Atlas of Interventional Orthopedics Procedures
Essential Guide for Fluoroscopy and Ultrasound-Guided Procedures
Chris J. Williams, MD
Adjunct Professor
Emory Rehabilitation Department Emory University, Atlanta Georgia USA
CEO/Owner
Interventional Orthopedics of Atlanta, Atlanta Georgia USA
Walter I. Sussman, DO
Assistant Clinical Professor Physical Medicine & Rehabilitation Tufts University, Boston Massachusetts USA
John Pitts, MD
Fellowship Director
Interventional Orthopedics
Centeno- Schultz Clinic, Broomfield Colorado USA
© 2023, Elsevier Inc. All rights reserved.
No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies, and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency can be found at our website: www.elsevier.com/permissions
This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein).
Notices
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. To the fullest extent of the law, no responsibility is assumed by Elsevier, authors, editors, or contributors for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
ISBN: 978-0-323-75514-6
Content Strategist: Humayra Khan
Content Development Specialist: Kim Benson/Grace Onderlinde
Project Manager: Andrew Riley
Design: Patrick Ferguson
Illustration Manager: Muthukumaran Thangaraj
Illustrator: Dr Patrick Nguyen
Marketing Manager: Kate Bresnahan
Foreword vii
Preface viii
Editor Biographies x
Contributors xii
Acknowledgments xx
Section I Introduction
1 Introduction to Interventional Orthopedics and Review of the Pathophysiology of Orthopedic Conditions, 1
Walter I. Sussman, John Pitts, and Chris Williams
2 Ultrasound Basics, 14
Matthew Sherrier, Allison N. Schroeder, Kentaro Onishi, and Daniel Lueders
3 Principles of Fluoroscopy Imaging in Spine and Musculoskeletal Interventional Orthopedics, 31
Katarzyna Iwan, Rahul Naren Desai, and John J. Wolfson
Section II Injectates
4 Principles of Injection Therapy, 41
Lee Kneer, Robert Bowers, and Cleo D. Stafford II
5 Autologous Tissue Harvesting Techniques: Bone Marrow Aspirate and Adipose Tissue, 50
Gerard Malanga, Jay E. Bowen, and Selorm L. Takyi
6 Autologous Tissue Harvesting Techniques: Platelet-Rich Plasma, 62
Peter A. Everts
7 Autologous Orthobiologics, 70
Prathap Jayaram, Peter Chia Yeh, Max Epstein, and Shiv J. Patel
8 Allograft Tissues, 89
Alberto J. Panero, Alan M. Hirahara, Luga Podesta, Amir A. Jamali, Wyatt Andersen, and Alyssa A. Smith
9 Therapeutic Dextrose Injection: Prolotherapy, Perineural Injection Therapy, and Hydrodissection, 102
Kenneth D. Reeves, Stanley K.H. Lam and David Rabago
10 Sclerosing Agents, 118
Colton L. Wood, David J. Berkoff, and Justin R. Lockrem
11 Toxins for Orthopedics, 124
Zach Bohart, Walter I. Sussman, Jacob Sellon, and Natalie Sajkowicz
Section III Atlas
12 Cervical Injection Techniques, 134
Marko Bodor, Stephen Derrington, John Pitts, Jason Markle, Sairam Atluri, Navneet Boddu, and Vivek Manocha
13 Thoracic Injection Techniques, 166
Marko Bodor, Stephen Derrington, John Pitts, Jason Markle, and Orlando Landrum
14 Lumbar Injection Techniques, 186
Di Cui, Lisa Foster, Brian Hart Keogh Jr., Jason Markle, Hassan Monfared, Jaymin Patel, Shounuck I. Patel, John Pitts, and Diya Sandhu
15 Sacrococcygeal Injection Techniques, 224
Joanne Borg-Stein, Catherine Mills, Carolyn Black, Oluseun Olufade, and Giorgio A. Negron
16 Shoulder Injection Techniques, 242
Jason Markle and Cleo D. Stafford II
17 Elbow Injection Techniques, 272
Chris Williams, Walter I. Sussman, and John Pitts
18 Wrist Injection Techniques, 290
Kevin Conley, Yoditi Tefera, Michael Erickson, Adam M. Pourcho, Phillip Henning, and Oluseun Olufade
19 Hand Injection Techniques, 313
Yodit Tefera, Kevin Conley, Michael Erickson, Adam M. Pourcho, Phillip Henning, and Oluseun Olufade
20 Hip Injection Techniques, 323
Ken Mautner, John Pitts, Oluseun Olufade, Heather Lynn
Saffel, and Adam Street
21 Knee Injection Techniques, 366
Josh Hackel, Todd Hayano, John Pitts, and Mairin A. Jerome
22 Ankle Region Injection Techniques, 428
Allison C. Bean, Allison N. Schroeder, Matthew Sherrier, Arthur Jason de Luigi, and Kentaro Onishi
23 Foot Injection Techniques, 465
Douglas Hoffman, Jacob Jones, Pierre D’hemecourt, John Pitts, and Arthur Jason De Luigi
Section IV Advanced
24 Calcific Tendonitis Barbotage/Lavage, 489
Jason Ian Blaichman and Kenneth S. Lee
25 High-Volume Ultrasound-Guided Capsular Distention for Adhesive Capsulitis, 496
Alyssa Neph Speciale and Brian Davis
26 Ultrasound-Guided Needle Tenotomy and Ultrasound-Guided Tenotomy and Debridement With Tenex Health TX System, 502
Ryan C. Kruse and Mederic M. Hall
27 High-Volume Image-Guided Injections, 506
Maria-Cristina Zielinski, Nicola Maffulli, Otto Chan, and Romain Haym
28 Ultrasound-Guided Release of Trigger Finger and de Quervain Tenosynovitis, 514
Ricardo E. Colberg and Javier A. Jurado
29 Compartment Pressure Testing, 524
Jonathan T. Finnoff and Jacob Reisner
30 Ultrasound-Guided Anterior and Lateral Compartment Fasciotomies for Chronic Exertional Compartment Syndrome, 527
Jonathan T. Finnoff and Jacob Reisner
31 Principles of Perineural Injections, 531
Jeffrey A. Strakowski
32 Ultrasound-Guided Release of the Transverse Carpal Ligament (Carpal Tunnel), 535
Adam M. Pourcho, Phillip Henning, and Jay Smith
