
Jordan Emery
Ambulance Tasmania Chief Executive, Jordan Emery, puts the love back into Leadership


Jordan Emery
Ambulance Tasmania Chief Executive, Jordan Emery, puts the love back into Leadership

For decades, the Sprinter has earned a reputation as a robust, versatile and capable work partner. Now, this renowned workhorse has been reborn with the launch of the new eSprinter Panel Van. For the first time, the Sprinter provides the opportunity to choose a vehicle powered by an all-electric drivetrain with high-voltage batteries up to 113 kWh in size. One of the world’s most versatile vans is now all-electric. Be among the first to register your interest to pre-order the eSprinter.
Register to pre-order.

Dear friends and colleagues,
Welcome to the Winter Issue of FIRST. As winter settles in, it’s an exciting time here at CAA because it’s Congress time. This event is our annual opportunity to gather, learn, and discuss the latest innovations and challenges in the ambulance sector.
Our cover story features an insightful interview with Jordan Emery, Chief Executive of Ambulance Tasmania. Jordan’s journey has been one of dedication, resilience, and continuous learning, shaping his unique leadership style which is deeply rooted in empathy and a genuine desire to make a positive impact. He emphasizes the importance of leading with love and compassion, particularly in the high-pressure environment of emergency services.
In this issue, we explore the potential of AI and emerging technologies in our sector through a selection of insightful articles, showcasing innovative advancements and their implications for improving healthcare delivery and efficiency. Our regular Wellness FIRST contributor Mitch Mullooly explores rebuilding paramedic resilience, while Jeanette Button from St John NT provides a compelling piece on working and living in beautiful Northern Territory.
This issue highlights local stories from across Australasia, including a feature on celebrating volunteers, the backbone of many of our services. Additionally, we cover the wonderful legacy gift to Wellington Free Ambulance, set to benefit the Wairarapa community for decades to come. And we report on an exciting new project by Hato Hone and ASB, delivering the very first electric ambulance in Australasia.
Our 2024 Congress in Melbourne promises to be another exciting event including speakers on leadership excellence, international collaboration, clinical excellence, disaster preparedness, and many networking opportunities, as well as celebrating our award winners at the CAA Awards for Excellence Gala Dinner.
Sit back, enjoy, and I look forward to seeing many of you at our 2024 CAA Congress in wintery Melbourne.
Love,

Mojca Bizjak-Mikic Editor-in-Chief FIRST magazine




Data First
2024 Workforce and Gender Report. 07 Industry First
Read the latest news from across the sector. 10 CAA First
Insights and relevant updates for the ambulance and emergency sector including CAA Board and comittee updates, 2024 Congress, 2024 Women in Leadership Scholarship, and Restart a Heart Day. 14 Focus First
Opinion First
The not so Challenging NT - a local's view on living and working in the northern capital.
30
Services First
Showcasing the latest projects and achievements from across CAA member services.
44
Healthcare's next frontier - how artificial intelligence (AI) is rapidly transforming emergency medical services. 26
Awards First
The 2024 CAA Awards for Excellence Gala Dinner will be held at the Melbourne Convention and Exhibition Centre on August 15th, 2024.
48 Feature First
FIRST speaks with CAA Board member and Chief Executive of Ambulance Tasmania, Jordan Emery about his perspective on leading with love.


58 Events First
A sneak peak into the highly anticipated 2024 CAA Congress.
60 Partners First
In this edition of FIRST we share articles from Australian Stroke Alliance, Paramedic Chiefs of Canada, and the Australasian College of Paramedicine.
74 Research First
Sharing the latest innovative research projects from around the ambulance world.
THE TEAM
Editor: Mojca Bizjak-Mikic
Relationship and Content Manager: Georgie Leach
Editorial Team: Georgie Leach & Kieren Vartuli
Publication Design: Kade Marsh, Alpha State
80 People First
Meet just some of the wonderful people that make up the Australasian Ambulance services.
82 The Directory
86 Wellness First
Rebuilding paramedic grit with Mitch Mullooly.
PUBLISHED BY:
The Council Of Ambulance Authorities
2/141 Sir Donald Bradman Drive Hilton SA 5033 Australia admin@caa.net.au

The CAA Workforce and Gender Report was created as an important tool to assist driving informed conversations and strategic initiatives aimed at promoting a more inclusive and equitable workforce for the Australasian ambulance sector.
Initially designed to capture and analyse the gender breakdown, it also provides a detailed analysis of employment types, age distribution, and attrition rates, offering essential insights into the workforce dynamics that shape the ambulance workforce today.
Over the past five years, female representation has steadily increased, reaching 53.5% in 2023. The report highlights major strides in gender equality across various roles and services, emphasising the importance of continued efforts to bridge existing gaps.
• See further breakdown of our workforce in the full report - caa.net.au/reports

The King's Birthday 2024 Honours List: Ambulance Service Medal (ASM)
The Ambulance Service Medal (ASM) recognises distinguished service by a member of an Australian Ambulance Service.
The CAA congratulates the following recipients who were recognised in The King's Birthday 2024 Honours List.
Australian Capital Territory
Joanne Louise Miles
Queensland
Christopher Robert Haswell
Rachel Veronica Latimer
South Australia
Anthony Cuzzocrea
Naomi Suzanne Stidiford
Tasmania
Laura Georgina Butler
Jordan David Emery
Western Australia
Brian David Gallop
Philip Mark Stanaitis


St John WA
St John Ambulances in the mid west of WA are now 5G compatible due to a $117,000 Ambulance Communications Upgrade Initiative. The partnership between Mitsui E&P (MEPAU) and Beach Energy has allowed 18 ambulances to be ahead of the curve, with the nation’s 5G network rollout not in the region. This upgrade will be highly beneficial for the continued success of SJWA after they responded to over 9,200 emergency ambulance calls last financial year.

St John WA
St John WA have held their first Recognition Awards for 2024, with over 180 operational team members getting recognised for their service. These Recognition Awards event is one of two team recognition events for SJWA with the second in October. Team members are eligible for an award through these categories: Paramedic graduates, 10-40 Year Service Award Recipient, National Medals to operational staff and First, Second and Third Clasp to National Medals. Congratulations to the team members who received an award.

May saw the opening of a new Mid North Coast Ambulance Station, with Lake Cathie Ambulance Station open for operation. This station is part of the Rural Ambulance Infrastructure Reconfiguration (RAIR) program. The $232 million dollar project is the largest investment into regional NSW Ambulance in their history. This new complex is complete with lodging facilities, parking for up to four ambulance vehicles as well as staff assembly areas.

Surf Lifesaving Australia have set out with a monumental goal of training High Performance CPR to 55,000 lifeguards over the next year. The group from SLSA who put forward this project has full support from Dr. Ned Douglas as well as the Chair of Lifesaving, Chris Jacobson. Accompanying this project is the inclusion of an operational training as well as a research arm for education going forward.

NSW Ambulance
National Reconciliation Week launched the NSW Ambulance Aboriginal Health Action Plan With not only the aim of closing the gap for Aboriginal people, NSW Ambulance endeavours to make sure that the systems and practices that take place are equitable and culturally safe. To see the entire Aboriginal Health Action Plan, scan the QR Code.

St John NT
After more than 18 months of discussion as well as negotiation with the Department of Health, St John NT received a fantastic $7.8-million dollar boost. With rising demand shown in the 2024 ROGS report, the funding boost is incredibly beneficial to operate across the geographically diverse state. Along with the growth in their patient numbers, over the last 5 years, the St John NT Emergency Communications Sector has also seen a huge 52% increase in Triple Zero (000) calls.

Hato Hone St John
Congratulations to Hato Hone St John for receiving their Toitu carbonreduce certificate for a second year. The Toitu carbonreduce certification, offered by Toitu Envirocare, is a program designed to help organizations measure, manage, and reduce their greenhouse gas emissions. By reaching this goal and receiving the recertificate, it showcases their “commitment to measuring greenhouse gas emissions in accordance with international standards”. In turn, this allows Hato Hone to St John to plan and execute against which aspects of their company is emitting the most.

SA Ambulance Service
SA Ambulance Services celebrated the opening of a new station located in Victor Harbour this June. This new facility will house Victor Harbour’s current 24 paramedics with the addition of another dozen in late 2024. Due to this new stations’ location, the team now can grow their ability to service the community across the popular region.


The team at The Council of Ambulance Authorities aims to provide insights and relevant updates for the ambulance and emergency sector. Within this issue, we provide information on relevant programs and events for 2024.
Halfway through the year, CAA marked another productive six months with all our committees, groups, and forums holding their first of two annual meetings. It is gratifying to support our services by facilitating opportunities to meet, exchange ideas, and discuss the sector's challenges and upcoming opportunities.
In May, we welcomed two new groupsAmbulance Sustainability Networking Group and The Diversity, Inclusion and Belonging Forum. CAA's new Sustainability Networking Group was created to bring together experts from our members who work in the sustainability space and is open to any member of our services, who are passionate about making ambulance services more sustainable. The Diversity, Inclusion, and Belonging Forum met in person in Sydney and began exploring various topics that will shape their work plan. These topics include addressing sexual harassment and promoting safe workplaces, sharing First Nations programs across Australia and New Zealand, investigating neurodiversity within our services, and highlighting the progress made by CAA in the Women in Ambulance and Leadership initiatives over the past six years.
CAA Group meetings continue to prove invaluable in fostering collaboration and innovation, ensuring that our services remain at the forefront of industry standards and practices. As we move into the second half of the year, we remain committed to driving positive change and supporting our community through continued engagement and proactive efforts.
CAA continues its vital work of aggregating service data to offer valuable insights and comparisons, helping us better understand the challenging times our services face. The Research and Data team has been particularly active, conducting CAA's annual Patient Experience Survey and finalising the 2023 Workforce and Gender Report. These efforts provide a comprehensive overview of patient satisfaction and workforce dynamics within the Australasian ambulance sectors.
Additionally, preparations for the 2023-24 data collections are well underway. These initiatives are crucial in guiding our strategies and ensuring that we meet the evolving needs of our services and communities effectively. Through the rigorous data collection and analysis efforts, CAA remains committed to supporting our services with the information necessary to drive positive change and improve outcomes across the board.


CAA Congress is Australasia's premier event for the Ambulance Health Sector. This year is set to be even bigger than previous years with more exhibitors, demonstrations, and delegates attending. The 2024 CAA Congress promises to be an exhilarating event for health professionals and partners within the ambulance healthcare sector. With the aim to bring top leaders, decision-makers and emergency management together, this years program is focused on areas that include leadership excellence, emergency management, sustainability in ambulance services and innovation and technology. CAA Congress also provides attendees with international perspectives as well as strong networking opportunities. CAA Congress will focus on critical issues that affect all levels of the ambulance health sector, which will provide a comprehensive overview of current challenges and future direction in the sector.
We are excited to recognise the entrants and finalists as well as announce the winners of the Awards for Excellence during our Gala Dinner. For more information regarding Congress, visit caacongress.net.au



Now in it’s third year, CAA are pleased to announce the continuation of the Women in Leadership Scholarship. CAA offers the Women in Leadership Scholarship to encourage more women to step into leadership roles, and to support the further development of current women leaders in ambulance health services. The Scholarship was formed through the CAA Women in Ambulance Forum, who sought to address the challenges and adversities for women in ambulance health services by encouraging leadership development and mentoring.
Applications closed on 15th July and the finalists will be announced via our CAA digital channels on 23rd September with the overall winner celebrated at the Women in Leadership Symposium in Sydney on 21st November. A huge thank you to our sponsors RAPP and Total Coaching Academy who provide the winner with a 12 month long leadership course and One Wild Coaching who also provide the runners up a 6 month leadership course. For more information, please visit caa.net.au
Restart a Heart Day is set for 16th October this year and is an initiative coordinated in Australia and New Zealand by the CAA to raise awareness and educate the community about CPR and AEDs. The day is centred around educating the public around how to perform CPR and use AEDs to save lives in emergency situations.
CAA and our member services will plan live events to recognise Restart a Heart Day on 16th October, as will our member services. To partner with, discuss Restart A Heart Day further or share news and survivor stories, please contact us at admin@caa.net.au or visit restartaheart.net
Artificial intelligence (AI) is rapidly transforming emergency medical services (EMS), ushering in a new era of enhanced efficiency and improved patient care in the ambulance sector. From AI-powered dispatch systems that optimise response times to advanced diagnostic tools that assist paramedics in the field, these emerging technologies are revolutionising how emergency medical care is delivered. By leveraging machine learning algorithms and real-time data analysis, AI is enabling faster and more accurate decision-making in critical situations.
One of the most promising applications of AI in ambulance services is in triage and diagnosis. AI algorithms can quickly assess patient data, including vital signs and symptoms, to provide paramedics with valuable insights for immediate assessment and intervention. Additionally, AIdriven predictive analytics are being used to optimise resource allocation, ensuring that ambulances are strategically positioned to respond to emergencies more efficiently. As these technologies continue to evolve, they hold the potential to significantly improve patient outcomes and streamline EMS operations, marking a new frontier in emergency medical care.
First Magazine spoke with Ole Paulsen Co-Founder from Sklls, and Simon Kos of Microsoft who are empowering emergency operators with generative AI. The team from Sklls help emergency operators and emergency preparedness teams perform with confident by training AI-based virtual callers. For readers, they have provided some insights to this rapidly changing and necessary technology.



Thehistory of medicine is marked by periods of steady progress punctuated by groundbreaking discoveries that propel the entire field forward.
Generative Artificial Intelligence (AI) promises to provide one of these revolutionary breakthroughs, offering clinicians two of the most powerful ingredients for healing –more time and better information. While past discoveries like penicillin saved millions of lives, generative AI's thousands of applications make it potentially the most innovative and effective tool yet.
Generative AI is a type of AI that uses sophisticated algorithms to provide insights, make predictions and generate new content, based on vast amounts of data. Unlike traditional AI, which relies on specific task-oriented programming, generative AI can understand and respond to natural language prompts, creating meaningful interactions and automating complex processes.
In health care, this means AI can assist with tasks such as drafting medical documentation, analysing patient data, expediting research and even simulating clinical scenarios for training purposes, all of which can significantly enhance the efficiency and effectiveness of healthcare delivery.
Through my journey in the health industry, I’ve witnessed the gradual impact of incremental technological advancements over decades.

