CDC estimates 1 in 7 experienced maltreatment in 2021. Of confirmed cases of child maltreatment in 2021
• Nationally: 76% was for neglect, 16% was for physical abuse, and 10% was for sexual abuse.
• In Missouri: 53% was for neglect, 30% was for physical abuse, and 32% was for sexual abuse.
• *Polyvictimization means some children have confirmed findings for more than 1 type of maltreatment.
• 1 in 10 children are sexually abused before their 18th birthday
• 93% of child sexual abuse victims know their abuser
• 34% are family members
• 59% are acquaintances
• 34% of child sexual abuse victims are under 12 years old
• 1 in 9 youth experience online sexual exploitation
• The average age of 1st time disclosure of child sexual abuse is 52
CHILD ADVOCACY CENTER... THE TIME HAS COME
by Jim Blaine, MD* This article is a reprint from the original article published in the September 1995 GCMS Journal
A couple of months ago, six GCMS physicians attended a day long SAFE (Sexual Abuse Forensic Exam) training session conducted by ex-Springfield pediatrician and now emergency pediatrician, Jim Kelly, M.D. The training session was held for the first time in Springfield. SAFE exams are not treatment exams; they are legal exams designed to assess guilt, or innocence, of alleged perpetrators, and they require special training and certification. Those of us attending the session were astounded at the number of interviews the children were enduring: medical, law enforcement, Division of Family Services, juvenile, prosecuting and defense attorneys and finally the trial. We commented on our concern, and Melody Dunlap, program development specialist, Children's Services, Jefferson City, suggested we should consider a "child advocacy center."

Child advocacy centers are operational in many cities across the country. The ideology is simple. Establish a child-friendly center that reduces the number of interviews and exams the child must endure to one. This is done by placing representation of all concerned agencies under one roof to enhance communication. Communication, along with a videotape and/or one-way glass, combine to spare the child victim what has been called "the revictimization by the system." We all liked the concept of the child advocacy center, and we held an informal dinner party and invited Melody to further enlighten us. She told us that 'two days before she arrived, Eileen Rogers, executive director, Together for Kids, St. Louis, was traveling through Springfield and heard on the radio about two abused children. She called Melody to see if Springfield had a child advocacy center and, if not, could we start
one? We decided to put together a larger meeting and invited every professional involved with sexually abused children. The guest list grew so large that we needed a larger meeting place and approached Dr. Don Landon of Southwest Missouri State University. He responded by giving us Glass Hall 101 and two additional breakout rooms. One hundred and thirty-two people attended the half-day conference, co-sponsored by GCMS and Ozarks Fighting Back. We heard Tom Mountjoy, Greene County prosecuting attorney, outline the present system, followed by presentations by representatives of the Las Vegas, Kansas City and St. Louis child advocacy centers. We then broke down into groups of ten to assess individual thoughts on the subject. We decided the following:
• We need a child advocacy center in Springfield as soon as possible.
• The center should be free standing, community owned, and not under any single existing agency's control.
• We need to hire a director and aggressively pursue funding. (Amy Lavalley, News-Leader, wrote an excellent story highlighting the meeting, and it is reprinted this month with permission.) Our planning committee (please see list) has subsequently met and elected a subcommittee, composed of Harold Bengsch, myself, Tom Mountjoy, Dottie Mullikin and Peggy Pearl, Ph.D., to advertise for and screen director candidates.
We also established a funding committee, composed of Norb Bagley, Harold Bengsch, Ron Carrier, Rebecca Cherry, Don Landon, Ph.D., Mary Kay Ross and Sister Fran Stein, RSM, that will also look at possible sites for the center.
Dr. Landon reported that he would support housing the child advocacy center in the same building as the new SMSU Child Development Center. He was quick to point out that the proposal would be a partnership and not a sponsorship; the center would be owned and controlled by the community. Mr. Bengsch has donated two attractive rooms at the LINK Clinic for space for SAFE exams. The LINK Clinic itself may be a possibility for a child advocacy center site if Medicaid children become covered by private physicians under managed care as planned.
The child advocacy center is no single person's idea. Everyone involved to date has been positive and proactive, and at this time it really seems that the time has come.

