

Power-PRO™ 2
The industry’s first connected ambulance stretcher
Discover Smart Equipment ManagementTM (SEMTM with dashboard access through LIFENET® Care
View stretcher diagnostics and remotely manage your fleet through a single dashboard, accessible through LIFENET Care.
Fleet Insights
• View stretcher activity and usage patterns
• Access stretcher analytics, including button press count, motor run time and lift statistics
• Ability to track battery usage on individual stretchers and expert data to analyse trends For more information contact your local Stryker Representative.
Status Updates
• Monitor fleet activity to help identify when stretchers may require review or maintenance
• Access diagnostic tools which can identify potential issues ahead of servicing
• Option to connect directly with ProCare for repair requests
Service Tools
• Access battery status and key device information
• View the last-known stretcher location of your fleet when connected*
• Review equipment usage metrics, fault types, temperature metrics and more





Dear friends and colleagues,
As spring settles across Australasia, it brings with it a quiet sense of renewal — a reminder of growth, care, and connection. These themes echo through this edition of FIRST, which celebrates the people and progress shaping our sector today.
We are honoured to feature an exclusive conversation with Her Excellency the Honourable Sam Mostyn AC, Governor-General of Australia, whose reflections on leadership and care resonate deeply with our community. Her lifelong commitment to equity, sustainability, and the well-being of those who serve others offers inspiration to us all, particularly as she champions careers grounded in purpose and care, from the frontlines of health to community service.
In this issue, we shine a light on First Nations leadership, sharing the stories of Michelle Crilly (Ambulance Victoria), Yvonne Gemmell (Wellington Free Ambulance), and Trent Jackson (Queensland Ambulance Service). Their voices remind us that the path toward equity in healthcare begins with listening, learning, and walking together — one conversation, one program, and one act of leadership at a time.
Looking to the horizon, we highlight a defining step toward a sustainable future: the introduction of the world’s first fully electric ambulance vehicles, now in service in Denmark, British Columbia (Canada), and right here in Aotearoa New Zealand at Hato Hone St John. These trailblazing efforts symbolise both courage and responsibility — showing what’s possible when innovation meets care for people and our planet.
This edition celebrates our Women in Leadership Scholarship finalists and features a heartfelt reflection from Justine Fletcher of St John WA, last year’s winner. Her journey through coaching and professional development captures exactly what this scholarship was designed to achieve; confidence, clarity, and connection that ripple far beyond one person’s experience.
As we reflect on the energy and ideas shared at our CAA Congress and IRCP Conference in Adelaide, we look forward to the 2025 Women in Leadership Symposium in Brisbane, where many of these conversations will continue to evolve.
This issue is, as always, a celebration of our shared purpose - to serve with compassion, lead with integrity, and care for those who care for others.
Love xx

Mojca Bizjak-Mikic Editor in Chief Chief Executive, CAA (Interim)




26
Opinion First
Hear from Justine Fletcher on her year as the 2024 CAA Women in Leadership Scholarship winner.
Data First
Read the latest Patient Experience Survey and Women in Ambulance Survey.
08 Industry First
The latest news from across the Australasian Ambulance Health Sector.
10 CAA First
Didn't make it #CAACongress25?
See what happened across the premier CAA event.
16 Focus First
First Nations voices in the ambulance sector across Australasia.
28
Services First
Showcasing the latest projects and achievements from across CAA member services.
35
Awards First
Meet the finalists of the Women in Leadership Scholarship and learn about two winners of the CAA Awards for Excellence.
44 Feature First
FIRST speaks with Her Excellency the Honourable Ms Sam Mostyn AC, Governor-General of the Commonwealth of Australia.
48 Events First
Have a look at where you'll find the CAA in 2026 along with wrap ups of Restart a Heart Day and IRCP 2025.



54 Partners First
In this edition of FIRST, we share updates from the Australasian College of Paramedicine, National Rural Health Alliance and TLC for Kids.
62 Research First
Sharing the latest innovative research projects from around the ambulance world.
70 Sustainability First
Learn about EV Ambulances in British Columbia, Denmark and New Zealand.
78 People First
Meet some of the wonderful people that make up the Australasian Ambulance services.
80
Leadership First
Introducing our newest column with Dr Erica Kreismann of OneWild Coaching
TEAM
Editor: Mojca Bizjak-Mikic
Relationship and Content Manager: Kieren Vartuli
Editorial Team: Courtney Waters & Gabrielle Anand
Publication Design: Kade Marsh, Alpha State
The Directory
PUBLISHED BY:
The Council Of Ambulance Authorities Inc
2/141 Sir Donald Bradman Drive Hilton SA 5033 Australia admin@caa.net.au
Magazine published from paper that is sustainably sourced.
Patient Experience Survey
The Council of Ambulance Authorities’ 2025 Patient Experience Survey once again highlights the strong trust and satisfaction that communities across Australia, New Zealand, and Papua New Guinea place in their ambulance services.
With consistently high scores across overall satisfaction, call-taking, response times, and quality of care, the findings provide clear evidence of the professionalism, compassion, and commitment of ambulance staff.

The survey results not only affirm the high standards of care provided but also reveal year-on-year improvements, particularly in Papua New Guinea, where patient satisfaction and confidence levels have risen significantly.

Women in Ambulance Survey
The Council of Ambulance Authorities’ 2025 Women in Ambulance Survey provides the most comprehensive picture yet of the experiences, challenges, and aspirations of women working across ambulance services in Australia, New Zealand, and Papua New Guinea.
With 1,176 responses from eleven member services, the survey highlights both the progress made and the areas where further change is needed. Women now make up 55% of the ambulance workforce, a 2% increase since 2022, with representation in executive roles rising to 44%.
While these shifts signal positive momentum, the findings also underscore the importance of continued focus on leadership development, mentorship, workplace flexibility, and support for women’s health to build a more inclusive and equitable sector.
Industry News

Ambulance Tasmania
Specialist Australian Aviation provider, StarFlight has been announced as Ambulance Tasmania’s new provider of air emergency helicopter services.
The organisation will partner with Ambulance Tasmania (AT) and Tasmania Police to provide aeromedical retrieval, search and rescue, and aerial law enforcement capabilities across the state.

Hato Hone St John
Hato Hone St John welcomes the introduction of the new Device Location Information (DLI) service, which expands on the existing Emergency Caller Location Information service, enhancing the ability of emergency services to rapidly locate individuals in life-threatening situations.
The DLI capability, announced by Minister of Police Mark Mitchell, allows emergency services to access the approximate location of a person’s mobile device, even when they haven’t called 111, when there are serious concerns for their safety or health.

Ambulance Victoria’s Reconciliation Working Group recently visited the Victorian Aboriginal Health Service (VAHS) in Fitzroy.
They learnt how Aboriginal Community Controlled Health Organisations (ACCHOS) work and the challenges they face compared to mainstream services.
This visit was part of their ongoing commitment to listening, learning and walking alongside Aboriginal communities.

NSW Ambulance
NSW Ambulance is proud to announce that the Newcastle community will be safer this bushfire season, thanks to the ongoing Hazardous Area Rescue Ambulance (HARA) training for specialist paramedics in the region.
Regular HARA training ensures their highly trained special operations paramedics are prepared to act in the toughest environments.
The fleet of eight new HARAs was launched by Minister for Health Ryan Park in October 2024, as part of a $14.8 million package to further build the state’s flood rescue capabilities.
Ambulance Victoria

Queensland Ambulance Service
A small but mighty team has developed an entirely new approach to the way Queensland Ambulance Service supports remote Aboriginal and Torres Strait Islander Communities in Cape York.
Deputy Commissioner Rural and Remote Operations Kari Arbouin said the Project was established to improve coverage across the Cape, integrating where possible with health clinics to provide greater access and safety across the numerous communities.

St John WA
St John WA’s Michael Eppen has been named a finalist for the 2025 Worksafe Work Health and Safety Excellence Awards for Health and Safety Representative (HSR) of the Year.
Michael is the Health and Safety Representative for St John WA’s busy Fleet and Radio Team. His proactive approach has directly contributed to creating a safe environment for team members, contractors, and visitors.
Since taking up the role, Michael has quickly made exponential changes in the workplace with a focus on traffic management improvements across multiple sites.

St John Ambulance Australia (NT)
St John NT is celebrating a record year of volunteer service, with dedicated Territorians delivering 20,909 hours of first aid support across 672 public events in the 2024-25 financial year, contributing an estimated $1.05 million in community value.
To build on this momentum and support the Territory’s ever-growing calendar of events, St John NT is inviting more locals to join its volunteer team through a new recruitment drive, Be the Difference. The campaign aims to welcome at least 40 new volunteers this year.
CAA CONGRESS WrapUp
Another CAA Congress has come and gone, and we at the CAA are incredibly grateful for those who help make this a must-attend event each year. This year's CAA Congress was officially the biggest, and we’re excited to continue to grow in the coming years.
The 2025 CAA Congress was held in Adelaide, South Australia, from 19 to 21 August at the Adelaide Convention Centre (ACC), and once again connected ambulance and emergency sector leaders, innovators and professionals from across the globe.
CAA Congress remains one of the most significant events on the ambulance sector calendar, as it continues to hold exciting social and networking events partnered with thought-provoking keynote speakers and presentations.
The three-day event consisted of presentations on various themes, including Cyber Security, Safety of Our People, The New Patient, Diversity and Inclusion and much more. With presenters from across Australasia and beyond, the presentations were incredibly insightful for attending delegates and visiting guests.
Alongside these themes was a bustling expo floor where industry stalwarts, leaders and newcomers showcased and demonstrated their innovative solutions to potentially common sector challenges. The expo floor was not only for businesses; the SA Ambulance Service also showcased its use of Virtual Reality (VR) and a driving simulator in its program— a truly eye-opening experience
The beginning of the CAA Congress was the ORH Welcome Function in the stunning foyer of the ACC overlooking the River Torrens, where delegates gathered in a relaxed environment to enjoy some light refreshments and canapes, while connecting with old friends and making new ones.




Day 1 kicked off with a delicious networking breakfast presented by Hexagon, fuelling delegates before the first plenary sessions. Former City of Adelaide Lord Mayor Stephen Yarwood was the first presenter to take the stage, addressing the potential of artificial intelligence in reshaping the sector and relevant medical industries.
Cyber Security was the first theme for delegates, as Assistant Commissioner (AC) of Cyber Command, Richard Chin, delivered an informative presentation surrounding how cyber criminals can and have targeted the health sector. While discussing this, he highlighted the requirement and significance of reporting incidents. A truly informative presentation, AC Chin left delegates with some knowledge of what to think about with newly released technologies.


With a plethora of concurrent sessions available, delegates had the opportunity to explore themed presentations delivered in a variety of styles. A truly valuable experience.
One recurring topic of discussion across the global ambulance sector is the psychological safety of our people. This theme featured outstanding presentations from Jason Killens, Chief Executive of London Ambulance Service; Sally Moton, Partner and Practice Group Leader at Lander & Rogers; and Todd Wehr, Director of Queensland Ambulance Service’s Priority One program.
They covered critical topics including sexual safety and harassment in the workplace, as well as psychological resilience in frontline roles.
Running alongside the CAA Congress was the coveted CAA Awards for Excellence. This year, the historic Adelaide Oval served as the venue, adding another chapter to the CAA’s storied history With close to 50 submissions across the six award categories, judges had yet another rigorous task to find the worthiest winners. Ultimately, Ambulance Victoria, St John WA, SA Ambulance Service and the National St John Ambulance Service of Papua New Guinea were victorious. After an evening full of wonderful memories, the National St John Ambulance Service of Papua New Guinea were handed the ultimate prize of the evening, the Star Award.
With the 2025 CAA Congress behind us, we look forward to 2026, where we partner with ACT Ambulance Service to hold CAA Congress in Canberra.
More details surrounding #CAACongress26 will be released soon. Be sure to follow the CAA on social media for the most up-to-date information surrounding the event.