Generative AI’s emergence from mid-20th-century machine learning to the sophisticated algorithms of today represents a steady march of progress. Now that we have robust digital infrastructure, accessible data and advanced computational capabilities, AI is set to transform healthcare systems.
AI’s potential on the front lines
Microsoft works closely with cutting-edge partners and leading health organisations globally, including ambulance services and first responders, to ensure the technology we develop is fit for purpose and helps make caring for people easier. Our vision is for technology to support professionals on the front lines who navigate the most challenging situations daily. By integrating advanced technologies like generative AI, we can help them provide better patient care and improve operational efficiency, ultimately transforming the healthcare landscape.
As generative AI continues to evolve, it remains in the early stages of adoption within the healthcare sector. This stage is characterised by cautious exploration, primarily focusing on low-risk applications such as administrative tasks, automated note-capture and business related tasks such as workflow optimisation and revenue cycle. These applications all have one thing in common: they save time for our health workforce so they can focus on patient care and service delivery.
Without comprehensive regulatory frameworks specifically for generative AI, healthcare providers must adopt a risk-adjusted approach to ensure safe and responsible use. Microsoft is playing a crucial role in this journey by supporting organisations with the tools and guidance they need to explore AI responsibly. And we’re seeing exciting applications emerge as our healthcare customers begin their generative AI journey.
For a start, large healthcare providers are using generative AI to improve efficiency, enhance patient care and foster innovation. For example, regional healthcare provider Grampians Health is deploying the technology for data classification and minute-taking in meetings, saving valuable time and allowing staff to focus more on patient care rather than administrative tasks. Quaternary hospital Austin Health is using machine learning for patient classification and natural language processing. This allows it to sift through extensive medical records, enhancing the clinician experience and streamlining search times.
At Monash Health, AI is facilitating more meaningful conversations with data to accelerate insights and improve patient outcomes. This organisation’s application of generative AI not only generates clinical summaries but also aids in research, driving innovation and elevating healthcare delivery.
A New Zealand–based company, Technion, initially used AI to count parasite eggs in livestock waste to combat drug resistance. Now, it’s applying its technology to human health. Leveraging Microsoft Cloud and Custom Vision AI, Technion is enabling remote analysis of microscope-based tests from regional clinics and hospitals, reducing geographical health inequities and ensuring patients receive timely diagnoses without the need to travel long distances.
Volpara, a New Zealand medical imaging specialist, is leading the way in breast imaging with innovative machine learning software that assists radiologists in identifying patients at higher risk of cancer due to dense breast tissue. Its technology can also screen for breast arterial calcification that indicate cardiovascular disease risk, thus helping to detect both cancer and heart disease in a single scan.
These early explorations into AI are paving the way for the healthcare industry to realise the full opportunity this new technology presents. According to a report by Microsoft and the Tech Council of Australia, generative AI could contribute between $5 billion and $13 billion annually to the healthcare sector by 2030. By reducing inefficiencies and enhancing productivity, generative AI holds the promise of not only better patient outcomes but also substantial economic benefits for the healthcare industry.
However, the power of AI must be tempered with responsibility. Microsoft’s guiding principles for AI in health care include fairness, reliability, safety, privacy, inclusiveness, transparency and accountability. As the technology evolves, these principles will need to be reassessed and upheld. It’s why we have invested significantly in privacy, security and ethical guardrails across our AI technologies. We also work with healthcare providers in our partner and customer network to maintain these standards in their organisations.
Looking ahead, I’m truly excited about the future of healthcare. As we embrace generative AI and new technologies, we stand on the brink of a new era. AI will continue to support healthcare professionals, allowing them to focus on empathy, patient relationships and accountable decision-making. This transformation will not only enhance practitioner workflows but also make health care more accessible and equitable.
With AI as our ally, we are poised to take a significant leap forward, revolutionising health care for the better.


Chief Medical Officer,























Transforming Emergency Call-Taker Training
When the stakes are life and death, emergency call centers need their operators to be at the top of their game. Enter a revolutionary new approach that's transforming how emergency call-takers prepare for their high-pressure roles.
Advanced AI powers the HiSklls simulator, creating high-fidelity, immersive scenarios that span a wide range of emergencies—think cardiac arrests, severe trauma, domestic violence, traffic accidents, and more.
Unlike traditional methods, this approach allows operators to practice repeatedly in a controlled environment, embedding critical skills to the point of subconscious mastery.

Lena Heimvik, Head of the Prehospital Clinic at Helse Stavanger, is witnessing the change firsthand.
"We've been using the HiSklls simulator for some time, and the improvement in our operators' skills is remarkable. They’re more confident and better prepared, which means they handle high-stress situations more effectively."
The beauty of this training lies in its continuous feedback system. Operators get to refine their techniques and build resilience by repeatedly handling diverse emergency scenarios.
Why does this work so well? Cognitive Load Theory (CLT) tells us that our working memory has limited capacity. By internalising essential skills, operators free up cognitive resources, making it easier to handle new and complex situations. Stress inoculation theory and experiential learning also play key roles by promoting controlled exposure to stress and learning through experience.

Ole Paulsen, founder of Sklls, elaborates, "What I have learnt in my 20+ years of simulator experience is that the high-density and continuous feedback loops in realistic simulation training build competence and mastery multiple times faster than traditional on-the-job training. In traditional settings, training is limited to what happens by chance, with no room for failure, immediate feedback, or repetitions."
Beyond technical skills, this training builds crucial emotional and psychological resilience.
For maximum effectiveness, training programs should include:
01 02 03 04
Intensive Initial Training:
Master fundamental skills and emergency protocols.
Progressive Scenario Complexity:
Start with simpler scenarios, increasing in complexity over time.
Regular Practice and Reinforcement:
Continuous low-dose/high-frequency training to prevent skill decay.
Realistic Simulations:
Use advanced tools to provide lifelike scenarios, preparing operators for the unpredictable nature of actual emergency calls.
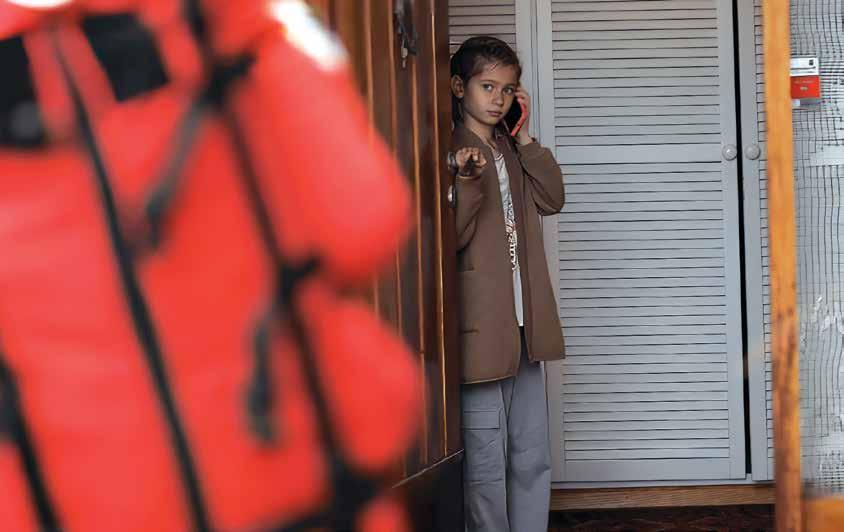
Unlike traditional training that crams information into overwhelming sessions, LDHF spreads learning over manageable, frequent intervals, boosting retention and seamless application of skills. This approach minimises downtime, trims resource use, and enhances productivity. Employees stay motivated with regular, relevant training, reducing turnover and fostering a culture of continuous improvement. With scalable, tailored training that meets immediate needs, organisations see direct support for strategic goals and operational efficiency. It's a smart investment that drives long-term growth and a stronger bottom line.
This advanced training method is not just a tool; it’s a revolution in emergency response. By equipping operators with the skills and resilience needed to excel in high-pressure environments, it enhances overall service quality and effectiveness, ultimately saving more lives.
Lena Heimvik sums it up perfectly: "With this innovative approach, our operators are better prepared, more confident, and more resilient, ensuring that we provide the highest quality of emergency response possible."
For more information, visit sklls.ai
Lena Heimvik sums it up perfectly:
With this innovative approach, our operators are better prepared, more confident, and more resilient, ensuring that we provide the highest quality of emergency response possible."


Ole Paulsen Founder, Sklls
Lena Heimvik Head of the Prehospital Clinic, Helse Stavanger


SDSI provides software and support services to public safety agencies that support 80% of Australia and New Zealand's population.





Challenges in emergency response are part of the everyday life of rescuers. Long distances and long transport times are problematic, as the oxygen supply is limited in most cases. With MEDUVENT Standard from WEINMANN Emergency you have a ventilator that works independently of oxygen. Thanks to turbine technology, it can ventilate patients without an external gas supply. With the low-flow supply you can easily supply patients with medical oxygen or concentrator oxygen.



A local’s view of living and working in the northern capital.
Jeanette Button, St John NT
Full disclosure – I am not a paramedic, but I have had the privilege of working with the Northern Territory’s ambulance service at St John NT for close to five years as their marketing, communication, PR and media manager.
Working in the Northern Territory comes with its own set of unique challenges. Unless you were born and/or raised here it generally means moving away from family and friends, learning to adapt to a different environment and expectations. When I first arrived 25 years ago, people would say that NT stands for not today, not tomorrow or more specifically not Tuesday or Thursday, alluding to the fact that we were so far away from the rest of the country that you just had to wait and be patient.
The Northern Territory is 1.4 million km2, France will fit into it twice with room to spare. Our total population of 250,000 is similar in size to Hobart and the entire population of Darwin would almost fit into the MCG! Our closest department stores are in Denpasar and Cairns. By air it takes us approximately four hours to fly to another Australian capital and it is only two and a half hours from Bali. In the big scheme of things, these are minor considerations.

Due to its remoteness, small and somewhat isolated population centres, we learn to make do and often to thrive.
From a professional perspective, the Northern Territory provides a great opportunity to become a master of many trades. For our paramedics, the NT presents opportunities that would be hard to duplicate in other parts of Australia. Clinical staff are exposed to a complex workload. Unlike other, more urban areas, paramedics in the Northern Territory treat a largely younger, but chronically unwell population.
In many cases NT paramedics frequently find themselves caring for patients with diseases like rheumatic heart disease, kidney disease, and chronic obstructive pulmonary disease.
The type of chronic conditions which contribute to approximately 77% of the life expectancy gap between the Aboriginal and Torres Strait Islander people and the non-Indigenous population, putting paramedics on the frontline of the nation’s biggest health crisis.
St John NT Director Ambulance Services, Andrew Thomas explains that while the diseases in the Territory present unique challenges, the need for flexibility in the role allows paramedics endless opportunities for adaptive and creative thinking.

“One of the biggest challenges faced by our crews is overcoming language and cultural barriers,” he said. "With over 100 First Nations languages in the Northern Territory, first responders are continuously building a vocabulary and developing resources to ensure patients continue receiving high-quality care.”
“With thirty percent of the Territory’s population identifying as Aboriginal, paramedics must also consider more holistic approaches against standard care models. The vast health disparities we see make the Territory seem foreign to most other parts of Australia in terms of healthcare.”
St John NT paramedics also find that they respond to a significant number of trauma cases, requiring them to expand their clinical skills and scope of practice to ensure that patients across the Territory receive the level of care and treatment they need in often life-saving situations.
As a non-clinical professional in this space, the Territory has meant having the opportunity to take on new challenges, work across industries and build skills and knowledge based on a range of experiences which may not be available in a much bigger pond.
For families, moving to the Territory often means moving away from family support. My own children learnt to fly as unaccompanied minors from a young age with eager grandparents waiting at the other end for the school holidays. Now that the kids are grown up, they have also experienced moving away to go to university but have returned to the Territory as their preferred place of residence.
In such a small population it is easy to get to know your community, where other places talk of six degrees of separation it is much more likely to be two degrees in the NT. With a great outdoor lifestyle and food markets you are likely to bump into your local MLA (read MP from other states) at the juice stall in Parap.
For sports enthusiasts, there are more opportunities to be on a state representative team when the selection pool is also so much smaller. The different football codes like to send a team or two north for a game each year and one day, in the hopefully not too distant future, we will even have our own team following the Tassie Devils into the big league with the AFL.

Did I mention that Darwin enjoys an average temperature of around 32 degrees all year round?
The only difference being the level of humidity, which can at times feel like walking around with a big wet blanket on, but hey we save money on hairstyling, makeup and stockings as there is no way any of these can be applied in our Wet Season.
When I meet with interstate colleagues somewhere “down south” the top three questions are: how long did it take to get here, how hot is it at the moment, and don’t you miss the big cities?
No – not really.
One of the good things we achieved through Covid-19 was an acceleration of technology and the ability to connect with our colleagues and do business easily online. And, while I love meeting face to face in one of those “big cities”, I also love the feeling of making that four-hour trek back home and grabbing my dogs for a walk on the beach, no matter the time of year.
Considering travelling north? It’s not as challenging as some make out – give it a go.

