
www.caa.net.au SAAS Accreditation MENTAL HEALTH & WELLBEING around the pre-hospital sector CAA AWARDS FOR EXCELLENCE Star Award Winner announcedThe first Australian service to achieve accreditation in the NSQHS Standards Program ISSUE 10 | SPRING 2022

SOMEONE’S WORST DAY DESERVES YOUR BEST RESPONSE. THANK YOU FOR GIVING YOUR BEST.
Wow, that was a fantastic week.
After 3 years of planning, we finally did it. We delivered an incredible week of education, networking, sharing, inspiring, a true peak industry event that still has us reflecting and buzzing.
5 days, 12 events, 400+ delegates from across CAA member services, health, police, fire sectors and our international guests from New Zealand, Papua New Guinea, Singapore, the UK, and Canada.
From the study tour of NSW Ambulance, CAA Board Meeting and AGM, NSW Ambulance Summit, Women in Leadership Forum, Global Resuscitation Alliance Forum, 2-days of CAA Congress and Expo, CAA Awards for Excellence Gala Dinner and many other networking events inbetween, the week was a wonderful gathering of ambulance sector. For all the low down read about the 2022 CAA Congress on pages 12-13.
Where to from this incredible high? Well, for the rest of the year we putting on a few more exciting events and campaigns.
Starting off with Restart a Heart Day on October 16 when we get to educate the public in hands-on, live events. CAA together with our partners will be running events in Canberra, Adelaide, Sydney, Wellington, and Auckland. And there will be many more events around Australasia ready to share the message CALL.PUSH.SHOCK.
If you haven’t already, check out all the plans and activations for 2022 Restart a Heart by jumping on restartaheart.net for all details and learn how your friends and family can get involved and support this life saving campaign.
Then we get to gather in Canberra on November 17 to celebrate the 60 years of Council of Ambulance Authorities. Back in 1962 ambulance service leaders first got together to talk all things ambulance, share knowledge, discuss arising challenges and opportunities and work collaboratively for a stronger and better ambulance sector. We are proud that CAA played an important role over last six decades growing, inspiring, and connecting the Australasian ambulance community. Join us in Canberra in November to help us celebrate.
For more information visit our website at caa.net.au/caa-60th-gala
As always, we bring you a jam-packed FIRST issue full of news from our sector. We are excited to feature the SA Ambulance Service NSQHS Accreditation, not only did they get their initial accreditation in 2018, they just got re-accredited last year, paving the pavement for the rest of the sector to follow.

Sit back, relax and enjoy reading all about Australasian ambulance happenings.


Mojca x
Contents
03
30 40 42
36
Letter from the Editor
06
Data First
Patient Experience Survey
08
Industry First
Latest news from around the ambulance sector


10
CAA First
Check in with what CAA has been up to
22
Focus First
Learn about mental health and wellbeing within the pre-hospital sector
Opinion First
Can Artificial Intelligence Increase Emotional Safety in Emergency Call Centers?
38
Services First
Showcasing the latest projects and achievements from across CAA member services
42 Awards First
Join us in congratulating the 2022 CAA Women in Leadership Scholarship winner and finalists, 2022 CAA Awards for Excellence Star Award winner, and 2022 Queens Birthday Honour List

48
Feature First
FIRST Interviews SA Ambulance Service’s Keith Driscoll on the National Safety & Quality Health Service (NSQHS) Standards Program
ISSUE 10 | SPRING 2022
4 www.caa.net.au
Need Hi Res Image
56
Events First
Read about the upcoming Restart a Heart campaign events, and CAA’s 60th Anniversary Gala
62
Partners First
Hear from our partners the Australian Institute of Police Management and the Australian Institute for Disaster Resilience

70
Research First
The FIrst Responder Shock Trial (FIRST) and Paediatric cardiac arrest: What you should know
80
Sustainability
St John New Zealand's Environmental Journey
82
People First
Meet the wonderful people that make up the Australasian Ambulance services

84 The Directory 86
Wellness First
Learn from Mitch on the Five Stages of Learning, and how to apply these to any skill
THE TEAM
Editor: Mojca Bizjak-Mikic
Relationship and Content Manager: Stephanie Hartley
Editorial Team: Chantelle Kaesler & Savanah Stouraitis
Graphic Design: Alpha State
PUBLISHED BY: The Council Of Ambulance Authorities 2/141 Sir Donald Bradman Drive Hilton SA 5033 Australia admin@caa.net.au
Magazine published from paper that is sustainably sourced.
For article submissions or to advertise in FIRST by CAA magazine please contact admin@caa.net.au
48 56 70
5
Patient Experience Survey
Since 2002 the CAA has been running the Patient Experience Survey designed to monitor patient experience across all our members with the aim of identifying the quality of ambulance services as reported by the patient. And in 2022, we again see that our members are doing a wonderful job looking after their patients with overall satisfaction sitting at 96% in Australia, 97% in New Zealand and 97% in Papua New Guinea.

6 www.caa.net.au
Australia ‘000’ calls 3,654,371 patients 3,987,615 incidents 4,077,396 operational staff 19,084 volunteers & first responders 14,144 overall satisfaction 96% rated the level of confidence & trust as high 92% found the call taker helpful & reassuring 92% answered in under 10 seconds 91% OF CALLS rated the paramedic/ ambulance care as good 97% found the quality of ride to be comfortable 94% found the staff explanation to be clear 94% Data First
staff
found the
taker
found the
of ride
found the staff explanation to be
the level of confidence & trust as
found the
ride to be

7 patients operational staff 577,909 1,988 incidents volunteers & first responders answered in under 10 seconds 619,013 4,526 90% OF CALLS ‘111’ calls 687,689 overall satisfaction 97% found the call taker helpful & reassuring 92% rated the level of confidence & trust as high 97% New Zealand Papua New Guinea For more detailed information please read the full report www.caa.net.au/patient-experience-survey * CAA Patient Experience Survey 2022 / CAA 2020-21 Consolidated Returns / PNG 2020-21
call
helpful & reassuring 90% rated
high 93% overall satisfaction 97%
quality
to be comfortable 94% found the
explanation to be clear 97% rated the paramedic/ ambulance care as good 90%
quality of
comfortable 91%
clear 93%
Industry
Paramedic Pilot Program Tests Cutting Edge Out-of-Hospital Care
A small group of experienced, high performing Intensive Care Paramedics were selected to undertake a Pilot Program to assess how SA Ambulance Service can further improve the care they deliver to critically unwell patients. A large component of the training was simulation based, with a collaboration achieved with Adelaide Health Simulation – offering clinicians exposure to the most technically advanced simulation facility in Australasia.
Farewell to Queensland Ambulance Service (QAS) Assistant Commissioner John Hammond



John Hammond worked in various areas of the organisation and finished his 23 years overseeing the QAS Strategic Operations team, saying goodbye at the same Kedron complex where his career started. QAS Commissioner Craig Emery awarded John a certificate of appreciation and a QAS plaque for John’s time, mateship, work ethic and support for his peers.
NSW Paramedic Student Paramedics to Help Fix Crisis

NSW Ambulance is now offering to pay students $65,000 a year to join the ambulance service while they study at university in a bid to bolster a workforce under pressure from the coronavirus outbreak. It is part of a $1.7 billion investment by the NSW Government in a bid to bring in an extra 1858 recruits at a time when they are needed most. Image credit: Sam Ruttyn from The Daily Telegraph
ACT ESA partners with Volvo Group Australia to Create a Sustainable Future
ACT ESA is partnering with Volvo Group Australia to co-design and develop up to seven vehicles. These vehicles will include current leading edge zero emission technology to meet operational requirements of an emergency service and the ACT Government’s goal of net zero emissions by 2045. There are currently no low or zero emissions emergency service vehicles available on the market.
News Industry First
8 www.caa.net.au
St John New Zealand receive 2022 Minster of Health Volunteer Awards


St John NZ’s Kaikohe Health Shuttle team have won 'Health Volunteer of the Year' for going above and beyond to help people in Kaikohe and Northland’s more remote communities get to their medical appointments. Darren Joyce and David Jones were also recognised at the awards for their work in supporting and training volunteers.
St John NZ – Inductions into the order of St John

A big congratulations to 23 people from St John NZ who were admitted to, or promoted within, the Order of St John - one of the oldest service organisations in the world which dates back to the crusades. This very special ceremony was presided over by the Governor-General of New Zealand Her Excellency The Rt Hon Dame Cindy Kiro GNZM, QSO, DStJ who is the New Zealand Prior.
SAAS Volunteer Exchange
SA Ambulance Service volunteers participated in an Inaugural Virtual Volunteer Exchange with Ambulance Victoria, Ambulance Tasmania, and St John New Zealand, held via Microsoft Teams over four evenings in November last year. The innovative exchange program, which was deemed so successful it will now run each year, also won the ‘Excellence in Strengthening Partnerships’ award at the 2022 SAAS Excellence Awards, which recognises successful and innovative collaborations with other agencies.
Launch of St John Ambulance Australia (NT) Reflect Reconciliation Action Plan (RAP)
St John NT is proud to join a network of more than 1,100 corporate, government and not-for-profit organisations that have made a formal commitment to reconciliation and acknowledgment of Aboriginal and Torres Strait Islander peoples through the Reconciliation Action Plans (RAP) program. The St John NT Reflect RAP which was recently endorsed by Reconciliation Australia, lays the foundations for workplace RAP initiatives. As part of the project, St John NT engaged Territory artist, Sarrita King, to help tell their story and illustrate how they contribute to the health and healing of their community through their work.
9

Our year so far has been filled with some of the biggest events and campaigns hosted by CAA to-date.
CAA First www.caa.net.au10
We can’t express enough how delighted we are that face-to-face events are back. It’s certainly something we won’t be taking for granted anytime soon. It felt great for our team to be planning meetings and events where we knew that our CAA members would be able to meet and network in person. With CAA Congress recently wrapped-up and the Triple Zero Campaign launched into full swing in June, the past few months have been absolutely jam-packed and we couldn’t be more thrilled about it.

www.caa.net.au
11
C ONGR
In August, CAA colleagues, friends and partners met up for a huge three days of CAA Congress that none of us will be forgetting any time soon.
Two highly anticipated forums kicked-off day 1. The Women in Leadership forum featured some dedicated and inspiring key-note speakers, while the GRA forum high-performance CPR masterclass



E S S W R AP-UP
was a true hit. That night the first social event took place, the Meet and Mingle Motorola Welcome Function, where delegates had a chance to network while looking over Darling Harbour. It was warming to see the sector being able to catch-up face to face for the first time in a long time.
The Delegate Networking Breakfast kicked-off day one of the concurrent sessions as well as the opening of the CAA Expo Hall. Our Expo space featured over 2000sqm of booths filled with best of the best in technology, innovation, vendors and manufacturers.
CAA First
12 www.caa.net.au


13
We watched ideas transform into realities as mini-masterclasses and demos lit up the expo floor. Of course, the Corvanta ideas board was a highlight with delegates gathering around to see a live artist bring their ideas to life.

Keynote speakers Jordan Ngyuen and Norman Swan were described by delegates to be a highlight of Congress.




14 www.caa.net.au
Last, but certainly not least, the Awards for Excellence Gala Dinner and ICU Later event wrapped up Congress. Attendees of the Gala enjoyed a delectable sit-down dinner at Cockle Bay Wharf, Dockside, overlooking Darling Harbour.
The night was filled with glamour and celebration and was the premiere event of CAA Congress 2022.
Ground-breaking projects were discussed, and some particularly memorable videos of flying ambulances featured by SDSI CEO David Leggett, piqued attendees’ curiosity as to what the pre-hospital sector may look like in years to come.
Ambulance Victoria was announced as the Star Award Winner for their project ‘Real-time COVID-19 Data Linkage to inform the Pandemic Response.’
Marinda Thomas was announced at the Gala as the winner of the inaugural CAA Women in Leadership Scholarship.

15
47 speakers, 12 masterclasses, 17 demonstrations, and two panels later and CAA Congress was over.



Thanks to everyone that joined us, supported us and partnered with us and who came along and learnt something new.

16 www.caa.net.au
WE SEE YOU SUCCEED
Further your clinical skills with the Graduate Diploma of Paramedic Science (Critical Care), or deepen your knowledge in critical care paramedic practice preparing you for clinical leadership opportunities with the Master of Paramedic Science (Critical Care Practice).
Or, study the Master of Paramedic Science (Primary Healthcare Practice) which has been designed in response to industry and qualify yourself to provide essential services in the non-emergency, out-of-hospital, low acuity or primary healthcare settings.
APPLY NOW TO START IN MARCH
ONLINE, FLEXIBLE STUDY
40+ years distance education experience, plus access to facilities and support at more than 20 national locations.


TOP 10 NATIONALLY*
We’re among the best for postgraduate skills development, starting salary and full-time employment.
CRICOS: 00219C | RTO: 40939
* The Good Universities Guide 2022 EXPAND YOUR SKILLS WITH POSTGRAD PARAMEDIC SCIENCE C_AD_2202_210x297_Para
For the past five years, the campaign has been growing bigger and bigger in Australia and New Zealand. We are very excited to share with you the newly launched updated Restart a Heart branding, along with a new line of merchandise. After two years of virtual events, live activations are back in the plan for this year.
The events will be held in various locations throughout October including flagship events in Adelaide, Sydney, Wellington, Christchurch, and Canberra, where the public will be educated on Restart a Heart and CPR education. The special event in Canberra will feature at the Government House Open Day on October 8.
A partnership with Build-a-Bear began in 2021 and has continued this year. Through this, there will be education sessions held at eight of the Build-a-Bear Workshop locations throughout Australia on Thursday 13 October. It will be a fun way to share CPR knowledge with children and parents nationwide. Be sure to follow all the developments of Restart a Heart on our social channels to stay up to date with the best ways to spread awareness and information on out-of-hospital cardiac arrest.
CAA has been lining up some seriously exciting events for Restart a Heart this year.
CAA First 18 www.caa.net.au
19
Triple Zero (000) Campaign
Over the last 2 years, ambulance services in Australia experienced an unprecedented level of demand with a 10% average increase in 000 calls.
In the 2020/21 financial year more than 500,000 incidents attended by paramedics in Australia did not end up with a patient being taken to hospital. Australian Ambulance services attempted to make changes to deal with these rising demands: from hiring more staff, to restructuring response, to refining operations and processes. Moving into the busy time of winter and the worst Australian flu season projected in a decade, it was more important than ever that the critical Triple Zero (000) lifeline was saved for emergencies.

