by Minh-Thu Le, MD
Hello to another edition of YOUR Greene County Medical Journal! We are so excited to be celebrating 150 years of GCMS in the next year and wanted to unveil a new graphic that you’ll be seeing throughout next year on media releases, website, and in this journal! We hope it reminds you of how vital we physicians are in the life and health of our community.
There are many ways to show your involvement in GCMS. One is participation in the many events that we have curated just for physicians and their families. (Also, save the dates to the social and CME events coming up in November!) As Physician Family Day at the Zoo wrapped up, we saw so many new and familiar faces come through and we hope you can pick out yours in the several dedicated pages of pictures in this journal. Another is by mentoring and encouraging the dozens of MD and DO students in our area training. We are so fortunate that Kenlee Jonas, M4, and her fellow colleagues from the MU School of Medicine worked on an original paper that is published here on melanoma mortality in our rural communities. It’s these articles that enlighten our readership and allow us to grow and make our community stronger and healthier.
The SGCHD, our local health department, celebrated a milestone of 150 years this past year as well. Dr. Nancy Yoon chronicles its history in these pages. A joint CME event with the SGCHD will be occurring soon. Please keep your calendar open for that!
We are starting a a new journal series on devices that our colleagues utilize in their daily jobs. Starting off, Dr. Jayaprabha LaFontaine reviews transcranial magnetic stimulation (TMS) in the treatment of depression and looks at a particular device that Burrell Behavioral Health uses at their clinic called Neurostar.
Two more physicians that serve on our executive board with their time and intelligence are highlighted in the President’s
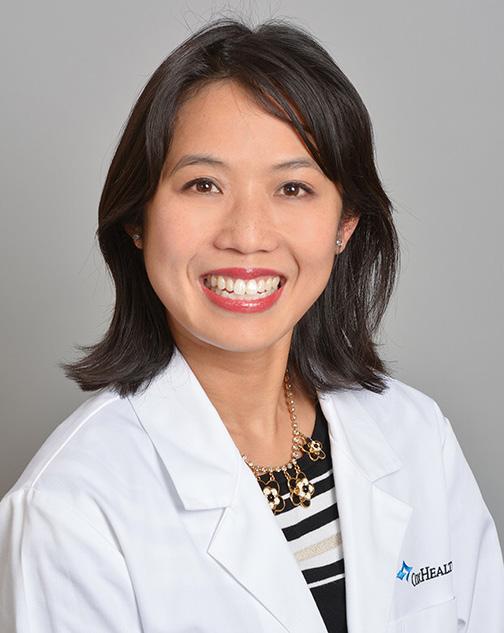
Page: Dr. Melissa Gaines and Dr. Vu Le. Involvement also means physical service to GMCS and we appreciate them for that! As past president, I encourage all of you to consider joining for our board if soonnominated (we accept self-nominations)!
Being informed in policies that directly affect our practices and patients is another way to stay engaged and at our legislative forum on October 17th, you will be able to ask the current candidates about what issues they would be willing to tackle while in office. From the weight of prior authorizations and appeals to the ever decreasing practice reimbursements from payors to “scope creep” and other important issues we physicians face from increased government regulatory bodies, this is where our concerns may be voiced. Make your vote count this election cycle by staying informed.
Forvis/Mazars has a 4-week physician financial health and readiness course in October as well. This is totally free and informative. This will be held on both the Cox and Mercy Campuses and starts with medical students and residents October 1st. We don’t learn about this in medical school, yet we have the means to make our money work for us and not the opposite. Please plan to join us for that!
Two final ways to get and stay involved in GCMS is by membership and now charitable giving to the foundation! It’s tax deductible and a great way to give back in programs that highlight the importance physicians play in the health of our community (Care to Learn and the Child Advocacy Center), and isn’t that what we are about? I think I heard a resounding, “YES!”
We appreciate the sponsors that allow us to bring this journal to you. Membership dues are not enough to keep this journal running, so please support them as they support us!

by James Rogers, MD
We are continuing our introductions to your Greene County Medical Society Council members. Please get to know Dr. Gaines and Dr. Le as we invite you to create a “physician community” in Greene County.

Dr. Melissa Gaines, MD, FACP
Growing up in the rural Midwest, Riverton Kansas, stability and continuity of location and purpose was second nature to Dr. Gaines' family. Growing up with two younger twin brothers and father working in the industrial printing industry, it was her mother's career as a nurse that greatly influenced her personal career path. Watching her mother migrate from hospital and clinic care to home health and hospice care helped clearly define the importance of relationships in addition to academic healing and care. She was able to participate in creating a Pittsburg Care Clinic for underserved patients that still exists today.
After attending Pittsburg State University with a biology major and music minor, she then attended the first two years at the University of Kansas Medical School in Kansas City. She then completed her final two years at the University of Kansas Medical School in Wichita to complete her medical training and then completed internal medicine residency. After serving a chief residency term, she transitioned over 9 years into a faculty appointment with responsibilities in geriatric and hospice medicine.
Her husband, a real estate investor, and their "baby," a miniature dachshund named Winnie, made the trek to Springfield eight years ago to join the geriatric practice at Cox Health and later becoming the Director of Palliative Care and Hospice at Cox Health. Her hobbies include: exercise, reading, and traveling. Her time in Springfield also finds her serving on the board of the Hospice Foundation of the Ozarks (HFO) as its president.
Her personal goals for the next few years include a focus on obtaining Fellowship in the American Academy of Hospice and Palliative Medicine and launch End of Life Care education through HFO.
She believes that GCMS focus should include being a
consistent, trusted voice for health information and stronger voice for the health of our community. "We should have a special emphasis for student and young doctors in training. We must continue to strengthen the commitment to balancing science, healing, and humanity."