Button Director Strategy, Brand and Engagement, St John NT
With more than thirty years’ professional experience, Jeannette Button has developed projects across the telecommunications, tourism, health, mining, government and not-for-profit sectors. She is now the Director Strategy, Brand and Engagement for St John NT, the ambulance service provider in the Northern Territory. Jeannette joined the organisation in November 2019 to develop its marketing and communication presence. But that was just before Covid, when everything took a different path. She is an accomplished public relations practitioner, experienced in crisis and media management and aware of the importance of safeguarding brand and reputation.
When not at work she can often be found walking her poodles on the beach.
St John NT is currently looking to recruit qualified paramedics to the Northern Territory, to find out more visit stjohnnt.org.au or email: jobs@stjohnnt.asn.au

NSW AmbulanceGraeme SA Ambulance Service - BBQ Kings

Not all volunteers are riding in the ambulances, some of the best are found on their own respective sets of tools. Pictured you have Trevor, Don and Malcolm who are support volunteers for the SA Ambulance Service cooking what looks to be a salivating BBQ for the team. While they might not be in an ambulance, their hard work doesn’t go unnoticed, as these volunteers help keep the teams fuelled and stations running around the clock.
Great work guys and thank you to all support volunteers.
For over one and a half decades, Graeme has been volunteering alongside the team at NSW Ambulance as a Service Chaplain. Graeme spent time as a combat medic during the Vietnam War and has transferred his experience and knowledge to NSW Ambulance by showcasing the importance of support when it is required most.
Thank you, Graeme.

St John WAIan Digweed
This year marks 47 years of voluntary service with St John WA for Ian Digweed. Starting his voluntary career at 11 years old as a cadet, the Emergency Ambulance Technician is part of the St John Pinjarra Sub Centre and is incredibly proud to be part of the St John WA organisation. After close to five decades with SJWA, Ian has seen plenty of significant changes including the introduction to defibrillators onboard ambulances.
We could imagine the changes you’ve seen Ian.


A very creative effort from the team at St John NT by using the seas around Australia to name and thank their volunteers.
Head to their Facebook post dated May 20th to see the list of names.
Ambulance Victoria celebrated all their volunteers this National Volunteer Week but highlighted Jan Ogle, Team Leader of the Blackwood Community Emergency Response Team (CERT) as well as the first CERT member to be an AV Peer Support Dog Handler with her labrador Pippa. Both a midwife and volunteer with Ambulance Victoria, she hasn’t been fortunate enough to have “the ultimate crossover” but has been told by her team, that the day it happens, she will be the first call out.
Thank you for your service, Jan.



St John WABob Hosken

Retiree Bob Hosken is putting his free time to good use. Bob has been working alongside St John WA Community Transport Service (CTS) for four years and counting, where he transports the community members from door to door for their medical appointments and activities. No stranger to St John, as back when he was 18 years old, he was a volunteer ambulance driver for St John South Australia. A conversationalist, Bob is a qualified Indonesian translator as well as having learnt French, Latin, Greek and Hebrew and loves chatting in the native language of the rare Indonesian or Malaysian passenger. You’re an inspiration Bob, congratulations on reaching 1,000 hours of CTS service this year.
The team of volunteers at SA Ambulance Service aren’t shy to award nominations and wins, with this year being no different. These four volunteers were nominated for SA Volunteer awards with VSU Manager Nicole (pictured) being a finalist in the Excellence in Volunteer Management Award category.
Keep up the great work team.

When people are in dire straits and they see you coming in this uniform, it gives them a sense of hope and a sense of relief that the cavalry has arrived.”
Ian Digweed

AmbulanceTasmaniaMultipleGenerations
AmbulanceTasmaniaMultipleGenerations
Ambulance Tasmania -MultipleGenerations

Strahan Ambulance Station in Tasmania has multiple generations working alongside one another. Mark started the team in 1990, with Christinne and Dianne joining throughout the decade. Longtime volunteers Vicki and Brian brought their experience to the team during 2010, and since its creation in 1990, several Ambulance Service Medals have been awarded. With the need to bring some “younger faces” to the team, Strahan Ambulance Station doubled their numbers after a recruitment drive and halved the average age in the process. Younger recruits Kiat, Harriet and Katy have fit in perfectly with the team and have taught and learnt much in the process.
That sounds like a successful recruitment drive to us.
Cody and Clint are part of the Community Emergency Response Team (CERT) that operate close to the NSW/Victorian border in Howlong. Both father and son have been involved in the CERT team since its inception in 2023 and have made plenty of memories working together including Clint’s proudest, where he and Cody treated a patient with a suspected heart attack alongside each other.
Thank you for your service and all the best.


They say many hands make light work, and in country communities like Kununoppin in WA’s Wheatbelt, they keep vital services alive.
Four generations of one family have given more than 90 years of volunteer service to ensure their region’s ambulance service runs around the clock.
Geoff Waters has been volunteering with St John WA Kununoppin Sub Centre for 44 years and has served as its chairperson for the past two decades.
His son Mark stepped up to help eight years ago, followed by his grandson John.
The Waters men continue the legacy of Geoff’s mother Evelyn, who was one of the founding members of the sub centre in 1952 and a volunteer for about 40 years.
The sub centre covers hundreds of kilometres of bush, with 12 ambulances spread across six locations responding to about 290 emergency calls a year.
With three generations of Waters ready to jump in an ambulance at all hours of the day and night, there have been plenty of family barbeques and even Christmas lunches interrupted by calls for help.
“I get a phone call from Dad, and he says, ‘put your uniform on, I am picking you up in five minutes’,” John said.
Mark and 24-year-old John usually come as a package deal on the road.
“Our co-ordinator says you need some quality father and son time together,” Mark said.
After decades of late night and early morning callouts, 72-year-old Geoff said it was all worth it to ensure his community was taken care of.
“I often get asked why I do so much, and I say, I hope one day if one of my family needs an ambulance someone will do it for us,” he said.
“We are here for the community – that is the bottom line.”
John said the beauty of volunteering in such a tight-knit community meant they were often assisting people they knew, so it was easy to keep them comfortable.
“No one wants to call an ambulance, but when you do and you see a local face, you spend half the time talking and it keeps the situation a lot calmer,” he said.

Mark got involved after seeing his dad and other older volunteers struggling to meet demand amid dwindling numbers.
He started with ambulance transfers in his spare time and quickly discovered the joy of helping elderly patients on jobs big and small.
“I enjoy talking to the patients, listening to their stories and making their trip to hospital or wherever they need to go more comfortable,” he said.
“The patients are always thankful and that’s what makes it more than worthwhile.
“Anyone can volunteer to be an ambulance officer; you’ve just got to have the right temperament and be willing to learn and work as a team.”
Having served his community in the fire brigade for 50 years and on the local council for 27 years, all while running the family farm, Geoff knows the value of giving back.
“I just love helping people in the local community, they know you and know you’ve got their best interests at heart,” he said.
“That’s always been my attitude, if we can’t help one another, then life is going to be pretty lonely out here.”
The born and bred Kununoppin local is a pillar of his community, known to go above and beyond to ensure every patient is well looked after.
Geoff said everyone had something to give.
“Every little bit helps and takes the pressure off the people who are doing a lot,” he said.
“We’ve got a diminishing community population, if we don’t have volunteers, we won’t have an ambulance service.”

St John WA Regional Manager Wheatbelt Matthew Guile said volunteers like the Waters family were the lifeblood of regional communities.
“The Waters family demonstrate the true spirit of volunteering – to give back to their community without expectation of recognition or reward,” he said.
“Without volunteers in regional communities, we would not be able to provide the same level of service with such professionalism, care and compassion – and the commitment of three generations of the Waters family to work together to support their community is truly inspiring.
“Their remarkable contribution spans decades, and on behalf of St John WA Kununoppin and the entire St John WA organisation, we thank them for their dedication to their communities and the service of humanity.”
A recent survey released for National Volunteer Week found nine in 10 Western Australians think favourably about people who volunteer, click here to learn more.
More than 5000 volunteers contribute their time across a range of roles with SJWA from on-road emergency ambulance response in country WA, to logistics, volunteer support, community transport and Event Health Services.
To become a volunteer visit, stjohnwa.com.au/changelives

Hato Hone St John (HHSJ) is on a mission to reduce emissions and find sustainable ways to deliver care to communities, with the launch of Australasia’s first electric emergency ambulance trial, supported by long-standing partner ASB.
After two years’ planning, designing, and assembly, the custom-built emergency ambulance was gifted to HHSJ by ASB at a special blessing ceremony in Ng ruaw hia and will be based in Hamilton for a trial to understand its full range and reliability.
At the blessing, Cameron Brill, Hato Hone St John Deputy Chief Executive Corporate Operations, said that with a fleet of almost 1400 vehicles (around half being ambulances), reducing vehicle emissions were where the organisation could have the biggest impact.
“It’s the biggest focus for us in how we can provide an efficient world-class health service to our communities but in a more environmentally friendly and sustainable way,” Mr Brill said.
He acknowledged the huge financial contribution of ASB in enabling HHSJ to build and test the feasibility and viability of an electric ambulance for the emergency ambulance service.

“In this fiscal environment investment in sustainable technologies becomes even more challenging. We would not be here today had it not been for ASB stepping forward to support this project,” Mr Brill said.
ASB Head of Sustainability, Carrie Gage, said ASB was proud to be a long-standing partner of Hato Hone St John, and to support them on this important initiative.
“Building a sustainable future for all New Zealanders is a core focus for us. We see potential for this project to have a rippling effect through other industries on the same path and are extremely excited to be able to pave the way for future work in this space,” Ms Gage said.
Colin Tan, Head of Service and Sustainability, said that ASB has been part of the process since 2022, supporting the idea and providing funding to build the vehicle from inception to realisation.
“We believe we are the first emergency service in Australasia to trial the feasibility of an electric emergency ambulance.”
Colin said the organisation could not have done this without the help of their supporters.
“ASB has been pivotal in us being able to build and trial the first EV (Electric Vehicle) emergency ambulance in Aotearoa New Zealand, but we are also especially grateful to Siemens and YHI for their generous donation of EV chargers, which have been installed at our Hamilton Station. A big thank you to everyone who has made this project possible.”
Colin said that while Hato Hone St John is very much in its infancy of EV exploration, our mahi towards a more sustainable fleet has been in motion since 2021 with our initial focus on moving non-emergency vehicles towards hybrid and electric models.
“We know that transitioning non-emergency vehicles makes sense and the trial will tell us whether it is also viable and affordable for our emergency vehicles.
“Not only are we keen to analyse the cost benefits of fuel savings, as well as carbon emissions reductions – we will also be closely analysing the clinical experience for our people and our patients.”

Bria Walker, National Youth Cadet of the Year, said during her speech at the ceremony that it was “truly awe-inspiring” that Hato Hone St John was actively taking steps towards becoming more environmentally sustainable.

“While pioneering the very first electric ambulance in Australasia may seem like a scary step for many, it fills me and our young people with confidence and satisfaction seeing Hato Hone St John constantly working to fulfill our responsibility as tiaki, looking after the environment for our future generations”, Bria said.
“Seeing Hato Hone St John being supported by and working with ASB to continue the journey of making this positive change makes me incredibly proud to be a kiwi, and I feel honoured to be a part of such an environmentally focused organisation that is committed to making another positive impact, changing our lives for the better.”
The Ford-Transit EV emergency ambulance was built in Hamilton by Action Manufacturing.
• It will be based at Hamilton Ambulance Station (Seddon Road) where two chargers, donated by YHI and Siemens, had been installed and will begin on 12-hour day shifts.
• While HHSJ is confident the vehicle’s range of around 250km would manage the average 180km distance ambulances typically covered in a shift, a back-up vehicle would always be available.
• HHSJ would run a year-long trial capturing data on the vehicle’s range and performance, as well as ambulance officers’ clinical experience on shift.
• The EV emergency is very responsive and goes from 0km to 100km in around nine seconds.
• Ambulance officers must undergo driver training prior to working shifts on the EV emergency ambulance.



Last shifts are always special for members of the ACT Ambulance Service, but for Gav, a 22-year veteran paramedic, his final day was particularly significant.
He got to work it with his best friend, and fellow paramedic, Jill.
Gav and Jill met 16 years ago at the previous ACT Emergency Services Agency headquarters in Curtin, on the day they were both applying to join the Ambulance Service.
“We met outside the building, before Gav went in to do the interview and exam,” remembers Jill.
“I got a little worried at how many pages of notes Gav seemed to be writing for his exam, and he saw my notes and started worrying he was writing too much, but, in the end, we were both accepted.”
The friendship struck on that day would prove to be enduring, and Jill, who originally worked as a paramedic in the Northern Territory, says she will forever be grateful for the support she was given by Gav and his wife during her early years in the nation’s capital.
“They really took me under their wing,” says Jill.
“Gav and his wife went out of their way to introduce me to people and show me around Canberra.
“Gav and I are both quite sporty, so every Sunday we would go for a bike ride together, then study all afternoon – it was like a religion!”

Over the years Gav and Jill would continue to catch up frequently outside of work hours, but they would only rarely talk shop.
“We have so much in common and our personalities have always gelled,” says Jill.
“The only times we talked about work was after one of us had dealt with a particularly difficult job and needed to talk it out.”
Gav’s sporty side is what would eventually lead him to leaving the ambulance service, as his running coaching side-business grew into a full-time job.
Jill, who was one of his first clients, says the positive signs were there early, with Gav being a multiple winner of the ESA’s Darren Wall Memorial fun run.
“He managed to beat the firies on a few different occasions,” laughs Jill.
“Gav is very proud to have his name on that trophy, which sits outside the Commissioner’s office.”
Despite for all the time they have spent together, and their longlasting friendship, during their time at ACTAS Gav and Jill were only paired to work together once, during a night shift.
However, once Gav had finalised his leaving date, he requested that Jill and he could partner up for his final day in an ACT ambulance.
Jill was only too happy to agree.
“It was a really special shift,” says Jill.
“In between attending jobs, we also found time for a coffee down by the lake, and some quick visits to Canberra’s monuments.
“We also talked through our careers, and everything we have achieved, I’ll never forget it.”
As the shift approached its end, Gav and Jill were tasked to one last emergency call, where a patient was suffering from a cardiac event.
Working together, these two old friends managed to save the patient’s life and deliver them safely to hospital.

