

FOR unmatched insight, VIS ion matters

FORward VISion thrives
We applaud that your goals and aspirations begin with a vision of achieving peace of mind. Our vision is helping make yours a reality. At FORVIS Private Client™ our forward-thinking advisors help high-net-worth individuals and multigenerational families, trusts, estates, investment partnerships, and private foundations thrive through complexity and change so you can prepare for what’s next.






Co-Editors:
Jim Blaine, MD
Minh-Thu Le, MD
Junior Co-Editor: Andrew K. Le
Graphic Designer:
Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
Frank Cornella, DDS, MD
C.J. Davis, PsyD
Jean Harmison
Barbara Hover
Thomas Kuich, MD
Vu Le, MD
Victor Pace, MD
Nancy Yoon, MD
Jana Wolfe
SOCIETY OFFICERS
Sanjay Havaldar, MD President
James Rogers, MD President-elect
Vu Le, MD Secretary
Jim Blaine, MD Treasurer
“IS
IT AUTUMN YET?”
Since early August, this question has been on a small letter board on my mantle at home. It’s when we were having record temperatures, and the crisp notes of fall seemed forever away. Fall is my favorite season in the Ozarks with the myriad of colors on the trees and the perfect temperatures that we have. It is also is when children are back in school, the business of our lives seems just a little more, and preparations begin for the holidays. It’s always the season that moves the quickest for me, and I’m always surprised how fast it goes. In this journal, we are looking at several topics that occur in the autumn, from worrying about food allergies in children going back to school, to new food allergies in adults that are getting tick bites, to seasonal affective disorder, and our Alliance’s own well-attended Physician Family Day zoo event that marks the end of summer and the beginning of fall.
Additionally, we have some original research from a guest writer at the VA, a doctor of pharmacology, writing about their ExIT plan for opioid weaning. Pace’s post also gives us some learning opportunities. How many questions can you answer correctly? Our own president has an article that challenges us to always look for an -

swers outside the box while Forvis Private Client always challenges us to make the most of our income for ours and our family’s future.
And introducing the board for the new and improved GCMS Foundation! Jean Harmison is introducing them and the goals of our foundation in this journal. I really think this will allow GCMS to remain relevant and increase our longevity in our community.
Keep our CME events and social events on your calendar as well. There will be one October 11th and one November 3rd. Remember to RSVP because space is limited and so we can give you the best experience we can. Also, please make note of our new advertisers. Without them and close partnerships with both Cox and Mercy hospitals in Springfield, we could not bring you this wonderful journal. We covet your support and membership. We welcome our new members that signed up at the zoo event! Please consider joining GCMS if you haven’t already or renew your membership before the end of the year. Our executive council is busy making your membership worthwhile with new programing and planning for next year as well! Happy Autumn!!!
Welcome New GCMS Members




Keeping an Open Mind
A recent article on Doximity referenced an article in the Washington Post: “A Catatonic Woman Awakened After 20 years. Her Story May Change Psychiatry," The Washington Post, by Richard Sima, June 1, 2023.
The article details the amazing finding that a few patients who had long been institutionalized with presumed severe psychiatric illness leading to psychosis and withdrawal actually had severe neuropsychiatric lupus. One of the cases cited was a young lady named April who was a healthy, well-rounded, high achieving accounting student in college who acutely decompensated in 1995, requiring psychiatric hospitalization. She was diagnosed with schizophrenia, which was severe enough to require long-term hospitalization.
A young medical student visiting from Amsterdam, Sander Markx, first encountered her in 2000. Twenty years later, Markx had become the director of precision psychiatry at Columbia University and crossed paths with her again. Noting that she had failed many courses of treatment such as antipsychotics, antidepressants and ECT, he convened a team of more than 70 experts from around the world to evaluate her case. Their research noted markedly elevated antibodies due to lupus, with imaging revealing damage to the temporal lobes. Interestingly, her lupus was not affecting any of her other organ systems as typically found.
After an intensive regimen of multiple courses of IV




steroids and dose of cyclophosphamide and rituximab, she began to improve. Initially, she had improvement in cognition tests and her psychosis to the point where she could be discharged to a rehabilitation center and reunited with her family.
Researchers in Germany have identified 94 psychiatric patients with suspected autoimmune diseases and reported that most of them benefited from immunotherapies. In addition to lupus, 17 additional diseases have been identified in which antibodies specifically target neurons, which can present with different neurological and psychiatric symptoms. Psychiatrists in Germany are regularly collecting CSF fluid to screen for potential immunologic disorders.
This is an amazing story of hope for a group of patients who were classified as having a chronic problem with no hope for improvement. Modern medicine is frequently criticized for many failings and shortcomings, but it is gratifying to read cases such as these where an innovative approach yields life-changing results. Reading these stories is inspirational and encourages us to keep a fresh mind when we come across patients with thick charts and long records of extensive tests and treatments. The challenge will be to avoid repeating unnecessary tests with increased costs and risks while keeping an open mind for other possibilities in their diagnosis and treatments.


GREENE COUNTY MEDICAL SOCIETY FOUNDATION
by Jean Harmison, GCMS Executive DirectorThe Greene County Medical Society is on the move and is generating new energy and excitement! One of the exciting changes includes expanding and reviving the Greene County Medical Society Foundation. Historically, GCMS has been doing charitable work since this foundation was established in 1960. Over the last 63 years, GCMS has been stewards over 2 CME funds, offering many hours of focused education, and directed scholarships to help numerous students through medical school loan programs.
While there are many opportunities for us to engage and improve the health of our community, this expansion will allow us to receive tax deductible funds and charitable grants that we can direct toward our mission for these causes.
Mission: The purposes of the Greene County Medical Foundation include promotion of community health through education, projects, and support of related charitable organizations with involvements and/or financial support.
We are pleased to announce that the following physicians have been appointed by GCMS Council volunteered to serve on the GCMS Foundation.
GCMS Foundation Board Members
James Rogers, MD, President
Jim Blaine, MD, Treasurer
Vu Le, MD
Kayce Morton, DO
Jacob Thomas, MD, FACS
Patricia Dix, MD
Keith Laferriere, MD
Jean Harmison, Executive Director
We are excited to launch this much-needed resource for the health of the people we serve in Southwest Missouri. If you are interested in serving on a committee or if you would like to donate to the GCMS Foundation, please send an email to director@gcms.us or call 417-887-1017.
Stay tuned! More to come!










TAX-EFFICIENT RETIREMENT PLANNING FOR PHYSICIANS
by John Davis, CFP Managing Advisor ForvisNobody enjoys paying taxes, especially high-earning physicians. Everyone understands the necessity, but it makes sense that no one wants to pay more than their fair share each year. The good news is there are multiple ways to help you reduce your tax liability while also saving for retirement. Proper planning throughout your lifetime can help you achieve adequate retirement savings in a tax-efficient manner.
Utilizing Employer-Sponsored Retirement Plans
One of the most effective ways for physicians to save for retirement while reducing tax liability is through employer-sponsored retirement plans. Physicians have access to various plans such as a 401(k), 403(b), 457(b), and others, which allow for pre-tax contributions from their paychecks to be invested for future use. These contributions directly reduce taxable income, and the earnings in the account grow tax-deferred. This not only results in immediate tax savings during high-earning years, but also defers taxation of the growth until distributions are taken in the future.
In recent years, many employer-sponsored plans have introduced Roth contribution options, offering additional choices that may be more tax advantageous in retirement based on individual tax situations, goals, and objectives.
Traditional vs. Roth Contributions
Physicians can choose between two main paths for tax-efficient retirement savings: Traditional or Roth contributions. Traditional retirement plans and individual retirement accounts (IRAs) may allow for contributions that reduce current taxable income. The contributions and investment gains grow tax-deferred until distributions are taken in the future. This is particularly beneficial during high-earning years when physicians are in higher tax brackets than they may be in during retirement.
On the other hand, Roth contributions are made with post-tax funds and grow tax-free. Unlike traditional distributions, Roth distributions can be made without taxation. Roth contributions are particularly advantageous for physicians in lower tax brackets before they become attendings.
Health Savings Accounts (HSAs)
Physicians often overlook the potential tax-saving benefits of HSAs when planning for retirement. HSAs allow individuals to set aside money specifically for qualified medical expenses. Similar to traditional IRAs, HSA contributions reduce current taxable income and can grow tax-deferred when left to grow until retirement. The key advantage is that distributions from HSAs are tax-free when used for qualified medical expenses. This can be a valuable tool for saving for both planned and unexpected medical costs for individuals and families either in the short term or in retirement. Many employers now offer HSAs as part of their benefit plans, al-