Discover. Connect. Thrive. Belong to our College community.
As a member, you’ll gain access to a powerful network of support, education, and advocacy designed to help you thrive in your profession.
Your Membership supports you with:
FREE high-quality, industry-informed CPD content
Podcasts – learn on the go with expert insights and inspiring stories
Advocacy for more career opportunities, workforce flexibility, recognition of capabilities, health and wellbeing
Self-paced eLearning, webinars and podcasts
Access to College education and research grants
Research opportunities and mentoring programs
Our FREE CPD tracker
Conferences and events
Professional practice programs for career progression
Student study resources

Artist: Annika Leslie - South Australian local artist and SA Ambulance Service Paramedic
STRENGTH & Voices of
CONNECTION
Honouring First Nations leadership across our ambulance services
Across our ambulance sector, First Nations leadership is shaping a more connected, inclusive, and culturally safe future. The stories shared in this FIRST Magazine Focus section offer a glimpse into the lived experiences, wisdom, and determination of First Nations people who are helping our services better understand and serve their communities.
Creating culturally safe and inclusive ambulance care is not a single initiative — it’s an ongoing journey of reflection, respect, and partnership. It’s about ensuring that every patient, colleague, and community member feels seen, understood, and valued. For our services, that means embedding cultural safety into systems, education, and everyday practice, while recognising the powerful role of First Nations voices in leading that change.
Across the sector, this progress happens in many forms — one conversation, one program, and one act of leadership at a time. Their stories remind us that the path toward equity in healthcare begins with listening, learning, and walking together.
This FIRST Magazine Focus section celebrates three remarkable individuals — Michelle Crilly from Ambulance Victoria, Yvonne Gemmell from Wellington Free Ambulance, and Trent Jackson from Queensland Ambulance Service — who each bring courage, authenticity, and cultural wisdom to their work. Their stories reflect different journeys, yet they share a united purpose: to ensure First Nations peoples are seen, respected, and supported in every aspect of care.
In May 2024, the Council of Ambulance Authorities (CAA) established the Diversity, Inclusion & Belonging Forum, bringing together representatives from across Australasia to share knowledge, strengthen collaboration, and champion initiatives that foster belonging. One of the Forum’s first priorities has been connecting First Nations leads and showcasing the outstanding work being done across our member services.
Together, these stories remind us that cultural safety is not an initiative, but a shared responsibility — one that belongs to all of us. Inclusion begins with understanding, and the strength of our sector lies in its people: in their diversity, their leadership, and their willingness to learn and grow together.
Providing Culturally Safe Ambulance Care
Michelle Crilly, Aboriginal and Torres Strait Islander Program Lead, Registered ALS Paramedic, Ambulance Victoria

My name is Michelle Crilly, my pronouns are she/her, and I am a proud Yorta Yorta woman. I am currently the Aboriginal and Torres Strait Islander Program Lead at Ambulance Victoria (AV) and I am a registered ALS paramedic.
As a proud advocate for my community, I am deeply committed to driving meaningful change in Aboriginal and Torres Strait Islander health. My passion is rooted in lived experience and a strong desire to create pathways for healing, empowerment, and equity.
I work to amplify First Nations voices, promote culturally safe practices, and influence policy and programs that honour our traditions, strengths, and aspirations. Through collaboration, leadership, and advocacy, I strive to ensure our communities thrive physically, emotionally, and spiritually.
My journey with AV began in 2017 as an Aboriginal Cadet while studying paramedicine. AV’s Cadet Program supported Aboriginal and Torres Strait Islander students through university and into their careers – offering funded placements, mentoring, and a pathway to increase representation in the ambulance service. Once my studies were complete, I began my graduate year with AV in 2018, and in 2019, became a registered Advanced Life Support paramedic working in Metropolitan Melbourne.
In 2022, I applied for and was appointed to the role of Aboriginal and Torres Strait Islander Program Lead at AV, a decision shaped by my experiences with racism and a vision for equitable, culturally safe healthcare. My goal is for Aboriginal and Torres Strait Islander peoples across Victoria to have access to world-class, responsive pre-hospital care grounded in self-determination and respectful partnerships.


In this role, I’ve proudly contributed to the development and launch of AV’s Reflect Reconciliation Action Plan (RAP), which laid the foundation for sustainable, longterm change. The relationships built through this process continue to guide our reconciliation journey and shape our actions.
One of my proudest achievements has been leading the initiative to make it mandatory for operational staff to ask every patient, where practical, if they identify as Aboriginal and/or Torres Strait Islander. This was a first for AV and a significant step toward reconciliation. Culturally safe care begins with understanding identity; this cannot be assumed, it must be respectfully asked. Collecting this data assists in identifying health disparities, informs targeted services, and monitors progress in improving patient outcomes.
My early career was marked by personal and cultural challenges. As a graduate paramedic, I often felt disconnected from my community and struggled to access my culture. One of the hardest lessons was learning to lead on scene, especially when directing senior colleagues. In my culture, Elders are deeply respected, and giving instructions felt uncomfortable. I had to learn to balance cultural values with professional responsibilities – navigating both worlds with integrity.
Driving cultural change is a long-term commitment. It requires persistence, thousands of conversations, and consistent advocacy. Progress can be slow, but it is built on trust, relationships, and sustained action. I encourage others to reflect on how they can contribute to meaningful change and remove barriers.
For me, coming to work each day is so much more than a job. Every day, it’s a chance to represent my people, honour our stories, and shape a future where our communities are strong and respected.
Elevating Aboriginal and Torres Strait Islander voices in healthcare is essential. Culturally safe care, delivered by our people, builds trust, improves engagement, and leads to better health outcomes.
Empowerment is the foundation of culturally safe care; it’s about shifting power, embedding cultural governance, and celebrating culture as a source of healing.
As we move forward, reflection is key. By learning from our challenges and insights, we can build a more inclusive, respectful, and culturally safe future, one that honours the voices, histories, and contributions of Aboriginal and Torres Strait Islander people.

Embedding te Ao Māori in Emergency Ambulance Care
Yvonne Gemmell, WFA Head of Maori and Equity (Kaihautu), Patient Transfer Officer, Peer Supporter
Yvonne Gemmell has worked for Wellington Free Ambulance for nearly 13 years, beginning as an Emergency Medical Call Taker and moving through the Patient Transfer Service and leadership roles.
Alongside this professional journey, she has carried her identity, culture, and responsibilities as a wahine Maori (Maori woman). This dual journey has shaped the path she has taken, the challenges she has faced, and the vision she holds for a more inclusive and culturally safe sector.

Her personal experiences have deeply influenced her work. In 2014, Yvonne lost both her Mum and Nana to cancer. Reflecting on their care, she saw not only the inequities in health services, but also the gaps in supporting culturally safe care for patients and their wh-anau (family). These lessons sharpened her focus: the ambulance sector, too, had work to do. She noticed unconscious bias in the system, cultural needs misunderstood, and times when she carried extra emotional labour such as educating colleagues, translating tikanga (custom) into ambulance practice, or softening the edges of conflict.
Over time, Yvonne learned that cultural perspective is not ancillary, it is central to equitable care, for Maori and for all. When ambulance teams understand Maori worldviews such as wh-anau-centred care, the dimensions of Maori health models, and relational approaches, they can deliver safer, more compassionate care. Mentoring colleagues, providing cultural input, and embedding Te Tiriti o Waitangi principles into Wellington Free Ambulance’s work have been pivotal to creating change.


At Wellington Free Ambulance, this vision has grown into action. They now provide all new staff with cultural competency and safety training, ensuring they understand tikanga, Te Tiriti o Waitangi (the Treaty of Waitangi), and the importance of wh-anau engagement from the very start.
Wellington Free Ambulance has developed AKORERO, a podcast led by the Maori and Equity team, which shares korero, history, and lived experiences to deepen cultural awareness across the organisation. They also support theOritetanga Manapou | Earn While You Learn program, creating pathwaysfor those who may not have traditionally accessed ambulance careers, ensuring the workforce reflects the communities served.
Yvonne believes there are four areas the sector must continue to embrace:
Maori health is relational: it involves whanau, whenua (land; identity), whakapapa (genealogy), and wairua (spirit). These are not “nice to have”, they are essential.
Cultural humility, not mastery: no one will know everything, but we can all commit to learning, listening, and responding with respect.
Whanau engagement:
wh-anau must be seen as integral to patient care. Training, protocols, and communication should reflect that.
Representation matters:
M-aori leadership and visibility send a powerful message to colleagues, patients, and communities that Te Tiriti o Waitangi is central to Wellington Free Ambulance’s work.
In Yvonne’s heart, she sees a service where cultural safety is as fundamental as clinical safety— where Maori patients and their wh-anau receive care that acknowledges their worldview, and where every staff member is equipped, encouraged, and held accountable for delivering culturally safe care. When respect and inclusion are centred, Wellington Free Ambulance doesn’t lose efficiency or excellence— it strengthens them.
Finding My Voice
Trent Jackson, Acting Executive Manager –Aboriginal and Torres Strait Islander Cultural Safety Unit

Iam a proud Murriwarri and Yuwaalaraay. My family is connected to the Tulladunna Reserve and Angledool mission in New South Wales. I joined the Queensland Ambulance Service (QAS) in 2012.
At the time, I was in my twenties with two young children. I was not sure what career path I would take, but I knew I wanted to help the community. An Aunty sent me an advertisement in an Indigenous newspaper for roles in the QAS, and something inside me said, “I could do that job.”
When I started, I didn’t see my culture represented in imagery, education and the people around me. It was challenging as my own family carried an inherited mistrust of the health system, which heightened a fear of acknowledging my identity. Being fairer-skinned, I had the privilege to conceal my identity and not identify openly with colleagues.
My everyday experience saw the gap, unconscious bias, and hidden racism against the mob. I saw a lack of understanding about the historical factors that contributed to disadvantage and intergenerational trauma, which was more evident while working in a town close to an old mission site. When people did become aware of my identity, it felt like they saw me as a deficit, rather than recognising my strengths and different perspectives.

For a long time, I struggled to find confidence being naturally introverted. Then, I began to see the Indigenous excellence in the service and at my own station, which inspired me.
I worked as a Local Area Response Unit (LARU) paramedic and was also provided with an opportunity to work in the Mental Health Coresponder Unit. These roles gave me a very different insight. Through my work with patients facing chronic, complex, and mental health conditions, I witnessed firsthand the differences in healthcare and the ways in which the system failed to support them.
Being very inquisitive, I began to question the healthcare system and to seek a deeper understanding of the impact of social, economic, and cultural determinants that shape health equity. Immersing myself in books, podcasts and research papers and became passionate about changing the system, which inspired me to pursue leadership opportunities.
I joined the Aboriginal and Torres Strait Islander Cultural Safety Unit as a Cultural Safety Support Officer. Over time, I took on other roles within the Unit and now serve as the Acting Executive Manager. I have the privilege of leading a strong and diverse team of Aboriginal, Torres Strait Islander, and multicultural staff, all sharing the same passion to improving outcomes for mob.
Together, we have advanced key initiatives that I am proud of. These include the Indigenous Paramedic Program, which creates pathways for First Nations people to become clinicians, the QAS Tertiary Scholarship Program for both paramedics and corporate roles, and the Cultural Safety Benchmarking Reflective Tool, which helps measure progress across the Service. These projects are steps toward a more equitable and culturally safe ambulance service.
Today, as a father of four daughters, my goal is to achieve equity for Aboriginal and Torres Strait Islander people. Although I may not achieve this in my lifetime, I hope to leave a legacy for the next generation to continue to carry the vision forward.

A Reflection of the Women In Leadership Scholarship
As I sit down to reflect on this whirlwind yet transformative year, I find myself overwhelmed with gratitude, pride, and a sense of deep personal growth.
Being the recipient of the 2024 CAA Women in Leadership Scholarship, with the extraordinary guidance of Coach Julie Piantadosi, has been one of the most pivotal experiences of my professional and personal life. What began as an opportunity for professional development became a journey of rediscovery, selfworth, and empowerment, not just for me, but also for my family, my colleagues, and the many women I hope to inspire.
I work in a rural and remote environment, where resources are scarce, demands are relentless, and leadership often means wearing multiple hats with little reprieve. When I took on the role of Station Manager in Port Hedland, while also completing my Master of Paramedic Practitioner, I knew I was stepping into one of my biggest challenges.
But what I didn't realise was how quickly I would begin to sacrifice the very parts of myself that fuel my ability to lead and care for others.


Justine Fletcher, St John WA, Station Officer – Hedland
The passion that had driven me for so long slowly gave way to burnout and compassion fatigue, silently creeping in until I was running on empty.
At the time, saying "yes" to everything felt like the only option. I wanted to be dependable, capable, and strong. But in doing so, I forgot the importance of setting boundaries, for my own well-being and for those I love most.
I am a mother to two beautiful teenage daughters, Maddison, 18, and Alyssa, 15. One of my deepest desires is to be the best role model for them—a woman who not only talks about strength and possibility, but lives it authentically. I want them to grow up knowing that they can achieve anything they set their mind to, and that self-care and boundaries are not weaknesses; they’re essential.
Stepping into the scholarship and working with Julie was a lifeline. From our very first session, she helped me realise something profoundly simple yet powerful: it's okay to prioritise myself, to respectfully say no, and not be everything to everyone all the time. This is how we become better leaders.
Julie has a way of holding up a mirror, one that reflects your potential, not your exhaustion.
She helped me understand that real leadership isn't just about pushing through, but about leading from a place of harmony, clarity, and selfawareness. Through her mentorship, I was given permission to breathe again, to reflect, and to rebuild myself with intention.
This scholarship has strengthened my leadership skills and redefined how I lead. I've become more present, more compassionate (toward myself and others), and more strategic. I've learnt to lead with purpose, not just productivity.
In the past, leadership was often synonymous with sacrifice for me. Now, I see it as an opportunity to inspire change, both by how I show up in my role and how I live my life. I want my daughters to see that success isn't about doing more, it's about doing what matters. I want them to see a mother who is brave enough to say no when it counts, who protects her energy, and who chooses growth, even when it's uncomfortable.
Throughout this year, I placed a strong value on supporting and mentoring. I've made it a priority to create space for those around me to grow, whether through sharing knowledge, offering practical advice, or simply being available when they need support. Leadership to me means bringing others along on the journey, not doing it alone.
One of the most empowering lessons I've taken from this experience, is that you don't have to wait to feel ready to lead; you just have to start! Too often, women, especially in high-pressure sectors like ambulance services, hold back, doubting if they're experienced enough, confident enough, or "qualified" enough to take the next step. The truth is we become ready by doing, by trying, by learning and by surrounding ourselves with mentors and support networks that uplift us.
This scholarship exists because of this very understanding. It was created to encourage more women to step into leadership roles and to support the continued development of women already leading professionally and personally.
This initiative doesn't just change careers, it changes lives. It changed mine.
To the incredible women behind this scholarship, thank you. Your vision shapes a future where leadership is diverse, inclusive, and deeply human. And to Julie, thank you for being the catalyst for so much of my internal 'make over'. Your honesty, humour, and wisdom have been a gift I will always carry.
I also couldn't have done this without the support of my amazing partner, Rachel. During my first session, Julie gave me a little affirmation. I told Rach about this, and she wrote it on our bathroom mirror, which is still there today. She has been my constant, the one I could laugh with, cry with, and lean on through the most challenging moments. Having her as my sounding board, my cheerleader, and my safe space has made all the difference. Her strength and presence have grounded me when I felt overwhelmed, and her belief in me forever stays.
As I look ahead, I feel something I haven't felt in a long timeexcitement. I'm excited about the challenges, the unknowns, and the new pathways I'll be walking down. The tools, confidence, and inner strength that I've gained during this scholarship year will stay with me, anchoring me in every decision I make and every space I step into.
This year has reminded me that leadership is not about being perfect; it's about being real. It's about showing up with courage, vulnerability, and conviction. And it's about reaching back to lift others up as we rise.
But perhaps most importantly, I'll carry the knowledge that my worth is not measured by how much I give to others but by how true I am to myself. That is the legacy I hope to pass on to every woman wondering if she's enough.
You are. I am. We all are!

