THE ART OF COMMUNICATION














A PHENOMENAL time to be part of the oral health community! After much anticipation, I am thrilled to announce that the Oral Health Association of Australia (OHAA) is officially registered. This milestone marks the beginning of a new era for our profession, and behind the scenes, our eight dedicated appointed directors have been meeting weekly to design and strengthen the foundations of this association. The passion and energy within our leadership team is truly inspiring, and I have no doubt that OHAA will be a driving force for positive change in years to come.
I am also excited to share that we are in the planning process of the first OHAA Congress Our team of volunteers has been pouring their heart and soul into creating an event that is not only educational but also deeply enriching. Held at The Star in the stunning Gold Coast, this Congress promises to be a game-changer, featuring esteemed speakers, hands-on workshops, and valuable networking opportunities. If there’s ever been a time to come together and celebrate our achievements, this is it. I hope to see you there to mark this historic moment.
As we prepare for this landmark Congress, we are also closing an incredible chapter, winding up our association while celebrating our achievements. So, don’t forget to join us for our last unforgettable destination CPD event in Bali in June. Please note that some events, like the upcoming 50-year celebration of dental hygiene in July in South Australia, will be carried forward by the new association. We have had a remarkable journey, and I can’t wait to celebrate these milestones in person with you.
We started 2025 on a high note with the launch of the Residential Aged Care Facility (RACF) Oral Health Service Guideline in February. This crucial guideline is a step forward in ensuring better oral health care for our elderly population. Alongside this, we recently hosted 17 enthusiastic young leaders in Melbourne for the face-to-face workshop of our Future Leaders Program facilitated by A/Professor Nicky Kilpatrick and Dr Trudy Lin. These incredible individuals represent the future of oral health, and their passion and dedication give me great confidence in what lies ahead.
This edition of the DHAA Bulletin focuses on Special Care Dentistry—an area close to many of our hearts. As we strive to improve access and care for those with special needs, it is heartening to see professionals stepping up to advocate, educate, and innovate in this field. I encourage you to engage with the insightful articles and discussions in this issue, as they highlight the incredible work being done to ensure equitable oral health care for all.
As we move forward, let’s take every opportunity to celebrate our achievements, support one another, and shape the future of our profession. We remain committed to our pledge to advocate under the existing association, and we hope that this spirit of advocacy continues to flourish under the new OHAA. We are also looking forward to seeing all our members at renewal time as we transition into this exciting new association.
I look forward to seeing you at our upcoming events, especially our OHAA Congress, and let us all continue to be ambassadors for oral health in our communities!
Jinous Eighani-Roushani DHAA President



04 OHAA Congress
We look forward to the firstever congress under our new assocation banner.
06 Rallying call
Support our Mouth Matters campaign.
09 Meet your new association
Say hello to the OHAA.
10 Ask DHAA
Your questions answered.
12 The power of connection
Building networks and relationships to grow your career.
16 Bridging the divide
Collaboration, respect, and self-reflection in modern dental teams.
20 50 years of dental hygiene in Australia
Celebrating the half century milestone for our industry.
22 Becoming deaf aware
How to manage hearing impairment and oral health.
30 Get your online CPD fix
Enjoy learning from home.
34 Handling special needs
Discussing our role as oral health professionals.
36 State of the Nation
Our regular round-up of state happenings.



By Shida Taheri
We are thrilled to announce the inaugural Oral Health Association of Australia (OHAA) Congress, set to take place from 16-18 of October 2025 in the beautiful sunny Gold Coast in Queensland. This historic event marks the first national congress uniting dental hygienists, dental therapists and oral health therapists under the OHAA banner.
The conference program will feature a dynamic lineup of keynote speakers, interactive sessions, and hands-on workshops designed to enrich your professional knowledge and skills. Delegates can participate in a full day of workshops and earn a full year’s CPD over three action-packed days. Topics will cover a broad range of subjects, including the latest advancements in dental hygiene, oral health therapy, and collaborative care models. We are honoured to welcome back the sponsors who made our
last conference so memorable. Their contributions have been instrumental in fostering knowledge and innovation within our community. We thank all of our 2025 sponsors but a special mention goes to our major congress sponsors: Piksters Erskine Dental (Platinum), Oral B (Gold) and Colgate (Bronze). We look forward to welcoming them back this year for what promises to be an exceptional trade hall.
We are very keen to hear from both researchers and practitioners sharing your work through the contributed paper and poster sessions. Call for abstracts is now open and we look forward to seeing you presenting at the Congress.
In addition to the educational sessions, there will be ample networking opportunities. Connect with industry leaders, fellow professionals, and exhibitors during our welcome reception, scheduled networking breaks, and the highly anticipated
Gala Dinner. Experience the vibrant trade displays and discover the latest products and technologies that are shaping the future of oral health care.
Registration for the OHAA Congress is now open – click here. This will be a three day congress offering over 18 hours of education. Take advantage of early bird discounts by registering now and get your first pick of workshops before they are filled!
This Congress represents a significant milestone in our profession, uniting all oral health practitioners under one cohesive association. Together, we can elevate the standards of oral health care in Australia and beyond. We look forward to welcoming you to this extraordinary event and collaborating to shape the future of our field.
So, save the date, mark your calendars, and plan your trips, because OHAA is coming to sunny Queensland this October. n



2024 DHAA & ADOHTA Congress feedback
“Excellent presentations and organisation. Value for money”
“Very well organised. Location was good, food was excellent and the vibe was great. Well done!”
“Worthwhile, feeling reinvigorated”
“Love having it at a hotel over a conference centre. Staying, learning and socialising all in one location makes it so simple”
“Fantastic networking, I met so many colleagues and made a lot of new contacts which was great”
TITLE: Can oral hygiene practices impact on the risk, incidence, and mortality in cardiometabolic diseases. A systematic review.
Presenter: Lauren Church, OHP, NSW
Rationale: To evaluate if oral hygiene practices including: toothbrushing, interdental cleaning, toothpaste and/or mouthwash use impact on the risk, incidence, and/or mortality rate of cardiometabolic conditions.
Method: This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement. The review protocol is registered with PROSPERO ID: CRD42021269584. Searches were conducted using electronic databases: MEDLINE, EMBASE, Scopus, and CINAHL, as well as grey literature and hand searching.
Results: Forty-eight eligible studies were identified. Toothbrushing and interdental cleaning were found to have positive impacts on cardiometabolic disease risk, incidence, and mortality.
Whilst the benefits of mouthwash proved inconclusive, with a potential detrimental impact. Toothpaste was not independently associated with disease outcomes.
Conclusion: Interdental cleaning daily, followed by twice daily toothbrushing for at least two minutes has significant positive impacts on cardiometabolic disease outcomes. The provision of basic oral health education should be expanded beyond dental setting and integrated into routine health messages for patients with cardiometabolic diseases.
Clinical significance: Oral and cardiometabolic diseases are major public health issues. Oral health education is rarely provided outside of the dental clinic. This systematic review highlights the importance of simple oral health practices in reducing cardiometabolic risk and could encourage non-dental clinicians to integrate this information into general health promotion for patients with chronic disease.
The DHAA Mouth Matters campaign needs your support to make a difference

Bill Suen DHAA CEO
IN THIS EDITION of the DHAA Bulletin, I would like to share with you the DHAA 2025-2026 Pre-budget Submission to the Federal Government.
The DHAA is now running a major campaign to advocate for our request in the submission. The campaign is called Mouth Matters (image right), and we are seeking the involvement of all DHAA members by calling on your local member of parliament to discuss our submission. There are briefing materials and a webinar available to guide your discussion.
therefore focused on utilising existing funding mechanisms to address two of the major challenges that the Government faces, namely oral health and aged care.
Good oral health is essential for overall wellbeing and general health

If you are interested to participate, please email ceo@dhaa.info.
The Dental Hygienists Association of Australia (DHAA) thanks the Assistant Treasurer and Minister for Financial Services for the opportunity to present our Pre-Budget submission for consideration in the development of the 2025-2026 Federal Budget. It is our view that addressing oral health presents an opportunity for sustainable and cost-effective investment in health outcomes for all Australians, particularly those with the greatest need.
We understand that there are economic and system constraints for the Government while addressing many competing demands. Our proposal is
Oral health is integral to overall health, affecting quality of life, diet, speech, and social interactions. However, many Australians have limited access to oral health services either due to cost or due to limited availability of local services. As a result, the overall oral health of the community is declining. The Senate Select Committee into the Provision of and Access to Dental Services
disease and cerebrovascular disease. The relationship between diabetes and periodontitis is also well-established, with hyperglycaemia negatively impacting oral health and severe periodontitis can negatively affect glycaemic control.