Dr. Vu Le, MD, Psychiatry
Director of Telehealth Services, VISN 23, Veterans Administration
Born in Vietnam, his family started a difficult and dangerous trek to the United States when he was only two years old. That path progressed through Thailand, threatened by pirates, and settling into a refugee camp in the Philippines. From there, the family connected with a sponsor to allow them to migrate to the United States. Dr. Johnson, a Fort Smith Arkansas dentist, acted as their sponsor and brought them "home."
From school in Fort Smith to his senior year at Arkansas School for Mathematics and Sciences in Hot Springs, he then went to Tulsa for college and University of Arkansas for the Medical Sciences for medical school. Afterwards, he completed his psychiatry training in Kansas City and then served three years in the Air Force. While in commissioned officer Air Force training in medical school, he met his future wife, Minh-Thu, a Springfield native, and then a natural migration to Springfield to be close to both families.
His choice of profession evolved around his ability to relate to others and an outgoing, honest persona. These talents led him to training in psychiatry and then into current administrative leadership.
His highly compatible hobbies are gardening, cooking, and hosting gatherings with friends and family. With these skills, he excels at making guests welcome.
Personal goals are to enhance his relationships with family and friends. His advice for Green County Medical Society is to expand beyond the "county" to include the area and region, and build strong community collaborations for the future.
Be on the lookout for these new DO students doing their clinical rotations from Kansas City University and A.T. Still in Kirskville, MO! Several have allowed us to tell you a little more about them below!
Henry Anderson
John Bohon
Amy Giemza
Laura Loyet
Madyson Lytton
Abigail Reese
Andrew Mielcuszny
Connor English
Jenny Funk
Megan Watson
Brett Stinogel
Andrew Payne
Adam Webb
Alex Dean
Alexandru Tunaru


Paige DeRemer-Young
Christian Troas
Jason Doheny
Joshua Huseby
Kaitlyn Sbarro
Kristie Chau
Ruchit Shah
Seth Rowling
Sukh Kaur
Abigail Baker
Jared Ezzell
Heleena Haberer
Philip Haynos
Nelson Jourdan
Karina Lucar Canchari
Richard Morsovillo
Prapti Patel

Mathuri Morgan - Hi! My name is Mathuri Morgan, and I’m originally from Howard County, Maryland. I studied biology at Penn State University and am currently in my third year of medical school at Kansas City University on the Kansas City campus. Alongside my medical degree, I’m also pursuing an MPH in environmental and occupational health, driven by a deep passion for environmental health and sustainability. My goal is to integrate my understanding of how our environment and workplaces impact health into my future practice to enhance patient care. Outside of my studies, I enjoy creating art, spending time with my two cats, and traveling—my solo trip to Japan after my second year was an incredible experience, and I hope to continue exploring the world when I can.
Gabrielle Davis - While I am originally from King, North Carolina, this is the start of my 3rd year calling Missouri home. A fun fact about me is that I’ve served four years in national volunteer service via AmeriCorps programs. In my off hours, I enjoy hiking, baking, music, and movies!

Liam Bloebaum - Hello. I am a thirdyear student doctor from ATSU in Kirksville. I was born in raised in St. Peters, MO, just outside of St. Louis. My undergraduate and gap years were spent in Kansas City, where I solidified my passion for medicine. Outside of academics, I'm an avid rock climber and guitarist!

Peter Khoury - Born and raised in Allentown, PA, I am a 3rd year medical student at Kansas City University. I currently serve on the American Osteopathic Association’s Bureau on Federal Health Programs (BFHP), advising the organization on regulatory and legislative matters. Prior to medical school, I spent ~10 years as a management consultant in the health care industry, where I focused on mergers and acquisitions, forensic investigations, legislative affairs, and strategy & operations.

Justin Hajicek -My name is Justin Hajicek and I am a 4th year medical student at A.T. Still University Kirksville College of Osteopathic Medicine. I grew up in Columbia, MO and feel grateful for the opportunity to complete my clinical rotations in Springfield. I studied biomedical engineering and medical missions as an undergraduate student. As a medical student, I find the intersection of biomechanics andmusculoskeletal medicine particularly exciting! In my spare time, I like to play tennis with my wife and take my dog for walks on the trail.
Zenobia Tucker - As the daughter of a six generation farming family north of Willard, I am happy to call Missouri home! After many exciting years of globe-trotting and working in the film and TV industry of Los Angeles, I returned to my original pursuit of a medical degree with Kansas City University and am now starting my third year rotating in Springfield. Having never lost my love of travel, I was accepted into KCU's Global Health Honors Track and am looking forward to a Kenya trip this fall to complete my Family Med rotation.

by Jayaprabha LaFontaine, MD, MPH, Southwest Regional Medical Director, Burrell Behavioral Health
The treatment of depression has long been associated with anti-depressants, and more recently, other classes of medications. The field of interventional psychiatry is not new, as electroconvulsive therapy has been used for over a century. The controversy surrounding ECT, though it has been proven to be the most effective treatment for depression, is an invasive procedure requiring the subject to have general anesthesia. Furthermore, it is associated with undesirable cognitive effects such as memory loss, confusion, headaches, and difficulty concentrating. The treatment of ECT has also had to endure the stigma surrounding the use of the method, made worse through depictions in media as a brutal, inhumane, punitive method of treating mental illness.
In 1881, the English physicist discovered that a magnetic field could be generated by a pulsing electrical current. Faraday used a coil held over a subject’s head to stimulate specific areas of the brain and in turn create physiological or behavioral effects in the subject. Almost a 100 years later, Dr. Anthony Barker and colleagues developed the first TMS device we recognize today. He used what is now called a “Faraday coil” to move the right hand of a subject by placing the coil over the left cerebral motor strip. This is now the same method used to orient the TMS technician to guide the coil over the dorsolateral prefrontal cortex.
Anthony Barker’s new device underwent several years of research and development and in 1998 a set of safety measures were published outlining clinical and laboratory settings. Over 90 clinical trials later, with data from multiple meta-analyses, TMS was designated to be an effective treatment for treating Major Depressive Disorder by the FDA in 2008.
Since then, the application of TMS continues to be investigated for a multitude of conditions including anxiety, migraines, Alzheimer’s etc. More recently, the FDA approved the use of TMS for adolescents 15 yo and above for the treatment of Major Depressive Disorder, and also for the treatment of OCD in adults.
Why: Depressed brains are hypoactive, especially in areas that regulate emotion. There is also a decrease in activity within the networks within the brain that connect the cortex to deeper parts of the brain. Anti-depressants cross through several organ systems as well as the blood brain barrier in order to increase neurotransmitter activity in these
hypoactive areas. This can take a long time before measurable results are seen in decreasing depression.


