The official newsletter of the Dental Hygienists Association of Australia Ltd


The official newsletter of the Dental Hygienists Association of Australia Ltd

Remembering the achievements of a forty-year career devoted to oral hygiene

Discover how chronic kidney disease is linked with oral health

the dream
We ask; is it okay for your job to be ‘good enough’?
in your local area

Available in autoclavable plastic and stainless steel T


plastic
previously hidden in the gap between tip is shown in between the below the contact point. Pull the area. second black band on the handle
Withdraw the probe 4mm and observe the black or white
(For example, in the picture below - see pic 3, the second teeth for easy visualisation, but in real life, it is hidden between
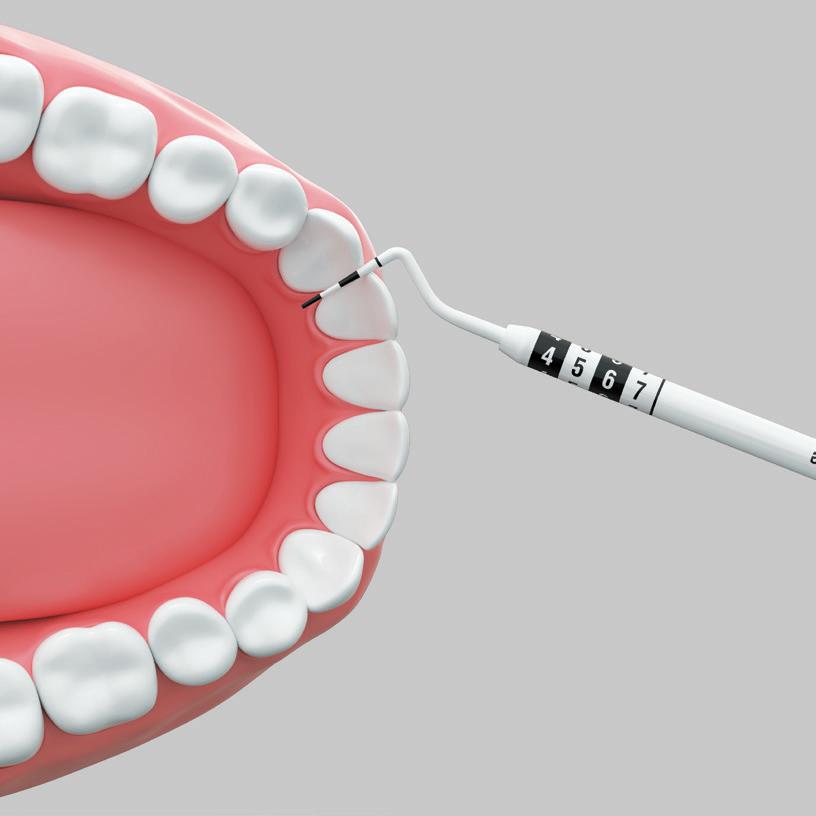



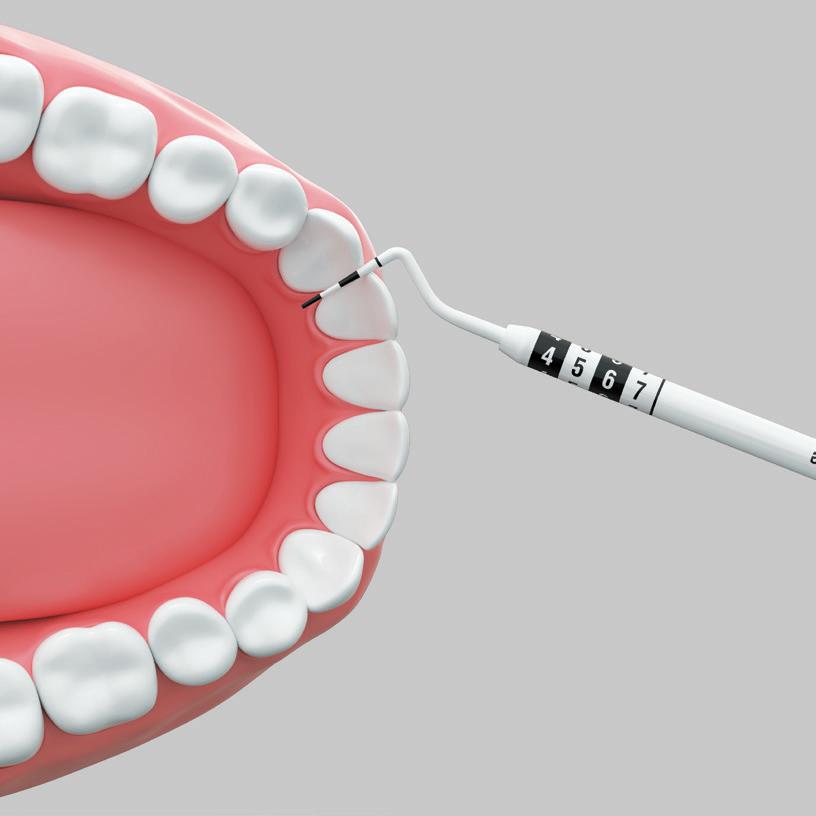





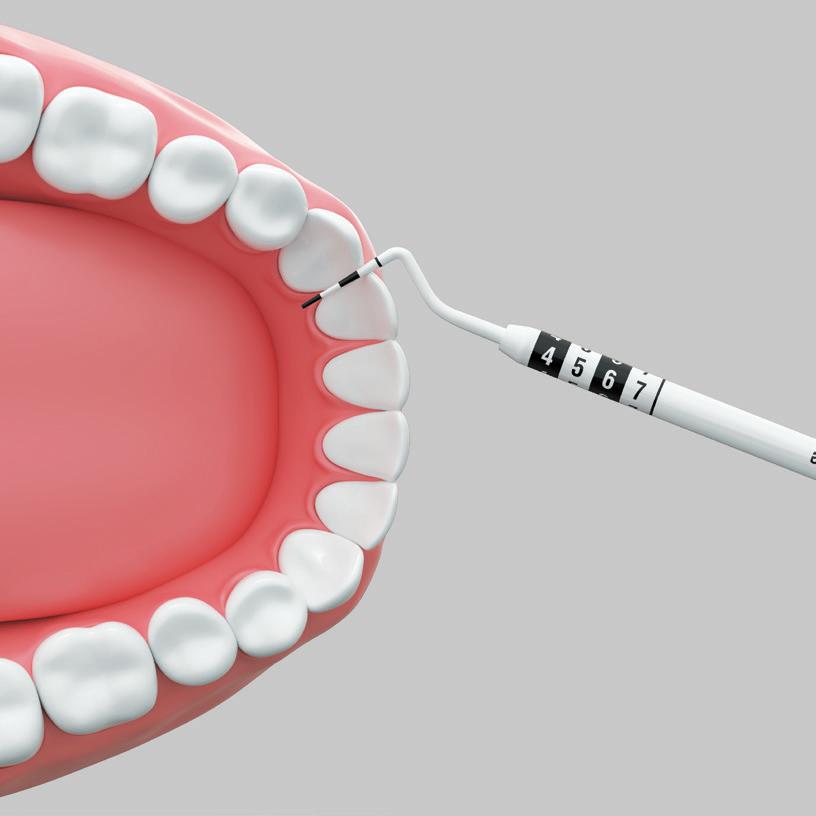












In this example the second black band on the probe corresponds






4.
This gap would use a size 6 Pikster.
In this issue, Margie Steffens OAM reflects on her stellar career. She has focused on equity in oral health care and we trust that her legacy continues. We thank her for her long and committed service to the DHAA and oral health community.
National Volunteers Week is coming up in May and I would like to acknowledge and thank our member volunteers, who without, we couldn’t achieve all that we do.
This is the time of the year that many state committee office bearers change over. We thank our retiring position holders for their time, enthusiasm and dedication to the DHAA and warmly welcome their replacements (see below).
Stepping down
• WA Chair - Carmen Jones
• WA Deputy Chair - Rhonda Kremmer
• VIC Chair - Desi Bolado
• VIC Deputy Chair - Aimee Mills

• SA Deputy Chair - Sally Hinora
• QLD Chair - Lizzy Horsfall
• NSW Chair - Jody Inouye

Stepping up
• NSW Chair - Jinous Eighani-Roushani

• TAS Chair - Karen Lam
• VIC Chair - Cathryn Carboon
• VIC Deputy Chair - Sarah Laing

• SA Deputy Chair - Courtney Rutjens
• QLD Chair - Stacey Billinghurst

• QLD Deputy Chair - Karen Smart
Please note: There are still vacancies for WA Chair/Deputy Chair and NT Chair
The DHAA continuously advocates for its members and the profession. Some of the issues your volunteer representatives have responded to over the last 12 months include: Federal Budget Submission 2022 & 2023; Department of Health - Dental Feasibility Study; A radiation regulations and code update; Child Dental Benefits Schedule Consultation; Provider Number Expert Advisory Group; Dental Board of Australia – position statement on Minamata Convention on Mercury and consultation on accreditation arrangements; support for Dietitians Australia National Nutrition Strategy; and South Australia Oral Health Plan
I would also like to remind you of the comprehensive range of products and services that the DHAA provides members with. These include; 20 hours of free CPD; the annual National Symposium and face-to-face events; peer support service; IR support service; jobs board; consumer resources and information; competitive professional indemnity insurance; plus The Bulletin, our regular professional newsletter.
Over the past year, the DHAA has recognised outstanding achievements by students at across the country.
Our National Salary (workforce) Survey is being conducted this year through the University of Sydney and has been circulated to DHAA members. Please respond when it hits your inbox as this establishes market rates for us all.
I hope 2023 started well for you and continues to be an excellent year.
Michelle Kuss DHAA Acting President/TreasurerKey Contacts
04 The power in your punch
An overview of the DHAA’s positive advocacy activity.
08 From the top
CEO Bill Suen shares the credit for recent successes.
09 Minding our language
The DHAA are supporting an innovative oral health project
10 Get your CPD fix online
Improve your skills and knowledge from home.
14 Ask DHAA
Your questions answered.
COVER STORY
16 Margie Steffens
Looking back at a stellar career full of achievement and recognition.
24 Living the dream
We ask; Is it okay for your job to be ‘good enough’.
26 First year out
A reflection on the first-year experiences of graduates.
30 Smile Squad
The new initiative looking to keep students smiling.
32 Acute kidney disease
How is chronic kidney disease linked with oral health?
38 State of the Nation
A countrywide round-up and 2023 event calendar.

Thanks to the persistence and dedication of DHAA members advocating for our profession over the years. We have achieved a significant milestone in acquiring access to Medicare provider numbers in July 2022. There are many other advocacy areas that the profession requires, and the DHAA has been working constantly to raise awareness and knocking on doors to have these matters heard.
The DHAA is an active member of the National Oral Health Alliance and the Victorian Oral Health Alliance. In addition, our state committees are proactively involved in local advisory committees and working groups in WA, SA, Qld and Vic to review various oral health plans and funding models. Through these activities, the DHAA supports the call for an increase in
With so much going on behind the scenes in our industry, it’s good to know that the DHAA advocacy team are in your corner
By Bill Suen
Some of the advocacy
activities that the DHAA undertook on behalf of its members and the profession
n 2023 Federal Pre-Budget Submission
DHAA provided a written submission calling for budget allocations in aged care and oral health promotion.
n Increasing dental and oral health training in rural and remote Australia feasibility study
DHAA participation in various focus groups –click here
n Review of the List of approved qualifications from overseas jurisdictions
DHAA provided an online submission – click here
n Australian Dental Council Board, FARM Committee, Accreditation and Assessment Committee vacancies
DHAA supported members’ applications to various roles.
n Dental Board of Australia
The president and CEO meet with DBA chair Dr Murray Thomas annually and as required.
n Dental Council of NSW
DHAA president and CEO met with the Council and provided support and access to professional material and resources for the Council.
n Position statement on Minamata Convention on mercury
DHAA provided a written submission to support the position.
n Evaluation of the Dental Practitioner Support Service
DHAA provided a written submission to review the service.
n Australian Radiation Protection and Nuclear Agency
DHAA sent a written request for the outdated standards to be updated and followed up with phone communications.
n Review of DBA Factsheet
DHAA provided online comments.
n Radiation Safety Victoria DHAA communicated with the Victorian Health Department to seek clarification on the use of lasers by Victorian dental practitioners.
Commonwealth and State government funding for public dental services to address the service gaps and waiting times.
The DHAA has taken the lead in setting our goals to have 50% of all residential aged care facilities in Australia receive regular onsite oral health service by 2026. To achieve this goal the we have been working on the following fronts:
n Department of Veterans Affairs
Communication sent to seek access to the DVA dental benefits with follow-up communications.