On Tuesday, 14th June 2022, CAA facilitated the roll-out of one of the Australian ambulance sector’s biggest national campaigns to date. CAA worked with member services to release a video ad urging Australians to save Triple Zero (000) for saving lives, for emergencies, for when it matters.
CAA and member services shared the video on a pre-determined date to ensure maximum impact and reach. Social media posts by services from across Australia helped to demonstrate the breadth of the issue and displayed a joint determination to make a change.
The campaign launched with a Press Conference held at NSW Ambulance with paramedic representation from other states, CAA CE, David Waters and Commissioner of NSW Ambulance Dr Dominic Morgan.
The campaign was featured on several programs and channels including Channel 7, Channel 9, Network 10 and ABC. Several of the programs the campaign was featured on are estimated to have an average of 1.4 million viewers nationally per program, per day, significantly expanding the reach of the campaign.
The campaign was a great success. The video gained traction, to raise public awareness on saving triple zero for emergencies. With the reach and media coverage achieved, we feel confident in saying that there is certainly a portion of the public that will now solely utilise and save Triple Zero (000) for saving lives, for emergencies, for when it matters.
20 www.caa.net.au CAA First
CAA
60th Anniversary Gala
We cordially invite you to the CAA 60th Anniversary Gala to celebrate every challenge, every milestone, and every ground-breaking innovation achieved by the sector in the last 60 years. On November 17th, we welcome you to a night of extravagance, bubbles, dinner, and plenty of entertainment for CAA’s 60th Anniversary to be held at the National Arboretum in Canberra.
Put on your best black-tie outfit and get ready for an enchanting night filled with wonder, excitement, and of course celebration. We invite you to join us in Canberra this November for a luxurious night at a world-class venue filled with entertainment, auctions, surprise announcements and some very special guests.
To purchase tickets for the Gala, visit eventbrite.com/e/ caa-60th-anniversary-galatickets-394859705007
You can read more about the CAA 60th Anniversary Gala on pages 57.
21
CAA’s contribution to Mental Health and Wellbeing in the Pre-Hospital Sector

Ambulance officers are often perceived as ‘strong people.’ When a medical emergency arises, ambulance officers, first responders, and volunteers are often the first people to be called and appear on scene.
It’s undeniably true that our sector’s officers remain strong and outstanding in times of emergency. However, while we see these incredible people working calmly through traumatic events, the reality of it is that they under extreme amounts of pressure. Just like anyone else, regardless of their level of training and professionalism, being in a demanding and triggering role can take a huge toll.
Focus First 22 www.caa.net.au

23
Whilst the public often see pre-hospital sector officers as relentlessly strong and determined individuals, the truth is the people in our sector come from all walksof-life and face everyday pressure, on top of traumatic events experienced on the job. Sometimes, it can be hard for the public and even our family and friends to look beyond the uniform.
Mental Health and Wellbeing Strategy
The CAA Mental Health and Wellbeing Strategy aims to
While ambulance services across Australia and New Zealand have a long history of peer and employee support programs, we are always looking to further grow and better

Sometimes, it can be hard for the public and even our family and friends to look beyond the uniform.
Playing a significant role in the pre-hospital sector, we understand how critical mental health and wellbeing is and how important it is for pre-hospital officers to take the time out to care for their own mental health. CAA will always go above and beyond to promote a stigma free environment amongst our member services, where officers don’t feel guilty about putting themselves first. We promote this through various campaigns and promotions and take great pride in sharing our projects and strategies with you today, especially in the lead-up to Global Mental Health Day (October 10).
pro-actively provide and strengthen effective leadership across CAA member ambulance services to significantly reduce the likelihood of psychological harm to staff due to workplace forces. CAA works to break the stigma around mental health and to provide guidance and opportunities to our members to support them in looking after their teams.
these important resources. The strategy outlines the direction we’re heading, how we’re going to get there, and why it’s so important.
To view our Mental Health and Wellbeing strategy, visit www.caa.net.au/world-mentalhealth-day-subpage
“There is support out there in the team, there is support out there in the workplace and there is support out there in the community. I think it’s really important that everyone takes time to access that.”
- Dave Robinson, CEO Wellington Free Ambulance
Focus First 24 www.caa.net.au
Me First
In connection with our strategy, we are pleased to run the Me First campaign once again this year. Me First was initially created to celebrate Global Mental Health Day (October 10), however the campaign now brings a months long focus on mental health. The campaign aims to recognise the importance of the industries’ workers prioritising their own mental health and wellbeing over their roles in the sector.
The campaign has been carefully designed in collaboration with Everymind through our online platforms to accessibly and easily offer our resources, recognising that social isolation, chronic illness, and exhaustion are common amongst ambulance workers and people suffering from mental health conditions. This year, we have worked to create content that is relatable, accurate, and helpful to pre-hospital sector workers, whatever their role may be. Keep an eye out on CAA socials for messages from member service CEOs and senior management, as well as helpful resources for sector workers and paramedics, that both encourage and support our workers to put themselves first in order to be the best they can be.
Webinar
This year, CAA collaborated with Everymind to put on a Webinar that was relatable, accurate, and helpful to ambulance workers. An expert team consisting of Dr Jaelea Skehan,
Wellness Column
If you’ve been following FIRST magazine since the beginning, then you would have noticed the Wellness column, tucked towards the back that appears in every
Dr Zac Seidler, Lucy Brogden, and Dr Sally Fitzpatrick discussed aspects of mental ill-health, suicidal distress, and trauma, with a specific focus on issues for paramedics and their family and friends. The team discussed the importance of not forgetting to put yourself first, prioritising self-care, and bought mental illness and suicide into the sphere of everyday reality. The presenters provided tools that paramedics could use to begin finding out what personally works for them in managing their mental health. As always, the Webinar was online and free to attend to ensure it could reach the people that might need it most. Almost all attendees provided feedback stating that they found the Webinar to be helpful.
“As people who work in emergency services, as people who work in an Ambulance service, we are exposed more than the average person to things that trigger poor mental health. I think it’s really important that people find what works for them in managing their own mental health.”- Judith Barker, St John Ambulance Australia (NT) CEO
issue. Our resident FIRST wellness columnist Mitch Mullooly, who specialises in the wellbeing of first responders, takes a holistic approach and provides wellness advice in the areas of physical activity, to nutrition, and everything in between. Mitch has been working with CAA to provide easy tips and activities to help pre-hospital sector workers keep their mental health and wellbeing on track. Head on over to page 87 to see what health and wellness tips Mitch has in store for the industry today.
“My team and I have a responsibility to create a workplace that is safe and has the equipment and culture to support our staff.”- Dominic Morgan, CEO NSW Ambulance

“From my perspective, mental health is about looking after ourselves to be the best we can be. This means that we have to care for ourselves before we can care for others.” – Tony Walker
25
Ambulance Victoria’s
‘No Wrong Door’ approach to Wellbeing Support
 By Dr Megan Dobbie – Principal Psychologist, Ambulance Victoria
By Dr Megan Dobbie – Principal Psychologist, Ambulance Victoria

26 www.caa.net.au Focus First
As the previous Action Plan (2019-2022) closed, a significant co-design and consultation process was undertaken to continue to build on Ambulance Victoria's (AV) commitment to the wellbeing of its people and their families.
The new plan, focuses on four key pillars – prevention and education, early intervention, building on our strengths and partnering for success – and has been designed to respond to the needs of our organisation in an integrated way. It retains the person-centred model of care that has been a key feature of our wellbeing programs and supports a suite of available services.
Our high-profile Peer Support Dog Program is often thought of synonymously with AV. Other support services available include our Peer Program (incorporating the Retired and Former Employee program), Pastoral Care Program, AV Psychology Team and Victorian Ambulance Clinicians Unit support network (comprising more than 120 clinicians and incorporating a 24/7 counselling line) . This is overseen by the wellbeing management team, ensuring people get access to the right person at the right time for the right support. We pride ourselves on a “no wrong door” approach to wellbeing support.
These independent parts of our service model work together to deliver a significant body of work to improve wellbeing at AV, but also ensure we can respond to the immediate needs of the workforce as required.
Our key focus points over the next year will be to:
• Build our Suicide Intervention Response and Engagement Network (SIREN) – evidence
• Begin a Peer and Pastoral Care Research Program to support a longitudinal study to determine the efficacy of the role of social support on wellbeing.
informed suicide prevention program based on education and skills training of frontline personnel, leadership teams, family and external stakeholders, tailored to the emergency service sector, with the aim of reducing stigma, increasing literacy and competency in supporting individuals at risk and ultimately reducing the prevalence of suicide in the emergency services sector.
• Review and evaluate our Graduate Ambulance Paramedic Program (GAPP) Mental Health and Wellbeing education program, incorporating Mindarma to support increased skill building and resilience in our early career operational staff.
• Develop, pilot, and evaluate a framework co-designed with our leaders and key stakeholders for Integrated Wellbeing Plans with the aim of building leadership knowledge and capacity to support wellbeing of their teams (including corporate teams) and integrate wellbeing into everyday practice.
Of course, these programs are not done in isolation or the sole focus for our teams. AV’s Wellbeing and Support Services continue to provide a suite of services across the continuum of mental health support. We deliver check-ins and buddy programs, prevention and early intervention screening programs such as the AV Stress Management And Resilience Tool 2.0® (AV SMART 2.0), the Skills for Life Adjustment and Resilience program (SOLAR), and training to embed our AV MANERS® Model of psychological first aid across all parts of the workforce. In addition, we continue to focus on the expansion of our Peer Support Dog Program and our Pastoral Care Program, which has grown extensively with a volunteer network of Chaplains across the state over the last 12 months.
Specialist clinical interventions such as Eye Movement Desensitisation and Reprocessing (EMDR) delivered by our Psychology Team at AV and other evidence-based clinical interventions through our VACU network of skilled mental health contracted clinicians also are available at AV Wellbeing and Support Services.
Comprehensive review, evaluation,
The blueprint for Ambulance Victoria’s (AV) mental health and wellbeing programs lies within the AV Mental Health and Wellbeing Action Plan (Action Plan) 2022-2025, which is in its third iteration.
27
collaboration, and consultation through surveys (e.g. Psychosocial Survey 2021; AV SMART 2.0 data) told us that our workforce has experienced increased rates of depression, anxiety, and stress. Post-Traumatic Stress Disorder (PTSD) and suicidal thinking continue to be a significant concern, as does intimate partner violence. When we look at these concerns, we see them as an opportunity for wellbeing services at AV to address these issues and provide mitigation strategies.
We also recognise that these complex mental health and psychosocial issues are reflected more broadly within the community of Victoria, in part because of a mental health pandemic related to the COVID-19 pandemic and extended periods of isolation through lockdowns for us, our families, our friends and supports. We also know that there is significant stress across the health sector for service provision and access to mental health services, just as there is for general health services and care. If we educate and respond to these complex needs in the workplace, we are hopeful and confident we can provide better care to the community we serve.
We will continue to work hard to make our organisation a more fair, safe and inclusive place to work and volunteer. Wellbeing and Support Services do not work in isolation from the rest of the business. We see it as our responsibility to partner across AV to address the drivers of key sources of distress, which we have identified as workload, COVID related changes to Clinical Practice Guidelines, working conditions (e.g. working from home – isolated and lack of connectedness), and organisational and welfare issues.
Over the next three years we are committed to:
• Focusing on ease of access to mental health and wellbeing support services

• Increasing education and awareness of interpersonal violence and supports for individuals impacted (including family members)
• Developing a state-wide wellbeing focused leadership training and education program
• Raising awareness of the organisational factors and leadership capabilities influencing wellbeing
• Continuing to develop prevention education and strategies
• Reducing stigma, in particular self-stigma
While there is a significant amount of work to do, we are committed and passionate about providing the highest level of support we can to AV employees, first responders and their families. So next time you see an AV Peer Support Dog, take time to look up to the Peer Dog Handler at the end of the lead and know that there is a large, skilled, committed, dedicated and proud team working in the background, determined to improve mental health and wellbeing at Ambulance Victoria.
Focus First 28 www.caa.net.au
Family and friends supporting the mental health of paramedics
Paramedics are nearly twice as likely as the general population to experience mental ill-health.

Family and friends provide most of the practical and emotional support and are therefore key to improving their mental health and wellbeing.
Our free, self-paced online program for family and friends features interactive activites, multimedia content, personal stories and peer support forums.
Minds Together provides practical ways to help family and friends:
Learn new strategies for supporting paramedics
Strengthen their coping and communication skills
Reduce their stress and worry

Connect with other people supporting paramedics.


Learn more about Minds Together at www.everymind.org.au/supportingparamedics



Managing the mental-ill health impacts of being a paramedic
By Dr Sally Fitzpatrick
Working as a paramedic provides a sense of identity, status and camaraderie. And as health services nationwide work tirelessly in the face of a once in a century pandemic, paramedics have come to play an even more crucial role on the frontline.
Additionally, almost a third of ambulance employees have reported either high (21%) or very high (8%) levels of psychological distress resulting from their work.
Paramedics are a respected and vital part of our community and healthcare system and are consistently ranked as one of the most trusted professions in Australia.
There are many strategies that can occur within organisations and by individuals for improving mental health and coping with distress. Self-care is one of the simplest strategies available and can be pivotal to making a real difference for both paramedics and those in their inner circles.
The day-to-day pressures, paired with facing traumatic events and the unpredictable nature of long and shifting working hours, can significantly affect the mental health of those who serve. These factors contribute to paramedics experiencing disproportionally higher rates of mental ill-health and suicidal distress.
Recent research has found ambulance personnel are at almost double the risk of having a diagnosis of mental ill-health compared to the general population with PTSD, anxiety and depression the most commonly experienced conditions.

Self-care is often referred to as activities we do to look after ourselves physically and mentally. These activities increase energy, improve our health, and reduce stress. There are many ways to do this, and self-care is something that can be personalised. Self-care can also be processing emotional reactions and doing things we might find difficult. Perhaps one of the most difficult is asking for help, but being able to do this is a real strength.
Being mentally healthy and living well is important to every single one of us. It’s about enjoying life and connecting to friends, family, community and culture.
Focus First 30 www.caa.net.au
Dr Sally Fitzpatrick
Dr Sally Fitzpatrick is a clinical psychologist, researcher and a program manager at Everymind, a leading institute dedicated to the prevention of mental ill-health and suicide.

Self-care is not always easy, but taking time to do something small each day, week or month is a good start, and we’ve added some tips to help:
Physical
• Be active and eat well
• Get enough sleep and rest
• Monitor and manage your stress in positive ways
• Limit the use of alcohol and other substances
Relationships
• Nurture and maintain your relationships
• Connect with others to keep strong
Time for you
• Make time for interests and things you enjoy
• Get involved and join a group with common interests
• Learn something new to help build your confidence
Spiritually
• If you have spiritual beliefs, make time for regular spiritual practice
• Connect with others who share your philosophy
And remember everyone needs support from time to time. This means reaching out. Talking to a family member, a friend, your doctor or one of the many services available can make all the difference. If you are supporting someone with mental ill-health, remember that you can also reach out for extra support.
Triple Zero (000) Paramedics can require emergency care or support too. If you or someone near you are in immediate danger, call 000 or present to the nearest hospital emergency department.

Lifeline For 24/7 crisis support call Lifeline on 13 11 14 or text 0477 13 11 14.
Beyond Blue Call Beyond Blue on 1300 22 4636 or visit beyondblue.org.au for free support.
Carer Gateway Call Carer Gateway on 1800 422 737 for free services and support for carers.
Everymind Learn more about Everymind’s programs: everymind.org.au
31
Staff Support Program notches up key milestone
By NSW Ambulance
NSW Ambulance is celebrating the 100th Wellbeing Workshop –a crucial program designed to support the mental and physical health of our staff.

COVID-19 has tested the resilience of our staff like nothing the organisation has ever experienced before. This is something you’ve read, heard and experienced time and time again over the past three years. It’s a credit to the workforce on how they have responded to challenges posed by this pandemic.
One of the key initiatives that has helped support staff through those challenges has been the Wellbeing Workshop program. And, despite several postponements of the program during the pandemic, in May our organisation celebrated the 100th edition of the Wellbeing Workshop.
The Senior Program Specialist of Wellbeing Workshops, Elizabeth Simeoli, said this significant milestone meant that more than 4800 members of our workforce had now completed the program, with approximately 1700 staff remaining.
“It’s such a significant achievement and celebration for the whole organisation, our participants and our workshop team,” Elizabeth said.
Focus First www.caa.net.au
32

33
“The workshop has experienced a number of changes and stoppages throughout the COVID-19 period, but there was always a commitment from all areas and levels of the organisation to keep the program running.
“We often receive feedback from participants during or after the workshop saying, ‘my workshop attendance was perfectly timed’ or ‘the workshop gave me the nudge or wake up I needed’ or ‘thank you for caring for
Also, part of the 100 club is Junee Paramedic Jono Finn. Jono said the program offers a great base for staff who haven’t previously placed a strong focus on their personal wellbeing (e.g. nutrition and fitness). He also said it provides a good refresher for those who have.
“Given COVID-19 was a huge distraction and a downer, this was a timely refresher to bring back some of those strategies to implement into my work life,” he said.
“I think it has given me the motivation to get back on track and start following those good habits again, like drinking more water, improving my nutrition and getting more sleep."
us and showing us help is available’. Comments like these bring our workshop team great joy. We are absolutely driven by the idea of supporting our staff in any way we can, especially knowing the incredibly intense and exhausting few years they have experienced.”
The workshop is a development program designed to support the mental and physical wellbeing of NSW Ambulance staff. Participants learn simple yet powerful strategies and skills to implement into daily life to enhance health, safety, self-awareness, wellbeing and quality of life. Kogarah Paramedic Jodie Anderson – who was part of the 100th workshop – said the three-day program (which runs for one and-a-quarter days for nonoperational staff) was “extremely beneficial.”