33 Ultrasound-Guided Percutaneous Bone Spur Excision and Cheilectomy, 544
Brian J. Shiple
34 Intraosseous Injections, 553
Steven Sampson, Hunter Vincent, and Sonali Lal
35 Advanced and Emerging Interventional Techniques, 573
Nidal Elbaridi, Virlyn Bishop, Orlando Landrum, Marko Bodor, and John Pitts
36 Needle Arthroscopy of the Knee, Shoulder, and Hip, 594
Don Buford, Brice W. Blatz, and Nicola Hyde
Section V Postprocedure Considerations
37 Rehabilitation Principles for Interventional Orthopedics and Orthobiologics, 599
Walter I. Sussman, Ken Mautner, and Abby Perone
38 Advanced Imaging in Interventional Orthopedics, 612
Rahul Naren Desai and Katarzyna Iwan
Editor Biographies
Chris J. Williams, MD
Christopher J. Williams, MD, was born and raised in Jacksonville, Florida. After high school, Dr. Williams entered the US Air Force and worked as a public health technician in England, Kuwait, and Mississippi. After serving 4 years in the Air Force, he decided to get his undergraduate degree from the University of North Florida, where he graduated summa cum laude. He then opted to attend medical school at Emory University where he also completed his residency training in physical medicine and rehabilitation. During residency, he was awarded the Resident of Year award for all 3 years of his residency training and was Chief Resident his last year of training. During residency, Dr. Williams spearheaded the development of a musculoskeletal (MSK) ultrasound training curriculum and started a prosthetics and orthotics annual symposium in collaboration with Georgia Tech.
Dr. Williams is board certified in physical medicine and rehabilitation and completed fellowship training in interventional orthopedics and regenerative medicine for 1 year at the Centeno-Schultz Clinic in Broomfield, CO. After completing his training, he was an attending physician at the Centeno-Schultz Clinic prior to opening his practice in Atlanta, GA: Interventional Orthopedics of Atlanta. In collaboration with Ken Mautner at Emory, they started a joint non-accredited fellowship program in interventional orthopedics and graduated their first fellow in July 2020.
Education is one of his passions, as he was raised by a very hardworking single parent who was also a teacher and instilled in him the principles of humility, hard work, and dedication. Currently, Dr. Williams is an adjunct faculty member at Emory University in the Department of Rehabilitation Medicine, providing didactics annually and also allowing the residents to get hands-on training while rotating with him during their elective time. He is an instructor and the educational committee co-chair for the Interventional Orthobiologics Foundation, teaching several courses annually. He also has lectured at the annual conference for The Orthobiologics Institute (TOBI).
Dr. Williams has published over 10 peer-reviewed research articles and book chapters on the topics of orthobiologics and rehabilitation medicine. He achieved best-selling author status on Amazon for his book Exercise 2.0 and was recognized by Emory University Alumni Association 40 Under 40 in 2019.
In his private practice at the Interventional Orthopedics of Atlanta, Dr. Williams specializes in the diagnosis
and treatment of musculoskeletal conditions in athletes, weekend warriors, adolescents, the underserved, and the elderly. He strives to provide exceptional care to everyone he encounters.
Dr. Williams resides in Atlanta, Georgia with his wife Layla, who is an ObGyn physician; two children, Kemet and Egypt; and enjoys cooking, fitness activities, art, music, and traveling.
Walter I. Sussman, DO
Dr. Walter I. Sussman is board certified in physical medicine and rehabilitation with fellowship training in sports medicine. He completed his undergraduate studies at Colgate University and medical school at the University of New England College of Osteopathic Medicine in Biddeford, Maine. During medical school, he completed a 1-year fellowship in anatomy and osteopathic manipulative medicine. He completed his residency in physical medicine and rehabilitation at Emory University, where he served as chief resident. He then pursued a fellowship in sports medicine at Emory University, where he provided coverage for the Atlanta Dream WNBA team, Georgia Tech athletics, and Emory University athletics.
Dr. Sussman currently works in private practice outside of Boston and serves as the Head Team Physician for the University of Massachusetts Dartmouth and provides care for many of the local high schools. He is a clinical Assistant Professor at Tufts University and is engaged in resident education. Dr. Sussman has published multiple book chapters and peer-reviewed articles on regenerative medicine, chronic tendon injuries, diagnostic musculoskeletal ultrasound, and concussion management.
Dr. Sussman takes pride in promoting the patient experience and individualizing the treatment to fit each patient. Dr. Sussman has a clinical interest in the use of ultrasound to diagnose musculoskeletal injuries, in post-concussion syndrome, in orthobiologics, and in minimally invasive procedures. Dr. Sussman manages chronic musculoskeletal conditions, acute sports injuries, and sports-related concussions.