WHAT A DIFFERENCE A YEAR
MAKES... CHILD ADVOCACY CENTER
by Marion Hancock, Former Executive Director, ChildAdvocacy
Center* This article is a reprint from the original article published in the September 1996 GCMS Journal
The Child Advocacy Center Inc. has recently reached another milestone. On September 21, 1996, we celebrated our first anniversary of providing services to victims of child abuse in our community. We celebrated the fact that the agencies mandated to report and investigate. and prosecute these cases are working harder than ever to coordinate services with those individuals requested to medically evaluate and treat children and those agencies which provide mental health and victim advocacy services to these children and their families.
Many of you have followed our progress closely in previous articles written for the Bulletin by Jim Blaine, M.D., President of the Greene County Medical Society. The Child Advocacy Center is also fortunate to have Dr. Blaine as the President of our Board of Directors. He has provided enthusiastic leadership in helping us reach many of our goals this past year.
Children's advocacy centers are child-focused, facility-based programs that use multi-disciplinary teams to coordinate the judicial and social systems' response to victims of child abuse. The teams work to prevent revictimization of abused children. Typically, these teams conduct joint interviews and make team decisions about the management of these cases and provision of services to child victims and their families.
The Child Advocacy Center's multi-disciplinary team members include physicians, nurse practitioners, prosecutors, juvenile officers, Division of Family Services investigators, victim advocates, and mental health providers. The goal of each of these representatives is to prevent revictimization of the child by:
• providing a comfortable, child-friendly atmosphere where children can talk to adults
• reducing the number of people involved in each case, if possible, which may eliminate unnecessary interviews
• continuing to build and strengthen relationships between agencies and professionals who work with these children;
• improving the outcome for the child and family by referring them to all of the available community resources to address long-term mental health issues.
Children are referred to the Child Advocacy Center by law enforcement officers, juvenile officers and DFS investigators for videotaped interviews and a comprehensive S.A.F.E. (Sexual Abuse Forensic Examination). The Child Advocacy Center also acts as a clearinghouse of information and referral resource for child victims and their families.
Since last September, certified S.A.F.E. providers have evaluated over 160 children. Since June of this year, we have provided a child-friendly environment for over 25 children to receive a video-taped interview.
We are currently located in a section of the Department of Health's L.I.N .K. Clinic. Harold Bengsch, Director of the Springfield-Greene County Department of Public Health has graciously allowed us to utilize this area as we develop our program.
At our September meeting, the Child Advocacy Center's Board of Directors approved the purchase of a home at 1111 East Walnut Street. This is an exciting accomplishment for a "community-owned” children's advocacy center as it enters only its second year! One of our future goals is to work with the existing and new children's advocacy centers in our state to find out how we can provide services and training to the entire state. Governor Carnahan and area legislators continue to give us the support we need to reach this goal.