“I think it has given me the motivation to get back on track and start following those good habits again, like drinking more water, improving my nutrition and getting more sleep. “All of those factors can help reduce the chance of fatigue or injury, while also helping me to look after myself better both off-duty and on-duty.” Jodie said she hoped the workshops can be an ongoing initiative.
The Wellbeing Workshop has also provided a good opportunity for staff to meet other colleagues from different parts of the organisation. Take for instance, Wauchope Paramedic Dave Moran and Critical Care Paramedic (CCP)/Aeromedical Control Centre Officer Michael Burrow. The two met at the 100th workshop, and, after being prompted during a session to think of ways to challenge themselves, they decided they would both do five pushups during each interval of the three-day course.
“Going forward, he (Michael) will be getting emails from me asking if he has done his push-ups,” Dave joked.
“This workshop has been a bit of a godsend for me, particularly around nutrition and being mindful of how we should think about ourselves a lot of the time.” Added Michael: “I’ve been in the job for more than 30 years and I’ve never had the opportunity to attend a workshop like this one before, where it encourages you to take time out to look after yourself.” “Because of this, I think the workshop can also help staff to be more efficient and effective in their job.”
34 www.caa.net.au
QAS experience with the Chnnl Application
By Queensland Ambulance Service
What is Chnnl?
Chnnl is a mental health and wellbeing app which takes up just a small portion of your day to have you answer it’s wellbeing questions. Complete anonymity empowers you to tell it like it is, to literally channel your feelings and note whether you’re only just coping or thriving, and what may be challenging you the most. By sharing these real-time insights it empowers leadership teams to take action by responding to employee feedback and cultivate a positive culture.
Our Experience
Staff mental health has always been an important focus area for Queensland Ambulance Service (QAS) which is why the Priority One Staff Support Program has been in place for more than 30 years. One of the important aspects of this program is that it has continued to evolve, based on the needs of the staff during this time.
During the development of the QAS Mental Health and Wellbeing Strategy staff identified that they wanted an easy to access electronic medium to self-monitor and to access peer support and counsellor contact numbers. Given that many ambulance personnel do not sit at a computer it was identified that a mobile application would be the best option.
Introduced through the Council of Ambulance Authorities (CAA), the QAS made the decision to trial Chnnl because the App utilised evidence informed/based information. Also, importantly, given Chnnl’s independence from any ambulance service, staff could feel confident that their information could remain anonymous from the organisation.
Prior to release, QAS undertook their due diligence to ensure security, legal and clinical governance of the App, therefore it wasn’t until Jan 2022 when the App was released to all staff.
Participants using the App have provided the following feedback in relation to its benefits.
The opportunity for:
• self-expression
• the recognition of positive and negative experiences
• self-monitoring to identify own wellbeing trends

• earlier identification of the need to access support
• convenient access to additional supports and resources
• reminders around wellbeing.
Since release, the uptake has been gradual and there are many limitations to a standalone App of any kind. However, Apps are never designed to be the whole answer to psychological wellbeing and are not for everyone. They are designed to simply augment the many other wellbeing strategies that people use such as connecting with others, exercise, diet, sleep, counselling etc.
35
Focus First
Can Artificial Intelligence Increase Emotional Safety in Emergency Call Centers?
 By Andreas Cleve, Corti CEO
By Andreas Cleve, Corti CEO
Throughout the COVID-19 pandemic, ambulance agencies worldwide saw a surge in call volume, increasing pressure on call takers and ambulance
Thought-leading ambulance agencies are turning to artificial intelligence (AI) to help reduce the pressure on emergency call-takers and create a better work environment with less stress and burnout.
To rewrite the rule book in this new world of postCOVID-19 healthcare, agencies across the United States and Europe started asking how to find scalable ways of caring for their staff. Staffers needed more emotional safety, less pressure, more coaching and training, and better access to sparing after the most gruelling cases.
crews alike. This pressure created a negative spiral for many agencies, leading to stress, burnout, and staff shortage, and if that wasn't enough, the consequences were severe for patients too.
In some cases, this spiral led to frustrating call queues, long response times, and even more ambulances docked at the hospitals. In rare cases, the demanding circumstances could cause the slightest problem or misstep to wreak havoc as the media jumped on the opportunity to weigh in, exacerbating a public blaming culture that further reduced the joy of work for the many critical staff members at their respective agencies.
Given the pressure-kettle environment and scarce resources, this was a big ask. Agencies were daunted. Quality improvement has long been manual and reactive, handled externally, and if not, then by overworked managers. Any of these lead many agencies to look for rocks unturned in search of a scalable, innovative solution.
Agencies like Seattle Fire Department and the NHS trust in Scotland welcomed the benefits of artificial intelligence. Their belief was that instead of qualityassuring a random sample of calls after they’ve long been completed, why not let the AI quality-assure all emergency calls in the background?
Opinion First
36 www.caa.net.au
Here the AI could help answer the most critical questions, such as how we can stop overtriaging low acuity calls to reduce ramping?
The technology company Corti.ai is the global leader in artificial intelligence for high and low acuity medical calls. Through a partnership with Medical Priority Dispatch, the two companies found a way to train the AI to understand the local dialect, the most prevalent call-taker protocols, and the quality assurance reporting format allowing the AI to help find cases where the staff needs support. After spending years trialing and testing the solution, the AI can now benefit call takers on every call.
The AI listens in and then fills out all the quality assurance and quality improvement forms, and finds opportunities for care. This gives every caring manager a real-time pulse of how the call takers in the operation centre are faring, so they don't have to wait weeks or months to come to their aid or support.
In the absence of managers acting as the second pair of ears on every call, the AI fills this gap and helps foster a more nurturing and caring culture in the call-centre that revolves around growth rather than blame. Administrative work is reduced and staff can get the bespoke care and training they actually need when they need it.

If you want to hear more about how you can get AI to help care for your call takers, so you can focus on reducing stress and burnout, then please contact info@corti.ai.
Andreas Cleve
Andreas is one of the founders of Corti, one of the leading artificial intelligence companies in global healthcare.

Andreas has been working in the healthcare sector for over a decade, first founding and later selling Ovivo, and in 2016 he co-founded Corti. Andreas graduated from Copenhagen Business School, and he has been nominated for a host of awards for his work in healthcare; among the most prominent, he was named as one of the 35 under 35 Innovators by MIT.
Corti is a Danish company founded in 2016. The company employs more than one hundred people and is building the world's leading support platform for low and high-acuity medical calls. Corti has offices in Europe and the United States and has several awards and media accolades for its peer-reviewed research and innovations. In 2021 Corti partnered with Medical Priority Dispatch to help accredit MPDS agencies automatically. Contact info@corti.ai for more information.
37
Unsung Heroes
From SA Ambulance Service
Outback
That’s exactly what happened though, to SA Ambulance Service volunteer Ambulance Officers Taryn Carey and Megan Burt. Megan, Taryn and their patient, injured in a motor vehicle accident, found themselves caught in floodwaters near Leigh Creek, after more than the annual average rainfall fell in one weekend in January 2022. The team and their patient were rescued from the creek by local farmers from nearby sheep stations. The three of them were eventually airlifted out the following day.
The efforts of all involved were recognised in June at the SAAS Excellence Awards with CEO Community Commendations for the farmers, while the officers accepted a CEO Commendation.
Taryn, who is also a local nurse, shares her story: “A massive shoutout to the people who are the backbone of the outback, the station guys. We were on a job that should have taken four hours at most retrieving a patient who had been involved in a vehicle rollover at Leigh Creek. The job took 28 hours in total due to weather and flooding. After six hours we were still en route trying to get back to the clinic. It was not going to happen. The creeks were raging something fierce, and we were stuck. We couldn't go further and South Australia Police and State Emergency Service couldn't get to us to help. They tried their best though, kudos to them.

South Australia is potentially the best and the worst place to find yourself stuck in flash flooding.
38 www.caa.net.au
Services First
Our knights in shining armour came in the form of Geoff and Major in their trusty 75 Series LandCruiser. They unbogged us and got us through the next creek but we were not getting over the one after that. We turned around thinking we would head back to Depot Springs and wait it out, all night if needs be. Alas, the previous creek had risen, and the ambulance wasn't getting back over that one either.
The guys radioed their station, told them what was happening, and asked for coffee and food to be sent out. The station further out joined forces bringing their grader to help. Enter Budgie and Luke from Angepena Station. They arrived with food from their place plus food from Depot Springs, more than two health workers could ever eat. But believe me we gave it our best shot. The ambulance was going nowhere, and our four heroes were weighing up the pros and cons of ferrying us across in the grader. However, the patient would not tolerate this. We were stuck with the ambulance looking at a night on the side of the road. Hey, we had food and coffee, but it would be a long one.
They decided to try grading the creek under the water so that we might just get back across. Back and forth Budgie went with that grader and hey presto, it worked. They could tow us back through safely and on to Depot Springs. On arrival we were greeted by Geoff and Majors' partners, Di and Kaeli. They brought roast lamb dinners eaten with much appreciation at 2400 once patient was settled in. We passed a busy night with our patient. In the morning hot breakfast was delivered. We were at risk of falling into a food coma. These guys helped with locating an ideal place for our chopper to land and were just willing to do anything. They wanted absolutely nothing in return. We couldn't thank them enough, but they were quite adamant that it was no big deal. But it was.

These guys risked their lives to get to us. They put their work on hold and made sure we were safe and comfortable. The way they jumped in, not looking for anything in return, just wanting to help, was very humbling. They are the unsung heroes of this country.”



 Pictured above is Adrian, Operations Manager, SAPOL’s Johnathon, Dianne, Kaeli, David and Dusty from Angepena Station, Lesley from Depot Springs Station, and Taryn and Megan from SAAS.
Adrian with Dianne, Kaeli, David and Dusty from Angepena Station
Adrian and SAPOL’s Johnathon
Adrian and Lesley from Depot Springs Station
Adrian and Taryn
Pictured above is Adrian, Operations Manager, SAPOL’s Johnathon, Dianne, Kaeli, David and Dusty from Angepena Station, Lesley from Depot Springs Station, and Taryn and Megan from SAAS.
Adrian with Dianne, Kaeli, David and Dusty from Angepena Station
Adrian and SAPOL’s Johnathon
Adrian and Lesley from Depot Springs Station
Adrian and Taryn
39
WA cricket stars learn St John first aid following Warne, Marsh and Campbell Cardiac Arrests
From St John WA
StJohn WA has answered the call of Australian cricket stars seeking to improve first aid among former, present and aspiring cricketers in light of recent heart attacks in the sport.
This year, famous Australian cricketers Shane Warne and Rod Marsh died of suspected heart attacks, while Ryan Campbell came dangerously close in April but first aid saved his life.
“If you actually get a chance to do a first aid course, make sure you do because you never know you could be the one to help someone out,” Campbell told reporters in May, shortly after his recovery.

www.caa.net.au40 Services First
Former international cricket star Michael Hussey partnered with Campbell for more than a decade in WA cricket.
“So grateful really for the young girl who was at the London Park with him and could do the CPR and virtually saved his life,” Hussey told Nine News exclusively. “It sort of really hit home, I need to get my skills back up to speed as well.”
This month, Hussey together with fellow WA cricket legends Adam Voges, Kade Harvey, Wayne Clark, Tom Hogan, Ross Edwards and Geoff Marsh took part in first aid conducted by St John WA senior trainer Hayden Clark in order to improve their skills and raise awareness.
“You just don't know when it's gonna happen and if you can just do something to help – I think it's important that everybody makes the effort,” Wayne Clark told Nine News.
Ross Edwards played all his cricket with Rod Marsh.
“One wonders if there had been somebody in the car or with him when that happened he might have been saved,” he said.
St John responds to about 2500 out of hospital cardiac arrests a year, but sadly most go unnoticed as 80 per cent occur in people’s homes.
In 2020, St John WA attended 2698 OHCA cases of which 40 per cent were attempted to be resuscitated. Thankfully almost 80 per cent of those were getting CPR from witnesses to the event before St John paramedics arrived. St John WA delivered 224 OHCA patients with a pulse to hospital and of the 128 OHCA survivors, four were children aged 15 or younger.
It is because of these sad statistics, St John WA offers free first aid in schools and communities which install St John issued defibrillators to vastly improve survival rates for cardiac arrest patients.
St John WA First Aid Training Manager Ross Pratt said first aid was vital to helping ambulance services save lives.
“Along with our Youth and Community Trainers more than 338,000 people were trained in first aid in WA this year, including school children starting as young as year one,” he said.
“St John offers 8000 first aid courses a year across the state for ages ranging from 16 to 79, which has resulted in 89,400 getting qualified this year alone.
“St John WA’s Restart a Heart Day on October 16 challenges people to share their CPR training on social media using the #9for9 hashtag and tag nine others,” he said. “We urge people to get behind it as it helps raise awareness for the nine out of 10 people who don’t survive out-of-hospital cardiac arrest.”

41
EVERY MINUTE SOMEONE’S HEART IS NOT PUSHING OXYGEN AROUND THEIR BODY AND BRAIN THE CHANCES OF SURVIVAL DROP BY 10 PER CENT. NINE OUT OF 10 PEOPLE WON’T SURVIVE AN OUT-OF-HOSPITAL CARDIAC ARREST. EIGHTY PERCENT OF OUT-OF-HOSPITAL CARDIAC ARRESTS HAPPEN IN PEOPLE’S HOMES. AFTER TEN MINUTES WITHOUT INTERVENTION, THE DAMAGE CAUSED BY A CARDIAC ARREST IS NEARLY IRREVERSIBLE. To learn more visit restartaheart.net 80%
CAA Women in Leadership Scholarship
Encouraging and supporting women in their professional development

This year the Council of Ambulance Authorities (CAA) launched the inaugural CAA Women in Leadership Scholarship. The scholarship was formed through the
There is indeed a need within the pre-hospital sector to help women flourish in their careers, assisting their development to become better leaders in the future.
CAA Women in Leadership working group, who sought to address the challenges and adversities for women in the pre-hospital sector by encouraging leadership development and mentoring. Specifically, the scholarship aims to encourage more women to step into leadership roles and to support the further development of current women leaders in the Ambulance services sector.
The winner received a fully funded one-on-one leadership course with Julie Piantadosi from Total Coaching Academy, valued at over $7,000.
Julie is one of Australia’s most sought-after coaches who is a specialist in empowering the mindset, leadership, and rapid acceleration. Through the program she helps make the shift from ordinary to extraordinary through simple and effective tools to improve your life personally and professionally.
Being the first year of introducing this scholarship we were not expecting the amount of excitement and interest it received. With over 100 applications, we were overwhelmed by the portfolios of the incredible women who applied and the stories shared.
We are grateful to all those who applied, and acknowledge that based on the number of applicants and content within, there is indeed a need within the pre-hospital sector to help women flourish in their careers, assisting their development to become better leaders in the future.
Awards First 42 www.caa.net.au
Our 2022 CAA Women in Leadership Fnalists:
Karen Stewart
Karen career started in the Scottish ambulance service as a transport officer when she was 20 years old. In 2012 she moved to St John Ambulance (WA) as a paramedic. Karen has had a number of roles throughout her career with St John WA including in clinical services. She is currently the Senior Operations Manager in the Country Ambulance Service and is a representative for St John WA on the Council of Ambulance Authorities Women in Leadership Forum.
Karen believes the scholarship will assist in enhancing her current skills to be able to take her leadership to the next level and provide support to emerging leaders in ambulance.
Kathryn Eastwood
Kathryn is a MICA Paramedic and a Clinical Instructor at Ambulance Victoria, as well as a Research Fellow at Monash University. She is passionate about paramedicine and through paramedicine research she hopes to contribute to strengthening and increasing the efficiency and effectiveness of the field. Her paramedicine research strives to create foundational systems and structures to allow ambulance services to improve patient care outcomes.
Kathryn believes that improving her leadership skills will provide her with additional skills to expand her research team and to incorporate more of her peers into the building of a paramedicine specific evidence base research which is the working environment she is striving for.
The CAA Women in Leadership Scholarship will be back in 2023, to keep up to date keep your eyes on the Council of Ambulance Authorities social channels and website.
Marinda is currently a Senior Aboriginal and Torres Strait Islander Cultural Safety Advisor in the Office of the Commissioner at QAS. She commenced her career in the public service in 2001 with the former Department of Emergency Services and has held various Human Resource positions for the department, incorporating Queensland Ambulance Service, Queensland Fire and Rescue Service and Emergency Management Queensland.
Marinda is a proud Birri Gubba and Gungalu woman from Central Queensland. She is very passionate about the advancement of Aboriginal and Torres Strait Islanders and has contributed to this agenda for her entire career.