Record volunteer effort calls on locals to ‘Be the Difference’
St John NT
StJohn NT is celebrating a record year of volunteer service, with dedicated Territorians delivering 20,909 hours of first aid support across 672 public events in the 2024–25 financial year, contributing an estimated $1.05 million in community value*.
To build on this momentum and support the Territory’s ever-growing calendar of events, St John NT is inviting more locals to join its volunteer team through a new recruitment drive, Be the Difference. The campaign aims to welcome at least 40 new volunteers this year.
“Our volunteers are the heartbeat of safe, successful Territory events,” said Mark Ferguson, Director Volunteer and Event Health Services at St John NT.
“The 2025 'Be the Difference' campaign is designed to inspire Territorians to see the power and impact of volunteering with St John NT.
At its heart, this campaign celebrates the real difference our volunteers make in the community while inviting new recruits to join a meaningful journey.”
“In the last financial year, they have delivered an extraordinary number of hours of care valued at over $1 million, and we’re excited to grow the team so even more communities can benefit. If you’ve ever thought about volunteering, now is the perfect time.”
In 2023–24, volunteers supported 526 events, attended to 1,730 patients, delivering 15,700 hours of first aid support, which delivered $802,788 in community value, showing strong year-on-year growth in both impact and participation.


St John NT welcomes clinical and non-clinical volunteers. No experience is needed; all volunteers receive free first aid training, ongoing mentoring and the chance to support many events across the Territory (and sometimes interstate). It’s a great way to gain skills, meet people, and give back.
“Even a few hours a month can make a real difference,” Mr Ferguson said. “You don’t have to be a paramedic, just someone who cares about their community. Join us and be part of something good.”
Grace Johnstone has been a volunteer for four years and says they got into volunteering because it was a great way to learn a new skill and be part of a welcoming community.
‘As a volunteer, I’ve not only learnt some life-saving skills, but been welcomed into the St John NT community.
“I would urge anyone who is curious about volunteering to give it a go.”
Key facts (2024–25) 20,909 volunteer hours (record) 672 events supported Territory-wide $1.05 million community value*
A total of 40 new volunteers sought in 2025-26
*Community value calculated using Volunteering SA & NT hourly rate of $50.30.
To learn more about volunteering with St John NT or to sign up, visit stjohnnt.org.au/volunteers

QAS Legacy Scheme helps Rhonda through treatment
Queensland Ambulance Service
Queensland
Ambulance Service’s (QAS) Operational Support Officer Rhonda Connors loves her job and the team she works in – which is lucky – last month she celebrated 17 years with the service, working with “the best team"; the Frontline Services Group (FSG).
During her time in FSG, Rhonda has provided high-level technical support to our frontline teams, helping them navigate technical issues with the systems they use, for example, Mobile Data Terminals (MDTs), Computer Aided Dispatch (CAD), eARFs, and radio, to name just a few of these many acronyms.
“I love my job’s variety and its opportunities, but most of all the team I work with – they are family,” Rhonda said.
And talking about family, Rhonda and her partner Pete and his three older children welcomed Tamzyn, the pair’s “miracle baby” in 2023, who Rhonda now describes as a typical precocious toddler.
“Tamzyn brings a light into our lives that makes everything worth it and my absolute favourite thing in the world is to make her giggle,” said Rhonda.
But on 28 January this year, Rhonda “was thrown a curve ball” with a cancer diagnosis.
“Pete was very much involved along the way, as I’d shared my initial inklings with him, kept him very much abreast of the steps I was taking and he was with me when I received my official diagnosis,” Rhonda said.
“It took a couple of days to process the news before I FaceTimed my family, as they live interstate.
“Surprisingly, that’s been the hardest part of this journey so far and they reacted as you would expect –with lots of tears.
“It’s really, really difficult to deliver such news remotely when all you want to do is give everyone a great big hug.”
Rhonda began chemotherapy in February and managed to make the most of her parents’ visits in between juggling treatments around Cyclone Alfred.
“Cancer treatment has very much affected my work, social, and home life, but I am so blessed to work with the incredible team that I do, to have amazing friends,
and an amazing team who’ve offered to help out where they can, and to have the most amazing partner who steps up whenever needed. This all makes everything that much easier,” Rhonda said.
“I’ve gone from working four compressed days a week, to working from home five days, only three hours on a treatment day to start with, but now I don’t work at all those days.”
Rhonda said FSG’s flexible work hours meant she could take breaks when she needed during her workday, but sometimes she’s had to have days or weeks off at a time which has also included a couple of hospital stays.
Rhonda said while she was fortunate to have had a fair amount of sick leave up her sleeve before her diagnosis, she has certainly burnt through it since.
“By the time I finish chemo, have surgery, radiation, and recover, I think I will have well and truly depleted my sick leave,” she said.
Rhonda’s changed workdays (from four to five) have also increased her toddler’s daycare needs and fees, at a time when the cost of living is already high and on top of her medical treatment.
“I always knew QAS Legacy Scheme was a wonderful charitable organisation that helps so many deserving people in their time of need - I just didn’t expect to be one of them."
QAS Legacy Scheme is an independent charity which has provided more than $600,000 in grants to QAS staff and their families during tough times since 2015.
QAS Legacy Scheme currently supports ten children from eight QAS families and another 16 children have graduated from the scheme, with three of those going on to study paramedicine.
The charity has also provided many grants to member and non-member QAS workers experiencing difficult times, either due to illness or natural disasters.
This charity is predominantly funded through fortnightly tax-deductible payroll contributions from current staff, but additional funding also comes from bequests and tax-free donations, often from retired employees, QAS volunteers, or members of the public expressing appreciation for work done by ambulance staff in the community.
QAS Legacy Scheme’s recent inclusion as a recipient in large scale fundraising events like Run Army (from 2024) and Bridge to Brisbane for the first time this year, has raised more than $30,000.
This additional funding has ensured the charity not only continues to support QAS staff and their families during tough times but can now expand its support to promote QAS employees’ health and wellbeing.
Rhonda said she first became aware of the QAS Legacy Scheme in 2015, and began donating to it regularly from 2018.
“I joined after a chat with QAS Legacy Scheme’s Secretary Mindy Thomas when I learnt a lot more about the charity, its wonderful work, and the assistance it provides,” Rhonda said.
“QAS Legacy Scheme has provided me with two grants of $1,500 each so far,” Rhonda said.
“Childcare costs have increased since I began my treatment, then there’s scan costs, procedure costs, consultancy costs, surgical costs, down to hospital parking and medication costs, and those grants have eased the financial burden our family is experiencing.
“While the financial contribution is so very much appreciated, also wonderful is the fact that a very special, beautiful person saw my need, and petitioned QAS Legacy for this grant on my behalf, that’s what makes me tear up every time I think about it - I am just so blessed!"
For more information about QAS Legacy Scheme including how to join as a member, donate, or get involved in coming events like Run Army 2026, go to qaslegacy.org.au.
Small toys making a big difference
Ambulance Victoria and Monash University launch paediatric distraction kits
Ambulance Victoria
Ambulance Victoria (AV) is proud to announce the rollout of a new Paediatric Distraction Kits pilot across every emergency road ambulance in Victoria, giving paramedics simple but powerful tools to reduce fear and anxiety in children during treatment and transport.
The first-of-its-kind, service-wide initiative follows years of advocacy, research, and consultation with paediatric Emergency Physicians and Child Life Therapy experts at The Royal Children’s Hospital.
The kits contain a selection of age-appropriate items such as bubbles, puzzles, stickers, squishy toys, and a magnetic drawing pad, along with a QR code linking to the TLC for Kids Tap 2 Distract app. Each item has been carefully chosen for safety, portability and effectiveness in clinical environments, and is designed to engage children and ease their distress while supporting paramedics to deliver safe, compassionate care.
The project was developed by Associate Professor Dr Kathryn Eastwood ASM, Intensive Care Paramedic at Monash University, and Katrina Sedgwick, ALS Paramedic and Team Manager, in collaboration with paediatric Emergency Physicians and Child Life Therapy experts at The Royal Children’s Hospital. Their research reviewed the most effective tools used in paediatric emergency departments and adapted them for the unique challenges of the ambulance setting.
Funding for the pilot was made possible thanks to the generosity of the Victorian community, with almost $60,000 in donations, ensuring every emergency ambulance can now carry a standardised kit.
For years, paramedics have been drawing faces on gloves to make balloon elephants or finding small toys to help calm children. Now, for the first time, every ambulance will have the same kit, so kids get consistent care wherever they are in Victoria,”
Katrina Sedgwick, ALS Paramedic and Team Manager
“These kits are only possible because of the generosity of the community,” Ms Sedgwick said. “It’s a wonderful example of the public helping us deliver better care for children.”
Ms Sedgwick said the kits would make a meaningful difference to the experience of young patients and their families. “As paramedics, we see how frightening it can be for children in an ambulance. These kits give us simple, effective tools to make that experience less scary and more supportive,” she said. “Something as small as a bubble wand or a sticker can change the whole tone of an interaction. It helps children feel safe, and it helps their parents feel reassured too.”
Paramedics have long improvised distraction techniques to comfort children, but this rollout ensures every crew has the same high-quality resources on hand.
The initiative also supports paramedics in their clinical work. Calmer children are more likely to cooperate with treatment, helping procedures run more smoothly and efficiently. Research shows distraction can reduce perceived pain, improve cooperation, and ease anxiety, with benefits flowing to both patients and clinicians.
AV, in partnership with Monash University, will be evaluating the impact of the kits on patient outcomes, paramedic confidence and service delivery. “Now we’re working with Monash University to measure how the kits are performing in real-world use,” Ms Sedgwick said.
“We’ll be looking at how they help children, how they support paramedics, and what the broader benefits are for the service.
Our goal is for distraction to become as routine in paediatric care as any other piece of equipment, and we’re exploring opportunities to build partnerships so this can become an ongoing program.”

This rollout is a tangible example of AV’s commitment to Best Care - safe, evidence-based, and person-centred care that recognises the physical and emotional needs of every patient.
To contribute to amazing initiatives like this, consider making a donation or bequest to Ambulance Victoria.
AWARDS FOR EXCELLENCE

The 2025 CAA Awards for Excellence showcased the sectoraltering projects submitted by ambulance services across Australasia. These projects highlighted innovation, progression, and commitment to patient care across a variety of disciplines.
This year, the CAA received more than 45 submissions across the 11 CAA member services for the six award categories. In the pages to follow, you will learn more about two of the winning projects from St John WA.
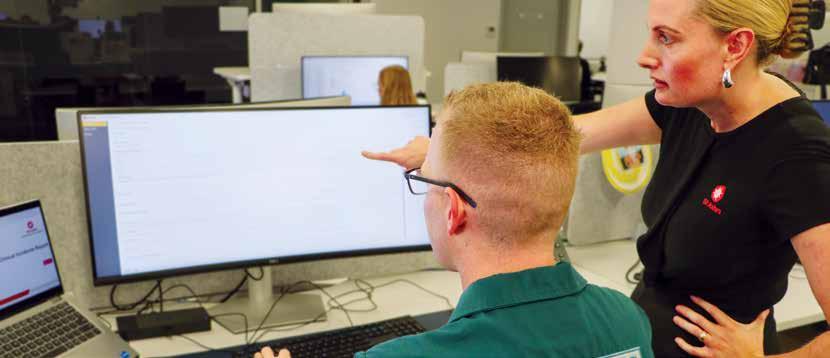
Excellence in Technology Implementation of a Dedicated Prehospital Clinical Incident Management System
Clinical incidents in ambulance services are rarely straightforward. They often involve complex systems and multiple contributing factors, requiring thorough investigation and informed, responsive action.
In 2024, St John WA’s Patient Safety and Quality (PSQ) team introduced a bespoke Clinical Incident Management System (CIMS)— a significant leap forward in how clinical safety is managed in the prehospital setting.
The previous incident management framework, centred around how the linear and administratively heavy Workflow platform, was no longer fit for purpose. It lacked capacity for real-time coordination, ambulancespecific taxonomies, and robust analytics. Most critically, it failed to support the proactive identification and prevention of harm in complex, dynamic ambulance environments.
Recognising these limitations, St John WA’s PSQ team undertook a comprehensive system overhaul. CIMS was custom-built to respond directly to the challenges of mobile healthcare delivery. The result is a cloud-based, scalable platform that captures the full spectrum of clinical incidents with accuracy, transparency, and speed.
CIMS is underpinned by several key innovations:
• Ambulance-specific clinical data architecture, capturing unique operational and environmental factors.
• Integrated workflow management, allowing simultaneous multi-stakeholder access and collaboration.
• Advanced analytics, seamlessly integrated with St John WA’s business intelligence tools.
Sponsored by
• Systematic action tracking, with clearly assigned responsibilities and transparent status updates.
• Mobile access, ensuring usability across St John WA’s geographically dispersed workforce.
• Role-based security, to protect sensitive data while maintaining accountability.
The platform was developed in collaboration with Frontline Clinicians, Clinical Quality Managers, and Data Experts. Critically, the solution was not off-the-shelf; it was built by adapting the existing MyOSH Safety System to meet complex clinical requirements. This approach maximised value while enabling deep customisation.

