2024 CAA Awards for Excellence
Highlighting innovation in our industry
To stay up to date with information on upcoming CAA activities please visit…


To stay up to date with information on upcoming CAA activities please visit…

The Council of Ambulance Authorities (CAA) is thrilled to announce and recognise the entrants in the 2024 Awards for Excellence, showcasing outstanding achievements and innovations across ambulance services in Australasia. This year, we received an impressive array of over 50 submissions, demonstrating the remarkable dedication and ingenuity of ambulance professionals throughout our region.
The 17th annual CAA Awards for Excellence attracted entries covering a wide range of topics within the judging categories, reflecting the diverse and dynamic nature of our industry. From clinical practice and patient care to leadership and technological advancements, the submissions highlighted the continuous efforts to improve and innovate within the ambulance sector.
We are incredibly proud of and grateful to all those who took the time to submit their projects and initiatives. The high quality of entries made the selection process challenging for our esteemed panel of judges, who had the difficult task of narrowing down the finalists from such a competitive field.
We extend our heartfelt thanks to our independent panel of industry experts who served as judges for this year's awards. Their expertise and dedication in evaluating the submissions have been invaluable in maintaining the high standards of the CAA Awards for Excellence.
The CAA Awards for Excellence not only recognise outstanding achievements but also serve as a platform for sharing best practices and inspiring further innovation across the ambulance sector. We are excited to celebrate these accomplishments and to showcase the remarkable work being done by ambulance professionals throughout Australasia.
Once again, congratulations and thank you to all of our entrants, and to everyone who has participated in the 2024 CAA Awards for Excellence. Your contributions continue to elevate the standards of the Australasian ambulance sector and improve the lives of the communities we serve.
David Waters Chief Executive, Council of Ambulance Authorities



Freddy Lippert MD
CEO, Copenhagen Emergency Medical Services
Associate Professor, University of Copenhagen, Denmark
Co-founder, Global Resuscitation Alliance, and the European EMS Leadership
Freddy is an Associate Professor and CEO of the Emergency Medical Services in Copenhagen, Denmark.
The EMS Copenhagen covers a population of 1.7 million, that is, one third of the Danish population.
The EMS Copenhagen includes the following: Emergency Medical Dispatch, ambulance services including physician manned mobile critical care units, psychiatric mobile unit, a medical hotline 24/7, responsibility and coordination of medical preparedness on behalf of all hospitals in the Capital Region.

Steve Irving
Executive Officer (retired), Association of Ambulance Chief Executives
Steve has recently retired after 40 years of ambulance service, initially working in London and more recently with the Association of Ambulance Chief Executives in the UK.
An extensive front line clinical career included secondments as both a HEMS and Motorcycle paramedic. Steve has been lucky enough to experience a variety of ambulance related roles and maintains an interest in various ambulance issues and the AACE’s Ambulance Leadership Forum (ALF) conference.

Neil Kirby
Previous CEO, Ambulance Tasmania
Industry Ambassador, Corvanta Neil has been involved within the ambulance sector since 1978. He played a significant role in the evolution of ambulance education in Queensland, introducing the Associate Diploma of Applied Science, the precursor to the modern-day Degree programs, and has a passion for rural and remote service, the subject of his Masters dissertation. He gained a NHMRC grant to undertake extensive research on the subject in Canada. He has served as Deputy Commissioner for QAS, Director of Operations for the Dubai Ambulance in UAE for eight years, and Chief Executive of Ambulance Tasmania. He was a founding member of the International Roundtable on Community Paramedicine (IRCP) and recently joined in the 20th anniversary of that gathering in Quebec Canada. His passion for ambulance continues as he consults with industry.

Tony Ahern
Board Member, St John WA
Board member, WA Primary Health Alliance
Tony Ahern joined St John Ambulance WA in 1973 as a 15-yearold cadet. In 1980 he moved from being a first aid volunteer to career ambulance officer.
In 1989 he moved into accounting and computing services taking a lead role in modernising St John’s administrative and financial systems while completing his Master of Business degree in Information Systems. In 1995, Tony was appointed to the position of Finance Director on the Executive, was made Deputy Chief Executive Officer in 2000 and Chief Executive Officer in 2006.
At a national level he chaired the Strategic Business Advisory Committee of the CAA for over a decade and was CAA Chairman from 2010 to 2013. Tony retired from the role of CEO at St John WA in 2018 and served on the St John WA Board from 2019 to 2023. Tony is a current Board member of the WA Primary Health Alliance.

Associate Professor
Belinda Flanagan (PhD)
Head of School, School of Paramedicine, University of Tasmania
Belinda is the Head of School at the University of Tasmania, leading the first School of Paramedicine in an Australian university. She has worked as a Paramedic & Registered Nurse/Midwife for 25 years.
Belinda collaborates with ambulance services in guideline development, education, research, and clinical governance.

Jennie Helmer
Chief Operations Officer, BC Emergency Health Services
Jennie has over 30 years of experience working in emergency health services. She has held various positions as an Advanced Care Paramedic, Research Lead, Director of Operations and is now the Executive Director of Emergency Dispatch, Clinical Operations for the British Columbia Emergency Health Services in Canada. Jennie has a Master’s in Education, a Master’s in Business Administration, and is currently enrolled in a PhD at the School of Population and Public Health at UBC.
Jennie is also a Sessional Instructor with the Justice Institute of BC Department of Paramedicine, and is a journal reviewer. With areas of interest in new models of outof hospital service delivery, and the use of innovative technologies to improve EMS dispatch and deployment, Jennie has over 15 peer reviewed academic publications.

Adjunct Professor Joe Acker
Adjunct Professor, University of Tasmania
Managing Director, Leader Tonic Solutions Inc
Joe Acker is a retired healthcare executive who served as Deputy Secretary of Health in Tasmania and Chief Executive of Ambulance Tasmania, where he led transformative healthcare and cultural reforms. His international career includes leadership roles in Canada with Alberta Health Services EMS and BC Emergency Health Services. Now based in Canada but maintaining strong ties to Australia, Joe leverages his international expertise as a leadership consultant and executive coach. He also holds an Adjunct Professorship at the University of Tasmania. Committed to global health improvement, Joe volunteers as Executive Director for EMS Global, a non-profit organisation focused on developing EMS capacity in low and middle-income countries, with current efforts concentrated in Mongolia.

Adjunct Professor
Vivienne Tippett
Director of Research, Queensland University of Technology’s School of Clinical Science
Adjunct Professor Vivienne Tippett has extensive experience as a researcher, author and consultant in health systems, with a special interest in emergency prehospital, disaster and emergency health systems. Her work has been recognised with an OAM for services to medical education (2018) and a Distinguished Service medal from Queensland Ambulance Service (2012) for services to paramedic research. Between 2013 and 2021 she was Lead Researcher for the Warnings and Communication Theme of the Bushfire and Natural Hazards CRC which was recognised with a CRC Association national award for research innovation (2019).
1 Chief Executive Letter
3 Judges
11 Excellence in Technology Entrants
Ambulance Victoria Introduction of the Patient Transport On-line Booking Form
Hato Hone St John EV Ambulance
NSW Ambulance Revolutionising Health Data With Innovative Dashboards
NSW Ambulance Hazardous Area Rescue Ambulance
SA Ambulance Service: Country Operations Interactive Map
St John WA
SJWA Ambulance Live
Dashboard: A Real Time Whole-of-Health-System Capability Which Builds in Innovations to Tackle Ramping
Finalists
Ambulance Victoria Video Assisted Secondary Triage
Ambulance Victoria Focus Analytical Dashboards
Ambulance Tasmania
ATOMS - Ambulance Tasmania
Online Medication System
23 Excellence in Clinical Practice Entrants
Ambulance Tasmania
My Emergency Doctor –In-field Referral
Ambulance Tasmania Safe for Waiting Room Referral Pathway
Ambulance Victoria Prehospital ECMO Program
NSW Ambulance
The Medication Safety Strategy (2024-2027)
Wellington Free Ambulance The Lloyd Morrison Foundation Heartbeat Programme
Finalists
Ambulance Victoria Blood Component Access Project
Hato Hone St John EMT Fentanyl Initiative
Queensland Ambulance Service Full Implementation of the Clinical Hub
35 Excellence in Staff Development Entrants
Ambulance Tasmania Wilderness Fit: Researching the Fitness of Wilderness Paramedics at Ambulance Tasmania
Ambulance Victoria Ambulance Victoria Shocktober Program 2023
Hato Hone St John International Recruitment
Hato Hone St John Peer Review and On Demand Learning
NSW Ambulance
Technical Solution for the New Ambulance Education Centre (AEC) Simulation Complex at the State Operations Centre
Wellington Free Ambulance The Focus of Pocus in Ambulance: the Development of Ultrasound Within an Ambulance Service
Finalists
Hato Hone St John Remote Triage
Queensland Ambulance Service Leadership Capability Development Framework
St John WA
Low Acuity Response Medic Pathway to Paramedic
47 Excellence in Patient Care
Entrants
SA Ambulance Service
Rural Emergency Responders
Network Transition Project
SA Ambulance Service
International Academies of Emergency Dispatch ACE Accreditation
Ambulance Tasmania
Ambulance Tasmania Critical Response Unit Project
Ambulance Victoria Partnering With the Victorian Virtual Emergency Department to Improve Access to Timely Emergency Care for Ambulance Patients, Using a Virtual Telehealth Service Delivery Model.
Ambulance Victoria
Pilot of New Operating Model for Complex Patient Ambulance Vehicle (CPAV)
Hato Hone St John Pre-Hospital, Pre-Antibiotic Blood Culture Collection in the Setting of Sepsis
Hato Hone St John Patient Experience Survey
Queensland Ambulance Service Implementation of the Adult Deterioration Score for Patients Waiting Offload at Hospital (QAS-QADDS)
Wellington Free Ambulance P neke Promise Initiative
Finalists
Ambulance Victoria A Strategy to Enhance Cardiac Arrest Survival After the Covid-19 Pandemic
Queensland Ambulance Service
The Queensland Ambulance Service Falls Co-Response Program
St John WA
State Obstetric Referral Call (STORC). Midwives Join Frontline Ambulance Crews to Improve Maternity Care for Women and Their Families
63 Excellence in Leadership
Entrants
Hato Hone St John Contemporary Rostering
NSW Ambulance
Clinical Practice – The NSW Ambulance Evidence to Decision (EtD) Framework Finalists
Ambulance Tasmania Working Flexibly at Ambulance Tasmania
Hato Hone St John Tactical Commander Training Framework
St John WA
Total Solar Eclipse 2023
71 Excellence in Mental Health and Wellbeing
Finalists
NSW Ambulance
Mental Health First Responder – A Real Time Virtual Mental Health Triage Service
SA Ambulance Service
Paramedic Telehealth Clinicians – Mental Health
St John WA
Inclusive Flexible Workplace Arrangements (FWA) to Support Work-Life Balance in Ambulance
76 Star Award



Recognising innovation or capability in the fields of equipment, communications, and information systems. When making their submission to this category, each service is encouraged to reflect on how their organisation has used technology in the past twelve months to enhance patient outcomes, staff performance or response capacity.