“All of the training we’ve done, and all the time we’ve spent together,” reflects Jill emotionally, “it was like everything about our friendship amalgamated on that final job.
“On the way home, I asked permission for Gav to do a last call over the radio, to officially sign off.
He’s just such a beautiful human being –I’m really proud of him, but Gav leaving is a big loss for the service.”
Thank you, Gav and Jill, for everything you’ve done for Canberra’s community.

Donald Forrest Jones is remembered by his family as a humble, kind, quiet and generous man with a quick wit and a wealth of stories from a life well lived.
He was always thinking about what was next in life and indeed even in the weeks leading up to his death was excited to be planning the next big project alongside his family.
After a life-long career as an accountant (he reluctantly relinquished his last client at age 90), it's not surprising that Donald has ensured his legacy will continue for many generations.
Last year, Donald and his family made a transformational gift to build Wairarapa Ambulance Station – committing $1 million to help fund this vital asset for Wellington Free and the community.
Donald was adamant that during his lifetime he was to remain anonymous, which fits with his humble and private nature. Since his passing in March 2024, it's now appropriate to publicly acknowledge and celebrate his life and legacy with the community that will benefit from his generosity.
Growing up and spending the majority of his life in Palmerston North, Donald was from a family of six – including two sets of twins. Donald’s father started William E Jones, a well-known monumental masons’ business, still serving the community almost 100 years later. Donald and several of his brothers worked for the family business at some point in a variety of roles, Donald taking care of the finances.
Donald began his career as an accountant learning on the job and working his way up, eventually starting his own accountancy firm which he worked in and managed for the majority of his professional life.
A life-long bachelor, Donald was hugely committed to his work as well as many community groups. He spent many years with Roller Skating NZ where his secretary / treasurer skills saw him travelling with the team to competitions during the height of roller-skating popularity in the 50s and 60s.
His entrepreneurial nature saw him involved in the establishment of the Guardian Newspaper in Palmerston North, a community newspaper that exists today as the Manawatu Guardian. Donald saw this as a business opportunity as well as a service to the community in terms of sharing news and current events across the city.
Over many years he travelled the world indulging his love of art and history. Often, he would bring back business ideas from things he had seen – a great example of this is Uncle Sam’s Americana – a burger bar that was iconic for Hawaiian burgers with steamed buns. A fond memory for many in Palmerston North.
Alongside his love of numbers, art and history, Donald was passionate about property and architecture. Designing his own home and building a number of commercial properties, including one of the first shopping centres in Palmerston North that included the first mini market for the area. As with all entrepreneurs he experienced huge success and also disappointment when things did not turn out as planned, however his desire to pursue the next thing was not dampened and he went on to have many successful business ventures.
Donald lived his final years in the Wairarapa, enjoying being closer to family. It's during this time in the Wairarapa Donald saw and experienced firsthand the need for and importance of Wellington Free Ambulance. The Fenix Foundation, a charitable trust Donald established, has supported well over 160 charities to varying degrees over many years, but the time had come to make a substantial donation that would potentially help everyone in the area, which is where the purpose built Wairarapa Wellington Free Ambulance Station came in.
Donald was thrilled to donate to a cause that supports everyone in the Wairarapa. He was particularly interested in this property project due to the IL4 building rating required to ensure this ambulance station is fully operational as a community hub in a civil defence emergency. He knew that at some stage anyone and everyone could benefit from his donation towards the Station as a service that is there for anyone.
The $1 million donation given by Donald and his family is historic for Wellington Free Ambulance as the largest ever single gift from a family made to the service.
Right up until his last days of life, Donald was wanting to get things done and achieve things, discussing his wish to donate the flag for Wairarapa Ambulance Station with his niece, a wish we will be proud to honour when the Station build is complete.
Donald will be remembered as a selfless man who wanted to help people. His private nature means his generosity and compassion for his community may have gone unnoticed during his lifetime, but with this tremendous gift to Wellington Free Ambulance his memory and legacy will live on for many generations to come and be appreciated by all.
Nga mihi nui Donald.




Further your challenging and rewarding career as quali ed paramedic by gaining advanced knowledge and practical skills in critical care.
» STUDY A GRADUATE DIPLOMA OR MASTER IN PARAMEDIC SCIENCE (CRITICAL CARE PRACTICE)
Equip yourself to take on a leadership role as a paramedic by specialising in primary healthcare practice and provide essential services in the non-emergency, out-of-hospital, low acuity or primary healthcare settings.
» STUDY A MASTER IN PARAMEDIC SCIENCE (PRIMARY HEALTHCARE PRACTICE)
Learn how to assess, plan, prepare and implement strategies for successful operations in high-threat environments.
CQU’s unique postgraduate courses provide rst responders, nurses, doctors and professionals similarly exposed to trauma medicine with a strong theoretical background and practical skills to successfully operate and manage patients within hostile environments.
» STUDY A GRADUATE CERTIFICATE OR GRADUATE DIPLOMA

APPLY NOW TO START ONLINE IN MARCH 2025
Our graduates are some of the most sought-after in Australia, due to our reputation for work integrated learning and industry-aligned courses.
We have over 40 years of experience delivering distance education, so you can study online with con dence. Plus, you can access facilities and support at more than 20 national locations.
In the top 8 Australian universities for postgraduate starting salary.*
Five-star rating for postgraduate student support*
* The Good Universities Guide 2024
Not sure which course is right for you? Book a one-on-one conversation about your individual journey with one of our CQU expert advisors. Search CQU Book a conversation.
August 15th 2024 CAA Awards for Excellence Gala Dinner at Melbourne Convention and Exhibition Centre, Australia
For 17 years, the Council of Ambulance Authorities has proudly presented the Awards for Excellence. The Awards recognise the hard work and innovative solutions of our member services from Australia, New Zealand, and Papua New Guinea across a range of areas, representing all the people, teams and job functions that go in to running and developing a truly world-class Ambulance service.
The awards are designed to encourage members services to learn and share from each other beyond the committees, forums and working groups that are also a vital and formal part of sharing best practice and information.
The awards are judged by a panel of independent, industry-respected judges from around the world. They give of their time and expertise freely, and we are truly grateful for their assistance and insights. Without our judges, our awards would not be as strong or held in as high esteem as they are.
Winners are announced at the Gala Dinner on August 15th at the Goldfields Theatre, MCEC, where the winner of the prestigious Star Award is also announced, selected by our judges from amongst the six category winners as doing something uniquely innovative in the ambulance sector, ultimately leading to better patient outcomes.
Here we share with you an overview of each Award category, along with the finalists.
To learn more about the 2024 CAA Awards for Excellence, scan this code with your camera or visit caa.net.au/awards


Recognising innovation or capability in the fields of equipment, communications, and information systems.
When making their submission to this category, each service is encouraged to reflect on how their organisation has used technology in the past twelve months to enhance patient outcomes, staff performance or response capacity.
Finalists
Ambulance Victoria –Video Assisted Secondary Triage
Ambulance VictoriaFOCUS Analytical Dashboards
Ambulance VictoriaATOMS - Ambulance Tasmania Online Medication System
Recognising innovation or capability in the fields of skills mix, pharmacology, and clinical intervention as they relate to patient treatments and outcomes.
When making their submission to this category, each service is encouraged to reflect on how their organisation has excelled in clinical practice with breakthrough moments that saw cutting edge techniques implemented to revolutionise the world of paramedicine.
Finalists
Ambulance Victoria –Blood Component Access Project
Hato Hone St John –EMT Fentanyl Initiative
Queensland Ambulance Service –Full Implementation of the Clinical Hub

Recognising education improvement or innovation in the fields of: programme design, delivery, assessment, and accreditation; professional development, skills maintenance, and practice standards, including community education; and research and/or innovation supporting evidence-based practice.
When making their submission to this category, each service is challenged to explore areas where improvements have been made in staff development, and how these resonating changes have improved the evolution of paramedicine.
Hato Hone St John –Remote Triage
Queensland Ambulance Service –Leadership Capability Development Framework
Queensland Ambulance Service –Low Acuity Response Medic Pathway to Paramedic
Recognising patient experience, improvement, or innovation.
When making their submission to this category, each service is emboldened to examine ways that their organisation has assisted specific patient cohorts where learnings were of benefit to the field of paramedicine.
Ambulance Victoria –
A Strategy to Enhance Cardiac Arrest Survival after the COVID-19 Pandemic
Queensland Ambulance Service –The Queensland Ambulance Service Falls Co-Response Program
St John WA –State Obstetric Referral Call – STORC. Midwives Join Frontline Ambulance Crews to Improve Maternity Care for Women and Their Families





Recognising management practise and operational improvement and innovation in: management culture, open communication, accountability, management development, professional standards, and diversity of workforce; and operational protocols and work practices relative to how service delivery is provided.
When making their submission to this category, each service is encouraged to analyse the programmes they have implemented that paves the way in leadership for future generations.
Finalists
Ambulance Tasmania –
Working Flexibly at Ambulance Tasmania
Hato Hone St John –
Tactical Commander Training Framework
St John WA –
Total Solar Eclipse 2023
First introduced in 2021, this category recognises innovation and excellence a service has provided both staff and patients in improvements in mental health and wellbeing, including programmes, training and support.
When making their submission to this category, each service is encouraged to share their undertakings in mental health and wellbeing for all stakeholders in the Ambulance sector, including patients, staff, and leaders.
Finalists
NSW Ambulance –
Mental Health First Responder - a Real Time Virtual Mental Health Triage Service
SA Ambulance Service –
Paramedic Telehealth Clinicians - Mental Health
St John WA –
Inclusive Flexible Workplace Arrangements (FWA) to Support Work-life Balance in Ambulance
Leading with Love. The New Frontier of Heart-Centred Leadership
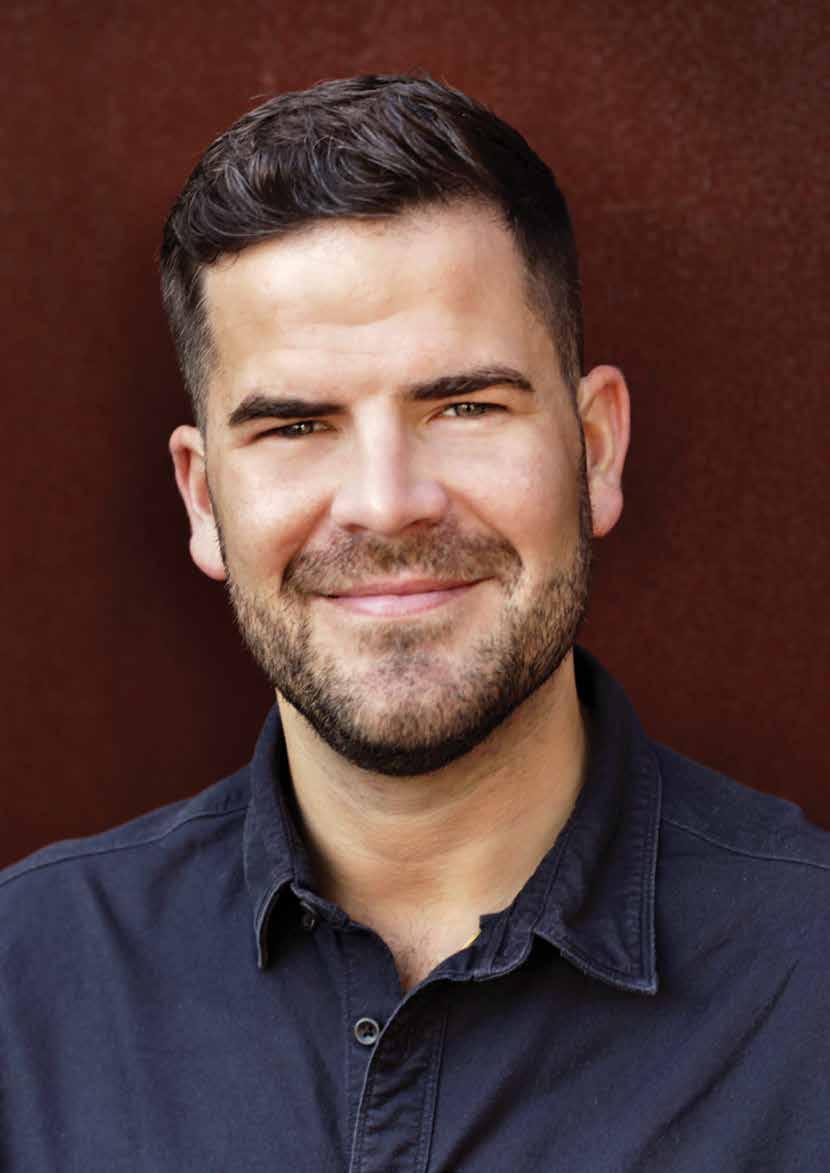
I am the leader I am because of the love, care and learnings I took (and continue to take) from my parents and four brothers and sisters.
Jordan
Emery, CAA Board Member Chief Executive, Ambulance Tasmania

Meet Jordan Emery, CAA Board Member and Ambulance Tasmania’s Chief Executive. Prior to relocating to Tasmania and assuming his current position in June 2023, Jordan has been within the health sector for almost 20 years working within clinical and non-for-profit organisations.
Self-confessed heart-centred leader, Jordan is passionate about delivering a high performing team that live and breathe psychological safety and put people first. CAA and the team from First sat down with Jordan to hear what it takes to create a supportive working environment within the ambulance industry.