Method and Implementation
The project began with systematic audits and detailed stakeholder consultation, aligning with WA Department of Health requirements and user feedback. This process revealed the urgent need for paramedicine-specific taxonomies and more dynamic workflows.
Implementation took a ‘safe parallel’ approach, running Workflow and CIMS concurrently during transition. Custom taxonomies were developed iteratively based on incident frequency, severity, and root cause analysis. The PSQ team worked hands-on with the software vendor and internal business units to embed these changes while maintaining continuous service delivery.
Following testing and User Acceptance Trials, the platform launched with immediate impact: faster triage, better case visibility, and reduced duplication. Dashboarddriven analytics now enable trend analysis across medication safety, dispatch errors, and procedural risks, enabling data-informed decisions in real time.
Impact and Outcomes
Post-implementation, CIMS has significantly improved classification precision and reduced administrative workload. Automated reporting has replaced hours of manual collation, freeing PSQ staff to focus on quality improvement. Real-time visibility has also improved leadership oversight, enabling faster escalation of risks.
Importantly, CIMS has strengthened the culture of safety within St John WA. Frontline managers are now actively involved in investigations, incident reporters receive timely updates, and the system encourages greater participation in learning from near misses.
Themed analysis of medication errors has already led to targeted interventions across multiple business areas—a clear demonstration of how data can drive system-wide change.
CIMS represents a paradigm shift from reactive incident recording to proactive clinical governance. It aligns with National Safety and Quality Health Service (NSQHS) standards, and its ambulance-specific design positions St John WA to lead the development of a national prehospital patient safety dataset.
With a scalable architecture and embedded governance pathways, the platform offers significant transferability across jurisdictions. Future developments may include AI integration for pattern recognition and predictive analytics — strengthening Australia’s emergency health safety net.
In a sector where seconds matter and systemic improvement saves lives, St John WA’s CIMS stands as a bold, practical, and data-driven innovation in clinical risk management.
Team photo (left to right) is: Ciaran Voyce, Lauren Davids, Alana Graham, Curtis Naylor, Camilla Quiceno (Not pictured: Jess Eddy, Des Bylund, Kevin Keane)

Excellence in Staff Development
Sponsored by
Deliver Sector-recognised Family and Domestic Violence Informed Education to Emergency Responders Across All of WA.
St John WA (SJWA) has launched a pioneering initiative to address Family and Domestic Violence (FDV) through targeted, sectorinformed, research-based education for emergency responders. In collaboration with Stopping Family Violence (SFV) and the Centre for Social Impact at the University of Western Australia (CSI UWA), SJWA has delivered the first structured FDV education program to paramedics, volunteers and State Control Centre (SCC) call takers, making it the largest regional education rollout in the organisation’s history and a national first in the ambulance sector.
Despite being a frontline responder, the ambulance sector has historically lacked formal FDV education, with no tertiary paramedicine curriculum or Council of Ambulance Authorities (CAA) member organisation offering structured training.
SJWA's project fills this gap with tailored education, co-developed with FDV experts and evaluated for real-world relevance and clinical applicability.
The program includes three core components:
• Identifying and Responding to FDV – Equips responders to recognise signs and respond supportively.
• Screening and Risk Assessment
– Provides practical tools for assessing safety and guiding appropriate communication and handover to hospitals.
• Information Transfer – Ensures accurate, timely communication with hospital services and supports continuity of care.
Training content has been tailored for three specific cohorts — Triple Zero (000) call takers, Paramedics, and Clinical Volunteers, acknowledging their distinct operational roles. Education delivery was staged accordingly: beginning with SCC in October 2023, followed by Paramedics in mid-2024, and continuing through to 2025 for regionally based Volunteers. To ensure program continuity, a Train-the-Trainer model was established in 2024, certifying SJWA facilitators under the guidance of SFV.

The initiative aligns with the WA Government’s Path to Safety: Strategy to Reduce FDV 2020–2030 and was funded through a $2.1 million commitment from the Department of Communities, announced during the 16 Days in WA campaign in 2022. This investment has enabled SJWA to lead a transformative shift in prehospital care by equipping emergency responders with the tools to safely and sensitively respond to Victim-Survivors of FDV.
Innovatively, a “Suspected Family and Domestic Violence” (SFDV) tick box has been added to operational platforms: Computer-Aided Dispatch (CAD) for SCC and the electronic Patient Care Record (ePCR) for Paramedics and Volunteers. This tool enhances documentation, ED handover and enables critical data capture. As of August 2025, 6.8 suspected FDV cases are being flagged daily, with high prevalence in the Kimberley and Pilbara regions in the north-west of WA.
Education delivery was carefully designed to meet the Enterprise Bargaining Agreement (EBA) and clinical education requirements. Content comprises two units: a foundational online module and an advanced, cohort-specific session delivered face-to-face. Topics cover the forms and impacts of FDV, intersectionality, perpetrator patterns of behaviour, and FDVinformed communication.
To support participants’ wellbeing, given the confronting nature of the content, SJWA’s internal Wellbeing & Support team was involved throughout. Disclaimers, clear communication, and escalation pathways were in place to provide psychological safety for all team members.
Despite the scope and complexity, feedback has been overwhelmingly positive. More than 2000 participants noted the content’s relevance, the professionalism of co-facilitators, and the benefit of real-world case examples. The iterative development process ensured the content was continually refined based on user feedback and cohort needs, ensuring the gravity of FDV, especially the gendered drivers and patterns, was the focus, while keeping it grounded in clinical applicability and responding to patients’ needs.
With CSI UWA leading the formal evaluation, SJWA will assess the long-term impact of this program on clinical practice, data accuracy, and patient outcomes.
This project demonstrates how sector leadership, government backing, and expert partnerships can reshape service capability. SJWA’s FDV education program is now positioned to serve as a blueprint for ambulance services nationally, fostering safety, compassion, and accountability for some of Australia’s most vulnerable people.






Ready for your next challenge?







TAKE YOUR CAREER FURTHER WITH A POSTGRADUATE COURSE IN PARAMEDIC SCIENCE OR COUNTER-TERRORISM AND OPERATIONAL MEDICINE.
Whether you’re looking to step into leadership, specialise in critical care, primary healthcare, or operate in high-threat environments, CQU’s specialist courses will support your next move. Apply in 2025 and save on tuition fees*. EXPERT TEACHERS CONTEMPORARY CONTENT FLEXIBLE STUDY






2025 Women in Leadership Scholarship Finalists
The CAA congratulates the following individuals who were recognised as the 2025 Women in Leadership Scholarship finalists.




















Our sincerest thank you to our 2026 Coaches: Julie Piantadosi of Total Coaching Academy and Dr Erica Kreismann of OneWild Coaching.
Thank

Sponsors:
SHer Excellency the Honourable Sam Mostyn AC, Governor-General of Australia
In this edition of First, we are honoured to share an exclusive conversation with Her Excellency the Honourable Sam Mostyn AC, Governor-General of Australia.

People in health and emergency services inherently understand this – care for others is at the core of everything they do.”
Her Excellency the Honourable Sam Mostyn AC, Governor-General of Australia

As Governor-General, Her Excellency has placed care, kindness and respect at the core of everything she does. With this focus, and her prior career spanning law, business, sport, the arts, sustainability, climate policy, mental health, and the not-for-profit sector, the Governor-General brings a wealth of insight to themes that resonate deeply with the ambulance and healthcare community.
From the role of care in shaping our national identity to safeguarding the wellbeing of frontline responders, advancing equity and sustainability, and building resilient services for the future, this thoughtful exchange highlights the values and vision guiding Australia’s new Governor-General and the inspiration they offer to those who serve on the frontline every day.


Thank you for accepting patronage of the Council of Ambulance Authorities – can you tell our readers why you have decided to give us your patronage?
It is an honour to be invited to serve as your Patron.
I have the deepest respect for all who work in the ambulance sector. Your work is critical and an important act of care for our broader community.
I’ve seen and learnt about many examples of the care first responders provide – particularly in visits to communities impacted by natural disasters. Through my involvement both with the Order of St John and at investiture ceremonies, I have been proud to recognise people with the Ambulance Service for the Order of Australia Medal.
I also know that your service can often come with a cost. As with others in our emergency and frontline services, those that work in the ambulance sector are generally put in extraordinary situations – faced with danger, stress and pressures that are unimaginable for many of us. I hope that my patronage sends a message to all that Australians value your service and recognise it as a significant and enduring act of care.


In your swearing-in address, you spoke beautifully about “care” being at the heart of Australia’s national identity. Could you share more about what that means to you?
I have placed care, kindness and respect at the core of my term.
When I was sworn in as your Governor-General I reflected that care has a deep and resonant place in our Australian identity. Care is the gentle thought and the outstretched hand that Australians have always been ready to share when great challenges present themselves. Care is the quieter, better part of ourselves.
Everything I have seen since taking office has reaffirmed that belief. I have seen so many examples of care in all of its forms – it is what makes me so optimistic about our future. It isn’t simply soft, feminine or an afterthought. Care is often hard – it requires showing up, being accountable and reliable. Care is measurable and when care is exercised – in individual moments and actions, and at scale to inform priorities and decisions that affect the community – we achieve better outcomes.
People in health and emergency services inherently understand this – care for others is at the core of everything they do.


Ambulance professionals are often the first to arrive in moments of crisis, and that comes with incredible emotional weight. With your background supporting mental health organisations, what do you think is most important when it comes to protecting the wellbeing of frontline responders?
A focus on mental health and wellbeing is vitally important for our whole community and, as you say, particularly for ambulance professionals and frontline responders.
It is important that we all know that help is available and that there is no barrier to accessing those services.
In the workplace this means that leadership and governance structures are in place to ensure there is support for the needs and wellbeing of everyone.
In modern Australia more broadly, it means continuing to remove any remaining stigma around mental health. There simply cannot be any barrier to accessing support, advice and help when needed.
I am particularly conscious of the mental wellbeing of frontline responders. It is, I believe, an area that has not received enough attention or care. I say that not to take away from the hard work of many working in this space, but simply to say that I think we can do more. I’m proud to also serve as Patron of Beyond Blue, Lifeline Australia, and Suicide Prevention Australia. My hope is that across my term I can draw different groups and perspectives together to identify ways to better support our frontline responders.
Caring for carers is a fundamental responsibility of those privileged to lead – to take responsibility, think strategically, and help prevent future risk, by ensuring those who are the first to help others are given the time they need to rest, recover and restore their strength to continue their work. Essentially, to always show care for the carers.