What: TMS is the induction of an electric current to the brain cortex through a magnetic field outside of the brain. rTMS is “repetitive TMS” and is a variation where stimulation is provided in sessions of the same condition to create longterm excitation in the brain cortex. The electromagnetic induction generated by rTMS passes through the skin and skull while the patient is fully awake and alert. Neurostar Advanced Therapy Systems (hereafter referred to as Neurostar) is an FDA approved rTMS method currently in use at Burrell Behavioral Health. Sessions consist of 36 sessions, 20 min sessions, 5 days a week for 7 weeks. Patients report that it feels like light tapping on the head. The most common side effect is temporary pain or discomfort at the site of treatment which subsides after first week of treatment. Neurostar has published results that show 83% of patients reported meaningful reduction of depression symptoms. For 62% of patients, MDD was in remission. It is covered by most insurance plans.
How: A cushioned coil is positioned on the head above the prefrontal cortex, and magnetic pulses similar in strength to MRI, are rapidly delivered up to a strength of 10 hz. The intensity of the signal is based on a percentage of each individual’s resting motor threshold which is determined during initial sessions. This increases the release of neurotransmitters within these specific areas of the brain and excites networks linking different parts of the brain which have been hypoactive. This process is thought to increase the brain’s neuroplasticity.
When: TMS can be used by those who have failed one to two anti-depressants. More recently, it has been FDA approved for adolescents 15 yo and older, as well as for the treatment of OCD.
If you are interested to learn more about the rTMS program at Burrell Behavioral Health, please contact the program at 417-761-5000.
References:
1) Michael Craig Miller for Harvard Health Publications. July 26, 2012. Magnetic stimulation: a new approach to treating depression?
2) Barker AT, Jalinous R, Freeston IL: Non-invasive magnetic stimulation of human motor cortex. Lancet 1985; 1:1106–1107.
3) Horvath JC, Mathews J, Demitrack MA, Pascual-Leone A. The NeuroStar TMS device: conducting the FDA approved protocol for treatment of depression. J Vis Exp. 2010 Nov 12;(45):2345
Everyone has different financial goals and priorities, and they change and grow as you do. That’s why it’s important for me to get to know you and understand what you’re working toward. Together, we can create a personalized financial plan that fits your needs today and helps you build the tomorrow you deserve. Penney, Murray & Associates

by Kenlee Jonas, Brooke Kronk, Emily Winfrey and affiliated with the University of MissouriColumbia, School of Medicine
Abstract:
Missouri residents face higher mortality rates and decreased 5-year survival rates for those diagnosed with melanoma, despite a lower incidence rate compared to the national average. While some cases are largely due to late-stage disease at the time of diagnosis, we postulate that this relationship is primarily due to Missouri being a desert for dermatologic care. We believe the number one drive for these statistics is the high proportion of rural residents. This research project aims to understand from the patient’s perspective, the barriers they face accessing dermatologic care in rural Missouri. A cross-sectional study was administered in primary care facilities in south and southwestern Missouri. The results of the study concluded the primary challenges in accessing a dermatologist are long wait times and difficulty locating a dermatologist within the area, aligning with our hypothesis. Additionally, our study highlights inadequate patient awareness and self-assessment of skin cancer manifestations that could be contributing to the dissonance between a lower incidence rate and higher mortality rate seen in these regions. This study highlights the critical need for dermatologic care in rural areas of Missouri. Primary care physicians may be able to aid in the education of early detection and preventive strategies. However, enhanced accessibility to specialized care is essential concerning skin manifestations to improve the overall well-being of patients and their communities.
Background:
Most patients from our study reside in Taney County, Howell County, and surrounding areas. Taney County, containing a majority of the residents from the Branson research location, is home to approximately 55,000 residents. In Taney County, access to healthcare services is limited from primary care to specialized care. According to the most recent community health reports completed in 2019, about 12% of those under 65 in Taney County did not have health insurance coverage, further complicating access to care. Concerns about health behaviors in the county also arise, with approximately 21% of adults reporting no leisure-time physical activity and about 20% smoking cigarettes. These factors contribute to a high prevalence of chronic diseases, with around 33% of adults being obese and about 13% diagnosed with diabetes. Uniquely, Taney County also has a higher prevalence of elderly population at 17% higher than the national and Missouri average. With the increased age of the population, increased prevalence of poor health

