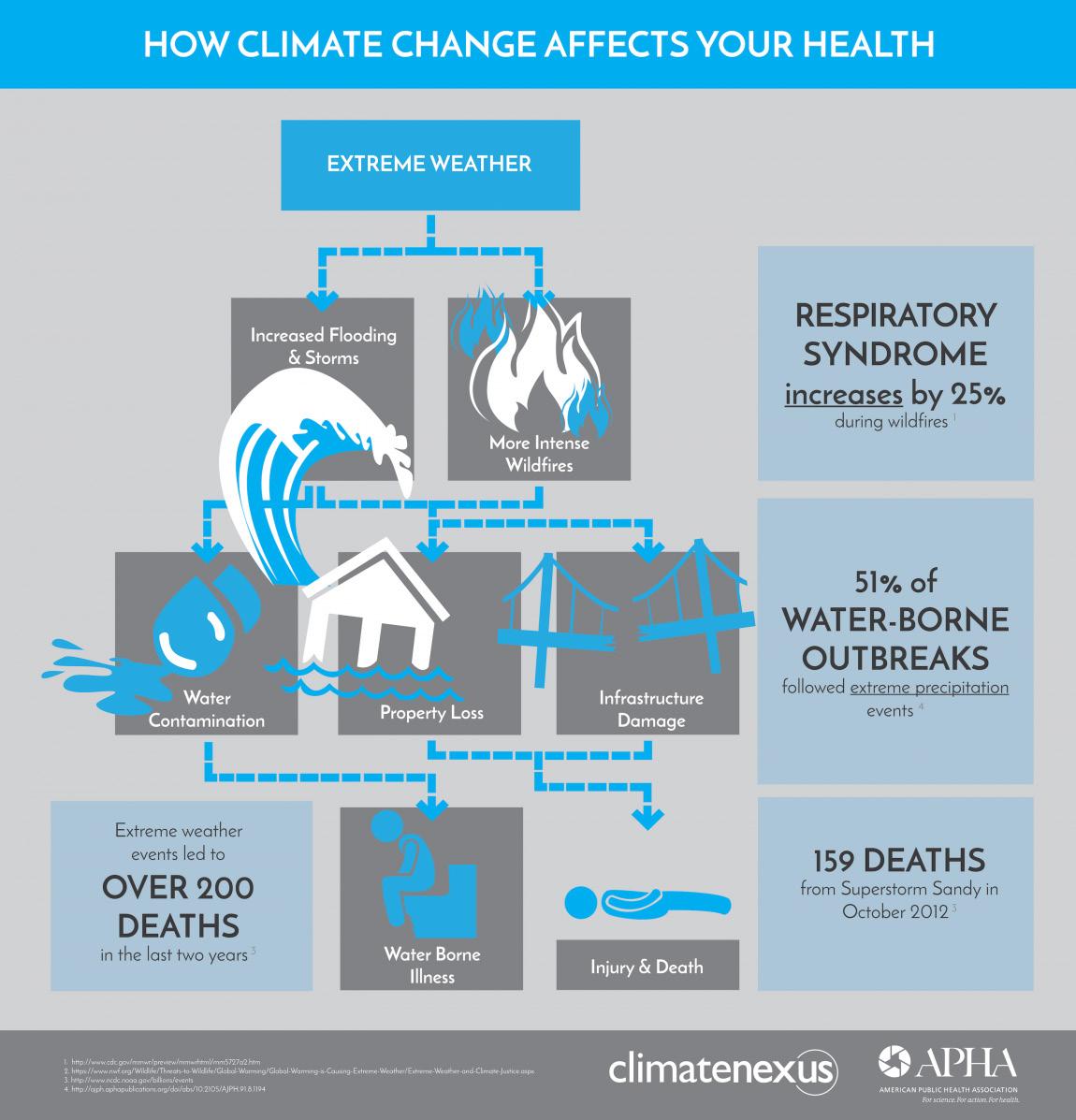
Chapter Three: Extreme Weather Events and Human Health
Increasing frequency and intensity of extreme weather events, such as heatwaves, hurricanes, and floods, pose immediate risks to human health.