As the second woman in Australian history to hold the role of Governor-General, what advice would you offer to young women and girls looking to step into leadership or service-focused careers?
I am proud to be Australia’s 28th GovernorGeneral and grateful for the advice, generosity and example set by all my predecessors, especially Dame Quentin Bryce, the first woman to serve in the role. She described the Office "as striking a balance between observing traditions and protocol and being thoroughly contemporary."
My hope – and I said this only recently at the swearing-in of the first woman Commissioner of the Australian Federal Police – is that by showing up, doing the job with care, kindness and respect. Over time I hope that our gender will be the least interesting thing about ourselves when we speak of leaders.
My advice to all young people –women and men – is to be curious and believe in yourself. When an opportunity presents itself, say yes. Don't let fear overcome your courage. Meet people where they are, and put care, kindness and respect at the centre of your approach.
20 26 EVENTS
10-11 MAR
Ambulance Leadership Forum (ALF) 2026
De Vere Beaumont Estate, Windsor
23-24 MAR
2026 NEMSMA Leadership Conference
Washington DC
3-5 JUN
The Paramedic Chiefs of Canada Leadership Summit 2026
Calgary, Alberta
12-14 AUG
CAA Congress
Australasia’s premier event for the Ambulance Health Sector, bringing together leaders, decision-makers and senior management teams from ambulance services, health, and emergency management sectors from across Australasia and abroad.
National Convention Centre, Canberra, ACT
13 AUG
CAA Awards for Excellence
Recognising the hard work and innovative solutions of our member services from Australia, New Zealand, and Papua New Guinea.
Canberra, ACT
14-17 SEP
18th National Rural Health Conference
Adelaide, South Australia
7-10 OCT
IRCP26
The International Round Table of Community Paramedicine Conference Regensburg, Germany
Other upcoming events
Dates yet to be announced.
2026 CAA Webinar Series
AEROMED, Darwin, NT
Critical Care Summit
ACP International Conference
16OCT
Restart a Heart Day
Restart a Heart is a global initiative to raise awareness and educate the community about CPR and AEDs.
restartaheart.net
NOV
Women in Leadership Symposium
Empowering women in ambulance leadership through professional development, mentorship, and career advancement opportunities.
NOV
Women in Leadership Scholarship Winner Announced
Keep an eye out for future editions of First Magazine.
Covering updates, insights and achievements within the ambulance and emergency services sector across Australasia.
Issue #21 APR 2026
Issue #22 AUG 2026
Issue #23 NOV 2026 Scan code for more information, and to stay up to date with all our

Restart a Heart Day 2025
A global initiative of the European Resuscitation Council, Restart a Heart is a campaign designed to raise awareness and educate communities about CPR and AEDs. Across Australasia, the CAA and its members coordinate the campaign and events, calling for people to Call, Push, Shock.
The campaign is designed to improve the survival rate for patients in Australia and New Zealand who experience out-of-hospital cardiac arrest (OHCA). Currently, the patient survival rate is 1 in 10, with the chance of surviving this event higher if the community is comfortable and able to provide CPR or use an AED in times of crisis.
October 16th saw the CAA partner with SA Ambulance Service (SAAS), St John SA, Surf Lifesaving SA, Flinders University, and the Heart Foundation for its annual Restart a Heart Day activation. This year, the heart of the Adelaide shopping district, Rundle Mall, again hosted the activation, aiming to educate shoppers, surrounding workers and passing patrons.
A resounding success, the event brought partnering organisations together, who emphasised the importance of CALL-PUSH-SHOCK, a message that will improve the chances of out-of-hospital cardiac arrest.
This event provides an opportunity for the CAA to gather insights with an anonymous survey that allows us to gauge community training levels, a valuable asset to the CAA and its member services.
Alongside the Adelaide activation, CAA Member Services and other organisations hosted their own events across Australasia, including fantastic experiences in Martin Place by NSW Ambulance and in Wellington Airport by Wellington Free Ambulance.
Alongside their airport opportunity, Wellington Free Ambulance had the privilege to attend parliament and share skills with Ministers as well as the public in the Parliamentary courtyard.
As part of broader campaigns, member services continue to educate their communities throughout October as part of their SHOCKTOBER campaigns. Inspirationally, Hato Hone St John surpassed their initial goal of teaching 15,000 members of the community.
By working together, we can increase the importance of this knowledge and help keep our communities and loved ones safe until help arrives, as every minute counts.
From the attending paramedics to the partnering organisations and all in between, the CAA sincerely thanks you for partnering and participating with us at this important event.
To see more of what our member services did throughout their campaigns across the region, head to their social media pages and get involved in the conversation.
If your organisation would like to be involved in Restart a Heart Day 2026, please contact admin@caa.net.au

amPHI’s collaborative platform supports:
• Realtime collaboration between ambulance crews and hospital teams
• Secure video, direct chat, ECG and image sharing
• On and offline handover of the ePCR
• FHIR standard real time secure information exchange to and from EHR/EMR for patient histories and prehospital event details.


When the system slows down, paramedics need tools that keep moving.


IRCP 2025
Alongside this year’s CAA Congress, Adelaide proudly hosted the International Roundtable on Community Paramedicine (IRCP).
The two-day event, held at the InterContinental Adelaide, brought together prominent speakers, researchers, and delegates from across the globe to explore the future of community paramedicine.
Held in a different location each year, 2025 was the first time they returned to Australasia since 2018. This was a fantastic opportunity for Australasian services and health providers to showcase their solutions, initiatives and healthcare requirements across demanding Australasian environments while learning about other global organisations' operations, challenges and outcomes.
Coinciding with the outstanding presentations and discussions, delegates enjoyed excellent networking opportunities throughout the event, during breaks, between sessions, and at a delightful welcome function hosted at the InterContinental Adelaide on Sunday evening.
Throughout the two days, presenters took to the stage covering a variety of topics that affected their respective communities and disciplines. Here, they discussed the specific challenges Community Paramedics face regularly and how they have overcome them.
Desiree O’Brien of NSW Ambulance provided an insight into volunteer workforces and the land they serve with a presentation on the Howlong Community Emergency Response Team (CERT). Howlong is a small NSW community with a population of 2551 and is 28km from Albury and 27km from Corowa, and since commencing operation in October 2023, the team have completed over 140 responses to 000 as of mid-February 2025 and provided initial clinical care in 98% of cases. This has since led to improving the health outcomes for the community, an incredible and inspiring result for the community.

A memorable presentation from Kevin Deramus of Washington County Emergency Medical Services included a combination of theory and case studies when discussing going the extra mile for patients in communities. Combining these aspects in his presentation showcased the benefit that the Washington County EMS provides for its community.
Delegates heard an eye-opening address from Susi Tegan of the National Rural Health Alliance as she spoke on the topic of how to keep the Australian rural health workforce thriving. Rural Australians currently make up close to 30% of the population, yet don’t receive an equitable portion of funding.
Towards the end of day 2, Captain Sherri Hercules of St Charles County Ambulance District, St Peters, presented on the Successes and Challenges in Treating Patients with Addiction. Sherri discussed the highs and lows of treating patients with addiction and how it can be rewarding when patients succeed or discouraging if unsuccessful or progress slowly. She emphasised that we are the bearers of hope as they tirelessly continue to work alongside agencies to provide the best for their patients. A truly striking presentation with a topic that affects all emergency services.
Beyond the individual presentations, the event featured lively panel discussions, where leaders explored pressing issues facing community paramedicine. Attendees were encouraged to exchange experiences and ideas, fostering a truly global dialogue on advancing the profession.
With a combination of various themes and topics, guests were able to learn, understand and discuss the landscape of community paramedicine and perhaps take back to their respective organisations different ways of thinking or approaches to challenges they face.
Thank you to the IRCP Council for partnering with the CAA in putting this phenomenal event together, and we look forward to its continued growth, support and influence in the future.
In 2026, IRCP heads to Germany, hosted by the Bavarian Red Cross (Regensburg Chapter), October 7-10, 2026.
Learn more about IRCP at ircp.info
Expanding Relief, Connection and Positive Distraction
TLC for Kids
Over the past year, TLC for Kids has continued to grow in both reach and innovation, with our services expanding nationally and our digital tools gaining momentum on the global stage.
Since our founding in 1998, our mission has remained the same: to deliver immediate relief, comfort, and care to sick children and their families. What has changed, however, is the scale at which we now operate and the new ways we are meeting the rising need for practical support and positive distraction in moments of stress.
TLC Ambulance Expanding into South Australia
One of the most exciting developments has been the expansion of our TLC Ambulance program into South Australia, in proud partnership with SA Ambulance Service.
The TLC Ambulance provides children in palliative care with a unique opportunity to create lasting memories with their families. Whether it’s a trip to the zoo, a visit to the beach, or simply time together outside the hospital, the TLC Ambulance brings moments of joy when they matter most.
We were honoured to be part of this year’s CAA Congress, where “Noah,” our new TLC Ambulance in South Australia, was proudly on display. The Congress created exciting conversations and connections with incredible paramedics and other members of the health sector, all of whom play a vital role in making programs like this possible.
Distraction Box Program
Consistently meeting demand, our Distraction Box Program continues to be a cornerstone of TLC for Kids in over 400 hospitals across Australia and New Zealand. These boxes provide healthcare professionals with immediate tools to calm and distract children during medical procedures. With combined usage now averaging 2.5 times per minute across the country, the program is delivering over 1.1 million meaningful moments of care every year.

Tap 2 Distract App
Our Tap 2 Distract App is continuing to increase its reach as both a digital wellbeing and distraction tool. Designed as a no-cost, ad-free, all-age and immediately accessible resource for anyone facing stress or anxiety, the app has now logged more than 1.3 million minutes of use, with users spanning Australia and reaching international audiences.
We are enhancing the app with age-specific content and trauma-informed tools, while continuing to integrate it into Ambulance Services, schools and immunisation programs to help children cope with needle phobia and everyday stress. Tap 2 Distract is on the way to being positioned as a global standard for scalable, accessible digital distraction, with growing interest from partners and organisations around the world. (learn more at tlcforkids.org.au/app)

Friends of TLC
Building a community of support to sustain and grow these vital services, we launched Friends of TLC, a membership program inviting individuals and businesses to become regular supporters. Small weekly contributions, collectively, are helping us reach more children and families every single day. With membership growing, this initiative is not just about fundraising but about creating a connected community that shares in our impact.
Relief that can't wait - what ties all our programs together is a simple truth: there are children and families who cannot wait for care, comfort, or relief. Every moment of distraction, every sigh of relief, every shared memory counts. With the support of our partners, donors, and community, TLC for Kids has now delivered more than 17 million moments of practical care since 1998.
Yet, demand continues to rise. By innovating, expanding, and staying true to our mission, we are working tirelessly to meet that demand, right when it matters most, right when the moment happens.
Building a Stronger Future: Insights
from the Australasian Paramedicine Workforce Survey 2024-2025.
John Bruning, CEO, Australasian College of Paramedicine
The Australasian College of Paramedicine has released its second Paramedicine Workforce Survey Report, offering a comprehensive and timely snapshot of the profession across Australia and Aotearoa New Zealand.
This report is more than a collection of statistics; it’s a reflection of the lived experiences, aspirations, and challenges of paramedics working in diverse settings and roles.

This generational shift presents both opportunities and responsibilities: to mentor, to lead, and to ensure that our systems are ready to support the next wave of paramedicine professionals.
At its heart, the survey underscores the evolving nature of paramedicine. It captures a workforce that is highly educated, deeply committed, and increasingly diverse. It also highlights areas where we must do better, particularly in supporting career progression, improving work-life balance, and addressing structural barriers to inclusion.
A Workforce in Transition
One of the most striking findings is the number of paramedics working across multiple employers - nearly one in four. This trend speaks to the flexibility and adaptability of our workforce, but also raises questions about sustainability, income security, and the need for more supportive employment structures.
The data also reveal a maturing workforce, with a significant proportion of clinicians aged over 50. At the same time, we’re seeing strong growth in early-career entrants, particularly women under 30, who now make up the majority of student paramedics.
Equity, Inclusion and Representation
Encouragingly, the report shows increasing representation of Aboriginal and Torres Strait Islander, and Maori and Pasifika peoples in paramedicine, particularly among students. However, both groups remain underrepresented in some clinical roles relative to population data. This is a call to action. We must continue to invest in culturally safe pathways, support Aboriginal and Torres Strait Islander, and Maori and Pasifika peoples into leadership roles, and ensure that our workforce reflects the communities we serve.
Gender equity also remains a challenge. While there is near parity in the 30–49 age group, men continue to dominate management roles. The underrepresentation of women in leadership is not unique to paramedicine, but it is something we must actively address through targeted development, mentorship, and structural reform.

Wellbeing and Career Intentions
The survey paints a mixed picture of wellbeing. While most paramedics report a sense of joy and accomplishment in their work, many also express concerns about resourcing, burnout, and turnover. Alarmingly, over 40% of clinical paramedics intend to leave their current employer within four years. This is a critical signal for policymakers, employers, and the College alike.
We must understand the drivers behind these intentions, whether they stem from workload pressures, lack of career progression, or organisational culture, and respond with evidence-based strategies that support retention and renewal.
Looking Ahead
The report confirms what many of us already know: paramedicine is no longer confined to emergency response. It is a dynamic, evidence-informed discipline delivering care across a broad spectrum of settings. Our future lies in advanced clinical roles, interprofessional collaboration, and a strong foundation of research and education.
As the peak professional body representing and supporting paramedics, we remain committed to leading this transformation. This report is a tool for advocacy, a guide for workforce planning, and a testament to the professionalism and passion of our members.
To every paramedic who responded to this survey, thank you. Your voice matters and your insights are shaping the future of paramedicine.
View the report here - paramedics.org/apws

Driving Connected Care for all Australians
Australian Digital Health Agency
Australia, New Zealand, and Papua New Guinea collectively have over 17,000 paramedics, supported by more than 11,000 trained volunteer first responders who work under extraordinary pressure, often making lifesaving decisions in seconds.
These professionals are often the first point of contact in medical emergencies, where access to real-time health information can be critical. When patients are unconscious or unable to communicate, every second counts and delays in accessing key health data can impact outcomes.
To address this, the Australian Government is advancing a modern, connected digital healthcare system. The Australian Digital Health Agency is central to this transformation, aiming to ensure Australians and healthcare providers can securely access real-time health information when needed.
Amanda Cattermole PSM, CEO of the Agency, highlights that having health data available at the point of care improves clinical decisions, reduces duplication, and enhances safety and outcomes. Beyond emergencies, digital health also eases pressure on the workforce, lowers costs and empowers consumers.
As the system evolves, paramedics may soon access a patient’s medical history, including medications on the spot, helping tailor treatment and reduce risks. They’ll also be able to share treatment details with hospital teams, improving continuity of care.
While there’s still work to be done, the Agency is committed to building a digitally enabled, person-centred, inclusive health system. Its efforts align with national reform agendas like Strengthening Medicare and Aged Care, guided by strategies such as the Digital Health Blueprint and the Aged Care Data and Digital Strategy