behaviors, and limited access to care, Taney County faces increased risk of chronic disease and poor health outcomes, such as decreased 5-year survival rate of melanoma. Addressing these challenges requires comprehensive efforts to improve healthcare access, promote healthy behaviors, and manage diseases effectively (1, 2).
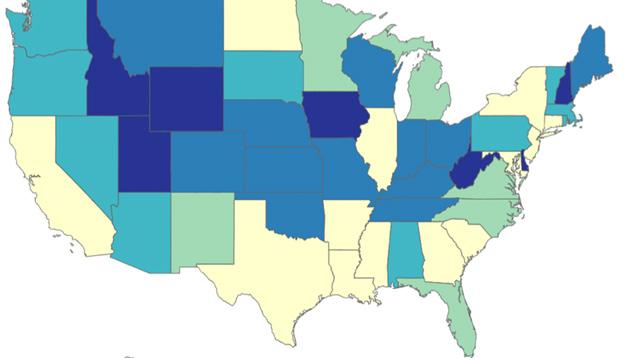
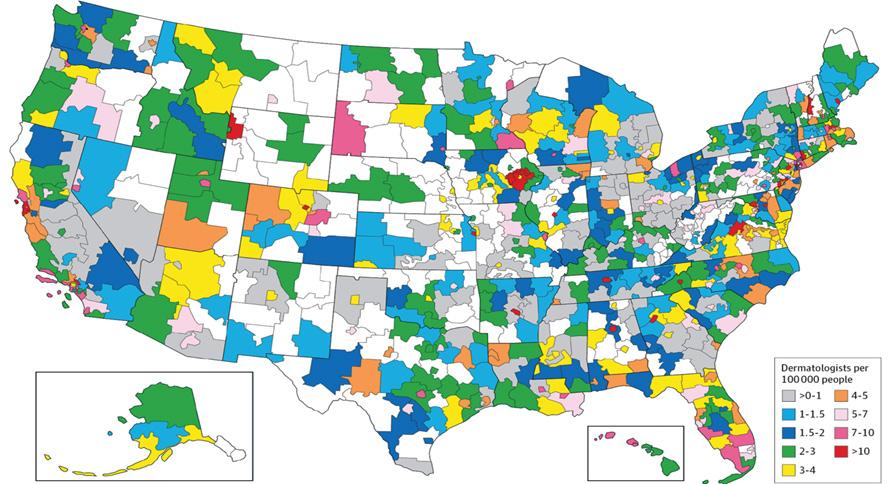
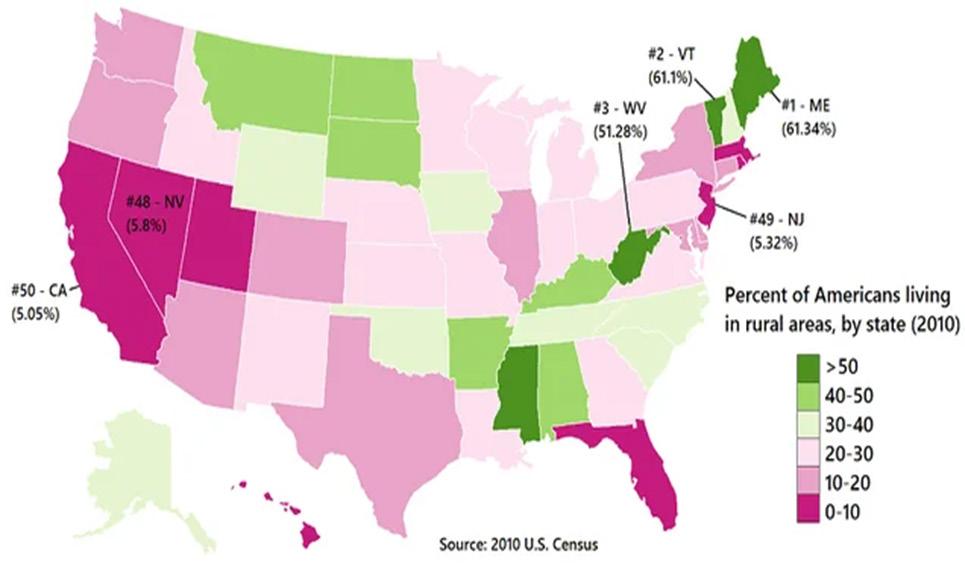
Melanoma is the third most common and the most lethal skin cancer. The survival rate for melanoma varies depending on the stage at diagnosis. In 2021, the overall 5-year survival rate for melanoma was estimated to be around 92% for all stages combined in the US, and 88.5% in Missouri. However, if detected at an early stage (localized melanoma), the 5-year survival rate is much higher, often exceeding 99%. However, metastatic melanoma or stage 4 melanoma has a poor 5-year survival rate of only 15-20%. Melanoma, while it can be lethal for those with late-stage presentations, can also be treatable with early detection and intervention (5). Missouri’s incidence is more than 20% lower than the national average rate at 18.7 vs. 22.5, 20% lower; however, Missouri’s mortality rate surpasses the national rate at 2.5 vs. 2.1, 16% higher (3). Additionally, Missouri has a higher incidence of late stage compared to the national average, 6% higher, 3.3 vs. 3.1 and a lower 5-year survival rate compared to the national average, 5.6% lower, 94.1 vs. 88.5 (3, 8, 11). This phenomenon illustrates the higher prevalence of late-stage disease likely due to the lack of dermatologic services available in these regions. A study performed on populations of North Carolina equated the distance of dermatologic providers to Breslow depth, the tool used for staging of melanoma. The median distance to the diagnosing provider was 8 miles (range, 0-386 miles). For each 1-mile increase in distance, Breslow thickness increased by 0.6% (P =.003). This demonstrates supporting evidence that rural areas lacking dermatologic providers are at an increased risk for advanced disease (4). 30.4% of Missouri’s population lives in rural areas doubling the national average rate, 30.4 vs 15. Missouri is ranked 11th in mortality due to melanoma in the US (8), despite ranking 21st economically based on Gross Domestic Product (9). Missouri’s increased proportion of rural communities contributes to the geographically imbalanced access to dermatologic care and the poor outcomes are correlated with rurality rather than poor economic status.
Geographic Distributions of Melanoma Mortality Rates, Dermatologists, and Rural USA – Trends Following Northwest to Midwest.
Cross-sectional study using a Qualtrics survey designed to assess patients' access to dermatology care, perceived barriers, as well as baseline knowledge of skin cancer within rural communities in Missouri. Specifically, the survey consisted of 18 questions, including both closedended, multiple choice, and open-ended questions. The questions were designed to gather information on (1) Access & Barriers to Dermatology Care and (2) Knowledge of Melanoma. Questions included covered topics including ease of scheduling dermatology appointments, waiting times, insurance coverage, past dermatology visits, perceived barriers, awareness of available services, and assessed knowledge about melanoma risk factors, signs, and the importance of skin cancer screenings. The survey was conducted over four months. Participants were recruited from primary care clinics across southern and southwest regions in Missouri. Participant demographics were collected, including information on age, sex, ethnicity, education level, county of residence in Missouri, and health insurance status. Patients with a known history of dermatological conditions were included to capture diverse perspectives. A survey instrument, Qualtrics, was developed based on a thorough review of existing literature on dermatology care access.
Quantitative data received were analyzed utilizing Qualtrics database using counts & percentages. Qualitative data received were documented verbatim and analyzed via Qualtrics data based on theme, if applicable. All participants provided informed consent before participating, and measures were taken to protect their confidentiality and privacy throughout the study. Data was analyzed anonymously.