She believes by further developing her leadership capabilities, she can assist in developing, mentoring and encourage others to advance not only within QAS, but the broader ambulance community.
 Marinda Thomas
Winner of the 2022 CAA Women in Leadership Scholarship
Marinda Thomas
Winner of the 2022 CAA Women in Leadership Scholarship
43
2022 CAA
Awards for Excellence Star Award Winner

Ambulance Victoria: Real-time COVID-19 data linkage to inform the pandemic response
Q1. Provide a quick recap of the project. What was the initial aim and end goal?
In Australia, the collection of surveillance data has been at the centre of the public health response to the COVID-19 pandemic and has supported critical decision-making around testing and hospital capacity. However, comparatively little is known about the way surveillance data is being used to inform the preparedness of emergency medical services (EMS) for the COVID-19 pandemic.

Our project, led by Ambulance Victoria’s (AV) Centre for Research and Evaluation, established Australia’s first ongoing data linkage initiative between AV’s clinical data and a register of confirmed COVID-19 patients managed by the Victorian Department of Health. The project aimed to:
1. Provide critical intelligence and real-time reporting of ambulance attendances to COVID-19 patients;
2. Establish a mechanism to identify high-risk staff exposure and initiate isolation procedures, and;
3. Provide an evidence-base for the clinical acuity and ambulance response priority to patients with COVID-19.
Awards First
44 www.caa.net.au
Q2. How did the project come to be?
The World Health Organisation advocates that real-time surveillance of the COVID-19 pandemic is critical to the preparedness of public health systems and the strategic incident response. International literature contains a myriad of examples of how COVID-19 surveillance data is being used to inform the preparedness and response of a range of health care providers. However, comparatively little is known about how EMS agencies are using surveillance data to inform their incident response.
At the beginning of the pandemic, ambulance services in Australia (including AV) lacked the critical information systems to have visibility on which patients accessing Triple Zero (000) were COVID-19 positive. This is particularly true for patients who presented to paramedics with symptoms suggestive of COVID-19 but required formal testing before diagnosis.
The absence of this data had significant impacts on ambulance services by reducing their ability to prepare for changes in COVID-19 demand, understand the drivers of demand (for example the epidemiology), monitor staff exposure to COVID-19, and to provide an evidence-base for the clinical acuity and response priority to COVID-19 patients.
The AV Centre for Research and Evaluation is a world leader in the integrated capture of clinical data. Faced with an escalating surge of community COVID-19 presentations in March 2020, the Centre established Australia’s first real-time linkage of ambulance patients with a register of confirmed COVID-19 patients managed by the Department of Health. As the linkage process needed to be timely to allow the early identification of potential paramedic exposure to COVID-19, the AV Centre for Research and Evaluation performed the linkage on daily basis.
Q3. Looking towards the future, what is the next step for this project?
Insights gained from the project have helped drive critical improvements to the pandemic response, including the isolation and quarantining of staff to mitigate the spread of COVID-19, ambulance resourcing decisions, changes to the ambulance response priority, and enhancements in clinical practice. The initiative now represents an easily transferrable model of surveillance that can be implemented into ambulance services internationally and will support the ongoing emergency response to the pandemic. The initiative has also facilitated the development of local research examining the impacts of COVID-19 on EMS demand/resourcing and clinical practice.
Q4. What is the ultimate goal for the project?
The introduction of rapid antigen testing by paramedics has significantly improved AV’s ability to identify COVID-19 patients at the point-of-care – a capability that was previously lacking. Nevertheless, this initiative will continue to shape how we adapt to the pandemic by informing trends in operational demand and the epidemiological drivers for demand, the clinical acuity of COVID-19 patients, clinical practice decisions, and the potential need to upscale or downscale the use of personal protective equipment (PPE) to maintain the saftey of frontline staff. Importantly, the project has now been embedded into normal business and forms part of AV’s comprehensive monitoring of the incident response.




Q5. What are the collateral benefits of a project like this?
A collateral benefit of the initiative has been its ability to support an ongoing research program and evidence-based practice. The AV Centre for Research and Evaluation has published several important analyses examining the impact of COVID-19 on operational demand. The team has also examined the impact of the COVID-19 pandemic on survival outcomes from out-ofhospital cardiac arrest (OHCA). This analysis helped AV to understand the risk/benefit profile of using PPE to manage patients in cardiac arrest. As we head into the future, the initiative will inform further research on the clinical acuity of COVID-19 patients and the epidemiological drivers of demand in these populations.
45
The Queen's Birthday 2022 Honours List
CAA
congratulates and celebrates all Australians recognised in the 2022 Queen’s Birthday Honours, especially those who were recipients of the Ambulance Service Medal (ASM).

The 2022 Queen's Birthday Honours list recognises 992 Australians, including 669 in the General Division of the Order of Australia, and awards for meritorious, distinguished and conspicuous service. A number of recipients were awarded the Ambulance Service Medal (ASM) in Queen’s Birthday Honour ceremonies this year.
The Ambulance Service Medal was instituted in 1999 to recognise those who have rendered distinguished service as a member of an Australian ambulance service. The Governor-General awards the Ambulance Service Medal on recommendation from the appropriate Commonwealth, state and territory ministers.
The medal is awarded sparingly, with no more than one award each year for each 1000, or part of 1000, full-time permanent members of a state’s ambulance service or one award for each 5000, or part of 5000, part-time volunteers or auxiliary members in a state. Only one award may be made each year for ambulance members in each of the ACT, NT and the combined external territories.
Photo courtesy of Richard Bugg
Awards First
www.caa.net.au46
“Recipients share some common traits – including selflessness, excellence and a commitment to service. They’re from different backgrounds, their stories are each unique, and each has served in different ways. This diversity is a strength and each has impacted their community and made it better.” - General David John Hurley, AC, DSC, FTSE
Of the significant individuals recognised this year, many were also included on the COVID-19 Honour Roll. The COVID-19 Honour roll was introduced by the Australian Government in January 2021 to further recognise individuals for their contribution, service or achievement relating to the pandemic. Many of the recipients this year were among individuals who made and lead critical developments in regar to the pandemic over the past two years.
CAA would like to acknowledge the significance of individuals who received the Ambulance Service Medal (ASM) and of the people that were recognised in the Queen’s Birthday 2022 Honours List. The individuals recognised have significantly shaped the Australian Ambulance sector. They have gone above and beyond to support a critical sector which fell under unprecedented demand over the past 2 years. Many of the individuals recognised have dedicated their life to the sector and are integral to the communities they serve. Many were outstanding in times of emergency. They remained poised in situations that would stretch and test the most experienced of professionals and took actions that saved lives.
To the individuals that were recognised, whether acknowledged as call-takers, frontline workers, first responders, volunteers, or something else, we thank you for your service and congratulate you on being recognised by your peers and nation.
Recipients of the Ambulance Service Medal in the 2022 Queen's Birthday Honours

 NSW Ambulance Wayne Cannon Mark Gibbs Queensland Ambulance Service
Grant Gamble
St John WA Wendy Price Craig Ronald Telford Ian Telfer Craig Telford
ACT Ambulance Service
Peter Andrew Le Lievre
SA Ambulance Service
Julie Appay John Noble Shaun Whales Catherine Wright Ambulance Tasmania Glenn Aslin
St John Ambulance Australia (NT) Taleaha Dawson Craig Garraway Andrew Thomas
NSW Ambulance Wayne Cannon Mark Gibbs Queensland Ambulance Service
Grant Gamble
St John WA Wendy Price Craig Ronald Telford Ian Telfer Craig Telford
ACT Ambulance Service
Peter Andrew Le Lievre
SA Ambulance Service
Julie Appay John Noble Shaun Whales Catherine Wright Ambulance Tasmania Glenn Aslin
St John Ambulance Australia (NT) Taleaha Dawson Craig Garraway Andrew Thomas
For the full Queen's Birthday 2022 Honours List, visit www.gg.gov.au/queens-birthday-2022-honours-list 47
SAAS Accreditation
SA Ambulance Service (SAAS) is the only service in Australia to have achieved accreditation for the National Safety and Quality Health Service (NSQHS) Standards, and they've done it not once but twice.
A
Feature First
48 www.caa.net.au

Our staff and volunteers are committed to ensuring our patients get the best possible care they deserve, and when they need it. ”
Keith Driscoll, Executive Director
49
The National Safety and Quality Health Service (NSQHS) Standards aim to protect the public from general harm and improve the overall quality of health services. The standards allow for a nationwide consistency of the level of care that can be expected from different health services.
Overseen by the Australian Council of Healthcare Standards (ACHS), the council assess the healthcare service based on:
• Clinical Governance
• Preventing and Controlling Infections
• Comprehensive Care
• Blood Management
• Partnering with Consumers

• Medication Safety
• Communicating for Safety
• Recognising and Responding to Acute Deterioration
SA Ambulance Service (SAAS) is the first and only service to be accredited, and this year they have done so for a second time. Although undertaking the accreditation is not mandatory for ambulance services, the program allows organisations to deeply assess their quality management and improve processes throughout their service.
Keith Driscoll, Executive Director for Clinical Services at SA Ambulance Service, joined us to discuss what led them to undertaking the assessment and the journey along the way to achieve double accreditation.
 Project Manager, Anna Rieck who received the Excellence in Improving Safety and Quality Award at the 2022 SAAS Excellence Awards
Paramedics, Tarnya Sykes and Mackenzie Grimmett
Project Manager, Anna Rieck who received the Excellence in Improving Safety and Quality Award at the 2022 SAAS Excellence Awards
Paramedics, Tarnya Sykes and Mackenzie Grimmett
Feature First
50 www.caa.net.au
Why did SAAS decide to apply for NSQHS standards, what was the driving force behind the decision?




SAAS has always had the patient at the centre of its focus and the driving force for change and improvement. Undertaking the NSQHS Standard accreditation was a natural choice for the service to ensure the health safety of patients and staff. We embarked on this journey because we believed it was the right thing to do, not because we had to. In 2018, we attempted and successfully gained accreditation. We were the first ambulance service in the country to be accredited. It was no easy feat, as the Standards are hospital focused and do not clearly align with the pre-hospital environment we work in. However, with a whole of organisation commitment, we were successful. And now, we have been accredited a second time and remain the only ambulance service to do so.
Keith, you mentioned this was a whole organisation approach, how did you get everyone on board and get their buy in?
Our staff and volunteers are committed to ensuring our patients get the best possible care they deserve, and when they need it. This can only be done with the right mechanisms, training and procedures to ensure the clinical care is safe, appropriate and patient focused. We regularly engaged with the workforce through many channels, including in print, in person and online to prepare them for the accreditation period. I am pleased to say that since our first accreditation, the NSQHS Standards are quite simply ‘business as usual’, and very much at the forefront of our thinking and continual development to ensure we can treat and care for patients in the best possible way.

51

Feature First 52 www.caa.net.au
What were some of the hurdles along the way?
Like any accreditation an organisation attempts, there is a huge body of work behind the scenes that must be done. The project team worked tirelessly collecting evidence and communicating with the workforce leading up, during and post-accreditation to get us over the line. Applying the hospital-based standards in a pre-hospital environment was challenging. We had some great assistance from the Australian Commission On Safety and Quality In Health Care to guide us on our journey and contextualise the standards for us.
What were some of the opportunities and benefits from the project?
Accreditation is awarded for meeting 148 core actions set out in the NSQHS Standards.
The final report outlined many areas that SAAS has excelled in, such as:
• SAAS’s commitment to engaging with consumers in service planning and delivery of care.


• SAAS staff were commended for knowledge of their roles and for the pride and passion demonstrated in the care they provide to their communities.
• It was specifically noted that SAAS staff have a high level of awareness and capacity for managing patients with challenging behaviour, while ensuring a respectful and compassionate approach to care.
• The assessment team also noted the broad range of care options administered by SAAS from Telehealth to quality medical retrieval systems, and the many health care options afforded during a routine ambulance response.



It also highlighted some areas where improvements can continue to be made, including further investigation into the temperature management of medications stored within ambulances. SAAS was also encouraged to improve on systems for promoting and recording mandated training.
MedSTAR Kids Retrieval Nurse Tara Fuller with patient Holly.
53
SAAS has achieved re-accreditation in 2022, after the initial accreditation in 2018. How did this second round compare, easier or more challenging?


No accreditation is easy! The second time around, while we knew what we were getting into, the Standards had been revised (from 10 to now 8) and we were really keen to show that we had in fact improved over the interim years and integrated the Standards as business as usual. It would also be fair to say it was expected that SAAS would be more mature in the Standards environment. In some areas we were, but in others we still had room for improvement.
What would be some of the advice and tips you can give fellow services who might decide to get their NSQHS accreditation?


As demand for our service grows, it is equally important that services continue to provide safe, high quality patient care. This accreditation can provide essential insight to ensure that the patient is always at the centre of our focus. It is a vastly rewarding process and a testament to SAAS’s hardworking and professional workforce. I would also advise that this is a whole of system and organisation program that requires commitment from the leadership of the organisation through to supporting the clinicians that are providing the care. There are no half measures in this space.
Hawker volunteers Esther and Charlie Eager with patient Adam.

As demand for our service grows, it is equally important that services continue to provide safe, high quality patient care.”
Feature First
54 www.caa.net.au

55
What's on in the ambulance world Industry Events

Events First 56
CAA 60th
Gala
For the past 60 years, the Council of Ambulance Authorities (CAA) has been facilitating fundamental collaboration in and beyond the Australasian pre-hospital sector.
60years
has taken us on a journey like no other. Through ground-breaking news, milestone achievements and innovative programs, CAA and member services have played a significant role in paving the refined and bright path to the pre-hospital sector as it is today.