Heatwaves can lead to heatstroke, dehydration, and cardiovascular stress, while floods and hurricanes can cause injuries, displacement, and psychological distress.(19)
Prolonged exposure to extreme heat can lead to heatstroke, a potentially lifethreatening condition. Heatstroke occurs when the body’s core temperature rises above 40°C (104°F), resulting in symptoms such as high body temperature, altered mental state, rapid heartbeat, and organ failure.(20) High temperatures and excessive sweating during heatwaves can cause dehydration. Dehydration can lead to dizziness, fatigue, confusion, and in severe cases, kidney damage or heat exhaustion (21). Heatwaves can also place a significant burden on the cardiovascular system, especially in vulnerable individuals with pre-existing heart conditions. The combination of high temperatures, humidity, and physical exertion can increase the risk of heart attacks, strokes, and other cardiovascular events.(22)
Hurricanes and floods can result in multiple health risks, both during and after the events. Strong winds, flying debris, and collapsing structures during hurricanes can cause injuries ranging from cuts and bruises to severe trauma. In flood situations, individuals may encounter drowning hazards, injuries from debris, or electrical hazards.(23) They often lead to forced displacement, with individuals seeking refuge in temporary shelters or unfamiliar environments. Displacement can disrupt access to healthcare, clean water, sanitation facilities, and necessary medications, increasing the risk of illness and exacerbating existing health conditions.(24)
Natural disasters can cause significant psychological distress, including post-traumatic stress disorder (PTSD). Individuals who experience or witness life-threatening situations, such as hurricanes or floods, may develop symptoms such as intrusive memories, flashbacks, nightmares, and hypervigilance. The ongoing stress and disruption caused by the aftermath of a natural disaster can contribute to the persistence of PTSD symptoms.
The fear of recurrence, coupled with the challenges of rebuilding, can create a prolonged state of psychological distress. Natural disasters can also cause anxiety, depression, and grief. The loss of homes, possessions, and community ties can have long-lasting psychological effects on individuals and communities affected by hurricanes and floods.(25)
Infectious Diseases
Climate change affects the distribution and transmission patterns of infectious diseases.
Warmer temperatures and altered precipitation patterns create favourable conditions for disease vectors like mosquitoes, resulting in the spread of diseases such as malaria, dengue fever, and Zika virus.(17) Altered precipitation patterns also play a role in the spread of infectious diseases. Heavy rainfall, often associated with climate change, creates breeding grounds for mosquitoes by creating stagnant water bodies, providing them with optimal conditions for reproduction.
The warmer temperatures associated with climate change boost the reproduction of mosquitoes and enhance their capacity to transmit diseases. Mosquitoes thrive in warm and humid environments, and as temperatures rise, their populations expand into new geographical regions. This expansion exposes previously unaffected areas to the risk of mosquito-borne diseases.(26)
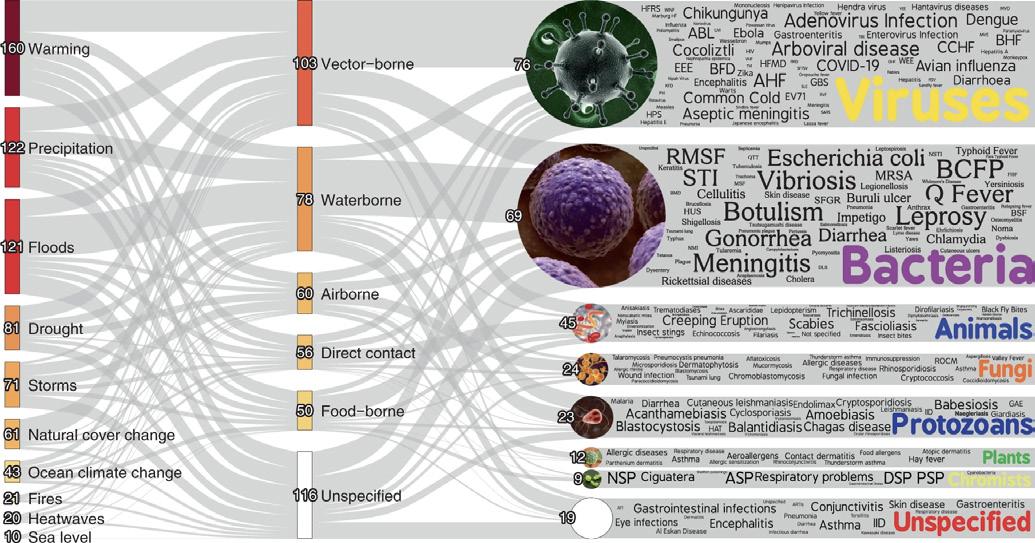
Pathogenic Diseases Aggravated by Climatic Hazards.