n Review of Guidelines on infection control
DHAA provided a written submission to the Dental Board.
n Review of Ahpra Data Strategy
DHAA provided an online submission.
n Review of the Aged Care Quality Standards
The DHAA participated in focus groups as well as providing a written submission.
n Commonwealth Department of Health and Aged Care Compliance Assessment Branch Providers Benefits Integrity meeting
DHAA is a member and attended the meeting to discuss relevant issues in relation to provider numbers and item codes.
n Child Dental Benefits Schedule Consultation
We provided a written submission.
1 Establishing an aged care chapter to provide support and resources to members to service the aged care sector.
2 Provide a flexible online aged care education program to provide oral health practitioners with the skills and knowledge to navigate the aged care system and meet the special needs of the older population.
3 Advocate the provision of onsite
n SA Environmental Protection Authority Consultation Draft Radiation Protection and Control Regulations 2022 and Codes of Compliance - DHAA attended the consultation meeting and sent a written submission.
n WA Oral Health Advisory Council
DHAA is a member of the Council and participated in regular meetings to provide advice to the WA Health Department on oral health matters.
n TGA Personalised Devices Dental Sector Working Group
DHAA is an active member and participated in discussions on the impact and follow-up actions for the implementation of the new personalised device guidelines.
n ACT Department of Health Allied Health Forum
We provided a presentation on our aged care project.
n SA Oral Health Plan Monitoring Group
DHAA is a member and participated in regular meetings to provide advice to the SA Government.
oral health service to residential aged care facilities and provide business to business marketing of this service to aged care providers.
4 Advocate for a senior dental benefits scheme.
With the gradual return to the endemic phase, the DHAA has commenced talks with a number of aged care providers, both government and private, to explore opportunities
on behalf of our members to provide onsite oral health service to residents of various aged care facilities.

We have also made written submissions to advocate for more prescriptive accreditation standards on oral health for aged care facilities.
The DHAA is constantly exploring opportunities to advocate for oral health promotion. This approach has been embedded in many of our submissions and activities. The DHAA 2023 Federal Budget presubmission, for example, calls for “A preventative, maintenance and minimal intervention approach to reduce the burden on the clinical paradigm that has shown to be ineffective within the current system”. Our recommendations include the provision of incentive payments to “entice and support oral health practitioners to establish their onsite oral health service to residential aged care facilities”, to «develop a multi-lingual website with oral health information and instruction”, and to “award a grant for oral health professionals to develop health promotion activities among CALD population groups”.
Ongoing work is being conducted to liaise with individual health funds to support the implementation of their systems to recognise the Medicare provider numbers for our profession. There are also issues that require clarification and negotiations with each fund such as specialist treatment plan claims.
The expert advisory group provides an avenue for stakeholders to review, discuss and recommend activities to foster the implementation and uptake of the provider numbers through the transition phase.
The DHAA is a member of the Dental Board of Australia Dental Stakeholder Liaison Group which meets regularly to discuss practice issues and consult on regulatory and policy reviews
and changes. It has made written submissions on behalf of our profession and our members to both the Dental Board and Dental Council.
Besides the Dental Board of Australia, there are many regulatory bodies responsible for practices that oral health practitioners are involved in. These include radiation, laser and drugs and poisons as well as therapeutic goods. Over the past year, the DHAA has had communications with various state and territory governments, the Commonwealth Department of Health and Aged Care, The Department of Veteran Affairs, the Therapeutic Goods Administration (TGA) and the Australian Radiation Protection and Nuclear Agency (ARPANSA) to advocate for our members’ treatment rights in OPGs, anaesthetics and other related matters. n
“The DHAA is constantly exploring opportunities to advocate for oral health promotion. This approach has been embedded in many of our submissions and activities”
3 days of CPD
5 exciting workshops
3 social networking events
Some of our exciting speakers:
- Dr Trudy Lin
- Geraldine Moses
We will explore the many ways these concepts can be interpreted - such as working with vulnerable groups to support their needs & human rights, investigating new and emerging technologies, working towards sustainability in dental and other settings, and our social responsibilities as practitioners. ADELAIDE

- Dr Sharon Liberali and Deirdre Flynn
- Dr Sarah Kelly
- Cathryn Carboon
21ST - 23RD SEPTEMBER 2023
The DHAA has supported its members through some of the hardest times and made significant advances for our profession. These successes are a credit to both the association and to the members that support us. High-fives all around
 Bill Suen DHAA CEO
Bill Suen DHAA CEO

TIME FLIES AS I reflect on my nearly four years on the job as the CEO of DHAA since May 2019. Our profession has changed so much with the waves of challenges that kept coming.
First was the declaration of the pandemic that triggered a series of challenges to the profession in terms of restricted practice to avoid aerosol transmission of the virus, the mandatory vaccination requirements that were further complicated by the different state and territorial governments all going their own ways with the applications of all these measures. The impact of all these included a surge of industrial relation matters that members sought advice on due to redundancies and entitlement disputes, followed by financial hardship to many. The DHAA provided exceptional services to its members throughout this period and offered prompt pandemic information, IT advice, and also raised many practical issues with the employer groups and the various Commonwealth and State Governments while liaising with key professional bodies for consistent messaging across our industry. The DHAA also dug deep in its reserve to offer both discounted and deferred membership and PI insurance renewal. The DHAA peer support
network was also found to be very useful in providing comfort to many who utilised it at the time.
Many face-to-face CPD events, including the flagship National Symposium, had to be cancelled. With the help of the dedicated staff and an army of passionate volunteers, many of these events were turned into online activities and the result was astonishing. We were able to reach out to a lot more participants, at a much lower cost and provide high-quality CPD for everyone. A win-win for all was achieved through this collective effort.
Our fight against the union’s effort to have our profession covered by the inferior Health Professionals and Support Services Award was not successful and the threat of a massive reduction in remuneration levels was real at the time. The DHAA immediately activated our contingency plan by joining up with ADOHTA to collect and publish the market rates for our profession widely so that both employers and employees are able to
access this important information. The strategy appears to be working with anecdotal information received through the DHAA employment services indicating that the remuneration level has been more or less maintained despite a constant downward pressure being exerted by the presence of the much lower award rates.
After decades of advocacy work, our profession finally gained access to provider numbers last year, making us truly independent practitioners in the health system. While there has been a lot of hard work done by many over a long period of time in
“Our profession and its members are in a much better place today compared to four years ago, and the DHAA can proudly claim credit for its part in this.”
laying the foundation, there is little doubt that the DHAA Bad Mouth Advocacy campaign was the trigger for the Federal Government to make the policy change. The campaign was a highly structured and coordinated effort of many DHAA members with consistent messaging to politicians and government officials across the country at the same time.
Other advocacy works are ongoing at both the Commonwealth and State levels and we hope with time, persistence and coordinated efforts through the DHAA, we will see more positive changes coming through for our profession.
We also note that the professional indemnity insurance costs of major insurance companies had dropped significantly over the past few years as a result of DHAA offering its members PI insurance, putting pressure on other companies to review their prices. We are also seeing the membership fee of the alternative association being reviewed to stay competitive as the DHAA has been working very hard to keep our membership fee among the lowest of all oral health and dental organisations.
I have little doubt that our profession and its members are in a much better place today compared to four years ago, and the DHAA can proudly claim credit for its part in this pleasing outcome. While many benefits of all our hard work in advocacy may extend to benefit the profession as a whole –whether you are a DHAA member or not – it is important to note that it is the support of DHAA members that makes it possible for all these to happen. So every DHAA member should be recognised for their part in this.
For the non-members, it is never too late to jump on board to support our collective effort to make our profession better. We are claiming credits, and so should you. n
The DHAA are supporting the University of Adelaide in an exciting and innovative oral health project
The DHAA congratulates Dr Paul Monaghan of the University of Adelaide for the implementation of the Closing the Gap through Oral Hygiene and Language in Remote SA Project. This project has received Commonwealth funding to proceed in 2023. The two-year project is designed for the Mobile Language Team to work with the Dental Hygienists Association of Australia and regional and remote Aboriginal health services to create a set of resources promoting everyday oral hygiene in the endangered Yankunytjatjara language. Better oral health outcomes will lead directly to better language health.
Oral health is a prerequisite to language health in the Indigenous language space. Health professionals stress that general health and well-being suffer when patients suffer repeated oral infections (teeth, gums, throat). What is often neglected is the negative effects of poor oral hygiene on speech and by extension the health of Indigenous languages. It is well known that children require healthy speech models through adults and also other children. Improving oral hygiene in remote communities will help to promote healthy models for healthy speech. This project will analyse and develop local ways of speaking about oral health practices, like brushing teeth and flossing regularly. Linguistic resources for talking about oral hygiene will be produced and lead to improved health and speech outcomes. The use of the Yankunytjatjara language in this pilot will increase its use in communities, broaden its resources, and strengthen its position in everyday life in remote communities.
The project involves the following steps:
1. Construct a culturally safe framework for speaking about oral hygiene in Yankunytjatjara.
2. Develop linguistic resources for talking about, practising and promoting oral hygiene in Yankunytjatjara
3. Produce promotional materials
4. Deliver oral hygiene workshops
5. Monitor pilot roll out and uptake of oral hygiene re- source packages
DHAA Oral Health Promotion and Public Health Committee member and Rural & Remote SIG chair Lyn Carman will be working on the project team to provide advice and support. Besides Lyn, the project team comprises aboriginal language workers, linguists and researchers from the Mobile Language Team of the University of Adelaide will commence work this year. n


We focus on a range of subjects including; dealing with patients with sensory impairments, special needs support, managing the global public’s oral health. Truly something for everyone.

This article discusses the different types of sensory impairments and their aetiology. It considers how the oral health status of patients with sensory impairments is impacted by their disability and the barriers these patients face in dental care. It also discusses legislation relevant to dental care professionals when caring for patients with disabilities, including the Mental Capacity Act (2005), the Equality Act (2010) and the Accessible Information Standard (2016). Finally, it provides recommendations to dental care professionals on how they can best manage patients with sensory impairments and communicate with
them effectively in order to provide them with quality dental care.
British Dental Journal volume 233, pages 627–633 (2022)
• Published online: 28 October 2022
• Authors: Tasnim Aniqa Ahmed, Natalie Bradley & Stephanie Fenesan
• Suggested CPD hours: 0.25 scientific
Universal health coverage cannot be universal without oral health
Oral diseases are major global public health problems that require urgent attention. An unprecedented 3·5 billion people have oral diseases, comprising tooth decay, severe gum disease, tooth loss, and oral cancer. The effect of these
Managing the unmet needs of children and adolescents can present special demands
diseases on general health, quality of life, and well-being is substantial. Moreover, productivity losses from oral diseases are estimated at US$323 billion, highlighting the great social and economic harm they cause, particularly in low-income and middle-income countries.
WHO’s Global Strategy on Oral Health clearly recognises that “achieving the highest attainable standard of oral health is a fundamental right of every human being”. This statement implies that oral health is a public good and that achieving good oral health is therefore also a public responsibility—particularly towards vulnerable and disadvantaged populations, who face the highest risks and disease burdens and the lowest access to health services.
There is no health without oral health, and there is no universal health coverage without oral health care.
• Published online: 11 December 2022
• Juliane Winkelmann, Stefan Listl, Ewout van Ginneken, Paula Vassallo & Habib Benzian
Suggested CPD hours: 0.25 nonscientific