Results: Introduction
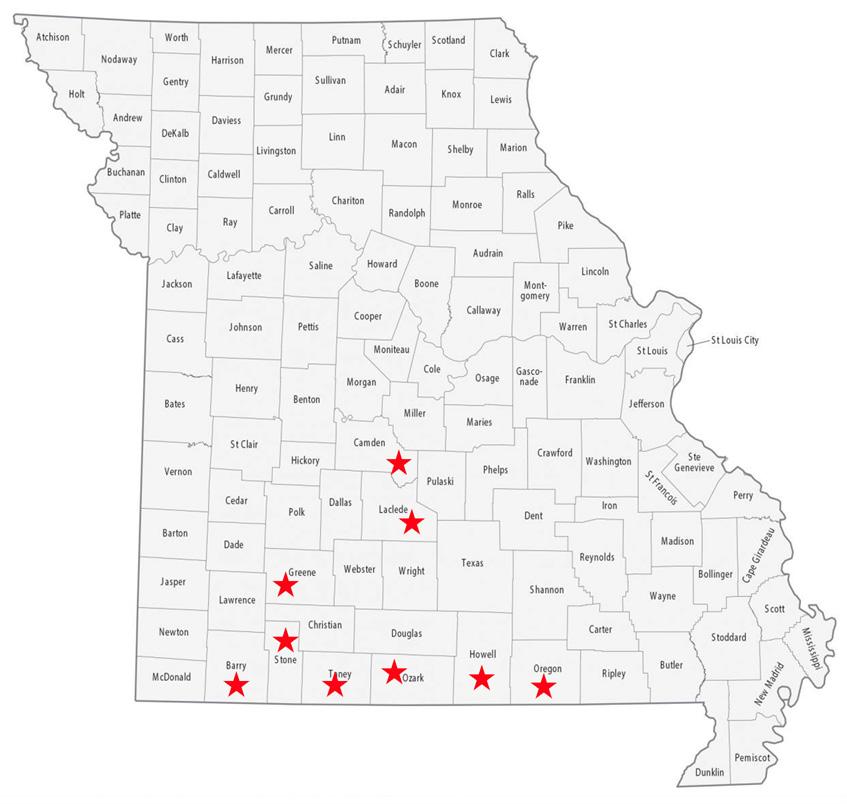
A patient survey obtained data from nine different counties. Below, we explore the data obtained from each of these three areas:
The study produced 46 patient responses across nine different counties in the southern and southwestern part of the state. Howell County accounted for most responses (20), followed by Taney (11), Stone (5), Camden (3), Oregon (2), Ozark (2), Barry (1), Greene (1), and Laclede (1) counties. Of the participants surveyed, 28% of respondents were between the ages of 25-34, followed by 13% in each age category of 18-24, 35-44, 45-54, and 55-64. Adults aged 65 and over accounted for 10.8% of responses. Female respondents made 70% of the survey responses with males accounting for the remaining 30%. White or Caucasian ethnicity respondents made up 98% of the surveyed population, followed by 1% each for Hispanic and Native American/American Indian/Alaskan populations. Over half of patients (62%) had received some sort of higher education certificate of degree, while 37% of patients had not. Most patients had health insurance (98%).
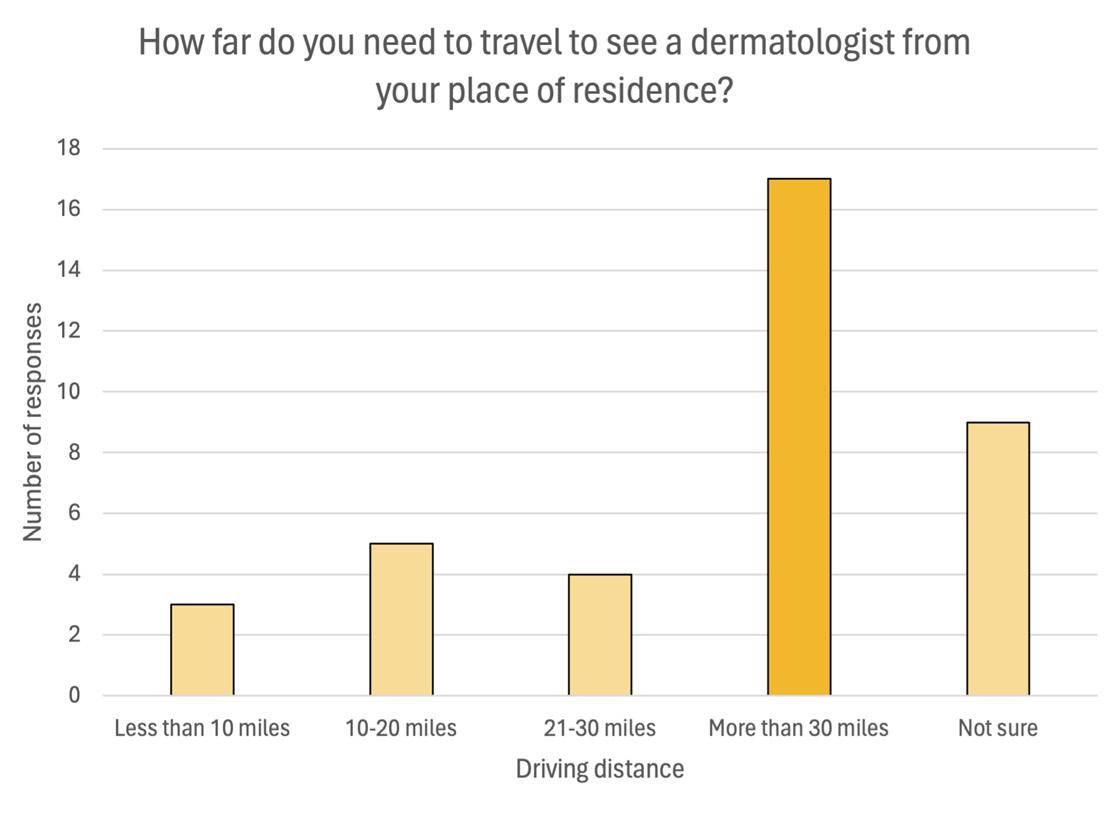
Half of respondents had previously visited a dermatologist and half had not. Over half of respondents (55%) said they must travel more than 20 miles to see a dermatologist. Patients were given an option to check all the challenges that apply to them. Of the options listed, the most consistent challenges cited by patient respondents were
long wait times, difficulty finding a dermatologist in the area, distance to travel, and prohibitive costs. Of the respondents who have seen a dermatologist in the past, 40% of them said they had to wait 1-2 months for an appointment. This was followed by respondents who had 3-6 month wait times (20%). Only 20% of patients had a wait time of less than one month. Telehealth services have been known to help allow more access to care, especially for patients who have greater distances of travel. However, despite this, only 3% of patients had ever used telehealth services for an appointment.
3. Patient Background Knowledge of Concerning Skin Findings
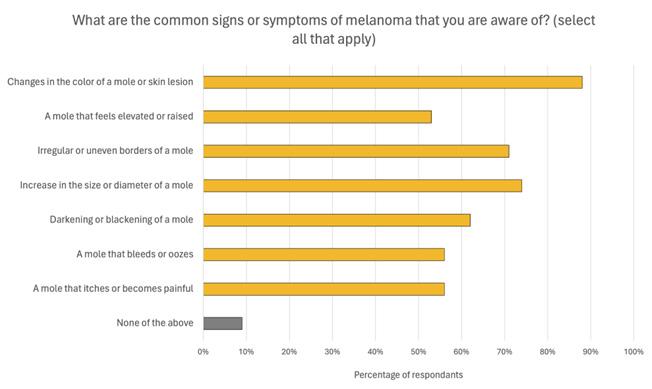
Because limited access to dermatology care can correlate with fewer people receiving proper education regarding skin care and therefore impact patient mortality and morbidity, part of the survey assessed baseline patient education about their skin health. Of respondents, 32% said that they had never received information regarding skin cancer and its warning signs. When asked about common signs and
symptoms of melanoma, a majority of patients knew to be concerned about signs such as changes in color or skin lesion (88%), increase in size or diameter of a mole (74%), and irregular or uneven borders of a mole (71%). However, only about half of patients knew that other warning signs also included moles that bleed or ooze or moles that itch or are painful. Knowledge of risk factors for melanoma were also assessed. Over 75% of respondents could correctly identify prolonged exposure to UV radiation from the sun and frequent use of tanning beds or sun lamps as risk factors for skin cancer. However, lesser-known risk factors such as weakened immune system, living in a high-altitude area, or old age could only be identified by 35%, 19%, and 51% of respondents, respectively. Also, 11% of respondents could not identify any risk factors for skin cancer.
The project made an impact in the communities it was performed in by bringing to light the major specific barriers that patients face to receiving dermatologic care. Assumptions could have been made about potential barriers including travel times and wait times. However, this had not been quantified, and other barriers were uncovered that were previously unknown before the surveys were collected. The project also made an impact by showing areas that were lacking in patient education of skin health. This provides physicians and other providers the opportunity to make changes in their practice in order to combat these discrepancies with the hope of improving patient knowledge and patient outcomes.
Discussion:
Plans to Sustain the Project
We plan to sustain the project through a few avenues: (1) Use this information we’ve learned and implement valuable insights in our future practice, such as being aware of Teledermatology and being intentional about educating our patients, (2) Continue our project through future students to continue to gather patient data to expand the geographic distribution and sample size and begin distributing resources to patients such as the CDC skin health and safety QR code (on the right) and information regarding the ABCDEs of melanoma awareness for documenting changing skin lesions, and (3) Aiding future students in connecting rural family medicine clinics with Mizzou ECHO Teledermatology to facilitate knowledge sharing and collaboration with local physicians, to improve access to specialized care in underserved areas.
Our project's limitations include a (1) a small sample size of 46 participants, (2) limited demographic diversity, consisting mostly of young, female, Caucasian individuals, the majority of whom have a high level of education and health insurance coverage, and (3) limitations regarding collecting data through a survey. These limitations could