John Pitts, MD
John Pitts, MD, was born and raised on the south side of Chicago, IL. He received a BA in Mathematics/Economics at Emory University in Atlanta, Georgia. Dr. Pitts received his medical education at Vanderbilt School of Medicine
in Nashville and then completed a physical medicine and rehabilitation residency back at Emory University. After residency he completed a 1-year fellowship (non-accredited) in regenerative medicine and interventional orthopedics at the Centeno - Schultz Clinic, where he works currently and is part of the Regenexx network of physicians. He serves as the fellowship director and helps to train new Regenexx physicians. He also regularly teaches procedural courses for the Interventional Orthopedics foundations and has given presentations at major conference for the American Academy of Physical Medicine and Rehabilitation (AAPMR), The Orthobiologics Institute (TOBI), and the American Association of Orthopedic Medicine (AAOM).
Dr. Pitts has been practicing regenerative Medicine and interventional orthopedics exclusively since 2013. He diagnoses and treats patients with a variety of orthopedic and musculoskeletal problems, including spine (cervical, thoracic, lumbar, sacroiliac joints), temporomandibular joint, upper extremity (shoulder, elbow, wrist, hand, fingers), lower extremity (hip, knee, ankle, foot, toes), and problems relating to peripheral
nerves, joints, ligaments, tendons, bones, and muscle. He regularly uses orthobiologics such as prolotherapy, neuroprolotherapy, platelet-rich plasma (PRP), platelet lysate, bone marrow concentrate, micronized adipose tissue graft, and amniotic membrane. Additionally, he works in Grand Cayman Island several times per year, where he is able to treat patients with cultured expanded bone marrow mesenchymal stem cells (MSCs). He utilizes other devices to be used in interventional orthopedics and helps to pioneer and advance many of the procedures.
Dr. Pitts has co-authored several peer-reviewed articles relating to regenerative treatments. He also authored a book named Nutrition 2.0, Guide to Eating and Living to Achieve a Higher Quality of Life Now and into Your Golden Years, and gives this to all his patients.
Dr. Pitts resides in Denver, CO, with his wife, Ria, and two young children, Malcolm and Camila. He enjoys working out, playing sports, snowboarding, scuba diving, being outdoors, traveling, watching movies, and spending time with his family.
Contributors
Associate Editors
Marko Bodor, MD Founder
Interventional Spine and Sports Medicine Bodor Clinic Napa, California USA
Assistant Professor
Physical Medicine and Rehabilitation University of California Davis Sacramento, California USA
Assistant Professor Neurological Surgery University of California San Francisco San Francisco, California USA
Don Buford, MD, RMSK Orthopedic Surgeon Sports Medicine
Texas Orthobiologic Institute Dallas, Texas USA
Rahul Naren Desai, MD CEO
Musculoskeletal Radiology Restore
PDX Spine & Sports Medicine Beaverton, Oregon USA
President
Interventional Orthopedic Foundation Broomfield, Colorado USA
Gerard Malanga, MD Partner
New Jersey Sports Medicine, LLC Cedar Knolls, New Jersey USA
Clinical Professor PM&R
Rutgers Medical School Newark, New Jersey USA
Jason Markle, DO Interventional Orthopedic Physician Orthopedics
The Centeno-Schultz Clinic Broomfield, Colorado USA
Ken Mautner, MD Assistant Professor
Physical Medicine & Rehabilitation Emory University, Atlanta USA
Contributors
Wyatt Andersen, BS, ATC Research Assistant Physical Medicine & Rehabilitation Sacramento, California USA
Sairam Atluri, MD Medical Director ReGen StemCures Cincinnati, Ohio USA
Allison C. Bean, MD, PhD Department of Physical Medicine and Rehabilitation University of Pittsburgh Medical Center Pittsburgh, Pennsylvania USA
David J. Berkoff, MD Professor Orthopedics and Emergency Medicine UNC Chapel Hill Chapel Hill, North Carolina USA
Virlyn Bishop Anesthesiology and Pain Medicine Center for Spine Interventions Acworth, GA USA
Carolyn Black, MD, PhD
Resident Physician
Physical Medicine and Rehabilitation
Harvard Medical School/Spaulding Rehabilitation Hospital
Boston, Massachusetts USA
Jason Ian Blaichman, MDCM, FRCPC
Adjunct Lecturer
Department of Medical Imaging
University of Toronto Toronto, Ontario
Canada
Staff Radiologist
Department of Diagnostic Imaging
Scarborough Health Network Scarborough, Ontario Canada
Brice W. Blatz, MD, MS
Physician/Owner
Sports and Regenerative Medicine
Pacific Regenerative and Interventional Sports Medicine
San Jose, California USA
Navneet Boddu, MD
Anesthesiologist
Anesthesiology
Anesthesia Service Medical Group
San Diego, California USA
Marko Bodor, MD Founder
Interventional Spine and Sports Medicine Bodor Clinic
Napa, California USA
Assistant Professor
Physical Medicine and Rehabilitation
University of California Davis Sacramento, California USA
Assistant Professor
Neurological Surgery
University of California San Francisco San Francisco, California USA
Zach Bohart, MD, MS
Associate Professor
Tufts University School of Medicine
Boston, Massachusetts USA
Joanne Borg-Stein, MD