Team: Andrea Darke, Sarah Collins, Patrick Orr, Umair Jilani, Renjith Kanavila, Sandhal 'Sandy' Fernando, Mal Reid, David Shearer, Susanne Scott, Catherine Ho, Luke Williams, and Michelle Hemetsberger
The Patient Transport (PT) on-line booking form was introduced in March 2023, replacing the traditional fax machine at 000Victoria (000Vic) as the main mode of bookings for AV Patient Transport services.
A significant driver for the introduction of the on-line booking form was the need to uplift overall patient transport data and more specifically, to be able to ascertain requests for “booked” services that do not meet the criteria under the NEPT Regulations, essentially “ineligible transports”.
Currently NEPT demand has outstripped AV’s ability to supply with traditional PT road resources which has resulted in increased spillage to taxis, air resources and emergency ambulances as well as budgetary pressure.
Non-emergency patient transport (NEPT) in Victoria is for patients who require clinical monitoring or supervision during transport, but do not require a time critical ambulance response. Most NEPT transfers occur between hospitals, or between home and outpatient appointments. Some aged care patients may also be transported to and from specialist health appointments and rehabilitation. The majority of non-emergency patient transports are provided by road, with a small number undertaken by air services.

Non-emergency patient transports need to be authorised as clinically necessary by an appropriate health professional. Authorisation considers whether there is a demonstrated clinical need as prescribed in Victoria’s NEPT Regulations 2016. Further to this, the NEPT Regulations clearly state what constitutes a compliant transport from a low, medium, and high acuity perspective.
Due to the limitations with the fax booking process, AV had historically found it difficult to separate bookings that did not align to the above definitions.
The introduction of the on-line form has provided AV with a significant uplift in the quality of data and information pertaining to cohorts of patients that do not meet the criteria within the regulatory framework, allowing AV for the first time to isolate these bookings, understand the cohorts of patients identified as ineligible transports, and consider a future state of enforced compliance.
AV intends to commence using this information to optimise the use of its finite NEPT service by ensuring that PT resources are reserved for patients with the greatest need, by commencing the rejection of ineligible transports. It is expected that the removal of these cases will reduce strain on air and road resources, reduce reliance on taxis, while resetting the PT service delivery model by offsetting over three years in growth
Team: Dr. Colin Tan, Scott Morris, Sam Holloway, and Maggie Butler
This feasibility study (trial) aims to develop the first Electric Vehicle (EV) frontline emergency ambulance in Australasia, offering knowledge to the Prehospital sector and the environment. It seeks to gather information and feedback to understand the requirements and impacts of an EV ambulance, contributing to environmental sustainability efforts and demonstrating commitment to the Kaitiakitanga | Environment Sustainability Strategy. Key objectives include testing technology, understanding support networks and infrastructure requirements, assessing operational capabilities, evaluating financial implications, and reducing carbon emissions.
Initiated by Hato Hone St John, the trial aligns with our sustainability strategy, aiming to reduce fleet emissions and meet carbon reduction targets. With funding secured from ASB and support from partners like YHI and Action Manufacturing, the EV ambulance trial commenced in late 2022.
Following the waterfall methodology, the trial undertook requirements analysis, chassis selection, real-world observations, charging infrastructure assessment, human factors analysis, and vehicle design. Through a multidisciplinary approach involving stakeholders and specialists, the trial aimed to ensure that the EV ambulance meets operational needs, safety standards, and environmental objectives.
The trial is conducted in the Kirikiriroa/Hamilton region, with support from stakeholders and champions across various departments. Training sessions were conducted for staff to familiarise themselves with the new vehicle and its capabilities. Response parameters and procedures were established to optimise vehicle usage and ensure safety.
Initial findings indicate the suitability of the Ford EV Transit for ambulance use, with satisfactory range and safety features. Data collected during testing will inform future EV deployments and charging infrastructure planning. The trial aims to provide quantifiable and qualitative insights into energy consumption, driving patterns, maintenance needs, and patient experience.
The successful trial sets the stage for wider EV adoption in the ambulance sector, paving the way for greener and more efficient emergency services. Insights gained will inform future EV initiatives, infrastructure development, and collaboration opportunities with automakers and charging/energy companies. The trial also prompts exploration into other alternative fuel vehicles, ensuring continuous progress towards environmental sustainability goals.
This ambulance will add to, not replace our existing fleet, it is a catalyst for that change. By using the EV ambulance, we hope to advance our knowledge and the transformation needed in the ambulance system in Aotearoa for us to replace our fleet sensibly whilst still being able to respond to the people in Aotearoa.
NSW Ambulance
Team: Joshua Strong
In an ambitious endeavour to enhance operational efficiency and patient outcomes, NSW Ambulance’s Metropolitan Operations Team in Southwest Sydney Sector have developed a comprehensive series of reporting processes and operational dashboards using Power BI and the Microsoft 365 suite. This initiation represents a pivotal leap in harnessing real-time data analytics for decision-making, efficiency, accountability, and resource allocation.
By integrating sophisticated data visualisation techniques, these tools optimise operational capabilities, promoting clinical excellence, patient care outcomes, and team performance. The EMR audit process, a flagship among these innovations, exemplifies the project’s impact, streamlining audits and feedback through automated systems to significantly improve documentation accuracy and patient care quality.


Team: Ols Duerr-Reuther, Patrick Matthes, Mark Deeley, and Guiseppe Crisafi
With the increasing frequency, scale, severity and spread of extreme environmental conditions and in response to recommendations made by the Flood Inquiry, the Premier announced a major funding package to further the states flood rescue capability. This included funding for NSW Ambulance to design and build eight Hazardous Area Rescue Ambulances.
NSW Ambulance is the only statutory emergency service organisation with responsibility for the care, treatment and extrication of patients in NSW. Despite a number of four-wheel drive ambulances, during recent flood and bushfire events it was noted that NSW Ambulances capability to access, treat and extricate patients was limited. This resulted in delays to patient care causing clinicians to wait for changes to conditions or seek assistance from other agencies, to enable access and treatment.
In response to the announced funding, a working group was formed with members from relevant areas. They reviewed and defined the vehicle functionality and capability requirements, as well as reviewed safety and operational process flows, throughout various stages of the design and development process. This includes 2D and 3D computer designs, vehicle mock ups and final product testing. Feedback was incorporated, and the design was endorsed by the working group. This resulted in a quality final product that was delivered on time and within budget.
The Hazardous Area Rescue Ambulance has improved 4WD access capability, including the ability to cross water up to 1.2m deep. It is capable of transporting staff, patients and bystanders with five rear cabin seats as well as provide active treatment to the patient being transported on an electronic stretcher with in-built suspension. The vehicle has crew protection systems that enable it to withstand a burn over for about five minutes, ensuring staff and patients are kept safe. It has improved communication platform that provides intelligent connections using radio frequency, terrestrial and satellite technologies along with inter-agency communication systems.
Feedback from the working group has been extremely positive, including “it’s actually exceeded all of our expectations”. The eight Hazardous Area Rescue Ambulances will all be completed by June 2024 and strategically placed across New South Wales. This capability improvement will further enhance the service to the New South Wales community in times of need.

Team: Hayley Rogers
The SAAS Country Operations Map was developed as part of the Rural Health Workforce Strategy Country Extended Practice Project.
The map allows SAAS clinicians and support staff to explore Country Operations in a virtual interactive map via mobile, tablet, and desktop devices providing detail relating to station location, type of crewing model, vehicle type and clinical practice levels.
It also provides detail around helicopter flight times and landing sites as well as locations of Regional Emergency Responder Network Doctors.

Team: Mike Ayre, Dan Humble, Luke Carpenter, Riyaz Budhwani, and Adam Hardisty
St John WA (SJWA) is evolving patient care for the better with the launch of its Ambulance Live Dashboard, which communicates real time information on the location, allocation, and status of every ambulance crew and patient across the state to improve coordination, patient flow and situation awareness with hospitals, other Health Service Providers (HSPs) and external stakeholders.
The dashboard is a key enabler of a whole of system effort to tackle ramping and addresses the information deficits that have limited prior efforts by providing a single source of truth for frontline, management, and senior executive staff across SJWA, emergency departments, partner agencies, and the broader health system. It is a blueprint for complete transparency and visibility across the health system despite differing IT system platforms and/or processes.
Since the Ambulance Live Dashboard launched in June 2023 there has been a consistent downward trend in ramping from 5370 hours in June 2023 to 3250 hours in February 2024. February’s result was the lowest level of ramping since April 2021.
Fiona Stanley Hospital, which has one of the busiest Emergency Departments in WA, has more than halved ramping levels over the same period, with the dashboard credited with enabling a marked improvement in ED patient flow and transforming how the hospital plans for severe patient admissions and demand spikes.
The dashboard provides visibility of ED diversion initiates by flagging patients selected for an alternate triage pathway by SJWA’s secondary triage team (STT) and/or Department of Health’s Western Australia Virtual Emergency Department (WAVED) – who previously were invisible in the overall patient queue.
It also includes SJWA’s innovation of Early Warnings Scores (essentially a traffic light system for patient condition based on clinical observations) to create greater oversight of potential patient deterioration on the ramp.
SJWA’s launch of new crews, being Low Acuity Response (LAR) and Extended Care Paramedics (ECP), has been easily integrated, while high acuity single responders, like Clinical Support Paramedics (CSPs) and Critical Care Paramedics (CCPs), have been using crew’s mapped locations in real time to provide situational awareness and close gaps in coverage.
The dashboard first and foremost provides WA health decision makers shared oversight not seen across the health system and ambulance service before, which is revolutionising communication about real-time operational strains between SJWA, EDs, and HSPs. Those discussions and tactical decisions are now supported by evidence provided by the Ambulance Live Dashboard and its specific functionality and capabilities.
Ambulance Victoria
Team: Charlotte Flaus, Scott Clarke, Nicole Magnuson, Diana Zimmermann, and Gareth Becker
Ambulance Victoria’s (AV) Secondary Triage Service provides a safety net for low acuity Triple Zero (000) callers, through provision of secondary assessment with the aim of connecting patients to appropriate care. Traditionally, secondary triage is conducted via voice-only telephone call, however this does not always provide Triage Practitioners (TPs) with the optimal information for accurate patient assessment and appropriate allocation of resources. Additionally, several clinical assessment criteria under Ambulance Victoria’s Secondary Triage Assessment Clinical Practice Guideline that are required to determine priority ambulance responses are limited by not being able to visualise the patient and their environment.
There is emerging evidence about telehealth’s safety and resource cost-effectiveness. We aimed to evaluate if innovative technology, in the form of video assessment capability would enhance patient assessment, improve staff confidence, and reduce unnecessary use of emergency ambulance resources.
We performed a prospective study of video assisted triage for emergency ambulance callers presenting with non-urgent health concerns in Victoria, Australia who underwent secondary triage between 27 November 2023 and 21 February 2024. A total of six Triage Practitioners (TP) per day participated in the trial with a total of 1004 video calls made. The trial group worked within an eligibility, exclusion and pause criteria to support them to provide safe patient care. Descriptive statistics were used to compare video triage with voice-only triage by a TP on emergency ambulance dispatch. Follow-up with patients and TPs was conducted.
A total of 3,046 patients were included of which 1,004 (33%) patients progressed to assessment using video triage. The introduction of video assessment in ST has been overwhelmingly positive. VAT has demonstrated increased rates of safe and effective diversion away from an emergency ambulance response, increased utilisation of alternate service providers and at home self-care, improved TP confidence in decision-making and improved ability to establish rapport and provide reassurance to patients/callers.
Video triage will be incorporated as business as usual for low-acuity Triple Zero (000) callers who are referred to AV Secondary Triage Services from April 2024.