proposed expanding access to oral and dental services in general practice and primary care settings. The Australian Government in its response has committed to exploring opportunities to support the primary care system to contribute to delivering better oral health outcomes.
Oral diseases not only impact general health, they are also linked directly to other chronic diseases such as cardiovascular disease, pulmonary disease, and diabetes. The relationship between oral health and chronic disease is bi-directional. Improving oral health decreases the risk of atherosclerotic disease, the primary cause of most coronary heart
In Australia, dental care comprises both preventative and surgical care and is delivered by dentists and specialist dentists. Oral care, on the other hand, is delivered by oral health practitioners, including dental hygienists, dental therapists, and oral health therapists, and focuses on oral health assessment, consumer education and early intervention, targeting conditions such as tooth decay and gum disease. Oral health practitioners assess oral health, use conservative but effective treatments such as fluoride varnish, and support consumers to self-manage their oral health. Both dental and oral health care services are predominantly self-funded or covered by private health insurance, with limited funding for public dental services meaning access is often constrained by underfunding and long wait times. Public funding for oral and dental care services for eligible children is available through the Child Dental Benefits Scheme (CDBS) and can be delivered in primary care settings. However, there is no direct Commonwealth funding for adult oral and dental care in the
health setting.
Integrating oral care into primary care
n Leveraging GPs for oral care
The role of general practice in supporting oral health is well established. Previous research published in the Australian Journal of General Practice have noted the volume of appointments with general practitioners (GPs) for dental problems and high rates of potentially preventable hospitalisations for medical conditions of dental origin. One article notes “while GPs commonly provide pain relief, antibiotics, advice on oral hygiene and referrals to dentists, primary dental problems often are not definitively resolved, resulting in return visits.”
n Expanding CDM to include oral health practitioners
The Chronic Disease Management (CDM) program supports coordinated
“The DHAA is now running a major campaign to advocate for our request in the submission. The campaign is called Mouth Matters”
care by allowing GPs to refer patients to allied health professionals under Medicare. The program provides an important complement to general practice services, allowing the GP to establish a multidisciplinary team to support the health needs of their patient. This provides an important opportunity to recognise and support the oral care role of general practice and the bi-directional connection between chronic diseases and oral health. Allowing general practitioners to refer patients for Medicare-funded oral care services delivered by oral health therapists, dental therapists, and dental hygienists provides an opportunity for evidence-based oral care for chronic
disease patients to be delivered as part of multidisciplinary arrangements. This will particularly benefit those with diabetes or cardiovascular conditions, where oral health can significantly impact overall health.
This proposal is not a dental service. It would allow oral health practitioners to assess oral health and provide early intervention support and advice focused on improving oral health management. This proposal would alleviate pressure on the GP network. The National Advisory Council on Dental Health estimated that there are more than 750,000 GP consultations each year for dental problems, the most common treatment being prescriptions for pain relief medication and antibiotics.
n Benefits of including oral health practitioners in CDM:
1. Oral Health Assessment and Education
Dental hygienists, dental therapists, and oral health therapists can provide essential oral care, addressing oral health issues that exacerbate chronic conditions. By incorporating these professionals into CDM, patients with chronic illnesses receive comprehensive care and education that supports oral and systemic health management.
2. Collaborative, Holistic Care
Expanding CDM to include oral health practitioners supports a collaborative approach, with GPs, dietitians, and diabetes educators working alongside dental professionals. This integrated model enhances chronic disease management, reducing inflammation and oral infections that may worsen systemic health.
3. Improved access for at-risk populations
CDM referrals to oral health practitioners offer at-risk populations accessible, early intervention care. Oral care services can be provided in GP clinics, residential aged care
facilities, and patient’s homes.
Patients, particularly children and adults with dental anxiety, benefit from receiving oral care in familiar GP, residential aged care facilities (RACFs) or home settings, reducing barriers to essential services.
Historically, dentistry adopts a treatment dominated, surgical interventions, invasive and hightech approach to care that is often expensive. Costs have always been a major barrier for consumers and governments. While incorporation of dental services into the universal health coverage would allow dental services to be integrated to overall health care services and improve access, the scheme is likely to be complex and takes time to develop.
A preventative, maintenance and minimal intervention approach will reduce the burden on the clinical paradigm that has shown to be ineffective within the current system. An approach that provides RACF residents with oral care, improvement in oral health literacy of residents, staff and carers, and provision of a referral pathway for timely medical care and complex dental treatment has been successful.
As most RACF residents would have multiple medical issues and chronic diseases, our proposal would enhance their access to oral care that address many of the oral health issues raised in the Royal Commission into Aged Care Quality and Safety Final Report.
The DHAA calls on the Commonwealth government to:
1. Expand the list of eligible allied health professions that can provide GPreferred Medicare Chronic Disease Management (CDM) services to include dental hygienists, oral health therapists and dental therapists.
2. Include dental hygienists, dental >>
therapists and oral health therapists in the list of eligible professions that can be employed by general practices under the Workforce Incentive Program – Practice Stream (WIP).
Evidence about the role and impact of oral disease on the health and wellbeing of the Australian community is clear. By implementing practical changes to the CDM and WIP programs, the Commonwealth government can take an important step towards improving the health and wellbeing of Australians with chronic disease and bridge the gap between primary care and dental services.
Our proposed practical and achievable changes will dramatically increase consumer access to oral care and recognise oral disease as a chronic condition with direct links to other chronic diseases and general health. We reiterate that this is not a proposal for dental services. Instead we seek inclusion of oral health practitioners into existing funding mechanisms that are already budgeted for. If implemented, we will expect a paradigm change towards a GP led, integrated approach to:
• improve the management of chronic diseases
• strengthen oral care in RACFs and at-risk population groups
• reduce the burden on high cost dental and medical treatments through early intervention and self care
Submitted by
Bill Suen Chief Executive Officer

THE DHAA ACT Tammie Birch Inspiration Award was created in memory Tammie Birch, a consciencious, dedicated and active ACT dental hygienist who passed away from osteosarcoma in 2019 at the age of 38.
This year’s recipient was Kathryn Novak, who received her award at the recent ACT dinner on Tuesday 18 February.
Kathryn was delighted and spoke of her journey and opportunity that came about through dental hygiene. She paid tribute to her mentors Liz Mendoza and Dr Scott Parsons where she worked as a dental assistant. She recalled her graduation from Gilles Plains (SA) in 1989, working in an orthodontic practice in Canberra, her marriage and family, being posted to big cities and small country towns creating different opportunities–including defence contracts–as a pioneer of our profession.
Returning to Canberra 2005, Kathryn was encouraged to fill in as
a national councillor for the DHAA, a position which led to many and varied roles both locally and nationally. She was involved in changing the federated association structure to the unified one truly national organisation in 2014. She gained a stack of experience and broadened her horizons in corporate governance, dealing with stakeholders such as AHPRA, ADA, ADOHTA, and was ultimately elected as DHAA National President.
Kathryn’s other career highlights include being chair of National Symposium 2014 in Canberra. This role provided the platform to network and develop friendships with many amazing people, as well as gaining new skills, knowledge and experiences. She is pleased to see changes in the profession and the emergence of new opportunities that are so varied, endless and unimaginable initially. She looks forward to celebrating the 50th anniversary of dental hygiene in Australia later this year. n

The creation of a new professional association brings many challenges and some equally exciting opportunities
Planning for the new Oral Health Association of Australia (OHAA) is well underway, with the company being registered with ASIC in January. The OHAA Board is composed of eight directors appointed by the current DHAA and ADOHTA Boards. The DHAA appointed directors are Jinous Eighani-Roushani, Roisin McGrath, Ron Knevel and Cheryl Dey, while Jessica Pennay, Burt, Tim Budden and Jude Ottaway have been appointed by the ADOHTA Board.
The inaugural OHAA Board has representation from all three divisions of the profession with an impressive mix of skills, experience as well as management and public health qualifications. In order to meet the 1 July target for OHAA to fully operational, the OHAA Board has been meeting on a weekly basis to go through the long list of implementation tasks.
Congratulations to Cheryl Dey who has been elected as the inaugural President and Tim Budden, Vice President at the recent OHAA Board meeting on 25 February 2025.
Recruitment for a CEO to lead the new organisation is well underway with the help of Brooker Consulting, a specialist agency with significant experience in executive recruitment for not for profit and professional associations in the heath area, particularly in dentistry. Find out more about the role here.
“The inaugural OHAA Board has representation from all three divisions of the profession with an impressive mix of skills, experience as well as management and public health qualifications”
We expect significant interest from both delegates and sponsors to this momentous event. Registration for the Congress is now open. For information and registration please follow the following link.
As the workshop choice is first in best dress, with all sessions are well sought after, it is advisable to register early to secure your place and make use of the early bird savings.
It is anticipated that all current DHAA and ADOHTA members will be contacted by email in May/June this year. Instead of renewal, you will be invited to join the OHAA. You will also have the opportunity to select the option to renew or subscribe to the Professional Indemnity Insurance that offers great savings and value to members. Let’s see who will become the first OHAA member in this historical moment.
The 2025 National Congress will be held at the Star Gold Coast between 16 and 18 October. This is the first annual Congress under the new OHAA banner. This is now a three-day education event with excellent value.
In the meantime, DHAA is operating as usual but with many activities being run as joint events with ADOHTA. Please email DHAA CEO Bill Suen at ceo@dhaa.info if you have any concerns or queries. n
Your opportunity to ask the questions, check the rules and share your knowledge
Dear DHAA... Just wanting to seek clarity regarding the correct approach for charging radiographs. Specifically if an OHT is working under a dentists provider number. If they are the one who is taking and interpreting the radiograph that code should be claimed under their code within the practice, and not to the dentist? Does this change if the dentist comes in for a check up and reviews the radiographs? Just wanting clarity from a legal perspective regarding the liability.
It is important to note that provider number and item code arrangements are purely commercial arrangements between the providers, the funding agencies and the patients regarding payment of service. It does not have any bearings on professional
and clinical practice. In addition, each funding agency also makes their own rules in terms of payment of claims and they may differ from each other.
How you and your practice claim for the treatment is a business decision.
Each practitioner must adhere to your own scope and Dental Board Guidelines, independent from the claiming procedure adopted by your practice.
The commercial liability usually rests with the person whose provider number is used for making the claim.
Dear DHAA... Just wondering if there are still any health funds that do not accept our provider numbers?
All health funds (except HBF) are accepting our provider
numbers. HBF is yet to set us up in their IT system, as they have just had a major system change recently so there will be some delays. Please note that they all set different rules on what item codes we can claim though. In addition, while we have access to the Commonwealth’s CDBS, we are still expected to claim any DVA dental benefits under a dentist’s provider number.
Dear DHAA... Have there been any cases under workers compensation for hearing loss due to exposure of high frequency sound over many years? Where can I get help if this has impacted on me working as a dental therapist for over 25 years? There is plenty of evidence indicating high frequency sound as part
of occupational hazard for dental practitioners and we have had many CPD on this over topic the past few years. You definitely could lodge a claim if you can prove that the damage is directly linked to your workplace. However, whether there are successful claims under worker’s compensation is the matter that a lawyer will have to advise. In addition, the circumstances surrounding each case is also different. You may wish to contact the DHAA IR advice line, but i think your query may be out of scope of our IR service which only provide basic information and not getting into such complex details.
I suggest you seek advice from a medical practitioner and audiologist in the first place to confirm the hearing loss and more importantly, to