lowing physicians to contribute directly from their paychecks, similar to a 401(k). Even if your employer does not provide this benefit, anyone enrolled in a high-deductible health plan (HDHP) is eligible to contribute to an HSA.
529 Plans
Saving for our children’s future education is a top priority for many physicians. A 529 plan is an effective way to prepare for these expenses. Contributions to 529 plans may qualify for state income tax deductions depending on your state of residence, and the investments in the account grow tax-deferred, similar to the retirement vehicles discussed earlier. When the time comes, distributions from the account are tax-free if used for qualified education expenses.
529 plans have become more flexible in recent years, offering cost-effective investment options and allowing distributions for various education expenses, including trade schools and private primary and secondary education. In addition, if your child does not use all the funds, the account can generally be transferred to other eligible beneficiaries. Recent law changes may allow a portion of unused 529 dollars to be transferred to a Roth IRA.
Considering the Whole Picture Taxes play a vital role in financial planning for physicians. It is crucial to consider tax implications when making any financial decisions, but do not let potential tax liabilities dictate all choices. Given the complexities of tax-efficient retirement planning, it is recommended to work with a CERTIFIED FINANCIAL PLANNER™ familiar with physicians who can help develop an in-depth plan that incorporates these strategies based on your personal goals and objectives as a physician.
FORVIS Private Client services may include investment advisory services provided by FORVIS Wealth Advisors, LLC, an SEC-registered investment adviser, and/or accounting, tax, and related solutions provided by FORVIS, LLP. The information in this article should not be considered investment advice to you, nor an offer to buy or sell any securities or financial instruments. The services, or investment strategies mentioned in this article may not be available to, or suitable, for you. Consult a financial advisor or tax professional before implementing any investment, tax or other strategy mentioned herein. The information herein is believed to be accurate as of the time it is presented and it may become inaccurate or outdated with the passage of time. Past performance does not guarantee future performance. All investments may lose money.
LIGHT FOR PATIENTS WHO WILT WITH THE TILT
by Thomas Kuich, MD, MBA, Clinical Psychiatry, Mercy HospitalIt's that time of year again when the rotational axis of the Earth tilts away from the sun, bringing us these shorter fall and winter days. Bright light treatment ("BLT") of clinical depressive episodes that have a fall or winter exacerbation can be an effective treatment adjunct in some cases. Some patients notice an increase of depression during the winter months, which is a phenomenon known as "seasonal depression." The recommendations for "Bright Light Therapy" can vary to some extent depending on the reference, but in general it is advised that the light used be sufficiently bright (10,000 Lux) and administered in the morning for 25 or 30 minutes before 9 o'clock in the morning. I have often advised this to patients when they spontaneously remark about increased depression in the fall and winter. When I was attending (virtually) a psychopharmacology course last fall, the psychiatrist presenting mentioned starting the treatment early. One would start late September or early October before the onset of the depressive episode, or the exacerbation of depression. I like the idea of using for "Bright Light Therapy" as a way to prevent or mitigate a seasonal depressive episode to begin with. However, a literature search I did for this article indicated the efficacy of Bright Light Therapy to prevent winter depression is "inconclusive." Nonetheless, it would seem to make sense, and I have advised some patients to "start the light treatment early."
The reference I have given patients for selecting a light that can be used for Bright Light Therapy is to Google "wirecutter light therapy." Wirecutter is the name of a sort of "consumer reports" review of products that is published by the New York Times with many of the articles available at no charge. This will pull up a review comparing some lights produced for light treatment of depression. They range in price, size and features and can give a patient a good idea about what they might want to look for in a light to use daily for 25 minutes before 9 AM to beat the winter blues. Many patients who use light treatment speak to its effectiveness. Of course, others will sometimes notice little or no effect. But given the few side effects it is usually worth a try for seasonal depression.
The mechanism of action of Bright Light Therapy has been thought to be due to correcting the "phase delay" which is thought to result in depression symptoms. Another postulate involves effects on the serotonin system.
When the patient uses Bright Light Therapy, they are advised
not to look directly at the light, but rather have it in the periphery at the recommended distance, which can vary from light to light, and they can be doing anyone a number of activities, eating breakfast, reading, or pairing socks.

In summary, consider telling your patients with seasonal depression to have a “BLT,” sandwiched in between when they wake up in the morning and 9 AM. That just might make them smile.
References
Campbell, P. D., Miller, A. M., & Woesner, M. E. (2017). Bright light therapy: Seasonal affective disorder and beyond. The Einstein journal of biology and medicine : EJBM. https://www.ncbi.nlm. nih.gov/pmc/articles/PMC6746555/
Clinical overviews │ recurrent major depressive disorder with a seasonal pattern. Elsevier. (n.d.). https://elsevier.health/en-US/ preview/recurrent-major-depressive-disorder-seasonal

PACE'S POST
by Victor Pace, MDTime to have a little interactive fun. Below are 25 medically-related questions across various medical fields. See how well you do.
1. Your patient with an abdominal aortic aneurysm (AAA) asks when they should be referred for surgical intervention. You tell them when their aneurysm reaches _____.
A. 3-3.5 cm B. 4-4.5 cm C. 5-5.5 cm D. 6-6.5 cm
2. The Centor criteria determine the likelihood of _____ in adults.
A. Otitis Media B. Group A Strep C. Syphilis D. Heart Disease
3. The Ottawa Ankle Rules for assessing acute ankle injuries help determine the need for _____.
A. Radiographs B. Casting C. Surgery D. Bracing
4. According to the United States Preventive Services Task Force (USPSTF), colon cancer screening for the average-risk adult should begin at age _____.
A. 40 B. 45 C. 50 D. 55
5. Fifth Disease, with the classic "slapped cheek" rash, is caused by _____.
A. Streptococcus B. Herpes Simplex C. Parvovirus 19 D. Human Papilloma Virus
6. The mood disorder _____ causes emotional ups and downs but is not as extreme as those seen in Bipolar 1 or Bipolar 2 disorders. According to the DSM-5, there are six diagnostic criteria, with one specifier.
A. Cyclothymia B. Dysthymia C. Panic Disorder D. Obsessional Compulsive Disorder
7. Pap Smears should be obtained in a sexually-active eighteen-year-old female.
A. True B. False
8. The lab test, _____, has the highest known sensitivity and is the preferred blood-based test for assessing myocardial injury/damage in acute emergencies.
A. Creatine Kinase B. CK-MB C. Myoglobin D. Troponin
9. The American College of Obstetricians and Gynecologists (ACOG) recommends _____ as the first-line pharmacologic treatment for nausea and vomiting in pregnancy.
A. Metoclopramide B. Pyridoxine C. Promethazine D. Ondansetron
10. _____ is a serious, uncommon disease in which calcium accumulates in small blood vessels of the fat and skin tissues.
A. Calciphylaxis B. Calcitonin C. Hypoparathyroidism D. CKD
11. Low-dose helical computed tomography (LDCT) is a testing modality recommended for adults 50-80 who meet specific criteria for _____ cancer screening.
A. Bone B. Colon C. Liver D. Lung
12. Bupropion is absolutely or relatively contraindicated in all but the following conditions.