Team: Rachel Atkinson, Jack Stelling, Diana Madonko, Thanh Hong, and Emma Wang
Introducing AV’s new revolutionary suite of analytics dashboards - FOCUS, a game-changing toolset designed to empower data-driven decision-making and propel our organisation to new heights. This comprehensive suite combines cutting-edge technology with user-friendly interfaces, offering a dynamic and visual approach to interpreting complex datasets.
The primary goal of our new analytics dashboards is to provide actionable insights across various facets of Ambulance Victoria. From monitoring key performance indicators to tracking operational efficiency and understanding clinical cohorts, these dashboards serve as a centralized hub for next day data visualization.
In terms of user experience, the dashboards are designed with simplicity and intuitiveness in mind. The visual representation of data, through charts, graphs, and interactive elements, facilitates quick comprehension and decision-making. The customisation options allow users to tailor their dashboard views to focus on the metrics that matter most to them, promoting a personalised and efficient workflow.
Furthermore, our analytics suite fosters a culture of transparency and accountability. By providing access to next day data, managers at all levels can take ownership of their performance metrics and contribute actively to organisational goals. This transparency not only enhances communication within the organisation but also empowers employees with the information they need to make informed decisions.
As AV embarks on this data-driven journey, we anticipate a transformative impact on our organisational efficiency, agility, and overall success. The suite of analytics dashboards represents a commitment to innovation, enabling us to stay ahead of the curve in an ever-evolving health landscape. Through these tools, we aspire to unlock new possibilities, drive strategic growth, and position our organisation as a leader in leveraging data for success.
In conclusion, our new suite of analytics dashboards is more than a technological advancement; it is a catalyst for positive change, equipping our teams with the insights they need to thrive in today’s data-driven medical environment. Together, let’s embrace the power of data and chart a course towards a future defined by informed decisions and unparalleled success.

Ambulance Tasmania
Team: Michelle Izard, Hamish Crisp, and Alex de Vries
ATOMS (Ambulance Tasmania Online Medication System) is a new way of thinking about and documenting specified medications transactions for Ambulance Tasmania (AT) clinicians using a fully electronic, cloud-based system. Taking a fully stocked Specified Medication Kit (SMK) out of the medication safe and into our possession, and documenting every medication transaction electronically in ATOMS, saves time getting ready to respond at the commencement of shift, improves medication management compliance and reduces medication breakages as ampoules are securely stored within the SMK. Manually auditing paper medication registers has been time consuming and prone to transcription errors. AT has found that by ambulance crews electronically registering medication transactions within ATOMS, it has improved transparency, accountability, and legislative compliance (Poisons Regulations 2018) as well as identifying areas for continuous quality improvement and further education.
The implementation of ATOMS complements and completes the Medication Management infrastructure upgrades AT has undertaken, including electronic access control medication safes and Closed-Circuit Television (CCTV) recording of medication safe transactions across the state. The aim of the overall medication management project was to strengthen the chain of custody of medications, apply contemporary systems approaches to the quality use of medicines, as well as enhancing medication security, audit capacity and documentation efficiency via technology, which is where ATOMS has come to the fore.
Implementation of ATOMS has provided the following for AT:
• A fit for purpose solution for ensuring consistent medication register compliant with Poisons Regulations 2018;
• Improved medication reporting and auditing processes for specified medications, including for stocks kept in medication safes at each AT station location;
• Availability of real-time information of specified medication transactions state-wide;
• Significantly streamlined compulsory medication management; and
• More robust medication management practices to keep our people and patients safe.



Recognising innovation or capability in the fields of skills mix, pharmacology, and clinical intervention as they relate to patient treatments and outcomes. When making their submission to this category, each service is encouraged to reflect on how their organisation has excelled in clinical practice with breakthrough moments that saw cutting edge techniques implemented to revolutionise the world of paramedicine.

Team: Tim Makrides, Debra Salter, and Tim Schmidtke
This project involved the development of a statewide referral pathway to a virtual care service for paramedics across Ambulance Tasmania working in the field. Ambulance Tasmania had already utilised a private provider of virtual healthcare, My Emergency Doctor, as a referral pathway for its Secondary Triage and Community Paramedic roles, and after extensive use by these groups a decision was made to expand this referral pathway to all paramedics in the field.
This is a significant and innovative step forward to expand virtual health beyond point of Triple Zero call (as with most Secondary Triage services) and provide virtual health and point of care in the community. This project also assists Ambulance Tasmania work towards the integration of ‘right care, right time, right place’ across the organisation by managing patients who are safe to do so in the community and avoiding unnecessary transportation to healthcare facilities.


Team: Tim Schmidtke and Tim Makrides
The Safe for Waiting Room Referral Pathway is a new guideline that allows Ambulance Tasmania paramedics to transport suitable patients directly to the emergency department waiting room, allowing the patient to self-triage and assisting in maximising ambulance availability to the community.
The project involved the development of an initial set of clinical criteria and draft guideline. Extensive consultation was undertaken with relevant stakeholders including hospital emergency departments, clinical networks, and health leaders to both communicate the intention of this project and refine the clinical criteria. This consultation and development were undertaken rapidly, with the original conception of the project to full implementation across the state occurring in eight weeks.

Team: Assoc Prof David Anderson, Prof Steve Bernard, Matthew Thornton, Jenna Schwarz, Vanessa Cross, Steve Musgrave, Paul Low, Dr. Sarah Hopkins, Dr. Ziad Nehme, Dr. Sacha Richardson, Dr. Julia Coull, Assoc Prof Aidan Burrell, Dr. Josh Ihle, Prof Andrew Udy, Dr. Brooke Riley, and Jayne Sheldrake
Ambulance Victoria (AV), in collaboration with Alfred Heath, is trialling an Australian first clinical innovation in the form of prehospital Extracorporeal CPR (ECPR). This highly advanced clinical service is only available in a handful of cities worldwide and may dramatically impact survival in refractory Out of Hospital Cardiac Arrest (OHCA).
The treatment involves using a complex portable heart-lung machine, known as extra-corporeal membrane oxygenation (ECMO). The ECMO machine allows blood to be pumped outside the body, with an artificial lung removing carbon dioxide and sending oxygen-filled blood back to the body. ECMO is an advanced form of life support that is usually only offered in specialist hospitals.
The prehospital ECMO response car (ECMO-1) runs on Monday through to Thursday from 0900-1700hrs. This resource is designed to support the work of on-road emergency response personnel treating patients with refractory cardiac arrest with the aim of increasing cardiac arrest survival rates and improving neurological outcomes post cardiac arrest.
A group of ECMO specialists from The Alfred Hospital collaborated with Ambulance Victoria to conduct a feasibility study. This was intended to identify whether ECMO CPR (ECPR) could be provided in the pre-hospital setting and whether this could potentially improve cardiac arrest survival and improve neurological recovery if this therapy were deployed earlier in the patient journey. We are now building on the feasibility study work.
The service brings cutting-edge technology from the hospital to the scene. It gives patients lifesaving treatment faster – hopefully improving their chances of survival. Nineteen patients have received ECPR in the pre-hospital environment and transported from scene to The Alfred Hospital in Melbourne. Several of these patients have had excellent cardiac and neurological recoveries and have been discharged home to their families.

Team: Jessica Mehegan
The Medication Safety Strategy (2024-2027) has been developed to guide NSW Ambulance’s strategic vision for medication safety and quality improvements. The strategy provides key deliverables NSW Ambulance aims to achieve in establishing a safety culture and excellence in the provision of safe, effective, and sustainable medication management. This is the first strategy of its kind within NSW Ambulance and other ambulance jurisdictions. Delivery of the strategy objectives will optimise the safety and quality of patient care, enhance the management of medications, and support the safety and wellbeing of our workforce.
The Medication Safety Strategy outlines three key focus areas to provide clear objectives and actions to improve medication safety:
• Leadership, culture, and stakeholder engagement;
• Governance and quality management; and
• System capabilities, integration, and infrastructure.
These objectives and actions will enable organisationwide governance, leadership, and commitment to achieving a safety culture that promotes the safe and effective use of medicines. Everyone working in NSW Ambulance has a shared and individual responsibility to be accountable for ensuring clinical quality and safety, and this strategy provides the roadmap to achieving this.

As a healthcare service, we are all accountable for improving our clinical governance and a commitment to maturing our safety culture. Together, we can all learn from one another, continually adapting and improving medication safety practices and processes, as a priority, within the care we provide patients, the community and one another.
Development of the Medication Safety Strategy utilised improvement science methodology with a problem-solving approach lead by curiosity and learning and identifying core business needs and requirements in medication safety and management. Fostering a culture of continuous improvement and continually seeking feedback from clinicians was imperative throughout the process. Consulting and collaborating with all directorates at different levels kept the drive amongst internal stakeholders to continue to buy-in to the development of the strategy. This included organisational wide consultation, presentation to relevant committees and external consultation and formal feedback from the Clinical Excellence Commission (CEC). Different forums and platforms were used to engage and negotiate with stakeholders, to develop fit for purpose solutions that are operational as well as innovative.
The NSW Ambulance Medication Safety Strategy provides the guidance and direction for other ambulance jurisdictions towards accreditation against the National Safety and Quality Health Service (NSQHS) Standards to improve the safety and quality of medicines use within their services.
Team: Rachel Evans
Last year Wellington Free Ambulance (WFA) trained more than 7,000 people in lifesaving CPR skills and AED use through The Lloyd Morrison Foundation Heartbeat Programme. This programme is unique as it is designed to be as accessible as possible to empower people from any background or community to undertake training and potentially save a life. We deliver this training free of charge to remove any financial barriers to this hugely important community capability.
Heartbeat focuses solely on the practical technique and rationale behind CPR, how important it is to immediately seek help and access an AED to give the person suffering a sudden cardiac arrest the best chance of survival. The Out of Hospital Cardiac Arrest Registry 2022/23 shows the impact this training is having across the WFA region with the highest bystander CPR rate (78%) in five years. The training is delivered to people aged 5-105 and during the lifetime of the programme over 35,000 people have been trained and more than 520 AEDs installed across Greater Wellington and Wairarapa. One of the publicly accessible AEDs has been used five times in a two-year period, with three successful outcomes.
WFA works in partnership with a local philanthropist who shares our vision to have as many people as possible CPR trained and accessible AEDs across our region. The philanthropic donation provided through this cornerstone partnership fully funds all aspects of the programme and provides annual funding for one fully equipped frontline emergency ambulance. In 2023 due to the success and expansion of the programme, our partner Julie Nevett and the Lloyd Morrison Foundation extended the support to include the purchase of two dedicated Heartbeat hybrid vehicles. These vehicles are visible across our community to further increase the profile of Heartbeat and as hybrid vehicles they are contributing to reducing our environmental impact and sustainability goals.
As demand continues to grow for Heartbeat training the tutor team has grown. During 2023 students working towards their Degree in Paramedicine were offered the opportunity to work as Heartbeat tutors to support the delivery of courses and public events. The tutoring experience supports their clinical practice as well as their soft interpersonal skills, crucial to working with patients and families.
With the continued demand and impact of the LMF Heartbeat Programme, WFA, through the ongoing support of our philanthropic partner are deeply committed to the ongoing development and expansion of this lifesaving programme.
Team: Assoc Prof Ben Meadley ASM, Andrew Allan ESM, and Rae French
Ambulance Victoria (AV) helicopters carry four units of red blood cells (RBC), however weather and resourcing limitations may affect the ability to deliver RBC.
Widespread carriage by intensive care paramedics on ground-based resources has several limitations. Until recently, if a helicopter was unavailable to respond to a critically unwell patient in rural areas, paramedics could request blood components from a local health service. In the metropolitan area, inconsistent availability of aeromedical teams via road platforms provided variable availability of blood components for trapped major trauma patients. These informal processes resulted in unclear clinical guidance, wastage, lack of governance, and health and aeromedical services being caught offguard regarding inventory management. To rectify this, the AV Operational Improvement team collaborated with key stakeholders to standardise and improve processes to enable blood component access for critically unwell patients in the field.
Using contemporary improvement science, educational and project management principles, the project team worked with transfusion scientists, hospitals, chief medical officers, paramedics, educators and audit and governance specialists to develop learning packages and systematic workflows to ensure patient-safe practice, and protection of the precious and life-saving resource that donated human blood is.