investigate if it is caused by your work. Once this is done, they may be in the position to advise you if you may seek the service of an IR lawyer.
Dear DHAA... Are there any support I can get from the DHAA regarding opening my own business as a dental hygienist? Would really appreciate any guidance or advice.
When you start up your own practice, there are also local and national obligations such as ATO, ASIC, consumer affairs etc. Please go to the DHAA member portal and your advice and support section (business advice) has links to various websites of relevant information.
You will need to engage a proper accountant to advise you with various business obligations.
You may also need business insurance as well, in addition to your professional indemnity insurance. You can contact our PI insurer (dhaa@ bmsgroup.com ) for further assistance and advice.
Dear DHAA... Is it true that dental hygienists (and dental therapists, oral health therapists) are not permitted to see patients who have not been examined by a dentist for 12 months or more? I have a patient booked to see me next week and he refuses to see a dentist for an examination.
Oral health practitioners (including DHs, DTs and OHTs) are independent dental practitioners registered under Ahpra. You are expected to act in a safe and competent manner when treating your patients. There is no
legislation prohibiting any member of the public seeking treatment from any health practitioner, nor prohibiting any health practitioner seeing any patient.
However, your query covers two important issues:
1. Professionally and clinically you can see any patients, provided that what you do is within your scope of practice. Any advice or treatment that is outside your scope must be referred to the correct practitioners (GP, dentists, diagnostic providers etc). In this case if the patient had not seen a dentist for a long period and he refuses to have an examination. If you professionally think that you providing treatment under this condition is unsafe for the patient, then you must advise the patient and where appropriate, refuse to provide
the treatment. If you deem the treatment safe and appropriate then you may proceed with it.
2. Some legislations or commercial rules set by various funding agencies (e.g. Medicare, individual health funds) may exclude certain health professionals in their payment/claims system. In this case the practitioner must inform the patient so that they are aware and make their own decision if they wish to seek treatment from someone that they can access the funding. I must emphasise that this is a commercial arrangement on financial transactions and does not affect your professional obligations and practice rights under Ahpra. n
If you have a question to ask then please email it to bulletin@dhaa.info
By Associate Professor Melanie Aley

“Whether
you’re working in private practice, academia, or public health, connections matter –and your network can serve as a springboard for career growth”
In the world of dentistry, clinical skills and technical expertise are vital—but they’re not the only keys to a successful career. Your ability to connect with others can be just as crucial.
Picture this: A dental hygienist attends a conference and, after a speaker’s presentation, musters the courage to stay behind and ask a question. The speaker’s response sparks a deeper conversation, leading to an invitation to contact them by email.
That connection not only enhances her professional knowledge but she later embarks on postgraduate studies under the supervision of the speaker. These chance encounters often pave the way to lasting professional growth and success. Building strong relationships is an investment that can transform your career trajectory.
The dental community is inherently collaborative. Whether you’re working in private practice, academia, or public health, connections matter – and your network can serve as a springboard for career growth. They can open the door to professional opportunities, with many dental professionals finding career shifts, such as moving into academia or corporate dentistry, through relationships they’ve nurtured over time.
Having a network of peers and mentors to learn from can make it easier to stay informed about new techniques, technologies, and industry trends. Dental practice can be demanding, and having a network of trusted colleagues
to share experiences or seek advice from can provide a support system that makes all the difference in navigating challenges.
To fully unlock the potential of connections, it’s important to build relationships with a variety of people. A mentor can provide guidance and advice based on their own experiences, helping you avoid pitfalls and seize opportunities. Your peers or colleagues in similar career stages can be invaluable sounding boards for ideas and collaborators for projects. Conversely, interdisciplinary networks can be valuable, so don’t limit your connections to dentistry alone. Relationships with medical professionals, business leaders, or academics can broaden your perspective and open unexpected doors. Also, online communities on platforms like LinkedIn, professional forums, and social media groups make it easier than ever to connect with others, even beyond your local area.
No need to think too big
If building connections with others feels intimidating, start small and build your confidence over time. Here are a few practical strategies:
• Attend events
Conferences, workshops, and local dental association meetings are great places to meet like-minded professionals.
• Be proactive
Don’t hesitate to reach out to colleagues or alumni for an informational interview or a casual chat.
• Offer value
Networking isn’t just about what you can gain; it’s about mutual benefit. Share your knowledge or offer help where you can.

• Use digital tools Online platforms make it easier to maintain relationships. A thoughtful follow-up message or sharing a useful article can go a long way.
Building connections doesn’t happen overnight, but small, consistent efforts can yield incredible results. This week, challenge yourself to take one step toward growing your network. Attend a local event, join a
professional group, or send a message to someone you admire in the field. Remember, your network is one of your greatest career assets, and it’s never too early or too late to start nurturing it.
Read Rachelle Johnson's connection adventure
For this month’s career column, I spoke with Rachelle Johnson, Tasmania’s first independent dental hygienist. As you can see from her story, connection has enriched her professional journey with knowledge, support, and inspiration, and enabled her to flourish in her career!

Tell us about your dental business, including your role in the business. Coastal Glo is located in beautiful Northwest Tasmania and I am really proud to be Tasmania’s first independent dental hygienist.
My business started initially as professional teeth whitening services and in 2024, expanded to include advanced dental hygiene care and orofacial myofunctional therapy. I am the sole practitioner in the business wearing all the hats, alongside my only employee, Col, the animal assisted therapy dog. Col is short for Colgate and also because we live in a cul-de-sac. He is always on time and he never talks back!
Did you need any specific education or experience in establishing or running your business?
I had no business education or experience prior to starting Coastal
Glo, just a lot of motivation, passion and belief that this was the right thing to do for me and patients in my community. I completed additional training and courses in OMT, biological hygiene and The Larkin Protocol to supplement my preventive proactive scope of practice.
What are the day-to-day activities in your business?
I love and thrive on the variety of work and knowledge I can acquire, adding the special touches of everything I’ve always wanted in my ideal hygiene department.
My typical day-to-day activities include juggling:
• Patient Administration: crosschecking clinical notes, researching before a patient appointment, personalised oral health homecare plans, handover letters back to a
“I love that my dog, Col, comes to work with me, the patients adore him and he loves it too!
patient's healthcare teams/dental clinics.
• Patient Cases: a variety of whitening, hygiene, OMT consults or progress visits, airway health screenings and sleep screening investigations, dealing with both adults and children, depending on what the day brings.
• Business Administration: liaising with the practice owner of the clinic I work within, health fund processing, patient bookings, follow-up calls and emails, referrals, financial processing and metrics, community education, networking and advocating, as well as social media content drafting.


On top of this workload, I work in a specialist orthodontic practice and regularly fulfil Navy Reserve Days for ADF Careers and Navy Community Engagements Team in Tasmania; I was formally in the Royal Australian Navy Dental Branch prior to commencing my dental hygiene studies.
What’s the most interesting/exciting part of owning your own business?
I love having independence: autonomy of the patient discussions and schedule flexibility to look after my patients better than I ever have before, without the conflict I have experienced in previous workplace environments, typically around scope of practice, communication, wage, leave and toxic workplace cultures.
I love that my dog Col comes to work with me, the patients adore him and he loves it too!
The most exciting part of owning my business is innovation; adding my own creative flare to the business processes and upcoming projects I am working on behind the scenes to truly set a new standard in individualised patient care. Watch this space!
What was the scariest/most challenging part of starting your business?
Stepping away from the traditional model of care that patients have always known. This meant re-educating patients, community and healthcare teams of the updated practice model/ legislative changes for independent dental practitioners.
I experienced self-doubt and judgement from others in my industry and the local dental community. One of the scariest moments was expanding to hygiene services when the major Tasmania Health Fund was not recognising our independent practice provider numbers; it took nine months of advocating at a local level before they finally came onboard.
After leaving my former full-time general dental practice, financially I struggled and survived with minimal work. I didn’t take out a business loan or ask for financial support from family

or friends. It was a blessing in disguise to have the time to set up the practice processes properly and continue to learn and expand in CPD/courses.
Were there people along the way who helped you get the career you wanted?
I feel very lucky to have some amazing colleagues and advocates in our industry who were happy to help and support me on this new pathway, including the wonder woman, Paulette Smith, who was a key mentor during my hygiene studies and in launching Coastal Glo initially – I know she is for many others as well!
Outside of the dental industry at a local level were SME’s in their fields for: insurance, accounting and design. A very small number of kind encouraging dentists on the northwest coast have significantly attributed to supporting the initial integration and ongoing movement.
My awesome community and existing patients are my biggest supporters and advocates to spread word of mouth.
In 2024, I invested in a formal business coach, Jamie-Lee Spencer from Elevate Rise. This has been the missing piece in the puzzle and a testament to the true growth, development and success; I have learnt so much!
Do you have any advice for dental practitioners who may have a business idea they want to put into action?
Don’t doubt yourself! Find and build connections and networks with likeminded people who are supportive of your business idea.
Law of attraction: attract what you are! n
You can discover more about Rachelle's journey on her social media channels: Facebook: @CoastalGlo; Instagram: @coastal_glo
Associate Professor Melanie Aley (nee Hayes) is a dental hygienist who has enjoyed a diverse career in clinical practice, teaching, research and management. She has a Masters of Education majoring in Career Development, and after working in multidisciplinary roles, is now an Associate Professor and the Bachelor of Oral Health Program Director at the University of Sydney.