A. Seizures B. Traumatic Brain Injury C. Smoking D. Anorexia
13. The leading type of injury in older people aged 65 and older is _____.
A, Gunshot Wounds B. Automobile Injuries C. Burns D. Falls
14. The USPSTF advises that most men over 50 obtain a prostate-specific antigen (PSA) lab test for prostate cancer screening.
A. True B. False
15. The Rome IV diagnostic criteria are used to diagnose _____.
A. Irritable Bowel Syndrome B. Migraine Headaches C. Epilepsy D. Colon Cancer
16. Medicare Part D provides _____ coverage.
A. Inpatient Hospital Care B. Outpatient Medical Care C. Prescription Drug D. Long-Term Care
17. This disease has a "herald" or "mother" patch, a large single oval or round sharply delineated lesion, in 50 to 90 percent of cases.
A. Lyme Disease B. Pityriasis Rosea C. Scarlet Fever D. Herpes Zoster
18. The symptomatic triad of Meniere Disease includes episodic vertigo, ______, and hearing loss.
A. Syncope B. Tinnitus C. Otitis D. Palpitations
19. In certain patients, orthognathic surgery can successfully treat obstructive sleep apnea.
A. True B. False
20. The International Classification of Headache Disorders, 3rd Edition (ICHD-3) criteria for migraine without aura include all but the following.
A. Photophobia B. Nausea C. Aphasia D. Unilateral Location
21. The classic presentation of the vaginal infection ______ includes a pH of 4 to 5, a Whiff test, often positive but can be negative, and a green-yellow frothy vaginal discharge.
A. Bacterial Vaginosis B. Trichomonas C. Candidiasis D. Chlamydia
22. A nine-month-old infant who reaches all their developmental milestones should be able to perform all but the following.
A. Sits Without Support B. Bangs Two Things Together C. Waves "Bye-Bye" D. Looks When You Call Their Name
23. The USPSTF recommends a daily supplement of ______ for all persons planning to or who could become pregnant.
A. Vitamin C B. Folic Acid C. Vitamin D3 D. Glucosamine 24. After placing a drug-eluting stent for acute coronary syndrome, a person should take aspirin along with _____for twelve months.
A. Apixaban B. Clopidogrel C. Warfarin D. Dabigatran
25. The Transtheoretical Model, also called the Stages of Change Model, involves six stages. These stages of change include Precontemplation, Contemplation, _____, Action, Maintenance, and Termination.
A. Preparation B. Consciousness C. Secure D. Practice
UPCOMING EVENTS & CME






GREENE COUNTY MEDICAL SOCIETY ALLIANCE’S
PHYSICIAN FAMILY DAY AT THE ZOO!
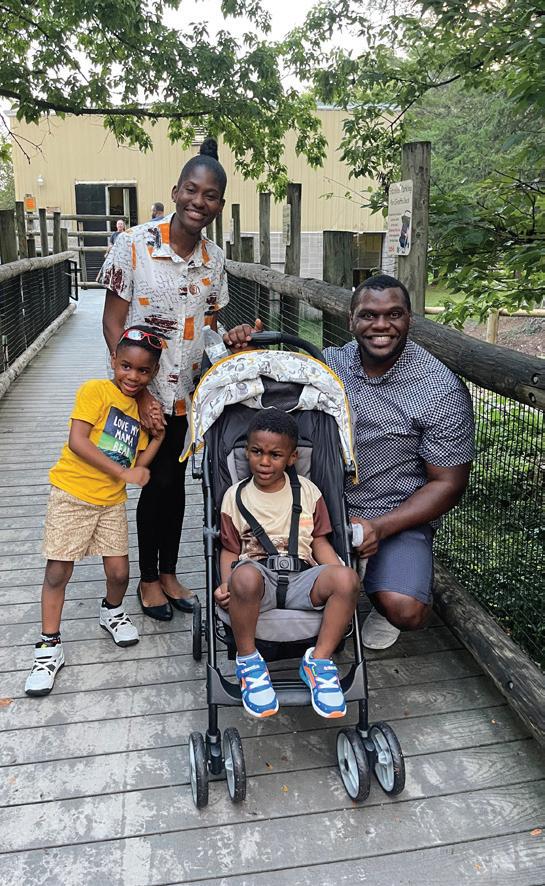
by Barbara Hover, GCMS Alliance co-presidentA brief rain shower did not dampen the festivities as physicians and their families enthusiastically enjoyed Physician Family Day at the zoo on August 26. Physician Family Day was established nationally by the AMA Alliance in 2018. It occurs every year on the last Saturday of August. The idea is to find time to thank physicians and their families for the contributions and sacrifices they make for excellence in health care.
Jana and I would particularly like to thank Cathy Leiboult, Gail Holand, and the GCMS directors and staff for their assistance in making the event such a success.
Physician Family Day at the Zoo was open to all physicians and their families in the greater Springfield area. It was made possible with special thanks to Ferrell Duncan Foundation and Mercy who have always been supportive of our Taking Care of Our Own program. Zoo entrance fees, picnic style meal, train ride, giraffe food and petting zoo feed were provided. It was an excellent opportunity to spend quality time with family, visit with old friends, and meet new physicians.
Physician wellness is a focus of both the AMA and the AMAA. Greene County Medical Society Alliance Taking Care of Our Own program strives to care and support the physician family. Time spent relaxing with friends and family is important to maintaining a healthy lifestyle. We plan to hold our annual Physician Family Night at the Museum in February. The Discovery Center evening has been one of our most popular events.























