Parental psychosocial factors, unmet dental needs and preventive dental care in children and adolescents with special health care needs: A stress process model
Children and adolescents with special health care needs (SHCN) have higher unmet dental needs, but the potential mechanisms by which parental factors
can influence dental care use have not been determined. Parenting a child with SHCN can present special demands that affect parents’ well-being and, in turn, their caregiving. Hence, the study’s overall aim was to apply the stress process model to examine the role of parental psychosocial factors in the association between child SHCN and dental care. Parents of children with (vs without) SHCN reported higher unmet child dental needs, higher parenting stress, and lower social support (instrumental and emotional). Instrumental, but not emotional, parental support was associated with lower odds of their child’s unmet dental needs in both age groups. The association between parenting stress and child dental care outcomes was modified by parental social support.
BMC Oral Health
Volume 22, Article number: 282 (2022)
• Published online: 11 July 2022
• Arwa Z. Gazzaz, Richard M. Carpiano, Denise M. Laronde & Jolanta Aleksejuniene
• Suggested CPD hours: 0.5 scientific
Factors associated with the oral health-related quality of life of patients with temporomandibular disorder at the final follow-up visit: a cross-sectional study
This cross-sectional study comprised 227 TMD patients to determine the oral health-related quality of life (OHRQoL) of temporomandibular disorder (TMD) patients at the final follow-up visit, and to investigate the associated factors. Bivariate analyses demonstrated higher OHIP-14 scores in younger patients, females, having TMDC, and lower mouth-opening distance. Multivariable analysis demonstrated
the association of higher OHIP-14 scores with being younger and having TMDC. Participants with TMDC demonstrated greater improvement in unassisted mouth-opening distance, compared with the other clinical diagnosis groups. At the final follow-up visit, oral health impact problems were reported mainly in physical pain and psychological discomfort domains. Better OHRQoL was found in older, and TMDM or TMDJ patients.
BDJ Open
Volume 8, Article number: 30 (2022)
• Published online: 2 October 2022
• Prangtip Potewiratnanond, Nareudee Limpuangthip, Varangkana Karunanon, Ansaya Buritep & Athitaya Thawai
Suggested CPD hours: 0.25 scientific
Oral health and oral health behaviour in young adults with caries disease
The aim of this study was to describe and analyse oral health, oral health behaviours, and oral health-related quality of life (OHRQoL) in relation to the level of caries disease among cariesactive young adults.
Multinominal logistic regression showed that poor OHRQoL and gingivitis were associated with caries severity in a gradient fashion in accordance with caries disease activity. Also, irregular dental care and frequent consumption of sugary soda were significantly associated with very high caries severity.
The risk factors related to caries severity among young adults were poor OHRQoL, gingivitis, consumption of sugary soda and irregular dental care attendance, indicating the need for a combination of different interventions
specifically health behaviour change. These findings may contribute to identifying high caries-risk individuals.
BDJ Open Volume 7, Article number: 28 (2021)
• Published online: 31 July 2021
• Jennie Hagman, Ulla Wide, Helene Werner & Magnus Hakeberg
• Suggested CPD hours: 0.25 scientific
‘It’s their mouth at the end of the day’: dental professionals’ reactions to oral health education outcomes
Research has established varying levels of efficacy of oral health education (OHE) efforts. However, little is known
regarding how outcomes impact dental professionals and their OHE practice. This study explores dental professionals’ reactions to varying OHE outcomes and their motivations to persist with their efforts. 30 interviews were conducted (17 dentists, six dental therapists and seven dental nurses). Pleasure was gained from improved patient oral health. Responses to nonadherence included disappointment, frustration and acceptance. Acceptance centred around a shared responsibility for oral care between clinician and patient and reassurance that they had ‘done their job’. The unpredictability of patient adherence aided OHE motivation; efforts might eventually inspire patient action or might align with patient readiness to change. This study reveals how OHE outcomes impact on dental professionals’ perceptions of their role and personal motivations for continued educational efforts with patients.

Greater emphasis on both preventative dentistry and self-care, coupled with an understanding of the complex factors influencing oral health behaviour, would aid motivation for OHE.

British Dental Journal
• Published online: 22 September 2022
• Emma Barnes, Alison Bullock & Ivor G. Chestnutt
• Suggested CPD hours: 0.25 scientific
This book is not one I imagine most of you would have heard of or would think would be recommended. This book came into my hands through a patient interaction. When talking to this patient we realised that we were both caring for a young man who had been in state care for some time. We were both struggling with the fact he had recently been convicted of murder and was now incarcerated. I mentioned I was finding it difficult to grasp how this boy ended up down such a road. The patient explained they had the same feeling until they were recommended a psychology textbook called ‘The boy raised as a dog’ by Dr Bruce Perry. We had a brief discussion about the book which left me intrigued and on the hunt for a copy.
Before I go any further, reader discretion is recommended for this book. This book contains emotional stories of not just victims but of perpetrators. It is a read that depending on your mental health at the time could be difficult, so please check in with yourself before heading down this road.

Dr Perry is an American psychiatrist who is currently a Professor (adjunct) in the Department of Psychiatry and Behavioural Sciences at the Feinberg School of Medicine, Northwest University in Chicago and the School of Allied Health, College of Science, Health and Engineering at La Trobe University, Melbourne, Victoria, Australia. Over the last thirty years, he has been an active teacher, clinician and researcher in children’s mental health and the neurosciences.
The boy raised as a dog was his first
published work co-authored with Maia Szalavitz which delves into his work with maltreated children. Perry describes a number of cases from his early days as a clinician, some are horrific much like my young man, and others just find themselves in situations of no doing of their own. What all these stories have in common is that they are heartbreaking. What takes this book from crime novel to educational text is after a brief overview of the case Perry discusses his thoughts regarding the patient and what he learnt from these cases
as a psychiatrist. I was so emotionally invested in the stories that learning the neuroscience or the ‘why’ behind the situation became easier to comprehend. The main link in all of these cases was the lack of nurturing they experienced from birth and does not support healthy brain growth – the old saying nature or nurture has never been truer. Perry goes on to discuss methods used to assist with the rehabilitation of his patients and I think these techniques will surprise you.
This newfound understanding of ‘why’ saw me empathising with the children who had become offenders themselves. The in-depth overview of child brain development (or the lack of in many of these cases) is truly fascinating. I read this book on my maternity leave which I know influenced how I cared for my child at the time. But why are you recommending this for dental practitioners I hear you say? I know myself I have had people from many walks of life end up in my chair. Most of these people I have been able to understand which has made treatment easier, right? I happen to know the young man’s story that I mentioned above which still did not help me comprehend his situation. I have no doubt there have been others in my chair who have had or are currently experiencing similar situations in which I did not have the level of understanding they deserved. This book has given me the ability to put more thought into the ‘whys’ of patient behaviour improving patient experiences and in turn outcomes.
I do not feel I have given this book justice with this review. It was such a thought-provoking and deeply interesting book, focusing on the brain in a way I have never experienced before. n
Do you have a book, journal, or podcast that you think others would love to know about? Send it through to be reviewed; email the details to bulletin@dhaa.info
series of book reviews, Danielle Gibbens slips between the covers of
The boy raised as a dog by Bruce D Perry and Maia Szalavitz
“This book has given me the ability to put more thought into the ‘whys’ of patient behaviour, improving patient experiences and outcomes”
Dear DHAA... I heard so much about the savings that DHAA members can make going through the special corporate discount member benefits portal. I just tried to log into the membership benefits portal to buy something and it says my email or password doesn’t match which it does as I have just logged into the DHAA page. I then tried to register and it said that my email was already in use.
To access the member benefits discount portal you need to first log in through the www.dhaa. info member portal. Then go to the drop-down menu of ‘my membership’ and click ‘Members Benefits’. Follow the link to the “Members Benefits Portal’.
The members› benefit portal is a different login to our DHAA website. They do not share the same password unless you set the password.
If you can’t remember the password that you set for the Member Benefits portal you will need to click ‘Forgot Password’ which will reset it for that portal only. Your DHAA website password will remain the same.
Dear DHAA... I just received my provider number from Services Australia and it states on the form that I cannot use this number to refer to specialists or request diagnostic X-rays services. Is this correct?
As a registered AHPRA dental practitioner, you are able to, and in fact, obliged to refer your patients to relevant specialists and/ or request diagnostic services. This is part of your professional and legal obligation.
As the provider number is merely a commercial arrangement for payment, the Commonwealth government (Medicare) has not recognised our provider numbers in the Medical and diagnostics arms of Medicare. All the changes made to date have been in the Dental Benefits Act. As a result, our provider numbers only entitle us to charge the CDBS and it is not yet recognised by the medical and pathology/radiology arms of Medicare. For patients to receive Medicare benefits that require a referral, the referral must come from a recognised provider in the respective
acts and regulations. The DHAA is working on this as our advocacy focus at the moment but it will take time.
In practice, you should refer patients according to their needs, but you need to explain to patients that your referral does not allow them to utilise Medicare. So the alternative is for you to refer to a GP and let the GP request the tests, or to a medical specialist. In cases where the tests are not covered by Medicare, or if patients are happy to meet the full cost, you can then provide the appropriate referral. However, we expect some confusion among diagnostic providers regarding us, as there has been very few order/refer from our profession in the past.
Dear DHAA... I was wondering if you could please send through some information on if the principal dentist needs to be on site for a hygienist to work. From my understanding, it’s okay for the dentist not to be on site but to be contactable via phone. All AHPRA registered Dental Hygienists, Dental
Therapists are independent health practitioners. You are independently accountable and responsible for all treatments, advice and services you provide. There is no legal requirement for any other health practitioners to be present or be available by phone when you practise within your scope. However, you may wish or be required to have other health professionals present or connected by phone when you work as a team, but you are still expected to be fully accountable and responsible for anything you do by law. The Dental Board of Australia›s scope of practice registration standard and guidelines, as well as the code of conduct, are excellent documents to refer to.
Dear DHAA... I am a DHAA member and I would like to organise my indemnity insurance through DHAA and am wondering how I can go about this. You can add insurance to your membership by heading to the DHAA website and checking the insurance selection box and then press the add to cart button.
Once you have selected and added the insurance (make sure the box is checked), please update the cart before proceeding to submit for payment. You will receive a confirmation email after you have completed the payment and order. You will be covered immediately you receive that order confirmation, and the insurance certificate will be emailed to you directly from the insurance company later.
Dear DHAA... I am interested in completing the Aged Care Chapter Education Program so that I have the skills and support to provide oral health services to aged care facilities. Can you assist me in how to enrol?
To join the program you need to be a member of the aged care chapter. Visit the DHAA website to add the aged care chapter membership to your membership subscription. Once you have joined the chapter, you can then subscribe to the education program here. n
If you have a question to ask then please email it to bulletin@dhaa.info
What would happen if a chair collapsed at your business, causing a client to fracture their hip? Or a patient slipped and fell in the waiting room? Whether or not the incident was caused by a direct failure on your part, you could be found liable. This is where public liability insurance could step in.
n What is Public Liability Insurance and how does it help?
Public liability insurance helps cover actual or alleged negligence caused either by you or your employees that results in bodily injury or property damage to a third party. That means if a client/patient files a claim against you regarding an injury they suffered due to negligence or an accident within your premises, this insurance could help cover you. Some examples include:
n Property damage
If you provide mobile services or meet clients offsite, public liability insurance could help cover potential property damages. For example, if you were to accidentally damage a client’s garage door while carrying your equipment, public liability insurance may provide cover.
n Slips and falls
In the event that a client/patient slips and falls on your premises, public liability insurance could offer cover.

n Who should have Public Liability insurance?
If you meet with clients at your business
location or off-site, you may want to carry public liability insurance. You may also want to have your own insurance as an employee. If, for example, a patient fell because you instructed them incorrectly, or you were not supervising them correctly, your public liability insurance could step in. Check your policy or speak to your broker or insurer if you have questions. n
Securing cover with BMS is easy! As long as you hold a current DHAA membership you can get a quote started.
Speak to a BMS broker at dhaa@bmsgroup.com or call 1800 940 762.
Disclaimer: In arranging this insurance for our members DHAA is acting as a distributor of BMS Risk Solutions Pty Ltd (BMS) AFSL 461594, ABN 45161187980. The insurance is issued by BMS under a binder with Certain Underwriters at Lloyds. When acting under a binder BMS acts as an agent for the insurer and not as your agent. This is general advice only and BMS has not considered whether it was suitable for your personal objectives, needs or financial situation. Please read the Policy Wording and Financial Services Guide before making any decision about purchasing this policy.
Being a relative latecomer to the dental world, it still surprises me how many years I have been a dental hygienist – 40 years in the profession and the past 30 of those years have been without a doubt the most rewarding, exciting and challenging years of my career.
A few people know from the very outset of their working life, and maybe earlier, what career they would like to pursue. For myself, I knew I was interested in health and people. This was a good start, but I had no idea where to begin. So I dabbled in many areas of health and hospitality before answering an advertisement in my local paper in the Adelaide Hills for a dental assistant.
Being up for a new challenge I successfully applied and realised very early that while I was learning new skills it was not where I wanted to be. I dutifully completed the required two years of dental assisting that would qualify my application for dental hygiene studies. I add here that my employers at the time were incredibly supportive of my seeking further education and happily recommended me for the course.
The course at that time was conducted at the Adelaide Dental Hospital (ADH), located on Frome
Road which was still considered part of the Royal Adelaide Hospital (RAH). We were very fortunate to have access to specialists from every field of health. This was very helpful for our electives and first aid that was conducted by a nursing sister in addition to visits to the Intensive Care Unit (ICU) supervised by one of the dental hospital-based dental hygienists, and visits to the dental clinic at the Queen Elizabeth Hospital (TQEH)
At this time the course was a jam-packed 15 months in duration. With a youthful brain and enthusiasm, there were no computers so all notes were handwritten during lectures. I must agree with Dr Montessori, the Italian doctor who began the Montessori teaching system, that posits with now >>
”A few people know from the very outset of their working life what career they would like to pursue. For myself, I knew I was interested in health and people“

good evidence that “the pathway to the brain is through the hand” – along with other systems for creating those everimportant neural pathways. That aside I am very pleased to have the advantage of computers as a means of electronic pathways and connections! We also had four periodontists, one of who is still very much part of our world, Dr Bryon Kardachi, and sadly no longer with us Drs Brian Shephard, Sven Johansson, and Rob Hirsch who many of you will remember as being a real champion of dental hygienists and a wonderful friend to many.
The final practical viva day is imprinted in my mind forever. An unseen patient, full examination, treatment plan, begin treatment followed with an oral viva. I don’t believe my patient had ever had a clean before and thankfully I was able to say to my examiners that I could rationalise truthfully that I had not performed a satisfactory debridement. There is no shame in admitting your lack of knowledge or expertise.
I went on to work for 10 years in private practice, and whilst recognising that this was not where my passion lay, it gave me very important underpinning values. These included patient care, respect and diligence for detail, working