Two separate education packages were developed. irstly, all intensive care paramedics were required to complete the BloodSafe Transfusion Practice Module, already available to in-hospital clinicians and aeromedical teams. Secondly, the project team created a bespoke blood management resource tailored to the out-of-hospital environment, aligned with AV clinical practice guidelines and logistical arrangements.
For the operational blood component access workflows, new processes were designed to be user-friendly, and enhanced to be compliant with the National Safety and Quality Health Standards (NSQHS) Blood Management Standard.1 For incidents in rural areas, ad-hoc requests were replaced by formal consultation with aeromedical and retrieval service coordination staff. A flight coordinator or physician assesses each case and determines the most suitable health service to request supply of blood components, cross-referencing the statewide blood component inventory database and organising delivery to a scene when a helicopter is not available. Additionally, a new process was developed to enable aeromedical teams to respond consistently via road in the metropolitan area.
After successful implementation, the project team continues to apply contemporary improvement science principles to ensure that the processes evolve as required. The team has worked hard to ensure this precious resource is reserved and available for our most critical patients, health service stock is preserved, and product wastage is avoided.
Team: Nicole Jones and Robbie Blankenstein
Hato Hone St John (HHStJ), along with many other ambulance providers, face geographic and resource challenges when delivering an equitable emergency ambulance service (EAS). Patients in rural/remote areas, many of whom are M ori, receive less analgesia compared to urban patients, due to a higher proportion of vehicles being staffed by Emergency Medical Technicians (EMTs) and lack of access to Paramedic backup.
Investigation into the viability and feasibility of several options to improve access to analgesia was undertaken by HHStJ. This resulted in implementation of a trial where EMTs on selected rural and remote stations were authorised to carry and administer intramuscular (IM) and intranasal (IN) fentanyl under direction from registered paramedics in the Ambulance Communications Centre (Clinical Desk).
Overall, both quantitative and qualitative data collected from the trial demonstrated that EMTs could safely administer fentanyl under guidance from the Clinical Desk, with a clinically significant improvement in pain score. This provided a foundation for the implementation of a national EMT fentanyl initiative, which included:
• Development of a comprehensive education package and assessment criteria;
• Ensuring adherence to organisational medicine management policy and processes; and
• Creation of robust reporting methods, feedback mechanisms, and sustainability monitoring processes.
Following the devastating effects of Cyclone Gabrielle on the East Coast of the North Island in February 2023, several areas of the region became inaccessible by road. This resulted in fast-tracking the EMT Fentanyl Initiative in two stations, Wairoa and Ruatoria, beginning in April 2023. Between September and December 2023, the initiative was implemented on another 21 stations across Aotearoa New Zealand.
The EMT Fentanyl Initiative is another step towards providing a more equitable level of service, particularly in areas of low workload where paramedics are not employed.
Team: Claire Bertenshaw, Samantha Herring, and Alex Thompson
The Queensland Ambulance Service (QAS) Clinical Hub is a multidisciplinary health unit initially established in 2019 during the COVID-19 pandemic to address increasing demand and mitigate patient safety risks. Since this time, the Clinical Hub has evolved to provide 24 hour-a-day state-wide secondary triage, risk mitigation, early clinical advice, alternate pathway, and health navigation for up to 1200 patients per-day at the point of the Triple Zero (000) call.
The Clinical Hub is now home to a multidisciplinary team of Paramedics, Doctors, Registered Nurses, Mental Health Clinicians and Social Workers who provide support to health consumers who can be safely navigated and supported into equivalent healthcare pathways in the community, including in-home care, outreach services and virtual care. The Clinical Hub is now at the stage of full implementation, with ongoing expansion of both the QAS workforce and the services provided to all Queenslanders Statewide.






Device Technologies proudly represents over 20 trusted brands in the pre-hospital sector with product solutions for defibrillation and monitoring, mechanical CPR, ventilation, airway management, vascular access and more.


• Customer focused education and technical services
• A comprehensive range of innovative products
• Digital services and telemedicine solutions
For more information contact your Device Technologies representative.


Recognising education improvement or innovation in the fields of: Programme design, delivery, assessment, and accreditation; professional development, skills maintenance, and practice standards, including community education; and research and/or innovation supporting evidence-based practice. When making their submission to this category, each service is challenged to explore areas where improvements have been made in staff development, and how these resonating changes have improved the evolution of paramedicine.
Team: Simon Harmsen, Jayson Turvey, and Corey Armstrong
Wilderness paramedics support complex patient search and rescue, treatment and recovery throughout Tasmania. Their role is both hazardous and demanding, often required them to trek for several hours or days to reach an injured patient in austere environments where conventional methods of access (i.e. road ambulance) is not possible. Additionally, wilderness paramedics train and respond in extreme weather conditions across Tasmania, including during blizzards and extreme weather events. Understanding the physical demands of the wilderness paramedic role and developing appropriate training and assessment methods to support future wilderness paramedic recruitment has been critically important.
In partnership with Ambulance Tasmania, the Tactical Research Unit (TRU) at Bond University has developed a PhD proposal to establish a scientific summation and evaluation of the findings of six cumulative studies and recommendations for physical fitness testing measures and frameworks for Ambulance Tasmania wilderness paramedics. The research will provide critical, evidence-based assessment frameworks for the recruitment and training of wilderness paramedics which will enable optimal task performance, mitigate injury risks and ensure the maintenance of health and wellbeing for individuals performing the task of wilderness paramedics.

Ambulance Victoria
Team: Joel Marley, Andrea Lenaghan, and Suzette Hafey
Shocktober is a month-long Ambulance Victoria (AV) community education and awareness campaign teaching cardiopulmonary resuscitation (CPR) and uplifting access to automated external defibrillators (AED) through delivery of AV’s ‘Call, Push, Shock’ program. Shocktober has been delivered annually since 2017 and is aligned with the global Restart a Heart Day (RAHD) campaign.
Shocktober engagement goals are to collaborate with our people and partners to:
• Improve knowledge of how to respond when someone is in cardiac arrest;
• Promote the three simple steps required to save a life: Call, Push, Shock;
• Increase the number of Victorians signed up as GoodSAM responders; and
• Register their local AED and make them publicly available 24/7.
The momentum of Shocktober continued in 2023, with 340 CPR sessions lead by paramedics across Victoria reaching 7,600+ community members delivering a 45% growth compared to 2022. In the period 2017-2023 AV has facilitated 575 Shocktober/ RAHD CPR and AED awareness sessions engaging 13,600+ people, and our cumulative digital reach is beyond 1.6 million. This growth underscores AV’s commitment to broadening its impact on CPR and AED community education and awareness.

As part of the 2023 Shocktober campaign, AV released its Cardiac Arrest Improvement Strategy (CAIS) 202328. The strategy aims to improve survival from out-ofhospital cardiac arrest (OHCA) and drive improvements in patient outcomes. The strategy was peer-reviewed by leading international experts to ensure alignment with the evidence-base and international best practice.
OHCA is a global health problem and a leading measure of quality for Ambulance Services globally.
In 2019, AV reported its highest ever survival rate for OHCA patients. The COVID-19 pandemic had a devastating impact on OHCA systems of care around the world, and ambulance services are developing strategic approaches to restore patient outcomes to pre-COVID levels.
“Enhance community-based participation in CPR and public access defibrillation” has been chosen as CAIS Strategic Priority One, recognising that the most important opportunity for driving significant improvement in OHCA outcomes occurs within the first few minutes of collapse.
Defibrillation by bystanders using an AED can halve the time to first AV defibrillation and has been associated with survival rates over 50%. Importantly, early defibrillation by bystanders is also associated with better long-term functional recovery outcomes.
Shocktober has the potential to become a national and international community education and awareness campaign – a month aimed at teaching CPR and uplifting access to AEDs, supporting the global Restart a Heart Day campaign held on 16 October annually.
Team: Rosanne Shaw, Robbie Blankenstein, and Melanie Johnson
“Paramedic Careers in New Zealand. Same purpose. New passion”.
What makes living and working in Aotearoa New Zealand so special is the focus of this ground-breaking digital campaign aimed at recruiting international paramedics. The innovative campaign – a first for Hato Hone St John (HHStJ) – was designed to help meet the increased need for paramedics throughout the motu. Hato Hone St John has a dedicated, highly skilled workforce of over 4,500 paid and volunteer ambulance officers. Given the size of the workforce and the fact that HHStJ is the largest employer of paramedics in Aotearoa, recruitment of experienced paramedics can be a challenge requiring an innovative talent attraction strategy which was developed specifically to attract internationally experienced paramedics to build an ongoing pipeline of candidates for the future.
The target audience was clearly defined as New Zealand, Australian or UK trained paramedics currently working as a paramedic on an emergency ambulance in Australia or the United Kingdom.
The highly successful campaign has seen unprecedented interest from international candidates, with over 5,500 candidate enquiries, and more than 100 paramedics from the UK and Australia hired over the last year. Hato Hone St John is already seeing the benefits of a boosted frontline team.
Team: Emily McCully
In Aotearoa New Zealand, EMS work under standing orders called the Clinical Procedures and Guidelines (CPGs). As part of independent practice working under CPGs there is a requirement for Clinical Peer Review. Clinical Peer Review is a process where patient care provided by Paramedic peers is reviewed to ensure adherence to CPGs and promote continuous improvement in clinical practice. Within Hato Hone St John around 5% of all patient care records undergo Clinical Peer Review by a group of 250 Peer Reviewers. Prior to September 2023 Clinical Peer Reviewers attended a live online training session with a Clinical Support Officer (CSO) to learn how to undertake Clinical Peer Review.
This process involved several hours of scheduled training sessions to support the availability of training around shiftwork. In September 2023, a new on-demand training tool was developed, and on-demand training went live on our online learning platform (MySitRep). This meant that instead of tailoring and scheduling live training, recruitment and training of Clinical Peer Reviewers could be continuous. This on-demand training now allows Paramedics to claim professional development hours for completing the training and for higher numbers of Clinical Peer Reviewers to be trained. A process that was time consuming for both the Clinical Support Officer and the trainee Clinical Peer Reviewers is now a streamlined, accessible, beneficial, and targetreaching system that is valuable and convenient.
NSW Ambulance
Team: Francisco Mota
Prior to the relocation of NSW Ambulance Education Centre (AEC) to Levels 1 and 2 at the State Operations Centre (SOC) facilities in Sydney Olympic Park, they operated one simulation room with an external camera at NSW Ambulance Headquarters in Rozelle.
Under the scope of the Relocation Program, a critical requirement was to increase educational simulation capabilities enabling the conduction of concurrent simulation sessions in a variety of settings, consisting of one enclosed area resembling a Studio apartment (lounge/bathroom and kitchen/living areas), two rooms that incorporates Virtual Reality technologies in the future, one wet lab where the use of various liquids is core component of the training experience, plus one control room that is equipped with three control desks.
Following the kick-off of the NSW Ambulance Strategic Workforce and Infrastructure Team (SWIFT) program - seeking an increase in the scale of operations and training needs – the southside of Level 2 was rearchitected to scope another three simulation spaces and a second wet lab, now totaling ten simulation rooms. Under the SWIFT works, the Skill Lab space on the northside of Level 2 was also repurposed to host an Ambulance Shell and this room was also incorporated to the Simulation Centre solution.
All rooms include a variety of wide angle and pantilt-zoom (PTZ) cameras, in-ceiling microphones for capturing audio and in-ceiling speakers for communicating to participants. The control desks have the equipment required for controllers to select devices (cameras, microphones, and speakers), listen/ communicate to participants, capture audio, select multiple video feeds, control audio visual inputs, record sessions, and playback feeds and/or broadcast content to classrooms or via Teams or Pexip.
Five of the ten rooms are also equipped with videoconferencing systems to facilitate debriefing, particularly for interaction with instructors and video playback to reflect on learning experiences for the next session.
During the conceptual design phase, the handling of inputs and outputs was revisited for enhanced flexibility to support concurrent operations: “any desk, any resources, any rooms” due to the future-state requirement for conducting concurrent simulations and broadcasts at any time. The new principle triggered the pursuit for an innovative and simple technical approach.
The implementation of simulation solutions for training healthcare professionals is not a new concept. The scale of the implementation at the SOC and the level of flexibility and versatility being fulfilled to turn it into a Simulation Complex make this solution unique across Emergency Services Organisations nationally.