lead to selection bias, response bias, issues with causality and reliability, respectively.
Our study illustrates that improving access to dermatological care for rural Missouri residents is important for improving survival rates of melanoma. Challenges such as long wait times and difficulty locating dermatologists underscore the need for enhanced access to specialized care in these areas. Strategies such as expanding the use of Dermatology ECHO, Teledermatology, services can help address these challenges and improve patient outcomes. In a study performed on the efficacy of Teledermatology, 53% of the skin lesions could be triaged, given a diagnostic hypothesis and treatment suggestions directed to the patients’ primary care physicians, referrals for in-person dermatologist were avoided in 57% of the cases. Another benefit was the option to refer the patients to the biopsy unit before the dermatologist's visit, optimizing the time available for more severe diagnostics such as skin cancer (6).
Our study showed that in our regions observed patient awareness and self-assessment of skin cancer symptoms were less than ideal that may be contributing to the higher melanoma-related mortality rates. Enhancing patient education and awareness programs is important to promote early detection and preventive strategies, potentially leading to improved outcomes and reduced mortality rates. This includes promoting self-examination for early detection, distributing informative infographics about the ABCDEs of Melanoma, and utilizing resources such as the CDC skin health and safety infographics. This study and the study on the effectiveness of Teledermatology suggests that primary care physicians may need to be more involved in dermatological care in rural areas where access to dermatologists is limited (6 ). Additionally, Teledermatology can help combat Missouri’s “geographical desert” to dermatologic care (7).
Despite a lower incidence rate of melanoma, certain regions, including Missouri, face higher mortality rates, indicating a prevalence of late-stage disease and difficulty accessing dermatologic care. The study identifies long wait times and difficulty locating dermatologists as primary barriers from the patient’s perspective to accessing specialized care in these areas. Additionally, inadequate patient awareness and self-assessment of skin cancer manifestations contribute to the disparity between incidence and mortality rates. Collaboration between primary care physicians and dermatologists is crucial in promoting early detection and preventive strategies, including the telemedicine ECHO dermatology collaboration. With Teledermatology, delay in disease diagnosis should decrease and treatment options should be more cost efficient due to improved lesion triage
and management. Overall, addressing these challenges is essential to improve the well-being of patients and communities in rural Missouri.
References:
1. Taney County Health Department 2019 Community Assessment. Retrieved from www.taneycohealth.org/wp-content/uploads/2021/05/CHA-2019Final_05_2021.pdf.
2. Ozarks Healthcare. (2022, November). Ozarks Healthcare Community Health Needs Assessment. Retrieved from https://www.ozarkshealthcare. com/app/files/public/8115308e-0106-4811-8025-e509cd8ccc70/Ozarks%20 Healthcare%20CHNA%202022.pdf
3. “State Cancer Profiles.” State Cancer Profiles > Quick Profiles, statecancerprofiles.cancer.gov/quick-profiles/index.php?statename=missouri &spacingHiddenBox=&stateNotSelected=Please%2Bselect%2Ba%2Bstate%2B to%2Bproceed. Accessed 14 Apr. 2024.
4. Stitzenberg KB, Thomas NE, Dalton K, Brier SE, Ollila DW, Berwick M, Mattingly D, Millikan RC. Distance to diagnosing provider as a measure of access for patients with melanoma. Arch Dermatol. 2007 Aug;143(8):991-8. doi: 10.1001/archderm.143.8.991. PMID: 17709657; PMCID: PMC3629703.
5. “Facts & Statistics.” AIM at Melanoma Foundation, 13 Mar. 2024, www. aimatmelanoma.org/facts-statistics/.
6. Giavina-Bianchi M, Santos AP, Cordioli E. Teledermatology reduces dermatology referrals and improves access to specialists. EClinicalMedicine. 2020 Nov 21;29-30:100641. doi: 10.1016/j.eclinm.2020.100641. PMID: 33437950; PMCID: PMC7788431.
7. Lewis H, Becevic M, Myers D, Helming D, Mutrux R, Fleming D, Edison K. Dermatology ECHO - an innovative solution to address limited access to dermatology expertise. Rural Remote Health. 2018 Feb;18(1):4415. doi: 10.22605/RRH4415. Epub 2018 Feb 7. PMID: 29409325.
8. Becevic M, Ge B, Braudis K, et al. Diagnostic and treatment concordance in primary care participants and dermatologists utilizing Extension for Community Health Outcomes (ECHO). Journal of Telemedicine and Telecare. 2023;0(0). doi:10.1177/1357633X221147074
9. https://meric.mo.gov/data/gross-domestic-product-data-series
10. Glazer AM, Farberg AS, Winkelmann RR, Rigel DS. Analysis of Trends in Geographic Distribution and Density of US Dermatologists . JAMA Dermatol. 2017;153(4):322–325. doi:10.1001/jamadermatol.2016.5411
11. https://seer.cancer.gov/statfacts/html/melan.html