From the creation of CAA in 1962, CAA has worked with member services to make significant changes to the operations and landscape of the Australasian prehospital sector. From working with telecommunications companies to making 000 the common number to be called for emergencies around Australia, to introducing national specifications for ambulances. We have truly accomplished so much together.
And so, we’re sure you will agree with us, it’s time to celebrate. On November 17th, we welcome you to a night of extravagance, bubbles, dinner, and plenty of entertainment for CAA’s 60th Anniversary Gala to be held at the National Arboretum in Canberra.
Put on your best black-tie outfit and get ready for an enchanting night filled with wonder, excitement, and of course celebration. As you pull into the National Arboretum, you’ll instantly be met with breathtaking views and spectacular architecture. You’ll be greeted by a mosaic of living forests and gardens. With over 44,000 rare and endangered trees across a 250-hectare site, the Arboretum is a place of beauty and conservation.
Events First
57
As you travel through the mosaic forest, you’ll come to the heart of the Arboretum where you’ll find the Village Centre, an award-winning architecturally designed building featuring soaring ceilings inspired by the fronds of the nearby Chilean wine palm forest. And, in the village centre, at twilight, you’ll find the CAA 60th Anniversary Gala lighting up the arboretum.
Step into a world-class venue that comes alive at twilight, adorned with lashes of green and gold, with spans of glass windows providing uninterrupted panoramic views across Lake Burley Griffin and Canberra.
The night will feature delectable cuisine, elegant blacktie attire, and exclusive entertainment, including a silent and live auction. The silent auction will feature a range of luxuriant and handpicked items. A live auctioneer will also light up the stage by conducting a live auction on the night, providing yet another source of excitement to the evening.
The night will also play hosts to the launch of the ‘60 Years of CAA’ anniversary book, that features some of the biggest and most impactful stories from CAA and member services over the last 60 years. To further tie in the remarkable milestone, we’ve organised a series of inspiring and engaging speakers, being some of the most influential people within the sector. Expect some very, very special surprises and announcements throughout the night which we think might just end up being the highlight of the evening.
The last few years have been extremely demanding on the entire emergency services sector. The Gala offers an opportunity for CAA to recognise all within the industry who have worked tirelessly to drive change and progression. On the night of the Gala, we aren’t just coming together to celebrate us, we’re celebrating you. Our incredible sponsors have spared no expense in hosting one of the most luxurious and magical Galas seen in the Australasian pre-hospital sector to date.
The CAA 60th anniversary Gala is expected to be a highlight on the Australasian sector’s social calendar, as one of the finest fundraising industry events to take place for 2022.

We cordially invite you to the CAA 60th Anniversary Gala in celebrating every challenge, every milestone, and every ground-breaking innovation achieved by the sector in the last 60 years. Join us in celebrating a 60-year-story that we here at CAA feel lucky and dignified to be a part of. In a stunning location surrounded by friends, colleagues, and partners, we look forward to seeing you in November for a glamorous night that won’t be forgotten for years to come.
To purchase tickets for the Gala, visit www.caa.net.au/caa-60th-gala
We look forward to seeing you for a night of wonder and celebration in November.
Events First
58 www.caa.net.au

Get Involved in the 2022 Restart a Heart Events

Out-of-hospital cardiac arrest (OHCA) affects thousands of Australians and their families every year. In our country, around 25,000 people will suffer OHCA. Unfortunately, nine in ten of those will not survive.
It’s a terrifying statistic. OHCA can strike otherwise healthy people at any stage of their lives, leaving young families without parents, children being taken away from their loved ones, and grandparents being robbed of their hard-earned retirement.
As a community, we can improve these horrifying statistics. A good starting point is to spread the phrase CALL. PUSH. SHOCK. CALL. PUSH. SHOCK. is an easy way to remember the steps of restarting a heart. When a bystander recognises that someone has suffered OHCA, they can:
1. CALL. – Call 000 AU / 111 NZ and ask for an ambulance. The emergency call taker will also provide assistance on the next two steps.
2. PUSH. – Begin Cardiopulmonary Resuscitation (CPR) compressions. Even if the responder is not trained in CPR, any attempt at compressions is better than no attempt.
3. SHOCK. – If an Automated External Defibrillator (AED) is available nearby, have someone run and get it. The call taker will be able to alert you to any community-accessible AEDs in the vicinity.
When someone suffers OHCA, the best way to give that person a chance at survival is to call 000 and begin CPR as soon as possible. One part of the problem is that not enough people know how to perform CPR. Just over half of Australian adults reported ever having undertaken CPR training, however only 22% of Australians had current (within 1 year) training. While any CPR is better than no CPR, untrained bystanders are far less likely to be comfortable beginning compressions.
Events First 60 www.caa.net.au
The Restart a Heart campaign aims to change this. By spreading awareness on how to recognise OHCA and how to respond, Restart a Heart is looking to drastically improve survival rates. For the past five years, the campaign has been growing bigger and bigger in Australia and New Zealand. In 2022, Restart a Heart have already launched an updated brand, along with a new line of merchandise.
Most excitingly, after two years of virtual events, live activations are back in the plan for this year.









The events will be held in various locations all throughout October.
One week prior to Restart a Heart Day, the crew will be holding an activation as part of the Government House Open Day in Canberra. This will run from 10am until 2pm on Saturday 8 October.

The exciting partnership formed with Build-a-Bear began in 2021 has continued this year, meaning more opportunities to spread the message. There will be education sessions held at many of the Build-a-Bear Workshop locations throughout Australia on Thursday 13 October. The Build-a-Bear events are going to be such a fun and engaging way to spread CPR knowledge to children and parents nationwide.
Restart a Heart is welcoming new supporters throughout 2022. Organisations looking to get involved can earn their own AED, a CPR education session and more goodies than you can poke a stick at (including Heartly, the Build-a-Bear).
Sports clubs, community groups, schools, and businesses large or small have specific ways to make the most of the support options offered. Head to restartaheart.net (or just google Restart a Heart) to find the level of support that best suits your organisation.
Be sure to follow all the developments of Restart a Heart on all social channels. You will constantly see the best ways to spread awareness and information on out-of-hospital Cardiac Arrest.
And always remember:
CALL PUSH SHOCK
Follow us on socials: Facebook: @restartheartday Instagram: @restartaheart.day Tik Tok: @restartaheartday Twitter: @RestartHeartDay
By partnering with local ambulance services on these events in these locations, Restart a Heart will be able to educate thousands of people on the importance of CALL. PUSH. SHOCK.
Restart a Heart Day events will be huge this year, with flagship events to be held in Adelaide, Sydney, Wellington, Canberra, and Christchurch.
61
Australian Institute for


Resilience
Disaster
Partners First 62 www.caa.net.au
The Australian Institute for Disaster Resilience (AIDR) is the National Institute for disaster risk reduction and resilience.
We collaborate across sectors to strengthen the resilience of Australian communities to disasters. AIDR creates, grows, and supports a range of networks; provides opportunities for learning, development, and innovation; shares knowledge and resources to enable informed decision making and action; and facilitates thought leadership through national conversations.
AIDR contributes to a more disaster resilient Australia through four key influencing strategies that encapsulate AIDR’s work:

• Actively supporting, growing and sustaining a range of networks across sectors and jurisdictions.
• Enabling those with a role in disaster risk reduction and resilience to come together to learn, develop and innovate.
• Collecting, developing, curating and sharing knowledge to educate and promote good practice in disaster risk reduction and resilience.
• Providing a central focus point for national thought leadership on disaster risk reduction and resilience.
63
Knowledge Hub
The Australian Disaster Resilience Knowledge Hub is a national, open-source platform that supports and informs policy, planning, decision making and contemporary good practice in disaster resilience.

Handbook Collection
AIDR’s Handbook Collection provides an authoritative, trusted and freely available source of knowledge about disaster resilience principles in Australia. There are currently 19 publications in
Education for Young People
The AIDR Education for Young People program promotes disaster resilience education for all young Australians, in schools and other educational settings. The program supports initiatives which enable young people to participate in resilient communities, applying knowledge and skills to reduce risk and take protective action before, during and after an emergency or disaster.
The Disaster Resilient AustraliaNew Zealand School Education Network (DRANZSEN) brings together educators, emergency services, community organisations, researchers and others working with young people to develop knowledge, skills and solutions for a disaster resilient future.

The Knowledge Hub highlights current and emerging themes in the resilience sector, linking national guidelines with research and fostering collaboration among leading agencies and organisations. This information is organised into themed collections that provide resources, research and tools to support disaster resilience and risk reduction. Collections cover topics such as recovery, lessons management, warnings, and evacuation.
Other features of the Knowledge Hub include:
Disaster Mapper – an interactive online record of historical disaster events
Disaster Resilience Glossary –a database of definitions of terms encountered in disaster and emergency management
Emergency Management Library – a nationally accessible source of emergency management information
Australian Journal of Emergency Management – a quarterly journal of analysis, considered views, lessons learned and insights into current and future issues from researchers and practitioners.
the Handbook Collection, which continues to grow through a program of revision and development of new handbooks. The Handbook Collection align national disaster resilience strategy and policy with practice, by guiding and supporting jurisdictions, agencies and other organisations and individuals in their implementation and adoption.
Topics covered in the handbooks include community recovery, land-use planning, public information and warnings, health and disaster management, emergency planning, and systemic disaster risk. The Handbook Collection is available via the AIDR Knowledge Hub and highlights and promotes the adoption of good practice in building disaster resilience in Australia.
The handbooks also build interoperability between jurisdictions, agencies, the private sector, local businesses and community groups by promoting use of a common language and coordinated, nationally agreed principles.
AIDR hosts DRANZSEN forums on a state and territory and national level to showcase leading examples of disaster resilience education.
Disaster Mapper – an interactive online record of historical disaster events featured on the Australian Disaster Resiliance Knowledge Hub.
Partners First
64 www.caa.net.au
Professional Development
AIDR’s Professional Development Program aims to equip individuals and groups to achieve improved resilience outcomes in their organisations and communities. AIDR offers regular professional development and learning opportunities to benefit those working and volunteering in disaster resilience across a range of sectors.
The regular program of curated professional development events and learning opportunities builds knowledge, skills, and connections that support disaster resilience. The program includes popular in-person events such as the annual Australian Disaster Resilience Conference and the Volunteer Leadership Program, hybrid events such as the Lessons Management Forum, and online offerings including various webinar series and virtual masterclasses.
Supported by experienced and knowledgeable facilitators, AIDR can deliver our range of professional development and learning opportunities broadly to our stakeholders or exclusively to an organisation by arrangement.
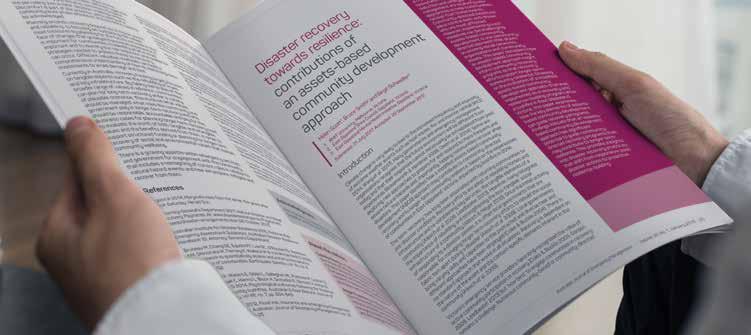
Find out more about AIDR and explore our resources and events online: www.aidr.org.au

65
Pictured above: Balance Program: 01-06 May 2022
The Australian Institute of Police Management: Preparing
Public Safety Leaders for the Practice of Leading in Complexity.
By Dr Jenny Cartwright & Superintendent Phil Green, Visiting Fellows, AIPM

Floods
and bushfires are natural disasters our public safety leaders are expected to contend with. Throw long-Covid and uncertainty into the mix, and this raises the level of complexity. So how do we prepare our public safety leaders to be able to rise to the challenge presented to them and operate in a VUCA world?1
Since the early 1960’s, the Australian Institute of Police Management (aipm.gov.au) has been integral in developing police and emergency service leaders and executives across Australia and New Zealand.

Partners First
www.caa.net.au66
Recognised for its international reputation as one of the leading educational institutions, and its accessibility to world-leading thinking, the programs on offer by the AIPM are continually evolving to stay current in today’s volatile and fast changing landscape of policing, wider law enforcement and public safety professions. These programs are developed and delivered in partnership with policing, wider law enforcement and public safety agencies, and this partnership approach is driven by the belief that better leaders are built together.
Embracing the need for leadership ambidexterity, the AIPM delivers an Executive Leadership Suite2 designed to enhance both personal and organisational leadership. These programs are delivered onsite at its world class executive training facilities at North Head, Manly, surrounded by the Sydney Harbour National Park.
Under its Executive Development Strategies (EDS1-3), the AIPM delivers personal leadership programs focussed on building on the leadership capabilities for emergent and established leaders (commencing at the Team Leader/ Middle Manager level through to Senior Executives).
For those more academically inclined, under the Executive Education Strategies stream, the AIPM offers the Graduate Certificate in Executive Leadership which leads into the Graduate Diploma. These are accredited courses under the Tertiary Education Quality and Standards Agency (TEQSA).

Under the Foundational Leadership Strategies focusing on personal and organisational leadership, there are three main programs: Facilitate – leading for learning; Frontline – leading for performance; and Balance –leading for inclusion.
The AIPM’s flagstaff women’s leadership program Balance won the ‘Excellence in Law Enforcement for Women Initiative 2017’ Award from the Australasian Council of Women and Policing.
Accommodation Buildings, Australian Institute of Police Management, Manly New South Wales.
Last day of Balance, May 2022 - Hybrid model due to Covid-19

The world has been digitally transformed as a result of the ongoing Covid-19 pandemic. This has had an impact on appetites for different ways of consuming leadership knowledge. Innovating and capitalising on technological innovations to enhance its impact and reach, the AIPM’s post-graduate programs and Balance are also delivered online. The latest online Balance program held in May 2022, brought together close to 80 women public safety leaders who were exposed to challenging presentations delivered by Elizabeth Broderick, Charmaine Burke, Jo O’Reilly, and Sam Bloom. At the end of the weeklong program, these women leaders were better equipped for the practice of leadership during complex times.
The AIPM’s programs are an enabler for public safety leaders “pushing the boundaries” and “leading edge thinking” in our VUCA world, better preparing them to tackle the challenges ahead in the practice of leadership.
Location of Australian Institute of Police Management Collins Beach Road, Manly, New South Wales

1 VUCA refers to volatility; uncertainty; complexity and ambiguity. See Bennett, N., & Lemoine, G. J. (2014) What VUCA Really Means for You. Harvard Business Review, (Jan-Feb). 2 See AIPM Business Plan 2021-22.pdf 67
Working together for our collective future
By John Bruning, CEO, Australasian College of Paramedicine
My
role sees me engage with a wide variety of stakeholders across the profession; from Ministers, advisors, and health departments to jurisdictional ambulances services, unions, universities, private medical services, and lots of individual paramedics and students. It is one of the things that I love about my role; the broad engagement and the dozens of things that are going on in paramedicine.
Of particular interest recently is that multiple stakeholders, including the College, have been looking at what the future looks like for paramedicine but, overall, we have all been doing this work in isolation from the other stakeholders. I reflect on a quote from Henry Ford, below, that highlighted that we need to be working together.
“Coming together is a beginning. Keeping together is progress. Working together is success.”
Achieving registration and then the impact of COVID has finally brought forward the opportunity for the health system to fully utilise paramedics, and we are all talking about this but not doing it together. There is immense power when a group of people with shared interests come together to work towards the same goals. From the engagements I have across paramedicine, we generally want to achieve the same goals, so it is time we worked more closely together.
The College established a Paramedicine Future Working Group in late-2021, with a broad cross-section of members from distinct parts of the profession who have been working on what the future for paramedicine looks like. We expect this work to run into 2023, but the importance of it means it cannot be rushed.
As we progress discussions on different topics we will engage with relevant stakeholders to provide input and collaborate to bring together the diversity of the profession to achieve our shared goals.
Our recent International Conference in mid-September was fittingly themed “Embracing Strengths, Shaping Futures”, and it brought together people from around the world to discuss key sectoral issues and research, with expert speakers spanning the full scope of paramedic education and practice.
As the profession continues to evolve in new directions, encompassing new work environments and different models of practice, it was an opportunity for us to share ideas as we gradually form a cohesive and mutually shared vision of what the future will look like for paramedicine, how it will work in practice, and the pathways and opportunities that exist to make that vision a reality.
It’s an exciting time for the profession, and one in which the seeds are already being planted across Australasia for future growth and expansion.
Partners First 68 www.caa.net.au
Paramedics are now working across a range of settings as part of multidisciplinary healthcare teams as their intrinsic value as skilled clinicians becomes increasingly acknowledged and recognised in broader health circles. Forwarding-thinking doctors, nurses and medical administrators understand that both our health systems and our public health outcomes are demonstrably improved when paramedics are given the opportunity to utilise their considerable skills and experience in primary healthcare and in broader patient care and treatment.

To keep the momentum going requires commitment, consensus, and unity among stakeholders. The future is ours to shape, and we look forward to making this journey in partnership with other stakeholders as we move ahead.