TOP RIGHT & ABOVE: The class of 1980 (Back row L-to-R) Sue Neeft, Sue Frazer (Senior Lecturer), Margie Steffens, Dr Rob Wiedenhofer (Senior Dentist), Di Synon, and Jean McNicoll; (Front row L-to-R) Liz Moreton, Sophie Karanicolas, Pina Romano, and Nelda Frolow



”I was able to say to my examiners that I could rationalise truthfully that I had not performed a satisfactory debridement. There is no shame in admitting your lack of knowledge or expertise”BELOW: The early days of CODP and our first patient; BOTTOM: Walking in aid of a local homeless support centre ABOVE: Australia really does have talent
in a team, attention to detail and time management (something I have always struggled with – however Special Needs Unit was my lifeline as this was not a driver for ‘productivity’.
After the birth of my second son, I was increasingly unsettled for a range of reasons working in private practice. Then an opportunity arose in a research clinic at the ADH High Caries Risk Clinic under the guidance of Dr John McIntyre. This was a chance to learn with the best. John is a published academic and had been involved with early research into the use of fluoride and minimal intervention techniques for remineralisation and maintenance of caries in very challenging populations e.g. drug and alcohol misuse, psychiatric, and homeless. The clinicians in this area were mostly dental hygienists (Marilyn Jolly, Virginia Street, Amanda Trennery, Di Synon and Sue McPherson). This was a fantastic opportunity to be part of an intervention that demonstrated that minimal intervention did indeed preserve even the most damaged dentitions, and if regular care and education were undertaken further deterioration could be circumvented. Unfortunately in the early 1990s, funding was taken away and the unit was closed, much to our frustration. It was at that time a seed was sown for me. This wasn’t good enough! Something had to be done and so an idea began to grow.
A position became available in 1992 in the Special Needs Unit (SNU). My life in private practice was finished and I began my career (the absolute joy of my life) working in this unit. I originally started under the guidance of Dr Liz Coates (a force of nature) and then with Associate Professor Sharon Liberali (a compassionate and loyal leader and a dear friend) until my retirement from the unit in 2022.
The past 30 years have enabled me to be true to my philosophy about >>
I REALLY DON’T remember the first time I met Margie Steffens. I think that’s because to me she has always been around.
After I qualified as a dental hygienist in 1990, Margie was already an active and well-known presence in the dental world in Adelaide. She struck me immediately in those early days as a calm, thoughtful and kind person, and I still hold this belief after all this time of knowing her.
Margie’s work through a wide range of projects, over many years, reflects the care and empathy she clearly feels towards people, especially those with unmet needs. Some of her outstanding work achievements include: Starting in the High Caries Risk Clinic in the early 1900s, visiting hospitals and assisting nursing staff with ICU patients, developing resources and lobbying for better oral health in aged care, working in the SRF (Supported Residential Facilities) project, lecturing undergraduate Oral Health students in Special Needs and Geriatric Care, and the establishment of a dental clinic for homeless and vulnerable people at Common Ground. We can see a theme in Margie’s choices.
Margie talks about her 30 years of working in the Special Needs Unit with great affection. She recounts patients’ personal stories and circumstances as she reinforces (through modelling) the importance of knowing the people we meet and treat in our dental chairs, and not to judge or make assumptions.
Her years of managing the Community Outreach Dental Program at Common Ground has expanded the reach of dental treatment to people who would not otherwise have access to care and has also allowed dental practitioners to be actively involved in providing services in an environment totally different to the usual dental practice. I know it is a project of which Margie is proud, as well as gratified to have improved the access to oral care for many people in need.
Along the way, Margie has made a large network of contacts, which means she has the ability to find exactly the right person for a particular task, job or even a procedure. Margie has proven time and again that she has a wide reach as well as great relationships with friends, colleagues, students and other industry representatives, that extend far beyond the dental community. The awards that Margie has received, such as the OAM (Medal of the Order of Australia), further highlight the value placed on her work. She continues to be a mentor for me and many others, whether she knows it or not.
It has been a true honour, as well as being fun, for me to know Margie and to have worked with her on various projects and initiatives such as the DHAA, University of Adelaide and TAFE SA. Margie has recently resigned from some of her long-held positions, however, Margie is an active person who is learning that she can enjoy a little time for herself after devoting many decades to the wellbeing of others. We can look forward to hearing about her current projects and activities, such as her yoga, painting, and continuing her learning journey through the University of the Third Age.
“She [Margie] continues to be a mentor for me and many others, whether she knows it or not”
what a healthcare professional truly is and what we learn every day from our patients.
The opportunities I was afforded whilst working in the public sector, higher education and being a member of the DHAA include:
• Collaboration with TAFE Paradental Studies program, hosting Japanese dental hygiene students that extended over 20 years. I even learnt a smattering of Japanese.
• Hosting international tour groups through the ADH. I had the immense pleasure of hosting the inimitable Dr Esther Wilkins. A prolific author of Clinical Practice of the Dental Hygienist.

• Along with Dr Dymphna Cudmore, we developed the Supported Residential
IF WE HAD to summarise Margie in words; mentor, friend, guide, and inspiration all modelled into one person come to mind. We could all agree, Margie is that brain to pick, that ear to listen and that push in the right direction.
We first met Margie in 2002, her special needs, public dentistry background, and life experience gave us amazing insights. Not only was she ever so patient with us, but her feedback was also kind, fair, supportive, valuable, and professional. Instrumentation with Margie as your tutor required few words, there’d be detection with the explorer, a slight head movement toward you and a raise of the right-hand side eyebrow; but

a demonstration of how to remove was always shown. Not only were there handy instrumentation techniques, but Margie also scaffolded us as clinicians from seeing a tooth, to seeing a mouth, to interactions with periosystemic health, to seeing the patient as a person, and developing professional relationships with the patient while caring for them in a customised and holistic manner.

Our very last undergraduate clinic session was spent with Margie as our Tutor; her persistent patience, support and confidence in our abilities made us feel like we were ready to enter the workforce and that’s something we’ll
both never forget and be grateful for.
However, the journey just didn’t end upon graduation, Margie has been a consistent mentor that pushes us in the right direction. After a December champagne breakfast, we suddenly found ourselves on the Executive Committee of the DHAA (SA Branch) Inc. Margie’s wisdom, support and guidance, accumulated knowledge helped us avoid some of the frustrating learnings of our antecedents. She scaffolded us starting with affordable but nice red wine selections for our functions, to speakers, and to organisational matters. Saying yes to these roles led us to the national committees. This valuable push and mentorship contributed to the next stage of development in our careers in becoming
lecturers at our respective educational institutions.
Observing Margie when speaking at DHAA functions has always been a moving experience with her interests in equity of oral health care within aged care, special needs and vulnerable people. Her ethos and values aligned with our values; the financial element of oral health is something that’s never sat right and Margie has been the one to show us a way out of that. Not only is Margie advocating to politicians for a publicly funded model of basic oral health care but she role models involvement in Oral Health outside of the dental clinic and within the community. Her connections to the community never cease to amaze us with how quickly she’s connected with colleagues. Last year she
Facilities (SRF) program for SA Dental Service (a project that has now become the homeless scheme with SA Dental)
• Inaugural chair for the Aged Care SIG (now incorporating the Aged Care Chapter in the capable hands of Lynda Van Adrighem and Ali Taylor).
• During this time, I attended the National Aged Care Alliance meetings. A time of learning about large groups with much political context and how to get a foot in the door.
• Past president and national councillor for DHAA SA, and attended State Oral Health Plan meetings. This was a very interesting time when much change occurred with the government taking a bigger role in the directives for the Oral Health Plan.
• I attended round table senate discussions in Canberra and had a particularly memorable meeting presided over by the Honourable Tanya Plibersek, a remarkable woman.
• Inaugural chair for Special Needs SIG
• The delight of being able to advocate on behalf of the DHAA and the CODP on radio and television interviews about the inequities in oral care and services for the older population and the various vulnerable and marginalised groups.
• Teaching BDS, BOH and ADOH undergraduates in clinical skills, lectures about Special Needs Dentistry and later about Homelessness and Community Outreach Dental Care.
• Taking students out of the clinic to visit aged care facilities, supported residential facilities and later homeless and refugee centres.
Was I up to the next challenge? Yes indeed I was! >>
connected the Kanggawodli accommodation service and the AKction Project [Aboriginal Kidney Care Together – Improving Outcomes Now] with TAFE SA.
We’ve always seen Margie as a role model for our profession; a person who has a social responsibility to make
than the implementation of the Community Outreach Dental Program, through the University of Adelaide. Margie aligned herself with supporters and has made an amazing clinic come off the ground. It’s truly humbling to see the number of links Margie has developed outside of the dental industry including
health, alcohol and/or other drugs, employment, community health and disability, ROSA: Registry of Senior Australians Project: uses evidence-based primary health care service delivery and policy for the Australian aged care sector and Catherine House: provides accommodation and support
provide a free clinic with the support of The University of Adelaide, Common Ground, and the ADA (SA Branch) Inc. is truly remarkable.
the world a better place. The reason why we see this as such a success, was that she was willing to do what others would view as impossible. She had the courage to bet on one’s idea and take a calculated risk to act. She’s a humble person who’ll underpromise and over-deliver and there is no better example
Common Ground, Housing Choices Australia, Workskil Australia, St Vincent De Paul Society, Salvation Army, Australian Red Cross, Hutt Street Centre, Australian Refugee Association, Sonder: A NFP organisation; supporting people across seven domains: mental health, homelessness, Aboriginal
for women experiences homelessness. Not only this, but this clinic then has connections back to the Special Needs Clinic at the ADH, OMS at the ADH and the Aboriginal Oral Health Program (SA Dental) as well as a range of specialists around Adelaide. To develop all those connections and
The lessons to be learnt from the way Margie approaches these community connections, is don’t start at the lowest point of an organisation, aim as high as you can go, target the influencer, have the facts, and research organisations. Take advantage of situations, if you’re invited to events or meetings and lastly, underpromise and over-deliver. While this is a small element of Margie’s story, we all can be thankful for Margie’s transfer of knowledge and the faith that she puts in all of us. We hope this small insight might encourage you to take a page out of Margie’s book and bring it into your own.
”The past 30 years have enabled me to be true to my philosophy about what a healthcare professional truly is and what we learn every day from our patients”
“We’ve always seen Margie as a role model for our profession; a person who has a social responsibility to make the world a better place.”
2009 – 2011 was the seed I mentioned earlier and it was about to burst forth, “how to provide care for people who either did not have a Health Care Card (HCC), were on such a low income they could not afford private health care, were homeless, refugees and generally marginalised through social circumstances”.
In between all this just to ensure I was busy enough I completed a B.Sc. Dent Honours!
In 2009 I formed a project group with the blessing of Professor Johann DeVries, then dean of the dental school, Prof Richard Logan (now dean of the dental school), Prof Lisa Jamieson (director of ACPOH), Dr Eleanor Parker and Dr Peter Cathro.