Source: Mora, C., McKenzie, T., Gaw, I. M., Dean, J. M., von Hammerstein, H., Knudson, T. A., Setter, R. O., Smith, C. Z., Webster, K. M., Patz, J. A., & Franklin, E. C. (2022). Over half of known human pathogenic diseases can be aggravated by climate change. Nature climate change, 12(9), 869–875
Malaria, a life-threatening disease caused by parasites transmitted through infected mosquitoes, is particularly sensitive to climate conditions. The increased availability of suitable habitats for mosquitoes due to climate change has expanded the geographical range of malaria transmission. Regions that were previously considered low risk have experienced an upsurge in malaria cases.(27)
Dengue fever, another mosquito-borne viral disease, has also exhibited increased prevalence in areas affected by climate change. The expansion of mosquito populations into new territories, driven by rising temperatures, has led to the geographic spread of dengue fever. This disease poses a significant health burden, with millions of cases reported annually.(28)
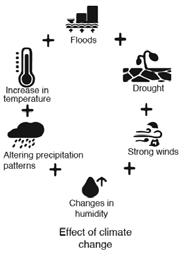
The Zika virus, which gained global attention in recent years, is primarily transmitted by Aedes mosquitoes. Climate change has expanded the distribution of Aedes mosquitoes to regions where the Zika virus was not previously endemic. This has resulted in localised outbreaks and increased the risk of Zika virus infection, which can have severe implications for pregnant women and their unborn children.(29)
Effects
of Climate Change and Spread of ‘Zika’ Virus
Source: Asad, Hina and Carpenter, David O.. “Effects of climate change on the spread of zika virus: a public health threat Reviews on Environmental Health, vol. 33, no. 1, 2018, pp. 31-42.
Excessive rainfall can overwhelm natural drainage systems, rivers, and urban infrastructure, leading to flooding. This is particularly problematic in areas with poor drainage systems or where urbanisation has altered natural water flow. Flooding can force people to evacuate their homes and communities, leading to the displacement of entire populations. This can overwhelm sanitation infrastructure, contaminating water sources with sewage and other pollutants. Disruption of sanitation systems increases the likelihood of contamination of drinking water, leading to a higher incidence of waterborne diseases such as cholera, dysentery, and typhoid. In crowded temporary shelters, the spread of these diseases can be rapid and difficult to contain.(30)
The Impacts of Climate Change on the Occurrence of Water-Borne Diseases
Environmental Temperature
Environmental Temperature
Climate Change
Climate Change
Flooding Intense Precipitation
Flooding Intense Precipitation
Drought
Drought
Seasonal variations in pathogen spread
Seasonal variations in pathogen spread
Intense precipitation impacts pathogen proliferation
Intense precipitation impacts pathogen proliferation
Elevated pathogen prevalence during floods
Elevated pathogen prevalence during floods
Water storage cleanliness and hygiene are compromised
Water storage cleanliness and hygiene are compromised
Increase in water-borne diseases
Increase in water-borne diseases
Air Quality and Respiratory Health
Climate change contributes to poor air quality, primarily due to increased levels of ground-level ozone and particulate matter.
These pollutants can exacerbate respiratory conditions, including asthma and chronic obstructive pulmonary disease (COPD), leading to increased morbidity and mortality.(31)
Climate Change and Your Lungs
Extreme Heat
Extreme heat can exacerbate respiratory conditions like asthma and COPD, leading to difficulty breathing and increased risk of lung infections. Prolonged exposure to high temperatures can also worsen air quality, triggering inflammation and respiratory distress in vulnerable individuals.
Flooding
Floods can worsen lung health by promoting mold growth, triggering respiratory issues, and exposing individuals to contaminated water, leading to respiratory irritation and infections.