Team: Hannah Latta and Dr. Andy Swain
The World Health Organization advises that access to diagnostic ultrasound equipment should be limited to individuals who have satisfactorily completed a suitable training course and exhibit proficiency in the use of focused ultrasound (Australasian Society for Ultrasound in Medicine, 2017).
The following proposed point-of-care ultrasound (POCUS) pathway for prehospital clinicians offers a comprehensive framework to enhance patient care through the timely establishment of more accurate diagnoses. By aligning with the Australasian Society for Ultrasound in Medicine (ASUM) and Australasian College of Emergency Medicine (ACEM) guidelines, this pathway ensures standardized education, training, and assessment, thereby promoting clinical proficiency amongst practitioners.
The emphasis on ongoing education, audit feedback, and maintenance of clinical skills reflects a commitment to continuous improvement and quality assurance. Furthermore, the consideration of costs, including potential discounts through partnerships, assists in the feasibility and sustainability of POCUS programs. Overall, this pathway not only addresses the critical need for standardized POCUS practices but also lays down the foundation for improved clinical outcomes and patient safety in prehospital settings.
Team: Johnny Mulheron, Jono Meadowcroft, Blair Andrews, Renee Yang, Jo Gallagher, Reuben Merrett, and Katie Carran
This Hato Hone St John (HHStJ) initiative develops the provision of Remote Triage (RT) which was initially created to increase telehealth capacity for the Covid19-Omicron surge in 2022. This initiative addresses the need for meaningful clinical engagement, particularly for personnel on alternate/light duties (for example, due to injury) or being stationed in low-utilisation areas.
Our objectives were clear: Integrate RT to offer clinically focused duties for personnel unable to work on the frontline, thereby maintaining their clinical skills and Authority to Practise (ATP). Additionally, extending Paramedic clinical skills to isolated provincial communities by stationing a Paramedic there which would not have been justified on community workload alone. This enables the provision of a Paramedic skill set into a low utilisation area, when coupled with the provision of RT by that practitioner. The community achieves a clinical skill set that would not normally be justified due to low community workload, and the clinician maintains currency due to the coupled provision of RT, improving overall Emergency Ambulance Service (EAS) delivery and staff work-life balance.
Significantly, HHStJ have expanded operational capacity by creating additional RT stations, anticipated to handle about 100 calls daily, which improves the safety of delayed ambulance jobs and contributes to reducing ambulance attendances. HHStJ have also commenced a qualitative evaluation feedback loop by developing mechanisms for direct staff feedback, ensuring the project’s continuous improvement and relevance.
Through RT, HHStJ has provided a work model enabling the delivery of Paramedicine via a contemporary virtual model, for alternative duties staff, and those in low utilisation stations. The dedication to this initiative reflects the broader commitment to healthcare excellence and the critical role our staff play in delivering quality daily outcomes.
RT is not just a response to operational challenges but a strategic investment in our staff’s future, ensuring they remain at the forefront of clinical practice and most importantly, ensuring their career has variety and is both fulfilling and enjoyable.
Team: David Lucas, Robert Stark, and Amanda Martin
The QAS Leadership Capability Development (LCD) framework is an all-inclusive framework that provides current and prospective leaders within QAS a clear pathway to map and develop the functional, technical, and leadership skills needed for their roles. Every supervisor level and role identified within the Queensland Ambulance certified agreement has a selfdirected, on-the-job learning guide, online development support modules and a series of sequential leadership development programs and extension modules to support the development journey for each role.
Underpinned by the 70/20/10 learning principle, where 70% of learning is gained from hands-on experience, the framework has been designed to provide clear, on-the-job guidance to all current and prospective supervisors on the functional, technical and leadership requirements of the role but delivered in a way that allows the learner to set their own pace and pathway.
The QAS Strategy 2022- 2027 identifies the critical need for sound leadership capability development, a dominant theme reflected in the Queensland Government Working for Queensland survey. Therefore, one of the fundamental principles employed in the development of the LCD framework was to ensure the framework reflected the needs of QAS. This resulted in intense collaboration across all levels of the organisation to ensure expectations, opinions, and ideas were captured, interrogated, and included as appropriate.
The first phase of the rollout of the framework saw the delivery of seven sequential leadership development programs and four additional elective modules, contextualised for QAS and delivered in partnership with Qld Health. These programs are delivered across the state to promote regional inclusion and practical accessibility.
The second phase was the release of the self-directed, on-the-job learning guides titled ’Business Essentials’. There is a specific learning guide for each supervisor role in QAS. These guides outline the functional requirements and how to develop them and are used to support the development of the functional knowledge and skills of the person undertaking that role.
The third phase, the online development modules, is nearing completion. These Business Essentials online support modules complement the learning guides in both core elements and role-specific modules.

This is a new and innovative concept offered within QAS. It has been built from the ground up to align with the QAS workforce plan 2023 - 2028, promote positive organisational change in the theme of leadership capability development, and create a positive workforce culture through staff engagement.
Team: Jo Ruck, Stephanie Greene, and Carole Donaldson
The St John WA (SJWA) Low Acuity Response (LAR) model represents a significant advancement in staff development because it tailors the progression from graduate paramedic (Medic) to emergency Ambulance Paramedic (AP1) with incremental and deliberate stages, which ensures supportive and safe clinical exposure while prioritising exceptional patient experience.
Clinical exposure for new graduates (Medics) through LAR’s service delivery includes:
• Royal Flying Doctor Service WA’s patient retrievals and interhospital transfers;
• Assessment and care of P3 patients;
• Assessment of appropriate and definitive care pathways; and
• Falls support.
Outside of Perth Metropolitan, LAR crews may be used to provide an emergency response as part of a multi-team approach and operate within the Medic authorised scope of practice.
An early pilot of LAR during the peak of COVID-19 quickly presented issues due to having stood up new graduates too quickly with not enough support. That model was quickly revised at the end of 2022 and a reformed LAR model for Medics transitioning to Paramedics launched at the start of 2023 and is still being trialled, with ongoing assessment and clinical input.
One key learning addressed in the current model was the bespoke in-house Clinical Education Program (CEP) designed to build resilience and support Medics as they commenced a paramedicine career. This program was developed by Strategic Projects Operations Manager
Stephanie Greene and LAR Manager Jo Ruck, with support from Head of Clinical Education Carole Donaldson and her team, to not only focus on clinical skill acquisition but also on the holistic wellbeing of paramedics. This innovative approach in emphasising resilience and support has ensured the growth of strong, skilled clinicians who can deliver high quality care now and into the future.
The program develops new graduates, particularly focusing on areas of patient communication and assessment, equipment familiarity, documentation, effective patient handover, and stress management.
Feedback from emergency paramedics and LAR participants has been overwhelmingly positive with a 94% satisfaction rating for its leadership model, with 88% of Medics successfully progressed to the Paramedic Internship before fully qualifying as AP1s.
By incorporating evidence-based practice set by National Safety and Quality Health Service (NSQHS) Standards into its core principles, the LAR model sets a new standard for clinician excellence since students are equipped with the most up-to-date knowledge and skills, which enhances the quality of care provided to patients. And responsible for returning about 50 hours emergency ambulance to the community.


Recognising patient experience, improvement, or innovation. When making their submission to this category, each service is emboldened to examine ways that their organisation has assisted specific patient cohorts where learnings were of benefit to the field of paramedicine.

Team: Simone O'Dea
The Rural Emergency Responders Network (RERN) Transition Project seamlessly transitioned the RERN Program in SA Ambulance Service (SAAS), enabling a more collaborative and streamlined emergency response for regional South Australian communities utilising regional GPs to supplement SAAS response capabilities.
The Rural Emergency Responders Network (RERN) program is unique to South Australia and was established in 2008 and was a framework for rural doctors to assist SA Ambulance Service (SAAS) in responding to out-of-hospital emergencies. Initially, doctors were locally recruited and managed through contractual agreements with their respective Local Health Networks (LHNs), while dispatch coordination was the responsibility of SAAS.
As circumstances evolved and the program grew this decentralised approach became increasingly challenging to oversee effectively. Consequently, issues such as inconsistency, limited training opportunities, and divergent clinical governance arrangements arose. In addition, a notable gap emerged between the management and clinical procedures of the LHNs and the SAAS dispatch protocols, leading to irregular RERN responses.
The coordination, primarily facilitated by regional health networks, contributed to a lack of influence by SAAS over dispatch and response processes. This evolving situation prompted the need for a more cohesive and streamlined approach to enhance the overall effectiveness of the RERN program.
The RERN Transition Project integrated the program completely into the statewide ambulance service and resulting in a cohesive and standard approach to dispatching resources to out-of-hospital emergencies as well as aligning the program with SAAS processes to ensure seamless integration for enhanced patient outcomes. Success is evident in streamlined resource allocation and logistical support, with SAAS providing RERN doctors standard emergency response kit, operational dispatch protocols, ongoing training and development opportunities and certainty in clinical governance and patient safety processes. This has enabled a more consistent patient handover, treatment and management while at scene between SAAS staff and RERN doctors.
A key factor in the successful integration of the program into SAAS was in its use of change management principles to navigate diverse stakeholder interests. Collaborating with Regional Doctors, Local Health Networks, Statewide services, regional hospitals, and clinical governance committees, the project achieved consensus for a smooth transition.
The RERN program is unique in Australia and the successful integration into SAAS has enabled the ambulance service to deliver exceptional care to critically unwell patients in regional and remote areas utilising the highly trained regional doctors. This program also plays a crucial role in supporting both volunteer and career ambulance staff.
Team: Kate Clarke
SA Ambulance Service has successfully continued to maintain Accredited Centre of Excellence (ACE) accreditation since 2015 for its Emergency Operations Centre (EOC). Accreditation means SAAS complies with a rigorous set of globally recognised best practices. The ACE accreditation is through the International Academies of Emergency Dispatch (IAED). SAAS continues to demonstrate an ongoing commitment to maintaining a nationally and internationally recognised level of service to the community of South Australia.
Team: Simone Haigh and Tim Schmidtke
Critical Response Units are staffed by specialist Intensive Care Paramedics with the aim to provide high quality care to complex and high acuity patients. Ambulance Tasmania has traditionally utilised Intensive Care Paramedic (ICPs) working on regular stretcher vehicles, however with growing demand on ambulance services and decreased Intensive Care Paramedic staffing, this traditional response model no longer provided optimal response.
The Southern Critical Response Unit has gone live on the 18th of March and will consist of dedicated ICPs as solo responders who are targeted towards high acuity and complex cases. In addition to this, existing Critical Response Units in the North West and North have now been included in a state-wide dispatch process to target these towards cases where they will add the most value.