With an Australian Dental Research Foundation Grant (ADRF) we undertook a year of visits to the homeless centres and from the research, education and screening sessions, we published some journal articles and presented posters at international conferences. The next step was to establish a clinic for these very people.



The new journey was at the same time frustrating and wonderful. It consisted of door knocking, phone calls, visits and meeting after meeting. Then persistence paid off when a door opened and I met with the CEO of Common Ground (now Housing Choices SA / Common Ground) Sue Crafter to discuss their new build at Light Square. I could not have timed it better, but how was I going to find the money for the inclusion of the dental and medical rooms?
A new grant round miraculously became available and the University (Professor Justin Beilby, Executive Dean of Health Sciences and Professor De Vries) asked me to apply as the grant was contingent on Increased Clinical Training capacity and the universities vision statement included better community engagement.
I was successful and so the rest
‘as they say is history. Community Outreach Dental Program (CODP) was built and the clinic had a home. 11 years on and I can look back at our achievements:
• Care is being provided through a referral system and our engagement with the homeless sector, refugee associations and numerous support agencies.
• It is a pro bono service that relies on volunteer dentists, grants and external funding which is always a huge challenge.
• Students from BDS, BOH and ADOH have the benefit of learning about their commitment as a health care
see young enthusiastic people who genuinely care about their profession, and to then be awarded Life Membership with the AUDSS
Somewhere in between I received the great honour of the Order of Australia Medal (OAM) for services to the community in the provision of dental and health care for the homeless and vulnerable in Adelaide in 2017. This was a most overwhelming experience.
In 2017 a service award from the DHAA and life membership, and Special Service award from the Pierre Fauchard Academy of Oral Health International, for service to the profession and
wind takes me.
What have I learnt?
Gratitude for the opportunities I have been given to improve my life and to be fully engaged in the community. I am reminding myself about the importance of self-care and to act with grace – a lesson for us all.
Joy in teaching and learning. Oh yes, and learning about the doubtful joys of grant writing. Joyful when you have success!
Enduring friendships with colleagues, students and patients.
The importance of truly listening and sitting down with my patients, and allowing them to tell me their
provider to utilise their skills to help all people in the community- a time to learn about their privileged positions in life and how much richer they are for being there to help people who truly need a kind word and a gentle hand.
• Through the CODP activities such as
• Screening sessions at some centres
• Dental Health Awareness week activities
• Homeless Connect Expo
• International Students visiting for electives
• Engaging more effectively with First Nations support groups and service provision – what an energising and educational experience for me.
• Annual Sleep-out organised by the Adelaide University Dental Students Association (AUDSS) help raised funds for CODP
• In 2020 I had the honour of being nominated to be Patron for the AUDSS. It was wonderful to
marginalised sector – the first nondentist to receive such an award in Australia.
In 2019 I was the first non-dentist to be awarded an Honorary Fellowship with the International College of Dentist – again such an honour to be considered for this and ICD have been such supporters of CODP in awarding grant money each year.
I cannot thank our industry partners enough for their generosity of donations and reduced cost of products (Henry Schein Cares and Dental Concepts –thank you) and also for dental practices that donate stock.
I can happily say after managing a tripartite agreement between the University of Adelaide, ADASA, and HCAU, and finding a great young dentist Dr Harry Perkins to take over my role I believe the CODP is in good hands.
For myself, am I retired?
Next chapter – project work with TAFE, ARCPOH including Indigenous oral health projects and where ever the
stories. Through their stories, I have learned to be patient, diligent in detail, kinder and more willing to accept they know so much more about their health and ultimately what they need from us as healthcare providers. We as health professionals have a duty to be advocates for people who don’t have a voice!
It’s OK to feel sad, discouraged and inadequate, but never to dwell on it. I have learnt to accept my own failings and frailties which makes me more accessible to my patientsbravery is allowing yourself to show your vulnerability honestly and thoughtfully.
Each person is unique and we are given particular gifts that we can either choose to hold onto – but I believe to give generously and wholeheartedly the world around you becomes more vibrant and joyful. Knowledge shared multiplies and increases the capacity for change that reaches further than you can imagine. n
”Somewhere in between I received the great honour of the Order of Australia Medal (OAM) for services to the community in the provision of dental and health care for the homeless and vulnerable”
Irecently listened to one of my favourite podcasts*, and the host was talking with Simone Stolzoff about his new book, The Good Enough Job: Reclaiming Life from Work. Simone really encourages listeners to stop placing so much of their self-worth on their work and to stop chasing the dream job, and instead consider whether our jobs are “good enough”. He goes on to explain that it is highly unlikely that any job is ever going to be ideal, and so we should think holistically about what we want out of life, and what aspects of our career or job are most important to us.
Listening to Simone talk about the idea of a “good enough” job reminded me of one of the key concepts I learned when I was studying career development, and one I like to remind myself and others about often. Your career does not exist in isolation from the rest of your life. The Systems Theory Framework of Career Development1 provides a wonderful tool for people to consider the range of individual, social, environmental and societal impacts on their careers. At an individual level, our knowledge, skills, attitudes, interests and values as well as personal characteristics such as
gender, health, disability and ethnicity, all impact the career choices we make. Beyond ourselves, our environment and society also influence our careers, and this might include our geographical location, peers, the employment market, socioeconomic status, family, media, politics, and historical trends. A common example of this is how our geographical location and having a family with school-aged children can influence job opportunities available to you or that you are willing to pursue. The Framework also considers how you and your circumstances might change over time. For instance, a job that seemed like your dream job five years ago, may not be your dream job today, and that’s okay.
The point is…. if you are striving for a happy, meaningful life (who isn’t?) we can’t just focus on our careers in isolation from our life. There is so much of our identity that impacts the career choices we make, which makes it near impossible to find what we might consider being our dream job. Then, when we aren’t ‘living the dream’ at work, we can get frustrated or demotivated, struggling to know where to take our career. What we should try to remember is that there might be
“Your career does not exist in isolation from the rest of your life”
enough about the job that is ‘good’ and allow you to live your best life. Does your job provide financial security, so that you can pay your mortgage, eat out at restaurants, go on overseas vacations (or fund any activity that fulfils you)? Does your job have flexible hours, which allows you to pick your children up from school? Are there parts of your job that are meaningful, that you get great satisfaction from? Thinking about whether our work supports us in having a meaningful life in a more holistic way can help us overcome the frustrations of not having the ‘perfect’ job.
If we have a ‘good enough’ job, one of the strategies we can employ to try and improve our job satisfaction is job crafting. Job crafting is “the physical and cognitive changes individuals make in the task or relational boundaries of their work”2. There are three potential avenues for job crafting. Firstly, you can look at task crafting –here you might look at what tasks in your job you find interesting and do more of those (and less of the ones you don’t like), or increase or decrease the responsibilities you have. Secondly, you can examine your workplace relationships, and change up who you work with on different tasks, or maybe look at creating new relationships through mentoring. Finally, we can shift our mindset, which might involve focusing on the importance of our
work or the positive impact it has on others. This last one is one we can all utilise in our oral health careers. It can be so easy to focus on the repetitive nature of scaling teeth as clinicians, or the million emails as an academic, but remembering our work has such a positive impact on our patients and students can shift our perspective and remind us our work is meaningful. n
Dr Melanie Aley (nee Hayes) is a dental hygienist who has enjoyed a diverse career in clinical practice, teaching, research and management. She has a Masters of Education majoring in Career Development, and after working in multidisciplinary roles, is now an Associate Professor and the Bachelor of Oral Health Program Director at the University of Sydney.

* The Happiness Lab with Dr Laurie Santos – listen through Spotify or Apple Podcasts; 1 Patton, W., & McMahon, M. (2006). A Systems Theory Framework of Career Development. In Career Development and Systems Theory (pp. 195-224). Brill; 2 Wrzesniewski, A., & Dutton, J. E. (2001). Crafting a job: Revisioning employees as active crafters of their work. Academy of Management Review, 26(2), 179-201.

Having finally secured that coveted first job, the reality of life after dental school slowly sets in. New to a land without tutors casting a watchful eye over our shoulders, impostor syndrome is rife. While setting forth empowered with four or five years of dental knowledge, the reality of stepping into practising life is that we frequently encounter difficult situations that make us feel out of our depth.

Adapting to the time pressures of real-world dentistry is one of the biggest hurdles that new graduates face. Gone are the days of three-hour appointments for exams and diagnostics. Building clinical agility while maintaining a high standard of care is notoriously gruelling, but it’s essential to avoid the temptation to cut corners to stay afloat. Thankfully, empowered with trusty assistants, I’ve grown to appreciate the joys of four- (and six-) handed dentistry in streamlining workflows and eliminating the need for contortion to achieve direct maxillary vision while suctioning with my non-dominant hand. More importantly, though, the insight and patient management skills that experienced staff can bring to every interaction is an exceptional asset to early-career dentists.
Clinical decision-making and committing to treatment plans can also present significant challenges. Without years of experience to anticipate how our chosen management plan will pan out, we’re often hesitant to make irreversible decisions when curly cases arise. To supplement this deficiency, we’re accustomed to having professors and clinical staff to hold our hands to validate our thinking, but how do we proceed in their absence? Input from specialists and discussions with mentors can help to set us in the right direction,
but, especially for patients with urgent needs, not having help directly on hand can be difficult. Being assertive and confident in one’s decision-making is something that does not come naturally to new grads in the trough of their professional Dunning-Kruger curves. While I maintain that self-awareness of our professional limitations is paramount to our practice of a safe scope of dentistry, talking to my newlygraduated peers has highlighted that we’re all in need of a gentle nudge in the right direction to facilitate our pursuit of the best treatment plan for our patients.
During our dental school years, we were exposed to a subset of knowledge required for basic clinical survival and are indubitably deficient in many areas of our practice. Additionally, while different tutors may introduce us to new techniques and alternative ways of approaching clinical scenarios, we are typically taught each discipline in one particular camp of thought. Navigating the real world of dentistry, we must continue to evolve our knowledge base to achieve an equilibrium between evidence-based dentistry, artisanal craftspersonship and remaining contemporary with recent developments. Albeit important to maintain a critical eye in appraising emerging techniques and technologies, it’s often not until we meet clinicians

outside our academic bubbles that we might realise that adopting an alternative modus operandi might make more practical or theoretical sense.
Assessing the difficulty of procedures is something that is generally neglected in dental school curricula. While we are proficient in diagnosing dental and periodontal disease, the mechanical “tooth is broken. I will fix/extract it” mindset that follows can rapidly come unstuck. Having now been tested by third roots on lower molars and cracked upper sixes with excellent
where treatment is left incomplete or has not progressed as intended. This could take the form of troubleshooting a repetitively debonded crown, identifying a barrier to the healing of a persistent periapical radiolucency or finally putting one’s finger on the underlying cause of plateaus in a patient’s periodontal health despite meticulous debridement and improvements in oral hygiene. With every clinical challenge comes a great learning opportunity.
Notwithstanding that it’s easy to feel isolated as our cohorts inevitably
cooperative kids, when the reality that we might face is of children whose concept of our profession has been shaped by parents who inadvertently create expectations of pain. While it’s important to celebrate our personal accomplishments and such content can be motivating to some that consume it, it can dissuade others who don’t enjoy the same successes. Our own personal growth should be our benchmark.
bone support, I’m more in tune with where my exodontic comfort zone lies, but there’s a long journey ahead. As new grads, part of our learning curve also involves coming to terms with the follies of our herodontic optimism in attempting to breathe life into teeth that an experienced clinician may deem unrestorable.
While we likely haven’t been in one place for long enough to have seen our own treatment fail, there’s plenty to be gained from witnessing clinical misadventures or inheriting cases
disperse on entry into the workforce, our generation is ever-connected through various online platforms. Such platforms can represent a valuable resource for the sharing of knowledge in a profession of predominantly sole practitioners, but they can also distort the perceived reality of our colleagues’ practising lives. The world of Instagram Dentistry is commonly used as a highlight reel for some who post ideal aesthetic outcomes without mention of the obstacles that they have faced along the way. We similarly encounter posts about blissfully
In a profession that attracts perfectionists, spiralling into a cycle of disparaging self-talk and despair over less-than-ideal treatment outcomes is a ubiquitous experience amongst dental students and professionals. Yes, this response rightfully signals that we care deeply about our patients and the standard of dentistry that we practise, and critical appraisal of one’s own work is fundamental to our growth. However, intense scrutiny of every detail can be incredibly destructive and overwhelming without perspective. We must all learn to self-regulate before such critiques make the survival of the workday a seemingly insurmountable challenge that culminates in a snowball of slip-ups if each appointment is marred by lost confidence and intrusive thoughts. This is where the art of compartmentalisation is crucial (although much more easily said than done), and taking a moment between patients to stretch, find some >>