TIMELINE Infographic
Air Pollution
Climate-driven air pollution intensifies respiratory issues by raising levels of harmful pollutants like particulate matter and ozone, exacerbating lung conditions and increasing the risk of respiratory diseases.
Plant Pollen
Climate change can extend the pollen season and boost pollen levels, intensifying respiratory symptoms like allergies and asthma, ultimately worsening lung health.
Infectious Disease
Infectious diseases worsened by climate change, like dengue fever or Zika virus, can directly affect lung health through respiratory symptoms. Additionally, increased transmission rates in warmer climates heighten the risk of respiratory infections, exacerbating respiratory distress in affected populations.
The ground-level ozone forms when pollutants like nitrogen oxides and volatile organic compounds react in the presence of sunlight. Warmer temperatures and higher levels of sunlight associated with climate change promote the formation of ground-level ozone. Increased levels of ozone in the air can trigger respiratory symptoms, such as coughing, wheezing, and shortness of breath, and can also cause inflammation and damage to the respiratory system.(32)
Particulate matter, consisting of tiny particles suspended in the air, is another pollutant influenced by climate change. These particles can be directly emitted from sources like vehicle exhaust and industrial emissions, or they can form through complex chemical reactions in the atmosphere.
Climate change can affect particulate matter levels through factors such as altered wind patterns, increased wildfires, and changes in the frequency and intensity of dust storms. Fine particulate matter, known as PM2.5, can penetrate deep into the lungs and even enter the bloodstream, leading to respiratory and cardiovascular problems.(33
Estimated Excess Mortality Attributed to Air Pollution In Europe, and the Contributing Disease Categories
Source: https://www.eurekalert.org
Europe sees a staggering 790,000 additional deaths attributed to the presence of ambient air pollution.
Other non-communicab le Diseases
The impact of poor air quality on respiratory health is particularly significant for individuals with pre-existing conditions such as asthma and COPD. Climate change-associated pollutants can exacerbate these conditions, triggering asthma attacks and worsening COPD symptoms. For individuals with COPD, exposure to air pollutants can lead to increased coughing, production of mucus, shortness of breath, and a decline in overall lung function. This exacerbation can result in hospitalisations and a decreased quality of life.
Food Security and Nutrition
Climate change can also contribute to more frequent and severe wildfires, leading to the release of particulate matter and other pollutants. Inhalation of wildfire smoke can exacerbate respiratory conditions and pose a significant threat to individuals with pre-existing respiratory issues. Long-term exposure to high levels of air pollution has been linked to the development of respiratory diseases and increased mortality rates. This is not only due to the immediate impacts on respiratory health but also the cumulative effects on cardiovascular health, which can further complicate respiratory conditions.(34)
Climate change impacts agriculture, leading to disruptions in food production and availability.
Changes in temperature and precipitation patterns can reduce crop yields, impair food quality, and contribute to malnutrition and food insecurity, particularly in vulnerable populations.(35) Changes in temperature patterns can have detrimental effects on agricultural productivity. Rising temperatures can accelerate the rate of evaporation, leading to increased water stress for crops. This can result in reduced yields and stunted growth for various crops, including staple food crops such as wheat, rice, and maize (36). Additionally, extreme heat events can cause heat stress in plants, leading to physiological damage and reduced crop productivity.(37)
Alterations in precipitation patterns, including changes in the timing, intensity, and distribution of rainfall, also impact agricultural production. Increased frequency and intensity of droughts, coupled with irregular rainfall patterns, pose significant challenges for farmers in maintaining crop productivity. Insufficient water availability can lead to crop failure, reduced yields, reduced nutrient content in crops, and increased vulnerability to pests and diseases.(38)
The effect of climate change on the nutritional composition of crops can be reducing the quality and availability of key nutrients.
This has serious implications for the nutritional status and health of individuals, particularly in regions heavily reliant on subsistence farming and with limited access to alternative food sources.(39)
Interplay Between Climate Change, Food Security, Nutrition, and Human Health
Source: Gioxari A, Amerikanou C, Nestoridi I, Gourgari E, Pratsinis H, Kalogeropoulos N, Andrikopoulos NK, Kaliora AC. Carob: A sustainable opportunity for metabolic health. Foods. 2022 Jul 20;11 (14):2154.