Key initiatives include:
• Standards and Health Identifiers (HIs): Supporting interoperability so health data flows seamlessly and is consistently understood across systems.
• Better and Faster Access - Sharing By Default: A framework for mandating that certain health information must be uploaded to My Health Record to ensure it is available when needed.
• Health Connect Australia: Creating a secure, efficient digital health ecosystem.
• Allied Health and Aged Care: Promoting continuity of care through better provider-patient connections.
• Cyber Security: Enhancing awareness and resilience across the healthcare sector.
The Agency also delivers services like Provider Connect Australia, which simplifies business information updates for providers, and the my health app, putting secure access to key health information in the palm of your hand. Other efforts include medicine safety, the Healthcare Information Provider Service (HIPS), and digital health education for the workforce.
But there is always more to do as advancements in digital health ramp up.
Just recently, the Agency has integrated My Health Record with Mantle software used by the Royal Flying Doctor Service. These advancements mean Australians and their healthcare providers are increasingly empowered with timely, secure access to vital health information.
Now more than ever, Australians and their healthcare providers can feel empowered, with access to key health information when and where they need it. It seems the sky is indeed the limit for digital health.
Rural Ambulances Under Pressure: Insights from the latest health expenditure report
The National Rural Health Alliance
Australians living in rural, regional, and remote areas experience greater social and biomedical risk factors compared to their metropolitan counterparts yet receive significantly less funding towards healthcare.
The Forgotten Rural Health Spend: A Report on the Expenditure Deficit in Rural Australia, commissioned by peak advocacy body the National Rural Health Alliance (NRHA), highlights the stark funding gap in healthcare between rural and urban Australia. Prepared in collaboration with independent consultants at Nous Group, the Report demonstrates the figures behind the reality experienced by rural Australians every day.
The total gap in health expenditure between rural and metropolitan Australia has increased to $8.35 billion annually, equating to a $1,090.47 deficit per person, per year. The deficit for MMM 51 increases to almost $6,000 per person. This gap translates into fewer services, longer wait times, and poorer health outcomes for rural Australians. The deficit is primarily contributed to by underfunded public and private hospitals, the MBS scheme, and private ancillary health insurance, dismantling the ease of equitable access and continuity of care for rural communities.
As isolation, lack of public transport, and inaccessibility of primary care compound with remoteness, the importance of ambulances in filling the gap of emergency care to rural, regional and remote communities cannot be overstated. Table 1 and Table 2 compare paramedic practitioners to other medical, nursing, and allied health professions across MMM classifications. 66% of paramedics work outside of MMM 1, with 5% working in MMM 6-7 locations.
Additionally, 53% of the workforce have experienced living in non-metropolitan areas2 and therefore have a complex understanding of the barriers faced by rural Australians.
Distribution of state and territory ambulance expenditure across MMM areas considers greater reliance on ambulance services in rural and regional areas. Regional and remote areas receive higher per capita expenditure than MMM 1, with MMM 4 receiving 2.6 times more per capita than Major cities.
Table 1
Nursing, aged care and medical-related workforce (FTE) across MMM areas, 2024
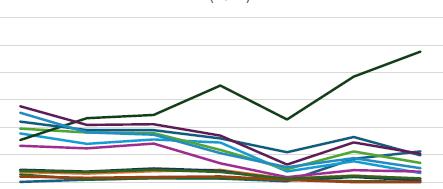
ATSI Health Practitioners
Chinese Medicine Practitioners
Medical Radiation Practitioners
Optometrists
Chiropractors
Dental Practitioners
Occupational Therapists
Osteopaths
Paramedicine Practitioners Pharmacists
Physiotherapists Podiatrists
Psychologists
Additionally, rural and remote areas have a disproportionately high number of paramedics relative to their population, likely due to additional staffing requirements resulting from longer travel distances, minimum safe staffing levels, and a lack of other health services. As such, expenditure generally aligns with this greater need.
The isolation of remote communities creates a complex interplay between expenditure and service delivery costs. MMM 6 and 7 receive relatively high per capita expenditure, at 97% and 137% greater than MMM 1, respectively, mostly driven by high spending in specific states (e.g., WA).
Whilst the figures look positive (Refer to Table 3), the relative level of service delivery in remote areas is influenced by high delivery costs and high need.
Ambulance services also often pick up other work in remote areas due to a lack of primary care, aged care, or disability transport. This greatly impacts the accessibility of services and the ability for ambulances to reach the most remote patients. Indeed, MMM 7 shows the largest age-standardised per capita deficits in ambulance expenditure.
Although ambulance funding in regional, rural and remote areas mostly reflects the greater need and difficulty of service delivery in each area, there is still a long way to go before reaching equitable healthcare and funding for our country communities.
The NRHA continuously works to improve the rural healthcare gap across the board, advocating for national prioritisation of healthcare, disability and aged care services for rural communities. Whilst this work occurs, the ambulance workforce is a lifeline for rural communities, and the quality of care and services provided does not go unrecognised. Paramedics are not only vital to rural healthcare, but are an integral part of the communities they live and work in. Your contribution to equitable access to care in rural and remote Australia is greatly valued – by patients, practitioners, and entire communities.
About the NRHA: The National Rural Health Alliance comprises 55 national organisations committed to improving the health and wellbeing of the over seven million people in rural and remote Australia.
Our diverse membership includes representation from health professional organisations, health and aged care service providers, health educators, researchers, the Aboriginal and Torres Strait Islander health sector, and students. The Alliance provides a united voice for sustainable and affordable health services.
Table 3
State and territory ambulance expenditure by MMM area, FY2023-24
Expenditure estimated using paramedicine practitioner workforce distributions (2023) from DoHDA's Health Workforce Dataset and the AIHW dataset on ambulance service organisation expenditure.
Standing Together: Suicide Prevention in the Paramedic Profession
Dr Shohreh Majd, The Council of Ambulance Authorities
September was Suicide Prevention Month, a time to deeply reflect on the emotional well-being of all ambulance personnel, paramedics, call-takers, dispatchers, communications staff, and management alike, whose work is both indispensable and profoundly challenging.
What Research Reveals
Paramedics face extraordinarily demanding conditions: exposure to trauma, shift work, high responsibility, and organisational pressures. These factors contribute to significantly elevated risks to their mental health.
• A retrospective study (2001–2017) using Australian coronial data revealed an age-standardised suicide rate of 14.3 per 100,000 among emergency service workers (ESWs), compared to 9.8 per 100,000 in other occupations. Among ESWs, ambulance personnel showed a trend toward elevated risk (Relative Risk = 1.41; 95% CI 1.00–2.00; p = 0.053).
• Another study (2001–2012) found age-adjusted suicide rates across emergency and protective service workers reaching 22.4 per 100,000 for males and 7.8 per 100,000 for females, compared to 15.5 (males) and 3.4 (females) in other occupations. Highest risk was among ambulance personnel.
• A landmark ABC report quantified that between 2000–2012, 26 paramedics died by suicide in Australia (out of 110 total emergency worker suicide deaths), with poisoning accounting for over 40% of paramedic suicides.
• A systematic review across 39 international qualitative studies (2000–2018) found that ambulance professionals report high levels of cumulative trauma, poorly managed shifts, lack of organisational support, and emotional isolation.
• A meta-analysis across high-income countries (17,045 paramedics) found the pooled 12-month PTSD prevalence in paramedics was 20%, significantly higher than both general working populations (3.1%) and those affected by disasters (12–15.6%).
• Broader studies report prevalence estimates among ambulance personnel of approximately 11% PTSD, 15% depression, 15% anxiety, and 27% general psychological distress; notably, one Canadian study found 44.5% screened positive for one or more diagnosable mental disorders, around four times higher than the general population (10.1%).
Why Paramedics and Their Support Teams Are Vulnerable
Paramedics, call-takers, dispatch staff, and managers alike are exposed to high-stress environments, cumulative trauma, stigma around seeking help, shift unpredictability, and emotional fatigue, which are the factors that heighten risk across the board.

Member Services: Wellbeing and Psychological Safety at the Forefront
At the Council of Ambulance Authorities (CAA), we acknowledge that our people, including those behind the scenes, face real emotional challenges. Our member services maintain robust programs to ensure psychological safety is integral, not optional. If you're struggling, reach out, whether you're on the frontline, behind the radio, or in a management role, your health matters.
Expanding the Scope: Inclusive Support for All Roles
• Paramedic wellbeing starts with recognising the entire ecosystem.
• Call centres and dispatch staff, who make critical decisions under pressure, are exposed to trauma and deserve equal access to mental health support.
• Managers and leaders, responsible for supporting others, often overlook their own needs; tailored support must reach them too.
Evidence-Based Initiatives in Australia and New Zealand
• Ambulance Victoria: Mental Health & Wellbeing Action Plan (2022–2025).
• NSW Ambulance: Staff Psychology Service.
• Ambulance Victoria: Peer Support Dog Program.
• Monash University & Ambulance Victoria: Telehealth Trauma Group Program.
• Everymind’s “Minds Together” Program for Families & Friends.
• Ambulance Victoria: Family Safe Space Resource.
• Beyondblue’s “Good Practice Framework” for First Responders.
• Beyondblue & Ambulance Victoria (2016): Paramedic Mental Health Training.
• NSW Ambulance: Wellbeing Workshop Program.

Evidence-Based Strategies to Support Wellbeing
• Peer Support and Debriefing: Informal and structured peer networks provide critical emotional containment and normalise vulnerability (e.g., Psychology Service check-ins, peer support dogs).
• Confidential Access to Mental Health Services: Ensuring paramedics can access psychological support and Employee Assistance Programs (EAPs) without fear of stigma or career consequences (e.g., counselling, telehealth programs).
• Mental Health Literacy Training: Educating all staff to recognise early warning signs in colleagues and self (e.g., beyondblue-AV training modules).
• Fatigue & Rostering Management: Implementing predictable shifts and mandatory rest reduces stress accumulation.
• Means Restriction: Given that poisoning is a common method among paramedics, safely managing access to lethal means may be lifesaving: (poisoning risk).
• Support for Families and Managers: (e.g., ‘Minds Together,’ Family Safe Space).
Final Thoughts
Every statistic represents a human: a colleague, a friend, a family member. Through acknowledging and addressing the mental health risks across all ambulance service roles, not just paramedics, we honour those who struggle, enhance resilience, and strengthen services.
This Suicide Prevention Month, the CAA pledges steadfast commitment to psychological safety, for every radio operator, dispatcher, manager, and paramedic. Compassion, action, and unity are our strongest tools.
Resources and Support
If you or someone you know needs help:
Lifeline (AU) 13 11 14
Beyond Blue (AU) 1300 22 4636
1737 (NZ)
Free call or text for support
References
ABC News. (2015, June 3). Figures reveal high suicide rates amongst emergency workers: 26 paramedics died by suicide, poisoning common. ABC. https://www.abc.net.au/news/2015-06-03/new-figures-revealhigh-suicide-rates-amongst-emergency-workers/6518250
Ambulance Victoria. (2022). Mental Health & Wellbeing Action Plan 2022–2025. https://www.ambulance.vic.gov.au/sites/default/ files/2024-11/Mental-Health-Wellbeing-Action-Plan-2022-2025.pdf
Ambulance Victoria. (n.d.). Family Safe Space. https://www.ambulance. vic.gov.au/family-safe-space
Ambulance Victoria. (n.d.). Peer Support Dog Program. https://www. ambulance.vic.gov.au/peer-support-dog/
Beyond Blue. (2020). Good practice framework for mental health and wellbeing in first responder organisations. https://esf.com.au/wp-content/ uploads/2020/05/BB-Good-Practice-Framework-for-MH-Wellbeing-in1st-responder-organisations.pdf
Everymind. (n.d.). Minds Together: Supporting the mental health of paramedics. https://everymind.org.au/programs/family-friends-andcarers-programs/minds-together/family-and-friends-supporting-themental-health-of-paramedics
Hoell, A., Kourmpeli, E., & Dressing, H. (2023). Work-related post-traumatic stress disorder in paramedics in comparison to data from the general population of working age: A systematic review and meta-analysis. Frontiers in Public Health. https://doi.org/10.3389/ fpubh.2023.1151248
Lawn, S., Roberts, L., Willis, E., Couzner, L., Mohammadi, L., & Goble, E. (2020). The effects of emergency medical service work on the psychological, physical, and social well-being of ambulance personnel: A systematic review of qualitative research. BMC Psychiatry, 20, 348. https://doi.org/10.1186/s12888-020-02752-4
Milner, A., Witt, K., Maheen, H., & Lamontagne, A. D. (2017). Suicide among emergency and protective service workers: A retrospective mortality study in Australia, 2001 to 2012. Work, 57(2), 281–287. https:// doi.org/10.3233/WOR-172554
Monash University. (2020). Telehealth trauma program to treat ambulance paramedics. https://www.monash.edu/turner-institute/newsand-events/latest-news/2020-articles/telehealth-trauma-program-totreat-ambulance-paramedics
NSW Ambulance. (2022). Two finalists in CAA Awards. https://www. ambulance.nsw.gov.au/news/news-items/two-finalists-in-caa-awards NSW Ambulance. (n.d.). Staff Psychology Service. https://www. ambulance.nsw.gov.au/careers/paramedic/staff-support-programs
Petrie, K., Butterworth, P., Gunnell, D., & Milner, A. (2023). Suicide among emergency service workers: A retrospective mortality study of national coronial data, 2001–2017. Psychological Medicine, 53(12), 5470–5477. https://doi.org/10.1017/S0033291722002653
Premier of Victoria. (2016). New mental health support to help paramedics cope with trauma. https://www.premier.vic.gov.au/newmental-health-support-help-paramedics-cope-trauma
Williams, B., et al. (2019). Monash study reveals high incidence of PTSD in paramedics and student paramedics. Monash University. https://www. monash.edu/medicine/news/latest/2019-articles/monash-study-revealshigh-incidence-of-ptsd-in-paramedics-and-student-paramedics