“It’s easy to feel isolated as our cohorts inevitably disperse into the workforce”
fresh air and rehydrate can make a huge difference.
There is truth to the cliché that dentistry lends itself to a career of lifelong learning. Everyone’s first year in practice inevitably alerts them to countless aspects of their practice that require development, but reflection with other early-career colleagues corroborates an appreciation of how far we’ve all come since our early days as qualified dentists. If we surround ourselves with bright minds and motivated colleagues, there’s immense scope for technical and interpersonal growth to serve our patients as we mature professionally throughout our careers. It’s also important to maintain friendships and hobbies outside of dentistry to remind ourselves that self-worth is independent of how nifty a contact point is or a root tip in a sinus. Here’s to hoping that every sleepless night of treatment planning rumination is offset by the joyful tears of grateful patients whose smiles we carefully restore. n



COLGATE HAS KICKED off the year welcoming the appointment of two new members, Dentists, Dr Arosha Weerakoon and Dr Isabel Evans to its Advocate Community, a group of dental and oral health professionals who have preventive oral care at the core of their professional beliefs.
Entering its fourth year the Advocate Community supports and encourages young and established oral health professionals through the sharing of their knowledge on a range of relevant and topical issues based on their experience in the profession.
Advocate content delivers practical information for young professionals to employ during university studies right through to the practice setting. It drives dialogue on a wide variety of topics including preventive oral health, social responsibility, career development, mental health, and sustainable dentistry, to name a few.
The community members include representation from across Australia and New Zealand, including:
• Haydyn Bathurst, Fifth Year Dental Student, NSW
• William Carlson-Jones, Lecturer and Oral Health Therapist, NSW
• Dr Isabel Evans, Dentist, ACT
• Dr Sam Koh, Dentist, VIC
• Christine Murthi, Oral Health Therapist, NZ

• Dr Kaejenn Tchia, Dentist, NT
• Dr Emma Turner, Dental Registrar, VIC
• Dr Arosha Weerakoon, Lecturer and Dentist, Qld
About the author: Dr Emma Turner, a founding member of the Colgate Advocates for Oral Health: Editorial Community, completed her Doctor of Dental Medicine at the University of Western Australia as the Australian Dental Graduate of the Year 2020. She is passionate about contributing to the future of oral health through dental education, community engagement and research. She hopes to share her insights to encourage members of the dental profession to reflect on opportunities for personal and professional growth to benefit our patients and the wider community.
Republished with permission from Colgate Advocate’s for Oral Health


If you live in Victoria, you might have noticed a bright orange dental van on your local streets, or even at your local school. School dental is back. It’s a free service and we call it Smile Squad.


Smile Squad provides free dental care to all Victorian government primary, secondary and specialist school students and is funded by the Victorian Government. Dental Health Services Victoria (DHSV) is responsible for the delivery of the program.


With a strong focus on education and prevention, we want to equip all school students with the tools and knowledge they need to eat well, drink well and clean well for life.
Our vision for Smile Squad is the delivery of consistent, accessible, highquality dental care, every time. The program has already reached thousands of students and families across the state to help them improve and maintain their oral health. Sound like something you’d like to be part of?
1 A career in public health can be very rewarding. Working with Smile Squad, you can directly improve the lives of students and families across the state.
2 Smile Squad focuses on prevention. 1-in-3 children enter primary school with caries and continue to have a high likelihood of poorer health outcomes for the rest of their lives.
3 Smile Squad focuses on minimally invasive dentistry. Including fissure sealants, fluoride varnish, stainless steel crowns, silver fluoride and oral health coaching.
4 You’ll be supported every step of the way with direct access to peer support and mentoring.
5 You’ll have the opportunity to work with and supervise student dental practitioners.
6 Be part of a close-knit team of like-minded professionals who are
dedicated to making a difference.
7 Enjoy working autonomously. You can manage your own appointment books for the day and get things done your way.
8 Access extensive clinical onboarding and resources, including ICDAS training and calibration.
9 Gain experience using a range of innovative dental technologies. Smile Squad uses red band handpieces and electric motors, NOMAD Pro 2 handheld X-ray units, high-quality portable dental equipment and modern dental vans.
One thing is for sure – no two days are the same.
When the clinical team arrives at the school for the first time, they’ll meet the staff before setting up the mobile clinic or treatment van and logging into Titanium (patient record system).
The team then confirms consent and reviews dental, social and medical histories. Most of the day is then spent providing examination and prevention, or treatment services to a range of students with differing needs and past experiences.
Care plans are developed by clinicians and discussed with the student or parent/guardian.
Some days are busier than others and teams visit schools of various sizes and types. The teams meet new people and build new relationships within their local communities. It is a challenging role, but one that is also rewarding and interesting.
Bendigo Lead Regional Oral Health Therapist Jemma Lang loves working in Smile Squad because it gives her variety in her workplace and the ability to travel around the state, spending her days’ meeting, and treating students from a range of different schools.
“Smile Squad enables me to provide
high-quality dental care to Victorian government school students in a setting that is familiar and comfortable to them,” Jemma says.
“It is rewarding to know that I am providing dental care to kids in regional and remote areas who need it most.
“It brings me a great sense of satisfaction providing dental care to kids, knowing I am saving parents from having to take time off work to attend appointments.
“Working in Smile Squad gives me a lot of flexibility and a great work-life balance.”
Clinical placements are a key requirement for all students studying dentistry and oral health therapy. Placements support students in consolidating their knowledge and offer a range of learning opportunities.
Student clinical placements don’t just benefit students. Placements assist in meeting workforce needs during periods of increased demand. Students can gain firsthand experience of the benefits of working in the public sector and many return following their graduation.
Key to training these much-needed new dental practitioners is Dr Roisin McGrath, Director of the Bachelor Oral Health Program at the University of Melbourne.
“We initially set up the Smile Squad clinical placement as a pilot when students were returning to clinical practice after a long break due to COVID,” Dr McGrath says.
We all know that Smile Squad is important for school students and their families, but it’s also vital for the continuing education and training of oral health students.
DHSV is busy helping to train the next generation of dental practitioners, in partnership with the Melbourne Dental School at the University of Melbourne, La Trobe University and Holmesglen/ Charles Sturt University.
DHSV has a proud history of building partnerships with tertiary institutions, and training dental practitioners across Victoria. As part of these strategic partnerships, DHSV offers clinical placements to eligible students, providing them with practical learning opportunities.
“It was so successful that we’ve set it up as a formal placement opportunity for students not only from the University of Melbourne but also from La Trobe and Holmesglen/Charles Sturt University.
“The students absolutely love this placement. They learn so much about communication, care coordination and patient management.
“I believe this placement ignites students’ passion for working with children and helps them to consider how to bring oral health care to people, rather than just delivering services in fixed clinics.
“I look forward to further growing and developing this important clinical placement program with Smile Squad.”
We’re employing staff both regionally and in metro Melbourne. You can contact us at any time to learn more at careers@dhsv.org.au. n
“ It brings me a great sense of satisfaction providing dental care to kids, knowing I am saving parents from having to take time off work to attend appointments”
Jemma Lang, Bendigo Lead Regional Oral Health Therapist
 By Margie Steffens OAM
By Margie Steffens OAM
Acute kidney injury is the temporary loss of kidney function lasting less than three months. It typically has a fast onset, in response to an injury or illness affecting the kidneys, drugs, blockages of the kidney or many other factors. Some people will need a short course of dialysis to help their kidneys recover. Most people recover however if the kidneys have been severely damaged this may progress to Chronic Kidney Disease (CKD).
CKD occurs when your kidneys have been damaged in a way that cannot be
reversed. To be diagnosed with CKD, the condition will need to have been present for at least three months. CKD may be caused by the following; genetics, infection, immune disorders that attack the kidneys, diabetes and high blood pressure.
Many people live a normal life with CKD with changes in lifestyle. However, many people will experience a continued decline in their kidney’s ability to filter their blood and will eventually need specific kidney therapy which may be in the form of dialysis or a kidney transplant. 1
The kidney is a critical organ that provides the following functions:
n Excretion of Waste
Urea, amino acids, Ammonia, Creatinine and Creatinine Sulphate and Drugs
n Blood Electrolyte Regulation
Sodium(Na), Potassium(K), Calcium(Ca), Chloride(Cl), Phosphate(HPO)
n Blood Ph Regulation
Conservation of Bicarbonate ions (HCO3) and excreting hydrogen ions (H)
n Hormone Production
Erythropoietin (red blood cell production), Calcitrol (calcium hemostasis), Renin (Blood pressure control)
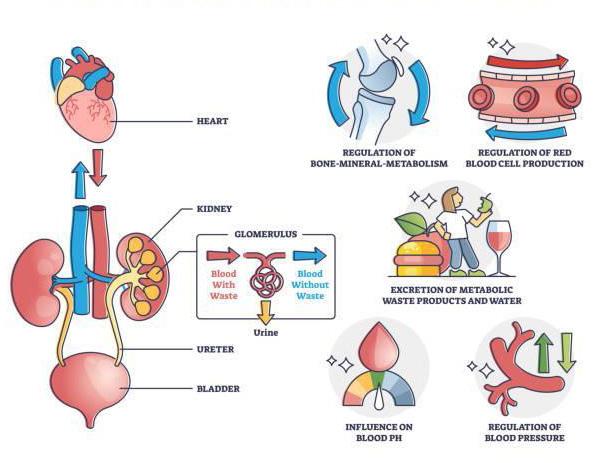
n Blood volume Regulator
Adjusting the volume of blood or eliminating water via urine production.
It is researched and documented that Aboriginal Australians with CKD had observable poorer oral health than the general Australian population and a general Aboriginal population from Australia’s Northern Territory. 4 The barriers they face include:
n Living in remote areas of Australia
n Inability to travel to a nearest dental clinic
n Poor nutrition
n Lack of support and education
n Poor health, family history of CKD and other illnesses
n Lots of infections that have not been properly treated
n Lack of money