ORIGINAL RESEARCH
EXPECTATIONS, INVESTIGATION, AND TAPER (EXIT): A SYSTEMATIC APPROACH TO OPIOID DOSE REDUCTION
by Vinh Dao,PharmD, BCPS (Corresponding Author), Paul Heideman, PhD, LP, Franz Macedo,
DO,Esther W Njau, PharmD , Vu Le, MD, FAPA All Authors are from the Minneapolis VA Health Care System
Conflict of Interest Statement: Authors of this publication do not have any financial or personal relationships with commercial entities that may have direct or indirect interest in the subject matter of this manuscript. The views expressed in this manuscript reflect those of the authors and do not represent the views of the Department of Veterans Affairs or of the United States.
Opioid Tapers: We Need a Gameplan
Millions of patients suffer from persistent pain and experience functional impairments and lowered quality of life. Many of these patients have been treated with chronic opioid therapy as the primary mechanism to cope with their pain. As research in chronic pain has grown in the past decade, so has our understanding of chronic pain management and the negative impact of long-term opioid therapy. A shift in philosophy towards encouraging mind-body based treatments rather than chronic opioid therapy became the focus of care. Similarly, a biopsychosocial model of care that emphasizes self-management replaced outdated biomedical and opioid-based treatment plans. The result is a concerted effort by the medical community to deprescribe or taper down chronic opioids. This process can be daunting for the inexperienced clinician. Poorly designed tapers can place patients at risk for adverse outcomes. The authors propose a strategic approach to opioid taper design in the form of a simple mnemonic-ExIT. The clinician is guided through three domains critical to opioid taper design: Expectations, Investigation and Taper. Each domain capitalizes on our understanding of psychology and behavior to create an individualized taper plan that enhances safety and patient engagement
When it Comes to Opioid Tapers, One Size Does Not Fit All
Much of the medical community agrees that after decades of uninhibited prescribing practices, systematic efforts to reduce opioid use amongst the general population is considered a step in the right direction. However, some clinicians lack experience with opioid management and the familiarity needed to design safe and patient-centered taper schedules. This lack of experience resulted in failed opioid tapers, or in some instances, adverse patient outcomes. Indeed, some existing guidelines have concluded that there is insufficient evidence to support specific or unilateral tapering strategies; instead suggesting a collaborative, patient-centered approach to opioid reduction.1 The unintentional adverse consequences of opioid tapers can include withdrawal, conversion to non-prescribed or illicit substance abuse, and increased suicidality.2 Although withdrawal symptoms are rarely fatal with the exception of fetal harm during pregnancy, the presence of nausea, vomiting, insomnia, gastrointestinal upset, worsening mood, and anxiety results in significant discomfort and can result in early termination of opioid taper and eventual failure of treatment.3,4 Fundamentals of psychology reminds us that we remember negative experiences and do our best to avoid them .5 This concept can influence the patient and hinder future attempts to taper down opioids.
Expectations, Investigation, and Taper (ExIT)
We have established that improper opioid taper designs can lead to poor patient outcomes.6 As a response, providers that manage pain have emphasized the need to incorporate shared decision-making and harm reduction approaches to reduce the risk of negative outcomes.7 Two primary contributors to an unsuccessful opioid taper attempt

includes inexperience and blanket standardization of taper protocols designed as a quick fix to compensate for inexperience. Rather than proposing yet another quantitative guide to opioid tapering, the authors of this paper offer a qualitative method that sets the framework for opioid taper care plans in the form of an easy to remember mnemonic- ExIT. The foundational core of ExIT emphasizes the assessment and collection of individualized patient characteristics that drive taper design as well as the creation of patient-centered goals which are divided into three broad domains that includes: Expectations, Investigation, and Taper (ExIT). Each domain consists of important points to ask or consider when designing opioid taper care plans such that each domain will incorporate psychological approaches to facilitate tapering. Human behavior is comprised of preconceptions, motivators, and physiological experiences that are interwoven to influence decisions; all which can be leveraged to create a successful, individualized taper.5,8 Expectations
Expectations is unique amongst the triad of domains as the information obtained modifies not just the behavior of the patient but impacts clinician decision-making as well. The importance of establishing early expectations during the development of care plans should not be trivialized. Patient expectations help establish early benchmarks of success. A failure to define expectations results in an ambiguous goal and serves as a barrier to progress. Imagine a long-distance swimmer in the Olympics who is not told how far they need to swim. The competitor who is deprived of the ability to plan, pace, and mentally prepare for a strenuous event may become demoralized. Similarly, unreasonable therapeutic goals can evoke a sense of failure prior to implementing an opioid care plan when the patient already perceives the feat as impossible. In the context of opioid tapers, success has historically been defined as tapering down to cessation. Although this may be the goal for many patients, it may be unachievable for some, thus we should consider that any sustained reduction in opioid use qualifies as success if the patient is at lowered risk for adverse opioid events. Equally as important is that this benchmark for success is communicated and shared with the patient as success and motivation are intertwined. Certainly, if the patient is at elevated risk for opioid overdose, is taking a dangerous combination of medications or illicit substances, then there is increased urgency to fully taper off opioids. However, there are many chronic pain patients at lowered risk of overdose with refractory pain and the benefits of chronic opioid therapy may outweigh the risks in these instances.
Investigation
If expectations are the appetizer of a 3-course meal, then investigation comprises the main course. The term investigation carries both positive and negative connotations. The investigation of a crime implies collection of evidence to determine wrongdoing. Clinicians should strive to avoid applying negative connotations of this term during
patient assessment. Instead, we define investigation in its more positive connotation; the scientific investigation of facts as it pertains to patient assessment. The latter definition emphasizes the collection of data rather than evidence thereby removing stigma that opioid tapers imply patient wrongdoing. In the context of opioid tapers, the investigation domain consists of questions and considerations that detects individual characteristics unique to the patient, which then further defines use, response, and personal preferences (See Table 1).
Table 1. ExIT- Key Questions of the Investigation Domain Investigation Category
1. How long has the patient utilized chronic opioid therapy (COT)? Pharmacological
2. What opioid formulations and regimens has the patient used? Pharmacological
3. What is the patient’s current MEDD? Pharmacological
4. What has historically been the highest MEDD that patient has been maintained on? Pharmacological
5. Has COT resulted in adverse medication side effects or drug interactions? Pharmacological
6. Has current COT improved function or quality of life (QOL)? Psychosocial
7. Has COT reduced patient’s quality of life in any aspect? Psychosocial
8. Does patient receive assistance from a caregiver with medication administration? Individual
9. Does patient have a history of compliance difficulties? Individual
10. What was the outcome of previous opioid taper attempts (if any)? How was the opioid taper conducted? Individual
11. Why does the patient want to taper down or off opioids? Individual Abbreviations: COT – Chronic Opioid Therapy, MEDD - Morphine Equivalent Daily Dose, QOL - Quality of Life
Taper
Our previous sections have primarily focused on defining expectations and incorporation of facts learned from the investigation domain to build an opioid taper plan. The possible combinations of opioid doses, formulations, and taper schedules that can comprise an opioid taper plan are nearly infinite. The importance of individualizing opioid tapers cannot be overstated. Recall that taper failure does not imply patient failure. More often than not, opioid tapers fail because there is a flaw in the design that precludes success. The old adage goes, “the reed that does not bend in the wind will break”. This statement is certainly true when the philosophical lesson is applied to opioid taper plans. A common error that occurs during the course of pain medication management is the belief that creation of an initial opioid taper plan represents the final step in the course of care. In truth, the initial opioid taper plan represents only the beginning and ongoing active clinician engagement is the most important component of the taper domain (See Table 2).
5. Empower the patient. Motivational
6. Utilize available interdisciplinary pain management resources to support opioid reduction. Therapeutic
7. Establish monitoring plan and follow-up schedule to include evaluation of mood and suicidal ideation. Therapeutic
8. Provide motivational coaching as appropriate. Motivational
9. Maintain momentum of opioid reduction but anticipate plateau effect. Therapeutic
10. Emphasize patient achievement and success.Motivational
11. Asses for aberrant behaviors and opioid dependance/opioid use disorder. Therapeutic
12. Maintain flexible taper timelines. Therapeutic
13. Maintain flexible taper increments. Therapeutic
14. Focus on patient progress rather than end-goal. Motivational
What is your ExIT Plan?
As clinicians adopt deprescribing practices and initiate opioid tapers to reverse the opioid epidemic, we must recognize that oversimplification of taper plans can place patients at risk for adverse outcomes and taper failure. Optimal taper designs should take into account the complex pharmacological, physiological, and psychosocial circuitry that guides decision-making and drives patient-centered care plans. ExIT represents a simple mnemonic that provides both seasoned and new clinicians with a sequential and strategic approach to opioid tapers that addresses three key domains: Expectations, Investigation, and Taper. At the core of ExIT is prioritization of individualized patient goals and collaborative care plans. The path to success is a journey-What is your ExIT plan?
REFERENCES:
1. VA/DoD Clinical Practice Guideline for the Use of Opioids in the Management of Chronic Pain (updated 2022). https://www.healthquality. va.gov/guidelines/Pain/cot/VADoDOpioidsCPG.pdf
2. Oliva, E. M., Bowe, T., Manhapra, A., Kertesz, S., Hah, J. M., Henderson, P., Robinson, A., Paik, M., Sandbrink, F., Gordon, A. J., & Trafton, J. A. (2020). Associations between stopping prescriptions for opioids, length of opioid treatment, and overdose or suicide deaths in US veterans: observational evaluation. BMJ (Clinical research ed.), 368, m283.
3. Berna, C., Kulich, R. J., & Rathmell, J. P. (2015). Tapering Long-term Opioid Therapy in Chronic Noncancer Pain: Evidence and Recommendations for Everyday Practice. Mayo Clinic proceedings, 90(6), 828–842.
4. Kosten, T.R. and Baxter, L.E. (2019), Review article: Effective management of opioid withdrawal symptoms: A gateway to opioid dependence treatment. Am J Addict, 28: 55-62.
5. Krypotos AM, Effting M, Kindt M, Beckers T. Avoidance learning: a review of theoretical models and recent developments. Front Behav Neurosci. 2015;9:189.
6. Mendoza M, Russell HA. Is it time to taper that opioid? (And how best to do it). J Fam Pract. 2019;68(6):324-331.
7. Larochelle M, Lagisetty PA, Bohnert ASB. Opioid Tapering PracticesTime for Reconsideration?. JAMA. 2021;326(5):388-389.
Taper Purpose
1. Emphasize safety and benefits of tapering down opioids. Education
2. Explain applicable regulatory policies and clinical guidelines. Education
3. Individualize opioid taper plan. Therapeutic
4. Be prepared to manage withdrawal with rapid tapers. Therapeutic
8. Sharma N, Gupta V. Human Behavior In A Social Environment. [Updated 2021 Nov 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
WHY THE GALAPAGOS ?