CHILD ADVOCACY CENTER WHAT THE BOARD MEMBERS SAY:
* This article is a reprint from the October 1996 GCMS Journal
''The Greene County Medical Society has for years assumed a leadership role concerning reducing violence in our community. We have been involved in the DWI Task Force, the SAFE Task Force, and E-911 Advisory Board. The GCMS Alliance has championed SAVE and other issues pertaining to family violence. No issue, however, has been so enthusiastically supported as the concept of the Child Advocacy Center. The image of sexually abused children being revictimized by multiple redundant interviews (no matter how individually appropriate) seems to literally scream for a solution. The Child Advocacy Center is a great solution! It has been implemented successfully across the nation and enjoys a broad based support in Springfield by our agencies, our community leaders, and by our medical community. The Greene County Medical Society remains in firm and enthusiastic support of this mission."
''This department has been very pleased to provide an interim location for the sexual abuse examinations. However, it is obvious to me that the need for an expanded facility is rapidly growing. I am therefore extending support of the Springfield /Greene Department of Public Health for the Child Advocacy Center to begin receiving funds at the earliest date possible so that immediate progress can be made to opening a standalone child advocacy center."
"As a Board Member of the Child Advocacy Center I am confident that our partnership with the community to address the serious problems facing abused and neglected children has been well received and will produce results. Purchasing a permanent facility ultimately saves money spent on interest or lease payments and allows us to focus on sustaining sound operations in the long run. In addition, housing this center in a permanent facility would take full advantage of our current momentum preserving our ability to provide services without commercialism, restrictions or potentially divisive affiliations."
"It is the goal of this office to successfully prosecute individuals who have sexually abused children, yet reach that result with as little trauma to the child as possible. The creation of The Child Advocacy Center, Inc., helps to minimize the number of times a child is interviewed, allows for a great part of the investigation (including the medical examination) to be conducted at one location, and assures that the best interests of the child is always the determining factor in choosing an appropriate course of action."
"It is very important for the children of Springfield and Southwest Missouri that we continue to work steadily to have a Child Advocacy Center open as soon as we possibly can. It is very important that we have in one year's time been able to identify and hire a competent executive director. The sooner we can get permanent housing and the equipment that we know we need, the sooner our needy children can be well served. I am very happy to work with this board on behalf of Bishop John Leibrecht."
"By Missouri Statute, Division of Family Services investigates all Child Abuse/ Neglect hot line reports. In order to do our job, we need the assistance of a variety of agencies, including law enforcement, juvenile office, etc ... The availability of a childfriendly facility where all of the agencies can come together to work for the good of the child would certainly enhance all of our jobs and make this a less traumatic experience for children we serve."
Ms. Kate Baldi Social Service Supervisor Missouri Department of Social Services
"Having served thirty years in public safety and as a board member of the Family Violence Center, I can assure you that the need to establish an advocacy center for the children of our region is real and on-going. Approximately 70%-80% of the children accompanying the mothers who seek refuge at family violence shelters have also been victims of abuse. I can personally attest that child abuse has existed prior to and throughout my years of public service. I think it is reasonable to conclude that this type of crime will continue long into our future. The history and analysis of domestic violence issues continue to illustrate the importance of intervention as the key to release from the pain and