The climate-related impacts on agriculture can have far-reaching consequences for food availability and quality.
Subsistence farming, often practiced in vulnerable regions, relies heavily on local crop varieties. Climate-induced changes can introduce uncertainties in crop yields due to altered growing conditions, affecting the stability of food production and availability. In regions where subsistence farming is a primary source of food, climate-induced changes that compromise the nutritional quality of crops can contribute to malnutrition. This is a serious public health concern, particularly for vulnerable populations, including children and pregnant women.(40)
Reduced crop yields and lower agricultural productivity can limit the availability of essential food commodities. When the availability of essential food commodities decreases, the basic economic principle of supply and demand comes into play. With lower supply and constant or increasing demand, food prices are likely to rise. This can result in financial strain for consumers, particularly those with limited resources. Vulnerable populations, including low-income households and communities in developing countries, are disproportionately affected by increases in food prices. A rise in the cost of staple foods can lead to food insecurity, malnutrition, and a decreased ability to access a balanced and nutritious diet.(37, 41)
Adopted from: https://farmingfirst.org
The Rising Costs of Staple Foods
Impacts of Climate Change on the Food System
REDUCED FOOD PRODUCTION
Higher food prices can lead to shifts in dietary patterns, with individuals and families opting for more affordable but less nutritious food options.
This can contribute to a decline in overall diet quality and an increased risk of malnutrition and diet-related health problems. Vulnerable populations, such as children, pregnant women, and the elderly, are particularly susceptible to the nutritional consequences of reduced access to nutritious foods.
This can have long-term implications for physical and cognitive development, especially in children. Vulnerable populations are particularly susceptible to the adverse impacts of climate change on agriculture. Small-scale farmers, rural communities, and low-income populations often lack the resources and adaptive capacity to cope with the challenges posed by climate change. These populations may face increased food insecurity, malnutrition, and poverty because of reduced agricultural productivity and limited access to markets (37).
Mental Health and Wellbeing
There is a consensus that climate change intensifies established risk factors associated with known mental disorders.
(42)
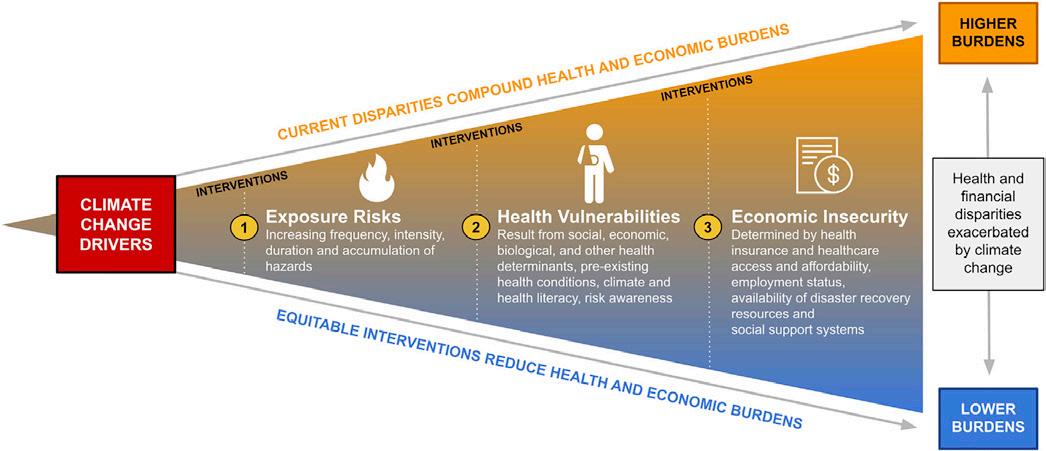
The impact of climate change on mental health vulnerability is expected through both direct pathways (e.g., severe weather events) and indirect pathways (e.g., heightened physical health burdens, disruptions to social and economic structures, compelled migration). Loss of homes, livelihoods, and social support networks can lead to psychological distress, anxiety, depression, and PTSD.(44)
Climate Change and Mental Health
Mental-health vulnerability increases in a nonlinear way through exposures that operate with additive, interactive, and cumulative effects (e.g., extreme weather events, heat exposure, worry about climate change).