Collaboration, respect, and self-reflection in modern dental teams
By Lyn Carman
The dental profession in Australia has changed dramatically over the last 50 years. What once consisted of a dentist, assistant, and receptionist has evolved into a team of hygienists, therapists, and oral health therapists. Along with these role expansions, the field has seen a massive increase in treatment options, including costly cosmetic and restorative procedures. While these roles were meant to enhance patient care, they’ve unfortunately led to division within teams. Rather than fostering collaboration, this evolution has caused a loss of camaraderie and a lack of understanding regarding the different scopes of practice.
This divide goes beyond individual practices, rippling through the entire dental profession. It often leads to competition, misunderstanding, and even disrespect, stemming from a lack of appreciation for each team member’s unique contributions. When self-interest and ego take centre stage, professionals may focus only on their expertise or success, overlooking how they contribute to the dental profession. This mindset creates barriers between roles, replacing collaboration and mutual respect with competition and isolation. Ultimately, this fragmentation undermines the profession’s unity and shared purpose, making delivering seamless, patient-centred care harder.
The evolution of dental teams: From dentist to diverse roles
Fifty years ago, introducing dental therapists into the public sector marked
a key turning point. Initially focused on preventive care for children, this role, alongside the evolving role of dental hygienists in private practice, became essential in improving patient outcomes. Today, oral health therapists (OHTs) provide both hygiene and therapy services with an expanded restorative scope. This shift has allowed these professionals to enter private practice, diversifying the skill set within teams and enhancing the ability to offer
“The impact of this egodriven culture stretches beyond the workplace. When team members feel undervalued, disengagement and mistrust set in”
dismissing colleagues’ contributions or dominating discussions, driven by a need for validation. Such behaviour hinders collaboration and fails to appreciate the diverse skills and perspectives within the team.
The impact of this ego-driven culture stretches beyond the workplace. When team members feel undervalued, disengagement and mistrust set in. This is particularly challenging for new graduates, who, entering the profession with a desire to prove themselves, may adopt a competitive mindset rather than one of collaboration. As these divisions deepen, frustration, miscommunication, and low morale rise. New graduates may struggle to find their place in such an environment, hindering their professional growth and integration into the team. As trust erodes, team dynamics weaken, ultimately compromising patient care.
more comprehensive care. However, the rise in roles has often created silos, with professionals focusing on their specific scope of practice rather than valuing each other’s contributions to the collective effort.
Ego-driven elitism subtly undermines dental teams. It happens when individuals elevate their own status— whether through recognition, financial reward, or other means—at the expense of others, undermining the value of teamwork. It often shows up in
As divisions grow within teams, so does their impact on the profession. It’s not about titles or roles; it’s how we view one another. When we fail to respect our colleagues—whether dentists, hygienists, therapists, or OHTs—we lose sight of our shared goal: improving patient care and delivering the best possible treatment.
The real damage happens when professionals see their colleagues as competitors instead of partners. This mentality creates a fragmented working environment where collaboration takes a backseat to selfpromotion. Unfortunately, this lack of teamwork spills into professional >>
communities, exacerbating the divide and fostering an “us versus them” mentality.
The key to rebuilding unity
A significant challenge in overcoming this divide is the difficulty of looking inward. Many professionals may not believe they contribute to the problem and are quick to point fingers. It’s easier to see flaws in others, but real change starts with self-reflection. This isn’t about blame—it’s about understanding how our actions, attitudes, and behaviours may contribute to the divisions within our profession. We must recognise how our actions impact others. We should ask ourselves: Am I unintentionally contributing to the division? Are we so focused on our success or viewpoint that we fail to listen to or respect others? It’s essential to understand that no two people experience a situation the same way, and this diversity of thought should be valued, not dismissed.
building stronger teams
Acknowledge the problem
Recognise that division and ego-driven behaviour exist. This awareness is the first step toward creating a culture of collaboration.
Examine your motives
Reflect on whether your actions are driven by a desire for recognition or a genuine commitment to patient care and team support.

“We must recognise how our actions impact others. We should ask ourselves: Am I unintentionally contributing to the division?”
approach fosters more substantial outcomes.
The Golden Rule—treat others how you want to be treated—provides a solid foundation. The Platinum Rule, however, goes further: Treat others how they want to be treated. It acknowledges their unique values, perspectives, and preferences. By applying the Platinum Rule, we foster more profound understanding, strengthen collaboration, and build unity within the team.
Remember, the ultimate goal is improving patient care and increasing access to dental services. Let this shared purpose guide our actions, helping us focus on collaboration rather than competition.
Understand others
Take time to learn about the roles and challenges your colleagues face. Respect the value each role brings to the team.
Communicate respectfully
Engage in constructive dialogue and respect differing opinions. Healthy communication is key to growth.
Seek feedback
Be open to feedback from colleagues. It helps identify areas for both personal and professional improvement.
Practice empathy
Appreciate each team member’s contribution to patient care. A unified
The evolution of dental teams was designed to improve patient outcomes. As the profession diversifies, we must move forward with collaboration, mutual respect, and understanding. Let’s set aside our egos, value differing viewpoints, and build a culture of trust. When we raise each other, we all rise. Embrace the strengths of your colleagues, learn from one another, and work together to improve patient care. By recognising the unique contributions of every professional, we can move the dental profession forward and create a healthier, more collaborative environment for all. n

Join us to celebrate 50 years of dental hygiene in Australia at our celebratory dinner. Dental hygiene in Australia started 50 years ago in Adelaide. Today, dental hygiene is practised by over 5,000 Oral Health Practitioners (OHPs) in every state and territory.
This event is hosted by the new Oral Health Association of Australia (OHAA) to reflect on the achievements of our colleagues over the past half century, and to celebrate the new era and future opportunities available in dental hygiene for OHPs.
Join us to be part of this momentous event to honour the past, celebrate the present and embrace the future of dental hygiene for our profession.
EVENT DETAILS
Date: 26/07/2025
Time: 6:30 PM - 11:00 PM AEST
Where: Adelaide Pavilion Veale Gardens, Cnr South Terrace & Peacock Rd, Adelaide 5000

BOOK YOUR PLACE

Dental hygiene in Australia has evolved into an integral part of the dental profession in a relatively short period of time. When you compare the profession in Australia to our global colleagues we have achieved a very high level of acceptance and respect since our humble beginnings in 1975 when the first training facility for dental hygiene had its first intake in Adelaide, South Australia.
To discuss the history of the Dental Hygienists’ Association of Australia you must first discuss the establishment of dental hygiene in Adelaide, South Australia as the events are mutually inclusive and linked.
Historically dental hygiene in Australia began in South Australia when enabling legislation was enacted in 1971 allowing dental hygienists to register and practise in South Australia. The first training facility was established in 1974 with the first intake in 1975. It was not until 1977 when the second intake of students began their studies that the registered dental hygienists and current students met to formally form the Dental Hygienist Association of South Australia Inc.
During the ensuing years the Association established itself as the representative body for dental hygienists in South Australia that was used as a point of reference and consultation on all matters relating to dental hygiene not only in South Australia but on a growing scale nationally. It was invited to participate in local and national dental workforce planning workshops and professional development programmes. It forged links internationally and became a member of the International Federation of Dental Hygienists (IFDH) in Oslo on 18 June, 1986. For many years South Australia

Sue Aldenhoven (Founding President of the DHAA), has written about the formation of the Association in 1991
was the only jurisdiction that allowed dental hygiene practice and offered dental hygiene education.
Over the ensuing years legislation allowing dental hygiene practice was enacted in ACT 1979, Northern Territory 1986, New South Wales 1986, Queensland 1987 and Victoria 1989 which eventually led to the formation of a dental hygiene association in all jurisdictions except the Northern Territory. Dental hygienist numbers were growing and the state associations established lines of communication.
Consultation on national dental
hygiene matters continued to be directed to South Australia. South Australia became increasingly aware that it was time for dental hygiene to become organised on a national level and took the initiative to invite representatives of all association to attend an inaugural national meeting in Adelaide on March 18th, 1991. This was an historic event in the evolution of dental hygiene in Australia and it was at this meeting that a resolution was passed to form the Dental Hygienists’ Association of Australia Inc.
Following the meeting a small working
“Historically dental hygiene in Australia began in South Australia when enabling legislation was enacted in 1971 allowing dental hygienists to register and practise in South Australia”
group from South Australia produced a draft constitution for approval by the associations. In preparation for their work they consulted widely and considered a range of national constitutions before they settled on the current model. A major consideration was to ensure that each association retained their autonomy. The national association was to be the collective voice and representative body of the branches nationally but the branches

hygiene on a state, national and international level
• To Promote access to quality preventive oral health services to all peoples
• To promote the art and science of dentistry and foster research in oral health
• To establish liaison between the Association and other allied health organisations, bodies, associations and companies
essential to laying sound foundations for the future. A code of ethics was written, yearly professional development programmes established and a national publication launched. National council met twice a year and the executive met with Federal ADA Executive yearly. Representation was secured on the ADA Auxiliaries Committee and participation in National Dental Health Week planning and activities.