suffering of the victims. The follow-up care is equally important. The Child Advocacy Center Board of Directors has developed a mission toward that intervention and a collaborative effort to protect the most precious resource of humankind ... our children."
John M. Brooks Advisory Board Member of Child Advocacy Center"As a board member, and as Chairman of the Health Collaborative of the Community Task Force, Advocates for a Healthy Community, I wholeheartedly support the ongoing development of the Child Advocacy Center for this area of the state."
friendly place and one that will bring together all of the agencies who deal with the child victims."
"In order to fully meet the needs of Southwest Missouri's children, it is important that the Child Advocacy Center be housed in a freestanding building that has room for growth. The Missouri Victim Center provides crisis intervention, counseling, and advocacy services to children who have been sexually abused. The staff of the Missouri Victim Center is fully supportive of the Child Advocacy Center and the enhanced services it will provide to our community."
"The new Child Advocacy Center will be a child-oriented, professional, and cooperative place for interviewing and assisting sexually abused children. I am glad to have helped bring this new facility to Springfield." "It will save children from multiple interviews they have had to face previously."
''As a Clinical Psychologist serving this community, it has long been apparent of the need for a Child Advocacy Center. Those of us who treat mental illness abuse and other aspects of behavioral medicine can best treat the illness and help the people when we can do so with the help of a multidiciplinary team. A center that provides comfort, support, professionalism and diagnostic treatment will achieve the help and support from many professionals. The community will welcome this Center."
"Being a victim of child abuse is devastating. The Center seeks to facilitate the resolution of these issues with as little trauma as possible and to support the professionals who provide direct services to the children and their families. This has long been needed in Springfield and the surrounding area. The number of cases seen during the past twelve months while being housed in a "borrowed" facility testify to this. It is meaningful that the Legislature and other branches of state government are supportive of these needed services. The community support for the Child Advocacy Center is likewise significant--the folks who give up time to attend 7:00 a.m. board meetings, who serve on sub committees with the blessing of their agencies, who help plan conferences, who approach City government on our behalf, who write grant applications. who provide pro bono legal services--the list could go on ... "
Dottie Mullikin Director, Ozarks Fighting Back"Our community has recently become committed to the concept of a Child Advocacy Center. We are pledged both as professionals within the justice system and as members of the community to provide comprehensive care for child victims of sexual abuse. By combining the services of legal, medical, and social services, we hope to avoid much duplication and increase the quality of treatment of child victims. In order to accomplish these goals, state of the art equipment is required if we are to professionally conduct Sexual Abuse Forensic Exams. In addition, we have a great need for a permanent facility for the Child Advocacy Center. We desire to establish both a child
"As the Superintendent for Springfield Public Schools, which has an enrollment of 24,600 students, I am well aware of the immediate need for funds to provide permanent housing and appropriate equipment for the Child Advocacy Center. As a member of the Board of Directors of CAC, I have been pleased with the community support demonstrated, which is a direct result of the increasing awareness of the growing child advocacy needs in this community. I encourage our area legislators to support the use of a portion of state funding for this effort."
Arnold J. Greve, Ed.D. Superintendent, Springfield Public SchoolsNEW INITIATIVE TO COMBAT OVERDOSE
FATALITIES IN GREENE COUNTY
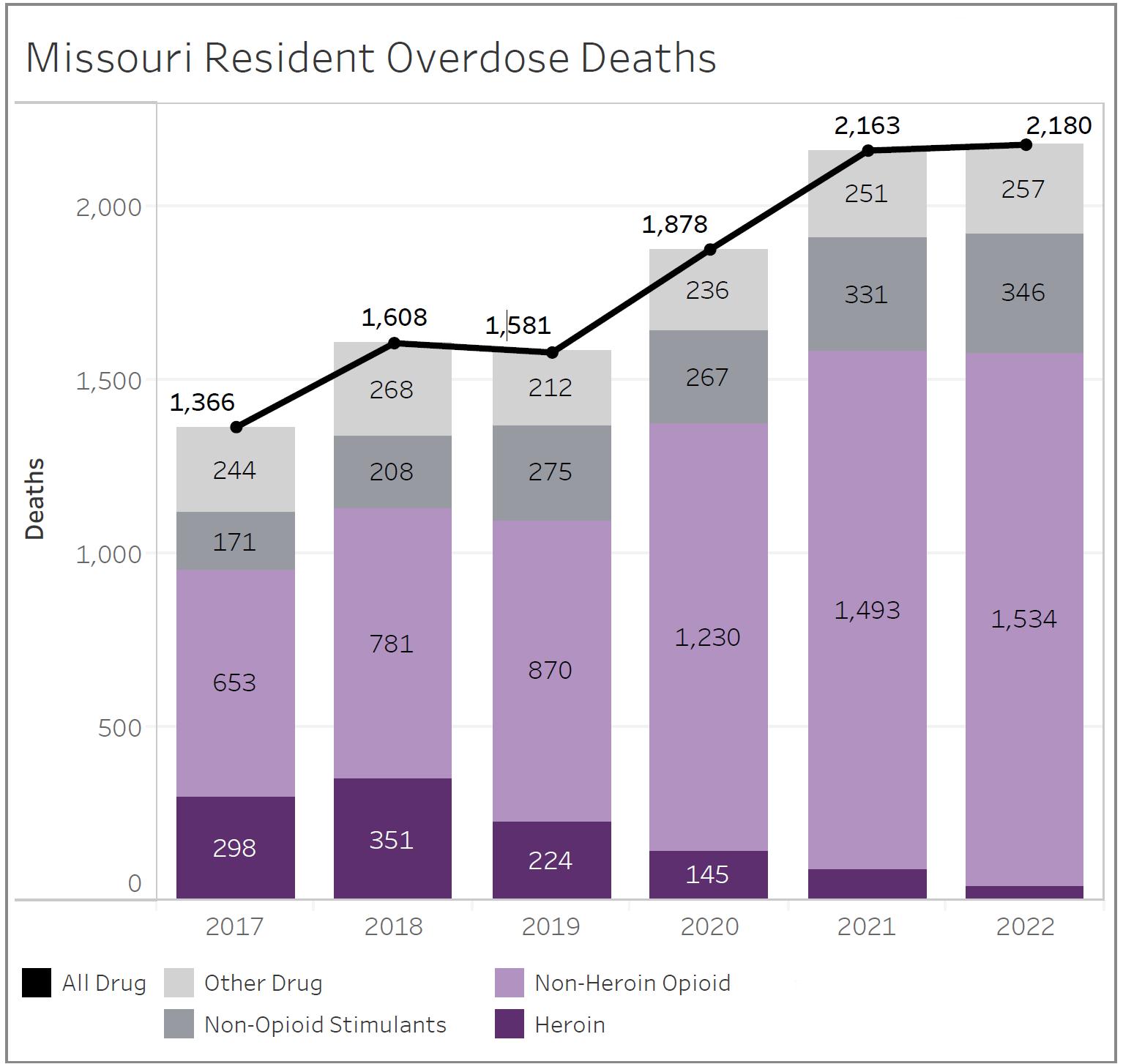
by Nancy Yoon, MD, MPHThe opioid epidemic has become a crisis in Missouri and nation-wide, with opioid-related deaths multiplying. Addiction can impact anyone, regardless of who they are, who they know, where they live, or how much money they make. In 2020, Missouri ranked 32nd in the nation for drug overdose death rates. There