First up, tell us a bit about your journey and how you’ve managed to become one of the leading Chief Executives in Australia within the health sector
My journey has been incredibly rewarding and I feel a deep sense of privilege for the opportunities I have been afforded along the way.
Without starting right from the beginning, I grew up in Sydney, the second youngest of five children and went to my local public primary school and high school. I share that because fundamentally, I am the leader I am because of the love, care and learnings I took (and continue to take) from my parents and four brothers and sisters.
When I finished school I relocated to Bathurst, NSW to study paramedicine at Charles Sturt University and in 2008 was incredibly fortunate to be accepted into a paramedic position at NSW Ambulance. I was naturally interested in leadership, initially in a clinical sense so I pursued my Intensive Care Paramedic training, and then moved into frontline people leadership roles, first as a Station Officer in South Western Sydney and then onto a Duty Operations Manager role.
A formative experience for me was undertaking the Executive Staff Officer role for the Commissioner of NSW Ambulance. It significantly expanded my understanding of ambulance service delivery and perhaps more broadly my appreciation for leading through complexity. Experiences in that role also taught me about the transformative power of duality – the ability to hold two competing ideas in tension, recognising that both can be true, and then to chart a path forward. It’s a learning that I think has been critical to all the leadership roles I have had since, and I actively try to resist black and white thinking, or arguing that someone else’s viewpoint is incorrect, but rather recognise their experience, offer alternate perspectives and seek to find common ground.
In 2016 I took a two-year career break and relocated to New York where I lived and worked for a global mental health non-government organisation (NGO) as their Business Development Manager. The organisation delivered community mental health programs in East Africa, predominantly to women with depression, anxiety and post traumatic stress disorder.

It was a life-changing experience to be part of an evidence-based, cost-effective and scalable model of care that had a profound impact on the lives of incredibly marginalised women and their families. It also allowed me to put into practice some of the academic learnings from my Master of Health Management and Master of Public Health which I had completed through the University of NSW.
The experience of working in a start-up, NGO setting in the global development space has also been a significant influence on my leadership journey. In my role as Business Development Manager, I led the organisation’s fundraising/ revenue generation efforts. Philanthropy taught me several powerful leadership lessons, particularly around communication and cultivating genuine engagement.
In mid-2018 I returned to NSW Ambulance and moved into senior operational leadership roles, initially as a Zone Manager and then as Associate Director of Operations leading all of Hunter New England Sector, based out of Newcastle.
I actively try to resist black and white thinking, or arguing that someone else’s viewpoint is incorrect, but rather recognise their experience, offer alternate perspectives and seek to find common ground.
My time in Newcastle was both challenging and rewarding. I had the privilege of leading the sector through some very significant cultural reform, and really forging out a new leadership approach focused on cultivating psychological safety, building trust and putting our people at the centre of everything we do, so that they could provide excellent care to the community.
In January of 2022 I relocated to beautiful Tasmania, first as the Executive Director of Operations and then I was appointed as the Chief Executive. Like all ambulance services, Ambulance Tasmania has wonderful strengths and areas of challenge that we continue to work through as a team. It’s significantly smaller than the three large eastern seaboard ambulance services, but it’s a mighty organisation fueled by incredibly good people doing important work in communities right across the state. Every day I reflect on the enormous privilege of leading the great people that make up Ambulance Tasmania, and I try to use this opportunity to create a kinder, more caring organisational culture. I truly believe that cultivating that will only expand the kindness and care we provide those in the community.



Jordan, you’ve got an amazing approach to heartcentred leadership, or leading with compassion and kindness. Can you explain to us what that means when it comes to the health sector?
I first spoke about heart-centred leadership, or leading with love, at the Australasian College of Paramedicine’s International Conference in September of 2022. Quite unexpectedly it seemed to really strike a chord with people, and in truth, whilst this has mostly been positive there have also been criticisms about what I have spoken about. I’m not troubled by that in any way, and I’ve learnt that some of the best transformation happens in disagreement, but I’ve also thought more about how I define and explain leading with love as both a concept and a leadership practice.
In 1978, M.Scott Peck, a psychiatrist, authored the book, The Road Less Traveled, which has which has sold millions of copies worldwide. Peck described love as “the will to extend one’s self for the purpose of nurturing one’s own or another’s spiritual growth”. He goes on to explain that “love is an act of will – namely, both an intention and action” and that “will” also implies choice, that is, we do not have to love, we choose to love. This definition might seem a little esoteric, but in my mind it really is the crux of leadership – the willingness to nurture yourself and others to achieve their growth, or described in another way, to achieve their fullest potential. When I’ve shared this definition by Peck, some people are thrown by the idea of spiritual growth and draw parallels with religion, but Peck describes spiritual growth as the dimension of our core reality, that when nurtured, enhances our capacity to be “more fully self-actualised and able to engage in communion with the world around us.”
In my mind, that is exactly what we want in our organisations - people who are achieving their fullest potential and contributing that potential to their team, because we as leaders have made an active choice to nurture them.
So if I was to take that definition and apply it practically to my role as a leader, I think it looks like four things (which for ease of reference I refer to as the four chambers of the heart):
1. Building trust through authenticity, empathy and logic (the work of Frances Frei and Anne Morriss).
2. Demonstrating vulnerability (the work of Brene Brown).
3. Practising radical candour (the work of Kim Scott).
4. Cultivating psychological safety (the work of Amy Edmonson).
These four leadership practices are what I think are the central tenets of heart-centered leadership. They are fundamentally about building meaningful connection with the people we lead and nurturing them to achieve their fullest potential. That is the calling for all healthcare leaders, and because the work we do in health services is so important to the community at large, we have a special obligation to embed this way of leading in everything we do – from direct patient care, to mentoring newer team members, to leading whole organisations.


We do not have to love, we choose to love… in my mind it really is the crux of leadership –the willingness to nurture yourself and others to achieve their growth.



Being in your role you must have some people you look to for support or mentorship. Do you have a role model or support network you find invaluable when it comes to work?
I’ve been so fortunate to have many people throughout my career that have supported me in my own leadership journey. Some of those have been formal or informal mentors, trusted colleagues, a coach and a psychologist. For me, it’s about building relationships with those individuals and knowing who to tap in to for support or guidance along the way –and most importantly how you can repay that support to others.
I should also say that some of the most powerful mentors have been people in my team ‘more junior’ to me – a concept called reverse mentoring. It’s been well adopted my big corporations such as General Electric (GE) and Estee Lauder as a way of ensuring wellrounded feedback and guidance for leaders on how they are performing, decisions they have made or intend to make, and workforce sentiment in general.
In my role as Chief Executive and even in other senior operational roles, I’ve deeply valued the honest, constructive feedback I’ve received from reverse mentors, who are typically much closer to the coal face than I am and can give me a perspective that I would otherwise not have had.
The Council of Ambulance Authorities has also been extremely beneficial as a network of support. I don’t just say that for the sake of this magazine article, but because I genuinely believe we are better when we collaborate instead of operating in competition with one another.
My experience having relocated to Ambulance Tasmania from NSW Ambulance is that so many of our organisational challenges are similar, and the support I have received from other Chief Executives right across Australia and New Zealand has been so invaluable to my own leadership.


Allyship is a term within the leadership space that’s become more relevant in recent times. Do you think allyship is important within our sector both personally and professionally?
Allyship is a critically important part of leadership if we want to create truly inclusive organisations where individuals can thrive. When I think about what it means to be an ally, I think of the individual as someone who is not part of a marginalised group but takes action to support or help those within that group. This is a fairly simple explanation and clearly there is more nuance to allyship than this basic description alone, but importantly, I think it is worthwhile emphasising that true allyship involves taking action and also that it is not about savourism. In my role I try to be a sincere ally to women, who I believe have been held back by our profession for far too long. I try to use my position of leadership, my position of privilege to partner with women and support their advancement, not by being a saviour, but by championing their interests, advocating for them, challenging the entrenched, obstructive or harmful ideas that hold them back, and perhaps most importantly, listening to and learning from the experiences of women in my team.
Of course, women in ambulance services reflects just one opportunity for men and indeed all leaders to be allies. In every way possible, I think it’s important for us to take stock of our own privilege and the opportunities that have been afforded to us, and use that to help advance the interests of others less fortunate. Positively, this is really aligned to the work of paramedicine and healthcare more broadly. The universal nature of healthcare in Australia and New Zealand means that we are accustomed to caring and advocating for all peoples regardless of their gender, race, ethnicity, religion, sexuality, disability status and so on. We strive to provide the same standard of care for all people as an inherent value in health service delivery, which means that as healthcare leaders, we must build on that approach and embed allyship into our everyday leadership practice.
There is a great book by Karen Catlin, called Better Allies: Everyday Actions to Create Inclusive, Engaging Workplaces that has helped me learn about ways I can embed allyship more into my leadership practice so that Ambulance Tasmania is a safe and inclusive workplace for all the awesome people that work and volunteer with us.


What are you personally passionate about when it comes to paramedicine and the clinical side of the health sector?
I’m passionate about clinical practice reform within paramedicine and the brave new opportunities that might exist for the profession in the near future.
The Commonwealth Government’s review of Medicare and thinking about scope of practice reforms has the potential to substantially change paramedicine practice in Australia and New Zealand in the years to come, so that we can provide the best healthcare to the communities we partner with. In Tasmania we are exploring new models of care that will see our Community Paramedics working in rural hospitals, which reflects just some of the exciting, interdisciplinary models of care that will unfold over time.
I do think it is critically important though that we don’t lose sight of the patient being at the centre of these reforms. For me, changes in the way paramedics and ambulance services operate is about exploring new ways to truly meet the needs of communities, particularly underserved communities, so that we can improve the health of Australians and New Zealanders altogether. There is a risk that we might make these reforms about us and our own professional identity (which isn’t something to be completely disregarded), but certainly shouldn’t form the basis of the reasons for reform.
In a decade’s time, I think paramedicine will look very different in Australasia, and I truly hope that whatever form that takes, our patients have better healthcare because of it. That in my mind is the most important indicator of success.



What are some key tips you’d give to someone who’s starting out in a managerial or leadership position?
There are so many great pieces of leadership wisdom others have shared with me along my own leadership journey - from mentors to peers, and thought leaders who have published some brilliant contemporary leadership literature, I’ve really tried to always keep learning.
In that respect, I humbly share one of the most important leadership lessons I have learnt, which is that leadership is not about you as the leader, but how you lead and take care of others. It sounds a little cliche, but I think all leaders can get caught up in themselves as the “hero of their own story”. It’s partly driven by ego, which is in many respects a normal part of being human.
Part of the way I’ve tried to buffer against this egocentricity is to never forget where I came from, as a frontline clinician, working with great teams and doing difficult work. That’s what our people continue to do each and every day. I also remind myself that any success I have achieved, which is largely a subjective construct, has been on the back of incredible love and support from my parents and siblings in the first instance and then my extended family, friends, colleagues and mentors. That helps to ground me in a sense of success that is more than me as an individual. And finally, I regularly take stock of the incredible privilege it is to lead others. The people of Ambulance Tasmania, no matter their role or contribution, are really remarkable people. To be given the opportunity to be their leader is a distinct privilege and I spend time reflecting on that with every leadership decision I make, especially ones that might leave some individuals upset or disappointed.
These practices have largely served me well, and I recognise that I am still growing as a leader each and every day. I hope this small bit of advice helps new leaders on their own journey.


What’s next for you Jordan, what would you love to see in the next 10 years when it comes to leadership within our industry globally?
I’m not entirely sure what is next for me. In the short to medium term, I am really focused on implementing Ambulance Tasmania’s new strategic plan - Our Future: 2024-2027. It sets the strategic agenda for our organisation with a view to delivering excellent care, everywhere in the state of Tasmania and creating a workplace where our people feel safe, valued and empowered to be the very best versions of themselves.
I’m also really focused on using my position to drive more diverse and inclusive ambulance services. In that respect, I have recently been appointed as the Chair of the CAA Diversity, Equity and Inclusion Forum, which has some incredible representatives from across the CAA member organisations. I think with our collective experience and focus, we can continue to promote outstanding initiatives that are already taking place across our profession and seek to have them adopted across all 11 member ambulance services.
And finally, what would I like to see in terms of leadership within our industry over the next decade - a whole lot more women in senior operational and executive leadership roles. With a workforce that is now more than 50% women, we have to ensure that barriers to the advancement of women into senior leadership roles are broken down, and that every incredible woman within our teams is given the space and support to thrive. For me, that is a matter of fundamental fairness - and our organisations will be so much better off for it.
I regularly take stock of the incredible privilege it is to lead others.




amPHI™ is a complete electronic prehospital solution that is scalable, secure, reliable, and resilient. amPHI provides an easy and efficient documenting platform, with real time information integration and sharing capabilities supporting collaborative care and powerful data mining opportunities across the entire episode.
amPHI™ is currently installed in more than 800 ambulance response units (road and air) with 15,000+ users, servicing over 9 million citizens. amPHI boasts a consistent uptime of more than 99.98% and is supported by 24/7 system surveillance.
Superior clinician designed multi–contributor AePCR – seamless information sharing and handover
Collaborative care model across the entire episode
Secondary Triage – supporting low acuity call management – decrease unnecessary ambulance dispatch

Advanced Mass Casualty Management – unique browser-based dashboards for collaborative mass casualty
Advanced Fleet/Resource Planning – planning, implementation monitoring and auditing
Cloud enabled solution – FHIR standards interoperability

The Council of Ambulance Authorities (CAA) is hosting it’s highly anticipated 2024 Congress, a premier event for the Australasian Ambulance Health Sector.
Set for August 14-16, 2024, at the Melbourne Convention and Exhibition Centre in Melbourne, Australia, the program promises to be a pivotal moment for professionals in emergency medical services and healthcare management.
The CAA Congress serves as a unique platform for top leaders, decision-makers, and senior management teams from ambulance services, health, and emergency management sectors across Australia, New Zealand and Papua New Guinea. Attendees will have the opportunity to engage with industry experts, share knowledge, and explore the latest innovations in pre-hospital care.
This year's event will feature an action-packed expo showcasing cutting-edge industry updates and technological advancements. Participants can expect to gain insights into the latest trends and best practices shaping the future of emergency medical services.
A highlight of the Congress will be the prestigious CAA Awards for Excellence, recognising outstanding contributions and achievements in the field. These awards celebrate the dedication and innovation of professionals who have made significant impacts in ambulance services and emergency care.
As the ambulance sector continues to evolve, the 2024 CAA Congress stands as a crucial event for networking, learning, and collaboration. It provides a unique forum for discussing challenges, sharing successes, and shaping the future of emergency medical services in the region.