Associate Professor
Physical Medicine and Rehabilitation
Harvard Medical School
Boston, Massachusetts USA
Jay E. Bowen, DO
Medical Director
New Jersey Regenerative Institute, LLC
Cedar Knolls, New Jersey
USA Clinical Assistant Professor PM&R, Rutgers Medical School, New Jersey USA
Robert Bowers, DO, PhD
Assistant Professor
Department of Orthopaedics
Emory University School of Medicine
Atlanta, Georgia USA
Assistant Professor
Department of Rehabilitation Medicine
Emory University School of Medicine
Atlanta, Georgia USA
Don Buford, MD, RMSK
Orthopedic Surgeon
Sports Medicine
Texas Orthobiologic Institute Dallas, Texas USA
Christopher J. Centeno, MD
Research and Development
Regenexx, LLC
Broomfield, Colorado USA
Centeno-Schultz Clinic Broomfield, Colorado USA
Otto Chan, MBBS, FRCS, FRCR Doctor
Radiology Department
Whittington Hospital London United Kingdom
Ricardo E. Colberg, MD, RMSK
Sports Medicine Physician
Andrews Sports Medicine & Orthopaedic Center Birmingham, Alabama USA
Kevin Conley, MD
Fellow
Swedish Sports & Spine
Providence-Swedish Health Alliance Seattle, Washington USA
Di Cui, MD
Assistant Professor
Department of Rehabilitation Emory University Atlanta, Georgia USA
Brian Davis, MD, FACSM
Volunteer Clinical Professor
Department of Physical Medicine & Rehabilitation
UC Davis Health System, Sacramento California USA
Arthur Jason De Luigi, DO Chair
Physical Medicine & Rehabilitation
Mayo Clinic Arizona Scottsdale, Arizona USA
Professor of Rehabilitation Medicine
Rehabilitation Medicine
Georgetown University School of Medicine Washington, District of Columbia USA
Associate Professor of Physical Medicine & Rehabilitation
Physical Medicine & Rehabilitation Mayo Clinic Alix School of Medicine Scottsdale, Arizona USA
Stephen Derrington, DO
President and Medical Director
Interventional Orthobiologics
Derrington Orthopedics – Interventional Sports and Spine Oceanside and Laguna Hills, California USA
Rahul Naren Desai, MD
CEO
Musculoskeletal Radiology
RestorePDX Spine & Sports Medicine Beaverton, Oregon USA
President Interventional Orthopedic Foundation Broomfield, Colorado USA
Pierre D’Hemecourt, MD Physician
Sports Medicine
Boston Children’s Hospital Boston, Massachusetts USA
Nidal Elbaridi, MD, PT
Medical Director
Interventional Pain Loop Medical Center Chicago, Illinois USA
Max H. Epstein, MD
Resident
Physical Medicine & Rehabilitation
Baylor College of Medicine Houston, Texas USA
Michael Erickson, MD
Swedish Sports Medicine Fellowship Director
Swedish Family Medicine Residency Swedish Medical Center Seattle, Washington USA
Clinical Instructor
Family Medicine University of Washington Seattle, Washington USA
Peter A. Everts, PhD, FRSM
Chief Scientific Officer EmCyte Program Director Gulf Coast Biologics Fort Myers. Florida USA
Jonathan T. Finnoff, DO, FAMSSM, FACSM
Chief Medical Officer
United States Olympic and Paralympic Committee, Colorado Springs Colorado USA
Professor
Department of Physical Medicine and Rehabilitation
Mayo Clinic College of Science and Medicine, Rochester Minnesota USA
Lisa Foster, MD
Assistant Professor Orthopedics
Emory University
Atlanta, Georgia USA
Josh Hackel, MD, RMSK, CAQSM
Fellowship Director USA/Andrews Research and Education Foundation
Primary Care Sports Medicine
Andrews Institute
Gulf Breeze, Florida USA
Mederic M. Hall, MD
Associate Professor
Orthopaedics and Rehabilitation University of Iowa Iowa City, Iowa USA
Todd Hayano, DO
Sports Medicine Fellow
Orthopedics & Sports Medicine
Andrews Research & Education Foundation
Pensacola, Florida USA
Romain Haym, MSc (MSK Ultrasound), MSc (Adv. Physiotherapy), MHCPC, MCSP, MMACPC
Tendon Clinic—Senior Physiotherapist Physiotherapy
BMI The London Independent Hospital, London
United Kingdom
MSK Sonographer Imaging
NHS Whittington Trust, London United Kingdom
Phillip Henning, DO
Medical Director of Sports Medicine
Rehabilitation and Performance Medicine
Swedish Medical Center, Seattle, Washington USA
Alan M. Hirahara, MD, FRCSC
Owner
Private Practice Sacramento, California USA
Douglas Hoffman, MD
Director of Musculoskeletal Ultrasound
Orthopedics and Radiology
Essentia Health
Duluth, Minnesota USA
Nicola Hyde
Sports Medicine and Family Medicine Physician
Seattle, Washington USE
Katarzyna Iwan, MD Doctor
Pain Medicine
RestorePDX
Beaverton, Oregon USA
Amir A. Jamali, MD
Medical Director
Orthopaedic Surgery
Joint Preservation Institute Walnut Creek, California USA
Prathap Jayaram, MD Director of Regenerative Sports Medicine
H. Ben Taub Physical Medicine & Rehabilitation
Department of Orthopedic Surgery
Baylor College of Medicine
Houston, Texas USA
Mairin A. Jerome, MD Fellow
Interventional Orthopedics Centeno-Schultz Clinic Broomfield, Colorado USA
Jacob Jones, MD Physician
Orthopedics and Sports Medicine
Boston Children’s Hospital Boston, Massachusetts USA
Javier A. Jurado
Medical Student
The University of Alabama at Birmingham School of Medicine Birmingham, Alabama USA
Brian Hart Keogh Jr., MD
East Carolina Pain Consultants
Interventional Pain Management
Vidant Medical Center
Greenville, North Carolina USA
Affiliate Clinical Faculty Department of Physical Medicine and Rehabilitation