were to retain total autonomy. In essence the national association exists because of the branches and does not have jurisdiction over their functions and rules other than their monetary and reporting obligations to the national. In preparation for the formation of the national association each association changed their name and conducted elections to appoint two national councillors. Later in the year the newly formed National Council, comprising of two elected representatives from each branch and branch presidents met to adopt the Constitution and elect officers. The DHAA Inc. was registered in South Australia on 2 November 1991.
The following four key objectives were adopted:
• To promote, represent and advance the profession of dental
Seed funds were provided to assist in the establishment of the DHAA Inc. through a gift of AU$1,000 from South Australia. Colgate provided corporate support in the form of a monetary donation as well as logo design, stationery and printing of stationery supplies.
An announcement was distributed to all dental organisations and registering authorities which resulted in a very positive response. Initial dialogue was established with the Australia Dental Association Inc. that resulted in a formal meeting of both Executives, which was held at the ADA office in Sydney. Open lines of communication and a professional relationship based on mutual goals established that has continued to this day.
Initially Association business dealt with organisational issue that were

Since this time the Association has gone from strength to strength. To celebrate its 10th Anniversary it successfully hosted the 15th International Symposium on Dental Hygiene and has become an independent and viable organisation that continues to represent the interests of the dental hygiene profession in Australia.
When I reflect over the past 16 years, I am so humble to have been a part of the evolution of such a dynamic organisation and most grateful to those who accompanied me on the journey and shared my vision. n

Sue Aldenhoven Founding President DHAA Inc.
Wishing you all the very best for 2025 and beyond from the Special Care in Dentistry SIG.
We are hoping you are all benefitting from the combined efforts of Oral Health Clinicians who care very much about the ever changing and complex general and oral health needs of our communities.
As a group we come from diverse backgrounds with a range of experiences across the lifespan, cultures, private sector, public sector, education to name a few. I would like to extend an invitation for you to come and share our meetings and your experience in various areas of your profession. Remember we all have something to offer and in a supportive environment you can learn and share your own unique experiences with some of the complex patients you may see in daily practice.
Over the years I have found that with everything I have shared and taught I have learned so much more from my patients and colleagues – so don’t ever think that your small piece of knowledge is not valued – you may surprise yourself.
With the formation of the new association we will be continuing with these special interest groups that provide CPD and support for all of us. With this in mind, consider how you may like to contribute or join our group, it is a wonderfully collaborative environment for sharing our learnings for any member.
We have pleasure in presenting the article, and hope that you enjoy it.
Margie, Victoria, Angie and Danielle

Hearing impairment and oral health: From patient to clinician – a narrative review
Hearing impairments affect a significant proportion of the global population, with implications for health, communication, education, and overall well-being. The relationship between hearing loss and oral health is often under-explored but vital for comprehensive healthcare. This article addresses the prevalence and causes of hearing impairments, their impact on oral health, and strategies to improve care for hearing-impaired patients. Additionally, it examines the implications for hearing-impaired dental practitioners, focusing on workplace accommodations and compliance with Dental Board of Australia (DBA) standards.
Navigating the terminology surrounding hearing loss can be a sensitive and complex task in the current era of heightened cultural awareness and inclusivity. The language we use has significant implications, as it shapes how individuals perceive themselves and their conditions. It is essential to use terminology >>
that reflects respect and inclusivity, particularly in healthcare interactions. For example, the World Federation of the Deaf disapproves of the term 'hearing impaired', as it implies a deficit or disability that is not universally accepted by all individuals with hearing loss. Instead, 'people living with hearing loss' is a more neutral and widely accepted term, particularly in the Australian context. Understanding these nuances helps build rapport with patients and fosters an inclusive care environment.
Key terminology distinctions include:
• Deaf (capital 'D')
Refers to individuals who identify as part of the collective Deaf Community and share a cultural and linguistic identity, often using sign language as their primary mode of communication.
• deaf (lower case 'd')
Refers to individuals with significant hearing loss who may not identify with Deaf culture or the Deaf Community.
• Hard of Hearing
A term that is less commonly used today but may still appear in older publications or be preferred by some older individuals.
• Hearing Impaired
While frequently used in healthcare and formal contexts, this term may not resonate well with those who do not view their hearing loss as a disability or impairment.
This article aims to provide thought-provoking insights and practical guidance for working with individuals experiencing hearing loss, emphasising the importance of sensitivity, respect, and adaptability in delivering care. Ultimately, it is about fostering an environment that prioritises the well-being, communication needs, and dignity of every patient.
Hearing loss affects over 430 million people worldwide, with projections suggesting 700 million individuals will require hearing rehabilitation by 2050.
In Australia, approximately 3.6 million people lived with hearing loss in 2017, a figure expected to double by 2060 due to the aging population. While the majority of disabling hearing loss cases occur in low-income countries, barriers to care also exist in high-income nations, including communication challenges and limited access to suitable healthcare.
The complex relationship between hearing impairments and oral health
“Hearing loss affects over 430 million people worldwide, with projections suggesting 700 million individuals will require hearing rehabilitation by 2050”
warrants attention, given its impact on both patients and clinicians. This article will explore the interplay of hearing loss and oral health, encompassing types of hearing loss, prevention strategies, challenges faced by hearing-impaired individuals, and implications for dental practitioners with hearing impairments. Hearing loss is broadly classified into three types: conductive, sensorineural, and mixed, each with distinct characteristics, causes, and implications. Understanding these categories is essential for effective diagnosis, treatment, and preventive strategies.
n Conductive hearing loss occurs when sound vibrations are obstructed from reaching the cochlea in the inner ear. Common causes include ear infections, perforated eardrums, blockages such as wax or foreign objects, and damage to the tiny bones
in the middle ear. This type of hearing loss often results in muffled hearing and a sensation of blocked ears. Conductive hearing loss is frequently reversible through medical or surgical interventions, especially in children with recurrent ear infections.
n Sensorineural hearing loss arises from damage to the inner ear structures or the auditory nerve. This form of hearing loss is often permanent and is associated with aging, prolonged noise exposure, certain diseases, or ototoxic medications. Sudden sensorineural hearing loss, which can occur abruptly or over several days, requires immediate medical attention to improve the likelihood of recovery. Individuals with this type of hearing loss often rely on assistive devices like hearing aids to manage their condition.
n Mixed hearing loss combines elements of both conductive and sensorineural hearing loss. For example, an individual with long-term noiseinduced damage (sensorineural) who also experiences an ear infection (conductive) may present with mixed hearing loss. While the conductive component may sometimes be treated medically, the sensorineural portion typically requires hearing aids or other assistive technologies.
By identifying the type of hearing loss, healthcare providers can develop targeted treatment and prevention plans, reducing the impact on quality of life and long-term health outcomes.
A vital connection
Hearing loss in children presents unique challenges that extend beyond communication and learning, influencing their oral health and dental care. This condition, whether congenital or acquired, requires a nuanced understanding to provide


• Acquired hearing loss can result from middle ear infections (otitis media), head trauma, exposure to loud noises, or ototoxic medications.
skin, and hair, often resulting in missing or malformed teeth that require specialised care.
• Treacher Collins Syndrome
Cranio-facial deformities associated with this condition can lead to malocclusion and challenges with speech and chewing.
• Cleft palate and lip
These conditions may co-occur with hearing loss due to recurrent ear infections and require coordinated care between dental and medical professionals.

Children with hearing impairments may face indirect oral health challenges due to communication barriers, gaps in oral health education, and limited access to care.
• Communication barriers Difficulty expressing dental concerns may lead to delays in identifying and addressing pain or other issues.

comprehensive and empathetic care to young patients.
Hearing loss in children is categorised into conductive, sensorineural, and mixed types:
• Congenital hearing loss often arises from genetic factors, maternal infections during pregnancy (e.g., rubella, cytomegalovirus), or developmental abnormalities such as Microtia (abnormally small external ear) or atresia (absence of an ear canal). Syndromes like Waardenburg, Usher, and Pendred also commonly involve hearing impairment.
• Education gaps
Limited understanding of oral hygiene practices can result in poor brushing habits, suboptimal dietary choices, and increased susceptibility to dental disease.
• Parental support
Hearing-impaired parents or caregivers may also face challenges understanding oral health instructions, compounding these issues.
Additionally, certain congenital conditions associated with hearing loss may directly impact oral health:
• Ectodermal Dysplasia
This genetic disorder affects teeth,
Hearing loss has a significant impact on oral health and dental care across all age groups. Communication barriers can lead to a lack of understanding of oral hygiene practices, reduced adherence to professional advice, and increased risks of dental caries, periodontal disease, and tooth loss. These challenges are particularly concerning for hearingimpaired children, who rely heavily on clear instruction and guidance during developmental years.
Untreated oral health conditions can exacerbate systemic issues like malnutrition and inflammation, highlighting the bidirectional relationship between oral and overall health. For elderly individuals with hearing loss, these challenges are compounded by age-related health concerns, increasing their vulnerability to oral health complications.
Dental professionals can play a pivotal role in improving oral health outcomes for hearing-impaired children by adopting inclusive and tailored approaches:
1. Using visual aids
Pictures, videos, and models can effectively explain oral hygiene techniques and dental procedures.
2. Clear communication
Facing the child while speaking, >>