Some highlights include;
• Industry updates and innovations:
The congress will feature an action-packed expo showcasing the latest developments in ambulance services and emergency medical care.
• Ambulance care advancement:
As the premier event for the Ambulance Health Sector in Australasia, the congress will focus on current trends and best practices in pre-hospital care.
• Leadership and management:
The event brings together top leaders, decision-makers, and senior management teams, suggesting discussions on leadership strategies and management practices in ambulance services.
• Emergency management: Topics related to emergency response and management across Australia, New Zealand, and Papua New Guinea are likely to be addressed.
• Technology in emergency services: Given the emphasis on innovation, sessions on technological advancements in ambulance and emergency services can be expected.
• Excellence in ambulance services:
The CAA Awards for Excellence will recognise outstanding contributions to the field, highlighting best practices and innovative approaches.
• Regional and international perspectives:
With attendees from various countries, the congress will likely cover regional and international issues in ambulance and emergency services.
• Collaboration and knowledge sharing:
The event serves as a platform for professionals to engage and learn from each other, suggesting sessions focused on collaborative approaches and knowledge exchange.

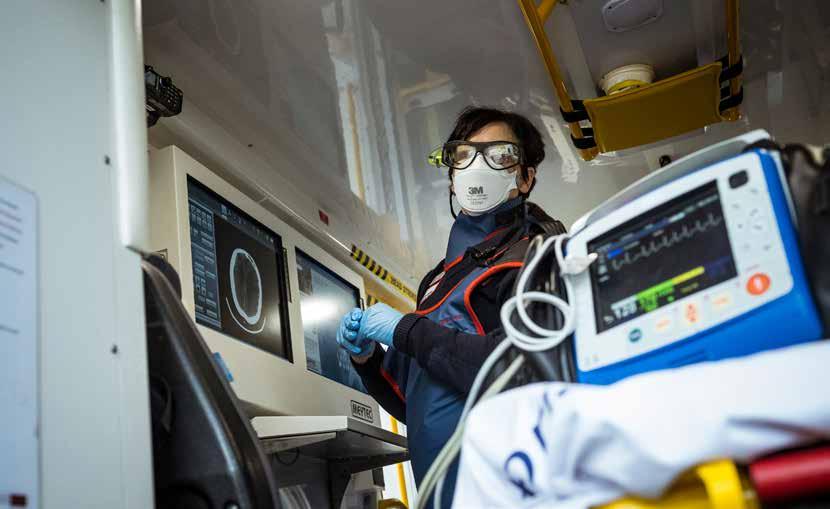
Stroke Alliance
Paramedics are at the heart of the Australian Stroke Alliance and Titan Prehospital Innovation’s early success, and the Council of Ambulance Authorities is an enthusiastic partner. The Stroke Alliance is a $40 million initiative taking urgent diagnosis and treatment to the nation’s stroke patients. Titan Prehospital Innovation is in a joint venture with the Australian Stroke Alliance to develop the Zeus tele health app, enabling connectivity between paramedics and neurologists to consult on acute stroke cases.
Determining the type of stroke – ischaemic or haemorrhage – is critical to determine the appropriate treatment required and ensure the best possible outcome for our patients. This differentiation can only happen in hospital with the use of conventional brain imaging. A core focus of the Australian Stroke Alliance’s research is the development of portable brain imaging devices for use by paramedics. These Australian-made devices are expected to be available for trials in 2025.
But while these portable, lightweight brain imaging devices are still being developed, The Australian Stroke Alliance and Titan Prehospital Innovation are undertaking several large scale trials of the Zeus app.
At the halfway mark of the five-year project, here’s a snapshot of progress so far:
Two pilot studies, involving telehealth-trained paramedics using the Zeus app in conventional ambulances, have been breaking records and returning patients to healthy life. The trials, in western Melbourne Vic and southwestern Sydney NSW, are preparing for the 2025 arrival of the alliance’s portable brain scanning devices capable of diagnosing the type of stroke.
The aim of the pilot studies? To improve the diagnosis of stroke and triage patients with a likely large vessel occlusion stroke that would require thrombectomy from a major stroke centre, requiring hospital bypass. Decision-making on-scene and connection with a neurologist is aimed to empower paramedics to collaboratively identify the best destination hospital for the patients and reduce the time to definitive treatment in a disease where time is brain.
Of 265 regional patients arriving at Liverpool Hospital, the median time to treatment was two hours faster with the new protocol, compared to the catchment’s five-year median. Also, during the study, the hospital door-toneedle time record was broken by over 15min.
In Victoria, as in NSW, patients received faster access to thrombolysis and thrombectomy thanks to informed bypass decisions made possible by highly trained paramedics, access to a tele-neurologist and prepped ED staff. According to Ambulance Victoria’s improvement lead, Grant Hocking: “The capacity to consult with a neurologist has certainly provided paramedics with extra confidence in their diagnostic capabilities to identify stroke and large vessel occlusive strokes, and confirms any decision to transport the patient to definitive care in the first instance”.
This study has completed recruitment and the results will be available later this year.
On the evening of 1 February, 2023, Garry experienced a severe stroke while driving with his partner Kim near Nowra in NSW.
Paramedics arrived quickly. Already trained to use our customised telehealth platform, they liaised with a rostered neurologist, Prof Mark Parsons, who was at home.
Telehealth provided enough info for the neurologist to direct the stroke smart ambulance to bypass the closest hospitals – Bowral, Wollongong and Campbelltown –and to travel at speed, straight for a specialist stroke centre, Liverpool Hospital, normally a two-hour drive when travelling at the speed limit, and 160km away.
The Liverpool team was primed, guided by our automated workflow. Garry was scanned and treated with clot-busting meds within 31 minutes of arrival – a record for the busy hospital which receives four stroke patients a day.
Just 90 minutes elapsed from stroke onset to treatment.
Garry has completely recovered and is pictured here on holiday with his partner Kim, just 17 days after his stroke.
This is the future of advanced prehospital stroke care.
World leading. Economical. Life-saving.

Telestroke
is delivering serious time savings. Garry’s door to treatment time was 31 minutes which is a record for Liverpool Hospital.
Neurologist, Professor Mark Parsons, South Western Sydney Local Health District

In Newcastle, specialist PICU paramedics have been given the Zeus app to connect to hospital based neurologists, as part of a study to see if they can effectively apply portable brain imaging before the units become available to the Australian Stroke Alliance. This important study is designed to identify the optimal workflow and conditions under which prehospital brain imaging can take place. Is it better in the home or on the stretcher in the back of the ambulance?
The Hunter study has enrolled 125 patients and results will be available later this year.
The Melbourne Mobile Stroke Unit (MSU) – Australia’s busiest clot dissolving service - now has a sibling; a second vehicle has been deployed. The new ambulance, an Iveco vehicle, carries a 726kg OmniTom Samsung NeuroLogica CT scanner which is about the size of a large washing machine.
It has a dual cabin so the crew (MICA and a paramedic, a stroke nurse and radiographer) can sit together when travelling, an improvement on the first model’s set-up where some of the team had to travel in the back.
Ambulance Victoria and the Royal Melbourne Hospital are working with the alliance to trial telehealth on the MSU. This workflow change will remove the neurologist from the vehicle to reduce costs and support a sustainable model of care with the help of the Zeus app. This study has involved over 250 patient and is expected to conclude soon.
The significant success of scanning on-scene in the MSU paves the way for lightweight, portable and affordable brain imaging in regular ambulances during the next decade.
According to alliance co-chair and co-founder of the MSU, Professor Stephen Davis: “After seven years of seeing the MSU’s on-scene scanning success, we know this model works so it’s heartening to anticipate the arrival of the smaller scanners in standard ambulances in 2025”.
Australia is lagging behind other advanced countries, failing to deliver time-critical thrombolysis and endovascular thrombectomy to many patients. In fact, the rate of thrombolysis is stagnant at 10 per cent of patients due to delays in access o a CT scan and subsequent diagnosis. As well, only 29 per cent receive thrombolysis within 60 minutes of arriving at hospital, compared to 60 per cent in both the US and UK.
The Stroke Alliance’s mission is to speed up informed decision-making, and to ensure receiving hospitals, with advanced stroke capacity, are ready for the patient’s arrival.
Paramedic at scene assesses patient with city-based stroke physician
Brain scan discussed
Video-call tech supports diagnosis
Patient flow
1 Pre-hospital data sent
2 Ambulance travel tracked
Research data captured Improved treatment time
3 Patient admitted
4 Work continues using pre-hospital data
South Australia was the worst performing state for urgent stroke care in 2007 but today it is, arguably, the best. A statewide telehealth service has been operating across SA since 2018 and has been enhanced by the introduction of the Zeus telehealth platform in the last 18 months, providing the most comprehensive stroke advice, to the biggest geographical area of any telestroke service in the world. The SA tele stroke service spans over all of SA, but also includes the NT.
The team has doubled the endovascular clot removal rate. One of its greatest achievements is a 70 per cent reduction in the number of unnecessary inter-hospital transfers.
Also, thanks to expert neurological assessment, coordination by SA Ambulance Service and primed hospital teams, rural patients are experiencing improved door-to-needle times in regional hospitals with a median time of 90 minutes now cut to 54 minutes.
The Zeus telehealth platform captures data and identifies areas requiring improvement, critical to workforce planning. Regular data feedback to health workers or regional health systems is essential to ensure the benefits continue to be delivered.
Due to proven success with 1350 patients treated using telehealth, the Rural Support Service is now serving Alice Springs 24/7 and Darwin, after hours. Adelaidebased neurologists provide expert advice and decisions on transfers to Royal Adelaide Hospital when necessary.
A paper is about to be published showing substantial cost savings from these modest but smart interventions. Data crunching shows that over five-years of telehealth, not only do we see improved patient outcomes, but the South Australia and Federal governments will save $9.8 million thanks to reduced patient management costs, nursing home care, and futile transfers.
According to Stroke Alliance co-chair, neurologist Professor Geoffrey Donnan: “The cooperation and coordination we have seen in SA is an exemplar for the whole country. We know how to dramatically improve treatment times. Now we need governments to adopt new protocols to build on the benefits we are seeing”.


Nanotube CT Technology
75kg (Likely weight)
High Portability Level
(Standard rotary wing aircraft and road ambulances)
Electromagnetic Technology
10-15kg (Likely weight)
Very High Portability Level
(Standard aircraft and rural road ambulances)

Two Australian companies, Micro-X and EM Vision are in a race to deliver an Australian-owned and built portable brain imaging device to be used in road and air ambulances.
Both are conducting feasibility clinical trials in hospital settings and are scheduled to begin in-field testing in 2025. The Royal Flying Doctor Service is preparing workflows for initial pilot studies to be conducted from Adelaide and Alice Springs, initially.
Do you ‘Ask the Question?’
The Stroke Alliance, with support from the CAA, is promoting a campaign to encourage all paramedics to ask their patients if they identify as having an Aboriginal or Torres Strait Islander backgrounds. This ensures Aboriginal liaison officers are available to support these patients in hospital, and it can alert care teams to the increased risk of stroke amongst this group – particularly as strokes happen at a much younger age.
The Australian Stroke Alliance is keen to help ambulance services roll-out innovations in stroke care across the nation. As pilot studies have shown, telehealth is already making a significant difference to patient outcomes and we need to accelerate its adoption across Australia to maintain the benefits seen in the pilot studies.
It also paves the way for the arrival of the imaging devices so a brain scan can be conducted at the scene of the stroke, further improving time to treatment.

EMVision's ambition is to help transform stroke and traumatic brain injury outcomes for all Australians, particularly in hard to reach locations. Learn more at www.emvision.com.au
Non-ionising radio signals
Rapid insights
Easy to operate

Medical Devices Ltd Suite 4.01, 65 Epping Rd, Macquarie Park, NSW Australia




The 2024 Paramedic Chiefs of Canada conference was held in stunning Quebec City during June. With several hundred attendees it proved to be an excellent networking event.
Our very own, Chief Executive, David Waters and CAA Chair and Board Member, Howard Wren attended the annual conference in Canada. Here we learn about some of the highlights from the two day program.
President’s Award
The PCC President’s Award was presented by current President Kevin Smith and vice-president Marc-André Périard to Past President Randy Mellow for his dedication and leadership to the PCC over many years.

100% Electric Ambulance with innovative ergonomic safe seating for paramedics
A highlight of the conference was a chance to experience the groundbreaking new ambulance model designed by Demers with cutting-edge innovations. This 100% electric ambulance enhances paramedic ergonomics, maximises safety, and elevates patient comfort to unprecedented levels.
Speakers: Leanne Douglas, Ryan Sneath, and Pierre Poirier
The speakers passionately discussed the importance of paying attention to an organisation’s health and fostering strong and agile workforces in ways that give staff and leaders a voice in times of change.


The discussion included:
• Culture in simplest terms
How do things work around here? What humans understand, what’s acceptable, not acceptable.
• Define with clarity what the culture really is today Getting as many voices as possible. Clearly define in behavioural terms what the culture is like. Constant re-evaluation and tweaks to get to where the culture should be.
• Common pitfall: leadership is key How much effort and consistency is required by leadership.
• People who become leaders do so for a reason What does it take to succeed around here? What got me here doesn’t necessarily work now.
• Not allowing excuses
Don’t focus on what we can’t do but what can be done.
• People looking to the organisation for a resolution Culture comes from individuals. Individuals are not an island unto themselves.
• Coaching style vs. performance management
Leave room for personal approach/journey to change – I want you to have a say on how you are going to get there.
• Kindness and belonging
What creates space for people to belong to the organisation.