ALPHA-GAL SYNDROME
by Nancy Yoon, MD,. MPH and co-author Kendra Findley, Administrator of the Division of Communicable DiseaseA recent Morbidity and Mortality Weekly Report (MMWR) from the CDC indicated that there is limited healthcare provider knowledge about Alpha-gal syndrome (AGS)¹. In a national survey of 1,500 healthcare providers, 42% were not aware of AGS, and 35% were not confident in their ability to diagnose or manage AGS patients. This is concerning, because the number of suspected cases is increasing, which is potentially life-threatening. Increased awareness by healthcare providers may facilitate more rapid diagnosis of AGS and improved patient care.
From 2010 to 2018, more than 34,000 suspected cases of AGS were identified in the United States². From 2017 to 2022, a total of 357,119 tests for alpha-gal-specific IgE were submitted to Eurofins Viracor lab, which was responsible for nearly all testing in the United States before 2022. ViracorIBT Laboratories in Lee’s Summit, Missouri developed the first FDA–approved alpha-gal IgE test commercially in 2010. 30.5% of people received a positive test result in the study period, and the number of people with positive test results increased from 13,371 in 2017 to 18,885 in 2021.

Alpha-gal Syndrome (AGS) is an IgE-mediated allergy and is characterized by delayed reactions after eating non-primate mammalian meat (e.g., beef, pork, lamb, venison, rabbit, etc.) or foods, medications and personal products that contain mammal-derived ingredients. AGS can be a challenging clinical diagnosis to make due to delayed reactions. Symptoms of AGS occur 4 to 6 weeks after tick bite, and 2 to 8 hours after exposure. AGS reactions can vary from personto-person. They can range from mild to severe or even lifethreatening with anaphylaxis. In addition, people may not have an allergic reaction after every alpha-gal exposure.
The primary cause of this allergy is the bite of the lone star tick. It is estimated that a tick must be attached to you for 24 to 50 hours to transmit the disease, and the risk of contracting AGS following a tick bite is between 1 and 3%. After being bitten by a lone star tick, some individuals may develop antibodies against the alpha-gal protein. It is estimated that cases of AGS are 32% higher in the Midwest than in other ar-


eas of the United States. In prior case studies, suspected cases predominantly occurred within the southern, midwestern, and mid-Atlantic U.S., which are areas where the lone star tick is known to be established.
IgE testing specific to alpha-gal should be done in tick-endemic areas in evaluation of cases of idiopathic anaphylaxis, recurrent urticaria and/or angioedema, as well as recurrent, episodic gastrointestinal symptoms of unestablished cause. In > 90% of cases, the diagnosis can be made based on a history of delayed allergic reactions after consuming nonprimate mammalian meat and a positive IgE antibody test to alpha-gal³.
Diagnosis
Confirmed laboratory evidence:
• Serum or plasma immunoglobulin E (IgE) specific to alpha-gal > 0.1IU/mL or > 0.1 kU/L. Higher levels of IgE do not correlate with severity of symptoms but do correlate with manifestation of symptoms⁴.
Presumptive laboratory evidence:
• An allergy skin test that demonstrates sensitivity or one or more mammalian meats or other mammalian-derived product.
Clinical Criteria:
• Acute onset of any one or more of the following allergic and/or gastrointestinal symptoms that occur 2 – 10 hours after ingestion of pork, beef, lamb, any other mammalian meat, or any mammalian-derived product OR within 2 hours after intramuscular, intravenous, or subcutaneous administration of alpha-gal-containing vaccination or medication:
o Abdominal pain
o Nausea
o Diarrhea
o Vomiting
o Heartburn/indigestion
o Hives
o Itching
o Anaphylaxis as diagnosed by provider
o Swelling of one or more of the following: lips, tongue, throat, face, eyelids, or other associated structures
o Shortness of breath
o Cough
o Wheezing
o Acute episode of hypertension
o The absence of a clear alternative diagnosis
Case Classification: The Council of State and Territorial Epidemiologists (CSTE) has established a case definition for AGS, and it may become a reportable condition5.
Suspect:
• Meets confirmatory laboratory evidence with no clinical information.
Probable:
• Meets clinical criteria AND presumptive laboratory evidence.
Treatment
As with management for any food allergy, AGS management is based on allergen avoidance. However, complete avoidance of mammalian-derived products can be challenging due to inadequate labeling. For < 10% of patients, avoidance of dairy and derivatives, as well as gelatin is also necessary to avoid allergic reactions. Due to numerous ‘hidden’ alpha-gal exposures beyond red meats (e.g. in foods, medications and vaccines) and the need for individualized guidance, referral to a dietician may be warranted.
There is no specific medical treatment for AGS. Recommendations for recovery include avoidance of further tick bites and no mammalian meat consumption. If followed, desensitization may occur between 8 months and 5 years. However, additional tick bites will reactivate allergic reactions or cause more severe reactions.
Prevention
The most effective way to prevent Alpha-Gal Syndrome is to avoid tick bites. When spending time outdoors, especially in wooded or grassy areas, wear long sleeves, pants tucked into socks, and closed-toe shoes. Applying a tick repellent to exposed skin and treating clothing with permethrin can also provide an extra layer of protection.
Perform thorough tick checks on yourself, your family, and pets after outdoor activities. Ticks can be tiny and easily missed, so paying attention to hidden areas like the scalp, behind the ears, and under the arms is crucial. If you see an attached tick, remove it immediately.
While the threat of Alpha-Gal Syndrome may create some caution, it’s important to remember that millions of people safely enjoy outdoor activities every year. By taking preventive measures and staying informed, you can minimize the
risk of tick bites and continue to relish the pleasures of nature without worry.