East Carolina University School of Medicine
Greenville, North Carolina USA
Lee Kneer, MD FAAPMR
Assistant Professor
Department of Orthopaedics
Emory University School of Medicine, Atlanta
Georgia USA
Assistant Professor
Department of Rehabilitation Medicine
Emory University School of Medicine, Atlanta
Georgia USA
Ryan C. Kruse, MD, CAQSM, RMSK
Assistant Professor
Orthopedics and Rehabilitation University of Iowa Iowa City, Iowa USA
Sonali Lal, MD
Assistant Professor, Columbia University
Attending Physician, New York
Presybyterian Hospital
Stanley K. H. Lam, MBBS, MScSEM, FHKIMM, RMSK, CIPS, FIPP, POCUS
President
Clinical Research
The Hong Kong Institute of Musculoskeletal Medicine
Kowloon Bay
Hong Kong
Clinical Associate Professor
Family Medicine
The Chinese University of Hong Kong
New Territory
Hong Kong
Clinical Assistant Professor
Family Medicine
The University of Hong Kong
Hong Kong
Orlando Landrum, MD, MBA
Physician CEO
Pain & Regenerative Medicine
Cutting Edge Integrative Pain Centers
Elkhart, Indiana
USA
Kenneth S. Lee, MD/MBA Professor of Radiology
Section Chief of Musculoskeletal Imaging & Intervention Fellowship Director
Musculoskeletal Imaging & Intervention
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin
USA
Justin R. Lockrem, MD
Sports Medicine Fellow
Sports Medicine
University of North Carolina Chapel Hill, North Carolina USA
Daniel Lueders, MD
Assistant Professor
Physical Medicine and Rehabilitation
University of Pittsburgh Medical Center Pittsburgh, Pennsylvania USA
Nicola Maffulli, MD, MS, PhD, FRCP, FRCS(Orth)
Full Professor
Medicine, Surgery and Dentistry
University of Salerno
Salerno Italy
Gerard Malanga, MD Partner
New Jersey Sports Medicine, LLC Cedar Knolls, New Jersey USA
Clinical Professor PM&R
Rutgers Medical School Newark, New Jersey USA
Vivek Manocha, MD
Medical Director
Pain Management
Midwest Spine Interventionalist Springboro, Ohio USA
Clinical Assistant Professor Surgery
Wright State University Boonshoft School of Medicine
Dayton, Ohio USA
Jason Markle, DO
Interventional Orthopedic Physician Orthopedics
The Centeno-Schultz Clinic Broomfield, Colorado USA
Ken Mautner, MD
Assistant Professor
Physical Medicine & Rehabilitation
Emory University, Atlanta USA
Catherine Mills, MD
Resident Physician
Physical Medicine & Rehabilitation
Harvard Medical School/Spaulding Rehabilitation Hospital Boston, Massachusetts USA
Hassan Monfared, MD
Assistant Professor
Physical Medicine and Rehabilitation Emory University Atlanta, Georgia USA
Residency Program Director
Physical Medicine and Rehabilitation Emory University Atlanta, Georgia USA
Giorgio A. Negron, MD
Resident Physician
Department of Rehabilitation Medicine Emory University Atlanta, Georgia USA
Oluseun Olufade, MD
Assistant Professor Department of Orthopedics
Emory School of Medicine Atlanta, Georgia USA
Assistant Professor
Department of Physical Medicine & Rehabilitation Emory School of Medicine Atlanta, Georgia USA
Kentaro Onishi
Assistant Professor Physical Medicine and Rehabilitation University of Pittsburgh Medical Center, Pittsburgh Pennsylvania USA
Alberto J. Panero, DO http://sacsportsmed.com
Sports Medicine
SAC Regenerative Orthopedics Sacramento, California USA
Jaymin Patel, MD
Assistant Professor Orthopaedics
Emory University Atlanta, Georgia USA
Shiv J. Patel, MD Resident
Orthopaedic Surgery
University of Texas Medical Branch, Galveston Texas USA
Shounuck I. Patel, DO
Functional & Interventional Orthopedics
Spine & Sports Physiatry
Regenexx Los Angeles Los Angeles, California USA
Clinical Assistant Professor
College of Osteopathic Medicine of the Pacific Western University Pomona, California USA
Clinical Assistant Professor
College of Osteopathic Medicine Touro University Harlem, New York USA
Abby Perone, DC
Love Health, Owner Movement Therapy & Functional Medicine
St. Petersburg, Florida USA
John Pitts, MD
Fellowship Director Interventional Orthopedics Centeno-Schultz Clinic Broomfield, Colorado USA
Luga Podesta, MD Director
Regenerative Sports Medicine Bluetail Medical Group-Naples Naples, Florida USA
Team Physician Florida Everglades Estero, Florida USA
Adam M. Pourcho, DO
Instructor of Sports Medicine
Physical Medicine and Rehabilitation
Swedish Medical Group Seattle, Washington USA
David Rabago, MD
Associate Professor Department of Family Medicine
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin USA
Kenneth D. Reeves, BS, MD
Private Practice
Physical Medicine and Rehabilitation and Pain Management
Roeland Park, Kansas USA
Formerly Clinical Assistant/Associate Professor 1986–2015
Physical Medicine and Rehabilitation
University of Kansas Medical Center
Kansas City, Kansas USA
Jacob Reisner, DO
Primary Care Sports Medicine Fellow
Physical Medicine and Rehabilitation
Mayo Clinic
Minneapolis, Minnesota USA
Heather Lynn Saffel, MD, MS
Primary Care Sports Medicine Fellow Department of Orthopedics
Emory Sports Medicine Center
Atlanta, Georgia USA
Natalie Sajkowicz, MD Physician
Physical Medicine and Rehabilitation
Tufts Medical Center Boston, Massachusetts USA
Steven Sampson, DO
Founder
PM&R
The Orthohealing Center
Los Angeles, California USA