Dr. Shohreh Majd Research and Policy Manager, The Council of Ambulance Authorities
A/Professor Shohreh Majd is a Neuroscientist, University Lecturer, and Research and Policy Manager with expertise in workplace stress and trauma.
With over 15 years in academia and policy, she focuses on workforce wellbeing in ambulance services, addressing critical issues like Occupational Violence in paramedicine through neuroscience and evidencebased strategies.
Compassionate Communication with Family in the Event of a Death:
Six Important Steps
Dr Natalie Anderson, The University of Auckland
Emergency ambulances are called to thousands of deaths in communities across Australasia every year. While some occur in the context of advanced illness or frailty, others are sudden or have unexpected elements.
Resuscitation may have been attempted. Information is often incomplete. Acutely bereaved family members may be experiencing the worst day of their lives, and need clear and compassionate communication from emergency services.
Paramedics’ technical proficiency can be developed through repetition and assessed against clear criteria. In contrast, the ability to connect with people during moments of profound uncertainty and distress relies on non-technical skills. The ability to connect with people in times of uncertainty, chaos and distress requires a combination of non-technical skills that are much harder to teach, learn and evaluate.
Communicating effectively with family in the context of a death is essential, yet even experienced paramedics can find these situations challenging. Modern societies have very poor death literacy. Despite death being universal, many people avoid discussing or planning for it. Few individuals articulate their wishes regarding aging, frailty, or end-of-life care, leaving families unprepared when death occurs.
Within emergency ambulance services, death is often framed as an adverse outcome. Care in the event of a death, receives little attention in clinical guidelines,1 quality indicators, or research.2 For decades, paramedics have reported feeling underprepared for situations involving death, dying, and grief.3 While contemporary education may include palliative care content, these principles can be difficult to apply in sudden or unexpected deaths. Paramedics consistently express a desire for more training in death notification and family support. Feeling ill-equipped for these encounters is associated with emotional distress and burnout.4
This article introduces a six-step model for compassionate communication with family when emergency services are called to death. It is not a prescriptive checklist but a framework highlighting key elements of skilled, empathetic interaction.
01 04 02 05 03 06
Connection
Warning Shots
Death Notification
Space and Empathetic Presence
Supportive Actions and Cultural Responsiveness
Next Steps
1 Connection
Begin by introducing yourself and your role. Ask inclusive questions to ascertain connections to the dying or deceased. Don’t guess or make assumptions. People’s closest social connections may involve LGBTQIA+ or extended family relationships. Assess whether you are being understood and identify any communication barriers, such as language differences or hearing impairments. Establishing connection early lays the foundation for trust and support.
2 Warning Shots
When possible, provide cues that the situation is serious. Phrases such as “Things aren’t looking good” can help prepare families for bad news. Skilled clinicians observe verbal and non-verbal cues to gauge understanding. In some cases, there is no opportunity for gradual disclosure, and you may need to begin with a clear preface such as “I have difficult news.”
3 Death Notification
Deliver the news clearly and without euphemism: “I’m sorry, [name] has died.” Families will seek additional details as and when they are ready. While your tone and body language should convey compassion, avoid softening the language to the point of ambiguity. Breaking bad news well does not make the news less tragic, but it can reduce confusion and distress.
4 Space and Empathetic Presence
This is probably the most difficult and often-avoided phase. Emergency clinicians are accustomed to alleviating suffering through action - administering medications, providing reassurance, restoring order. Sitting with raw grief can feel very uncomfortable. However, quiet presence is often the most powerful form of support. Do not leave the bereaved alone unless they request it. Avoid minimising statements such as “At least he died at home” or “At least she lived a long life.” Instead, allow space for expression of emotion, without rushing to provide solutions or additional information. Sometimes, kindness is best demonstrated through quiet, attentive presence.
5 Supportive Actions and Cultural Responsiveness
Family members will often signal when they are ready to consider next actions. Resist the urge to rush this transition. Supportive actions may include contacting relatives, repositioning the deceased, or offering to make a cup of tea or coffee. Food frequently serves as a cultural ritual, marking a shift from immediate grief to communal support, but take care to ensure the timing and location are appropriate.
Cultural, spiritual, and emotional responses to death are highly diverse. Emergency services are used to arriving with the answers, the kit, the skills, the knowledge –but this is not the time to impose your assumptions. Instead, offer time, patience, and openness. You do not need to be an expert in every cultural practice – people know their own cultural needs.
Ask questions such as:
“What are you most worried about right now?”
“Who should we contact to support you?”
“What is most important for you to know or do at this point?”
These questions empower families to identify and articulate their priorities and values.
6
Next Steps
Most deaths do not require coronial investigation, but unexpected deaths or those where a certifying practitioner cannot be identified will often involve police attendance. Explain that this is routine and does not imply wrongdoing; it ensures legal and procedural requirements are met. Guiding families through next steps may also include facilitating contact with a funeral director or providing information about available support services.

Dr Natalie Anderson Senior Lecturer, University of Auckland & Emergency Nurse, Health New Zealand
Final Thoughts
Every death is unique, as is every family’s response. Listening, observing, and responding with empathy are essential. When paramedics connect early, communicate clearly, and demonstrate compassion, they offer humanity at a time when it is most needed. Families may not remember your every action or word, but will forever remember that you were there, supporting them, guiding them and making sure they weren’t alone.
References
1. Satchell E, Gott M, Juhrmann M, Dicker B, Anderson NE. Emergency ambulance care of families during death, dying, and bereavement: A document analysis of Australian and Aotearoa New Zealand clinical practice guidelines. Australas Emerg Care. 2025.
2. Satchell E, Carey M, Dicker B, Drake H, Gott M, Moeke-Maxwell T, Anderson N. Family & bystander experiences of emergency ambulance services care: a scoping review. BMC Emerg Med. 2023;23(68).
3. Anderson NE, Slark J, Gott M. When resuscitation doesn’t work: A qualitative study examining ambulance personnel preparation and support for termination of resuscitation and patient death. Int Emerg Nurs. 2020;49:100827.
4. Campos A, Ernest EV, Cash RE, Rivard MK, Panchal AR, Clemency BM, et al. The association of death notification and related training with burnout among emergency medical services professionals. Prehosp Emerg Care. 2021;25(4):539-48.
Dr Natalie Anderson was invited to present on this topic at the ACPIC 25 conference because she is an internationally recognised expert in resuscitation decision-making and death, dying and bereavement in emergency care. Natalie is a currently practising emergency nurse academic with decades of clinical, teaching and research experience and a background in psychology.
AMBULANCE ELECTRIC Rise of the
Global ambulance services have been working tirelessly to move towards greener and more sustainable solutions for their services, including the introduction and implementation of EV ambulances.
First Magazine has spoken with various services from around the world about their implementation of these sector-changing vehicles. The CAA continue to be committed to supporting Ambulance Health Services to work towards a more sustainable future.
British Columbia Emergency Health Services (BCEHS), Falck and Hato Hone St John have provided an insightful snippet into the effectiveness of these vehicles in their services.


BCEHS MAKES HISTORY WITH
CANADA’S FIRST EV AMBULANCE PATIENT TRANSPORT

Sam Starr Manager, Sustainability & Fleet Decarbonization, BC Emergency Health Services
OnJune 11, 2025, BC Emergency Health Services (BCEHS) successfully completed Canada’s first emergency patient transport, using a Type 2 electric ambulance—a groundbreaking milestone in the evolution of sustainable emergency healthcare.
This historic event follows BCEHS’s earlier achievement in 2024, when it deployed North America’s first Code 3 Mustang Mach-E Paramedic Response Unit (PRU)—a high-performance electric response vehicle that demonstrated EVs can meet the rigorous demands of emergency services.
These innovations are part of a broader Strategic Sustainability and Decarbonization Plan, supported by a Clean Fleet Plan that aligns with Provincial climate mandates. The strategy of ‘Optimise > Rightsize > Electrify’ reflects the understanding that decarbonization goes beyond simply switching to electric vehicles; it requires smarter fleet management, platform innovation, and strategic infrastructure investment. Currently, 93% of BCEHS’s reportable emissions stem from its 650 active Type 3 ambulances. In response, BCEHS is piloting a Type 3 Ford Transit platform, which is achieving approximately 20% lower emissions in an operational duty cycle. At the same time, due to the limited availability of OEM electric ambulance platforms, BCEHS is assessing the feasibility of repowering existing
ambulances with electric drivetrains, a pioneering approach in Canada’s healthcare sector.
Though BCEHS remains carbon neutral through the purchase of annual offsets, the organisation is focused on making real emissions reductions. Backed by the Province’s Carbon Neutral Capital Planning budget, BCEHS is expanding its EV support fleet and building out critical charging infrastructure across ambulance stations and hospitals.
To guide this transformation, BCEHS has developed advanced simulations and modelling to determine infrastructure requirements and operational feasibility, key steps in preparing for the launch of a pilot Electric Repower Ambulance program. These efforts are being coordinated under the leadership of BCEHS’s Fleet Operations team. With each milestone, BCEHS is redefining what’s possible in emergency healthcare, proving that sustainability, innovation, and top-tier patient care can move forward together.

Sustainability First
OVERCOMING BARRIERS
of the Electrification of Ambulance Vehicles at Falck.
Where are we now?

Hildur María Hólmarsdóttir Bergmann Ambulance Sustainability Business Partner

David Nri Head of Environmental Sustainability, Falck
Falck operates ambulance and patient transport services in more than ten countries around the world. Falck has ambitious climate targets and has been working to decarbonise our fleet for several years. While decarbonising smaller vehicles has progressed at pace, larger vehicles with more complicated operational requirements (such as emergency and qualified patient transport ambulances) have presented substantial barriers. Here we discuss six primary challenges, the strategies employed to overcome them, and the impending launch of a global ambulance decarbonisation network to collaborate on solutions.
Firstly, payload restriction. EVs' higher weight, often exceeding the 3.5-ton limit for light commercial vehicles, complicates operational viability. However, regulatory frameworks are evolving as demands for specialised equipment increase payloads beyond this limit, even for fossil-fuelled vehicles.
Secondly, range limitations were, and to an extent still are, a concern. Rapid advancements in battery technology have mitigated this; Falck now procures QPTS EVs with a theoretical range of approximately 400 km. This extended range allows for full shifts in urban areas without mid-shift recharging, if dispatching is adjusted to account for the limitations.
Thirdly, integration with internal power systems. EVs feature complex electrical architectures, making it challenging to seamlessly integrate essential equipment like blue lights and sirens. Close collaboration with manufacturers and conversion companies has largely overcome this, leading to standardised interfaces for bespoke emergency systems.
vehicles

The fourth challenge has been certifications and compliance. Ambulance vehicles must adhere to stringent European standards (e.g., CEN 1789). Converting an EV chassis into a compliant vehicle necessitates a time-consuming certification process. Increasing experience and collaboration are streamlining these procedures.
The fifth barrier has been the price. While historically higher, total cost of ownership (TCO) analysis now shows electric vehicles are demonstrably lower than fossil-fuelled equivalents in most cases, without subsidies. This is driven by significantly lower fuel and maintenance costs.
Finally, charging infrastructure. While public and private charging has rapidly developed: charging points where ambulances already are required to wait, particularly at hospitals, remain rare. Charging during patient handovers would radically increase viable range during shifts. Addressing this infrastructure gap, remains a critical future objective for Falck.
No one actor can solve these challenges; they demand innovation and collaboration across suppliers, ambulance services, and hospital systems. That’s why we are planning to launch the Ambulance Decarbonisation Network in 2026, bringing together interest and expertise from across the world. Through a series of webinars, this network will holistically explore the challenges inside and out of the ambulance, including recognising that the most sustainable ambulance trip is the one that never needs to happen.
If you are interested in being a part of this network, then please reach out to either author on LinkedIn or email hildur.bergmann@falck.com
One of Falck’s electric QPTS
that entered operation in Copenhagen in 2024.
MINIMISING IMPACT MAXIMISING PERFORMANCE
Asa partner to the New Zealand health system, Hato Hone St John (HHStJ) delivers emergency ambulance services to over 90% of the country.
With around 350 sites and 1,300 vehicles in its fleet, HHStJ is conscious that the important services provided also contribute significant greenhouse gas (GHG) emissions.
They are also conscious of a growing risk to assets, infrastructure, and access to communities most affected by extreme weather events that are increasing because of climate change.
The diesel used (predominantly to fuel ambulances) accounts for around 88 per cent of HHStJ's Scope 1 emissions and 65 per cent of their total emissions.
To put that into perspective, if electricity, domestic travel and waste were added up, collectively these contribute a total of 10 per cent of HHStJ's total emissions, so becoming less reliant on diesel and petrolpowered vehicles would be a big win for more sustainable health care delivery in New Zealand.
With the support and investment of partner ASB Bank, in June 2024, HHStJ launched a 12-month trial of the first electric vehicle (EV) emergency ambulance in Australasia, to better understand how an EV ambulance could perform within a metropolitan area of New Zealand.
Hato Hone St John