were 1,386 drug overdose deaths; 142 of these were in the DHSS Southwest Region. This represents a 21% increase statewide and 15% increase in Southwest Missouri compared to 2019. Approximately 3/4 of these deaths involved opioids – an increase statewide by 30%. Among adults aged 18-44 in Missouri, drug overdose is the leading cause of death, and more than 70% of all drug overdose deaths in the state involve opioids. The opioid class of drugs includes heroin, fentanyl, methadone, morphine, oxycodone and many other prescription and non-prescription pain relievers.
The 2022 Springfield Community Health Needs Assessment identified substance use as a priority due to the prevalence of substance use disorders and drug poisoning mortality in our community. To decrease these concerning trends, multiple interventions at different levels are needed. The Overdose Fatality Review (OFR) Board is one strategy of the Community Health Improvement Plan (CHIP). Participants of the board will include representatives from public health, coroner/medical examiner, medical and health

care staff, emergency medical services, behavioral health, police and fire departments, sheriff’s department, prosecutor’s office, and the treatment court.
What are the goals of OFRs?
The primary goals of OFRs in local communities are to better understand the context of these deaths and to take action to prevent future deaths, as well as drug misuse and nonfatal overdoses. This is accomplished through:
• Recognizing and addressing gaps and barriers in services.
• Identifying underlying causes of substance use disorders.
• Determining prevention strategies targeting opioids and other substances.
• Developing recommendations for policy and program changes at local and state levels.
• Building a community of multi-disciplinary partners to collaborate across public health, healthcare and public safety agencies.
What is the review process?
An OFR is a systematic process used to examine the underlying causes of overdose fatalities in real time and problem solve. This process includes:
• In-depth case reviews shared by multi-disciplinary partners.
• Timely information sharing and dissemination of findings.
• Identification of risk and protective factors.
• Identification of trends, gaps, and deficits within and across the already existing programs and systems designed to prevent and reduce overdose.
• Actionable recommendations to strengthen these programs and systems.
In the American Medical Association’s 2023 Overdose Epidemic Report, all stakeholders are encouraged to come together to help reverse the national epidemic. Harm reduction is a key pillar in the U.S. Department of Health and Human Services' Overdose Prevention Strategy and is part of a comprehensive prevention strategy and the continuum of care. These approaches have proven to prevent death, injury, disease, overdose, and substance misuse. One component of harm reduction is the distribution of opioid overdose
reversal medications (e.g., naloxone) to individuals at risk of overdose, or to those who are likely to respond to an overdose. Physicians are urged to educate patients on naloxone and prescribe to patients at risk of overdose.
To decrease barriers to access, naloxone is available at various sites in the community at no charge. The fire department has also been providing leave-behind kits at the homes of people who have had an overdose. Agencies can contact the health department’s Community Health Advocates (advocate@springfieldmo.gov or 417-864-2029) with questions about naloxone, or to get naloxone training for your business. Requests for nalaxone can also be made at getmonaloxone.com.
According to the American Society of Addiction Medicine, addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. Prevention efforts and treatment approaches can be as successful as those for other chronic diseases. Clear, non-stigmatizing language is critically important in communicating current understandings of disease, prognosis, and treatment options to patients, the public, policy makers, media, and others. Stigma is often faced by people who have substance use disorders. These include labeling, negative beliefs and discrimination. Stigma is often rooted in the belief that addiction is a personal choice, due to a lack of and individual’s lack of willpower and moral failing. This belief neglects the acknowledgement of the systemic barriers
that make it difficult to access treatment and care. Experiencing stigma can reduce the willingness of people with SUD to seek treatment. It can also cause negative perceptions and biases among providers, which can impact the care they provide.
One way to reduce addiction stigma is to use nonstigmatizing language when addressing and referring to people with SUD. Person-first language is a way to remove language that equates a person with their condition or has negative connotations. For example, instead of using terms like “addict, user or substance/drug abuser,” a way to use person-first language would be to refer to them as a “person with opioid or substance use disorder.” By being mindful of the language we use, we can reduce the burden of stigma, improve access to healthcare for people with substance use disorders, and save lives.
Additional actions that can be taken to remove barriers and increase access to evidence-based care are listed in the AMA’s Overdose Epidemic Report (https://end-overdose-epidemic.org) and in the Department of Health & Human Services Overdose Prevention Strategy (https://www.hhs.gov/overdoseprevention/).
Resources:
National Academies of Sciences, Engineering, and Medicine. 2016. Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. Washington, DC: The National Academies Press. https://doi.org/10.17226/23442.
The Addictionary. The Recovery Research Institute developed a glossary of over 200 top addiction-related words defined, to help medical professionals and the general public modify their language about addiction: https://www.recoveryanswers.org/addiction-ary/ Harm Reduction, Naloxone distribution, Trainings: https:// time2actmissouri.com/ getmonaloxone.com
American Society of Addiction Medicine: https://www.asam.org/qualitycare/definition-of-addiction
https://www.hopkinsmedicine.org/stigma-of-addiction
https://www.shatterproof.org/our-work/ending-addiction-stigma 988 Suicide and Crisis Lifeline (988lifeline.org): The 988 Suicide & Crisis Lifeline provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week, across the United States.
Revive417.com: Revive is an app designed to prevent overdose deaths which provides step-by-step rescue instructions to follow when someone 's experiencing an opioid overdose. The app also features information about where to access naloxone in Greene County, Good Samaritan laws, information about treatment and recovery services and more.
https://www.samhsa.gov/find-help/harm-reduction
GCMSA FUN AT THE "NIGHT AT THE MUSEUM"
by Barbara Hover, co-president GCMSA
Once again, physicians and their families enjoyed a night of fun and fellowship at the Physician Family Night at the Museum. If you haven’t been there recently, the Discovery Center has a number of new exhibits including a state of the art dinosaur exhibit. You could stroll through the inner workings of an eyeball, play golf, and even ride the HighWire bike. The opportunity to visit all the exhibits at the museum after hours is a real treat. It allows handson exploration of the sciences and is fun for all ages. If you missed this year’s event, make sure you join us next year. Children friendly food and cookie decorating was part of the festivities. This was our 6th celebration at the Discovery Center and everyone who attended had a great time.
This event is held as part of our Taking Care of Our Own Project which focuses on physician wellness. Family oriented activities and socializing with others who understand the stress of the profession is seen as a way to fight against physician burnout. We wish to thank Ferrell Duncan Clinic Foundation and Mercy for their continued efforts in helping us to address this issue for community physicians.





















