Founder
The Orthobiologic Institute Los Angeles, California USA
Clinical Instructor
Medicine
David Geffen School of Medicine UCLA Los Angeles, California USA
Diya Sandhu, MD
Assistant Professor Orthopaedics
Emory University
Atlanta, Georgia USA
Assistant Professor
Physical Medicine and Rehabilitation
Emory University
Atlanta, Georgia USA
Allison N. Schroeder, MD
Resident Physician
Physical Medicine and Rehabilitation University of Pittsburgh Medical Center Pittsburgh, Pennsylvania USA
Jacob Sellon, MD
Associate Professor
Physical Medicine and Rehabilitation/Sports Medicine Center
Mayo Clinic
Rochester, Minnesota USA
Matthew Sherrier, MD
Resident Physician
Physical Medicine and Rehabilitation University of Pittsburgh Medical Center Pittsburgh, Pennsylvania USA
Brian J. Shiple, DO, CAQSM, RMSK
President AAOM
Board Certified Sports Medicine
The Center for Sports Medicine Philadelphia, Pennsylvania USA
Alyssa A. Smith, BSc Medical Assistant
Joint Preservation Institute, Sacramento, California USA
Jay Smith, MD
Professor
Physical Medicine & Rehabilitation
Mayo Clinic
Rochester, Minnesota USA
Alyssa Neph Speciale, MD
Assistant Clinical Professor, PM&R Sports Medicine
UC Davis Health System
Sacramento, California USA
Cleo D. Stafford II, MD, MS, CAQSM, RMSK, FAAPMR
Assistant Professor
Department of Orthopaedics
Emory University School of Medicine, Atlanta Georgia USA
Assistant Professor
Department of Rehabilitation Medicine
Emory University School of Medicine, Atlanta Georgia USA
Jeffrey A. Strakowski, MD
Clinical Professor
Physical Medicine and Rehabilitation
The Ohio State University Columbus, Ohio USA
Associate Director of Medical Education
Physical Medicine and Rehabilitation
Riverside Methodist Hospital Columbus, Ohio USA
Director of Musculoskeletal Research
The McConnell Spine, Sport and Joint Center Columbus, Ohio USA
Adam Street, BS, DO Fellow
Emory Sports Medicine Center
Emory University Atlanta, Georgia USA
Walter I. Sussman, DO
Assistant Clinical Professor
Physical Medicine & Rehabilitation
Tufts University Boston, Massachusetts USA
Selorm L. Takyi, MD
Regenerative Orthopedics and Musculoskeletal Medicine Physician
Physical Medicine & Rehabilitation
Revive Spine and Pain Center, Marlton
New Jersey USA
Yodit Tefera, MD
Physician
Swedish Spine, Sports, & Musculoskeletal Medicine
Swedish Medical Center
Seattle, Washington USA
Hunter Vincent, DO
Pain Fellow
Physical Medicine and Rehabilitation
University of California: Los Angeles
Los Angeles, California USA
Chris J. Williams, MD
Adjunct Professor
Emory Rehabilitation Department
Emory University
Atlanta, Georgia USA
CEO/Owner
Interventional Orthopedics of Atlanta Atlanta, Georgia USA
John J. Wolfson, RT (R), ASRT, (ARRT)
Imaging and Interventional Coordinator OR
Injury Solutions
Greenwood Village, Colorado USA
Instructor
Pain Imaging Education Englewood, Colorado USA
Colton L. Wood, MD
Primary Care Sports Medicine Fellow
Family Medicine
University of North Carolina at Chapel Hill
Chapel Hill, North Carolina USA
Peter Chia Yeh, MD
Chief Resident
Physical Medicine and Rehabilitation
Baylor College of Medicine
Houston, Texas USA
Maria-Cristina Zielinski, MD, PGDip, PGCert, AECC
Centre for Sports and Exercise Medicine
Barts and The London School of Medicine
Queen Mary University of London London, UK
1 Introduction to Interventional Orthopedics and Review of the Pathophysiology of Orthopedic Conditions
WALTER I. SUSSMAN, JOHN PITTS, AND CHRIS WILLIAMS
Interventional orthopedics is a developing field that attempts to bridge the gap between traditional non-operative orthopedics (e.g., sports medicine, interventional spine or pain medicine) and surgical interventions. This field expands the traditional approach to orthopedic problems, broadening the number of diagnoses and pathology that can be targeted with minimally invasive injections and procedures. For instance, instead of only evaluating orthopedic pathology as severe enough versus not severe enough for surgery, we offer alternative interventions for patients that have not responded to conservative therapy such as patients with partial tendon or ligament tears, ligament laxity, and nerve entrapment syndromes where surgical options are limited. The use of diagnostic ultrasound to complement the traditional orthopedic history and examination allows the clinician to more accurately diagnose and then target the underlying soft tissue and joint pathology.
Instead of traditional interventions being limited to unguided injections and surgery, interventional orthopedics utilizes interventional musculoskeletal ultrasound and fluoroscopy to guide injections to expand treatment options with the goal of precisely targeting and treating common orthopedic problems. The use of image guidance for procedures has increased over the past decades, largely driven by decreased equipment costs, patient safety initiatives, and higher-resolution imaging.1–3 In many cases, “blind” injections have been supplanted by image guidance, which gives the clinician the ability to directly visualize the target tissues and more accurately target specific pathology.