n Having heart failure, or having had a heart attack or stroke
n Having kidney disease in the family
n Being overweight or obese
n Smoking or having ever smoked
n Being over 60
n Being of Aboriginal or Torres Strait Islander origin
n A kidney injury, infection or cyst in the past
n Kidneys can also be damaged by misuse of some painkillers, prescription medication
n Less common but should not be discounted – genetic
Clinical features depend on underlying systemic or renal issues and the rate of renal function impairment.
n Arterial Hypertension- common
complication- retention of sodium and activation of RAAS (renin angiotensinaldosterone system).
n Uraemia - Generalised pallor (second to anaemia) brown hyperpigmentation (secondary to retention to dietary pigmentation).
n Anaemia – secondary to impaired erythropoiesis (red blood cell production).
n Haemostatic impairment can be altered due to platelet dysfunction and anticoagulant use in dialysis.
n Platelet dysfunction - Increased risk of bleeding due to:
– Diminished platelet count due to mechanical trauma from dialysis
– Reduced platelet adhesion due to increased prostacyclin activity, decreased platelet factor and decreased capillary strength.
n Immunosuppression due to Uraemia and resulting in decreased cellular immune function and impaired chemotaxis.
n Renal Osteodystrophy - Impaired mineral metabolism, increase risk of fracture, bone defects and calcifications. >>
n Endocrine dysfunction - increased risk of hyperparathyroidism, delayed growth, infertility in women and erectile dysfunction in men.
When managing CKD, it is important to consider the following:
n Diagnosis timing
n Stage of disease
n What other functions are affected?
In order to preserve the deteriorating kidney health, the following may be considered:
n Lifestyle modification
n Medications - antihypertensives, lipid lowering agents, iron supplements and RBC stimulation drugs
n Calcium and phosphate metabolism
– restrictions in diet- e.g. calcium carbonate
n Supplementation with Vit D may be needed.
n Aspirin and other NSAID’s – on advice
The kidney compensates for the loss of nephrons through remaining nephrons until approx. 50% of functional nephrons have been lost.
Sequelae
n Acute renal failure (ARF) significant reduction in glomerular filtration rate (GFR )– typically not suitable for
elective dental treatment.
n Chronic renal failure (CRF) progressive loss of functional nephrons and reduction in GFR –final point is End-stage renal Failure (ESRF) - only managed with dialysis and or kidney transplants.
n CRF - is frequently called a ‘silent disease’ as up to 90% of kidney function may be lost before symptoms appear. Generally, urine and blood tests can identify most cases of CRF when the disease is in its early stages
Haemodialysis
Filtration is carried out by a machine called a Dialyzer. It carries blood through a semipermeable membrane to filter out toxins and metabolites. This procedure is performed three days a week and requires a permanent catheter or arteriovenous fistula which is usually placed in a day centre or hospital. Heparin is used to ensure permeable vascular access and constant blood flow through the dialyzer.
Peritoneal Dialysis requires the placement of a catheter in the peritoneum of the abdomen.
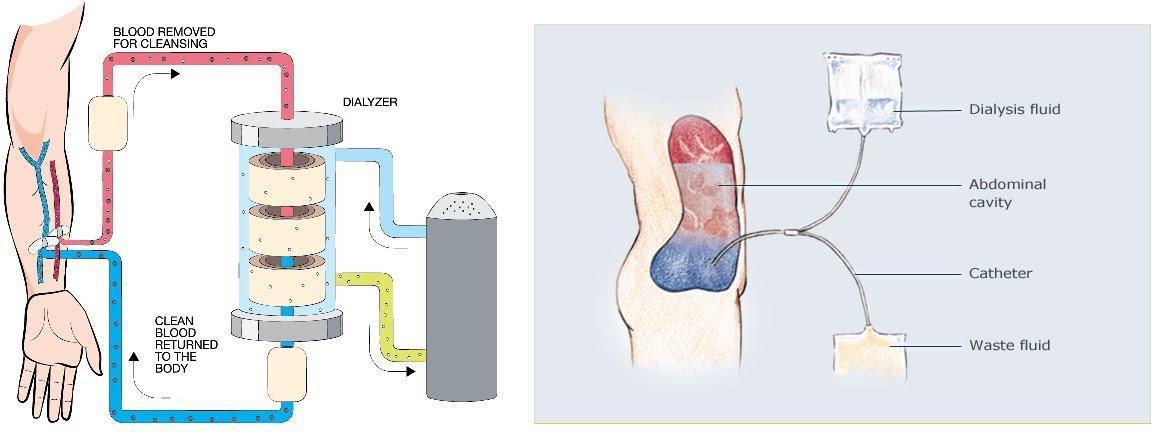
A hypertonic glycosated solution (this creates greater osmotic pressure to
remove toxic products).
This filtration occurs using the peritoneal membrane of the patient to filter blood waste products.
This form of dialysis can be performed at home but must be done every day.5
Dialysis Risks and Considerations
Dialysate constituents diffuse into the patient’s blood.
Arteriovenous fistulae create a potential portal of infection. Alternatives may be polytetrafluoroethylene (PTFE), or an indwelling cuffed catheter.
2-9% of haemodialysis patients develop infective endocarditis secondary to staphylococcal infections that develop at the site of the graft (PTFE newly placed, arteriovenous fistula, or long-term cuffed venous catheters).
Antibiotic prophylaxis will be discussed in relation to oral care.
Transplant
Renal transplantation is indicated in patients with irreversible renal failure.
Immunosuppressive therapy before and after surgery to prevent rejection.
Immunosuppressive therapy persists for life unless donated by an identical twin.
There may not be any specific symptoms
of CKD, however, oral manifestations may be present secondary to the disease.
Poor oral health may imply more infections and therefore greater impact on systemic inflammation. Some signs and symptoms to watch out for can include:
Uraemia- Bad Odour, metallic taste. Xerostomia – due to reduced fluid intake, polypharmacy, salivary gland dysfunction and sleep apnoea.
Pallor – pale mucous membranes.
Uraemic stomatitis (uncommon)painful bleeding, hyperkeratotic ventral tongue and buccal mucosa.
Bleeding- Petechiae, Ecchymosis (Bruising) resultant from Platelet dysfunction.
Gingival Hyperplasia – secondary to the use of cyclosporin, calcium channel blockers.
Erosion- particularly lingual surfaces due to persistent vomiting and nausea.
Periodontal disease, pulp obliteration, enamel hypoplasia, delayed dental eruption- related to calcium and phosphate metabolism.
Altered bone composition- Renal osteodystrophy resulting in decreased
trabeculation, loss of cortication, giant cell radiolucencies and soft tissue calcifications. This may increase risk of fracture during extractions. Caries – Decreased due to the bacteriostatic effect of urea.
Infections – Candidiasis, Cytomegalovirus (CMV) following transplantation- and immunosuppression.
Mucosal lesions – Lichenoid and oral hairy leucoplakia secondary to immunosuppression.
Malignisation- Potential risk of epithelial dysplasia and carcinoma post renal transplant. Immunosuppression predisposes mucosa to viral tumours such as Kaposis Sarcoma or nonHodgkin’s lymphoma.
Systemic diseases - CKD can cause changes in the periodontium exacerbating the inflammatory response and causing degeneration of the gingivae
Uraemia causes lymphocyte response suppression, granulocyte dysfunction and cell-mediated immunity suppression.
A study by Carthilho et al 2007, Klassen and Krasko 2002 ,
Tadakamadala et al, 2014 suggest that patients undergoing haemodialysis are more prone to poorer oral health conditions than the general population. Another study by Gomes do Nascimento et al in 2018 suggest that CDK patients undergoing haemodialysis may present with a decrease in leukocyte production – triggering severe periodontal predisposition.
Formation of dental calculus due to decreased magnesium, increased urea and phosphorus, may lead to increased precipitation and thus dental calculus formation.
When treating and providing care to patients with CKD, dental practitioners need to be aware of the patient’s medication history. Check if there are contraindications you need to consider when using or recommending treatment and products, for example some products contain excess potassium, sodium, magnesium, certain antibiotics, NSAID’s, herbal or complementary medications may be a problem. Checking with the treating specialist or GP is recommended.
Frequently used medications in CKD include:
– anti-hypertensives to control blood pressure.

– medications to keep the heart healthy, for example, cholesterol tablets.
– medications to control other health conditions the patient may be living with such as diabetes, thyroid disorders, pain and arthritis.
– diuretics (such as frusemides) to increase urine output.
– phosphate binders to control your phosphate levels.
– vitamin D to maintain strong bones and other benefits.
– injections, including erythropoietin and iron, to control anaemia.
What level of dental treatment can be provided to CKD patients?
Stage 1- 3 do not pose any >>
contraindications for routine dental treatment.
Stage 4 – 5 (advanced kidney disease) – risks- hypertension, anaemia, risk of bleeding, infection, medication in use, oral manifestations associated with CKD and haemodialysis.
Patients on Peritoneal dialysis DO NOT generally require special measures apart from avoiding nephrotoxic drugs ( e.g. tetracycline, erythromycin, neomycin, cephalosporins and some NSAID’s.
Patients on Haemodialysis
1. Patients with systemic problems
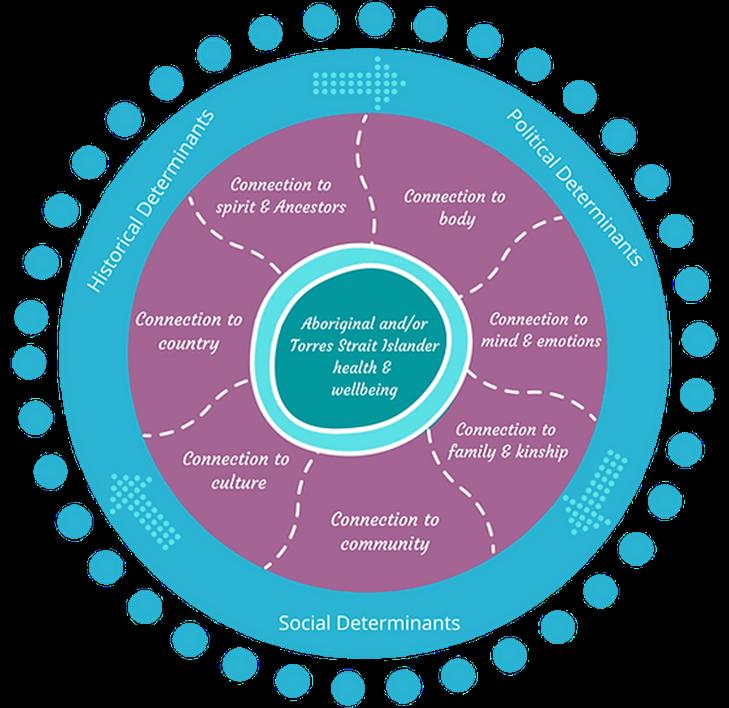
– Consult with the Nephrologist and the treating dentist

– Review medical history thoroughly
2. Bleeding Risk
Dental treatment should be on NON Dialysis day
– Platelet function optimal and Heparin will have worn off
– Prolonged bleeding may occur so ensure protocols are in line with Nephrologist recommendations
– Some patients may still be taking blood thinning agents
Antibiotic Prophylaxis
There is a lack of evidence to support the ongoing use of Antibiotic prophylaxis unless specified.
It is likely the specialist would advise the 6months following the creation of vascular access –
BEST PRACTICE – discuss with Nephrologist (case by case) – consider general health and any other comorbidities
Medications for dental purposes:
n Local Anaesthesia can be safely used as they are via hepatic elimination
n Paracetamol remains best choice for analgesia ( including codeine)
n NSAID’s – e.g. Ibuprofen, Naproxen can cause hypertension and worsen bleeding
n Aspirin contraindicated – increases platelet dysfunction, risk of gastric haemorrhage and contributes to the
deterioration of renal function
n If the patient is on long-term Corticosteroids (may require supplementation) on advice.
Pre-transplant dental assessment:
n Indications for extractions – risk of bacteraemia post transplant when the ability to cope with systemic infection decreases.
n tooth mobility – periodontal pocket > 5mm
n endo- perio lesions
n periapical lesions
n extensive caries
n Usually, dental hygiene preventive care is provided to provide an environment that minimises bacterial load
Critical period is during the first 6 months - receiving highest dose of immunosuppressive medication.
n Highest risk for post-op complications – opportunistic viral and fungal infections, risk of graft rejections.
n Emergency dental care only under antibiotic prophylaxis.
n Preventive regimes, smoking cessation and eliminate alcohol.
n Even when debridement cannot be provided – oral health education and simple strategies for care are invaluable.
n Educational and preventive opportunities are never wasted and builds a valuable relationship
Immunosuppressive regimes.
Prednisolone
Combined with non-steroid immunosuppressive medications to allow decreasing dose of prednisolone.
n cyclosporin (gingival hyperplasia) sirolimus, azathioprine.
Tacrolimus, mycophenolate
* Immunosuppression implications.
n Antibiotic cover for high-risk dental procedures at least two years post transplant.
n susceptible to oral fungal/ viral infections.
n Increase in malignancy risk: lymphoma, cutaneous cancer e.g. basal cell, SCC - leucoplakia, Kaposis sarcoma.
n Preventive care
n Education
n Timed debridement keeping in mind stage of treatment
n Tailored preventive and therapeutic care
n Considerations what is the most critical need for this person – today!
n Be prepared to go off script
n Know your products and consider simple advice
As a team and integrated approach, please note that:
n Patients at any stage of CKD will require some dental care in their life
n Early stages of kidney disease may be asymptomatic
n The risks of infection in this population is a potential threat for both dialysis and transplant recipients
n It is our collective responsibility to seek input from each other
n To recognise the importance of a multidisciplinary approach
If you are working in remote areas –get to know your team.
n Nephrologist
n General Practitioner
n Dental Health Care team. Dentist, DA, Dental Hygienist, OHT
n Aboriginal HCW
n Practice Nurse
n Dietician
n Pharmacist
Besides the clinical aspects of CKD, practitioners must also consider
• Special Needs Unit Adelaide Dental Hospital and the University of Adelaide for their support and information, in particular Associate Professor Sharon Liberali, Dr Keng Yeoh who are always so generous with their time.
• Margie Steffens OAM ADDH, B.Sc Dent ( Hons) FICD Chair for Special Needs Dentistry SIG (Suggested CPD 0.75 hour scientific)
1. https://kidney.org.au/your-kidneys/what-is-kidney-disease/types-ofkidney-disease#
2. https://www.istockphoto.com/photos/kidney-function
3. https://kidney.org.au/uploads/resources/state-of-the-nation-kidney-healthweek-2016-chronic-kidney-disease-hot-spots.pdf pg.6
the psychosocial aspect of care. Education that allows for fundamental understanding relative to the individuals is important and useful. Practitioners must take time to listen and understand individual patient’s culture and beliefs. Their values and needs must be respected. Practitioner should also familiarise themselves of relevant support services available in order to offer best advice to patients.
n Comprehensive medical histories
n Understanding your roles and responsibilities
n Knowing the questions to ask your patients
n When not to provide active dental treatment
n Minimal intervention/ palliative dental care
n Knowing your boundaries and who to ask for information
n Inter-professional teams provide the most sustainable care
n Never make assumptions
Universal right to Health Care
The right to health is the right to the enjoyment of the highest attainable standard of physical and mental health.
The UN Committee on Economic Social and Cultural Rights has stated that health is a fundamental human right indispensable for the exercise of other human rights. Every human being is entitled to the enjoyment of the highest attainable standard of health conducive to living a life in dignity.8 n
5. https://kidney.org.au/your-kidneys/treatment/medications-kidney-disease
6.https://www.sjkdt.org/article.asp?issn=13192442;year=2018;volume= 29;issue=4;spage=766;epage
7. https://www.ruralandremotehealth.org.au/indigenous
8. https://www.ag.gov.au/rights-and-protections/human-rights-and-antidiscrimination/human-rights-scrutiny/public-sector-guidance-sheets/righthealth#what-is-the-right-to-health
ACT contacts:
Director Amy McDermott directoract@dhaa.info
Chair Kate Spain. chairact@dhaa.info
n After a great preChristmas catch-up at the East Hotel, the ACT team has been busy planning for the 2023 program.
The first face-to-face event for 2023 is a dinner on Tuesday 7 March at the Southern Cross Yacht Club with Dr Joseph Ryan discussing the importance of the oral biome in health and disease. This is something all oral health professionals need to take a keen interest in. The presentation of the ACT Tammie Birch Inspiration Award is included in the agenda for the night.
Amy McDermott and
Kate Spain also attended the ACT Allied Health Professional Association Forum earlier. The forum has been a regular feature allowing allied health professionals to share information, discuss challenges and network with peers and government agencies.