using simple language, and employing sign language or interpreters when needed fosters understanding.
3. Creating a supportive environment
Building trust through a calm demeanour and explaining procedures beforehand can reduce anxiety and improve cooperation.
4. Collaborative care
Coordinating with paediatricians, audiologists, and speech therapists ensures holistic support for the child’s needs.
5. Assistive technologies
Employing written instructions, communication cards, and assistive tools bridges communication gaps.
Summary. Hearing-impaired children deserve equitable and empathetic oral health care. By understanding the unique challenges they face and employing inclusive communication methods, dental professionals can bridge gaps in care, fostering improved oral and overall health outcomes. This
“Dental professionals can play a pivotal role in improving oral health outcomes for hearingimpaired children by adopting inclusive and tailored approaches”
comprehensive approach not only enhances the child’s quality of life but also strengthens trust and confidence in healthcare systems, ensuring a brighter and healthier future.
The DBA requires practitioners to declare any health condition likely to detrimentally affect their practice, emphasising that most health conditions do not qualify as impairments. Hearing-impaired practitioners contribute valuable skills
and perspectives to dentistry but may encounter unique challenges that necessitate workplace accommodations and adherence to legal and professional standards.
Dental practitioners with hearing loss must assess whether their condition impacts their ability to practice safely and effectively. Communication, predominantly through hearing and speech, is essential in healthcare settings. To mitigate potential barriers, practitioners must implement measures to ensure effective communication, such as:
• Procedural measures
Implementing special consent procedures, such as using written materials or third-party assistance (e.g., online Auslan interpreters or dental assistants), to facilitate treatment discussions.
• Written communication Utilising communication cards or template information sheets to aid patient-practitioner dialogue. >>
hearing loss and oral health A patient’s perspective
The following interview highlights the lived experiences of a person with hearing loss, offering insight into the challenges they face and emphasising the importance of awareness and open communication in healthcare settings.
Thank you for taking the time to share your experiences. Can you start by telling us a bit about your hearing loss?
Certainly. I have Otosclerosis, a condition that affects the bones in the middle ear, particularly the stapes bone. The stapes is one of three tiny bones that help transmit sound vibrations to the inner ear. I first became aware of my hearing issues after giving birth to my twins in 2013 while I was still in the hospital. I clearly remember a doctor speaking to me, and I struggled to hear what they were saying. They asked if I had any known hearing problems, which took me by surprise. Although I didn’t believe I had any hearing issues at the time, I decided to undergo a hearing test for clarity. Following the test, I saw my GP, who referred me to an ENT specialist who diagnosed me with Otosclerosis and explained my treatment options: hearing aids or surgery, specifically a stapedectomy.
While surgery could potentially improve my hearing, it comes with risks. Although my hearing loss affects my daily life, it has remained moderate and relatively stable since my diagnosis. For this reason, I’ve
opted not to pursue surgery unless my hearing worsens more rapidly. Currently, I use two hearing aids, although for a long period, I only used one.
My ENT also explained that Otosclerosis is often hereditary, with symptoms typically starting in adulthood and sometimes worsening during pregnancy or due to hormonal changes. After discussing it with my family, I learned that my paternal aunt also has this condition, although hers didn’t develop until she was in her 50s.
How does this affect your day-to-day life?
Otosclerosis affects my daily life, particularly in social interactions. While my hearing aids work well, I still often find myself struggling to hear others, especially in noisy environments or when speaking with someone I don’t know. I also find it more challenging to understand male voices, as their tone tends to be harder to decipher. To help, I sometimes rely on lip-reading. While I’m not particularly skilled at it, it does help improve understanding.
During the COVID-19 pandemic, wearing masks made things even more difficult. The inability to lip-read and the muffled sound only added to the challenge. Most people I interact with are aware of my hearing condition, which makes things easier, but I tend to struggle more in unfamiliar settings where the context isn’t as clear.
How does this affect your experience at appointments, such as dental visits?
While I don’t usually have major concerns at the dentist, I do find it challenging to hear the dental professional during my appointments, much like in other everyday interactions. I completely understand the necessity of wearing masks, and at the start of each appointment, I make sure to inform the dental team about my hearing condition.
This allows the dentists, nurses, and hygienists to be aware of the situation, and they make an effort to speak more
“Overall, my experience with oral health professionals has been positive, but I do feel there’s a need for greater awareness of hearing conditions”
clearly and louder while also making eye contact whenever possible. Even though they’re still wearing masks, their awareness of my condition and their efforts to face me and adjust their volume make a big difference. I appreciate their understanding, and I often let them know they may need to repeat things or speak more slowly to ensure I fully understand. This open
communication helps to create a more comfortable experience.
What do you wish healthcare workers, such as OHPs, took into consideration when caring for you?
Overall, my experience with oral health professionals has been positive, but I do feel there’s a need for greater awareness of hearing conditions. My hearing aids are discreet, so when I have difficulty hearing, I often mention that I am deaf. However, the response I sometimes receive is, “Oh, don’t worry, so are we” or “I’m the same.” At that point, I have to clarify that it’s not just a casual remark—I really do have a hearing condition. Once they understand, it leads to better communication and a more supportive experience.
Do you have anything you would like to add?
Overall, my experiences have been positive, but I truly appreciate the opportunity to discuss my condition and how it impacts my daily life. I’m grateful for the hearing aids that help me navigate day-to-day activities, and I take comfort knowing that surgery is an option should I need it in the future to address this condition. For now, I’m content with managing my hearing loss as I have been, making sure to maintain open communication in my interactions—whether I’m meeting new people, visiting new places, or attending medical appointments.
• Technological solutions
Employing assistive technologies to convert spoken words into written messages and vice versa, enabling seamless communication.
• Disclosure
Informing patients about the measures being taken and assuring them that the quality of care meets expected standards.
• Notification
Reporting the condition to the Dental Board and detailing the compensatory measures in place to ensure compliance and public safety.
Dental practices play a critical role in creating an inclusive and supportive environment for hearing-impaired practitioners. Key responsibilities include:
1. Compliance
• Adhering to the Disability Discrimination Act 1992 and standards set by the Dental Board of Australia.
2. Accommodations
• Providing assistive devices such as captioning tools and amplified equipment.
• Arranging for Auslan interpreters as needed for patient care or staff communication.
• Allocating support staff, such as dental assistants, to facilitate effective workflows.
• Implementing appropriate infection control measures if frequent mask removal is required for lip-reading purposes.
• Offering professional development opportunities to train staff in accommodating hearing-impaired colleagues and patients.
Benefits of supporting hearing-impaired practitioners
By implementing these measures, dental practices can foster a more
“Healthcare professionals must recognise and address the unique needs of hearing-impaired individuals, whether they are patients or practitioners.”
inclusive and supportive work environment, which benefits the entire team. Supporting hearing-impaired practitioners aligns with ethical and legal standards, promotes diversity, and enhances patient care by integrating varied perspectives into the dental profession.
Hearing loss, in its various forms, is a condition with far-reaching implications for individuals, affecting their social interactions, access to care, and quality of life. This narrative review highlights the complex interplay between hearing impairments and oral health, focusing on both patient experiences and the challenges faced by hearing-impaired dental practitioners. Key takeaways from this review include:
The categorisation of hearing loss into conductive, sensorineural, and mixed types allows for tailored prevention and management strategies, which are crucial for improving patient outcomes.
Hearing-impaired individuals may encounter unique oral health challenges, including communication barriers during appointments and limited access to information. Addressing these issues requires patient-centred approaches such as clear communication, visual aids, and assistive technology.
n Hearing-Impaired Practitioners
Practitioners with hearing loss can excel in dentistry with appropriate workplace accommodations and support. Their experiences underscore the importance of inclusivity and adherence to professional standards to ensure patient safety and effective care.
Healthcare professionals must recognise and address the unique needs of hearing-impaired individuals, whether they are patients or practitioners. Promoting awareness, employing innovative communication strategies, and fostering an inclusive environment will contribute to better health outcomes and more equitable care. As oral health professionals, we play a critical role in bridging gaps, building trust, and ensuring that no one is left behind due to hearing impairments.
This comprehensive review underscores the need for continued dialogue and research in this domain to enhance care for individuals with hearing impairments and to foster a more inclusive healthcare system. n
References
• World Health Organisation. (2021). World Report on Hearing. Retrieved from https:// www.who.int
• Australian Bureau of Statistics. (2017). Disability, Ageing, and Carers, Australia: Summary of Findings. Retrieved from https:// www.abs.gov.au
• Cunningham, L. L., & Tucci, D. L. (2017). Hearing loss in adults. The New England Journal of Medicine, 377(25), 2465–2473.
• Dental Board of Australia. (2022). Code of Conduct for Registered Health Practitioners. Retrieved from https://www.dentalboard. gov.au
• Disability Discrimination Act 1992 (Cth). Commonwealth of Australia.
• Wilson, B. S., & Dorman, M. F. (2018). Cochlear implants: Current designs and future possibilities. Journal of Rehabilitation Research and Development, 45(5), 695–730.
• National Acoustic Laboratories. (2020). Hearing loss prevention and management. Retrieved from https://www.nal.gov.au
• Clark, J. G. (1981). Uses and abuses of hearing loss classification. ASHA, 23(7), 493–500.
Join the DHAA for a long weekend in Nusa Dua!
Featuring speakers:
n Dr Carol Tran
New model of oral health service in primary care setting
n Jinous Eighani-Roushani
How to apply best practice and put a stop to white spots
n Associate Professor Roisin McGrath
Working together, working better: Interprofessional collaborative practice
n Cheryl Dey
AI in Orthodontics
n Dr Elizabeth Milford

EVENT DETAILS
Date: 7/06/2025
Time: 8:30 AM - 4:00 PM AWST
Where: Hilton Bali
Jl. Raya Nusa Dua Selatan, Benoa, Kec. Kuta Sel., Bali 80361, Indonesia
BOOK YOUR PLACE
This will be the last event run by the DHAA before handing the baton over to the Oral Health Association of Australia.
Please join us to celebrate our great success.
Our regular update on some great reading to improve your skills and top up your CPD hours
Maximise any downtime by studying at home and keep racking up your CPD points. Subjects in this edition include; the refinement of cancer screening, a push for better funding from Federal Government and two papers relating to molar hypomineralisation.
Whatever your interest, we strive to include something for everyone.
Improving care for people with intellectual disability
• Croakey Health Media 12 February 2025
• CPD hours: 0.5 scientific for reviewing all materials
FIND OUT MORE
New fact sheets are available to accompany the National Safety and Quality Health Service (NSQHS) Standards User Guide for the Health Care of People with Intellectual Disability, released in October 2024.