Team: Nicole Magnuson, Amanda Thornton, Brad Gin, Darcy Johnson, Bernadette Miller, David Shearer, James Oswald, Emily Mahony, Susanne Scott, Diana Zimmermann, Dr. Ziad Nehme, Loren Sher, Suzie Miller, Richard Nasra, and Richard Penberthy
In response to increased Triple Zero (000) demand and hospital delays, Ambulance Victoria (AV) partnered with Northern Health to establish a Healthcare Professional (HCP) pathway to the Victorian Virtual Emergency Department (VVED). The service provides paramedics and patients with direct access to an ED physician or nurse practitioner, via real-time audio-visual consultation.
Utilising a video telehealth consultation service delivery model, the service aimed to provide low to medium acuity ambulance patients with timely access to emergency healthcare services who may not need to attend the emergency department (ED).
The HCP to VVED was implemented state-wide over several iterations between 7th October 2021 and 28th July 2022. An evaluation of the HCP model post-implementation showed that the VVED service contributed to significant improvement in AV operational performance. In particular, the VVED model was associated with a 18.4% relative increase in the proportion of emergency cases not transported, and a 9.4% improvement in Code 1 cases responded to within 15-minutes as ambulance resources spend less time delayed at hospital.
Ambulance patients who used the VVED service also reported a very positive experience, with 91% of survey respondents indicating that the VVED service met their needs and 87% who would recommend the service to their friends and family.
Given the tremendous success of the HCP VVED model, AV have embedded the service to operate as business-as-usual, with further expansion of the service in AV Secondary Triage in November 2023. Patients who contact Triple Zero (000) now have direct access to emergency healthcare services when receiving an emergency ambulance or at point-of-call prior to emergency ambulance dispatch.
Results to date show an 87% diversion rate from emergency ambulance dispatch through this additional pathway.

Team: Andrea Darke, Sarah Collins, Patrick Orr, Peter Collins, Brodie white, Emily Mahony, David Shearer, Susanne Scott, and Ross Salathiel
During 2022/23, the Operational Improvement team within AV undertook an all-inclusive review of The Complex Patient Transport Ambulance (CPAV) service which had not been holistically reviewed since inception.
In light of two CPAV related sentinel events, the objective of the review was to systematically evaluate all aspects of the operations and ensure that any findings and recommendations for improvement consider the impacts and consequences for policy, process, people, systems, and performance statewide.
The Review identified a complex and inefficient service delivery model which had eroded operational confidence and willingness to use the service. This was reflected in declining demand for use of the CPAV service, that was misaligned with operational expectations and obesity data.
With evidence of adverse outcomes for patients and staff, and limited confidence in the service delivery model, it was necessary to reconsider the CPAV service operating model and offer alternative options.
A pertinent issue driving the reduced confidence was the convoluted operating model - a hybrid arrangement consisting of four distinctly different models, resulting in confusion and uncertainty. Furthermore, the efficiency of the dispatch process was impacted by the differences across and within the staffing models with one model allowing for between 60 and 90 minutes to locate staff, followed by time to travel.
The delay in CPAV arriving resulted in many situations where crews felt compelled to take unsafe risks by attempting to extricate and transport complex patients.
As part of the overall Improvement Plan included within the Review, a proposal was endorsed to assess a 24/7 staffing model, as opposed to the on-call model, allowing for the opportunity to evaluate the benefits before making systemic change.
A trial of a 24/7 staffed model for provision of CPAV services within Gippsland commenced. The trial improved CPAV availability, responsiveness and safety for both patients and paramedics with the key successes being:
• CPAV utilisation increased from 39 cases to 106 cases, a growth of 167%;
• Prior to the trial, staff requests for the CPAV averaged 1.3 cases per month compared to six requests per month during the trial;
• The median activation time of the trial CPAV was 34 minutes shorter than the activation time for CPAV cases in Gippsland between 2018 and 2022 (three minutes vs. 37 minutes);

• During the trial, the CPAV roster was filled consistently and there were no unfilled shifts; and
• There were no patient safety events associated with the CPAV service during the trial.
Team: Nicole Jones
Blood cultures are used to aid in the diagnosis of patients with suspected sepsis, ideally collected prior to antibiotic therapy. Evidence suggests that early diagnosis and early administration of antibiotics, along with prompt identification of pathogens through analysis of blood cultures can reduce mortality and morbidity from sepsis.
Although current Clinical Practice Guidelines (CPGs) used by Hato Hone St John (HHStJ) contain a directive for ambulance personnel to collect blood cultures when there is a local protocol in place, due to previous fiscal challenges and variable local hospital engagement, there are no active protocols. Anecdotally, feedback has raised questions relating to the validity of ambulance personnel collecting blood cultures, particularly with aseptic technique and potential contamination through the collection process. In addition, lack of a clear and concise processes post collection, resulted in confusion and wastage through recollection of cultures in emergency departments.
In 2022, HHStJ was approached by Te Whatu Ora –Health New Zealand Waitaha Canterbury (HNZWC) to discuss the opportunity to run a feasibility study through a pilot, with laboratory support to determine the viability of ambulance personnel obtaining blood cultures, prior to antibiotic administration in the setting of sepsis.
Following HHStJ senior leadership approval, the Canterbury pre-hospital blood culture collection pilot was implemented and run from 21 October 2022 to 21 April 2023. Pilot results were collated and reviewed by:
• Te Whatu Ora – Health New Zealand Waitaha Canterbury;
• Canterbury Health Laboratories;
• Microbiology and Infection Management Services;
• Christchurch Hospital Emergency Medicine;
• Hato Hone St John Ambulance; and
• University of Otago.
The results, published in the March 2024 issue of the New Zealand Medical Journal found that HHStJ personnel were appropriately diagnosing sepsis and appropriately administering antibiotics. In addition, the pilot found that the contamination rates were not significantly higher than those expected in the emergency department setting. This informed a decision by HHStJ senior leadership to approve the national implementation of pre-hospital blood culture collection in the setting of sepsis by HHStJ personnel.
The collecting of blood cultures post and/or during antibiotic therapy is associated with a significant loss of pathogen detection. Supporting HHStJ personnel to collect blood cultures prior to antibiotic administration can improve the ability for accurate pathogen identification and subsequent initiation of targeted treatments.
Team: Jon Moores
Patient Experience and Artificial Intelligence
In 2023 Hato Hone St John (HHSJ) migrated its Patient Experience Survey to a new platform using artificial intelligence (AI) analysis tools. Working together with its partner Yabble, HHSJ redesigned its survey format to encourage open ended, qualitative responses to better capture patient experience. By relying on the patient’s own words, HHSJ has been better able to analyse and respond to issues and feedback.
HHSJ’s platform using Yabble’s suite of tools can analyse unstructured text data and identify themes, sub-themes and sentiments within patient experience responses allowing almost instant theme identification and reducing the need for manual qualitative analysis. The data set can be queried with open-ended questions and the AI tools provide reliable, detailed insights. This allows for the identification of patients’ primary concerns, areas for improvement and service successes.
This is the first application of artificial intelligence to patient experience data in the New Zealand ambulance sector.

Team: Claire Bertenshaw and Brendan Schultz
In February 2024, the Queensland Ambulance Service (QAS) implemented an adapted version of the Queensland Adult Deterioration Detection System (Q-ADDS) to assist ambulance clinicians in monitoring patients that are delayed offloading to hospital emergency departments.
Q-ADDS is a validated vital sign observation chart that is currently used by nurses and doctors in all hospitals in Queensland. Briefly, Q-ADDS assigns a numerical value to each of the patient’s vital signs, with these individual numbers then combined to calculate the patient’s total score. If this score reaches a predetermined threshold, the patient must be escalated for immediate review. The implementation of this adjunct is designed to identify clinical deterioration in patients that are awaiting offload and provide a clear escalation process for ambulance clinicians in instances that this occurs.
The use of Q-ADDS by ambulance clinicians was first successfully piloted at four hospitals and has since been implemented for use at all hospital facilities state-wide.
QAS is committed to continually improving patient safety and the introduction of this tool aligns with the Australia Commission on Safety and Quality in Health Care (NSQHS) national consensus statement on recognising and responding to acute deterioration.

The integration and collaboration with Queensland Health have been pivotal to the success of the project implementation. Clinical Excellence Queensland, Queensland Health Patient Safety Committee provided valuable support including facilitating an expert in human factors to review the form and providing constructive feedback about usability. Feedback was also provided by the paramedics who were using the form, and this was incorporated in the final version.
The implementation of QAS-QADDS has enhanced patient safety while waiting for offload at the hospital with improving the structure of the observation periods and enabling the Ambulance Clinicians and Queensland Health staff to speak the same language about patient condition, deterioration and required escalation in care. This enables the two interfacing organisations to clearly communicate for improved quality care and patient safety outcomes.
Team: Kate Worthington and Dan Ashcroft
The P neke Promise Initiative is a community driven partnership working towards making central Wellington safe, vibrant, and welcoming. The central city has a proud history as Wellington’s gathering place – the home of Te Aro P and has been developed into P neke’s leading hospitality and entertainment district. The precinct has a high concentration of retail, nightclubs and bars that bring our capital city to life day and night contributing to both the economy and vibrancy of our city. In recent years the perceptions of safety in the area have fallen driving initiatives for positive change.
The P neke Promise Initiative seeks to enhance patient experience through accessible paramedical care. P neke Promise is delivered through the collaborative approach of Wellington Free Ambulance (WFA) and NZ Police. It provides a joint patrol within Wellington that provides a solution to increased demand within Central Wellington, resulting in better patient outcomes through immediate and accessible assessment and care.


Team: Ziad Nehme, Belinda Delardes, KImberley Magain, Emily Nehme, and Nicola Reinders
Out-of-hospital cardiac arrest (OHCA) is a global health problem and a leading measure of quality for Ambulance Services around the world. The COVID-19 pandemic has had a devastating impact on OHCA systems-of-care globally, with estimates from Victoria indicating that as many as 200 excess deaths from OHCA were observed during the COVID-19 pandemic. Although the restoration of patient outcomes is a key priority for Ambulance Victoria, strategised and evidence-based approaches to improve survival are urgently needed.
In 2023, Ambulance Victoria developed an Australian-first, Cardiac Arrest Improvement Strategy 2023-2028 to tackle this significant unmet need. The aim of the Strategy was to determine priority areas and initiatives to drive improvements in patient care for OHCA over the next five years. The strategy is a culmination of international best practice, local input from subject matter experts, and over two-decades of evidence-based insights and learnings informed by the Victorian Ambulance Cardiac Arrest Registry. It has been shaped by the insights of over 100 senior leaders at Ambulance Victoria and reviewed by a panel of leading international experts to ensure alignment with international best practice.