Therapeutic injections may include corticosteroids, but there is a focus on understanding the appropriate role of alternative injectates, which can be utilized to more accurately address the underlying pathophysiology. With the advent and expansion of regenerative treatments and orthobiologics, there is an increasing emphasis on tissue preservation, restoration of tissue function, and healing rather than solely procedures that target “inflammation” and only provide temporary pain relief, or more invasive surgical procedures carrying increased cost and risk of complications.
The traditional approach to the management of musculoskeletal pathology has largely been driven by locating and treating the primary pain generator. A good example is the treatment of low back pain. Typically, the interventionalist would try and identify a primary pain (i.e., the nerve root, facet joint, sacroiliac joint dysfunction, myofascial pain, or intradiscal pathology) and construct a treatment plan to specifically address the area of the spine most likely responsible for the patient symptoms. Conversely, an interventional orthopedics approach would take an approach of addressing the entire spine as a “functional spinal unit” and consider the interplay of these structures and the biomechanical role of adjacent ligaments, tendons, and muscles. The overall goal extends beyond general pain management and looks to address the underlying etiology of musculoskeletal pathology for long-term improvements in functional outcomes. With this in mind, the treatment plan for low back pain may include treating the lumbar facets, corresponding level epidurals if there is myoneural dysfunction on examination
(e.g., weakness or gluteal enthesopathy at the posterior iliac crest), supraspinous and interspinous ligaments for stability, and possibly the multifidus muscle if there is decreased activation on examination and atrophy on magnetic resonance imaging (MRI).
The convergence of advances in imaging, an evolving understanding of the pathophysiology of both acute and chronic degenerative pathology, and a growing interest in minimally invasive approaches to orthopedic pathology has fueled this field and has expanded the type of injections and procedures performed.1 Some of the procedures discussed in this text did not exist before the widespread adoption of ultrasound. Many of these new procedures have become more common, including nerve hydrodissection, barbotage of calcific tendinosis, and percutaneous needle tenotomy procedures. Others are characterized by using specialized surgical tools or devices to duplicate surgical procedures using a percutaneous approach that will expand and continue to be adopted due to improved safety and morbidity.
The growth of regenerative injections, including but not limited to dextrose, platelet-rich plasma, and autologous stem cells, has also driven the emergence of new techniques and procedures. In some cases, the use of these treatments clinically has outpaced the scientific data. The scientific literature will undoubtedly evolve, and the field of interventional orthopedics will continue to mature and as we explore alternatives to many of the more traditional injectates and many surgical techniques that have limited evidence and efficacy.4,5 Several studies have been published that question whether nonsurgical conservative measures, sham surgeries, or placebo therapy is as effective as management. In some cases, it is unclear if the traditional injections with corticosteroids or surgical interventions are better than non-operative management, placebo, or sham surgery, including the intermediate and long-term benefit of corticosteroids,6–9 arthroscopic meniscectomy, and debridement in patients with arthritis,9–17 or subacromial decompression surgery for rotator cuff impingement.18–21
This introductory chapter focuses on the composition and organization of different tissue types and the current concepts in the pathophysiology of orthopedic conditions and how our understanding of common musculoskeletal conditions has influenced current and future management strategies. Conventional nonoperative therapies have targeted inflammation, but inflammation is important to the healing process. Treatment strategies must be tailored to the underlying tissue involved (nerve, muscle, tendon, ligament, bone, and cartilage) and the underlying pathology.
Tendinopathy
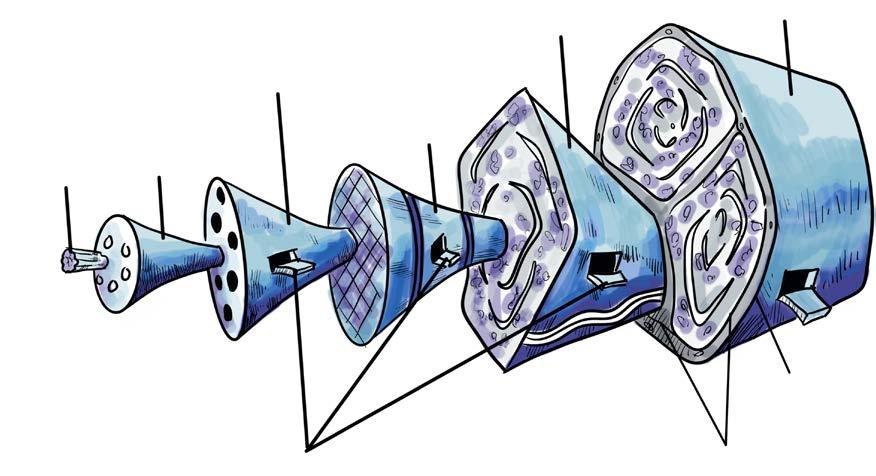
Tendons come in various shapes and sizes and connect muscle to bone. The normal tendon structure is largely composed of collagen and proteoglycans. Type I collagen comprises approximately 65% to 80% of the dry mass of the tendon, with smaller amounts of type II, III, IV, V, IX, and X collagen also present.22 Collagen molecules are
cross-linked polypeptide chains, and their principal role is to resist tension, while proteoglycans are primarily responsible for the viscoelastic behavior of the tendon.23 The tendon is organized in a helical architecture, comparable to man-made ropes.24 This helical organization of the tendon components is present at various levels or organizations, including when collagen fibers are bundled together to form fascicles, and fascicles are bundled to form the tendon itself.