NSW contacts: Director Warrick Edwards directornsw@dhaa.info
Chair Jinous Eighani-Roushani chairnsw@dhaa.info
n We thank Jody Inouye’s tireless service as she stepped down as NSW chair this year to pursue further studies. Jody will continue to serve on the TOPA working group to support the development of a brand new peak association for the
profession. Jinous ElghaniRoushani kindly agreed to step up as chair and has already worked hard on the sold-out NSW springs fullday CPD held on 25 February at Peats Ridge.
We were so fortunate to have Cathy Boyce travel from interstate to present on the management of hypomineralised molars using silver fluorides, Professor Dileep Sharma on diagnosis and management of periodontal diseases, Dr Ying Shi Chang on oral surgery referrals and Steven Chu discussing oral health for older persons. The event was well attended with many attendees spending the weekend enjoying great accommodation and sightseeing in the region.
The next NSW event will be a half-day get-together in Sydney on Saturday 29 April, so please mark this in your diary and keep an eye out for further details.
NT Contact: Director Hellen Checker. directornt@dhaa.info
Staff Bill Suen bill.suen@dhaa.info
n The NT is still seeking a local member to be the DHAA representative/chair. The role is to be the local eyes and ears for issues pertaining to the Northern Territory. Please contact either Hellen or Bill for further details or discussion regarding the role. We are joining forces with ADOHTA to provide a hands-on workshop on Ergonomics & Edges - a practical approach to hand and scaler health. The workshop is to be held on Saturday 17 June at the Oaks Darwin Elan Hotel in Darwin. Early registration is highly recommended so that you can secure your place as numbers are limited in the hands-on workshop. For more information and registration, please click here:
“ We
“ We were so fortunate to have Cathy Boyce travel from interstate to present on the management of hypomineralised molars using silver fluorides ”
are joining forces with ADOHTA to provide a handson workshop on Ergonomics & Edges ”All smiles at the ACT Christmas catch-up
For all the latest info on DHAA events please visit www.dhaa.info/events
Qld Contacts:
Director Carol Tran. directorqld@dhaa.info
Chair Stacey Billinghurst chairqld@dhaa.info
Deputy Chair Karen Smart contactqld@dhaa.info
n After serving as acting chair last year, Stacey Billingshurst has officially taken over the chair’s role, with Karen Smart joining the team as deputy. We also welcome Lizzy Horsfall back to the Queensland committee after a spell away from official duties over the last couple of years.
On Saturday 11 March, the Queensland committee is presenting a three-hour CPD program at the CQ University Rockhampton campus. They are also streaming the event live via ZOOM so everyone can benefit from the great lineup of presenters and topics. This includes Dr Narelle Eckersley on dental trauma and Dr Justus Pienaar who has dual qualifications in both medicine and dentistry to present on medical history and consent. Please follow this link to register for either face-to-face or to attend the webinar.

SA Contacts: Director Michelle kuss michelle.kuss@dhaa.info
Chair Sue Tosh chairsa@dhaa.info
Deputy Chair Courtney Rutjens contactsa@dhaa.info
n Deputy chair Sally Minors passed her baton onto new deputy Courtney Rutjens but continued to provide support to Chair Sue Tosh at the SA Committee. We are grateful to all of them for their passion and dedication in supporting our SA members through lots of hard work.
The SA Committee hosted its end-of-year celebration on Sunday 4 December at Jarmer’s
Kitchen. With Christmas champagne flowing freely and a presentation by Dr Julie Monis-Ivett OAM on her work to help people in developing countries was incredibly inspiring and moving to all.
SA Committee member Lyn Carman attended the 2022 SA TAFE graduation and awards ceremony and presented the DHAA awards on 9 December. Congratulations to the following students:
n DHAA Academic Excellence
Katie Best
n DHAA Jean McNicol Award
Ella Wakely
n DHAA & GC Jane Chalmers Memorial Award
Kimberly Falco
The 18 March 2023
Destination weekend
will be held at the scenic Willunga with a full day 6 hours CPD program with an impressive array of speakers, including Dr Michaela von Geijer from Sweden presenting on implants and diabetes, Dr Michael Findlay on substance abuse, Dr Arthur Drouganis on LANAP & LAPIP as well as a forensic dentistry session from Dr Harry Perkins. Click here for registration and further information.
TAS Contacts:
Chair Karen Lam chairtas@dhaa.info
Staff Bill Suen bill.suen@dhaa.info
n We welcome Karen Lam of Launceston as our new Tasmanian chair; and within days of her tenure, she attended the February DHAA Board meeting in Melbourne and hosted the joint DHAA-ADOHTA handson workshop roadshow in Hobart.
Karen is also liaising with another Tasmanian member, Danielle Gibbons, to organise our World Oral Health Day Community Program that will reach out to local Asylum Seekers >>
and promote oral health. Tasmanian practitioners are encouraged to contact Karen if they are interested in getting involved and make a difference to both the profession and the public.
Vic ContactsDirector Roisin McGrath directorvic@dhaa.info
Chair Cathryn Carboon chairvic@dhaa.info
Deputy Chair Sarah Laing contactvic@dhaa.info
n As we farewell outgoing Chair Desi Bolado and Deputy Chair Aimee Mills and thank their valuable contributions over the past couple of years, we also welcome new Chair Cathryn Carboon and Deputy Chair Sarah Laing Cathryn is highly regarded as a crusader in oral health promotion, in particular her book Who is the Tooth Fairy’s Best Friend, and work with the Caravan Foundation, while Sarah has been our former state committee chair. Both were present at our end-of-year Christmas celebration at the Kooyong Tennis Club in December to network with members and sponsors. This event is now a Victorian DHAA tradition with growing popularity. Cathryn attended the February DHAA Board
meeting in Melbourne and has provided valuable input to the board on behalf of Victorian members.
CEO Bill Suen attended the 2022 Melbourne University Dental School graduation ceremony on 10 December and extended the DHAA’s congratulations to all graduates.

The joint DHAA-ADOHTA Hanson Workshop was held at the Rendezvous Hotel in Melbourne on Saturday 4 March. The workshop was delivered by Amanda Tomlin and Paulette Smith, both are well-known in the profession, and the set has proven to be very popular.

The Victorian Committee is now focusing on the
planning of its next event which will be a full-day CPD event on Saturday 22 July. Please mark this date in the diary and look out for further information on its topics and speakers.
to fill these roles. These are great opportunities for members to get involved, build networks and make a difference to both the DHAA, the profession and the public through work of the DHAA WA committee. Please contact either Phoebe or Bill if you wish to get more information about the work of the committee.
The WA Half-day CPD event on Sunday 26 February at the QT Hotel in Perth was a full house great success. Attendees were presented with upto-date clinical knowledge on intra-oral burning, Jaw Physiotherapy on TMJ and oral hygiene aids from Dr Lilima Toward, Ms Leigh Ray and Dr Tina Choo respectively. It was a great start for CPD learnings for WA members and the Committee is already planning for the rest of the 2023 program.
WAWA Contacts
Director: Phoebe Thomas . directorwa@dhaa.info
Staff: Bill Suen bill.suen@dhaa.info
n As we say thanks and farewell to outgoing Chair Carmen Jones and Deputy Chair Rhonda Kremmer, we are seeking expressions of interest from WA members
The next WA event will be the 20 May joint DHAAADOHTA Hands-on Workshop. As the number is very limited, we recommend early registration to secure your place. Click here to reserve your spot n

“ The WA Half-day CPD event on Sunday 26 February at the QT Hotel in Perth was a full house great success”DHAA Vic Director Roisin McGrath joins the Melbourne Uni graduates The Kooyong Tennis Club event is now an annual tradition
Get your diaries out and book your time off – these events should not be missed
MARCH 2023
n 4 March
Joint Hands-On Workshop with ADOHTA
Victoria
n 7 March
Dinner Meeting
Australian Capital Territory
CPD: 1 hour
n 8 March
Webinar
Online
CPD: 1 hour
n 11 March
Half Day
Brisbane, Qld
CPD: 3 hours
n 18 March
Destination Full Day
South Australia
CPD: 6 hours
n 23 March
Webinar
Online
CPD: 1 hour
APRIL 2023
n 12 April
Webinar Online
CPD: 1 hour
n 27 April
Webinar
Online
CPD: 1 hour
n 29 April
Half Day
New South Wales
CPD: 3 hours
MAY 2023
n 6 May
Joint Hands-On Workshop with ADOHTA
South Australia
n 10 May Webinar Online
CPD: 1 hour
n 20 May
Joint Hands-On Workshop with ADOHTA
Western Australia
n 25 May
Webinar
Online
CPD: 1 hour
JUNE 2023
n 14 June
Webinar
Online
CPD: 1 hour
n 17 June
Joint Hands-On Workshop with ADOHTA
Northern Territory
n 17 June
Full Day
Western Australia
CPD: 6 hours
n 23 June
Dinner Meeting
South Australia
CPD: 1.5-2 hours
n 29 June
Webinar Online
CPD: 1 hour
JULY 2023
n 12 July
Webinar Online
CPD: 1 hour
n 15 July
Full Day
Victoria
CPD: 6 hours
n 22 July
Full Day
Sydney, NSW
CPD: 6 hours
n 22 July
Webinar Online
CPD: 1 hour
AUGUST 2023
n 2 August
Dinner Meeting
Australian Capital Territory
CPD: 1 hour
n 5 August
Full Day
Queensland
CPD: 6 hours
n 9 August
Webinar Online
CPD: 1 hour
n 24 August
Webinar Online
CPD: 1 hour
Continued from previous page...
n 13 September
Webinar
Online
CPD: 1 hour
n 21-23 September
National Symposium
Adelaide
OCTOBER 2023
n 11 October
Webinar Online
CPD: 1 hour
n 21 October
Joint Hands-On Workshop with ADOHTA
New South Wales
n 26 October
Webinar Online
CPD: 1 hour
n 28 October
Joint Hands-On Workshop with ADOHTA
Australian Capital Territory
Be sure to bookmark the 2023 DHAA National Symposium

NOVEMBER 2023
n 8 November
Webinar Online
CPD: 1 hour
n 12 November
Half Day
Western Australia
CPD: 2 hours
n 18 November
Joint ADOHTA
Full Day
Launceston, Tas
n 23 November
Webinar
Online
CPD: 1 hour
n 25 November
Half Day
Australian Capital Territory
CPD: 3 hours
n 2 December Christmas Brunch
Victoria
CPD: 4 hours
n 2 December Christmas Brunch
Queensland
n 3 December
Christmas Brunch
South Australia
n 13 December
Webinar Online
CPD: 1 hour