These resources will assist health service organisations and clinicians support people who live with intellectual disability, by addressing the barriers faced in accessing health care.
The three fact sheets provide information on communication and positive behaviour support, transitions of care, and polypharmacy. They outline strategies to provide better support and improve care for people with intellectual disability.
Putting a wellbeing economy, oral health leadership and workforce priorities on the Federal Budget agenda
• CPD hours: 0.25 non scientific
FIND OUT MORE
Peak Australian health organisations are urging the Federal Government in its upcoming budget to invest in preventive health measures and
strategies to address health inequities and social and cultural determinants of health. Key initiatives, including the Measuring What Matters Framework, National Preventative Health Strategy 2021-2030, National Health and Climate Strategy and the next National Oral Health Plan, should also be properly funded and implemented for sustainable and long-term benefits.
prevalence of burnout
Five decades of debate on burnout
• Med J Aust || doi: 10.5694/mja2.52512
• CPD hours: 0.25 non-scientific
FIND OUT MORE
First described in the mid-1970s, “burnout” has elicited continued interest among occupational health specialists. Fifty years of research on burnout have allowed investigators to refine their views of the syndrome.
Many of the narratives that accompanied the introduction of the burnout construct have been
debunked. Some misconceptions have reached the status of urban legends, continuing to haunt the field despite their lack of validity. Somewhat disconcertingly, the most pressing issue for burnout researchers may be to agree on the basic nature of their entity of interest.
The question of whether burnout reflects a “genuine phenomenon”, irreducible to classical manifestations of distress (ie, anxiety and depressive symptoms) may require special attention as researchers further elucidate the burnout enigma.
Cancer screening: putting people at the centre
• The Lancet Public Health EDITORIAL Volume 10, Issue 2E71
• February 2025
• CPD hours: 0.25 non-scientific
From a public health perspective, although population-based screening
programmes have been key to lowering cancer mortality, risks of over-diagnosis and over-treatment have highlighted the limitations of one-size-fits-all policies and supported, instead, a shift towards more personalised approaches to screening aimed at identifying individuals most likely to benefit from screening.
Putting people at the centre, one should seek the views of those concerned by personalised cancer screening: the general population and health-care professionals. >>

Analysing whether burnout is a genuine phenomenon

Social inequalities in eligibility rates and use of the Australian National Disability Insurance Scheme, 2016–22: an administrative data analysis
• Med J Aust 2025; 222 (3): 135-143. || doi: 10.5694/mja2.52594
• CPD hours: 0.25 non-scientific
This paper assesses differences in eligibility rates and use of the National Disability Insurance Scheme (NDIS).
Women and girls and applicants over 55 years of age or living in socio-economically disadvantaged areas with certain disability types are less likely to be deemed eligible for NDIS support than other applicants. Inequalities in plan allocation and use of personal NDIS budgets are less marked. Changes to NDIS eligibility processes could reduce these inequalities.
The advantages of AI
AI in the health sector: Systematic review of key skills for future health professionals
• Journal of Medical Internet Research (JIMR) Vol 11, Feb 2025
• CPD hours: 0.25 non-scientific
Technological advancements have significantly reshaped health care, introducing digital solutions that enhance diagnostics and patient care.
Artificial intelligence (AI) stands out, offering unprecedented capabilities in data analysis, diagnostic support, and personalised medicine. However, effectively integrating AI into health care necessitates specialised competencies among professionals, an area still in its infancy in terms of comprehensive literature and formalised training programs.
This systematic review aims
to consolidate the essential skills and knowledge health care professionals need to integrate AI into their clinical practice effectively, according to the published literature.
Pathogenesis of molar hypomineralisation: Aged albumin demarcates chalky regions of hypomineralised enamel
• Front. Physiol., Volume 11 - 2020
• CPD 0.25 hours scientific
Molar hypomineralisation (MH) is becoming globally recognised as a significant public health problem linked to childhood tooth decay. However, with causation and pathogenesis unclear after 100 years of investigation, better pathological understanding is needed if MH is to become preventable.
Studies have implicated serum
Molar hypominerallisation is globally recognised as a public health problem

albumin in an extracellular pathomechanism for chalky enamel, opposing long-held dogma about systemic injury to enamel-forming cells. Its findings justify pursuit of an extracellular paradigm for the pathogenesis of MH and offer exciting new prospects for alleviating childhood tooth decay through medical prevention of MH.
chalky teeth (Pt #2)
A breakthrough in understanding the pathogenesis of molar hypomineralisation: The mineralisation-poisoning model
• Front. Physiol., 21 December 2021
Volume 12 - 2021
• CPD 0.25 hours scientific
FIND OUT MORE
Popularly known as “chalky teeth”, molar hypomineralisation (MH) affects over 1-in-5 children worldwide, triggering massive amounts of suffering from toothache
and rapid decay.
Recent biochemical studies provided a pathomechanistic breakthrough by explaining several hallmarks of chalky opacities for the first time. This article outlines these findings in context of previous understanding and provides a working model for future investigations. n

As oral health professionals we need to be prepared to accommodate patients with special needs
By Christine Murthi (Jan 2022)
Patients with special needs are classified as all individuals who present physical, sensory, mental, developmental, medical or cognitive limitations, and who require special consideration when receiving dental treatment. The scope is broad considering the range of cases that may fit under these categories. These conditions necessitate special dental treatment plans, medical management and use of specialised programs or services to prevent or treat oral health problems.
Dental health professionals need to be prepared to accommodate patients with special needs, such as patients with:
• Behavioural Disorders: anxiety, attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD)
• Developmental conditions: cerebral palsy, down syndrome, blindness
• Intellectual disabilities: fetal alcohol spectrum disorders (FASD).
• Physical: cleft lip and palate, hearing
disorders, paraplegia, quadriplegia, vision impairment
• Learning Disabilities
• Sensory Processing Disorder
• Traumatic Brain Injury
• Complex medical histories: cancer, organ failure, cardiac concerns or compromised immune system
Patients with special needs may exhibit poor oral hygiene due to difficulty in performing self-care, effects of medications and/or medical condition(s) which may cause negative oral health side effects. Poor plaque control can lead to a high prevalence of dental caries and periodontal disease.
When planning care for special needs patients the whole dental care journey must be considered and carefully planned from initial presentation to home care, to everything in between such as time of day and length of appointments, physical access into the clinic, need for a carer, scheduled breaks

during treatment and removal of mask when communicating (e.g. if patient lip reads). Moreover, performing a thorough medical/dental history in consultation with physicians, dental team, social workers and caregivers is essential. Things that may require consideration before the appointment are antibiotic cover, use of local anaesthetics and possible sedation, timing of dental treatment during chemotherapy, haemoglobin levels and international normalised ratios, for instance. During treatment modifications can be made to make the patient feel more comfortable, for example, protective and stabilising techniques such as holding head or hand, supportive pillows or pads and a mouth prop. Treatment may also be carried out in a wheelchair if the patient is unable to transfer to a dental chair. A dental environment may trigger stress and/or anxiety therefore using the tell-show-do technique, or soothing and distracting techniques are useful. Post-treatment, the continuation of care and improving long

term oral health outcomes are equally important. To achieve these oral health goals the patient and family need the appropriate resources and support. Oral health care teams should embrace an interdisciplinary and inter-professional approach to care when treating this patient cohort, such as working with allied health services, medical teams, social services and community support services. The support can make a difference to accessing oral health services for the patient.
• Hygienists can help improve the effectiveness of homecare through improved oral hygiene regimens. Modifications can be suggested for toothbrushes and interdental cleaning devices.
• Use of an electric toothbrush is recommended with a wide handle grip. The addition of bicycle grips, tennis balls or soft plastic to toothbrush handles can aid in
manipulation of the brush.
• An extender (ruler, rod or wooden sticks) can be taped to the handle of a toothbrush to provide assistance for patients with a limited range of motion
• Floss holders or water flossers are helpful for patients with limited dexterity for interdental cleaning
• Caregivers should also receive education on the importance of oral health, the oral/systemic link, optimal nutrition with a noncariogenic diet and oral hygiene techniques so they can help patients maintain their oral health. Resources and support should be provided for this purpose
• Setting a shorter recall may be useful to carry out preventive measures in a timely way
• Preventative measures may include: fluoride varnish, high fluoride toothpaste, non-SLS toothpaste, fluoridated mouth rinse
• Appropriate and timely referrals are important. n
References Singh, N. (2019). Providing Care to Patients With Special Needs. The Journal of Professional Excellence. Retrieved from, https://dimensionsofdentalhygiene.com/article/ caring-%E2%80%A8for-patients-with-special-needs/ Mandasari M., Rahmayanti, F., Derbi, H., & Wimardhani, Y. S. (2021). Special care dentistry perception among dentists in Jakarta: An online survey study. PloS one, 16(4). https:// doi.org/10.1371/journal.pone.0249727
American Academy of Pediatric Dentistry. (2021). Management of dental patients with special health care needs. The Reference Manual of Pediatric Dentistry.