It’s our turn to care for

ANOTHER SUCCESSFUL CRAP!
by John Trombold, MD, FACS, FASCRS Cox Health15 years ago, surgeons at CoxHealth realized an increase in patients struggling to obtain a needed colonoscopy. Colorectal Cancer (CRC) screening clearly decreases not only the chances of developing CRC but also detects cancers that already exist at an earlier stage.
Unfortunately, many of the highest risk patients-- those with concerning personal or family history, and those with concerning bowel symptoms-- were unable to obtain the recommended colonoscopy. Frequently, those patients are either uninsured, underinsured or their needs fall outside of the typical “covered” recommendations. For instance, a patient’s brother had colon cancer and colonoscopies are recommended every 3-5 years or a 41 year old has rectal bleeding but no evidence of an anorectal source on exam, they clearly need colonoscopy but are not able to afford it.
Partnering with CoxHeath and the CoxHealth Foundation, surgeons and gastroenterologists developed a novel program called the Colo Rectal Awarness Program. Those patients identified by physicians are referred and their situation is reviewed. If eligible, CoxHealth provides the colonoscopy “atcost” (around $1,800) and the performing endoscopist submits no charges.

In 2010, the first Colo-Rectal Awareness Party (aka CRAP) raised over $23,000. As CRAP grew, more space was required and since 2015 the Spring event occurs at White River Conference Room, typically during Colon Cancer Awareness month. Despite not



being able to have the traditional event during the COVID-19 pandemic, “virtual events” continued to raise money, except in 2020.

On Friday March 1, 2024, the 14th CRAP event brought together over 400 people and raised nearly $150,000! Since its creation, CRAP has raised nearly $950,000 and provided over 700 colonoscopies to those patients with the greatest need. If patients need assistance, they can contact the CoxHealth Foundation at 417-269-7109 or to donate in support of the program you can give online at https://www. coxhealthfoundation.com/to-give/donate-now/.

DECODING ADHD: A SILENT COMORBIDITY IN CLINICAL PRACTICE
by Amit Jagtiani, MD Child and Adolescent Psychiatrist, Burrell Behavioral Health, Springfield, MOAttention-Deficit/Hyperactivity Disorder (ADHD) has long been perceived primarily as a childhood ailment. However, its impact extends far beyond youth, persisting into adulthood for a substantial number of individuals. This neurodevelopmental condition, characterized by inattention, hyperactivity, impulsivity, and organizational difficulties, permeates multiple facets of life. Often overlooked or misinterpreted in clinical practice, ADHD emerges as a silent comorbidity, significantly influencing overall health and well-being.
The Prevalence of ADHD Across Ages
Research based on national data between 2017 and 2022 reveals an estimated ADHD prevalence of 10.08% to 10.47% among children and adolescents aged 4 to 17 years.1 However, the disorder doesn't confine itself to childhood; it persists in 30-60% of cases into adulthood, with an estimated prevalence of around 2.5%.2 This condition frequently intertwines with other mental health issues, such as mood disorders (50-60%), anxiety disorders (40-60%), and substance use disorders (20-40%), creating intricate diagnostic challenges due to overlapping symptoms.3
Diagnostic Challenges
Recognizing ADHD, especially in older adolescents and adults, remains a challenge due to its varied symptoms that mimic other mental health conditions. The conspicuous hyperactivity of childhood evolves into subtler traits— inattentiveness, distractibility, and poor time management— manifesting as chronic procrastination, forgetfulness, and strained relationships. This overlapping symptomatology often leads to misdiagnoses of anxiety, depression, or personality disorders in clinical settings.3
Impact on Comorbid Psychiatric Conditions
ADHD intensifies the complexities of comorbidities, complicating treatment strategies and prognoses. For instance, its coexistence with depression can exacerbate the severity of both conditions, affecting familial relationships and hindering treatment efficacy. Failure to recognize and address underlying ADHD can lead to frustration and ineffective treatments, perpetuating the cycle of difficulties.3
Impact of ADHD on Physical Health
While ADHD is primarily known for its cognitive and behavioral symptoms, its ramifications extend beyond mental health, significantly affecting physical well-being.
1. Sleep Disorders: Individuals with ADHD commonly experience sleep disturbances, such as insomnia or restless sleep. Poor sleep quality can lead to chronic fatigue, impacting overall physical health and cognitive function.4