References
1. Carpenter A, Drexler NA, McCormick DW, et al. Health Care Provider Knowledge Regarding Alpha-gal Syndrome
— United States, March–May 2022. MMWR Morb Mortal Wkly Rep 2023;72:809–814. DOI: http://dx.doi.org/10.15585/mmwr. mm7230a1
2. Commins S. Diagnosis & management of alphagal syndrome: lessons from 2,500 patients, Expert Review of Clinical Immunology, 2020;16:7, 667-677, DOI: 10.1080/1744666X.2020.1782745
3. Thompson JM, Carpenter A, Kersh GJ, Wachs T, Commins SP, Salzer JS. Geographic Distribution of Suspected Alpha-gal Syndrome Cases — United States, January 2017–December 2022. MMWR Morb Mortal Wkly Rep 2023;72:815–820. DOI: http://dx.doi.org/10.15585/mmwr.mm7230a2
4. Binder A, Commins S, Altrich M, et al. Diagnostic testing for galactose-alpha-1,3-galactose, United States, 2010 to 2018. Ann Allergy Asthma Immunol 126 (2021) 411-416, DOI: https://doi.org/10.1016/j.anai.2020.12.019.
5. Alpha-gal syndrome (AGS) 2022 Case Definition. NNDSS. 9/19/2022. Retrieved from https://ndc.services.cdc. gov/case-definitions/alpha-gal-syndrome-ags/.
6. Alpha-gal Syndrome. CDC. 4/12/2022. Retrieved from https://www.cdc.gov/ticks/alpha-gal/index.html. VEL
THE FOOD CONUMDRUM: MANAGEMENT OF FOOD ALLERGIES IN THE 21ST CENTURY
By Minh-Thu Le, MD, FAAAAI, FACAAI, Allergy/Clinical Immunology, CoxHealth, Ferrell Duncan Clinic"The scariest 30 min of my life,” was what Brittany Mahomes wrote on her Instagram feed after a peanut allergy sent her and Patrick Mahomes’ eight month old son, Bronze, to the ER in August. Patrick Mahomes, arguably the best quarterback in the history of the Kansas City Chiefs, has also reported that he is allergic to most nuts, peanuts, and grass.
I had plans to publish this article with the last journal, but as timing would have it, a new food allergy diagnosis happen in the family of a very prominent and well-known athlete of this generation before I had the chance to finish it. But that timing also drives home a very important point of food allergy, that it is not uncommon, and that the lay press will always keep it in the forefront of people’s minds.
It might surprise you to know that the study of food allergies is a recent development, only being prominent in the past 30 years. Prior to the 1990’s there was a paucity of studies on food allergies. Whether it wasn’t seen much, or people just had the common sense to avoid their allergic foods and didn’t seek medical care for them, it’s really only since the 90’s that there became this contested “epidemic” of food allergies.
The National Institute of Allergy and Infectious Diseases (where Dr. Anthony Fauci, MD was director) expert panel defines food allergy as an adverse health effect arising from a specific immune response that occurs reproducibly on exposure to a given food. This definition is not limited to the IgE-mediated immune mechanism for “allergy.” On the other hand, food sensitization is the presence of IgE antibodies to a certain food, often in the absence of clinical symptomatology. As you can see, it is not surprising that there is some confusion in the mind of the lay public of what constitutes a food “allergy” versus a “sensitivity” or “GI intolerance” to foods, when “allergy” is defined by a national organization as ANY immunologic reaction and would include celiac disease or gluten intolerance. Sensitization to a food aligns with the IgE-mediated immune response, where a person may have antibodies, but they are not reactive when exposed to the food. However, this can be confusing for patients and physicians who see a “positive” test and their first response would be avoidance. I will talk about the dangers of avoidance in sensitized individuals later. For the purposes of this article, I will be speaking of the IgE-mediated, type 1 hypersensitivity response to foods that we understand could be life-threatening and cause anaphylaxis.
The NIAID has made food allergy research a public health priority due to an 18% increase in the reports of food allergy from 1997-2007. According to the NIAID, food allergy affects

about 8% of children and 11% of adults in the US. Other reports suggest that it is probably >1-2% but <10% of the total population. Selfreported allergy is higher at 12-13% versus about 3% in oral food challenge studies. Oral food challenge is still the “gold standard” in food allergy diagnosis, but difficult to accomplish. 85% of food allergies are due to peanut, tree nut, milk, eggs, soy, and wheat, and significant reactions also include seeds.
The emergence of the food allergy “epidemic” is quite contested, but probably started in 1990 when the British Medical Journal devoted several letters to the editor regarding the seriousness of peanut allergies and “sounded the alarm” so to speak. The US advocacy group Food Allergy Research and Education (FARE) was founded in 1991, and continues to be a very influential patient advocacy group today with many prominent and well-respected allergists on their board. Over the next two decades, the NIH and other organizations made it a priority to study food allergies. In 2010, a review noted that many reported “food allergies” are not allergies at all. (We are seeing this now with alpha-gal IgE-mediated beef and pork allergy, a newer food allergy diagnosis that has really only been known for the past 15-20 years. Many are being diagnosed, especially in our area, but may not really have symptoms suggestive of food allergy at all. They may be sensitized, but not actually allergic. Dr. Nancy Yoon has a timely article in this journal about mammalian meat allergy.)
In 2003, the American Academy of Pediatrics recommended a delayed introduction of highly allergenic foods, starting with cow’s milk at 12 months, eggs at 24 months and then nuts and fish at 36 months. This was based on epidemiological studies and was not grounded in any placebo-controlled studies (blinded studies are almost impossible with foods that have taste). Also, IgE RAST and immunocap testing marketed to primary care physicians to diagnose and treat food allergies allowed many sensitized individuals without allergic responses to be incorrectly labeled as food allergic. Research in the meantime showed a relationship between sensitization and the development or non-development of food allergy.
Epidemiological studies previously suggested that early introduction to allergic foods was what contributed to allergen sensitization. We now know how false that tenet was. Most agree that it is the dysfunction of the skin-gut mucosal barrier that is the predominant cause for allergic sensitization. (I want to stop here and remind everyone that sensitization is NOT allergy.) There is likely a role for antibiotics in infancy
and childhood disruption of the gut biome and disruption of the skin barrier with atopic dermatitis causing sensitization as well.
So how do you go about diagnosing food allergies? You could do a blood test in your clinic. The PhadiaTM Immunocap system (ELISA test for IgE) is highly specific and sensitive for food IgE. It gives a number from 0 to >100 kUA/l and also a class from 1 to 6 based on the likelihood someone may have a food allergy (Table 1). Notice I said “likelihood,” because a history of a reaction is the other half of the equation. A positive test in the absence of clinical symptoms is not enough to diagnose allergy. If one is unsure of the diagnosis, we have friendly and knowledgeable board-certified allergists in our community that can be consulted to help or do a food challenge to confirm. As allergists, we typically do a thorough history, percutaneous skin testing (which is arguably more sensitive) and counsel on the pros and cons of testing and avoidance. We are leaning towards not avoiding foods more and more, even if positive, if they are tolerated and not causing life-threatening anaphylaxis. If a history of anaphylaxis is encountered, allergists will also preferentially use the IgE immunocap test to decrease risk of anaphylaxis from skin testing in office. We would not do skin intradermal testing for foods for this reason.
I’d like to segue for a minute and talk about Bronze Mahomes and why he had a reaction at eight months. Didn’t I just say that the AAP recommends not to eat peanuts and nuts until 36 months? They did, up until 2019, when the recommendations changed after some very good studies indicating that we had it all wrong about early introduction of foods. In 2005, the NIH established The Consortium for Food Allergy Research (CoFAR), a group of allergy research centers with this current four-fold mission:
ry antibody associated with allergic reactions
• To identify the genes associated with food allergy
We now have studies showing that there is a natural progression of the resolution of food allergies, and also studies on the oral and epicutaneous desensitization of food allergies. For milk and egg allergy, about 50% of children will outgrow their allergy by 63 and 72 months, respectively.