The cellular component of the tendon is made up of tenoblasts and tenocytes arranged in parallel rows among the collagen fibers. Tenoblasts are immature tendon cells and transform into tenocytes as they mature. Tenocytes function to synthesize collagen and other components of the extracellular matrix (ECM). Tenoblasts and tenocytes comprise 90% of the cellular component of the tendon, with the remaining 5% to 10% made up of chondrocytes, synovial cells, and vascular cells.22,25
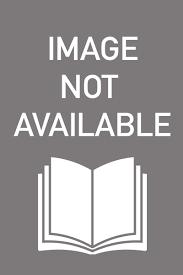
A thin film of loose connective tissue (endotenon) is present between the fascicles, allowing the fascicles to slide independently against each other. The endotenon is continuous with the connective tissue (epitenon) that surrounds the tendon as a whole (Fig. 1.1). Some tendons, such as the Achilles tendon, have a paratenon that surrounds the tendon but separate from the tendon itself.23 The paratenon is made up of type I and III collagen fibers, and the inner surface is lined by synovial cells. In some cases, the tendon is surrounded by a true synovial sheath. There is often great confusion when describing the tissue that surrounds the tendon.
The tendon inserts on bone in the form of a myo-enthesis or cartilaginous entheses. Myo-enthesis have superior blood supply and are less prone to degenerative pathology. Intrinsic blood supply to the tendon is located at the myotendinous and osteotendinous junction, with extrinsic blood supply coming from the paratenon and synovial sheath. The musculotendinous junctions and entheses are vulnerable sites, and increased age and mechanical loading can decrease vascular supply to these areas. Small afferent nerves throughout the paratenon form plexuses with penetrating branches innervating the tendon.
Areas of the tendon with poor blood supply are at increased risk of injury. While tendon injuries can occur in the mid-tendon (i.e., Achilles), most pathology and pain arise at the enthesis. Poor blood supply predisposes damaged tendons to tissue hypoxia. Tendinopathy is thought to develop from excessive loading and tensile strain. Although load is a major component in the development pathology, the etiology of tendinopathy is likely multifactorial and includes genetics,26 age,27 body composition,28 comorbidities (e.g., dyslipidemias, rheumatoid disease, tumors, infections, heritable connective tissue diseases, endocrinopathies including thyroid disease, metabolic diseases including diabetes), and medication exposure (e.g., statin, fluoroquinolones).29
The interplay between structural change, dysfunction, and pain is still not fully understood. Historically, tendon pain has been described as tendinitis, implying that inflammation was the central pathologic process. At the cellular level in early and chronic tendinopathy, there are
an increased number of leukocytes (primarily macrophages and mast cells).30–32 However, compared to rheumatoid arthritis and other immune-driven pathology, the number of leukocytes is small,29 and there has been widespread recognition that the terminology of tendinitis, tendinosis, and paratenonitis should reflect the histopathologic feature of the tendon.33
Histopathologic studies have shown the progression from normal ECM to reactive response and tendon disrepair, characterized by greater tissue matrix breakdown, collagen separation, neovascularization, and proliferation of abnormal tenocytes. The new model of tendon pathology is of a continuum that has three stages: reactive tendinopathy, tendon disrepair (failed healing), and degenerative tendinopathy.34–36 While these are described as three distinct stages for convenience, the idea of a continuum recognizes that the tendon can move forward or back along this continuum. This model highlights the need to tailor treatments to the specific tendon pathology and that a single intervention is unlikely to be efficacious in every case.
Ligament Injury
Similar to tendon tissue, ligaments are constructed from dense regular connective tissue and can vary in size, form, orientation, and location.37 Skeletal ligaments stabilize the joint and guide the joint through a normal range of motion and provide proprioception to coordinate movements.37,38 The orientation of collagen fibrils tends to be in the direction of applied force, and while tendon collagen fibrils tend to be in parallel, the ligament collagen fibrils are not uniformly oriented as forces are applied in more than one direction.38 Type I collagen makes up 85% of the ligament, depending on the type of ligament, with the rest of the
ligament composed of type III, VI,V, XI, and XIV collagen.37 Collagen bundles within ligaments have a crimped appearance, and with stress, the ligament elongates as collagen fibers uncrimp. This allows the ligament to elongate without sustaining damage, contributing to the viscoelastic property of the ligament.37
In both tendons and ligaments, the major cell type is the fibroblast, or ligamentoblast and ligamentocytes.37 Epiligamentous plexus forms a net-like branching anastomotic pattern on the surface of the ligament with branches that penetrate the ligament and become intraligamentous vessels distributed into longitudinal channels within the ligament.39 The distribution of blood vessels varies among ligaments, and compared to the synovial tissue or bone, ligaments appear to be relatively hypovascular.39
Ligaments are most often injured in traumatic injuries and follow the three phases of healing (inflammation, proliferative, and remodeling).40 Although the ligament may heal, the scar tissue that forms has major differences in collagen types,41 failure of collagen crosslinking,42 altered cell connections,43 small collagen fibril diameter,44 and increased vascularity.45 Even after fully healing, the ligament matrix apparels grossly, histologically, and biomechanically different from normal ligament tissue.46 The remodeled ligament can contain material other than collagen, including blood vessels, adipose cells, and inflammatory cells, resulting in weakness.37,46,47 In studies of injured medial collateral ligaments (MCLs), the ligament typically remains weaker after healing and only regains 40% to 80% of the strength and stiffness compared to normal MCLs.46,48 The viscoelastic property of an injured ligament has a somewhat better recovery, returning to within 10% to 20% of normal.46
Ligaments have a poor regenerative capacity due to the low cell density and lack of blood flow, and after an injury,
Secondar y fiber bundle
Ter tiar y fiber bundle
Tendon
Paratenon
Epitenon
Endotenon
Primar y fiber bundle
Collagen fibril
Collagen fiber
• Fig. 1.1 Hierarchy of a Tendon.