At the same time, plasticity decreases, and risk of exposures to new threats rises with time and because of unmitigated climate change (green-yellow triangle and yellow-orange triangle). Adaptation and prevention efforts (e.g., effective disasterresponse planning, climate-change education) that begin early are more successful at reducing mental-health risk (low-risk trajectory) compared with efforts that begin in adolescence or adulthood (high-risk trajectory), especially for vulnerable populations.
The effect of timing of adaptation and prevention on mental-health vulnerability in the context of climate change
Source: World health organisation; Climate change. 12 October 2023
The experience of natural disasters, such as hurricanes, floods, and wildfires, can have immediate and long-term psychological effects on individuals and communities.
The sudden loss of property, personal belongings, and even loved ones can lead to profound grief, shock, and trauma. Studies have shown that survivors of natural disasters are at an increased risk of developing mental health disorders, including anxiety and depression.(45, 46)
Displacement, another consequence of climate change-related events, further compounds mental health challenges. When individuals are forced to leave their homes and communities due to rising sea levels, droughts, or other environmental factors, they face a multitude of stressors. Displaced individuals often experience a sense of loss, disconnection, and uncertainty about the future. The loss of familiar surroundings and social support networks can contribute to feelings of isolation, depression, and a loss of identity.(47, 48) PTSD is a common mental health outcome following climate change-related events. Individuals who have experienced or witnessed traumatic events, such as surviving a natural disaster, may develop symptoms such as intrusive thoughts, flashbacks, nightmares, and hyper-vigilance. These symptoms can persist long after the event and significantly impact daily functioning and overall wellbeing.(49)
Of particular concern are children and adolescents, given their rapidly evolving brains, heightened susceptibility to diseases, and limited ability to navigate or adapt to the emerging threats and consequences. This demographic group, more than any other, tends to harbor significant worries about the implications of climate change.
Considering a developmental life-course perspective it appears that climatechange-related threats can synergistically, interactively, and cumulatively elevate the risk of psychopathological outcomes from conception onwards. Importantly, these effects are not theoretical. They are already unfolding and pose a substantial threat to healthy human development on a global scale. The mental health implications of climate change-related events are not limited to immediate survivors. First responders, healthcare workers, and community leaders involved in disaster response and recovery efforts are also at risk of experiencing mental health challenges. The stress and emotional toll associated with providing support and witnessing the suffering of others can lead to burnout, compassion fatigue, and secondary traumatic stress.(50)
The main consequences of climate change and potential mental health effects are presented in Appendix 1.
Chapter 4: Healthcare Sector Contribution to
During the same period, Australia’s overall CO2e emissions amounted to 494,930 kilotonnes.
Therefore, healthcare accounted for 35,772 kilotonnes, constituting 7% of the total 494,930 kilotonnes of CO2e emissions in the country during 2014–15.
The environmental impact of the healthcare sector extends across various facets, including energy-intensive medical facilities, pharmaceutical production processes, and the disposal of medical waste. From the construction and maintenance of healthcare infrastructure to the energy consumption required for medical equipment and the carbon footprint associated with emergency services and pharmaceutical manufacturing, the sector inadvertently amplifies its environmental footprint. This phenomenon creates a self-perpetuating cycle wherein the healthcare sector, while striving to alleviate health issues, inadvertently exacerbates environmental challenges.
On a global scale, healthcare contributes approximately 4.4% to net emissions, a figure comparable to the annual emissions output of over 500 coal-fired power plants. To put it in perspective, if the global healthcare sector were considered a nation, it would stand as the fifth-largest emitter of greenhouse gases (59). In Australia, the healthcare sector’s contribution to climate change is substantial, with approximately seven percent of the national carbon footprint attributed to this sector.(60)
This emphasises the urgent need for the healthcare industry to take proactive and comprehensive actions towards sustainability to minimise its impact on the Earth’s environment.
One of the key contributors to the healthcare sector’s carbon footprint is the generation of greenhouse gas emissions. Australia’s healthcare system predominantly relies on coal-generated power. Healthcare facilities, such as hospitals, consume significant amounts of energy for heating, cooling, lighting, and medical equipment, which often rely on fossil fuel-based sources.