There is immense power when a group of people with shared interests come together to work towards the same goals”
69
The FIrst Responder Shock Trial (FIRST)
A cluster randomised controlled trial of smartphoneactivated first responders with ultraportable defibrillators in out-of-hospital cardiac arrest
By Ambulance Victoria and St John New Zealand
Combining smartphoneactivated first responders (GoodSAM) with an ultraportable AED solution, such as the CellAED®, has the potential to significantly increase the number of shocks provided by bystanders during an alert for Out-of-Hospital Cardiac Arrest (OHCA).
Background
Out-of-hospital cardiac arrest (OHCA) is the ultimate prehospital emergency and a leading cause of mortality globally.1 In Australia and New Zealand, the incidence of OHCA is one of the highest in the world, with over 30,000 OHCAs annually.2 Typically, less than one in ten patients survive to hospital discharge.3
The most significant opportunity for improving outcomes in OHCA is within the first few minutes of arrest. Early intervention by bystanders, such as cardiopulmonary resuscitation (CPR) and defibrillation, remains a crucial factor driving better short-term and long-term functional recovery outcomes.3

Research First 70
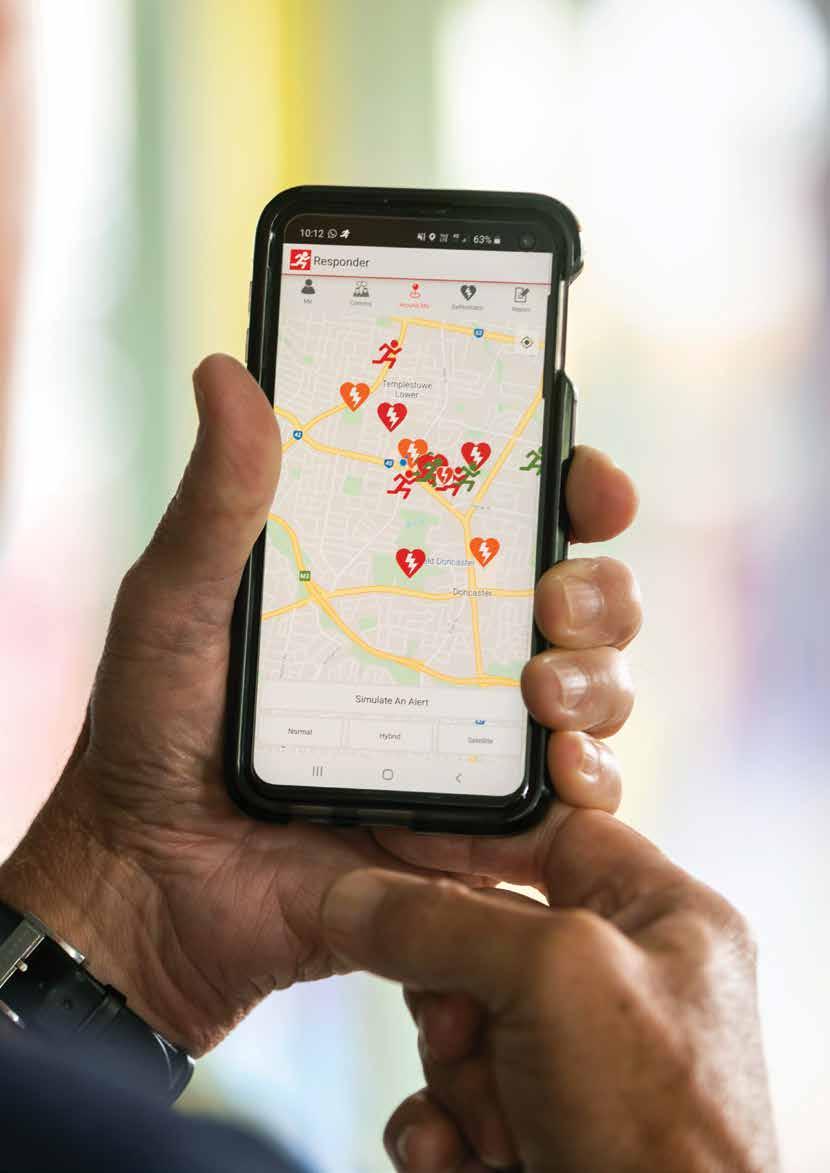
71
In recognition of bystanders' significant impact on resuscitation efforts, many regions focus on strengthening the community response to OHCA. In 2018, Ambulance Victoria and St John, New Zealand rolled out the GoodSAM (Smartphone Activated Medics) smartphone application. Read more about GoodSAM responders at www.goodsamapp.org
Briefly, the GoodSAM app is integrated into the emergency call system (Triple Zero (000) in Australia or Triple One (111) in New Zealand) and, if available, alerts members of the public to potential OHCA events nearby, allowing them to respond and deliver life-saving CPR and defibrillation. Notably, the app also alerts first responders to a nearby automated external defibrillator (AEDs) location if one exists.
The GoodSAM app has significantly influenced systems of care for OHCA patients in Victoria and New Zealand, and patients who receive a GoodSAM attendance are significantly more likely to receive bystander CPR and a shock from a bystander using an AED. Although the GoodSAM app aims to increase bystanders' access to AEDs in the community, public access defibrillation (PAD) use rates remain low even among GoodSAM responders (16%).4 This likely reflects the socio-economic, geographical, and practical inequities in the current placement of AEDs across our communities.4 GoodSAM responders' desire to assist OHCA patients as quickly as possible also creates a reluctance to detour to retrieve an AED.
A novel defibrillation strategy
New defibrillation technology has been developed to improve cost-effectiveness and provide greater accessibility of AED for the public. One such device is the CellAED®, an ultraportable, single-use, transit-operable, fully automated AED. In 2021, the device received regulatory approval from the Therapeutic Goods Administration and is currently sold in Australia and New Zealand. There is a considerable public interest in the device, which is expected to help address the socio-economic and geographical barriers to PAD use. The device's limitations, which require careful consideration in PAD programs, are that they are singleuse and have a short service life of approximately 13 months, although its short service life would suggest that their utility may be more cost-effective in the hands of bystanders with frequent exposure to OHCA.
Defibrillation by bystanders using an AED halves the time to first defibrillation and produces survival often over 65% in Australia and New Zealand.5 6 Developing strategies to improve timely response and defibrillation by bystanders has been identified as a leading research priority.7
The FIRST trial is a multicentre cluster randomised controlled trial led by Dr Ziad Nehme, Ambulance Victoria; and Associate Professor Bridget Dicker and Dr Verity Todd, St John New Zealand. The trial will be conducted in Victoria, Australia, and New Zealand to examine whether equipping high-frequency GoodSAM responders with an ultraportable defibrillator (CellAED®) can increase survival to 30 days in OHCA compared with the current strategy of retrieving the closest available AED.

Improving first responder access to AEDs is a strategic priority and will drive significant improvements in outcomes for OHCA.
72 www.caa.net.au
This trial will also determine the feasibility, efficiency, cost effectiveness and acceptability of the CellAED® for use by targeted GoodSAM responders dispatched to suspected OHCA in Victoria and New Zealand.
The rationale behind this trial is simple: the single most significant barrier to increasing the use of AEDs by bystanders is their location.5 Despite evidence supporting the clinical effectiveness of PAD programmes, there is relatively little evidence informing their optimal placement and cost-effectiveness.7 Significant limitations exist in the current model of the PAD programme, and AED is rarely available in the first minutes of OHCA. Although 75% of OHCA currently occurs in the home, most PADs are located in high-density public locations, typically stored in cabinets within major buildings, and their deployment assumes low utility after business hours.6 Unfortunately, this strategy has resulted in relatively little penetration of AEDs into homes, where less than 1% of initially shockable OHCA are currently receiving bystander-initiated defibrillation.5
Research question
This study's population will include high-frequency GoodSAM responders with an annual alert accept frequency 0.5 since initial registration and OHCA patients from Australia (Victoria) and New Zealand. The intervention is to equip and maintain high-frequency GoodSAM responders with an ultraportable defibrillator (CellAED®), while the comparator is the current paradigm of retrieving the closest PAD by GoodSAM responders during an alert for OHCA. The primary outcome of this study is survival to 30 days.
Eligibility Criteria
A pragmatic eligibility criterion reflecting the real-world application of PAD in the community will be utilised in this study. All OHCA, as assessed by emergency medical services (EMS), and eligible GoodSAM responders who accept an OHCA alert and arrive on scene before EMS, will be included in the study. Patients with a Do Not Resuscitate (DNR) order or Advanced Care Directive, OHCA secondary to trauma or hanging, and a location or events where scene safety issues apply will be excluded from this study.
Procedures
For GoodSAM responders randomised to the intervention arm, each responder will receive a CellAED® and will be asked to watch a short (10-minute) instructional video on its application. An instructional pamphlet detailing the operation, storage, and carriage of the CellAED® will be provided. Routine GoodSAM activation procedures will apply according to the region’s default response radius, and responders will be flagged within the GoodSAM app as having an AED in their possession.
For alerts where two or more GoodSAM responders with a CellAED® device accept the alert, one of the responders will still be instructed to retrieve the closest
AED according to standard operating procedures. CellAED® will be replaced as needed, and monthly emails and push notifications will be sent to GoodSAM responders with reminders about the optimal storage and carriage of the CellAED® device.
For GoodSAM responders randomised to the comparator arm, routine activation procedures will apply according to the region’s default response radius, and responders will continue with the current protocols of retrieving the closest PAD during an alert for OHCA.
Overall, the FIRST study is examining a novel, community-based model of care for OHCA that will challenge the current paradigm and significantly impact this patient population. We will establish the practicality of using the ultraportable AED as an added element of first-line resuscitation efforts and the acceptability of this strategy to foster earlier community intervention during OHCA. The results of this trial have the potential to address the limitations of the current PAD programme and improve cardiac arrest survival in our most at-risk communities. It will enhance GoodSAM responders' access to AEDs, which will drive significant improvements in outcomes for OHCA. This study is well placed for translation as a border model of care and has the potential to overcome the socio-economic, geographical, and practical inequities in the current placement of AEDs across our communities.
References
1. Valenzuela TD, Roe DJ, Cretin S, et al. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation 1997;96(10):3308-13. doi: 10.1161/01.cir.96.10.3308 [published Online First: 1997/12/13]
2. Bray J, Howell S, Ball S, et al. The epidemiology of out-of-hospital cardiac arrest in Australia and New Zealand: A binational report from the Australasian Resuscitation Outcomes Consortium (Aus-ROC). Resuscitation 2022;172:74-83. doi: 10.1016/j.resuscitation.2022.01.011 [published Online First: 2022/01/26]
3. Berdowski J, Berg RA, Tijssen JG, et al. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010;81(11):1479-87. doi: 10.1016/j.resuscitation.2010.08.006 [published Online First: 2010/09/11]
4. Dicker B, Garrett N, Wong S, et al. Relationship between socio-economic factors, distribution of public access defibrillators and incidence of outof-hospital cardiac arrest. Resuscitation 2019;138:53-58. doi: 10.1016/j. resuscitation.2019.02.022 [published Online First: 2019/02/26]
5. Nehme Z, Andrew E, Bernard S, et al. Trends in survival from out-of-hospital cardiac arrests defibrillated by paramedics, first responders and bystanders. Resuscitation 2019;143:85-91. doi: 10.1016/j.resuscitation.2019.08.018 [published Online First: 2019/08/21]
6. Lijovic M, Bernard S, Nehme Z, et al. Public access defibrillation-results from the Victorian Ambulance Cardiac Arrest Registry. Resuscitation 2014;85(12):1739-44. doi: 10.1016/j.resuscitation.2014.10.005 [published Online First: 2014/12/03]
7. Kleinman ME, Perkins GD, Bhanji F, et al. ILCOR Scientific Knowledge Gaps and Clinical Research Priorities for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: A Consensus Statement. Circulation 2018;137(22):e802-e19. doi: 10.1161/CIR.0000000000000561 [published Online First: 2018/04/28]
73

Research First Paediatric cardiac arrest: What you should know www.caa.net.au74
Our anxiety around these calls stems from many factors: unfamiliarity due to low exposure rates, smaller equipment, weight-based calculations, and the enormous emotional burden that's often associated with these calls.
Let’s strip away the complexities and by removing the cognitive burdens, focus on providing high-quality resuscitation to our smallest patients.
By James Yates MSc DipIMC MCPara
Specialist Paramedic Critical Care (Great Western Air Ambulance)
Advanced Paramedic Neonatal Retrieval (Newborn Emergency Stabilisation and Transport Team)
When we get a call involving a child, it strikes fear into our hearts –especially when it's a paediatric cardiac arrest.
75
Let's start with a quick review of the paediatric arrest algorithm from the Resuscitation Council UK.1 Local protocols might look slightly different from those from the UK Council, all of the rest of the information is going to be widely applicable to all ambulance services wherever they are based.
How to recognize cardiac arrest
• Clinical grounds: if the patient is unconscious and apneic with absent pulses
• Monitored vital signs: if the patient is already monitored and ECG rhythm shows a rhythm incompatible with life or loss of end-tidal carbon dioxide trace
• If a paediatric patient is unconscious with a heart rate less than 60 and signs of poor perfusion
• Once you’ve identified the patient as being in an arrest:
• Open the airway and deliver five rescue breaths.
• Start CPR at a ratio of 15 compressions to 2 breaths.
• Apply defib pads during this early part of the resuscitation. Generally, these will be in the standard anterior-lateral orientation, but in infants less than one year – and perhaps in older children if they're particularly small – the anterior-posterior position might be useful. Make sure the pads don’t touch each other to eliminate the possibility of a spark.
• Once the pads are placed, pause chest compressions to analyze the rhythm. Just as in adult advanced life support, the goal is to categorize the rhythm as either shockable (VF or VT), or non-shockable (PEA or asystole).
• If there's a shockable rhythm, deliver a shock of 4 joules per kilogram before immediately resuming high-quality CPR and then subsequently reassessing the rhythm after two minutes. If the shockable rhythm persists, continue that cycle: Shocks at 4 joules per kilogram every two minutes. There's no escalating shock strategy here.
• After the third and ongoing alternate shocks, deliver 10 micrograms per kg of adrenaline (0.1 ml per kg of one in 10,000 adrenaline). Also give Amiodarone: 5 milligrams per kg after the third and the fifth shocks.
• For a non-shockable rhythm, focus on high-quality CPR and adrenaline. Give 10 micrograms per kg of adrenaline as early as possible and then every three to five minutes after.
• For both sides of the algorithm, address the four H's and the four T’s.
Optimizing your approach to paediatrics
Let’s start with which skills to focus on. According to the UK National Cardiac Arrest Audit,2 which includes data from all paediatric arrests from 203 hospitals over the last six years, only 4.3% of patients presented in shockable rhythms.
That means, aside from addressing the H's and T's, focusing on ventilation and chest compressions.
Ventilation
As mentioned above, the first step after identifying cardiac arrest is opening the airway and delivering five rescue breaths. In the prehospital setting, those are likely to be delivered with a bag valve mask (BVM).
Select the right size mask, ensuring that it fits over the patient's nose and mouth whilst not extending below the chin or projecting up into the eye sockets to reduce risk of leaks. If possible, a two-person technique can help provide the best possible quality mask seal.
Attach the BVM to high flow oxygen. Do not consider titrating oxygen during CPR.
Although the BVM is likely to be first line method for delivering ventilations, supraglottic devices like the laryngeal mask airway (LMA) and the I-gel are an alternative for providers trained in their use.
The Guidelines focus on cuffed tracheal tubes in pediatric advanced life support. For intubated patients, once you've secured the tube, you can move to synchronous chest compressions, with ventilations now delivered at an age-targeted rate:
Infants 25 breaths/ min
1-8 yr olds 20 breaths/ min 8-12 yr olds 15 breaths/ min >12 yrs old 10-12 breaths/ min
Data to guide the decision of which device to use is limited. But some results suggest that better outcomes were achieved with BVM compared to either tracheal intubation or supraglottic airways. While far from definitive, these results suggest that you shouldn't rush to place an advanced airway if you can deliver good ventilations with a BVM.
On the other hand, resources can be limited in the prehospital setting and I-gels enable you to focus on other areas of arrest management. And while supraglottics don't seal the airway completely, they're also likely to reduce the amount of air entering the stomach, and therefore they will help to improve the efficacy of ventilations and provide some protection against passive regurgitation.
Research First 76 www.caa.net.au
Rate
For a BVM, the Resuscitation Council UK recommends a rate of 15 compressions to two breaths.1 If the trachea is intubated, deliver age-targeted ventilation rates and continuous compressions. It is unclear which strategy to adopt when using a supraglottic airway. If a continuous compression strategy is used, adherence to the guidelines on ventilation rates is important as over-ventilation can cause barotrauma to the lungs. This increases intrathoracic pressure, which can reduce venous return and reduce the efficacy of chest compressions. It can also fill the stomach with air, which impairs ventilation due to splinting of the diaphragm, or cause regurgitation. The decision on which strategy to use must be considered carefully on a case-by-case basis. Always adhere to the guidance on ventilation rates, which are difficult to assess accurately. An in-hospital observational study by Sutton, et al.3 found that none of the 47 paediatric patients who received ventilation during cardiac arrest had an average ventilation rate within the guidelines. Although this was an in-hospital study, you're probably kidding yourself if you think that these results won't be replicated out of hospital.
How can you address the problem of delivering ventilations accurately?
The first step is to raise awareness of the issue so that you can consciously focus on these parameters and try to adapt your practice accordingly. But when it comes to respiratory rates, there's no excuse for not achieving the recommended parameters because we should all be using end-tidal CO2 with every arrest.
The patient monitor displays an accurate ventilatory rate, which introduces another key issue: focus. If you're responsible for delivering the ventilation, that is your sole job. Don't get distracted or drawn into other clinical interventions or conversations.
Don't try and run the arrest from the airway if at all possible. You are breathing for the patient and optimizing their respiratory care. That is a huge responsibility.
Volume
The Resuscitation Council UK doesn't make any recommendations on tidal volumes, and the evidence on tidal volumes delivered during paediatric arrest is lacking.
In the absence of guidelines, it’s reasonable to extrapolate from the standard lung protective ventilation strategies, which advise delivery of 5 to 8 ml per kilogram.
For a typical five-year-old child weighing around 18 kilograms, that’s a tidal volume of six ml per kilogram. They'll need a tidal volume of 106 ml – significantly less than the volume that can be delivered using a paediatric BVM, which can easily approach 650 ml. Delivering the appropriate volume is not as easy as just squeezing the bag.
The European Resuscitation Council4 advises using only the force and total volume necessary to just make the chest rise. If you're doing continuous chest compressions, however, that is difficult to assess. Maybe we need to look to technology for the answer.
Real-time ventilation feedback, such as Real BVM Help® technology from ZOLL®, has a growing evidence base to support its use, although it has not been tested on paediatrics. In one adult manikin study5, paramedics who used real-time ventilation and chest compression feedback adhered to guideline recommendations for both respiratory rates and volume for 75% of delivered ventilations, compared to only 22% of ventilations delivered by the control group who didn’t have ventilation feedback. This technology has significant potential to improve the ventilations we deliver during paediatric arrest.