2. Unhealthy Lifestyle Habits: Impulsivity and difficulty with executive functioning often lead to challenges in maintaining healthy habits. Poor dietary choices, irregular eating patterns, and a sedentary lifestyle are frequently observed in individuals with ADHD, contributing to obesity, cardiovascular issues, and metabolic disorders.5
3. Increased Risk of Accidents and Injuries: Impulsivity and inattention increase the likelihood of accidents and injuries. This propensity for risk-taking behaviors can result in physical harm, ranging from minor accidents to more severe injuries.6
4. Chronic Stress and Its Effects: Managing the symptoms of ADHD, coupled with societal challenges and stigma, can lead to chronic stress. Prolonged stress negatively impacts the immune system, making individuals more susceptible to illnesses.7
5. Impact on Chronic Health Conditions: ADHD often coexists with chronic health issues such as migraines, gastrointestinal problems, and chronic pain conditions. The interplay between ADHD symptoms and these conditions can exacerbate each other, leading to increased discomfort and decreased quality of life.8
Addressing ADHD's impact on physical health is crucial in comprehensive patient care. Interventions aimed at managing ADHD symptoms, promoting healthy lifestyle modifications, and addressing associated health concerns holistically are imperative for improving overall health outcomes. Highlighting these physical health aspects emphasizes the need for a multi-dimensional approach in managing ADHD, focusing not only on cognitive and behavioral aspects but also on physical well-being.
Implications for Clinical Practice
1. Enhanced Screening Protocols: Implementing comprehensive screening tools and assessments that encompass ADHD symptoms across different age groups can aid in early detection.
2. Integrated Treatment Approaches: Incorporating ADHD assessments into routine psychiatric evaluations can facilitate more holistic treatment plans.
3. Educating Healthcare Providers: Continuous education and training for healthcare professionals regarding the nuances of ADHD across the lifespan are pivotal in improving recognition and diagnosis.
Addressing the Stigma
Overcoming the stigma associated with ADHD is crucial. Perception of ADHD as merely a childhood disorder often prevents adults from seeking help or clinicians from considering it as a potential comorbidity. Normalizing discussions around ADHD across all age groups is essential in mitigating this stigma.9
Conclusion
ADHD, as a silent comorbidity, poses significant challenges in clinical practice. Recognizing its presence and understanding its impact on overall health is pivotal. By implementing improved screening measures, integrating ADHD evaluations into routine assessments, and fostering awareness, clinicians can address this silent comorbidity effectively, ultimately enhancing patient care and outcomes.
For further exploration and insight into managing ADHD, consider consulting resources such as Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD), The American Academy of Child and Adolescent Psychiatry (AACAP), The National Institute of Mental Health (NIMH), and The Attention Deficit Disorder Association (ADDA).
References:
1. Li Y, Yan X, Li Q, Li Q, Xu G, Lu J, Yang W. Prevalence and Trends in Diagnosed

ADHD Among US Children and Adolescents, 2017-2022. JAMA Netw Open. 2023 Oct 2;6(10):e2336872. doi: 10.1001/jamanetworkopen.2023.36872.
2. Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attentiondeficit hyperactivity disorder: A global systematic review and meta-analysis. J Glob Health. 2021;11:04009. Published 2021 Feb 11. doi:10.7189/jogh.11.04009
3. Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. 2017 Aug 22;17(1):302. doi: 10.1186/s12888-017-1463-3.
4. Wajszilber D, Santiseban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep. 2018 Dec 14;10:453-480. doi: 10.2147/NSS.S163074.
5. Cortese S. The Association between ADHD and Obesity: Intriguing, Progressively More Investigated, but Still Puzzling. Brain Sci. 2019;9(10):256. Published 2019 Sep 27. doi:10.3390/brainsci9100256
6. Barkley RA. Health problems and related impairments in children and adults with ADHD. In Barkley RA. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th Ed). New York, NY: Guilford Press; 2015. pp. 267–313.
7. Saccaro LF, Schilliger Z, Perroud N, Piguet C. Inflammation, Anxiety, and Stress in Attention-Deficit/Hyperactivity Disorder. Biomedicines. 2021 Sep 24;9(10):1313. doi: 10.3390/biomedicines9101313.
8. Battison EAJ, Brown PCM, Holley AL, Wilson AC. Associations between Chronic Pain and Attention-Deficit Hyperactivity Disorder (ADHD) in Youth: A Scoping Review. Children (Basel). 2023 Jan 11;10(1):142. doi: 10.3390/children10010142.
9. Mueller AK, Fuermaier AB, Koerts J, Tucha L. Stigma in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2012 Sep;4(3):101-14. doi: 10.1007/s12402-012-0085-3. Epub 2012 Jul 8.