Kelly Nash, Executive Director, Paramedic Chiefs of Canada (PCC)
PCC Research committee Chair Jan Jensen moderated a discussion on how Paramedic leaders can leverage research with panellists Jennie Helmer (BCEHS), Dr. Peter O'Meara, and Carla Roy (Medavie Health Services West).
The panel discussed how they had introduced research capability into their paramedic services including:
• Funded research position – embedded in the future vision of BCEHS – more important is the participation levels of current staff.
• Leverage provincial crisis and insert a component of research to learn from disasters.
• Level partners for research projects.
• Strong value between Culture and upbringing.
• Timing and consideration of the project.
• Participating and being in other research projects, drives research and develops colleagues
• Challenges to fund research and developing research
• Research fundamentals are sill not all there. Apply and take tools as a lesson going forward
• Be honest, and open to findings.
Keynote Speaker: Ron Tite
Ron is famous for THINK. DO. SAY. A Guide for Personal and Corporate Success in a Busy, Busy World
In today’s busy, busy world, for brands, organizations, and leaders to succeed it’s about:

Thinking is your beliefs and values. It’s not your product, it’s your purpose.
Doing is the decisions you make and actions you take to live your values.
Saying is how you communicate your values and actions: the internal or external selling, marketing, and promotion.
When an organization and all its people think, do, and say the same things, it creates complete alignment. But when an organization and its people DON’T think or do or say the same things, the result is an integrity gap. That’s not good for careers. And it’s certainly not good for business.
• Embraces the limitation and reconnect with purpose and love what you do, this changes everything.
• The only thing worse than the great resignation is the great resignation – acceptance of the worse
• Efficiency and quality of service – true growth doesn’t happen until we commit to growth
• Don’t spend too much time on low-value items; not providing a return to membership.
• Leadership: trying new stuff and operationalising things. Working out the kinks – shut up and solve my problem. That’s why I’m coming to you.
• Identify the problems. Try to solve them one by one vs. solving the biggest problem.
• What is the gap between experience and reality?
• Looked at a customer's experience/journey and solved them one by one.
• Customer Experience & Employee Experience
• The problem isn’t the only problem – tech, logistics, etc. There are a variety of problems.
• Leaders don’t have to solve all the problems –a vetted connection to help you solve the problem works. Someone to has experience on the journey to hold my hand.
• Community are people from all walks of life who share your sense of purpose.
• Who we do it with is more important than who you do it for.
• These are the people who share your experiences and help solve your problems
• True growth happens when people adopt your ideas –how it works is how it is communicated and is how to get people on your side. Repeat repeat repeat.
• Authenticity is being comfortable with your imperfections
Overall an informative and enjoyable conference and a great opportunity to catch up with old friends.

John Bruning, CEO, Australasian College of Paramedicine
Throughout Australia, undergraduate paramedic students are required to undertake up to 18 weeks of unpaid clinical placement as a mandatory degree requirement. For many, the costs involved can lead to severe financial hardship and debt, and for some they can simply be prohibitive.

Throughout Australia, undergraduate paramedic students are required to undertake up to 18 weeks of unpaid clinical placement as a mandatory degree requirement. For many, the costs involved can lead to severe financial hardship and debt, and for some they can simply be prohibitive.
Placements can be located hundreds of kilometres from their homes, requiring students to travel and seek accommodation while managing paid jobs and meeting existing rent/mortgage commitments and family responsibilities.
The College’s latest Advocacy in Conversation podcast on “Placement poverty”, explores the many challenges students are facing and the accompanying economic and psychological stress being experienced, from travel expenses, chronic housing shortages in regional areas and exorbitant short-term rents, to sleeping in cars and operating on little sleep as they work to pursue a career in paramedicine in a system that offers little respite from the pressures being borne.
The stories of hardship and deprivation on placements are rife and, as our podcast highlights, are the norm rather than the exception for those posted to outlying communities beyond metropolitan areas or in areas not readily accessible from their places of residence. The financial toll exacted can be crippling and places unrealistic burdens on students and their families.
In May, the Australian Government announced it would invest $427.4 million from 2024-25 to 2027-28 to introduce a new Commonwealth Prac Payment from 1 July 2025 to support eligible teaching, nursing and midwifery, and social work students in higher education and VET in completing their placements. Regrettably, paramedic students were not included despite receiving little support via bursaries or grants compared with other student cohorts.
While the progress of paramedics working in primary and urgent care continues and federal support will arrive to make this a reality, the main beneficiaries of a quality graduate workforce are the jurisdictional ambulance services and the state, territory and Aotearoa health systems. More can and should be done to support paramedicine students at a jurisdictional level.

The lack of support for student placements has significant longer-term ramifications for the profession and risks driving workforce inequality by financially disadvantaging those who are unable to afford placement costs and who, as a result, may have to relinquish their career ambitions. This in turn undermines the profession at a time when it is striving to better represent the culturally and socioeconomically diverse communities it serves. Placements, which accrue a HECS debt, are also often a prerequisite to progress in the degree which can impact student retention.
Paramedics are a key health workforce, whether in emergency, urgent or primary care, and the increasing shift towards multidisciplinary team-based healthcare sees paramedics working across a range of different practice settings in primary and community care. We need a commitment at federal and jurisdictional levels reflected in placement support for the future paramedic workforce. We cannot continue to see those who are committed to a career in paramedicine be unduly financially burdened in pursuit of that goal.
As such, the College is advocating for the government to broaden the scope of the Commonwealth Prac Payment to include paramedic students who are facing “placement poverty” to ensure a sustainable and genuinely representative profession.
The College will also be engaging with state, territory and Aotearoa governments to identify opportunities to support student paramedics and align with health workforce strategies.
At the College, we are committed to supporting paramedics from the start of their professional journey as students and throughout their careers. We understand the transition from university to the workforce can be difficult to negotiate, and to help assist the process we have launched our Grad Start (Pilot) Program.
Beginning this month, the 12-week initiative is tailored for new paramedics, focusing on career initiation, professional identity formation, and professional attitude development. The pilot program offers interactive learning, case-based approaches, and peer networking, all at no cost. It is one of a growing range of initiatives aimed at both students and graduates that we are undertaking.
For student paramedics, it is important that they have the support needed to complete their degrees, and we will continue our efforts to advocate for workforce equity.





NOV 2024 21

NOVOTEL SYDNEY
Olympic Park, Sydney, Australia
The CAA Women in Leadership Symposium is an empowering one-day event designed to foster and celebrate female leadershipin the ambulance and pre-hospital sector. Full 2024 program plus tickets now on sale via caa.net.au/symposium

SimX offers a robust VR solution tailored for EMS providers to prepare for the unpredictability of emergency scenarios.


Lindsay Bent, Ambulance Victoria
The number of people living with dementia is set to rise dramatically in the years ahead. Throughout the UK, NHS ambulance Trusts are working hard to address this challenge, making their Trusts dementia friendly and ensuring that people who live with dementia, as well as their carers, are treated with sensitivity and compassion.
People with dementia will be affected differently and will present differently depending on what stage of the dementia they are at, and the type of dementia they have. Some people who use ambulance services may be profoundly affected, others moderately, some with mild symptoms, and there may well also be a cohort who will not wish to disclose that they are living with dementia. There will be others who may not be aware that they are living with dementia.
When a person who is living with dementia experiences a change in their routine or is removed from their home environment (e.g.: to be taken to hospital by ambulance), these people find this experience to be very distressing, confusing, and the cause of high levels of anxiety. These people are confused already. And by taking them out of their familiar environments, we are giving them a little more confusion. This can often lead to the development of delirium which can contribute to negative patient outcomes.
Whilst it is understood that a journey to hospital or other medical service may have negative impacts on the person’s mental state, there are times when such a trip is unavoidable.
When paramedics (or other frontline workers) attend a person living with dementia, they may be confronted with a scene that they may not be prepared for or have been given the skills to manage.
The person’s presentation may be challenging, they may be resistive, they may not be able to articulate what they are feeling or what their needs are, or they may even be in possession of something that could inadvertently be used as a weapon.
• Are frontline workers given the knowledge to understand what’s actually happening to that person at that particular time?
• Have they been given the necessary skills to de-escalate the situation and gain the confidence and cooperation of the person?
• Do we provide a transport environment that alleviates the associated anxiety and stress?
• Are we delivering person centred care, specific to their dementia?
There is a real opportunity to address our capacity and capability to improve the experience people living with dementia, and their carers have when they use ambulance services.
UK Ambulance Trusts have worked to address this challenge.


• Dementia Leads – to direct and manage all initiatives associated with the Trust to become dementia friendly.
• Dementia Strategy & Action Plans – the formulation of organisational commitment to provide a clear roadmap as to how the Trust will transform its approach to provide person centred care for people living with dementia.
• Dementia Awareness Training
– The provision of Tier 1, Tier 2, and Tier 3 dementia awareness training for all ambulance staff.
• Tier 1 for all staff including corporate
• Tier 2 for frontline staff
• Tier 3 for subject matter experts and leaders in this area
• Association of Ambulance Chief Executives ‘Dementia – Best Practice Guide for Ambulance Services’. AACE published a best practice pre-hospital standard for the care of people living with dementia based on recognised national standards.
• Emergency Services Commitment on Dementia – Each emergency service comes into contact with people living with dementia on a daily basis. This emergency services commitment is a strategy to all become dementia friendly, ensuring that each respective service is better prepared to support those living with dementia.
• Changing the interior colours of the ambulance vehicles so they are more contrasting, providing better visibility for the patient.

• Modifications to Emergency and Non-Emergency Ambulance Fleet
• Changing the floor colour from blue to grey as research has shown that people may see the blue floor and think they are about to step into water.
• Addition of yellow piping around the seats in the vehicles to make them more discernible.
• The addition of imagery on window blinds that can be opened or closed, to provide key points to talk to, or reminisce about. The blinds may include images of poppy fields or children playing which reminds them of their youth. Some Ambulance Trusts have used an image of a significant landmark in their area such as the Yorkshire Moors in Yorkshire Service Trust Ambulance.


• The addition of USB ports in the vehicles to play music from a person’s chosen era or genre.
• Reconsideration of the patient care equipment location in the vehicle so that as much of it is as out of sight as possible (behind the patient or covered over).
• Reminiscence Therapy –through an electronic tablet named “RITA” (Reminiscence Interactive Therapy Activities). It is designed for the individual to unlock some older memories and reminisce about their past. RITA provides a means of supporting people therapeutically, reducing boredom, agitation or distress during long distance journey’s, or when delayed at hospital waiting for admission.


Lindsay Bent Mobile Intensive Care Ambulance (MICA) Paramedic, Ambulance Victoria
• “twiddlemuffs” – which are handmade, knitted sleeve decorated internally and externally with buttons and ribbons designed to reduce anxiety. These have been introduced onto vehicles in order to, where necessary, occupy a person’s hands and reduce the chance of them attempting to undo their stretcher restraint during transport.
• Community Partnerships –new relationships created with local dementia support groups so that ambulance Trusts can hear first hand what’s important about ambulance services to people living with dementia.
For more information, please contact linday.bent@ambulance.vic.gov.au
Lindsay Bent is a Mobile Intensive Care Ambulance (MICA) Paramedic and has worked with Ambulance Victoria for almost 35 years, where he currently holds the role of Clinical Lead, Communications Centre.
He was awarded the Ambulance Service Medal (ASM) in the 2024 national honours for distinguished service to Ambulance Victoria. He was also admitted as Officer of the Order of St John (OStJ) for sustained loyalty, commitment, and service to St John Ambulance Australia.
In 2022, Lindsay was awarded a Winston Churchill Fellowship to study Dementia Friendly Ambulance Services and associated action plans within the NHS in the UK. His full report can be found here Lindsay Bent - Churchill Trust

Here at CAA, we're committed to participating in this important movement. To help you begin your plastic-free journey, here are four steps inspired by the CAA Sustainability in Ambulance Services report.

By taking these small steps, you can make a significant impact on reducing plastic waste. Remember, even minor changes in our daily habits can contribute to cleaner streets, oceans, and communities.
Choose recycled latex gloves Use recycled medical equipment Remember to use reusable bags Keep your keep cup nearby
Proudly supported by

Membership fees are tax deductible and we support you with:
advocating for more career opportunities, workforce flexibility, recognition of capabilities, health and wellbeing
free high-quality, industry-informed CPD content
self-paced eLearning, webinars and podcasts
access to College education and research grants
research opportunities and mentoring programs
our free CPD tracker
conferences and events
a range of publications designed to provide information on all aspects of your career

St John WA: Reunited
Over 10 years ago, aspiring singer Jana Biddle suffered serious injuries in a car accident leaving her with years of surgeries and hours of rehabilitation. With a long road to recovery, Jana worked in the marketing industry while also finding her recovery treatment fascinating. From this fascination, she made the decision to study Paramedicine. Earlier this year, Jana was reunited for the first time with Barry Donelan, one of the SJWA team members involved in saving her life that night in 2013. Fast forward to today, Jana has decided to start a two-year program which will allow her to become an ambulance paramedic.

Queensland Ambulance Service: Emergency Services Assemble Teamwork makes the dream work, and that is what the students at a Queensland high school in Mossman were fortunate enough to see, as Paramedics and emergency services staged a road traffic accident involving multiple casualties. This educational exercise was to showcase the importance of road safety and the effects of being irresponsible while driving. Great work by the Queensland Emergency Services to bring further awareness to the community.