Feasibility study measures include:
• Stakeholder buy-in: How do various stakeholders, including the New Zealand public, feel about EV use within an emergency ambulance service?
• EV technology: How does the battery perform under high-demand conditions (e.g. long shifts and high-speed travel), and what are the battery replacement or future upgrade options?
• Design and fit-out requirements: How can we reduce the weight of onboard equipment to maximise driving performance and range, and provide supplementary power to house batteries required for equipment?
• Operational capabilities: How do response times compare to those of standard ambulances in the fleet, and how do terrain and climate variables impact range?
• Charging infrastructure requirements and networks: Site electrical capacity constraints for charging infrastructure and charge time considerations.
• Financial implications: How does the whole-of-life cost of this EV ambulance compare to standard internal combustion engine (ICE) ambulances, and what’s the break-even point?
• Environmental impact: How do operating GHG emissions compare between this EV and other ICE ambulances in a New Zealand context, and what about emissions associated with the material, part production and batteries?
Early insights showed the EV emergency ambulance can successfully complete a metropolitan 12-hour shift.
HHStJ’s ambulance operations team report that it is comfortable, stable and fast to drive, and the patient compartment is 15 percent quieter than a standard ambulance. HHStJ is excited to share further findings with the Council of Ambulance Authorities once the 12-month report is finalised.
#ThankAFirstResponder
Our community
#ThankAFirstResponder

R U OK Day in ACT
Some members of the ACT Emergency Services team have a special way of lending a paw; meet Banksy, Lachie, and Maddie. While emergency services personnel are always ready to help others, they often face challenging and emotionally demanding situations. That’s where these incredible support dogs come in.
#PeopleFIRST
Banksy is based at ESA Headquarters, where he plays a vital role in supporting staff across the agency. Lachie is the team’s Chaplaincy Support Dog, working full-time alongside the Associate Chaplain to provide comfort and connection. Maddie is ACTSES’ dedicated peer support mascot, a natural conversation starter who’s always ready to lift spirits and support the SES team.

Palliative Care in Tassie
Meet Lauren, Emma and Kim, Ambulance Tasmania’s Palliative Care Project team, who has developed new frameworks to support paramedics and operational staff to deliver better palliative and end-of-life care within the community.
Ambulance Tasmania clinicians, volunteers and patient transport officers all have an important role to play in the provision and education of palliative care to ensure the patients, their loved ones and the wider community are empowered to make decisions that adhere to their values and wishes.
HHSJ’s Community Cupboard
Hato Hone St John's Franklin team has a warm and fuzzy update about their Community Cupboard this winter. Thanks to the generosity of the local community, there have been some incredible donations, including handmade blankets, kids' toys, hot water bottle covers, and basic hygiene products. These donations ensure the Community Cupboard can continue to help over 350 babies, children and adults in need per month, keeping them warm, clean, and healthy, and truly making a life-changing difference in their lives.
#PeopleFIRST
#MeFirst
#PeopleFIRST

Ambulance Victoria Wear It Purple
#ThankAFirstResponder
Ambulance Victoria (AV) was proud to stand with LGBTQIA+ young people on Wear It Purple Day. A day founded to foster supportive, safe, empowering and inclusive environments for rainbow youth across the country. At AV, they understand that meaningful inclusion goes beyond one day. That’s why they continue to invest in safer practices, policies, and workplaces for LGBTQIA+ staff, volunteers, and communities guided by our Diversity and Inclusion Framework and informed by lived experiences.

#restartaheart
Team Effort

NAIDOC Week with St John WA
#ThankAFirstResponder
St John WA celebrated NAIDOC Week by supporting Aboriginal-led conferences and delivering first aid training all around Perth in a yarning style. Led by their First Nations First Aid Yarning Crew and the Youth and Community Engagement team, they engage with Elders first and then bring first aid education to community members in culturally appropriate language and places from local parks to community sheds.
Volunteer Star

Meet Eleisha, raising four kids, including baby Frankie and still smashing her volunteer goals. While on maternity leave, Eleisha completed her Ambulance Responder Training with SA Ambulance Service, adding to her Ambulance Assist qualification. She’s now back with Lameroo ‘team in green’, supported by her husband Ryan, a National Parks Ranger. Eleisha was able to pursue her long held dream of joining an ambulance service – a goal inspired by her grandfather, who once volunteered with St John Ambulance in Lameroo.
#ThankAFirstResponder
Recently, Sam and members of his care team reunited to celebrate his 61st birthday, a special occasion marking both his survival and resilience. While doing routine yard work at his parents’ property in Jimboomba, Sam didn’t see a tree stump hidden in the grass until his tractor’s front tyre hit it, throwing him under the rear tyre and causing a severe injury to his right leg. Queensland Ambulance Service Emergency Medical Dispatcher
Tegan Gillman guided Sam’s son Frank through using a belt as a tourniquet, a critical step that helped save Sam’s life. Paramedics Chelsey Orr, Eseta Reupena and Critical Care Paramedic Brendon Leech arrived quickly on scene, followed by senior supervisors and specialist clinicians. Despite intense pain and trauma, Sam remained positive and joked with the crew, sharing that his humour had been a key part of his recovery.

50 Years of Independence for PNG
In September, the National St John Ambulance Service of Papua New Guinea celebrated the golden milestone in their nation’s history –50 years of Independence. This historic milestone is a proud moment for every Papua New Guinean. It is a time to celebrate their unity, diversity, and resilience as people, while reflecting on how far they have come together as a nation.

#SustainableAmbulance
#ThankAFirstResponder

BUSTING
LEADERSHIP
Myths in Emergency & Prehospital Care
Dr Erica Kreismann – OneWild Coaching

Dr. Erica Kreismann
Founder and Executive Coach, OneWild Coaching
Erica Kreismann, MD, FACEM, is an Emergency Medicine specialist and boardcertified executive coach. Her passion for leadership and developing people to their greatest potential led her to found OneWild Coaching in 2022. OWC is grounded in the belief that leading with courage and kindness is the foundation for all great leadership and when we lead from the heart in a way that is authentic and real, we will change the world.
Erica moved to Tasmania 15 years ago, recently returning to the US to continue her adventures in building community and connection across continents. She can often be found tucked away with a book in front of the fire, or by following her oversized laugh. You can also follow her daily on LinkedIn.

Spend a few hours in the pre-hospital space; an ambulance on a busy shift, the communication centre at midnight, any scene, any jurisdiction - and you’ll see leadership everywhere. It might not always look like it does in the textbooks, but it’s there - in the calm reassurance, the decisive action, or wrapped up in quiet courage.
And yet, for all of us who have stepped into leadership roles - formally or informally –we have also inherited a whole set of myths and expectations. Stories we’ve been told about what it means to lead, what leadership “should” look like and how to do it “right.”
Stories that often do more harm than good.
It’s time we start busting those myths.
Leadership First

When we hold on to outdated or unhelpful beliefs, when we buy into the stories, we risk not only burning ourselves out but also perpetuating a model that doesn’t reflect contemporary leadership. If we want to change the narrative, it starts with rewriting the story.
Below are four of the most common leadership myths I’ve seen across 25 years in emergency medicine, in and out of the hospital - and what the truth really looks like.
Myth 1:
Leaders must have all the answers.
The truth: Leaders don’t need to know everything - they need to create the conditions where the right answers can emerge.
This sounds simple, yet by the time many of us have climbed the endless hierarchies, we have along the way also internalised expectations of those around us. Interestingly, it is the immature or insecure leader who feels compelled to have the final say. Leadership lives in the nuance. There are always (at least) two sides to a story, and the truth inevitably lives somewhere in between. A real leader can hold this tension and honour the complexities of it.
Leadership is, at its heart, imbued with deep curiosity, wells of courage and a capacity for extending grace. In healthcare, where the stakes are high and the pressure relentless, it’s easy to fall into the trap of believing you must be the allknowing authority. The problem? That belief is not only exhaustingit’s dangerous. It stifles conversation, inhibits innovation and makes trust impossible.
Teams function best when curiosity and collaboration drive decisionmaking. A strong leader is one who can say, “I don’t know - what do you think?” and mean it.
This isn’t about indecision. It’s about harnessing collective intelligence, embedding trust, and showing that humility is strength, not weakness. In fact, psychological safety - where people feel safe to speak up and challenge, is one of the strongest predictors of high-performing teams.
Myth 2: Leadership is about being in control.
The truth: Leadership is about influence, not control.
Control is a seductive fantasy. But in emergency and prehospital care, we know better than anyone that control is often an illusion. The temptation in those moments is often to shout louder – yet trust is forged in those fires, and it comes from a knowledge of ‘we’ve got this.’ Whatever that may look like.
The paradox is this: when we stop trying to control everything, our impact actually grows. Influence builds from steadiness, from role modelling, from showing up consistently, especially when things are hard, and from empowering others to step into their own agency.
Leadership does not sit with the loudest voices in the room, but rather with those whom the team would choose to follow anywhere.

Myth 3: Leadership means being tough, not tender.
The truth: Compassion and candour can - and must - coexist.
Too often, toughness gets mistaken for strength. We’ve been told to “leave emotions at the door,” to push through, never to let them see us sweat. But the reality is, teams don’t need stone-faced leaders. They need human ones. Leadership is fundamentally about our people. In all our/their messy, human glory. To deny that is to set ourselves up for failure.
Compassion doesn’t mean sugarcoating. Radical candour and its framework of ‘care deeply, challenge directly’ is one of the greatest gifts a leader can give. When leaders are present, empathetic, and still willing to have the hard conversations, they create teams that are resilient, loyal, and ready to go the distance.
Myth 4:
Leadership is about sacrifice - putting yourself last.
The truth: Sustainable leadership starts with the self.
Many of us in emergency and prehospital care wear sacrifice like a badge of honour. The skipped meals, the missed sleep, the family events traded for extra shifts. But here’s the hard truth: when we chronically put ourselves last, we erode not just our own health, but also our capacity to lead well.
Burnt-out leaders can’t model clarity, compassion, or courage. Our teams notice when we’re running on empty, and they hear the message that we are sending loud and clear. Availability is not the same as leadership. Constant presence creates dependency. True leadership is about building capacity.
Self-leadership is not selfish - it’s essential, and it’s one of the toughest lessons for many of us to learn. It means setting boundaries, asking for help, taking recovery seriously, and recognising that our wellbeing is not optional if we want to sustain our ability to serve others.
Bringing it home
Leadership in any iteration – but especially in the emergency and prehospital space - will never be neat or easy. It’s messy, unpredictable, and profoundly human. But by letting go of these old myths, we can step into something better - leadership that is honest, courageous, and deeply connected to the people we serve.
So, I’ll leave you with this:
• Where in your practice are you still clinging to the myth of control?
• When was the last time you let yourself say, “I don’t know”?
• How might your team shift if you led with both compassion and candour?
• What would it look like to lead yourself with the same care you give your patients?
At the end of the day, leadership isn’t about being the hero at the centre of the story. It’s about creating the conditions where everyonepatients, colleagues, and yes, even ourselves - can thrive.

cqu.edu.au

globalpointofcare.abbott

sdsi.com.au

acu.edu.au

corvanta.com

paramedics.org

agili8.com

www.angels-initiative.com

bluelightcard.com.au

careopinion.org.au

device.com.au

hexagon.com
austrokealliance.org.au
belgraviaapparel.com

bmw.com/en-au/home.html

deccanintl.com

emvision.com.au

home.id.com.au
bus4x4.com.au

dedalus.com/anz

goodsamapp.org

theinsgroup.com.au
amtek.net.au

belgraviahc.com.au

carecompany.com.au
dementia.org.au

healthcaresoftware.com.au
jdhealthcare.com.au
CAA helps provide an important link between the ambulance sector and businesses that provide goods and services for this industry. It’s instrumental in providing networking and partnering opportunities. Don’t hesitate to reach out to organisations of interest.

laerdal.com/au

livingstone.com.au


medicaldev.com

mercedes-benz.com.au/vans midmed.com.au

orhltd.com

prioritydispatch.net/en

stryker.com/au/en

outcomehealth.org.au

rappaustralia.com.au

tacmedaustralia.com.au

tollgroup.com
totalmobilesolutions.com.au

workweargroupuniforms.com.au
zoll.com
mesha.org.au
medicalert.org.au

motorolasolutions.com
philips.com.au/healthcare prehos.com

solventum.com
stemlogic.co

titanprehospital.com

utas.edu.au
tlcforkids.org.au

wla.edu.au
Interested in becoming a part of The Directory? Contact admin@caa.net.au






Follow us on Facebook
The Council of Ambulance Authorities
Find us on X
@CAAAustralasia
Connect with us on LinkedIn
The Council of Ambulance Authorities Inc.
Subscribe to our channel Council of Ambulance Authorities

For information on other CAA activities please visit