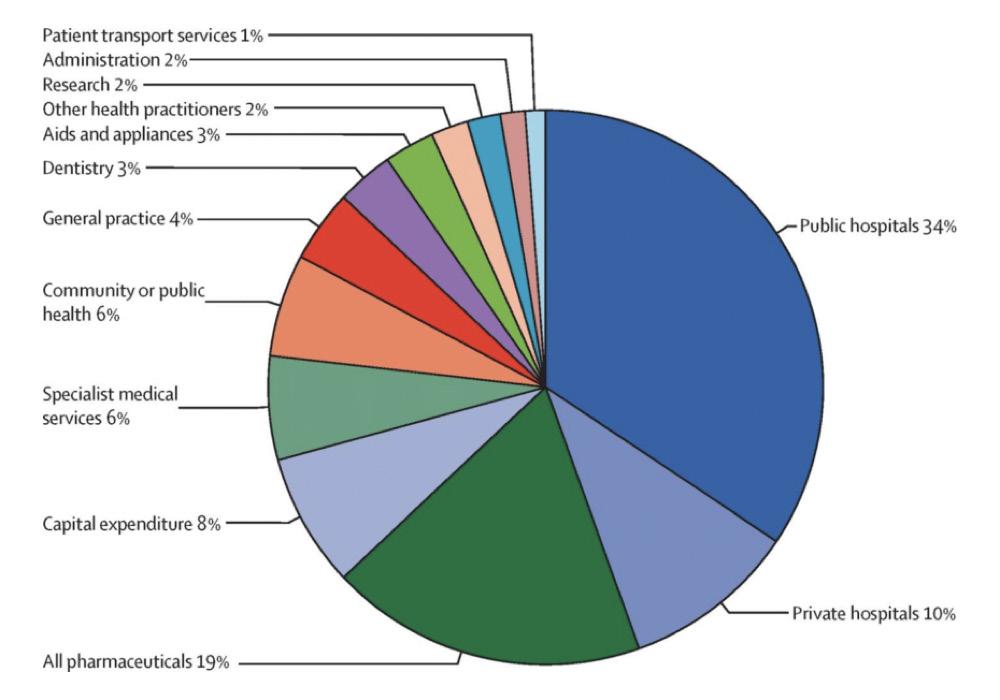
This constitutes approximately 7% of the country’s overall carbon footprint. To put this into perspective, it equals the carbon footprint of South Australia. Within this sector, hospitals and health services emerge as the largest consumers of electricity within a state or territory, contributing to 44% of the sector’s national emissions.
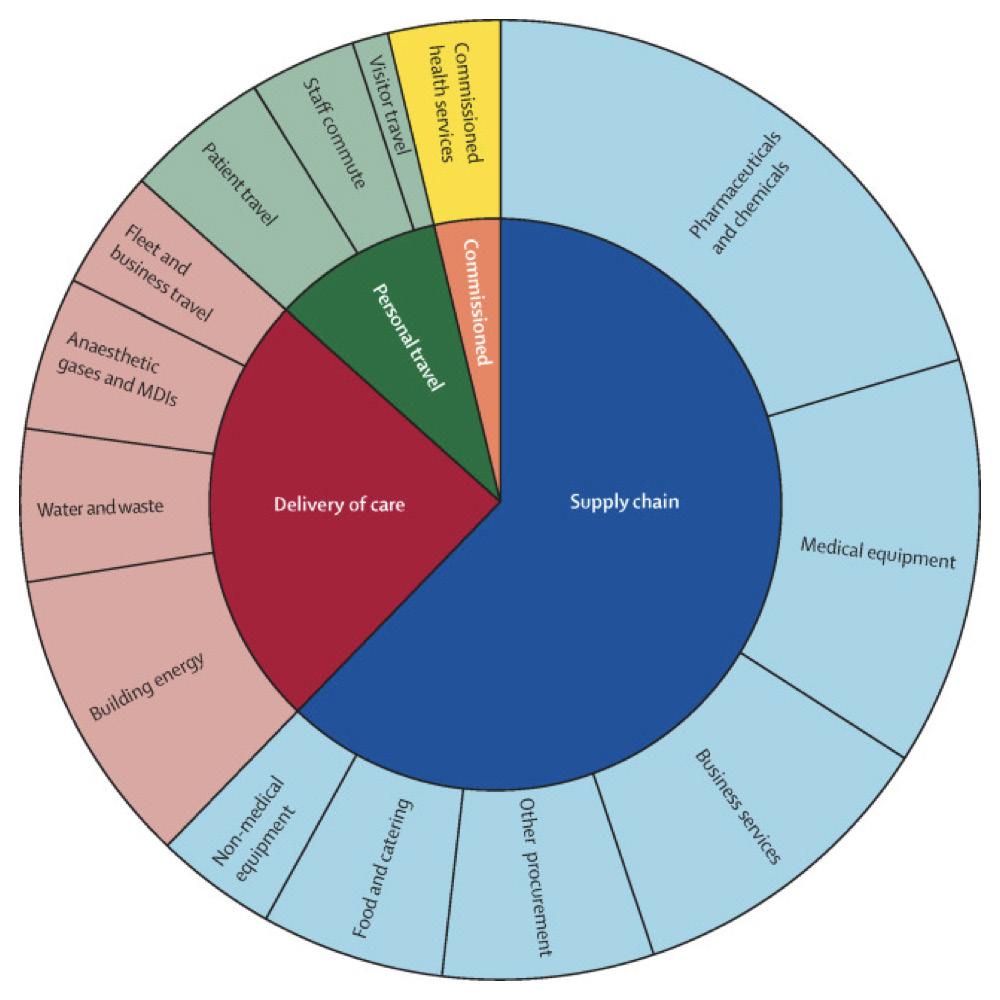
Total and Relative Co2e Emissions for Thirteen Health-Care Expenditure Categories
Source: Bolton A. From health sector waste minimisation towards a circular economy
Pharmaceuticals make up 18% of the emissions, while other sources, including specialist and General Practice (GP) services, contribute 10%, followed by capital works at 8%.
These energy-intensive operations contribute to the release of carbon dioxide and other greenhouse gases into the atmosphere.(85, 61) Additionally, the healthcare sector produces substantial amounts of waste, including hazardous materials, pharmaceuticals, and medical supplies. Improper management of healthcare waste can lead to the release of toxic substances and pollutants into the environment, further contributing to environmental degradation.(62)
In confronting these challenges, it becomes necessary for healthcare entities to accept sustainable strategies aimed at mitigating their ecological footprint. Such initiatives encompass the incorporation of energyefficient technologies, the streamlining of waste management systems, active promotion of recycling and reuse programs, and the incorporation of sustainable procurement practices.
The potential benefits of green infrastructure in healthcare facilities, like the integration of green spaces, not only contribute to environmental sustainability but also enhance patient wellbeing and recovery outcomes (63). Recent studies also highlight the importance of incorporating renewable energy sources, such as solar and wind power, into healthcare facilities to further reduce their environmental impact and enhance overall sustainability.(64)