• To identify the mechanisms underlying the development of new food allergy and the mechanisms of loss of food allergy (i.e., emergence of oral tolerance to food allergens)
• To develop immune intervention strategies for the treatment of food allergy
• To identify the role of food allergy in eosinophilic esophagitis (EoE) and compare the genetic markers of EoE with those of food allergy, like immunoglobulin E, the prima-
However, the paradigm-shifting study on early food introduction was published in 2015-2017, through the LEAP and LEAPON studies. Learning Early About Peanut (LEAP) was a landmark study published in the New England Journal of Medicine that compared a total of 640 Jewish children in Israel versus Jewish children in Europe, introducing these infants to a peanut-coated snack common in Israel from 4-11 months of age. They were to eat 6 grams of peanut protein a week (about 3-4 roasted peanuts). They found strikingly significant results that even in infants (and all had eczema, egg allergy, or both) who were already sensitized to peanut with a positive skin test, prevalence of allergy was 35.3% in the avoidance group at 60 months of age, and only 10.6% in the consumption group. For a negative skin test cohort, peanut allergy was seen in 13.7% in the avoidance group, versus only 1.9% in the consumption group. This substantiated the hypothesis that late introduction of peanut in infancy contributes to the development of peanut allergy. This should make sense on a biochemical/ immunological level as well. Infants and the infant immune system are constantly trying to distinguish self from non-self, as they are introduced to a myriad of bacteria, viruses, fungi, and would-be allergens that older immune systems are already desensitized or immune to. Waiting too long may be more detrimental because the immune system has already distinguished harmful non-self from not-harmful non-self by the time the food is introduced. This makes the immune system do a double take, like, “Where have you been all my life?” and “Why are you just here invading me now?” to “You must be harmful to me if I’m just seeing you now!” Now, there is a more elegant immunological reason for this, the loss of tolerance, introduction of food allergens through the skin barrier verses the gut mucosa, Th2-mediated cytokines, dendritic cell and t-cell
interactions, but I’ll spare you the details.
PACE’S POST
The LEAP-ON study took 556 children from the LEAP trial and continued to see the effect of avoidance for another 12 months. Significantly more prevalent allergy was noted in the peanut-avoidance group as well (18.6% vs 4.8%).
Prevention of other food allergies was the goal in the Enquiring About Tolerance (EAT) study, also published in 2015, with early peanut and egg early introduction being significantly associated with lower prevalence of peanut and egg allergy in that cohort.
Cow milk protein is typically introduced in infancy within a couple weeks of birth. Infants who are introduced to cow’s milk at 6 months or older have the highest risk for adverse reaction according to data from 1300 children in the Boston area born between 1999-2002.
We should now be comfortable with early introduction of peanut, egg, and milk in our practices and with recommending this to families who would want to decrease the likelihood of food allergies in their children.
But what about treatment? It sounds like Bronze was introduced to peanuts pretty early (4-6 months would have been what I would have recommended), so it looks like they followed the new AAP guidelines (we don’t actually know when he was introduced, if it was at the right dosing, or if his first introduction may have caused a reaction). He would have been part of the 10% in the LEAP study that still developed allergy even though introduced to peanut early. Is Baby Mahomes destined to a life of avoidance of peanuts and possibly other nuts like his father? Luckily for him, research has gotten to a point where there is a viable and very successful treatment option, Oral Immunotherapy (OIT). Whether or not they pursue this option remains to be seen, but as a mother of a peanut and tree nut allergic child and an allergist treating several children with OIT, I have witnessed firsthand what a life-changing option this is for individuals and their families.
Dr. A. Wesley Burks, then of Duke University and currently at UNC-Chapel Hill, published his landmark study with Dr. Stacy Jones, of the University of Arkansas Medical School, on peanut desensitization in 2009, and since then numerous academic allergists have followed. (Fun fact: Dr. Burks’ father taught at Drury College when he was a child, and he lived in Springfield for a time. I only know this anecdote from an interview with Dr. Burks when I was applying for allergy/ immunology fellowship.) He saw that he could desensitize individuals to 3.9 grams of peanut protein and keep them at a 1.8 gram maintenance dose allowing patients to freely eat peanuts.
PalforziaTM is the first and only FDA-approved food product available for food allergy desensitization at this time. It is peanut protein, measured for accuracy of dosing and pre-
scribed by allergists in conjunction with desensitization visits in office every two weeks to updose. Palforzia is not meant to be used for full desensitization but only to 300 mg a day for accidental food ingestion to decrease risk of anaphylaxis. Many private allergy practices are using commercial peanut protein to accomplish the same thing and some to full desensitization as well. There are protocols published through studies from 300 to 3000 mg of peanut protein, with the latter amount affording patients the option of eating peanuts freely. Studies on sustained unresponsiveness have landed on keeping at least 300 mg of protein in the diet daily to continue to be desensitized. Interestingly, studies show that desensitization is effective when started prior to 18 years of age, but not typically after this age. Also, I should mention that OIT does come with the inherent risk of anaphylaxis and potentially EoE. Evidence-based guidelines coming out of Europe endorse the use of OIT in the treatment of milk, peanut, and egg allergy for children over four years of age. The US is still debating exactly how this will look in practice here, especially in light of FDA versus non-FDA approved products. ViaskinTM is another treatment that is pending FDA-approval. Remember the CoFAR group? This product is being studied by them through the NIH. This epicutaneous patch is a novel way to introduce the allergen through the skin and therefore induce tolerance to a very small amount, which may be encountered on accidental exposure. It has had some problems getting approval, with <50% efficacy in studies. However, it is close, so studies are ongoing. You can imagine that with people with eczema and other skin issues, this option would be more difficult. It does seem that anaphylaxis risk is lower. It also gets past the natural taste aversion to allergenic foods that most OIT patients have.
Other novel approaches for the treatment of food allergies include the use of sublingual immunotherapy, placed under the tongue. A toothpaste phase 1 trial with a similar idea of introducing peanut protein through the oral mucosa is in process and may minimize the risk of EoE. An IV delivered nano-particle encapsulated purified peanut protein extract (CNP-201) study is also currently underway. By shielding the peanut antigen from recognition by IgE and other mediators within a nanoparticle matrix, investigators aim to prevent allergic reactions while the allergen is in circulation and present allergen to naïve T cells in a tolerogenic environment in the liver and spleen. Biologics are everywhere, and also in the treatment of food allergy. Omalizumab, an IgE monoclonal antibody that prevents IgE crosslinking on mast cells and basophils, thereby inhibiting degranulation and release of allergic and anaphylactic mediators from those cells, shows promise when started in conjunction with food protein in the early steps of OIT to decrease anaphylaxis during OIT. It is also being studied as monotherapy in CoFAR studies to quantify dosing and frequency. A study in 2018 already established that peanut allergy patients could
tolerate more protein after an Omalizumab injection than prior to injection. Dupilumab, an IL-13 and IL-4 receptor antagonist, is being used to study milk OIT and also in a combination study with Omalizumab for concomitant allergen OIT and the induction of sustained unresponsiveness.
Management of food allergies in the 21st century is much more advanced and looks entirely different than in the 20th century. Where late introduction of highly allergenic foods and avoidance of allergic foods was advocated, we have replaced this with early introduction and desensitization. More and more foods will be available for desensitization to younger and younger patients in the future. It is an exciting time to be in the field of allergy, and new treatment options for food allergy will remain in the forefront of this specialty.
References:
1. Patrick Mahomes’s Infant Son Was Brought to ER Thursday, Wife Brittany Says. https://www.si.com/nfl/2023/08/18/patrickmahomes-infant-son-emergency-room-wife-brittany
2. Karen M. Switkowski PhD, MPH, et.al. Cow’s Milk Protein Introduction and Childhood Adverse Reactions to Cow’s Milk. JACI: InPractice. Vol.10 (10):2713-2721.e2. October 2022.
3. AAP NEWS: Dietary interventions to prevent atopic disease: Updated Recommendations. March 2019. https://www.aappublications.org/news/2019/03/18/atopy031819
4. Addendum Guidelines for the Prevention of Peanut Allergy in the United States. January 2017. https://www.niaid.nih.gov/ sites/default/files/peanut-allergy-prevention-guidelines-clinician-summary.pdf\
5. AR101 Oral Immunotherapy for Peanut Allergy. The PALISADE Group of Clinical Investigators. N Engl J Med 2018; 379:1991-2001. https://www.nejm.org/doi/full/10.1056/NEJMoa1812856
6. Bird, JA, et. al. Prevention of food allergy: Beyond peanut. JACI. Vol 143 No 2: 545-547. Feb 2019.
7. Centers of Disease Control website: Food allergy. www.cdc. org.
8. Du Toit George, et. al. Effect of Avoidance on Peanut Allergy after Early Peanut Consumption. https://www.nejm.org/doi/ full/10.1056/NEJMoa1514209
9. Du Toit George, et. al. Randomized Trial of Peanut Consumption in Infants at Risk for Peanut Allergy. https://www.nejm.org/ doi/full/10.1056/NEJMoa 1414850
10. FARE website: www.foodallergy.org ; https://www.foodallergy.org/sites/default/files/migrated-files/file/facts-stats.pdf
11. Sampson, Hugh A and Randolph, Christopher, chief editors. Food allergy: A practice parameter update – 2014. https://www. aaaai.org/Aaaai/media/MediaLibrary/PDF%20Documents/Practice%20and%20Parameters/Food-Allergy-A-Practice-Parameter-Update-2014.pdf
12. Hemmings, O. et.al. Basophil Activation Test: Old and New
Applications in Allergy. Curr Allergy Asthma Rep. 2018; 18(12): 77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6244909/
13. Simpson EL et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014 Oct; 134(4): 818–823.
14. Phadia Immunocap allergy blood testing. https://nrl.ae/public/uploads/downloads/ImmunoCAP%C2%AE_allergy_blood_ testing_lowres.pdf
15. Waggoner, MR. Parsing the Peanut Panic: The Social Life of a Contested Food Allergy Epidemic. Soc Sci Med. 90: 49–55. Published online 2013 May 6. doi: 10.1016/j.socscimed.2013.04.031
16. Wassermann, RL, et.al. Real-World Experience with Peanut Oral Immunotherapy: Lessons Learned From 270 Patients. JACI: In Practice. Volume 7, Issue 2, Pages 418–426.e4 Feb 2019. https://www.jaci-inpractice.org/article/S2213-2198(18)30345-3/ abstract
17. Wood RA. Oral Immunotherapy for Food Allergy Pediatric Allergy and Immunology. J Investig Allergol Clin Immunol. Vol. 27(3): 151-159. 2017.
18. Zeiger, RS, MD, PhD. Food Allergen Avoidance in the Prevention of Food Allergy in Infants and Children. PEDIATRICS. Vol. 111 No. 6 June 2003.
19. Arianna Cafarotti, et.al. Management of IgE mediated food allergy in the 21st century. Clin Exp Allergy. 53(1): 25–38. Jun 2023. Published online 2022 Oct 19. doi: 10.1111/cea.14241
20. Sayantani B. Sindher, et.al. Food allergy, mechanisms, diagnosis and treatment: Innovation through a multi-targeted approach. Allergy: European Journal of Allergy and Clinical Immunology. 22 June 2022 .
21. Guilliminault, L, et.al. Combining Anti-IgE Monoclonal Antibodies and Oral Immunotherapy for the Treatment of Food Allergy. Clin Rev Allergy Immunol. Feb; 62(1):216-231. E-pub 22 Sep 2021.
YOU!
The editorial team would like to thank all our members, Cox and Mercy hospitals and all our advertisers for supporting the GCMS Journal! We could not do this without you!
Membership “A” Denotes GCMS Applicant
GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq directory
Eye Surgery/Ophthalmology
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H
Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H
Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804
Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
Eye Surgery/Ophthalmology
MATTAX • NEU • PRATER
EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H
American Board of Ophthalmology
LEO T. NEU III, MD, FACS H
American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
Dermatology, Procedural
MICHAEL H. SWANN, MD H
AUTUMN COURTNEY, PA-C
PATSY DUGGAN, PA-C
WESLEY N. WORMINGTON, PA-C
3850 S. National Ave, Suite 705 Springfield, MO 65807
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine
www.ascentdpc.com
417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
THOMAS PRATER, MD, FACS H
American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H
American Board of Ophthalmology
BENJAMIN P. HADEN, MD H
American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
LESTER E. COX
FAMILY MEDICINE RESIDENCY PROGRAM
FAMILY MEDICAL CARE CENTER
1423 N. Jefferson B 100 Springfield, MO 65802 (417) 269-8817
AmericAn BoArd of fAmily PrActice
Cameron Crymes, MD
Kristi Crymes, DO
Gabrielle Curtis, MD
Katie Davenport-Kabonic, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Michael Kabonic, DO
Jessica Standeford, MD
Audrey Williams, DO
Brian Williams, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
VANESSA MCCONNELL,
ERIC P. GUILLIAMS, MD, FACS H
American Board of Urology
ROBERT D. JOHNSON, MD, FACS H
American Board of Urology
TYRUN K RICHARDSON, MD
American Board of Urology
MARK J. WALTERSKIRCHEN, MD, FACS
American Board of Urology
Internal Medicine
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
Nephrology

SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100
www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
Neurosurgery
SPRINGFIELD
NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700
Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
BLAKE MARTIN, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
BILL HAMPTON, ANP-BC
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
Obstetrics/Gynecology
COXHEALTH
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
Obstetrics/Gynecology
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology
909 E. Montclair, Suite 120
Springfield, MO 65807
Phone 417/882-4466
• Fax 417/890-5631
Oncology/Hematology
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic
3850 S. National, Ste. 600
Springfield, Missouri 65807
Monett Clinic
802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880
Fax 882-7843
Visit our website: www.ohaclinic.com
Rheumatology
417 RHEUMATOLOGY
Independent rheumatology care and infusion services
DAVID TRUE, DO, FACR H
Board Certified in Internal Medicine and Rheumatology by American Board of Internal Medicine
Phone 417-501-2644
Fax 877-540-0429
909 E. Republic Rd., Building D200
Springfield, MO 65807 www.417ra.com
Otolaryngology
MERCY CLINIC–
EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
A. DANIEL PINHEIRO, MD, PhD, FACS H
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP
Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750
Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
Plastic Surgery
MERCY CLINIC–
FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS
American Board of Facial Plastic & Reconstructive Surgery
American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
Psychiatry
JAMES E. BRIGHT, MD H
Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804

CONNECTED.
We believe when we work together, big change happens. Families get healthier. Communities grow stronger. Lives change. Right now, side by side, our providers are shaping our future –strengthening it and making it a little bit brighter for everyone. coxhealth.com 417-269-INFO

When neighbors help neighbors, it makes all the difference.