The strategy recommends investment in 38 programs of work across four priority areas, including:
1. Community CPR and public access defibrillation:
- The strategy recommends investment in community education programs,
- Identifying barriers to the use of public access defibrillation, and
- Enhancing the use of GoodSAM;
2. Comprehensive system response: The strategy recommends an increase in first responder capacity, providing improved feedback and monitoring of call performance and examining the value of audio-visual connection to the scene;
3. High-performance CPR: The strategy recommends high-fidelity training for paramedics, feedback and debriefing, and education on end-of-life decision making; and
4. Culture of excellence: The strategy recommends enhanced monitoring of care and data analytics, local champions to promote training, and improved accountability for monitoring and review of care.
The strategy underpins an organisation-wide culture of excellence in OHCA care and sets an ambitious goal to achieve a 30% relative improvement in survival for OHCA by 2028. It has identified 25 measures of success to guide the monitoring and evaluation of the strategy over its implementation timeline and progress reporting will be embedded into the Victorian Ambulance Cardiac Arrest Registry Annual Reports, which are released to the public. The strategy now represents a contemporary, innovative and evidence-based model of improvement that can be adopted by Ambulance Services internationally.
Team: Sandra Garner, Scott Nash, and Kym Murphy
People who experience a fall requiring assistance are the most common call for service to the Queensland Ambulance Service (QAS). In 2020 and 2021, falls related incidents represented 8.7% of all incidents attended by QAS paramedics following a Triple Zero (000) call. Falls disproportionally affect those in the older adult population (aged 65 years and older). Across the Metro North and Metro South Health Regions, this cohort represents approximately 67% of the people who fall requiring the assistance of the QAS. With the Australian Bureau of Statistics projecting a 70% increase in older adults residing in the Metro North and Metro South catchments by 2036, demand for falls related incidents is expected to also increase.
The QAS Falls Co-Response (CoRe) Program is a Queensland Health funded pilot between the QAS and two metropolitan hospital districts, providing a tiered, multidisciplinary response to Triple Zero (000) calls where a patient’s condition relates to a fall. This is the first falls co response service to be provided by an ambulance service in Australia.
Each unit comprises a two-member crew consisting of a paramedic and allied health practitioner (occupational therapist or physiotherapist). These units provide an accelerated assessment, management and disposition planning service for falls incidents received via Triple Zero (000) to the QAS.
This initiative facilitates greater integration between the existing Queensland Health post fall follow-up and referral pathways, by providing on scene presence of an appropriately qualified allied health professional who can undertake a comprehensive assessment of the patient in their home environment to inform falls assessment and management plans in a timely manner.
Patients assessed by the QAS Falls CoRe Program are transported to a hospital Emergency Department (ED) significantly less frequently than those seen by standard acute paramedic crews (49% vs 77%), and response time is quicker (41 minutes vs 58 minutes).

Team: Melissa Gardiner
St John WA (SJWA) dual registered Paramedic and Midwife Melissa Gardiner is revolutionising emergency patient care in the field of Obstetrics thanks to an Australian-first initiative called the State Obstetrics Referral Call (STORC). STORC provides a 24-hour helpline service, staffed by six experienced midwives with extensive knowledge of the Clinical Practice Guidelines of the SJWA ambulance service. The STORC team provides real time infield expertise, support, and guidance to frontline crews. By employing midwives, SJWA can provide woman-centred care which enables and empowers all pre-hospital staff regardless of rank to manage complex and challenging obstetric cases. The initiative has been highly successful since its inception on Mother’s Day in 2023 and has saved lives on several occasions when assisting with un-planned out-of-hospital (UOOH) births.
Obstetrics is an area which is often neglected due to its esoteric nature. Maternity patients represent less than 1% of all ambulance cases and are often approached with apprehension by even the most experienced paramedics. Yet babies and their mothers’ lives are at stake given UOOH births have increased risks associated with newborn hypothermia, infection, neonatal withdrawal, and death. For every baby’s life saved there are multiple lives touched, not only within the family but also for the ambulance crews present. The STORC team give all onroad staff the confidence to provide safe and evidencebased care to all women throughout Western Australia thanks to Melissa’s expertise and passion in pre-hospital maternity care.
Melissa’s unique skill set has enabled her to develop STORC to support on-road staff having been a frontline paramedic across the metropolitan and regional communities at SJWA for 22 years. Melissa continues to improve Clinical Practical Guidelines that govern how women, and their newborns are cared for in the pre-hospital environment and holds instructional and educational roles in SJWA and Edith Cowan University. Her ECU Master’s project is to augment the feasibility of the STORC program and its development.
STORC, which has been rolled out for almost ten months and has ongoing support, has been recognised by the Western Australian Country Health Service (WACHS) for its contribution to improving outcomes for regional women after STORC responded to a case in November 2023. STORC has responded to 70 calls and assisted in the births of 22 babies, with positive outcomes for women, their babies, and the crews managing their care.

Provide your EMS team with faster, more accurate information using ProQA® emergency calltaking software. ProQA gives your calltakers a standardised, proven set of medical protocols to assess the situation and deliver key information to your EMS team. Your team needs accurate and pertinent information fast —ProQA delivers.
Learn how the most trusted solution worldwide for safety of your EMS team at prioritydispatch.net.

Recognising management practise and operational improvement and innovation in: Management culture, open communication, accountability, management development, professional standards, and diversity of workforce, and operational protocols and work practices relative to how service delivery is provided.
When making their submission to this category, each service is encouraged to analyse the programmes they have implemented that paves the way in leadership for future generations.
Team: Robbie Blankenstein, Stuart Cockburn, Andrew Everiss, Oliver Tyack, AJ Gabriel, and Steph Rushby
Roster patterns are a key element of the work experience of frontline staff in many industries.
Contemporary rostering has the ability to benefit staff, the organisation and ultimately the patients and communities we serve.
As a key element of our daily work experience changing rosters can be an involved process with multiple influences, often competing with each other. Hato Hone St John (HHStJ) has successfully introduced new rosters in two area of our service. In one case staff feedback indicated a ‘back to the drawing board’, approach which resulted in a win-win outcome, achieving Hato Hone’s objectives while also meeting the staff’s desire for what is a fundamental component of kamahi’s (staff’s) experience.
Team: Clare Beech
All healthcare decision-making is complex. Decisionmakers may not have clear criteria, may sometimes neglect important criteria, may give inappropriate importance to certain criteria, or may not use the best available evidence to inform their judgments. Structured and transparent systems for decision-making can help to ensure that all important criteria are considered and that the best available research evidence is used.
Explicit and transparent systems for decision making can help to ensure that all important criteria are considered and that decisions are informed by the best available research evidence. The purpose of Evidence to Decision (EtD) frameworks is to help people use evidence in a structured and transparent way to inform decisions in the context of clinical recommendations, coverage decisions,
The main purpose of EtD frameworks is to help panels use evidence in a systematic and transparent way to inform decisions. EtD frameworks support panels by informing panel members about the relative pros and cons of the interventions or options being considered; ensuring that panel members consider all the important factors (criteria) for making a decision; providing panel members with a concise summary of the best available evidence about each criterion to inform their judgments; helping panels structure and document discussion; and helping panels identify reasons for disagreements, making the process and the basis for decisions transparent.
In 2022 NSW Ambulance introduced an Evidence to Decision making framework to support high quality decision making in the Clinical Practice Committee (CPC). The CPC is the peak decision-making body on issues relating to clinical practice, procedures, medications, and clinical equipment. A small team led by the Director Medical Services developed, tested, and implemented the use of the EtD framework (based on the GRADE (Grading of Recommendations Assessment, Development and Evaluation) EtD to support decision clinical decision making at a system level.

Team: Jane Sweeney and Jordan Emery
At Ambulance Tasmania (AT), we recognise our people have a range of personal priorities, responsibilities and commitments at home and in their communities, which need to be balanced with their professional responsibilities. We know that our ability to attract, retain, engage and support our people is improved by enabling them to work in ways that better support achieving this balance. We acknowledge that providing and supporting flexibility enables the full inclusion of people in our workplaces that may otherwise experience disadvantage.
Working Flexibly at Ambulance Tasmania – Guide and Toolkits for Employees and Managers are our new resources to support our employees who make requests for flexibility in their working arrangements, as well as our managers who have responsibilities for considering and making decisions about these requests.
Included in the materials is an overarching Guide, and two supporting Toolkits, one for Managers and one for Employees. The materials introduce a set of Principles to guide how decisions are made about requests for flexibility. Employees are encouraged to carefully review and consider their requests for flexibility against each of these Principles and Managers are required to make decisions against these Principles.