Healthcare professionals play a crucial role in advocating for and implementing sustainable healthcare practices, through raising awareness among staff and patients, promoting environmentally friendly practices, and integrating sustainability principles into healthcare policies and guidelines.
This approach can assist the sector in reducing its carbon footprint and contribute to a healthier environment.
In Australia and New Zealand, the Australian and AoNZ (Aotearoa New Zealand) region of the Global Green and Healthy Hospitals (GGHH) network boasts active participation from over 200 health systems, health networks, and individual hospitals, collectively representing approximately 1,700 facilities and services.
This collaborative effort signifies a robust commitment within the healthcare sector to address environmental challenges and promote sustainable practices.
Upon joining the GGHH network, these healthcare institutions voluntarily pledge to reduce their carbon footprint and enhance environmental sustainability. The focus is not solely on environmental aspects but also extends to fostering public health. To achieve these objectives, participating entities commit to working on a minimum of two out of the ten sustainability goals outlined by GGHH.
These goals contain a wide spectrum, including energy efficiency, waste reduction and management, water conservation, sustainable building practices, transportation, food sustainability, pharmaceutical usage, chemical management, responsible procurement, and leadership initiatives.
Source: Singh H, Eckelman M, Berwick DM, Sherman JD. Mandatory reporting of emissions to achieve net-zero health care New England Journal of Medicine. 2022 Dec 29;387(26):2469-76.
Major Greenhouse Gas Emissions