With Private Banking at Central Bank, you have exclusive access to a host of financial services and products, where we take care of the details across the full spectrum of the bank. You will have access to higher deposit rates, custom credit solutions and home financing, as well as individualized guidance with your investments. Our main goal is to help you maximize your money seamlessly. You have complex needs. We have the concierge level solutions you want.



STEVE GASSEL
Senior Vice President - Director of Private Banking | NMLS # 554828
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4213
Steve.Gassel@centralbank.net
KARA TURNER
Vice President - Private Banking | NMLS # 1833785
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4253
Kara.Turner@centralbank.net
JOYCE WONG-HSU
Officer - Private Banking | NMLS # 1239617
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4214
Joyce.Wong-Hsu@centralbank.net


by Nancy Yoon, MD MPH, Chief Medical Officer Springfield-Greene County Health Department
In 2023, we celebrated the enduring legacy of our department with the remarkable milestone of 150 years of service! Since June 30, 1873, when the department was founded, we have witnessed the transformative power of public health, and enriched the lives of individuals in our community for generations.
Public health has evolved in form and function to deliver the services necessary to address the most pressing health issues of the time. Although health threats have changed, our dedication and service to the community has been strong and steadfast. In return, we’ve been supported by a community that values health.
Through strategic partnerships aimed at creating collective impact, we have been able to adapt and respond to emerging challenges effectively. Our collaborative efforts not only strengthen our capabilities but also amplify our impact, allowing us to reach more individuals and address the specific needs of our community.
For a remarkable 150 years, Springfield-Greene County Health has proudly served our community, offering essential services and fostering connections to enable all individuals to live longer, healthier and happier lives. As a cornerstone of public health, we have continually adapted to meet the emerging and urgent needs of the people we serve. From addressing historical health challenges to navigating contemporary crises, we continue to stand as a resilient institution, dedicated to the health and vitality of Springfield and Greene County. Our enduring legacy underscores the significance in promoting the health and happiness of generations past, present and future.