77
Chest compressions
As the second vital component of high-quality resuscitation, chest compressions should always be delivered with extreme focus. Pay attention to all components of each compression: rate, depth, and adequate time for full chest recoil.
Aim for a rate of between 100 and 120 compressions per minute for both infants and children. Compress the lower half of the sternum by at least one-third of the anterior posterior dimension of the chest – that's approximately 4 centimeters for an infant and 5 centimeters for a child.
Deliver compressions on a firm surface; otherwise, it will be difficult to achieve the depth of the compression. Focus on the release of pressure and allow for complete chest recoil when coming off the chest.
Minimize chest compression pauses so that 80% or more of the CPR cycle is comprised of chest compressions.
Unfortunately, the findings of chest compression studies echo those of ventilation studies, suggesting that we're not very good at adhering to the guidance.
One prospective observational study6 of children who received CPR in a pediatric intensive care unit using data from arterial waveform, found that the percentage of chest compressions with average rates that correlated with the guidance was 32.9%. Yikes - only one third of patients had the right chest compression rate delivered to them!
Are we any better at minimizing time off a chest? An observational study7 of CPR quality in two paediatric emergency departments reviewed videos of pediatric arrests to determine whether pulse checks adhere to the guidelines, which state that they should take no longer than 10 seconds. Over a 30-month period, 81 cardiac arrests were analyzed, which included 900 pauses. Of these 900 pauses, 22% were prolonged. That might not sound like much, but that's nearly 200 pulse checks that were too long.
So, our time off the chest isn't great either!
I'd like to address a related prehospital-specific issue. Often there's a temptation to leave the scene early when patients continue CPR to hospital. That temptation is exacerbated by the ease of moving these little people compared to adults.
That makes it even more important to question how good we are at delivering chest compressions during transport. A prospective cohort study from Russi, et al.8 analyzed adult patients in cardiac arrest both on scene and during transport. Data was collected with CPR feedback devices that analyze the rates and the depth of compressions.
The findings: During transport, the correct compression depth was delivered only 8% of the time and the correct rate was delivered only 11% of the time. While this data is based on adults, it’s hard to imagine how, in a moving vehicle, it would be any different in children.
So, how can you optimize chest compressions? Let's start with time off the chest.
Strategies can be used such as checking a single pulse site. For a child older than one, feel for a carotid pulse in the neck. For an infant, feel for a brachial pulse on the inner aspect of the upper arm. However, for both infants and children, the femoral pulse in the groin is also an option, which might help avoid confusion of where the check for pulses in the heat of the moment.
Have your fingers ready on the pulse site before compressions are stopped. Often you can feel a weak pulsatile flow when doing chest compressions; that can help you to identify the pulse sites.
Utilize cardiac arrest team leaders, who should have oversight over the whole arrest, whenever possible. They can monitor timings and pulse checks, and even provide guidance on chest compressions. Having someone who isn't involved in hands-on care, can often provide a more accurate overview than the person delivering the interventions.
Another way to improve the accuracy of chest compression rates is to use a CPR metronome. These are built into many monitors and provide a helpful audio guide.
Real-time CPR feedback technology, such as Real CPR Help® from ZOLL, is an increasingly common prehospital tool, offering guidance on compression rate and depth as well as time off the chest and whether or not complete recoil of the chest has occurred.
In a simulation-based study9 with three groups undertaking paediatric life support, Group One received feedback on their performance from an instructor.
Group Two used a real-time visual feedback device, and Group Three received verbal feedback from an instructor who was reviewing the trainee's performance using the visual feedback device.
The primary outcome of this study was the total compression score: a composite marker consisting of correct hand position, adequate depth, compression rate, and complete release per two-minute cycle.
Group One earned a total compression score of 82%, showing the value of a cardiac arrest team leader. However, Groups Two and Three both achieved scores of 92% – a statistically significant result. Another win for feedback devices.
Next, the issue of ineffective chest compressions during transport, the only option is to stay on scene and resuscitate. We've seen how poor our CPR performance is during transport. Leaving scene condemns a child to an inadequate resuscitation attempt. You wouldn't leave scene with an adult patient in arrest – don't do it with children. A study by Banerjee10 reports on a package of interventions that demonstrate the value of staying on scene for a period of time and not rushing off.
Research First 78 www.caa.net.au
The importance of training
Prior to 2014, Polk County Fire and Rescue, an ambulance service in Florida, provided rapid transport of all of their paediatric out-of-hospital cardiac arrests. Survival with good neurological outcome for these patients was zero percent.
To improve this dismal rate, PCFR completely restructured their approach to paediatric arrest, focusing on high-quality advanced life support on scene before making the decision to transport. To facilitate this shift, they embarked on a simulation-based, interactive training program that focused on improving paramedics' confidence and addressing emotional challenges. The result? Mean on-scene times increased by only three minutes, but neurologically intact survival rates rose from zero to 23%.
So don't rush away from scene. Take the time to deliver impeccable paediatric advanced life support on scene before you make any transport decisions.
Finally, I’d like to acknowledge the fact that paediatric out-of-hospital cardiac arrest is rare. Approximately 500 cases happen each year in England, compared to about 30,000 adult arrests.11 That reality increases the anxiety around attending these cases, exacerbated by core skill fade, which further erodes confidence.
Training is clearly the answer, but how often should we be doing life support courses? Studies show that CPR skills begin to deteriorate just months after completing these courses, so more regular training is strongly recommended. Take a few minutes whenever you can to run through a paediatric arrest scenario with a manikin – it doesn't have to be complicated or prolonged; just take the time to refresh your memory and practice your skills.
Be critical of your performance, use technology, and focus on delivering every element of the resuscitation in an exemplary fashion. You are the prehospital resuscitation expert, and delivering an excellent pediatric resuscitation is in your hands.
References
1. Resuscitation Council website, www.resus.org.uk. Accessed 17 August 2022.
2. Skellett S, Orzechowska I, Thomas K, Fortune PM. The landscape of paediatric in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2020;155:165–171.
3. Sutton RM, Reeder RW, Landis WP, et al. Ventilation rates and pediatric inhospital cardiac arrest survival outcomes. Crit Care Med. 2019;47(11):1627–1636.
4. European Resuscitation Council, www.cprguidelines.eu/assets/guidelines/ European-Resuscitation-Council-Guidelines-2021-Pa.pdf. Accessed 17 August 2022.
5. Lyngby RM, Clark L, Kjoelbye JS, et al. Higher resuscitation guideline adherence in paramedics with use of real-time ventilation feedback during simulated out-of-hospital cardiac arrest: A randomized controlled trial. Resusc Plus. 2021;5:100082.
6. Sutton RM, Reeder RW, Landis W, et al. Chest compression rates and pediatric in-hospital cardiac arrest survival outcomes. Resuscitation. 2018;130:159–166.
7. O’Connell KJ, Keane RR, Cochrane NH, et al. Pauses in compressions during pediatric CPR: Opportunities for improving CPR quality. Resuscitation. 2019; 145:158–165
8. Russi CS, Myers LA, Kolb LJ, Lohse CM, Hess EP, White RD. A Comparison of Chest Compression Quality Delivered During On-Scene and Ground Transport Cardiopulmonary Resuscitation. West J Emerg Med. 2016; 17(5):634–639

9. Wagner M, Bibl K, Hrdliczka E, et al. Effects of feedback on chest compression quality: a randomized simulation study. Pediatrics. 2019;143(2):e20182441.
10. Banerjee PR, Ganti L, Pepe PE, Singh A, Roka A, Vittone RA. Early on scene management of pedicatric out-of-hospital cardiac arrets can result in improved likelihood for neurologically-intact survival. Resuscitation. 2019; 135:162-167
11. Out-of-Hospital Cardiac Arrest Outcomes Registry Epidemiology Report, 2018: English Ambulance Services.” University of Warwick website, 2019. https://warwick.ac.uk/fac/sci/med/research/ctu/trials/ohcao/publications/ epidemiologyreports/ohcao_epidemiology_report_2018_published.pdf. Accessed 17 Aug 2022.
79
is improving itsenvironmental footprint
Every single day the people of Hato Hone St John are working with communities across Aotearoa New Zealand.
Our people can be found throughout the motu (country), on every corner. They're all sorts and all ages, those whose families have lived here for generations, and those who have chosen Aotearoa New Zealand more recently to be their home. What draws us together is our common purpose: to make life-changing differences with our communities.
Building Sustainability for Future Generations is one of Hato Hone St John’s strategic aims. Environmental sustainability is considered within Hato Hone St John’s Maanaki Ora Strategy and is core to our Environmental Sustainability/Kaitiakitanga (Guardianship of the sky, sea and land) Strategy.

Direct impacts of climate change, such as floods and storms can increase drowning, respiratory conditions, and waterborne infectious diseases, whilst biologically mediated (such as those that occur through a biological or natural mechanism or carrier), impacts can increase spread of viruses and disease, and socially mediated impacts can increase inequality, access to healthy food and housing and disrupted education.
We understand that human health and environmental health are interdependent, and there are significant potential health gains of ambitious and effective climate action - creating stronger, more resilient, and more equitable communities.
In M aori culture, there is an intrinsic relationship between people, identity, culture and aio (place). Harm to the environment or relationships with the environment can negatively impact M aori health, wellbeing, and equity. The natural environment is a taonga (treasure) and must be protected.
Over the next five years we will increase our understanding of the impact our organisation has on the environment and aim to reduce our carbon emissions and improve sustainability across our transport, property, waste, procurement, and supply chain functions. Our short-term goal is to become carbon reduce certified in 2023 and then to progress toward net carbon zero in years to come.
Hato Hone St John
Sustainability
www.caa.net.au80
Although this is just the beginning of St John’s environmental sustainability journey, there have been strides in sustainability which include:
• St John have recently been trialing recycling of disposable facemasks, with the materials being used by third party manufacturers to make various new products – such as outdoor furniture and park benches. This important step will help to divert waste from landfill where these masks can take around 450 years to biodegrade.
• We have also introduced 99+ hybrid vehicles on the road. By the end of 2024, we have forecast for 100 percent of St John SUV and smaller vehicles to be hybrid for models that have that option.v
• Our St John Retail Stores played a huge role in the reuse of 1.5 million items per year
• The St John digital programme, which includes First Aid training, has seen around 200,000 paper transactions per year removed.
Looking ahead, we would love to see environmental sustainability incorporated as part of everyday business practice in all areas of Hato Hone St John, providing a lens for decision making and becoming normalised within our organisational culture.

Manaaki
(Take care of the people, take care of the land, and we can all move forward together).
tangata, manaaki whenua, haere whakamua.
81
community
SA Ambulance Service donatesDefibrillators to Ukraine
SAAS proudly donated 70 decommissionedMRX defibrillators to Ukraine to offersupport to Ukrainian communities in lightof recent events. Messages of support werealso hand-written on the boxes for thehealth care workers who will receive themuch-needed aid.
NAIDOC Week
Queensland Ambulance Service (QAS) was proud to be involved in several NAIDOC week events, celebrating the history, culture, and achievements of Aboriginal and Torres Strait Islander peoples. QAS crews were kept busy at the Townsville NAIDOC march and celebrations with almost 1000 CPR sessions across the week.

ACTESA Assistant CommissionerWayne Phillips, ACTF&R Chief OfficerMatthew Mavity, and ACTSES ChiefOfficer Anthony Draheim took part inthe Vinnies CEO Sleepout. They raisedover $5,000 with funds going directlytowards providing people in need withvital access to food and accommodation.

SA Ambulance supports International Men’s Health Week


International Men’s Health Week is a week that focuses on promoting physically, mentally and SA Ambulance shows support and engages with men’s physical and mental health initiatives all year round, but used the week to really help raise critical awareness around all aspects of men’s health, especially in the ambulance sector.