About the author
Christine Murthi is an oral health therapist graduated from Auckland University of Technology. Prior to this she obtained qualifications in pharmacology and secondary teaching from the University of Auckland. She has teaching/ tutoring experience spanning more than ten years. Through this teaching experience combined with her diverse cultural background she has developed a passion for promoting diversity in clinical practice, overcoming communication barriers and connecting with the community. As a member of the Colgate Advocates for Oral Health: Editorial Community, her contributions to the dental community aim to promote good oral health for all and keeping a healthy smile for life.
Republished with permission from Colgate Advocate’s for Oral Health
colgateprofessional.com.au/Advocates

ACT contacts:
Director Amy McDermott directoract@dhaa.info
Chair Kate Spain chairact@dhaa.info
n The first 2025 ACT event was a dinner meeting at the Southern Cross Yacht Club on Tuesday 18 February with presentation from Dr Bill Vass, an audiologist. He covered the issues of hearing health for dental professionals as an invisible disability that affects many of us. This is the first of the joint ADOHTA-DHAA state events and the ACT committee extended a warm welcome to our ADOHTA colleagues.
Congratulations to Kathryn Novak who received her ACT Tammie Birch Inspiration Award at the dinner. Kathryn is a former DHAA National President and has served on the ACT Committee for many years.
ACT’s next event is going to be a full day seminar on Saturday 16 August. Planning has already underway so please look out for further information.
“ Congratulations to Kathryn Novak who received her ACT Tammie Birch Inspiration Award at the dinner ”




NSW contacts:
Director Jinous Eighani-Roushani directornsw@dhaa.info
Chair. Belinda Hines chairnsw@dhaa.info
Deputy Chair Angelee Murdock contactnsw@dhaa.info

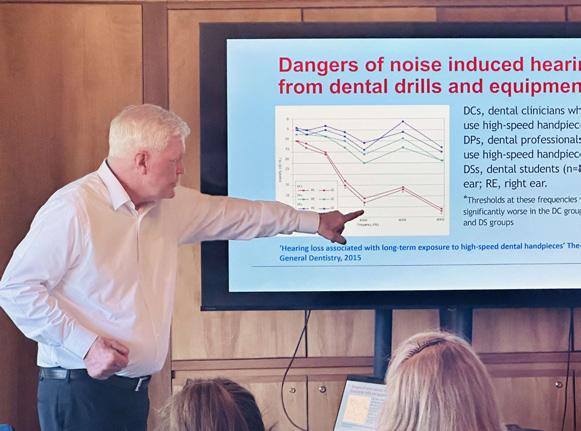

n The 2025 NSW program kicked off with a full day event. “Managing the Complex Patient” was held on Saturday 22 February at the destination Mercure Kooindah Waters on the Central Coast.
The event was well attended by members of both ADOHTA and DHAA and had an impressive list of expert presenters covering the subjects of eating disorders, medically complex patients, oral microbiome, chronic diseases and difficult patients.
We extend a big thank you to Laura Church, ADOHTA NSW chair for presenting a joint ADOHTA and DHAA session to BoH students at the University of Sydney on Monday 24 February, attracting great interests from attendees on the day.
Qld Contacts:
Director Carol Tran. directorqld@dhaa.info
Chair Gabby Williamson chairqld@dhaa.info
Deputy Chair Courtney Dicken contactqld@dhaa.info
n The Queensland event on Saturday 8 March in Toowoomba had to be postponed to May due to the threat from Cyclone Alfred. We are grateful to orthodontist Dr Deven Naidu, periodontist Dr Michael Barber and oral medicine specialist A/ Prof Michael Stubbs who agreed to move their presentations to May. Attendees will be able to work with three local specialists to discuss current practice for recognition, referral and review processes in orthodontic planning,
“ A reminder that the 2025 Oral Health Congress will be held at the Star Gold Coast between 16 and 18 October.
Please mark this in the diary”
periodontics and maxillofacial treatments.
We will announce the new date soon.
A reminder that the 2025 Oral Health Congress will be held at the Star Gold Coast between 16 and 18 October.
Our Queensland Chair Gabby Williamson, Deputy Chair Courtney Dicken and Board Director Carol Tran had been working with colleagues at the organising committee to finalise the program. Please mark these dates in your diary as the organisers are keen to see everyone there.
QLD Director Dr Carol Tran, CEO Bill Suen and Aged Care SIG Chair Gemma Collins presented a webinar to over 50 management and clinical staff from Queensland residential aged care facilities (RACFs). The event was organised by the Commonwealth Department of Health and Aged and the DHAA, with the recording sent to all QLD RACFs. We have received a number of connects from the local facilities seeking advice and connection to local oral health practitioners to assist them in on site oral health services. If you are interested to support local facilities, particularly in rural areas, please email ceo@dhaa.info.
SA Contacts: Director Cheryl Dey cheryl.dey@dhaa.info
Chair Courtney Rutjens chairsa@dhaa.info
Deputy Chair Jesse Kourakis contactsa@dhaa.info
n A big welcome to Cheryl Dey who returned as SA Director when Michelle Kuss completed her term at the end of last year. Cheryl had served on the DHAA Board and was president before retiring from the role. She is also appointed by the DHAA Board to sit on the new OHAA board.
SA’s 2025 destination event is scheduled for Saturday 29 March at the Mount Lofty Retreat. This special weekend combines CPD with wellness experience for both the practitioners and patients. Facilitated by dental hygienists, hypnotherapist and wellness coach Hellen Checker and supported by professional strongman Jordan Steffens, the day will include Qi Gong, breathing exercises, Yoga, complementary medicines and reliance building. This event is well sought after by members so please REGISTER as soon as possible as we are nearing capacity.
South Australia is proud to be playing host to attendees of the Gala Dinner being held to celebrate 50 years of dental hygiene in Australia on Saturday 26 July at the Adelaide Pavilion. Dental hygiene in Australia started 50 years ago in Adelaide. Today, dental hygiene is practised by over 5,000 Oral Health Practitioners (OHPs) in every state and territory. This event is hosted
“ South Australia is proud to be playing host to attendees of the Gala Dinner being held to celebrate 50 years of dental hygiene in Australia ”
by the new Oral Health Association of Australia to reflect on the achievements of our colleagues over the past half century, and to celebrate the new era and opportunities in dental hygiene moving forward for OHPs. REGISTER to be part of this momentous event to honour the past, celebrate the present and embrace the future of dental hygiene for our profession.
SA will also run a full day seminar at the Adelaide Pavilion on the same day
of the Gala Dinner. The SA Committee is currently finalising the program which will be published over coming weeks.
TAS Contacts:
Staff Bill Suen bill.suen@dhaa.info
n TAS hosted the February board meeting at the Old Woolstore at the February 1516 weekend. Board directors took the opportunity to meet with local members and stakeholders from the ADOHTA and ADA.
The next local full day event will be held at the Tailrace Centre in Launceston on Saturday 17 May between 8:30am and 5pm. This will be jointly organised by the ADOHTA and DHAA and we hope to release the program and registration very soon.
VicVic Contacts
Director Roisin McGrath directorvic@dhaa.info
Chair Cathryn Carboon chairvic@dhaa.info
Deputy Chair Sarah Laing contactvic@dhaa.info
n Victoria’s next full day seminar is scheduled for Saturday 16 August at the Courtyard by Marriott at Flagstaff Gardens. This will be the first local event run by the new OHAA in Victoria. The committee is working very hard to finalise the program so please mark your diary and register as soon as registration is open.
On Friday 7 February, Melbourne hosted the DHAA Future Leader’s workshop. 17 participants across Australia attended the full day event at the Marriott Hotel in the city. This DHAA program

is run by A/Prof Nicky Kilpatrick and Dr Trudy Lin to develop leadership skills and co-design a mentoring program for the oral health profession. This six-month program will conclude in May with the plan to have a mentoring program designed for future generation of leaders for our profession.
WA Contacts
Chair: Michelle Wright contactwa@dhaa.info
Staff: Bill Suen bill.suen@dhaa.info
n WA will run two local events with ADOHTA over the next few weeks. On Wednesday 19 March, there will be an after-work evening session where Clinical Psychologist Lan Chen will deliver a presentation on 'Understanding and

Managing Burnout and Other Occupational Stressors' at the ADA House in West Perth between 6:30 and 8:00pm. This presentation aims to provide clarity on burnout and its contributors, as well as to outline other occupational stressors that health care workers commonly face, with the goal of providing insights and tips for ways to mitigate and manage them. REGISTER HERE
On Saturday 5 April, come along to Aloft Perth at Rivervale for a full day’s education to listen to local experts including Oral Medicine Specialist Dr Amanda Phoon Nguyen, Periodontist A/Prof Leticia Algarves Miranda, Radiologist Dr Mary Lam, Periodontal Therapist
Jennine Bywaters and OHT Chelsea Rohekar covering a wide range of interesting topics. REGISTER HERE n “ On 19 March, there will be an evening session where Clinical Psychologist Lan Chen will deliver a presentation on 'Understanding and Managing Burnout and Other Occupational Stressors' ”

www.dhaa.info