St John WA: Rockstar RN
It is said that it is normal for you to change your career path several times throughout your professional life… this isn’t the case for Colleen Henderson who celebrates her 50th anniversary in nursing. Joining the industry during the 1970s in New Zealand as an aged care nurse, it was here that she received some advice that she kept close to her chest ever since, “if you can do this, you can do anything in life, and to never lower your expectations to anyone else’s, always make them rise to yours”. Colleen has been a part of St John WA Cockburn for a decade has recently been honoured as a St John WA Outstanding Woman for International Women’s Day after receiving a remarkable 11 nominations from her team. Congratulations on a stellar career Colleen, you’re an inspiration to us all.


After a stellar career spanning close to 5 decades, Brian White has decided to call it a day after a 47 year long shift. Holding a variety of roles including the Director of Metropolitan Clinical Operations, Brian is ecstatic with his career as he is finishing without “a single regret”. Brian began his career in 1979 at the Goulburn Ambulance Station and has since developed his career and skillset to earn him nominations for many prestigious awards including the Ambulance Service Medal which was awarded to him earlier this year for outstanding service.to respond quickly to medical emergencies in the crowd.
During May, the team at National St John Ambulance Service Papua New Guinea held a training session for journalists and media teams in Port Moresby. This First Aid Course was held so the attendees can lend a hand in emergency situations if they are required. It is fantastic to see our PNG member doing their part for their communities.
Imagine walking for 71km per day for 30 days, just the thought is exhausting right? Okay now imagine running it. Chris from the Wairarapa community set out to do just that to fundraise for the new Wairarapa Ambulance Station. Unfortunately, due to ill health, he had to pull out of the challenge, but not before raising $1600. Great work Chris, we hope you’re feeling better and can get out to the Colin Pugh Sports Bowl again.
#ThankAFirstResponder



The team at Queensland Ambulance Service have been busy inspiring the next generation of their team at Camp Hill Kindy and MacKillop Catholic School recently. The teams that visited were very busy showing off the ambulances, lights and sirens and were very popular in front of the camera. These memories may last a lifetime for these children. Great work team.
#ThankAFirstResponder
Hato Hone St John: ASB Super Savers.
Not all heroes wear caps, but in this case, they are. St John Cadets, James, Ryan and Lilly found themselves at an event where a 3-yearold suffered severe burns. After immediately alerting the St John staff, they followed the instructions given by the team to get water from the on-site MIST (Major Incident Support Team) truck. The trio went one step further and guided the ambulance to where the St John team were as well as kept the little boys’ brother comfortable. Fantastic work James, Ryan and Lilly.


#ThankAFirstResponder
Long serving Association of Ambulance Chief Executives (AACE) Steve Irving has called it a day after a four-decade career in the NHS ambulance sector. Affectionately coined ‘Mr ALF’ by his peers due to his heavy involvement in the AACE Ambulance Leadership Forum (ALF), began his career on 21st May 1984 as a trainee and since then, held a variety of roles including some at national level. Steve retired 24th May 2024, almost exactly 40 years from his start date. All the best in the next chapter of your life Steve.

St John NT were all in when it came to fundraising for the Alan Walker Cancer Centre at the Hidden Valley Racetrack. Holding a nice morning tea and raffle the day before for the team as well as at the event, the team at St John NT raised money for a great cause all while having a bit of fun on the track.

cqu.edu.au

acu.edu.au

belgraviahc.com.au

chivaunetechnologies.com.au

dedalus.com/anz

gaam.com.au

healthcaresoftware.com.au

sdsi.com.au

amtek.net.au

bluelightcard.com.au

corvanta.com

device.com.au

goodsamapp.org

https://hexagon.com

stryker.com/au/en
austrokealliance.org.au
bmw.com/en-au/home.html

deccanintl.com

emvision.com.au

harcor.com.au

home.id.com.au

laerdal.com/au/

mindray.com/au

paramedics.org

stemlogic.co

medicalert.org.au

motorolasolutions.com

prioritydispatch.net/en

asutherlandmedical.com.au

mercedes-benz.com.au/vans

orhltd.com

rappaustralia.com.au

teleflex.com/anz

titanneuro.com

wla.edu.au
tollgroup.com
workweargroupuniforms.com.au
totalmobilesolutions.com.au

zoll.com
Interested in becoming a part of The Directory? Contact admin@caa.net.au
CAA helps provide an important link between the ambulance sector and businesses that provide goods and services for this industry. It’s instrumental in providing networking and partnering opportunities. Don’t hesitate to reach out to organisations of interest.

Provide your EMS team with faster, more accurate information using ProQA® emergency calltaking software. ProQA gives your calltakers a standardised, proven set of medical protocols to assess the situation and deliver key information to your EMS team. Your team needs accurate and pertinent information fast —ProQA delivers.
Learn how the most trusted solution worldwide for safety of your EMS team at prioritydispatch.net.




Mitch Mullooly Health and Wellness Strategist
Specialising in the wellbeing of first responders, Mitch is a Professional Advisor for Te Kaunihera Manapou, Paramedic Council of New Zealand; Senior Advisor for Fire and Emergency New Zealand; Advisory Board member for Te Kiwi Maia, The Courageous Kiwi; and proud CAA Women in Ambulance honour recipient.
Mitch is also a published author, speaker and feature columnist for several sector related magazines, communiques, webinars, and podcasts, and the creator of Eat|Train|Be - Fit for Duty.

As
a paramedic, we're the frontline hero in times of crisis, the beacon of hope in life's darkest moments
Our ability to remain calm and effective under extreme pressure is nothing short of remarkable. However, the very nature of our work - the high-stakes decisionmaking, the traumatic scenes, the long and sometimes unpredictable hours - can steadily chip away at even the most resilient of us.
Resilience though, we preach it, we teach it, we strive for it… but what happens when our mental armour cracks despite our best efforts? When the well of grit runs dry and the superhero cape feels too heavy? It's time to talk about the elephant in the ambulance - when resilience itself needs resuscitation.
Before we delve into strategies, it's vital to understand the signs that your resilience might be wearing thin. These symptoms can be subtle at first, gradually intensifying if left unaddressed:
Emotional Exhaustion: Feeling drained, detached, or emotionally numb, even on your days off. You might find yourself unable to engage emotionally with loved ones or feel apathetic towards activities you once enjoyed.
Increased Irritability: A short temper with colleagues, patients, or loved ones. Small inconveniences that you once brushed off now feel like major annoyances.
Difficulty Concentrating: Struggling to focus during calls or when completing paperwork. You might find your mind wandering during critical moments or have trouble retaining information.
Sleep Disturbances: Insomnia, nightmares, or excessive sleeping. You might have trouble falling asleep, wake up frequently, or experience vivid dreams related to work.
Physical Symptoms: Headaches, muscle tension, or gastrointestinal issues that don't have a clear medical cause.
Loss of Motivation: Dreading shifts or feeling disconnected from your purpose as a paramedic. The passion that once drove you might feel dimmed or extinguished.
Heightened Anxiety: Excessive worry about calls or potential scenarios, even when off-duty. You might find yourself constantly "on edge," unable to relax.
Compassion Fatigue: Feeling unable to empathise with patients or their families. You might notice a sense of detachment or indifference creeping into your interactions.
Intrusive Thoughts: Replaying traumatic scenes in your mind or excessively worrying about past calls and decisions made.
Isolation: Withdrawing from social interactions or team activities. You might find yourself avoiding gatherings or preferring to be alone more often than usual.
Recognising these signs is the first step. The next is taking active measures to rebuild and strengthen your resilience. Here are some strategies to help you do just that:

It's crucial to remember that feeling overwhelmed doesn't make you weak; it makes you human. The stoic culture often prevalent in emergency services can make it difficult to admit when you're struggling. However, acknowledging your vulnerability is the first step towards addressing it.
Strategy in Action:
- Start a journal to track your emotions and experiences. This private outlet can help you process feelings and identify patterns.
- Share your experiences with a trusted colleague or mentor. Often, you'll find they've had similar struggles, which can be incredibly validating.
- Practice positive selftalk. When you catch yourself being self-critical, consciously replace those thoughts with more compassionate ones.
Mindfulness isn't about clearing your mind of all thoughts; it's about becoming aware of your thoughts and feelings without judgment. This practice can help you stay grounded in the present moment, reducing anxiety about the future or rumination about the past.
Strategy in Action:
- Start with short, 2–3-minute mindfulness sessions between calls or during breaks. Use apps like Headspace or Calm for guided exercises.
- Practice "box breathing" during stressful moments: Inhale for 4 counts, hold for 4, exhale for 4, hold for 4, and repeat.
- Incorporate mindful movement, like gentle stretching or yoga, into your routine. This can help release physical tension and centre your mind.
- Limit work discussions during off-hours. While debriefing is important, constant work talk can prevent true mental rest. 1 2 3
In a profession where you're constantly giving of yourself, it's crucial to establish and maintain healthy boundaries. This includes both professional and personal boundaries.
Strategy in Action:
- Learn to say no to extra shifts when you're running on empty. It's not selfish; it's necessary for sustainable service.
- Establish a "wind-down" routine after shifts to separate work life from personal life. This could include changing clothes, taking a shower, or engaging in a calming activity.
4 5
Your colleagues are uniquely positioned to understand the challenges you face. Peer support can provide validation, practical advice, and a sense of community.
Strategy in Action:
- Participate in or initiate regular "check-in" sessions with your team where everyone can share their experiences and challenges.
- Consider joining or starting a support group specifically for paramedics or first responders in your area.
- If your organisation has a structured peer support program, don't hesitate to use it. If one doesn't exist, consider advocating for its creation.

6
Structured debriefing after challenging calls helps process emotions and prevents them from festering. It also provides an opportunity for learning and improvement.
Strategy in Action:
- Advocate for regular, structured debriefing sessions after significant incidents.
- Use a framework that your organisation uses as a model to guide these sessions.
- Practice personal debriefing by journaling or talking through challenging calls with a trusted colleague or supervisor.
We know that mental resilience is intrinsically linked to physical wellbeing. Regular exercise, balanced nutrition, and adequate sleep form the foundation of resilience, but these are often the first to go.
Strategy in Action:
- Schedule your workouts like you would any other important appointment. Even short, high-intensity workouts are beneficial.
- Meal prep healthy options for your shifts to avoid relying on fast food or vending machines.
- Create a sleep-conducive environment at home. Use blackout curtains, white noise machines, or sleep masks to improve sleep quality, especially if you work night shifts.
The greatest glory in living lies not in never falling, but in rising every time we fall."
Nelson Mandela

7 8 9
Everyone has different activities that help them decompress. Identifying yours and making time for them regularly is crucial for maintaining resilience.
Strategy in Action:
- Experiment with different activities to find what works best for you. This could be reading, writing, gardening, playing music, fishing, or any other hobby that helps you relax.
- Schedule dedicated time for these activities, treating them as important as any work commitment.
- Consider learning a new skill or hobby. The process of learning and improving can be a powerful distraction from work-related stress.
There's no shame in seeking professional mental health support. In fact, it's aproactive step towards maintaining your wellbeing and effectiveness as a paramedic.
Strategy in Action:
- Familiarise yourself with the mental health resources available through your employer or professional association.
- Consider regular checkins with a counsellor or psychotherapist, even when you're not in crisis. This can help you develop coping strategies and process experiences over time.
- Look for a mental health professional who has experience working with first responders, as they'll have a better understanding of your unique challenges.
Treat yourself with the same kindness and understanding you offer your patients. Self-compassion is not selfindulgence; it's a crucial component of resilience.
Strategy in Action:
- When you make a mistake or face a challenging situation, ask yourself, "How would I respond if a colleague were in this situation?" Then, offer yourself that same compassion.
- Practice positive self-talk. Replace self-critical thoughts with more supportive ones.
- Engage in self-care activities without guilt. Remember, taking care of yourself enables you to take better care of others.
Regularly reminding yourself of the reasons you became a paramedic can reignite your sense of purpose and motivation.
Strategy in Action:
- Keep a "gratitude journal" where you record positive outcomes or moments of connection from your shifts.
- Create a visual reminder of your purpose - perhaps a photo collage or a quote that inspires you and place it where you'll see it regularly.
- Share stories of impactful calls or patient outcomes with your colleagues. Celebrating successes together can boost morale and reaffirm your collective purpose.

Remember, resilience isn't about never faltering; it's about having the tools to bounce back when you do. By recognising the signs of depleted resilience early and actively working to replenish your mental and emotional reserves, you ensure that you can continue to provide the highest level of care to those who need you most.
Your wellbeing is not just important for you - it's crucial for the countless lives you touch in your role as a paramedic. By taking care of yourself, you're ultimately taking better care of your patients and community. In the high-stakes world of emergency medical services, your resilience is your most valuable tool. Nurture it, strengthen it, and don't hesitate to seek support when you need it. After all, even heroes need a helping hand sometimes.

Olympic Park, Sydney, Australia
The CAA Women in Leadership Symposium is an empowering one-day event designed to foster and celebrate female leadership in the ambulance and pre-hospital sector.
This dynamic symposium aims to unlock the hidden potential of women currently in leadership roles or aspiring to take the next step in their careers.
Attendees can expect a rich program featuring:
- Practical skills development and tools for career advancement
- Inspiring talks from industry leaders and successful women in ambulance services
- Networking opportunities with like-minded professionals
- Announcement of the annual Women in Leadership Scholarship winner.
Full 2024 program plus tickets now on sale via caa.net.au/symposium Visit caa.net.au/symposium and subscribe to receive updates about the 2024 Women in Leadership Symposium and other news, offers and information from CAA.


Device Technologies proudly represents over 20 trusted brands in the pre-hospital sector with product solutions for defibrillation and monitoring, mechanical CPR, ventilation, airway management, vascular access and more.


• Customer focused education and technical services
• A comprehensive range of innovative products
• Digital services and telemedicine solutions
For more information contact your Device Technologies representative.

Follow us on Facebook CouncilofAmbulanceAuthorities
Find us on Twitter @CAAAustralasia
Connect with us on LinkedIn council-of-ambulance-authorities-australasia

For information on other CAA activities please visit