It’s Not the Kind of Emergencythat Needs Lights and Sirens,but one Equally as Important
#WomenInAmbulance #inthistogether #charitygolf #lovefromWA #WorldEnvironmentDay #bakeoff #stayathome #PeopleFIRST #SustainableAmbulance #HandHygiene #HandHygiene #NationalVolunteerWeek20 #restartaheart #restartaheart #MeFirst #WomenInAmbulance #inthistogether #dogsofambulance #lovefromWA #WorldEnvironmentDay #WorldEnvironmentDay #stayathome #StJohnDay #PeopleFIRST #HandHygiene #NationalVolunteerWeek20 #restartaheart #restartaheart #WomenInAmbulance #WomenInAmbulance #inthistogether #dogsofambulance #dogsofambulance #lovefromWA #lovefromWA #lovefromWA #WorldEnvironmentDay #stayathome #stayathome #StJohnDay #PeopleFIRST #PeopleFIRST #SustainableAmbulance #HandHygiene #HandHygiene #HandHygiene #HandHygiene #ThankAFirstResponder #NationalVolunteerWeek20 #MeFirst #MeFirst #MeFirst #dogsofambulance #charitygolf #charitygolf #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #bakeoff #stayathome #StJohnDay #StJohnDay #StJohnDay #StJohnDay #PeopleFIRST #SustainableAmbulance #ThankAFirstResponder #ThankAFirstResponder #restartaheart #restartaheart #restartaheart #restartaheart #MeFirst #MeFirst #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #dogsofambulance #dogsofambulance #charitygolf #bakeoff #bakeoff #bakeoff #stayathome #stayathome #stayathome #PeopleFIRST #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst #WomenInAmbulance #WomenInAmbulance #inthistogether #dogsofambulance #charitygolf #bakeoff #bakeoff #bakeoff #bakeoff #stayathome #PeopleFIRST #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #NationalVolunteerWeek20 #MeFirst #MeFirst #MeFirst #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #inthistogether #charitygolf #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #bakeoff #bakeoff #bakeoff #bakeoff #bakeoff #stayathome #stayathome #stayathome #stayathome #StJohnDay #StJohnDay #StJohnDay #PeopleFIRST #PeopleFIRST #PeopleFIRST #PeopleFIRST #SustainableAmbulance #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder#ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #restartaheart #restartaheart #restartaheart #restartaheart #restartaheart #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst People First EmergencyServicesBloodChallenge inMostCAAmemberservicesaretakingpart encouragingtheEmergencyServicesBloodChallenge, everyonewhocantodonate bloodbeforethechallengeends.Picturedis Ambulance Tasmania CEO Joe Acker who kickedoffthechallengeforAmbulanceTasmania.
Our
82 www.caa.net.au
Thank a First Responder Day
On 8 June 2022, all Australians were asked to take the time out to say thank you to the 300,000 first responders who risk their lives protecting the communities in which they live. NSW Ambulance were delighted to receive a special delivery of hampers from a team of children and elderly to mark Thank a First Responder Day. The gifts facilitated by not-for-profit organisation ‘Little Helpers’ will be distributed to flood affected ambulance stations across the state.
St John PNG Educate (and Feed)
the Local Community
St John Ambulance PNG was invited to host a sausage sizzle at the Theodist carpark, helping raise funds to subsidize the cost of providing free emergency pre-hospital care. They took the opportunity to also train customers, provide knowledge required to perform life-saving CPR, respond to emergency situations, and manage unconscious casualties.

As part of the Premier's Reading Challenge, St John WA unveiled, Land of Legends, a book about hope, inspiration, kindness, and the many events and rescues the St John WA team attend. The Premier’s Reading Challenge sought out author Deb Fitzpatrick and paramedic Derek to read and teach children the great acts of kindness paramedics contribute.

St John WA
Wellington Free Ambulance Launch Onesie Day Ambulance

A unique Onesie Ambulance (because Wellington Free Ambulance are the 111s!) launched for Wellington Free Ambulance. Fundraised by the community for the community, our supporters donated over $300,000 to fully fund this emergency ambulance vehicle.


Push Up Challenge
Run by ‘The Push for Better Foundation’, the Push Up Challenge aims to raise awareness and engage people in mental health through connection, education and health and wellbeing. Throughout June, Ambulance Tasmania’s incredible EMSO team members managed to drop down and give a whopping 18,759 press ups and raise a huge $3,170.
#dogsofambulance #charitygolf #charitygolf #bakeoff #StJohnDay #StJohnDay #SustainableAmbulance #HandHygiene #ThankAFirstResponder #NationalVolunteerWeek20 #NationalVolunteerWeek20 #restartaheart #restartaheart #MeFirst #WomenInAmbulance #dogsofambulance #dogsofambulance #charitygolf #stayathome #StJohnDay #PeopleFIRST #SustainableAmbulance #restartaheart #restartaheart #MeFirst #bakeoff #stayathome #PeopleFIRST #PeopleFIRST #HandHygiene #ThankAFirstResponder #NationalVolunteerWeek20 #MeFirst #MeFirst #MeFirst #WomenInAmbulance #dogsofambulance #charitygolf #charitygolf #charitygolf #lovefromWA #WorldEnvironmentDay #WorldEnvironmentDay #StJohnDay #StJohnDay #SustainableAmbulance #HandHygiene #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #restartaheart #restartaheart #restartaheart #MeFirst #MeFirst #WomenInAmbulance #inthistogether #lovefromWA #WorldEnvironmentDay #bakeoff #bakeoff #bakeoff #bakeoff #stayathome #stayathome #stayathome #stayathome #SustainableAmbulance #HandHygiene #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst #WomenInAmbulance #WomenInAmbulance #lovefromWA #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #bakeoff #bakeoff #bakeoff #stayathome #stayathome #stayathome #SustainableAmbulance #SustainableAmbulance#HandHygiene #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #WomenInAmbulance #lovefromWA #WorldEnvironmentDay #WorldEnvironmentDay #WorldEnvironmentDay #bakeoff #bakeoff #bakeoff #bakeoff #bakeoff #stayathome #stayathome #StJohnDay #StJohnDay #SustainableAmbulance#HandHygiene #ThankAFirstResponder #ThankAFirstResponder #ThankAFirstResponder #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #NationalVolunteerWeek20 #restartaheart #restartaheart #restartaheart#restartaheart #restartaheart #restartaheart #restartaheart #MeFirst #MeFirst #MeFirst #MeFirst #MeFirst
83
CQU
CQUniversity believes higher education should be for everyone. Our accessibility, flexibility, student support, and wide range of courses available online and on campus help our students be what they want to be.
cqu.edu.au

Ferno
The only organisation in Australia specialising in the supply of a complete suite of products to meet the needs of Ambulance, Emergency, Rescue, and Height Safety. Trusted supplier to Emergency Services, Government Hospitals, and general industry for more than 40 years.

ferno.com.au NEANN
Through the NEANN brand RAPP Australia Pty Ltd specialises in designing, manufacturing, and distributing a wide variety of products for use in the wider emergency services industry throughout Australia and overseas.
neann.com.au

ORH
Supporting ambulance services in Australia for over 20 years, we have helped solve station location problems, quantify demand and capacity challenges, and set efficiency targets throughout our consultancy-based approach. orhltd.com
Philips
Philips is a health technology company focused on improving people’s lives through meaningful innovation across the health continuum – from healthy living and prevention to diagnosis, treatment, and homecare. philips.com.au/healthcare
Pulsara
Pulsara is a mobile-first telehealth and communication platform that connects teams across organizations. What makes Pulsara unique is its ability to enable dynamic networked communications for any illness or injury. pulsara.com

Stryker

For decades, we’ve been focused on innovations that help improve patient outcomes, help prevent caregiver injuries, and increase operational efficiencies so you can do what you do best: save lives. stryker.com/au/en Corvanta

Corvanta partners with out-of-hospital care providers, to advance and deliver the technology they need to deliver timely, integrated, patientcentric services to improve healthcare outcomes.
corvanta.com


84 www.caa.net.au
ZOLL
ZOLL® Medical Corporation, an Asahi Kasei company, develops and markets medical devices and software solutions that help advance emergency care and save lives, while increasing clinical and operational efficiencies. With products for defibrillation and cardiac monitoring, circulation enhancement and CPR feedback, supersaturated oxygen therapy, data management, ventilation,
and therapeutic temperature management, ZOLL provides a comprehensive set of technologies that help clinicians, EMS and fire professionals, as well as lay rescuers, improve patient outcomes in critical cardiopulmonary conditions.

www.zoll.com/au
Tactical Medical Degrees
Learn to deal with acute trauma situations and be uniquely qualified to respond in resource limited, dynamic and high threat environments with a qualification in Tactical Medicine. These online, highly flexible courses are ideal for paramedics and first-responders. Gain the critical skills needed to assess, plan, prepare and implement strategies for successful operations and patient management within a tactical environment. www.cqu.edu.au
Integrated Patient Care Records
The next generation of ePCR, the Corvanta iPCR is our complete, end-to-end solution for the out-ofhospital care sector – from the emergency call to the clinical handover. It’s the only solution of its kind. The Corvanta iPCR is more than a patient record system; the solution is also an intuitive decision support tool capable of improving patient safety and decision support, increasing operational resource availability, streaming of diagnostic quality vital signs, a seamless transfer of records, and more! Our iPCR technology is used by over 12,000 paramedics, is installed in 2,700 ambulances, and handles over 200,000 patients every month. corvanta.com
CAA helps provide an important link between the ambulance sector and businesses that provide goods and services for this industry. It’s instrumental in providing networking and partnering opportunities. Don’t hesitate to reach out to organisations of interest.
Interested in becoming a part of The Directory? Contact partnerships@caa.net.au

85
The Five Stages of Learning and How to Apply Them To Any Skill
Mitch Mullooly
Health and Wellness Strategist

Specialising in the wellbeing of first responders, Mitch is Council member of Te Kaunihera Manapou, New Zealand Paramedic Council; Advisory Board member for Te Kiwi Maia, The Courageous Kiwi; and proud CAA2020 Women in Ambulance honour recipient.
Mitch is also a published author, speaker and feature columnist for several sector related magazines, blogs, webinars, and podcasts.

Wellness First
www.caa.net.au86
Beginning a new learning journey can be exciting. Beginnings are full of hope and possibilities. Starting something new can give us a glimpse of what could be if we stick with something long enough to see it through.

I’ve been a beginner many times in my life, and most recently, training for a marathon. When I first started training, I was excited and hopeful about the possibilities ahead of me, and the challenge. Then came the rude awakening of just how long and winding of a road I had ahead of me. It’s not uncommon for the stark reality of running 42kms to become extremely overwhelming, and then not see it through. My training has already been very stop/start due to the ongoing restrictions and cancellations of events.
Still, I haven’t let that dampen my enthusiasm for achieving my goal, which is more about the mental achievement than the physical one. In the past, I tried to skip steps to attempt to speed up the learning process. But I’m now wise (or old!) enough to know that being grounded in reality and starting where I am currently at, will result in faster progress than trying to rush through.
This up and down cycle doesn’t just apply to learning the mindset hacks of an endurance race. Psychologists have found certain universal stages that apply to all new learning. Whether you’re learning a new sport or athletic skill or taking up art, business, or music, there are five distinct stages to learning anything new. Becoming aware of these learning stages and knowing that what you’re going through is completely normal may help you push through the sticking points of the learning process and keep going, even when you might have otherwise given up hope and quit.
A certain naïveté is prerequisite to all learning. A certain optimism is prerequisit to all action.”
George Leonard
87
Stage One: Unconscious Incompetence
The first stage of learning is called unconscious incompetence. In this stage of learning, we don’t know what we don’t know. Usually, we are filled with hope and optimism for our new pursuit. Every little thing we learn feels like we are doubling our knowledge base. And for a good reason: we probably are. For most people, whether you’re trying to learn a new language, play a new instrument, or learn a new skill, this first stage of learning starts as fun and exciting. In the beginning, any flashes of success feel monumental.
Once you know just enough to get by, you can start experimenting a little, making it even more fun. You’re not judging yourself yet because you don’t have enough knowledge yet to do so. Because you only know a little, you aren’t thinking much, which makes you more likely to catch small moments of flow; those magical moments when you lose track of time, and everything feels right with the world.
This is the most fragile stage of learning for two main reasons:
First, it’s common to believe you’re further along than you are. In psychology, this is known as the Dunning-Kruger effect. Many beginners may even get bored and lose interest during this stage, thinking they know so much that there’s no challenge to be had. On the contrary, they just don’t know how much they don’t know yet.
Second, because you think you know more than you do during this stage, what you do know is inadequate and unlikely to give you the results you want. Again, this ties back to not knowing how much you don’t know.
Whatever the reason, many people make excuses during this early stage of learning because it feels easier than confronting reality: you have a long road ahead of you, and you don’t have enough knowledge to start on your own. Both reasons make this blissful beginner stage the one during which most people give up.

Stage Two: Conscious Incompetence
Once you get past the unconscious incompetence stage, if you make it that far, and many people don’t, you arrive at the second stage of learning, or the conscious incompetence stage.
This is the rude awakening you get when you realise all you don’t know. For many people, if they didn’t already quit in the blissful beginner stage, this second stage, or what I call the suck, does them in.
The suck is where it slowly dawns on you just how much you don’t know. You start learning the rules of the game. You start trying to apply those rules, and as you do, get more in your head. You start to force things and can no longer get into flow. Even if you are making progress, you may feel like you’re going backwards because you’re now aware of all you’re doing wrong.
This is also the stage where most people get overwhelmed at the magnitude of their undertaking and daunted by the long road ahead. So how do you make it through the suck? Accept that it’s inevitable. Learn to recognise it and trust that you will make progress with time and intentional practice.
Wellness First 88 www.caa.net.au
Stage Three: Conscious Competence
If you’re one of the few that make it past the suck, you then reach the next stage of learning: conscious competence.
During the conscious competence learning stage, you know how to reach your goal but have to concentrate hard on your task. Nothing is automatic.

In this stage, your new learnings are still fragile and not yet cemented in your neural circuits, meaning you haven’t committed your new learning to your long-term memory.
Because of this, you have to practice diligently and often or risk forgetting what you’ve learned. The key in this stage of learning is to keep practicing. Consistent, focused practice is what will help make those conscious learnings automatic.
Stage Four: Unconscious Competence
Stage four of learning is when you fully internalise all that you’ve learned. You can execute your new skills automatically and without having to think beforehand. This is the stage of learning when you’re most likely to regularly get into the zone because you can stop thinking so much. Instead, you just let your body or mind take over and do what you already know how to do. Whatever your new skill, this is when things feel less like a struggle and more flowy. Reaching this stage starts to feel fun and rewarding, like all your hard work has finally paid off.
Stage Five: Conscious Unconscious Competence
The last stage of learning is when you can teach what you do unconsciously to others. It requires a deep understanding of what you’ve learned and an ability to communicate it to beginners.
Many people never get here, and the reality is that the younger you learned, the less likely you will be able to teach well. This is why high-level athletes that have been training since they were young are not always the best teachers. They have so deeply internalised all they’ve learned that they’re not always sure how to teach it to others.
On the contrary, some of the best coaches are people who learned their skill or sport slightly later in life. This is because they can still remember those early, uncomfortable stages of learning and better emphasize with beginners.
No matter where you’re at in the learning process, try not to get discouraged or think you need to jump steps. Put in the time and don’t give up in each stage.
And keep going… you’ve got this!
89



MCN EP 2101 0356 • Immediate post-call data deliver y: quickly and seamlessly transmit essential clinical data • Same-day debriefing: review all data related to patients in respirator y distress and sudden cardiac arrest events • System-wide quality improvement: identify trends and areas for improvement • Training metrics: establish quality standards for training purposes ZOLL ® RescueNet CaseReview suppor ts Ambulance Crews by providing insights that can help providers improve patient outcomes. © 2022 ZOLL Medical Corporation. All rights reserved. RescueNet and ZOLL are trademarks or registered trademarks of ZOLL Medical Corporation in the United States and/or other countries RescueNet® CaseReview PR O V ID I NG I NS I GH T S T O IM P RO V E OUTCO M E S For more information, call 1800 605 555 or email: info.aus@zoll.com
Mingle
An incredible opportunity to mingle with friends and colleagues from within the pre-hospital sector.

Reflect
On the night CAA will walk you through the past 60 years of milestones and innovations decade by decade, sharing top stories and achievements over the years.




Learn
Our guests will be gifted with a commemorative 60th anniversary book which will share the case studies mentioned throughout the night and expand more on the variety of achievements and innovations within CAA from 1962 to 2022.
Support
Aiming to raise funds to allow CAA to continue to provide helpful programs, resources, and campaigns, the 60th Gala will host both a silent and live auction for all to get involved in, both through donation and bidding.

Join us in celebrating CAA’s 60th Anniversary Gala 17 November 2022