The Principles are:
• Flexibility is for everyone, no matter the reason;
• Conversation about flexibility start from ‘if we can, we will’;
• Flexible work arrangements must be mutually beneficial, for the individual, for teams and for Ambulance Tasmania;
• Flexibility must be considered within the context of the position, the organisational purpose and supports our service to community; and
• Focus on outcomes.
The materials also provide clarification on the types of flexibility that may be available (depending on the role and context), under broad categories of when you work, where you work and how you work. It also recognises arrangements can be both formal and informal.
The Toolkit for Employees provide an overview of the process for making a flexible work arrangements request, including considering needs, identifying options, submitting the request, preparing for and having the conversation with your manager. The Toolkit for Managers includes information about designing roles for flexibility and managing flexible work arrangements in psychologically safe teams.
We thank our people who worked with us in the development of this work, with a particular thanks to Health and Community Services Union and our Women in Ambulance Advisory Committee.
Team: Chris Harrison, Doug Gallagher, and Karen Connolly
Aotearoa New Zealand is facing an exponentially increasing risk of catastrophic major incidents, particularly of seismic origin. The changing weather patterns associated with global warming have increased the frequency and significance of storms including cyclones with lethal effect. There is an increasing prevalence of terrorism, also, with the number of active armed offender incidents in recent years increasing.
Additionally, a recent re-structure added an extra tier of leadership to HHStJ with 98 new management positions. These positions were filled with people with a range of experience within and outside of HHStJ.
These combining factors dictated the need for training in the role of management at major incidents at the tactical level to improve our readiness, resilience, and response to the multitude of inevitable future major incidents.
A Tactical Commander Training Framework was created by a core group of subject matter experts (SME). The brief for the group was to develop and implement training to our 189 ambulance operations managers across twelve courses to prepare our Organisation for the inevitable future major incidents.
An online pre-requisite course was created with three modules delivered already, and another in development:
1. Ambulance Tactical Commander: Introduction;
2. Ambulance Tactical Commander: Response;
3. Ambulance Tactical Commander: Recovery; and
4. Ambulance Tactical Commander: General Operations.
Some of the key takeaways of this project are:
• Outcomes-focused major incident training for all ambulance operations managers;
• Pre and post course online learning packages that can be reflected upon and referenced at any time by ambulance operations managers;
• Increased manager confidence in managing incidents with improved incident responses as a result already;
• Improved interagency engagement and relationships allowing a more cohesive and structured multi-agency response; and
• Commitment to the ongoing development of HHStJ managers in key competencies.
Team: Joe Cuthbertson, Stacey Abbott, and Aja Styles
St John Western Australia (SJWA) was among a huge multiagency prepared response to a 1-in-100-year ‘Total Solar Eclipse’ (TSE), which NASA attended.
The best global vantage point for the TSE lasting 62 seconds at 11.29am on April 20, 2023 was in WA’s isolated coastal town of Exmouth, more than 1200 kilometres north of Perth and engulfed by 47,655-hectare Cape Range National Park, during the cyclone season.
About 35,000 campers, including overseas tourists, flooded into the area where town capabilities peaked at 10,000, with a less than 50-bed hospital, one airstrip and SJWA ambulance staffed by volunteers and one Community Paramedic (CP). While multiple events were planned around the eclipse, visibility over visitors remained a high risk. Mass sea rescues due to four international cruise ships docking offshore was also a potential factor, with COVID-19 still a concern.
Traditionally a mass casualty incident in a regional area meant mobilising metropolitan operational staff to take over from the local response in managing the crisis. This leads to a delay in support reaching the targeted areas and taking resources from other areas creates unplanned operational deficits and potential risks.
Instead, with the benefit of preparation time, an Emergency Management approach which utilised PPRR (Prevention, Preparedness, Response, and Recovery) to effectively and systematically address risks associated with mass gatherings.
This process was led by SJWA’s Emergency Management Unit (EMU) led by then-Head of Special Operations Dr. Joe Cuthbertson and Emergency Management Operations Manager Stacey Abbott who flipped the management model to build up and support local subcentre resilience, with Community Paramedic (CP) Kyle Thompson and volunteer subcentre chairpersons across Exmouth, Coral Bay, Carnarvon, and Onslow helping preparations for SJWA’s Total Solar Eclipse Response (TSER), while creating leadership opportunities for the broader workforce through an Expressions of Interest (EOI) Surge Workforce.
Volunteer teams were supported by a highly-skilled Surge Workforce, including ten paramedics and resources being deployed across the four subcentres to provide a 24/7 hybrid response, and underwent emergency incident management training to participate in a Department of Health (DOH) mass casualty exercise.
A key learning was that regional volunteers can be highly engaged alongside the paramedic workforce, with the opportunity to work in a hybrid model being vigorously embraced.
The result was a seamless operation with feedback across all stakeholders being positive to glowing and the model of equipping local subcentres for future disasters being considered for all future regional disaster planning.
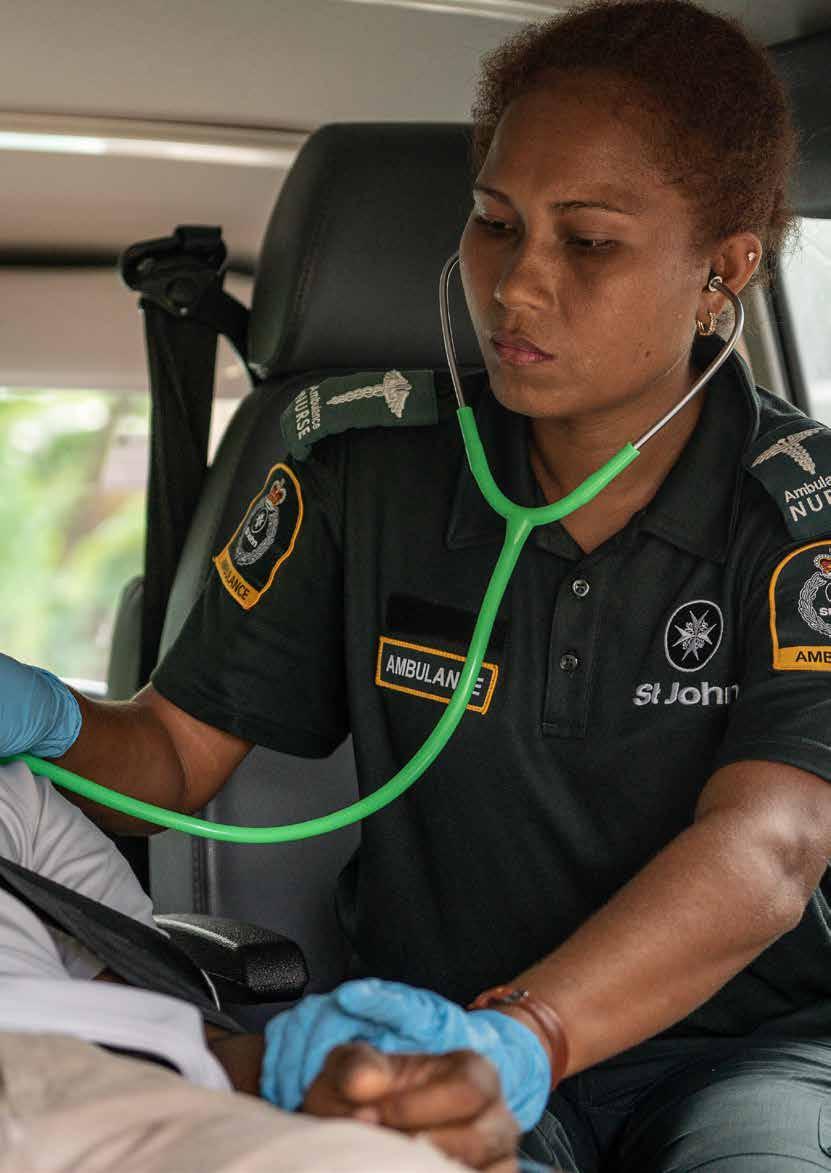

First introduced in 2021, this category recognises innovation and excellence a service has provided both staff and patients in improvements in mental health and wellbeing, including programmes, training and support. When making their submission to this category, each service is encouraged to share their undertakings in mental health and wellbeing for all stakeholders in the ambulance sector, including patients, staff, and leaders.
Team: Stephanie Looi, Luke Wiseman, Claire Walker, Jennifer Lavers, Mark Goodger, Liam McDermott, Drew Edwards, Aaron Casey, Philip Walker, and Robert Jones
Hunter New England Local Health District (HNELHD) is a large Local Health District (LHD), with a high demand for unplanned mental health services. HNE LHD, like other remote and rural regions are impacted by distance in being able to provide care to patients in a timely manner. Transporting people with mental health issues to Emergency Departments and/or declared mental health facilities can be time intensive, with many people not requiring inpatient admission and care for their health needs. The experience of care for patients can be traumatising, especially when it is necessary to enact powers under the NSW Mental Health Act (2007) No 8 for involuntary transport.
To address this need, the Mental Health First Responder (MHFR) project was developed – a real-time virtual mental health triage service for NSW Police and NSW Ambulance clinicians in the Hunter New England LHD.
The program is an innovative partnership between HNE LHD, NSW Ambulance and NSW Police, aiming to provide timely and equitable access to specialised mental health care for people with mental health concerns in contact with NSW Ambulance clinicians and NSW Police across the diverse regional, rural and remote communities within the district.

MHFR uses an Ipad and NSW Health custom-built web based videoconferencing platform to provide a mental health triage, linking patients that have contact with Police and Ambulance to mental health clinicians. It aims to provide an enhanced patient experience, improving health outcomes by offering alternative community care options that are timely and close to home.
MHFR provides individualised plans to meet the needs of consumers whilst supporting more efficient use of emergency resources, preventing unnecessary transport to and waits in Emergency Departments. MHFR uses existing Mental Health Line infrastructure to deliver fully integrated, responsive, cost-effective access to service on demand 24/7.
To date, MHFR results show over 85% of people able to remain safely at home with appropriate supports recommended to meet their needs. Each case would vhave resulted in on average a two hour round trip with average time spent in these EDs between six to seven hours.
“The person doing the triage treated the person in need with care and respect and gave him some great strategies and a plan to improve his social situation. The person in need was desperate for help when Paramedics arrived and after the triage he had a smile on his face and hope for the future.” - NSW Ambulance clinician
Team: Nicholas Mark, Rachel Peake, Linda Tame, and Joclyne
Zaitidis
SA Ambulance Service has established a small team of paramedics with additional mental health education, training and experience to improve the ambulance response to people who call Triple Zero (000) with a mental health crisis.
They are known as Paramedic Telehealth Clinicians – Mental Health (PTC-MH) and work in the SAAS Emergency Operations Centre to:
• Conduct mental health assessments by telephone
• Utilise mental health databases to understand the caller’s history;
• Contact their existing service providers to arrange care, where this is the most appropriate approach;
• Identify callers who require a more urgent response and ambulance dispatch; and
• Provide ambulance crews with additional patient information to enable informed and collaborative decision-making.
This service is providing:
• An assessment sooner than if the caller waited for an ambulance;
• Safeguards for high-risk callers by providing a faster ambulance response with face-to-face assessment; and
• Continuity of care and more individualised solutions by accessing callers’ health records and engaging directly with their existing service providers.
This service helps people avoid unwarranted emergency department presentations and ambulance transports which can increase mental distress for people in this situation.
It has also helped to increase SAAS referrals to mental health pathways, where previously many would have been taken to a hospital emergency department.
Importantly, it also supports the safety and clinical decision-making of SAAS crews by informing them about the consumer’s mental health history.
Innovative aspects of this service include:
• Using telephone assessment in the emergency mental health space, instead of emergency ambulance dispatch and face-to-face assessment;
• Utilising the Odyssey clinical telephone assessment platform for mental health consumers;
• Direct engagement between the SAAS EOC and mental health and other service providers, with direct referrals to these services; and
• Utilising paramedics with a mental health specialty and training in an exclusively mental health related telehealth role.
Team: Naomi Powell, Rebecca Boughton, Joel Moore, Julie Comito, and David Cutler
St John WA (SJWA) identified before the pandemic struck an issue within the workforce where ambulance team members were not provided a diversity of options for inclusiveness when returning from extended leave or enabling a transition to retirement.
Trends were noticed during exit interviews where clinical officers were departing due to long shift hours and SJWA’s lack of flexibility in meeting their needs. Those with family or caring commitments would often depart the organisation with an initial desire to return, however would gain employment elsewhere, breaking their career path and losing their clinical confidence. Experienced paramedics also lacked a pathway to slowly transition to retirement which caused disengagement and an increasing trend in time lost due to injury, with SJWA workers compensation claims rising by 10.1% in 2021 at a substantial cost to the organisation. A Safe Work Australia Return to Work Survey in 2021 found the associated cost of work-related injury or illness every year to the national economy was $61.8 billion.
Losing experienced officers impacts SJWA’s community response and the ability to provide skilled mentors for student paramedics and others within the organisation.
The need to smoothly transition returning officers back into the frontline workforce or those looking at retirement through flexible workplace arrangements (FWAs) was proposed in 2022, with a focus on ensuring officers were supported and engaged throughout the process. However, demands of COVID-19 stalled the project until 2023.
A business case for an 8-hour shift pattern, dedicated resources page and process review was approved in May 2023 and launched in June 2023. Employees who need to balance multiple commitments are now being supported to maintain their clinical competencies. Unlike previous part-time or job-share arrangements, extensive 13-hour rostered shifts failed to recognise external personal requirements, such as daycare, school hours, medical appointments etc.
SJWA is committed to supporting officer wellbeing though the use of alternate rostering options, which is not restricted to primary female carers and includes males who make up about a quarter of the program’s cohort. By being more inclusive, SJWA stands out from other ambulance jurisdictions and the feedback has been phenomenal. Seeking ongoing feedback enables continued refinements and improvement to the program, which has proven to this part-time cohort that they are heard, supported, and valued.
The organisation benefits from increased resources during peak times and retaining valued paramedics for the benefit of patients, colleagues and students, now and into the future.

Chosen from amongst each of the six category winners, the Star Award is the ultimate recognition of excellence in the ambulance sector. A Star Award winner is recognised as doing something uniquely innovative in the ambulance sector, ultimately leading to better patient outcomes.

With special thanks to our
Major Sponsor Excellence in Technology
Special Thanks to
Excellence in Clinical Practice

Excellence in Staff Development
Excellence in Patient Care

Excellence in Leadership
Excellence in Mental Health & Wellbeing


Olympic Park, Sydney, Australia
The CAA Women in Leadership Symposium is an empowering one-day event designed to foster and celebrate female leadership in the ambulance and pre-hospital sector.
This dynamic symposium aims to unlock the hidden potential of women currently in leadership roles or aspiring to take the next step in their careers.
Attendees can expect a rich program featuring:
- Practical skills development and tools for career advancement
- Inspiring talks from industry leaders and successful women in ambulance services
- Networking opportunities with like-minded professionals
- Announcement of the annual Women in Leadership Scholarship winner.
Full 2024 program plus tickets now on sale via caa.net.au/symposium Visit caa.net.au/symposium and subscribe to receive updates about the 2024 Women in Leadership Symposium and other news, offers and information from CAA.
To stay up to date with information on upcoming CAA activities please visit…