Champions Committed to KIDS was formed with one purpose – to give KIDS who are fighting chronic illnesses or a disability a chance to feel what it’s like to be part of an athletic team while building lifelong friendships. Champions Committed to KIDS gives hope and inspiration to the KIDS and their parents. Athletes and coaches witness the increase in selfconfidence and self-esteem in our KIDS. Not only do the KIDS show confidence when they are with the team, but it carries into their daily routine. CCK is committed to helping your child and making them feel like a champion. We believe that children and the athletes can learn life lessons from each other. We want them to draw inspiration, to never quit, to never give up, to be driven by passion, to be empowered by being part of a team, to know that they are in this fight together, to have hope and share in building character in sports and in life. We want them to live the life of a CHAMPION!




Both athlete and child will learn from and inspire each other, creating a greater feeling of purpose that will impact our community and develop future leaders. The child will have the chance to be a part of a sports team and in return, the athletes will discover the benefits of helping others. To develop champions by creating a special bond between children with medical conditions and/or disabilities with local athletic teams as they inspire each other.
ONE KID, ONE TEAM, ONE POWERFUL BOND ChampionsCommittedToKids.com
professional
directory
Mission Statement
Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
3850 S. National Ave, Suite 705 Springfield, MO 65807 (Located inside Hulston Cancer Building-7th floor)
1240 E. Independence Springfield, MO 65804 Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672
PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care)
2200 E. Cleveland Ave
Monett, MO 65708
Phone: 417-888-0858 • Fax: 417-889-0476
To Advertise in this directory call Jean Harmison at the Society office: 417-887-1017.
Please Note: Changes to ads will be made quarterly and must be submitted in writing. H Denotes GCMS Membership “A” Denotes GCMS Applicant
GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq.
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine
www.ascentdpc.com 417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
Eye Surgery/Ophthalmology
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H
Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H
Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804 Phone 417-887-1965 • Fax 417-887-6499
417eyecare.com
Eye Surgery/Ophthalmology
MATTAX • NEU • PRATER EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H
American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD 1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
COXHEALTH FAMILY MEDICINE RESIDENCY FAMILY MEDICAL CARE CENTER
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AmericAn BoArd of fAmily medicine
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Katie Davenport-Kabonic, DO
Michael Kabonic, DO Jessica Standeford, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
VANESSA MCCONNELL, APRN, DNP, FNP-C
1135 E. Lakewood, Suite 112 Springfield, MO 65810
Located inside
Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500
Fax 883-8964
or toll free 877-966-2607
Monday-Thursday 8am-4:30pm
Friday 8am-12pm
Internal Medicine
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H
Board Certified in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD
Board Certified in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA
COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD
Board Certified in Internal Medicinee
2115 S. Fremont, Suite 2300 Springfield, MO 65804
Phone 417-820-5600
Fax 417-820-5606
Urology
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD
American Board of Urology
MARK J. WALTERSKIRCHEN, MD, FACS
American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Springfield, MO 65804
Internal Medicine
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology

SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100
www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine American Board of Nephrology
Neurosurgery
SPRINGFIELD
NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth
Jared Neuroscience
West Tower • 3801 S National, Ste 700 Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD KELLY OWN, MD
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
BLAKE MARTIN, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
BILL HAMPTON, ANP-BC
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
Obstetrics/Gynecology
COXHEALTH
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
Obstetrics/Gynecology
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology
909 E. Montclair, Suite 120 Springfield, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
Oncology/Hematology
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic
3850 S. National, Ste. 600 Springfield, Missouri 65807
Monett Clinic
802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880
Fax 882-7843
Visit our website: www.ohaclinic.com
Rheumatology
417 RHEUMATOLOGY
Independent rheumatology care and infusion services
DAVID TRUE, DO, FACR H Board Certified in Internal Medicine and Rheumatology by American Board of Internal Medicine
Phone 417-501-2644
Fax 877-540-0429
909 E. Republic Rd., Building D200 Springfield, MO 65807 www.417ra.com
Otolaryngology
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
A. DANIEL PINHEIRO, MD, PhD, FACS H
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP
Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750
Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
Plastic Surgery
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS
American Board of Facial Plastic & Reconstructive Surgery
American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
Psychiatry
JAMES E. BRIGHT, MD H
Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804
CONNECTED.
We believe when we work together, big change happens. Families get healthier. Communities grow stronger. Lives change. Right now, side by side, our providers are shaping our future –strengthening it and making it a little bit brighter for everyone.


When neighbors help neighbors, it makes all the difference.
chAnge Service requeSted