A look through the history of SpringfieldGreene County Health is a testament to our evolution as a leader in public health for our community. The core focus of the department has always been to control the spread of disease within the community. As disease and spread have changed throughout the years, we have grown and adapted to meet the needs of the evolving landscape. Our proactive and often modern approaches to meet people where they are have allowed us to lead critical public health initiatives for the last 150 years.
Our founding mission was to curb the spread of communicable diseases such as cholera through basic sanitation and clean water supply. In the early 1900s, we shifted to include testing and treatment of other illnesses present in the community. These included: tuberculosis, Hepatitis A, Venereal Disease (sexually transmitted infection) and other diseases of the time. As immunizations became a standard of care, public health nurses became crucial in preventative worked to ensure vaccine uptake across the City and County, which helped reduce the negative diseases, such as polio, that were common. With their help, Springfield-Greene County Health several vaccination efforts in our history.
• April 12, 1889 City of Springfield ordinance creates office of Health Commissioner
• April 23, 1889 L. K. Anderson named first Health Commissioner
• July 1909 Anti-Tuberculosis Commission formed
• 1918 Springfield health board takes precautions to prevent spread of Spanish Flu
• January 22, 1924 First female director, Brella (Berdella) S. Finch appointed as Commissioner
• June 30, 1940 Primary focus becomes providing primary care for medically indigent citizens
• August 1953 Eleven cobras escape Springfield pet shop, roam city for three months. Health director Del Caywood drives truck blaring “snake charming music” to assist capture
• May 20, 1954 Greene County selected as field trial site for Salk polio vaccine
• July 30, 1961 Health department begins counting pollen
• 1974 Lead poisoning prevention program begins
• May 26, 1976 Ground broken on city-county health center, which will later be known as the Harold K. Bengsch Building
• March 1977 City and County Health Services officially merge
• September 17, 1987 Harold Bengsch appointed director of executive committee of Missouri AIDS Task Force
• July 15, 1992 Baby Your Baby program debuts to expand prenatal resources for women at risk for poor pregnancy outcomes
• 1996 Hepatitis A outbreak
• 2009 h1N1 first identified by Springfield Greene County Health
• September 1, 2017 Prescription Drug Monitoring Program begins data collection
• October 2, 2018 Health Department accreditation through the Public Health Accreditation Board
• July 17, 2019 City Council raises age to purchase tobacco to 21
• March 12, 2020 First COVID-19 case in Greene County
2023 HIGHLIGHTS
• Establishment of the Mental Health 417 online resource hub and the campaign focused on men, “Hey Man, You Good?” (mentalhealth417.com)
• In 2023, the community health advocate team devoted considerable effort to enhancing the accessibility and awareness of Naloxone within the community. The “Revive” app was launched in June 2023, which provides step-by-step rescue instructions on how to administer Naloxone, information on Good Samaritan laws, where to access Naloxone, and local treatment and recovery services.
• In April 2023, the Disease Intervention Specialist (DIS) program launched to combat the spread of sexually transmitted infections in Greene County, specifically syphilis and HIV.
• In 2024, the Family Connects began free home nurse visits, offered to all newborns in Greene County.
Looking ahead, SGCHD is committed to furthering our vision to help all people live longer, healthier, and happier lives. Our focus remains firm on protecting and improving community health. Through collaboration, outreach, and a commitment to accessibility, we’re dedicated to making a positive impact on everyone we serve.
As we move forward, we’re excited to continue to lean into our important work through valuable partnerships and community involvement. Better health outcomes can be achieved for all.
The full timeline and annual report can be downloaded at: https:// www.springfieldmo.gov/DocumentCenter/View/65879/AnnualReport-2023

by Barbara Hover, Co-president GCMS Alliance
Greene County Medical Society Alliance hosted area physicians and their families at the Dickerson Park Zoo to celebrate Physician Family Day 2024. Thanks to the support of Ferrell-Duncan Clinic Foundation and Mercy, families were able to tour the zoo at their leisure for this very popular, private event. Zoo entrance fees, picnic style meal, train ride, giraffe and petting zoo feed were all provided. The weather was perfect and the docents and volunteers at the zoo did an outstanding job providing personal encounters with various animals.
We were also honored to have in attendance MSMA President Dr. David Pohl and his wife Kathy, Jeff Howell Executive Vice President of MSMA, and his wife Cyndee and MSMA Alliance President Donna Corrado as well as 400 physician and family members. Medical students, and both active and retired physicians and their families all enjoyed the fun, food and fellowship.
GCMSA will once again host Physician Family Night at the Museum at the Discovery Center in February or early March. It is an after -hours event with children friendly food and access to the exhibits at the museum. This will be our 7th year there and it is always a nice way to celebrate and visit with your friends in the medical profession. There is always something to interest every age group at the Discovery Center.
The Greene County Medical Society Alliance is happy to host these events as part of our Taking Care of Our Own Program which is dedicated to physician wellness. Socializing with friends and family in the same profession who understand the pressures of the occupation is a stress reliever. If you are the spouse of a physician, please consider becoming a member of GCMSA and help us to plan new and fun activities for your families to enjoy. You can join online at the Greene County Medical Society website.













































Mission Statement Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H
BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
3850 S. National Ave, Suite 705 Springfield, MO 65807 (Located inside Hulston Cancer Building-7th floor)
1240 E. Independence Springfield, MO 65804
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672 PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care) 2200 E. Cleveland Ave Monett, MO 65708 Phone: 417-888-0858 • Fax: 417-889-0476
To
Please Note: Changes to ads will be made quarterly and must be submitted in writing. H Denotes GCMS Membership “A” Denotes GCMS Applicant
GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq.
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine
www.ascentdpc.com 417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804 Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
MATTAX • NEU • PRATER EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
COXHEALTH
FAMILY MEDICINE RESIDENCY
FAMILY MEDICAL CARE CENTER
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AmericAn BoArd of fAmily medicine
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Katie Davenport-Kabonic, DO
Michael Kabonic, DO
Jessica Standeford, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
VANESSA MCCONNELL, APRN, DNP, FNP-C
1135 E. Lakewood, Suite 112 Springfield, MO 65810
Located inside Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500 Fax 883-8964 or toll free 877-966-2607 Monday-Thursday 8am-4:30pm Friday 8am-12pm
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H
Board Certified in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD
Board Certified in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA
COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD
Board Certified in Internal Medicinee 2115 S. Fremont, Suite 2300 Springfield, MO 65804
Phone 417-820-5600 Fax 417-820-5606
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD
American Board of Urology
MARK J. WALTERSKIRCHEN, MD, FACS American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Springfield, MO 65804
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-C, CCD
KELLEY R. JENKINS, FNP-C, ALINA CUMMINS, PA-C
HILARI HENDERSON, PA-C
AMBERLY EVERSOLE, PA-C
DESYRAE RIDENOUR, PA-C
STACY GHOLZ, FNP-C
MURIEL L. GO, MD
American Board of Endocrinology
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology
SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100 www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
SPRINGFIELD NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700 Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
BLAKE MARTIN, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
BILL HAMPTON, ANP-BC
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP Obstetrics/Gynecology
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology 909 E. Montclair, Suite 120 Springfield, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic 3850 S. National, Ste. 600 Springfield, Missouri 65807
Monett Clinic 802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880
Fax 882-7843
Visit our website: www.ohaclinic.com
Otolaryngology
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
A. DANIEL PINHEIRO, MD, PhD, FACS H
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP
Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750
Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS
American Board of Facial Plastic & Reconstructive Surgery
American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
JAMES E. BRIGHT, MD H Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804

4730
chAnge Service requeSted